- 1School of Nursing and Health, Zhengzhou University, Zhengzhou, China
- 2Department of Neurology, First Affiliated Hospital of Zhengzhou University, Zhengzhou, China
Introduction: As stroke patients may have impaired motor function, there may have increased sedentary behavior. Factors associated with sedentary behavior need to be explored to develop targeted interventions. Although studies explore the effects of exercise self-efficacy and perceived social support on sedentary behavior, the relationship is not clear. The aim of this study was to explore the mediating effect of exercise self-efficacy on perceived social support and objective measured sedentary behavior in stroke patients.
Methods: The random sampling method was adopted to select 275 stroke patients from the neurology department of a third-grade hospital of Henan Province from June 2023 to March 2024 in a cross-sectional descriptive study. A general data questionnaire, exercise self-efficacy scale, perceived social support scale, and ActiGraph GT3X accelerometer were used to investigate. The structural equation model was used to analyze the mediating effect of exercise self-efficacy between perceived social support and sedentary behavior.
Results: The mean sedentary behavior time in stroke patients in this study was (479.65 ± 112.65) min, the mean score of perceived social support was (47.53 ± 17.16), and the mean score of exercise self-efficacy was (24.19 ± 6.25). The correlation analysis revealed that, the sedentary behavior of stroke patients was negatively correlated with exercise self-efficacy and perceived social support. The results of the mediation analysis showed that exercise self-efficacy played a partial mediating role between perceived social support and sedentary behavior.
Conclusion: Perceived social support and exercise self-efficacy were influential factors in sedentary behavior. Moreover, the impact of perceived social support on sedentary behavior was partially mediated by exercise self-efficacy. Therefore, to decrease the sedentary behavior, it is crucial to improve the level of perceived social support in stroke patients. Patients with less perceived social support can improve their exercise self-efficacy and thus perceive more social support.
Introduction
Stroke is a prevalent chronic illness that poses a severe threat to human health, which is characterized by high rates of incidence, recurrence, mortality, disability, and disease burden. Globally, stroke is currently the second leading cause of death and long-term disability (Tsao et al., 2023), with more than 400,000 survivors living with complications (Krueger et al., 2015).
Stroke affects 1,115 individuals per 100,000 in China, with a mortality rate of 115 per 100,000, and over 2 million new cases are reported annually. Nearly 50% of stroke patients exhibit motor dysfunction after a stroke (Einstad et al., 2021). The incidence of stroke is significantly affected by a multitude of factors, encompassing behavioral, psychological, and socio-environmental elements. Among these, behavioral risk factors, notably sedentary behavior, contribute substantially to the rising prevalence of chronic diseases (O'Donnell et al., 2010).
Sedentary behavior (SB) is recognized behavioral factors critical for health (Sabia et al., 2022). Sedentary behavior, also known as static behavior, refers to the consumption of 1.5 metabolic equivalents (METs) in any awake state, including all sitting, reclining or lying, using electronic devices, writing, reading, talking and driving (Tremblay et al., 2017). SB causes many health problems and has been shown to be independently associated with cardiovascular-related mortality (Bull et al., 2020), disease morbidity (Biswas et al., 2015), hospitalization rates (Biswas et al., 2015), metabolic syndrome (Palmer et al., 2019), diabetes (Bull et al., 2020), cognitive function (Falck et al., 2017), and poorer mental health (Hallgren et al., 2018). In addition, stroke patients are the least active population of all cardiovascular and cerebrovascular patients (Ezeugwu and Manns, 2017), and about three-quarters of their waking time is spending in SB (English et al., 2016). Thus, SB in stroke patients should be valued.
Reduction and interruption of SB can improve the health indicators such as waist circumference, blood glucose level, insulin level, and body mass index, which is of positive significance for improving the quality of life (Healy et al., 2015). Current guidelines state that adults should spend < 8 h of SB per day (Piercy and Troiano, 2018). However, existing studies have found that SB in stroke patients does not meet the guideline requirements. Scholars Sjöholm et al. (2014) and Barrett et al. (2018) investigated hospitalized stroke patients and found that 74% and 86.9% of their daily time were sedentary, respectively. Wondergem et al. (2019) found that stroke patients spend an average of 9.3 h on SB per day. All the above studies show that stroke patients have too long SB, how to decrease the level of SB in stroke patients is the key. However, stroke survivors have many problems (Hamre et al., 2021), such as limbs disturbance, which makes it difficult for patients to complete SB recommended by the guidelines. Stroke prevention and treatment are facing bottlenecks, so it is crucial to explore how to reduce the sedentary behavior of stroke patients.
Previous studies have shown that various factors, including perceived social support (Northcott et al., 2016) and exercise self-efficacy (Wen et al., 2018), play a significant role in influencing the SB of patients who had a stroke. Perceived social support is a significant impact factor on health behavior (Blanton et al., 2019). It is widely recognized that social support constitutes an interactive process that encompasses both the provision and receipt of assistance. Crucially, for social support to be effective, it must be perceived as such by the individuals receiving it (Northcott et al., 2016). Studies (Kruithof et al., 2013; Holder et al., 2023) have shown that individuals who feel encouraged, understood, and supported by their social networks are more inclined to adopt and maintain healthy behaviors, including physical activity. Hall et al. (2020)'s study highlights the willingness of stroke patients to reduce SB with appropriate support from caregivers and professionals, and the Choi et al. (2022) study found that stroke patients who were married and lived with their spouse were less likely to tend to have SB. It can be seen that perceived social support is an important influencing factor of SB in stroke patients. Therefore, we propose hypothesis (a), perceived social support is negatively associated with SB.
Psychological aspects, such as exercise self-efficacy, were reported to have an effect on exercise (Trost et al., 2002). Self-efficacy, a central tenet of social cognitive theory, refers to the “belief in one's capabilities to organize and execute the courses of action required to manage given situations” (Bandura, 1977). It has been reported that a high level of exercise self-efficacy can predict the start and sustenance of exercise over time in patients with stroke (Nicholson et al., 2014), while low self-efficacy is the strongest barrier to behavior change in stroke patients (Mirkarimi et al., 2017). Wondergem et al. (2019) found that patients with higher self-efficacy had shorter time spending on SB. After stroke, short exercise cannot make patients see the effect of physical rehabilitation, resulting in low exercise self-efficacy and the increase of SB. Therefore, we propose hypothesis (b), exercise self-efficacy is negatively associated with SB.
Social cognitive theory (SCT) (Bandura, 2001) was constructed in 1986 by American psychologist Bandura. SCT posits that behavior is shaped by a combination of individual and environmental factors, which in turn influence changes in health-related behaviors. In our research, sedentary behavior was regarded as a key behavioral factor. For stroke patients, a high level of perceived social support can bolster their confidence in resuming a normal life. Concurrently, companionship and support can modulate the patients' negative emotions, sustain a stable psychological state, and enhance their self-efficacy, thereby potentially reducing sedentary behavior. Consequently, it is justifiable to adopt SCT as the theoretical framework for our study. Although studies have been conducted to explore the link between self-efficacy and social support and SB, the mechanisms underlying these three variables are unclear and require further research. According to the SCT, we propose hypothesis (c), the perceived social support on SB was partly mediated by exercise self-efficacy.
In summary, SB was hypothesized to be related to exercise self-efficacy and perceived social support, and that exercise self-efficacy may be a potential mediator between perceived social support and SB. This study aimed to quantify the levels of SB, exercise self-efficacy and perceived social support in stroke patients and to explore the potential relationship between SB and exercise self-efficacy and perceived social support. The results would provide a theoretical basis for developing interventions to improve SB in such patients.
Methods
Design
A descriptive cross-sectional design was utilized in this study, which followed the guidelines of the Strengthening Reports of Observational Studies in Epidemiology (STROBE) for cross-sectional studies.
Participants
In this study, the convenience sampling method was used to select the research subjects in the department of Neurology of the First Affiliated Hospital of Zhengzhou University. Data were collected over a period spanning from June 2023 to March 2024. Participants were eligible for the study if they met the following inclusion criteria: (a) diagnosis of stroke, (b) age 18 years or older, (c) absence of cognitive dysfunction, as evidenced by a Montreal Cognitive Assessment (MoCA) score of 26 or higher; (d) consent from patients and their families to wear a Actigraph GT3X accelerometer following discharge from the hospital. Subjects were excluded from the study if they: (a) suffered from severe heart failure, respiratory failure, cancer, or were in other terminal stages of illness; (b) did not wear the triaxial accelerometer for a minimum of 3 valid days per week.
Questionnaire data collection
The self-report questionnaires, including demographic and clinical information, exercise self-efficacy scale and perceived social support scale were used to complete the data collection. Before data collection begins, uniform training was conducted to ensure homogeneous object selection and reduce sample selection errors. First, the patients were screened according to the admission cases, and then patients are comprehensively evaluated to select patients who meet the criteria. Guiding language were used during the design of the questionnaire to facilitate patients to understand the questionnaire requirements, informing participants of the purpose of the study and the right not to participate or to withdraw from the survey at any time. Before discharge, paper questionnaires were distributed on-site, and the participants were asked to complete the questionnaires according to their actual situations. The average time to complete the questionnaire was approximately 25 min. In the data entry, the form of two-person entry should be adopted, and the incomplete data should be removed to ensure the accuracy of the data. A total of 280 questionnaires were distributed, with 275 valid questionnaires, achieving a valid recovery rate of 98.21%.
Tools
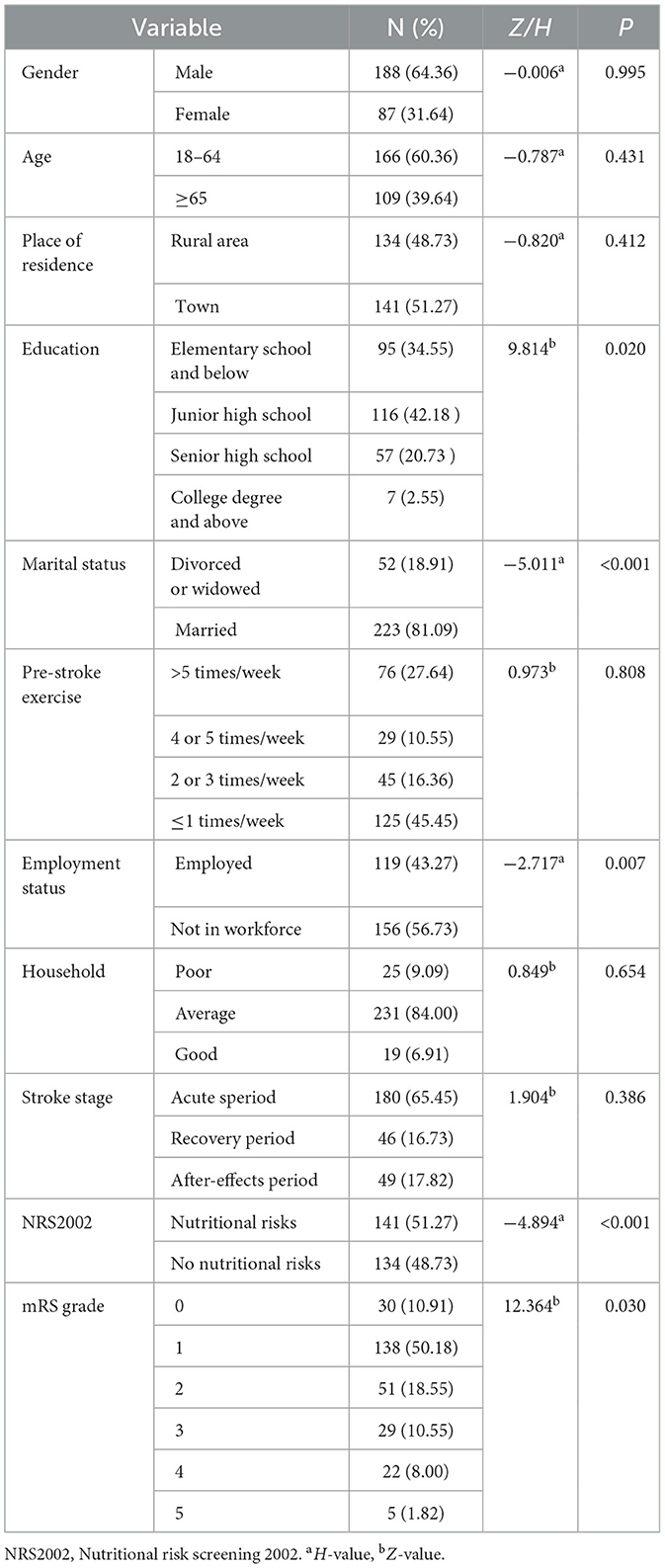
Demographic and clinical information
The demographic information included age, gender, place of residence, education, marital status, physical activity before stroke, work status, and household, etc. Meanwhile, health specifics like the Nutritional Risk Screening 2002 (NRS2002), stroke stage, and the modified Rankin scale were collected from electronic health records of the patients.
Perceived social support scale
The PSSS is an instrument to measure the individual's self-perception of multidimensional social support. The scale was developed by Zimet et al. (1990) in 1987. The 12-item scale is designed to evaluate the level of support an individual perceives from family, friends, and others. The highest score of this 7-point Likert-type scale is 84, and higher scores mean better perceived social support. The Cronbach's alpha value of PSSS is 0.92. This scale has been applied to patients who had a stroke in other studies (Dong et al., 2022; Wang et al., 2019).
Exercise self-efficacy scale
The Exercise Self-Efficacy Scale, a self-reported scale invented by Kroll et al. (2007), measures self-efficacy to perform exercise in spite of numerous difficult situations. The scale is designed to assess individuals' confidence in their ability to engage in exercise a minimum of three times per week despite potential challenges. It encompasses 10 items and employs a 4-point Likert scoring system, with scores ranging from 10 to 40 points. The Cronbach's a coefficient of the Chinese ESES scale was 0.879 (P < 0.01), and the split-half reliability coefficient of the scale was r = 0.858 (P < 0.01). The test-retest reliability was 0.657 (P < 0.01) (Dong et al., 2016).
Accelerometry measurement
Participants were instructed to wear the ActiGraph GT3X (Pensacola, FL, USA) on the left wrist (if the left wrist was affected by stroke, the right wrist was selected) on the day of discharge and for 7 consecutive days at a time outside of any aquatic activity. They were set to record three axes of acceleration (e.g., vertical, anterior-posterior and medium-lateral) at 30 Hz (30 times per s) with data smoothed using 1 s epochs. When receiving the accelerometer, participants were shown and carefully instructed, verbally and in writing, on how to properly wear and handle the ActiGraph GT3X accelerometer.
Raw accelerometer data (activity counts) were downloaded via ActiLife software (v 6.13.4, ActiGraph, Pensacola, FL, USA) for processing. Requirements for participants' data to be included in the analyses implied 3 valid days out of the 7-day period, with ≥480 min of wear time each day (English et al., 2016; Troiano et al., 2008; Joseph et al., 2020), given that 3-day accelerometer data have proved valid and reliable when measuring free-living sedentary behavior (English et al., 2018; Hendrickx et al., 2019). In addition, accelerometer non-wear time was defined as periods of ≥90 min of consecutive zeroes and were not included in the analysis (Choi et al., 2011). In agreement with previous research work about actigraphy in stroke population and elders (English et al., 2016; Troiano et al., 2008; Choi et al., 2011), Freedson et al. (1998)'s cut-points were applied to the data to classify SB intensity as ≤ 99 counts/min. Participants were excluded from the analysis if they did not meet valid wear criteria (Freedson et al., 1998).
Ethical considerations
The study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University (2022-KY-1157-002). The study followed the principles of anonymity and confidentiality, and informed consent was obtained from the participants.
Data analysis
The SPSSAU software V.21was used to analyze the data. Count data were described by frequency and composition ratio, whereas measurement data were described by ± SD and compared between groups using independent samples t-test and one-way ANOVA. The measurement data that did not conform to a normal distribution were described by median and quartiles, and the Mann–Whitney U test and Kruskal–Wallis H test were used for comparison between groups. Pearson correlation analysis was used to analyze the interrelationships between the three variables. The pathways of action among perceived social support, exercise self-efficacy, and sedentary behavior were analyzed using SPSSAU, and indirect effects were estimated by the bootstrap resampling method with 5,000 replicate samples, and 95% confidence intervals (CI) were calculated. A mediating effect was considered significant if the 95% CI did not include zero. P < 0.05 (two-sided test) was considered statistically significant.
Results
Participant characteristics
A total of 275 participants successfully completed the data collection, resulting in a questionnaire response rate of 98.21%, as outlined in Table 1. The demographic composition of the participants was primarily male (64.36%), with a significant majority being married (81.09%), over half were unemployed (56.73%), and most mRS ratings were rated at level 1 (50.18%). In addition, participants had the most exercise once a week before the illness (45.45%), and most of them were in the acute phase of stroke (65.45). Detailed information of the sample population can be found in Table 1.
Correlation analysis between variables
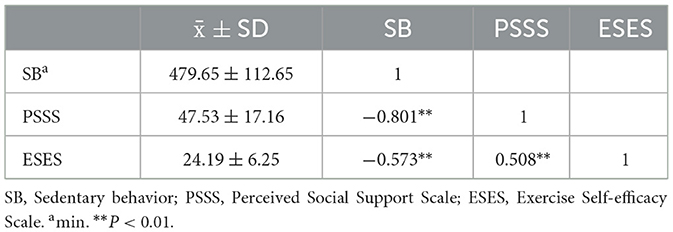
The results of this study showed that all three variables, SB, PSSS, and ESES were correlated with each other. The mean SB time in stroke patients in this study was (479.65 ± 112.65) minutes, the average effective wear duration was (1,026.42 ± 165.85) minutes (see in Supplementary Table S1), while the mean score of PSSS was (47.53 ± 17.16), and the mean score of ESES was (24.19 ± 6.25), as displayed in Table 2. The correlation analysis is shown in Table 2, where SB was negatively correlated with both PSSS (r = −0.801, P < 0.01) and ESES (r = −0.573, P < 0.01).
Intermediary analysis
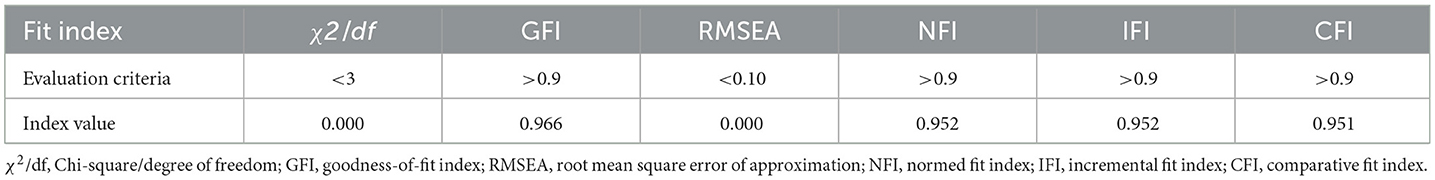
Building on our initial findings from the correlation analysis, we next performed mediation analysis to explore the potential association underlying the relationship between a stroke patient's SB, PSSS, and ESES. PSSS was set as the independent variable, with ESES as the mediating variable and SB as the dependent variable, and path analysis was used to fit the hypothetical model. The model fitting results revealed that the chi-squared degrees of freedom ratio showed a good model fit, with the chi-square freedom ratio (χ2/df) = 0.000, the fitness index (GFI) = 0.966, the benchmarked fitness index (NFI) = 0.952, the comparative fitness index (CFI) = 0.951, and the asymptotic residual mean square and root square (RMSEA) = 0.000, as detailed in Table 3 and Figure 1.
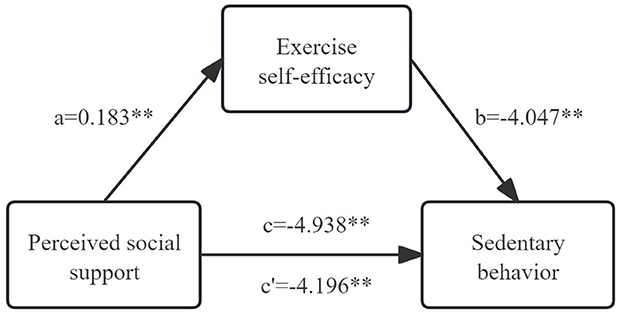
Figure 1. Mediating effect of exercise self-efficacy between perceived social support and sedentary behavior. a, effect of perceived social support on self-efficacy; b, effect of self-efficacy on sedentary behavior; c, total effect of perceived social support on sedentary behavior; c', direct effect of perceived social support on sedentary behavior. **p < 0.01.
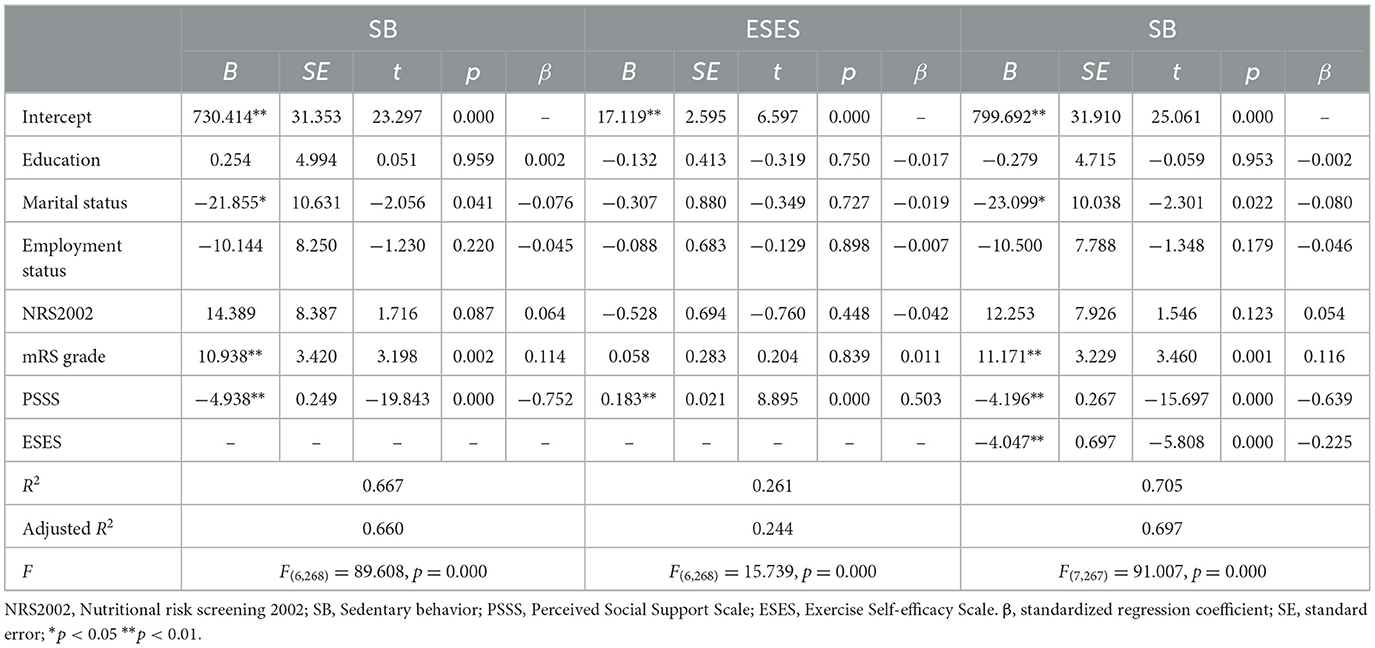
We controlled for some factors (such as education, marital status, employment status, NRS2002 and mRS) which are considered important predictors that affect SB in patients with stroke. The results showed that PSSS predicted exercise self-efficacy (β = 0.183, t = 8.895, p < 0.001), and ESES significantly predicted SB (β = −4.047, t = −5.808, p < 0.001). Meanwhile, PSSS had a direct effect on SB was also significant (β = −4.196, t = −15.697, p < 0.001), but the comparison of the effect coefficients showed that the effect of PSSS on SB was diminished from −4.938 to −4.196, which meant that ESES partially mediated the effect between PSSS and SB, as shown in Table 4.
Discussion
Understanding the mediators of the relationship between PSSS and ESES is crucial for developing strategies to reduce SB in stroke patients. Previous studies have only explored the relationship between SB, PSSS, and ESES separately, but ESES has been neglected as a mediator. This study confirmed our hypothesis, revealing a negative association between PSSS and ESES and SB. More importantly, ESES partly mediated the relationship between PSSS and SB. Our findings provide directions for the development of interventions to manage SB in such patients.
We found that the daily SB in stroke patients was 479.65 ± 112.65 min, nearly 8 h a day, that is, higher levels of SB in stroke patients, which is consistent with previous findings (Sjöholm et al., 2014; Barrett et al., 2018). Some stroke patients have problems of limb dysfunction after illness, especially those with impaired lower limb function, with longer SB. This suggests that further research and focus on SB and its influencing factors in stroke patients are urgently needed to lay the basis for subsequent designation of SB-related interventions. In this study, the average PSSS score was 47.53 ± 17.16, which means in a medium social support state. In other words, the social support for stroke patients is generally at a low or moderate level. Our study also found that the degree of PSSS in stroke patients was negatively associated with SB (r = −0.801, P < 0.01), which is consistent with our study hypothesis. We speculate that the reason for this result is that most stroke patients will leave physical disorders, which will affect the normal activities, and the accompanying support from relatives and friends can help patients to actively participate in rehabilitation exercise programs and promote the occurrence of healthy behaviors such as physical activity (Pauly et al., 2021). And the importance of social support is indicated in the existing studies, a cross-sectional study (Wen et al., 2022) enrolled 133 hypertensive stroke patients 6 months after discharge in China have shown the perceptions of chronic illness resources received from healthcare teams, family and friends, and the community were positively correlated with health behavior. Brouwer-Goossensen et al. (2021) have found social support was a positive factor in health behavior change in interviews with 18 patients who had a stroke. Therefore, perceived social support is an important factor in reducing SB in patients with stroke.
Our study suggests a negatively correlation between ESES and SB in patients with stroke, that is, stroke patients with higher levels of ESES have lower levels of SB. A higher level of self-efficacy can effectively change some's perception of the disease and improve psychological adaptation and the enthusiasm to participate in rehabilitation (Dong et al., 2022). However, the patients in this study had a mean ESES score of 24.19 ± 6.25, with longer SB. Most importantly, we found that SB appeared to correlate with health behavior via two pathways, a direct pathway and an indirect pathway mediated by ESES. High level of PSSS can improve patients' confidence to increase physical activity, regulate negative emotions with companionship and communication, and increase self-efficacy. Meanwhile, influenced by PSSS, they are more willing to seek help from others when ESES is low, which also promotes the reduction of SB.
Overall, our study found that PSSS was not only directly and negatively associated with the SB of patients with stroke, but also further related to SB via ESES. This was consistent with the connotation of the SCT (Bandura, 1978). In other words, our findings provided practical support for the SCT. That's to say, PSSS may influence patients' ESES and, in turn, their SB. Additionally, a positive correlation between PSSS and ESES has been shown, in order to reduce SB in stroke patients, we can start with both PSSS and ESES.
Strengths and limitations
The strengths of this study are as follows. Firstly, the main outcome of this paper, sedentary time, was measured by an objective accelerometer, which is more accurate and reliable than a questionnaire. Second, there have been many studies on the factors influencing sedentary behavior, which include the independent effects of exercise self-efficacy and social support. However, this study is the first time to consider the two together to verify the mediating role of exercise self-efficacy, which can be used as a breakthrough point in future intervention research to conduct a new form of intervention.
Nevertheless, the limitations of the study should be acknowledged. Firstly, owing to the cross-sectional design of this study and the application of mediation analysis, only correlations between the variables were demonstrated, while the causal relationships between perceived social support, exercise self-efficacy, and sedentary behavior could not be determined. A longitudinal study is needed to determine the causal relationship between the variables in the future. Secondly, this study used the convenience sampling technique, which may lead to some degree of bias. In future study planning, alternative sampling methods are recommended to reduce the possibility of bias. Thirdly, the subjects of this study came from one hospital, and could be sampled from multiple hospitals or communities in the future to increase the sample size of the study. Furthermore, SB in this study was affected by the accelerometer wear duration, although we considered the total wear duration and effective percentage, measurement bias should be considered in designing more rigorous experiments in future studies. Finally, most of the stroke patients included in this study were mild, which may cause some shift in the interpretation of the results, such as sedentary time may be less relative to severe patients.
Relevance to future research direction
The present study further confirms the high level of SB in stroke patients. As SB affects the prognosis of stroke patients and significantly impacts their recovery, elucidating the factors that contribute to SB and exploring measures to reduce SB is essential in stroke patients. The results of this study suggest that PSSS can indirectly influence SB in stroke patients due to the mediating role of ESES. On the basis of this study, future studies can be carried out in the following directions. First, the subjects of this study are stroke patients, and there are many people with SB in real life, such as hypertension patients and diabetes patients, so future studies can explore whether the conclusions of this study are applicable in other populations. Secondly, there are many intervention programs for sedentary behavior, and this study proposes the mediation role of exercise self-efficacy, which can provide some basis for the development of future intervention methods. Moreover, this study is a cross-sectional study, and a future longitudinal study design can be adopted to explore the causal relationship among the three variables. Finally, most of the stroke patients included in this study were mild and severe patients were excluded, and patients with different disease severity should be included in the future to provide a more comprehensive outcome.
Conclusion
In conclusion, this study shows that PSSS and ESES are key correlates of SB in stroke patients, and that after controlling for the effects of confounders, ESES partly mediates the relationship between PSSS and SB. This suggests that healthcare professionals should pay attention to the assessment of patient' ESES in their clinical work. Appropriate measures should be taken to increase patients' ESES, such as educating stroke patients about the disease, the disadvantages of SB and the benefits of increased physical activity. Encourage patients to actively participate in social life, face the disease with a positive attitude, and reduce negative emotions, which is important to reduce SB.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JW: Data curation, Investigation, Writing – original draft, Writing – review & editing. FY: Data curation, Investigation, Writing – original draft. XD: Data curation, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was supported by Medical Science and Technology project of Henan Province (LHGJ20220430) and Nursing Research Fund of the First Affiliated Hospital of Zhengzhou University (HLKY2023017).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1444214/full#supplementary-material
References
Bandura, A. (1977). Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 84, 191–215. doi: 10.1037/0033-295X.84.2.191
Bandura, A. (1978). The self system in reciprocal determinism. Psychology 33, 344–358. doi: 10.1037/0003-066X.33.4.344
Bandura, A. (2001). Social cognitive theory: an agentic perspective. Annu. Rev. Psychol. 52, 1–26. doi: 10.1146/annurev.psych.52.1.1
Barrett, M., Snow, J. C., Kirkland, M. C., Kelly, L. P., Gehue, M., Downer, M. B., et al. (2018). Excessive sedentary time during in-patient stroke rehabilitation. Top. Stroke Rehabil. 25, 366–374. doi: 10.1080/10749357.2018.1458461
Biswas, A., Oh, P. I., Faulkner, G. E., Bajaj, R. R., Silver, M. A., Mitchell, M. S., et al. (2015). Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann. Internal Med. 162, 123–132. doi: 10.7326/M14-1651
Blanton, S., Scheibe, D. C., Rutledge, A. H., Regan, B., and O'Sullivan, C. S. (2019). Family-centered care during constraint-induced therapy after chronic stroke: a feasibility study. Rehabilit. Nursing J. 44, 349–357. doi: 10.1097/rnj.0000000000000197
Brouwer-Goossensen, D., den Hertog, H. M., Mastenbroek-de Jong, M. A., van Gemert-Pijnen, L. J., and Taal, E. (2021). Patient perspectives on health-related behavior change after transient ischemic attack or ischemic stroke. Brain Behav. 11:e01993. doi: 10.1002/brb3.1993
Bull, F. C., Al-Ansari, S. S., Biddle, S., Borodulin, K., Buman, M. P., Cardon, G., et al. (2020). World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 54, 1451–1462. doi: 10.1136/bjsports-2020-102955
Choi, L., Liu, Z., and Matthews, C. E. (2011). Validation of accelerometer wear and nonwear time classification algorithm. Med. Sci. Sports Exer. 43:357. doi: 10.1249/MSS.0b013e3181ed61a3
Choi, Y. A., Lee, J. S., Park, J. H., and Kim, Y. H. (2022). Patterns of physical activity and sedentary behavior and their associated factors among nondisabled stroke survivors. Maturitas 158, 10–15. doi: 10.1016/j.maturitas.2021.11.009
Dong, X., Liu, Y., Wang, A., and Wang, M. (2016). The psychometric properties of Chinese version of SCI Exercise Self-Efficacy Scale in patients with stroke. Patient Prefer. Adherence. 10, 1235–1241. doi: 10.2147/PPA.S106938
Dong, X., Yang, S., Guo, Y., Lv, P., and Liu, Y. (2022). Exploring psychoneurological symptom clusters in acute stroke patients: a latent class analysis. J. Pain Res. 15, 789–799. doi: 10.2147/JPR.S350727
Einstad, M. S., Saltvedt, I., Lydersen, S., Ursin, M. H., Munthe-Kaas, R., Ihle-Hansen, H., et al. (2021). Associations between post-stroke motor and cognitive function: a cross-sectional study. BMC Geriatr. 21, 1–10. doi: 10.1186/s12877-021-02055-7
English, C., Healy, G. N., Coates, A., Lewis, L. K., Olds, T., Bernhardt, J., et al. (2016). Sitting time and physical activity after stroke: physical ability is only part of the story. Top. Stroke Rehabil. 23, 36–42. doi: 10.1179/1945511915Y.0000000009
English, C., Janssen, H., Crowfoot, G., Bourne, J., Callister, R., Dunn, A., et al. (2018). Frequent, short bouts of light-intensity exercises while standing decreases systolic blood pressure: Breaking Up Sitting Time After Stroke (BUST-Stroke) trial. Int. J. Stroke 13, 932–940. doi: 10.1177/1747493018798535
Ezeugwu, V. E., and Manns, P. J. (2017). Sleep duration, sedentary behavior, physical activity, and quality of life after inpatient stroke rehabilitation. J. Stroke Cerebrovasc. Dis. 26, 2004–2012. doi: 10.1016/j.jstrokecerebrovasdis.2017.06.009
Falck, R. S., Davis, J. C., and Liu-Ambrose, T. (2017). What is the association between sedentary behaviour and cognitive function? A systematic review. Br. J. Sports Med. 51, 800–811. doi: 10.1136/bjsports-2015-095551
Freedson, P. S., Melanson, E., and Sirard, J. (1998). Calibration of the computer science and applications, Inc. accelerometer. Med. Sci. Sports Exerc. 30, 777–781. doi: 10.1097/00005768-199805000-00021
Hall, J., Morton, S., Fitzsimons, C. F., Hall, J. F., Corepal, R., English, C., et al. (2020). Factors influencing sedentary behaviours after stroke: findings from qualitative observations and interviews with stroke survivors and their caregivers. BMC Public Health. 20:967. doi: 10.1186/s12889-020-09113-6
Hallgren, M., Owen, N., Stubbs, B., Zeebari, Z., Vancampfort, D., Schuch, F., et al. (2018). Passive and mentally-active sedentary behaviors and incident major depressive disorder: a 13-year cohort study. J. Affect. Disor. 241, 579–585. doi: 10.1016/j.jad.2018.08.020
Hamre, C., Fure, B., Helbostad, J. L., Wyller, T. B., Ihle-Hansen, H., Vlachos, G., et al. (2021). Factors associated with level of physical activity after minor stroke. J. Stroke Cerebrovasc. Dis. 30:105628. doi: 10.1016/j.jstrokecerebrovasdis.2021.105628
Healy, G. N., Winkler, E. A., Owen, N., and Anuradha, S. (2015). Replacing sitting time with standing or stepping: associations with cardio-metabolic risk biomarkers. Eur. Heart J. 36, 2643–2649. doi: 10.1093/eurheartj/ehv308
Hendrickx, W., Riveros, C., Askim, T., Bussmann, J. B., Callisaya, M. L., Chastin, S. F., et al. (2019). Identifying factors associated with sedentary time after stroke. Secondary analysis of pooled data from nine primary studies. Top. Stroke Rehabilit. 26, 327–334. doi: 10.1080/10749357.2019.1601419
Holder, C., Krishnamurthi, R., and Theadom, A. (2023). Exploring facilitators and barriers to long-term behavior change following health-wellness coaching for stroke prevention: a qualitative study conducted in Auckland, New Zealand. Brain Behav. 13:e2671. doi: 10.1002/brb3.2671
Joseph, C., Rhoda, A., and Conradsson, D. M. (2020). Levels and patterns of physical activity in stroke survivors with different ambulation status living in low-income areas of Cape Town, South Africa. Top. Stroke Rehabil. 27, 494–502. doi: 10.1080/10749357.2020.1741242
Kroll, T., Kehn, M., and Ho, P. S. (2007). The SCI exercise self-efficacy scale (ESES): development and psychometric properties. Int. J. Behav. Nutr. Phys. Activity 4, 1–6. doi: 10.1186/1479-5868-4-34
Krueger, H., Koot, J., Hall, R. E., O'Callaghan, C., and Bayley, M. (2015). Prevalence of individuals experiencing the effects of stroke in Canada: trends and projections. Stroke 46, 2226–2231. doi: 10.1161/STROKEAHA.115.009616
Kruithof, W. J., van Mierlo, M. L., Visser-Meily, J. M. A., van Heugten, C. M., and Post, M. W. M. (2013). Associations between social support and stroke survivors' health-related quality of life–a systematic review. Patient Educ. Couns. 93, 169–176. doi: 10.1016/j.pec.2013.06.003
Mirkarimi, K., Eri, M., Ghanbari, M. R., Kabir, M. J., Raeisi, M., Ozouni-Davaji, R. B., et al. (2017). Modifying attitude and intention toward regular physical activity using protection motivation theory: a randomized controlled trial. East. Mediterr. Health J. 23, 543–550. doi: 10.26719/2017.23.8.543
Nicholson, S. L., Donaghy, M., Johnston, M., Sniehotta, F. F., Van Wijck, F., Johnston, D., et al. (2014). A qualitative theory guided analysis of stroke survivors' perceived barriers and facilitators to physical activity. Disab. Rehabilit. 36, 1857–1868. doi: 10.3109/09638288.2013.874506
Northcott, S., Moss, B., and Harrison, K. (2016). A systematic review of the impact of stroke on social support and social networks: associated factors and patterns of change. Clin. Rehabilit. 30, 811–831. doi: 10.1177/0269215515602136
O'Donnell, M. J., Xavier, D., Liu, L., Zhang, H., Chin, S. L., Rao-Melacini, P., et al. (2010). Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 376, 112–123. doi: 10.1016/S0140-6736(10)60834-3
Palmer, V. J., Gray, C. M., Fitzsimons, C. F., Mutrie, N., Wyke, S., Deary, I. J., et al. (2019). What do older people do when sitting and why? Implications for decreasing sedentary behavior. Gerontologist 59, 686–697. doi: 10.1093/geront/gny020
Pauly, T., Ashe, M. C., Murphy, R., Gerstorf, D., Linden, W., Madden, K. M., et al. (2021). Active with whom? Examining the social context of physical activity in individuals after stroke and their partners. Front. Public Health. 9:754046. doi: 10.3389/fpubh.2021.754046
Piercy, K. L., and Troiano, R. P. (2018). Physical activity guidelines for Americans from the US department of health and human services. Circ. Cardiovasc. Qual. Outc. 11:e5263. doi: 10.1161/CIRCOUTCOMES.118.005263
Sabia, S., Yerramalla, M. S., and Liu-Ambrose, T. (2022). Importance of characterising sleep breaks within the 24-h movement behaviour framework. Int. J. Behav. Nutr. Phys. Act. 19:3. doi: 10.1186/s12966-021-01241-5
Sjöholm, A., Skarin, M., Churilov, L., Nilsson, M., and Bernhardt, J. (2014). Sedentary behaviour and physical activity of people with stroke in rehabilitation hospitals. Stroke Res. Treatment 2014:591897. doi: 10.1155/2014/591897
Tremblay, M. S., Aubert, S., Barnes, J. D., Saunders, T. J., Carson, V., Latimer-Cheung, A. E., et al. (2017). Sedentary behavior research network (SBRN) - terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Act. 14:75. doi: 10.1186/s12966-017-0525-8
Troiano, R. P., Berrigan, D., Dodd, K. W., Masse, L. C., and Tilert, T. (2008). Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exer. 40:181. doi: 10.1249/mss.0b013e31815a51b3
Trost, S. G., Owen, N., Bauman, A. E., and Sallis, J. F. (2002). Correlates of adults' participation in physical activity: review and update. Med. Sci. Sports Exer. 34, 1996–2001. doi: 10.1097/00005768-200212000-00020
Tsao, C. W., Aday, A. W., Almarzooq, Z. I., Anderson, C. A., Arora, P., Avery, C. L., et al. (2023). Heart disease and stroke statistics−2023 update: a report from the American Heart Association. Circulation 147, e93–e621. doi: 10.1161/CIR.0000000000001123
Wang, X., Shang, S., Yang, H., Ai, H., Wang, Y., Chang, S., et al. (2019). Associations of psychological distress with positive psychological variables and activities of daily living among stroke patients: a cross-sectional study. BMC Psychiatry. 19:381. doi: 10.1186/s12888-019-2368-0
Wen, H., Weymann, K. B., Wood, L., and Wang, Q. M. (2018). Inflammatory signaling in post-stroke fatigue and depression. Eur. Neurol. 80, 138–148. doi: 10.1159/000494988
Wen, K., Shen, M. J., Deng, C. S., Li, Y. F., Kang, Y. N., and Wan, L. H. (2022). Association between chronic illness resources and health behaviors in hypertensive stroke patients at 6 months after discharge: a cross-sectional study. Ann. Transl. Med. 10:460. doi: 10.21037/atm-22-1193
Wondergem, R., Veenhof, C., Wouters, E. M., de Bie, R. A., Visser-Meily, J. M., and Pisters, M. F. (2019). Movement behavior patterns in people with first-ever stroke. Stroke 50, 3553–3560. doi: 10.1161/STROKEAHA.119.027013
Keywords: stroke, sedentary behavior, social support, self-efficacy, mediation
Citation: Wei J, Yang F and Dong X (2024) Perceived social support on objective measured sedentary behavior of stroke patients: the mediating role of exercise self-efficacy. Front. Psychol. 15:1444214. doi: 10.3389/fpsyg.2024.1444214
Received: 07 June 2024; Accepted: 09 September 2024;
Published: 25 September 2024.
Edited by:
Tommaso Piccoli, University of Palermo, ItalyReviewed by:
María Antonia Parra Rizo, Miguel Hernández University of Elche, SpainMaria-Arantzazu Ruescas-Nicolau, University of Valencia, Spain
Copyright © 2024 Wei, Yang and Dong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaofang Dong, ZG9uZ3hpYW9mYW5nMTIxMEAxMjYuY29t
 Jianing Wei
Jianing Wei Fanjiayi Yang
Fanjiayi Yang Xiaofang Dong
Xiaofang Dong