- Research Methods in Health Science, University of Education, Freiburg, Germany
Introduction: Vaccination readiness refers to psychological motives and beliefs that decisively determine individual and collective vaccination prevention behavior. Readiness to be vaccinated depends on expected individual and social benefits and harms. Differences exist in the perception of the threat of potential influenza vs. COVID-19 infection and its significance for the social environment. The study aimed to compare the 7C components of vaccination readiness for influenza and COVID-19 vaccination in adulthood.
Methods: A total of 317 adults answered the 7C vaccination readiness scale in two vaccination-specific versions (influenza vs. COVID-19) in an online survey from September 2022 to March 2023. Data were analyzed using repeated measures, including analysis of covariance, correlations, and multiple regression.
Results: For COVID-19, there is a higher readiness to be vaccinated compared to influenza regarding complacencyR (ηp = 0.683), constraintsR (ηp = 0.684), collective responsibility (ηp = 0.782), and compliance (ηp = 0.365). However, confidence (ηp = 0.161) and conspiracyR (ηp = 0.256) indicate an enhanced readiness for influenza vaccination (interaction scales × vaccination type: ηp = 0.602). Individual influenza vaccination recommendations and age do not or only marginally moderate these effects (interaction vaccination type × recommendation: ηp = 155).
Discussion: The 7C subscales reveal a differentiated pattern of readiness for the two vaccination types. This emphasizes the relevance of the multidimensional structure of the construct of vaccination readiness as well as the relevance of moderating effects of the respective vaccination type on the underlying motives and beliefs. Vaccination attitudes are influenced by cultural and social conditions as well as medical standards of care. Comparing attitudes to different vaccinations in different countries thus represents an important research desideratum in order to understand the concept of vaccination readiness more comprehensively.
1 Introduction
Vaccinations are highly effective in preventing communicable diseases such as influenza, COVID-19, or measles and their societal spread (Wilder-Smith et al., 2017; Zheng et al., 2022). However, the compelling evidence (Du et al., 2024; Wu et al., 2024) that the benefits clearly outweigh the potential harm of vaccination has not proven to be sufficient for all people to consider vaccination positive for themselves and to decide to be vaccinated (Dubé et al., 2013; Omer et al., 2009; Petráš et al., 2022). The significance of this critical attitude in terms of vaccination hesitancy and refusal has been the subject of public debate and scientific research since the introduction of vaccinations for preventing infectious diseases, especially regarding vaccinations that are required to maintain population or herd immunity (e.g., against measles or polio) (MacDonald et al., 2020; Spier, 2001; Abate et al., 2024). Accordingly, WHO (2013) identified overcoming vaccination hesitancy as one of the 10 most essential goals to secure and improve public health.
In Germany, public health strategies for influenza and COVID-19 vaccination focus on ensuring widespread coverage, particularly for vulnerable populations (RKI, 2022). The German Standing Committee on Vaccination (STIKO) recommends annual influenza vaccinations, especially for high-risk groups such as the elderly (above 60 years), individuals with chronic illnesses, pregnant women, healthcare workers, and those who have close contact with at-risk populations. Vaccinations are generally provided free of charge through health insurance for these high-risk groups, making them easily accessible. Employers are also encouraged to offer vaccines, particularly in healthcare settings (RKI, 2023). During the COVID-19 pandemic, Germany introduced legal measures such as the Infection Protection Act, allowing for mandates like mask-wearing, lockdowns, and vaccination requirements for healthcare workers (Eurofound, 2021). While a general vaccination mandate was debated, it was not implemented nationwide. Initially, public health efforts focused on prioritizing high-risk groups and ensuring broad access through vaccination centers, mobile units, and pharmacies. In 2022, it was ensured that all those willing to be vaccinated could actually take advantage of a vaccination. This was also insistently promoted by health (political) campaigns and public media. In 2022, awareness campaigns promoted vaccination and countered misinformation, while booster shots were emphasized as new variants emerged. Despite the intensive public measures and high social importance, 22.1% of the adult population was unvaccinated at the end of 2022, mostly due to vaccine hesitancy (RKI, 2024a).
1.1 Generic and vaccine-specific aspects of vaccination readiness
Vaccination readiness or hesitancy can be partially understood as a generic attitude, as people tend to have an overarching attitude toward vaccination and vaccination uptake regardless of the specific vaccine (Geoghegan et al., 2020; Larson et al., 2014). However, vaccine-specific aspects of vaccination readiness must be considered due to both the individual health constitution and the properties of the specific vaccine (Anas et al., 2023; Rahbeni et al., 2024; Troiano and Nardi, 2021). According to MacDonald (2015), attitude toward a specific vaccine depends on a risk–benefit assessment, which is particularly important for newly introduced vaccines. For instance, critical concerns emerged with the newly developed COVID-19 vaccine, as it utilized mRNA technology for the first time in vaccines (Abate et al., 2024; Peretti-Watel et al., 2024).
Moreover, the type of vaccine administration, the design of the vaccination program (e.g., routine program or mass vaccination campaign), the vaccination schedule, the costs, the strength of the vaccination recommendation, the level of knowledge, and the attitude of the healthcare professionals can be decisive for the individual willingness to receive a specific vaccination (Dubé et al., 2013; MacDonald, 2015). For example, the decision to be vaccinated against influenza is primarily based on the subjective expected benefit-harm balance regarding one’s own health, in which both the protection against infection and the vaccination reactions must be considered. Risk-associated individual person characteristics (e.g., age, chronic illnesses, occupational contacts) are decisive for the decision of the respective individual, as well as for official recommendations (Grohskopf et al., 2024; de Fougerolles et al., 2024). These risk indicators contribute to the systematic variance in the population’s willingness to be vaccinated. In general, a valid assessment of readiness to be vaccinated must thus take into account (i) the objective threat of a potential infection, (ii) the individual susceptibility to an infection, and (iii) the subjective perception of the threat in an integrated manner. Accordingly, Betsch et al. (2015; see also: Eitze et al., 2024) emphasize the importance of five central vaccination readiness facets: Confidence, ComplacencyR, ConstraintsR, CalculationR, and Collective Responsibility. Confidence reflects trust in the effectiveness and safety of vaccinations, the healthcare system, and decision-makers’ motives. ComplacencyR describes the perception of health risks and threats that should be avoided through vaccinations and whether vaccinations are considered necessary (Dubé et al., 2013; Betsch et al., 2015). ConstraintsR refers to obstacles to taking up vaccinations (e.g., stress, [time] expenditure) and whether vaccination is considered sufficiently important to protect from health obstacles. CalculationR refers to the extent of active information search that is accompanied by a conscious risk–benefit appraisal. High CalculationR is associated with enhanced false knowledge and a lower willingness to be vaccinated (Betsch et al., 2019). Collective Responsibility refers to the extent of prosocial motivation to be vaccinated. Vaccinating oneself is seen as helpful as it reduces the risk of transmission of the infectious disease and can, therefore, support the health of other individuals (e.g., children, chronically ill relatives) or society (esp. herd immunity). Confidence in safety and effectiveness, underestimated disease risk (ComplacencyR), and ConstraintsR have proven to be important predictors of making use of influenza vaccination (Eitze et al., 2024). It must be noted that the 7C subscales ComplacencyR, ConstraintsR, CalculationR, and ConspiracyR are named contrary to the scale polarity so that their designation would misleadingly imply a negative readiness to be vaccinated. Thus, the superscript “R” indicates that the scale semantics are inverted. MacDonald (2015) considers the sub-facets of vaccination readiness to be decisive components of an individual consideration and decision-making process that results in a comprehensive vaccination attitude. According to the levels and weighting of these individual facets, people are assumed to be positioned on a continuum between the poles of “full approval” and “complete rejection” of the respective vaccinations.
1.2 Relevance of vaccination readiness during the COVID-19 pandemic
The COVID-19 pandemic has brought the individual and social significance of vaccinations and characteristics of public perception of vaccinations to the focus of public interest to an unprecedented extent (Prada et al., 2023). After the extensive restrictions on everyday social interaction and the comprehensive hygiene requirements to minimize the risk of infection in the early times of the pandemic, vaccinations were the most effective means of overcoming the pandemic (Wu et al., 2024). Vaccine hesitancy and readiness were key factors influencing the success of COVID-19 vaccination campaigns in all OECD countries (Abate et al., 2024). For example, Israel, which was one of the first countries to start the comprehensive vaccination of its population in December 2021, faced hesitancy primarily among ultra-Orthodox communities and younger populations, slowing the rate of booster uptake despite a strong initial rollout (Rosen et al., 2021). Misinformation and conspiracy theories circulating in rural and conservative areas contributed to lower vaccine acceptance, particularly for boosters. They were found to be important in European countries in general (Jabkowski et al., 2023) and the United States (Robinson et al., 2022). Vaccine hesitancy proved to be more pronounced, fueled by widespread misinformation (Enria et al., 2024), distrust in government policies, and lower health literacy, which posed a significant challenge to any vaccination efforts (Lee et al., 2022). Such effects were reported especially for Turkey (Alper et al., 2020) and Russia (Loseva, 2022). In China, high trust in the government and social conformity drove higher vaccine uptake, contrasting with the hesitancy rooted in misinformation and mistrust in Western countries (Huang et al., 2022; Leong et al., 2022). Japan’s initial skepticism, due to fears about side effects, was mitigated by trust in government health campaigns, though lingering concerns slowed full population coverage (Harada and Watanabe, 2021).
Thus, trust in and acceptance of the newly developed vaccines and the willingness to be vaccinated were of utmost individual and public interest, transnational and cross-cultural (Anand and Stahel, 2021; Sprengholz et al., 2021; Watson et al., 2022). Accordingly, an appropriate appraisal of disease risk (i.e., ComplacencyR), Compliance, and Collective Responsibility are assumed to be enhanced for COVID-19 vaccination (see below: Hypothesis 2b). The pro arguments for ConstraintsR and CalculationR regarding COVID-19 vaccination should also be supported (see below: Hypothesis 2c). However, there were also particular reservations about COVID-19 vaccines, most of which were associated with a generally critical or dismissive attitude toward vaccination (Geoghegan et al., 2020; Rahbeni et al., 2024). In addition, skeptics pointed out or suspected (i) that the COVID-19 vaccines were developed unusually quickly and may not have been tested according to the usual standards, (ii) that mRNA vaccines are based on a vaccine principle that has not been implemented before and uses genetic engineering to influence the genetic information in cells (Krause et al., 2023), and (iii) that infections, severe courses of disease and even infection-related deaths have also occurred in vaccinated people (Anand and Stahel, 2021; Seddig et al., 2022; Soares et al., 2021). This implies that Confidence is assumed to be reduced for COVID-19 vaccination (see below: Hypothesis 2a). Furthermore, contra arguments regarding ConstraintsR and CalculationR for COVID-19 vaccination should be conveyed (see below: Hypothesis 2c). Moreover, the immediate reaction to the vaccination could result in side effects (e.g., absence from work, Anand and Stahel, 2021; Dhamanti et al., 2023), which could have led non-risk persons to assess the immediate negative effects as disproportionately high (see Hypothesis 2b below: contra arguments regarding ConstraintsR and CalculationR for COVID-19 vaccination).
Furthermore, public and political discussions on a possible vaccination policy emphasized the tension between individual freedom and social responsibility (Cardona, 2021; Sprengholz et al., 2021). As a result, this health prevention issue was particularly subject to individual opinion formation, which was linked to basic political attitudes (Ward et al., 2020). Irrational or conspiratorial narratives and myths that imputed opaque and manipulative motives to the public vaccination recommendations of the pharmaceutical industry and official health authorities were abundant in vaccination skeptic circles during the pandemic (Seddig et al., 2022; Soares et al., 2021). Fake news spread on social media, and information bubbles became a prominent topic in health research. Accordingly, ConspiracyR should be reduced for COVID-19 vaccination (see below: Hypothesis 2a).
Due to the experiences within the COVID-19 pandemic, Geiger et al. (2021) supplemented the structural model of vaccination readiness (Betsch et al., 2015, 2019) by two further facets. Compliance corresponds to the willingness to adhere to preventive health behavioral rules and provisions. This proved to be an essential aspect of the COVID-19 pandemic to reconcile the overall societal effectiveness of vaccination protection with the individual intention to take advantage of being vaccinated (Sprengholz et al., 2021). ConspiracyR reflects individual susceptibility to belief in misinformation and conspiracy myths and proved to be a relevant predictor for vaccination hesitancy (Nicholls et al., 2021). The very good criterion validity of the 7C scale was demonstrated by the 85% multiple variance explanation in the willingness to be vaccinated (Geiger et al., 2021). In summary, readiness for vaccination against COVID-19 must be regarded in certain aspects as vaccine- or pandemic-specific.
1.3 Present study and research hypotheses
To shed light on this COVID-19 vaccination-specific hesitancy aspect, the study presented here focuses on whether and to what extent sub-facets of readiness for COVID-19 vaccination differ from those for influenza vaccination (see hypotheses 1 and 2 below). For these two vaccinations, different individual and social appraisals can be assumed (Dombrádi et al., 2021; SteelFisher et al., 2023). Due to the long-term development and the proven and widespread implementation over a long period of the influenza vaccination, it seems reasonable that the common vaccination reservations (i.e., general skepticism or refusal of vaccination among critical persons) are more prominent for COVID-19 than for the influenza vaccination (see below: Hypothesis 2a: Confidence enhanced for influenza vaccination; Hypothesis 2c: pro arguments ConstraintsR for influenza vaccination). The Standing Committee on Vaccination in Germany first recommended the annual influenza vaccination in 1982. Since 2002, the influenza vaccination has been recommended for people aged 60 and over, chronically ill people, and medical personnel, and since 2010, also for pregnant women (RKI, 2023). In contrast, a general vaccination recommendation applies for the COVID-19 vaccination. Thus, differences in readiness for vaccination against influenza vs. COVID-19 should be more pronounced in the group of people without influenza vaccination recommendation (see Hypothesis 3 below). Furthermore, the decision for or against influenza vaccination is usually made primarily to protect one’s own health, while the protection of the community and the protection of vulnerable groups can be considered particularly important for COVID-19 vaccination, especially for younger adults without particular health risks (see Hypothesis 2b below Collective Responsibility enhanced for COVID-19 vaccination).
The main research hypotheses 1–3 of the study relate to the differences in the 7C components of vaccination readiness between the two vaccination types. In addition, Hypothesis 4 concerning the differential criterion validity of the versions of the 7C scale adapted for the two vaccination types is examined, as these results are also decisive for the validity of the interpretation of the results in general.
Hypothesis 1: Vaccination readiness differs for influenza vaccination and COVID-19 vaccination (i.e., the main effect of vaccination type).
Hypothesis 2: The seven subscales of the 7C scale indicate varying differences in readiness for influenza vs. COVID-19 vaccination (i.e., interaction of the 7C single scales and vaccination type).
Hypothesis 2a: Confidence and ConspiracyR is higher for influenza vaccination than for COVID-19 vaccination.
Hypothesis 2b: The ComplacencyR, Collective Responsibility, and Compliance scales indicate a higher readiness to be vaccinated for COVID-19 than for influenza.
Hypothesis 2c: No differences for the COVID-19 vs. influenza vaccination exist for the ConstraintsR and the CalculationR scales, as both pros and cons regarding immediate and long-term effects, benefits, and harms may be relevant.
Hypothesis 3: The difference in readiness for influenza vs. COVID-19 vaccination is enhanced if there is no influenza vaccination recommendation (i.e., the interaction of influenza vaccination recommendation with the 7C differences in readiness for influenza vs. COVID-19 vaccination).
Hypothesis 4a: The 7Cs of influenza vaccination readiness correlate more strongly with influenza vaccination-related importance rating and influenza vaccination status than the 7Cs of COVID-19 vaccination readiness.
Hypothesis 4b: The 7Cs of COVID-19 vaccination readiness correlate more strongly with COVID-19 vaccination-related importance assessment and COVID-19 vaccination status than the 7Cs of influenza vaccination readiness.
Hypothesis 4c: The 7Cs of COVID-19 vaccination readiness correlate more strongly with the relevance and implementation of COVID-19 infection prevention measures than the 7Cs of influenza vaccination readiness.
Thus, the central objective of this study is to empirically determine the differences in the seven sub-facets of vaccination readiness regarding COVID-19 and influenza vaccination. The insights into these differences and their correlations with further vaccine-related characteristics should enhance the understanding of the construct of vaccination readiness and its vaccine-specific characteristics.
2 Methods
This study is an extension of a study conducted in the DFG project “Structural Modeling and Assessment of Health Literacy in Allergy Prevention of New Parents” [G.Z.: WI-3210/7-1]. For this DFG-funded study, an Ethics Statement was approved by the Ethics Committee of the German Psychological Society,1 and the study protocol has been preregistered at the Leibniz Institute of Psychology (ZPID; Wirtz et al., 2021). There, (expectant) parents of infants were surveyed, in particular on attitudes toward COVID-19 vaccination. In the present study, in which adults were surveyed, the same standards were adhered to and implemented. Informed consent was obtained from all participants. The study was performed in accordance with the ethical principles in the Declaration of Helsinki.
2.1 Measures
The 7C scale (Geiger et al., 2021; Rees et al., 2022) was used in particular within the COVID-19 Snapshot Monitoring Study (COSMO study) to assess and monitor vaccination-related barriers and support factors using subjective self-reported data. The 7C scale uses three items each to measure the 7C facets: Confidence, ComplacencyR, ConstraintsR, CalculationR, Collective Responsibility, Compliance, and ConspiracyR. It should be noted that the 7C subscales ComplacencyR, ConstraintsR, CalculationR, and ConspiracyR are named contrary to the scale polarity, so that their designation would misleadingly imply a negative readiness to be vaccinated. To ensure that this reversed naming is taken into account and to avoid apparently contradictory statements, these scales are labeled with R (reversed) (e.g., “high ConspiracyR” corresponds to “low conspiracy”). The 21 individual items are answered on a 7-point rating scale (1 = strongly disagree to 7 = strongly agree). The scale structure can be modeled using a bifactor model with a dominant general factor, “Readiness to vaccinate” (Geiger et al., 2021). While the general factor, according to McDonald’s ω (omega), exhibits good internal consistency at 0.88, the internal consistency for the individual factors is considerably weaker: range ω = 0.27 (ConstraintsR) to ω = 0.59 (Compliance).
In the study presented here, the 21 7C items were used in two versions, which were adapted for COVID-19 and influenza vaccination by replacing the general wording “vaccination” with “influenza vaccination” or “COVID-19 vaccination,” respectively. A content revision was only necessary for two items of the Compliance scale: The adapted influenza formulations refer to the special attention and compliance with hygiene measures (item 18: originally: excluding people from public events) and behavioral rules (item 19: originally: legal sanctions). All items proved to be comprehensible in both a cognitive pre-test and a cross-sectional pre-test of the instrument involving 187 participants. Both adapted versions and the original item formulation are attached in Supplementary material 1. In addition, participants self-reported the current COVID-19 vaccination status (“1”—“no”; “2”—“yes, but not completely”; “3”—“yes, completely”), influenza vaccination use (“1”—“never”; “2”—“at least once”) and general vaccination status (e. g. measles, polio; “1”—“no”; “2”—“yes”), the subjective importance of being vaccinated (“1”—“extremely unimportant” to “6”—“extremely important”) and the relevance of adhering to COVID-19 protective measures (“1”—“not important at all” to “6”—“very important”) and their implementation in daily life (“1”—“very bad” to “6”—“very good”) were surveyed using single items. Furthermore, sociodemographic information, socioeconomic status (MacArthur Scale; Hoebel et al., 2015), and indicators of influenza vaccination recommendation (age at least 60 years, regular contact with people at risk, working in a healthcare profession, previous illness) were assessed.
2.2 Data collection and study sample
The cross-sectional data were collected online from August 2022 to March 2023 via the “SoSciSurvey” platform. The average processing time was 16.5 min (SD = 4.9 min). Missing data were avoided due to the default settings. While limited statutory COVID-19 protective measures were still mandatory in autumn 2023 (e.g., obligatory mask-wearing on local public transport), the special statutory requirements for public COVID-19 infection protection ended in the first months of 2023. We opted for an online-based convenience sample, as the extensive restrictions on public life considerably limited the possibilities for ensuring a population-based, representative sample. Instead, we targeted specific groups of people to cover a broad age spectrum and to be able to reach target groups of younger adults for whom a recommendation for influenza vaccination prevailed. The study call was distributed via social networks and Kiel University mailing lists. People who were at least 18 years old and had sufficient knowledge of the German language were eligible to take part in the survey. Since the digital study call primarily reached young adults, older individuals and those with increased health risks were also contacted.
The study sample predominantly consisted of people of young adults (M = 29.95 and a median of 23 years; see Supplementary material 2). The proportion of people with influenza vaccination recommendations was 42.6%. 54.9% of those had already been vaccinated at least once against influenza. Since the proportion of vaccinated people in Germany is considerably below 50% even among groups with influenza vaccination recommendations (2021/22: e.g., over 60-year-old: 43.3%, chronic illness: 35.4%, pregnant women: 17.5%; Statista, 2022a), this indicates increased vaccination acceptance in the study sample. This is also reflected as 90.3% of participants had already received a COVID-19 vaccination (full vaccination: 84.9%). In the general population, the proportion of people with a first COVID-19 vaccination was stable between 77 and 78% in the second half of the year 2022 (Statista, 2022b). According to the MacArthur scale, the more educated (90.6% high school graduates) and female (73.8% women) sample has an above-average socioeconomic status according to the arithmetic mean M = 6.22 (general population: M = 5.25; Hoebel et al., 2015). However, the median of 5 indicates that the proportion of people with lower socioeconomic status can be considered appropriate.
2.3 Statistical analysis
Multivariate analysis of variance (ANOVA) with repeated measures is used to test the study hypotheses (Tabachnick and Fidell, 2019). The vaccination type (influenza vs. COVID-19) is a repeated measures factor with two levels. The influenza vaccination recommendation (yes, no) is included as a 2-level between-subjects factor. In order to test the interaction of the items with the vaccination type (Hypothesis 2), the seven factors are defined as a further 7-level repeated measures factor. The variance analysis approach thus enables an integrated and maximally test-economic examination of the effects that refer to mean differences. In addition to the main effects, which reflect fundamental differences in the factor levels under consideration, the interaction effects are particularly important in this study: These indicate in particular which internal sub-facets of the readiness to vaccinate are specifically pronounced for the respective vaccination types. Due to the multi-factorial variance decomposition within the framework of the ANOVA approach, this information is tested much more rigorously than if non-variance analysis methods were used (Tabachnick and Fidell, 2019). In addition, the Pearson product–moment correlation is determined for the within components. This depicts the similarities between the individual variables: The more positive the correlation, the higher the common information share of the corresponding characteristics, which may indicate an overarching underlying latent source of information (Roettele and Wirtz, 2020).
The ANOVA assumption of equal covariance matrices between groups with and without an influenza vaccination recommendation was tested using the BOX-M test (Tabachnick and Fidell, 2019). The Levene test is used to test the equality of the variances between the groups. In principle, the ANOVA is (a) robust against corresponding violations for sufficiently large samples (ni per group >30) and (b) for similarly large samples (Tabachnick and Fidell, 2019). In the present study, the ratio of group sizes (135 vs. 180) is 0.75, so the validity of the test can be considered at most weakly affected. Nevertheless, the results of the BOX-M- and the Levene-test are documented in order to ensure the transparency of the data characteristics.
The internal consistencies of the 7C scale and the seven individual scales are calculated using McDonald’s ω (omega), which is determined using the item-specific maximum likelihood estimated unstandardized factor loadings and error variances (assumption: τ-congeneric measurements; Geiger et al., 2021). To ensure an overall nominal α-level of 0.05 despite multiple testing, an α-error adjustment according to Bonferroni (α/k; where k = number of individual tests performed; Tabachnick and Fidell, 2019) is adopted for each hypothesis or each statistical procedure, respectively. Hedges g is used as a measure of the effect size for pairwise mean differences, with g = 0.2, 0.5, and 0.8 as orientation values for small, medium, and large effect sizes (Tabachnick and Fidell, 2019). For the comparison of k > two mean values, the effect size is determined using the partial ηp, with ηp = 0.10, 0.24, and 0.37 as reference values for small, medium, or large effect sizes. Linear correlations are calculated using product–moment correlation (reference values: 0.1 = small, 0.3 = medium, 0.5 = large). All statistical analyses are computed using the SPSS 29.0 software. Differences in dependent correlations were tested by Hotellings-T statistic (Wilcox and Tian, 2008) using Hemmerich’s (2017) online calculation tool.
3 Results
3.1 Differences in the 7Cs of vaccination readiness for influenza vs. COVID-19 vaccination
The 7C total scale indicates a higher readiness for COVID-19 vaccination than for influenza vaccination (F1,315 = 179.659***; ηp = 0.602; Table 1) (Hypothesis 1). However, this effect is strongly moderated by the seven individual scales, as the seven scales reflect significantly varying differences in readiness to be vaccinated between the influenza vs. COVID-19 vaccination types. In accordance with Hypothesis 2a, Confidence and ConspiracyR proved to be enhanced for influenza vaccination with medium effects size (ηp = 0.161, 0.256). ComplacencyR, Collective Responsibility, and Compliance indicate a higher readiness to vaccinate against COVID-19 with a high effect size (ηp = 0.683, 0.728, 0.365), which confirms Hypothesis 2b. The higher values of ConstraintsR (ηp = 0.684) for the COVID-19 vaccination and the higher values of CalculationR (ηp = 0.228) for the influenza vaccination do not confirm Hypothesis 2c, according to which the pros and cons should be balanced. In an additional overall 2 × 2 × 7-ANOVA, in which the seven scales are also included as a repeated measurement factor, the scale dependence of the influenza vs. COVID-19 differences reveals a high effect size ηp = 0.602 (Table 2, interaction of vaccination type and scales; F6,1890 = 179.818***) (Hypothesis 2).
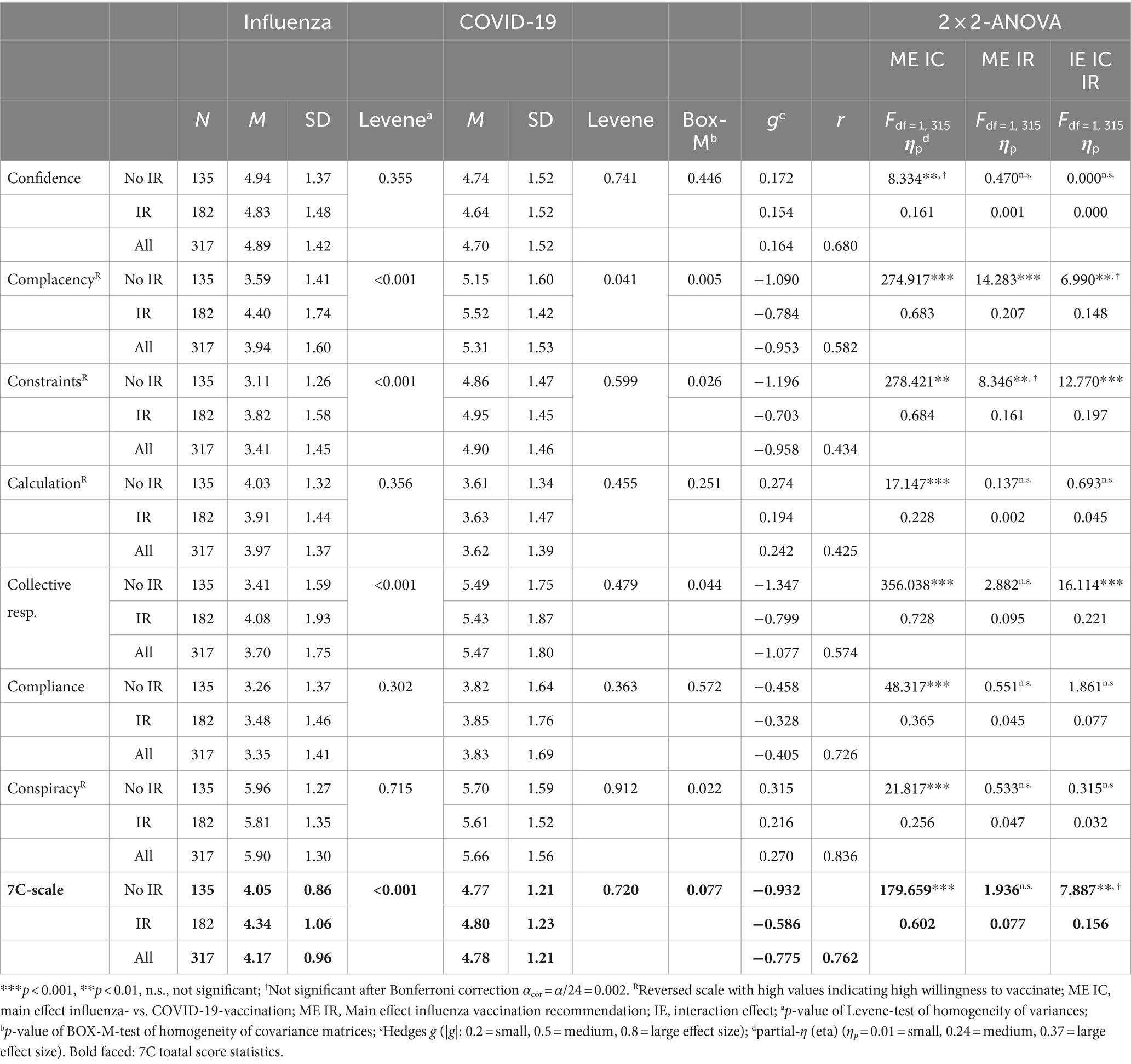
Table 1. Descriptive statistics and results of the 2 × 2-ANOVAs testing the effects of vaccination type (influenza vs. COVID-19) and influenza vaccination recommendation (yes vs. no) for each 7C-scale and total score.
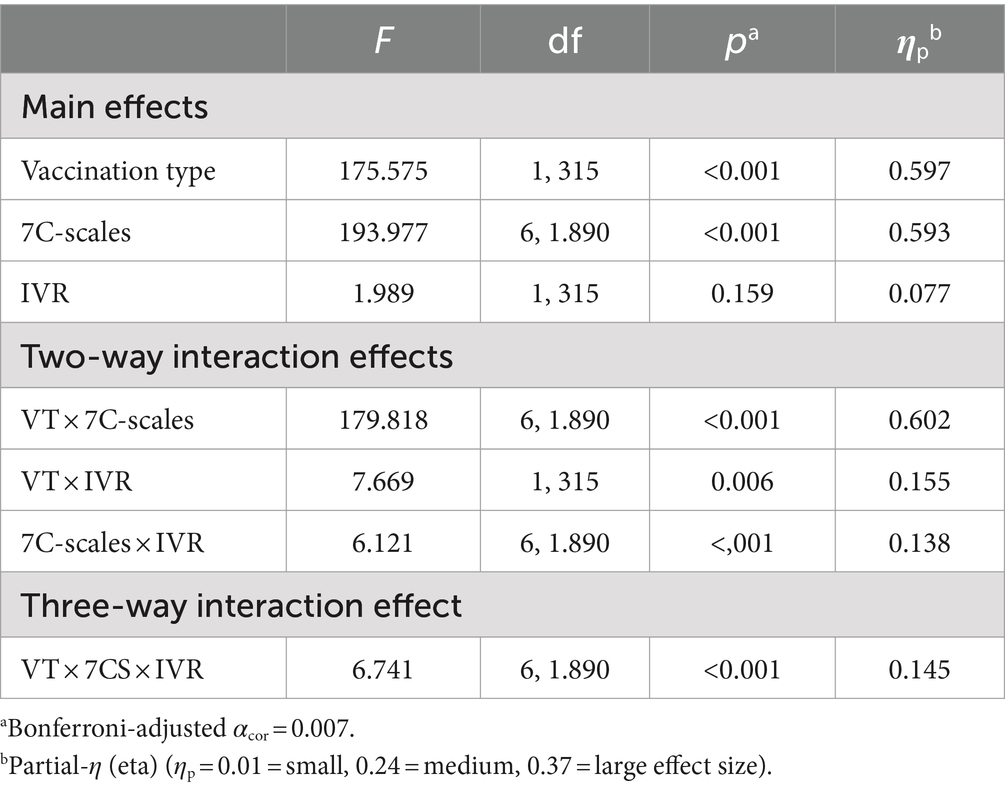
Table 2. Results of the 2 × 2 × 7-ANOVAs testing the within-subject effects of vaccination type (VT: influenza vs. COVID-19) and the seven scales of the 7C scale as well as the between-subject effect of influenza vaccination recommendation (IVR: yes vs. no).
These effects are mostly independent of whether an influenza vaccination recommendation exists (Hypothesis 3). After Bonferroni correction, only ConstraintsR (ηp = 0.197) and Collective Responsibility (ηp = 0.221) exhibit a significant interaction effect: For both scales, the difference between influenza and COVID-19 vaccination is, as expected in Hypothesis 3, larger for people without influenza vaccination recommendation (g = −1.196, −1.347) than for people with recommendation (g = −0.703, −0.799). A main effect of the influenza vaccination recommendation is only present for ComplacencyR (after Bonferroni correction): ComplacencyR is higher for both the influenza vaccination (M = 4.4 vs. 3.59) and the COVID-19 vaccination (M = 5.52 vs. 5.15) when an influenza vaccination recommendation exists.
3.2 Correlations of the 7 Cs regarding influenza and COVID-19 vaccination
Table 3 displays the correlations of the seven single scales and total scale scores for the two vaccination types. The correlation between the 7C influenza and COVID-19 vaccination readiness total score is high at r = 0.764. For the single scales, the highest correlation of r = 0.836 is found for ConspiracyR between vaccination types. Confidence and Compliance are associated between the two vaccination types about r = 0.7, ComplacencyR and Collective Responsibility about r = 0.58. For ContraintsR and CalculationR, a medium correlation between the vaccination types results (r about 0.43).
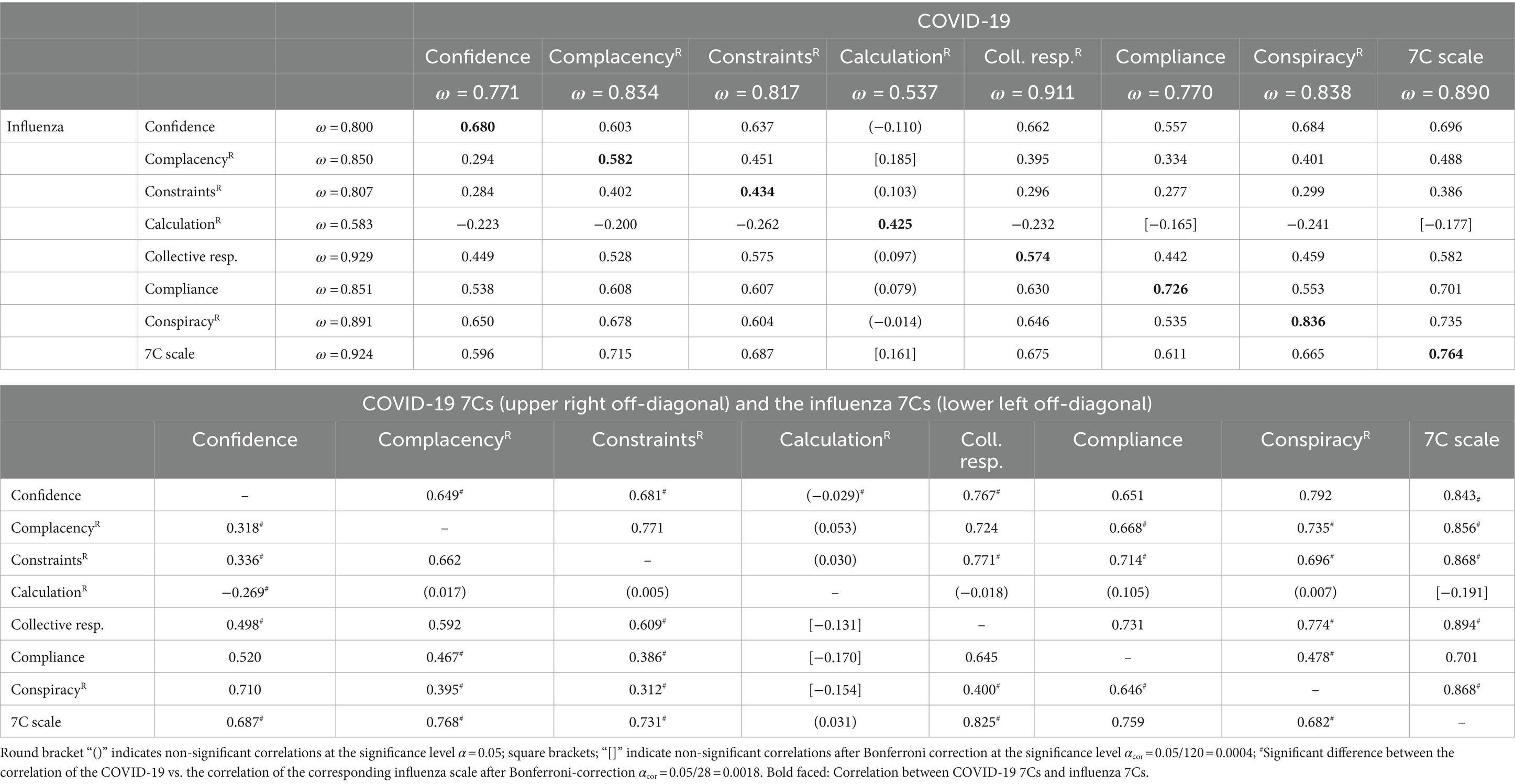
Table 3. Upper table: intercorrelations between the influenza and COVID-19 7Cs and internal scale consistency according to McDonald’s ω (omega); lower table: intercorrelations within the COVID-19 and the influenza 7Cs.
With regard to the scale intercorrelations between the vaccination types (upper Table 4), only the CalculationR scale is revealed to be not, or at most, weakly correlated (max |r| = 0.262) with the other 7C subscales between the vaccination types. Contrary to expectations, the influenza vaccination-related CalculationR is even consistently negatively correlated with the other COVID-19 vaccination-related 7C subscales. All other scale intercorrelations are significantly positive between the vaccination types, consistent with expectations. Influenza vaccination-related Confidence (r = 0.557–0.684; row data), Compliance (r = 0.538–0.630) and ConspiracyR (r = 0.535–0.678) correlate most highly with aspects of COVID-19 vaccination readiness. For COVID-19 vaccination-related Confidence, ComplacencyR, and ConspiracyR (column data), correlations prove to be mostly considerably lower, especially for influenza vaccine-related ComplacencyR and ConstraintsR (r = 0.284–0.402).
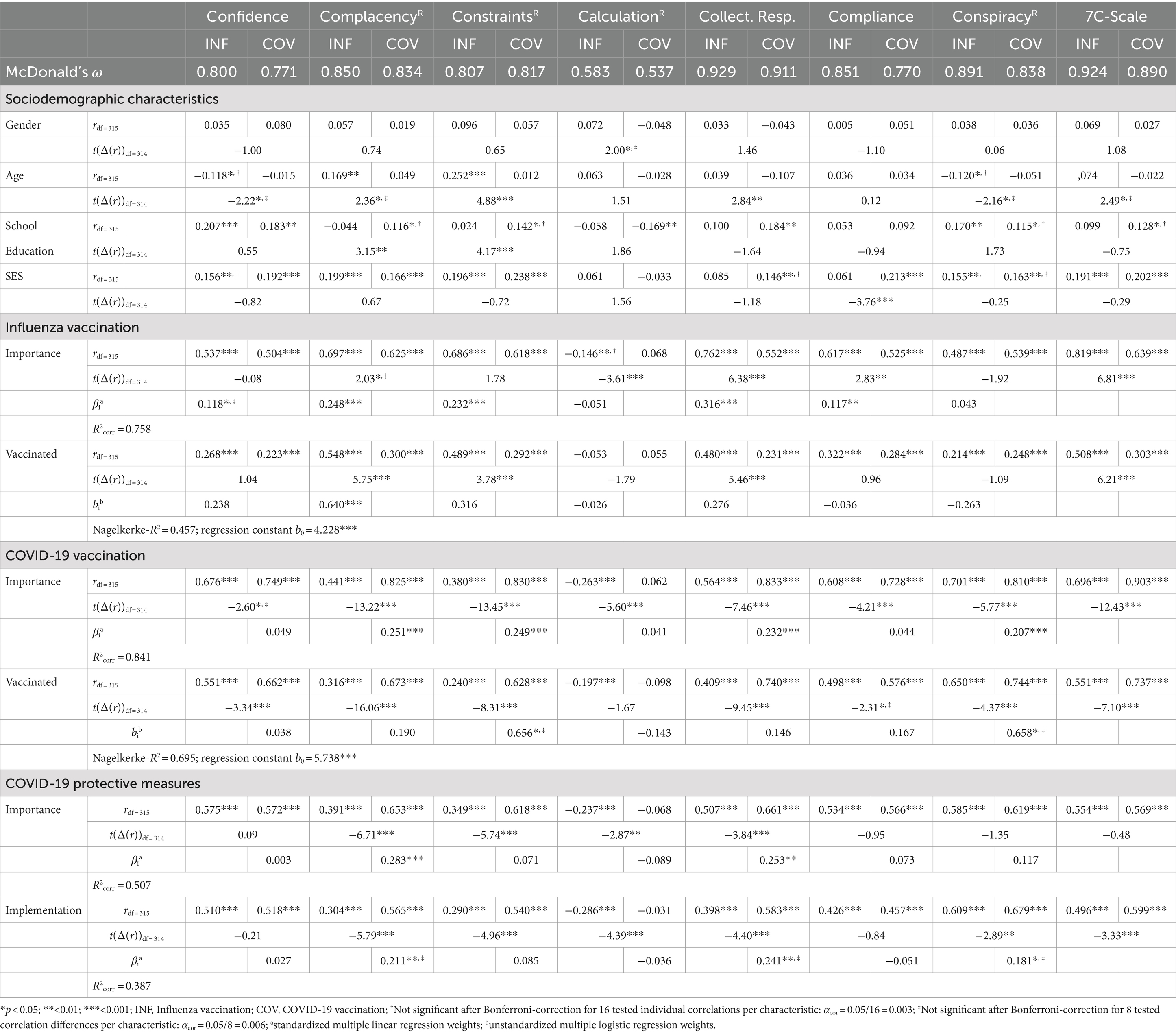
Table 4. Internal consistencies and correlations of 7Cs on readiness for influenza (INF) and COVID-19 vaccination (COV) with sociodemographic characteristics and aspects of infection prevention, testing of correlation differences between vaccination types using Hoteling’s t-statistics (t(Δ(r))) and multiple regression prediction.
At the level of the 7C overall scale, the influenza vaccination-related 7C scale is similarly strongly associated with the other COVID-19 vaccination-related individual scales—except CalculationR—in the range r = 0.596–0.715 (last row upper Table 3). For the COVID-19 vaccine-related overall scale, however, there is a considerably weaker association with the influenza vaccine-related ComplacencyR and ConstraintsR (r = 0.488, 0.386) (last column, upper Table 3).
Except for the Calculation scale, in general, the 7C individual scales for COVID-19 vaccination readiness proved to be considerably more highly correlated with each other (see upper-right-off-diagonal in lower Table 3: range: 0.478–0.792; median: 0.724) than the 7C individual scales for influenza vaccination readiness (lower-left-off-diagonal in lower Table 3: range: 0.312–0.710; median: 0.498).
3.3 Correlations of 7Cs for influenza and COVID-19 vaccination with sociodemographic characteristics and aspects of infection prevention
Among the socio-demographic characteristics, the highest correlations were found for SES (Table 4): Readiness to be vaccinated correlates positively with SES for the 7C total scale for both vaccination types (influenza: r = 0.191; COVID-19: r = 0.202). ComplacencyR and ConstraintsR are also associated with higher SES for both vaccine types (influenza: r = 0.199/0.196; COVID-19: r = 0.166/0.238). COVID-19-related Confidence (r = 0.192) and Compliance (r = 0.213) are also positively associated with SES, with the correlation for Compliance also being stronger in contrast (tdf = 314 = −3.76, p < 0.001) than the correlation for influenza vaccination-related Compliance (r = 0.061). School education correlates significantly higher with ComplacencyR (r = 0.116 vs. −0.044; tdf = 314 = 3.15, p = 0.002) and ConstraintsR (r = 0.142 vs. 0.024; tdf = 314 = 4.17, p < 0.001) for COVID vaccination than for influenza vaccination. Furthermore, the influenza vaccine-related ConstraintsR are significantly more highly correlated with age (r = 0.252 vs. 0.012; tdf = 314 = 4.88, p < 0.001).
For the validation criteria addressed in hypotheses 4a–c, considerably higher correlations were found overall (Table 4). Only the correlations for CalculationR proved to be strikingly weak here. The correlation differences between the two vaccination types of the other subscales and the 7C scale are almost always in the direction formulated in hypotheses 4a to c. Regarding Hypothesis 4c, the importance of the COVID-19 vaccination was correlated more positively with COVID-19 vaccination-related 7C facets than with the corresponding influenza vaccination-related 7C scale values (tdf = 314 = −2.60 to −13.45). Similar effects resulted for COVID-19 vaccination status, though there is no significant difference in correlation for CalculationR (tdf = 314 = −1.67). Complementarily, the importance of the influenza vaccination correlated significantly more strongly with the influenza vaccination-related 7C facets Collective Responsibility and Compliance as well as the 7C total score than with the corresponding COVID-19 vaccination-related 7C scale values (tdf = 314 = 2.83–6.81) (Hypothesis 4a). For the use of the influenza vaccination, there are, as expected, higher correlations with the influenza vaccination-related 7Cs ComplacencyR, ConstraintsR, Collective Responsibility, and the 7C total score than with the corresponding COVID-19 vaccination-related 7Cs (tdf = 314 = 3.78–6.21). Contrary to Hypothesis 4a, the influenza vaccination-related CalculationR (r = −0.146) is associated significantly lower than the COVID-19 vaccination-related CalculationR (r = 0.068) with the importance of the influenza vaccination (tdf = 314 = −3.61).
With regard to Hypothesis 4c, both the importance and the implementation of COVID-19 protective measures show, as expected, mostly high correlations with the COVID-19 vaccination-related 7C scales. COVID-19 vaccine-related ComplacencyR (tdf = 314 = −6.71, −5.79), ConstraintsR (tdf = 314 = −5.74, −4.96), CalculationR (tdf = 314 = −2.87, −4.39), Collective Responsibility (tdf = 314 = −3.84, −4.40) are more positively correlated with both criteria variables than corresponding influenza vaccine-related 7C scales. Here, as for the other criterion variables, CalculationR is the only scale for which negative correlations were found.
According to Nagelkerke’s R2, the dichotomous information of influenza vaccination uptake is explained at 0.457 by the influenza vaccination-related 7C scales (significant single predictor: ComplacencyR) and the information of COVID-19 vaccination status at 0.695 by the COVID-19 vaccination-related 7C scales. The corrected multiple variance explanation of the importance assessment of influenza vaccination by the influenza vaccination-related 7C scales is 75.8% (significant predictors: ComplacencyR, ConstraintsR, Collective Responsibility and Compliance), and the importance of COVID-19 vaccination by the COVID-19 vaccination-related 7C scales is 84.1% (significant individual predictors: ComplacencyR, ConstraintsR, Collective Responsibility and ConspiracyR). The importance (significant individual predictors: ComplacencyR, Collective Responsibility) of the general COVID-19 measures and their implementation (no significant individual predictors after Bonferroni corrector) is also high at 50.7 and 38.7%, respectively.
4 Discussion
Using the 7C scale adapted for both influenza and COVID-19 vaccination, a differentiated picture of the facets of vaccination readiness in the final phase of the COVID-19 pandemic could be obtained. The 7C total score indicates a significantly increased readiness to be vaccinated for the COVID-19 vaccination than for the influenza vaccination (Hypothesis 1 confirmed). However, the 7C individual facets should be considered essential, as evidenced by their strong interaction with vaccination types (Hypothesis 2 confirmed): Higher Confidence and ConspiracyR for influenza vaccination (Hypothesis 2a confirmed) are in line with skeptical concerns discussed in the media and in public due to the unusually short-term development of the COVID-19 vaccine based on a new vaccination principle (Anand and Stahel, 2021; Krause et al., 2023; Peretti-Watel et al., 2024). In contrast, Collective ComplacencyR, Responsibility, and Compliance regarding readiness for COVID-19 vaccination proved to be particularly high (Hypothesis 2b confirmed). This reflects the urgent public relevance of overcoming health risks resulting from the pandemic, esp. for vulnerable risk groups (Anas et al., 2023), as well as the restrictions in public, social, and economic life (Sprengholz et al., 2021) caused by the comprehensive infection protection measures (Terrell et al., 2023).
Contrary to Hypothesis 2c, the benefits of COVID-19 vaccination seem to subordinate potential constraints associated with vaccination (e.g., immediate vaccination reaction). However, a considerable interaction effect in line with Hypothesis 3 must be regarded: If there is no influenza vaccination recommendation, the ContraintsR differences between the two vaccination types are significantly greater than if influenza vaccination is recommended. Similarly, Collective Responsibility also differs for the two types of vaccination only if an influenza vaccination recommendation is given, which is in line with expectations, as these people are more likely to have contact with risk groups, e.g., professionally or due to their own age. No interaction effect with the influenza vaccination recommendation was found for the other 7C scales (Hypothesis 3 rejected), indicating that these responses on vaccination readiness were largely independent of the risk perception for oneself and for social interaction partners.
Geiger et al. (2021) emphasize the research desideratum to examine the differential measurement properties of the 7C subscales in various application contexts and for different types of vaccination. In their study, the psychometric properties of the seven individual scales proved to be rather unsatisfactory, as the cross-scale main factor “General vaccination readiness” turned out to be the dominant source of variance. Our study made a significant contribution to this by demonstrating the strong vaccine type-dependent profiles according to Hypothesis 2. Furthermore, the selective responsiveness of the individual scales (Hypothesis 2b), which are theoretically most closely related to the special circumstances of the COVID-19 pandemic (especially infection control, social coexistence; Sprengholz et al., 2021; Watson et al., 2022), underpin their factorial validity (Messick, 1995). In addition, the satisfactory internal consistencies (ω > 0.770) of 6 of the seven individual scales with moderate scale intercorrelations for both vaccination types also indicate an overall psychometrically stable factorial structure. It should be noted here that Geiger et al. (2021) determined the internal consistencies according to McDonald’s ω within the framework of bi-factor modeling, where the main factor, “General vaccination readiness” related variance, is partialized out before calculating the factor reliabilities. Thus, the reliability estimates reflect the internal consistency of the residual variance components that are not explained by the main factor. For the CalculationR factor, however, the internal consistency estimates of ω = 0.537 and 0.583 are similar to those of Geiger et al. (2021; ω = 0.520): Since only the CalculationR items, in contrast to the other 18 items, proved to be very weakly associated with the general factor, in our study similar estimates resulted as for the bi-factor modeling (Geiger et al., 2021). Furthermore, in accordance with Geiger et al. (2021), Schindler et al. (2020), and Neufeind et al. (2021), the CalculationR scale was found to be strikingly weaker associated with the validation criteria in the correlation and regression analyses than the other 7C subscales. The contents of CalculationR items reflect the assumption that a conscious risk–benefit calculation indicates a limited readiness to be vaccinated. However, the empirical findings suggest that a cost–benefit assessment could also indicate a desirable characteristic of rational user behavior in people who are willing to be vaccinated (Rees et al., 2022; Wilder-Smith et al., 2017).
The findings of Geiger et al. (2021) regarding the criteria validity of the 7C scale were well replicated, with 84.1% of the variance in importance assessment and information modeling for dichotomous vaccination status explained (Nagelkerke-R2 = 0.695). The lower variance explanation for influenza vaccination (75.8%; Nagelkerke-R2 = 0.457) may indicate that willingness to be vaccinated against COVID-19 is more closely linked to actual behavior (Betsch et al., 2015), likely due to the heightened emphasis on individual and social protection during the pandemic (Chevallier et al., 2021). This is further supported by the fact that for COVID-19 vaccination, vaccination status is significantly more correlated with COVID-19-related ConstraintsR and Collective Responsibility (r = 0.628, 0.740) than is the case for influenza vaccination status and the corresponding influenza-related 7C subscales (r = 0.489, 0.480).
4.1 Limitations
One of the limitations of this study was that it used only a convenience sample, which was carried out via online channels under the special contact restrictions of the COVID-19 pandemic. Due to the corresponding representativeness restrictions, conclusions about the general conditions in the German population are limited. However, as the questions are not epidemiological but instead refer in particular to differential measurement properties of the 7C scale for two vaccination types, this restriction was accepted as being of minor importance for the study design. The information on vaccination status and the criteria for an influenza vaccination recommendation are based on self-reporting within an anonymous online collection setting. Although there are no indications that incorrect information may have been provided here (e.g., due to memory biases, social desirability, or self-serving biases), it would have been desirable to objectively verify this information. The sample is dominated by young people with a more academic background. A comparatively high percentage of people were vaccinated against COVID-19. Despite the low average age, it was possible to include 135 people (42.6%) in the study for whom an influenza vaccination recommendation was available. Contrary to Hypothesis 3, the presence of an influenza vaccination recommendation only had a marginal effect on the data structure. The associated distortions should be rather moderate. Despite the multitude of statistical tests calculated, economic data analysis was realized by prioritizing the hypotheses (3 main hypotheses), testing the main hypotheses using an integrated ANOVA and hypothesis-specific α-error adjustment, and applying Bonferroni correction of the significance level. Although the high COVID-19 vaccination rate (91%) is highly encouraging for infection protection, it statistically led to the problem of a very skewed distribution of the dichotomous criterion variable in the logistic regression. Accordingly, the ß-weight tests exhibit low test power. Thus, the non-significance (after Bonferroni correction) of all predictors should be interpreted with caution.
The original items of the 7C scale were reformulated specifically for COVID-19 and influenza vaccination. The influenza vaccination-related adaptation proved to be challenging for the Compliance scale, as its contents refer to restrictive protective measures (e.g., exclusion of non-vaccinated persons from public events) appearing inappropriately restrictive for influenza vaccination. Due to this adaptation, the content and difficulty of the corresponding COVID-19 vs. influenza-related Compliance items may limit the fairness of the comparison between vaccination types. Since individual and public living conditions were subject to considerable changes during and after the pandemic due to the dynamics of the risk of infection, the findings presented can only claim validity with regard to the final phase of the pandemic. For this observational study, it should be noted that causal conclusions are not permissible due to the correlative statistics and mean value comparisons. As we have chosen a diagnostic or assessment focus for the study content, this is not considered critical in terms of our study objective. However, no statements about mechanisms of action or time courses may be regarded as confirmed by the study findings. It would have been desirable to be able to analyze qualitative survey data in addition to the quantitative data. This could have contributed to a deeper understanding of the significance of the assessed data, particularly with regard to the qualitative differences between the two forms of vaccination. Such a mixed-methods approach could be considered in future research to test and increase the validity of the study findings on vaccine-specific readiness to be vaccinated.
4.2 Future research
The conditions underlying the hypotheses on the different readiness to be vaccinated for the two types of vaccine are subject to changes over time (Abate et al., 2024; Harada and Watanabe, 2021; Leonardelli et al., 2023): By now, the special pandemic-related living conditions have passed, and the risk of COVID-19 infections is no longer a dominating factor in individual and societal everyday life. This is due to both a higher immunity in the population and a weakening of the virus variants (RKI, 2024b). In this respect, the experience of threat should be reduced, and it could be assumed that this will have an impact at least on the facets of Collective Responsibility, ComplacencyR, ConstraintsR and Compliance for COVID-19.
In contrast, the increasing experience and approval of COVID-19 vaccinations (Geoghegan et al., 2020) should lead to an improvement in the previously lower Confidence and ConspiracyR. Thus, it would be instructive to investigate whether and which vaccine- and risk-related aspects (Dombrádi et al., 2021; Enria et al., 2024; Jabkowski et al., 2023; Dubé et al., 2013; SteelFisher et al., 2023) and associated changes in public perception influence attitudes toward COVID-19 vaccination. This should provide valuable insights into the nature of the construct of vaccination readiness and contribute to a differentiated and more valid understanding (Dubé et al., 2013; MacDonald, 2015; Spier, 2001). A future convergence of readiness for vaccination against COVID-19 and influenza would indicate that more general, vaccine-independent attitudes determine vaccination readiness and its structural components.
Across different countries, varying levels of trust in government, healthcare systems, and social influences were found to be determinants of vaccine acceptance (Abate et al., 2024; Alper et al., 2020; Shi et al., 2024; Huang et al., 2022; Leong et al., 2022; Rosen et al., 2021). Future studies should strive to shed light on how different cultural contexts interact with individual vaccination-related beliefs and attitudes (Petráš et al., 2022; Shi et al., 2024). First, for a deeper understanding of vaccination-related attitudes and valid conception interventions, the level of the individual and the level of informing and supplying health authorities must be understood in their interplay. For e.g., trust in public health authorities and the government is known to moderate vaccine acceptance systematically (Leong et al., 2022). Considering the sub-factors of vaccination readiness according to the 7C approach enables a more differentiated understanding (i) of the facets of the construct of vaccination readiness as well as (ii) the influences of the healthcare system and the provision of information on these construct facets (Guan et al., 2024; Terrell et al., 2023). Evidence on these aspects is important in order to shape communication and political measures in such a way that the acceptance of the vaccine can be effectively increased. Second, research should investigate the impact of social influence and conformity in shaping vaccination attitudes and behavior, particularly in contrast to collectivist cultures like China, where community norms affect individual choices more strongly, and more individualistic Western cultures (Shi et al., 2024). Finally, further work is needed on developing and testing multi-layered interventions, such as combining education, regulatory frameworks, and behavioral nudges, to ensure that strategies are effective across varying health systems and socio-political contexts (Abate et al., 2024; Petráš et al., 2022; Shi et al., 2024; Terrell et al., 2023).
It is reasonable to assume that the fit between the aspects of public health intervention and individual, vaccine-specific attitudes is crucial to the success of interventions to increase willingness to vaccinate (Terrell et al., 2023). The study findings presented here are exemplary in helping to provide a differentiated picture of vaccination readiness in contrast between the two types of vaccination. If future research would succeed in investigating temporal trends in different countries or depending on different intervention approaches, this should prove to be particularly informative for studying the construct of readiness to vaccinate, both with regard to the characteristics of the construct itself and with regard to the determinants that affect its characteristics.
Finally, the fundamental importance of a differentiated understanding of vaccination readiness for appropriate communication on the subject of vaccination, especially between healthcare professionals and laypeople, needs to be emphasized (Ulrich et al., 2022). The COVID-19 pandemic has shown impressively the importance of vaccinations as a crucial tool for preventing severe illnesses, hospitalization, and death from infectious diseases (Wu et al., 2024; Du et al., 2024). Vaccination readiness is a central determinant of the successful implementation and utilization of vaccinations in prevention practice (Geiger et al., 2021; Harada and Watanabe, 2021). Thus, health professionals need to be sensitized and trained to understand and address people’s vaccination-related attitudes effectively (Chou et al., 2021; Dubé et al., 2013; European Centre for Disease Prevention and Control (ECDC), 2024; MacDonald, 2015; WHO, 2021a,b).
The results presented here clarify critical vaccine-specific attitudinal profiles, helping professionals to adopt a more competent and informed approach to vaccination attitudes (Jackson et al., 2023). In a comparison of influenza and COVID-19 vaccination, it was shown that it is important to distinguish sub-facets of vaccination readiness in order to understand and validly assess the individual’s perspective and attitudes toward vaccinations. From the 7C perspective, the overarching construct Vaccination Readiness is differentiated into attitudes toward the vaccine or vaccination offer (Confidence), perception of threat and the need for vaccination (ComplacencyR), cost–benefit assessment (CalculationR), efforts required to receive the vaccine (ConstraintsR), willingness to protect the health of other people and to contribute to community protection (herd immunity; Collective Responsibility), adherence to recommended and socially agreed behaviors (Compliance), as well as resistance to ConspiracyR (esp. fake news and myths). Depending on the individual, medical, and social situation, it is necessary to reflect on these sub-facets to adequately address the phenomenon of vaccination readiness or vaccination hesitancy both situationally and generally (Abate et al., 2024; Chou et al., 2021; Ulrich et al., 2022; WHO, 2021a,b). Depending on the specific risks of infection and the threat of infectious diseases, these findings can help health professionals support those receiving care in making informed decisions about the prevention of infectious diseases through vaccination.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the studies involving humans because this study was conducted parallel and linked to the DFG project “Structural Modeling and Assessment of Health Literacy in Allergy Prevention of New Parents” [G.Z.: WI-3210/7-1]. There, (expectant) parents of infants were surveyed in particular on attitudes toward COVID-19 vaccination. For this DFG funded study an Ethics Statement was approved by Ethics Committee of the German Psychological Society (www.dgps.de/serviceangebote/ethikkommission/; registration number MAW 112018), and the study protocol has been preregistered at the Leibniz Institute of Psychology (ZPID; Wirtz et al., 2021). In the present study the same standards were adhered to and implemented. Informed consent has been obtained for all participants. The study was performed in accordance with the ethical principals in the Declaration of Helsinki. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AS: Validation, Writing – review & editing, Writing – original draft, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. YA: Writing – review & editing, Writing – original draft, Investigation, Data curation, Conceptualization. LO: Writing – review & editing, Writing – original draft, Data curation. MW: Supervision, Resources, Project administration, Methodology, Investigation, Formal analysis, Conceptualization, Writing – review & editing, Writing – original draft, Data curation.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank the study participants who supported our study with their dedicated cooperation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1437942/full#supplementary-material
Abbreviations
5C, 7C, Five, Seven components of vaccination readiness; ANOVA, Analysis of variance; COVID-19, Coronavirus infection prevention 19; ESM, Electronic supplementary material; R, revised; SES, Socioeconomic state; ZPID, Leibniz Insitut for Psychology (Zentraler psychologischer Infrmationsdienst).
Footnotes
1. ^www.dgps.de/serviceangebote/ethikkommission/; registration number MAW 112018.
References
Abate, B. B., Tilahun, B. D., and Yayeh, B. M. (2024). Global COVID-19 vaccine acceptance level and its determinants: an umbrella review. BMC Public Health 24:5. doi: 10.1186/s12889-023-17497-4
Alper, S., Bayrak, F., and Yilmaz, O. (2020). Psychological correlates of COVID-19 conspiracy beliefs and preventive measures: evidence from Turkey. Curr. Psychol. 40, 5708–5717. doi: 10.1007/s12144-020-00903-0
Anand, P., and Stahel, V. P. (2021). Review the safety of COVID-19 mRNA vaccines: a review. Patient Saf. Surg. 15:20. doi: 10.1186/s13037-021-00291-9
Anas, A. L., Salifu, M., and Zakaria, H. L. (2023). COVID-19 pandemic and vaccination skepticism. Hum. Arenas 26, 1–25. doi: 10.1007/s42087-023-00334-w
Betsch, C., Böhm, R., and Chapman, G. B. (2015). Using behavioral insights to increase vaccination policy effectiveness. Policy Insights Behav. Brain Sci. 2, 61–73. doi: 10.1177/2372732215600716
Betsch, C., Schmid, P., Korn, L., Steinmeyer, L., Heinemeier, D., Eitze, S., et al. (2019). Impfverhalten psychologisch erklären, messen und verändern. Bundesgesundheitsblatt 62, 400–409. doi: 10.1007/s00103-019-02900-6
Cardona, B. (2021). The pitfalls of personalization rhetoric in time of health crisis: COVID-19 pandemic and cracks on neoliberal ideologies. Health Promot. Int. 36, 714–721. doi: 10.1093/heapro/daaa112
Chevallier, C., Hacquin, A. S., and Mercier, H. (2021). COVID-19 vaccine hesitancy: shortening the last mile. Trends Cogn. Sci. 25, 331–333. doi: 10.1016/j.tics.2021.02.002
Chou, W.-Y. S., Burgdorf, C. E., Gaysynsky, A., and Hunter, C. M. (2021). COVID-19 vaccination communication: applying behavioral and social science to address vaccine hesitancy and foster vaccine confidence. Bethesda (Maryland): National Health Institute (NIH).
de Fougerolles, T. R., Baïssas, T., Perquier, G., Vitoux, O., Crépey, P., Bartelt-Hofer, H., et al. (2024). Public health and economic benefits of seasonal influenza vaccination in risk groups in France, Italy, Spain, and the UK: state of play and perspectives. BMC Public Health 24:1222. doi: 10.1186/s12889-024-18694-5
Dhamanti, I., Suwantika, A. A., Adlia, A., Yamani, L. N., and Yakub, F. (2023). Adverse reactions of COVID-19 vaccines: a scoping review of observational studies. Int. J. Gen. Med. 16, 609–618. doi: 10.2147/IJGM.S400458
Dombrádi, V., Joó, T., Palla, G., Pollner, P., and Belicza, É. (2021). Comparison of hesitancy between COVID-19 and seasonal influenza vaccinations within the general Hungarian population: a cross-sectional study. BMC Public Health 21:2317. doi: 10.1186/s12889-021-12386-0
Du, H., Saiyed, S., and Gardner, L. M. (2024). Association between vaccination rates and COVID-19 health outcomes in the United States: a population-level statistical analysis. BMC Public Health 24:220. doi: 10.1186/s12889-024-17790-w
Dubé, E., Laberge, C., Guay, M., Bramadat, P., Roy, R., and Bettinger, J. (2013). Vaccine hesitancy. Hum. Vaccines Immunother. 9, 1763–1773. doi: 10.4161/hv.24657
Eitze, S., Felgendreff, L., Horstkötter, N., Seefeld, L., and Betsch, C. (2024). Exploring pre-pandemic patterns of vaccine decision-making with the 5C model: results from representative surveys in 2016 and 2018. BMC Public Health. 24:1205. doi: 10.1186/s12889-024-18674-9
Enria, L., Dwyer, H., Marchant, M., Beckmann, N., Schmidt-Sane, M., Conteh, A., et al. (2024). Political dimensions of misinformation, trust, and vaccine confidence in a digital age. BMJ 385:e079940. doi: 10.1136/bmj-2024-079940
Eurofound (2021). German infection protection act, measure DE-2021-48/2043 (measures in Germany). Dublin: EU PolicyWatch.
European Centre for Disease Prevention and Control (ECDC) (2024). Effective communication around the benefit and risk balance of vaccination in the EU/EEA. Stockholm: ECDC.
Geiger, M., Rees, F., Lilleholt, L., Santana, A. P., Zettler, I., Wilhelm, O., et al. (2021). Measuring the 7Cs of vaccination readiness. Eur. J. Psychol. Assess. 38, 261–269. doi: 10.1027/1015-5759/a000663
Geoghegan, S., O’Callaghan, K. P., and Offit, P. A. (2020). Vaccine safety: myths and misinformation. Front. Microbiol. 11:372. doi: 10.3389/fmicb.2020.00372
Grohskopf, L. A., Ferdinands, J. M., Blanton, L. H., Broder, K. R., and Loehr, J. (2024). Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices—United States, 2024–25 influenza season. MMWR Recomm. Rep. 73, 1–25. doi: 10.15585/mmwr.rr7305a1
Guan, H., Zhang, L., Chen, X., Zhang, Y., Ding, Y., and Liu, W. (2024). Enhancing vaccination uptake through community engagement: evidence from China. Sci. Rep. 14:10845 (2024). doi: 10.1038/s41598-024-61583-5
Harada, T., and Watanabe, T. (2021). Changes in vaccine hesitancy in Japan across five months during the COVID-19 pandemic and its related factors. Vaccines 10:25. doi: 10.3390/vaccines10010025
Hemmerich, W. (2017). Comparing correlations statistically, in German. Available at: statistikguru.de/rechner/korrelationen-vergleichen.html (Accessed May 15, 2024).
Hoebel, J., Müters, S., Kuntz, B., Lange, C., and Lampert, T. (2015). Measuring subjective social status in health research with a German version of the MacArthur scale; in German. Bundesgesundheitsblatt 58, 749–757. doi: 10.1007/s00103-015-2166-x
Huang, Y., Su, X., Xiao, W., Wang, H., Si, M., Wang, W., et al. (2022). COVID-19 vaccine hesitancy among different population groups in China: a national multicenter online survey. BMC Infect. Dis. 22:153. doi: 10.1186/s12879-022-07111-0
Jabkowski, P., Domaradzki, J., and Baranowski, M. (2023). Exploring COVID-19 conspiracy theories: education, religiosity, trust in scientists, and political orientation in 26 European countries. Sci. Rep. 13:18116. doi: 10.1038/s41598-023-44752-w
Jackson, C., Smith, S., Aghasaryan, A., Andreasyan, D., Aregay, A. K., Bach, K., et al. (2023). Barriers and drivers of positive COVID-19 vaccination behaviours among healthcare workers in Europe and Central Asia: a qualitative cross-country synthesis. Humanit. Soc. Sci. Commun. 10:926. doi: 10.1057/s41599-023-02443-x
Krause, N. M., Beets, B., Howell, E. L., Tosteson, H., and Scheufele, D. A. (2023). Collateral damage from debunking mRNA vaccine misinformation. Vaccine 41, 922–929. doi: 10.1016/j.vaccine.2022.12.045
Larson, H. J., Jarrett, C., Eckersberger, E., Smith, D. M., and Paterson, P. (2014). Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine 32, 2150–2159. doi: 10.1016/j.vaccine.2014.01.081
Lee, S. K., Sun, J., Jang, S., and Conelly, S. (2022). Misinformation of COVID-19 vaccines and vaccine hesitancy. Sci. Rep. 12:13681. doi: 10.1038/s41598-022-17430-6
Leonardelli, M., Mele, F., Marrone, M., Germinario, C. A., Tafuri, S., Moscara, L., et al. (2023). The effects of the COVID-19 pandemic on vaccination hesitancy: a viewpoint. Vaccine 11:1191. doi: 10.3390/vaccines11071191
Leong, C., Jin, L., Kim, D., Kim, J., Teo, Y. Y., and Ho, T. H. (2022). Assessing the impact of novelty and conformity on hesitancy towards COVID-19 vaccines using mRNA technology. Commun. Med. (Lond) 2:61. doi: 10.1038/s43856-022-00123-6
Loseva, P. (2022). Data and distrust hamper Russia’s vaccination programme. BMJ 376:o321. doi: 10.1136/bmj.o321
MacDonald, N. E. (2015). Vaccine hesitancy: definition, scope and determinants. Vaccine 33, 4161–4164. doi: 10.1016/j.vaccine.2015.04.036
MacDonald, N., Mohsni, E., Al-Mazrou, Y., Kim Andrus, J., Arora, N., Elden, S., et al. (2020). Global vaccine action plan lessons learned I: recommendations for the next decade. Vaccine 38, 5364–5371. doi: 10.1016/j.vaccine.2020.05.003
Messick, S. (1995). Validity of psychological assessment. Am. Psychol. 50, 741–749. doi: 10.1037/0003-066X.50.9.741
Neufeind, J., Betsch, C., Zylka-Menhorn, V., and Wichmann, O. (2021). Determinants of physician attitudes towards the new selective measles vaccine mandate in Germany. BMC Public Health 21:566. doi: 10.1186/s12889-021-10563-9
Nicholls, L. A. B., Gallant, A., Cogan, N., Rasmussen, S., Young, D., and Williams, L. (2021). Older adults’ vaccine hesitancy: psychosocial factors associated with influenza, pneumococcal, and shingles vaccine uptake. Vaccine 39, 3520–3527. doi: 10.1016/j.vaccine.2021.04.062
Omer, S. B., Salmon, D. A., Orenstein, W. A., deHart, M. P., and Halsey, N. (2009). Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N. Engl. J. Med. 360, 1981–1988. doi: 10.1056/NEJMsa0806477
Peretti-Watel, P., Verger, P., and Ward, J. K. (2024). To understand mRNA vaccine hesitancy, stop calling the public anti-science. Nat. Med. 30, 923–924. doi: 10.1038/s41591-024-02816-y
Petráš, M., Máčalík, R., Janovská, D., Čelko, A. M., Dáňová, J., Selinger, E., et al. (2022). Risk factors affecting COVID-19 vaccine effectiveness identified from 290 cross-country observational studies until February 2022: a meta-analysis and meta-regression. BMC Med. 20:461. doi: 10.1186/s12916-022-02663-z
Prada, E., Langbecker, A., and Catalan-Matamoros, D. (2023). Public discourse and debate about vaccines in the midst of the covid-19 pandemic: a qualitative content analysis of twitter. Vaccine 41, 3196–3203. doi: 10.1016/j.vaccine.2023.03.068
Rahbeni, T. A., Satapathy, P., Itumalla, R., Marzo, R. R., Mugheed, K. A. L., Khatib, M. N., et al. (2024). COVID-19 vaccine hesitancy: umbrella review of systematic reviews and meta-analysis. JMIR Public Health Surveill. 10:e54769. doi: 10.2196/54769
Rees, F., Geiger, M., Lilleholt, L., Zettler, I., Betsch, C., Böhm, R., et al. (2022). Measuring parents' readiness to vaccinate themselves and their children against COVID-19. Vaccine 40, 3825–3834. doi: 10.1016/j.vaccine.2022.04.091
RKI (2022). Recommendations of the standing committee on vaccination at the Robert Koch institute 2022; in German. Epid. Bull. 4, 3–67. doi: 10.25646/9285
RKI (2023). Vaccination against influenza (flu); in German. Available at: www.rki.de/DE/Content/Infekt/Impfen/ImpfungenAZ/Influenza/Influenza.html (Accessed May 15, 2024).
RKI (2024a). Digital vaccination rate monitoring for COVID-19 vaccination; in German. Available at: www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Daten/Impfquoten-Tab.html (Accessed September 03, 2024).
RKI (2024b). COVID-19 (coronavirus SARS-CoV-2); in German. Available at: www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/nCoV.html (Accessed September 28, 2024).
Robinson, R., Nguyen, E., Wright, M., Holmes, J., Oliphant, C., Cleveland, K., et al. (2022). Factors contributing to vaccine hesitancy and reduced vaccine confidence in rural underserved populations. Humanit. Soc. Sci. Commun. 9:416. doi: 10.1057/s41599-022-01439-3
Roettele, N., and Wirtz, M. A. (2020). Analyzing the informational content of observational and raring data, in German. Rehabilitation 59, 182–192. doi: 10.1055/a-0955-6470
Rosen, B., Waitzberg, R., Israeli, A., Hartal, M., and Davidovitch, N. (2021). Addressing vaccine hesitancy and access barriers to achieve persistent progress in Israel's COVID-19 vaccination program. Isr. J. Health Policy Res. 10:43. doi: 10.1186/s13584-021-00481-x
Schindler, J., Schindler, S., and Pfattheicher, S. (2020). The role of intuition in vaccination attitudes. J. Health Psychol. 26, 2950–2957. doi: 10.1177/1359105320925160
Seddig, D., Maskileyson, D., Davidov, E., Ajzen, I., and Schmidt, P. (2022). Correlates of COVID-19 vaccination intentions: attitudes, institutional trust, fear, conspiracy beliefs, and vaccine skepticism. Soc. Sci. Med. 302:114981. doi: 10.1016/j.socscimed.2022.114981
Shi, J., Kim, H. K., Salmon, C. T., Tandoc, E. C., and Goh, Z. H. (2024). Cultural tightness–looseness and normative social influence in eight Asian countries: associations of individual and collective norms with vaccination intentions. Soc. Sci. Med. 340:116431. doi: 10.1016/j.socscimed.2023.116431
Soares, P., Rocha, J. V., Moniz, M., Gama, A., Laires, P. A., Pedro, A. R., et al. (2021). Factors associated with COVID-19 vaccine hesitancy. Vaccines 9:300. doi: 10.3390/vaccines9030300
Spier, R. E. (2001). Perception of risk of vaccine adverse events: a historical perspective. Vaccine 20, S78–S84. doi: 10.1016/S0264-410X(01)00306-1
Sprengholz, P., Felgendreff, L., Böhm, R., and Betsch, C. (2021). Vaccination policy reactance: predictors, consequences, and countermeasures. J. Health Psychol. 27, 1394–1407. doi: 10.1177/13591053211044535
Statista (2022a). Influenza in Germany; in German. Available at: https://de.statista.com/themen/7721/influenza-in-deutschland/ (Accessed May 15, 2024).
Statista (2022b). Vaccination rate against the coronavirus (COVID-19) in Germany since the start of the vaccination campaign in December 2020; in German. Available at: https://de.statista.com/statistik/daten/studie/1196966/umfrage/impfquote-gegen-das-coronavirus-in-deutschland/ (Accessed May 15, 2024).
SteelFisher, G. K., Findling, M. G., Caporello, H. L., McGowan, E., Espino, L., and Sutton, J. (2023). Divergent attitudes toward COVID-19 vaccine vs influenza vaccine. JAMA Netw. Open 6:e2349881. doi: 10.1001/jamanetworkopen.2023.49881
Terrell, R., Alami, A., and Krewski, D. (2023). Interventions for COVID-19 vaccine hesitancy: a systematic review and narrative synthesis. Int. J. Environ. Res. Public Health 20:6082. doi: 10.3390/ijerph20126082
Troiano, G., and Nardi, A. (2021). Vaccine hesitancy in the era of COVID-19. Public Health 194, 245–251. doi: 10.1016/j.puhe.2021.02.025
Ulrich, A. K., Sundaram, M. E., and Basta, N. E. (2022). Supporting individual vaccine decision-making: a role for vaccination counselors. Vaccine 40, 2123–2125. doi: 10.1016/j.vaccine.2022.02.012
Ward, J. K., Alleaume, C., Peretti-Watel, P., Seror, V., Cortaredona, S., Launay, O., et al. (2020). The French public's attitudes to a future COVID-19 vaccine: the politicization of a public health issue. Soc. Sci. Med. 265:113414. doi: 10.1016/j.socscimed.2020.113414
Watson, O., Barnsley, G., Toor, J., Hogan, A. B., Winskill, P., and Ghani, A. C. (2022). Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect. Dis. 22, 1293–1302. doi: 10.1016/S1473-3099(22)00320-6
WHO (2021b). Communicating with patients about COVID-19 vaccination: evidence-based guidance for effective conversations to promote COVID-19 vaccine uptake. Geneva: WHO.
Wilcox, R. R., and Tian, T. (2008). Comparing dependent correlations. J. Gen. Psychol. 135, 105–112. doi: 10.3200/GENP.135.1.105-112
Wilder-Smith, A., Longini, I., Zuber, P. L., Bärnighausen, T., Edmunds, W. J., Dean, N., et al. (2017). The public health value of vaccines beyond efficacy: methods, measures and outcomes. BMC Med. 15:138. doi: 10.1186/s12916-017-0911-8
Wirtz, M. A., Dresch, J., and Schulz, A. A. (2021). Structural modelling and assessment of health literacy in allergy prevention of new parents by means of Item-Response-Theory. Psych Archives. doi: 10.23668/psycharchives.4551
Wu, N., Joyal-Desmarais, K., Ribeiro, P. A. B., Vieira, A. M., Stojanovic, J., and Sanuade, C. (2024). Long-term effectiveness of COVID-19 vaccines against infections, hospitalisations, and mortality in adults: findings from a rapid living systematic evidence synthesis and meta-analysis up to December, 2022. Lancet Resp. Med. 11, 439–452. doi: 10.1016/S2213-2600(23)00015-2
Keywords: vaccination readiness, vaccination hesitancy, 7C-scale, motives for vaccination, beliefs about vaccination, health prevention behavior, collective responsibility
Citation: Schulz AA, Abt Y, von Oppen L and Wirtz MA (2024) Readiness for influenza and COVID-19 vaccination in Germany: a comparative analysis. Front. Psychol. 15:1437942. doi: 10.3389/fpsyg.2024.1437942
Edited by:
Rizwan Ahmed Laar, Hubei Normal University, ChinaCopyright © 2024 Schulz, Abt, von Oppen and Wirtz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Markus A. Wirtz, bWFya3VzLndpcnR6QHBoLWZyZWlidXJnLmRl
 Anja A. Schulz
Anja A. Schulz Yvonne Abt
Yvonne Abt Linus von Oppen
Linus von Oppen Markus A. Wirtz
Markus A. Wirtz