- 1Occupational Health and Medicine Department-CRPPE Hospices Civils de Lyon, Lyon, France
- 2Univ Lyon, University Lyon 1 Transport Work and Environmental Epidemiology Research and Surveillance Unit – UMRESTTE (UMR T9405), Lyon, France
- 3Service de Santé Universitaire, University Claude Bernard Lyon, Lyon, France
- 4University Claude Bernard Lyon 1, Lyon, France
- 5Department of Radiotherapy, Léon Bérard Cancer Center, Lyon, France
- 6Direction Qualité Usagers et Santé Populationnelle, Hospices Civils de Lyon, Lyon, France
- 7Research On Healthcare Performance (RESHAPE), Université Claude Bernard Lyon INSERM U1290, Lyon, France
- 8SUAL, Hospices Civils de Lyon, Bron, France
- 9Institut des Agents Infectieux, Hospices Civils de Lyon, Lyon, France
- 10Waking Team, CRNL University Claude Bernard Lyon, Bron, France
- 11SUAL Le Vinatier, Hospices Civils de Lyon, Bron, France
- 12Inserm U1028, CNRS UMR5292, University Claude Bernard Lyon 1, Bron, France
Introduction: The mental health of residents is a growing significant concern, particularly with respect to hospital and university training conditions. Our goal was to assess the professional, academic, and psychological determinants of the mental health status of all residents of the academy of Lyon, France.
Materials and methods: The Health Barometer of Lyon Subdivision Residents (BASIL) is an initiative which consists in proposing a recurrent online survey to all residents in medicine, pharmacy, and dentistry, belonging to the Lyon subdivision. The first of these surveys was conducted from May to July 2022. Participants should complete a series of validated questionnaires, including the Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS), and the Kessler Psychological Distress Scale (K6), respectively, and ad-hoc questions assessing their global health and hospital and academic working conditions. A Directed Acyclic Graph (DAG) analysis was conducted prior to multivariable analyses, to explore the determinants associated with low wellbeing (WEMWBS <43) and high psychological distress (K6 ≥ 13).
Results: A total of 904 residents (response rate: 46.7%) participated in the survey. A low level of wellbeing was observed in 23% of participants, and was significantly associated to job strain (OR = 2.18; 95%CI = [1.32–3.60]), low social support (OR = 3.13; 95%CI = [2.05–4.78]) and the experience of very poor university teaching (OR = 2.51; 95%CI = [1.29–4.91]). A high level of psychological distress was identified for 13% of participants, and associated with low social support (OR = 2.41; 95%CI = [1.48–3.93]) and the experience of very poor university teaching (OR = 2.89, 95%CI = [1.16–7.21]).
Conclusion: Hospital working conditions, social support, and the perception of teaching quality, were three major determinants of wellbeing and psychological distress among health profession residents. Demographic determinants, personal life and lifestyle habits were also associated. This supports a multilevel action in prevention programs aiming to enhance wellbeing and reduce mental distress in this specific population and local organizational specificities.
1 Introduction
The overall state of health of healthcare professionals, including mental health is a growing major concern at the international level. According to the World Health Organization (WHO), “mental health is a state of mental wellbeing that enables people to cope with the stresses of life, realize their abilities, learn well and work well, and contribute to their community.” It lies on a complex continuum, with widely varying levels of difficulty and distress. From a bio-psycho-social perspective, mental health stems from individual, social and structural determinants. Individual biological and psychological factors, such as emotional competence or personality traits, and exposure to adverse circumstances (social, academic, professional, political, economic, environment etc.), contribute to the risk of poor mental health. Protective factors are resources to be supported throughout life, such as individual social and emotional skills, social support, decent work, community cohesion, etc. (Mental Health, World Health Organization, 2022).
According to the Big Five model, the five major personality traits (neuroticism, conscientiousness, extraversion, agreeableness and openness to experience) are involved in the way individuals behave and interact with their environment, in their personal and professional relationships, in life experiences. They also influence the way individuals make choices and transform their environment (McCrae and John, 1992). They influence mental health along with stress exposure and coping strategies. In complex work environments such as hospitals, high levels of neuroticism and conscientiousness could be linked to poorer mental health, in contrast to extraversion, openness to experience and agreeableness, especially when those two traits are combined (Doherty and Nugent, 2011; Delafontaine et al., 2024).
Risks and protective factors of mental health are found in society at different levels, for example in the workplace. According to the Job Strain model, poor working conditions result from an unbalanced relationship between job control (high/low) and psychological job demand (high/low), and are associated with negative effects on occupational stress and health, including mental health (low wellbeing, psychological distress, anxiety, etc.). A high level of occupational stress is associated with high job demand and low job control, known as “job strain.” If little support from superiors and/or colleagues is added, job stress is increased (Karasek, 1979; Niedhammer, 2002; Laditka et al., 2023).
Thus, the impact of psycho-social risk factors, workplace stress and violence, has been identified as crucial determinants of psychological wellbeing (Rugulies et al., 2023) in particular in the healthcare sector (Hu et al., 2019; Kansoun et al., 2019; Dres et al., 2023). The overall proportion of healthcare workers who report experiencing violence at work has been estimated to reach nearly 80% (Rossi et al., 2023). While all healthcare professionals can be affected by stress and violence, young healthcare professionals display specific vulnerability features. Residents in medicine, pharmacy, and dentistry, have a dual status as both students and caregivers, and they may experience specific, cumulative, and recurring stress factors. Their working conditions in hospital involve heavy workloads, emotionally demanding situations, and high professional expectations (Mara, 2018). They are in the process of constructing their knowledge, their experience and professional identity within a competitive work environment and an uncertain professional future. From this perspective, academic conditions are essential. Their status as university students requires them to take and validate training courses (theoretical knowledge), and follow a hospital residency program (experiential knowledge). The imperative to continue their residency course may impede their ability to extricate themselves from potentially harmful situations.
The combination of these factors can have adverse consequences on their mental health (Papp et al., 2004; Sen et al., 2010; Ogawa et al., 2018; Zhou et al., 2020; Awan et al., 2022). International reviews suggest that the prevalence of burnout among medical residents ranges from 35.7% (Rodrigues et al., 2018) to 51% (Low et al., 2019), and depression or depressive symptoms from 20.9% to 43.2 (Mata et al., 2015), respectively. Moreover, it has been consistently found a more degraded sense of personal accomplishment and depersonalization among residents, compared to senior doctors (Kansoun et al., 2019). In France, the exact annual number of work-related suicides among residents is poorly known due to the lack of any reporting obligation, families’ desire for discretion, and the lack of knowledge regarding the exact cause of death, particularly the causality of working conditions (Santé Publique France, 2021). Another important point is that the mental health of residents was particularly impacted by the coronavirus pandemic in 2019. Two French national studies found a deterioration in the level of psychological distress (high for 83% of students, compared with 21% initially), with a consumption of psychotropic medications which has more than doubled (Frajerman et al., 2022; Rolland et al., 2022). Previous studies have highlighted the use of psychoactive substances by individuals, including health professionals, as a strategy to cope with difficult working conditions, regulate stress and reduce unpleasant emotions. As young caregivers, residents could present higher levels of psychological distress, and thus, be more at risk of substance use, as poor mental health has been associated, for instance, with increased alcohol consumption (Lebensohn et al., 2013; Stimpfel et al., 2020).
The consequences of poor mental health among residents are substantial for themselves and the healthcare system (e.g., interrupted studies), but also for patients, as they lead to risks for the quality and safety of care, including the risk of medical errors (Dewa et al., 2014, 2017; Pereira-Lima et al., 2019; Frajerman, 2020a; Mangory et al., 2021; Hodkinson et al., 2022). A medical error may have a deep and lasting emotional impact, may affect the ability to provide patient care, can lead to medical malpractice lawsuits and increased healthcare costs (Burlison et al., 2017; Robertson and Long, 2018; Rodziewicz et al., 2024).
More generally, the impact of residents’ occupational and training conditions on their overall health is a growing concern, and action is needed to promote their mental health at work (Lietor et al., 2021). In this perspective, the University of Claude Bernard Lyon 1 (UCBL) and the University Hospital of Lyon have developed an action plan based on a socio-ecological model (Wold and Mittelmark, 2018; Frajerman, 2020b) to enhance the mental health, training and working conditions of residents in the Lyon subdivision. A collaborative approach to health program planning, inspired by the intervention mapping protocol (Bartholomew et al., 2016), has been implemented by University Health Unit (« SSU ») and the hospital Occupational Medicine Unit (« SMST »). The first step of this protocol involved a recurrent assessment of residents’ health condition, aiming to guide the decisions on which actions should be implemented (Mara, 2018). The Health Barometer of Lyon Subdivision Residents (« Baromètre Santé des Internes de la Subdivision de Lyon », BASIL) is a recurrent survey created to serve as a recurrent “diagnostic” step. To date, only one survey was conducted in 2022, while the next one is planned in 2024.
The primary objective of the 2022 BASIL survey was to assess the mental health of health profession residents of the Lyon subdivision. The secondary objectives were to explore the relationships between their mental health, and their working and academic conditions, taking into account lifestyle habits, and personality traits.
2 Methods
2.1 Study design
BASIL is an online survey, using both validated self-reported questionnaires and ad hoc questions. Here, only the data of the 2022 edition were used.
2.2 Study population and data collection methods
The survey was offered to all registered residents in the Lyon subdivision (n = 1,936), encompassing those in medicine, pharmacy and dentistry. Residents were invited to participate by an email sent on their personal address provided by the school departments. The email contained explanations on the study and the link to the survey (unique URL). Three reminders were sent on June 15th, June 27th, and July 4th, 2022, respectively. The survey was also relayed on social networks by Lyon resident unions, and on the Lyon University hospital and Claude Bernard Lyon 1 University intranet sites. Data were collected through an online survey on the Lime survey platform that was accessible from May 30 to July 15, 2022.
2.3 Assessment tools
The study questionnaire was constructed by a participatory working group, including residents and their representatives (unions), as well as representatives from hospital and university management, and researchers from various disciplines (i.e., occupational medicine, mental health and addiction medicine, university student health service, public health, and sleep medicine).
The variables collected were:
- socio-demographic: sex, age, familial status.
- academic: year of residency, specialty, evaluation of the postgraduate university courses, satisfaction with the choice of specialty, wish of an academic career.
- occupational: working conditions, work-time characteristics, work-organization constraints, violence at work.
- lifestyle: food, sleep, sport, drug use.
The following validated self-reported questionnaires were used:
- Wellbeing: Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS) (Tennant et al., 2007; Trousselard et al., 2016): The WEMWBS is a 14-item scale validated in French, designed to assess psychological wellbeing in adults by exploring both hedonic (absence of suffering and pleasure) and eudemonic (sense of self and accomplishment) dimensions. The total score ranges from 14 to 70 with a score below 43 indicating low psychological wellbeing (according to the excel spreadsheet for calculating scores with WEMWBS sent after completing the registration for a License to use WEMWBS for non-commercial purposes).
- Working conditions: The Job Content Questionnaire (Niedhammer, 2002; Niedhammer et al., 2006) is an international questionnaire validated in French, based on the “Karasek” model and evaluating psychological demand, decision latitude and social support at work. It comprises 26 items on a 4-point Likert scale. Thresholds are set at 21 for psychological demand, 70 for decision latitude and 23.9 for social support. The combination of psychological demand and decision latitude scores defines the four work situations (“passive,” “active,” “relaxed” and “stressed”).
- Personality traits: Big Five Inventory BFI-10 French items (Plaisant, 2010; Courtois et al., 2020): this concise self-reported questionnaire consists of 10 items extracted from the 44-item BFI, deemed the most representative of the various facets.
- Psychological distress: Kessler Psychological Distress Scale (K6) (Kessler et al., 2003; Gouvernement du Canada, 2016): the K6 is a self-reported questionnaire whose items are classified on a five-point scale, with a highest score of 24. A score ≥13 indicates a high probability of severe psychological distress, while a score < 13 indicates that severe psychological distress is unlikely.
- Alcohol consumption: AUDIT-C (Bush et al., 1998) is a condensed version comprising the first 3 items of AUDIT (10-item scale). The three items of this self-reported questionnaire use a 4-point scale with a maximum score of 12 points.
According to epidemiological models (Stoltzfus, 2011), the variables of interest for mental health were categorized in two groups for both the wellbeing and the psychological distress. The first outcome was the low wellbeing which was defined by having a WEMWBS score below 43. The second outcome was the high level of psychological distress which was defined by having a K6 score equal or greater than 13.
The entire questionnaire is available in English in Supplementary material.
2.4 Statistical analysis
Compared with data from the university’s education department, preliminary results indicated an over-representation of women, and a different distribution across age groups and specialties. Consequently, a margin calibration was conducted (Sautory, 1993; INSEE, 2021). The SAS CALMAR macro (“CALage sur MARges”) is used to adjust a sample from a sample survey, by re-weighting individuals, utilizing auxiliary information available on several variables, referred to as calibration variables.
The chosen calibration method was margin calibration - logit method (initial weights between zero and three). The decision was made to incorporate gender, age groups (6 categories) and specialties (grouped into 12 categories). This method yielded the least dispersion in calibration weights. Thus, the margin calibration method ensure the representativeness of the sample.
Descriptive statistics are presented as frequency, percentage and 95% confidence interval (95%CI) for categorical variables, and as mean and 95% confidence interval for continuous variables.
Descriptive statistical analyses were conducted using the surveyfreg and surveymeans (Koch et al., 1975; Bedrick, 1983) procedures of SAS software version 9.4 account for these sampling weights.
2.5 Directed acyclic graph
Mental health status was assessed independently, based on both the WEMWBS (wellbeing) and K6 (psychological distress) questionnaire. To assess the association between working conditions, academic conditions and the mental health of residents, a Directed Acyclic Graph (DAG) analysis was conducted prior to the analyses (Digitale et al., 2022). DAGs serve as a method to address causal questions in clinical and epidemiologic research, guiding study design and statistical analysis. DAGs are constructed to illustrate existing knowledge about biological and behavioral systems relevant to specific causal research questions. Through this, DAGs can identify variables sufficient to eliminate confounding and some forms of selection bias.
The authors developed four DAGs (wellbeing/working conditions; wellbeing/academic conditions; psychological distress/working conditions; psychological distress/academic conditions) (Supplementary material). The variables required for fitting the regression models were defined using the free DAGitty software, accessible at https://www.dagitty.net/.
The adjustment variables for investigating the connection between low wellbeing (Model 1 = M1) or a high probability of severe psychological distress (Model 2 = M2), and the main occupational explanatory variables (low social support and the quadrants of the Job content Questionnaire) were age, year of residency, specialty, and four dimensions of the BFI (Extraversion, Conscientiousness, Neuroticism, Openness).
The adjustment variables for examining the association between low wellbeing (Model 3 = M3) or a high probability of severe psychological distress (Model 4 = M4), and academic conditions (Evaluation of the contribution of the postgraduate teaching to the training, frequency of weekly half a day of university training, frequency of weekly half a day of personal training, tutor) were age, year of residency, specialty, and four dimensions of the BFI (Extraversion, Conscientiousness, Neuroticism, Openness).
We performed separate models for working conditions and academic conditions because we wanted to independently assess the effects of working conditions and academic conditions, for both low wellbeing and high psychological distress. For each model, we performed multivariable logistic regression based on the variables required for fitting the regression models according to each of the four DAG. Analyses were carried out using weighted logistic regressions (Cassel, 2006). The SAS “surveylogistic” procedure was employed to consider the sample design (Koch et al., 1975; Bedrick, 1983). Results were presented as weighted odd ratio (OR) and 95% confidence interval (95%CI).
2.6 Research ethics
The BASIL survey protocol was agreed on April 14, 2022, by the University of Lyon’s research ethics committee (CER-UdL n° 2022-03-17-002).
A CNIL declaration was made through the University of Claude Bernard Lyon 1’s data protection officer on March 18, 2022 (n°2022–006).
An information notice was attached to the e-mail inviting participation in the survey. Participation in the survey was anonymous and voluntary. No identifying data was collected.
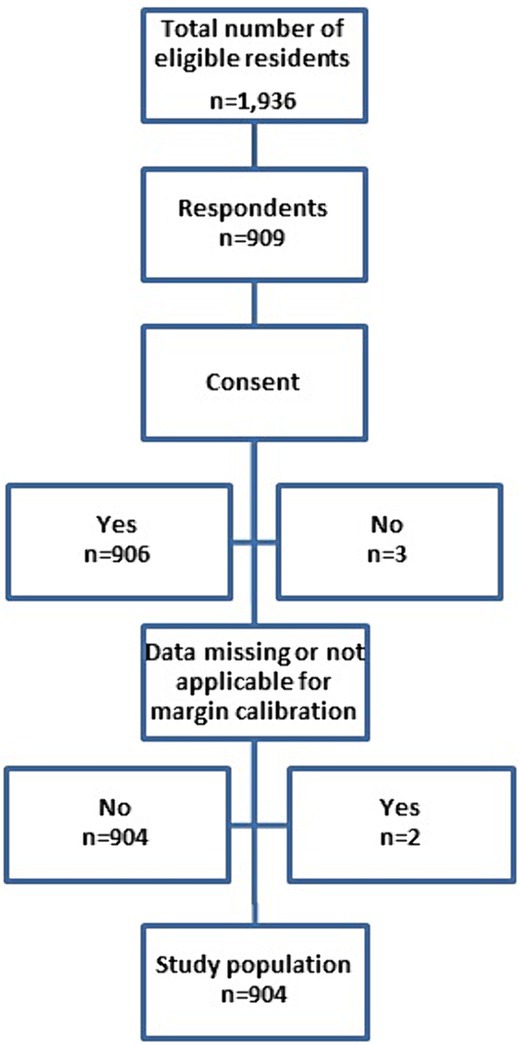
At the start of the online questionnaire, a message explained participants’ rights and collected their consent to participate, with a box that had to be ticked in order to access the rest of the BASIL questionnaire (Figure 1).
3 Results
3.1 Study population
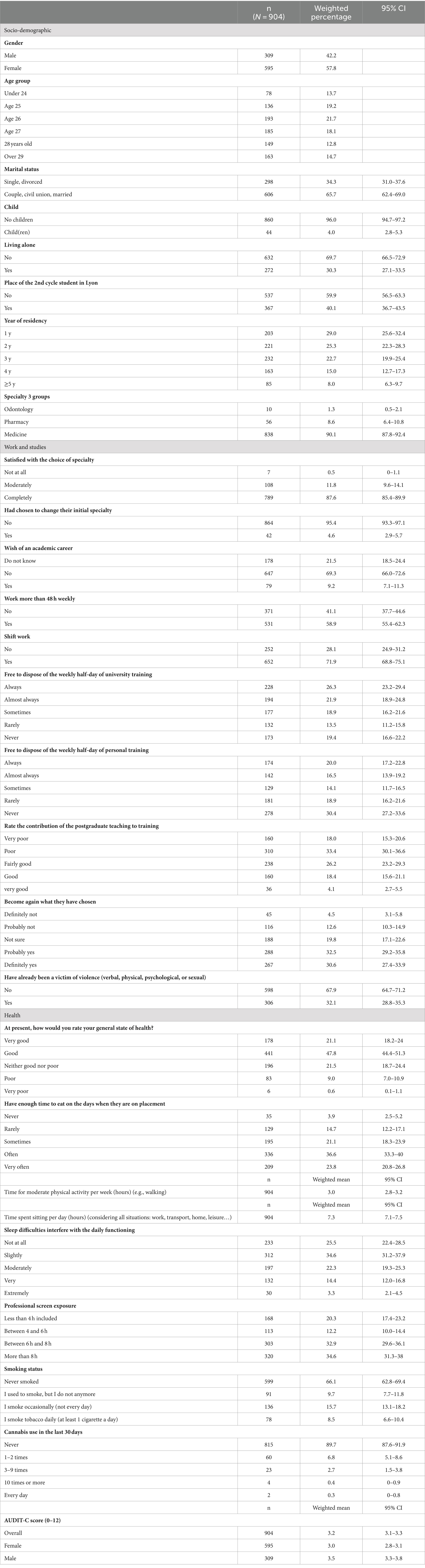
Of the 1,936 registered residents in the Lyon subdivision, a total of 904 residents completed the entire questionnaire (participation rate: 46.7%) (Figure 1). Residents in medical studies (90.1%), pharmacy (8.6%) and dentistry (1.3%), were categorized into eight classes of specialties. Among medical residents, 101 (12.5%) were in Anaesthesia-intensive care or Emergency and critical care, 234 (24.6%) in General medicine, 50 (4.1%) in Pediatrics, 56 (8.6%) in Pharmacy (excluding medical biology), 51 (5.6%) in Psychiatry, 61 (6.5%) in Radiology or Nuclear Medicine or Genetics or Anatomopathology or Medical Biology, 121 (16.0%) in other surgical specialties or dentistry or Gynecology-Obstetrics and 230 (22.2%) in other medical specialties or Occupational medicine or Public health (Table 1).
The majority of participants were female (n = 595, 57.8%), lived with a partner (n = 606, 65.7%), and had no children (n = 860, 96.0%). Approximately 30.3% of residents (n = 272) reported living alone. The average age of respondents was 27 years (SD = 2.2 years).
Most residents had studied outside the Lyon subdivision (n = 537, 59.9%). Participants were proportionally more numerous in the first (n = 203, 29.0%) and second year of residency (n = 221, 25.3%).
3.2 Working and study conditions
In total, 58.9% of respondents (n = 531) reported working more than 48 h, with an average weekly workload of 51.2 h, including on-call duty. Additionally, over 3.2% reported working 80 h or more per week. Nearly 10% of residents expressed a desire to pursue an academic career (n = 79, 9.2%) (Table 1).
The majority of residents were satisfied with the choice of their specialty (n = 789, 87.6%), and 4.3% (n = 42) had previously opted to change their initial specialty.
Among interviewees, 68.9% rated their overall health during the survey period as good or very good (n = 619, 68.9%). Residents reported sitting for an average of 7.3 h a day. They reported being engaged in 2 h of intense physical activity per week and 3 h of moderate activity. Unsatisfactory sleep disrupted daily life for 17.7% of residents (n = 162). Only 60.4% (n = 545) of residents often/very often had time to eat at work. Over a half of residents (n = 488, 54.5%) had a positive AUDIT-C score. Anxiolytics and hypnotics had been taken more than once a month during the past 12 months for 10.3% (n = 100) and 6.7% (n = 56) of the residents, respectively.
More than a third of residents (n = 306, 32.1%) reported having experienced at least one form of violence during their studies. Last, 17.1% (n = 161) of the respondents reported that they would not choose to be a resident a second time if they had to make that choice again.
3.3 Level of wellbeing and related determinants
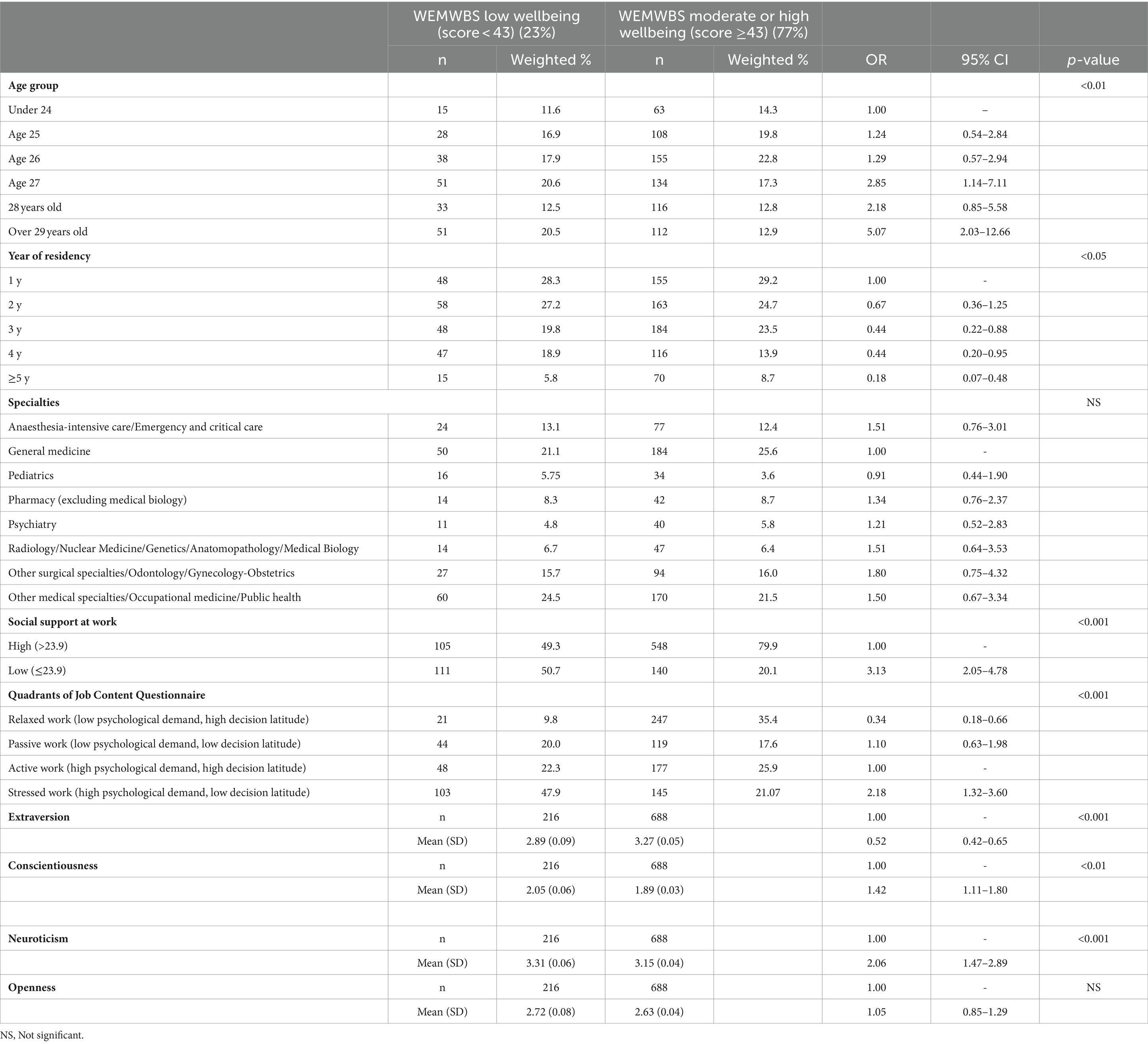
A low level of wellbeing (WEMWBS <43) was found in 23% of respondents. The outcomes of the multivariable analysis of wellbeing and working conditions in residency are presented in Table 2.
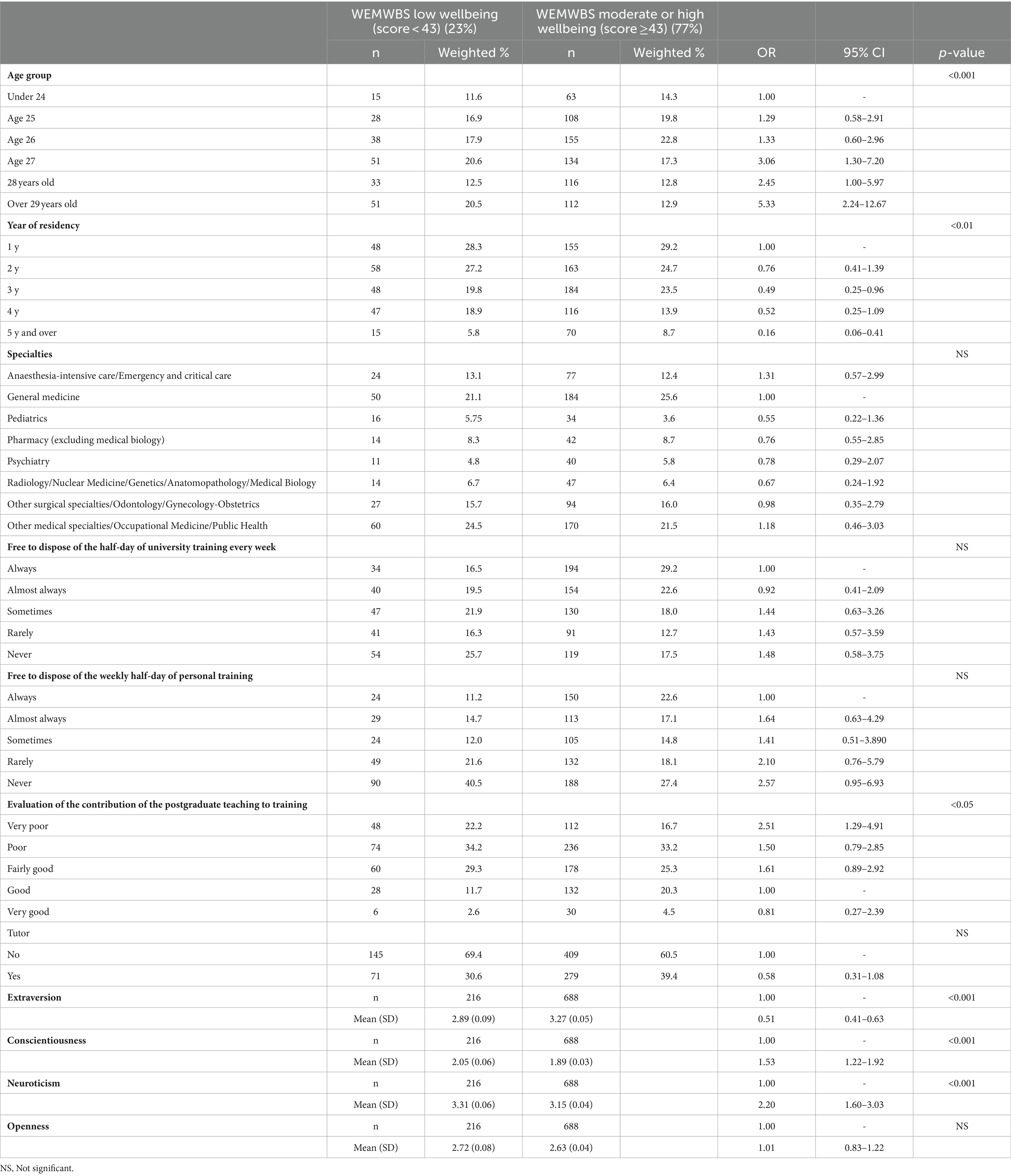
The results of the multivariable analysis of wellbeing and academic conditions in residency are presented in Table 3.
3.3.1 Working conditions (model 1 = M1) and academic conditions (model 3 = M3) and low wellbeing
Exhibiting a low level of wellbeing was associated with job strain (OR = 2.18; 95%CI = [1.32–3.60]), low social support (OR = 3.13; 95%CI = [2.05–4.78]), and reporting the experience of a very poor contribution from university training (OR = 2.51; 95%CI = [1.29–4.91]). However, there was no significant association between a low level of wellbeing and specialty type, weekly half-day of university or personal training, or having a tutor.
3.3.2 Personal determinants and low wellbeing
Variables associated with a low level of wellbeing included being older (for M1: p < 0.01 and for M3: p < 0.01), and simultaneously in the first part of residency (year 1 and 2) (for M1: p < 0.05 and for M3: p < 0.01). Regarding personality traits, a low level of wellbeing was positively associated with neuroticism (for M1: p < 0.001; for M3: p < 0.001), conscientiousness (for M1: p < 0.005; for M3: p < 0.01) while, in contrast, it was negatively associated with extraversion (for M1: p < 0.001; for M3: p < 0.001). There was no significant association with the openness dimension.
3.4 Level of psychological distress and related determinants
A high level of psychological distress (K6 ≥13) was identified in 13% of residents. The outcomes of the multivariable analysis of psychological distress and working conditions in residency are presented in Table 4.
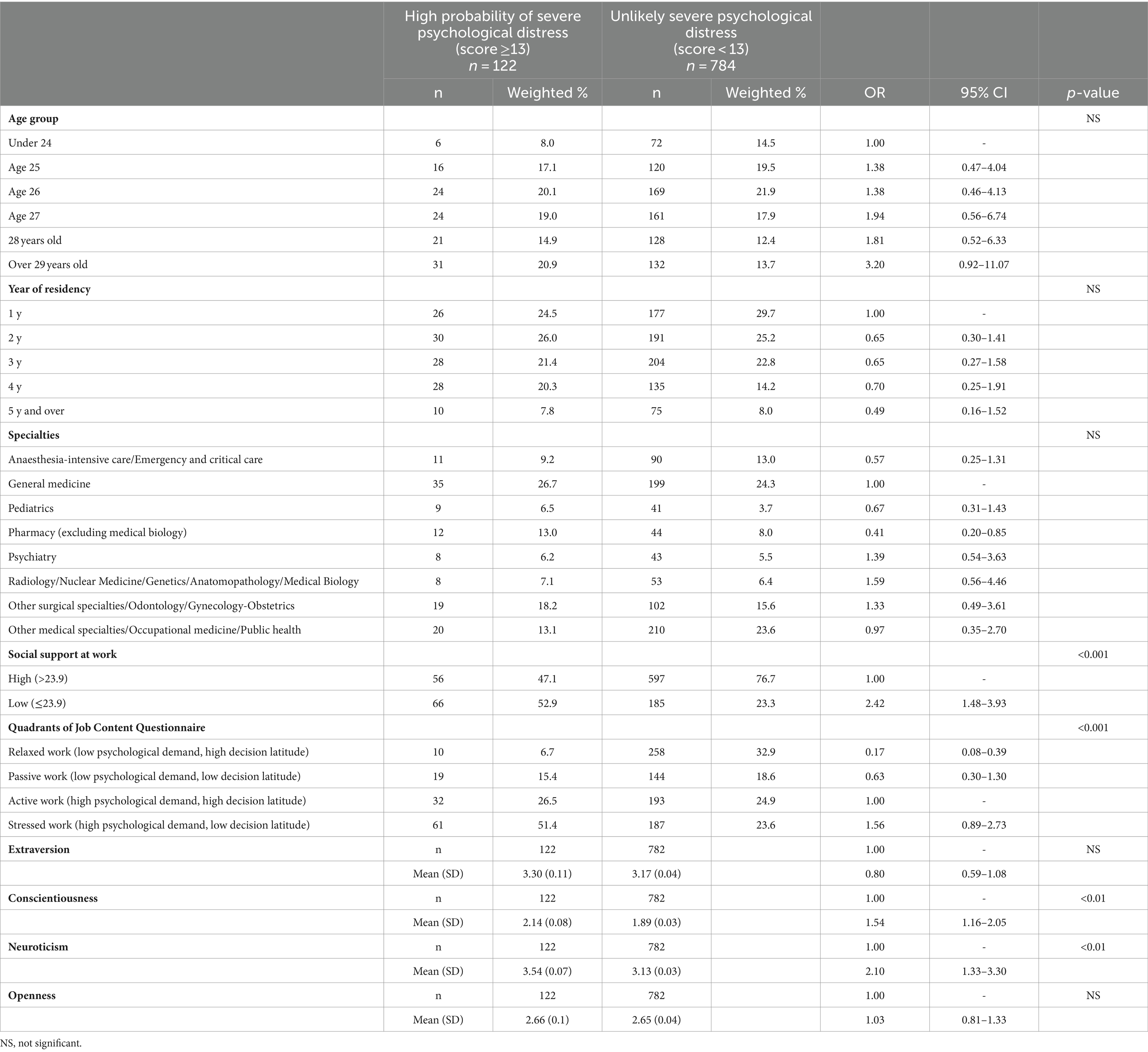
Table 4. Multivariable analysis by level of psychological distress (Kessler) and working conditions in residency.
The results of the multivariable analysis of psychological distress and academic conditions in residency are presented in Table 5.

Table 5. Multivariate analysis by level of psychological distress (Kessler) and academic conditions.
3.4.1 Working conditions (model 2 = M2) and academic conditions (model 4 = M4) and high level of psychological distress
A high level of psychological distress (K6 ≥13) was significantly (p < 0.01) associated with low social support (OR = 2.41; 95%CI = [1.48–3.93]).
Low psychological distress (K6 < 13) was highly significantly (p < 0.001) associated with “relaxed work” (OR = 0.17; 95%CI = [0.08–0.39]). A high level of psychological distress was significantly (p < 0.05) associated with an increased risk of judging the contribution of university teaching as very poor (OR = 2.89; 95%CI = [1.16–7.21]).
There was no significant association between the high level of psychological distress and the type of specialty or the fact of having a half-day of weekly university training or personal training or the fact of having a tutor.
3.4.2 Personal determinants and high level of psychological distress
The variables associated with a high level of psychological distress were a higher average level of neuroticism (for M2: p < 0.001; for M4: p < 0.001) and conscientiousness (for M2: p < 0.01; for M4: p < 0.01).
There was no significant association between high level of psychological distress and age, year of boarding, openness dimension or extraversion.
4 Discussion
4.1 Main findings
The main aim of the BASIL 2022 survey was to assess resident wellbeing, working and academic conditions, and personal lifestyle habits, and to explore the features associated with low wellbeing, and high level of psychological distress.
The results show that overall, most of the participants have an acceptable to very good level of wellbeing. However, other indicators give cause for concern, with a significant number of respondents reporting poor health, low levels of wellbeing and high levels of psychological distress. Multivariable analyses found that the residents’ mental health was significantly influenced by factors related to their hospital and faculty work conditions, personal life, and psychological factors associated with their personality trait. These results emphasize the need for a comprehensive approach to prevent and promote the mental health of residents, considering their working, training and personal conditions.
The WEMWBS questionnaire is not widely used among residents and thus, which makes comparisons with other studies in this specific population difficult. For instance, in 2019, Swiss general medicine residents reported a mean Wellbeing score of 51 (SD = 7.6) which is quite similar to that found in our study. Moreover, Swiss residents reported stress factors such as the lack of time for private life, heavy workload, including administrative work, and high perceived professional demands (Lindemann et al., 2019). Moreover, the prevalence of high psychological distress in BASIL is comparable to the prevalence of depressive symptoms identified in 12% of the French population aged between 25 and 34 (Hazo et al., 2022).
Regarding working conditions in the hospital residency, our survey assessed several psychosocial risk factors. A lower level of social support was associated with a poorer level of wellbeing and mental health, while the presence of support had the opposite effect. Job strain, characterized by high demand and low decision latitude, was associated with a poorer level of wellbeing. These results align with previous studies (Amiri and Behnezhad, 2020) and a recent literature review (Rugulies et al., 2023). French and European standards enforce a maximum working week of 48 h (République Française, 2015). In a previous study, it was found that working over 80 h per week increased the risk of depression among residents (Awan et al., 2022). However, in contrast with previous findings (Ogawa et al., 2018; Li et al., 2023), the BASIL study did not find a significant association between working hours and mental health status. This difference could be attributed to the fact that our study pertained to wellbeing and psychological distress rather than to depression. Another possibility is that the heavy workload is too recent for the impact to occur. Moreover, the negative effects of workload could be mitigated by the fact that workload is chosen rather than suffered (Lunau et al., 2014; Gerdenitsch, 2017). Indeed, 10% of respondents in our study were considering to pursue an academic career, which requires a greater personal investment. Moreover, the rate of residents reporting exposure to violence during their medical studies is a cause for concern (Hu et al., 2019) given the associated risks for health (post-traumatic stress disorder, anxiety, depression), as well as potential consequences for the curriculum (failed exams, dropping out of medical education). However, in our study, there was no specific association between exposure to violence and mental health. It is possible that the survey questions lacked precision by not exploring typical symptoms. Violence is a growing occupational risk in healthcare (Kannan et al., 2019; Sari et al., 2023). Further studies should explore more specifically the health and academic consequences for residents subjected to different types of violence in various contexts, such as hospitals, medical school, or private life.
In relation to university training conditions, a significant association was observed among one-third of the participants in the BASIL study between the perception of poor-quality training and a deterioration in mental health (low wellbeing, high level of psychological distress). Prior research has highlighted the imperative to enhance the quality of resident training, incorporating adaptations to new technologies (Mattar et al., 2013; Mann et al., 2020). Another study underscores the advantages of ensuring non-clinical training time, which may reduce burnout and enhance wellbeing (Stevens et al., 2020; Schlosser et al., 2023). Our results emphasize the importance of exploring the criteria influencing residents’ perception of training quality and understanding the mechanisms through which it correlates with their mental health. This original finding sheds light on the challenges faced by this specific population, as both emerging healthcare professionals in clinical settings and medical students still undergoing training.
Regarding personal determinants influencing residents’ mental health, various elements related to demographics, lifestyle habits and personality trait were identified. The duration of residency in France varies from 3 to 6 years, depending on the specialty. Being in the first part of residency (year 1 and 2) was associated with a lower level of wellbeing among BASIL participants, which is consistent with reported increases in depression in the literature (Mata et al., 2015). Younger age (i.e., below 30 years) is commonly associated with a lower sense of fulfillment (Shalaby et al., 2023). This association may be attributed to reduced resources and latitude at the beginning of residency, coupled with heightened adaptation demands during this transitional period. Approximately 60% of BASIL respondents had completed their externship outside the Lyon subdivision, requiring them to transition from their familiar environment to a new one, and to adapt accordingly. Being older (>29 years) was also associated with a lower level of wellbeing. This seemingly contradictory finding can be interpreted in different ways. Older residents may include those with children (4% of participants), who face greater challenges in balancing personal and professional responsibilities (Kocalevent et al., 2020). Additionally, they may be individuals preparing for a forthcoming period of adaptation between the end of their residency and the commencement of their professional career, which could be a potential source of anxiety and uncertainty.
In terms of lifestyle habits, residents most commonly reported unfavorable health behaviors included sleep problems, risky alcohol consumption, and sedentary behavior coupled with insufficient physical activity. Although no significant association was identified with their mental health at the time of the study, these behaviors remain a cause for concern for residents’ overall health, and is consistent with findings reported in other studies (Markwell and Wainer, 2009).
Concerning their personality traits, our study identified significant associations between certain personality traits and the mental health of residents. Specifically, the personality traits of “neuroticism” and “conscientiousness” were associated with a lower level of mental health. While the diversity of measures used in the literature complicates direct comparisons, these elements are crucial for comprehending and enhancing self-awareness and coping strategies (Louwen et al., 2023). Limited research has explored this subject, particularly among residents. Further studies are necessary to deepen our understanding of the connections between personality, environmental factors influencing residents’ coping strategies, and the subsequent impact on academic performance, wellbeing and overall health.
One of the most unexpected findings was that 17% of residents would not opt to undergo the same studies to become a doctor/dentist/pharmacist again. This result is particularly worrying, considering that mental health problems impact doctors of all categories and all ages in France. In a recent study involving 2,390 French teaching hospital physicians, almost 40% of respondents reported severe burnout, and 12% experienced job strain (Dres et al., 2023). A 2019 meta-analysis estimated the prevalence of burnout at 49% among French doctors, and at 52% among residents (Kansoun et al., 2019). Therefore, it is crucial to coordinate the prevention and promotion of residents’ mental health with that of the doctors who are tasked with supervising and collaborating with them during their studies.
4.2 Implications
The interweaving of environmental factors (hospital and university) and individual factors (lifestyle, personality) associated with residents’ mental health clearly illustrates the necessity of adopting an ecological approach to mental health promotion and prevention among residents.
According to French regulations, it is the responsibility of the employers to assess psychosocial risk factors for employee health and to implement necessary improvements. In this context, the University of Lyon and the Lyon University Hospitals consortium have collaborated to establish a prevention and health promotion plan specially tailored for residents.
Skills, motivation and personality traits are essential factors in shaping the development of excellent doctors (Khawar et al., 2022). The results concerning the different specialties of the residents need to be studied in greater depth, and merit a specific study. Working and academic conditions must be in line with this expectation. Emerging training opportunities, such as mentoring, provides avenues for improvement (Mann et al., 2020). In Lyon, the formal adoption of mentoring is limited (38.6% have a tutor and 35.2% have an equivalent mentor), despite its potential to enhance satisfaction with the chosen specialty (Enson et al., 2022). Exploring the impact of mentoring on resident mental health represents a significant area for intervention that warrants investigation. The mentoring approach holds particular promise in addressing the diverse challenges identified. Individualized support from a senior doctor for each resident has the potential to foster a gradual assumption of professional responsibility, accommodating individual personality and functioning. This, in turn, may reduce cognitive load and anxiety while expanding the autonomy and empowerment.
The individual determinants of mental health provide valuable insights into potential levers. Prevention initiatives targeting coping skills could contribute to enhancing residents’ individual experiences. In secondary and tertiary prevention, the implementation of specialized consultations have demonstrated the potential to improve health (Jacob et al., 2020). Healthcare professionals, at any stage in their training or career, can strengthen their professional and psychosocial skills, self-awareness and empowerment. Social support stands out as a pivotal factor at the intersection, positively contributing to primary prevention and mitigating various risk situations in healthcare work organizations (Blanch, 2016).
However, interventions must not be limited to individual determinants, but must also include professional and social determinants. Presently, knowledge available on the prevention and promotion of mental health in the workplace predominantly focuses on individual interventions, and it is necessary to develop interventions targeting modifications in the work environment (Tamminga et al., 2023; Waddell et al., 2023). Attention to workload and fostering a professional culture that values the right to disconnect emerged as crucial elements in the findings from BASIL. As per existing literature, work-family imbalance is a predictive factor for burnout symptoms among caregivers, doctors and residents. Conversely, maintaining a good work-life balance serves as a lever for reducing the risk of poor mental health and intention to leave the profession (Hämmig, 2018; Häusler et al., 2018; Kocalevent et al., 2020).
4.3 Study strengths and limitations
The participation rate of 46.7% among residents ensures the representativeness of the sample and the validity of the results. A comprehensive study examining mental health, working conditions, academic conditions and lifestyle habits provides an integrated perspective on health. Collaboration among residents, university and hospital management, the occupational health service, the university health service and multidisciplinary researchers in designing the study facilitated the development of a questionnaire that addressed the concerns of the various stakeholders. This collaboration also aided in relaying information about the study, encouraging resident participation.
Nevertheless, this study has several limitations. The results are specific to the Lyon subdivision and cannot be generalized to the 36,520 residents in France in 2021 (Castaing, 2021). There is a potential for selection bias, as residents more aware of mental health issues might have had a higher participation. However, efforts to minimize this bias were made through the survey’s dissemination across several channels and peer networks (resident unions). Likewise, the majority of the sample was female, which is usual in epidemiology surveys (Slauson-Blevins and Johnson, 2016). Although statistical analysis attempted to account for this over-representation, the lack of diversity of our sample is a limitation. Moreover, the use of the BFI-10 only allows the detection of personality dimensions based on the Big Five model. A technical issue with the online questionnaire prevented the collection of data on the agreeableness dimension of the BFI-10. According to the questionnaire’s validators, the factor structure of the BFI-10 is identical to that of the full BFI-Fr, with a very satisfactory rating for the factors “extraversion,” “conscientiousness,” “neuroticism” and “openness,” and an acceptable rating for “agreeableness” (Courtois et al., 2020). Finally, relying on self-reported questionnaires introduces inherent limitations.
5 Conclusion
The results of this survey confirm the concerns about the mental health status of health profession residents, and provide new data about the determinants influencing mental health, in particular within the work environment both at the hospital and the faculty. Additional determinants related to personal life, and lifestyle habits.
Efforts to prevent and promote mental health among residents at work must not be confined to providing individual support, and should be extended with evaluated actions implemented in the working and academic environments. These initiatives must be tailored to the complexity and local specificities of the evolving work organizations.
Collaboration among occupational health units, institutions (hospital and university), researchers, residents and senior professionals from hospitals and health universities is essential. As demonstrated in the BASIL barometer, this collaborative effort is crucial for formulating and endorsing ongoing actions to improve resident mental health at work.
Data availability statement
The datasets presented in this article are not readily available because data analysis in progress. Requests to access the datasets should be directed to bHVkaXZpbmUubm9oYWxlc0BjaHUtbHlvbi5mcg==.
Ethics statement
The studies involving humans were approved by the University of Lyon Research Ethics Committee (Comité d’éthique de la recherche de l’Université de Lyon, CER-UdL). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LN: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft. EF: Data curation, Formal analysis, Investigation, Methodology, Writing – review & editing. SP: Conceptualization, Formal analysis, Investigation, Methodology, Writing – review & editing. CC: Investigation, Writing – review & editing. PL: Investigation, Writing – review & editing. JT: Formal analysis, Investigation, Methodology, Writing – review & editing. MW: Investigation, Writing – review & editing. BR: Conceptualization, Formal analysis, Investigation, Methodology, Writing – review & editing. J-BF: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft.
Consortium: Basil Study Group
Unions (SYREL MG, SAIHL and SIPHL), Senior scientists (J Haesebaert, F Haesebaert, S Mazza, P Michel, E Poulet, E Leaune, AM Schott), residents (L Lestienne, R Varnier, L Rodriguez-Borlado Salazar, V Arigault, X Balmelle), Sophie Granger (DAM).
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Publication costs were covered by the Hospices Civils de Lyon.
Acknowledgments
The authors would like to thank all individuals who participated in this survey, the BASIL study group participants, the BASIL report reviewers, the general management of the Hospices Civils of Lyon (HCL), the presidency of the Medical Establishment Commission of the HCL, the management of the University Claude Bernard Lyon 1, particularly the Committee for Coordination of Medical Studies (CCEM), the management of the Occupational Medicine and Health Service-CRPPE and the University Health Service of Lyon.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1347513/full#supplementary-material
Supplementary DATA SHEET 1 | The health barometer of lyon subdivision residents.
Supplementary FIGURE 1 | DAG: working conditions-psychological distress.
Supplementary FIGURE 2 | DAG: academic conditions-psychological distress.
Supplementary FIGURE 3 | DAG: academic conditions-wellbeing.
Supplementary FIGURE 4 | DAG: working conditions-wellbeing.
References
Amiri, S., and Behnezhad, S. (2020). Job strain and mortality ratio: a systematic review and meta-analysis of cohort studies. Public Health 181, 24–33. doi: 10.1016/j.puhe.2019.10.030
Awan, S., Diwan, M. N., Aamir, A., Allahuddin, Z., Irfan, M., Carano, A., et al. (2022). Suicide in healthcare workers: determinants, challenges, and the impact of COVID-19. Front. Psych. 12:792925. doi: 10.3389/fpsyt.2021.792925
Bartholomew, K., Markham, C. M., Ruiter, R. A. C., Fernandez, M. E., Kok, G., and Parcel, G. S. (2016). Planning health promotion programs: an intervention mapping approach. 4th ed. Wiley. Available at: https://www.wiley.com/en-us/Planning+Health+Promotion+Programs%3A+An+Intervention+Mapping+Approach%2C+4th+Edition-p-9781119035497 (Accessed August 31, 2023).
Bedrick, E. J. (1983). Adjusted chi-squared tests for cross-classified tables of survey data. Biometrika 70, 591–595. doi: 10.2307/2336494
Blanch, A. (2016). Social support as a mediator between job control and psychological strain. Soc. Sci. Med. 157, 148–155. doi: 10.1016/j.socscimed.2016.04.007
Burlison, J. D., Scott, S. D., Browne, E. K., Thompson, S. G., and Hoffman, J. M. (2017). The second victim experience and support tool: validation of an organizational resource for assessing second victim effects and the quality of support resources. J. Patient Saf. 13, 93–102. doi: 10.1097/PTS.0000000000000129
Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D., and Bradley, K. A. (1998). The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory care quality improvement project (ACQUIP). Alcohol use disorders identification test. Arch. Intern. Med. 158, 1789–1795. doi: 10.1001/archinte.158.16.1789
Courtois, R., Petot, J.-M., Plaisant, O., Allibe, B., Lignier, B., Réveillère, C., et al. (2020). Validation française du Big Five Inventory à 10 items (BFI-10). L’Encéphale 46, 455–462. doi: 10.1016/j.encep.2020.02.006
Delafontaine, A.-C., Anders, R., Mathieu, B., Salathé, C. R., and Putois, B. (2024). Impact of confrontation to patient suffering and death on wellbeing and burnout in professionals: a cross-sectional study. BMC Palliat. Care 23:74. doi: 10.1186/s12904-024-01393-8
Dewa, C. S., Loong, D., Bonato, S., Thanh, N. X., and Jacobs, P. (2014). How does burnout affect physician productivity? A systematic literature review. BMC Health Serv. Res. 14:325. doi: 10.1186/1472-6963-14-325
Dewa, C. S., Loong, D., Bonato, S., and Trojanowski, L. (2017). The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: a systematic review. BMJ Open 7:e015141. doi: 10.1136/bmjopen-2016-015141
Digitale, J. C., Martin, J. N., and Glymour, M. M. (2022). Tutorial on directed acyclic graphs. J. Clin. Epidemiol. 142, 264–267. doi: 10.1016/j.jclinepi.2021.08.001
Doherty, E. M., and Nugent, E. (2011). Personality factors and medical training: a review of the literature. Med. Educ. 45, 132–140. doi: 10.1111/j.1365-2923.2010.03760.x
Dres, M., Copin, M.-C., Cariou, A., Mathonnet, M., Gaillard, R., Shanafelt, T., et al. (2023). Job strain, burnout, and suicidal ideation in tenured university hospital faculty staff in France in 2021. JAMA Netw. Open 6:e233652. doi: 10.1001/jamanetworkopen.2023.3652
Enson, J., Malik-Tabassum, K., Faria, A., Faria, G., Gill, K., and Rogers, B. (2022). The impact of mentoring in trauma and orthopaedic training: a systematic review. Ann. R. Coll. Surg. Engl. 104, 400–408. doi: 10.1308/rcsann.2021.0330
Frajerman, A. (2020a). La santé mentale des étudiants en médecine. Fondation Jean-Jaurès. Available at: https://www.jean-jaures.org/publication/la-sante-mentale-des-etudiants-en-medecine/ (Accessed October 27, 2022).
Frajerman, A. (2020b). Quelles interventions pour améliorer le bien-être des étudiants en médecine? Une revue de la littérature. L’Encéphale 46, 55–64. doi: 10.1016/j.encep.2019.09.004
Frajerman, A., Rolland, F., Falissard, B., Bertschy, G., Diquet, B., and Marra, D. (2022). COVID-19 pandemic’s impact on French health students: a cross-sectional study during the third wave. J. Affect. Disord. 311, 165–172. doi: 10.1016/j.jad.2022.05.087
Gerdenitsch, C. (2017). “New ways of working and satisfaction of psychological needs” in Job demands in a changing world of work: impact on workers’ health and performance and implications for research and practice. eds. C. Korunka and B. Kubicek (Cham: Springer International Publishing), 91–109.
Gouvernement du Canada, S. C. (2016). Validation de l’échelle de détresse psychologique à 10 questions de Kessler (K10) à partir de l’Enquête auprès des peuples autochtones de 2012. Available at: https://www150.statcan.gc.ca/n1/pub/82-003-x/2016001/article/14307-fra.htm (Accessed April 21, 2021).
Hämmig, O. (2018). Explaining burnout and the intention to leave the profession among health professionals - a cross-sectional study in a hospital setting in Switzerland. BMC Health Serv. Res. 18:785. doi: 10.1186/s12913-018-3556-1
Häusler, N., Bopp, M., and Hämmig, O. (2018). Effort-reward imbalance, work-privacy conflict, and burnout among hospital employees. J. Occup. Environ. Med. 60, e183–e187. doi: 10.1097/JOM.0000000000001287
Hazo, J., Boulch, A., and group EpiCov,. (2022). [Santé mentale: une amélioration chez les jeunes en juillet 2021 par rapport à 2020 mais des inégalités sociales persistantes.] DRESS [Internet]. Études et Résultats (1233). Available at: https://drees.solidarites-sante.gouv.fr/publications-communique-de-presse/etudes-et-resultats/sante-mentale-une-amelioration-chez-les
Hodkinson, A., Zhou, A., Johnson, J., Geraghty, K., Riley, R., Zhou, A., et al. (2022). Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ 378:e070442. doi: 10.1136/bmj-2022-070442
Hu, Y.-Y., Ellis, R. J., Hewitt, D. B., Yang, A. D., Cheung, E. O., Moskowitz, J. T., et al. (2019). Discrimination, abuse, harassment, and burnout in surgical residency training. N. Engl. J. Med. 381, 1741–1752. doi: 10.1056/NEJMsa1903759
INSEE (2021). La macro SAS CALMAR | Insee. Available at: https://github.com/InseeFr/Calmar (Accessed February 19, 2024).
Jacob, R., Li, T.-Y., Martin, Z., Burren, A., Watson, P., Kant, R., et al. (2020). Taking care of our future doctors: a service evaluation of a medical student mental health service. BMC Med. Educ. 20:172. doi: 10.1186/s12909-020-02075-8
Kannan, L., Wheeler, D. S., Blumhof, S., Gotfried, J., Ferris, A., Mathur, A., et al. (2019). Work related post traumatic stress disorder in medicine residents. Acad. Psychiatry 43, 167–170. doi: 10.1007/s40596-018-0911-9
Kansoun, Z., Boyer, L., Hodgkinson, M., Villes, V., Lançon, C., and Fond, G. (2019). Burnout in French physicians: a systematic review and meta-analysis. J. Affect. Disord. 246, 132–147. doi: 10.1016/j.jad.2018.12.056
Karasek, R. A. (1979). Job demands, job decision latitude, and mental strain: implications for job redesign. Adm. Sci. Q. 24, 285–308. doi: 10.2307/2392498
Kessler, R. C., Barker, P. R., Colpe, L. J., Epstein, J. F., Gfroerer, J. C., Hiripi, E., et al. (2003). Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 60, 184–189. doi: 10.1001/archpsyc.60.2.184
Khawar, A., Frederiks, F., Nasori, M., Mak, M., Visser, M., van Etten-Jamaludin, F., et al. (2022). What are the characteristics of excellent physicians and residents in the clinical workplace? A systematic review. BMJ Open 12:e065333. doi: 10.1136/bmjopen-2022-065333
Kocalevent, R., Pinnschmidt, H., Selch, S., Nehls, S., Meyer, J., Boczor, S., et al. (2020). Burnout is associated with work-family conflict and gratification crisis among German resident physicians. BMC Med. Educ. 20:145. doi: 10.1186/s12909-020-02061-0
Koch, G. G., Freeman, D. H., and Freeman, J. L. (1975). Strategies in the multivariate analysis of data from complex surveys. Int. Stat. Rev. 43, 59–78. doi: 10.2307/1402660
Laditka, J. N., Laditka, S. B., Arif, A. A., and Adeyemi, O. J. (2023). Psychological distress is more common in some occupations and increases with job tenure: a thirty-seven year panel study in the United States. BMC Psychol. 11:95. doi: 10.1186/s40359-023-01119-0
Lebensohn, P., Dodds, S., Benn, R., Brooks, A. J., Birch, M., Cook, P., et al. (2013). Resident wellness behaviors: relationship to stress, depression, and burnout. Fam. Med. 45, 541–549.
Li, Z., Liu, D., Liu, X., Su, H., and Bai, S. (2023). The Association of Experienced Long Working Hours and Depression, anxiety, and suicidal ideation among Chinese medical residents during the COVID-19 pandemic: a multi-center cross-sectional study. Psychol. Res. Behav. Manag. 16, 1459–1470. doi: 10.2147/PRBM.S408792
Lietor, M. D. C. M., Cuevas, I., and Prieto, M. B. (2021). Suicidal behaviour in medicine students and residents. Eur. Psychiatry 64:S581. doi: 10.1192/j.eurpsy.2021.1551
Lindemann, F., Rozsnyai, Z., Zumbrunn, B., Laukenmann, J., Kronenberg, R., and Streit, S. (2019). Assessing the mental wellbeing of next generation general practitioners: a cross-sectional survey. BJGP Open 3:bjgpopen19X101671. doi: 10.3399/bjgpopen19X101671
Louwen, C., Reidlinger, D., and Milne, N. (2023). Profiling health professionals’ personality traits, behaviour styles and emotional intelligence: a systematic review. BMC Med. Educ. 23:120. doi: 10.1186/s12909-023-04003-y
Low, Z. X., Yeo, K. A., Sharma, V. K., Leung, G. K., McIntyre, R. S., Guerrero, A., et al. (2019). Prevalence of burnout in medical and surgical residents: a Meta-analysis. Int. J. Environ. Res. Public Health 16:E1479. doi: 10.3390/ijerph16091479
Lunau, T., Bambra, C., Eikemo, T. A., van der Wel, K. A., and Dragano, N. (2014). A balancing act? Work-life balance, health and well-being in European welfare states. Eur. J. Pub. Health 24, 422–427. doi: 10.1093/eurpub/cku010
Mangory, K. Y., Ali, L. Y., Rø, K. I., and Tyssen, R. (2021). Effect of burnout among physicians on observed adverse patient outcomes: a literature review. BMC Health Serv. Res. 21:369. doi: 10.1186/s12913-021-06371-x
Mann, S., Truelove, A. H., Beesley, T., Howden, S., and Egan, R. (2020). Resident perceptions of competency-based medical education. Can Med Educ J 11, e31–e43. doi: 10.36834/cmej.67958
Mara, D. (2018). Rappport sur la Qualité de vie des étudiants en santé. Available at: https://solidarites-sante.gouv.fr/IMG/pdf/180403_-_rapport_dr_donata_mara.pdf
Markwell, A. L., and Wainer, Z. (2009). The health and wellbeing of junior doctors: insights from a national survey. Med. J. Aust. 191, 441–444. doi: 10.5694/j.1326-5377.2009.tb02880.x
Mata, D. A., Ramos, M. A., Bansal, N., Khan, R., Guille, C., Di Angelantonio, E., et al. (2015). Prevalence of depression and depressive symptoms among resident physicians: a systematic review and Meta-analysis. JAMA 314, 2373–2383. doi: 10.1001/jama.2015.15845
Mattar, S. G., Alseidi, A. A., Jones, D. B., Jeyarajah, D. R., Swanstrom, L. L., Aye, R. W., et al. (2013). General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann. Surg. 258, 440–449. doi: 10.1097/SLA.0b013e3182a191ca
McCrae, R. R., and John, O. P. (1992). An introduction to the five-factor model and its applications. J. Pers. 60, 175–215. doi: 10.1111/j.1467-6494.1992.tb00970.x
Mental Health, World Health Organization (2022). Who. Int. Available at: https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response (Accessed November 30, 2023).
Niedhammer, I. (2002). Psychometric properties of the French version of the Karasek job content questionnaire: a study of the scales of decision latitude, psychological demands, social support, and physical demands in the GAZEL cohort. Int. Arch. Occup. Environ. Health 75, 129–144. doi: 10.1007/s004200100270
Niedhammer, I., Ganem, V., Gendrey, L., David, S., and Degioanni, S. (2006). Propriétés psychométriques de la version française des échelles de la demande psychologique, de la latitude décisionnelle et du soutien social du « Job Content Questionnaire » de Karasek: résultats de l’enquête nationale SUMER. Sante Publique 18, 413–427. doi: 10.3917/spub.063.0413
Ogawa, R., Seo, E., Maeno, T., Ito, M., Sanuki, M., and Maeno, T. (2018). The relationship between long working hours and depression among first-year residents in Japan. BMC Med. Educ. 18:50. doi: 10.1186/s12909-018-1171-9
Papp, K. K., Stoller, E. P., Sage, P., Aikens, J. E., Owens, J., Avidan, A., et al. (2004). The effects of sleep loss and fatigue on resident-physicians: a multi-institutional, mixed-method study. Acad. Med. 79, 394–406. doi: 10.1097/00001888-200405000-00007
Pereira-Lima, K., Mata, D. A., Loureiro, S. R., Crippa, J. A., Bolsoni, L. M., and Sen, S. (2019). Association between physician depressive symptoms and medical errors: a systematic review and Meta-analysis. JAMA Netw. Open 2:e1916097. doi: 10.1001/jamanetworkopen.2019.16097
Plaisant, O. (2010). Validation par Analyse Factorielle du Big Five Inventory français (BFI-Fr) Analyse Convergente avec le NEO-PI-R. Ann Méd Psychol Rev Psychiatr 168, 97–106. doi: 10.1016/j.amp.2009.09.003
République Française. Décret n° 2015-225 du 26 février 2015 relatif au temps de travail des internes. (2015).
Robertson, J. J., and Long, B. (2018). Suffering in silence: medical error and its impact on health care providers. J. Emerg. Med. 54, 402–409. doi: 10.1016/j.jemermed.2017.12.001
Rodrigues, H., Cobucci, R., Oliveira, A., Cabral, J., Medeiros, L., Gurgel, K., et al. (2018). Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS One 13:e0206840. doi: 10.1371/journal.pone.0206840
Rodziewicz, T. L., Houseman, B., and Hipskind, J. E. (2024). Medical error reduction and prevention. in StatPearls, Treasure Island, FL: StatPearls Publishing. Available at: http://www.ncbi.nlm.nih.gov/books/NBK499956/ (Accessed February 18, 2024).
Rolland, F., Frajerman, A., Falissard, B., Bertschy, G., Diquet, B., and Marra, D. (2022). Impact of the first wave of the COVID-19 pandemic on French health students. L’Encéphale 49, 219–226. doi: 10.1016/j.encep.2021.12.004
Rossi, M. F., Beccia, F., Cittadini, F., Amantea, C., Aulino, G., Santoro, P. E., et al. (2023). Workplace violence against healthcare workers: an umbrella review of systematic reviews and meta-analyses. Public Health 221, 50–59. doi: 10.1016/j.puhe.2023.05.021
Rugulies, R., Aust, B., Greiner, B. A., Arensman, E., Kawakami, N., LaMontagne, A. D., et al. (2023). Work-related causes of mental health conditions and interventions for their improvement in workplaces. Lancet 402, 1368–1381. doi: 10.1016/S0140-6736(23)00869-3
Santé Publique France (2021). Surveillance des suicides en lien potentiel avec le travail. Définition des suicides en lien potentiel le travail; Résultats de l’étude de faisabilité menée auprès de 8 Instituts de médecine légale. Propositions pour le renforcement de la surveillance. Santé Publique France. Available at: https://www.santepubliquefrance.fr/import/surveillance-des-suicides-en-lien-potentiel-avec-le-travail.definition-des-suicides-en-lien-potentiel-le-travail-resultats-de-l-etude-de-faisabil (Accessed November 26, 2023).
Sari, H., Yildiz, İ., Çağla Baloğlu, S., Özel, M., and Tekalp, R. (2023). The frequency of workplace violence against healthcare workers and affecting factors. PLoS One 18:e0289363. doi: 10.1371/journal.pone.0289363
Sautory, O. (1993). La macro Calmar. Redressement d’un échantillon par calage sur marges. Available at: https://www.insee.fr/fr/statistiques/fichier/2838097/5-les-methodes-de-calage.pdf (Accessed February 19, 2024).
Schlosser, S., Garbe, J., Hamesch, K., Dimitriadis, S., and Staudacher, J. J. (2023). How we achieve satisfaction in training - a German-wide survey on preferred training conditions among trainers and trainees for board certification in gastroenterology. Z. Gastroenterol. 62, 388–398. doi: 10.1055/a-2119-3069
Sen, S., Kranzler, H. R., Krystal, J. H., Speller, H., Chan, G., Gelernter, J., et al. (2010). A prospective cohort study investigating factors associated with depression during medical internship. Arch. Gen. Psychiatry 67, 557–565. doi: 10.1001/archgenpsychiatry.2010.41
Shalaby, R., Oluwasina, F., Eboreime, E., El Gindi, H., Agyapong, B., Hrabok, M., et al. (2023). Burnout among residents: prevalence and predictors of depersonalization, emotional exhaustion and professional Unfulfillment among resident doctors in Canada. Int. J. Environ. Res. Public Health 20:3677. doi: 10.3390/ijerph20043677
Slauson-Blevins, K., and Johnson, K. M. (2016). Doing gender, doing surveys? Women’s gatekeeping and Men’s non-participation in multi-actor reproductive surveys. Sociol. Inq. 86, 427–449. doi: 10.1111/soin.12122
Stevens, K., Davey, C., and Lassig, A. A. (2020). Association of weekly protected nonclinical time with resident physician burnout and well-being. JAMA Otolaryngol. Head Neck Surg. 146, 168–175. doi: 10.1001/jamaoto.2019.3654
Stimpfel, A. W., Liang, E., and Goldsamt, L. A. (2020). Early career nurse reports of work-related substance use. J. Nurs. Regul. 11, 29–35. doi: 10.1016/S2155-8256(20)30058-2
Stoltzfus, J. C. (2011). Logistic regression: a brief primer. Acad. Emerg. Med. 18, 1099–1104. doi: 10.1111/j.1553-2712.2011.01185.x
Tamminga, S. J., Emal, L. M., Boschman, J. S., Levasseur, A., Thota, A., Ruotsalainen, J. H., et al. (2023). Individual-level interventions for reducing occupational stress in healthcare workers. Cochrane Database Syst. Rev. 2023:CD002892. doi: 10.1002/14651858.CD002892.pub6
Tennant, R., Hiller, L., Fishwick, R., Platt, S., Joseph, S., Weich, S., et al. (2007). The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual. Life Outcomes 5:63. doi: 10.1186/1477-7525-5-63
Trousselard, M., Steiler, D., Dutheil, F., Claverie, D., Canini, F., Fenouillet, F., et al. (2016). Validation of the Warwick-Edinburgh mental well-being scale (WEMWBS) in French psychiatric and general populations. Psychiatry Res. 245, 282–290. doi: 10.1016/j.psychres.2016.08.050
Waddell, A., Kunstler, B., Lennox, A., Pattuwage, L., Grundy, E. A. C., Tsering, D., et al. (2023). How effective are interventions in optimizing workplace mental health and well-being? A scoping review of reviews and evidence map. Scand. J. Work Environ. Health 49, 235–248. doi: 10.5271/sjweh.4087
Wold, B., and Mittelmark, M. B. (2018). Health-promotion research over three decades: the social-ecological model and challenges in implementation of interventions. Scand. J. Public Health 46, 20–26. doi: 10.1177/1403494817743893
Keywords: academic conditions, job strain, mental health, psychological distress, resident, wellbeing
Citation: Nohales L, Fort E, Pelloux S, Coste C, Leblanc P, De Ternay J, Wallon M, Rolland B, Fassier J-B and BASIL Study Group (2024) Occupational, academic, and personal determinants of wellbeing and psychological distress in residents: results of a survey in Lyon, France. Front. Psychol. 15:1347513. doi: 10.3389/fpsyg.2024.1347513
Edited by:
Cornelia Sindermann, University of Stuttgart, GermanyReviewed by:
Sonja Mostert, University of Pretoria, South AfricaErmanno Vitale, Kore University of Enna, Italy
Copyright © 2024 Nohales, Fort, Pelloux, Coste, Leblanc, De Ternay, Wallon, Rolland, Fassier and BASIL Study Group. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ludivine Nohales, bHVkaXZpbmUubm9oYWxlc0BjaHUtbHlvbi5mcg==
 Ludivine Nohales
Ludivine Nohales Emmanuel Fort
Emmanuel Fort Sophie Pelloux3
Sophie Pelloux3 Martine Wallon
Martine Wallon