- Department of Human, Social, and Health Sciences, University of Cassino, Cassino, Italy
This health literacy intervention study, conducted on adolescent students, aimed to evaluate the impact of a comprehensive educational program on promoting healthy eating habits. The intervention sought to enhance adolescents’ knowledge about nutrition, foster self-regulation skills, and ultimately improve their overall health, including their body mass index (BMI). Through a multi-component approach that combined theoretical learning with practical activities and the integration of digital tools such as the MyFitnessPal app, the study targeted improvements in food literacy, which encompasses nutrition knowledge, food label interpretation skills, and cooking abilities. These elements are critical in influencing adolescents’ food choices and eating behaviors, with a focus on increasing the consumption of fruits and vegetables while reducing the intake of fast food and processed snacks. The intervention was structured around a series of educational workshops and interactive sessions, facilitated by professionals experienced in nutrition. These sessions covered topics such as food composition, the importance of a balanced diet, and strategies for avoiding excessive consumption of processed and high-energy-density foods. A distinctive feature of the program was its use of digital tools to enhance engagement and allow for the practical application of learned concepts through food tracking and activity monitoring. Preliminary results indicate positive outcomes in terms of increased food knowledge and improved dietary habits among participants. Notably, there was a significant improvement in adolescents’ BMI, highlighting the potential of food literacy interventions to contribute to better physical health outcomes. The study underscores the importance of adopting multidisciplinary and technology-enhanced approaches in educational programs aimed at promoting healthy eating among adolescents. The study’s findings suggest that well-structured food education programs, tailored to address the specific needs of adolescents, can facilitate positive changes in eating behavior. This highlights the critical role of food literacy in adolescents’ health and wellbeing and points to the need for continued investment in research and development to optimize intervention strategies. The integration of digital technologies and a focus on self-regulation strategies are identified as promising avenues for future research and educational practice, reinforcing the call for innovative investments in food education and health promotion among the youth.
1 Introduction
Health literacy among adolescents is critical for empowering them to make informed decisions about their health, encompassing not only knowledge of health topics but also the ability to effectively analyze and apply this information in various contexts (Koca and Arkan, 2020; Sørensen et al., 2012). This skill set directly impacts their health behaviors, such as dietary choices and physical activity, which are crucial during the developmental phase of adolescence (Schulenkorf et al., 2022; Cavicchiolo et al., 2022; Tsubakita et al., 2020; Guo et al., 2018).
Research has shown that health literacy among adolescents is linked to various health outcomes, such as medication adherence, mental health, and obesity (Ramos et al., 2023; Malloy-Weir et al., 2016; Murphy et al., 2010). Low levels of health literacy have been associated with negative health behaviors, poorer health status, and an increased risk of overweight and obesity (Guo et al., 2020). Health literacy plays a significant role in promoting positive health behaviors and empowering adolescents to take control of their health (Taba et al., 2022; Mallia et al., 2020; Awofeso et al., 2017).
Food literacy, which includes nutrition knowledge, food label interpretation skills, and cooking abilities, is a crucial aspect of adolescent health and wellbeing. Studies have highlighted that higher levels of food literacy significantly influence adolescents’ food choices and eating behaviors, leading to increased consumption of fruits and vegetables and reduced intake of fast food and processed snacks (Murad et al., 2021; Koca and Arkan, 2020; Vaitkeviciute et al., 2014).
Interventions aimed at enhancing food literacy among adolescents have shown promising results in improving dietary intake and overall health. School-based culinary programs and nutrition education initiatives have successfully increased adolescents’ food skills, nutrition knowledge, and cooking confidence, leading to healthier eating patterns (Labbé et al., 2023; Ruiz et al., 2021; LeRouge et al., 2019). Social media literacy programs have proven effective in reducing risk factors for eating disorders among adolescents, particularly by addressing body dissatisfaction and disordered eating behaviors (Muth et al., 2022; Agam-Bitton et al., 2018; McLean et al., 2017).
The link between health literacy and dietary behaviors in adolescents is well-documented, with higher levels of health literacy being associated with better preventive and healthy eating behaviors (Sarhan et al., 2022; Bektaş et al., 2021). Adolescents with higher health literacy are more aware of unhealthy foods and more likely to develop healthier eating habits. Also, parental health literacy has been correlated with adolescent health behaviors, highlighting the crucial role of parental involvement and support in promoting healthy eating habits among adolescents (Champion et al., 2023).
Adolescents’ eating habits are critical to their health and wellbeing as this life stage is marked by increased nutritional needs due to rapid growth and development (Yoshida-Montezuma et al., 2020). Poor dietary choices during adolescence can lead to serious health issues such as obesity, glucose intolerance, high blood pressure, and dyslipidemia (Kim and Lim, 2019).
Nutritional education and targeted interventions have proven effective in improving adolescents’ eating behaviors and nutrition knowledge (Bektaş et al., 2021; Qutteina et al., 2021; Raikar et al., 2020; Wang et al., 2015). Equipping adolescents with the information and skills necessary to make healthy food choices can significantly improve their long-term health outcomes (Grover and Choudhary, 2017; Yang et al., 2017; LeRouge et al., 2019; Depboylu, 2023).
However, many adolescents have limited food literacy skills, which can hinder their ability to plan, manage, select, prepare, and consume healthy foods (Bereznay et al., 2019). Interventions focused on promoting health literacy related to eating disorders in non-clinical settings have the potential to reduce the disease burden associated with common eating disorders in adolescence (Patton et al., 2008).
In this context, our study aims to evaluate the effectiveness of a targeted health literacy intervention designed to improve adolescents’ food literacy and promote healthier eating habits. The intervention focuses on enhancing their understanding of nutrition, improving their self-regulation skills, and ultimately contributing to better overall health outcomes, including a reduction in body mass index (BMI). The health literacy intervention implemented in this study combines educational workshops, interactive sessions, and the use of digital tools such as the MyFitnessPal app to enhance food literacy, which encompasses nutrition knowledge, food label interpretation skills, and cooking abilities.
2 Materials and methods
The study methodology involved the use of a health literacy intervention on healthy eating conducted on 200 adolescent students. The intervention employed was a multifaceted health literacy program specifically designed to enhance food literacy among adolescents and informed by Velardo (2015) who emphasizes the importance of health literacy, nutrition literacy, and food literacy when designing interventions aimed at improving dietary behaviors, with each playing a role in shaping individuals’ dietary behaviors and overall health outcomes. Food literacy, for example, requires a base of nutrition literacy but also includes practical skills such as cooking and an understanding of where food comes from. Velardo argues that effective interventions should be tailored to address the specific components of food literacy, recognizing that improving food-related knowledge alone is insufficient without also developing practical skills and critical thinking about food choices. Our program integrated educational workshops, practical exercises, and digital tools such as the MyFitnessPal app to improve participants’ knowledge of nutrition, food label interpretation, and self-regulation skills. The intervention was theoretically grounded in social cognitive theory (Bandura, 1986), which emphasizes the role of observational learning, social influence, and self-efficacy in behavior change. According to this theory, individuals learn new behaviors not only through direct experience but also by observing the actions of others and the resulting consequences. This approach is particularly relevant for adolescents, who are strongly influenced by their peers and authority figures. The intervention also incorporated elements of self-determination theory (Deci and Ryan, 1985; Ryan and Deci, 2017; Ryan and Deci, 2000), which focuses on the importance of fulfilling three fundamental psychological needs: autonomy, competence, and relatedness. By promoting these aspects, the intervention aimed to intrinsically motivate adolescents to make healthier food choices by feeling competent in their dietary decisions and supported by their environment.
This methodology was aimed at evaluating the effects of such an intervention on food knowledge, eating habits, and the overall health of adolescents. The method included the use of specific tools to assess these effects and collected quantitative and qualitative data. The study sample consisted of adolescent students selected from various high schools. The health literacy intervention was based on a series of educational workshops, interactive sessions, and educational materials aimed at improving students’ knowledge and eating habits. Before full implementation, the intervention underwent a pilot phase to assess its feasibility and preliminary effectiveness. During this phase, feedback was collected from participants to identify potential issues and opportunities for improvement. Adjustments were made to the educational content and delivery methods to ensure they were appropriately tailored to the target group. During the main intervention, a process evaluation was conducted to ensure fidelity and consistency in its delivery. This process included monitoring the sessions, reviewing practical activities, and tracking participants’ use of digital tools. We primarily focused on enhancing self-regulation skills related to dietary habits, such as goal-setting, planning, and resisting temptations. However, we acknowledge that self-regulation is distinct from practical skills such as cooking or food label interpretation. While our educational workshops did include components aimed at improving these practical skills, the study did not include direct assessments of these competencies. The study was approved by the Institutional Review Board, and all participants (and their legal guardians, in the case of minors) provided written informed consent before participation.
2.1 Participant selection
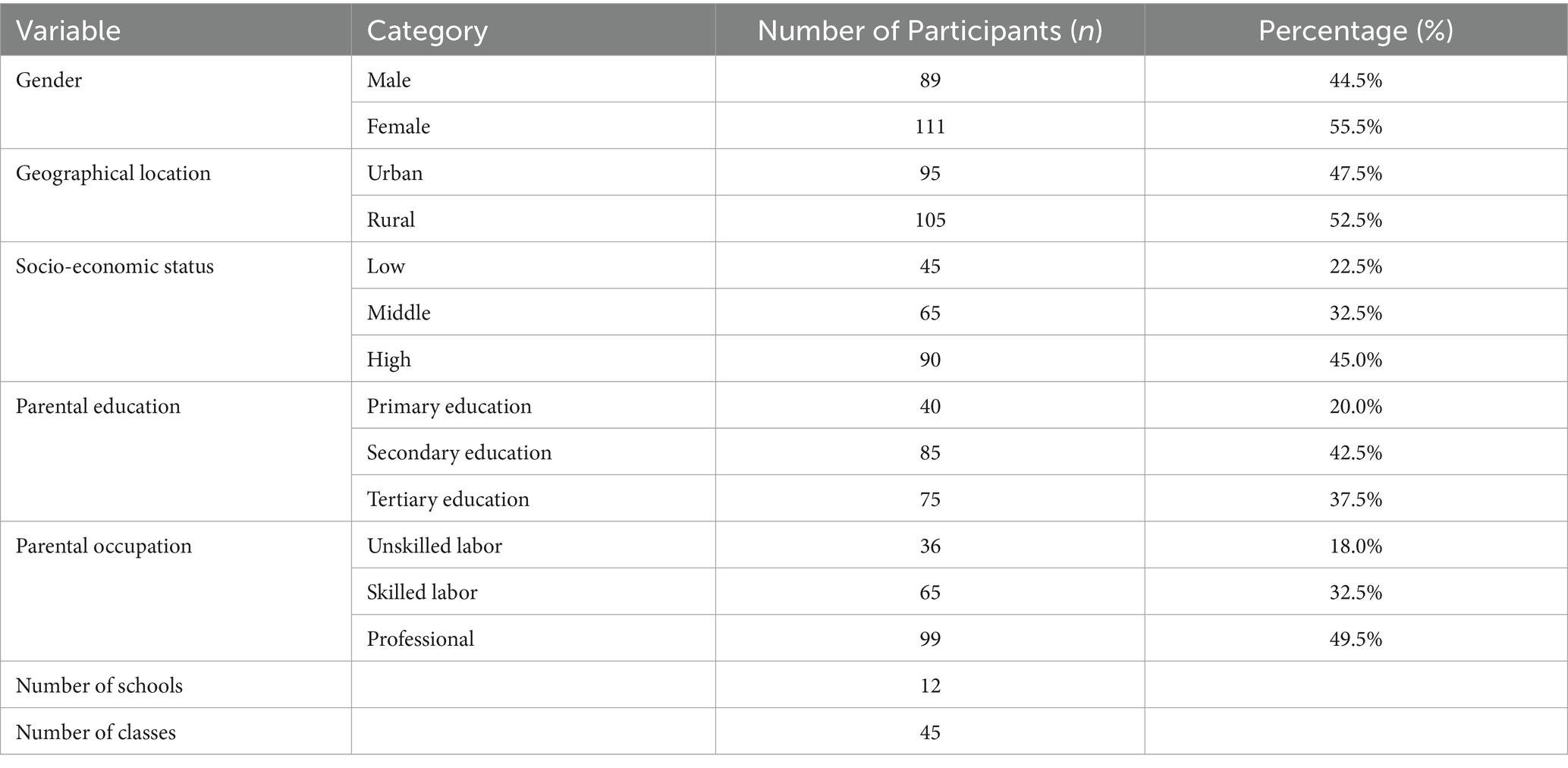
Participants were selected through voluntary sampling, with inclusion criteria that included being aged between 14 and 18 years and attending high schools. Exclusion criteria included the presence of diagnosed eating disorders and participation in previous food education programs in the last year. Participant selection was carried out by considering a sample of 200 adolescent students. The sample comprised boys and girls from various schools across the Lazio Region, including both urban and rural areas, to ensure a diverse representation of socio-economic and cultural backgrounds. Participants were selected from schools in urban centers as well as from more rural settings to capture a broad spectrum of experiences and contexts. Socio-economic status was assessed based on parental education and occupation, household income, and access to resources, with the aim of including students from low, middle, and high socio-economic backgrounds. The selection was made randomly among eligible students, thus ensuring the representativeness of the sample in the study context. To further enhance the diversity and inclusivity of our participant recruitment process, we employed multiple strategies to reach a broader demographic. This included leveraging social media platforms and school newsletters to disseminate information about our study, as well as engaging directly with community organizations that work closely with adolescents. Efforts were made to ensure our recruitment message was culturally sensitive and accessible, using clear, jargon-free language to appeal to both adolescents and their guardians. We hosted informational sessions at participating schools, providing a forum for potential participants and their parents to ask questions and express concerns. These sessions not only served to inform but also to build trust within the community, an essential element in encouraging participation. Our approach aimed at not only fulfilling our recruitment targets but also ensuring a sample that accurately reflects the diversity of dietary habits and health literacy levels among adolescents in the region. Following Table 1 provides a detailed breakdown of the sample’s demographic and socio-economic characteristics. This table includes information on the distribution of participants by gender, geographical location (urban vs. rural), and socio-economic status, as measured by parental education, occupation, and household income. The table provides details on the number of schools and classes involved in the study, highlighting the breadth of the sample across different educational settings.
2.2 The health literacy intervention
The health literacy intervention procedure typically involves several key steps designed to enhance individuals’ understanding and skills regarding health information, particularly in the context of nutrition and healthy eating. Here is a summarized version of a typical procedure:
1. Pre-assessment: The procedure often starts with a pre-assessment phase, where participants’ baseline knowledge and attitudes toward nutrition and healthy eating are evaluated. This could be done through structured questionnaires or interviews to establish a starting point for measuring the intervention’s effectiveness.
2. Design of educational content: Based on the pre-assessment results, educational materials and sessions are tailored to address the specific needs and gaps in knowledge identified. This content usually covers topics such as the basics of a balanced diet, the role of different nutrients in the body, how to read food labels, and strategies for making healthier food choices.
3. Delivery of educational sessions: The core of the intervention involves delivering the designed educational content. This is often done through interactive sessions that could include presentations, workshops, group discussions, and practical activities. These sessions are usually led by health professionals or trained educators who specialize in nutrition and dietetics.
4. Practical activities: To reinforce learning, participants might engage in practical activities such as meal planning exercises, cooking demonstrations, and grocery shopping tours. These activities help participants apply what they have learned in real-life settings.
5. Post-intervention assessment: After the educational sessions, a post-intervention assessment is conducted to evaluate the impact of the health literacy intervention. This involves measuring changes in participants’ knowledge, attitudes, and behaviors related to nutrition and healthy eating. The same tools used in the pre-assessment phase can be employed to facilitate a comparative analysis.
6. Follow-up: Depending on the intervention’s design, a follow-up phase might be included to assess the long-term effectiveness of the program. This could involve additional surveys or interviews conducted several months after the intervention.
7. Analysis and reporting: The final step involves analyzing the data collected during the pre- and post-assessment phases to determine the intervention’s effectiveness. The findings are then reported to stakeholders, which can include participants, school officials, healthcare providers, and the wider community.
This procedure is designed to be flexible and adaptable to different contexts and target populations. The ultimate goal is to empower participants with the knowledge and skills needed to make informed decisions about their dietary habits and overall health.
2.3 The intervention
The health literacy intervention procedure involved several phases. Initially, an initial assessment of the adolescents’ food knowledge and eating self-regulatory skills was conducted through a structured questionnaire. Then, an educational intervention focusing on promoting healthy eating was carried out. This intervention was conducted through health education sessions led by professionals experienced in the field of nutrition. The sessions included information on food composition, planning a balanced diet, and the importance of nutrition for health. Finally, a post-intervention evaluation was conducted to assess the effectiveness of the health literacy intervention on the adolescents’ food knowledge. The intervention consisted of a 6-week health literacy program, with weekly meetings of approximately 1 h each. Each session was structured to cover different aspects of nutrition and healthy eating, including the principles of a balanced diet, the importance of various nutrients, strategies to avoid excessive consumption of processed and high-energy-density foods, and how to read and interpret food labels. Following the post-intervention assessment (3 months after the conclusion of the seminars), a final group feedback session was run to discuss the adolescents’ progress, challenges encountered, and strategies for sustaining their healthy eating habits.
The intervention was run by a team of four experts and involved, respectively, a dietitian creating personalized nutrition plans, a nutritionist offering educational workshops on healthy eating, a health educator developing engaging activities to promote lifestyle changes, and a psychologist supporting students in overcoming barriers to healthy eating. This multidisciplinary approach ensured a comprehensive educational experience, addressing both the nutritional knowledge and emotional aspects of adopting healthier eating habits.
2.4 Educational materials
Educational materials included informational brochures, educational videos, and mobile applications for diet tracking. Students also received food diaries to record their daily diet. A diverse array of formats was utilized to cater to different learning preferences among adolescents. This included interactive, multimedia content on nutrition and health for a hands-on approach to learning about food groups and nutritional values and podcasts featuring discussions with nutrition experts and peers sharing their healthy eating journeys. These materials were designed not only to educate but also to inspire and motivate adolescents by showcasing relatable success stories and practical tips for adopting healthier eating habits. Among the applications recommended for adolescents, the following were presented and utilized: (1) App MyFitnessPal: This app is widely used for tracking nutrition and physical activity. It offers an extensive database of foods, including many products available on the Italian market, allowing users to monitor their caloric intake and nutrient consumption. (2) App Yazio: Another app for diet and exercise tracking, Yazio provides personalized meal plans and challenges to encourage healthy lifestyles. This app is also accessible in Italy and can be an excellent educational tool for adolescents. (3) YouTube Italia Nutrizione: This YouTube channel offers educational videos on various aspects of nutrition in an easily accessible and engaging format for adolescents. (4) Fooducate: Although not specifically Italian, Fooducate is an app that allows users to scan the barcodes of food products to receive detailed information about their nutritional quality, suggestions for healthier alternatives, and much more. It can be used to teach adolescents to make informed food choices.
2.5 Evaluation methods
The evaluation tools used in the study were selected based on the goal of assessing the effect of the health literacy intervention on healthy eating and self-regulatory skills among adolescents. To assess the impact of health literacy interventions, we used the Italian version of the Nutritional Literacy Scale, which measures knowledge and skills related to nutrition (Vettori et al., 2021; Gibbs and Chapman-Novakofski, 2012). The tool was developed to assess nutrition literacy in terms of nutrition knowledge and skills in making food choices. The instrument has six subscales, with 64 items: (1) ‘Nutrition & Health’ which measures reading comprehension of the summarized Dietary Guidelines for Italians; (2) ‘Energy Sources in Food’ which measures knowledge of the macronutrient sources in food; (3) ‘Household Food Measurement’ which measures identification of recommended portions; (4) ‘Food Label and Numeracy’ which measures ability to apply information obtained from the nutrition facts panel; (5) ‘Food Groups’ which measures ability to classify foods by nutrition category, and (6) ‘Consumer Skills’ which measures ability to navigate food products to make healthy food choices. This tool allowed for the collection of quantitative data on the understanding and skills of adolescents in the field of nutrition. In the present study, the coefficient omega ranged from 0.78 to 0.80 for the six subscales.
In addition, an instrument focusing on the emotional compensation aspects of feeding was included in the evaluation protocol, that is, the Emotional Eating Scale (EES, Arnow et al., 1995); It. Valid. Lombardo and San Martini (2005) that includes 25 items assessing the desire to eat after negative emotions, and it is composed of three subscales: emotional eating after depression (EES-D), emotional eating after anxiety/confusion (EES-A), and emotional eating after anger (EES-R). Participants are asked to indicate the extent to which certain feelings lead them to feel an urge to eat (e.g., when they felt depressed, bored, angry, and agitated) on a five-point scale ranging from 1 (“no desire to eat”) to 5 (“an overwhelming urge to eat”). In the present study, the coefficient omega for the EES-D subscale was 0.79, for the EES-A, it was 0.75, and finally for the EES-R, it was 0.78.
Finally, a behavioral questionnaire tailored to Italian dietary patterns, the Tempest Self-Regulation Questionnaire for Eating (TESQ-E) (De Vet et al., 2014; It.valid.: Diotaiuti et al., 2022), has been used to evaluate changes in eating habits and eating self-regulation. The instrument assesses self-regulation and self-control strategies to counteract the desire and temptation to eat unhealthy food and to choose healthy foods. It includes 24 items, which are to be answered using a five-point scale, ranging from 1 (“never”) to 5 (“always”). The instrument is organized into six self-regulation strategies [first-order factors: avoidance of temptations (four items); controlling temptations (four items); distraction (four items); suppression (four items); goal and rule setting (four items); and goal deliberation (four items)] which loaded on three general self-regulation approaches (second-order factors: strategies that directly address temptations; strategies that address the meaning of temptations; and strategies that directly address the objectives) (Stok et al., 2013). In the present study, the coefficient omega for the Addressing directly Temptations (ADT) subscale was 0.82, for the Addressing Psychological Meaning of Temptations (APM), it was 0.81, and finally for the Addressing Goals (AG) subscale, it was 0.83.
Students were encouraged to use the digital food tracking app, MyFitnessPal, to track daily food intake, including details on macro- and micronutrients, allowing users to easily record meals consumed and physical activities performed, helping them better understand their daily caloric balance (calories consumed vs. calories burned). Health parameters were also collected before the intervention, at its conclusion, and after 3 months. These included body weight and height to calculate participants’ body mass index (BMI).
2.6 Statistical analysis
To analyze the results of the intervention study on food literacy among adolescents, the following statistical analyses were conducted using the statistical software SPSS v. 26:
1. Descriptive analysis: to provide a summary of the sample characteristics, including age, gender, initial BMI, and levels of food knowledge. This includes calculations of means, standard deviations, frequencies, and percentages.
2. Paired Student’s t-test: used to compare pre- and post-intervention scores on continuous variables (such as food knowledge and BMI) to assess whether there have been significant improvements due to the intervention.
3. Repeated measures analysis of variance (ANOVA): to examine differences in pre-intervention, post-intervention, and follow-up scores among study groups, if applicable. This can help to identify whether changes remain significant over time. Friedman’s non-parametric test was used if data dо not follow a normal distribution.
4. Correlation analysis: to explore relationships between variables, such as the relationship between food knowledge levels and changes in BMI, or between self-regulation strategies and the reduction of emotional eating.
5. Multiple logistic or linear regressions: to assess the impact of multiple variables (such as age, gender, and initial level of food knowledge) on the outcomes of the intervention (e.g., BMI improvement or changes in eating habits).
6. Wilcoxon rank sum analysis: a non-parametric test used if the data dо not follow a normal distribution, to compare median scores pre- and post-intervention on variables such as food knowledge or emotional eating.
3 Results
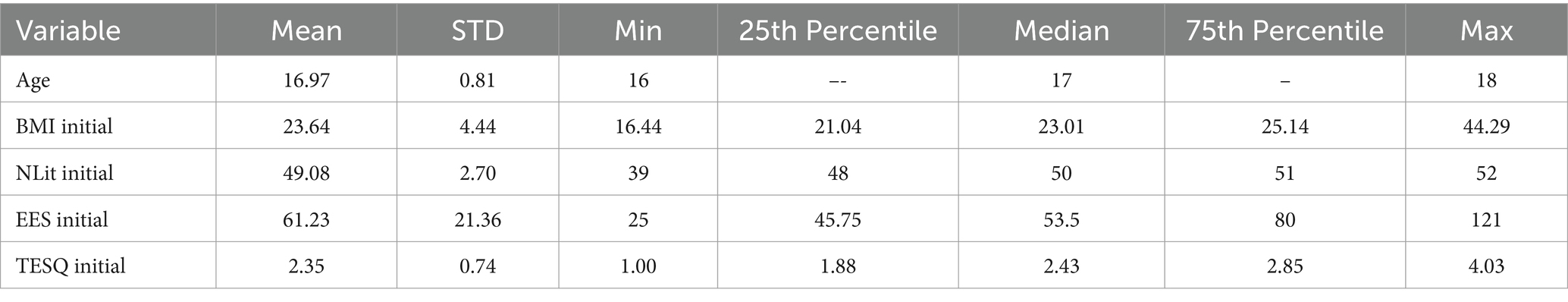
As reported in Table 2, the mean age of participants was approximately 17 years, with a small standard deviation, indicating a relatively homogenous group in terms of age. The initial BMI had a mean of 23.64 with a wider standard deviation, suggesting variability in participants’ body mass index. The Nutritional Literacy (NLit) and Emotional Eating Scale (EES) scores also varied, indicating diverse levels of nutritional knowledge and emotional eating behaviors among participants. The TESQ scores, which measure self-regulation in eating, had a mean of 2.35, with a standard deviation indicating some variability in participants’ ability to regulate their eating behavior.
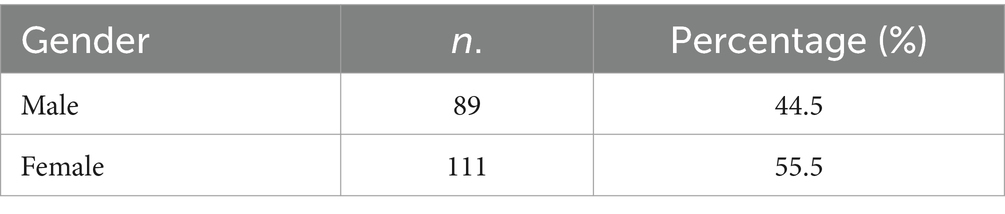
According to Table 3, there were 89 male participants, constituting 44.5% of the sample, and 111 female participants, making up 55.5% of the sample. This distribution shows a slightly higher representation of female participants in the study.
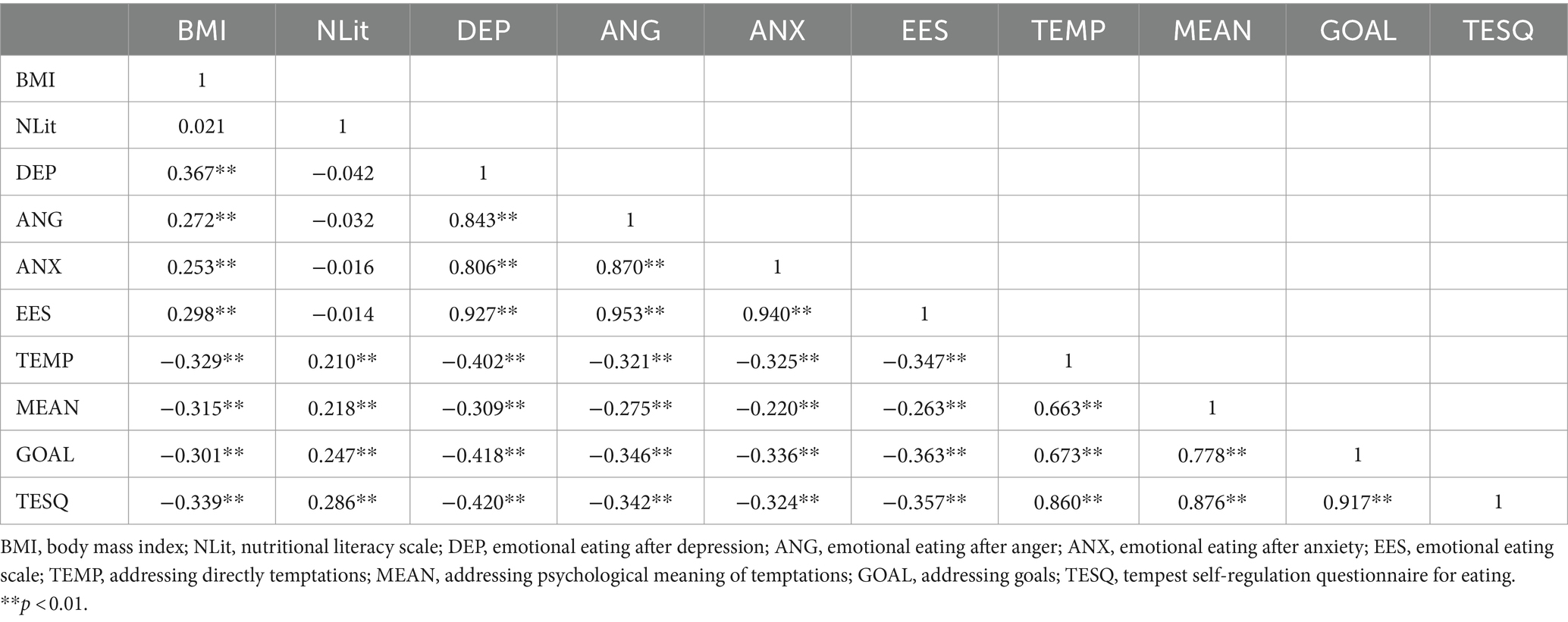
Table 4 presents Spearman’s bivariate correlations for several variables, including body mass index (BMI), Nutritional Literacy (NLit), Emotional Eating after Depression (DEP), Emotional Eating after Anger (ANG), Emotional Eating after Anxiety (ANX), Emotional Eating Scale (EES), and several self-regulation strategies as measured by the Tempest Self-Regulation Questionnaire for Eating (TESQ) among others. The table provides correlation coefficients that measure the strength and direction of association between pairs of these variables, with **p < 0.01 indicating statistically significant correlations. Key findings from Table 3 include the following:
Significant positive correlations among emotional eating measures (DEP, ANG, ANX, and EES) indicate that higher levels of emotional eating in one category (e.g., depression) are associated with higher levels of emotional eating in other categories (e.g., anger and anxiety).
Negative correlations between Emotional Eating Measures and Self-Regulation Strategies (TEMP, MEAN, and GOAL) suggest that individuals who report higher use of self-regulation strategies to manage their eating behavior tend to report lower levels of emotional eating. This highlights the potential protective role of self-regulation skills against emotional eating behaviors.
BMI’s correlation with Emotional Eating and Self-Regulation Strategies is notable. BMI shows a positive correlation with emotional eating measures, indicating that higher BMI values are associated with higher levels of emotional eating. Conversely, BMI is negatively correlated with self-regulation strategies, suggesting that individuals with higher BMIs may utilize fewer self-regulation strategies in their eating behaviors, or that effective use of such strategies could be associated with lower BMI.
Nutritional Literacy (NLit) shows very low or insignificant correlations with most other variables, indicating that nutritional knowledge alone may not be strongly associated with emotional eating behaviors or the use of specific self-regulation strategies. This suggests that while knowledge is important, it might not directly influence these behaviors without the support of practical skills or interventions designed to change behaviors.
As reported in Table 5, the mean BMI at baseline was 23.64, with a slight decrease post-intervention (M = 23.45) and at follow-up (M = 23.04). There was a noticeable increase in mean nutrition literacy from baseline (M = 49.08) to post-intervention (M = 56.06) and slightly decreasing at follow-up (M = 54.42), indicating an improvement after the intervention. The mean EES score decreased from baseline (M = 61.23) to post-intervention (M = 59.26) and further at follow-up (M = 57.92), suggesting a reduction in emotional eating. The self-regulation questionnaire scores showed an increasing trend from baseline (M = 2.35) to post-intervention (M = 2.62) and follow-up (M = 2.75), indicating improved self-regulation skills over time.
The Shapiro–Wilk test results for normality indicated that the distributions of BMI, NLit, EES, and TESQ at baseline were not normally distributed (p-values <0.05), which suggests that non-parametric tests should be used for further analyses.
Given that the data dо not follow a normal distribution for most variables, we used the Wilcoxon test (a non-parametric alternative to the t-test) to compare pre- and post-intervention scores, which indicated significant changes for some variables.
The Wilcoxon signed-rank tests comparing baseline versus post-intervention and baseline versus follow-up measurements for body mass index (BMI), Nutrition Literacy (NLit), Emotional Eating Scale (EES), and Tempest Self-Regulation Questionnaire for Eating (TESQ) yielded the following p-values:
• BMI Changes. Baseline vs. Post-intervention: p-value <0.001; Baseline vs. Follow-up: p-value <0.001. The significant change in BMI indicates that the intervention had a marked effect on reducing BMI from pre-intervention values to post-intervention values. This suggests success in achieving the goal of improving body weight or body composition of the individuals involved.
• Nutrition Literacy (NLit) Changes. Baseline vs. Post-intervention: p-value <0.001; Baseline vs. Follow-up: p-value <0.001. An extremely low p-value indicates that there was significant growth in food knowledge following the intervention. This implies that the intervention was very effective in improving the understanding of nutritional topics among the participants.
• Emotional Eating Scale (EES) Changes. Baseline vs. Post-intervention: p-value = 0.71; Baseline vs. Follow-up: p-value = 0.34. The p-value does not indicate significant changes in emotional eating pre- and post-intervention. This suggests that, despite the intervention, there were no significant variations in emotional eating behaviors among the participants.
• Changes in the Tempest Self-Regulation Questionnaire for Eating (TESQ). Baseline vs. Post-intervention: p-value <0.001; Baseline vs. Follow-up: p-value <0.001. The p-value indicated significant improvements in individuals’ self-regulation skills regarding their eating behavior following the intervention.
These results suggested that the intervention significantly impacted BMI, Nutrition Literacy, and self-regulation skills (as measured by TESQ), with improvements evident both immediately post-intervention and at follow-up. However, changes in Emotional Eating (as measured by EES) were not statistically significant, indicating that the intervention may not have had a clear impact on emotional eating behaviors.
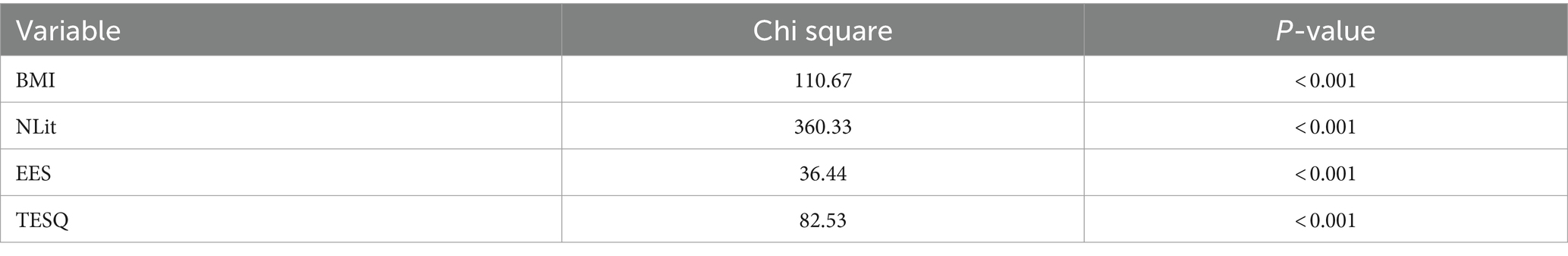
The Friedman test results clearly show that there were significant differences between the scores of all the considered variables (BMI, NLit, EES, and TESQ) at the three measurement times (pre-intervention, post-intervention, and follow-up) (see Table 6). This demonstrates the lasting impact of the intervention beyond the period immediately following its conclusion. For BMI and NLit, not only the immediate impact was confirmed but also the persistence over time of this effect on body mass index and nutritional knowledge. For EES, although there were no significant changes in the pre- and post-analysis, the Friedman test indicated that, considering the follow-up, there were significant changes over time (p-value <0.001). For TESQ, similarly, it was confirmed that the intervention had a substantial and lasting effect on improving food self-regulation skills.
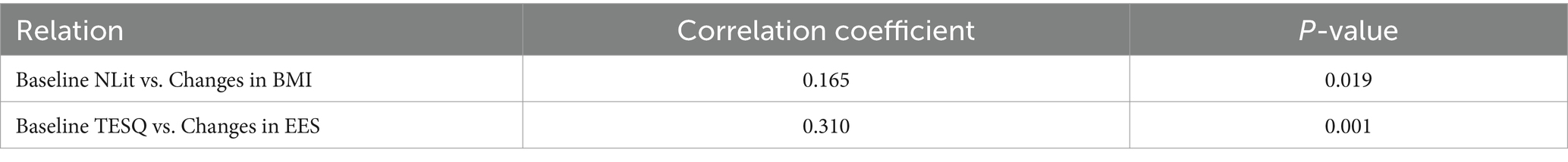
Table 7 provides correlation coefficients along with p-values, highlighting the strength and significance of the relationships between the variables.
Baseline NLit vs. Changes in BMI: The correlation coefficient of 0.165 with a p-value of 0.019 suggests a statistically significant, albeit weak, positive relationship between initial nutritional literacy levels and changes in BMI. This indicates that higher baseline levels of nutritional literacy might be associated with greater changes in BMI, suggesting that a better understanding of nutrition could positively influence BMI outcomes to some extent.
Baseline TESQ vs. Changes in EES: A stronger correlation coefficient of 0.310 with a p-value of 0.001 demonstrates a statistically significant, moderate relationship between initial self-regulation skills (as measured by TESQ) and changes in emotional eating (as measured by EES). This suggests that individuals who initially report better self-regulation in eating are more likely to experience significant changes in their emotional eating behaviors. This could imply that enhancing self-regulation skills may be an effective strategy in addressing emotional eating.
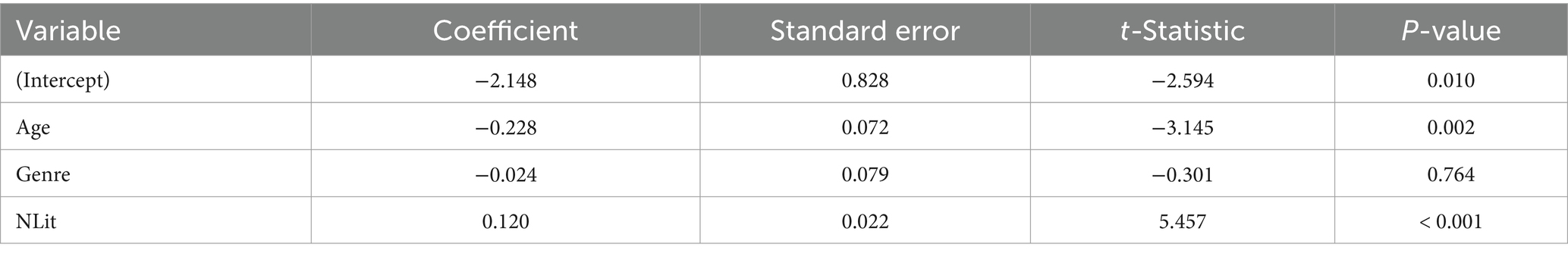
The regression analysis in Table 8 highlights the nuanced dynamics between demographic factors, nutritional literacy, and their collective impact on BMI changes. The significance of nutritional literacy underscores the value of targeted nutritional education in influencing positive health outcomes. The lack of a significant gender effect suggests that, in this sample, gender does not have a meaningful impact on the intervention’s effectiveness regarding BMI changes. The coefficient for age is −0.228 with a statistically significant p-value of 0.002. This suggests that age negatively affects BMI changes, implying that older adolescents might experience smaller changes in BMI compared to younger ones. This could be due to various factors, including differences in metabolic rates, lifestyle choices, or responsiveness to the intervention based on age. The initial level of nutritional literacy has a coefficient of 0.120 with a p-value of less than 0.001, indicating a positive and statistically significant impact on BMI changes. This implies that higher initial nutritional literacy is associated with greater changes in BMI, reinforcing the importance of nutritional education as part of interventions aimed at BMI management.
4 Discussion
The food literacy intervention carried out has demonstrated the importance of combining different strategies to promote healthy nutrition among adolescents. Going deeper into the results, it is possible to better understand how these strategies have contributed to improving food knowledge, eating habits, self-regulation, and the overall health of adolescents.
The increase in food knowledge among adolescents is a key outcome of the intervention. By educating students on the principles of a balanced diet, the importance of various nutrients, and how to read and interpret food labels, the intervention has provided them with the necessary tools to make informed food choices. This aspect is fundamental as the ability to understand and apply nutritional information is an essential first step toward adopting healthy eating habits.
The evident result of the increase in food knowledge among the participating adolescents is not only an indicator of the success of the educational intervention but also a critical foundation for the adoption of informed food choices. In-depth knowledge about nutrients, the caloric values of foods, and the composition of healthy meals is essential to combat improper eating habits that can lead to long-term health problems, such as obesity and diseases related to diet (Lee et al., 2022; Liu et al., 2022).
The intervention highlighted how self-regulation practices can positively influence adolescents’ eating habits. Strategies such as avoiding temptations, setting dietary goals and rules, and reflecting on personal goals can help resist the temptations of unhealthy foods and prefer more nutritious options. This approach proved effective in promoting an increase in fruit and vegetable consumption and a reduction in the intake of fast food and processed snacks. The improvement in self-regulation in eating habits testifies to the effectiveness of the intervention in promoting effective coping strategies in the face of temptations of unhealthy foods and in portion management. Self-regulation skill is crucial for maintaining a balanced diet and managing body weight, especially in an era where adolescents are constantly exposed to unhealthy food stimuli through media and social environment (Diotaiuti et al. (2021a); Guzek et al., 2022; Guo et al., 2023).
The adoption of apps for tracking food and physical activity, such as MyFitnessPal, provided adolescents with a practical and interactive method to monitor their diet and caloric balance. This not only increased their awareness of their eating habits but also facilitated the management and optimization of nutrient and calorie intake. The use of digital technologies in food education offers significant potential to improve engagement and learning among adolescents (König et al., 2021).
The positive effect of the intervention on adolescents’ BMI underscores the importance of food literacy for overall health. An improved BMI reflects not just a better body composition but also a reduced risk of developing health problems related to diet, such as obesity and metabolic diseases. These results confirm that well-structured educational interventions can have a significant impact on the long-term health of adolescents (Reid et al., 2021; Taleb and Itani, 2021).
The improvement in body mass index (BMI) signals a direct positive impact of the intervention on the physical health of adolescents. BMI is a key indicator of health status and the risk of developing chronic diseases associated with overweight and obesity. An improvement in this parameter reflects not only a reduction in the intake of high-energy-density foods but also an increase in physical activity, highlighting the importance of a holistic approach to health that integrates nutrition and exercise (Koca and Arkan, 2020; Ruiz et al., 2021).
The interpretation of the results obtained from the food literacy intervention conducted on adolescents reveals a series of significant considerations that warrant detailed exploration to fully understand their impact and implications. These results lay the groundwork for further investigations and implementations in the field of food education and health promotion among adolescents. It is crucial to recognize that food literacy is not limited to the mere acquisition of knowledge but also includes the development of practical competence, such as reading food labels, preparing healthy meals, and effectively managing food resources (Ares et al., 2023; Li et al., 2022).
The study also indicated that there was no statistically significant change in Emotional Eating Scale (EES) scores following the eating literacy intervention among adolescents, suggesting that the intervention did not significantly alter emotional eating behaviors, which are often triggered by negative emotions such as anxiety, anger, or depression. Emotional eating, the act of consuming food in response to emotional rather than physical hunger, can lead to unhealthy eating patterns and potentially contribute to weight gain or the development of eating disorders (Erdem et al., 2023; Joseph et al., 2023; Xiang et al., 2023; Limbers and Summers, 2021).
The lack of significant change in emotional eating behaviors post-intervention highlights the complexity of addressing such behaviors through eating literacy programs alone. It underscores the necessity of integrating more targeted psychological or behavioral strategies within food literacy interventions to effectively manage emotional triggers for eating. This outcome emphasizes the importance of a multifaceted approach to food literacy interventions that not only educates adolescents about nutritional knowledge and self-regulation skills but also addresses the emotional aspects of eating (Bektas and Gürkan, 2023; Francis et al., 2023; Aloudah, 2021; Diotaiuti et al., 2020).
By incorporating strategies to better manage emotional responses that lead to eating, such interventions can contribute to more balanced eating behaviors and improve overall mental and physical health among adolescents. Future research should explore the incorporation of emotional regulation techniques and psychological support within eating literacy programs to enhance their effectiveness in reducing emotional eating among adolescents (Bui et al., 2021; Diotaiuti et al. (2021b); Woods-Townsend et al., 2021; Shriver et al., 2020).
The comparison of the results of the food literacy intervention among adolescents with those of previous studies highlights some interesting aspects and confirms the growing evidence on the effectiveness of educational interventions in promoting healthy eating habits in this critical age group.
Previous studies have already highlighted the importance of food education among adolescents, showing how targeted interventions can improve nutritional knowledge and positively influence food choices. For example, the effectiveness of school nutritional education programs in improving understanding and adoption of healthier diets has been documented in various research (Heikkilä et al., 2021; Noronha et al., 2020; Asakura et al., 2017; Egg et al., 2020). These programs, similar to the described intervention, have utilized multi-component educational approaches to influence both the knowledge and behavior of students.
A distinctive aspect of the intervention under examination is the intensive use of digital tools, such as the MyFitnessPal app, to promote self-regulation and the tracking of food intake and physical activity. This approach aligns with the research by Kloss and Bittlingmayer (2017), which emphasized the importance of eHealth literacy in promoting healthy eating behaviors among adolescents. The inclusion of digital technologies represents a relatively new feature in the field of food education and reflects the adaptation of interventions to the habits and preferences of modern adolescents.
The impact of the intervention on the BMI of adolescents echoes the findings of studies such as those reported by Jacob et al. (2021), which demonstrated how school-based interventions can have positive effects not only on knowledge and behavior but also on physical health measures such as BMI. This reinforces the idea that well-designed and well-executed interventions can have tangible beneficial effects on the physical health of adolescents.
However, it is important to note that, while the described intervention and similar studies show promising results, the literature also indicates the need for long-term interventions and follow-ups to maintain behavioral changes (Bailey et al., 2019; Diotaiuti et al. (2021c); Forray et al., 2021; Larose et al., 2023). Many studies underline the importance of continuous support, education, and environment to sustain healthy eating habits over time (Chaudhary et al., 2020; Medeiros et al., 2022; Nagy-Pénzes et al., 2022).
Our study highlights the importance of self-regulation in improving dietary behaviors among adolescents. However, we recognize the need to directly measure practical skills in future research. Practical skills, such as cooking and food preparation, are critical components of food literacy that were addressed in our intervention but not formally assessed. Future studies should incorporate these measures to provide a more comprehensive evaluation of food literacy interventions.
4.1 Limitations of the study
The limitations of a study are crucial for understanding the context in which the results can be interpreted and for guiding the direction of future research. Examining the food literacy intervention among adolescents, we can identify several limitations that deserve attention:
1. Study sample and generalizability: The sample might have been limited in size, geographical, or socio-economic diversity, which could affect the generalizability of the results. If the study was conducted in a specific area or with a homogeneous group of students, the results might not be applicable to other populations with different cultural, economic, or educational contexts.
2. Lack of a control group: The absence of a control group limits the ability to definitively attribute observed changes to the intervention alone. Future studies should incorporate a control group to strengthen the causal inferences regarding the effectiveness of health literacy interventions.
3. Duration of the intervention and follow-up: The duration of the intervention and the follow-up period might not have been long enough to assess the long-term effects on adopting healthy eating habits and maintaining changes in behavior and food knowledge. Long-term interventions and extended follow-ups are crucial for understanding the sustainability of behavioral changes.
4. Dependence on self-reporting: If the study relied on self-reported data from adolescents to track food intake, physical activity, or other behaviors, this could introduce a social desirability bias or inaccuracies due to faulty memory. These factors can lead to an overestimation or underestimation of behavioral changes.
5. Control of confounding variables: There might have been limitations in the ability to control all confounding variables that affect the eating habits and health of adolescents, such as peer influence, family support, access to healthy foods, and the school environment. The presence of these uncontrolled variables can obscure the interpretation of the results.
6. Measurement of outcomes: The metrics used to assess the outcomes of the intervention might not cover all relevant aspects of food literacy or eating behavior. For example, focusing on specific indicators such as BMI or fruit and vegetable intake might neglect other important dietary or lifestyle aspects.
7. Technology-based intervention: The use of digital tools, although innovative and engaging, might limit the participation of individuals with limited access to technology or less developed digital skills. This could create a disparity in the ability to benefit from the intervention.
Recognizing these limitations is fundamental not only for cautiously interpreting the study’s results but also for guiding the development of future food literacy interventions. Identifying these areas for improvement can contribute to designing more robust, inclusive, and representative studies that can provide more solid and generalizable evidence on the most effective strategies for promoting healthy eating habits among adolescents.
5 Implications for clinical practice and future research
The food literacy intervention among adolescents, despite its limitations, offers significant implications for both clinical practice and future research. These insights can guide the evolution of health education programs and inform the direction of subsequent investigations.
5.1 For clinical practice
1. Customization of interventions: the importance of tailoring food literacy interventions to the specific needs of different groups of adolescents, considering factors such as age, socio-economic context, culture, and technological predisposition. This can enhance the effectiveness of interventions and the adoption of healthy eating habits.
2. Integration of technology: clinical practice can benefit from integrating digital tools and apps for tracking nutrition and physical activity, encouraging adolescents to become more aware of their habits and to better manage their health.
3. Education of parents and caregivers: emphasizing the role of parents and caregivers in influencing adolescents’ eating habits, and promoting programs that also involve families in food education and health promotion.
4. Interdisciplinary collaboration: encouraging collaboration among health professionals, educators, and communities to develop and implement holistic, sustainable, and accessible food literacy programs for all adolescents.
5.2 For future research
1. Study of long-term interventions: conducting research on longer-duration interventions with extended follow-ups to assess the long-term impact on food literacy, eating habits, and health indicators.
2. Exploration of diversity and inclusivity: expanding research to include a greater diversity of participants, considering geographical, economic, and cultural variations, to improve the generalizability of the results.
3. Evaluation of new outcome metrics: developing and using assessment tools that capture a wide range of outcomes related to food literacy, including behavioral, psychological, and social changes, as well as physical health indicators.
4. Analysis of the impact of confounding variables: deepening the understanding of how factors such as peer influence, family and school environment, and access to healthy foods affect the effectiveness of food literacy interventions.
5. Use and impact of technology: further investigating the effect of digital tools on food education, exploring how different platforms and formats can be used to maximize engagement and learning among adolescents.
6. Future research should include a control group to provide a more robust evaluation of the intervention’s impact and enhance the generalizability of the findings.
Adopting a holistic, personalized, and collaborative approach can significantly improve the effectiveness of food literacy interventions, with the potential to positively impact public health in the long term.
6 Conclusion
The insights derived from this study emphasize the need for multidisciplinary approaches and the use of digital technologies in food education for adolescents. A well-designed program that combines theory with practical activities and the use of digital tools can significantly improve food knowledge, eating habits, and the overall health of adolescents. The importance of these findings lies in their applicability to future health education programs, indicating ways to further enhance the effectiveness of food literacy interventions.
The intervention has demonstrated that food education and literacy can have a significant impact on adolescents’ eating habits, improving their overall health and long-term wellbeing. These results highlight the importance of well-structured food education programs that are capable of addressing the specific needs of this age group and promoting positive change in eating behavior. It is crucial to continue investing in research and development in this field to expand our understanding and optimize intervention strategies, in order to ensure a healthier future for younger generations.
In conclusion, our intervention is situated within a well-established research context that supports the effectiveness of food education and nutritional literacy among adolescents. The addition of digital elements and focus on self-regulation strategies represent significant evolutions in intervention design, offering new directions for future research and educational practice. The convergence between the results of the intervention and those of previous studies strengthens the argument for continuous and innovative investments in food education and health promotion among adolescents.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Institutional Review Board of the University of Cassino and Southern Lazio. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
SM: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. SC: Data curation, Investigation, Writing – review & editing. BT: Data curation, Investigation, Writing – review & editing. GS: Data curation, Investigation, Writing – review & editing. FDS: Writing – review & editing. FM: Supervision, Writing – review & editing. PD: Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the publication of this article. Project ECS 0000024 “Ecosistema dell’innovazione—Rome Technopole” financed by EU in NextGenerationEU plan through MUR Decree n. 1051 23.06.2022 PNRR Missione 4 Componente 2 Investimento 1.5— CUP H33C22000420001.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Agam-Bitton, R., Ahmad, W., and Golan, M. (2018). Girls-only vs. mixed-gender groups in the delivery of a universal wellness programme among adolescents: a cluster-randomized controlled trial. PLoS One 13:e0198872. doi: 10.1371/journal.pone.0198872
Aloudah, M. A. (2021). Exploring Saudi adolescents’ perceptions of emotional eating with the purpose of informing the Design of an Online Health Awareness Programme (Doctoral dissertation. London, UK: University of Reading). Available at: http://centaur.reading.ac.uk/101352 (Accessed September 6, 2024).
Ares, G., De Rosso, S., Mueller, C., Philippe, K., Pickard, A., Nicklaus, S., et al. (2023). Development of food literacy in children and adolescents: implications for the design of strategies to promote healthier and more sustainable diets. Nutr. Rev. 82, 536–552. doi: 10.1093/nutrit/nuad072
Arnow, B., Kenardy, J., and Agras, W. S. (1995). The emotional eating scale: the development of a measure to assess coping with negative affect by eating. Int. J. Eat. Disord. 18, 79–90. doi: 10.1002/1098-108x(199507)18:1<79::aid-eat2260180109>3.0.co;2-v
Asakura, K., Todoriki, H., and Sasaki, S. (2017). Relationship between nutrition knowledge and dietary intake among primary school children in Japan: combined effect of children’s and their guardians’ knowledge. J. Epidemiol. 27, 483–491. doi: 10.1016/j.je.2016.09.014
Awofeso, N., Zarooni, A., Rabih, Z., and Bamidele, M. (2017). Health literacy measurements with the newest vital sign instrument among adolescents from Dubai, United Arab Emirates. Turkish J. of Family Med. Primary Care. 11, 164–170. doi: 10.21763/tjfmpc.336147
Bailey, C. J., Drummond, M., and Ward, P. (2019). Food literacy programmes in secondary schools: a systematic literature review and narrative synthesis of quantitative and qualitative evidence. Public Health Nutr. 22, 2891–2913. doi: 10.1017/s1368980019001666
Bandura, A. (1986). The explanatory and predictive scope of self-efficacy theory. J. Soc. Clin. Psychol. 4, 359–373. doi: 10.1521/jscp.1986.4.3.359
Bektas, İ., and Gürkan, K. P. (2023). Investigation of the relationships between mindfulness, emotional eating, weight control self-efficacy, and obesity in adolescents. J. Pediatr. Nurs. 73, e381–e387. doi: 10.1016/j.pedn.2023.10.004
Bektaş, İ., Kudubeş, A., Ayar, D., and Bektaş, M. (2021). Predicting the healthy lifestyle behaviors of turkish adolescents based on their health literacy and self-efficacy levels. J. Pediatr. Nurs. 59, e20–e25. doi: 10.1016/j.pedn.2021.01.016
Bereznay, M., Kopp, C., Nyakwol, A., and Howe, C. (2019). Promoting food literacy in teens. J. Pediatr. Nurs. 47, 171–172. doi: 10.1016/j.pedn.2019.04.003
Bui, C., Lin, L. Y., Wu, C. Y., Chiu, Y. W., and Chiou, H. Y. (2021). Association between emotional eating and frequency of unhealthy food consumption among Taiwanese adolescents. Nutrients 13:2739. doi: 10.3390/nu13082739
Cavicchiolo, E., Sibilio, M., Lucidi, F., Cozzolino, M., Chirico, A., Girelli, L., et al. (2022). The psychometric properties of the behavioural regulation in exercise questionnaire (BREQ-3): factorial structure, invariance and validity in the Italian context. Int. J. Environ. Res. Public Health 19:1937. doi: 10.3390/ijerph19041937
Champion, K., Hunter, E., Gardner, L., Thornton, L., Chapman, C., McCann, K., et al. (2023). Parental information needs and intervention preferences for preventing multiple lifestyle risk behaviors among adolescents: cross-sectional survey among parents. JMIR Pediatrics Parenting 6:e42272. doi: 10.2196/42272
Chaudhary, A., Sudzina, F., and Mikkelsen, B. E. (2020). Promoting healthy eating among young people—a review of the evidence of the impact of school-based interventions. Nutrients 12:2894. doi: 10.3390/nu12092894
De Vet, E., De Ridder, D., Stok, M., Brunso, K., Baban, A., and Gaspar, T. (2014). Assessing self-regulation strategies: development and validation of the tempest self-regulation questionnaire for eating (TESQ-E) in adolescents. Int. J. Behav. Nutr. Phys. Act. 11, 106–115. doi: 10.1186/s12966-014-0106-z
Deci, E. L., and Ryan, R. M. (1985). The general causality orientations scale: self-determination in personality. J. Res. Pers. 19, 109–134. doi: 10.1016/0092-6566(85)90023-6
Depboylu, G. (2023). Nutrition literacy status and its association with adherence to the mediterranean diet, anthropometric parameters and lifestyle behaviours among early adolescents. Public Health Nutr. 26, 2108–2117. doi: 10.1017/s1368980023001830
Diotaiuti, P., Girelli, L., Mancone, S., Valente, G., Bellizzi, F., Misiti, F., et al. (2022). Psychometric properties and measurement invariance across gender of the Italian version of the tempest self-regulation questionnaire for eating adapted for young adults. Front. Psychol. 13:941784. doi: 10.3389/fpsyg.2022.941784
Diotaiuti, P., Valente, G., Mancone, S., and Grambone, A. (2020). Psychometric properties and a preliminary validation study of the Italian brief version of the communication styles inventory (CSI-B/I). Front. Psychol. 11:1421. doi: 10.3389/fpsyg.2020.01421
Diotaiuti, P., Corrado, S., Mancone, S., and Falese, L. (2021a). Resilience in the endurance runner: The role of self-regulatory modes and basic psychological needs). Front. Psychol. 11:558287. doi: 10.3389/fpsyg.2020.558287
Diotaiuti, P., Valente, G., Mancone, S., Grambone, A., and Chirico, A. (2021b). Metric goodness and measurement invariance of the italian brief version of interpersonal reactivity index: A study with young adults. Front. Psychol. 12:773363. doi: 10.3389/fpsyg.2021.773363
Diotaiuti, P., Valente, G., and Mancone, S. (2021c). Validation study of the Italian version of Temporal Focus Scale: psychometric properties and convergent validity. BMC Psychol. 9:1–13. doi: 10.1186/s40359-020-00510-5
Egg, S., Wakolbinger, M., Reisser, A., Schätzer, M., Wild, B., and Rust, P. (2020). Relationship between nutrition knowledge, education and other determinants of food intake and lifestyle habits among adolescents from urban and rural secondary schools in Tyrol, western Austria. Public Health Nutr. 23, 3136–3147. doi: 10.1017/s1368980020000488
Erdem, E., Efe, Y. S., and Özbey, H. (2023). A predictor of emotional eating in adolescents: social anxiety. Arch. Psychiatr. Nurs. 43, 71–75. doi: 10.1016/j.apnu.2022.12.016
Forray, A. I., Gologan, A., Coman, M. A., Cherecheş, R., Petreuş, D., Vizitiu, S., et al. (2021). A pilot study to examine the effects of a school-based intervention for promoting food and nutrition literacy (fnlit) in romanian school children. Acta Medica Transilvanica 26, 12–17. doi: 10.2478/amtsb-2021-0041
Francis, L. A., Rollins, B. Y., and Lozinski, R. H. (2023). Measuring adolescents’ eating in the absence of hunger in the home environment using subjective and objective measures. Appetite 180:106354. doi: 10.1016/j.appet.2022.106354
Gibbs, H. D., and Chapman-Novakofski, K. (2012). Establishing content validity for the nutrition literacy assessment instrument. J. Acad. Nutr. Diet. 112:A23. doi: 10.5888/pcd10.120267
Grover, K., and Choudhary, M. (2017). Effectiveness of long term community based nutrition intervention for prevention and management of anaemia among adolescent girls. Asian J. Dairy Food Res. 36, 235–240. doi: 10.18805/ajdfr.v36i03.8961
Guo, S., Davis, E., Yu, X., Naccarella, L., Armstrong, R., Abel, T., et al. (2018). Measuring functional, interactive and critical health literacy of chinese secondary school students: reliable, valid and feasible? Glob. Health Promot. 25, 6–14. doi: 10.1177/1757975918764109
Guo, H., Huang, R., and Lu, X. (2023). The relationship between eating disorders and self-regulation among adolescent. J. Educ. Human. Soci. Sci. 8, 1906–1912. doi: 10.54097/ehss.v8i.4611
Guo, S., Yu, X., Davis, E., Armstrong, R., Riggs, E., and Naccarella, L. (2020). Adolescent health literacy in Beijing and Melbourne: a cross-cultural comparison. Int. J. Environ. Res. Public Health 17:1242. doi: 10.3390/ijerph17041242
Guzek, D., Skolmowska, D., and Głąbska, D. (2022). Analysis of self-regulation of eating behaviors within polish adolescents’ COVID-19 experience (PLACE-19) study. Nutrients 14:1679. doi: 10.3390/nu14081679
Heikkilä, L., Korpelainen, R., Aira, T., Alanko, L., Heinonen, O. J., Kokko, S., et al. (2021). The associations between adolescents’ sports club participation and dietary habits. Trans. Sports Med. 4, 617–626. doi: 10.1002/tsm2.249
Jacob, C. M., Hardy-Johnson, P. L., Inskip, H. M., Morris, T., Parsons, C. M., Barrett, M., et al. (2021). A systematic review and meta-analysis of school-based interventions with health education to reduce body mass index in adolescents aged 10 to 19 years. Int. J. Behav. Nutr. Phys. Act. 18, 1–22. doi: 10.1186/s12966-020-01065-9
Joseph, P. L., Gonçalves, C., and Fleary, S. A. (2023). Psychosocial correlates in patterns of adolescent emotional eating and dietary consumption. PLoS One 18:e0285446. doi: 10.1371/journal.pone.0285446
Kim, J., and Lim, H. (2019). Nutritional management in childhood obesity. J. Obesity Metabolic Syndrome 28, 225–235. doi: 10.7570/jomes.2019.28.4.225
Kloss, I., and Bittlingmayer, U. H. B. (2017). The effect of ehealth literacy interventions for adolescents-results of a systematic research: Inga Kloss. Eur. J. Public Health 27:ckx186-305. doi: 10.1093/eurpub/ckx186.305
Koca, B., and Arkan, G. (2020). The relationship between adolescents’ nutrition literacy and food habits, and affecting factors. Public Health Nutr. 24, 717–728. doi: 10.1017/s1368980020001494
König, L. M., Attig, C., Franke, T., and Renner, B. (2021). Barriers to and facilitators for using nutrition apps: systematic review and conceptual framework. JMIR Mhealth Uhealth 9:e20037. doi: 10.2196/20037
Labbé, C., Ward, S., Dupuis, J., and Johnson, C. (2023). Effectiveness of a school-based culinary programme on 9-and 10-year-old children’s food literacy and vegetable, fruit, and breakfast consumption. Nutrients 15:1520. doi: 10.3390/nu15061520
Larose, D., Chen, M. C., Panahi, S., Yessis, J., Tremblay, A., and Drapeau, V. (2023). Interventions to promote healthy lifestyle behaviors in children and adolescents in summer day camps: a scoping review. BMC Public Health 23:773. doi: 10.1186/s12889-023-15521-1
Lee, Y., Kim, T., and Jung, H. (2022). The relationships between food literacy, health promotion literacy and healthy eating habits among young adults in South Korea. Food Secur. 11:2467. doi: 10.3390/foods11162467
LeRouge, C., Durneva, P., Sangameswaran, S., and Gloster, A. (2019). Design guidelines for a technology-enabled nutrition education program to support overweight and obese adolescents: qualitative user-centered design study. J. Med. Internet Res. 21:e14430. doi: 10.2196/14430
Li, S., Zhu, Y., Zeng, M., Li, Z., Zeng, H., Shi, Z., et al. (2022). Association between nutrition literacy and overweight/obesity of adolescents: a cross–sectional study in Chongqing, China. Front. Nutr. 9:893267. doi: 10.3389/fnut.2022.893267
Limbers, C. A., and Summers, E. (2021). Emotional eating and weight status in adolescents: a systematic review. Int. J. Environ. Res. Public Health 18:991. doi: 10.3390/ijerph18030991
Liu, K. S., Chen, J. Y., Sun, K. S., Tsang, J. P., Ip, P., and Lam, C. L. (2022). Adolescent knowledge, attitudes and practices of healthy eating: findings of qualitative interviews among Hong Kong families. Nutrients 14:2857. doi: 10.3390/nu14142857
Lombardo, C., and San Martini, P. (2005). “Psychometric properties of the Italian version of the emotional eating scale (EES)” in XIII general meeting of the International Society for Research on emotions (ISRE). 11–15.
Mallia, L., Chirico, A., Zelli, A., Galli, F., Palombi, T., Bortoli, L., et al. (2020). The implementation and evaluation of a media literacy intervention about PAES use in sport science students. Front. Psychol. 11:368. doi: 10.3389/fpsyg.2020.00368
Malloy-Weir, L., Begoray, D., and Tatlock, J. (2016). Public health nurses’ perceptions of health literacy in adolescent patients. J. Nurs. Educ. Pract. 6, 1–6. doi: 10.5430/jnep.v6n11p1
McLean, S., Wertheim, E., Masters, J., and Paxton, S. (2017). A pilot evaluation of a social media literacy intervention to reduce risk factors for eating disorders. Int. J. Eat. Disord. 50, 847–851. doi: 10.1002/eat.22708
Medeiros, G. C. B. S. D., Azevedo, K. P. M. D., Garcia, D., Oliveira Segundo, V. H., Mata, Á. N. D. S., Fernandes, A. K. P., et al. (2022). Effect of school-based food and nutrition education interventions on the food consumption of adolescents: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health 19:10522. doi: 10.3390/ijerph191710522
Murad, M., Alford, A., and Davis, K. (2021). Farm to future: a virtual summer nutrition culinary camp for kids. J. Nutr. Educ. Behav. 53, 445–448. doi: 10.1016/j.jneb.2020.10.006
Murphy, D., Lam, P., Naar-King, S., Harris, D., Parsons, J., and Muenz, L. (2010). Health literacy and antiretroviral adherence among hiv-infected adolescents. Patient Educ. Couns. 79, 25–29. doi: 10.1016/j.pec.2009.07.014
Muth, L., Leven, K., Moll, G., Kratz, O., and Horndasch, S. (2022). Effects of the covid-19 restrictions on eating behaviour and eating disorder symptomology in female adolescents. Int. J. Environ. Res. Public Health 19:8480. doi: 10.3390/ijerph19148480
Nagy-Pénzes, G., Vincze, F., and Bíró, É. (2022). A school intervention’s impact on adolescents’ health-related knowledge and behavior. Front. Public Health 10:822155. doi: 10.3389/fpubh.2022.822155
Noronha, D. C., Santos, M. I. A. F., Santos, A. A., Corrente, L. G. A., Fernandes, R. K. N., Barreto, A. C. A., et al. (2020). Nutrition knowledge is correlated with a better dietary intake in adolescent soccer players: a cross-sectional study. J. Nutr. Metabol. 2020, 1–7. doi: 10.1155/2020/3519781
Patton, G., Coffey, C., Carlin, J., Sanci, L., and Sawyer, S. (2008). Prognosis of adolescent partial syndromes of eating disorder. Br. J. Psychiatry 192, 294–299. doi: 10.1192/bjp.bp.106.031112
Qutteina, Y., Hallez, L., Raedschelders, M., Backer, C., and Smits, T. (2021). Food for teens: how social media is associated with adolescent eating outcomes. Public Health Nutr. 25, 290–302. doi: 10.1017/s1368980021003116
Raikar, K., Thakur, A., Mangal, A., Vaghela, J., Banerjee, S., and Gupta, V. (2020). A study to assess the effectiveness of a nutrition education session using flipchart among school-going adolescent girls. J. Educ. Health Prom. 9:183. doi: 10.4103/jehp.jehp_258_18
Ramos, N., Kielmann, K., Martins, M., and Fronteira, I. (2023). Health Liter. African Countries. 3:156619. doi: 10.21203/rs.3.rs-3156619/v1
Reid, A. L., Porter, K. J., You, W., Kirkpatrick, B. M., Yuhas, M., Vaught, S. S., et al. (2021). Low health literacy is associated with energy-balance-related behaviors, quality of life, and BMI among rural Appalachian middle school students: a cross-sectional study. J. Sch. Health 91, 608–616. doi: 10.1111/josh.13051
Ruiz, L. D., Radtke, M. D., and Scherr, R. E. (2021). Development and pilot testing of a food literacy curriculum for high school-aged adolescents. Nutrients 13:1532. doi: 10.3390/nu13051532
Ryan, R. M., and Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 55:68. doi: 10.1037/0003-066X.55.1.68
Ryan, R. M., and Deci, E. L. (2017). Self-determination theory: Basic psychological needs in motivation, development, and wellness. New York, NY: Guilford Press.
Sarhan, M., Fujiya, R., Shibanuma, A., Giacaman, R., Kiriya, J., Kitamura, A., et al. (2022). Health literacy as a key to improving weight status among palestinian adolescents living in chronic conflict conditions: a cross-sectional study. BMJ Open 12:e061169. doi: 10.1136/bmjopen-2022-061169
Schulenkorf, T., Sørensen, K., and Okan, O. (2022). International understandings of health literacy in childhood and adolescence—a qualitative-explorative analysis of global expert interviews. Int. J. Environ. Res. Public Health 19:1591. doi: 10.3390/ijerph19031591
Shriver, L. H., Dollar, J. M., Calkins, S. D., Keane, S. P., Shanahan, L., and Wideman, L. (2020). Emotional eating in adolescence: effects of emotion regulation, weight status and negative body image. Nutrients 13:79. doi: 10.3390/nu13010079
Sørensen, K., Broucke, S., Fullam, J., Doyle, G., Pelikan, J., Słońska, Z., et al. (2012). Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 12, 1–13. doi: 10.1186/1471-2458-12-80
Stok, M., De Ridder, D., De Vet, E., and De Wit, J.the Tempest Consortium (2013). The TEMPEST handbook: Strategies to support healthy eating in adolescents. The Hague, Netherlands: Dutch Nutrition Centre.
Taba, M., Allen, T., Kang, M., McCaffery, K., and Scott, K. (2022). Adolescents’ self-efficacy and digital health literacy: a cross-sectional mixed methods study. BMC Public Health 22:1223. doi: 10.1186/s12889-022-13599-7
Taleb, S., and Itani, L. (2021). Nutrition literacy among adolescents and its association with eating habits and BMI in Tripoli, Lebanon. Diseases 9:25. doi: 10.3390/diseases9020025
Tsubakita, T., Kawazoe, N., Ichikawa, M., Matsumoto, S., and Sugawara, M. (2020). Assessing knowledge-based and perceived health literacy among japanese adolescents: a cross-sectional study. Global Pediatric Health 7:2333794X2094431. doi: 10.1177/2333794x20944311
Vaitkeviciute, R., Ball, L., and Harris, N. (2014). The relationship between food literacy and dietary intake in adolescents: a systematic review. Public Health Nutr. 18, 649–658. doi: 10.1017/s1368980014000962
Velardo, S. (2015). The nuances of health literacy, nutrition literacy, and food literacy. J. Nutr. Educ. Behav. 47, 385–389. doi: 10.1016/j.jneb.2015.04.328
Vettori, V., Lorini, C., Gibbs, H. D., Sofi, F., Lastrucci, V., Sartor, G., et al. (2021). The nutrition literacy assessment instrument for Italian subjects, NLit-IT: exploring validity and reliability. Int. J. Environ. Res. Public Health 18:3562. doi: 10.3390/ijerph18073562
Wang, D., Stewart, D., Chang, C., and Shi, Y. (2015). Effect of a school-based nutrition education program on adolescents’ nutrition-related knowledge, attitudes and behaviour in rural areas of China. Environ. Health Prev. Med. 20, 271–278. doi: 10.1007/s12199-015-0456-4
Woods-Townsend, K., Hardy-Johnson, P., Bagust, L., Barker, M., Davey, H., Griffiths, J., et al. (2021). A cluster-randomised controlled trial of the LifeLab education intervention to improve health literacy in adolescents. PLoS One 16:e0250545. doi: 10.1371/journal.pone.0250545
Xiang, G., Li, Q., Xiao, Y., Liu, Y., Du, X., He, Y., et al. (2023). Mediation of self-concept clarity and self-control between negative emotional states and emotional eating in Chinese adolescents. Appetite 183:106457. doi: 10.1016/j.appet.2023.106457
Yang, S., Luo, Y., and Chiang, C. (2017). The associations among individual factors, ehealth literacy, and health-promoting lifestyles among college students. J. Med. Internet Res. 19:e15. doi: 10.2196/jmir.5964
Keywords: adolescent health literacy, nutritional education, eating habit intervention, self-regulation in diet, BMI improvement strategies, digital learning tools, emotional eating reduction, food knowledge enhancement
Citation: Mancone S, Corrado S, Tosti B, Spica G, Di Siena F, Misiti F and Diotaiuti P (2024) Enhancing nutritional knowledge and self-regulation among adolescents: efficacy of a multifaceted food literacy intervention. Front. Psychol. 15:1405414. doi: 10.3389/fpsyg.2024.1405414
Edited by:
Roberta Masella, National Institute of Health (ISS), ItalyReviewed by:
Beatrice Scazzocchio, National Institute of Health (ISS), ItalyElena Sturchio, National Institute for Insurance Against Accidents at Work (INAIL), Italy
Copyright © 2024 Mancone, Corrado, Tosti, Spica, Di Siena, Misiti and Diotaiuti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pierluigi Diotaiuti, cC5kaW90YWl1dGlAdW5pY2FzLml0
 Stefania Mancone
Stefania Mancone Stefano Corrado
Stefano Corrado Beatrice Tosti
Beatrice Tosti Giuseppe Spica
Giuseppe Spica Francesco Di Siena
Francesco Di Siena Francesco Misiti
Francesco Misiti Pierluigi Diotaiuti
Pierluigi Diotaiuti