- 1Pediatric Department, the Second People’s Hospital of Jingdezhen, Jingdezhen, Jiangxi, China
- 2Emergency Department, the Second People’s Hospital of Jingdezhen, Jingdezhen, Jiangxi, China
Background: Globally, there is an increasing trend in the incidence of premature births and low birth weight. Neonatal intensive care unit (NICU) care has become indispensable for these newborns. Nevertheless, this mode of care poses substantial economic, psychological, and health challenges to the families of preterm infants. Despite abundant evidence concerning the parents’ needs in the NICU, the needs of grandparents—vital family members—are frequently disregarded. This exploratory study aimed to assess the grandparents’ needs of preterm infants in the NICU, exploring the impact of demographic elements on these needs to offer guidance for clinical care practices.
Methods: This study employed a cross-sectional design and the Chinese version of the NICU Family Needs Inventory (NICU-FNI) to investigate the needs of grandparents. A total of 280 grandparents participated in the study, providing data by completing structured questionnaires related to their demographic profiles and needs. Statistical analyses were utilized to analyze the data, including descriptive statistics, chi-square tests, Pearson’s correlation, and multiple linear regression.
Results: Six items about Assurance emerged as significant among the top 10 important needs, with two items for Information, one for Proximity, and one for Support; among the least important needs, nine items related to Comfort and Support were identified. The subscale “Assurance” achieved the highest mean score of 4.07 ± 0.49, followed by the subscales of “Information” and “Proximity,” registering mean scores of 3.50 ± 0.47 and 3.50 ± 0.46, respectively. This explorative study identified a correlation between the needs for Assurance and employment status, place of residence, gestational age, and birth weight (p < 0.05). Employment status, place of residence, and gestational age were identified as significant correlates for Assurance (p < 0.05).
Conclusion: The foremost need identified by grandparents is Assurance of quality care for preterm infants, closely followed by the demand for thorough Information and the ability to be in Proximity to the infant. This exploratory study highlights that mitigating the strain on families with preterm infants, as well as recognizing and meeting the needs of grandparents, is of paramount importance.
Introduction
The neonatal intensive care unit (NICU) offers life-saving care; however, the exorbitant expenses and intricate caregiving procedures can impose considerable emotional and psychological burdens on the entire family, precipitating conditions such as depression, anxiety, and trauma (Geng et al., 2022; Grunberg et al., 2022). Generally, neonates necessitating urgent medical intervention are admitted to the NICU (Chow et al., 2015). Such infants are commonly characterized by preterm birth (i.e., occurring prior to 37 weeks of gestation), low birth weight, and/or the presence of severe medical ailments (Chow et al., 2015). As per the WHO’s “Global Report on Preterm Births,” the worldwide occurrence rate of preterm or low birth weight deliveries increased from 9.6% in 2005 to 11.1% in 2012 (WHO, 2012). Furthermore, in a 2011 nationwide survey in China, the preterm birth incidence was recorded at 7.1% (Zou et al., 2014). Following the relaxation of China’s two-child policy in 2015, the surge in advanced maternal age, multiparous women, and multiple gestation pregnancies has significantly led to an escalation in the preterm birth rate (Yang et al., 2017; Zhang et al., 2021).
Parents of premature infants are frequently confronted with a variety of challenges pertaining to economic, psychological, and physical health. Upon the admission of their infants to the NICU, these parents often undergo emotions of anxiety, depression, guilt, and a sense of helplessness, potentially adversely (Kim, 2018; Lorié et al., 2021). Identifying and addressing parental needs in the NICU is a crucial factor in achieving the best outcomes for newborns and their families. Specifically, parents of preterm infants have emphasized the significance of obtaining infants’ health information and guidance (Arockiasamy et al., 2008; Harris et al., 2024), trusting medical staff (Bernaix et al., 2006), and benefiting from Support from staff to meet their needs (Bernaix et al., 2006; Pepper et al., 2012).
The emergence and evolution of the concept of “family-centered care” has led to active parental involvement as primary caregivers in the care of preterm infants, representing critical factor in enhancing the post-discharge survival quality of preterm infants; the majority of research on the family needs in NICU has mainly concentrated on newborn parents (Arockiasamy et al., 2008; Diffin et al., 2013), particularly on mothers of preterm infants (Govindaswamy et al., 2020). Usually, mothers may suffer physical discomfort after delivery, making it impossible to care for the baby; fathers serve as the initial point of contact between the family and the NICU staff and are the ones who decide on the need for emergency treatment (Arockiasamy et al., 2008; Johnson, 2008). Nevertheless, grandparents play a pivotal role in the family, especially for parents of preterm infants in single-child households. In China, they hold an especially significant position, often enjoying relatively high economic status and social standing (Zhang et al., 2022). Moreover, there is a high prevalence of grandparents living with their grandchildren in China. These resident grandparents play a vital role in raising the children, particularly once the child has passed their first birthday. While caring for the children, grandparents often work with healthcare professionals to ensure the children’s wellbeing. This includes regular health checkups, vaccinations, and monitoring of the children’s development, requiring the active involvement and cooperation of the grandparents (Chen et al., 2011; Chen and Lewis, 2015). Chinese fathers often rely on grandparents for support to reduce their stress, considering the mother’s need for care. Grandparents are viewed as the most trusted individuals (Sun et al., 2024).
Studies have demonstrated that, in the context of a family member’s acute severe illness, the concept of family resilience is instrumental in facilitating adaptive responses and preserving familial equilibrium in the face of both internal and external crises (Gao et al., 2022; Shao et al., 2023; Walsh, 2016). The critical role of grandparents in enhancing family resilience is unmistakable; they provide support and comfort to younger parents, thereby strengthening the family’s collective resilience through shared confrontations with adversities (Lambiase et al., 2024). In the high-pressure environment of the NICU, grandparental support helps alleviate the emotional strain on parents, increases familial cohesion, and enhances the family’s ability to navigate hardships (Brødsgaard et al., 2017). Hence, grasping the needs of grandparents with a premature infant in the NICU is of utmost importance; healthcare professionals should be adequately prepared to meet grandparents’ needs by offering the necessary support and assistance. Such proactive measures can significantly reduce the grandparents’ emotional burden, by extension, on the parents, establishing a constructive dialog between patient families and healthcare providers, thereby reducing the incidence of medical disputes (Brødsgaard et al., 2017; Jain et al., 2021; Sun et al., 2024). This exploratory study aims to investigate the unique needs of grandparents with preterm infants in the NICU. The primary aim is to generate initial insights that will assist healthcare professionals in understanding how to provide more tailored and effective support and to offer foundational information to regulatory authorities as a basis for potential considerations in developing NICU policies.
Materials and methods
Study design and setting
The NICU-Family Need Inventory (NICU-FNI) is a specialized adaptation of the Critical Care Family Needs Inventory (CCFNI) by Ward (2001), incorporating the research by Jacono et al. (1990) and Kirschbaum (1990), explicitly designed to address the needs of parents with NICU infants. The NICU-FNI is divided into five domains (Leske, 1991; Ward, 2001): Support (interpersonal and emotional needs); Comfort (personal and physical comfort); Information (pragmatic information about the infant); Proximity (remain in the range of infant); and Assurance (experience confidence about the infant). The NICU Family Needs Inventory comprised 56 items to measure the importance attributed to parents’ needs using a 5-point Likert scale incorporated into each item: 5 = extremely important, 4 = important, 3 = moderately important, 2 = unimportant, and 1 = extremely unimportant. Zhang et al. (2016) translated the NICU-FNI scale into Chinese and evaluated the reliability and validity of the scale, with results indicating Cronbach’s alpha coefficient of 0.957 for the translated NICU-FNI scale, a test–retest reliability of 0.875, and a content validity index (CVI) of 0.934. The correlation coefficients between each dimension and the total score ranged from 0.753 to 0.872, thus demonstrating good reliability and validity in the preliminary testing of the Chinese version of the NICU-FNI scale among parents with a premature infant in the NICU in China. In this study, we utilized the Chinese version of the NICU-FNI scale (Zhang et al., 2016) and re-evaluated its reliability and validity. The findings indicated Cronbach’s alpha coefficient of 0.963 and a test–retest reliability of 0.792 for the NICU-FNI scale, demonstrating good reliability and validity in preliminary testing among grandparents of premature infants in the NICU in China. Building on previous studies (Ward, 2001; Zhang et al., 2016), this questionnaire (see Supplementary material) was developed in two parts: the first part collected demographic information on grandparents, mothers, and newborns, while the second part consisted of the Chinese version of the NICU-FNI scale (40 items).
Study population and sample size
The cross-sectional study was conducted at the Obstetrics and Gynecology office of the Second People’s Hospital of Jingdezhen between February and December 2023. Stringent selection procedures identified a cohort of grandparents visiting infants hospitalized in the NICU as the study sample. In order to uphold the strictness and precision of the research, obstetric nurses were tasked with issuing research invitations to them and delivering comprehensive research information sheets in print format. Upon reception of the information sheets, these grandparents were asked to read and comprehend the contents diligently. Following this, we instructed the grandparents who agreed to participate in the research to complete a questionnaire survey. The inclusion criteria for this study were grandparents whose premature grandchildren were still receiving treatment in the NICU at the time of questionnaire completion. Using the mother’s admission number for preterm infants or the infants’ own admission numbers as unique identifiers, one grandparent was chosen to participate in the survey. In cases involving twins, two grandparents were chosen for the study. Exclusion criteria included grandparents of infants whose grandchildren had completed NICU treatment and were discharged and grandparents who did not understand Chinese.
We calculated the sample size using the Power Analysis and Sample Size (PASS) Version 15.0 software (NCSS, LLC, Kaysville, Utah, USA). A sample of 258 participants, each responding to 40 items, achieves 90% power to detect the difference between the coefficient alpha under the null hypothesis of 0.80 and the coefficient alpha under the alternative hypothesis of 0.85. This is accomplished using a two-sided F-test with a significance level of 0.05 (Bonett, 2002). Considering the estimated 10% non-response rate, we calculated the expected sample size to be 287 participants.
Ethical clearance for this research was granted by the Ethics Committee of the Second People’s Hospital of Jingdezhen, documented by Approval No: 2023-LLLW-07. Moreover, it conformed to the Declaration of Helsinki principles, guaranteeing that informed consent was obtained from all participants.
Statistical analysis
Utilizing descriptive statistics, the study summarized survey responses, representing data in tables with counts and percentages for response categories, assessing response frequency differences across groups using a chi-square test, conducting a one-way ANOVA for comparisons among three or more groups, and investigating correlations between dependent and independent variables through Pearson’s correlation analysis. Univariate linear regression and multivariate multiple linear regression analyses were conducted to find factors relevant to identifying grandparents’ needs. All statistical analyses were performed using SPSS statistical software (version SPSS 20.0, IBM SPSS Inc., Chicago, IL, USA). p-values <0.05 were considered to indicate statistical significance.
Results
Demographics of the respondents
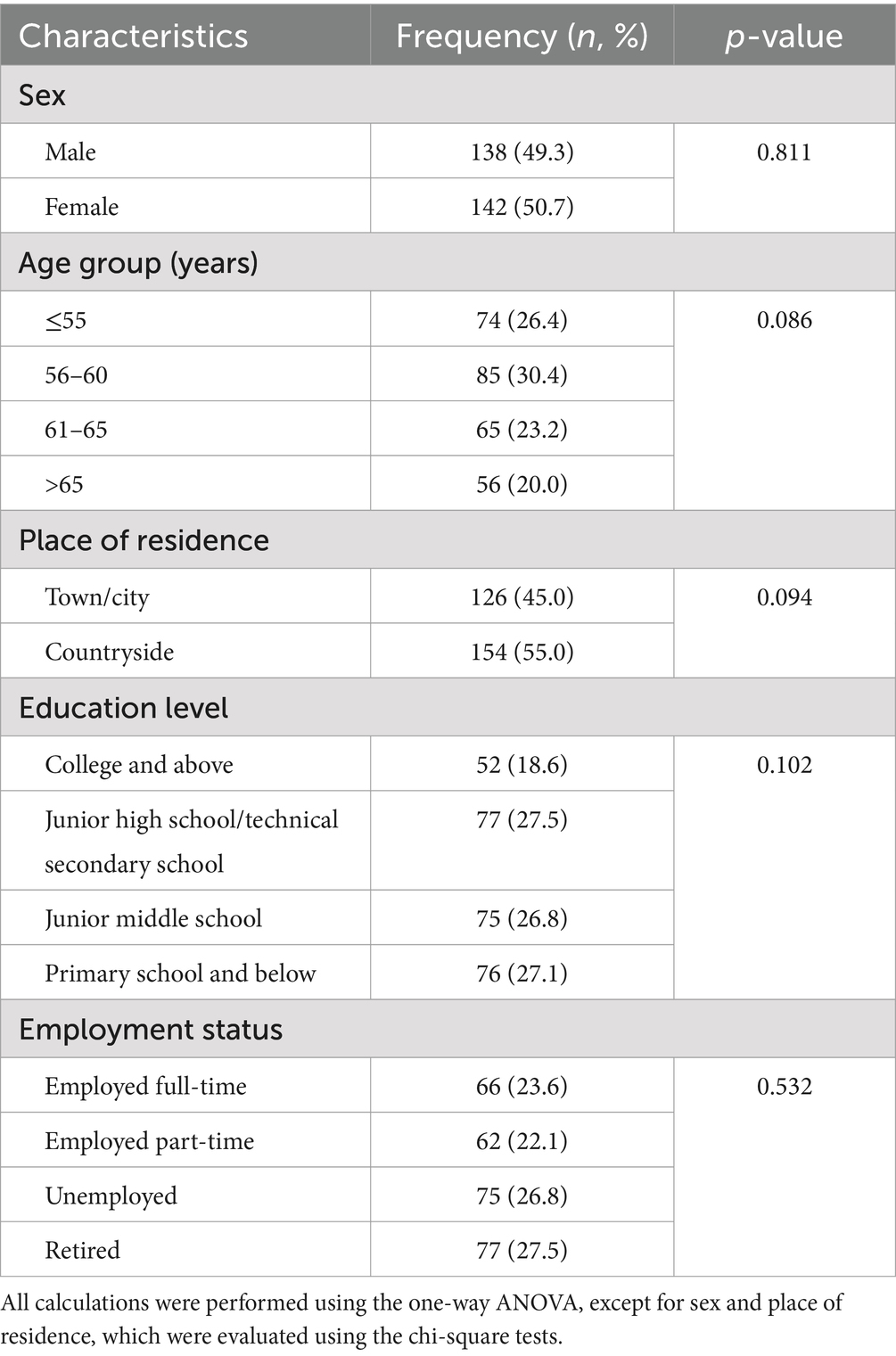
The questionnaires were distributed to 287 grandparents, with 280 completed and returned. All respondents belonged to independent families associated with the NICU, meaning that each family had only one grandparent complete the questionnaire, resulting in a response rate of 97.6%. As shown in Table 1, among these 280 participants, grandmothers constituted 50.7%. The mean age of participants was 59.6 years (S.D. = 7.2 years). Regarding age groups, the proportions were as follows: ≤55 years (26.4%), 56–60 years (30.4%), 61–65 years (23.2%), and > 65 years (20.0%). In terms of place of residence, 45.0% of the grandparents lived in towns or cities, whereas 55.0% resided in the countryside. In terms of education level, the proportions were as follows: college and above (18.6%), junior high school/technical secondary school (27.5%), junior middle school (26.8%), and primary school and below (27.1%). Furthermore, employment status distribution includes full-time employment (23.6%), part-time employment (22.1%), unemployment (26.8%), and retirement (27.5%).
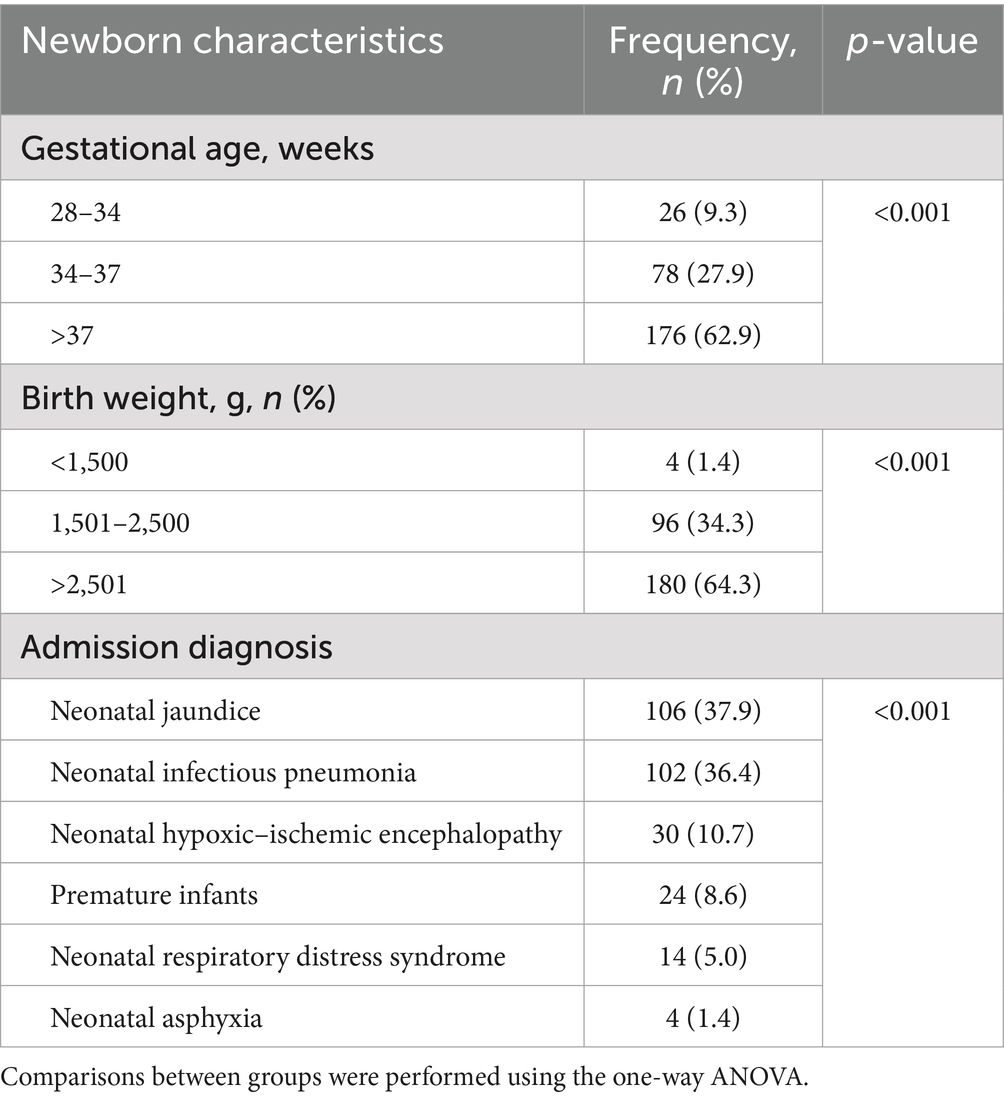
As shown in Table 2, the distribution of newborn characteristics revealed significant variations in gestational age, birth weight, and admission diagnosis. Gestational age categories were as follows: 28–34 weeks (9.3%), 34–37 weeks (27.9%), and over 37 weeks (62.9%), showing a statistically significant difference (p < 0.001). Birth weight categories included under 1,500 g (1.4%), 1,501–2500 g (34.3%), and over 2,501 g (64.3%), with a notable statistical significance (p < 0.001). In terms of admission diagnosis, the frequencies were as follows: neonatal jaundice (37.9%), neonatal infectious pneumonia (36.4%), neonatal hypoxic–ischemic encephalopathy (10.7%), premature infants (8.6%), neonatal respiratory distress syndrome (5.0%), and neonatal asphyxia (1.4%). The differences in admission diagnoses were also found to be statistically significant (p < 0.001).
The most and least important needs of grandparents
The 10 most and least important aspects, based on the results from the NICU-FNI scale, can be found in Table 3. Among the top 10 most important needs, six items for Assurance emerged as a significant factor, with grandparents expressing a strong desire for their infant to receive the best care even in their absence from the hospital. Additionally, grandparents emphasized the importance of being informed about their baby’s condition and treatments, having their questions answered honestly, and receiving explanations in a clear and understandable manner. The need for Proximity and Information regarding the baby’s progress also ranked high. On the other hand, among the 10 least important needs, aspects related to Comfort and Support were prominent. Specific requirements, such as restroom availability in the waiting room and private areas in the hospital, were ranked lower in importance. Overall, the findings highlight the crucial role of Assurance, Information, and Support in addressing the needs of grandparents in the NICU while suggesting that certain Comfort-related factors may be of lesser priority.
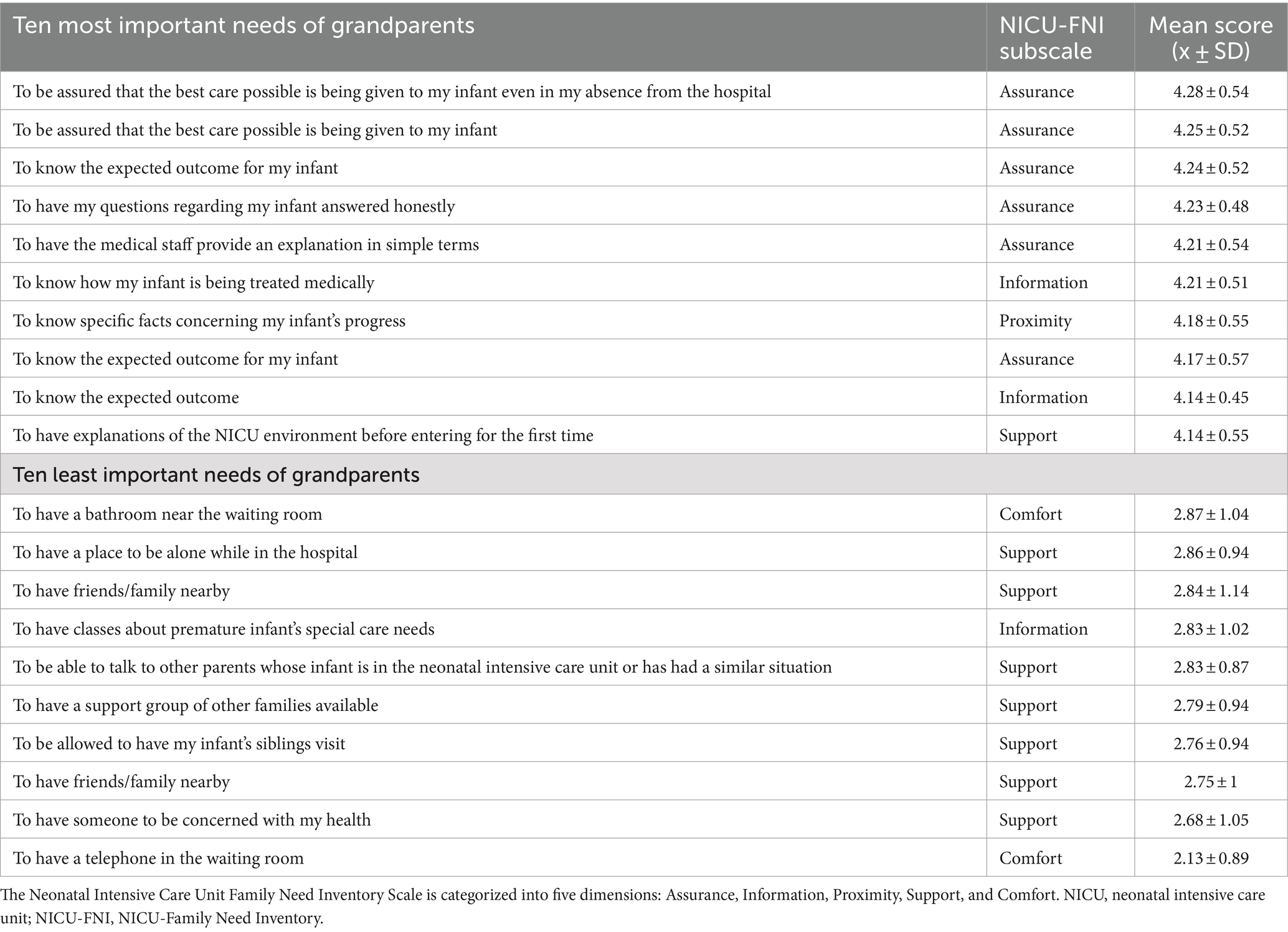
Table 3. Ten most and least important needs of grandparents according to NICU-FNI scale scores (n = 280).
NFNI subscale scores and their rankings
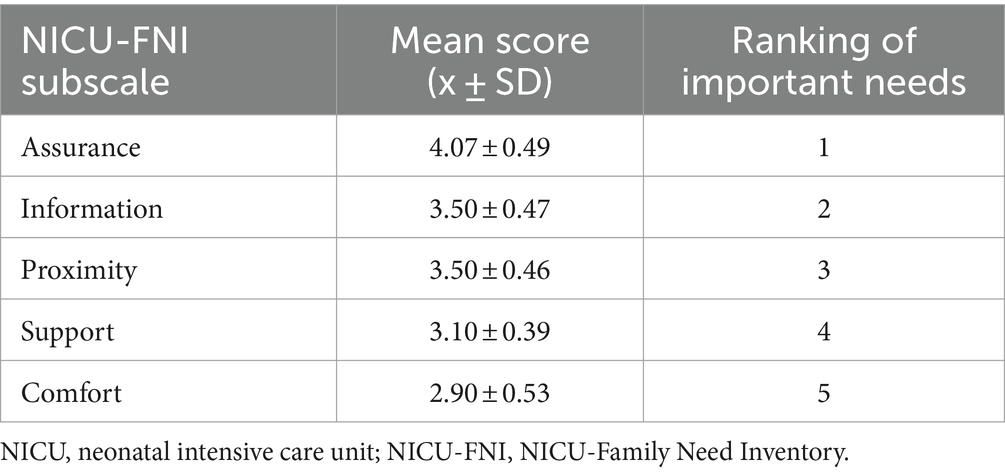
Among the identified subscales, “Assurance” received the highest mean score of 4.07 ± 0.49, ranking it as the most important need for grandparents in the NICU setting. This underscored the significance of providing reassurance and emotional Support to grandparents during this difficult time. The subscales “Information” and “Proximity” obtained identical mean scores of 3.50 ± 0.47 and 3.50 ± 0.46, respectively, indicating their equal importance in the second and third positions. These findings highlight the value of clear and comprehensive Information about the infant’s condition and the opportunity for grandparents to be physically close to their grandchild. The “Support” subscale had a mean score of 3.10 ± 0.39, placing it fourth in importance. This suggests that grandparents greatly benefit from various forms of Support, such as emotional, practical, and social support, while their grandchild is in the NICU. Finally, the “Comfort” subscale received the lowest mean score of 2.90 ± 0.53; it ranked fifth, indicating that although Comfort is still important, it may be less prioritized by grandparents than other needs. In conclusion, grandparents in the NICU setting primarily value Assurance, followed by the need for Information and Proximity. Support is also crucial, whereas Comfort holds a slightly lower priority. These findings shed light on the needs of grandparents and emphasize the importance of addressing them to provide optimal Support and care during their grandchild’s NICU stay (Table 4).
Correlation between grandparents’ needs and demographic characteristics
In Table 5, we identify statistically significant correlations between the needs of grandparents and their demographic attributes, as well as those of preterm infants. Specifically, the age of the grandparents is positively associated with the need for Proximity (r = 0.143; p < 0.05), suggesting older grandparents have more demand for proximity to preterm infants. The educational attainment of grandparents is positively related to the need for Information (r = 0.135; p < 0.05), yet inversely related to the need for Proximity (r = 0.159; p < 0.01), revealing that grandparents with lower education levels may seek less Information but desire greater Proximity to their grandchildren. The employment status of grandparents is associated with Assurance (r = 0.122; p < 0.05), Proximity (r = 0.219; p < 0.01), and Support (r = 0.138; p < 0.05), suggesting that retired grandparents may seek a more profound connection with grandchildren. The place of residence of grandparents is positively associated with the need for Assurance (r = 0.179; p < 0.01), Proximity (r = 0.168; p < 0.01), and Comfort (r = 0.118; p < 0.05), indicating that grandparents residing in rural areas may exhibit a greater need for these aspects than those in urban settings.
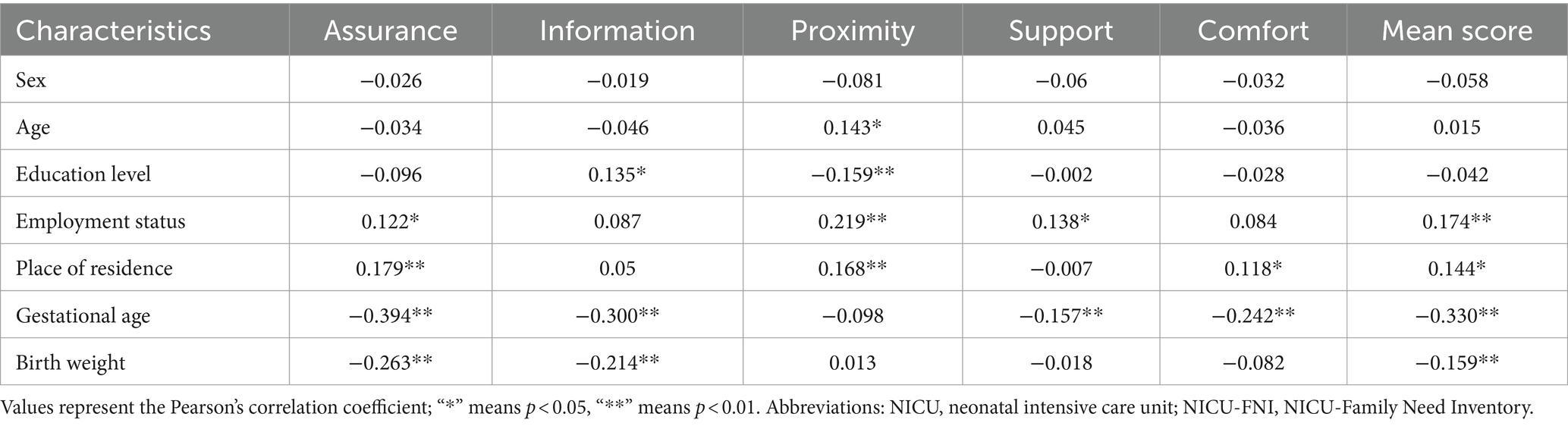
Table 5. Statistically significant correlations between grandparents’ needs and demographic characteristics.
Regarding the attributes of preterm infants, there is a negative correlation between gestational age and the grandparents’ needs for Assurance, Information, Support, and Comfort, as well as the overall need score. This indicates that as the gestational age of a premature infant at birth increases, the needs of the grandparents decrease. The birth weight is inversely related to the need for Assurance (r = −0.263; p < 0.01) and Information (r = −0.214; p < 0.01), potentially indicating heightened concern among grandparents for the health issues pertaining to infants with lower birth weights.
Multiple linear regression analysis of needs among grandparents
Multiple linear regression analysis was employed to elucidate the determinants of grandparents’ needs. Six family needs models were identified for the analysis (covering the grandparents’ needs), focusing on the mean scores of NICU-FNI, including the needs for Assurance, Information, Proximity, Support, and Comfort.
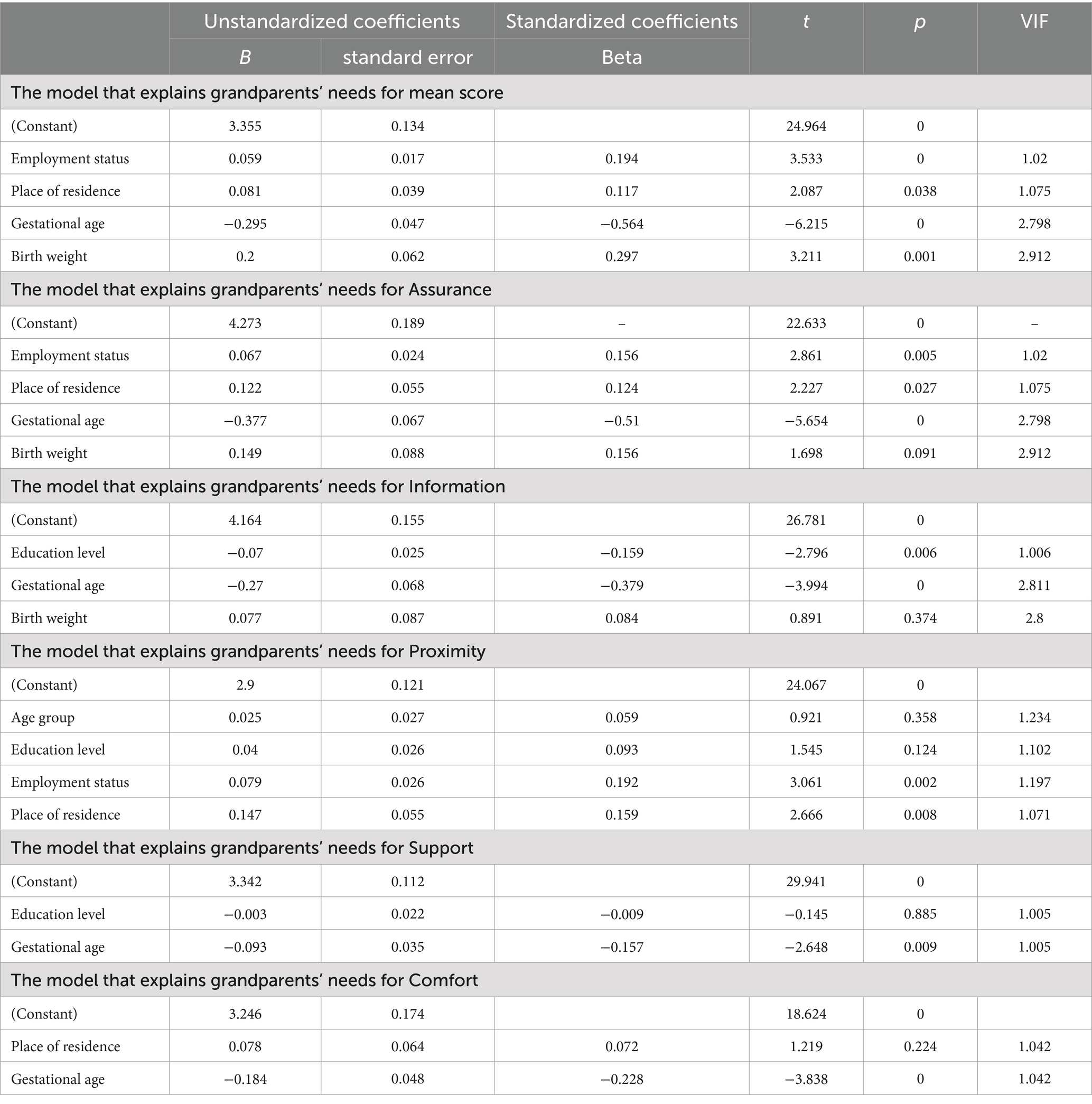
The results from the multiple regression models, which analyzed the needs of grandparents across different dimensions, identify key predictors that are associated with various aspects of Support in the NICU as depicted in Table 6. The mean score model highlights significant associations between the mean score and employment status (p = 0), place of residence (p = 0.038), and birth weight (p = 0.001). This indicates that grandparents who are retired, live in rural areas, and have grandchildren with lower birth weights have greater needs. In the domain of Assurance, the predictors of significance were employment status (p = 0.005), place of residence (p = 0.027), and gestational age (p = 0), indicating that grandparents who are retired and residing in rural locales, along with their grandchildren of lower birth weights, possess an augmented need for Assurance. The Information model revealed that the level of education (p = 0.006) and gestational age (p = 0) exert significant impacts on the need for Information, indicating that grandparents possessing higher educational qualifications and their grandchildren with reduced birth weights exhibit a more substantial need for Information. The Proximity model identified employment status (p = 0.002) and place of residence (p = 0.008) as significant predictors, suggesting that grandparents who are retired and reside in rural areas have an increased need for Proximity. In the Comfort model, gestational age (p = 0) was the only factor identified as a significant predictor, whereas the Support model showed no significant predictors. The findings highlight the importance of considering specific factors when addressing the diverse needs of grandparents in the NICU, providing valuable insights for tailored Support interventions.
Discussion
The care provided in the neonatal intensive care unit (NICU) is vital for preterm infants (Cao et al., 2021). However, this type of care presents significant economic, psychological, and health challenges for the families of preterm infants (Geng et al., 2022; Grunberg et al., 2022). Despite ample evidence regarding the needs of parents in the NICU, the needs of other family members, such as grandparents, are often overlooked (Adama et al., 2022; Maleki et al., 2022). Grandparents, however, play a crucial role in providing support to the family (Hillis et al., 2021), and it is important to understand their needs in order to improve NICU care practices. This study aimed to provide a comprehensive investigation of the needs of this particular group, thereby making an additional contribution to the existing body of literature.
The findings of this study reveal that grandparents’ foremost concern is the Assurance of the infant’s safety and wellbeing. Studies involving parents of preterm infants in the NICU have consistently identified Assurance as the top priority (Alsaiari et al., 2019; Govindaswamy et al., 2020). Similarly, family members of critical care patients have emphasized the importance of Assurance (Kang et al., 2020), and nurses have also deemed Assurance as the most critical need for family members of patients admitted to critical care units (Khatri Chhetri and Thulung, 2018). It is both expected and understandable that all family members, including grandparents and parents, prioritize health assurance for these infants, recognizing it as a crucial necessity.
In the hierarchy of importance among the remaining four dimensions, the needs of grandparents of preterm infants in the NICU are prioritized as follows: Information, Proximity, Support, and Comfort. In comparison, the needs of Saudi parents of preterm infants are ranked as Proximity, Information, Comfort, and Support (Alsaiari et al., 2019), while another study focused on the needs of fathers, ranking them as Proximity, Information, Support, and Comfort (Govindaswamy et al., 2020). The variations in family member inclusion across research studies and differences in hospital policies regarding visitation for preterm infants in the NICU may elucidate this discrepancy. In Saudi hospitals, parents are permitted to visit their infants around the clock; thus, Alsaiari et al. excluded two Proximity-related items from the NICU-FNI scale: “to be able to visit my infant at any time” and “to see my infant frequently” (Alsaiari et al., 2019). In China, NICUs employ a closed management approach alongside the traditional practice of “sitting the month.” This results in minimal opportunities for mothers of premature infants to observe their newborns after birth, and even fewer opportunities for other relatives to have contact with the baby at that time (Ling et al., 2022). Consequently, our research emphasizes the heightened significance of Information and Proximity for grandparents. Prior research suggests that the Information needs of family members of patients in critical care are the second most significant, irrespective of the family’s educational or cultural background (Kang et al., 2020; Wesson, 1997). Studies indicate that family members of patients admitted to critical care units frequently seek Proximity and Information as coping mechanisms to alleviate anxiety (Baharoon et al., 2017; Wang et al., 2018). This aligns with the family resilience framework, which underscores the importance of clear communication and emotional closeness as factors that bolster resilience. When family members are well-informed and have opportunities for meaningful involvement, they are better equipped to manage the emotional and psychological stress associated with NICU experiences (Walsh, 2016).
The results of this study reveal a significant negative correlation between the gestational age of preterm infants and the grandparents’ need for Assurance, Information, Support, and Comfort, as well as the overall need score. This suggests that as the gestational age of a premature infant at birth increases, the needs of the grandparents decrease. It is worth noting that previous studies have indicated a similar trend: as an infant spends more time in the NICU, family members place less emphasis on seeking Information about the infant (Nicholas, 2018; Alsaiari et al., 2019). Furthermore, the psychological stress, anxiety, and fear experienced by family members are found to escalate as the infant’s condition deteriorates. However, when there is an improvement in the infant’s health, these negative emotions gradually subside (Heidari et al., 2012; Jackson et al., 2003). This inverse relationship between the severity of the infant’s condition and the emotional state of the family members could be attributed to the fact that the occurrence and severity of multiple diseases are linked to gestational age and birth weight. Conditions such as respiratory distress syndrome (Mikolajcikova et al., 2022), bronchopulmonary dysplasia (Trembath and Laughon, 2012), and necrotizing enterocolitis (Battersby et al., 2017) are more likely to occur in infants with lower gestational age and birth weight.
The needs related to Support (interpersonal and emotional) and Comfort (personal and physical) are the lowest priority for grandparents. Concerning the hospital infrastructure, elements such as the Proximity of a bathroom to the waiting area, the provision of a solitary space within the hospital, and the presence of a phone in the parental waiting room are not the foremost considerations of grandparents. This underscores grandparents’ tendency to place the Comfort and Support needs of the mother and baby above their personal needs, a perspective that aligns with findings on paternal needs (Ireland et al., 2016).
This study does not negate the fact that parental involvement in newborn care within the NICU is a currently favored healthcare approach (Zanoni et al., 2021). Furthermore, decisions regarding emergency treatment for NICU patients and communication with doctors position parents as taking a leading position among family members (Govindaswamy et al., 2020). However, upon the admission of their newborn to the NICU, parents often experience anxiety, depression, guilt, and helplessness due to their unpreparedness and lack of parenting experience, the unpredictability associated with their preterm infant’s stay in an unfamiliar NICU environment, the closed management system of the NICU, the uncertainty of their infant’s medical condition, prognostic worries, and substantial hospital expenses (Diffin et al., 2016; Whittingham et al., 2014). These challenges often result in their inability to understand nurses’ explanations or engage in the caregiving process (Ladani et al., 2017). Moreover, fathers particularly wish for grandparents to assist in alleviating their stress, as mothers require care following childbirth, thereby positioning grandparents as their most trusted allies (Aliabadi et al., 2014). Hence, grandparents could serve as a vital communication bridge between nurses and parents, lowering the communication burden on nurses and fostering a collaborative relationship, ultimately contributing to improved care and expectations for the newborn (Wigert et al., 2013).
As with any survey-based research, our study has certain limitations. First, because of the cross-sectional design of this study, we are unable to assess changes in the needs of grandparents of preterm infants in the NICU over time. Additionally, our sample was limited to grandparents from a specific region in China, which may limit the broader applicability of our findings. Third, the self-completion nature of the questionnaires introduces the potential for bias due to social desirability. Given these factors, it is important to interpret the research findings with caution.
Conclusion
This study aimed to broaden the scope of research concerning the needs of grandparents with preterm infants in NICU, complementing the existing studies that have predominantly centered on the needs of parents. The research reveals that grandparents primarily desire Assurance regarding the safety and health of their grandchild, indicating a substantial level of concern about the quality of care. Additionally, secondary needs related to Information and Proximity were identified.
The findings demonstrate a significant negative correlation between the gestational age of preterm infants and the grandparents’ needs for Assurance, Information, Support, and Comfort. As the gestational age increases, the expressed needs of grandparents tend to diminish, supporting previous findings that suggest family members experience less anxiety and a decreased demand for information as infants stabilize.
The results underscore the critical role grandparents play within the family support system and highlight the necessity of recognizing and addressing their needs in clinical practice. Recognizing these needs is essential not only for alleviating family stress but also for enhancing overall care quality within NICUs. By emphasizing family-centered care, the study advocates for policies and practices that acknowledge and support the involvement of grandparents during such challenging times.
While this research provides valuable insights, its cross-sectional design constrains the ability to monitor changes in needs over time. Moreover, the sample was limited to a specific region in China, potentially affecting the generalizability of the findings. Future research should employ longitudinal designs to assess the evolution of grandparents’ needs and to explore these needs across diverse cultural and healthcare contexts.
In conclusion, this study serves as a call to action for healthcare providers and policymakers to integrate the needs of grandparents into NICU care practices, ensuring they receive appropriate support, communication, and engagement during challenging periods for the entire family. This approach could enhance the psychological wellbeing of families and improve the quality of care in NICUs.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Second People's Hospital of Jingdezhen, documented by Approval No: 2023-LLLW-07. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HH: Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. JT: Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. YL: Investigation, Methodology, Writing – original draft, Writing – review & editing. RC: Investigation, Methodology, Writing – review & editing. HF: Conceptualization, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Science and Technology Plan of Jiangxi Provincial Health (no. 202311670).
Acknowledgments
The authors thank all the participants involved in the survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1433391/full#supplementary-material
References
Adama, E. A., Adua, E., Bayes, S., and Mörelius, E. (2022). Support needs of parents in neonatal intensive care unit: an integrative review. J. Clin. Nurs. 31, 532–547. doi: 10.1111/jocn.15972
Aliabadi, F., Kamali, M., Borimnejad, L., Rassafiani, M., Rasti, M., Shafaroodi, N., et al. (2014). Supporting-emotional needs of Iranian parents with premature infants admitted to neonatal intensive care units. Med. J. Islam Repub. Iran 28:53
Alsaiari, E. M., Magarey, J., and Rasmussen, P. (2019). An investigation of the needs of Saudi parents of preterm infants in the neonatal intensive care unit. Cureus 11:e3887. doi: 10.7759/cureus.3887
Arockiasamy, V., Holsti, L., and Albersheim, S. (2008). Fathers' experiences in the neonatal intensive care unit: a search for control. Pediatrics 121, e215–e222. doi: 10.1542/peds.2007-1005
Baharoon, S., AlYafi, W., Al Qurashi, A., Al Jahdali, H., Tamim, H., Alsafi, E., et al. (2017). Family Satisfaction in Critical Care Units: Does an Open Visiting Hours Policy Have an Impact? J. Patient Saf. 3, 169–174. doi: 10.1097/pts.0000000000000140
Battersby, C., Longford, N., Mandalia, S., Costeloe, K., and Modi, N. (2017). Incidence and enteral feed antecedents of severe neonatal necrotising enterocolitis across neonatal networks in England, 2012-13: a whole-population surveillance study. Lancet Gastroenterol. Hepatol. 2, 43–51. doi: 10.1016/s2468-1253(16)30117-0
Bernaix, L. W., Schmidt, C. A., Jamerson, P. A., Seiter, L., and Smith, J. (2006). The NICU experience of lactation and its relationship to family management style. MCN Am. J. Matern. Child Nurs. 31, 95–100. doi: 10.1097/00005721-200603000-00008
Bonett, D. G. (2002). Sample size requirements for testing and estimating coefficient alpha. J. Educ. Behav. Stat. 27, 335–340. doi: 10.3102/10769986027004335
Brødsgaard, A., Helth, T., Andersen, B. L., and Petersen, M. (2017). Rallying the troops: how sharing knowledge with grandparents supports the family of the preterm infant in neonatal intensive care unit. Adv. Neonatal Care 17, E1–e10. doi: 10.1097/anc.0000000000000360
Cao, Y., Jiang, S., Sun, J., Hei, M., Wang, L., Zhang, H., et al. (2021). Assessment of neonatal intensive care unit practices, morbidity, and mortality among very preterm infants in China. JAMA Netw. Open 4:e2118904. doi: 10.1001/jamanetworkopen.2021.18904
Chen, H.-M., and Lewis, D. C. (2015). Chinese grandparents’ involvement in their adult Children’s parenting practices in the United States. Contemp. Fam. Ther. 37, 58–71. doi: 10.1007/s10591-014-9321-7
Chen, F., Liu, G., and Mair, C. A. (2011). Intergenerational ties in context: grandparents caring for grandchildren in China. Soc. Forces 90, 571–594. doi: 10.1093/sf/sor012
Chow, S., Chow, R., Popovic, M., Lam, M., Popovic, M., Merrick, J., et al. (2015). A selected review of the mortality rates of neonatal intensive care units. Front. Public Health 3:225. doi: 10.3389/fpubh.2015.00225
Diffin, J., Shields, M. D., Cruise, S., and Johnston, L. (2013). Parents' experiences of caring for their infant following surgery in the neonatal period: a literature review. J. Neonatal Nurs. 19, 271–289. doi: 10.1016/j.jnn.2012.10.002
Diffin, J., Spence, K., Naranian, T., Badawi, N., and Johnston, L. (2016). Stress and distress in parents of neonates admitted to the neonatal intensive care unit for cardiac surgery. Early Hum. Dev. 103, 101–107. doi: 10.1016/j.earlhumdev.2016.08.002
Gao, J., Li, J. X., Chen, W. Y., Song, J. Y., Zhou, M. K., Zhang, S. S., et al. (2022). A randomized controlled trial of a coping-focused family resilience intervention program for breast cancer patients: study protocol. Front. Psychol. 13:968154. doi: 10.3389/fpsyg.2022.968154
Geng, K., Yu, C., Gao, C., Liu, S., Zhou, L., Zhu, B., et al. (2022). Translation and reliability and galidity testing of the Chinese version of the perceived stressors in intensive care units. Chin J Nurs Educ 19, 927–932. doi: 10.3761/j.issn.1672-9234.2022.10.012
Govindaswamy, P., Laing, S. M., Waters, D., Walker, K., Spence, K., and Badawi, N. (2020). Fathers' needs in a surgical neonatal intensive care unit: assuring the other parent. PLoS One 15:e0232190. doi: 10.1371/journal.pone.0232190
Grunberg, V. A., Geller, P. A., Hoffman, C., Njoroge, W., Ahmed, A., and Patterson, C. A. (2022). Parental mental health screening in the NICU: a psychosocial team initiative. J. Perinatol. 42, 401–409. doi: 10.1038/s41372-021-01217-0
Harris, L. M., Shabanova, V., Martinez-Brockman, J. L., Leverette, D., Dioneda, B., Parker, M. G., et al. (2024). Parent and grandparent neonatal intensive care unit visitation for preterm infants. J. Perinatol. 44, 419–427. doi: 10.1038/s41372-023-01745-x
Heidari, H., Hasanpour, M., and Fooladi, M. (2012). The Iranian parents of premature infants in NICU experience stigma of shame. Med. Arh. 66, 35–40. doi: 10.5455/medarh.2012.66.35-40
Hillis, S. D., Unwin, H. J. T., Chen, Y., Cluver, L., Sherr, L., Goldman, P. S., et al. (2021). Global minimum estimates of children affected by COVID-19-associated orphanhood and deaths of caregivers: a modelling study. Lancet 398, 391–402. doi: 10.1016/s0140-6736(21)01253-8
Ireland, J., Minesh, K., Cescutti-Butler, L., van Teijlingen, E., and Hewitt-Taylor, J. (2016). Experiences of fathers with babies admitted to neonatal care units: a review of the literature. J. Neonatal Nurs. 22, 171–176. doi: 10.1016/j.jnn.2016.01.006
Jackson, K., Ternestedt, B. M., and Schollin, J. (2003). From alienation to familiarity: experiences of mothers and fathers of preterm infants. J. Adv. Nurs. 43, 120–129. doi: 10.1046/j.1365-2648.2003.02686.x
Jacono, J., Hicks, G., Antonioni, C., O'Brien, K., and Rasi, M. (1990). Comparison of perceived needs of family members between registered nurses and family members of critically ill patients in intensive care and neonatal intensive care units. Heart Lung 19, 72–78.
Jain, N. J., Faiz, A. S., Ohman-Strickland, P. A., Smulian, J. C., and Rhoads, G. G. (2021). Educational attainment of grandmothers and preterm birth in grandchildren. Matern. Child Health J. 25, 293–301. doi: 10.1007/s10995-020-03021-2
Johnson, A. N. (2008). Engaging fathers in the NICU: taking down the barriers to the baby. J. Perinat. Neonatal Nurs. 22, 302–306. doi: 10.1097/01.Jpn.0000341361.37822.34
Kang, J., Cho, Y. J., and Choi, S. (2020). State anxiety, uncertainty in illness, and needs of family members of critically ill patients and their experiences with family-centered multidisciplinary rounds: a mixed model study. PLoS One 15:e0234296. doi: 10.1371/journal.pone.0234296
Khatri Chhetri, I., and Thulung, B. (2018). Perception of nurses on needs of family members of patient admitted to critical care units of teaching hospital, Chitwan Nepal: a cross-sectional institutional based study. Nurs. Res. Pract. 2018, 1369164–1369167. doi: 10.1155/2018/1369164
Kim, H. N. (2018). Social support provision: perspective of fathers with preterm infants. J. Pediatr. Nurs. 39, 44–48. doi: 10.1016/j.pedn.2018.01.017
Kirschbaum, M. S. (1990). Needs of parents of critically ill children. Dimens. Crit. Care Nurs. 9, 344–353. doi: 10.1097/00003465-199011000-00009
Ladani, M. T., Abdeyazdan, Z., Sadeghnia, A., Hajiheidari, M., and Hasanzadeh, A. (2017). Comparison of nurses and Parents' viewpoints regarding the needs of parents of premature infants in neonatal intensive care units. Iran. J. Nurs. Midwifery Res. 22, 367–371. doi: 10.4103/1735-9066.215672
Lambiase, C. V., Mansi, G., Salomè, S., Conelli, M. L., Vendemmia, M., Zurlo, M. C., et al. (2024). The financial burden experienced by families during NICU hospitalization and after discharge: a single center, survey-based study. Eur. J. Pediatr. 183, 903–913. doi: 10.1007/s00431-023-05352-y
Leske, J. S. (1991). Internal psychometric properties of the critical care family needs inventory. Heart Lung 20, 236–244.
Ling, Y., Wang, T., Zhang, X., Wang, A., and Zhang, H. (2022). Meta-synthesis of qualitative research on parental experience and needs of premature in fants in NICU during hospitalization. J. Nur. Train. 37, 1025–1038. doi: 10.16821/j.cnki.hsjx.2022.11.014
Lorié, E. S., Wreesmann, W. W., van Veenendaal, N. R., van Kempen, A., and Labrie, N. H. M. (2021). Parents' needs and perceived gaps in communication with healthcare professionals in the neonatal (intensive) care unit: a qualitative interview study. Patient Educ. Couns. 104, 1518–1525. doi: 10.1016/j.pec.2020.12.007
Maleki, M., Mardani, A., Harding, C., Basirinezhad, M. H., and Vaismoradi, M. (2022). Nurses' strategies to provide emotional and practical support to the mothers of preterm infants in the neonatal intensive care unit: a systematic review and meta-analysis. Womens Health 18:17455057221104674. doi: 10.1177/17455057221104674
Mikolajcikova, S., Lasabova, Z., Holubekova, V., Skerenova, M., Zibolenova, J., Matasova, K. Sr., et al. (2022). The common haplotype GATGACA in surfactant-protein B gene is protective for respiratory distress syndrome in preterm neonates. Front. Pediatr. 10:851042. doi: 10.3389/fped.2022.851042
Nicholas, Amy Lynne . (2018). An examination of the needs of mothers with infants in the neonatal intensive care unit. Digital Repository at the University of Maryland, Available at: https://drum.lib.umd.edu/handle/1903/3465
WHO (2012). Born too soon: The global action report on preterm birth, vol. 380. Geneva: World Health Organisation.
Pepper, D., Rempel, G., Austin, W., Ceci, C., and Hendson, L. (2012). More than information: a qualitative study of Parents' perspectives on neonatal intensive Care at the Extremes of prematurity. Adv. Neonatal Care 12, 303–309. doi: 10.1097/ANC.0b013e318265b3d5
Shao, M., Yang, H., Du, R., Zhang, M., Zhu, J., Zhang, H., et al. (2023). Family resilience in cancer treatment and key influencing factors: a systematic review. Eur. J. Oncol. Nurs. 66:102403. doi: 10.1016/j.ejon.2023.102403
Sun, X., Chen, S., Teng, Y., Wang, H., and Liu, D. (2024). Status and influencing factors of the discharge readiness of fathers of preterm infants in NICU. Chin. J. Nurs. 59, 455–461. doi: 10.3761/j.issn.0254-1769.2024.04.010
Trembath, A., and Laughon, M. M. (2012). Predictors of bronchopulmonary dysplasia. Clin. Perinatol. 39, 585–601. doi: 10.1016/j.clp.2012.06.014
Walsh, F. (2016). Applying a family resilience framework in training, practice, and research: mastering the art of the possible. Fam. Process 55, 616–632. doi: 10.1111/famp.12260
Wang, L., He, J. L., and Fei, S. L. (2018). Perceived Needs of Parents of Premature Infants in NICU. West. J. Nurs. Res. 5, 688–700. doi: 10.1177/0193945916683679
Ward, K. (2001). Perceived needs of parents of critically ill infants in a neonatal intensive care unit (NICU). Pediatr. Nurs. 27, 281–286
Wesson, J. S. (1997). Meeting the informational, psychosocial and emotional needs of each ICU patient and family. Intensive Crit. Care Nurs. 2, 111–118. doi: 10.1016/s0964-3397(97)80271-6
Whittingham, K., Boyd, R. N., Sanders, M. R., and Colditz, P. (2014). Parenting and prematurity: understanding parent experience and preferences for support. J. Child Fam. Stud. 23, 1050–1061. doi: 10.1007/s10826-013-9762-x
Wigert, H., Dellenmark, M. B., and Bry, K. (2013). Strengths and weaknesses of parent-staff communication in the NICU: a survey assessment. BMC Pediatr. 13:71. doi: 10.1186/1471-2431-13-71
Yang, H., Yu, Y., Liu, K., and Shen, R. (2017). Analysis on the effect of two-child policy on the incidence rate and outcome of premature infants in Beijing. Mat. Child Health Care China 32, 10–12. doi: 10.7620/zgfybj.j.issn.1001-4411.2017.01.04
Zanoni, P., Scime, N. V., Benzies, K., McNeil, D. A., and Mrklas, K. (2021). Facilitators and barriers to implementation of Alberta family integrated care (FICare) in level II neonatal intensive care units: a qualitative process evaluation substudy of a multicentre cluster-randomised controlled trial using the consolidated framework for implementation research. BMJ Open 11:e054938. doi: 10.1136/bmjopen-2021-054938
Zhang, J., Fokkema, T., and Arpino, B. (2022). Loneliness among Chinese older adults: the role of grandparenthood and grandparental childcare by gender. J. Fam. Issues 43, 3078–3099. doi: 10.1177/0192513x211041992
Zhang, S., Liu, Y., Liu, Y., Huang, S., and Zhang, X. (2016). Reliability and validity of the Chinese version of neonatal intensive care unit newborns' family needs. Chin. J. Nurs. 51:6. doi: 10.3761/j.issn.0254-1769.2016.06.011
Zhang, Y., Zhu, Y., and Chen, C. (2021). Incidence and changing trend of preterm infants. Chin. J. Neonatol. 36, 74–77. doi: 10.3760/cma.j.issn.2096-2932.2021.04.021
Keywords: preterm infants, neonatal intensive care unit, grandparents, critical illness, family needs, China
Citation: Huang H, Tao J, Lei Y, Chen R and Fang H (2024) Assessing the needs of grandparents of preterm infants in neonatal intensive care units: a cross-sectional study. Front. Psychol. 15:1433391. doi: 10.3389/fpsyg.2024.1433391
Edited by:
Livio Provenzi, University of Pavia, ItalyReviewed by:
Benedetta Ragni, Libera Università Maria SS. Assunta, ItalyChristine Tuden Neugebauer, Texas Tech University Health Sciences Center, United States
Copyright © 2024 Huang, Tao, Lei, Chen and Fang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haixia Fang, Zmh4MTM5Nzk4MzU0ODJAMTYzLmNvbQ==
 Huamin Huang
Huamin Huang Jingyun Tao
Jingyun Tao Ying Lei
Ying Lei Rui Chen
Rui Chen Haixia Fang
Haixia Fang