- 1Postgraduate School, University of Harbin Sport, Harbin, China
- 2School of Sport Science and Health, University of Harbin Sport, Harbin, China
- 3Physical Education Department of Xiamen University, Xiamen, China
Background: A substantial amount of research has explored the intricate relationship between exercise and sleep quality, consistently confirming that exercise can effectively enhance sleep quality. Nevertheless, previous studies have yet to conclusively determine which specific exercise program is most efficacious in improving sleep quality. To address this gap, the present study systematically evaluated the differential effects of various types of exercise, as well as exercise dosages (including duration, intervention period, frequency, and intensity), on sleep outcomes using a network meta-analysis approach. This endeavor aims to provide evidence-based support for the development of scientifically effective exercise programs tailored to improve sleep quality.
Methods: Through the Web of Science, PubMed, Cochrane Library, Embase, and Scopus databases, we conducted a search for randomized controlled trials investigating the effects of exercise interventions on sleep, with a search cutoff date of April 30, 2024. We rigorously selected the literature according to the PICOS principle, and two independent researchers extracted the data. We would like to change this passage to: Bias risk assessment was conducted using the RevMan 5.4 software, and traditional meta-analysis and network meta-analysis were performed using Stata 17.0 software to generate forest plots, network evidence plots, and funnel plots. Furthermore, we adopted the surface under the cumulative ranking curve (SUCRA) to evaluate and rank the intervention effects of different exercise types and dosages on sleep quality. To verify the robustness of our study results, we performed a sensitivity analysis using the leave-one-out method.
Results: The study strictly adhered to the PRISMA guidelines and included 58 RCT papers with a total of 5,008 participants. The network meta-analysis revealed significant variations in the impact of exercise frequency on sleep outcomes when compared to the control group. Interventions of 1–2 times per week [SMD = −0.85, 95% CI (−1.43, −0.26)], 3 times per week [SMD = −0.45, 95% CI (−0.80, −0.11)], and 4 times per week [SMD = −1.09, 95% CI (−1.92, −0.26)] demonstrated the most notable effects. Interventions lasting ≤30 min and 60–65 min were significantly more effective than the control group, with ≤30 min proving significantly more effective than 40–55 min [SMD = 0.75, 95% CI (0.01, 1.49)]. Interventions lasting 9–10 weeks [SMD = −1.40, 95% CI (−2.37, −0.44)], 12–16 weeks [SMD = −0.55, 95% CI (−0.90, −0.20)], and ≥ 24 weeks [SMD = −0.71, 95% CI (−1.31, −0.10)] were all significantly more effective than the control group. Additionally, the 9–10 weeks intervention period was found to be significantly more effective than the 6–8 weeks period [SMD = −1.21, 95% CI (−2.37, −0.04)]. Furthermore, interventions of moderate intensity [SMD = −1.06, 95% CI (−1.52, −0.61)] and high intensity [SMD = −1.48, 95% CI (−2.55, −0.40)] exercise interventions yielded significantly greater benefits compared to the control group. Specifically, high intensity interventions [SMD = −1.97, 95% CI (−3.37, −0.56)] and moderate intensity [SMD = −1.55, 95% CI (−2.57, −0.54)] exercise interventions were found to be significantly more effective than moderate-high intensity interventions. In terms of exercise types, aerobic exercise [SMD = −0.56, 95% CI (−0.86, −0.27)], traditional Chinese exercises [SMD = −0.57, 95% CI (−0.97, −0.18)], and combined exercise [SMD = −0.99, 95% CI (−1.66, −0.32)] interventions all produced significant improvements compared to the control group. The study determined that the most effective combination of exercise prescription elements for enhancing sleep quality includes a frequency of 4 times per week (SUCRA = 84.7), a duration of ≤30 min (SUCRA = 92.2), a period of 9–10 weeks (SUCRA = 89.9), and high-intensity (SUCRA = 92.9) combined exercise (SUCRA = 82.7).
Conclusion: The current evidence indicates that combined exercise with a frequency of 4 times per week, a duration of ≤30 min, a period of 9–10 weeks, and high intensity is most effective for improving sleep quality. Nevertheless, due to the limited number of studies included, further research is needed to enhance the reliability of the findings.
Systematic review registration: https://www.crd.york.ac.uk/prospero/, identifier: CRD42024555428.
1 Introduction
The quality of sleep serves as a crucial physiological metric that evaluates an individual’s sleep status, incorporating subjective perception and objective sleep parameters (Ohayon et al., 2017). Adequate sleep is a fundamental component of a healthy lifestyle, as it can bolster memory consolidation, enhance attention and immune function (Moosavi-Movahedi et al., 2021), efficiently replenish expended energy from daily activities (Chandrasekaran, 2020), and promote overall well-being (Vandekerckhove and Wang, 2018). Furthermore, it plays a critical role in safeguarding cardiovascular health (Plante, 2006; Holfinger et al., 2021); regulating bodily processes, and sustaining optimal brain function (Plante, 2006; Pickersgill et al., 2022). Due to the crucial role of sleep in regulating and preserving human health, the quality of sleep has emerged as a key indicator for evaluating health status and overall quality of life (Dzierzewski et al., 2021). Presently, concerns regarding sleep quality have garnered widespread attention in society.
Sleep issues are present across all age groups, from adolescents to middle-aged and older adults. Relevant survey data show that among adolescents, about two-thirds are observed to have less than 6 h of sleep (Ohida et al., 2004; Paruthi et al., 2016). Furthermore, globally, over one-third of adults face varying degrees of sleep disturbances (Panel et al., 2015; Liu, 2016; Galinsky et al., 2018). Among the elderly population, the problem is even more pronounced, with up to 50% of older adults experiencing difficulty falling asleep or maintaining sleep (Paruthi et al., 2016; Schroeck et al., 2016). Epidemiological studies consistently indicate that sleep problems tend to intensify with increasing age (Almondes et al., 2021), a decline in sleep quality not only hampers individual learning capabilities but also compromises immune function (Dzierzewski et al., 2021). In addition, poor sleep quality is not only associated with a heightened susceptibility to chronic illnesses and an elevated likelihood of suicidal behaviors (Mikula et al., 2020; Bjorvatn et al., 2021), but also places a substantial financial strain on both families and society. For instance, in Canada, sleep-related issues lead to an estimated loss of $484 million (Streatfeild et al., 2021), while in Australia, the economic impact of sleep disorders is calculated at $35.4 billion (Chaput et al., 2022). This underscores the importance of addressing sleep quality as a critical public health concern that requires collective action on a global scale.
Pharmacological treatment, as a conventional means of improving sleep, although effective, is associated with potential dependency, a higher risk of drug-related mortality (especially in cases of overdose) (Bushnell et al., 2022), and uncertainty in therapeutic outcomes (Sys et al., 2020). These factors have driven the search for safer and more efficient non-pharmacological alternatives (Morrison et al., 2022). Non-pharmacological interventions, particularly exercise interventions, are gradually becoming the preferred choice for improving sleep quality due to their low risk and significant effects (Rios et al., 2019). Physical activity, sport, and exercise are terms often used interchangeably in research (Chennaoui et al., 2015). Physical activity refers to any form of body movement that results in energy expenditure, encompassing all activities of daily life, whether professional, household, or recreational (Bull et al., 2020). Sport typically refers to competitive physical activities. Exercise is a component of physical activity; it is planned, structured, and characterized by its frequency, intensity, and duration (Chennaoui et al., 2015). It includes aerobic exercises, resistance training, jogging, dancing, Tai Chi, Baduanjin, etc., with specific types of exercise depending on an individual’s physical capacity (Hasan et al., 2022). Research has shown that sustained engagement in exercise has a notable positive impact on sleep quality. For instance, a 12-week moderate-intensity exercise program implemented by Tseng et al. demonstrated significant improvements in sleep quality. Furthermore, the study demonstrated a notable impact on enhancing sleep quality among elderly individuals (Tseng et al., 2020). Additionally, Siu’s investigation revealed that both Tai Chi and traditional sports activities were effective in improving sleep quality, with lasting effects for up to 24 months (Siu et al., 2021). Although meta-analyses have assessed the therapeutic effects of exercise on sleep quality and generally recognized the positive impact of exercise in improving sleep quality (Banno et al., 2018), there are still certain limitations in existing studies. Firstly, previous research has focused on the immediate effects of exercise on short-term sleep (such as the following day), and there is a lack of in-depth research on the impact of long-term exercise programs on sleep quality (Stutz et al., 2019). Secondly, studies have mostly concentrated on the assessment of a single or a few exercise doses (such as exercise type, duration of intervention), lacking a comprehensive evaluation of the integrated effects of exercise types and dosages. For example, Xie et al. only analyzed the impacts of exercise type and intervention duration on sleep quality (Xie et al., 2021), which limits our comprehensive understanding of the effects of exercise types and dosages. Furthermore, due to the methodological limitations of traditional meta-analyses, while they can confirm the positive impact of exercise on sleep quality (Banno et al., 2018), there is still a lack of evidence to prove which types of exercise and dosages are most effective in enhancing sleep quality. There is a need for systematic reviews and meta-analyses of randomized controlled trials (RCTs) in this field (Kreutz et al., 2019).
Network meta-analysis, implemented within the Bayesian framework with the aid of Markov Chain Monte Carlo simulation technology (Moher et al., 2015; Vats et al., 2019), is an advanced statistical method that can assess and compare the efficacy differences among multiple interventions (Lei et al., 2022). One of the advantages of network meta-analysis is its ability to integrate direct and indirect comparative evidence from randomized controlled trials into a network evidence map, allowing not only direct but also indirect evaluations of intervention effects (Tonin et al., 2017). Furthermore, it can compare and rank the effects of different interventions to identify the optimal intervention (Kodama et al., 2021). Compared to traditional meta-analysis, network meta-analysis demonstrates significant advantages in assessing precision (Cipriani et al., 2013). To our knowledge, no study has yet explicitly identified which combination of exercise type and dosage can most effectively improve sleep quality. Therefore, this study utilizes the network meta-analysis method, combined with data from randomized controlled trials, to analyze the differences in the effects of exercise on improving sleep quality from the perspective of exercise type and dosage, thus providing evidence-based support for the development of scientific and effective exercise programs.
2 Materials and methods
This study, adhering to the PRISMA guidelines for reporting systematic reviews and meta-analyses (Hutton et al., 2015), has been registered on the international platform PROSPERO with the registration number CRD42024555428.
2.1 Literature search
A thorough review of the literature was carried out by searching five databases, including Web of Science, PubMed, Embase, Cochrane Library, and Scopus, with a search timeframe up to April 30, 2024. Three sets of keywords were utilized to enhance the comprehensiveness of the search: ①exercise, physical activity, sport, tai chi, aerobic exercise, walking, pilates, yoga, qi gong, resistance exercise, combined exercise; ② insomnia, sleep disorder, sleep complaint, sleep disturbance, sleep quality, sleep problem; ③ intervention, Randomized Controlled Trial (RCT), experiment, trial. Boolean logical operators were used to connect the keywords. In addition to this, the reference lists of the retrieved articles were reviewed to identify potentially relevant studies. Additionally, a literature trace was performed by examining the included studies and their reference lists from published systematic reviews and meta-analyses to ensure the thoroughness of the search.
Taking the Web of Science as an example, the search strategy is as shown in the Table 1.
2.2 Inclusion and exclusion criteria
The study strictly formulated the inclusion and exclusion criteria for the selection of literature, adhering to the PICOS principle (Li et al., 2014).
The inclusion criteria for literature consist of the following:
1. Population: There are no age restrictions for the participants included in the study. Additionally, there are no limitations regarding gender or ethnicity.
2. Intervention: The experimental group engaged in long-term exercise, encompassing various types such as aerobic exercise, Traditional Chinese exercises, resistance training, and combined exercise. Moreover, this study imposes no mandatory guidelines regarding the duration of exercise intervention, the intensity of exercise, the exercise environment, nor are there any limitations on the exercise intervention protocol or the approach to blinding.
3. Comparisons: The control group refrains from engaging in any type of exercise intervention and instead continues with their regular daily routines, receiving health education, or undergoing standard care.
4. Outcome: The Pittsburgh Sleep Quality Index (PSQI), a standardized questionnaire comprising 19 items divided into 7 component dimensions, is employed as the metric for measuring sleep quality. It evaluates sleep patterns over the past month, differentiating between individuals with good and poor sleep quality (Bertolazi et al., 2011). Recognized internationally as a reliable sleep quality assessment tool, the PSQI exhibits good internal consistency and test–retest reliability (Hita-Contreras et al., 2014), and has been proven useful in examining sleep quality (Aloba et al., 2007; Mollayeva et al., 2016). Widely applicable and effective (Alsaadi et al., 2013), its validity is widely acknowledged, ensuring high reliability in research and clinical practice (Manzar et al., 2015).
5. Study design: The study includes only Randomized Controlled Trials (RCTs), which ensures the highest level of evidence and minimizes bias (Hannan, 2008), providing a strong guarantee for the reliability of the research results (Lu et al., 2024).
Exclusion criteria were: ① The study methodology excluded non-randomized controlled trials, case reports, animal experimental studies, etc., by categorizing studies based on their type; ② Additionally, literature was classified by type, excluding systematic review articles, qualitative studies, and duplicate publications; ③ Data quality was assessed by excluding literature with unclear measurement indicators or incomplete data, such as studies that do not report PQSI data, or studies that report PSQI data either before or after the intervention.
2.3 Data extraction
The study was conducted independently by two researchers, who screened and processed the literature according to predefined criteria, followed by cross-checking. In cases of discrepancies, a third researcher facilitated discussion to reach a consensus before proceeding with data extraction. The extracted data encompassed various key elements, such as the primary author, publication date, country of origin, sample size, age distribution of both experimental and control groups, type of intervention, intervention duration, frequency, exercise duration, intensity, as well as mean, standard deviation, and sample size for sleep quality measurements in both groups.
2.4 Basic information extraction
The following is a basic introduction to the data extraction process of this study (for detailed content, see Table 2), all extracted from various studies: participant characteristics (age), exercise characteristics (type of exercise, duration, intervention frequency, period, intensity), and year of publication.
2.5 Statistical analysis
Bias risk assessment was conducted using Revman 5.4 software, and network meta-analysis was performed using STATA 17.0 software. Considering the outcome measures as continuous numerical values with significant variations in the measurements across different studies, the Standardized Mean Difference (SMD) was selected, combined with the 95% confidence interval (CI) as the effect size for the synthesis of effect sizes (Chandler et al., 2019). This method effectively pools data from studies of varying sizes (Lu et al., 2024), enhancing the reliability of the conclusions. If the 95% CI of a continuous variable does not include 0, it is considered statistically significant.
When performing network meta-analysis, a network evidence plot should first be drawn to visually display the relationships between direct and indirect comparisons of various exercise interventions. In cases where closed loop structures exist, to ensure the robustness of the results, an inconsistency test is required. If p > 0.05, it indicates good consistency between direct and indirect comparisons, meaning the inconsistency test is successful (Salanti et al., 2011). Conversely, if p < 0.05, it suggests the presence of inconsistency. Furthermore, when closed loops are present, we also assess the consistency between direct and indirect evidence by calculating the Inconsistency Factors (IF). If the 95% CI of the IF includes 0, it indicates good consistency between direct and indirect evidence, which enhances the reliability of the results.
To more comprehensively assess the robustness of the results, this study employs a leave-one-out method for sensitivity analysis to further verify the reliability of the results. By comparing the surface under the cumulative ranking (SUCRA), the best intervention measures for sleep quality are determined, with a higher SUCRA value indicating a better intervention effect (Daly et al., 2019).
3 Results
3.1 Literature screening results
The literature screening process was strictly conducted in accordance with the PRISMA flow diagram (Page et al., 2021). A total of 4,181 articles were initially identified through the search process. Following multiple rounds of screening, 58 randomized controlled trials involving 5,008 participants were ultimately included in the analysis. The screening process is illustrated in Figure 1.
3.2 Basic characteristics of included studies
Among the 58 studies analyzed, the sample sizes varied from 16 to 393 participants, with ages ranging from 13 to 85 years old. The studies included various types of exercise such as aerobic exercise, traditional Chinese exercises, resistance exercise, and Combined exercise. The intervention periods were conducted at ≤4 weeks, 6–8 weeks, 9–10 weeks, 12–16 weeks, and ≥ 24 weeks, with intervention frequencies of 1–2 times, 3 times, 4 times, 5 times, and ≥ 6 times. The intervention durations were ≤ 30 min, 40–55 min, 60–65 min, and ≥ 70 min. Interventions were conducted at low intensity, low-to-moderate intensity, moderate intensity, moderate-high intensity, and high intensity. All studies are randomized controlled trials (RCTs), and all employ a parallel group design. The basic characteristics of the included literature can be found in Table 3 (When an element represents a range, the average of that range is taken).
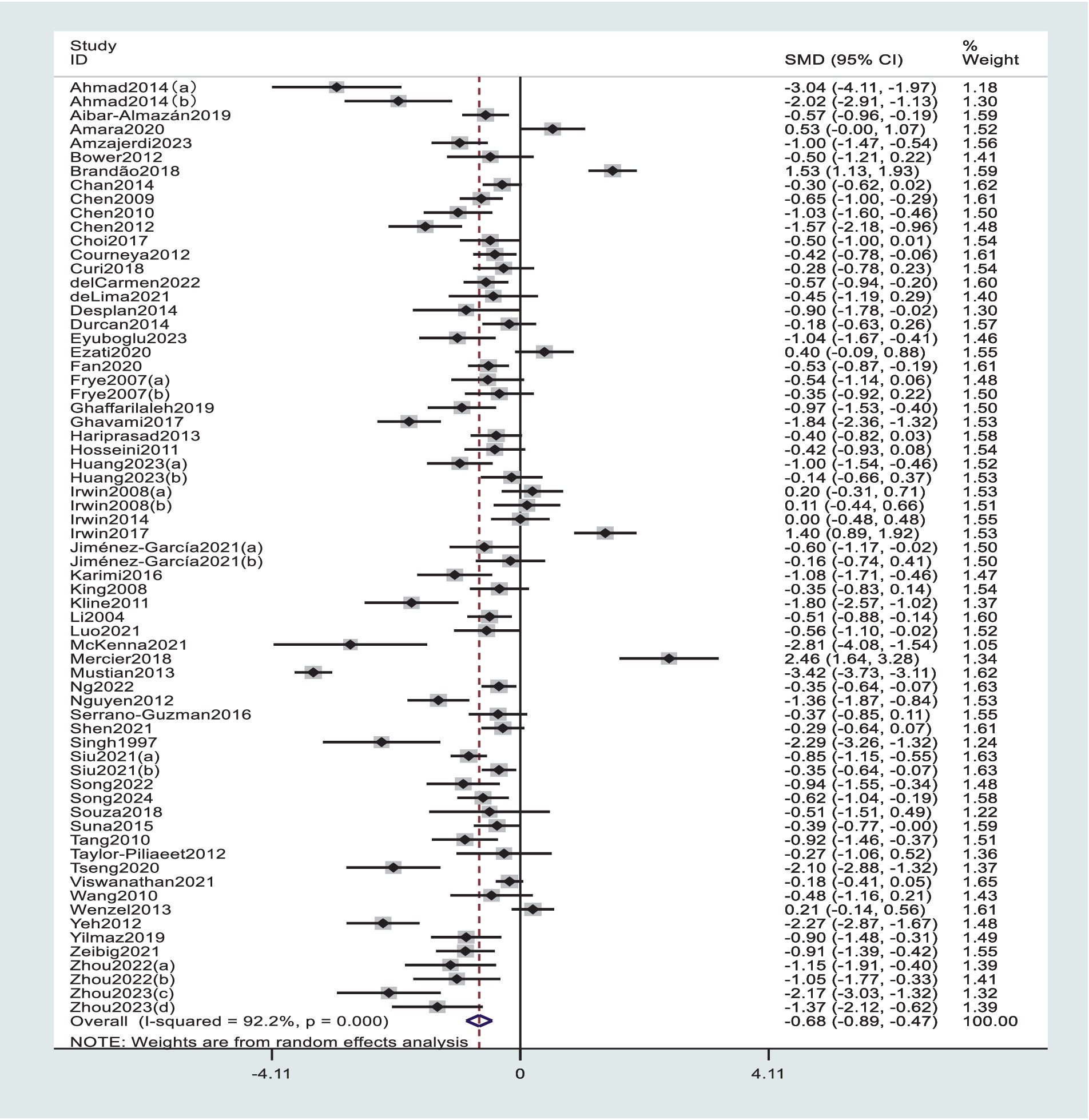
3.3 Traditional meta-analysis
Due to the presence of high heterogeneity, a random-effects model was used for the meta-analysis, and the results are depicted in Figure 2. The pooled effect size SMD is −0.68 (p < 0.0001), with a 95% confidence interval of (−0.89, −0.47). This indicates that exercise intervention has a significant promoting effect on the improvement of sleep quality. p < 0.0001 indicates that the pooled effect size from multiple studies is statistically significant, thus suggesting that compared to the control group, exercise intervention can effectively enhance sleep quality.
3.4 Risk of bias assessment
The quality assessment of the studies was conducted using the Cochrane Risk of Bias tool (Higgins, 2011), which evaluates seven aspects: Random Sequence Generation, Allocation Concealment, Blinding of Participants and Personnel, Blinding of Outcome Assessment, Incomplete Outcome Data, Selective Reporting, and Other Bias. Each item in the assessment offers three options: “Low risk of bias,” “Unclear risk of bias,” and “High risk of bias” (Jadad et al., 1996). This assessment was carried out independently by two researchers, with a third researcher involved in resolving any discrepancies through discussion to reach a consensus. The risk of bias is visually represented in Figure 3.
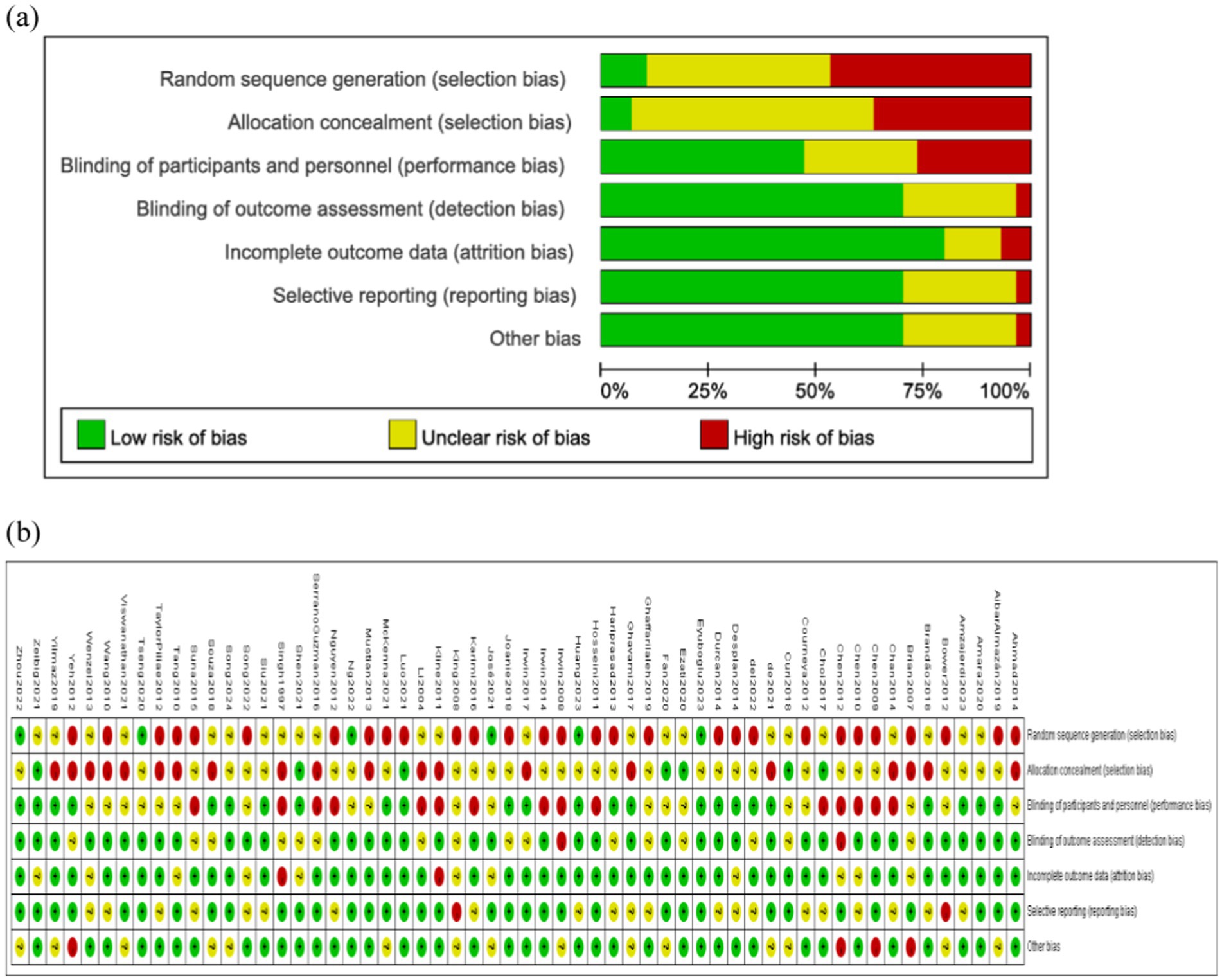
Figure 3. Bias risk assessment of included studies. (a) Risk of bias summary. (b) Risk of bias graph.
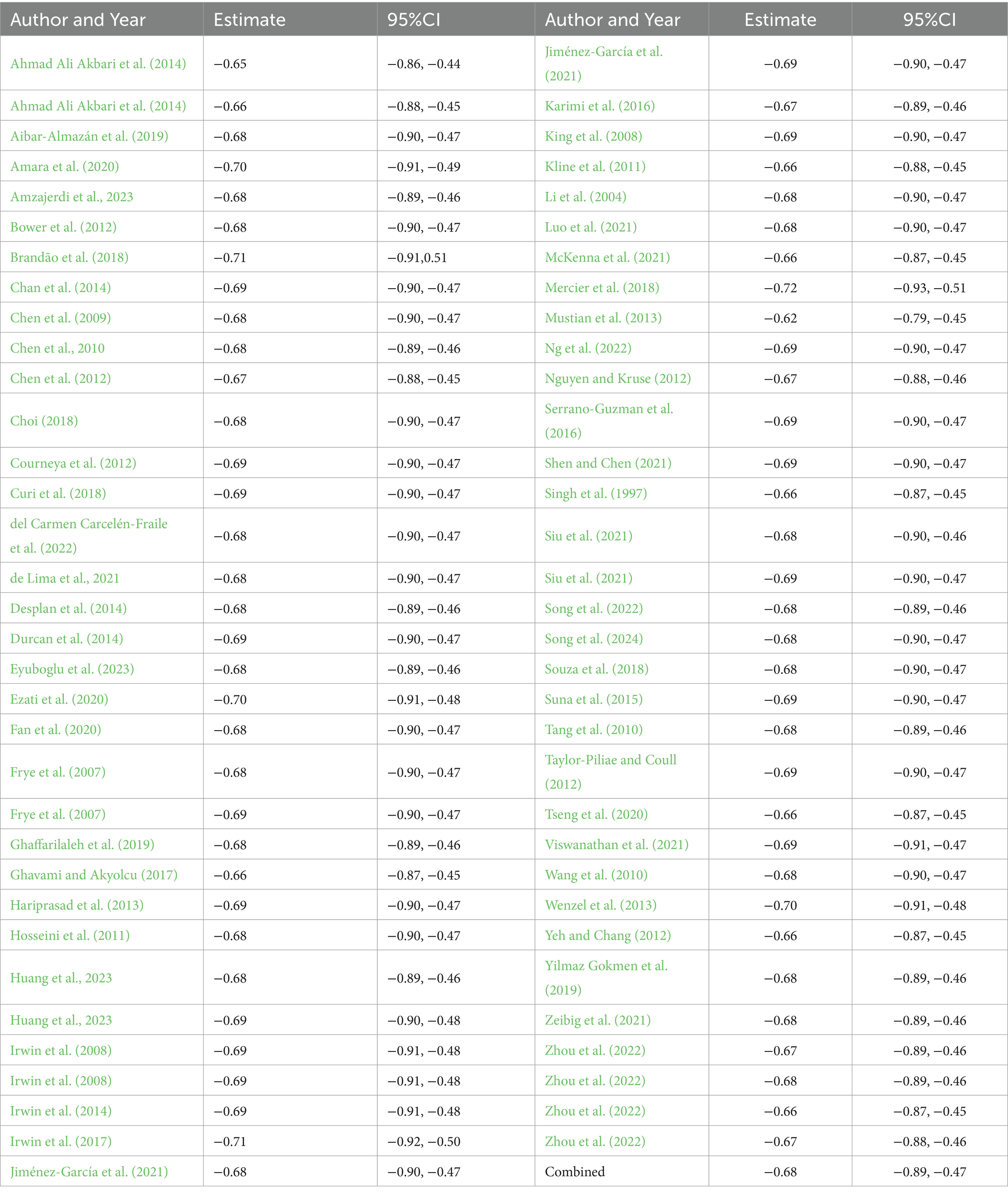
3.5 Sensitivity analyses
From Table 4, it can be seen that after the examination using the one-by-one exclusion method, the change in the effect size is minimal. This indicates that the removal of any single document did not significantly affect the overall combined effect size, suggesting that the analysis results of this study are robust, and the combined effect size is minimally influenced by any individual document.
3.6 Consistency tests
Network meta-analysis relies on the assumption of consistency, where consistency tests evaluate the coherence between specific direct and indirect evidence (defined as comparisons) (Dias et al., 2013). During the process of conducting a network meta-analysis, when a closed loop structure exists among various interventions, consistency testing is required to assess the degree of agreement between the results of direct and indirect comparisons (White et al., 2012). The p-value for the global consistency test of exercise type was 0.59, exceeding the significance threshold of 0.05, suggesting satisfactory overall consistency. Further examination of the consistency within each closed loop of exercise type revealed 95% confidence intervals (CI) of [0.00,3.60], [0.00,2.86], [0.00,2.99], and [0.00,1.76], with all lower bounds of the inconsistency factors including 0, suggesting good loop consistency. The global consistency test for exercise intensity (Intensity) resulted in a p-value of 0.065, which is also greater than 0.05, indicating good global consistency. Further examination of the consistency within each closed loop of exercise intensity showed 95% CI of [0.00,2.55] and [0.00,2.76], with both lower bounds of the inconsistency factors including 0, indicating good loop consistency. Consequently, a consistency model was adopted for analysis. Exercise frequency, exercise duration, and exercise period did not form closed loops, hence no consistency tests were required.
3.7 Network meta-analysis results
3.7.1 Network plot
In the network plot, the size of the circles corresponds to the sample size for each intervention, with larger circles indicating a greater number of samples. The lines connecting the circles represent comparisons between different interventions, and the thickness of the lines reflects the number of studies included in each comparison. The specific network plot is depicted in Figure 4 (The average number of elements is considered for elements that fall within a certain range).
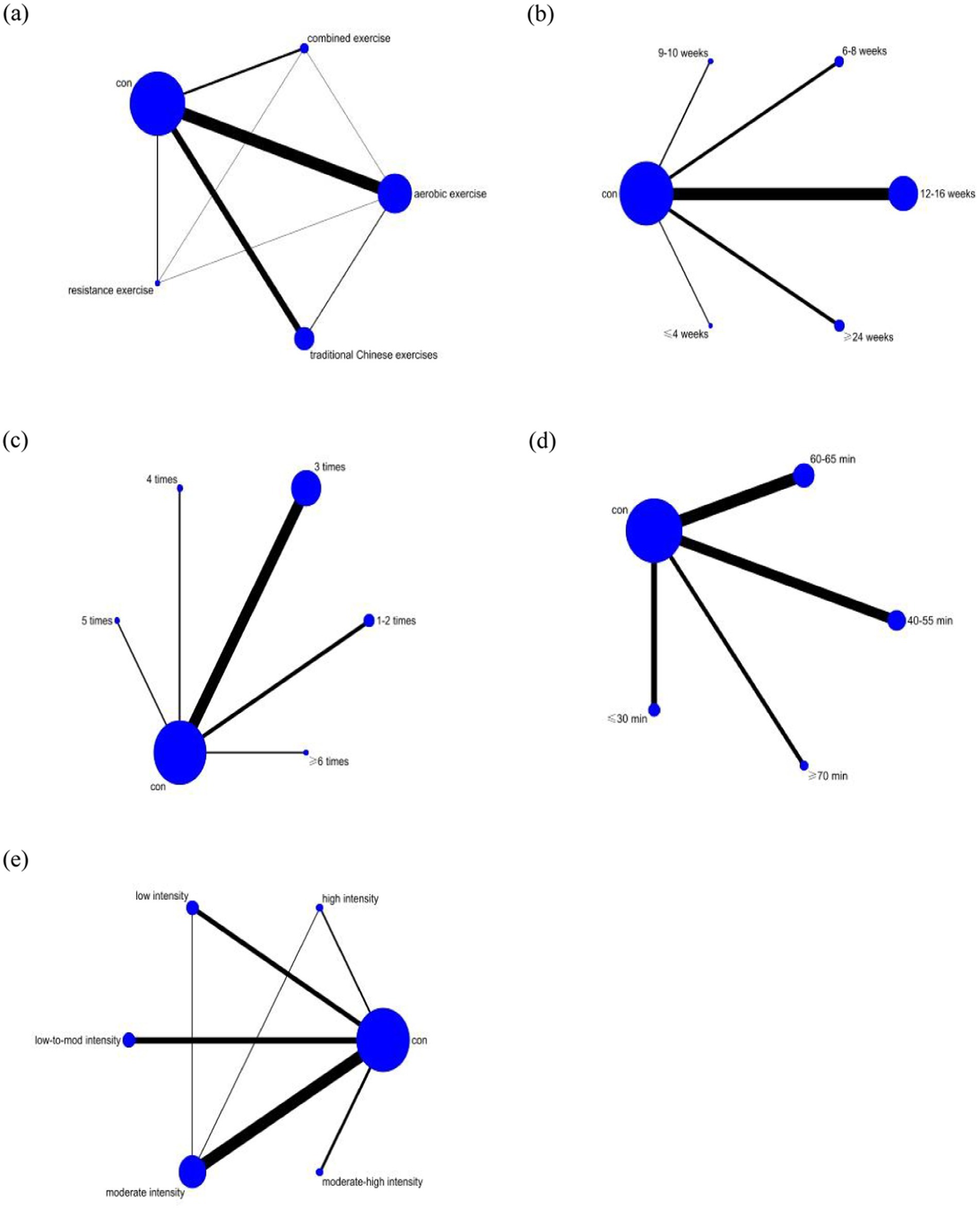
Figure 4. Network meta-analysis intervention diagram. (a) Type of exercise. (b) Exercise duration. (c) Exercise frequency. (d) Duration of a single exercise session. (e) Exercise intensity. Con, control group.
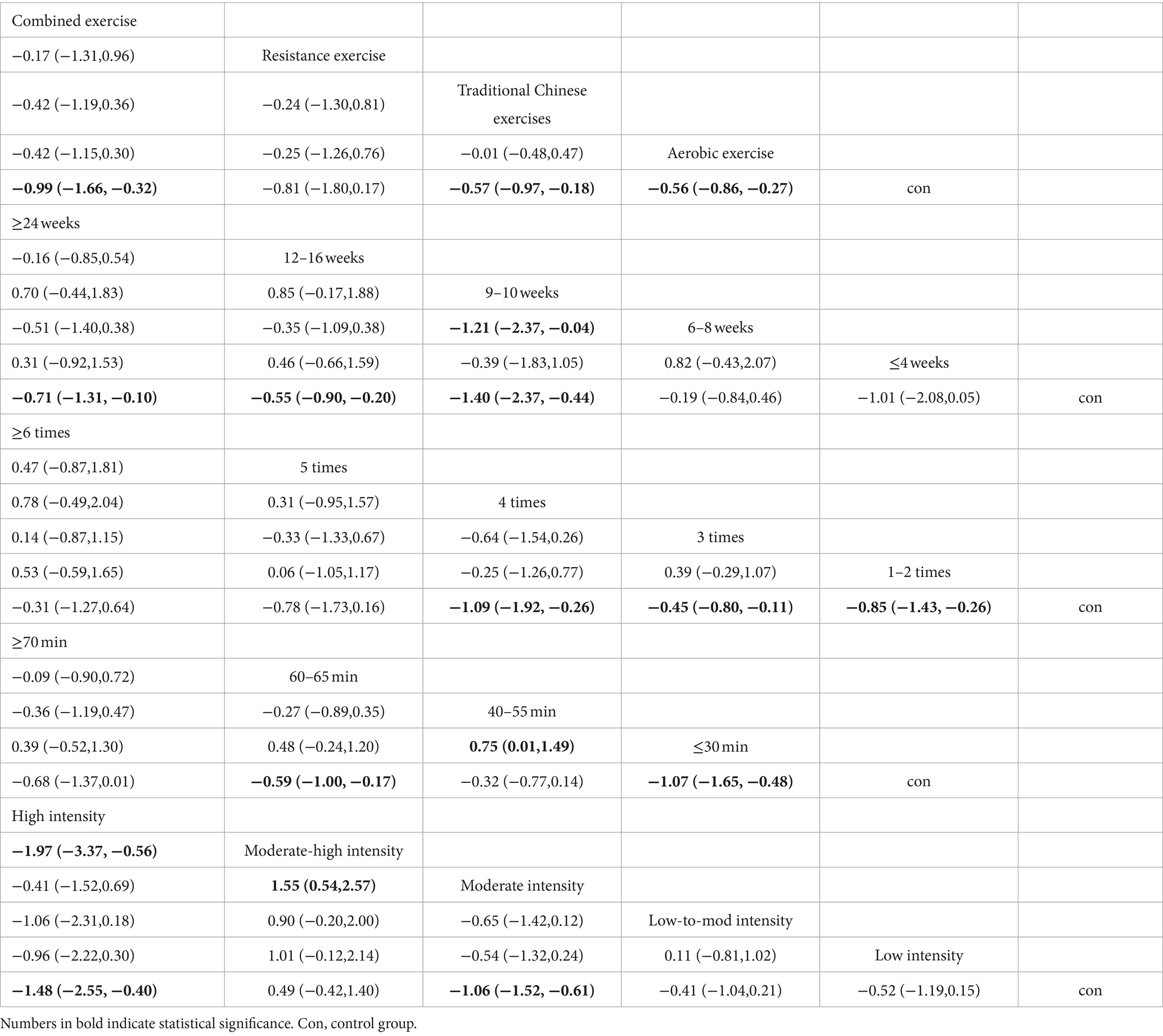
3.7.2 Pairwise meta-analysis results
As shown in Table 5, through pairwise comparisons, it was found that the intervention effects of aerobic exercise [SMD = −0.56, 95% CI (−0.86, −0.27)], traditional Chinese exercises [SMD = −0.57, 95% CI (−0.97, −0.18)], and combined exercise [SMD = −0.99, 95% CI (−1.66, −0.32)] were significantly better than those of the control group. This indicates that, compared to the control group, aerobic exercise, traditional Chinese exercises, and combined exercise are more effective in promoting sleep quality. The intervention periods of 9–10 weeks [SMD = −1.40, 95% CI (−2.37, −0.44)], 12–16 weeks [SMD = −0.55, 95% CI (−0.90, −0.20)], and ≥ 24 weeks [SMD = −0.71, 95% CI (−1.31, −0.10)] were significantly better than the control group, and the intervention effect of 9–10 weeks was significantly better than that of 6–8 weeks [SMD = −1.21, 95% CI (−2.37, −0.04)]. This suggests that, compared to the control group, intervention periods of 9–10 weeks, 12–16 weeks, and ≥ 24 weeks are more effective in promoting sleep, and the 9–10 weeks period is more conducive to improving sleep quality than the 6–8 weeks period. The intervention frequency of 1–2 times per week [SMD = −0.85, 95% CI (−1.43, −0.26)], 3 times per week [SMD = −0.45, 95% CI (−0.80, −0.11)], and 4 times per week [SMD = −1.09, 95% CI (−1.92, −0.26)] was significantly better than the control group. This indicates that, compared to the control group, intervention frequencies of 1–2 times, 3 times, and 4 times per week are more effective in promoting sleep. The intervention duration of ≤30 min and 60–65 min was significantly better than the control group, and the intervention effect of ≤30 min was significantly better than that of 40–55 min [SMD = 0.75, 95% CI (−1.49, −0.01)]. This suggests that, compared to the control group, interventions of ≤30 min and 60–65 min are more effective in promoting sleep, and the intervention of ≤30 min is more conducive to improving sleep quality than the 40–55 min intervention. The intervention intensity of moderate intensity [SMD = −1.06, 95% CI (−1.52, −0.61)] and high intensity [SMD = −1.48, 95% CI (−2.55, −0.40)] was significantly better than the control group, and both high intensity [SMD = −1.97, 95% CI (−3.37, −0.56)] and moderate intensity [SMD = −1.55, 95% CI (−2.57, −0.54)] interventions were significantly better than moderate-high intensity. This indicates that, compared to the control group, interventions of moderate and high intensity are more effective in promoting sleep, and interventions of moderate and high intensity are more conducive to improving sleep quality than moderate-high intensity interventions.
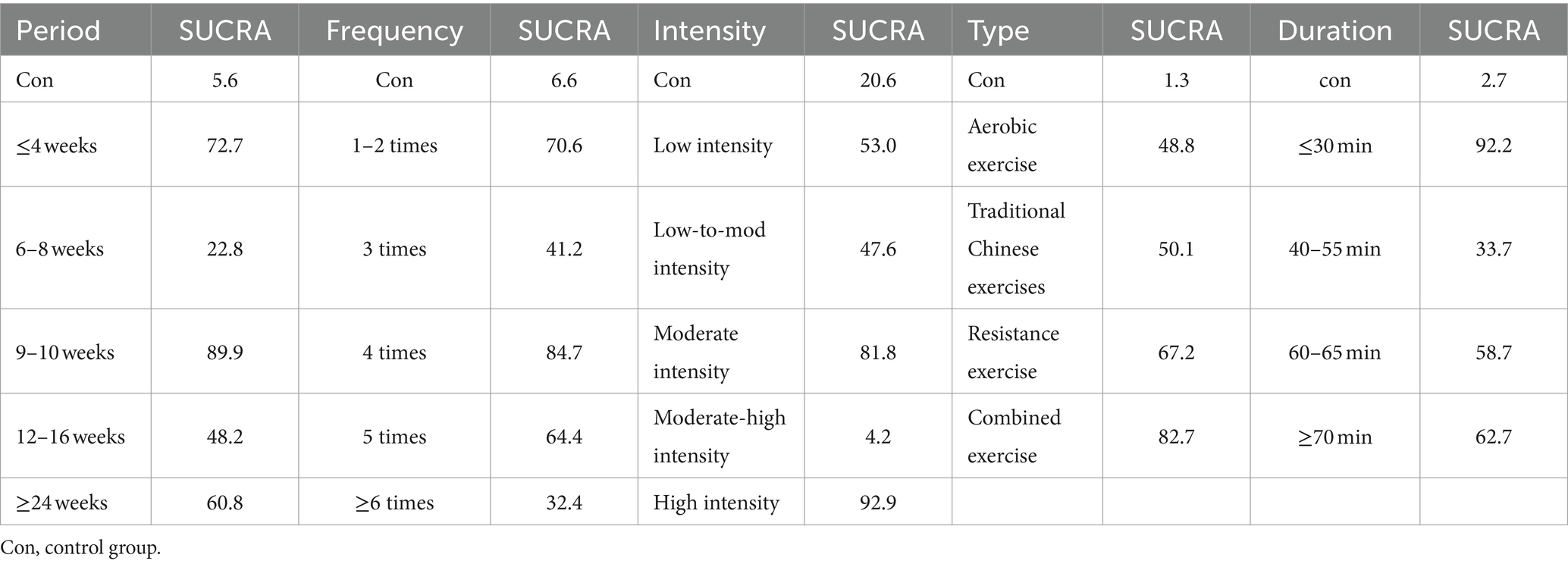
3.7.3 Ranking of the effectiveness of each exercise prescription element
According to the SUCRA method, the ranking of the impact of various types of exercise on sleep quality, as illustrated in Table 6, is as follows: combined exercise (SUCRA = 82.7) > resistance exercise (SUCRA = 67.2) > traditional Chinese exercises (SUCRA = 50.1) > aerobic exercise (SUCRA = 48.8). The ranking of the impact of different frequencies of exercise interventions on sleep quality is as follows: 4 times per week (SUCRA = 84.7) > 1–2 times per week (SUCRA = 70.6) > 5 times per week (SUCRA = 64.4) > 3 times per week (SUCRA = 41.2) > ≥6 times per week (SUCRA = 32.4). The ranking of the impact of various intensities of exercise interventions on sleep quality is as follows: high intensity (SUCRA = 92.9) > moderate intensity (SUCRA = 81.8) > low intensity (SUCRA = 53.0) > low-to-mod intensity (SUCRA = 47.6) > moderate-high intensity (SUCRA = 4.2). The ranking of the impact of various exercise durations on sleep quality is as follows: 9–10 weeks (SUCRA = 89.9) > ≤4 weeks (SUCRA = 72.7) > ≥24 weeks (SUCRA = 60.8) > 12–16 weeks (SUCRA = 48.2) > 6–8 weeks (SUCRA = 22.8). The ranking of the impact of different single intervention durations on sleep quality is as follows: ≤30 min (SUCRA = 92.2) > ≥ 70 min (SUCRA = 62.7) > 60–65 min (SUCRA = 58.7) > 40–55 min (SUCRA = 33.7) (Figure 5).
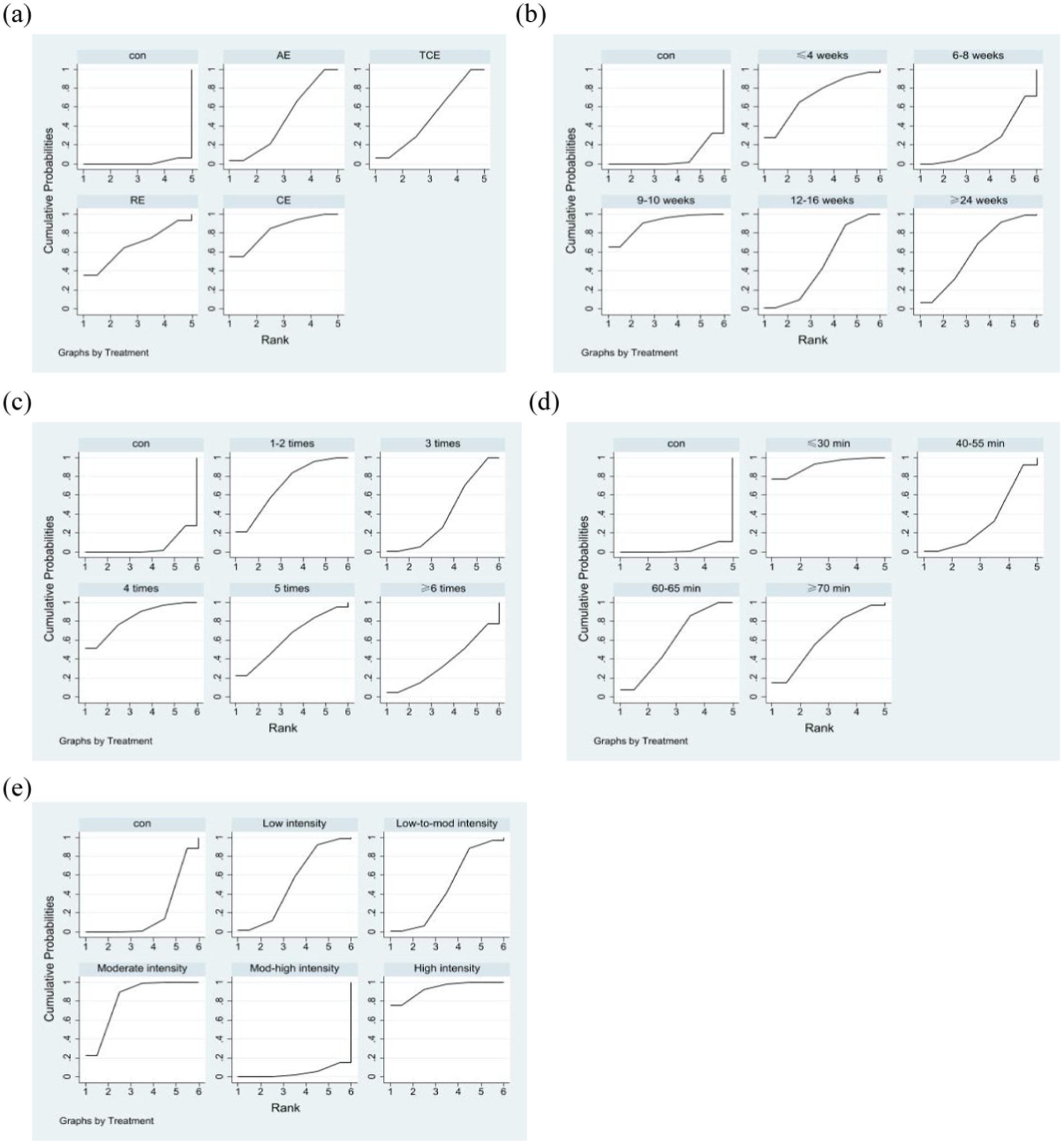
Figure 5. Probability ranking plot of the intervention effects of various exercise prescription elements. (a) Type of exercise. (b) Exercise duration. (c) Exercise frequency. (d) Duration of a single exercise session. (e) Exercise intensity. Con, control group.
3.7.4 Publication bias test
To examine the potential publication bias in network meta-analysis that may be caused by small-scale studies, funnel plots are used for analysis. Funnel plots can be visually inspected for symmetry, which effectively helps us determine whether there is bias caused by small-scale studies, providing an important basis for the reliability of the research results (Khera et al., 2016). From Figure 6, it can be observed that the distribution of study points on both sides of the inverted funnel plot is relatively regular, with only a few study points scattered, suggesting that the included literature has a low likelihood of publication bias.
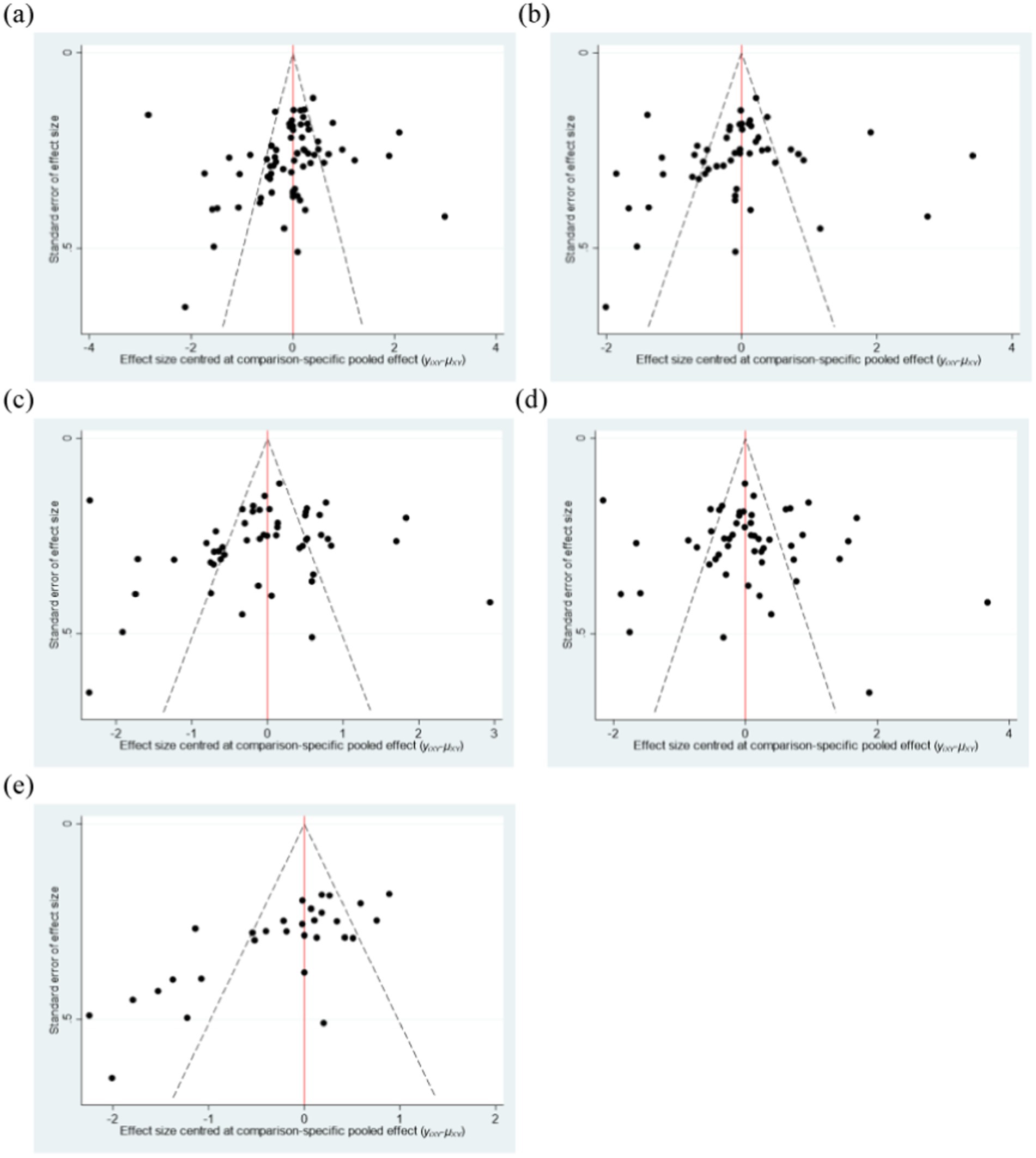
Figure 6. Funnel plot of the intervention effects of various elements of the exercise program. (a) Type of exercise. (b) Exercise duration. (c) Exercise frequency. (d) Duration of a single exercise session. (e) Exercise intensity. Con, control group.
Furthermore, this study also conducted a test for publication bias using the Egger method. The p-value was 0.167, with a 95% CI (−4.417, 0.777). This indicates that there is no significant publication bias.
4 Discussion
This study compares the effects of different interventions on sleep quality through a network meta-analysis of existing research. We conducted a comprehensive and in-depth synthesis analysis, including direct and indirect evidence from 58 randomized controlled trials involving 5,008 participants who underwent various exercise programs to analyze their impact on sleep quality. The purpose of this study is to address the limitations of previous meta-analyses that were often confined to a single aspect or immediate exercise effects by exploring the impact of exercise frequency, duration, period, intensity, and type on multiple dimensions of sleep quality.
In recent years, exercise has been widely recognized for its role in improving sleep quality. Specifically, aerobic exercise, traditional Chinese exercises, resistance exercise, and combined exercise have shown unique therapeutic effects, each promoting the enhancement of sleep quality through different mechanisms. Aerobic exercise can increase aerobic capacity parameters, reduce REM latency, and decrease wakefulness (Santos et al., 2012). Traditional Chinese exercises, such as Qigong and Tai Chi, significantly enhance the tone of the vagus nerve by slowing down bodily movement and respiratory frequency, thereby promoting the balance of the autonomic nervous system (ANS). This physiological regulatory process not only adjusts the reactivity of the hypothalamic–pituitary–adrenal axis (HPA axis) but also leads to a significant reduction in serum cortisol levels. This effectively alleviates stress responses and significantly improves sleep quality (Mudano et al., 2019). Resistance exercise is an enhancer of brain-derived neurotrophic factor (BDNF), with increased BDNF concentration levels in the brain after exercise (Babaei et al., 2013), promoting the connection and reorganization of neurons in the brain, further optimizing neural networks related to sleep regulation, and thus facilitating sleep initiation and maintenance (Chennaoui et al., 2015). Combined exercise has been found to be more effective than single exercise modalities in improving sleep quality (Zhou et al., 2022). The network meta-analysis concluded that: a frequency of exercise four times per week is more effective in improving sleep quality; a single exercise session duration of ≤30 min is more effective in improving sleep quality; a 9–10 weeks exercise intervention period is more effective in improving sleep quality; high-intensity exercise is more effective in improving sleep quality; and combined exercise is more effective in improving sleep quality.
This study found that combined exercise is the best type of exercise to improve sleep quality, which is inconsistent with some existing research results. Previous meta-analysis results have shown that aerobic exercise has the most significant effect on improving sleep quality (Fang et al., 2019). The reason may be that combined exercise can leverage the advantages of various types of exercise. Research has indicated that a combined program of aerobic and resistance exercise demonstrates superior effects in improving sleep quality (Brellenthin and Lee, 2022). This is due to the fact that aerobic exercise has been shown to positively impact the release of serotonin and noradrenaline, essential neurotransmitters for enhancing sleep quality (Dolezal et al., 2017). Additionally, aerobic exercise can increase melatonin levels, which aid in improving sleep propensity (Kline et al., 2011), regulating the sleep–wake cycle, and facilitating better and faster sleep at night (Chen et al., 2024). On the other hand, resistance exercise has been found to reduce sleep onset latency, promote faster sleep onset, decrease the number of awakenings after sleep onset, and improve sleep efficiency (Zhou et al., 2022). Consequently, the combined exercises demonstrate enhanced effects on improving sleep quality.
A frequency of exercise four times per week is most effective for improving sleep quality, a finding that is consistent with previous research conclusions (Feitl et al., 2009). Ezati’s investigation proposes that exercise regimens consisting of four to seven sessions weekly are linked to improved sleep quality (Ezati et al., 2020), while other studies have demonstrated that exercising at least three times per week yields more significant enhancements in sleep quality (Hasan et al., 2022). This phenomenon may be attributed to the modulatory impact of exercise frequency on mood, as evidenced by studies indicating that regular exercise at a frequency of four times per week can enhance the release of endorphins (Huang et al., 2023). Elevated levels of endorphins have been shown to mitigate stress and anxiety, induce relaxation, and regulate circadian rhythms, ultimately enhancing the quality of sleep (Ye et al., 2022). Additionally, Wu’s study suggests that exercising less than three times per week does not significantly improve sleep quality (Wu et al., 2015). Therefore, engaging in physical activity four times per week may yield more favorable results in terms of sleep quality.
This study demonstrates that an exercise duration of ≤30 min is most effective for enhancing sleep quality, aligning with previous research (Wu et al., 2015). Izci-Balserak suggests that, prolonged exercise sessions exceeding 60 min may result in significant muscle fatigue and elevated lactate levels (Izci-Balserak et al., 2022), hastening lymphocyte apoptosis and potentially causing discomfort and lengthening recovery periods, ultimately disrupting nighttime sleep patterns. As exercise duration extends beyond 90 minutes, it may adversely affect psychological and physical health, leading to excessive arousal at night, which can impact sleep quality. (Medic et al., 2017; Chekroud et al., 2018). On the other hand, brief bouts of exercise lasting between 10–30 min have been shown to stimulate the secretion of hormones, including endorphins, which can enhance the quality of sleep by increasing the amount of deep and rapid eye movement sleep (Chan et al., 2019). Other studies have demonstrated that engaging in a 30 min exercise regimen can lead to notable improvements in mental well-being (Tanaka et al., 2002). Maintaining a positive mental state before bedtime has been linked to reduced cognitive arousal prior to sleep onset (Dressle et al., 2023), facilitating quicker and more restful sleep (Lowe et al., 2019; Fank et al., 2022). Moreover, engaging in physical activity for less than 30 min can prevent the prolonged elevation of cortisol levels that may result from extended exercise sessions (Chan et al., 2019). This is significant as heightened cortisol secretion has been linked to disturbances in sleep patterns, including reduced deep sleep stages and disrupted sleep continuity and depth (Athanasiou et al., 2023). Consequently, limiting exercise duration to 30 min or less is shown to be more beneficial in enhancing the quality of sleep.
The study concluded that an exercise intervention lasting 9–10 weeks is most effective in enhancing sleep quality, aligning with previous research findings. A meta-analysis further supports the notion that short-term (<3 months) exercise interventions can notably improve sleep quality (Xie et al., 2021). Hasan’s study suggests that an exercise intervention lasting a minimum of 8 weeks is necessary for significant improvements in sleep quality (Hasan et al., 2022). Moreover, research findings indicate that a 9-week exercise regimen has been linked to notable enhancements in sleep quality, subjective sleep perception, and reduced sleep onset latency. These improvements in subjective sleep quality have been observed to persist for up to 3 months following the conclusion of the exercise intervention (Chan et al., 2014). Additionally, a 10-week exercise program has been demonstrated to effectively decrease sleep fragmentation and elevate melatonin levels, thereby promoting quicker sleep onset (Cai et al., 2014; Bonardi et al., 2016). It is important to note that engaging in exercise for a year may actually lead to difficulties in falling asleep (Tworoger et al., 2003). Thus, a moderate exercise intervention period is more beneficial for enhancing sleep quality.
The results of this study indicate that high-intensity exercise has the best effect on sleep quality. This is inconsistent with existing research results, where meta-analysis results have shown that moderate-intensity exercise interventions have the most significant effect on improving sleep quality (Zhao et al., 2023). This variation may arise from the distinct physiological effects of exercise intensity on the body. Lower exercise intensities have a limited stimulating impact on the sympathetic nervous system (SNS) (Daniela et al., 2022), which is insufficient to induce a significant transition from the SNS to the parasympathetic nervous system (PNS), a shift that is advantageous for enhancing deep sleep and overall sleep quality during the night (Garbarino et al., 2019). Conversely, high-intensity exercise elicits a more pronounced activation of the SNS; following exercise, the heightened SNS activation prompts a robust shift toward PNS activity (Druică et al., 2018), a mechanism that significantly promotes the onset of deep sleep (Trinder, 2012). Additionally, high-intensity exercise has been found to reduce daytime sleepiness (Chekroud et al., 2018), facilitate falling asleep at night (Xie et al., 2022), and decrease the number of awakenings after sleep onset (Larsen et al., 2019), ultimately leading to an overall improvement in sleep quality (Frimpong et al., 2021). Thus, high-intensity exercise is more conducive to the improvement of sleep quality.
At present, systematic comparative studies on the impact of exercise type and dosage combinations on sleep quality effects are still insufficient. In addition, previous studies have often used passive control methods in the setting of control groups, which may to some extent limit the comprehensiveness and accuracy of the results. In light of this, future research should focus on constructing an analytical framework based on different combinations of exercise types and dosages, delving into the specific effects of various types of exercise and their dosage changes on sleep quality, in order to scientifically evaluate the effectiveness of exercise interventions in enhancing sleep quality and to identify the optimal exercise type and dosage combination strategies. At the same time, to strengthen the rigor of research design, it is recommended to use active control methods to effectively reduce the potential impact of the placebo effect, ensuring the reliability and universality of research conclusions. By precisely analyzing the effects of exercise types and dosages on sleep quality, a basis can be provided for developing personalized and precise exercise intervention programs.
This network meta-analysis further supports the efficacy of exercise interventions in enhancing sleep quality. Based on the findings, we recommend the continuation of exercise routines. The research indicates that combined exercises performed four times a week, at a high intensity, over a period of 9–10 weeks, with each session lasting ≤30 min, are more effective in improving sleep quality. We hope that the results of this study will provide evidence for healthcare professionals, educators, and policymakers to make informed decisions. Subsequent research should prioritize the design of exercise types and dosages based on individual attributes, including gender and health status, to enhance the effectiveness of strategies for improving sleep quality.
Several limitations exist for this NMA: ① This study encompassed 58 randomized controlled trials with a total of 5,008 participants; however, the distribution of sample sizes across various types of exercise, exercise periods, durations, intensities, and frequencies were uneven. This disparity somewhat hinders the validity of the statistical analysis. ② The study predominantly evaluated sleep quality using the Pittsburgh Sleep Quality Index, a subjective self-assessment method that may introduce bias into the measurement results. ③ Our research centered on assessing the impact of exercise on sleep quality and did not involve a comparison with alternative intervention measures, such as cognitive behavioral therapy. ④ Furthermore, numerous randomized controlled trials lacked comprehensive descriptions of their randomization procedures, potentially compromising the generalizability and reliability of the study’s conclusions. ⑤ The control groups in the randomized controlled trials selected for this study all employed passive control, which is insufficient to completely rule out the presence of Hawthorne/Placebo effects.
5 Conclusion
This study systematically integrates 58 RCTs and analyzes the effectiveness of various exercise programs in improving sleep quality through a network meta-analysis approach. The research focuses on the perspective of exercise type and dosage combinations, comprehensively analyzing these elements of exercise programs to identify the optimal exercise program to improving sleep quality. The results show that a combined exercise program with a frequency of four times per week, a duration of ≤30 min, a period of 9–10 weeks, and a high-intensity level exhibits superior effectiveness in improving sleep quality. This finding transcends the limitations of previous studies that often focused on a single exercise element or short-term exercise effects, and by thoroughly analyzing all five exercise dimensions, it helps to determine a more effective exercise program for improving sleep quality. However, due to the limitations in the number and quality of included literature, as well as potential selection biases, caution should be exercised in interpreting the results of this study. Therefore, future research should further expand the sample size, optimize study designs, and notably in the selection of control groups, active controls should be adopted to effectively control the interference of placebo effects, thereby enhancing the reliability of the research findings.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
LL: Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing. CW: Data curation, Formal analysis, Writing – original draft. DW: Data curation, Methodology, Writing – original draft. HL: Formal analysis, Methodology, Writing – original draft. SZ: Methodology, Software, Writing – original draft. YH: Conceptualization, Formal analysis, Software, Writing – original draft, Writing – review & editing. PW: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the National Social Science Fund of China (Grant No. 22BTY011).
Acknowledgments
We would like to thank all authors for their encouragement and guidance throughout this project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1466277/full#supplementary-material
References
Ahmad Ali Akbari, K., Amir, S., Parvaneh Shamsipour, D., and Robabeh, M. (2014). Effect of low and moderate intensity aerobic exerciseson sleep quality in elderly adult males. Pak J Med.
Aibar-Almazán, A., Hita-Contreras, F., Cruz-Díaz, D., de la Torre-Cruz, M., Jiménez-García, J. D., and Martínez-Amat, A. (2019). Effects of Pilates training on sleep quality, anxiety, depression and fatigue in postmenopausal women: a randomized controlled trial. Maturitas 124, 62–67. doi: 10.1016/j.maturitas.2019.03.019
Almondes, K. M. D., Marín Agudelo, H. A., and Jiménez-Correa, U. (2021). Impact of sleep deprivation on emotional regulation and the immune system of healthcare workers as a risk factor for COVID 19: practical recommendations from a task force of the Latin American association of sleep psychology. Front. Psychol. 12:564227. doi: 10.3389/fpsyg.2021.564227
Aloba, O. O., Adewuya, A. O., Ola, B. A., and Mapayi, B. M. (2007). Validity of the Pittsburgh sleep quality index (PSQI) among Nigerian university students. Sleep Med. 8, 266–270. doi: 10.1016/j.sleep.2006.08.003
Alsaadi, S. M., McAuley, J. H., Hush, J. M., Bartlett, D. J., Henschke, N., Grunstein, R. R., et al. (2013). Detecting insomnia in patients with low back pain: accuracy of four self-report sleep measures. BMC Musculoskelet. Disord. 14, 1–9. doi: 10.1186/1471-2474-14-196
Amara, A. W., Wood, K. H., Joop, A., Memon, R. A., Pilkington, J., Tuggle, S. C., et al. (2020). Randomized, controlled trial of exercise on objective and subjective sleep in Parkinson's disease. Mov. Disord. 35, 947–958. doi: 10.1002/mds.28009
Amzajerdi, A., Keshavarz, M., Ezati, M., and Sarvi, F. (2023). The effect of Pilates exercises on sleep quality and fatigue among female students dormitory residents. BMC Sports Sci. Med. Rehabil. 15:67. doi: 10.1186/s13102-023-00675-7
Athanasiou, N., Bogdanis, G. C., and Mastorakos, G. (2023). Endocrine responses of the stress system to different types of exercise. Rev. Endocrine Metabolic Disord. 24, 251–266. doi: 10.1007/s11154-022-09758-1
Babaei, P., Azali Alamdari, K., Soltani Tehrani, B., and Damirchi, A. (2013). Effect of six weeks of endurance exercise and following detraining on serum brain derived neurotrophic factor and memory performance in middle aged males with metabolic syndrome. J. Sports Med. Phys. Fitness 53, 437–443
Banno, M., Harada, Y., Taniguchi, M., Tobita, R., Tsujimoto, H., Tsujimoto, Y., et al. (2018). Exercise can improve sleep quality: a systematic review and meta-analysis. PeerJ 6:e5172. doi: 10.7717/peerj.5172
Bertolazi, A. N., Fagondes, S. C., Hoff, L. S., Dartora, E. G., da Silva Miozzo, I. C., de Barba, M. E. F., et al. (2011). Validation of the Brazilian Portuguese version of the Pittsburgh sleep quality index. Sleep Med. 12, 70–75. doi: 10.1016/j.sleep.2010.04.020
Bjorvatn, B., Jernelöv, S., and Pallesen, S. (2021). Insomnia–a heterogenic disorder often comorbid with psychological and somatic disorders and diseases: a narrative review with focus on diagnostic and treatment challenges. Front. Psychol. 12:639198. doi: 10.3389/fpsyg.2021.639198
Bonardi, J. M., Lima, L. G., Campos, G. O., Bertani, R. F., Moriguti, J. C., Ferriolli, E., et al. (2016). Effect of different types of exercise on sleep quality of elderly subjects. Sleep Med. 25, 122–129. doi: 10.1016/j.sleep.2016.06.025
Bower, J. E., Garet, D., Sternlieb, B., Ganz, P. A., Irwin, M. R., Olmstead, R., et al. (2012). Yoga for persistent fatigue in breast cancer survivors: a randomized controlled trial. Cancer 118, 3766–3775. doi: 10.1002/cncr.26702
Brandão, G. S., Gomes, G. S. B. F., Brandão, G. S., Callou Sampaio, A. A., Donner, C. F., Oliveira, L. V., et al. (2018). Home exercise improves the quality of sleep and daytime sleepiness of elderlies: a randomized controlled trial. Multidiscip. Respir. Med. 13, 1–9. doi: 10.1186/s40248-017-0114-3
Brellenthin, A. G., and Lee, D.-C. (2022). Comparative effects of aerobic, resistance, and combined exercise on sleep. Circulation 145:A038–A038. doi: 10.1161/circ.145.suppl_1.038
Brown, W. J., Hayman, M., Haakstad, L. A., Lamerton, T., Mena, G. P., Green, A., et al. (2022). Australian guidelines for physical activity in pregnancy and postpartum. J. Sci. Med. Sport 25, 511–519. doi: 10.1016/j.jsams.2022.03.008
Bull, F. C., Al-Ansari, S. S., Biddle, S., Borodulin, K., Buman, M. P., Cardon, G., et al. (2020). World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 54, 1451–1462. doi: 10.1136/bjsports-2020-102955
Bushnell, G. A., Gerhard, T., Keyes, K., Hasin, D., Cerdá, M., and Olfson, M. (2022). Association of benzodiazepine treatment for sleep disorders with drug overdose risk among young people. JAMA Netw. Open 5:e2243215. doi: 10.1001/jamanetworkopen.2022.43215
Cai, Z.-Y., Chen, K. W.-C., and Wen, H.-J. (2014). Effects of a group-based step aerobics training on sleep quality and melatonin levels in sleep-impaired postmenopausal women. J. Strength Cond. Res. 28, 2597–2603. doi: 10.1519/JSC.0000000000000428
Chan, J. S., Ho, R. T., Chung, K.-F., Wang, C.-W., Yao, T.-J., Ng, S.-M., et al. (2014). Qigong exercise alleviates fatigue, anxiety, and depressive symptoms, improves sleep quality, and shortens sleep latency in persons with chronic fatigue syndrome-like illness. Evid. Based Complement. Alternat. Med. 2014:106048. doi: 10.1155/2014/106048
Chan, J. S., Liu, G., Liang, D., Deng, K., Wu, J., and Yan, J. H. (2019). Special issue–therapeutic benefits of physical activity for mood: a systematic review on the effects of exercise intensity, duration, and modality. J. Psychol. 153, 102–125. doi: 10.1080/00223980.2018.1470487
Chandler, J., Cumpston, M., Li, T., Page, M. J., and Welch, V. (2019). Cochrane handbook for systematic reviews of interventions. Hoboken: Wiley.
Chandrasekaran, B. (2020). Science of sleep and sports performance-a scopin. Sci. Sports 35, 3–11. doi: 10.1016/j.scispo.2019.03.006
Chaput, J.-P., Carrier, J., Bastien, C., Gariépy, G., and Janssen, I. (2022). Economic burden of insufficient sleep duration in Canadian adults. Sleep Health 8, 298–302. doi: 10.1016/j.sleh.2022.02.001
Chekroud, S. R., Gueorguieva, R., Zheutlin, A. B., Paulus, M., Krumholz, H. M., Krystal, J. H., et al. (2018). Association between physical exercise and mental health in 1· 2 million individuals in the USA between 2011 and 2015: a cross-sectional study. Lancet Psychiatry 5, 739–746. doi: 10.1016/S2215-0366(18)30227-X
Chen, K.-M., Chen, M.-H., Chao, H.-C., Hung, H.-M., Lin, H.-S., and Li, C.-H. (2009). Sleep quality, depression state, and health status of older adults after silver yoga exercises: cluster randomized trial. Int. J. Nurs. Stud. 46, 154–163. doi: 10.1016/j.ijnurstu.2008.09.005
Chen, K.-M., Chen, M.-H., Lin, M.-H., Fan, J.-T., Lin, H.-S., and Li, C.-H. (2010). Effects of yoga on sleep quality and depression in elders in assisted living facilities. J. Nurs. Res. 18, 53–61. doi: 10.1097/JNR.0b013e3181ce5189
Chen, M.-C., Liu, H.-E., Huang, H.-Y., and Chiou, A.-F. (2012). The effect of a simple traditional exercise programme (Baduanjin exercise) on sleep quality of older adults: a randomized controlled trial. Int. J. Nurs. Stud. 49, 265–273. doi: 10.1016/j.ijnurstu.2011.09.009
Chen, R., Wang, S., Hu, Q., Kang, N., Xie, H., Liu, M., et al. (2024). Exercise intervention in middle-aged and elderly individuals with insomnia improves sleep and restores connectivity in the motor network. Transl. Psychiatry 14:159. doi: 10.1038/s41398-024-02875-2
Chennaoui, M., Arnal, P. J., Sauvet, F., and Léger, D. (2015). Sleep and exercise: a reciprocal issue? Sleep Med. Rev. 20, 59–72. doi: 10.1016/j.smrv.2014.06.008
Choi, M.-J., and Sohng, K.-Y. (2018). The effects of floor-seated exercise program on physical fitness, depression, and sleep in older adults: a cluster randomized controlled trial. Int. J. Gerontol. 12, 116–121. doi: 10.1016/j.ijge.2017.06.003
Cipriani, A., Higgins, J. P., Geddes, J. R., and Salanti, G. (2013). Conceptual and technical challenges in network meta-analysis. Ann. Intern. Med. 159, 130–137. doi: 10.7326/0003-4819-159-2-201307160-00008
Courneya, K. S., Sellar, C. M., Trinh, L., Forbes, C. C., Stevinson, C., McNeely, M. L., et al. (2012). A randomized trial of aerobic exercise and sleep quality in lymphoma patients receiving chemotherapy or no treatments. Cancer Epidemiol. Biomarkers Prev. 21, 887–894. doi: 10.1158/1055-9965.EPI-12-0075
Curi, V., Vilaça, J., Haas, A., and Fernandes, H. (2018). Effects of 16-weeks of Pilates on health perception and sleep quality among elderly women. Arch. Gerontol. Geriatr. 74, 118–122. doi: 10.1016/j.archger.2017.10.012
Daly, C. H., Neupane, B., Beyene, J., Thabane, L., Straus, S. E., and Hamid, J. S. (2019). Empirical evaluation of SUCRA-based treatment ranks in network meta-analysis: quantifying robustness using Cohen’s kappa. BMJ Open 9:e024625. doi: 10.1136/bmjopen-2018-024625
Daniela, M., Catalina, L., Ilie, O., Paula, M., Daniel-Andrei, I., and Ioana, B. (2022). Effects of exercise training on the autonomic nervous system with a focus on anti-inflammatory and antioxidants effects. Antioxidants 11:350. doi: 10.3390/antiox11020350
de Lima, B. E., Passos, G. S., Youngstedt, S. D., Júnior, L. C. B. S., and Santana, M. G. (2021). Effects of Xbox Kinect exercise training on sleep quality, anxiety and functional capacity in older adults. J. Bodyw. Mov. Ther. 28, 271–275. doi: 10.1016/j.jbmt.2021.07.029
del Carmen Carcelén-Fraile, M., Aibar-Almazán, A., Martínez-Amat, A., Jiménez-García, J. D., Brandão-Loureiro, V., García-Garro, P. A., et al. (2022). Qigong for mental health and sleep quality in postmenopausal women: a randomized controlled trial. Medicine 101:e30897. doi: 10.1097/MD.0000000000030897
Desplan, M., Mercier, J., Sabaté, M., Ninot, G., Prefaut, C., and Dauvilliers, Y. (2014). A comprehensive rehabilitation program improves disease severity in patients with obstructive sleep apnea syndrome: a pilot randomized controlled study. Sleep Med. 15, 906–912. doi: 10.1016/j.sleep.2013.09.023
Dias, S., Welton, N. J., Sutton, A. J., Caldwell, D. M., Lu, G., and Ades, A. (2013). Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Med. Decis. Mak. 33, 641–656. doi: 10.1177/0272989X12455847
Dolezal, B. A., Neufeld, E. V., Boland, D. M., Martin, J. L., and Cooper, C. B. (2017). Interrelationship between sleep and exercise: a systematic review. Adv. Prev. Med. 2017:1364387. doi: 10.1155/2017/1364387
Dressle, R. J., Riemann, D., Spiegelhalder, K., Frase, L., Perlis, M. L., and Feige, B. (2023). On the relationship between EEG spectral analysis and pre-sleep cognitive arousal in insomnia disorder: towards an integrated model of cognitive and cortical arousal. Sport & Society/Sport si Societate 32:e13861. doi: 10.1111/jsr.13861
Druică, A., Anton-Păduraru, D., and Mocanu, V. (2018). The effects of high intensity training on salivary markers of the sympathetic nervous system. Sport & Society/Sport si Societate 18, 16–20. doi: 10.1186/s12885-020-07295-1
Durcan, L., Wilson, F., and Cunnane, G. (2014). The effect of exercise on sleep and fatigue in rheumatoid arthritis: a randomized controlled study. J. Rheumatol. 41, 1966–1973. doi: 10.3899/jrheum.131282
Dzierzewski, J. M., Sabet, S. M., Ghose, S. M., Perez, E., Soto, P., Ravyts, S. G., et al. (2021). Lifestyle factors and sleep health across the lifespan. Int. J. Environ. Res. Public Health 18:6626. doi: 10.3390/ijerph18126626
Eyuboglu, F., Inal-Ince, D., Karamancioglu, B., Vardar-Yagli, N., Kaya-Utlu, D., Dalkilic, O., et al. (2023). Effect of tele-yoga on aerobic capacity, respiratory muscle strength, and cognitive performance in patients with obstructive sleep apnea syndrome. Heart Lung 62, 157–167. doi: 10.1016/j.hrtlng.2023.07.005
Ezati, M., Keshavarz, M., Barandouzi, Z. A., and Montazeri, A. (2020). The effect of regular aerobic exercise on sleep quality and fatigue among female student dormitory residents. BMC Sports Sci. Med. Rehabil. 12, 1–8. doi: 10.1186/s13102-020-00190-z
Fan, B., Song, W., Zhang, J., Er, Y., Xie, B., Zhang, H., et al. (2020). The efficacy of mind-body (Baduanjin) exercise on self-reported sleep quality and quality of life in elderly subjects with sleep disturbances: a randomized controlled trial. Sleep Breathing 24, 695–701. doi: 10.1007/s11325-019-01999-w
Fang, Y. Y., Hung, C. T., Chan, J. C., Huang, S. M., and Lee, Y. H. (2019). Meta-analysis: exercise intervention for sleep problems in cancer patients. Eur. J. Cancer Care 28:e13131. doi: 10.1111/ecc.13131
Fank, F., da Silva Pereira, F., Dos Santos, L., De Mello, M. T., and Mazo, G. Z. (2022). Effects of exercise on sleep in older adults: an overview of systematic reviews and meta-analyses. J. Aging Phys. Act. 30, 1101–1117. doi: 10.1123/japa.2021-0444
Feitl, K., Millett, A., Colin, S., Dabiri, J. O., and Costello, J. H. (2009). Functional morphology and fluid interactions during early development of the scyphomedusa Aurelia aurita. Biol. Bull. 217, 283–291. doi: 10.1086/BBLv217n3p283
Frimpong, E., Mograss, M., Zvionow, T., and Dang-Vu, T. T. (2021). The effects of evening high-intensity exercise on sleep in healthy adults: a systematic review and meta-analysis. Sleep Med. Rev. 60:101535. doi: 10.1016/j.smrv.2021.101535
Frye, B., Scheinthal, S., Kemarskaya, T., and Pruchno, R. (2007). Tai chi and low impact exercise: effects on the physical functioning and psychological well-being of older people. J. Appl. Gerontol. 26, 433–453. doi: 10.1177/0733464807306915
Galinsky, A. M., Ward, B. W., Joestl, S. S., and Dahlhamer, J. M. (2018). Sleep duration, sleep quality, and sexual orientation: findings from the 2013-2015 National Health Interview Survey. Sleep Health 4, 56–62. doi: 10.1016/j.sleh.2017.10.004
Garbarino, S., Lanteri, P., Feeling, N. R., Jarczok, M. N., Quintana, D. S., Koenig, J., et al. (2019). Circadian rhythms, sleep, and the autonomic nervous system. Boston, MA: Hogrefe Publishing.
Ghaffarilaleh, G., Ghaffarilaleh, V., Sanamno, Z., Kamalifard, M., and Alibaf, L. (2019). Effects of yoga on quality of sleep of women with premenstrual syndrome. Altern. Ther. Health Med. 25, 40–47.
Ghavami, H., and Akyolcu, N. (2017). The impact of lifestyle interventions in breast cancer women after completion of primary therapy: a randomized study. J. Breast Health 13, 94–99. doi: 10.5152/tjbh.2017.3342
Hannan, E. L. (2008). Randomized clinical trials and observational studies: guidelines for assessing respective strengths and limitations. J. Am. Coll. Cardiol. Intv. 1, 211–217. doi: 10.1016/j.jcin.2008.01.008
Hariprasad, V., Sivakumar, P., Koparde, V., Varambally, S., Thirthalli, J., Varghese, M., et al. (2013). Effects of yoga intervention on sleep and quality-of-life in elderly: a randomized controlled trial. Indian J. Psychiatry 55, S364–S368. doi: 10.4103/0019-5545.116310
Hasan, F., Tu, Y.-K., Lin, C.-M., Chuang, L.-P., Jeng, C., Yuliana, L. T., et al. (2022). Comparative efficacy of exercise regimens on sleep quality in older adults: a systematic review and network meta-analysis. Sleep Med. Rev. 65:101673. doi: 10.1016/j.smrv.2022.101673
Higgins, J. (2011). The Cochrane Collaboration’s tool for assessing risk of Bias in randomised trials. Cochrane Collab. 343:d5928. doi: 10.1136/bmj.d5928
Hita-Contreras, F., Martínez-López, E., Latorre-Román, P. A., Garrido, F., Santos, M. A., and Martínez-Amat, A. (2014). Reliability and validity of the Spanish version of the Pittsburgh sleep quality index (PSQI) in patients with fibromyalgia. Rheumatol. Int. 34, 929–936. doi: 10.1007/s00296-014-2960-z
Holfinger, S., Chan, L., and Donald, R. (2021). All you need is sleep: the effects of sleep apnea and treatment benefits in the heart failure patient. Curr. Heart Fail. Rep. 18, 144–152. doi: 10.1007/s11897-021-00506-1
Hosseini, H., Esfirizi, M. F., Marandi, S. M., and Rezaei, A. (2011). The effect of Ti chi exercise on the sleep quality of the elderly residents in Isfahan, Sadeghieh elderly home. Iran. J. Nurs. Midwifery Res. 16, 55–60
Huang, X., Wang, X., Shao, Y., Lin, A., Zhang, Z., Qi, H., et al. (2023). Effects of health qigong exercise on sleep and life quality in patients with drug abuse. Hong Kong J. Occup. Ther. 36, 13–19. doi: 10.1177/15691861231156002
Hutton, B., Salanti, G., Caldwell, D. M., Chaimani, A., Schmid, C. H., Cameron, C., et al. (2015). The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann. Intern. Med. 162, 777–784. doi: 10.7326/M14-2385
Irwin, M. R., Olmstead, R., Carrillo, C., Sadeghi, N., Breen, E. C., Witarama, T., et al. (2014). Cognitive behavioral therapy vs. tai chi for late life insomnia and inflammatory risk: a randomized controlled comparative efficacy trial. Sleep 37, 1543–1552. doi: 10.5665/sleep.4008
Irwin, M. R., Olmstead, R., Carrillo, C., Sadeghi, N., Nicassio, P., Ganz, P. A., et al. (2017). Tai chi Chih compared with cognitive behavioral therapy for the treatment of insomnia in survivors of breast cancer: a randomized, partially blinded, noninferiority trial. J. Clin. Oncol. 35, 2656–2665. doi: 10.1200/JCO.2016.71.0285
Irwin, M. R., Olmstead, R., and Motivala, S. J. (2008). Improving sleep quality in older adults with moderate sleep complaints: a randomized controlled trial of Tai Chi Chih. Sleep 31, 1001–1008. doi: 10.5665/sleep/31.7.1001
Izci-Balserak, B., Zhu, B., Wang, H., Bronas, U. G., and Gooneratne, N. S. (2022). Independent associations between sleep duration, gamma gap, and cognitive function among older adults: results from the NHANES 2013-2014. Geriatr. Nurs. 44, 1–7. doi: 10.1016/j.gerinurse.2021.12.019
Jadad, A. R., Moore, R. A., Carroll, D., Jenkinson, C., Reynolds, D. J. M., Gavaghan, D. J., et al. (1996). Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control. Clin. Trials 17, 1–12. doi: 10.1016/0197-2456(95)00134-4
Jiménez-García, J. D., Hita-Contreras, F., de la Torre-Cruz, M. J., Aibar-Almazán, A., Achalandabaso-Ochoa, A., Fábrega-Cuadros, R., et al. (2021). Effects of HIIT and MIIT suspension training programs on sleep quality and fatigue in older adults: randomized controlled clinical trial. Int. J. Environ. Res. Public Health 18:1211. doi: 10.3390/ijerph18031211
Karimi, S., Soroush, A., Towhidi, F., Makhsosi, B. R., Karimi, M., Jamehshorani, S., et al. (2016). Surveying the effects of an exercise program on the sleep quality of elderly males. Clinical Interven Aging, 11, 997–1002. doi: 10.2147/CIA.S106808
Khera, R., Murad, M. H., Chandar, A. K., Dulai, P. S., Wang, Z., Prokop, L. J., et al. (2016). Association of pharmacological treatments for obesity with weight loss and adverse events: a systematic review and meta-analysis. JAMA 315, 2424–2434. doi: 10.1001/jama.2016.7602
King, A. C., Pruitt, L. A., Woo, S., Castro, C. M., Ahn, D. K., Vitiello, M. V., et al. (2008). Effects of moderate-intensity exercise on polysomnographic and subjective sleep quality in older adults with mild to moderate sleep complaints. J. Gerontol. Ser. A Biol. Med. Sci. 63, 997–1004. doi: 10.1093/gerona/63.9.997
Kline, C. E., Crowley, E. P., Ewing, G. B., Burch, J. B., Blair, S. N., Durstine, J. L., et al. (2011). The effect of exercise training on obstructive sleep apnea and sleep quality: a randomized controlled trial. Sleep 34, 1631–1640. doi: 10.5665/sleep.1422
Kodama, S., Fujihara, K., Horikawa, C., Yamada, M., Sato, T., Yaguchi, Y., et al. (2021). Network meta-analysis of drug therapies for lowering uric acid and mortality risk in patients with heart failure. Cardiovasc. Drugs Ther. 35, 1217–1225. doi: 10.1007/s10557-020-07097-4
Kreutz, C., Schmidt, M. E., and Steindorf, K. (2019). Effects of physical and mind–body exercise on sleep problems during and after breast cancer treatment: a systematic review and meta-analysis. Breast Cancer Res. Treat. 176, 1–15. doi: 10.1007/s10549-019-05217-9
La Touche, R., Fernandez Perez, J. J., Proy Acosta, A., Gonzalez Campodonico, L., Martinez Garcia, S., Adraos Juarez, D., et al. (2020). Is aerobic exercise helpful in patients with migraine? A systematic review and meta-analysis. Scand. J. Med. Sci. Sports 30, 965–982. doi: 10.1111/sms.13625
Larsen, P., Marino, F., Melehan, K., Guelfi, K. J., Duffield, R., and Skein, M. (2019). High-intensity interval exercise induces greater acute changes in sleep, appetite-related hormones, and free-living energy intake than does moderate-intensity continuous exercise. Appl. Physiol. Nutr. Metab. 44, 557–566. doi: 10.1139/apnm-2018-0503
Lei, H., Ma, Z., Tian, K., Liu, K., Wang, J., Zhu, X., et al. (2022). The effects of different types of tai chi exercises on motor function in patients with Parkinson's disease: a network meta-analysis. Front. Aging Neurosci. 14:936027. doi: 10.3389/fnagi.2022.936027
Li, F., Fisher, K. J., Harmer, P., Irbe, D., Tearse, R. G., and Weimer, C. (2004). Tai chi and self-rated quality of sleep and daytime sleepiness in older adults: a randomized controlled trial. J. Am. Geriatr. Soc. 52, 892–900. doi: 10.1111/j.1532-5415.2004.52255.x
Li, H.-J., He, L.-Y., Liu, Z.-S., Sun, Y.-N., Yan, S.-Y., Liu, J., et al. (2014). On-site quality control of acupuncture randomized controlled trial: design of content and checklist of quality control based on PICOST. Zhongguo Zhen Jiu 34, 183–185.
Liu, Y. (2016). Prevalence of healthy sleep duration among adults—United States, 2014. MMWR 65, 137–141. doi: 10.15585/mmwr.mm6506a1
Lowe, H., Haddock, G., Mulligan, L. D., Gregg, L., Fuzellier-Hart, A., Carter, L.-A., et al. (2019). Does exercise improve sleep for adults with insomnia? A systematic review with quality appraisal. Clin. Psychol. Rev. 68, 1–12. doi: 10.1016/j.cpr.2018.11.002
Lu, J., Yang, Y., Chen, H., Ma, H., and Tan, Y. (2024). Effects of different psychosocial interventions on death anxiety in patients: a network meta-analysis of randomized controlled trials. Front. Psychol. 15:1362127. doi: 10.3389/fpsyg.2024.1362127
Luo, L., Song, N., Yang, H., Huang, J., Zhou, L., and Zhang, L. (2021). Intervention effect of long-term aerobic training on anxiety, depression, and sleep quality of middle school students with depression after COVID-19. Front. Psych. 12:720833. doi: 10.3389/fpsyt.2021.720833
Manzar, M. D., Moiz, J. A., Zannat, W., Spence, D. W., Pandi-Perumal, S. R., BaHammam, A. S., et al. (2015). Validity of the Pittsburgh sleep quality index in Indian university students. Oman Med. J. 30, 193–202. doi: 10.5001/omj.2015.41
McKenna, S. G., Donnelly, A., Esbensen, B. A., Comber, L., Ng, W. L., Anjum, A. M., et al. (2021). The feasibility of an exercise intervention to improve sleep (time, quality and disturbance) in people with rheumatoid arthritis: a pilot RCT. Rheumatol. Int. 41, 297–310. doi: 10.1007/s00296-020-04760-9
Medic, G., Wille, M., and Hemels, M. E. (2017). Short-and long-term health consequences of sleep disruption. Nature Sci. Sleep 9, 151–161. doi: 10.2147/NSS.S134864
Mercier, J., Ivers, H., and Savard, J. (2018). A non-inferiority randomized controlled trial comparing a home-based aerobic exercise program to a self-administered cognitive-behavioral therapy for insomnia in cancer patients. Sleep 41:zsy 149. doi: 10.1093/sleep/zsy149
Mikula, P., Timkova, V., Linkova, M., Vitkova, M., Szilasiova, J., and Nagyova, I. (2020). Fatigue and suicidal ideation in people with multiple sclerosis: the role of social support. Front. Psychol. 11:504. doi: 10.3389/fpsyg.2020.00504
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 4, 1–9. doi: 10.1186/2046-4053-4-1
Mollayeva, T., Thurairajah, P., Burton, K., Mollayeva, S., Shapiro, C. M., and Colantonio, A. (2016). The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep Med. Rev. 25, 52–73. doi: 10.1016/j.smrv.2015.01.009
Moosavi-Movahedi, A. A., Moosavi-Movahedi, F., and Yousefi, R. (2021). Good sleep as an important pillar for a healthy life. Rational. Scient. Lifestyle Health, 167–195. doi: 10.1007/978-3-030-74326-0_10
Morrison, M., Halson, S. L., Weakley, J., and Hawley, J. A. (2022). Sleep, circadian biology and skeletal muscle interactions: implications for metabolic health. Sleep Med. Rev. 66:101700. doi: 10.1016/j.smrv.2022.101700
Mudano, A. S., Tugwell, P., Wells, G. A., and Singh, J. A. (2019). Tai chi for rheumatoid arthritis. Cochrane Database Syst. Rev. 9:4849. doi: 10.1002/14651858.CD004849.pub2
Mustian, K. M., Sprod, L. K., Janelsins, M., Peppone, L. J., Palesh, O. G., Chandwani, K., et al. (2013). Multicenter, randomized controlled trial of yoga for sleep quality among cancer survivors. J. Clin. Oncol. 31, 3233–3241. doi: 10.1200/JCO.2012.43.7707
Ng, S.-M., Yin, M. X., Chan, J. S., Chan, C. H., Fong, T. C., Li, A., et al. (2022). Impact of mind–body intervention on proinflammatory cytokines interleukin 6 and 1β: a three-arm randomized controlled trial for persons with sleep disturbance and depression. Brain Behav. Immun. 99, 166–176. doi: 10.1016/j.bbi.2021.09.022
Nguyen, M. H., and Kruse, A. (2012). A randomized controlled trial of tai chi for balance, sleep quality and cognitive performance in elderly Vietnamese. Clin. Interv. Aging 7, 185–190. doi: 10.2147/CIA.S32600
Ohayon, M., Wickwire, E. M., Hirshkowitz, M., Albert, S. M., Avidan, A., Daly, F. J., et al. (2017). National Sleep Foundation's sleep quality recommendations: first report. Sleep Health 3, 6–19. doi: 10.1016/j.sleh.2016.11.006
Ohida, T., Osaki, Y., Doi, Y., Tanihata, T., Minowa, M., Suzuki, K., et al. (2004). An epidemiologic study of self-reported sleep problems among Japanese adolescents. Sleep 27, 978–985. doi: 10.1093/sleep/27.5.978
Oliveira, C., Simões, M., Carvalho, J., and Ribeiro, J. (2012). Combined exercise for people with type 2 diabetes mellitus: a systematic review. Diabetes Res. Clin. Pract. 98, 187–198. doi: 10.1016/j.diabres.2012.08.004
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. J. Clin. Epidem. 134, 178–189. doi: 10.1136/bmj.n71
Panel, C. C., Watson, N. F., Badr, M. S., Belenky, G., Bliwise, D. L., Buxton, O. M., et al. (2015). Joint consensus statement of the American Academy of sleep medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussion. J. Clin. Sleep Med. 11, 931–952. doi: 10.5664/jcsm.4950
Paruthi, S., Brooks, L. J., D'Ambrosio, C., Hall, W. A., Kotagal, S., Lloyd, R. M., et al. (2016). Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of sleep medicine. J. Clin. Sleep Med. 12, 785–786. doi: 10.5664/jcsm.5866
Pickersgill, J. W., Turco, C. V., Ramdeo, K., Rehsi, R. S., Foglia, S. D., and Nelson, A. J. (2022). The combined influences of exercise, diet and sleep on neuroplasticity. Front. Psychol. 13:831819. doi: 10.3389/fpsyg.2022.831819
Plante, G. E. (2006). Sleep and vascular disorders. Metabolism 55, S45–S49. doi: 10.1016/j.metabol.2006.07.013
Rios, P., Cardoso, R., Morra, D., Nincic, V., Goodarzi, Z., Farah, B., et al. (2019). Comparative effectiveness and safety of pharmacological and non-pharmacological interventions for insomnia: an overview of reviews. Syst. Rev. 8, 281–216. doi: 10.1186/s13643-019-1163-9
Salanti, G., Ades, A., and Ioannidis, J. P. (2011). Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J. Clin. Epidemiol. 64, 163–171. doi: 10.1016/j.jclinepi.2010.03.016
Santos, R. D., Viana, V., Boscolo, R., Marques, V., Santana, M., Lira, F., et al. (2012). Moderate exercise training modulates cytokine profile and sleep in elderly people. Cytokine 60, 731–735. doi: 10.1016/j.cyto.2012.07.028
Schroeck, J. L., Ford, J., Conway, E. L., Kurtzhalts, K. E., Gee, M. E., Vollmer, K. A., et al. (2016). Review of safety and efficacy of sleep medicines in older adults. Clin. Ther. 38, 2340–2372. doi: 10.1016/j.clinthera.2016.09.010
Senna, S. M., Ferraz, J. C. Jr., and Leandro, C. G. (2015). Perinatal malnutrition and the protective role of the physical training on the immune system. Nutr. Hosp. 32, 967–976. doi: 10.3305/nh.2015.32.3.9041
Serrano-Guzman, M., Valenza-Pena, C. M., Serrano-Guzman, C., Aguilar-Ferrandiz, E., Valenza-Demet, G., and Villaverde-Gutierrez, C. (2016). Effects of a dance therapy programme on quality of life, sleep and blood pressure in middle-aged women: a randomised controlled trial. Medicina Clínica 147, 334–339. doi: 10.1016/j.medcle.2016.11.016
Shen, W.-C., and Chen, C.-H. (2021). Effects of non-supervised aerobic exercise on sleep quality and maternal-fetal attachment in pregnant women: a randomized controlled trial. Complement. Ther. Med. 57:102671. doi: 10.1016/j.ctim.2021.102671
Singh, N. A., Clements, K. M., and Fiatarone, M. A. (1997). A randomized controlled trial of the effect of exercise on sleep. Sleep 20, 95–101. doi: 10.1093/sleep/20.2.95
Siu, P. M., Angus, P. Y., Tam, B. T., Chin, E. C., Doris, S. Y., Chung, K.-F., et al. (2021). Effects of tai chi or exercise on sleep in older adults with insomnia: a randomized clinical trial. JAMA Netw. Open 4:e2037199. doi: 10.1001/jamanetworkopen.2020.37199
Song, J., Wei, L., Cheng, K., Lin, Q., Xia, P., Wang, X., et al. (2022). The effect of modified tai chi exercises on the physical function and quality of life in elderly women with knee osteoarthritis. Front. Aging Neurosci. 14:860762. doi: 10.3389/fnagi.2022.860762
Song, D., Yu, D., Liu, T., and Wang, J. (2024). Effect of an aerobic dancing program on sleep quality for older adults with mild cognitive impairment and poor sleep: a randomized controlled trial. J. Am. Med. Dir. Assoc. 25, 494–499. doi: 10.1016/j.jamda.2023.09.020
Souza, A. K. F., Dornelas de Andrade, A., de Medeiros, A. I. C., de Aguiar, M. I. R., Rocha, T. D. D. S., Pedrosa, R. P., et al. (2018). Effectiveness of inspiratory muscle training on sleep and functional capacity to exercise in obstructive sleep apnea: a randomized controlled trial. Sleep Breath 22, 631–639. doi: 10.1007/s11325-017-1591-5
Streatfeild, J., Smith, J., Mansfield, D., Pezzullo, L., and Hillman, D. (2021). The social and economic cost of sleep disorders. Sleep 44:zsab132. doi: 10.1093/sleep/zsab132
Stricker, P. R., Faigenbaum, A. D., McCambridge, T. M., LaBella, C. R., Brooks, M. A., Canty, G., et al. (2020). Resistance training for children and adolescents. Pediatrics 145:1011. doi: 10.1542/peds.2020-1011
Stutz, J., Eiholzer, R., and Spengler, C. M. (2019). Effects of evening exercise on sleep in healthy participants: a systematic review and meta-analysis. Sports Med. 49, 269–287. doi: 10.1007/s40279-018-1015-0
Suna, J. M., Mudge, A., Stewart, I., Marquart, L., O’Rourke, P., and Scott, A. (2015). The effect of a supervised exercise training programme on sleep quality in recently discharged heart failure patients. Eur. J. Cardiovasc. Nurs. 14, 198–205. doi: 10.1177/1474515114522563
Sys, J., Van Cleynenbreugel, S., Deschodt, M., Van der Linden, L., and Tournoy, J. (2020). Efficacy and safety of non-benzodiazepine and non-Z-drug hypnotic medication for insomnia in older people: a systematic literature review. Eur. J. Clin. Pharmacol. 76, 363–381. doi: 10.1007/s00228-019-02812-z
Tanaka, H., Taira, K., Arakawa, M., Urasaki, C., Yamamoto, Y., Okuma, H., et al. (2002). Short naps and exercise improve sleep quality and mental health in the elderly. Psychiatry Clin. Neurosci. 56, 233–234. doi: 10.1046/j.1440-1819.2002.00995.x
Tang, M.-F., Liou, T.-H., and Lin, C.-C. (2010). Improving sleep quality for cancer patients: benefits of a home-based exercise intervention. Support. Care Cancer 18, 1329–1339. doi: 10.1007/s00520-009-0757-5
Taylor-Piliae, R. E., and Coull, B. M. (2012). Community-based Yang-style tai chi is safe and feasible in chronic stroke: a pilot study. Clin. Rehabil. 26, 121–131. doi: 10.1177/0269215511419381
Tonin, F. S., Rotta, I., Mendes, A. M., and Pontarolo, R. (2017). Network meta-analysis: a technique to gather evidence from direct and indirect comparisons. Pharmacy Practice 15:943. doi: 10.18549/PharmPract.2017.01.943
Trinder, J. (2012). Cardiac activity and sympathovagal balance during sleep. Sleep Med. Clin. 7, 507–516. doi: 10.1016/j.jsmc.2012.06.012
Tseng, T.-H., Chen, H.-C., Wang, L.-Y., and Chien, M.-Y. (2020). Effects of exercise training on sleep quality and heart rate variability in middle-aged and older adults with poor sleep quality: a randomized controlled trial. J. Clin. Sleep Med. 16, 1483–1492. doi: 10.5664/jcsm.8560
Tworoger, S. S., Yasui, Y., Vitiello, M. V., Schwartz, R. S., Ulrich, C. M., Aiello, E. J., et al. (2003). Effects of a yearlong moderate-intensity exercise and a stretching intervention on sleep quality in postmenopausal women. Sleep 26, 830–836. doi: 10.1093/sleep/26.7.830
Vandekerckhove, M., and Wang, Y.-L. (2018). Emotion, emotion regulation and sleep: an intimate relationship. AIMS Neurosci. 5, 1–17. doi: 10.3934/Neuroscience.2018.1.1
Vats, D., Flegal, J. M., and Jones, G. L. (2019). Multivariate output analysis for Markov chain Monte Carlo. Biometrika 106, 321–337. doi: 10.1093/biomet/asz002
Viswanathan, V., Sivakumar, S., Prathiba, A. S., Devarajan, A., George, L., and Kumpatla, S. (2021). Effect of yoga intervention on biochemical, oxidative stress markers, inflammatory markers and sleep quality among subjects with type 2 diabetes in South India: results from the SATYAM project. Diabetes Res. Clin. Pract. 172:108644. doi: 10.1016/j.diabres.2020.108644
Wang, X. Q., Pi, Y. L., Chen, P. J., Liu, Y., Wang, R., Li, X., et al. (2016). Traditional chinese exercise for cardiovascular diseases: systematic review and meta-analysis of randomized controlled trials. J. Am. Heart Assoc. 5:e002562. doi: 10.1161/JAHA.115.002562
Wang, W., Sawada, M., Noriyama, Y., Arita, K., Ota, T., Sadamatsu, M., et al. (2010). Tai chi exercise versus rehabilitation for the elderly with cerebral vascular disorder: a single-blinded randomized controlled trial. Psychogeriatrics 10, 160–166. doi: 10.1111/j.1479-8301.2010.00334.x
Wenzel, J. A., Griffith, K. A., Shang, J., Thompson, C. B., Hedlin, H., Stewart, K. J., et al. (2013). Impact of a home-based walking intervention on outcomes of sleep quality, emotional distress, and fatigue in patients undergoing treatment for solid tumors. Oncologist 18, 476–484. doi: 10.1634/theoncologist.2012-0278
White, I. R., Barrett, J. K., Jackson, D., and Higgins, J. P. (2012). Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Res. Synth. Methods 3, 111–125. doi: 10.1002/jrsm.1045
Wu, W.-W., Kwong, E., Lan, X.-Y., and Jiang, X.-Y. (2015). The effect of a meditative movement intervention on quality of sleep in the elderly: a systematic review and meta-analysis. J. Altern. Complement. Med. 21, 509–519. doi: 10.1089/acm.2014.0251
Xie, Y., Liu, S., Chen, X.-J., Yu, H.-H., Yang, Y., and Wang, W. (2021). Effects of exercise on sleep quality and insomnia in adults: a systematic review and meta-analysis of randomized controlled trials. Front. Psych. 12:664499. doi: 10.3389/fpsyt.2021.664499
Xie, X., Xu, Y., Wang, R., Lei, X., and Yu, J. (2022). Wake after sleep onset time moderated age-related emotional memory bias. Exp. Aging Res. 48, 362–372. doi: 10.1080/0361073X.2021.1985359
Ye, J., Jia, X., Zhang, J., and Guo, K. (2022). Effect of physical exercise on sleep quality of college students: chain intermediary effect of mindfulness and ruminative thinking. Front. Psychol. 13:987537. doi: 10.3389/fpsyg.2022.987537
Yeh, S.-C. J., and Chang, M.-Y. (2012). The effect of qigong on menopausal symptoms and quality of sleep for perimenopausal women: a preliminary observational study. J. Altern. Complement. Med. 18, 567–575. doi: 10.1089/acm.2011.0133
Yeung, A., Chan, J. S., Cheung, J. C., and Zou, L. (2018). Qigong and tai-chi for mood regulation. Focus 16, 40–47. doi: 10.1176/appi.focus.20170042
Yilmaz Gokmen, G., Akkoyunlu, M. E., Kilic, L., and Algun, C. (2019). The effect of T'ai chi and Qigong training on patients with obstructive sleep apnea: a randomized controlled study. J. Altern. Complement. Med. 25, 317–325. doi: 10.1089/acm.2018.0197
Zeibig, J.-M., Seiffer, B., Sudeck, G., Rösel, I., Hautzinger, M., and Wolf, S. (2021). Transdiagnostic efficacy of a group exercise intervention for outpatients with heterogenous psychiatric disorders: a randomized controlled trial. BMC Psychiatry 21:313. doi: 10.1186/s12888-021-03307-x
Zhao, H., Lu, C., and Yi, C. (2023). Physical activity and sleep quality association in different populations: a meta-analysis. Int. J. Environ. Res. Public Health 20:1864. doi: 10.3390/ijerph20031864
Zhou, Y., Wu, W., Zou, Y., Huang, W., Lin, S., Ye, J., et al. (2022). Benefits of different combinations of aerobic and resistance exercise for improving plasma glucose and lipid metabolism and sleep quality among elderly patients with metabolic syndrome: a randomized controlled trial. Endocr. J. 69, 819–830. doi: 10.1507/endocrj.EJ21-0589
Keywords: exercise, sleep, sleep quality, randomized controlled trial, network meta-analysis
Citation: Li L, Wang C, Wang D, Li H, Zhang S, He Y and Wang P (2024) Optimal exercise dose and type for improving sleep quality: a systematic review and network meta-analysis of RCTs. Front. Psychol. 15:1466277. doi: 10.3389/fpsyg.2024.1466277
Edited by:
Chong Chen, Yamaguchi University Graduate School of Medicine, JapanReviewed by:
Teresa Bento, Polytechnic Institute of Santarém, PortugalPéter Przemyslaw Ujma, Semmelweis University, Hungary
Copyright © 2024 Li, Wang, Wang, Li, Zhang, He and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuanchun He, aGV5dWFuY2h1bkBocmJpcGUuZWR1LmNu; Ping Wang, d2FuZ3BpbmdAaHJiaXBlLmVkdS5jbg==
 Li Li
Li Li Chunxiao Wang2
Chunxiao Wang2 Hua Li
Hua Li