- 1Family Renewal, Inc., Vancouver, WA, United States
- 2University of East London, London, United Kingdom
- 3Transformation Evoked, Reston, VA, United States
- 4University of Oxford, Oxford, United Kingdom
Introduction: The application of ketogenic dietary interventions to mental health treatments is increasingly acknowledged within medical and psychiatric fields, yet its exploration in clinical psychology remains limited. This article discusses the potential implications of ketogenic diets, traditionally utilized for neurological disorders, within broader mental health practices.
Methods: This article presents a perspective based on existing ketogenic diet research on historical use, biological mechanisms, and therapeutic benefits. It examines the potential application of these diets in mental health treatment and their relevance to clinical psychology research and practice.
Results: The review informs psychologists of the therapeutic benefits of ketogenic diets and introduces to the psychology literature the underlying biological mechanisms involved, such as modulation of neurotransmitters, reduction of inflammation, and stabilization of brain energy metabolism, demonstrating their potential relevance to biopsychosocial practice in clinical psychology.
Conclusion: By considering metabolic therapies, clinical psychologists can broaden their scope of biopsychosocial clinical psychology practice. This integration provides a care model that incorporates knowledge of the ketogenic diet as a treatment option in psychiatric care. The article emphasizes the need for further research and training for clinical psychologists to support the effective implementation of this metabolic psychiatry intervention.
1 Introduction
Most first-line treatments for psychiatric disorders consist of psychotherapy and pharmacology. Psychotherapy exhibits positive effects independently of pharmacological treatments (Cuijpers et al., 2023) but often individuals are prescribed a combination of treatments.
Although psychotropic medications have increased substantially in recent decades (Brauer et al., 2021), the global burden of mental illness is rising across diverse populations (GBD 2019 Mental Disorders Collaborators, 2022). Given the persistent rise in mental illness despite advancements in psychotherapy and pharmacology, there is a pressing need for innovative, low-risk, and practical interventions that enhance the efficacy of psychotherapy.
This article intends to inform psychologists about the use of ketogenic diets as a treatment for mental illness and provide a better understanding of how their use in psychiatry informs the biopsychosocial model of practice. It introduces ketogenic diets, detailing their historical use for neurological disorders, relevant underlying biological mechanisms, their potential application in mental health treatment, and the relevance of ketogenic diets to clinical psychology research and practice.
According to the research, fasting has been used as a treatment for epilepsy since the Hippocratic era (Barzegar et al., 2021; Ferraris et al., 2023). In 1911 the first research study on fasting in epilepsy was published (Guelpa, 1911). As fasting could not be maintained indefinitely, Wilder et al. created a fasting-mimicking diet, by increasing ketones and called it the ‘Classic’ ketogenic diet because of its ketone-producing effects (Wilder, 1921; Kim, 2017). This was a significant medical breakthrough at a time when few treatments for epilepsy existed. This fasting-mimicking ketogenic diet has been studied for over 100 years for the treatment of neurological disease, particularly treatment-resistant strains of epilepsy in children (Martin-McGill et al., 2020). In the literature, there are compelling reasons to suggest that a therapeutic ketogenic diet may be effective in treating other neurological and psychiatric disorders (Kraeuter et al., 2020). Some case series and small studies have shown early promise in this supposition, including major depressive disorder (MDD), schizophrenia (Sethi et al., 2024), and bipolar disorder (BPD) (Danan et al., 2022; Sethi and Ford, 2022).
So far, there has been limited integration of dietary interventions in the clinical setting, apart from the practice of dieticians and nutritionists, although there have been calls to do so (La Puma, 2016; Unwin et al., 2022). Given the prominent role played by clinical psychologists in mental health diagnosis and treatment, there is potential for them to incorporate into their practice the support of valid and effective dietary interventions adjunct to their therapies and treatments. Specialized training for clinical psychologists in supporting therapeutic ketogenic dietary interventions may empower the successful backing of such interventions, which could lead to improved mental health outcomes for individuals with mental illness.
In addition to ketogenic metabolic therapy, psychologists are also encouraged to expand their knowledge and professional application to include other metabolic interventions. These interventions, like ketogenic diet implementation, often involve multi-step, individualized processes that require adaptation to the unique needs and circumstances of each patient. A considerable number of patients seen by general practitioners suffer from stress-related conditions, anxiety, depression, sleep issues, somatoform disorders, addictions, and metabolic problems. Unfortunately, many of these individuals do not receive adequate psychiatric care, representing a critical public health issue. However, those who are hesitant to pursue psychiatric treatment may still benefit significantly from receiving medical and psychological support for metabolic interventions. Psychologists’ understanding and support of ketogenic diets as a treatment for mental illness could enhance patient care in primary settings by providing additional therapeutic options for those not receiving specialized psychiatric services.
The relevance of extending knowledge of ketogenic diets to clinical psychologists lies in their biopsychosocial model of practice. Clinical psychologists are trained to utilize this biological pillar of practice to inform their work with patients, and the research evidence regarding therapeutic ketogenic diets as a treatment for neurological disorders and mental illness has reached a point in which this must be considered for adoption into informed psychological practice.
A therapeutic ketogenic diet, also known as ketogenic therapy, is a specific dietary regimen with a distinctive macronutrient distribution featuring high fat, moderate protein, and low carbohydrate levels (Ferraris et al., 2023). Carbohydrates are a nonessential macronutrient in the body, as the liver can create its own glucose on demand, so there is no risk of carbohydrate deficiency (Bier et al., 1999). The diet’s main mechanism of action is switching from the body’s primary fuel source, glucose via carbohydrates, to fat. This way of eating has been shown to mimic the effects of fasting by achieving a natural and safe metabolic state called “ketosis” (Kim, 2017). Ketosis is a process that converts dietary fat or liberated fat stores into ketone bodies in the liver which then supplies energy to the body and brain. For this reason, the ketogenic diet is often discussed informally as a metabolic psychiatry intervention. By adjusting brain metabolism, the diet not only addresses symptoms but potentially alters the underlying metabolic disturbances associated with various mental health disorders (Sethi and Ford, 2022).
Often, concerns around the safety of the ketogenic diet and the potential for negative side effects have been raised (McDonald and Cervenka, 2018). Though the ketogenic diet is considered a safe treatment for pediatric epilepsy (Faheem et al., 2024), various adverse effects have been reported in the research literature (Patikorn et al., 2023). However, side effects are often preventable and treatable if the diet is implemented correctly (Wells et al., 2020).
2 Treatment effects and mechanisms of action
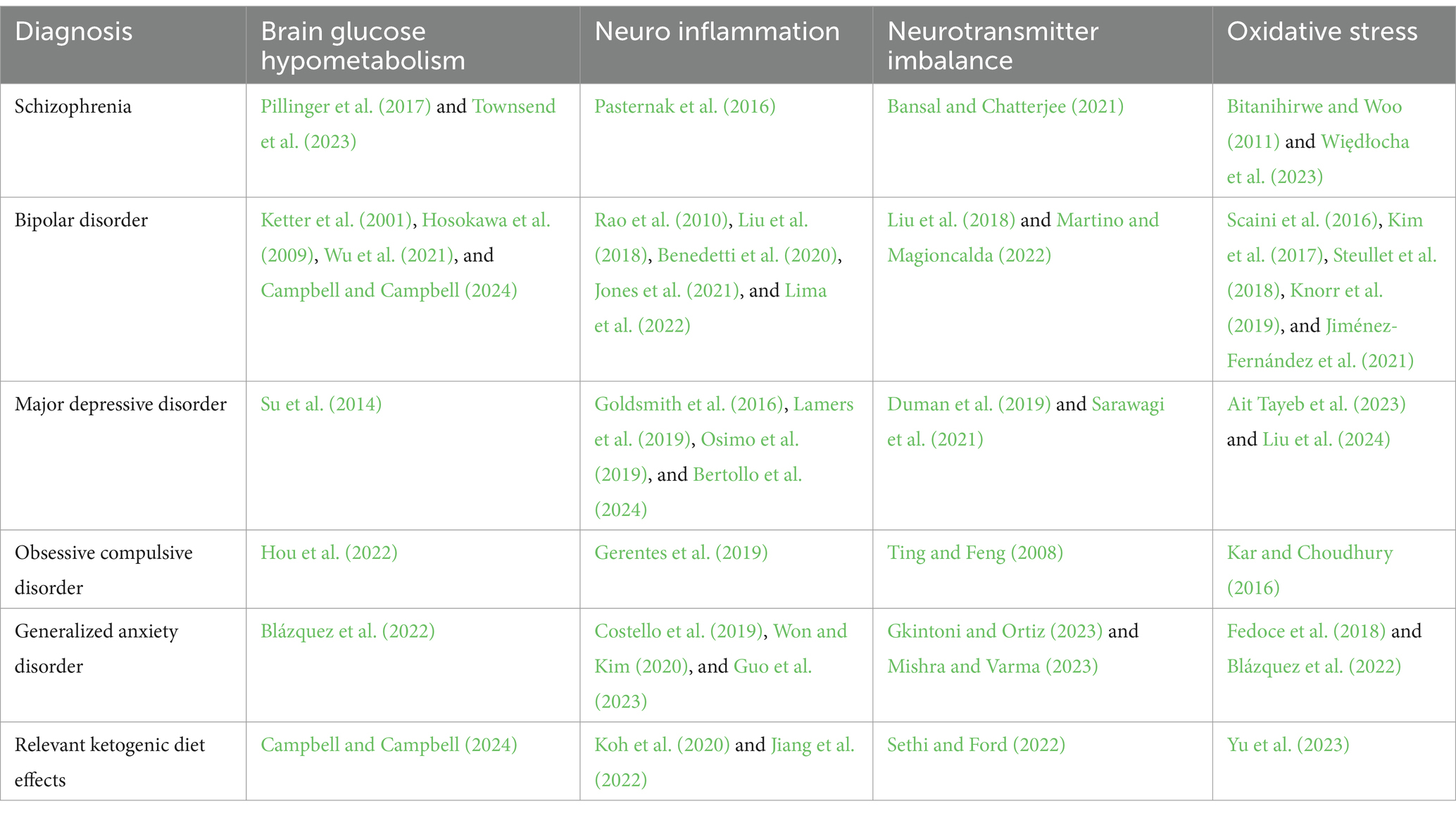
Many mechanisms have been proposed to ensure the efficacy of a ketogenic diet in neurological and psychiatric disorders. Several relevant pathological states, for example, cerebral glucose hypometabolism, insulin resistance, neurotransmitter imbalances, mitochondrial dysfunction, oxidative stress, and inflammation, may be improved by following a ketogenic diet. Table 1 provides an overview of literature published showing relevant states of pathology seen in certain mental illnesses that are modifiable by ketogenic diets. Ketogenic diets have been shown to improve mitochondrial energy metabolism, inflammatory processes, oxidative stress, monoaminergic activity, and neuro-degeneration (Norwitz et al., 2020).
A ketogenic diet may also improve cognitive function, in both working memory and speed of processing (Mohorko et al., 2019). Beyond comorbid metabolic disorders characterized by insulin resistance, MDD and BPD medications frequently negatively impact metabolism (Chokka et al., 2006; Gramaglia et al., 2018). The ketogenic diet has been shown to significantly improve metabolic syndrome and metabolism (Bhanpuri et al., 2018; Miller et al., 2018; Sethi et al., 2024). Therefore the ketogenic diet may serve to mitigate some negative side effects of medications and could offer additional benefits on pathology (Sethi et al., 2024).
Improvements from a ketogenic diet have also been observed in neurological illnesses such as traumatic brain injury (TBI) (Prins et al., 2005), autism spectrum disorder (ASD) (Evangeliou et al., 2003), Parkinson’s disease, and Alzheimer’s disease (Paoli et al., 2014), along with improved memory (Krikorian et al., 2012), increased cognitive performance (Xu et al., 2010) and protection against cognitive impairment (Davidson et al., 2013). The positive effects of the ketogenic diet for multiple sclerosis (Storoni and Plant, 2015) due to the diet’s immunomodulating effects have also been reported (Brenton et al., 2022). In one study, participants with Parkinson’s disease also found improvements in anxiety after 12 weeks of following a ketogenic diet with <16 g carbohydrates per day (Murphy et al., 2004).
While using the ketogenic diet to treat epilepsy, it was observed that attention and cognition improved, and the diet appeared to have mood stabilizing effects (Murphy et al., 2004; Brietzke et al., 2018; Campbell and Campbell, 2019; Norwitz et al., 2020). Closer investigations in some studies showed that the ketogenic diet exhibited potential mood stabilization effects through modifications in metabolite levels, such as regulation of neurotransmitters including GABA, glutamatergic neurotransmission, mitochondrial function, and oxidative stress in patients following the ketogenic diet (Kraeuter et al., 2020; Norwitz et al., 2020). Some studies have proposed that changes in brain energy metabolism and the increased utilization of ketones for energy influence the neurotransmitter levels (Norwitz et al., 2020; Myette-Côté et al., 2022).
Further, when ketones are present in the blood, a reduction in neuronal excitability and anticonvulsant effects have been observed (Masino and Rho, 2012; Sethi and Ford, 2022; Omori et al., 2023). The anticonvulsant drugs prescribed for epilepsy treatment (e.g., lithium) are also prescribed for mood stabilization in mood disorders such as bipolar disorder, suggesting that epilepsy and bipolar disorder share some aspects of their etiologies (Qaswal, 2020). A ketogenic diet elicits beneficial effects without needing to administer the anticonvulsant drug and, in some cases, can exceed the levels of mood stabilization achieved with medications (Phelps et al., 2013).
3 Ketogenic diet in the context of the biopsychosocial model
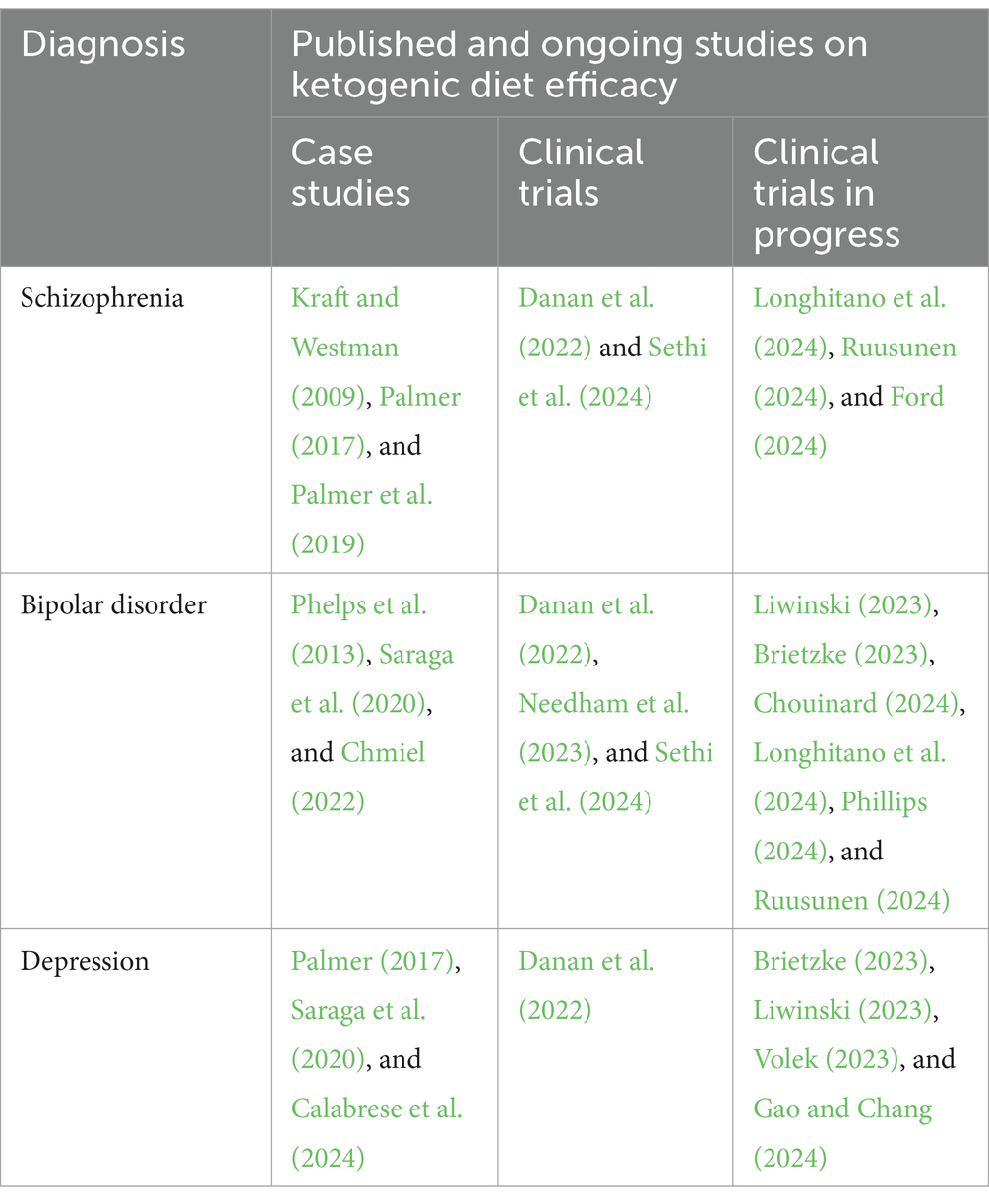
The role of brain metabolism in the etiology of mental illness has largely been an uncharted territory within the field of psychology, primarily addressed within psychiatric literature (Sarnyai and Palmer, 2020). This oversight has meant that psychologists, for the most part, may not be aware of the significance of metabolic factors in mental health conditions. The robust body of evidence emerging from psychiatric research, particularly concerning the effects of ketogenic diets as a metabolic therapy for mental illness, presents an opportunity for its integration into psychological practice, as summarized in Table 2, which outlines a sample of completed and ongoing research using ketogenic diets for psychiatric disorders.
This integration, as stated earlier, aligns with the biological pillar of the biopsychosocial model, enhancing the understanding of mental disorders from a metabolic perspective and offering a new dimension to psychological treatment approaches. Building on this enhanced metabolic understanding, psychologists are uniquely equipped to translate these biological insights into practical psychological interventions that support patient care.
The established research using a therapeutic ketogenic diet as a metabolic treatment for mental illness (Sethi and Ford, 2022; Mentzelou et al., 2023) has potential implications for clinical psychology. There is a growing interdisciplinary recognition of the interplay between metabolism and mental illness that challenges existing paradigms and necessitates a reevaluation of conventional treatment approaches in psychiatry (Omori et al., 2023). The field of clinical psychology benefits from this conversation, discussing the relevance of ketogenic diets as a treatment for mental illness, aligning with Sim’s broader advocacy for the inclusion of diverse, empirically supported treatments in clinical psychology, a principle that extends to innovative approaches like the ketogenic diet (Sim, 2006).
The adoption of ketogenic diet as a metabolic therapy in clinical psychology is grounded in scientific research and evidence. It represents a commitment to an evidence-based approach in the field, where interventions are chosen based on empirical support for their efficacy and safety. This approach does not challenge existing paradigms but offers an expanded understanding of the neuroendocrine and neurobiological mechanisms involved in mental disorders (Norwitz et al., 2020; Giel et al., 2022; Campbell and Campbell, 2023). Supplementary Table S1 provides an overview of potential competencies where psychological expertise may support the integration and implementation of ketogenic metabolic therapy in mental health practice. Psychologists, with their proficiency in supporting medical treatments like medication adherence using well-established psychosocial interventions (Depp et al., 2008), are well-equipped to extend support to metabolic therapies like the ketogenic diet.
Extending their role in medical treatment support, psychologists can be trained to incorporate support for the ketogenic diet as a metabolic therapy into their clinical practice. Their extensive training in psychological and social factors plays an important role in the effective implementation and integration of this therapy into the patients’ lives, providing essential support for patients engaging with the ketogenic diet as a therapeutic intervention. Support provided by psychologists may include psychoeducation, addressing misconceptions about the ketogenic diet, utilizing strategies to enhance adherence and collaboration with other healthcare professionals, and ensuring a comprehensive and multidisciplinary care plan for patients.
Psychological interventions can help patients use ketogenic diets as a metabolic therapy in their treatment of mental illness and are well-trained in providing behavioral and emotional support to individuals attempting to make changes in alignment with their mental health goals. Psychologists can use existing theoretical orientations and choose treatment targets to assist patients in the exploration and implementation of the ketogenic diet as a treatment option. Psychologists who provide support to patients attempting to use ketogenic diets already benefit from the long-standing use of models traditionally used to support medication compliance in patients working with prescribers. Their role as important members of multi-disciplinary teams is well-established (Bisbey et al., 2019; Proctor and Vu, 2019; Wood et al., 2019) and may benefit research and treatment teams that consist of medical professionals such as psychiatrists, dieticians, or nutritionists.
Psychologists’ deep understanding of social and cultural influences plays a pivotal role in guiding patients through the adoption of ketogenic diets, and their expertise enables them to facilitate patient exploration of how societal norms and individual dietary choices impact the successful integration of this therapy. This allows psychologists to implement an approach that is essential for a comprehensive understanding of mental health care, bridging individual behavioral changes with broader social and cultural contexts. Recognizing the intricate interplay between societal norms, individual dietary choices, and mental health care, psychologists are uniquely positioned to understand and navigate the diverse cultural and social factors that influence the adoption of ketogenic diets as a therapeutic intervention. Cultural traditions, personal beliefs, and existing social norms deeply affect individuals’ food choices, their relationship with food, and their sense of self. Food choices have deeply embedded cultural significance, playing roles in social gatherings, and can impact the adoption of ketogenic diets as a treatment modality for diverse populations. Psychologists have expertise in understanding these diverse influences and the ability to appreciate the complexity of making dietary choices within different cultural contexts, which can assist patients in being able to implement the therapy successfully while maintaining their relationships and cultural identity (Clauss-Ehlers et al., 2019).
Psychologists not only provide these potentially invaluable contributions in assisting patients using ketogenic diets as metabolic therapy for mental illness, but their contributions to the research literature in the form of quantitative and qualitative analysis can also help ensure improved treatment outcomes. This research is particularly important for tailoring the therapy to meet the unique needs of diverse populations, including those with dual diagnoses. Beyond patient support, psychologists’ insights are vital in research, potentially enhancing understanding of how cultural and social factors influence the effectiveness of ketogenic diets in mental health treatment and providing additional relevant data on treatment outcomes.
4 Conclusion
The inclusion of accurate knowledge of this intervention offers a promising complement to the existing array of evidence-based interventions in the biopsychosocial model of psychology practice, paving the way for advancements in mental health treatment. Such integration marks a meaningful broadening of clinical psychology’s scope that mirrors the profession’s commitment to stay abreast of and responsive to evolving scientific insights as part of competent psychological practice.
In their role as clinicians and researchers, psychologists are uniquely equipped to explore and support patient use of the ketogenic diet in mental health care. Their expertise in psychological assessment and intervention is critical for understanding and optimizing the use of this therapy in diverse patient populations. As the field continues to evolve, psychologists’ engagement with current research and clinical applications of the ketogenic diet as a therapeutic intervention will be instrumental in shaping effective, evidence-based mental health treatments.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
NL: Conceptualization, Writing – original draft, Writing – review & editing. EB: Writing – original draft, Writing – review & editing. DH: Writing – original draft, Writing – review & editing. AH: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
NL is employed by and owns Family Renewal, Inc. DBA Mental Health Keto and offers NBCC-certified training for psychotherapists on supporting individuals using ketogenic diets. ELB is employed by and owns Integrative Ketogenic Research and Therapies Ltd. DH is employed by and owns Transformation Evoked. AH is employed by and owns MetPsy.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1468894/full#supplementary-material
Supplementary Table S1 | Areas of psychological expertise relevant to ketogenic metabolic therapy or some variation?
Abbreviations
ASD, Autism spectrum disorder; BED, Binge eating disorder; BPD, Bipolar disorder; GABA, Gamma-aminobutyric acid; GAD, Generalized anxiety disorder; KD, Ketogenic diet; MDD, Major depressive disorder; NT, Neurotransmitter; OCD, Obsessive-compulsive disorder; TBI, Traumatic brain injury.
References
Ait Tayeb, A. E. K., Poinsignon, V., Chappell, K., Bouligand, J., Becquemont, L., and Verstuyft, C. (2023). Major depressive disorder and oxidative stress: a review of peripheral and genetic biomarkers according to clinical characteristics and disease stages. Antioxidants 12:942. doi: 10.3390/antiox12040942
Bansal, V., and Chatterjee, I. (2021). Role of neurotransmitters in schizophrenia: a comprehensive study. Kuwait J. Sci. 48:9264. doi: 10.48129/kjs.v48i2.9264
Barzegar, M., Afghan, M., Tarmahi, V., Behtari, M., Rahimi Khamaneh, S., and Raeisi, S. (2021). Ketogenic diet: overview, types, and possible anti-seizure mechanisms. Nutr. Neurosci. 24, 307–316. doi: 10.1080/1028415X.2019.1627769
Benedetti, F., Aggio, V., Pratesi, M. L., Greco, G., and Furlan, R. (2020). Neuroinflammation in Bipolar Depression. Front. Psych. 11:71. doi: 10.3389/fpsyt.2020.00071
Bertollo, A. G., Mingoti, M. E. D., and Ignácio, Z. M. (2024). Neurobiological mechanisms in the kynurenine pathway and major depressive disorder. Rev. Neurosci. doi: 10.1515/revneuro-2024-0065
Bhanpuri, N. H., Hallberg, S. J., Williams, P. T., McKenzie, A. L., Ballard, K. D., Campbell, W. W., et al. (2018). Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: an open label, non-randomized, controlled study. Cardiovasc. Diabetol. 17:56. doi: 10.1186/s12933-018-0698-8
Bier, D. M., Brosnan, J. T., Flatt, J. P., Hanson, R. W., Heird, W., Hellerstein, M. K., et al. (1999). Report of the IDECG working group on lower and upper limits of carbohydrate and fat intake. International dietary energy consultative group. Eur. J. Clin. Nutr. 53 Suppl 1, S177–S178. doi: 10.1038/sj.ejcn.1600759
Bisbey, T. M., Reyes, D. L., Traylor, A. M., and Salas, E. (2019). Teams of psychologists helping teams: the evolution of the science of team training. Am. Psychol. 74, 278–289. doi: 10.1037/amp0000419
Bitanihirwe, B. K. Y., and Woo, T.-U. W. (2011). Oxidative stress in schizophrenia: an integrated approach. Neurosci. Biobehav. Rev. 35, 878–893. doi: 10.1016/j.neubiorev.2010.10.008
Blázquez, E., Hurtado-Carneiro, V., LeBaut-Ayuso, Y., Velázquez, E., García-García, L., Gómez-Oliver, F., et al. (2022). Significance of brain glucose Hypometabolism, altered insulin signal transduction, and insulin resistance in several neurological diseases. Front. Endocrinol. 13:873301. doi: 10.3389/fendo.2022.873301
Brauer, R., Alfageh, B., Blais, J. E., Chan, E. W., Chui, C. S. L., Hayes, J. F., et al. (2021). Psychotropic medicine consumption in 65 countries and regions, 2008–19: a longitudinal study. Lancet Psychiatry 8, 1071–1082. doi: 10.1016/S2215-0366(21)00292-3
Brenton, J. N., Lehner-Gulotta, D., Woolbright, E., Banwell, B., Bergqvist, A. G. C., Chen, S., et al. (2022). Phase II study of ketogenic diets in relapsing multiple sclerosis: safety, tolerability and potential clinical benefits. J. Neurol. Neurosurg. Psychiatry 93, 637–644. doi: 10.1136/jnnp-2022-329074
Brietzke, D. E. M. (2023). Effects and mechanistic aspects of ketogenic diet in individuals with major depressive disorder: a pilot study. Available at: https://clinicaltrials.gov/study/NCT05558995 (Accessed December 31, 2023)
Brietzke, E., Mansur, R. B., Subramaniapillai, M., Balanzá-Martínez, V., Vinberg, M., González-Pinto, A., et al. (2018). Ketogenic diet as a metabolic therapy for mood disorders: evidence and developments. Neurosci. Biobehav. Rev. 94, 11–16. doi: 10.1016/j.neubiorev.2018.07.020
Calabrese, L., Frase, R., and Ghaloo, M. (2024). Complete remission of depression and anxiety using a ketogenic diet: case series. Front. Nutr. 11:1396685. doi: 10.3389/fnut.2024.1396685
Campbell, I. H., and Campbell, H. (2019). Ketosis and bipolar disorder: controlled analytic study of online reports. BJPsych Open 5:e58. doi: 10.1192/bjo.2019.49
Campbell, I., and Campbell, H. (2023). The metabolic overdrive hypothesis: Hyperglycolysis and Glutaminolysis in Bipolar Mania. Mol Psychiatry 29, 1521–1527. doi: 10.31234/osf.io/48dba
Campbell, I. H., and Campbell, H. (2024). The metabolic overdrive hypothesis: hyperglycolysis and glutaminolysis in bipolar mania. Mol. Psychiatry 29, 1521–1527. doi: 10.1038/s41380-024-02431-w
Chmiel, I. (2022). Ketogenic diet in therapy of bipolar affective disorder -- case report and literature review. Psychiatria Polska EBSCOhost 56:1. doi: 10.12740/PP/OnlineFirst/136356
Chokka, P., Tancer, M., and Yeragani, V. K. (2006). Metabolic syndrome: relevance to antidepressant treatment. J. Psychiatry Neurosci. 31:414
Chouinard, V.-A. (2024). A randomized controlled clinical trial of ketogenic and nutritional interventions for brain energy metabolism and psychiatric symptoms in first episode bipolar disorder. Available at: https://clinicaltrials.gov/study/NCT06221852 (Accessed December 31, 2023)
Clauss-Ehlers, C. S., Chiriboga, D. A., Hunter, S. J., Roysircar, G., and Tummala-Narra, P. (2019). APA multicultural guidelines executive summary: ecological approach to context, identity, and intersectionality. Am. Psychol. 74, 232–244. doi: 10.1037/amp0000382
Costello, H., Gould, R. L., Abrol, E., and Howard, R. (2019). Systematic review and meta-analysis of the association between peripheral inflammatory cytokines and generalised anxiety disorder. BMJ Open 9:e027925. doi: 10.1136/bmjopen-2018-027925
Cuijpers, P., Miguel, C., Harrer, M., Ciharova, M., and Karyotaki, E. (2023). Does the use of pharmacotherapy interact with the effects of psychotherapy? A meta-analytic review. Eur. Psychiatry J. Assoc. Eur. Psychiatr. 66:e63. doi: 10.1192/j.eurpsy.2023.2437
Danan, A., Westman, E. C., Saslow, L. R., and Ede, G. (2022). The ketogenic diet for refractory mental illness: a retrospective analysis of 31 inpatients. Front. Psych. 13:951376. doi: 10.3389/fpsyt.2022.951376
Davidson, T. L., Hargrave, S. L., Swithers, S. E., Sample, C. H., Fu, X., Kinzig, K. P., et al. (2013). Inter-relationships among diet, obesity and hippocampal-dependent cognitive function. Neuroscience 253, 110–122. doi: 10.1016/j.neuroscience.2013.08.044
Depp, C. A., Moore, D. J., Patterson, T. L., Lebowitz, B. D., and Jeste, D. V. (2008). Psychosocial interventions and medication adherence in bipolar disorder. Dialogues Clin. Neurosci. 10, 239–250. doi: 10.31887/DCNS.2008.10.2/cadepp
Duman, R. S., Sanacora, G., and Krystal, J. H. (2019). Altered connectivity in depression: GABA and glutamate neurotransmitter deficits and reversal by novel treatments. Neuron 102, 75–90. doi: 10.1016/j.neuron.2019.03.013
Evangeliou, A., Vlachonikolis, I., Mihailidou, H., Spilioti, M., Skarpalezou, A., Makaronas, N., et al. (2003). Application of a ketogenic diet in children with autistic behavior: pilot study. J. Child Neurol. 18, 113–118. doi: 10.1177/08830738030180020501
Faheem, Y., Jaiswal, A., Shergill, K., Boppana, K., Almansouri, N. E., Bakkannavar, S., et al. (2024). Keto clarity: a comprehensive systematic review exploring the efficacy, safety, and mechanisms of ketogenic diet in pediatric epilepsy. Cureus 16:e54863. doi: 10.7759/cureus.54863
Fedoce, A. D. G., Ferreira, F., Bota, R. G., Bonet-Costa, V., Sun, P. Y., and Davies, K. J. A. (2018). The role of oxidative stress in anxiety disorder: cause or consequence? Free Radic. Res. 52, 737–750. doi: 10.1080/10715762.2018.1475733
Ferraris, C., Guglielmetti, M., Neri, L., Allehdan, S., Mohsin Albasara, J., Fareed Alawadhi, H., et al. (2023). A review of ketogenic dietary therapies for epilepsy and neurological diseases: a proposal to implement an adapted model to include healthy Mediterranean products. Food Secur. 12:1743. doi: 10.3390/foods12091743
Ford, J. M. (2024). Study Details | Can Neural Network Instability in Schizophrenia be Improved With a Very Low Carbohydrate Ketogenic Diet? Available at: https://clinicaltrials.gov/study/NCT05268809?intr=Ketogenic%20Diet&aggFilters=status:rec&page=1&rank=3 (Accessed July 19, 2024)
Gao, M., and Chang, M. K. (2024). A randomised controlled trial evaluating the efficacy and mechanisms of a ketogenic diet as an adjunctive treatment for people with treatment-resistant depression. Available at: https://clinicaltrials.gov/study/NCT06091163 (Accessed December 31, 2023)
GBD 2019 Mental Disorders Collaborators (2022). Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry 9, 137–150. doi: 10.1016/S2215-0366(21)00395-3
Gerentes, M., Pelissolo, A., Rajagopal, K., Tamouza, R., and Hamdani, N. (2019). Obsessive-compulsive disorder: autoimmunity and Neuroinflammation. Curr. Psychiatry Rep. 21:78. doi: 10.1007/s11920-019-1062-8
Giel, K. E., Bulik, C. M., Fernandez-Aranda, F., Hay, P., Keski-Rahkonen, A., Schag, K., et al. (2022). Binge eating disorder. Nat. Rev. Dis. Primer 8, 16–19. doi: 10.1038/s41572-022-00344-y
Gkintoni, E., and Ortiz, P. S. (2023). Neuropsychology of generalized anxiety disorder in clinical setting: a systematic evaluation. Healthcare 11:2446. doi: 10.3390/healthcare11172446
Goldsmith, D. R., Rapaport, M. H., and Miller, B. J. (2016). A meta-analysis of blood cytokine network alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder and depression. Mol. Psychiatry 21, 1696–1709. doi: 10.1038/mp.2016.3
Gramaglia, C., Gambaro, E., Bartolomei, G., Camera, P., Chiarelli-Serra, M., Lorenzini, L., et al. (2018). Increased risk of metabolic syndrome in antidepressants users: a Mini review. Front. Psych. 9:621. doi: 10.3389/fpsyt.2018.00621
Guelpa (1911). La lutte contre l’epiepsie par la desintoxication et par la reeducation alimentaire. Rev Ther Med Chir :78.
Guo, B., Zhang, M., Hao, W., Wang, Y., Zhang, T., and Liu, C. (2023). Neuroinflammation mechanisms of neuromodulation therapies for anxiety and depression. Transl. Psychiatry 13, 5–12. doi: 10.1038/s41398-022-02297-y
Hosokawa, T., Momose, T., and Kasai, K. (2009). Brain glucose metabolism difference between bipolar and unipolar mood disorders in depressed and euthymic states. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 33, 243–250. doi: 10.1016/j.pnpbp.2008.11.014
Hou, X., Wang, H., Cheng, M., and Yue, J. (2022). A study of brain glucose metabolism in obsessive-compulsive disorder patients. Ann. Palliat. Med. 11, 3503–3512. doi: 10.21037/apm-22-1161
Jiang, Z., Yin, X., Wang, M., Chen, T., Wang, Y., Gao, Z., et al. (2022). Effects of ketogenic diet on Neuroinflammation in neurodegenerative diseases. Aging Dis. 13, 1146–1165. doi: 10.14336/AD.2021.1217
Jiménez-Fernández, S., Gurpegui, M., Garrote-Rojas, D., Gutiérrez-Rojas, L., Carretero, M. D., and Correll, C. U. (2021). Oxidative stress parameters and antioxidants in patients with bipolar disorder: results from a meta-analysis comparing patients, including stratification by polarity and euthymic status, with healthy controls. Bipolar Disord. 23, 117–129. doi: 10.1111/bdi.12980
Jones, G. H., Vecera, C. M., Pinjari, O. F., and Machado-Vieira, R. (2021). Inflammatory signaling mechanisms in bipolar disorder. J. Biomed. Sci. 28:45. doi: 10.1186/s12929-021-00742-6
Kar, S. K., and Choudhury, I. (2016). An empirical review on oxidative stress markers and their relevance in obsessive-compulsive disorder. Int. J. Nutr. Pharmacol. Neurol. Dis. 6:139. doi: 10.4103/2231-0738.191641
Ketter, T. A., Kimbrell, T. A., George, M. S., Dunn, R. T., Speer, A. M., Benson, B. E., et al. (2001). Effects of mood and subtype on cerebral glucose metabolism in treatment-resistant bipolar disorder. Biol. Psychiatry 49, 97–109. doi: 10.1016/s0006-3223(00)00975-6
Kim, J.-M. (2017). Ketogenic diet: old treatment, new beginning. Clin. Neurophysiol. Pract. 2, 161–162. doi: 10.1016/j.cnp.2017.07.001
Kim, Y., Santos, R., Gage, F. H., and Marchetto, M. C. (2017). Molecular mechanisms of bipolar disorder: Progress made and future challenges. Front. Cell. Neurosci. 11:30. doi: 10.3389/fncel.2017.00030
Knorr, U., Simonsen, A. H., Roos, P., Weimann, A., Henriksen, T., Christensen, E.-M., et al. (2019). Cerebrospinal fluid oxidative stress metabolites in patients with bipolar disorder and healthy controls: a longitudinal case-control study. Transl. Psychiatry 9, 325–310. doi: 10.1038/s41398-019-0664-6
Koh, S., Dupuis, N., and Auvin, S. (2020). Ketogenic diet and Neuroinflammation. Epilepsy Res. 167:106454. doi: 10.1016/j.eplepsyres.2020.106454
Kraeuter, A.-K., Phillips, R., and Sarnyai, Z. (2020). Ketogenic therapy in neurodegenerative and psychiatric disorders: from mice to men. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 101:109913. doi: 10.1016/j.pnpbp.2020.109913
Kraft, B. D., and Westman, E. C. (2009). Schizophrenia, gluten, and low-carbohydrate, ketogenic diets: a case report and review of the literature. Nutr. Metab. 6:10. doi: 10.1186/1743-7075-6-10
Krikorian, R., Shidler, M. D., Dangelo, K., Couch, S. C., Benoit, S. C., and Clegg, D. J. (2012). Dietary ketosis enhances memory in mild cognitive impairment. Neurobiol. Aging 33, 425.e19–425.e27. doi: 10.1016/j.neurobiolaging.2010.10.006
La Puma, J. (2016). What is culinary medicine and what does it do? Popul. Health Manag. 19, 1–3. doi: 10.1089/pop.2015.0003
Lamers, F., Milaneschi, Y., Smit, J. H., Schoevers, R. A., Wittenberg, G., and Penninx, B. W. J. H. (2019). Longitudinal association between depression and inflammatory markers: results from the Netherlands study of depression and anxiety. Biol. Psychiatry 85, 829–837. doi: 10.1016/j.biopsych.2018.12.020
Lima, D. D., Cyrino, L. A. R., Ferreira, G. K., Magro, D. D. D., Calegari, C. R., Cabral, H., et al. (2022). Neuroinflammation and neuroprogression produced by oxidative stress in euthymic bipolar patients with different onset disease times. Sci. Rep. 12:16742. doi: 10.1038/s41598-022-21170-y
Liu, Y., Zhang, B., Zhou, Y., Li, M., Gao, Y., Qin, W., et al. (2024). Plasma oxidative stress marker levels related to functional brain abnormalities in first-episode drug-naive major depressive disorder. Psychiatry Res. 333:115742. doi: 10.1016/j.psychres.2024.115742
Liu, Y., Zhao, J., and Guo, W. (2018). Emotional roles of mono-Aminergic neurotransmitters in major depressive disorder and anxiety disorders. Front. Psychol. 9:2201. doi: 10.3389/fpsyg.2018.02201
Liwinski, T. (2023). KETO-MOOD: Ketogenic Diet for Microbiome Optimization and Overcoming Depression. Available online at: https://clinicaltrials.gov/study/NCT06105762 (Accessed July 19, 2024)
Longhitano, C., Finlay, S., Peachey, I., Swift, J.-L., Fayet-Moore, F., Bartle, T., et al. (2024). The effects of ketogenic metabolic therapy on mental health and metabolic outcomes in schizophrenia and bipolar disorder: a randomized controlled clinical trial protocol. Front. Nutr. 11:1444483. doi: 10.3389/fnut.2024.1444483
Martin-McGill, K. J., Bresnahan, R., Levy, R. G., and Cooper, P. N. (2020). Ketogenic diets for drug-resistant epilepsy. Cochrane Database Syst. Rev. 2020:CD001903. doi: 10.1002/14651858.CD001903.pub5
Martino, M., and Magioncalda, P. (2022). Tracing the psychopathology of bipolar disorder to the functional architecture of intrinsic brain activity and its neurotransmitter modulation: a three-dimensional model. Mol. Psychiatry 27, 793–802. doi: 10.1038/s41380-020-00982-2
Masino, S. A., and Rho, J. M. (2012). “Mechanisms of ketogenic diet action” in Jasper’s basic mechanisms of the epilepsies. eds. J. L. Noebels, M. Avoli, M. A. Rogawski, R. W. Olsen, and A. V. Delgado-Escueta (Bethesda, MD: National Center for Biotechnology Information (US)).
McDonald, T. J. W., and Cervenka, M. C. (2018). Ketogenic diets for adult neurological disorders. Neurotherapeutics 15, 1018–1031. doi: 10.1007/s13311-018-0666-8
Mentzelou, M., Dakanalis, A., Vasios, G. K., Gialeli, M., Papadopoulou, S. K., and Giaginis, C. (2023). The relationship of ketogenic diet with neurodegenerative and psychiatric diseases: a scoping review from basic research to clinical practice. Nutrients 15:2270. doi: 10.3390/nu15102270
Miller, V. J., Villamena, F. A., and Volek, J. S. (2018). Nutritional ketosis and Mitohormesis: potential implications for mitochondrial function and human health. J. Nutr. Metab. 2018, 5157645–5157627. doi: 10.1155/2018/5157645
Mishra, A. K., and Varma, A. R. (2023). A comprehensive review of the generalized anxiety disorder. Cureus 15:e46115. doi: 10.7759/cureus.46115
Mohorko, N., Černelič-Bizjak, M., Poklar-Vatovec, T., Grom, G., Kenig, S., Petelin, A., et al. (2019). Weight loss, improved physical performance, cognitive function, eating behavior, and metabolic profile in a 12-week ketogenic diet in obese adults. Nutr. Res. N. Y. N 62, 64–77. doi: 10.1016/j.nutres.2018.11.007
Murphy, P., Likhodii, S., Nylen, K., and Burnham, W. M. (2004). The antidepressant properties of the ketogenic diet. Biol. Psychiatry 56, 981–983. doi: 10.1016/j.biopsych.2004.09.019
Myette-Côté, É., Soto-Mota, A., and Cunnane, S. C. (2022). Ketones: potential to achieve brain energy rescue and sustain cognitive health during ageing. Br. J. Nutr. 128, 407–423. doi: 10.1017/S0007114521003883
Needham, N., Campbell, I. H., Grossi, H., Kamenska, I., Rigby, B. P., Simpson, S. A., et al. (2023). Pilot study of a ketogenic diet in bipolar disorder. BJPsych Open 9:e176. doi: 10.1192/bjo.2023.568
Norwitz, N. G., Sethi, S., and Palmer, C. M. (2020). Ketogenic diet as a metabolic treatment for mental illness. Curr. Opin. Endocrinol. Diabetes Obes. 27, 269–274. doi: 10.1097/MED.0000000000000564
Omori, N. E., Malys, M. K., Woo, G., and Mansor, L. (2023). Exploring the role of ketone bodies in the diagnosis and treatment of psychiatric disorders. Front. Psych. 14:1142682. doi: 10.3389/fpsyt.2023.1142682
Osimo, E. F., Baxter, L. J., Lewis, G., Jones, P. B., and Khandaker, G. M. (2019). Prevalence of low-grade inflammation in depression: a systematic review and meta-analysis of CRP levels. Psychol. Med. 49, 1958–1970. doi: 10.1017/S0033291719001454
Palmer, C. M. (2017). Ketogenic diet in the treatment of schizoaffective disorder: two case studies. Schizophr. Res. 189, 208–209. doi: 10.1016/j.schres.2017.01.053
Palmer, C. M., Gilbert-Jaramillo, J., and Westman, E. C. (2019). The ketogenic diet and remission of psychotic symptoms in schizophrenia: two case studies. Schizophr. Res. 208, 439–440. doi: 10.1016/j.schres.2019.03.019
Paoli, A., Bianco, A., Damiani, E., Bosco, G., Paoli, A., Bianco, A., et al. (2014). Ketogenic diet in neuromuscular and neurodegenerative diseases. Biomed. Res. Int. 2014, 1–10. doi: 10.1155/2014/474296
Pasternak, O., Kubicki, M., and Shenton, M. E. (2016). In vivo imaging of neuroinflammation in schizophrenia. Schizophr. Res. 173, 200–212. doi: 10.1016/j.schres.2015.05.034
Patikorn, C., Saidoung, P., Pham, T., Phisalprapa, P., Lee, Y. Y., Varady, K. A., et al. (2023). Effects of ketogenic diet on health outcomes: an umbrella review of meta-analyses of randomized clinical trials. BMC Med. 21:196. doi: 10.1186/s12916-023-02874-y
Phelps, J. R., Siemers, S. V., and El-Mallakh, R. S. (2013). The ketogenic diet for type II bipolar disorder. Neurocase 19, 423–426. doi: 10.1080/13554794.2012.690421
Phillips, M. (2024). Elucidating Neurobiological Mechanisms Underlying the Therapeutic Effect of the Ketogenic Diet in Bipolar Disorder (BD): a Multidisciplinary Mechanistic Study. Available online at: https://clinicaltrials.gov/study/NCT06081426 (Accessed December 31, 2023)
Pillinger, T., Beck, K., Gobjila, C., Donocik, J. G., Jauhar, S., and Howes, O. D. (2017). Impaired glucose homeostasis in first-episode schizophrenia: a systematic review and meta-analysis. JAMA Psychiatry 74, 261–269. doi: 10.1001/jamapsychiatry.2016.3803
Prins, M., Fujima, L. S., and Hovda, D. A. (2005). Age-dependent reduction of cortical contusion volume by ketones after traumatic brain injury. J. Neurosci. Res. 82, 413–420. doi: 10.1002/jnr.20633
Proctor, R. W., and Vu, K.-P. L. (2019). How psychologists help solve real-world problems in multidisciplinary research teams: introduction to the special issue. Am. Psychol. 74, 271–277. doi: 10.1037/amp0000458
Qaswal, A. B. (2020). Lithium stabilizes the mood of bipolar patients by depolarizing the neuronal membrane via quantum tunneling through the sodium channels. Clin. Psychopharmacol. Neurosci. 18, 214–218. doi: 10.9758/cpn.2020.18.2.214
Rao, J. S., Harry, G. J., Rapoport, S. I., and Kim, H. W. (2010). Increased excitotoxicity and neuroinflammatory markers in postmortem frontal cortex from bipolar disorder patients. Mol. Psychiatry 15, 384–392. doi: 10.1038/mp.2009.47
Ruusunen, A. , (2024). Dietary intervention for psychotic disorders: a pilot intervention study of ketogenic diet for psychotic symptoms-PsyDiet pilot study. Available at: https://clinicaltrials.gov/study/NCT03873922 (Accessed December 31, 2023)
Saraga, M., Misson, N., and Cattani, E. (2020). Ketogenic diet in bipolar disorder. Bipolar Disord. 22:765. doi: 10.1111/bdi.13013
Sarawagi, A., Soni, N. D., and Patel, A. B. (2021). Glutamate and GABA homeostasis and Neurometabolism in major depressive disorder. Front. Psych. 12:637863. doi: 10.3389/fpsyt.2021.637863
Sarnyai, Z., and Palmer, C. M. (2020). Ketogenic therapy in serious mental illness: emerging evidence. Int. J. Neuropsychopharmacol. 23, 434–439. doi: 10.1093/ijnp/pyaa036
Scaini, G., Rezin, G. T., Carvalho, A. F., Streck, E. L., Berk, M., and Quevedo, J. (2016). Mitochondrial dysfunction in bipolar disorder: evidence, pathophysiology and translational implications. Neurosci. Biobehav. Rev. 68, 694–713. doi: 10.1016/j.neubiorev.2016.06.040
Sethi, S., and Ford, J. M. (2022). The role of ketogenic metabolic therapy on the brain in serious mental illness: a review. J. Psychiatry Brain Sci. 7:9. doi: 10.20900/jpbs.20220009
Sethi, S., Wakeham, D., Ketter, T., Hooshmand, F., Bjornstad, J., Richards, B., et al. (2024). Ketogenic diet intervention on metabolic and psychiatric health in bipolar and schizophrenia: a pilot trial. Psychiatry Res. 335:115866. doi: 10.1016/j.psychres.2024.115866
Sim, L. (2006). Severe mental illness needs empirically supported assessment and treatments. Clin. Psychol. Sci. Pract. 13, 384–387. doi: 10.1111/j.1468-2850.2006.00052.x
Steullet, P., Cabungcal, J.-H., Bukhari, S. A., Ardelt, M. I., Pantazopoulos, H., Hamati, F., et al. (2018). The thalamic reticular nucleus in schizophrenia and bipolar disorder: role of parvalbumin-expressing neuron networks and oxidative stress. Mol. Psychiatry 23, 2057–2065. doi: 10.1038/mp.2017.230
Storoni, M., and Plant, G. T. (2015). The therapeutic potential of the ketogenic diet in treating progressive multiple sclerosis. Mult. Scler. Int. 2015:e681289, 1–9. doi: 10.1155/2015/681289
Su, L., Cai, Y., Xu, Y., Dutt, A., Shi, S., and Bramon, E. (2014). Cerebral metabolism in major depressive disorder: a voxel-based meta-analysis of positron emission tomography studies. BMC Psychiatry 14:321. doi: 10.1186/s12888-014-0321-9
Ting, J. T., and Feng, G. (2008). Glutamatergic synaptic dysfunction and obsessive-compulsive disorder. Curr. Chem. Genomics 2, 62–75. doi: 10.2174/1875397300802010062
Townsend, L., Pillinger, T., Selvaggi, P., Veronese, M., Turkheimer, F., and Howes, O. (2023). Brain glucose metabolism in schizophrenia: a systematic review and meta-analysis of 18FDG-PET studies in schizophrenia. Psychol. Med. 53, 4880–4897. doi: 10.1017/S003329172200174X
Unwin, J., Delon, C., Giæver, H., Kennedy, C., Painschab, M., Sandin, F., et al. (2022). Low carbohydrate and psychoeducational programs show promise for the treatment of ultra-processed food addiction. Front. Psych. 13:1005523. doi: 10.3389/fpsyt.2022.1005523
Volek, J. (2023). Study Details | Ketogenic Intervention in Depression. Available online at: https://www.clinicaltrials.gov/study/NCT06080932?cond=depression&term=Ketogenic%20Diet&rank=2&limit=10 (Accessed July 19, 2024)
Wells, J., Swaminathan, A., Paseka, J., and Hanson, C. (2020). Efficacy and safety of a ketogenic diet in children and adolescents with refractory epilepsy-a review. Nutrients 12:1809. doi: 10.3390/nu12061809
Więdłocha, M., Zborowska, N., Marcinowicz, P., Dębowska, W., Dębowska, M., Zalewska, A., et al. (2023). Oxidative stress biomarkers among schizophrenia inpatients. Brain Sci. 13:490. doi: 10.3390/brainsci13030490
Wilder, R. M. (1921). The effects of ketonemia on the course of epilepsy. Mayo Clin. Proc. 2, 307–308.
Won, E., and Kim, Y.-K. (2020). Neuroinflammation-associated alterations of the brain as potential neural biomarkers in anxiety disorders. Int. J. Mol. Sci. 21:6546. doi: 10.3390/ijms21186546
Wood, L., Williams, C., Billings, J., and Johnson, S. (2019). The role of psychology in a multidisciplinary psychiatric inpatient setting: perspective from the multidisciplinary team. Psychol. Psychother. Theory Res. Pract. 92, 554–564. doi: 10.1111/papt.12199
Wu, C., Ren, C., Teng, Z., Li, S., Silva, F., Wu, H., et al. (2021). Cerebral glucose metabolism in bipolar disorder: a voxel-based meta-analysis of positron emission tomography studies. Brain Behav. 11:e02117. doi: 10.1002/brb3.2117
Xu, K., Sun, X., Eroku, B. O., Tsipis, C. P., Puchowicz, M. A., and LaManna, J. C. (2010). Diet-induced ketosis improves cognitive performance in aged rats. Adv Exp Med Biol 662, 71–75. doi: 10.1007/978-1-4419-1241-1_9
Keywords: psychology, clinical psychology, ketogenic diet, ketogenic metabolic therapy, metabolic psychiatry, bipolar disorder, schizophrenia, depression
Citation: Laurent N, Bellamy EL, Hristova D and Houston A (2024) Ketogenic diets in clinical psychology: examining the evidence and implications for practice. Front. Psychol. 15:1468894. doi: 10.3389/fpsyg.2024.1468894
Edited by:
Zoltan Sarnyai, James Cook University, AustraliaReviewed by:
Jaymee-Leigh Swift, James Cook University, AustraliaIstván Szendi, University of Szeged, Hungary
Copyright © 2024 Laurent, Bellamy, Hristova and Houston. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erin L. Bellamy, ZS5sLmJlbGxhbXlAdWVsLmFjLnVr
 Nicole Laurent
Nicole Laurent Erin L. Bellamy
Erin L. Bellamy Donika Hristova
Donika Hristova Ally Houston4
Ally Houston4