
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 04 April 2024
Sec. Psychology for Clinical Settings
Volume 15 - 2024 | https://doi.org/10.3389/fpsyg.2024.1336631
This article is part of the Research Topic Attachment, Trauma and Alexithymia View all 6 articles
Purpose: This study analyzes the relationship of alexithymia, childhood trauma, and body investment to non-suicidal self-injury (NSSI) behaviors in adolescents with depressive disorder and whether they have predictive and diagnostic value for non-suicidal self-injury (NSSI) behaviors in adolescents with depressive disorder.
Patients and methods: A total of 225 patients with a diagnosis of adolescent depressive disorder were included in the study and were divided into two groups according to the DSM-5 criteria: 98 cases without NSSI and 127 cases with NSSI. Compare the demographic data, 24-item Hamilton Depression Scale (HAMD-24), 20-item Toronto Alexithymia Scale (TAS-20), Childhood Trauma Questionnaire-Short Form (CTQ-SF), and Body Investment Scale (BIS) scores between two groups. Binary logistic regression was used to analyze the independent risk factors contributing to NSSI behaviors in adolescents with depression, and establish four predictive models. Based on the models’ predictive probability, the ROC curves were plotted to calculate the value of the predictive diagnostic effect.
Results: The group without NSSI had lower scores than the group with NSSI on HAMD-24 total score, TAS-20 total score, difficulty identifying feelings, difficulty describing feelings, and externally focused thinking, as well as lower scores on CTQ-SF total score, physical neglect, emotional neglect, physical abuse, and emotional abuse. In contrast, the BIS total score, body image feelings and attitudes, body care, and body protection factor scores were higher for the group without NSSI. The BIS body care factor score and the CTQ-SF emotional abuse factor score were significantly linked with adolescents diagnosed with depressive disorder who exhibited NSSI behaviors. These results provide a good diagnostic model for adolescents with depressive disorder.
Conclusion: Low levels of body care and childhood emotional abuse may independently contribute to the implementation of NSSI in adolescents with depressive disorder. Body investment and childhood trauma are valuable in diagnosing and predicting NSSI behaviors and should be considered as potentially important factors in clinical treatment.
Non-suicidal self-injury (NSSI) is deliberate injury to body tissues without suicidal intention, which occurs on five or more days within the past year (Buelens et al., 2020; van der Venne et al., 2023). The main forms include scratching, cutting the skin, pulling hair, and hitting oneself, with the most common form being cutting (Halpin and Duffy, 2020). Non-suicidal self-harm is a significant psychiatric problem among adolescents worldwide. During the DSM-5 revision process, NSSI was included as a disease diagnosis. This called for increased attention and more research into the NSSI among adolescents. A recent Meta-analysis found that the global lifetime prevalence of NSSI in children and adolescents is 22.1% (Lim et al., 2019). However, the lifetime prevalence of NSSI in clinical samples can be as high as 80% (Zetterqvist, 2015; Plener et al., 2016). Previous research indicates that depressive disorder and NSSI frequently co-occur (Liang et al., 2023). A survey conducted in China revealed that as many as 55.1% of NSSI patients were diagnosed with depression (Wang et al., 2021). Likewise, about 34.2% of Chinese young people with major depression had a history of self-injury (Kang et al., 2021). Some studies have reported that adolescents with depressive disorder accompanied by NSSI behaviors have significantly higher rates of suicidal ideation than adolescents without self-injurious behaviors (Hepp et al., 2021; Kim et al., 2022). With the increasing prevalence of NSSI in the adolescent population, it has become one of the leading causes of death in young people. Therefore, early identification of risk factors for NSSI in adolescents with depression can prevent adverse events such as death.
Nock’s (2010) integrative theoretical model proposed several psychological and social risk factors that contribute to the development of NSSI behaviors. These factors include both intrapersonal and interpersonal relationships. Several risk factors for NSSI have been identified, including alexithymia, childhood trauma, and low levels of body investment (Liu et al., 2018; Cipriano et al., 2020; Iskric et al., 2020). However, there is still much to be explored about how these factors interact and ultimately lead to the development of NSSI behaviors in adolescents. Alexithymia is a difficulty in regulating emotions, defined as a disorder characterized by a failure to recognize and describe feelings (Dong et al., 2023). Numerous studies have shown a strong association between alexithymia and NSSI (Ying et al., 2023; Zhang et al., 2023). In their study, Tang et al. (2022) discovered that alexithymia has a positive relationship with NSSI and that depression may act as a mediator between alexithymia and NSSI. In addition, Lüdtke et al. (2016) also concluded that alexithymia significantly predicts NSSI in female adolescent hospitalized patients. It is theorized patients who lack the language to express negative emotions (alexithymia) are more likely to express themselves by venting or hurting themselves (self-injury) (Raffagnato et al., 2020). In this respect, alexithymia and NSSI both serve as a pathway for expressing psychological and emotional problems in the adolescents.
Childhood trauma refers to the abusive and traumatizing experiences that an individual suffers before the age of 16. These experiences encompass five forms: physical abuse, emotional abuse, sexual abuse, emotional neglect, and physical neglect (Ying et al., 2023). Childhood trauma may be associated with self-injury in adolescents with depressive disorder. More than one-third of the population has reported experiencing adverse childhood experiences, which is more prevalent among adolescents diagnosed with depression (Zhang et al., 2020). According to Xie et al. (2018), 55.5% of adolescents with depression had suffered at least one form of child abuse. Several studies have suggested that childhood trauma is a risk factor for NSSI in adolescents (Brown and Plener, 2017; Sun et al., 2023). Nock’s (2010) comprehensive theoretical model of self-injury also supports this. According to the theory, many psychological and social factors play a mediating role in childhood trauma and NSSI. For example, in a study of medical students, social support was shown to mediate the relationship between childhood maltreatment and NSSI in only children (Xu et al., 2019). Huang et al. (2022) concluded that psychological sub-health partially mediates the relationship between childhood trauma and NSSI. Additionally, childhood trauma has a positive predictive on self-injury through psychological sub-health. These studies indicate that childhood trauma is another essential influence/predictor of NSSI among adolescents. However, existing reports on the association between different types of childhood trauma and self-injury are inconsistent (Thomassin et al., 2016; Baiden et al., 2017). In this paper, we will evaluate the predictive power of each maltreatment subtype on non-suicidal self-injury after accounting for all available covariates.
Body investment is another important factor that affects the occurrence and development of NSSI, referring to the importance of the body in cognition, behavior and emotion in one’s self-assessment (Marco et al., 2018). This paper employs the Body Investment Scale (BIS) to evaluate the level of body investment in adolescents with depressive disorder. The Body Investment Scale comprises four dimensions: body feelings, body touch, body protection, and body care (Orbach and Mikulincer, 1998). Body investment is associated with self-preservation and represents an attraction to life. This implies active body care and protection. Specifically, individuals may reduce their body investment when experiencing psychological pain or trauma. Such a change influences body’s perception and experience, which may lead to self-harm behaviors (Brausch et al., 2021). Duggan et al. (2013) found that negative attitudes and feelings about the body may be predictors of self-injury and suicide attempts. Research has shown that ninth graders with a history of self-injury and body dissatisfaction are three times more likely to repeat self-injury than those without a history of self-injury (Brunner et al., 2007). Based on this evidence, negative body investment could be a significant factor in self-injury and provides new perspectives for understanding NSSI. To the best of our knowledge, this study is the first cross-sectional research that considers alexithymia, child maltreatment, and body investment as predictors of NSSI in adolescents with depressive disorder.
Therefore, this study aimed to exam the diagnostic and predictive power of alexithymia, childhood trauma, and body investment on NSSI in adolescents with depressive disorder. Based on the available evidence, we propose the following hypotheses: first, alexithymia and childhood trauma are risk factors for NSSI in adolescents with depressive disorder, and body investment is a protective factor for it; Secondly, alexithymia, childhood trauma, and body investment can predict NSSI in adolescents with depressive disorder.
A total of 225 outpatients or hospitalized adolescents with depressive disorder were included in this study. All participants were recruited through convenience sampling from the Chaohu Hospital of Anhui Medical University (Hefei, Anhui, China) and the Second Affiliated Hospital of Anhui Medical University (Hefei, Anhui, China) between January 2022 and June 2023. Both hospitals are tertiary hospitals directly affiliated with Anhui Medical University, wherein Chaohu Hospital is the psychiatric center of Anhui Province, and both have a large number of adolescents with depressive disorder. Participants must meet the following criteria: (a) 11–19 years old; (b) diagnosed individually by a chief psychiatrist and an attending physician, according to the diagnostic criteria for depressive disorder in the Diagnostic and Statistical Manual of Mental Disorder, fifth edition (DSM-5); (c) the 24-item Hamilton Depression Scale (HAMD-24) score ≥ 8; and (d) able to cooperate in completing relevant questionnaires and scale evaluations for this study. Exclusion criteria: (a) Presence of co-morbidity with other mental disorder, including neurocognitive disorder, substance-related and addiction disorder, schizophrenia, delusional disorder, schizoaffective disorder, transient psychotic disorder, bipolar disorder, intellectual disorder, autism spectrum disorder, eating disorder, borderline personality disorder, hair-pulling fetishism, stereotypical self-injury, and grasping disorder. (b) Presence of co-morbidities with organic brain disorder or other physical diseases; (c) Presence of religious self-injury or customary self-injury. This study was approved by the Ethics Committee of Chaohu Hospital of Anhui Medical University (KYXM-202201-003). All participants and legal guardians gave written consent.
The patient and their legal guardian sign an informed consent form when the patient meets the inclusion criteria and expresses a willingness to participate. Subsequently, the patient was invited to a quiet room for a face-to-face meeting with a psychiatric attending physician and a postgraduate psychiatry student. A self-made general information questionnaire was used to collect data on patients’ age, gender, education level, whether they were the only child, parents’ marital status, family financial situation, history of smoking, and alcohol consumption. NSSI presence or absence is evaluated using the DSM-5 diagnostic criteria for NSSI behaviors. NSSI is defined by fulfilling the criteria: The patient has engaged in three or more non-suicidal self-injury behaviors within the past six months, with at least one occurrence in the last month. The standardized self-report scale was completed autonomously by all participants. Any ambiguities were explained by the interviewer. Then, the questionnaires were coded, and the answers were entered into EpiData before they were exported to a form. Finally, two graduate students in psychiatry reviewed and organized the data.
A general information questionnaire was self-administered to collect data on participants’ gender, age, level of education, only child, parents’ marital status, father’s level of education, mother’s level of education, family economic status, active smoking, and active drinking.
Bagby et al. (1994) developed the scale as a standardized self-report questionnaire for assessing the presence and severity of alexithymia. The scale includes 20 items grouped into 3 dimensions: difficulty identifying feelings, difficulty describing feelings, and externally focused thinking. The rating is based on a 5-point Likert scale, ranging from ‘1 strongly disagree to 5 strongly agree’. The total score of this scale ranges from 20 to 100, with ≤ 50 being no alexithymia, 51–60 being possible alexithymia, and ≥ 61 being the presence of alexithymia, with higher scores representing more severe alexithymia (Franz et al., 2008). The Chinese version of this scale has good reliability and validity indicators (Zhu et al., 2007). In this study, the Cronbach’s α coefficient was 0.83.
The CTQ-SF is a 28-item self-report questionnaire used to assess individuals’ experiences of childhood abuse and neglect (Bernstein et al., 2003). This questionnaire is composed of five dimensions: emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect. Responses are rated on a 5-point Likert scale ranging from 1 (never) to 5 (always), with higher scores indicating greater severity of abuse and trauma. Each dimension can be categorized as none, mild, moderate or severe based on the score, and a trauma severity of mild and above in any dimension can be defined as positive for trauma in that dimension (Davidson et al., 2009). The Chinese version of the questionnaire has good reliability among Chinese adolescents, with a Cronbach′s α coefficient of 0.73 in this study (He et al., 2019).
The BIS is a brief self-report scale that consists of 24 items to assess emotional investment in the body (Orbach and Mikulincer, 1998). The scale contains four subscales: feelings and attitudes toward the body (for example, “I feel anger toward my body”), comfort in physical touch (for example, “I enjoy physical contact with others”), body care (for example, “I pay attention to my appearance”), and body protection (for example, “Sometimes I purposely injure myself”). Each subscale consists of six items. This scale is scored on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree). The scores for the four independent subscales were obtained by averaging all entries for each respective subscale. Scores from all subscales were summed to obtain a total score, with lower scores indicating lower emotional investment in the body. The scale is not available in Chinese, so the English translation was used. Orbach and Mikulincer (1998) validated in adolescents and found good internal consistency for the original scale. In this study, the Cronbach’s α coefficient was 0.78.
The HAMD-24 was developed by Hamilton (1960) in 1960 and is widely used for clinical assessment of depressive states. This study used a 24-item version with seven factors: anxiety/somatization, weight loss, cognitive impairment, day/night changes, retardation, sleep disturbance, and despair. The scale is based on a 5-point system ranging from 0 to 4, with a total of 96 points. A score of less than 8 points indicates a lack of depressive symptoms, while scores between 8–19 points indicate possible depression. Scores between 20–34 points indicate mild or moderate depression, and scores of 35 points or higher indicate severe depression. HAMD-24 has good reliability and validity, and the Cronbach’s α coefficient in this study was 0.90.
The study’s data underwent statistical analysis using SPSS 26.0. We performed descriptive statistics on the NSSI and non-NSSI groups and calculated the differences between these two groups. Conduct a normality test on the measurement data. If it conforms to the normal distribution, use represents, independent samples t-test is used for comparison between groups. Since the TAS-20, CTQ-SF, and BIS all have multiple subscales, we will utilize one-way multivariate ANOVA to compare the scores of these scales between groups. Count data were expressed as frequencies and percentages, while comparisons between groups were performed using the chi-square test. Moreover, binary logistic regression analyses were conducted to examine the risk of independent effects of dysphoria, childhood trauma and physical commitment on NSSI behaviors after adjusting for general demographic information such as gender, age, education, only-child status, parental marital status, parental literacy, and family economic status in order to create predictive models. Based on the predictive probabilities of the models, we plotted the receiver operator characteristic (ROC) curves to evaluate the diagnostic ability of different models to implement the NSSI for adolescents with depressive disorder. Specifically, firstly, the Youden index was computed by subtracting the ROC curve’s Y-axis value from its X-axis value. Subsequently, the maximal Youden index value was found, indicating the optimal critical diagnostic value, also known as the cutoff value, of the ROC curve. Lastly, the corresponding sensitivity and specificity were determined and reported based on the optimal critical value.
A comparison of general demographic data between adolescent depression patients with and without NSSI behaviors is provided in Table 1. Out of the total of cases, there were 98 (43.6%) in the group without NSSI and 127 (56.4%) in the group with NSSI. No statistically significant differences were found between the two groups with regards to only child status, parents’ marital status, father’s education, mother’s education, family economic status, and active smoking (p > 0.05). However, significant differences were observed in gender (χ2/t = 5.13, p = 0.024), age (χ2/t = 2.01, p = 0.046), education (χ2/t = 8.73, p = 0.013), and active drinking (χ2/t = 4.73, p = 0.030). Table 2 shows the comparison of the scale scores for the group without NSSI and the group with NSSI. Statistically significant results were obtained for the total and factor scores for the scale, except for body touch in BIS (F = 3.86, p = 0.051) and sexual abuse in CTQ-SF (F = 1.70, p = 0.194). Specifically, the group without NSSI showed significant differences in HAMD-24 total score (t = −3.89, p < 0.001), TAS-20 total score (F = 11.92, p = 0.001), difficulty identifying feelings (F = 6.74, p = 0.010), difficulty describing feelings (F = 7.53, p = 0.007), externally focused thinking (F = 4.26, p = 0.040), CTQ-SF total score (F = 16.97, p < 0.001), physical neglect (F = 5.73, p = 0.017), emotional neglect (F = 4.06, p = 0.045), physical abuse (F = 7.14, p = 0.008) and emotional abuse (F = 24.21, p < 0.001) were lower than the group with NSSI. The BIS total score (F = 52.32, p < 0.001) and its three factor scores for body feelings (F = 26.40, p < 0.001), body care (F = 78.25, p < 0.001), and body protection (F = 19.72, p < 0.001) were higher than the scores of the group with NSSI.
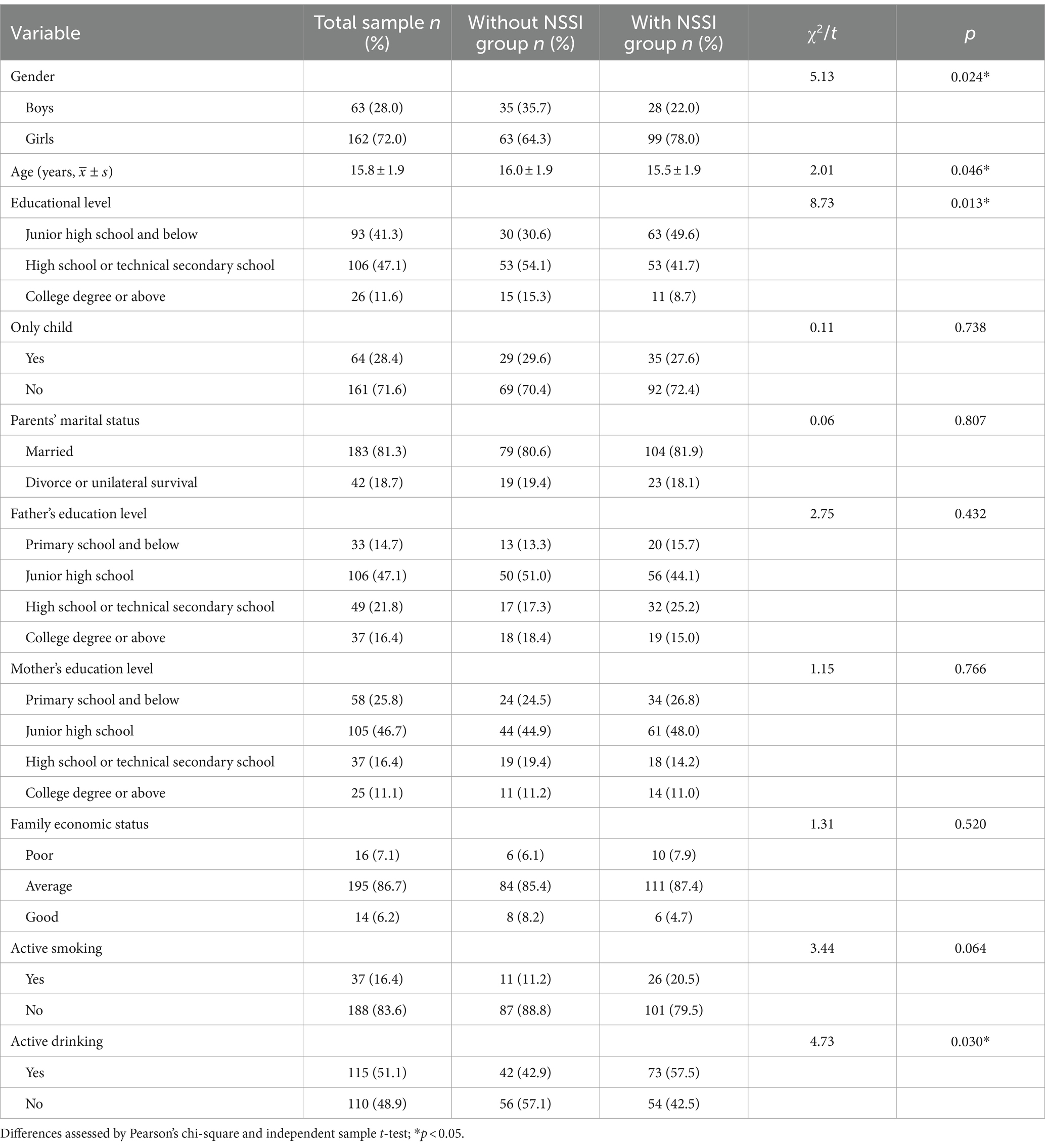
Table 1. Comparison of general demographic data between the group without and with non-suicidal self-injury (NSSI) in adolescents with depressive disorder (n = 225).
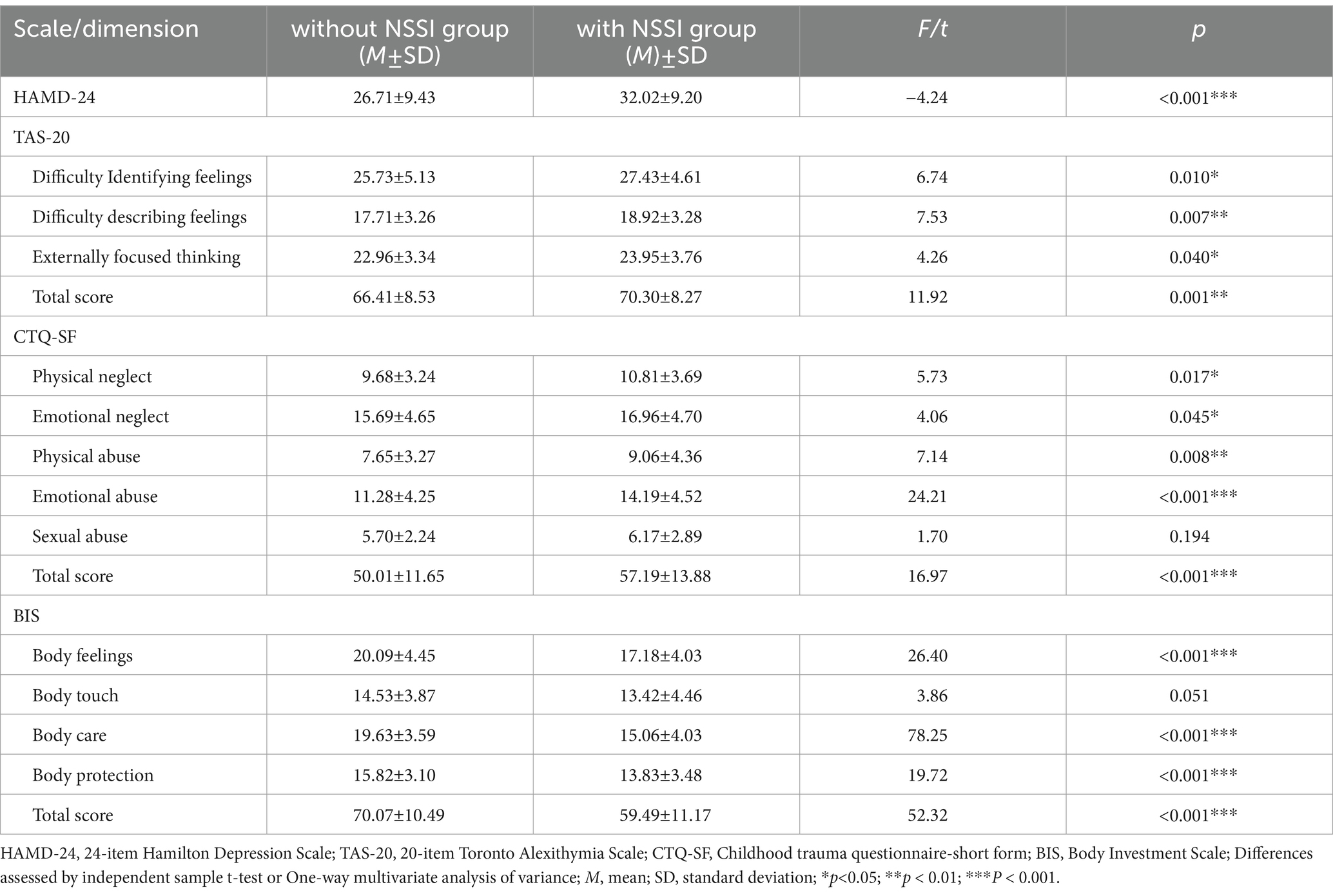
Table 2. Comparison of scale scores between the group with and without non-suicidal self-injury (NSSI) in adolescents with depressive disorder (n=225).
In multivariate analyses, we used four binary logistic regression models to analyze the relationship between predictor variables and the NSSI among adolescents with depressive disorder. Model 1 included general demographic data as predictor variables for analysis. The model was found to be significant (χ2 = 23.27, p < 0.001) with variances of 0.10 (Cox and Snell R2) and 0.13 (Nagelkerke R2). Among the variables, gender, level of education, and active drinking significantly predicted NSSI behaviors (p < 0.05). Model 2 included three factors from the TAS-20 (difficulty identifying feelings, difficulty describing feelings, and externally focused thinking) and 24-HAMD scores in addition to the variables in Model 1. The model was significant (χ2 = 35.60, p < 0.001), and the variance increased to 0.15 (Cox and Snell R2) and 0.20 (Nagelkerke R2). Among the variables, education level, active drinking, and 24-HAMD significantly predicted NSSI behaviors (p < 0.05). Model 3 included five factors from the CTQ-SF (physical neglect, emotional neglect, physical abuse, emotional abuse and sexual abuse) in addition to the variables in Model 2. The model was significant (χ2 = 47.05, p < 0.001), and the variance increased to 0.19 (Cox and Snell R2) and 0.25 (Nagelkerke R2). Among the variables, education level, active drinking, 24-HAMD and emotional abuse significantly predicted NSSI behaviors (p < 0.05). Model 4 included four factors from the BIS (body feelings, body touch, body care, and body protection) in addition to the variables in Model 3. The final logistic regression model was significant (χ2 = 70.85, p < 0.001), and the variance increased to 0.27 (Cox and Snell R2) and 0.36 (Nagelkerke R2). Among these variables, emotional abuse (OR = 1.08, 95% CI = 1.00–1.16, p = 0.044) and body care (OR = 0.76, 95% CI = 0.67–0.83, p < 0.001) significantly predicted NSSI behavior in adolescents with depressive disorders (Table 3).
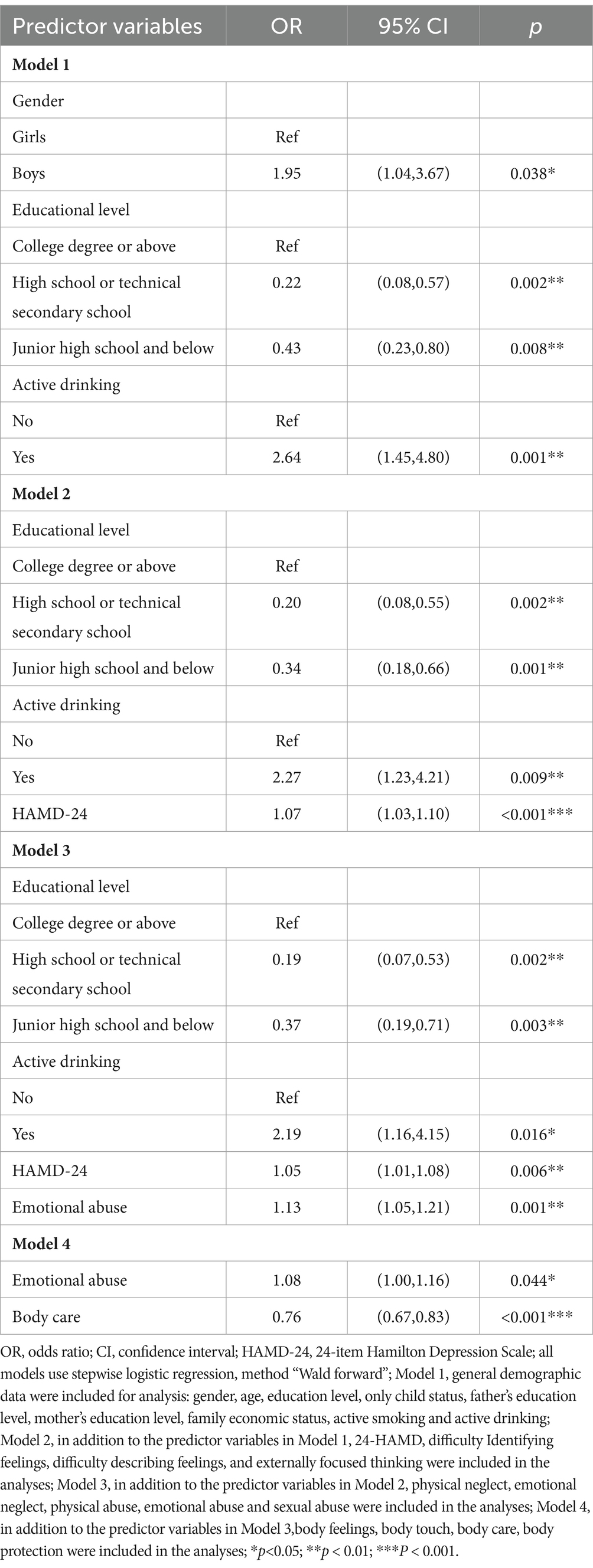
Table 3. Logistic regression predicting non-suicidal self-injury (NSSI) behaviors in adolescents with depressive disorder (n=225).
Four ROC curves were plotted based on the predictive models described above. The area under the ROC curve plotted based on model 1 was 0.66 (SE = 0.04, 95%CI = 0.59–0.73, p < 0.001),with an optimal critical point of 0.50, corresponding to sensitivity = 75.6% and specificity = 51.0% (Figure 1A). The area under the ROC curve plotted based on model 2 was 0.73 (SE = 0.03, 95%CI = 0.67–0.80, p < 0.001),with an optimal critical point of 0.54, corresponding to sensitivity = 73.2% and specificity = 65.3%(Figure 1B). The area under the ROC curve plotted based on model 3 was 0.76 (SE = 0.03, 95%CI = 0.70–0.82, p < 0.001),with an optimal critical point of 0.66, corresponding to sensitivity = 58.3% and specificity = 85.7% (Figure 1C). The area under the ROC curve plotted based on model 4 was 0.82 (SE = 0.03, 95%CI = 0.76–0.87, p < 0.001),with an optimal critical point of 0.57, corresponding to sensitivity = 75.6% and specificity = 79.6%(Figure 1D).
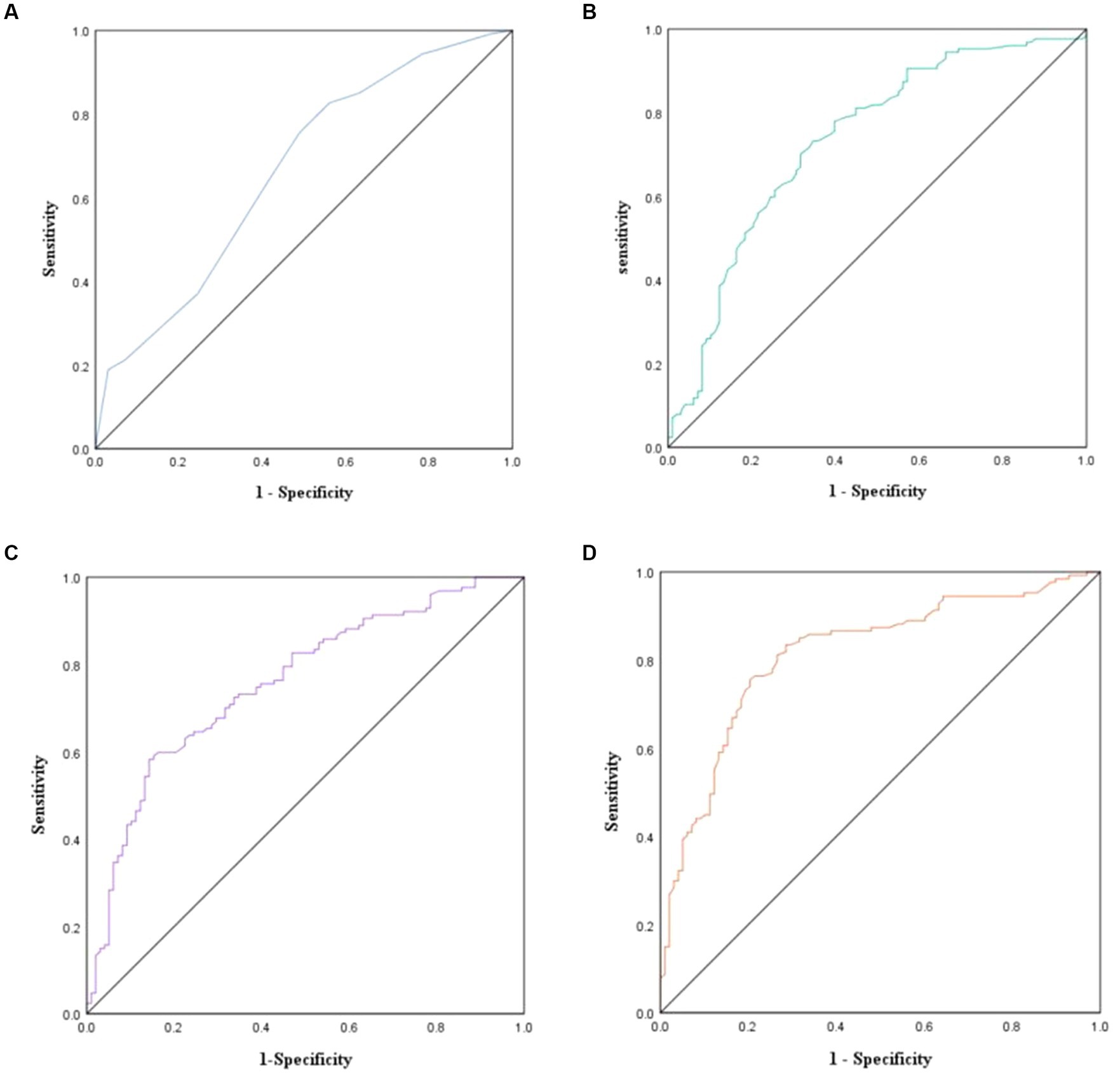
Figure 1. Predictive models for adolescents with depressive disorders with and without non-suicidal self-injurious (NSSI) behaviors ROC curves (n = 225). (A) ROC curve analysis based on model 1; (B) ROC curve analysis based on model 2; (C) ROC curve analysis based on model 3; (D) ROC curve analysis based on model 4. ROC, Receiver Operating Characteristic.
This study explored the predictive effects of alexithymia, childhood trauma, and body investment on NSSI behaviors in adolescents with depression and evaluated the diagnostic value of these factors for the occurrence of NSSI in adolescents with depression. Adolescents with depressive disorder and NSSI scored higher than those with depressive disorder without NSSI on HAMD-24, TAS-20 total score, and all its dimensions, CTQ-SF total score, and the other four dimensions except sexual abuse. By contrast, all subscale scores on the BIS, except for body touch, were lower in the group with NSSI compared to the group without NSSI. Our findings support the first hypothesis and are consistent with previous research indicating that childhood trauma and alexithymia increase the risk of NSSI (Kautz et al., 2020; Zhao et al., 2023), while bodily investment serves as a protective factor against NSSI (Pérez et al., 2018). In the final prediction model, childhood trauma and body investment were significant predictors of NSSI behavior, which consistent with previous research (Cipriano et al., 2020; Kautz et al., 2020). Unexpectedly, none of the three narcissistic factors were predictors of NSSI. These findings partially support the second hypothesis.
This study analyzed the general demographic characteristics of depressed adolescents with and without non-suicidal self-injury (NSSI) behaviors. The results indicate that the percentage of girls in the group with NSSI was significantly higher than in the group without NSSI, while the age of adolescents in the former group was significantly lower. Correspondingly, there was a significant difference in the level of education between the two groups. This gender difference supports the results of a meta-analysis that identifies female gender as a risk factor for NSSI (Rahman et al., 2021). However, it has also been demonstrated that gender does not have a significant effect on self-injury (Swannell et al., 2014). The difference in conclusions may be attributed to variations in the definition and assessment of self-injury across different studies (Bresin and Schoenleber, 2015). Males are more likely than females to use more violent methods of self-injury, such as hitting and burning (Sornberger et al., 2012). It is important to note that these methods used by males are often not included in the definition of self-injury. Additionally, due to the smaller sample size of males, precise calculations of male self-harm rates can be challenging. A systematic review of the effects of age on self-injury reported a gradual increase in self-injurious behaviors between 12.5 and 15 years of age, followed by a peak and then a decline (Plener et al., 2015). Our findings regarding the age differences between the two groups of adolescents support this perspective. However, it remains difficult to determine how self-injury in adolescents changes with age. Future research should conduct additional longitudinal studies to explore changing patterns of self-injury at all ages from early adolescence to early adulthood. This finding was consistent with previous research. The group with NSSI exhibited significantly higher levels of active drinking compared to the group without NSSI. This finding supports the conclusion that high alcohol abuse is a significant risk factor for repetitive self-injury (Martiniuk et al., 2015). The reason for this may be that adolescents with self-injurious behaviors are more likely to use alcohol to relieve stress.
The study found that adolescents in the group with NSSI had significantly higher scores on the TAS-20 total and subscales than those in the group without NSSI. This indicates that alexithymia may be a risk factor for NSSI behaviors in adolescents with depressive disorders. In a longitudinal study of community-based adolescents, it was found that alexithymia scores at baseline were significantly and positively associated with self-injury. Additionally, these scores predicted self-injurious behaviors 5 months later (Garisch and Wilson, 2015). The connection between alexithymia and non-suicidal self-injury can be explained by the emotion regulation model of self-injury. This model suggests that self-injury is a coping mechanism used by individuals to alleviate or reduce negative emotions and free themselves from unwanted emotional states (Klonsky, 2007). Based on this, we should consider alexithymia as an important target for the treatment of non-suicidal self-injurious behaviors in adolescents. Research indicates that mindfulness-based interventions may be an effective approach to alleviate alexithymia (Norman et al., 2019). However, individuals with alexithymia often exhibit primitive defenses and poor empathy, which can make it challenging to achieve positive outcomes with traditional psychotherapy (Casagrande et al., 2020).
Childhood trauma has been associated with both the lifetime prevalence of NSSI and the recent rise in self-injurious behaviors in community samples of adolescents and clinical samples in adults (Weierich and Nock, 2008; Swannell et al., 2012; Thomassin et al., 2016). Childhood trauma is an independent remote risk factor for NSSI that may cause internal personal vulnerabilities (e.g., emotional regulation difficulties) and interpersonal vulnerabilities (e.g., poor communication skills), thereby increasing the risk of engaging in NSSI (Hooley and Franklin, 2018). More specifically, childhood trauma can lead to an increase in negative emotional responses and even difficulty controlling such emotional responses. To cope with this response, adolescents often resort to using the inappropriate method of NSSI. This is well-supported by the four-function model of self-injury, the biosocial theory of mood disorder, and the integrative theoretical model of the development and maintenance of NSSI (Nock, 2010; Courtney-Seidler et al., 2014). Childhood maltreatment is associated with subsequent neurobiological abnormalities. As adolescents are in a sensitive period of development, childhood trauma can negatively impact them, affecting structural brain development (Kim et al., 2020),diminished HPA axis responses, and circulating inflammatory factors (Klaassens et al., 2009). Due to these neurobiological vulnerabilities, adolescents who have experienced childhood trauma are more likely to develop inadequate coping mechanisms, including NSSI (Westlund Schreiner et al., 2020).
Orbach et al. (1995) suggested that a person’s attitude toward protecting their body and investment to their body are key factors in understanding NSSI. He believed that indifference and dissatisfaction with the body leads to a lack of bodily pleasure, which manifests itself in a reduced sensitivity to physical pain. Therefore, when individuals are suffering internally, they are more likely to engage in NSSI and cause harm to their bodies. Hooley et al. (2010) found in a related study that community-based adolescents with a history of self-injury had significantly higher pain tolerance. The longer an individual tolerates pain, the more intense their self-criticism becomes, thereby creating a negative body image. According to clinical experience, Walsh (2012) argues that a person’s relationship and attitude toward their body play a central role in the initiation and maintenance of NSSI. Ross et al. (2009) presented qualitative evidence that adolescents who engaged in NSSI reported more discomfort and dissatisfaction with their bodies. These individuals perceived that their bodies were out of control when compared to adolescents who did not engage in NSSI. It is widely acknowledged that NSSI often takes place in the early to middle stages of adolescence (He et al., 2023). Adolescence is the period when the body is believed to become more significant in one’s self-concept (Markey, 2010),which helps to understand why NSSI manifests itself primarily during this developmental stage. Thus, low levels of bodily investment may be an important risk factor for NSSI and support the inclusion of body investment in etiological models of NSSI.
The logistic regression analyses indicated that none of the factors of alexithymia were significant predictors of NSSI. Adolescents suffering from alexithymia are unable to express their negative emotions verbally and rely on NSSI behaviors to hurt themselves in coping with their psychological pain (Cerutti et al., 2018). This is an unanticipated discovery given the connection between alexithymia and NSSI, as demonstrated in earlier research (Lee, 2016). One reason for this may be the high prevalence of alexithymia in our sample, both in the group with and without NSSI. The difference is likely because we chose young people with depressive disorder as our research participants. Patients with depressive disorder tend to have higher TAS-20 scores and show higher levels of alexithymia (Bordalo and Carvalho, 2022). Furthermore, a study has reported that the relationship between alexithymia and NSSI is fully mediated by depression (Garisch and Wilson, 2010). Consequently, in regression models predicting NSSI behaviors, when both alexithymia and depression are included, alexithymia is no longer a significant predictor. It is possible that depression has a more significant role in NSSI than alexithymia based on this. Although, we cannot ignore the role of alexithymia in non-suicidal self-injury in adolescents with depressive disorders. This is because individuals with depression who also have alexithymia are more likely to engage in self-injury as a way of expressing their feelings or getting rid of unpleasant emotional experiences (Iskric et al., 2020).
In line with our hypothesis, childhood maltreatment was a notable predictor of NSSI behaviors, which corresponds with the existing literatures (Bunting et al., 2023; Kyei, 2023). Interestingly, there was no significant variation in scores for sexual abuse between the two groups. However, adolescents in the group with NSSI scored slightly higher than those in the group without NSSI. This may be due to the fact that under the influence of traditional Chinese culture, participants were unwilling to reveal excessive information about sexual abuse when accomplishing the scale. In addition, parental education related to sexual bullying and societal awareness of this problem have considerably risen in recent years, leading to a positive outcome in reducing sexual violence among teenagers. After controlling for all available covariates, emotional abuse continued to be an independent risk factor for NSSI in the CTQ-SF. This finding is in keeping with a previous study (Zhang et al., 2022). Similar to our findings, Kang et al. (2018) discovered that emotional abuse was a significant predictor of self-injury in a sample of Chinese adolescents. In contrast, physical abuse was not found to have a substantial impact. Emotional abuse, also called psychological abuse, is a type of emotional harm, unlike physical abuse. It comprises a recurrent behavioral pattern which involves criticism, threats, humiliation, blame, insults, and so on, directed toward children. According to Nock’s (2009) integrative model, experiences of emotional abuse can interfere with a child’s capacity to control intense negative emotions like anger, sadness, fear or shame. Subsequently, the child may adopt NSSI behaviors to assuage these emotions. Previous studies indicated that there is a positive association between childhood emotional abuse and adolescent self-injury (Marco et al., 2018; Zhang et al., 2020). A meta-analysis found that people with a history of childhood emotional abuse had a 3.03 times higher risk for NSSI compared to people with no emotional abuse (Liu et al., 2018). Despite this significance, emotional abuse has garnered less attention in prior research and clinical practice on NSSI than sexual and physical abuse. There is evidence that the pathogenic effects of emotional abuse and other subtypes of abuse on mental health outcomes are similar (Etain et al., 2010; Liu, 2017). As emotional abuse is the most common form of abuse, neglecting emotional abuse may lead to more serious consequences (Stoltenborgh et al., 2015). It is evident that additional attention should be given to emotional abuse within risk assessment and research on NSSI.
Research indicates that negative experiences and perceptions of the body can lead to bodily devaluation and bodily detachment (Muehlenkamp et al., 2013). Aoki et al. (2023) found that trauma can cause individuals to dissociate from their bodies and that NSSI behaviors can be effectively discontinued through the acquisition of self-understanding and stress coping skills. These studies support the role of body attitudes and experiences in the development of non-suicidal self-injury. After controlling for all available covariates, body care remained the most significant predictor of NSSI. Body care refers to taking care of one’s body through enjoyable behaviors such as bathing or using body care products that indicate how much care and attention one pays to one’s body (Brausch and Muehlenkamp, 2007). Body care not only predicts NSSI directly, but it also acts as a mediator for NSSI behaviors. A model of body investment mediating self-injury suggests that all four aspects of body investment mediate the relationship between negative emotions and NSSI in adolescents. This means that adolescents who have negative perceptions of their bodies or neglect them may have a higher likelihood of engaging in NSSI when faced with an overwhelming, aversive emotional state (Muehlenkamp and Brausch, 2012). Body care may be a significant vulnerability factor to consider when attempting to comprehend the risk of NSSI. However, there are also studies that come to the opposite conclusion. A study by Marco et al. (2018) on body investment in patients with eating disorder discovered that body care did not significantly differentiate between patients with self-injury or suicidal ideation. Instead, the remaining three aspects of body investment were independent factors influencing self-injury. Reasons for this discrepancy may include two aspects. Firstly, patients diagnosed with eating disorder predominantly exhibit body checking and body avoidance behaviors in their body care, which are not included in the body care subscale. Secondly, it is crucial to note that our research was conducted on adolescents with depression, and the two research populations are distinct. Yet, there are fewer previous studies related to body care in body investment, and the mechanisms by which body care affects the performance of NSSI in adolescents with depressive disorder need further investigation. In conclusion, we found that low levels of body care were significant predictors of NSSI in adolescents with depressive disorder. Therefore, reconnecting an individual to their body could prove a vital approach in reducing NSSI behaviors. There are studies suggesting that Positive Mindfulness Training’s therapeutic or body acceptance methods have a useful effect on NSSI (Mehlum et al., 2014; Dibaj et al., 2023). In both a 1-year and 3-year follow-up of adolescents exhibiting self-injurious behaviors, Mehlum et al. discovered that those treated with Dialectical Behavior Therapy to Adolescents (DBT-A) showed a substantial and persistent reduction in the frequency of self-injurious behaviors over the long term compared to those receiving Enhanced Usual Care (EUC) (Mehlum et al., 2016, 2019). This indicates that DBT-A could be a viable substitute treatment choice for teenagers experiencing repetitive NSSI behaviors. We ought to assist adolescent patients with low-level investment in the body and concomitant NSSI behaviors to carry out this training, thereby significantly reducing the feelings of body transcendence or objectification required to carry out NSSI.
We applied ROC curves to evaluate the diagnostic efficacy of alexithymia, childhood trauma, and body investment in predicting NSSI behaviors in adolescents with depressive disorder. The results indicate a continuous increase in the area under the ROC curves from Model 1 to Model 4. The sensitivity and specificity of the ROC curves drawn from Models 1 and 2 were smaller than this of the ROC curve drawn from Model 4. Although the ROC curve based on Model 3 had the highest sensitivity among all ROC curves, its specificity was lower. In conclusion, among all ROC curves, the ROC curve based on model 4 was significantly better than the other three curves. This suggests that childhood trauma and body investment have a better predictive diagnostic value for NSSI behaviors in adolescents with depressive disorder. This study’s results have clinical relevance, providing a theoretical foundation for professionals to diagnose NSSI behaviors among depressed adolescents. However, this study primarily focuses on the diagnostic utility of NSSI in adolescent depression patients. The applicability of this model to other NSSI co-morbid patient populations, such as social phobia, post-traumatic stress disorder, borderline personality disorder, and eating disorder, requires further validation through additional research.
There are some limitations in this study. Firstly, the present study was cross-sectional and could not establish a causal relationship between childhood trauma, body investment and the occurrence of NSSI behaviors in depressed adolescents. Secondly, a healthy control group was not established due to difficulties in finding suitable adolescents who had never engaged in self-injury. This was primarily because the sample collection was conducted among outpatient or inpatient patients. Thirdly, we assessed the NSSI using clinical judgment instead of a structured interview, which may introduce diagnostic bias. Also, we have not included other potential risk factors for self-injury, such as borderline personality traits, mood disorder or other negative emotional states such as anxiety and anger. So, we cannot rule out the possibility that these factors influenced the results of the study. Finally, the data for this survey was collected via questionnaire completion, making recall bias inevitable. Additionally, sensitive questions were included, potentially influencing the accuracy of the information provided by participants. Future research should include more extensive longitudinal studies with independent samples from diverse populations to validate the associations between emotional indifference, childhood trauma, body investment, and NSSI. Additionally, potential mediating or moderating effects among the variables should be further analyzed.
In summary, the study findings indicate that there is an association between NSSI behaviors in adolescent depression and alexithymia, childhood trauma, and body investment. In logistic regression and ROC analyses, emotional abuse from childhood trauma and body care in terms of body investment were significant predictors of NSSI in this population, with good diagnostic value, allowing us to gain a deeper understanding of the onset and progression of the disease. Therefore, when treating adolescent with NSSI, it is important to consider the role of childhood trauma and levels of body investment in NSSI behaviors. In particular, the significance of body investment should be acknowledged and appreciated as a potential important clinical treatment for adolescent NSSI behaviors. This will enable early intervention to decrease or prevent the perpetration of NSSI behaviors in adolescents with depressive disorder.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
PC: Conceptualization, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. RP: Conceptualization, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. QY: Conceptualization, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. RZ: Conceptualization, Investigation, Writing – review & editing. MY: Conceptualization, Investigation, Writing – review & editing. XZ: Conceptualization, Investigation, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Scientific Research Program for Graduate Students of Universities in Anhui Province in China (YJS20210316).
The authors sincerely thank Chaohu Hospital of Anhui Medical University and the Second Affiliated Hospital of Anhui Medical University for their help. We would also like to thank all participants for their active participation.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
NSSI, Non-suicidal self-injury; HAMD-24, 24-item Hamilton Depression Scale; CTQ-SF, Childhood Trauma Questionnaire-Short Form; BIS, Body Investment Scale; TAS-20, 20-item Toronto Alexithymia Scale; ROC, Receiver Operating Characteristic.
Aoki, S., Kogayu, N., and Ono, S. (2023). Persistence and cessation of nonsuicidal self-injury under psychotherapy. Rorschachiana. doi: 10.1027/1192-5604/a000171
Bagby, R. M., Parker, J. D., and Taylor, G. J. (1994). The twenty-item Toronto alexithymia scale—I. Item selection and cross-validation of the factor structure. J. Psychosom. Res. 38, 23–32. doi: 10.1016/0022-3999(94)90005-1
Baiden, P., Stewart, S. L., and Fallon, B. (2017). The role of adverse childhood experiences as determinants of non-suicidal self-injury among children and adolescents referred to community and inpatient mental health settings. Child Abuse Negl. 69, 163–176. doi: 10.1016/j.chiabu.2017.04.011
Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., Ahluvalia, T., et al. (2003). Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl. 27, 169–190. doi: 10.1016/S0145-2134(02)00541-0
Bordalo, F., and Carvalho, I. P. (2022). The role of alexithymia as a risk factor for self-harm among adolescents in depression–a systematic review. J. Affect. Disord. 297, 130–144. doi: 10.1016/j.jad.2021.10.029
Brausch, A. M., and Muehlenkamp, J. J. (2007). Body image and suicidal ideation in adolescents. Body Image 4, 207–212. doi: 10.1016/j.bodyim.2007.02.001
Brausch, A. M., Nichols, P. M., Laves, E. H., and Clapham, R. B. (2021). Body investment as a protective factor in the relationship between acquired capability for suicide and suicide attempts. Behav. Ther. 52, 1114–1122. doi: 10.1016/j.beth.2021.02.008
Bresin, K., and Schoenleber, M. (2015). Gender differences in the prevalence of nonsuicidal self-injury: a meta-analysis. Clin. Psychol. Rev. 38, 55–64. doi: 10.1016/j.cpr.2015.02.009
Brown, R. C., and Plener, P. L. (2017). Non-suicidal self-injury in adolescence. Curr. Psychiatry Rep. 19, 1–8. doi: 10.1007/s11920-017-0767-9
Brunner, R., Parzer, P., Haffner, J., Steen, R., Roos, J., Klett, M., et al. (2007). Prevalence and psychological correlates of occasional and repetitive deliberate self-harm in adolescents. Arch. Pediatr. Adolesc. Med. 161, 641–649. doi: 10.1001/archpedi.161.7.641
Buelens, T., Luyckx, K., Kiekens, G., Gandhi, A., Muehlenkamp, J. J., and Claes, L. (2020). Investigating the DSM-5 criteria for non-suicidal self-injury disorder in a community sample of adolescents. J. Affect. Disord. 260, 314–322. doi: 10.1016/j.jad.2019.09.009
Bunting, L., McCartan, C., Davidson, G., Grant, A., Mulholland, C., Schubotz, D., et al. (2023). The influence of adverse and positive childhood experiences on young people's mental health and experiences of self-harm and suicidal ideation. Child Abuse Negl. 140:106159. doi: 10.1016/j.chiabu.2023.106159
Casagrande, M., Boncompagni, I., Forte, G., Guarino, A., and Favieri, F. (2020). Emotion and overeating behavior: effects of alexithymia and emotional regulation on overweight and obesity. Eating Weight Disord. 25, 1333–1345. doi: 10.1007/s40519-019-00767-9
Cerutti, R., Zuffianò, A., and Spensieri, V. (2018). The role of difficulty in identifying and describing feelings in non-suicidal self-injury behavior (NSSI): associations with perceived attachment quality, stressful life events, and suicidal ideation. Front. Psychol. 9:318. doi: 10.3389/fpsyg.2018.00318
Cipriano, A., Cella, S., and Cotrufo, P. (2020). Non-suicidal self-injury among Italian adolescents: the role of parental rejection, self-concept, anger expression, and body investment. Clin. Neuropsychiatry 17, 330–338. doi: 10.36131/cnfioritieditore20200602
Courtney-Seidler, E. A., Burns, K., Zilber, I., and Miller, A. L. (2014). Adolescent suicide and self-injury: deepening the understanding of the biosocial theory and applying dialectical behavior therapy. Int. J. Behav. Consult. Ther. 9, 35–40. doi: 10.1037/h0101638
Davidson, G., Shannon, C., Mulholland, C., and Campbell, J. (2009). A longitudinal study of the effects of childhood trauma on symptoms and functioning of people with severe mental health problems. J. Trauma Dissociation 10, 57–68. doi: 10.1080/15299730802485169
Dibaj, I. S., Tørmoen, A. J., Klungsøyr, O., Haga, E., and Mehlum, L. (2023). Trajectories and predictors of change in emotion dysregulation and deliberate self-harm amongst adolescents with borderline features. Clin. Child Psychol. Psychiatry 13591045231177374:135910452311773. doi: 10.1177/13591045231177374
Dong, Z., Zhou, J., Conti, A., Westwood, S. J., Fu, X., Liu, Q., et al. (2023). Association between alexithymia and non-suicidal self-injury in psychiatric patients: the mediating role of self-esteem and the moderating role of emotional intelligence. J. Psychiatr. Res. 162, 57–64. doi: 10.1016/j.jpsychires.2023.04.006
Duggan, J. M., Toste, J. R., and Heath, N. L. (2013). An examination of the relationship between body image factors and non-suicidal self-injury in young adults: the mediating influence of emotion dysregulation. Psychiatry Res. 206, 256–264. doi: 10.1016/j.psychres.2012.11.016
Etain, B., Mathieu, F., Henry, C., Raust, A., Roy, I., Germain, A., et al. (2010). Preferential association between childhood emotional abuse and bipolar disorder. J. Trauma. Stress. 23, 376–383. doi: 10.1002/jts.20532
Franz, M., Popp, K., Schaefer, R., Sitte, W., Schneider, C., Hardt, J., et al. (2008). Alexithymia in the German general population. Soc. Psychiatry Psychiatr. Epidemiol. 43, 54–62. doi: 10.1007/s00127-007-0265-1
Garisch, J. A., and Wilson, M. S. (2010). Vulnerabilities to deliberate self-harm among adolescents: the role of alexithymia and victimization. Br. J. Clin. Psychol. 49, 151–162. doi: 10.1348/014466509X441709
Garisch, J. A., and Wilson, M. S. (2015). Prevalence, correlates, and prospective predictors of non-suicidal self-injury among New Zealand adolescents: cross-sectional and longitudinal survey data. Child Adolesc. Psychiatry Ment. Health 9, 1–11. doi: 10.1186/s13034-015-0055-6
Halpin, S. A., and Duffy, N. M. (2020). Predictors of non-suicidal self-injury cessation in adults who self-injured during adolescence. J. Affect. Disord. Rep. 1:100017. doi: 10.1016/j.jadr.2020.100017
Hamilton, M. (1960). A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62. doi: 10.1136/jnnp.23.1.56
He, H., Hong, L., Jin, W., Xu, Y., Kang, W., Liu, J., et al. (2023). Heterogeneity of non-suicidal self-injury behavior in adolescents with depression: latent class analysis. BMC Psychiatry 23:301. doi: 10.1186/s12888-023-04808-7
He, J., Zhong, X., Gao, Y., Xiong, G., and Yao, S. (2019). Psychometric properties of the Chinese version of the childhood trauma questionnaire-short form (CTQ-SF) among undergraduates and depressive patients. Child Abuse Negl. 91, 102–108. doi: 10.1016/j.chiabu.2019.03.009
Hepp, J., Störkel, L. M., Wycoff, A. M., Freeman, L. K., Schmahl, C., and Niedtfeld, I. (2021). A test of the interpersonal function of non-suicidal self-injury in daily life. Behav. Res. Ther. 144:103930. doi: 10.1016/j.brat.2021.103930
Hooley, J. M., and Franklin, J. C. (2018). Why do people hurt themselves? A new conceptual model of nonsuicidal self-injury. Clin. Psychol. Sci. 6, 428–451. doi: 10.1177/2167702617745641
Hooley, J. M., Ho, D. T., Slater, J., and Lockshin, A. (2010). Pain perception and nonsuicidal self-injury: a laboratory investigation. Personal. Disord. Theory Res. Treat. 1, 170–179. doi: 10.1037/a0020106
Huang, C., Yuan, Q., Ge, M., Sheng, X., Yang, M., Shi, S., et al. (2022). Childhood trauma and non-suicidal self-injury among Chinese adolescents: the mediating role of psychological sub-health. Front. Psych. 13:798369. doi: 10.3389/fpsyt.2022.798369
Iskric, A., Ceniti, A. K., Bergmans, Y., McInerney, S., and Rizvi, S. J. (2020). Alexithymia and self-harm: a review of nonsuicidal self-injury, suicidal ideation, and suicide attempts. Psychiatry Res. 288:112920. doi: 10.1016/j.psychres.2020.112920
Kang, N., Jiang, Y., Ren, Y., Gong, T., Liu, X., Leung, F., et al. (2018). Distress intolerance mediates the relationship between child maltreatment and nonsuicidal self-injury among Chinese adolescents: a three-wave longitudinal study. J. Youth Adolesc. 47, 2220–2230. doi: 10.1007/s10964-018-0877-7
Kang, L., Li, R., Liu, H., Ma, S., Sun, S., Zhang, N., et al. (2021). Nonsuicidal self-injury in undergraduate students with major depressive disorder: the role of psychosocial factors. J. Affect. Disord. 290, 102–108. doi: 10.1016/j.jad.2021.04.083
Kautz, M. M., Burke, T. A., Siegel, D. M., Case, J., and Alloy, L. B. (2020). The role of reward sensitivity and childhood maltreatment in predicting nonsuicidal self-injury. Suicide Life Threat. Behav. 50, 1250–1263. doi: 10.1111/sltb.12718
Kim, D. J., Job, A., Gokarakonda, S., Huang, C., Chekuri, L., Carbajal, J. M., et al. (2022). Synergistic effect of chronic pain and nonsuicidal self-harm on pain sensitivity. Eur. Arch. Psychiatry Clin. Neurosci. 272, 371–380. doi: 10.1007/s00406-021-01283-7
Kim, H.-J., Song, C., Bang, M., and Lee, S.-H. (2020). Early sexual trauma is related with the tapetum in patients with panic disorder. J. Affect. Disord. 267, 107–113. doi: 10.1016/j.jad.2020.02.019
Klaassens, E. R., van Noorden, M. S., Giltay, E. J., van Pelt, J., van Veen, T., and Zitman, F. G. (2009). Effects of childhood trauma on HPA-axis reactivity in women free of lifetime psychopathology. Prog. Neuro Psychopharmacol. Biol. Psychiatry 33, 889–894. doi: 10.1016/j.pnpbp.2009.04.011
Klonsky, E. D. (2007). The functions of deliberate self-injury: a review of the evidence. Clin. Psychol. Rev. 27, 226–239. doi: 10.1016/j.cpr.2006.08.002
Kyei, J. J. (2023). As the twig is bent so the tree is inclined? Exploring the associations of adverse childhood experiences and adult relational impairments in Ghana. J. Interpers. Violence 38, 11272–11289. doi: 10.1177/08862605231179722
Lee, W. K. (2016). Psychological characteristics of self-harming behavior in Korean adolescents. Asian J. Psychiatr. 23, 119–124. doi: 10.1016/j.ajp.2016.07.013
Liang, Y., Chen, J., Xiong, Y., Wang, Q., and Ren, P. (2023). Profiles and transitions of non-suicidal self-injury and depressive symptoms among adolescent boys and girls: predictive role of bullying victimization. J. Youth Adolesc. 52, 1705–1720. doi: 10.1007/s10964-023-01779-6
Lim, K.-S., Wong, C. H., McIntyre, R. S., Wang, J., Zhang, Z., Tran, B. X., et al. (2019). Global lifetime and 12-month prevalence of suicidal behavior, deliberate self-harm and non-suicidal self-injury in children and adolescents between 1989 and 2018: a meta-analysis. Int. J. Environ. Res. Public Health 16:4581. doi: 10.3390/ijerph16224581
Liu, R. T. (2017). Childhood adversities and depression in adulthood: current findings and future directions. Clin. Psychol. Sci. Pract. 24, 140–153. doi: 10.1111/cpsp.12190
Liu, R. T., Scopelliti, K. M., Pittman, S. K., and Zamora, A. S. (2018). Childhood maltreatment and non-suicidal self-injury: a systematic review and meta-analysis. Lancet Psychiatry 5, 51–64. doi: 10.1016/S2215-0366(17)30469-8
Lüdtke, J., In-Albon, T., Michel, C., and Schmid, M. (2016). Predictors for DSM-5 nonsuicidal self-injury in female adolescent inpatients: the role of childhood maltreatment, alexithymia, and dissociation. Psychiatry Res. 239, 346–352. doi: 10.1016/j.psychres.2016.02.026
Marco, J. H., Cañabate, M., García-Alandete, J., Llorca, G., Real-López, M., Beltrán, M., et al. (2018). Body image and nonsuicidal self-injury: validation of the B ody I nvestment S cale in participants with eating disorders. Clin. Psychol. Psychother. 25, 173–180. doi: 10.1002/cpp.2142
Markey, C. N. (2010). Invited commentary: Why body image is important to adolescent development. 39, pp. 1387–1391). Berlin: Springer.
Martiniuk, A. L., Chen, H.-Y., Glozier, N., Patton, G., Senserrick, T., Williamson, A., et al. (2015). High alcohol use a strong and significant risk factor for repetitive self-harm in female and male youth: a prospective cohort study. Am. J. Drug Alcohol Abuse 41, 465–473. doi: 10.3109/00952990.2015.1062023
Mehlum, L., Ramberg, M., Tørmoen, A. J., Haga, E., Diep, L. M., Stanley, B. H., et al. (2016). Dialectical behavior therapy compared with enhanced usual care for adolescents with repeated suicidal and self-harming behavior: outcomes over a one-year follow-up. J. Am. Acad. Child Adolesc. Psychiatry 55, 295–300. doi: 10.1016/j.jaac.2016.01.005
Mehlum, L., Ramleth, R. K., Tørmoen, A. J., Haga, E., Diep, L. M., Stanley, B. H., et al. (2019). Long term effectiveness of dialectical behavior therapy versus enhanced usual care for adolescents with self-harming and suicidal behavior. J. Child Psychol. Psychiatry 60, 1112–1122. doi: 10.1111/jcpp.13077
Mehlum, L., Tormoen, A. J., Ramberg, M., Haga, E., Diep, L. M., Laberg, S., et al. (2014). Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: a randomized trial. J. Am. Acad. Child Adolesc. Psychiatry 53, 1082–1091. doi: 10.1016/j.jaac.2014.07.003
Muehlenkamp, J. J., Bagge, C. L., Tull, M. T., and Gratz, K. L. (2013). Body regard as a moderator of the relation between emotion dysregulation and nonsuicidal self-injury. Suicide Life Threat. Behav. 43, 479–493. doi: 10.1111/sltb.12032
Muehlenkamp, J. J., and Brausch, A. M. (2012). Body image as a mediator of non-suicidal self-injury in adolescents. J. Adolesc. 35, 1–9. doi: 10.1016/j.adolescence.2011.06.010
Nock, M. K. (2009). Why do people hurt themselves? New insights into the nature and functions of self-injury. Curr. Dir. Psychol. Sci. 18, 78–83. doi: 10.1111/j.1467-8721.2009.01613.x
Nock, M. K. (2010). Self-injury. Annu. Rev. Clin. Psychol. 6, 339–363. doi: 10.1146/annurev.clinpsy.121208.131258
Norman, H., Marzano, L., Coulson, M., and Oskis, A. (2019). Effects of mindfulness-based interventions on alexithymia: a systematic review. Evid. Based Ment. Health 22, 36–43. doi: 10.1136/ebmental-2018-300029
Orbach, I., Lotem-Peleg, M., and Kedem, P. (1995). Attitudes toward the body in suicidal, depressed, and normal adolescents. Suicide Life Threat. Behav. 25, 211–221. doi: 10.1111/j.1943-278X.1995.tb00920.x
Orbach, I., and Mikulincer, M. (1998). The body investment scale: construction and validation of a body experience scale. Psychol. Assess. 10, 415–425. doi: 10.1037/1040-3590.10.4.415
Pérez, S., Marco, J. H., and Cañabate, M. (2018). Non-suicidal self-injury in patients with eating disorders: prevalence, forms, functions, and body image correlates. Compr. Psychiatry 84, 32–38. doi: 10.1016/j.comppsych.2018.04.003
Plener, P. L., Allroggen, M., Kapusta, N. D., Brähler, E., Fegert, J. M., and Groschwitz, R. C. (2016). The prevalence of nonsuicidal self-injury (NSSI) in a representative sample of the German population. BMC Psychiatry 16, 1–7. doi: 10.1186/s12888-016-1060-x
Plener, P. L., Schumacher, T. S., Munz, L. M., and Groschwitz, R. C. (2015). The longitudinal course of non-suicidal self-injury and deliberate self-harm: a systematic review of the literature. Borderline Pers. Disord. Emotion Dysregulat. 2, 2–11. doi: 10.1186/s40479-014-0024-3
Raffagnato, A., Angelico, C., Valentini, P., Miscioscia, M., and Gatta, M. (2020). Using the body when there are no words for feelings: alexithymia and somatization in self-harming adolescents. Front. Psych. 11:262. doi: 10.3389/fpsyt.2020.00262
Rahman, F., Webb, R. T., and Wittkowski, A. (2021). Risk factors for self-harm repetition in adolescents: a systematic review. Clin. Psychol. Rev. 88:102048. doi: 10.1016/j.cpr.2021.102048
Ross, S., Heath, N. L., and Toste, J. R. (2009). Non-suicidal self-injury and eating pathology in high school students. Am. J. Orthopsychiatry 79, 83–92. doi: 10.1037/a0014826
Sornberger, M. J., Heath, N. L., Toste, J. R., and McLouth, R. (2012). Nonsuicidal self-injury and gender: patterns of prevalence, methods, and locations among adolescents. Suicide Life Threat. Behav. 42, 266–278. doi: 10.1111/j.1943-278X.2012.0088.x
Stoltenborgh, M., Bakermans-Kranenburg, M. J., Alink, L. R., and van IJzendoorn, M. H. (2015). The prevalence of child maltreatment across the globe: review of a series of meta-analyses. Child Abuse Rev. 24, 37–50. doi: 10.1002/car.2353
Sun, K., Li, A., Li, Y., Xie, J., Tong, Y., Ma, J., et al. (2023). A cross-sectional study of non-suicidal self-injury in a Chinese adolescent inpatient cohort. Front. Psych. 14:1109334. doi: 10.3389/fpsyt.2023.1109334
Swannell, S., Martin, G., Page, A., Hasking, P., Hazell, P., Taylor, A., et al. (2012). Child maltreatment, subsequent non-suicidal self-injury and the mediating roles of dissociation, alexithymia and self-blame. Child Abuse Negl. 36, 572–584. doi: 10.1016/j.chiabu.2012.05.005
Swannell, S. V., Martin, G. E., Page, A., Hasking, P., and St John, N. J. (2014). Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threat. Behav. 44, 273–303. doi: 10.1111/sltb.12070
Tang, W.-C., Lin, M.-P., Wu, J. Y.-W., Lee, Y.-T., and You, J. (2022). Mediating role of depression in the association between alexithymia and nonsuicidal self-injury in a representative sample of adolescents in Taiwan. Child Adolesc. Psychiatry Ment. Health 16:43. doi: 10.1186/s13034-022-00477-8
Thomassin, K., Shaffer, A., Madden, A., and Londino, D. L. (2016). Specificity of childhood maltreatment and emotion deficit in nonsuicidal self-injury in an inpatient sample of youth. Psychiatry Res. 244, 103–108. doi: 10.1016/j.psychres.2016.07.050
van der Venne, P., Mürner-Lavanchy, I., Höper, S., Koenig, J., and Kaess, M. (2023). Physiological response to pain in female adolescents with nonsuicidal self-injury as a function of severity. J. Affect. Disord. 339, 64–73. doi: 10.1016/j.jad.2023.06.041
Wang, L., Liu, J., Yang, Y., and Zou, H. (2021). Prevalence and risk factors for non-suicidal self-injury among patients with depression or bipolar disorder in China. BMC Psychiatry 21, 1–12. doi: 10.1186/s12888-021-03392-y
Weierich, M. R., and Nock, M. K. (2008). Posttraumatic stress symptoms mediate the relation between childhood sexual abuse and nonsuicidal self-injury. J. Consult. Clin. Psychol. 76, 39–44. doi: 10.1037/0022-006X.76.1.39
Westlund Schreiner, M., Mueller, B. A., Klimes-Dougan, B., Begnel, E. D., Fiecas, M., Hill, D., et al. (2020). White matter microstructure in adolescents and young adults with non-suicidal self-injury. Front. Psych. 10:1019. doi: 10.3389/fpsyt.2019.01019
Xie, P., Wu, K., Zheng, Y., Guo, Y., Yang, Y., He, J., et al. (2018). Prevalence of childhood trauma and correlations between childhood trauma, suicidal ideation, and social support in patients with depression, bipolar disorder, and schizophrenia in southern China. J. Affect. Disord. 228, 41–48. doi: 10.1016/j.jad.2017.11.011
Xu, H., Song, X., Wang, S., Zhang, S., Xu, S., and Wan, Y. (2019). Mediating effect of social support in the relationship between childhood abuse and non-suicidal self-injury among Chinese undergraduates: the role of only-child status. Int. J. Environ. Res. Public Health 16:4023. doi: 10.3390/ijerph16204023
Ying, W., Shen, Y., Ou, J., Chen, H., Jiang, F., Yang, F., et al. (2023). Identifying clinical risk factors correlated with addictive features of non-suicidal self-injury among a consecutive psychiatric outpatient sample of adolescents and young adults. Eur. Arch. Psychiatry Clin. Neurosci., 1–10. doi: 10.1007/s00406-023-01636-4
Zetterqvist, M. (2015). The DSM-5 diagnosis of nonsuicidal self-injury disorder: a review of the empirical literature. Child Adolesc. Psychiatry Ment. Health 9, 1–13. doi: 10.1186/s13034-015-0062-7
Zhang, Y., Hu, Z., Hu, M., Lu, Z., Yu, H., and Yuan, X. (2022). Effects of childhood trauma on nonsuicidal self-injury in adolescent patients with bipolar II depression. Brain Behav. 12:e2771. doi: 10.1002/brb3.2771
Zhang, S., Lin, X., Yang, T., Zhang, S., Pan, Y., Lu, J., et al. (2020). Prevalence of childhood trauma among adults with affective disorder using the childhood trauma questionnaire: a meta-analysis. J. Affect. Disord. 276, 546–554. doi: 10.1016/j.jad.2020.07.001
Zhang, B., Zhang, W., Sun, L., Jiang, C., Zhou, Y., and He, K. (2023). Relationship between alexithymia, loneliness, resilience and non-suicidal self-injury in adolescents with depression: a multi-center study. BMC Psychiatry 23, 1–11. doi: 10.1186/s12888-023-04938-y
Zhao, K., Tong, S., Hong, L., Yang, S., Yang, W., Xu, Y., et al. (2023). Childhood trauma, peer victimization, and non-suicidal self-injury among Chinese adolescents: a latent variable mediation analysis. BMC Psychiatry 23:436. doi: 10.1186/s12888-023-04848-z
Keywords: depression, adolescent, non-suicidal self-injury, childhood trauma, body investment, alexithymia
Citation: Cao P, Peng R, Yuan Q, Zhou R, Ye M and Zhou X (2024) Predictors of non-suicidal self-injury in adolescents with depressive disorder: the role of alexithymia, childhood trauma, and body investment. Front. Psychol. 15:1336631. doi: 10.3389/fpsyg.2024.1336631
Received: 11 November 2023; Accepted: 27 February 2024;
Published: 04 April 2024.
Edited by:
Dawid Konrad Scigala, The Maria Grzegorzewska University, PolandReviewed by:
Filippo Aschieri, Catholic University of the Sacred Heart, ItalyCopyright © 2024 Cao, Peng, Yuan, Zhou, Ye and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoqin Zhou, emhvdXhxbHVsdUAxMjYuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.