
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychol. , 11 March 2024
Sec. Neuropsychology
Volume 15 - 2024 | https://doi.org/10.3389/fpsyg.2024.1360057
This article is part of the Research Topic Visuospatial and Visuoconstructional Abilities and Disorders Across the Life Span View all 6 articles
 Pasquale Moretta1*
Pasquale Moretta1* Nicola Davide Cavallo2
Nicola Davide Cavallo2 Eleonora Fonzo2
Eleonora Fonzo2 Antonio Maiorino1
Antonio Maiorino1 Cesario Ferrante1
Cesario Ferrante1 Pasquale Ambrosino3
Pasquale Ambrosino3 Cinzia Femiano1
Cinzia Femiano1 Gabriella Santangelo2
Gabriella Santangelo2 Laura Marcuccio1
Laura Marcuccio1Vertical neglect represents a visuospatial deficit occurring as a possible consequence of acquired brain injury (ABI). Differently from unilateral spatial neglect on horizontal space, vertical neglect is poorly studied in the literature and rarely assessed in clinical practice. In the available studies, the terms “radial,” “vertical,” and “altitudinal” neglect are often used interchangeably, although they do not describe the same spatial dimension. “Altitudinal” and “vertical” refer to the sagittal plane, whereas “radial” refers to the transverse plane. The term “vertical” is sometimes used interchangeably with respect to both axes. The aim of this systematic review was to identify the main characteristics of vertical neglect after ABI, the diagnostic tools used, and the treatment options. We also proposed a clarification of the manifestations and characteristics of vertical and radial neglect. The 23 articles reviewed, showed that the vertical neglect occurred more frequently on the lower space than on the upper space, that its presence was associated with horizontal neglect, and that it could also occur with compromise of the radial space, with the near radial being more common. The most frequent etiology associated with vertical neglect is vascular, particularly ischaemic. The lesions side are very heterogeneous and include both cortical and subcortical areas and all lobes, although the temporal lobe is most affected. With regard to the assessment tools, paper and pencil tasks are the most commonly used diagnostic tools to identify vertical neglect, although in recent years the use of computer-based tasks increased. Taken together, our results suggest that vertical neglect may be underestimated in patients with right hemisphere lesions and should always be assessed, especially in cases where the patient shows signs of horizontal neglect. The clinical assessment of vertical neglect is very important since it can lead to important functional limitations in everyday life, such as poor wheelchair handling, stumbling over unnoticed obstacles located below (or above), walking down stairs, taking off shoes.
Unilateral Spatial Neglect (USN) is a common neurological syndrome in which patients fail to detect and respond to stimuli presented on the side of the body or the physical and imaginal space contralateral to the hemispheric lesion (Terruzzi et al., 2023); this deficit cannot be attributed to any elemental sensory or motor impairment. The estimated prevalence of USN after unilateral stroke is 30% and it is more common after right brain damage than after left (Esposito et al., 2021).
USN is a heterogeneous syndrome and may present itself in different ways: it may affect different sensory modalities (Van der Stoep et al., 2013), different spatial reference frames (i.e., egocentric vs. allocentric neglect; Buxbaum et al., 2004), and different regions of space (i.e., peri-personal or extra-personal neglect) or visual imagery (Bisiach and Luzzatti, 1978).
Although neglect may often be characterized by a spatial attentional bias in the horizontal dimension, attention may be oriented in three dimensions of space: horizontal, vertical, and radial (Mennemeier et al., 1992). Most studies of patients with USN focused on horizontal spatial dimension (left–right), with left USN being more frequent (43%) than right USN (19%; Osaki et al., 2022); nevertheless, USN may also occur in vertical (upper-lower) and radial (proximal-distal) spatial dimensions. Spatial bias is also described in healthy subjects who when bisecting vertical lines (intersection of the coronal and sagittal planes) demonstrate a slight upward, forward, and leftward bias (pseudo-neglect) (Chapin et al., 2022).
In addition, spatial neglect may occur in several different spatial reference frames, including head- and body-centered (egocentric), environmental-centered, and object-centered (allocentric) (Morris et al., 2020). The term egocentric neglect is used when a patient is inattentive or unaware of the stimuli that are on one side of his or her body or head. In contrast, allocentric neglect is the condition where a patient is inattentive or unaware of a part of an object or objects and this unawareness appears to be unrelated to the position of this object in relation to the patient’s head and body (Turgut et al., 2017).
Vertical neglect is rarely assessed in clinical practice and is little described in the scientific literature. It was first described by Bender and Teuber (1948), who reported two cases of patients who systematically placed the midpoint of vertically presented lines too high. A similar case of “altitudinal neglect” was later reported by Rapcsak et al. (1988), which is often considered the first article about vertical neglect (e.g., Kim et al., 2001; Hromas et al., 2020). From the available literature, it seems that the vertical bias in patients with ABI may concern both the lower part (Ergun-Marterer et al., 2001; Müri et al., 2009) and the upper part of the space (Shelton et al., 1990; Adair et al., 1995). One possible explanation for the bias in the vertical spatial dimension is that ventral occipitotemporal lesions could lead to upper vertical neglect and occipitoparietal lesions to lower vertical neglect (Halligan and Marshall, 1989; Mark and Heilman, 1997; Pitzalis et al., 1997).
Vertical neglect has often been described in combination with horizontal neglect, to the point that some authors suggested using the terms “diagonal neglect” or “quadrantic neglect” (Mark and Heilman, 1997; Osaki et al., 2022), and in co-occurrence with radial neglect.
Radial neglect (i.e., relative to the transverse plane) was first described by Shelton et al. (1990) and can be assessed both within peripersonal space (e.g., paper and pencil line bisection tasks) and between peripersonal and extrapersonal space.
Although the terms “radial,” “vertical,” and “altitudinal” neglect are often used interchangeably, they do not actually describe the same spatial dimension. “Altitudinal” and “vertical” refer to the sagittal plane, whereas “radial” refers to the transverse plane; however, “vertical” is sometimes used interchangeably concerning both axes (e.g., Halligan and Marshall, 1989, 1991). Confusion increases when radial tasks (e.g., bisecting a vertical line on a sheet of paper on the table, with the lines oriented along the intersection of the midsagittal plane of the viewer) are defined as vertical. This is not entirely incorrect, since a vertical line drawn on a piece of paper on the table can be used to measure the vertical allocentric dimension.
Thus, in these cases, the vertical direction assessed concerns the stimuli and not the subject’s point of view; it could be, therefore, defined as vertical-allocentric neglect, or radial-egocentric neglect (Figure 1).
The presence of vertical and radial spatial neglect is rarely assessed in patients with acquired brain injury (ABI); however, it is reasonable to assume that, as horizontal neglect, it may affect quality of life by predicting longer hospitalization and poorer outcomes in functional recovery (Terruzzi et al., 2023). Visual vertical neglect may also increase the risk of falling and, therefore, the probability of injuries and disabilities in these patients (Julayanont et al., 2019).
Within this context, the main aim of this systematic review is to provide a synthesis of the studies in the literature addressing visual vertical neglect in patients with ABI, with special reference to its clinical manifestations, and etiology and site of lesions.
Another possible aim of this paper is to clarify any differences and common points between vertical and radial neglect. Last, we also aim to suggest potential guidelines in the methods of assessment and treatment of patients with vertical neglect following an ABI.
This systematic review was registered in the PROSPERO International Prospective Register of Systematic Reviews, registration number CRD42023478713. It was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA, Moher et al., 2009).
The focus of this systematic review was to analyze the current literature on vertical spatial neglect in patients with acquired brain injury (ABI). Specifically, we aimed to identify clinical manifestations, assessments, and treatment options.
Peer-reviewed English studies were included if they met the following criteria: (i) patients with ABI (etiology traumatic or vascular or anoxic); we did not select patients with a particular etiology or hemispheric lesion; (ii) presence of vertical spatial neglect (we included patients with visual vertical neglect even if they had no horizontal neglect); (iii) patients over 18 years old; and (iv) specific neuropsychological assessments or treatment for visual vertical neglect were performed. Only studies on visual vertical neglect were eligible for inclusion. We included observational studies such as cross-sectional, case report, and case series studies.
We excluded studies that reported: (i) meta-analyses, reviews or overviews; (ii) book, comments, dissertations; (iii) patients with evidence of horizontal spatial neglect but no evidence of vertical neglect; (iv) vertical neglect due to non-acquired brain injury (e.g., dementia); and (v) not relevant studies to our aims (e.g., studies aimed to indagate verticality judgment but not vertical spatial neglect).
A systematic literature search was comprehensively conducted on 16 October 2023 in the PsycInfo (PROQUEST), PubMed, and Scopus databases. Search query utilized the term string: (vertical OR altitudinal) AND (neglect OR “unilateral visual inattention” OR hemi-inattention OR hemiagnosia OR hemineglect) AND (diagnosis OR rehabilitation OR treatment). No restrictions or filters were added.
To avoid multiple publication bias, the potential series overlap between studies was evaluated, and if there was overlap (studies referred to the same patients and outcomes), the most relevant study was chosen based on the most informative outcomes (e.g., both vertical and radial neglect), sample size, risk of bias, age of publication, choice of neuropsychological test (better if there was a validate tests).
Article screening (title, abstract, and full-text), data extraction, and quality evaluation were independently conducted by two investigators (NDC and EF) by using a double-blinded approach. Disagreements between reviewers were resolved by discussion. Rayyan software was used to record decisions (Ouzzani et al., 2016).
The extracted information included: (i) publication characteristics; (ii) sample characteristics; (iii) characteristics of vertical neglect (up/down) and associated manifestations (e.g., horizontal neglect, visual field deficit); (iv) injury characteristics (etiology, time post-onset, lesion type, and brain areas); (v) assessment modalities (i.e., paper-and-pencil or computer-based); and (vi) neuropsychological tests used to assess vertical neglect.
The critical appraisal of the methodological quality of the studies was performed using the appropriate Joanna Briggs Institute (JBI) checklist for each study design employed in the included articles (Moola et al., 2020). The JBI checklists for analytical cross-sectional, case series, and case report study designs were used. According to each study design, the checklist contained each assessment criterion (Supplementary material S1). Each criterion was given a rating of “yes,” “no,” “unclear” or “not applicable.” For cross-sectional and case report studies there are eight criteria, however, for case series are 10. No article was excluded on the basis of these assessments.
A total of 550 studies were identified after removing duplicates, and 133 met the criteria for full-text review. Thirty-eight articles were excluded for not reporting an ABI population (e.g., healthy population or dementia patients) or because the participants did not show neglect (e.g., ABI patients without neglect); 71 were excluded because they presented wrong outcomes (e.g., absence of vertical neglect) and 2 reported overlapped data. We included after full-text screening 23 studies (Figure 2).
The included studies are: 10 cross-sectional (Halligan and Marshall, 1989; Kageyama et al., 1994; Làdavas et al., 1994a,b; Pitzalis et al., 1997, 2001; Müri et al., 2009; Cazzoli et al., 2011; Moreh et al., 2014; Osaki et al., 2022); 10 case reports (Butter et al., 1989; Shelton et al., 1990; Halligan and Marshall, 1991; Mennemeier et al., 1992; Nichelli et al., 1993; Adair et al., 1995; Kori and Geldmacher, 1999; Ergun-Marterer et al., 2001; Morris et al., 2020; Numao et al., 2021); and 3 case series (Burnett-Stuart et al., 1991; Halligan and Marshall, 1993; Cappelletti et al., 2007). They were published between 1989 and 2022.
The quality assessment tool is designed to evaluate the risk to the target population, the recruitment procedures, the description of the subjects and the setting, the methods used for identification, the measurement of exposure, the condition and outcomes, and the appropriate analysis and treatment procedures. The methodological quality of the included studies is summarized in Table 1.
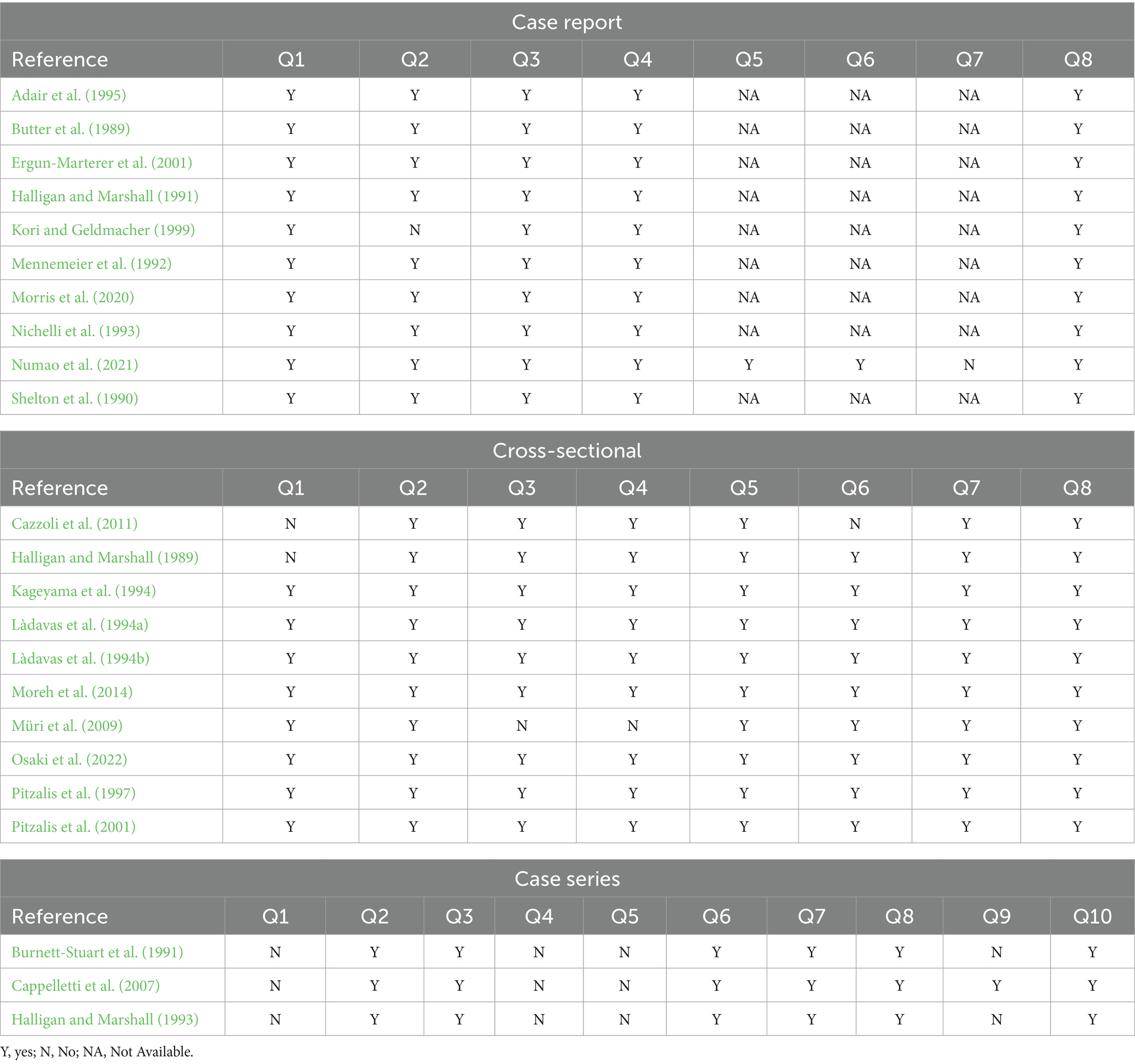
Table 1. JBI critical appraisal checklist for analytical case report, cross-sectional, and case series studies.
In total, 241 ABI participants were selected (mean age = 62.11 years, SD = 13.56 years; female n = 112, but we do not have data on the sex of 7 participants) and all of these reported significant impairment in the vertical dimension. The majority of these subjects (94.6% of the participants) showed lower vertical neglect although in 7 studies (Shelton et al., 1990; Burnett-Stuart et al., 1991; Halligan and Marshall, 1993; Kageyama et al., 1994; Adair et al., 1995; Kori and Geldmacher, 1999; Morris et al., 2020) were reported subjects with upper vertical neglect (5.4% of the participants).
All studies showed that horizontal neglect occurred together with vertical neglect except for two where the presence of horizontal neglect is not specified (Butter et al., 1989) or not significant (Adair et al., 1995). Horizontal neglect was always on the left except in two patients with right horizontal neglect (Pitzalis et al., 2001; Morris et al., 2020).
In addition, vertical neglect can also occur alongside radial neglect. In particular, we found a concomitance between lower vertical neglect and near radial neglect in 11 participants (Mennemeier et al., 1992; Kageyama et al., 1994; Ergun-Marterer et al., 2001; Pitzalis et al., 2001; Numao et al., 2021), and a co-occurrence of lower vertical neglect and far radial neglect in 3 participants (Kageyama et al., 1994; Pitzalis et al., 2001). Furthermore, upper vertical neglect can occur along with far radial neglect in 3 participants (Shelton et al., 1990; Kageyama et al., 1994; Adair et al., 1995), and with near radial neglect in only one (Kori and Geldmacher, 1999). Finally, Nichelli et al. (1993) described a case report involving a patient who showed lower and upper vertical neglect (the latter being less severe) associated with left horizontal neglect, left neglect dyslexia, and lower neglect dyslexia.
Finally, visual field deficits are described in 37 participants (Butter et al., 1989; Halligan and Marshall, 1989, 1991, 1993; Shelton et al., 1990; Burnett-Stuart et al., 1991; Nichelli et al., 1993; Kageyama et al., 1994; Kori and Geldmacher, 1999; Ergun-Marterer et al., 2001; Pitzalis et al., 2001; Cappelletti et al., 2007) and ocular motility deficits are present in 3 of them (Shelton et al., 1990; Mennemeier et al., 1992; Adair et al., 1995).
Demographic and clinical characteristics of participants are detailed in Table 2.
The majority of the selected studies reported patients with vascular etiology, except in two studies where the etiology was traumatic (Butter et al., 1989; Nichelli et al., 1993). The studies on non-vascular patients did not show different characteristics compared to the rest of the selected studies. The most represented vascular etiology was ischaemic (n = 32 participants) and the haemorrhagic pathology was described in 12 participants.
The time post-onset was very heterogeneous with a range from 3 days to 78.9 months (Table 2).
The vast majority of selected studies reported a unilateral right brain lesion that could affect either cortical or subcortical regions or both. The most represented is the right cortical lesion. Instead, only 4 studies (Butter et al., 1989; Shelton et al., 1990; Mennemeier et al., 1992; Adair et al., 1995) reported bilateral lesions, and one study (Pitzalis et al., 2001) described a patient with extensive left cortical lesion with right horizontal neglect. In addition, in only one study there is a lesion confined to subcortical regions (Numao et al., 2021).
However, in examining the selected studies that reported inclusion criteria for sample selection (i.e., cross-sectional and case series), we found that the majority of them used right brain lesions and vascular etiology as inclusion criteria (e.g., Làdavas et al., 1994a; Müri et al., 2009; Osaki et al., 2022). Only three studies included patients with both right- and left-brain injuries (Halligan and Marshall, 1989; Kageyama et al., 1994; Pitzalis et al., 2001).
The lesion sites were very heterogeneous in the selected articles, but the most representative lesions involved the temporal lobe, which was affected in 17 studies; the occipital lobe was affected in 13 studies, the parietal lobe in 13 studies, and the frontal lobe in 8 studies. Subcortical lesions mainly affected the basal ganglia, internal capsule, corona radiate, and thalamus.
Details on the characteristics of the injuries suffered by participants are shown in Table 2.
In the selected studies, vertical neglect was measured employing a wide variety of tools that can be grouped into three categories: paper-and-pencil, computer-based, and multimodal assessments.
Paper-and-pencil assessments consisted of tasks where the stimuli were on paper usually positioned 30 centimeters from the subject and comprised line bisection tasks, cancelation tasks, line drawing, copy of drawing, landmark, and point the center of figures tasks, and single word reading.
This method of assessing vertical neglect is the most representative among the selected studies and was used as the only method in 11 studies (Halligan and Marshall, 1989, 1991, 1993; Shelton et al., 1990; Burnett-Stuart et al., 1991; Nichelli et al., 1993; Kageyama et al., 1994; Adair et al., 1995; Pitzalis et al., 1997; Kori and Geldmacher, 1999; Morris et al., 2020) and in addition to multimodal assessment in 5 studies (Butter et al., 1989; Shelton et al., 1990; Mennemeier et al., 1992; Ergun-Marterer et al., 2001; Cappelletti et al., 2007) or computer-based assessment in 2 studies (Pitzalis et al., 1997; Osaki et al., 2022) (see Table 2). The description of the tests utilized is reported in Table 3, along with the corresponding study.
Computer-based assessments were utilized in 9 studies and consisted of tasks administered through a computer screen (Làdavas et al., 1994a,b; Pitzalis et al., 2001; Moreh et al., 2014; Osaki et al., 2022) or other technology such as an eye-tracker system (Müri et al., 2009; Cazzoli et al., 2011), virtual reality (Numao et al., 2021) or electrophysiological tests (Pitzalis et al., 1997). Table 3 provides a detailed description of the computer-based tests used in the selected studies.
Some selected studies used a multimodal assessment to measure vertical neglect, consisting of a visual and tactile/kinesthetic bisection task (Butter et al., 1989; Shelton et al., 1990; Mennemeier et al., 1992; Ergun-Marterer et al., 2001), or an auditory bisection task (Butter et al., 1989), or a mental number bisection task (Cappelletti et al., 2007) in addition to a paper-and-pencil task (e.g., bisection task). It was applied in 4 studies. A detailed description of the multimodal assessment tests that were used in the selected studies is given in Table 3.
In the reviewed studies, some paper-and-pencil tasks used to assess vertical neglect (e.g., line bisection or cancelation tasks) measured the vertical allocentric component of the stimuli, i.e., the radial component, taking the subject’s egocentric coordinates as reference. Specifically, 11 studies (Halligan and Marshall, 1989, 1991, 1993; Shelton et al., 1990; Burnett-Stuart et al., 1991; Nichelli et al., 1993; Kageyama et al., 1994; Pitzalis et al., 1997; Ergun-Marterer et al., 2001; Cappelletti et al., 2007; Morris et al., 2020; Osaki et al., 2022) utilized, solely or partially, paper-and-pencil tasks that assess the radial (vertical allocentric) neglect and not the vertical (up-down based on egocentric space) neglect. On the other hand, computer-based tasks always evaluate the vertical (egocentric) space (Table 2).
Finally, 8 selected studies (Shelton et al., 1990; Mennemeier et al., 1992; Kageyama et al., 1994; Adair et al., 1995; Kori and Geldmacher, 1999; Ergun-Marterer et al., 2001; Numao et al., 2021; Osaki et al., 2022) evaluated both vertical and radial dimensions and one of them reported results considering both dimensions together (Pitzalis et al., 2001).
Of the 22 studies reviewed, only one addressed the treatment of vertical neglect. Numao et al. (2021) developed a virtual reality-based method that randomly generates balloons in the left–right, up-down, and near-far space on a monitor using a head-mounted display. The patient’s task was to perceive these appearing balloons. This method was used to detect mild neglect that was not detected by conventional paper-and-pencil assessments and as a treatment for unilateral spatial neglect. After virtual reality (VR) treatment, the patient showed a reduction in the time taken to perceive the appearing balloons, especially in the upper left space, suggesting a possible therapeutic effect; however, there were poor improvements in the lower area.
To the best of our knowledge, this is the first review study that addressed vertical neglect, specifically the vertical neglect in ABI. We aimed to identify the main characteristics of vertical neglect after ABI, the diagnostic tools used, and the treatment options. We also proposed a clarification of the manifestations and characteristics of vertical and radial neglect.
In the 23 articles reviewed, we found that the lower space was more compromised than the upper space, that vertical neglect manifestations occurred together with horizontal neglect, and that they could also occur with compromise of the radial space, with the near radial being more common. The most frequent etiology is vascular, particularly ischaemic. The brain regions affected are very heterogeneous and include both cortical and subcortical areas and all lobes, although the temporal lobe is the most affected. Paper and pencil tasks are the most commonly used diagnostic tools to identify vertical neglect, although in recent years there has been an increase in the use of computer-based tasks (Moreh et al., 2014; Numao et al., 2021; Osaki et al., 2022). There is still limited experience in treating vertical neglect, and of the results that have been found, only one study deals with treatment (Numao et al., 2021).
The findings reported in this systematic review showing that inferior vertical space is more commonly impaired in ABI patients (Halligan and Marshall, 1989; Mennemeier et al., 1992; Pitzalis et al., 2001) but we also found deficits in upper vertical space.
Experimental and clinical evidence suggests the existence of separate neural systems involved in the distribution and manipulation of information along spatial dimensions.
Visual information from the retina is transmitted to the primary visual cortex in the occipital lobes. From here this pathway divides into two: a ventral pathway that runs within the temporal lobes; and a dorsal pathway that runs into the parietal lobes (Adair et al., 1995; Chieffi et al., 2018).
The ventral occipitotemporal pathway carries visual information from the inferior portion of the retina, which receives afferent information from the superior portion of the visual field, and the dorsal occipitoparietal pathway carries information from the superior portion of the retina, which receives information from the inferior portion of the visual field (Chieffi et al., 2018).
Studies in brain-damaged patients have suggested that the ventral occipitotemporal visual network mediates processing in upper visual space (Previc, 1990; Shelton et al., 1990; Adair et al., 1995; Drain and Reuter-Lorenz, 1996) and the dorsal occipitoparietal visual network mediates attention in lower visual space (Rapcsak et al., 1988; Drain and Reuter-Lorenz, 1996; Chieffi et al., 2017).
Drain and Reuter-Lorenz (1996) suggested that the two systems exert mutual inhibitory control over the orientation of attention. That is, occipitotemporal activity directing attention to upper space would override occipitoparietal activity directing attention to lower space. An injury to the occipitoparietal regions could lead to a simultaneous disinhibition of occipitotemporal activity and an upward orientation. Conversely, the occipitotemporal injury would result in the disinhibition of occipitoparietal activity and a downward orientation bias (Drain and Reuter-Lorenz, 1996).
The results of this systematic review show that the presence of occipitoparietal injury can lead to inferior space neglect (Rapcsak et al., 1988; Butter et al., 1989; Mennemeier et al., 1992), whereas occipitotemporal damage can lead to superior space neglect (Shelton et al., 1990; Adair et al., 1995; Morris et al., 2020). However, some participants showed inferior space neglect after a temporal lesion (Burnett-Stuart et al., 1991; Halligan and Marshall, 1991; Nichelli et al., 1993; Pitzalis et al., 2001; Cappelletti et al., 2007) and superior space neglect after a parietal lesion (Burnett-Stuart et al., 1991; Halligan and Marshall, 1993).
The attentional functions of these association areas of the parietal cortex depend on input from several other areas of the brain (Heilman et al., 2000). Therefore, a lesion in the subcortical white matter below the parietal and temporal lobes could affect attentional functions related to the ventral and dorsal pathways.
Another possible explanation lies in the lateralization of the lesion. Some evidence of neglect, manifested by a spatial attentional bias, may be caused by a reduction in attention to the contralesional hemispace by the injured hemisphere (Mesulam, 1981), or by disinhibition of the opposite non-injured hemisphere and an increase in the distribution of attention to ipsilesional space (Kinsbourne, 1993). As in the case of horizontal neglect in which each hemisphere primarily attends to the contralateral egocentric hemispace, it may be possible that while the left hemisphere mediates attention toward the body and downward, and the right hemisphere away from the body and upward (Heilman et al., 1995; Morris et al., 2020).
Many left-hemisphere-mediated visual activities, such as reading and writing, are performed below eye level, in lower space. In contrast, many right-hemisphere-mediated visual tasks, such as face recognition or orientation, are performed above eye level, in upper space.
Furthermore, from an evolutionary point of view, the lower visual field is more closely associated with peripersonal space, where the hands interact with objects, tools, and food, whereas the upper visual field is more closely associated with extrapersonal space, where stimuli are distant and high precision of visual movement performance is not required (Previc, 1990).
Therefore, a possible right hemispheric dominance may mediate spatial attention and be responsible for the upward bias (Morris et al., 2020) but it does not explain the downward neglect shown by patients. Further studies are required to investigate the role of each hemisphere in vertical neglect and to determine the laterality and precise location of lesions.
We found that vertical bias may occur in conjunction with a deficit in radial space, according to the findings of this systematic review and previously reported in the literature (Chieffi et al., 2019; Julayanont et al., 2019; Pisanuwongrak et al., 2020). The vertical and radial tasks (e.g., line bisection tasks) may overlap in part; indeed, a classic pencil-and-paper line bisection task, where participants are asked to mark the center of a line placed on a sheet of paper about 30 cm from the participant, could be either a radial egocentric (head-or-body-centered coordinate) or a vertical allocentric (object-centered coordinate) task. Several studies selected in this systematic review (Halligan and Marshall, 1989, 1991, 1993; Nichelli et al., 1993; Kageyama et al., 1994; Pitzalis et al., 1997; Ergun-Marterer et al., 2001; Osaki et al., 2022) use paper-and-pencil tasks and thus measure the egocentric radial/allocentric vertical dimension. Furthermore, when people perform the radial line bisection task, in addition to moving their eyes downward, they often flex their necks and thus a radial line, at least in part, might be perceived as a vertical line. For this reason, there might have been significant differences in the way in which the images of the central and lateral lines were projected onto the retina. In addition, when the radial line is positioned along the midsagittal plane, the gaze crosses the line perpendicularly, and the image of the distal part is projected onto the inferior retina field, which then projects to the occipitotemporal ventral visual attention stream. In contrast, the image of the proximal portion is projected onto the superior retina field, and this portion of the retina projects to the occipitoparietal dorsal visual attentional stream.
Instead, in the bisection of the vertical line, the upper part of the line projects to the inferior retina and is transmitted to the ventral attentional pathway, while the lower part projects to the superior retina and is transmitted to the dorsal pathway. Thus, both retinotopic and spatiotopic factors may have contributed to the vertical and distal bias. Support for this hypothesis comes from the work of Geldmacher and Heilman (1994) who found that when healthy subjects are asked to bisect lines below eye level, they deviate distally. However, this radial deviation is not observed when these radial lines are placed above eye level.
Previous studies on patients with ABI (Rapcsak et al., 1988; Butter et al., 1989; Shelton et al., 1990; Mennemeier et al., 1992; Adair et al., 1995) have suggested that the occipitoparietal stream directs attention to near space, whereas the occipitotemporal stream directs attention to far space. Therefore, an occipitoparietal brain lesion can distort attentional orientation toward far and upper space, and an occipitotemporal brain lesion can produce a distortion toward near and lower space.
Contrary to some findings in the literature (Mennemeier et al., 1992; Mark and Heilman, 1997; Chieffi et al., 2019; Pisanuwongrak et al., 2020), which suggest a possible overlap of neural networks important for mediating attention in proximal/inferior and distal/superior space, we have found that near/lower and far/upper do not always co-occur. Indeed, the presence of manifestations of lower neglect and deficit for both far (Kageyama et al., 1994; Pitzalis et al., 2001) and near (Mennemeier et al., 1992; Kageyama et al., 1994; Ergun-Marterer et al., 2001; Pitzalis et al., 2001; Numao et al., 2021) space, and of upper neglect and deficit for both far (Shelton et al., 1990; Kageyama et al., 1994; Adair et al., 1995) and near space (Kori and Geldmacher, 1999) suggests that processing of vertical and radial space may be partially independent.
In addition, our results show that horizontal neglect almost always co-occurs with vertical neglect. This evidence might suggest considerable overlap in the mechanisms controlling vertical and horizontal spatial processing, but several studies, that have examined leftward and upward biases in the same participants (Shelton et al., 1990; Halligan and Marshall, 1991, 1993; Kageyama et al., 1994; Adair et al., 1995; Pitzalis et al., 2001), have shown that there is no reliable correlation between the extent of the biases in each of the dimensions (Nicholls et al., 2004), suggesting the existence of co-occurring but distinct constructs.
Therefore, our results, together with the available evidence, support the view that horizontal, vertical, and radial spatial asymmetries may be driven by only partially independent cognitive and neural mechanisms.
We also observed that some patients in selected studies had visual field defects in addition to vertical neglect. Patients with vertical visual field defects (altitudinal hemianopia), but without manifestations of neglect, in vertical line or bar bisection tasks, tend to place their midline (or bisection) toward the blind field (Kerkhoff, 1993). Contrarily individuals with vertical neglect position their midline away from the neglected field. Given that cancelation tasks are frequently utilized to evaluate vertical neglect, it is crucial to recognize that vertical field defects can produce an opposing effect. Additionally, individuals with oblique visual field defects (quadrantanopia) similarly demonstrate an oblique shift of their bisection or straight ahead into the blind quadrant (Kuhn et al., 2010).
From this systematic review, it emerges that the most used tools to assess vertical neglect are paper-and-pencil tests and in particular line bisection and cancelation tasks. We found also experience with computer-based or VR assessment. As mentioned previously, the nature of the tasks can influence both the behavioral measure and the spatial dimension explored.
The line bisection task is a perceptual-motor task, which mainly involves allocentric coordinates and is therefore mediated by the occipitotemporal system (Chieffi et al., 2017). It primarily involves magnitude estimates that are affected by attentional bias (Lee et al., 2004). Although sensory-attentional bias most often influences performance on the line bisection test, this test requires eye and hand movements; therefore, it may also reveal action-intentional biases. In contrast, cancelation tests require a systematic visual search and require greater levels of exploration, attentional focusing, attentional disengagement, and sustained vigilance compared to the line bisection task (Lee et al., 2004). These activities are primarily mediated by frontal lobes but an injury to the temporal or parietal lobe can reveal impairment in the cancelation task as well as in the bisection lines task (Morris et al., 2020).
Unlike paper-and-pencil tasks, computer-based tasks primarily assess vertical (egocentric) space because the direction of the stimulus to be processed usually coincides with the up-down body-centered spatial frames. In this way, the upper part of the stimulus is transmitted to the ventral visual pathway and the lower part to the dorsal visual pathway.
Finally, the VR method used by Numao et al. (2021) is a promising tool capable of evaluating the different spatial coordinates together and maintaining a certain ecological value. In addition, VR could facilitate the identification of spatial bias in patients with ABI (Numao et al., 2021). Taking into account horizontal, radial, and vertical coordinates, it not only aids in the detection of neglect but also shows potential therapeutic effects in its treatment.
To our knowledge, this is the only study that aims to rehabilitate vertical neglect and the only one that uses virtual reality as a diagnostic and rehabilitative tool in vertical neglect. However, Numao et al. (2021) results must be interpreted critically. They found an improvement in reaction time to the balloon search task. After treatment, awareness in the left space, especially in the upper left, was significantly improved but this awareness was poor in the lower area. This latter result may be due to the authors setting the tilt angle to 10° from the initial position, which may have affected awareness in the lower left space. In addition, the reported improvements could also be due to an iterative learning effect, as the treatment was based on repeated searching for the balloons. Furthermore, this is a case report without a control group and a possible effect of spontaneous remission cannot be excluded. Finally, changes in reaction times measured in this study may not be related to vertical neglect (Hurford et al., 2013). These promising findings should be approached with caution, and additional studies are warranted to validate these preliminary results.
In the last decades, different VR-based protocols have been proposed for the rehabilitation and assessment of neglect. VR may be an innovative and potentially powerful tool, to be used in conjunction with, or as an alternative to, those already widely used in clinical and rehabilitation practice of patients with ABI with USN regardless of the immersion level (Bohil et al., 2011; Pedroli et al., 2015; Salatino et al., 2023).
However, VR is not the only possible therapeutic tool for the treatment of vertical neglect. Treatments that can benefit the clinical manifestations of neglect in the horizontal dimension, such as non-invasive brain stimulation (Kashiwagi et al., 2018; Yang et al., 2023) or visual scanning training (Gammeri et al., 2020), could be promising tools to also improve vertical symptoms.
To date, traditional paper-and-pencil tests may be inadequate for detecting USN symptoms (Rengachary et al., 2009). In fact, paper-and-pencil tools use static, two-dimensional stimuli that are very different from those of a real or virtual environment (i.e., they are not ecological).
Paper-and-pencil tasks typically require a simple visual search in near space and only allow the diagnosis of peripersonal USN (Kim et al., 2010; Aravind and Lamontagne, 2014), whereas neglect can instead present two subtypes, peripersonal and extrapersonal, which can be dissociated (Halligan et al., 2003).
Instead, everyday life requires dynamic responses to relevant stimuli in both personal and extrapersonal space, which change every time (Kim et al., 2010). With VR, it is possible to recreate this dynamism and build more ecological tasks.
Contrary to paper-and-pencil, in computer-based tasks different reaction time gradients have been observed for both static and moving stimuli (Cazzoli et al., 2011), with a progression from the ipsilesional field toward the midline and in the contralesional field (Dvorkin et al., 2007).
Thus, computer-based tasks are generally more sensitive than paper-and-pencil tests (Rengachary et al., 2009; Bonato et al., 2012).
Therefore, from the evidence presented in this study, computerized and VR-based tests could be a valid alternative to traditional paper-and-pencil tasks in the assessment of USN. These new tools could overcome the radial-egocentric and vertical-allocentric problems present in some paper-and-pencil tasks, making the assessment more sensitive to deficits and more ecological.
Furthermore, in the case of VR, they could facilitate the detection of deficits for each spatial dimension simultaneously and promote the study of vertical coordinates, which are usually little studied.
This systematic review has some limitations that must be considered.
The first limitation concerns a bias in the selection of the studies. We selected the studies that concern visual vertical neglect in ABI; in some of these (e.g., Kageyama et al., 1994 or Pitzalis et al., 2001), we selected only the patients with signs of vertical neglect. There might be a bias in the selection of studies and patients, which does not allow us to make strong inferences about the relationship between vertical neglect and other neglect types, different lesion territories, or aetiologies. Moreover, most of the selected studies reported right brain injury and/or vascular etiology as inclusion criteria for patient selection. Therefore, it is difficult to make statements about the prevalence of vertical neglect among different aetiologies and lesion sites. However, we described what we observed, that is the co-occurrence of visual vertical neglect following ABI. Future review studies should investigate the phenomenon of vertical neglect more extensively, also including patients with other types of neglect who do not show signs of vertical neglect.
The second limitation involves potential functional deficits in vertical neglect. Given that the vast majority of included patients have both horizontal and vertical neglect, we cannot exclude that is the horizontal neglect which may lead to a functional deficit in everyday life. Conversely, we cannot exclude that it is the weight of vertical neglect that leads to a functional deficit in daily life. More likely, the presence of both, vertical and horizontal neglect, leads to greater functional deficits.
Third, we selected several single-case studies that are particularly effective in detecting peculiar patterns of performances, but the results of which must be taken with particular caution. Therefore, these studies may reduce the overall quality of the studies analyzed.
Fourth patients may omit targets in the lower quadrants in cancelation tasks because they are fatigued but in the included studies, we could not control this possibility. However, some studies demonstrated that fatigue could not affect vertical bias in cancelation task (Robertson and North, 1993; Mark and Heilman, 1997).
A further limitation identified in all studies, except one (Numao et al., 2021) concerns the lack of rehabilitation for vertical neglect.
Moreover, some studies may not have been identified with the search strategy we used. This could be due both to the heterogeneity of the names indicating neglect syndrome and to the fact that some studies could report vertical biases described as radial.
Lastly, it should be noted that comparison between studies may be biased by the heterogeneity of patients with ABI and brain lesions, the variability of clinical manifestations, the small sample size of most studies, and the year of publication, which reflects the differences in terminology regarding vertical bias (e.g., altitudinal) and in the progress in the use of different tools for assessment (computerized devices and VR). Although there was heterogeneity, the results were relatively consistent, suggesting that vertical bias is a manifestation of USN that should be taken into account.
Future studies should focus on the presence of vertical neglect after ABI trying to identify specific patterns of clinical manifestation, resolving the possible role of cerebral hemispheres and lesion sites in the verticality bias. Furthermore, the possible relationship between vertical neglect and functional impairment in everyday life should be investigated with greater systematic rigor.
Vertical neglect is poorly studied in the literature and rarely assessed in clinical practice. Our results suggest that vertical neglect may be underestimated in patients with right hemisphere lesions and should always be assessed, especially in cases where the patient shows signs of horizontal neglect. Furthermore, vertical neglect can lead to important functional limitations in everyday life, such as poor wheelchair handling, stumbling over unnoticed obstacles located below (or above), walking downstairs, and taking off shoes. However, assessing vertical dimensions with paper and pencil, computer-based and VR tasks could help ABI patients to take fewer risks and pay more attention to the neglected space, and could guide the clinician toward more personalized and decisive therapies.
Based on this review it may be important to test for neglect in all three body-cantered directions horizontal, vertical, and, radial.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
PM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. NC: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft. EF: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft. AM: Data curation, Validation, Visualization, Writing – review & editing. CeF: Data curation, Validation, Visualization, Writing – review & editing. PA: Formal analysis, Supervision, Validation, Visualization, Writing – review & editing. CiF: Conceptualization, Data curation, Formal analysis, Validation, Visualization, Writing – review & editing. GS: Formal analysis, Supervision, Validation, Visualization, Writing – review & editing. LM: Conceptualization, Formal analysis, Supervision, Validation, Visualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was partially supported by the “Ricerca Corrente” funding scheme of the Ministry of Health, Italy. The authors report no involvement in the research by the sponsor that could have influenced the outcome of this work.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1360057/full#supplementary-material
Adair, J. C., Williamson, D. J., Jacobs, D. H., Na, D. L., and Heilman, K. M. (1995). Neglect of radial and vertical space: importance of the retinotopic reference frame. J. Neurol. Neurosurg. Psychiatry 58, 724–728. doi: 10.1136/jnnp.58.6.724
Aravind, G., and Lamontagne, A. (2014). Perceptual and locomotor factors affect obstacle avoidance in persons with visuospatial neglect. J. Neuroeng. Rehabil. 11:38. doi: 10.1186/1743-0003-11-38
Bender, M. B., and Teuber, H. L. (1948). Spatial organization of visual perception following injury to the brain. Arch. Neurol. Psychiatr. 59, 39–62. doi: 10.1001/archneurpsyc.1948.02300360049004
Bisiach, E., and Luzzatti, C. (1978). Unilateral neglect of representational space. Cortex 14, 129–133. doi: 10.1016/S0010-9452(78)80016-1
Bohil, C. J., Alicea, B., and Biocca, F. A. (2011). Virtual reality in neuroscience research and therapy. Nat. Rev. Neurosci. 12, 752–762. doi: 10.1038/nrn3122
Bonato, M., Priftis, K., Marenzi, R., Umiltà, C., and Zorzi, M. (2012). Deficits of contralesional awareness: a case study on what paper-and-pencil tests neglect. Neuropsychology 26, 20–36. doi: 10.1037/a0025306
Burnett-Stuart, G., Halligan, P. W., and Marshall, J. C. (1991). A Newtonian model of perceptual distortion in visuo-spatial neglect. Neuroreport 2, 255–257. doi: 10.1097/00001756-199105000-00010
Butter, C. M., Evans, J., Kirsch, N., and Kewman, D. (1989). Altitudinal neglect following traumatic brain injury: a case report. Cortex 25, 135–146. doi: 10.1016/S0010-9452(89)80013-9
Buxbaum, L. J., Ferraro, M. K., Veramonti, T., Farne, A., Whyte, J., Ladavas, E., et al. (2004). Hemispatial neglect. Neurology 62, 749–756. doi: 10.1212/01.WNL.0000113730.73031.F4
Cappelletti, M., Freeman, E. D., and Cipolotti, L. (2007). The middle house or the middle floor: bisecting horizontal and vertical mental number lines in neglect. Neuropsychologia 45, 2989–3000. doi: 10.1016/j.neuropsychologia.2007.05.014
Cazzoli, D., Nyffeler, T., Hess, C. W., and Müri, R. M. (2011). Vertical bias in neglect: a question of time? Neuropsychologia 49, 2369–2374. doi: 10.1016/j.neuropsychologia.2011.04.010
Chapin, B. A., Pisanuwongrak, K., Williamson, J. B., and Heilman, K. M. (2022). Vertical pseudoneglect: sensory-attentional versus action-intentional. J. Clin. Exp. Neuropsychol. 44, 163–170. doi: 10.1080/13803395.2022.2098934
Chieffi, S., Castaldi, C., Di Maio, G., La Marra, M., Messina, A., Monda, V., et al. (2019). Attentional bias in the radial and vertical dimensions of space. C. R. Biol. 342, 97–100. doi: 10.1016/j.crvi.2019.03.003
Chieffi, S., Messina, G., Messina, A., Villano, I., Monda, V., Ambra, F. I., et al. (2017). Memory for spatial locations in a patient with near space neglect and optic ataxia: involvement of the occipitotemporal stream. Front. Neurol. 8:231. doi: 10.3389/fneur.2017.00231
Chieffi, S., Messina, G., Villano, I., Messina, A., Ilardi, C. R., Monda, M., et al. (2018). Hemispheric asymmetries in radial line bisection: role of retinotopic and spatiotopic factors. Front. Psychol. 9:2200. doi: 10.3389/fpsyg.2018.02200
Drain, M., and Reuter-Lorenz, P. A. (1996). Vertical orienting control: evidence for attentional bias and “neglect” in the intact brain. J. Exp. Psychol. Gen. 125, 139–158. doi: 10.1037/0096-3445.125.2.139
Dvorkin, A. Y., Rymer, W. Z., Settle, K., and Patton, J. L. (2007). Perceptual assessment of spatial neglect within a virtual environment. In 2007 Virtual Rehabilitation. 175–179. IEEE.
Ergun-Marterer, A., Ergun, E., Mentes, M., and Oder, W. (2001). Altitudinal neglect in a patient with occipital infarction. Brain Inj. 15, 363–370. doi: 10.1080/02699050010004644
Esposito, E., Shekhtman, G., and Chen, P. (2021). Prevalence of spatial neglect post-stroke: a systematic review. Ann. Phys. Rehabil. Med. 64:101459. doi: 10.1016/j.rehab.2020.10.010
Gammeri, R., Iacono, C., Ricci, R., and Salatino, A. (2020). Unilateral spatial neglect after stroke: current insights. Neuropsychiatr. Dis. Treat. 16, 131–152. doi: 10.2147/NDT.S171461
Geldmacher, D. S., and Heilman, K. M. (1994). Visual field influence on radial line bisection. Brain Cogn. 26, 65–72. doi: 10.1006/brcg.1994.1042
Halligan, P. W., Fink, G. R., Marshall, J. C., and Vallar, G. (2003). Spatial cognition: evidence from visual neglect. Trends Cogn. Sci. 7, 125–133. doi: 10.1016/S1364-6613(03)00032-9
Halligan, P. W., and Marshall, J. C. (1989). Is neglect (only) lateral? A quadrant analysis of line cancellation. J. Clin. Exp. Neuropsychol. 11, 793–798. doi: 10.1080/01688638908400936
Halligan, P. W., and Marshall, J. C. (1991). Figural modulation of visuo-spatial neglect: a case study. Neuropsychologia 29, 619–628. doi: 10.1016/0028-3932(91)90097-R
Halligan, P. W., and Marshall, J. C. (1993). The bisection of horizontal and radial lines: a case study of normal controls and ten patients with left visuospatial neglect. Int. J. Neurosci. 70, 149–167. doi: 10.3109/00207459309000571
Heilman, K. M., Chatterjee, A., and Doty, L. C. (1995). Hemispheric asymmetries of near-far spatial attention. Neuropsychology 9, 58–61. doi: 10.1037/0894-4105.9.1.58
Heilman, K. M., Valenstein, E., and Watson, R. T. (2000). Neglect and related disorders. Semin. Neurol. 20, 463–470. doi: 10.1055/s-2000-13179
Hromas, G., Polejaeva, E., Sozda, C. N., Heilman, K. M., Schmalfuss, I. M., and Perlstein, W. M. (2020). The influence of traumatic brain injury on the allocation of vertical spatial attention. J. Clin. Exp. Neuropsychol. 42, 101–110. doi: 10.1080/13803395.2019.1685650
Hurford, R., Charidimou, A., Fox, Z., Cipolotti, L., and Werring, D. J. (2013). Domain-specific trends in cognitive impairment after acute ischaemic stroke. J. Neurol. 260, 237–241. doi: 10.1007/s00415-012-6625-0
Julayanont, P., Burks, D. W., and Heilman, K. M. (2019). Vertical and radial attentional neglect in corticobasal syndrome. Cogn. Behav. Neurol. 32, 208–213. doi: 10.1097/WNN.0000000000000204
Kageyama, S., Imagase, M., Okubo, M., and Takayama, Y. (1994). Neglect in three dimensions. Am. J. Occup. Ther. 48, 206–210. doi: 10.5014/ajot.48.3.206
Kashiwagi, F. T., El Dib, R., Gomaa, H., Gawish, N., Suzumura, E. A., da Silva, T. R., et al. (2018). Noninvasive brain stimulations for unilateral spatial neglect after stroke: a systematic review and meta-analysis of randomized and nonrandomized controlled trials. Neural Plast. 2018, 1638763–1638725. doi: 10.1155/2018/1638763
Kerkhoff, G. (1993). Displacement of the egocentric visual midline in altitudinal postchiasmatic scotomata. Neuropsychologia 31, 261–265. doi: 10.1016/0028-3932(93)90090-m
Kim, D. Y., Ku, J., Chang, W. H., Park, T. H., Lim, J. Y., Han, K., et al. (2010). Assessment of post-stroke extrapersonal neglect using a three-dimensional immersive virtual street crossing program. Acta Neurol. Scand. 121, 171–177. doi: 10.1111/j.1600-0404.2009.01194.x
Kim, G.-M., Yoon, S. J., Hyang Jeong, J., and Na, D. L. (2001). Neglect in radial and vertical axes after a unilateral left temporo-occipital lesion. Eur. Neurol. 46, 96–98. doi: 10.1159/000050771
Kinsbourne, M. (1993). “Orientation bias model of unilateral neglect: evidence from attentional gradients within hemispace” in Unilareral neglect: clinical and experimental studies. eds. I. H. Robertson and J. C. Marshall (Hillsdale, NJ: Lawrence Erlbaurn Associates Inc.)
Kori, A., and Geldmacher, D. S. (1999). Three-dimensional neglect phenomena following right anterior choroidal artery infarction. J. Int. Neuropsychol. Soc. 5, 567–571. doi: 10.1017/S1355617799566113
Kuhn, C., Heywood, C. A., and Kerkhoff, G. (2010). Oblique spatial shifts of subjective visual straight ahead orientation in quadrantic visual field defects. Neuropsychologia 48, 3205–3210. doi: 10.1016/j.neuropsychologia.2010.06.035
Làdavas, E., Carletti, M., and Gori, G. (1994a). Automatic and voluntary orienting of attention in patients with visual neglect: horizontal and vertical dimensions. Neuropsychologia 32, 1195–1208. doi: 10.1016/0028-3932(94)90102-3
Làdavas, E., Farnè, A., Carletti, M., and Zeloni, G. (1994b). Neglect determined by the relative location of responses. Brain 117, 705–714. doi: 10.1093/brain/117.4.705
Lee, B. H., Kang, S. J., Park, J. M., Son, Y., Lee, K. H., Adair, J. C., et al. (2004). The character-line bisection task: a new test for hemispatial neglect. Neuropsychologia 42, 1715–1724. doi: 10.1016/j.neuropsychologia.2004.02.015
Mark, V. W., and Heilman, K. M. (1997). Diagonal neglect on cancellation. Neuropsychologia 35, 1425–1436. doi: 10.1016/S0028-3932(97)00067-5
Mennemeier, M., Wertman, E., and Heilman, K. M. (1992). Neglect of near peripersonal space. Evidence for multidirectional attentional systems in humans. Brain 115, 37–50. doi: 10.1093/brain/115.1.37
Mesulam, M. M. (1981). A cortical network for directed attention and unilateral neglect. Ann. Neurol. 10, 309–325. doi: 10.1002/ana.410100402
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6:e1000097. doi: 10.1371/journal.pmed.1000097
Moola, S., Munn, Z., Tufanaru, C., Aromataris, E., Sears, K., Sfetcu, R., et al. (2020). Chapter 7: Systematic reviews of etiology and risk in Joanna Briggs Institute Reviewer’s Manual. eds. E. Aromataris and Z. Munn The Joanna Briggs Institute, 2017. Available at: https://reviewersmanual.joannabriggs.org/
Moreh, E., Malkinson, T. S., Zohary, E., and Soroker, N. (2014). Visual memory in unilateral spatial neglect: immediate recall versus delayed recognition. J. Cogn. Neurosci. 26, 2155–2170. doi: 10.1162/jocn_a_00603
Morris, M., Mańkowska, A., and Heilman, K. M. (2020). Upper vertical spatial neglect with a right temporal lobe stroke. Cogn. Behav. Neurol. 33, 63–66. doi: 10.1097/WNN.0000000000000221
Müri, R. M., Cazzoli, D., Nyffeler, T., and Pflugshaupt, T. (2009). Visual exploration pattern in hemineglect. Psychol. Res. 73, 147–157. doi: 10.1007/s00426-008-0204-0
Nichelli, P., Venneri, A., Pentore, R., and Cubelli, R. (1993). Horizontal and vertical neglect dyslexia. Brain Lang. 44, 264–283. doi: 10.1006/brln.1993.1018
Nicholls, M. E. R., Mattingley, J. B., Berberovic, N., Smith, A., and Bradshaw, J. L. (2004). An investigation of the relationship between free-viewing perceptual asymmetries for vertical and horizontal stimuli. Cogn. Brain Res. 19, 289–301. doi: 10.1016/j.cogbrainres.2003.12.008
Numao, T., Amimoto, K., and Shimada, T. (2021). Examination and treatment of unilateral spatial neglect using virtual reality in three-dimensional space. Neurocase 27, 447–451. doi: 10.1080/13554794.2021.1999478
Osaki, S., Amimoto, K., Miyazaki, Y., Tanabe, J., and Yoshihiro, N. (2022). Reaction time analysis in patients with mild left unilateral spatial neglect employing the modified Posner task: vertical and horizontal dimensions. Exp. Brain Res. 240, 2143–2153. doi: 10.1007/s00221-022-06400-z
Ouzzani, M., Hammady, H., Fedorowicz, Z., and Elmagarmid, A. (2016). Rayyan—a web and mobile app for systematic reviews. Syst. Rev. 5:210. doi: 10.1186/s13643-016-0384-4
Pedroli, E., Serino, S., Cipresso, P., Pallavicini, F., and Riva, G. (2015). Assessment and rehabilitation of neglect using virtual reality: a systematic review. Front. Behav. Neurosci. 9:226. doi: 10.3389/fnbeh.2015.00226
Pisanuwongrak, K., Julayanont, P., and Heilman, K. M. (2020). Degenerative dementia with proximal radial and lower vertical spatial neglect. Neurocase 26, 183–187. doi: 10.1080/13554794.2020.1769138
Pitzalis, S., Di Russo, F., Spinelli, D., and Zoccolotti, P. (2001). Influence of the radial and vertical dimensions on lateral neglect. Exp. Brain Res. 136, 281–294. doi: 10.1007/s002210000580
Pitzalis, S., Spinelli, D., and Zoccolotti, P. (1997). Vertical neglect: behavioral and electrophysiological data. Cortex 33, 679–688. doi: 10.1016/S0010-9452(08)70725-1
Previc, F. H. (1990). Functional specialization in the lower and upper visual fields in humans: its ecological origins and neurophysiological implications. Behav. Brain Sci. 13, 519–542. doi: 10.1017/S0140525X00080018
Rapcsak, S. Z., Cimino, C. R., and Heilman, K. M. (1988). Altitudinal neglect. Neurology 38:277. doi: 10.1212/WNL.38.2.277
Rengachary, J., d’Avossa, G., Sapir, A., Shulman, G. L., and Corbetta, M. (2009). Is the posner reaction time test more accurate than clinical tests in detecting left neglect in acute and chronic stroke? Arch. Phys. Med. Rehabil. 90, 2081–2088. doi: 10.1016/j.apmr.2009.07.014
Robertson, I. H., and North, N. (1993). Fatigue versus disengagement in unilateral neglect. J. Neurol. Neurosurg. Psychiatry 56, 717–719. doi: 10.1136/jnnp.56.6.717
Salatino, A., Zavattaro, C., Gammeri, R., Cirillo, E., Piatti, M. L., Pyasik, M., et al. (2023). Virtual reality rehabilitation for unilateral spatial neglect: a systematic review of immersive, semi-immersive and non-immersive techniques. Neurosci. Biobehav. Rev. 152:105248. doi: 10.1016/j.neubiorev.2023.105248
Shelton, P. A., Bowers, D., and Heilman, K. M. (1990). Peripersonal and vertical neglect. Brain 113, 191–205. doi: 10.1093/brain/113.1.191
Terruzzi, S., Albini, F., Massetti, G., Etzi, R., Gallace, A., and Vallar, G. (2023). The neuropsychological assessment of unilateral spatial neglect through computerized and virtual reality tools: a scoping review. Neuropsychol. Rev., 1–39. doi: 10.1007/s11065-023-09586-3
Turgut, N., Mödden, C., Brumund, T., Eling, P., and Hildebrandt, H. (2017). A study on the independence of egocentric and allocentric neglect. Cortex 96, 95–104. doi: 10.1016/j.cortex.2017.09.005
Van der Stoep, N., Visser-Meily, J. M. A., Kappelle, L. J., de Kort, P. L. M., Huisman, K. D., Eijsackers, A. L. H., et al. (2013). Exploring near and far regions of space: distance-specific visuospatial neglect after stroke. J. Clin. Exp. Neuropsychol. 35, 799–811. doi: 10.1080/13803395.2013.824555
Yang, F. A., Lin, C. L., Cho, S. Y., Chou, I. L., Han, T. I., and Yang, P. Y. (2023). Short- and long-term effects of repetitive transcranial magnetic stimulation on poststroke visuospatial neglect: a systematic review and meta-analysis of randomized controlled trials. Am. J. Phys. Med. Rehabil. 102, 522–532. doi: 10.1097/PHM.0000000000002151
Keywords: visual vertical neglect, visuospatial disorders, acquired brain injury, rehabilitation, clinical neuropsychology
Citation: Moretta P, Cavallo ND, Fonzo E, Maiorino A, Ferrante C, Ambrosino P, Femiano C, Santangelo G and Marcuccio L (2024) Visual vertical neglect in acquired brain injury: a systematic review. Front. Psychol. 15:1360057. doi: 10.3389/fpsyg.2024.1360057
Received: 22 December 2023; Accepted: 28 February 2024;
Published: 11 March 2024.
Edited by:
Irene Cristina Mammarella, University of Padua, ItalyReviewed by:
Michele Allegra, Dipartimento di Fisica e Astronomia “G. Galilei”, ItalyCopyright © 2024 Moretta, Cavallo, Fonzo, Maiorino, Ferrante, Ambrosino, Femiano, Santangelo and Marcuccio. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pasquale Moretta, cGFzcXVhbGUubW9yZXR0YUBpY3NtYXVnZXJpLml0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.