- 1Department of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 2Hubei Province Key Laboratory of Molecular Imaging, Wuhan, China
- 3Department of Rehabilitation, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 4Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 5Department of Thoracic Surgery, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 6Department of Emergency Surgery, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 7Department of Geriatrics, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Purpose: Depression and anxiety are prevalent mental health challenges among college students. Music therapy has shown effectiveness in addressing depressive symptoms and enhancing psychosomatic functioning. This study aimed to evaluate the effectiveness of a 4-step structured music therapy program in improving mood and reducing symptoms of depression and anxiety among medical school students.
Materials and methods: The self-controlled study involved 45 medical school students (21 men and 24 women) aged 18–24 years to examine the prevalence of depression and anxiety, common mental health issues among medical school students. Participants underwent psychological assessment using the Symptom Checklist-90 (SCL-90), Self-Rating Anxiety Scale (SAS), and Self-Rating Depression Scale (SDS). An 8-week music therapy intervention, comprising four steps—sociality, interaction, music lessons, and creative expression—was administered.
Results: Before-intervention, 55.6% and 15.6% students were identified as suffering from depression and anxiety respectively. Post-intervention, significant reductions in psychological distress, particularly in the Global Severity Index (GSI) and Positive Symptom Total (PST) on the SCL-90 scale, were observed (P < 0.05). Male students exhibited notable improvements in various psychological symptoms compared to females. Junior grade students demonstrated greater improvements, and clinical medicine students exhibited significant enhancements in specific areas post-intervention.
Conclusion: The structured music therapy program showed promising results in improving mood and regulating emotions among medical school students. Music therapy holds potential as a holistic approach to address mental health challenges in this demographic.
1 Introduction
Depression and anxiety are prevalent mental health challenges among college students, with global statistics ranking them fourth and sixth, respectively, in the major burdens faced by individuals aged 10–24 years (Global Burden of Disease Study and Injuries, 2020). These disorders significantly contribute to self-harm and injury, particularly among adolescents and young adults (Li et al., 2023). Notably, research indicates that depression is a primary emotional concern for college students, particularly those in university settings (Pratt and Brody, 2014; Rotenstein et al., 2016). The prevalence of common mental health issues, including depression and anxiety, has been on the rise among college students in recent years (Lattie et al., 2019; Li et al., 2023). Notably, medical school students, due to the prolonged duration required for acquiring knowledge and skills in the field of medicine, face heightened levels of mental and physical stress (Adams, 2004; O'Rourke et al., 2010; Quek et al., 2019; Zeng et al., 2019). Various studies consistently show that medical school students experience a higher prevalence of depression and anxiety compared to the general population (Adams, 2004; Dyrbye et al., 2006; Khan et al., 2006; Ahmed et al., 2009; Hope and Henderson, 2014; Tabalipa et al., 2015; Azad et al., 2017; Quek et al., 2019).
Music therapy, recognized as the professional use of music and its elements for therapeutic purposes, has emerged as a promising intervention in medical, educational, and everyday settings (Maratos et al., 2008). It utilizes musical activities to stimulate individuals and elicit physical responses, with the goal of enhancing health through tools such as music, relationships, and reflection. Music therapy is comprised of active and receptive approaches that also integrate verbal processing. These approaches include various ways of engaging with music, including receptive, improvisational, compositional, and recreative (Bruscia, 2014). Research involving patients diagnosed with mental disorders has consistently shown significant improvements in mental health following interventions that utilize music as a primary tool (Edwards, 2006; Mössler et al., 2011; Rebecchini, 2021; Zhang et al., 2022). Additionally, numerous studies have highlighted the multifaceted benefits of music, ranging from enhancements physical and mental wellbeing (Fancourt et al., 2014; Khan et al., 2018; Wang and Agius, 2018). However, the potential of music therapy to improve emotional wellbeing, alleviate depression, or reduce anxiety among medical school students—a unique demographic group—remains largely unexplored. In this study, our aim was to address the psychological challenges encountered by medical school students through the use of comprehensive screening tools, including the SCL-90, SDS, and SAS scales. Our primary objective was to evaluate the efficacy of music therapy as a non-pharmacological intervention in enhancing mood and alleviating symptoms of depression and anxiety among medical school students.
By specifically targeting this demographic group, our research seeks to fill a crucial gap in the literature and provide valuable insights into the effectiveness of music therapy as a tailored intervention for improving the mental health and wellbeing of medical school students. The integration of music therapy into mental health support strategies for this population shows promise and merits further investigation.
2 Materials and methods
2.1 Participants
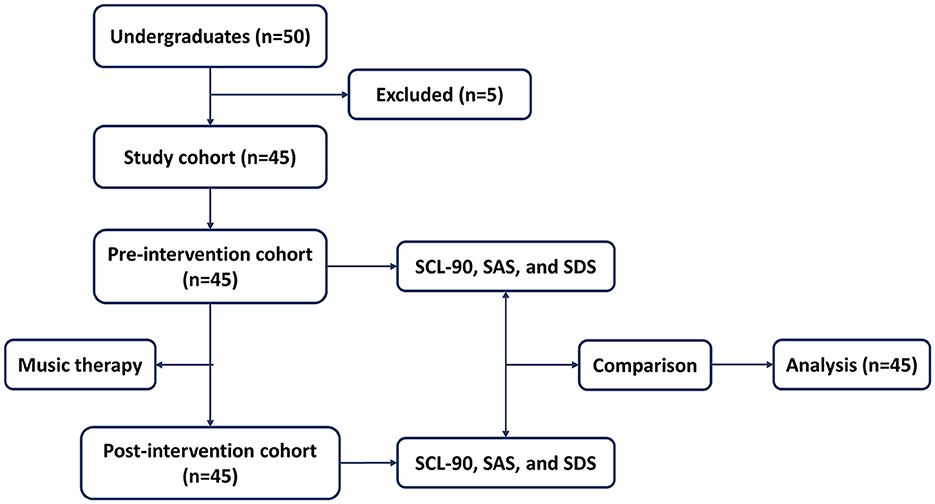
The research, conducted at Tongji Medical College, Huazhong University of Science and Technology in Wuhan, Hubei, China, spanned from April to November 2023 and received ethical approval from the Ethics Committee of Tongji Medical College. This collaborative effort involved three trained music therapists, two clinical doctors, and facilitators who are educators at the medical college. The study focused on medical school students, with inclusion criteria comprising individuals aged between 18 and 24 years. The investigation aimed to assess the efficacy of scales (SCL-90, SAS, and SDS) before and after music therapy. Exclusion criteria encompassed immediate suicidal thoughts or behaviors, a history or current presence of mental illnesses, and concurrent music or antidepressant therapy elsewhere. The participant workflow is elucidated in Figure 1.
2.2 Music therapy intervention
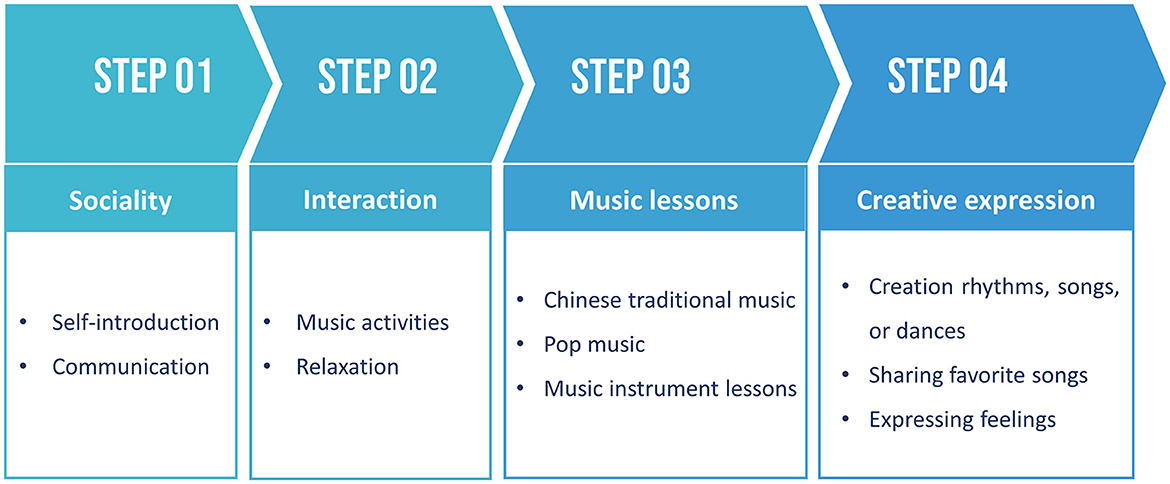
A total of 8 weekly music therapy sessions, each lasting 2 h, were implemented. The music therapy protocol involved four sequential steps outlined in Figure 2.
Music therapy interventions were structured as follows:
Step 1: social interaction
• Introduction: This step served as an icebreaker, introducing participants to the concept of music therapy and facilitating self-introductions among group members to foster familiarity.
• Communication: Participants were encouraged to share their experiences, technical knowledge, social skills, music backgrounds, or emotions. This facilitated exploration of individuality and self-expression within the group dynamic.
Step 2: interactive music activities
• Music Activities: Participants engaged in various music-related group activities such as listening to music, playing musical instruments, singing, rhythmic interventions, and dancing. These activities helped participants identify emotions, connect mind and body through music, alleviate social anxiety, and promote self-expression.
• Mediation and Progressive Relaxation: Directed listening sessions guided participants through mediation, progressive relaxation, or breathing exercises, aiding in emotional processing and relaxation (Gallego-Gómez et al., 2020; Hwang et al., 2023).
Step 3: Music lessons
• Chinese Traditional Music: Participants received lessons on Chinese pentatonic songs, which are familiar to Chinese students and are known for their calming and mood-stabilizing effects. These lessons aimed to improve self-esteem and overall wellbeing (Zhang and Gao, 2022; Fu and Tu, 2023; Wu et al., 2023).
• Popular music: Lessons encompassed various genres including folk, jazz, blues, reggae, funk, pop, and rock, catering to diverse musical preferences. Popular music, known for its widespread acceptance and catchy lyrics, was included to promote relaxation and emotional awareness, contributing positively to mental health (Kulinski et al., 2022; Zhang and Hu, 2023).
• Music instrument lessons: rhythm instruments (drums, cymbals, gongs, etc.) and melody instruments (guitar, piano, guzheng, dulcimer, erhu, flute, etc.).
Step 4: creative expression
• Creating and sharing: Participants engaged in creative expression through rhythm creation, songwriting, dance improvisation, and musical improvisation. This allowed them to express their feelings through music, fostering cognitive health and wellbeing (Dingle et al., 2021).
• Sharing favorites: Participants shared their favorite songs or melodies, discussing their meanings and enhancing social connections within the group, thus uplifting mood and fostering a sense of community (Dingle et al., 2021).
2.3 Scales
This study employed the SCL-90, SDS, and SAS to screen and evaluate psychological disorders, depression, and anxiety in medical school students. Validity and reliability studies of the SCL-90, SAS, and SDS scales yielded good psychometric qualities (Yu et al., 2019; Wang et al., 2022). In our study, Cronbach's α values were found to be above 0.97, 0.78, and 0.88, respectively.
The SCL-90, a self-report questionnaire, gauges psychological symptoms experienced in the past 7 days. Each of its 90 items is rated on a five-point scale (0. Normal; 1. Mild; 2. Moderate; 3. Severe; 4. Extreme), contributing to nine scores across major symptom dimensions: Somatization, Obsession-Compulsion, Interpersonal Sensitivity, Depression, Anxiety, Hostility, Phobic Anxiety, Paranoid Ideation, Psychoticism, and Additional items. Additionally, three global indices—Global Severity Index (GSI), Positive Symptom Total (PST), and Positive Symptom Distress Index (PSDI)—can be calculated (Holi et al., 1998; Schauenburg and Strack, 1999; Schmitz et al., 2000; Maremmani et al., 2010, 2018; Dang et al., 2020).
The SDS and SAS, commonly used scales for assessing depression and anxiety (Dunstan et al., 2017; Dunstan and Scott, 2020). each comprise 20 items with raw scores ranging from 20 to 80. Questions are rated on a 1–4 Likert scale, from “a little of the time” to “most of the time.” SDS scores categorize depression levels: 20–44 (normal); 45–59 (mild depression); 60–69 (moderate depression); 70 and above (severe depression). SAS scores categorize anxiety levels: 20–44 (normal range); 45–59 (mild to moderate anxiety); 60–74 (severe anxiety); 75 and above (extreme anxiety) (Zung, 1971, 1974; Guo and Huang, 2021).
2.4 Data analysis
All data were processed and analyzed utilizing SPSS 26.0 software. Data normality was evaluated using the Shapiro-Wilk test in SPSS. As a result of non-normality, the paired Wilcoxon signed-rank test was utilized to assess differences in psychological indexes between cohorts. Count data were analyzed using the χ2 test. A significance level of P < 0.05 was considered indicative of statistical significance.
3 Results
3.1 Participant characteristics
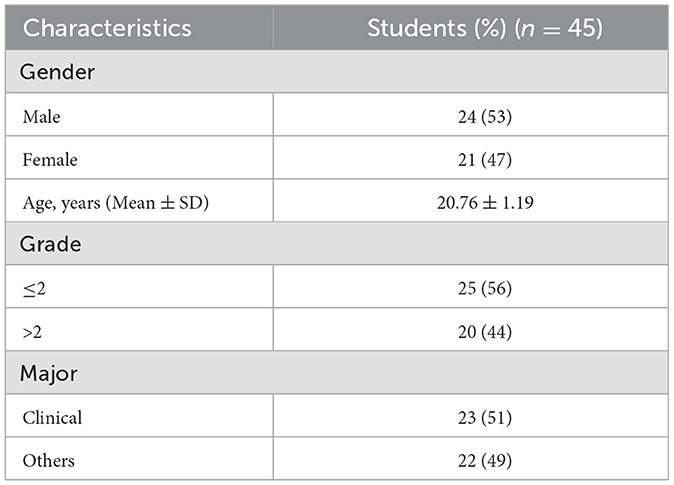
The study included 45 medical school students, comprising 21 males and 24 females, who were divided into two groups: the pre-music therapy cohort and the post-music therapy cohort. Table 1 presents the participants' characteristics, including age, gender, grade, and major.
3.2 Music therapy helps to improve mood and regulate emotions
Before and after music therapy, the enrolled students' scores on the SCL-90, SDS, and SAS scales were recorded. Initially, the mean values for GSI, PST, and PSDI were 0.39, 24.0, and 1.47, respectively. Of the total 45 students, 25 were identified as suffering from depression, accounting for 55.6%, while 7 students (15.6%) were in a state of anxiety (Table 2).

Table 2. Participant characteristics of the SCL-90, SAS, and SDS scales among medical students in the pre- and post-intervention cohorts.
Post-intervention, a significant decrease in GSI (P = 0.024) and PST (P = 0.007) was observed, indicating a lower overall psychological distress and reduced symptom severity. These findings suggest that music therapy effectively improved mood and may serve as a means to regulate emotions. However, there were no significant differences observed in SDS or SAS scores following the intervention.
3.3 Improvement of interpersonal sensibility and hostility after music therapy
Following music therapy intervention, the total score of SCL-90 significantly decreased compared to pre-intervention levels, while no notable difference was found in SAS or SDS scores post-intervention (Table 3). Further analysis of the nine subscales of SCL-90 revealed significant reductions in students' interpersonal sensibility and hostility (P = 0.007 and P = 0.005, respectively) post-intervention. Additionally, improvements in anxiety and paranoid ideation were observed, although they did not reach statistical significance at the 0.05 level.

Table 3. Comparison of SCL-90, SCL-90 subscale, SAS, and SDS of medical students in the pre- and post-intervention cohorts (n = 45).
3.4 Gender differences in music therapy
Regarding gender differences in SCL-90 and its subscales, SAS, and SDS, male students exhibited significant improvements in somatization, interpersonal sensibility, and hostility post-intervention (P = 0.04, P = 0.023, P = 0.021, respectively, Table 4). However, females showed no statistically significant differences in any subscales, SDS, or SAS. Paranoid ideation and SDS exhibited trends of improvement, but the P-values did not reach 0.05.
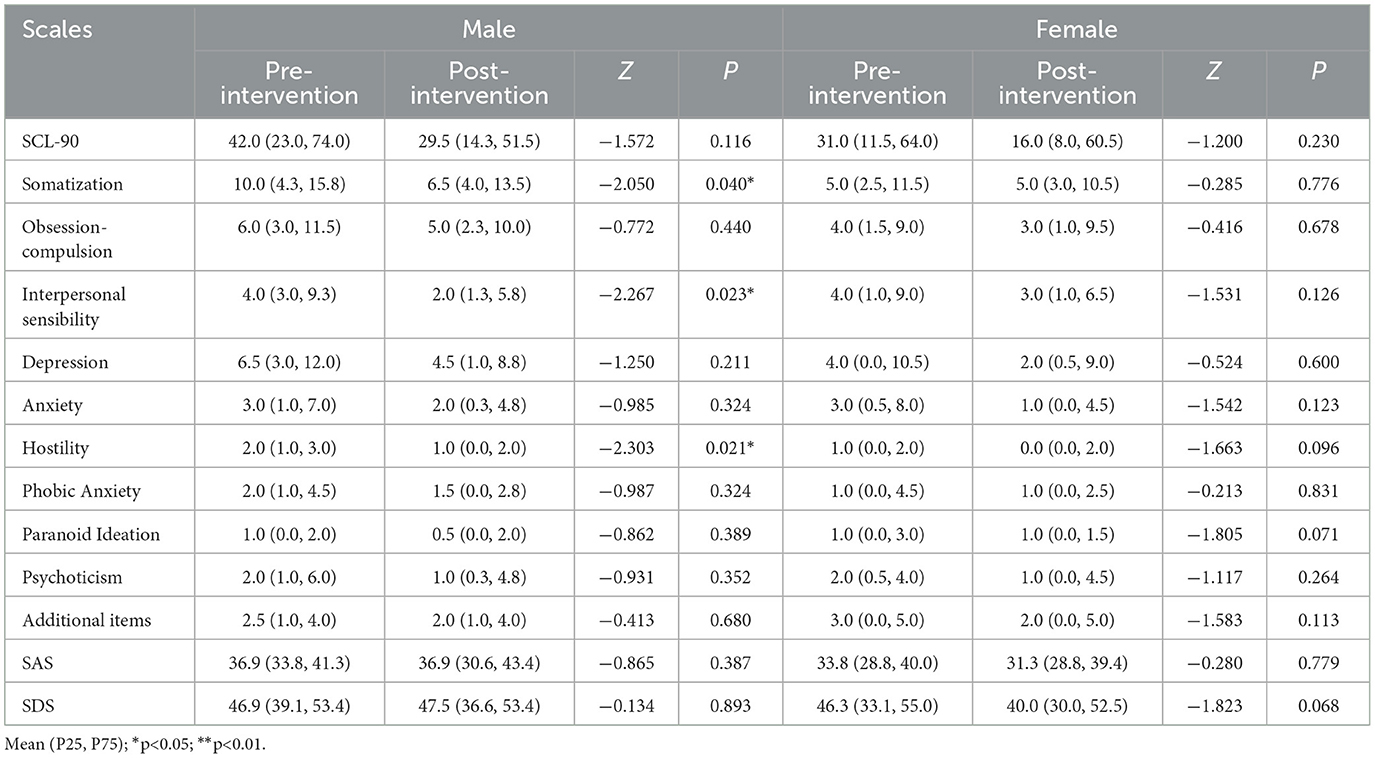
Table 4. Comparison of SCL-90, SCL-90 subscale, SAS, and SDS of medical students in the pre-intervention and post-intervention cohorts with gender (female and male).
3.5 Junior grades showed significant improvements after music therapy
To assess the effects of music therapy on students at different grades, scales were analyzed for 25 junior ( ≤ 2) grade students and 20 senior (>2) grade students. Interestingly, junior students demonstrated significantly lower scores in SCL-90 total score (P = 0.0039), interpersonal sensibility (P = 0.015), hostility (P = 0.007), and paranoid ideation (P = 0.044) post-intervention. However, no significant differences were observed in the senior group after music therapy (Table 5). These results suggest that music therapy may be more effective or suitable for junior medical school students.

Table 5. Comparison of SCL-90, SCL-90 subscale, SAS, and SDS of medical students in the pre-intervention and post-intervention cohorts with grade ( ≤ 2 and >2).
3.6 Clinical medicine students exhibited significant improvements after music intervention
The enrolled students represented various healthcare majors, including Clinical Medicine, Pharmacy, Nursing, Radiology, Public Health, Stomatology, and Laboratory Medicine, with clinical medicine students comprising 51.0% of the total. A comparison of the effects of music therapy on clinical medicine students and those in other majors revealed significant improvements in hostility (P = 0.002), paranoid ideation (P = 0.037), and additional items (P = 0.004) among clinical medicine students, while no significant difference was observed in students from other majors post-intervention (Table 6).
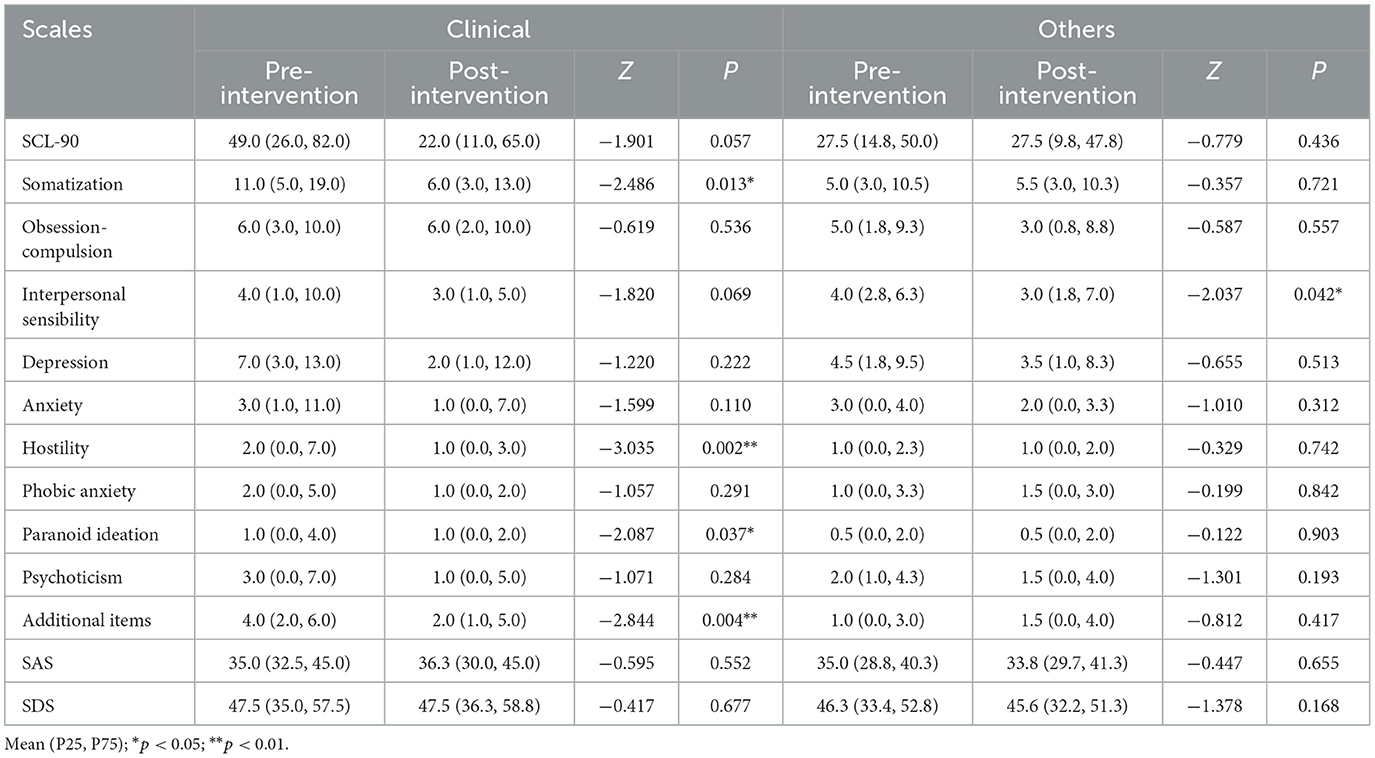
Table 6. Comparison of SCL-90, SCL-90 subscale, SAS, and SDS of medical students in the pre-intervention and post-intervention cohorts with major (Clinical and Others).
4 Discussion
This pioneering study is the first to utilize the SCL-90, SDS, and SAS scales to assess the impact of a 4-step structured music therapy program on medical school students. The results revealed promising outcomes, especially among male, junior grade, and clinical medicine students, indicating improvements in mood regulation and emotional wellbeing. This highlights the potential of music therapy as a non-pharmacological intervention for addressing mental health challenges among medical school students.
Medical school students are under immense academic, interpersonal, and emotional pressures, which often lead to heightened levels of anxiety and depression (Dyrbye et al., 2006; Hope and Henderson, 2014; Brenneisen Mayer et al., 2016). Our research found that the prevalence of depression and anxiety among Chinese medical school students was 55.6% and 15.6%, respectively, surpassing global rates (Brenneisen Mayer et al., 2016). While previous studies have shown the positive impact of music therapy on college students' mental wellbeing (Finnigan and Starr, 2010; Zhang et al., 2022; Finnerty et al., 2023; Nwokenna et al., 2023), no research has explored its efficacy specifically among medical school students. By focusing on this demographic, our study aims to bridge this gap in the literature and provide valuable insights into the effectiveness of music therapy as a tailored intervention.
In response, we designed an 8-week, 4-step music therapy program tailored specifically for medical school students. The program included various components aimed at fostering social interaction, engaging in music activities, learning music theory, and encouraging creative expression. Step 1 focused on fostering social connections through self-introduction and communication exercises, helping students acclimate to their environment, alleviate tension, and build trust with peers and instructors. Step 2 incorporated common music therapy techniques such as playing instruments, singing, and rhythmic interventions, along with progressive relaxation exercises to directly improve students' mental state, divert attention, and reduce tension and anxiety (Robb, 2000; Kim, 2008). Step 3 involved teaching students music theory, including different music genres, Chinese pentatonic songs, and various musical instruments. This aimed to enhance students' music appreciation skills and aesthetics, thereby improving subjective wellbeing and amplifying the therapeutic effects of music therapy (Robb, 2000; Che et al., 2022; Fu and Tu, 2023). The final step encouraged students to engage in creative expression by creating rhythms, songs, or dances through improvisation. This was followed by sharing favorite songs and expressing feelings, enabling students to understand and acknowledge their own emotional states and needs, express themselves freely, and build self-confidence, ultimately alleviating stress and anxiety. This comprehensive approach addresses various aspects of psychological wellbeing, providing medical school students with a holistic therapeutic experience tailored to their unique challenges and needs.
This study employed an innovative approach by utilizing three psychological scales—SCL-90, SDS, and SAS—to screen for mental health issues among medical school students. While various psychological scales, such as the Beck Depression Inventory (BDI) (Baldassin et al., 2008) and State-Trait Anxiety Inventory (STAI) (Du et al., 2022), are commonly used to assess depression and anxiety, they primarily focus on cognitive and affective aspects. In contrast, the combination of SCL-90, SDS, and SAS offers a more comprehensive understanding of psychological symptoms and provides a broader evaluation of depression and anxiety symptoms (Zung, 1971, 1974; Dunstan et al., 2017; Dunstan and Scott, 2020).
Using these methods, we observed a significant reduction in the GSI and PST on the SCL-90 scale following music therapy intervention. These findings indicate that music therapy may effectively improve mood and regulate emotions among medical school students. Notably, there were gender differences in response to music therapy, with male students showing significant improvements in somatization, interpersonal sensibility, and hostility compared to females. This suggests the need for gender-specific approaches in mental health interventions. Furthermore, the study explored the differential effects of music therapy based on academic grade and major. Junior grade students exhibited significant improvements across various scales post-intervention, consistent with previous research (Ludwig et al., 2015). Additionally, our investigation uncovered noteworthy insights into students majoring in clinical medicine, who demonstrated significant enhancements in hostility, paranoid ideation, and other factors compared to peers from different healthcare majors. These results emphasize the importance of tailoring music therapy interventions according to both academic progression and field of study, highlighting the nuanced nature of mental health interventions within academic contexts. Recognizing the unique needs and challenges faced by students in different healthcare disciplines is crucial for designing effective intervention strategies. By acknowledging these variations, healthcare professionals can develop targeted approaches to address specific issues and promote overall wellbeing among students pursuing diverse paths within the healthcare field. Furthermore, our findings suggest the potential benefits of integrating music therapy as a complementary intervention in clinical medicine education, potentially enhancing students' mental health and overall academic experience. Such integration could contribute to their professional development, fostering a healthier and more resilient future healthcare workforce.
While the results of this study are promising, several limitations should be acknowledged. The sample size was relatively small, and the study duration was limited to 8 weeks. Long-term follow-up and larger-scale studies would provide more robust evidence of the sustained effectiveness of music therapy in this context.
5 Conclusion
In conclusion, this study underscores the potential of music therapy as a non-pharmacological intervention for mitigating mental health challenges among medical school students. The structured music therapy protocol employed here demonstrated promising outcomes in enhancing mood and emotional regulation, notably among male students, those in junior grades, and pursuing clinical medicine. By introducing an alternative or complementary treatment approach, this research contributes to addressing the mental wellbeing of students, achieving its primary aim of mood improvement.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Affiliated Union Hospital in Tongji Medical College of Huazhong University of Science and Technology (no.ChiCTR2200056141). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
QC: Writing—original draft, Formal analysis, Data curation. CM: Writing—original draft, Data curation. LQ: Writing—original draft, Data curation. YL: Writing—original draft, Formal analysis, Data curation. GY: Writing—original draft, Validation, Software. LW: Writing—original draft, Investigation. CL: Writing—original draft, Resources. CZ: Writing—review & editing. JZ: Writing—review & editing. CF: Writing—review & editing, Project administration.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by Teaching Reform Research Project of the First Clinical School, Huazhong University of Science and Technology (No:2023XH007), Hubei Provincial Natural Science Foundation of China (No:2023AFB720), and Hubei Province Key Laboratory of Molecular Imaging Foundation of China (No:2022fzyx007).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Adams, J. (2004). Straining to describe and tackle stress in medical students. Med. Educ. 38, 463–464. doi: 10.1111/j.1365-2929.2004.01810.x
Ahmed, I., Banu, H., Al-Fageer, R., and Al-Suwaidi, R. (2009). Cognitive emotions: depression and anxiety in medical students and staff. J. Crit. Care 24, e1–7. doi: 10.1016/j.jcrc.2009.06.003
Azad, N., Shahid, A., Abbas, N., Shaheen, A., and Munir, N. (2017). Anxiety and depression in medical students of a private medical college. J. Ayub. Med. Coll. Abbottabad 29, 123–127.
Baldassin, S., Alves, T. C., de Andrade, A. G., and Nogueira Martins, L. A. (2008). The characteristics of depressive symptoms in medical students during medical education and training: a cross-sectional study. BMC Med. Educ. 8:60. doi: 10.1186/1472-6920-8-60
Brenneisen Mayer, F., Souza Santos, I., Silveira, P. S., Itaqui Lopes, M. H., Souza, A. R., de Campos, E. P., et al. (2016). Factors associated to depression and anxiety in medical students: a multicenter study. BMC Med. Educ. 16:282. doi: 10.1186/s12909-016-0791-1
Che, Y., Jicol, C., Ashwin, C., Petrini, K., and An, R. C. T. (2022). study showing few weeks of music lessons enhance audio-visual temporal processing. Sci. Rep. 12:20087. doi: 10.1038/s41598-022-23340-4
Dang, W., Xu, Y., Ji, J., Wang, K., Zhao, S., Yu, B., et al. (2020). Study of the SCL-90 scale and changes in the Chinese norms. Fron.t Psychiatr. 11:524395. doi: 10.3389/fpsyt.2020.524395
Dingle, G. A., Sharman, L. S., Bauer, Z., Beckman, E., Broughton, M., Bunzli, E., et al. (2021). How do music activities affect health and well-being? A scoping review of studies examining psychosocial mechanisms. Front. Psychol. 12:713818. doi: 10.3389/fpsyg.2021.713818
Du, Q., Liu, H., Yang, C., Chen, X., and Zhang, X. (2022). The development of a short Chinese version of the state-trait anxiety inventory. Front. Psychiatr. 13:854547. doi: 10.3389/fpsyt.2022.854547
Dunstan, D. A., and Scott, N. (2020). Norms for Zung's self-rating anxiety scale. BMC Psychiatr. 20:90. doi: 10.1186/s12888-019-2427-6
Dunstan, D. A., Scott, N., and Todd, A. K. (2017). Screening for anxiety and depression: reassessing the utility of the Zung scales. BMC Psychiatr. 17:329. doi: 10.1186/s12888-017-1489-6
Dyrbye, L. N., Thomas, M. R., and Shanafelt, T. D. (2006). Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad. Med. 81, 354–373. doi: 10.1097/00001888-200604000-00009
Edwards, J. (2006). Music therapy in the treatment and management of mental disorders. Ir. J. Psychol. Med. 23, 33–35. doi: 10.1017/S0790966700009459
Fancourt, D., Ockelford, A., and Belai, A. (2014). The psychoneuroimmunological effects of music: a systematic review and a new model. Brain Behav. Immun. 36, 15–26. doi: 10.1016/j.bbi.2013.10.014
Finnerty, R., McWeeny, S., and Trainor, L. (2023). Online group music therapy: proactive management of undergraduate students' stress and anxiety. Front. Psychiatr. 14:1183311. doi: 10.3389/fpsyt.2023.1183311
Finnigan, E., and Starr, E. (2010). Increasing social responsiveness in a child with autism. A comparison of music and non-music interventions. Autism 14, 321–348. doi: 10.1177/1362361309357747
Fu, H., and Tu, J. (2023). Exploring the influence of national music lessons on subjective well-being, self-esteem, and national identity among university students: a case study from China. Front. Psychol. 14:1151007. doi: 10.3389/fpsyg.2023.1151007
Gallego-Gómez, J. I., Balanza, S., Leal-Llopis, J., García-Méndez, J. A., Oliva-Pérez, J., Doménech-Tortosa, J., et al. (2020). Effectiveness of music therapy and progressive muscle relaxation in reducing stress before exams and improving academic performance in Nursing students: a randomized trial. Nurse Educ. Today 84, 104217. doi: 10.1016/j.nedt.2019.104217
Global Burden of Disease Study and Injuries (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222. doi: 10.1016/S0140-6736(20)30925-9
Guo, C., and Huang, X. (2021). Hospital anxiety and depression scale exhibits good consistency but shorter assessment time than Zung self-rating anxiety/depression scale for evaluating anxiety/depression in non-small cell lung cancer. Medicine 100:e24428. doi: 10.1097/MD.0000000000024428
Holi, M. M., Sammallahti, P. R., Aalberg, V. A., and Finnish, A. (1998). Validation study of the SCL-90. Acta Psychiatr. Scand. 97, 42–46. doi: 10.1111/j.1600-0447.1998.tb09961.x
Hope, V., and Henderson, M. (2014). Medical student depression, anxiety and distress outside North America: a systematic review. Med. Educ. 48, 963–979. doi: 10.1111/medu.12512
Hwang, M. H., Bunt, L., and Warner, C. (2023). An eight-week zen meditation and music programme for mindfulness and happiness: qualitative content analysis. Int. J. Environ. Res. Public Health 20:140. doi: 10.3390/ijerph20237140
Khan, M. S., Mahmood, S., Badshah, A., Ali, S. U., and Jamal, Y. (2006). Prevalence of depression, anxiety and their associated factors among medical students in Karachi, Pakistan. J. Pak. Med. Assoc. 56, 583–586.
Khan, S. H., Kitsis, M., Golovyan, D., Wang, S., Chlan, L. L., Boustani, M., et al. (2018). Effects of music intervention on inflammatory markers in critically ill and post-operative patients: a systematic review of the literature. Heart Lung 47, 489–496. doi: 10.1016/j.hrtlng.2018.05.015
Kim, Y. (2008). The effect of improvisation-assisted desensitization, and music-assisted progressive muscle relaxation and imagery on reducing pianists' music performance anxiety. J. Music Ther. 45, 165–191. doi: 10.1093/jmt/45.2.165
Kulinski, J., Ofori, E. K., Visotcky, A., Smith, A., Sparapani, R., Fleg, J. L., et al. (2022). Effects of music on the cardiovascular system. Trends Cardiovasc. Med. 32, 390–398. doi: 10.1016/j.tcm.2021.06.004
Lattie, E. G., Adkins, E. C., Winquist, N., Stiles-Shields, C., Wafford, Q. E., Graham, A. K., et al. (2019). Digital mental health interventions for depression, anxiety, and enhancement of psychological well-being among college students: systematic review. J. Med. Int. Res. 21:e12869. doi: 10.2196/12869
Li, F. B., Lu, P., Wu, H. T., Wang, M. H., and Wang, J. D. (2023). Effects of music, massage, exercise, or acupuncture in the treatment of depression among college students: a network meta-analysis. Neuropsychiatr. Dis. Treat 19, 1725–1739. doi: 10.2147/NDT.S416643
Ludwig, A. B., Burton, W., Weingarten, J., Milan, F., Myers, D. C., Kligler, B., et al. (2015). Depression and stress amongst undergraduate medical students. BMC Med. Educ. 15:141. doi: 10.1186/s12909-015-0425-z
Maratos, A. S., Gold, C., Wang, X., and Crawford, M. J. (2008). Music therapy for depression. Cochrane Database Syst. Rev. 1:CD004517. doi: 10.1002/14651858.CD004517.pub2
Maremmani, A. G. I., Gazzarrini, D., Fiorin, A., Cingano, V., Bellio, G., Perugi, G., et al. (2018). Psychopathology of addiction: Can the SCL90-based five-dimensional structure differentiate Heroin Use Disorder from a non-substance-related addictive disorder such as Gambling Disorder? Ann. Gen. Psychiatr. 17:3. doi: 10.1186/s12991-018-0173-7
Maremmani, I., Pani, P. P., Pacini, M., Bizzarri, J. V., Trogu, E., Maremmani, A. G., et al. (2010). Subtyping patients with heroin addiction at treatment entry: factor derived from the Self-Report Symptom Inventory (SCL-90). Ann Gen. Psychiatr. 9:15. doi: 10.1186/1744-859X-9-15
Mössler, K., Chen, X., Heldal, T. O., and Gold, C. (2011). Music therapy for people with schizophrenia and schizophrenia-like disorders. Cochrane Database Syst. Rev. 12:Cd004025. doi: 10.1002/14651858.CD004025.pub3
Nwokenna, E. N., Sewagegn, A. A., and Falade, T. A. (2023). Effect of educational music intervention on college students' aggressive behaviour. Medicine 102:e32472. doi: 10.1097/MD.0000000000032472
O'Rourke, M., Hammond, S., O'Flynn, S., and Boylan, G. (2010). The medical student stress profile: a tool for stress audit in medical training. Med. Educ. 44, 1027–1037. doi: 10.1111/j.1365-2923.2010.03734.x
Pratt, L. A., and Brody, D. J. (2014). Depression in the U.S. household population, 2009-2012. NCHS Data Brief 172, 1–8.
Quek, T. T., Tam, W. W., Tran, B. X., Zhang, M., Zhang, Z., Ho, C. S., et al. (2019). the global prevalence of anxiety among medical students: a meta-analysis. Int. J. Environ. Res. Public Health 16:735. doi: 10.3390/ijerph16152735
Rebecchini, L. (2021). Music, mental health, and immunity. Brain Behav. Immun. Health 18:100374. doi: 10.1016/j.bbih.2021.100374
Robb, S. L. (2000). Music assisted progressive muscle relaxation, progressive muscle relaxation, music listening, and silence: a comparison of relaxation techniques. J. Music Ther. 37, 2–21. doi: 10.1093/jmt/37.1.2
Rotenstein, L. S., Ramos, M. A., Torre, M., Segal, J. B., Peluso, M. J., Guille, C., et al. (2016). Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA 316, 2214–2236. doi: 10.1001/jama.2016.17324
Schauenburg, H., and Strack, M. (1999). Measuring psychotherapeutic change with the symptom checklist SCL 90 R. Psychother. Psychosom. 68, 199–206. doi: 10.1159/000012333
Schmitz, N., Hartkamp, N., and Franke, G. H. (2000). Assessing clinically significant change: application to the SCL-90-R. Psychol. Rep. 86, 263–274. doi: 10.2466/pr0.2000.86.1.263
Tabalipa, F. D. O., Souza, M. F. D., Pfützenreuter, G., Lima, V. C., Traebert, E., and Traebert, J. (2015). Prevalence of anxiety and depression among medical students. Revista Brasileira de Educação Médica 39, 388–394. doi: 10.1590/1981-52712015v39n3e02662014
Wang, Q., Zhang, B., Zhang, S., Wei, C., Fu, D., Zhao, H., et al. (2022). Anxiety and depression and their interdependent influencing factors among medical students in Inner Mongolia: the cross-sectional survey. BMC Med. Educ. 22, 787. doi: 10.1186/s12909-022-03839-0
Wang, S., and Agius, M. (2018). The use of music therapy in the treatment of mental illness and the enhancement of societal wellbeing. Psychiatr. Danub 30, 595–600.
Wu, Y., Li, J., Qiao, J., Jia, D., Pang, K., Yang, F., et al. (2023). Effects of traditional Chinese medicine five-element music therapy combined with mirtazapine on depression and limb function recovery after ischemic stroke. Altern. Ther. Health Med. (2023). [Epub ahead of print].
Yu, Y., Wan, C., Huebner, E. S., Zhao, X., Zeng, W., Shang, L., et al. (2019). Psychometric properties of the symptom check list 90 (SCL-90) for Chinese undergraduate students. J. Ment. Health 28, 213–219. doi: 10.1080/09638237.2018.1521939
Zeng, W., Chen, R., Wang, X., Zhang, Q., and Deng, W. (2019). Prevalence of mental health problems among medical students in China: a meta-analysis. Medicine 98:e15337. doi: 10.1097/MD.0000000000015337
Zhang, L., and Hu, J. (2023). Pop music singing in education with modern innovative technologies: how the chinese language shapes the creation of popular singing. J. Psycholinguist. Res. 52, 2677–2691. doi: 10.1007/s10936-023-10014-z
Zhang, M., Ding, Y., Zhang, J., Jiang, X., Xu, N., Zhang, L., et al. (2022). Effect of group impromptu music therapy on emotional regulation and depressive symptoms of college students: a randomized controlled study. Front. Psychol. 13:851526. doi: 10.3389/fpsyg.2022.851526
Zhang, Y., and Gao, S. H. (2022). Chinese traditional five-tone music therapy. Zhonghua Yi Shi Za Zhi 52, 323–327.
Zung, W. W. (1971). A rating instrument for anxiety disorders. Psychosomatics 12, 371–379. doi: 10.1016/S0033-3182(71)71479-0
Keywords: music therapy, medical students, depression, anxiety, SCL-90
Citation: Chen Q, Mao C, Qi L, Luo Y, Yang G, Wang L, Liu C, Zheng C, Zhang J and Fan C (2024) Music-based therapeutic interventions for medical school students with emotional regulation and mental health: a pre-post cohort study. Front. Psychol. 15:1401129. doi: 10.3389/fpsyg.2024.1401129
Received: 04 April 2024; Accepted: 14 May 2024;
Published: 30 May 2024.
Edited by:
Han Zheng, Wuhan University, ChinaReviewed by:
Qian Wu, Nanyang Technological University, SingaporeAnnie L. Heiderscheit, Anglia Ruskin University, United Kingdom
Copyright © 2024 Chen, Mao, Qi, Luo, Yang, Wang, Liu, Zheng, Zhang and Fan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cheng Fan, a3Jpc3R5ZmFuQGh1c3QuZWR1LmNu; Jinxiang Zhang, emhhbmdqaW54aWFuZ0BodXN0LmVkdS5jbg==; Chuansheng Zheng, aHF6Y3N4aEBzaW5hLmNvbQ==
 Quan Chen
Quan Chen Chaoqin Mao3
Chaoqin Mao3 Yang Luo
Yang Luo Chuansheng Zheng
Chuansheng Zheng Jinxiang Zhang
Jinxiang Zhang Cheng Fan
Cheng Fan