- Applied Health, School of Health and Biomedical Sciences, RMIT University, Melbourne, VIC, Australia
Background: The healthcare sector is acknowledged as a complex and challenging field. Increasingly, research highlights the importance of healthcare workers’ internal social and emotional skills in managing their well-being and enhancing their capacity to provide patient care and support to colleagues. Emotional Intelligence (EI) has been identified as a key factor in improving the health and performance of healthcare workers, leading to the implementation of numerous programs aimed at enhancing EI.
Objective: This meta-analysis aims to evaluate the effectiveness of EI training interventions among healthcare workers, focusing on various intervention designs and their impact on EI improvement.
Methods: The review encompassed 17 longitudinal studies, each implementing EI training interventions for healthcare workers aged 18 and over. The studies employed a variety of research designs.
Results: All studies demonstrated an increase in EI following the intervention. However, methodological limitations within these studies might have led to an overestimation of the actual effects of the interventions.
Conclusion: While the reviewed studies indicate a positive trend in EI enhancement post-intervention, the potential overestimation of effects due to methodological flaws necessitates caution. The findings underline the need for future research to explore the optimal duration and delivery methods for EI training in healthcare settings.
Systematic review registration: The systematic review and meta-analysis have been pre-registered with PROSPERO [CRD42023393760]. Further details can be accessed at: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023393760.
1 Introduction
The global healthcare sector is facing an escalating crisis in sustaining its workforce (Liu et al., 2017). This multifaceted challenge encompasses three key areas: (1) availability, referring to the existing pool of healthcare professionals; (2) distribution, focusing on the successful recruitment and retention of qualified staff; and (3) performance, relating to the productivity and quality of healthcare services provided (Liu et al., 2017). Numerous factors contribute to this complex issue. The healthcare environment is inherently challenging, marked by unique stressors such as demanding shift patterns, intense working conditions, and high workload pressures. Additionally, healthcare professionals often encounter workplace aggression (Mento et al., 2020), experience burnout, and face various psychosocial hazards, including job insecurity, workplace satisfaction issues, and the delicate balance between work and family life (Coutinho et al., 2018). Despite these hurdles, the effectiveness of patient-centred healthcare relies heavily on the collaborative efforts of healthcare personnel, who must work in unison with each other, the patients, and the broader health system (Santana et al., 2018).
The inherent occupational challenges impact patient care/experiences, healthcare team dynamics/efficiencies and workforce wellbeing. In relation to healthcare provision, the interpersonal behavior and approach of healthcare workers has shown to have a demonstrable direct impact on patient satisfaction, with kindness and empathy by physicians and nurses ranking only behind clinical outcomes as the most important predictor of global patient satisfaction (Schoenfelder et al., 2011). The pressures of these roles, combined with a range of psychosocial hazards discussed, can lead to occupational burnout (Dyrbye et al., 2017). Occupational burnout is associated with chronic exposure to work stress and is characterised by the qualitative dimensions of emotional exhaustion, cynicism, depersonalisation, and reduced sense of efficacy and meaning. Burnout also impacts patients as it worsens the quality of care, increases the risk of medical errors (Hall et al., 2016), and further reduces patient satisfaction and the therapeutic relationship (Panagioti et al., 2018).
More broadly, burnout among healthcare workers not only profoundly affects their health and well-being but also significantly impacts the functionality of healthcare systems at large. There has been a recent surge in focus on how burnout in healthcare providers correlates with diminished quality of patient care (Karimi et al., 2021). A growing corpus of primary research and systematic reviews has identified links between burnout and various critical aspects of healthcare delivery (Søvold et al., 2021). These include adherence to practice guidelines, communication effectiveness, the incidence of medical errors, patient outcomes, and safety metrics. Occupational burnout is directly linked to heightened occurrences of mental illnesses, psychological distress, trauma, and substance use disorders among healthcare professionals (Søvold et al., 2021; Dyrbye et al., 2019). From a systemic perspective, burnout contributes to increased staff turnover, higher rates of absenteeism, and presenteeism, which is characterized by reduced work performance (Dyrbye et al., 2019; Felton, 1998). These factors collectively lead to a deterioration in the overall quality of clinical care (Felton, 1998).
The potential risks to workers and patients have led to extensive research into factors that encourage positive interactions and effective coping among healthcare workers. A promising area of study is Emotional Intelligence (EI), which has been conceptualized in various ways to capture different facets of emotional and interpersonal skills. Mayer and Salovey (1997: p.10) ability-based model defined EI as “a set of interrelated skills concerning the ability to perceive accurately, appraise, and express emotion; the ability to access and/or generate feelings when they facilitate thought; the ability to understand emotion and emotional knowledge; and the ability to regulate emotions to promote emotional and intellectual growth.” Complementing this, Bar-On’s mixed model, as operationalized by the EQ-i, extends EI to include a broad spectrum of personality-linked traits, such as stress management and interpersonal skills, which are particularly relevant in the healthcare context (O'Connor et al., 2019; Tommasi et al., 2023; Sergi et al., 2021). Additionally, Trait EI, as introduced by Petrides and Furnham, explores self-perceived emotional abilities, such as resilience and adaptability, that align well with the psychological demands experienced by healthcare workers (O'Connor et al., 2019; Tommasi et al., 2023; Sergi et al., 2021). Research in the EI field has demonstrated that a specific set of interpersonal and intrapersonal skills and approaches have a positive impact on both healthcare workers (Vlachou et al., 2016) and the patients they treat (Karimi et al., 2021; O'Connor et al., 2019; Mattingly and Kraiger, 2019; Vlachou et al., 2016; Tawfik et al., 2019). While the prevalence of EI skills training in the healthcare sector is well-documented (Mattingly and Kraiger, 2019; Meyer et al., 2004; Baudry et al., 2018; Aldaod et al., 2019; Jiménez-Picón et al., 2021), the true scope and impact of such training on healthcare professionals remain largely unexplored.
EI training interventions, when effectively applied, have the potential to enhance adaptability, problem-solving skills, and coping strategies, which are critical for healthcare workers facing high-stress environments. Enhanced EI skills have been shown to build psychological resilience and promote improved emotional well-being. This association has some foundation in construct validity as the EI traits described initially by Goleman (2020), comprising empathy, self-awareness, social skills, self-regulation, and motivation, align with many of the characteristics that are impactful in the complex and challenging healthcare environment. There is a need to synthesise the extensive research on emotional intelligence, particularly focusing on the needs of healthcare workers. Recognising this, the present systematic review and meta-analysis aimed to assess the efficacy and workplace impact of EI skills training among healthcare workers.
2 Method
The review was conducted per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist (Page et al., 2021) and the Synthesis Without Meta-analysis (SWiM) guidelines (Campbell et al., 2020) for reporting this study.
2.1 Study selection and eligibility
2.1.1 Participants
Healthcare workers employed in a health setting, aged between 18 to 65 years old.
2.1.2 Condition or domain
This study has focused on EI training intervention among healthcare workers. Only studies that used a validated measure of EI will be considered.
2.1.3 Exposure of interest/intervention
EI training intervention.
2.1.4 Comparator(s)/control
Control groups were present for randomised controlled trials, quasi-experimental control trials, and controlled before-after study designs. In non-randomised experimental groups with before-after scores were employed, treating baseline data as data for the “control” group.
2.1.5 Outcomes
EI, measured as a dependent variable, was the primary outcome. All other meaningful outcome variables were considered as secondary outcomes (e.g., burnout, well-being, and mental health).
2.1.6 Types of studies
Longitudinal design studies examining EI training interventions among healthcare workforces.
2.2 Search strategy
With the help of an experienced librarian, the systematic search was conducted from the 1st of January 1995 until the 31st of August 2022. A three-step search strategy was used.
1. An initial limited search of MEDLINE and PsycINFO were undertaken, followed by an analysis of text words contained in the title and abstract and of the index terms used to describe the article.
2. All identified keywords and index terms have been used to conduct a second search using the following databases: MEDLINE, PsycINFO, and Embase.
3. The reference lists of the retrieved articles and reports were hand-searched.
The following keywords have been used to search the databases with the article title, abstracts and body all searched: emotional intelligence, emotional quotient, EQ, EI, emotional competence; intervention, training, healthcare workers, healthcare, healthcare workforce, and longitudinal study.
2.2.1 Inclusion criteria
The studies that met the following criteria were included in the systematic review:
1. Were written in English, used original data and were published in a peer-reviewed journal;
2. Were conducted among the healthcare workforce (minimum 10 workers per group);
3. Used EI training as an intervention;
4. Measured improvement in EI skills over time as an outcome; and
5. Had a longitudinal design, reporting pre and post-EI skills intervention assessments.
2.2.2 Exclusion criteria
Studies that failed to meet the following criteria were excluded:
1. Only the abstract was available and/or a full-text version could not be located.
2. Secondary data, systematic review, grey literature, non-peer-reviewed publications, or conference abstracts.
2.3 Data collection and analysis
2.3.1 Study selection
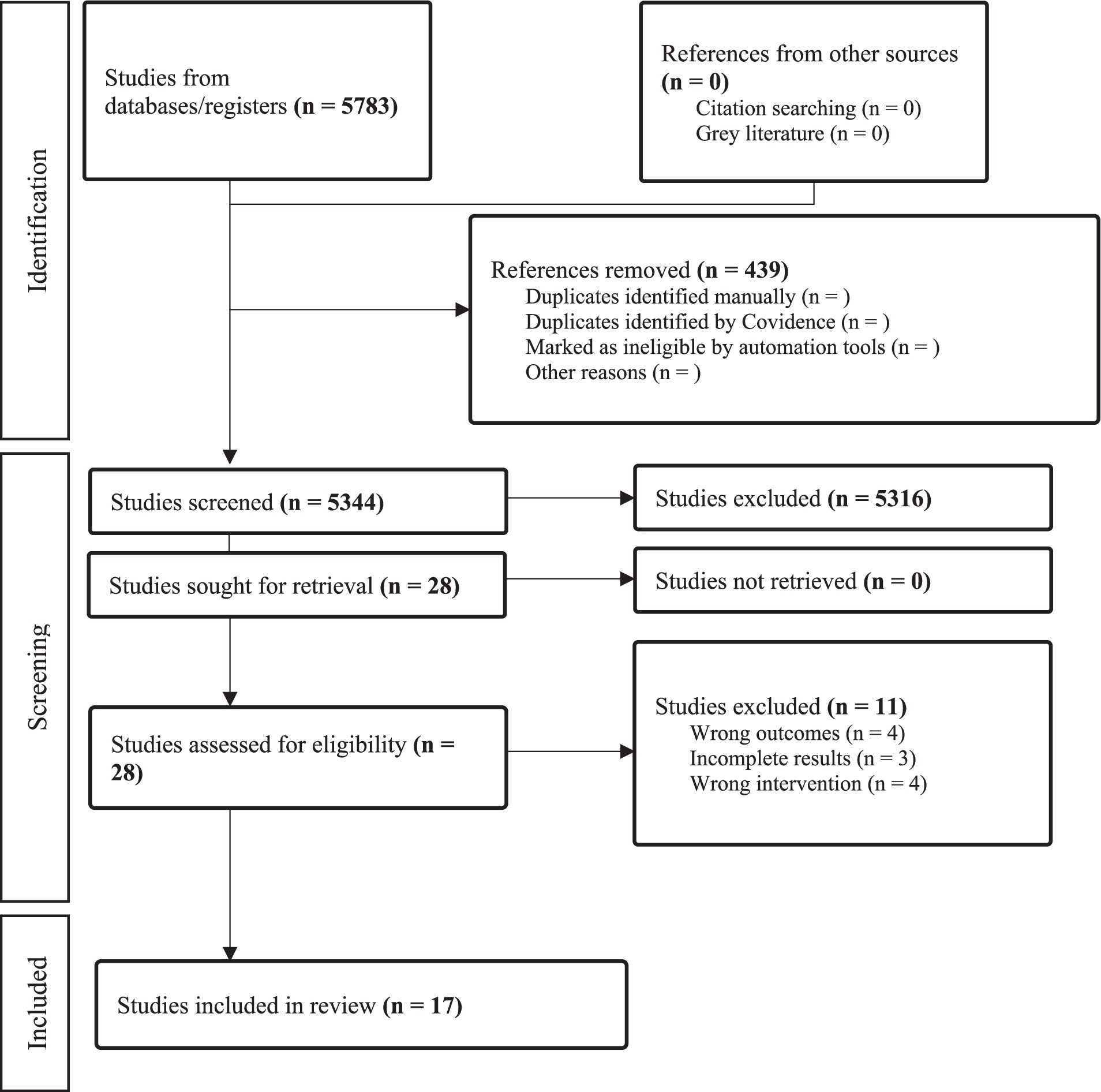
Web-based systematic review software COVIDENCE was used for data selection and screening. All the searched studies were imported to Covidence. The duplicates were removed, and two independent reviewers (CP, YY) screened the references after creating the inclusion and exclusion criteria. The screening was performed in two steps: (a) the title and abstract screening and (b) full-text screening of the selected references. In both steps of the screening, the references were equally distributed between two reviewers, while a third independent reviewer (LK) was consulted when required. Reasons for the exclusion of full-text studies were recorded. The search results for article selection are presented in Figure 1.
2.3.2 Data extraction and management
A template for data extraction was formed using the Synthesis Without Meta-analysis (SWiM) guidelines. Two reviewers (CP, YY) extracted and checked the data of the included studies. The information extracted from each study included:
1. Study characteristics (date of study, title, authors, and research question);
2. Methods (study design, primary outcome, secondary variables, exposure/s, potential confounders, and any other outcomes);
3. Participants’ demographics (country, age, sex, socioeconomic background, hours/week OR working arrangements, e.g., full-time, part-time, casual; and years of experience),
4. Outcomes (name and definition, how it was measured and reported), 5- control group,
5. Statistics (mean differences, their standard errors, p-values or confidence intervals). A second reviewer (CP/YY) cross-checked all extracted data.
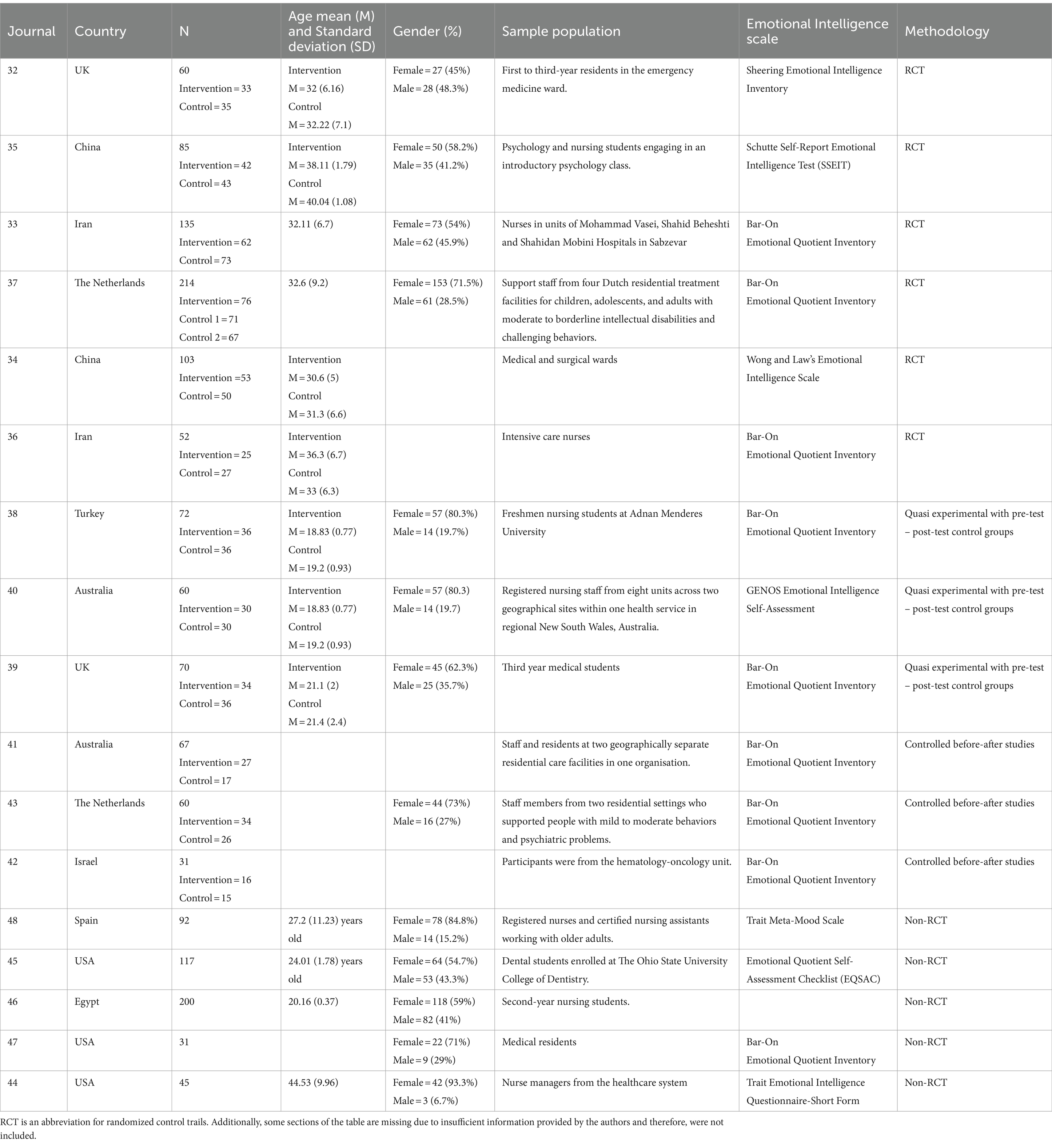
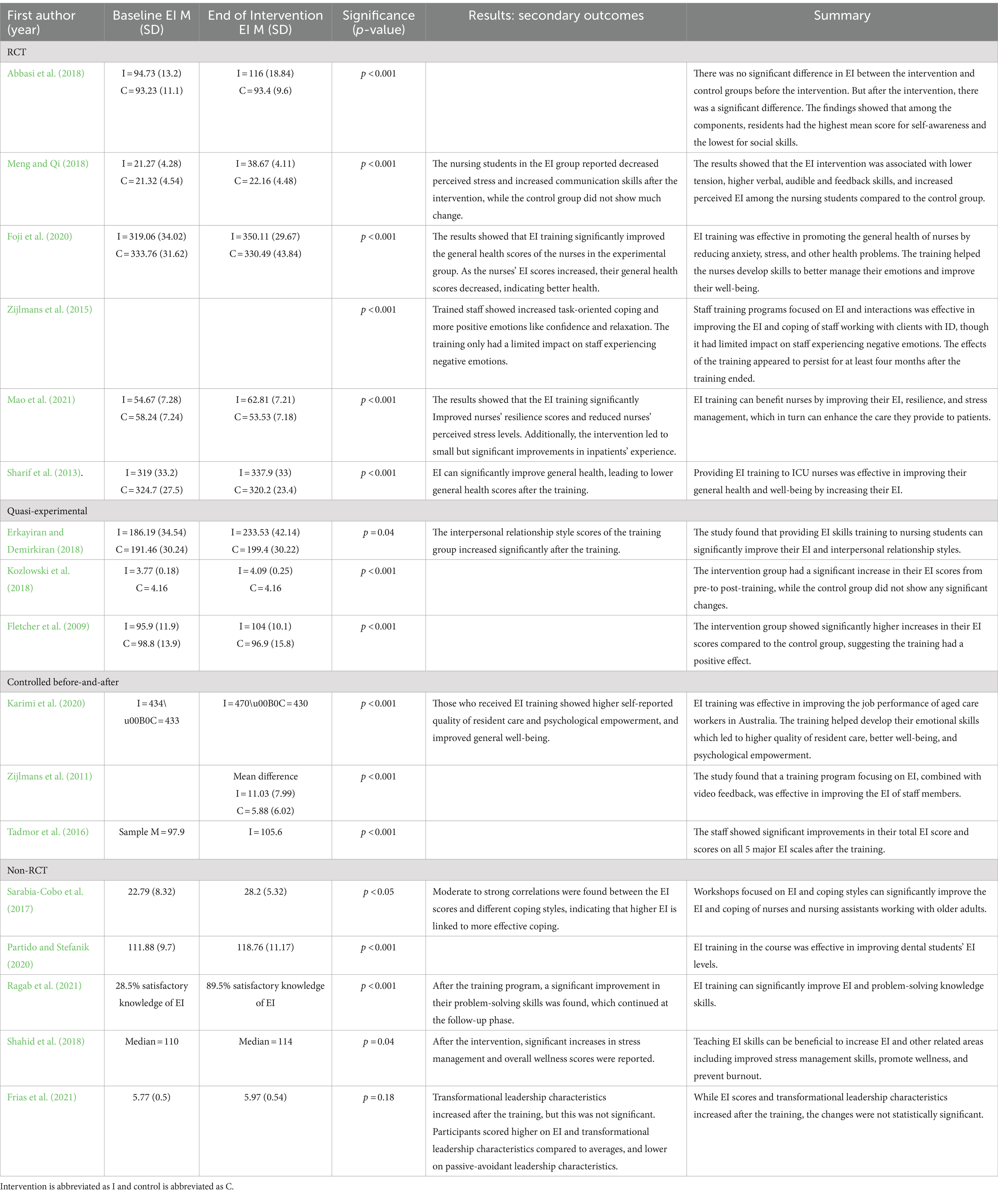
A summary of the included articles is detailed in Table 1.
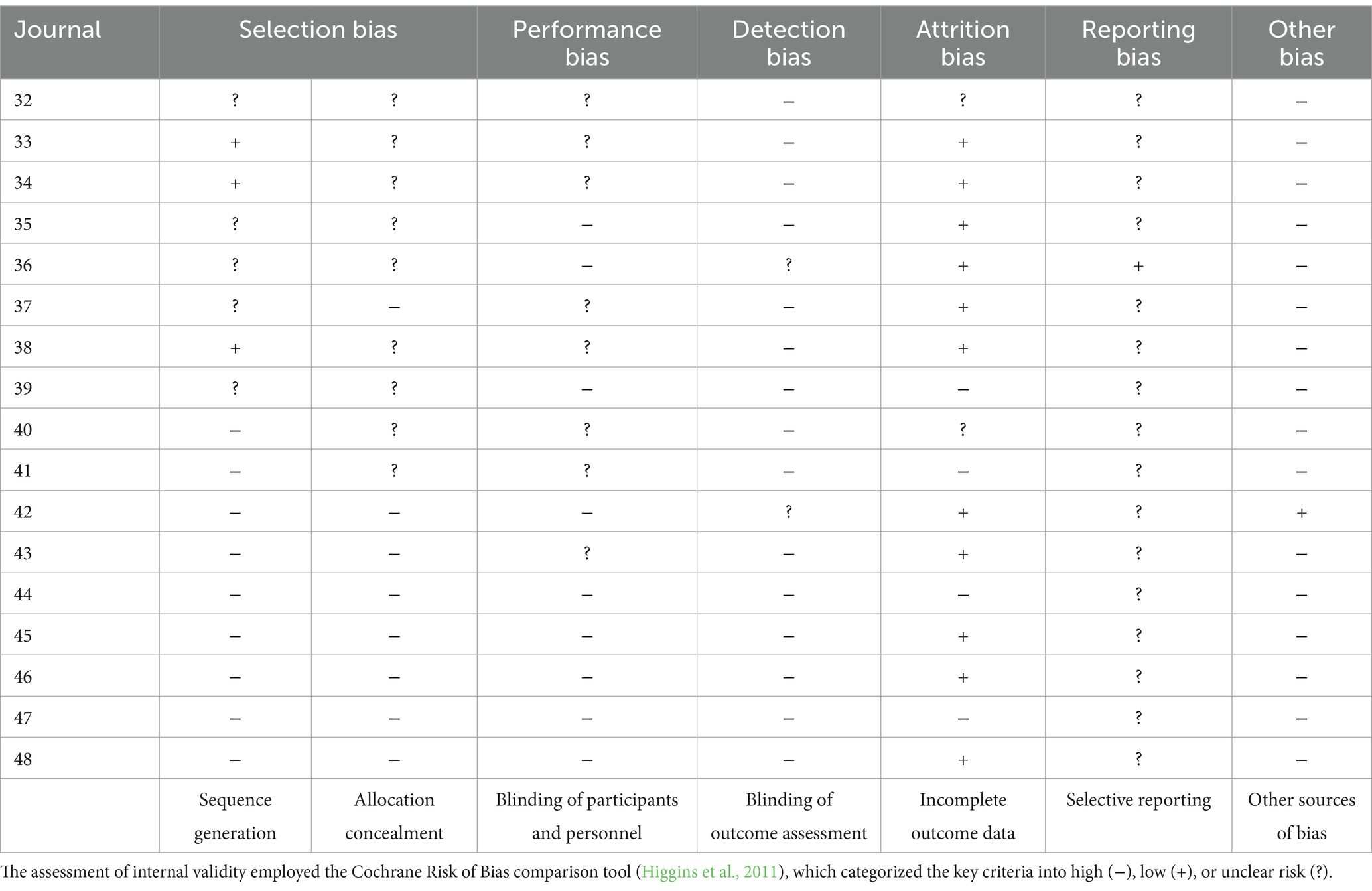
2.3.3 Risk of bias
The present study employed the adapted Cochrane Collaboration risk of bias assessment tool (Higgins et al., 2011), facilitated by the Covidence software, to rigorously evaluate the risk of bias in randomised trials. This tool appraises six distinct domains:
1. Unbiased participant distribution across study groups via random sequence generation and allocation concealment (selection bias);
2. Systematic differences between groups in the control and intervention group, addressed through participant and personnel blinding (performance bias);
3. Examination of outcome assessment blinding with consideration for potential prediction of intervention assignments (detection bias);
4. Addressing the systematic differences between the groups concerning participant withdrawals and information completeness pertaining to attrition and exclusions within the study (attrition bias);
5. Verifying the inclusion of all pre-specified outcomes in the study report (selective outcome reporting) and preventing the omission of outcomes based on their perceived significance or alignment with desired results (reporting bias);
6. Evaluating any unaddressed bias concerns, this broad domain encompasses factors such as disparities in heterogeneity and deviations from intended intervention as reported in the protocol (other biases).
Two independent reviewers (CP/YY) systematically employed the tool to assess each included study, documenting rationale and supporting details for risk of bias judgments in each domain (low, high, unsure). Discrepancies in bias judgments or reasoning were resolved through discussion between the two reviewers, and if needed, a third reviewer adjudicated as a mediator. Following the guidance outlined by Higgins et al. (2011), each domain was analysed, and a summary of bias judgments (low, high, unclear) was furnished.
2.4 Data analysis
The measurement of treatment effects was approached following the recent guidelines for systematic reviews that include both randomised and non-randomised studies (Higgins et al., 2023). For randomised controlled trials (RCTs), the analysis of continuous data employed standardised mean differences (SMD). SMDs were calculated when different instruments or scales were used to measure outcomes. This approach involved dividing the mean score difference between the intervention and control groups by an estimate of the pooled standard deviation, resulting in a ‘scale-free’ effect estimate. This ‘scale-free’ estimate allows for pooling across studies, regardless of the specific measurement scales employed in each study. Effect sizes were interpreted using common thresholds: SMDs less than 0.4 indicated a small effect, SMDs between 0.4 and 0.7 represented a moderate effect, and SMDs greater than 0.7 indicated a large effect (Cohen, 2013). Similarly, this procedure was repeated for studies using quasi-experimental control trials and controlled before-after study designs. In non-randomised experimental groups with before-after score SMD were employed, treating baseline data as data for the “control” group. When feasible, meta-analyses were conducted using MAJOR, a Meta-Analysis tool in Jamovi (Hamilton, 2018).
2.5 Assessment of heterogeneity
Given the diverse range of interventions, measures of EI, and follow-up durations in the included studies, our approach involves combining results from studies with similar designs. A random-effects model was employed to account for the anticipated heterogeneity among these studies. The degree of heterogeneity, represented as tau2, was calculated using the restricted maximum-likelihood estimator (Viechtbauer, 2005). Additionally, the assessment of heterogeneity includes the Q-test (Cochran, 1954) and the I2 statistic. If any level of heterogeneity is identified, signified by tau2 exceeding zero, an accompanying prediction interval for the actual outcomes is furnished.
3 Results
3.1 Study selection
The initial database search yielded a total of 5,783 studies. Following the removal of 439 duplicate records, 5,344 unique studies remained for thorough eligibility assessment. Upon conducting title and abstract screenings, a total of 5,316 studies were identified as irrelevant and subsequently excluded. The remaining 28 articles were independently assessed for eligibility by two reviewers based on the full-text review inclusion and exclusion guidelines. In alignment with these criteria, 11 studies were excluded due to including the wrong intervention of interest (n = 4), wrong outcomes (n = 4), or incomplete reporting of the results (n = 3). Consequently, the systematic review encompassed 17 studies for the final review. These studies included six randomised controlled trials (RCT) (Abbasi et al., 2018; Foji et al., 2020; Mao et al., 2021; Meng and Qi, 2018; Sharif et al., 2013; Zijlmans et al., 2015), three quasi-experimental with pre-test-post-test control designs (Erkayiran and Demirkiran, 2018; Fletcher et al., 2009; Kozlowski et al., 2018), three controlled before-after studies (Karimi et al., 2020; Tadmor et al., 2016; Zijlmans et al., 2011), and five non-randomised experimental designs (Non-RCT) (Frias et al., 2021; Partido and Stefanik, 2020; Ragab et al., 2021; Shahid et al., 2018; Sarabia-Cobo et al., 2017). The PRIMSA flowchart is presented in Figure 1.
3.2 Characteristics of included studies
The studies selected for this review span a publication timeline ranging from July 2009 to December 2021. Participants in the qualified studies were recruited from a range of settings. Twelve studies focused on healthcare settings (Abbasi et al., 2018; Foji et al., 2020; Mao et al., 2021; Sharif et al., 2013; Zijlmans et al., 2015; Kozlowski et al., 2018; Karimi et al., 2020; Tadmor et al., 2016; Zijlmans et al., 2011; Frias et al., 2021; Shahid et al., 2018; Sarabia-Cobo et al., 2017), whereas five studies centred around educational institutions (Meng and Qi, 2018; Erkayiran and Demirkiran, 2018; Fletcher et al., 2009; Partido and Stefanik, 2020; Ragab et al., 2021). Within healthcare settings, participants hailed from various medical domains, including hospital nursing and resident contexts (Foji et al., 2020; Mao et al., 2021; Zijlmans et al., 2015; Kozlowski et al., 2018; Frias et al., 2021), residential care facilities (Karimi et al., 2020; Zijlmans et al., 2011), nursing homes (Sarabia-Cobo et al., 2017), intensive care units (Sharif et al., 2013), hematology-oncology departments (Tadmor et al., 2016), emergency departments (Abbasi et al., 2018), paediatric settings (Sharif et al., 2013), and intense care units (Sharif et al., 2013). Further information concerning the characteristics of the included studies is provided in Table 1.
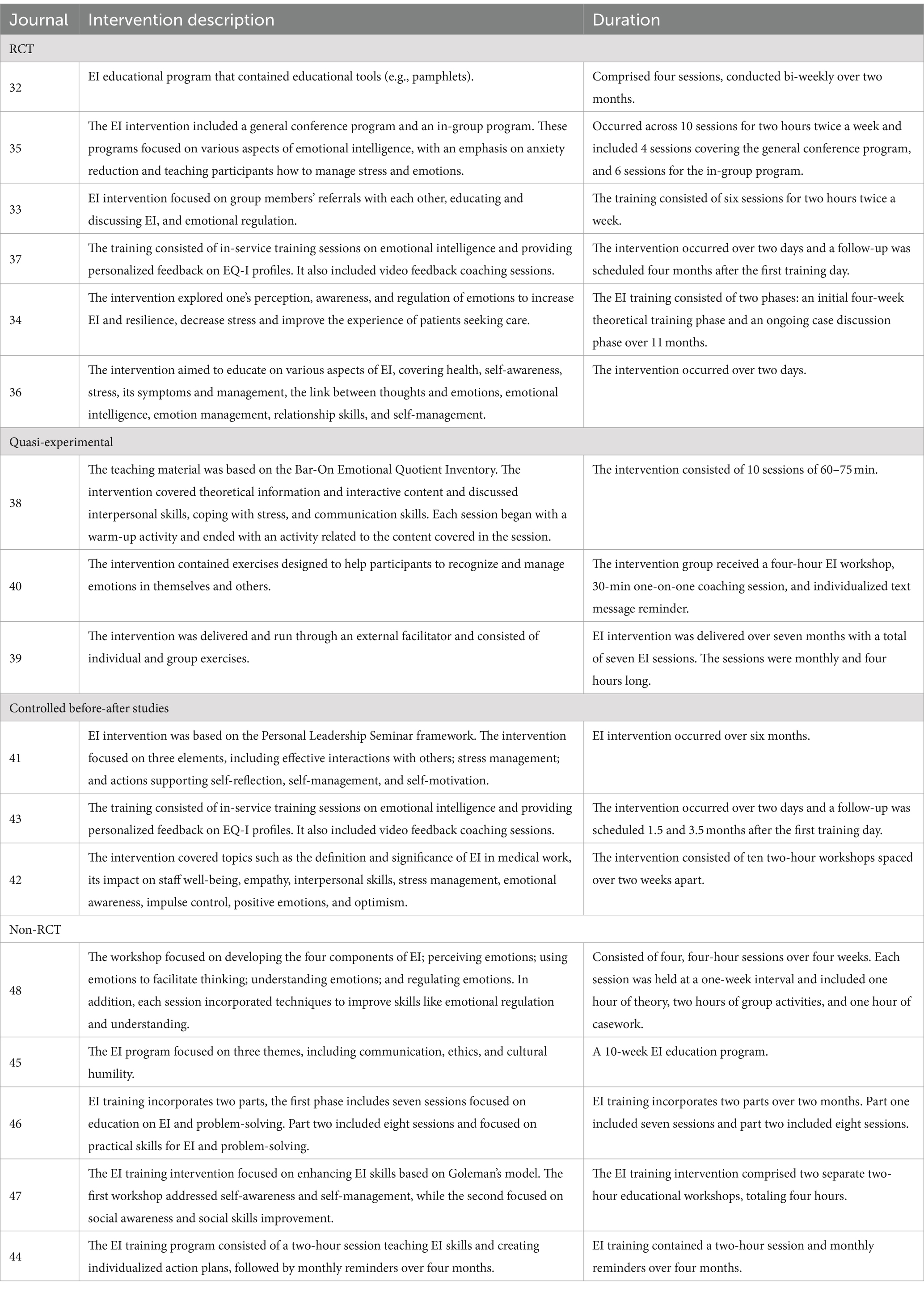
3.2.1 Intervention
The included studies adopted diverse intervention methods to enhance EI among healthcare workers. Four studies focused on enhancing knowledge and understanding of EI (Abbasi et al., 2018; Foji et al., 2020; Sharif et al., 2013; Partido and Stefanik, 2020). This encompassed educational sessions focusing on learning and discussing EI (Foji et al., 2020; Sharif et al., 2013; Partido and Stefanik, 2020) and included educational tools such as pamphlets to further enhance knowledge (Abbasi et al., 2018). In contrast, one study implemented a persuasion intervention using a single, individualised text message (SMS) reminders (Kozlowski et al., 2018). Furthermore, five studies placed a significant emphasis on training to enhance EI skills (Zijlmans et al., 2015; Erkayiran and Demirkiran, 2018; Fletcher et al., 2009; Karimi et al., 2020; Zijlmans et al., 2011). These EI training programs took various forms, encompassing feedback mechanisms (Zijlmans et al., 2015; Zijlmans et al., 2011), group exercises (Erkayiran and Demirkiran, 2018; Fletcher et al., 2009), and skill development sessions (Karimi et al., 2020). Additionally, one study employed enablement techniques, incorporating two behavior change strategies (Frias et al., 2021). In this approach, an individualized action plan was created to integrate EI techniques into daily workflow. Furthermore, seven studies embraced a combination of two or more intervention types (Mao et al., 2021; Meng and Qi, 2018; Kozlowski et al., 2018; Tadmor et al., 2016; Shahid et al., 2018; Sarabia-Cobo et al., 2017). These interventions are summarised in Table 2.
3.2.2 Duration of intervention
Furthermore, the durations of interventions in these studies exhibit noteworthy variations. Some interventions are relatively short-term, spanning just a few hours to a couple of days. For instance, Frias et al. (2021) delivered a concise two-hour training session, while Shahid et al. (2018) and Sharif et al. (2013). Conducted two separate two-hour workshops. In contrast, other interventions reviewed in the studies extended over several weeks to multiple months. For example, both Sarabia-Cobo et al. (2017) and Zijlmans et al. (2011, 2015) incorporated interventions potentially spanning 4 months, while Abbasi et al. (2018) structured the training program over two months with four sessions. A ten-session intervention appeared most popular, with four papers adopting this approach (Meng and Qi, 2018; Erkayiran and Demirkiran, 2018; Tadmor et al., 2016; Partido and Stefanik, 2020). Ragab et al. (2021) divided their intervention into two parts, with the first part comprising seven sessions and the second, eight sessions; however, they did not note the duration of these sessions. On the other hand, several interventions employed a long-term approach, extending over several months (Fletcher et al., 2009; Karimi et al., 2020). For further details on the characteristics of the included studies, refer to Tables 1, 2.
3.3 Risk of bias within studies
The assessment of internal validity employed the Cochrane Risk of Bias comparison tool (Higgins et al., 2011), which categorised the key criteria into high, low, or unclear risk. Two independent assessors (CP/YY) conducted an impartial evaluation of the identified citations. Most studies exhibited a high risk of selection bias. Specifically, approximately 53% were deemed to have a high risk, except for three studies, which were assessed as low risk (Foji et al., 2020; Mao et al., 2021; Erkayiran and Demirkiran, 2018) concerning random sequence generation. The remaining studies fell into the category of unsure risks, primarily attributed to a lack of adequate information regarding the employed randomisation methods, accounting for about 29% of the studies. This uncertainty also extended to attempts to conceal the allocation sequence, with eight studies identified as having a high risk (Zijlmans et al., 2015; Tadmor et al., 2016; Zijlmans et al., 2011; Frias et al., 2021; Partido and Stefanik, 2020; Ragab et al., 2021; Shahid et al., 2018; Sarabia-Cobo et al., 2017). The remaining articles were characterised as unsure risks (~53%), often due to insufficient information on the implementation of allocation sequencing measures and the study design used, such as pre-post designs, leading to inherent high bias risk.
Performance bias was assessed as high in nine of the studies (Meng and Qi, 2018; Sharif et al., 2013; Fletcher et al., 2009; Tadmor et al., 2016; Frias et al., 2021; Partido and Stefanik, 2020; Shahid et al., 2018; Sarabia-Cobo et al., 2017). Furthermore, a large proportion of the studies (~88%) were identified as having a high risk of detection bias. In contrast, attrition bias received a low-risk rating across all studies (~65%). The risk assessment ratings are available in Table 3 (with additional supporting judgment details in Supplementary Table S1).
3.4 Effectiveness of EI interventions
The subsequent sections outline the efficacy of EI interventions tailored for healthcare professionals, and this analysis has been be categorised based on study design, encompassing randomised controlled trials (RCT), quasi-experimental studies with control groups, controlled before-after investigations, and non-randomised experimental designs (non-RCT). Out of the 17 studies encompassed within this review, seven studies (Zijlmans et al., 2015; Kozlowski et al., 2018; Karimi et al., 2020; Tadmor et al., 2016; Zijlmans et al., 2011; Ragab et al., 2021; Shahid et al., 2018) were excluded from the meta-analysis due to the unavailability of data, rendering re-analysis unfeasible.
3.4.1 Results of individual studies
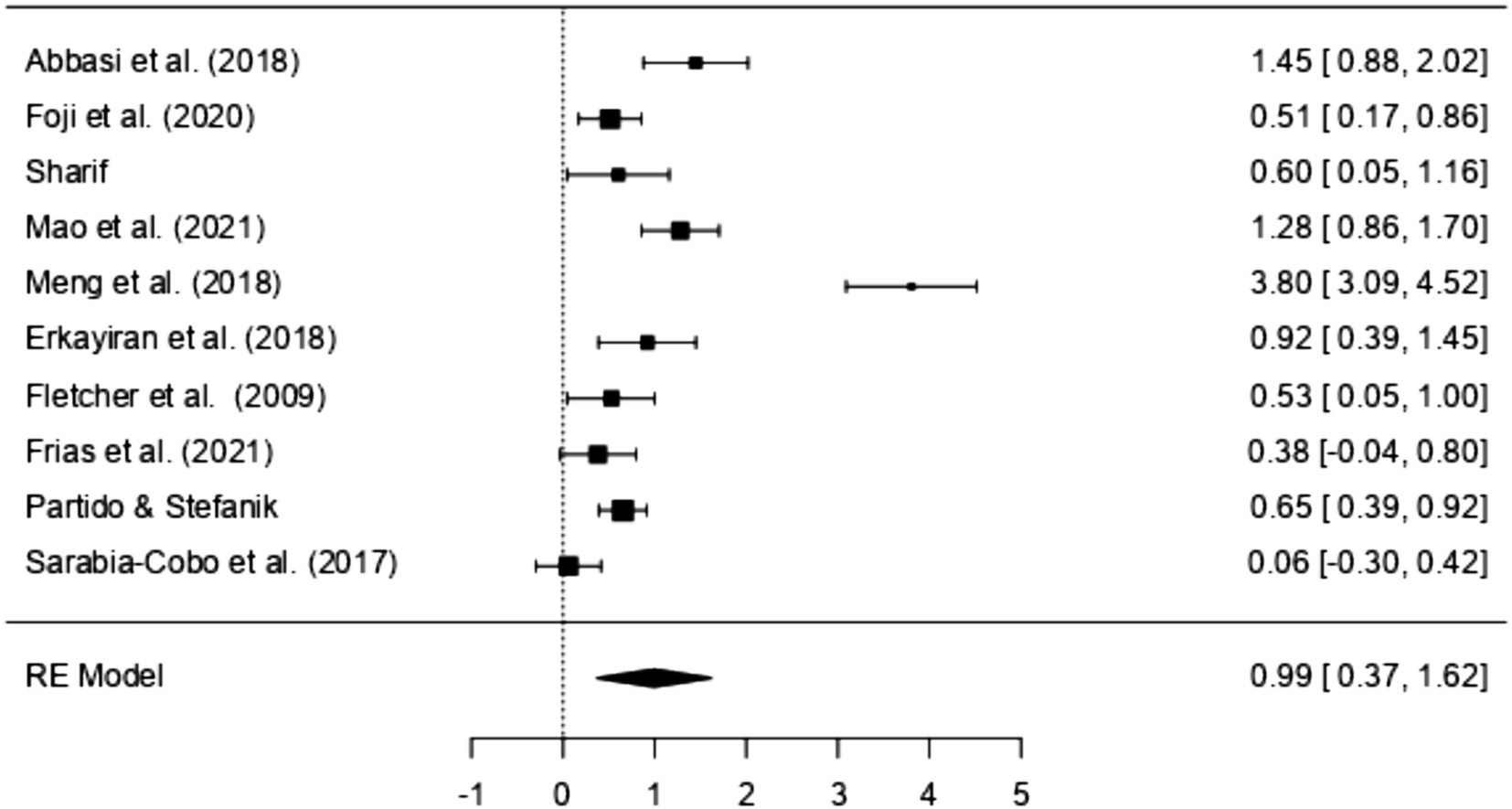
A review of several studies, categorised into different research methodologies, sheds light on the effectiveness of EI interventions within the healthcare workforce. Nearly all included studies in this review reported statistically significant increases in EI after participating in an EI-related intervention, except for one non-randomised experimental study (Frias et al., 2021), which reported an improvement that was not statistically significant. Five of these studies employed an RCT design (Abbasi et al., 2018; Foji et al., 2020; Mao et al., 2021; Meng and Qi, 2018; Sharif et al., 2013; Zijlmans et al., 2015). All these RCT studies reported statistically significant increases in EI following participation in educational and training EI interventions, with effect sizes varying between 0.51 to 3.8. When considering the effect size threshold as small (SMD < 0.4), moderate (0.4 to 0.7), and large (> 0.7), most studies had between-group effect sizes that were large (n = 3) for increasing participants EI, followed by medium (n = 2). The most substantial effect sizes were observed in Meng and Qi (2018) (SMD = 3.8), Abbasi et al. (2018) (SMD = 1.45), and Mao et al. (2021) (SMD = 1.28).
In addition to RCT studies, three studies employed a quasi-experimental design with control groups (Erkayiran and Demirkiran, 2018; Fletcher et al., 2009; Kozlowski et al., 2018). However, it is essential to note that due to data unavailability in Kozlowski et al. (2018) study, re-analysis was infeasible, rendering it unaccounted for in the meta-analysis. Yet, this study reported a significant increase in EI following a single EI training session, although the effect remains unclear due to limited findings. Both Erkayiran and Demirkiran (2018) and Fletcher et al. (2009) reported improvements in EI among medical students after the EI training programs, with the largest effect size observed in Erkayiran and Demirkiran (2018) (SMD = 0.93) and Fletcher et al. (2009) reporting a moderate effect (SMD = 0.53).
Three studies in this review adopted controlled before-after designs (Karimi et al., 2020; Tadmor et al., 2016; Zijlmans et al., 2011). These studies utilised Bar-On’s conceptualisation of EI and assessed EI levels through the Bar-On EQ-i scale (Bar-On, 1997). These studies were not included in the meta-analysis due to limited available data. However, a summary of their findings based on available information is provided in Table 4.
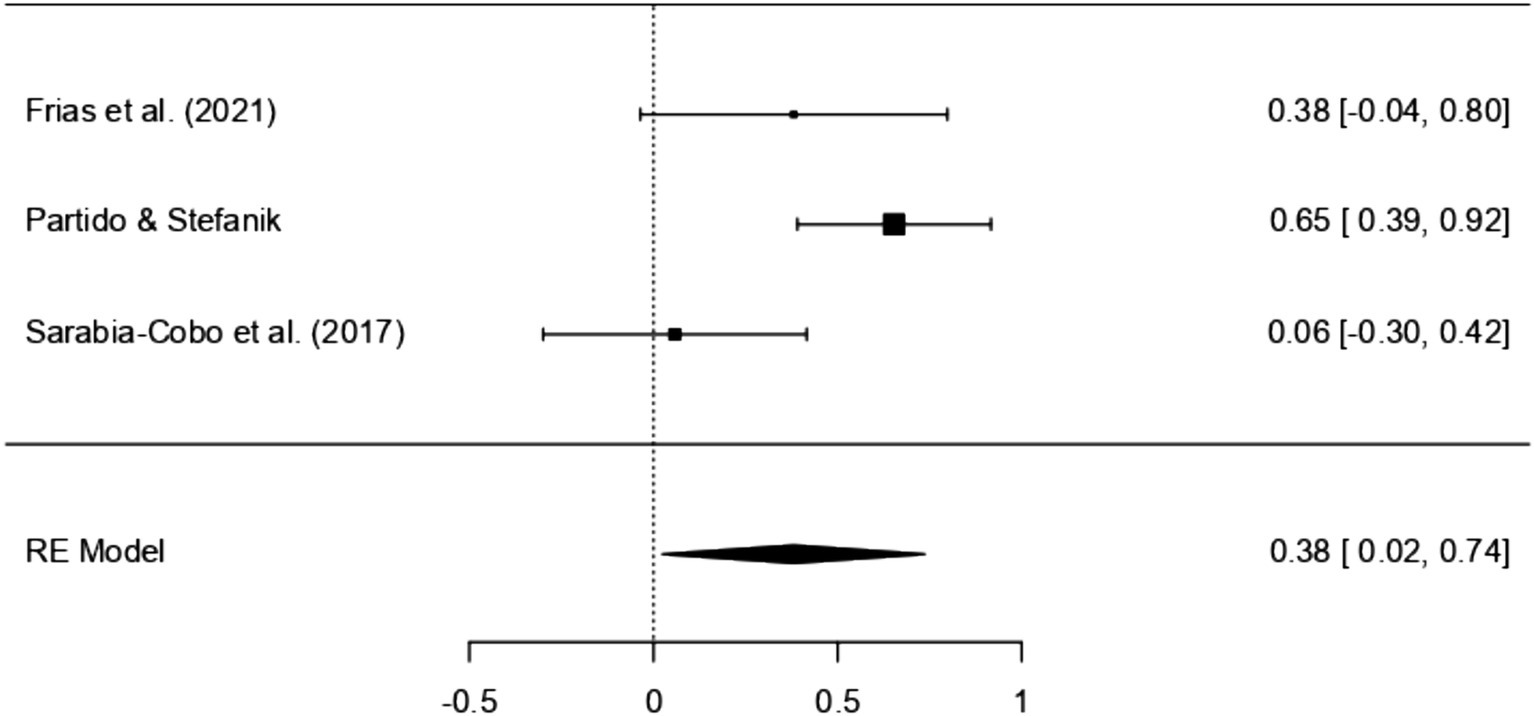
In the case of non-RCT studies, three studies were included in the meta-review (Frias et al., 2021; Partido and Stefanik, 2020; Sarabia-Cobo et al., 2017). The SMD within these studies ranged from 0.06 to 0.65. Interestingly, all three studies concurred in reporting a noticeable increase in EI as a result of the intervention. However, it is essential to highlight that most of these studies indicated a small effect size (n = 2), besides the study conducted by Partido and Stefanik (2020) which was found to have a moderate effect size (SMD = 0.65).
In terms of secondary measures, EI-derived interventions generally increased various aspects both in individual and workplace contexts. The studies revealed positive outcomes, with reported enhancements in general health and stress management (Foji et al., 2020; Mao et al., 2021; Sharif et al., 2013; Karimi et al., 2020). Moreover, the interventions contributed to increased resilience (Mao et al., 2021) and empowerment (Karimi et al., 2020). Skill development was a prominent feature, with reported improvements in communication (Meng and Qi, 2018) and problem-solving abilities (Ragab et al., 2021). In workplace settings, the interventions were associated with an improved quality of care (Mao et al., 2021; Karimi et al., 2020) and the development of transformative leadership skills (Frias et al., 2021). For a more detailed breakdown of the study results, examine Table 4.
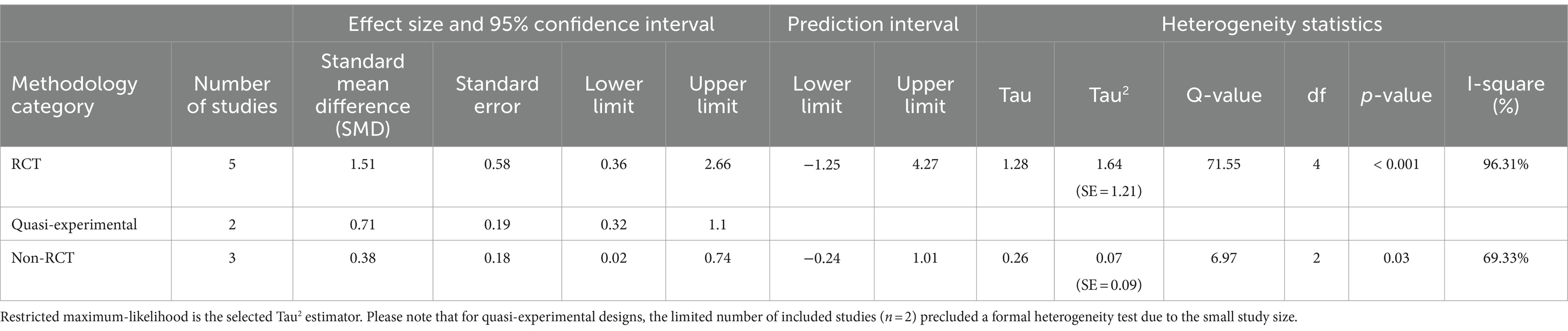
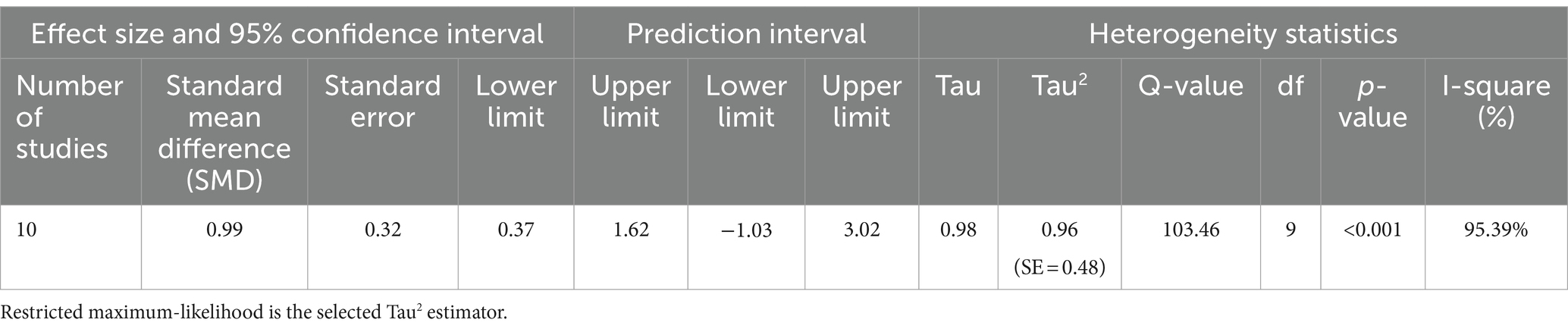
3.4.2 Random effects model: effectiveness of EI intervention
The results of the Random Effects Models are presented in Table 5. Within the RCT model, which incorporates five distinct studies, there appears to be a significant positive correlation between the interventions employed in the studies and the corresponding EI scores (SMD = 1.51, 95% CI [0.36, 2.66], p < 0.01). An examination of the 95% prediction interval for the actual outcomes reveals a range spanning from −1.25 to 4.27. Consequently, while the overall estimated outcome leans towards a positive effect, it is important to acknowledge that, in certain studies, the actual effect might, in fact, be negative. A similar pattern is observed in studies adopting Quasi-experimental designs (SMD = 0.71, 95% CI [0.32, 1.1], p < 0.001), suggesting a large effect according to Cohen’s criteria (Cohen, 2013). However, when non-RCT designs are employed, effect sizes diminish and reflect a lower impact (SMD = 0.38, 95% CI [0.02, 0.74], p < 0.05). Once again, the prediction interval for the actual outcome ranges from −0.24 to 1.01, implying that while the average effect is positive in some studies the true outcome may be negative. Further examination of the data distribution is permitted by Figures 2, 3, which display the effect size, and observed direction of the interventions on EI levels detected in each selected study.
3.5 Heterogeneity
The results of the heterogeneity test are summarised in Table 5. In the realm of RCTs, our assessment of the five studies included in the meta-review unveiled substantial heterogeneity in their outcomes (Q = 71.55, p < 0.001). A similar observation was made for non-RCT designs, where our investigation of the three included studies indicated heterogeneity in their results (Q = 6.97, p < 0.05). This implies statistically significant differences between study outcomes, potentially stemming from variations in effects or study populations. However, it is important to acknowledge that, owing to the limited number of studies available for Quasi-experimental designs (n = 2), a formal heterogeneity test was not conducted in this case.
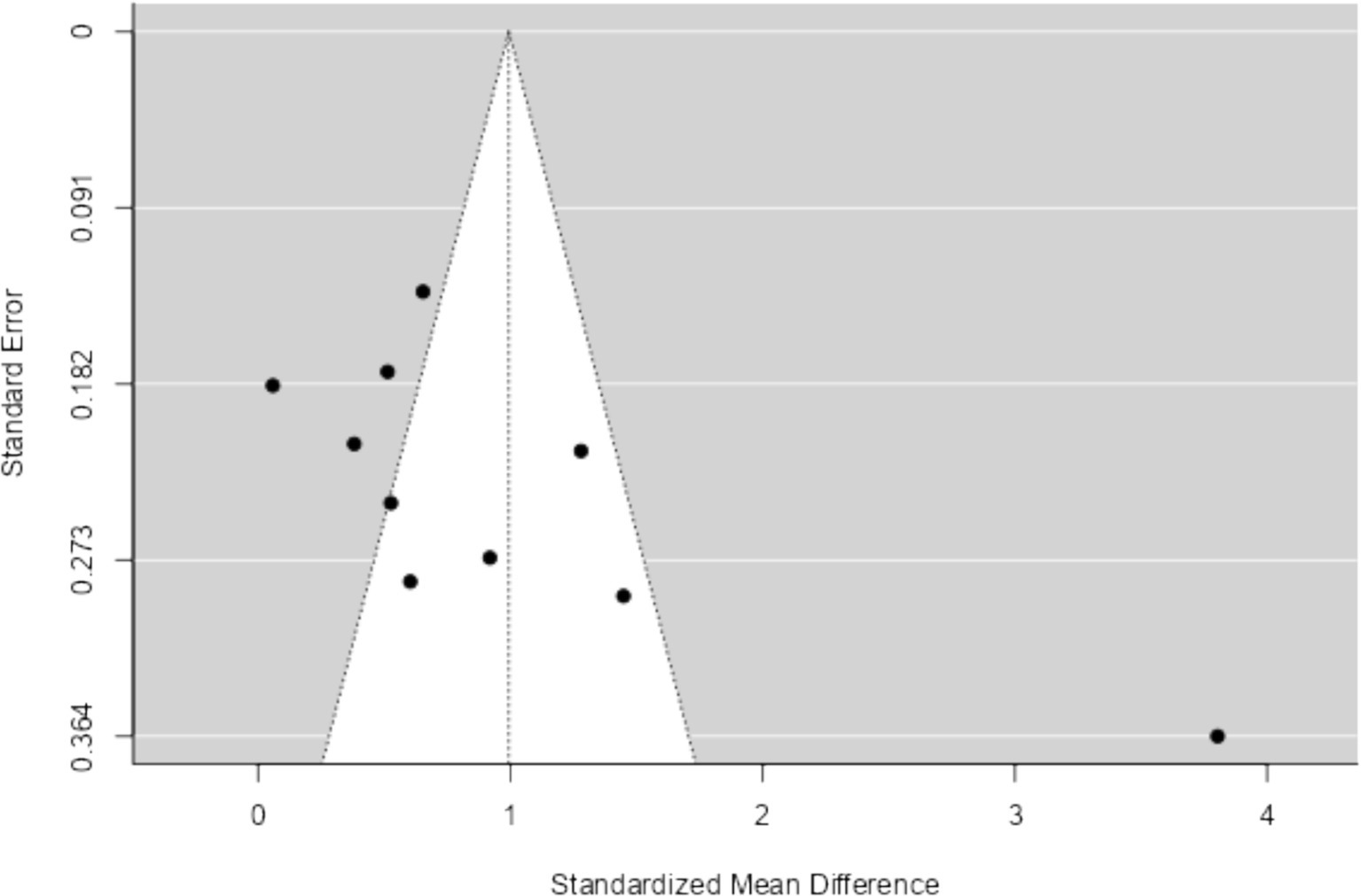
3.6 Reporting bias assessment
The results of Funnel Plot Analyses examining the intervention effect on EI are presented in Figure 4. Following the recommendation by Higgins et al. (2011) for a minimum of ten studies to investigate small study effects or publication bias, all ten available studies were pooled together for this analysis. Both the visual inspection of the figure and Egger’s regression test indicated funnel plot asymmetry (p < 0.05), suggesting the presence of potential bias. Notably, one study (Meng and Qi, 2018) appeared to be particularly influential and emerged as an outlier in this analysis. The results of the overall Random Effects Model (n = 10) can be found in Table 6 and Figure 5.
4 Discussion
4.1 Main findings
The present systematic and meta-analysis reviewed 17 studies to examine the effectiveness of EI interventions as a trainable skill among healthcare workers. These studies exhibited noticeable variations in terms of intervention duration, the types of interventions applied, and methodologies. The duration of interventions ranged from brief two-hour training sessions (Frias et al., 2021) to more extensive training programs extending up to seven months (Fletcher et al., 2009). Moreover, various intervention methods were employed to bolster EI among healthcare professionals, including the use of educational tools (Abbasi et al., 2018; Foji et al., 2020; Sharif et al., 2013; Partido and Stefanik, 2020), persuasion techniques (Kozlowski et al., 2018), training methods (Zijlmans et al., 2015; Erkayiran and Demirkiran, 2018; Fletcher et al., 2009; Karimi et al., 2020; Zijlmans et al., 2011), and behavior change strategies (Frias et al., 2021). Some studies adopted a hybrid approach by combining two or more of these intervention types (Mao et al., 2021; Meng and Qi, 2018; Kozlowski et al., 2018; Tadmor et al., 2016; Ragab et al., 2021; Shahid et al., 2018; Sarabia-Cobo et al., 2017). Remarkably, with the exception of a single study, all reported a significant improvement in EI following the interventions. The effect size for EI enhancement in RCTs and quasi-experimental studies ranged from moderate to large, while the effectiveness of EI interventions appeared to decrease with non-RCT designs, yielding smaller effect sizes. This result supports previous findings confirming the effectiveness of interventions to increase EI (Mattingly and Kraiger, 2019; Hodzic et al., 2018; Kotsou et al., 2019). However, a major limitation across the reviewed studies was the scarcity of empirical data and flawed methodologies (including unconcealed participant allocation and poor randomisation), which contributed to a high risk of bias in many studies. Due to this publication bias, it can be assumed that the true effect of EI intervention across these methodologies is much smaller than reported. In terms of secondary measures, although not extensively explored in this review, the findings suggest potential benefits to the healthcare workforce following EI training. These benefits encompassed those for the individual including improved health, stress management, resilience and empowerment (Foji et al., 2020; Mao et al., 2021; Sharif et al., 2013; Karimi et al., 2020) and systemic benefits such as improved communication, problem-solving abilities, quality of care and transformative leadership skills (Mao et al., 2021; Meng and Qi, 2018; Karimi et al., 2020; Frias et al., 2021). The findings present valuable contributions to the current body of knowledge on EI and offer important insights and recommendations for shaping future intervention strategies.
Despite the noted limitations, these findings provide preliminary insights into the potential benefits of EI interventions. Notably, the included studies bring to light the diversity in the duration of interventions, with longer interventions (typically spanning over ten sessions across several months) being the predominant choice among the reviewed studies. These preliminary findings suggest that employing a longer duration may be conducive to more substantial EI development. For instance, studies that embraced lengthier interventions frequently reported more favourable outcomes in terms of EI enhancement [(e.g., Mao et al., 2021; Meng and Qi, 2018)]. Conversely, when the duration of the intervention was shorter, typically less than one month, it often resulted in less pronounced impacts on EI development [(e.g., Sharif et al., 2013; Sarabia-Cobo et al., 2017)]. This contrast is exemplified in the study conducted by Frias et al. (2021), which revealed a non-significant difference in EI following their brief two-hour intervention. They identified a limitation in their approach, notably the minimal interaction between researchers and participants during the four months of the intervention and post-survey, which may have contributed to the less substantial effects observed. This suggests that an essential component to enhance the effectiveness of these interventions requires a more gradual dissemination of information to sustain learning transfer and the acquisition of EI competencies. This might involve more detailed skill training and providing participants with additional time to become accustomed to thinking in more adaptive ways, which might not be achievable in a short two-hour intervention (Kotsou et al., 2019). Considering that EI is often considered trait-related, it is plausible that more extended durations, suggested to be between four to eight weeks, are required for the newly acquired EI skills to become internalised and automatic (Roberts et al., 2017). However, it is important to note that these conclusions may vary among scholars. Kruml and Yockey (2011) examined whether different modes of training delivery and training lengths (ranging from a 7-week to 16-week intervention) would lead to different outcomes and reported no significant differences in effectiveness among the different settings. Additionally, when comparing a long-term (13-week) with a short-term (2-days) coaching skills training program, Grant (2007) found that EI increased only with the long-term intervention. Therefore, these findings serve as a preliminary basis for further exploration of the optimum intervention length. Given the methodological variability and limited scope of high-quality studies in this field, future research is needed to establish the optimal duration and structure of EI interventions more reliably. One suggestion outlined by Roberts et al. (2017) is for researchers to consider longitudinal studies that assess changes on a more frequent basis, such as every week or month, to capture when and how these changes occur.
Beyond the varied intervention durations, the reviewed studies also displayed substantial diversity in their approaches and models for enhancing EI. For example, many of the included studies used didactic training [(e.g., Abbasi et al., 2018; Sharif et al., 2013)], while others used reflective or collaborative approaches [(e.g., Karimi et al., 2020)], or a combination of both [(e.g., Meng and Qi, 2018; Ragab et al., 2021; Sarabia-Cobo et al., 2017)]. While the exact reasons why the intervention was effective are beyond this review’s scope, previous literature has indicated that EI scores tend to improve when participants engage actively in practising and receive constructive feedback (Mattingly and Kraiger, 2019). An illustrative example of an effective EI intervention can be found in Mao et al. (2021) study, which employed a two-phase approach. The first phase encompassed formal lectures based on Mayer and Salovey’s abilities model of EI (comprising the abilities to perceive, use, understand and manage emotions), while the second phase focused on case management related to emotional control. During this phase, participants engaged in group discussions and received feedback from educators regarding their performance and strategies. The incorporation of both didactic and pedagogical approaches in this model might have contributed to its effectiveness in enhancing EI compared to other approaches reported in studies. The multifaceted nature of this training, designed to expand participants’ emotional knowledge and skills while increasing their emotional competence and confidence through practice, suggests that the combination of both approaches could be optimal. This aligns with prior literature endorsing the use of multiple methods for their potential to enhance EI (Mattingly and Kraiger, 2019; Hodzic et al., 2018; Geßler et al., 2021) and could serve as a valuable reference for those intending to develop future EI interventions.
An additional implication to highlight from this review pertains to the diversity of methodologies employed within the studies. They encompass a range of approaches, including RCT (Abbasi et al., 2018; Foji et al., 2020; Mao et al., 2021; Meng and Qi, 2018; Sharif et al., 2013; Zijlmans et al., 2015), quasi-experimental designs with pre-test-post-test control groups (Erkayiran and Demirkiran, 2018; Fletcher et al., 2009; Kozlowski et al., 2018), controlled before-after studies (Karimi et al., 2020; Tadmor et al., 2016; Zijlmans et al., 2011), and non-RCT (Frias et al., 2021; Partido and Stefanik, 2020; Ragab et al., 2021; Shahid et al., 2018; Sarabia-Cobo et al., 2017). From the meta-analytic, it can be inferred that RCTs and quasi-experimental designs were particularly useful in assessing the intervention’s effectiveness, as evidenced by the positive correlations found with EI. Random assignment, as well as quasi-experimental designs, have been extensively researched and are considered advantageous in the context of EI interventions, as they help control for motivation and demand effects, ultimately supporting the establishment of causal relationships and allowing rigorous empirical comparison of results (Mattingly and Kraiger, 2019; Hodzic et al., 2018). Therefore, it is recommended that future studies consider incorporating randomisation and active control groups to engage in similar activities during the EI intervention (e.g., a mindfulness or relaxation control group conducted for the same duration). However, given the notable publication bias reported within these studies, possibly explained by the poor methodological quality or non-reporting of results, it is essential to interpret these findings cautiously. This bias emphasises the need for future researchers to explore these varied methodological properties more comprehensively to gain a deeper understanding of their impact on intervention effectiveness.
4.2 Limitations and future research directions
While the findings of this review offer intriguing insights that could enhance our understanding of EI interventions for healthcare workers, several limitations should be acknowledged. A notable limitation of this review is the substantial variability in study characteristics among the included studies, particularly regarding intervention duration, types of interventions, and methodologies. Interventions ranged from brief two-hour training sessions to extensive programs lasting up to seven months, with differing approaches and evaluation methods. This heterogeneity may limit the comparability of study outcomes and the generalizability of our findings. While our analysis aimed to account for these variations, the diversity in intervention designs and durations makes it challenging to draw definitive conclusions about the overall effectiveness of interventions targeting healthcare workers. Future research would benefit from more standardized intervention protocols to facilitate clearer comparisons and more robust conclusions. Furthermore, the relatively small sample sizes across the included studies may have impacted the certainty of the results, and the actual effect could differ significantly from what was observed in this review, making real-world effects uncertain. Moreover, the predominant presence of female participants in the study sample aligns with the global representation of the healthcare workforce, where women constitute around 70% (Boniol et al., 2019). However, given the ongoing efforts to enhance gender diversity in the healthcare sector, future studies should consider larger and more gender-diverse samples.
Another limitation that may have resulted in an overestimation of the true effect concerns the consistent methodological flaws found in the reviewed studies. As mentioned earlier, several of the studies lacked crucial elements like randomisation and allocation concealment. Moreover, since all these studies relied on self-reported measures, concerns about potential biases and their impact on the true effects of the interventions arise. While it is possible that some studies did incorporate these vital elements, the scarcity of specific details within their documentation introduces an element of uncertainty. This uncertainty extends to basic statistical information, such as sample sizes, means, and standard deviations, which were often missing from the results section. This omission complicates the calculation of effect sizes. Additionally, many authors provided only vague descriptions of their intervention programs, lacking comprehensive information. Consequently, it is strongly recommended that future researchers furnish relevant data regarding their results and offer detailed descriptions of the treatment modalities. This not only eases the application of meta-analytic procedures but also advances our understanding of the effectiveness of EI interventions. Such knowledge facilitates the dissemination of effective interventions for this population and aids in better replication, assessment, and comprehension of the actual effects of EI interventions.
Furthermore, clear evidence of publication bias is discernible among these studies. Given that nearly all included studies reported a significant effect, it can be inferred that studies with substantial effects are more readily published. This phenomenon, which has also been reported in other studies evaluating EI interventions (Hodzic et al., 2018), suggests that effect sizes in additional unpublished works examining the impact of training on EI may deviate significantly from the effect sizes documented in peer-reviewed journals and dissertations/theses. Therefore, it is recommended that future reviews consider including dissertations and unpublished reports to access a more accurate representation of the true results.
Future research should also consider conducting a subgroup analysis comparing the outcomes of EI interventions assessed through self-report tools versus performance-based tools. Self-report measures and performance-based assessments capture different dimensions of EI, self-perceived abilities versus objective emotional processing skills, and comparing these tools could provide valuable insights into how each type reflects changes following interventions. Such a distinction would contribute to a more nuanced understanding of EI training efficacy in healthcare settings and beyond.
4.3 Conclusion
In conclusion, this review underscores the potential benefits of implementing EI interventions for healthcare workers. The moderate positive effect observed suggests that EI is a trainable skill, offering opportunities for improving EI-related outcomes. Notably, interventions of longer duration and those incorporating multiple methods appear to be more effective. However, it is essential to approach these findings cautiously due to the methodological limitations and publication bias prevalent in the reviewed studies. To advance the field, future research should prioritise robust methodologies, including RCTs and quasi-experimental designs, and should also aim for larger and more diverse samples to assess intervention effectiveness.
Author’s note
This manuscript includes original work not previously published or presented and not under current review elsewhere. All data and syntax supporting the findings of this study are available with the article and its Supplementary materials. The present systematic and meta-analysis has been pre-registered with PROSPERO [CRD42023393760]. Further details about the registration can be accessed at: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023393760.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
CP: Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing. TB: Formal analysis, Writing – original draft, Writing – review & editing. YY: Formal analysis, Writing – original draft, Writing – review & editing. KH: Writing – original draft, Writing – review & editing. MT: Writing – original draft, Writing – review & editing. TQ: Writing – original draft, Writing – review & editing. SX: Writing – original draft, Writing – review & editing. LK: Conceptualization, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1437035/full#supplementary-material
References
Abbasi, S., Rakhshani, T., Rezaie, M., Ebrahimi, M. R., and Taravatmanesh, S. (2018). A study of emotional intelligence and the effect of educational intervention in emergency medicine residents. Arch. Psychiatry Psychother. 20, 45–52. doi: 10.12740/APP/82317
Aldaod, S. M., Sweis, R. J., Alawneh, A. R., and Jaradat, M. (2019). Emotional intelligence effect in health sector: a literature review. Int. J. Inform. Bus. Manag. 11, 08–94.
Bar-On, R. (1997). Bar-On Emotional Quotient Inventory (EQ-i): Technical manual. Multi-Health Systems.
Baudry, A. S., Grynberg, D., Dassonneville, C., Lelorain, S., and Christophe, V. (2018). Sub-dimensions of trait emotional intelligence and health: a critical and systematic review of the literature. Scand. J. Psychol. 59, 206–222. doi: 10.1111/sjop.12424
Boniol, M., McIsaac, M., Xu, L., Wuliji, T., Diallo, K., and Campbell, J. (2019). Gender equity in the health workforce: analysis of 104 countries. World health Organization. (Report No. WHO/HIS/HWF/Gender/WP1/2019.1).
Campbell, M., McKenzie, J. E., Sowden, A., Katikireddi, S. V., Brennan, S. E., Ellis, S., et al. (2020). Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ 368:368. doi: 10.1136/bmj.l6890
Cochran, W. G. (1954). The combination of estimates from different experiments. Biometrics 10, 101–129. doi: 10.2307/3001666
Coutinho, H., Queirós, C., Henriques, A., Norton, P., and Alves, E. (2018). Work-related determinants of psychosocial risk factors among employees in the hospital setting. Work 61, 551–560. doi: 10.3233/WOR-182825
Dyrbye, L. N., Shanafelt, T. D., Johnson, P. O., Johnson, L. A., Satele, D., and West, C. P. (2019). A cross-sectional study exploring the relationship between burnout, absenteeism, and job performance among American nurses. BMC Nurs. 18, 57–58. doi: 10.1186/s12912-019-0382-7
Dyrbye, L. N., Shanafelt, T. D., Sinsky, C. A., Cipriano, P. F., Bhatt, J., Ommaya, A., et al. (2017). Burnout among health care professionals: a call to explore and address this underrecognized threat to safe, high-quality care. NAM Perspect. 7, 1–11. doi: 10.31478/201707b
Erkayiran, O., and Demirkiran, F. (2018). The impact of improving emotional intelligence skills training on nursing Students' interpersonal relationship styles: a quasi-experimental study. Int. J. Caring Sci. 11, 1901–1912.
Felton, J. S. (1998). Burnout as a clinical entity—its importance in health care workers. Occup. Med. 48, 237–250. doi: 10.1093/occmed/48.4.237
Fletcher, I., Leadbetter, P., Curran, A., and O'Sullivan, H. (2009). A pilot study assessing emotional intelligence training and communication skills with 3rd year medical students. Patient Educ. Couns. 76, 376–379. doi: 10.1016/j.pec.2009.07.019
Foji, S., Vejdani, M., Salehiniya, H., and Khosrorad, R. (2020). The effect of emotional intelligence training on general health promotion among nurse. J. Educ. Health Promotion. 9:4. doi: 10.4103/jehp.jehp_134_19
Frias, A., Hampton, D., Tharp-Barrie, K., and Thomas, J. (2021). The impact of an emotional intelligence training program on transformational leadership. Nurs. Manag. 52, 18–25. doi: 10.1097/01.NUMA.0000731924.03153.df
Geßler, S., Nezlek, J. B., and Schütz, A. (2021). Training emotional intelligence: does training in basic emotional abilities help people to improve higher emotional abilities? J. Posit. Psychol. 16, 455–464. doi: 10.1080/17439760.2020.1738537
Grant, A. M. (2007). Enhancing coaching skills and emotional intelligence through training. Ind. Commer. Train. 39, 257–266. doi: 10.1108/00197850710761945
Hall, L. H., Johnson, J., Watt, I., Tsipa, A., and O’Connor, D. B. (2016). Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS One 11:e0159015. doi: 10.1371/journal.pone.0159015
Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:343. doi: 10.1136/bmj.d5928
Higgins, J., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M., et al. (2023). Cochrane handbook for systematic reviews of interventions. 6.4 ed. Cochrane; Available at: https://www.training.cochrane.org/handbook
Hodzic, S., Scharfen, J., Ripoll, P., Holling, H., and Zenasni, F. (2018). How efficient are emotional intelligence trainings: a meta-analysis. Emot. Rev. 10, 138–148. doi: 10.1177/1754073917708613
Jiménez-Picón, N., Romero-Martín, M., Ponce-Blandón, J. A., Ramirez-Baena, L., Palomo-Lara, J. C., and Gómez-Salgado, J. (2021). The relationship between mindfulness and emotional intelligence as a protective factor for healthcare professionals: systematic review. Int. J. Environ. Res. Public Health 18:5491. doi: 10.3390/ijerph18105491
Karimi, L., Leggat, S. G., Bartram, T., Afshari, L., Sarkeshik, S., and Verulava, T. (2021). Emotional intelligence: predictor of employees’ wellbeing, quality of patient care, and psychological empowerment. BMC Psychol. 9, 93–97. doi: 10.1186/s40359-021-00593-8
Karimi, L., Leggat, S. G., Bartram, T., and Rada, J. (2020). The effects of emotional intelligence training on the job performance of Australian aged care workers. Health Care Manag. Rev. 45, 41–51. doi: 10.1097/HMR.0000000000000200
Kotsou, I., Mikolajczak, M., Heeren, A., Grégoire, J., and Leys, C. (2019). Improving emotional intelligence: a systematic review of existing work and future challenges. Emot. Rev. 11, 151–165. doi: 10.1177/1754073917735902
Kozlowski, D., Hutchinson, M., Hurley, J., and Browne, G. (2018). Increasing nurses' emotional intelligence with a brief intervention. Appl. Nurs. Res. 41, 59–61. doi: 10.1016/j.apnr.2018.04.001
Kruml, S. M., and Yockey, M. D. (2011). Developing the emotionally intelligent leader: instructional issues. J. Leaders. Org. Stud. 18, 207–215. doi: 10.1177/1548051810372220
Liu, J. X., Goryakin, Y., Maeda, A., Bruckner, T., and Scheffler, R. (2017). Global health workforce labor market projections for 2030. Hum. Resour. Health 15, 1–2. doi: 10.1186/s12960-017-0187-2
Mao, L., Huang, L., and Chen, Q. (2021). Promoting resilience and lower stress in nurses and improving inpatient experience through emotional intelligence training in China: a randomized controlled trial. Nurse Educ. Today 107:105130. doi: 10.1016/j.nedt.2021.105130
Mattingly, V., and Kraiger, K. (2019). Can emotional intelligence be trained? A meta-analytical investigation. Hum. Res. Manag. Rev. 29, 140–155. doi: 10.1016/j.hrmr.2018.03.002
Mayer, J. D., and Salovey, P. (1997). “What is emotional intelligence?” in Emotional development and emotional intelligence: educational implications. eds. P. Salovey and D. J. Sluyter (New York: Basic Books), 3–34.
Meng, L., and Qi, J. (2018). The effect of an emotional intelligence intervention on reducing stress and improving communication skills of nursing students. Neuro Quantol. 16:1175. doi: 10.14704/nq.2018.16.1.1175
Mento, C., Silvestri, M. C., Bruno, A., Muscatello, M. R., Cedro, C., Pandolfo, G., et al. (2020). Workplace violence against healthcare professionals: a systematic review. Aggress. Violent Behav. 51:101381. doi: 10.1016/j.avb.2020.101381
Meyer, B. B., Fletcher, T. B., and Parker, S. J. (2004). Enhancing emotional intelligence in the health care environment: an exploratory study. Health Care Manag. 23, 225–234. doi: 10.1097/00126450-200407000-00006
O'Connor, P. J., Hill, A., Kaya, M., and Martin, B. (2019). The measurement of emotional intelligence: a critical review of the literature and recommendations for researchers and practitioners. Front. Psychol. 10:1116. doi: 10.3389/fpsyg.2019.01116
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int. J. Surg. 372:105906. doi: 10.1136/bmj.n71
Panagioti, M., Geraghty, K., Johnson, J., Zhou, A., Panagopoulou, E., Chew-Graham, C., et al. (2018). Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern. Med. 178, 1317–1331. doi: 10.1001/jamainternmed.2018.3713
Partido, B. B., and Stefanik, D. (2020). Impact of emotional intelligence training in a communication and ethics course among second-year dental students. J. Dent. Educ. 84, 704–711. doi: 10.1002/jdd.12142
Ragab, S. M., Shazly, M. M., and Mostafa, H. A. (2021). Emotional intelligence training program and its effect on nursing students problem solving skills. Indian J. Foren. Med. Toxicol. 15, 2324–2335. doi: 10.37506/ijfmt.v15i4.17054
Roberts, B. W., Luo, J., Briley, D. A., Chow, P. I., Su, R., and Hill, P. L. (2017). A systematic review of personality trait change through intervention. Psychol. Bull. 143, 117–141. doi: 10.1037/bul0000088
Santana, M. J., Manalili, K., Jolley, R. J., Zelinsky, S., Quan, H., and Lu, M. (2018). How to practice person-centred care: a conceptual framework. Health Expect. 21, 429–440. doi: 10.1111/hex.12640
Sarabia-Cobo, C. M., Suárez, S. G., Crispín, E. J., Cobo, A. B., Pérez, V., de Lorena, P., et al. (2017). Emotional intelligence and coping styles: an intervention in geriatric nurses. Appl. Nurs. Res. 35, 94–98. doi: 10.1016/j.apnr.2017.03.001
Schoenfelder, T., Klewer, J., and Kugler, J. (2011). Determinants of patient satisfaction: a study among 39 hospitals in an in-patient setting in Germany. Int. J. Qual. Health Care 23, 503–509. doi: 10.1093/intqhc/mzr038
Sergi, M. R., Picconi, L., Tommasi, M., Saggino, A., Ebisch, S. J., and Spoto, A. (2021). The role of gender in the association among the emotional intelligence, anxiety and depression. Front. Psychol. 12:747702. doi: 10.3389/fpsyg.2021.747702
Shahid, R., Stirling, J., and Adams, W. (2018). Promoting wellness and stress management in residents through emotional intelligence training. Adv. Med. Educ. Pract. 9, 681–686. doi: 10.2147/AMEP.S175299
Sharif, F., Rezaie, S., Keshavarzi, S., Mansoori, P., and Ghadakpoor, S. (2013). Teaching emotional intelligence to intensive care unit nurses and their general health: a randomized clinical trial. Int. J. Occup. Environ. Med. 4, 141–148
Søvold, L. E., Naslund, J. A., Kousoulis, A. A., Saxena, S., Qoronfleh, M. W., Grobler, C., et al. (2021). Prioritizing the mental health and well-being of healthcare workers: an urgent global public health priority. Front. Public Health 9:679397. doi: 10.3389/fpubh.2021.679397
Tadmor, T., Dolev, N., Attias, D., Lelong, A. R., and Rofe, A. (2016). Emotional intelligence: a unique group training in a hematology-oncology unit. Educ. Health 29, 179–185. doi: 10.4103/1357-6283.204221
Tawfik, D. S., Scheid, A., Profit, J., Shanafelt, T., Trockel, M., Adair, K. C., et al. (2019). Evidence relating health care provider burnout and quality of care: a systematic review and meta-analysis. Ann. Intern. Med. 171, 555–567. doi: 10.7326/M19-1152
Tommasi, M., Sergi, M. R., Picconi, L., and Saggino, A. (2023). The location of emotional intelligence measured by EQ-i in the personality and cognitive space: are there gender differences? Front. Psychol. 13:985847. doi: 10.3389/fpsyg.2022.985847
Viechtbauer, W. (2005). Bias and efficiency of meta-analytic variance estimators in the random-effects model. J. Educ. Behav. Stat. 30, 261–293. doi: 10.3102/10769986030003261
Vlachou, E. M., Damigos, D., Lyrakos, G., Chanopoulos, K., Kosmidis, G., and Karavis, M. (2016). The relationship between burnout syndrome and emotional intelligence in healthcare professionals. Health Sci. J. 10:1. doi: 10.4172/1791-809X.1000100502
Zijlmans, L. J., Embregts, P. J., Gerits, L., Bosman, A. M., and Derksen, J. J. (2011). Training emotional intelligence related to treatment skills of staff working with clients with intellectual disabilities and challenging behaviour. J. Intellect. Disabil. Res. 55, 219–230. doi: 10.1111/j.1365-2788.2010.01367.x
Keywords: emotional intelligence, EI, healthcare, burnout, systematic review, meta-analysis
Citation: Powell C, Brown T, Yap Y, Hallam K, Takac M, Quinlivan T, Xenos S and Karimi L (2024) Emotional intelligence training among the healthcare workforce: a systematic review and meta-analysis. Front. Psychol. 15:1437035. doi: 10.3389/fpsyg.2024.1437035
Edited by:
Estelle Michinov, University of Rennes 2 – Upper Brittany, FranceReviewed by:
Joann Farrell Quinn, University of South Florida, United StatesMaria Rita Sergi, University of G. ‘d’Annunzio, Italy
Copyright © 2024 Powell, Brown, Yap, Hallam, Takac, Quinlivan, Xenos and Karimi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Leila Karimi, TGVpbGEuS2FyaW1pQHJtaXQuZWR1LmF1
 Chris Powell
Chris Powell Taylor Brown
Taylor Brown Yang Yap
Yang Yap Leila Karimi
Leila Karimi