- 1Department of Clinical Psychology, School of Behavioral Science and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran
- 2Department of Psychology, Faculty of Medical, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran
- 3Gastroenterology and Hepatology, Internal Medicine Department, Iran University of Medical Sciences, Tehran, Iran
Studies have provided evidence for the effectiveness of intensive short-term dynamic psychotherapy (ISTDP) in treating medically unexplained symptoms (MUS). This study aimed to examine the effectiveness of ISTDP on individuals living with irritable bowel syndrome (IBS) in terms of, emotion regulation (ER) abilities, defense mechanisms, quality of life (QOL), and IBS symptoms. A total of 30 patients diagnosed with IBS were recruited and randomly assigned to either the intervention (n = 15) or control (n = 15) group. Pre- and post-treatment assessments were conducted, along with a follow-up assessment after ten weeks. Repeated measures analyses of variance were employed to analyze the data. The findings revealed that ISTDP led to significant improvements in ER, defense mechanisms, and QOL, as well as a reduction in the severity and frequency of IBS symptoms. These results provide further support for the efficacy of ISTDP as a treatment modality for individuals with IBS.
Introduction
Irritable bowel syndrome (IBS) is a chronic functional gastrointestinal disorder (FGD) that involves recurring instances of abdominal pain, discomfort, and changes in bowel movements that are not explained by any biochemical or structural irregularities (Chey et al., 2015). IBS is currently one of the most common medical disorders encountered by healthcare providers, affecting up to 20% of the population in developed countries (Chang et al., 2010; Bokic et al., 2015). Within primary care settings, around 12% of individuals seek medical attention for IBS-related issues, establishing it as the predominant subgroup observed in gastroenterology clinics (Saha, 2014). While IBS is not life-threatening, it can significantly impair a person’s life and hinder daily functioning, leading to high rates of work absenteeism, hospital visits, and physician appointments. Additionally, severe cases of IBS pose a substantial financial burden on individuals. This strain comes from recurring costs for consultations, tests, medications, and additional treatments. Lost income due to reduced work productivity and absenteeism, plus expenses for mental health support and specialized care, also contribute. In summary, managing severe IBS affects physical and mental well-being, and creates considerable financial challenges (Jung et al., 2014; Chey et al., 2015).
The exact cause of IBS remains elusive, posing a challenge for physicians in identifying suitable treatment options. Thus far, many treatments have proven ineffective, highlighting the complexity of addressing this condition. However, recent research indicates that the pathogenesis of IBS involves a complex interplay of genetic factors, environmental influences, microbiota composition, and immune response (Loddo and Romano, 2015; Guan, 2019; Eijsbouts et al., 2021). Concurrently, there is emerging evidence suggesting a correlation between the development of IBS and various psychological variables. Individuals with IBS commonly experience psychological disorders, pathological personality traits, and mental health issues (Zomorrodi et al., 2015; Knowles et al., 2017; Pellissier and Bonaz, 2017). A study has shown that between 50 to 90% of IBS patients seeking treatment have a history of mental health disorders, including major depressive disorder, generalized anxiety disorder, panic disorder, social anxiety disorder, somatization disorder, and post-traumatic stress disorder (Keough et al., 2011). Another study found that 25% of IBS patients reported somatization disorder (Craske et al., 2011). Therefore, psychological disturbances may represent a significant risk factor for the development or exacerbation of gastrointestinal symptoms in individuals with IBS.
Research has found a correlation between IBS and emotional processing difficulties, particularly with alexithymia, which refers to difficulty identifying, describing, and experiencing emotions (e.g., Kano et al., 2007; Phillips et al., 2013; Lee et al., 2017; Sibelli et al., 2018; Selvi and Bozo Özen, 2022). These findings suggest that individuals with IBS may experience challenges with regulating their emotions. Emotion regulation (ER) pertains to an individual’s capacity to modulate emotional arousal and engage in goal-directed behaviors regardless of their emotional state. Deficits in ER, or emotion dysregulation (ED), can lead to challenges in monitoring, evaluating, or adapting emotional reactions (Gratz and Roemer, 2004; Gross, 2013). Research has identified adaptive ER as a protective factor against psychological problems, while ED is considered a vulnerability factor (Gross and Muñoz, 1995; Gross and Jazaieri, 2014). Furthermore, although few studies have been conducted on the subject, some have found a positive relationship between ED and gastrointestinal symptoms (Mazaheri, 2015; Sibelli et al., 2018; Selvi and Bozo Özen, 2022). Studies have indicated relationships between ED and susceptibility to physical illnesses such as breast cancer, rheumatoid arthritis, and infertility (Yıldız and Duy, 2019). For instance, research has linked ED and the experience of negative emotions, such as anger and anxiety, to exacerbation of breast cancer (Brandão et al., 2016), rheumatoid arthritis (van Middendorp et al., 2005), and chronic pain (Koechlin et al., 2018). Additionally, some studies have shown that difficulties in conscious experience, regulation, and expression of emotions are associated with the onset and progression of somatoform disorders (Begley, 1994). Moreover, other studies have suggested that anger can significantly impact antral intestinal movement activity in individuals with IBS (Stanculete et al., 2019). In one study, it was found that IBS patients who do not employ anger suppression as a coping mechanism may experience increased abdominal pain and more severe bowel movements following meals (Prat et al., 1996).
Also, the way in which patients with IBS react to emotional events may be influenced by their use of defense mechanisms, which are automatic psychological processes that help individuals cope with stress (American Psychiatric Association, 2013). Limited research has assessed defense mechanisms in patients with IBS, but some studies have found that they tend to use more immature defense mechanisms, such as projection and passive-aggression, and less mature mechanisms compared to healthy individuals (Saeed et al., 2019). Specifically, patients with IBS are more likely to use escape-avoidance and turning-against-self mechanisms, which may indicate that they are consciously trying to avoid or escape problems instead of effectively coping with them. The use of immature defense mechanisms, such as turning-against-self and passive-aggression, may be a form of self-punishment for patients with IBS, which may lead to the exacerbation of IBS symptoms (Ihilevich and Gleser, 1986; Pokroy et al., 1999; Saeed et al., 2019). Furthermore, IBS significantly impacts an individual’s quality of life (QOL) through various mechanisms. Research indicates that IBS can lead to a decreased QOL due to its debilitating symptoms, such as abdominal pain, altered bowel habits, and unpredictability of symptom onset (e.g., Trindade et al., 2022). These symptoms often result in heightened levels of depression, anxiety, and psychological distress, further diminishing QOL (Kopczyńska et al., 2018). IBS can also disrupt daily life, affecting work productivity and social engagements (Kopczyńska et al., 2018; Trindade et al., 2022). All these taken into account, addressing these psychological factors, such as through psychotherapy, may be important in the management and treatment of IBS. By targeting these underlying variables, individuals with IBS may experience improvements in their physical symptoms and overall quality of life.
The limited success of medical treatments for IBS has led to the emergence of various psychological therapies (Guthrie et al., 1993; Hetterich and Stengel, 2020). Meanwhile, multiple systematic reviews and meta-analyses have demonstrated the significant efficacy of psychotherapy in improving IBS symptoms and daily functioning (Laird et al., 2016, 2017; Weibert and Stengel, 2019; Shah et al., 2020). For instance, psychodynamic therapies provide a well-defined framework for addressing the unconscious emotional processing that plays a central role in MUS, and they have been further refined based on neuroscientific findings (Cooper et al., 2017). These therapies specifically focus on emotional and relational processing, aiming to explore the connections between unresolved conflicts and past adverse experiences (Cretton et al., 2020). Several meta-analyses showed that short-term psychodynamic psychotherapies (STPPs) were found to be effective in treating MUS and should be included in treatment guidelines (Lilliengren, 2017; Abbass et al., 2021). Intensive short-term dynamic psychotherapy (ISTDP) is among the most extensively researched STPPs for MUS. A review by Russell et al. (2022) on 11 randomized controlled trials, two control trials, and ten case series studies that examined the use of ISTDP for MUS suggested that ISTDP holds promise as a treatment modality for MUS. Nevertheless, despite evidence for the effectiveness of ISTDP on MUS, there is currently a lack of research examining the effectiveness of this treatment approach for individuals living with IBS specifically. ISTDP theory suggests that somatic symptoms in patients with IBS may result from anxiety caused by the unconscious avoidance of emotional experiences (Abbass et al., 2012). The treatment approach of ISTDP involves helping patients deal with their unconscious conflicts and emotions. Patients with IBS exhibit similar characteristics to those with other MUS conditions, including high levels of negative emotions, emotional dysregulation, and dysfunctional defense mechanisms. As a result, ISTDP may offer a promising treatment option for this group of patients. In an attempt to fill this gap in the literature, this study aimed to examine the effectiveness of ISTDP in improving emotion regulation, defense mechanisms, quality of life, and disease symptoms in individuals with IBS.
Methods
Participants and procedure
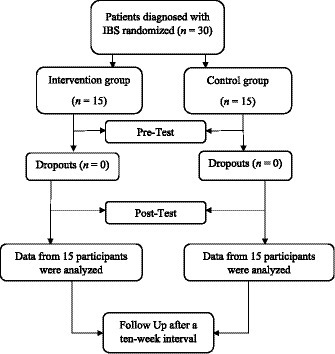
A randomized pre-test, post-test, and follow-up (RPPF) design with an intervention and a control group was used in this study. Participants were recruited from the gastroenterology clinic of Hazrat Rasool Hospital in Tehran using purposeful sampling methods. A total of 30 patients who met the diagnosis of IBS based on the judgment of gastroenterology specialists using the Rome III criteria were recruited. Participants were randomly assigned to either the intervention (n = 15) or control (n = 15) group. A graphic depiction of the recruitment process is presented in Figure 1. The inclusion criteria required participants to have a diagnosis of IBS based on the judgment of gastroenterology specialists and Rome III criteria, be between 20 and 50 years old, and have at least a high school diploma. Exclusion criteria were serious physical illness, psychiatric disorders with symptoms of psychosis [assessed by the Structured Clinical Interview for DSM-IV (SCID-l; First and Gibbon, 2004)], and absence of more than two treatment sessions. Both groups received usual medical care, while the control group was informed that they were on a waiting list and would receive treatment after a specified time. Participants provided informed consent after being informed about the aims and procedure of the study, as well as the confidentiality of their data. Participants completed pre-questionnaires and then received 16 weekly individual psychotherapy sessions based on the published treatment manual (Frederickson, 2013). Both groups completed post-questionnaires at the end of the 16th week and then completed questionnaires again after a ten-week interval. This study was first reviewed and approved by the Research Deputy of Iran University of Medical Sciences (Code Number = IR.IUMS.REC.1400.566) and was retrospectively registered in the Iranian Registry of Clinical Trials (ID Number = IRCT20221101056369N1, Registration Date: 2023-07-25).
Intervention
Intensive short-term dynamic psychotherapy
ISTDP is an active therapeutic approach that involves identifying the patient’s defensive system and making them aware of its self-sabotaging consequences in their life. This process helps the patient turn against their defenses and mobilize their own will to overcome pathogenic forces. The therapist confronts the patient respectfully but relentlessly, which leads to the emergence of an unconscious therapeutic alliance. At the same time, this work with defenses mobilizes unresolved feelings in the transference and triggers corresponding anxiety. Davanloo, the founder of ISTDP identified three neurobiological discharge pathways of unconscious anxiety and the process of motor conversion. The first pathway is observable as hand clenching and sighing respirations, accompanied by what he called “isolation of affect” where clients primarily use intellectual awareness devoid of emotional experience. The second pathway affects the muscles of the gastrointestinal tract, blood vessels, and airways, resulting in problems such as migraines, irritable bowel syndrome, and hypertension, and leads to instant repression of emotions and major depression. The third pathway leads to cognitive perceptual disruption, where the person experiences visual blurring, mental confusion, and hallucinations. Clients with motor conversion, with focal or global muscle weakness, also experience repression of emotions. In ISTDP, it is crucial to continuously observe the neurobiological channels of anxiety and the patient’s tolerance capacity to keep the process within their capacity. The process helps the patient experience their repressed feelings in the transference, leading to a subsequent shift to the person in their life toward whom the repressed feelings were generated. Through this process, the patient can work through the corresponding feelings of rage, guilt, grief, and affection, overcome their defensive system, and improve their tolerance capacity. The patient’s will poses a challenge and pressure to overcome defenses and anxiety and to experience their repressed feelings (Frederickson, 2013).
Our intervention incorporated a psychoeducational component, specifically educating participants about the triangle of conflict (i.e., defense, anxiety, and feeling) using insights gleaned from patient communications during the sessions. However, the intervention did not include homework assignments. To ensure consistency and adherence to the study protocol, the ISTDP treatment followed a meticulously manualized approach delivered identically across all participants, regardless of their initial level of distress. Every participant received the full 16 planned sessions, a fact that was communicated before the commencement of therapy. Each session lasted 50 min, with initial sessions extending to 1.5 h per participant. As the manualized intervention predetermined conclusion after 16 sessions, this endpoint was conveyed to participants initially. Thus, no specific indicators were used to determine therapy completion, as it was based solely on the predetermined session count.
Intervention instructor
The ISTDP sessions were facilitated by the first author, a doctoral candidate in clinical psychology, who had undergone extensive training and continued mentoring in this therapeutic approach. With the full consent of those participating, all treatment sessions were documented through audio recordings to enable examination of procedural integrity and protocol adherence. The supervising faculty member carried out periodic reviews of randomly selected recorded sessions as a means to guarantee the uniformity of the administered interventions. This oversight mechanism enabled ongoing quality assurance and standardization of the supplied therapeutic techniques.
Outcome measures
The irritable bowel syndrome quality of life
The IBS-QOL is a self-report measure of quality of life for patients with IBS (Patrick et al., 1998). It has 34 items rated on a five-point Likert scale ranging from 1 (“not at all”) to 5 (“extremely”) and load on eight domains: dysphoria, interference with activities, body image, health worry, food avoidance, social reactions, sexual health, and effect on relationships. The Persian version of IBS-QOL showed acceptable psychometric properties (Masaeli et al., 2013).
Difficulties in emotion regulation scale
The DERS (Gratz and Roemer, 2004) is a 36-item self-report questionnaire that assesses emotion dysregulation. The DERS items load on six subscales, including Lack of Emotional Awareness (6 items), Lack of Emotional Clarity (5 items), Difficulties Controlling Impulsive Behaviors When Distressed (6 items), Difficulties Engaging in Goal-Directed Behavior When Distressed (5 items), Nonacceptance of Negative Emotional Responses (6 items), and Limited Access to Effective ER Strategies (8 items). Participants rate items on a 5-point scale ranging from 1 (almost never) to 5 (almost always). A total score is obtained by summing all items. The internal consistency and validity of the Persian version of DERS were supported with the Iranian sample in previous studies (Besharat and Bazzazian, 2013; Vafa et al., 2021).
Defensive styles questionnaire
The DSQ-40 (Andrews et al., 1993) is a self-report measure of defense mechanisms, which comprises 40 items rated on a 9-point Likert scale. The 40 items are used to derive scores for 20 defense mechanisms, with two items for each. Immature, neurotic, and mature defensive styles scores are yielded by averaging the ratings for relevant items. The Persian version of the DSQ-40 yielded acceptable psychometric properties (Heidari Nasab et al., 2007).
Data analyses
We used SPSS 20 software for data entry and statistical analyses. The normality of the distribution for outcome measures was tested using the Kolmogorov–Smirnov test, and the results supported the normality of the data (p > 0.05). We then analyzed the pre-test differences in demographic and outcome variables between the two groups via the independent t-tests for continuous variables and chi-squared tests for categorical variables. We analyzed the outcome measures by means of repeated measures ANOVAs, with the group as between-subject factor and the time (pre-test, post-test, and follow-up) as within-subject factors. For testing the assumption of the sphericity in repeated-measures ANOVA, we examined the epsilon (ε) value; if the ε value did not fall in the acceptable range (i.e., 0.75 <), we relied on the Huynh-Feldt correction when reporting the results (Girden, 1992). The following rules of thumb are used to interpret values for partial eta squared: ηp2 = 0.01 indicates a small effect; ηp2 = 0.06 indicates a medium effect; ηp2 = 0.14 indicates a large effect. When necessary, post-hoc tests were performed to conduct detailed pairwise comparisons between assessments across the groups, with Bonferroni adjustment applied.
Results
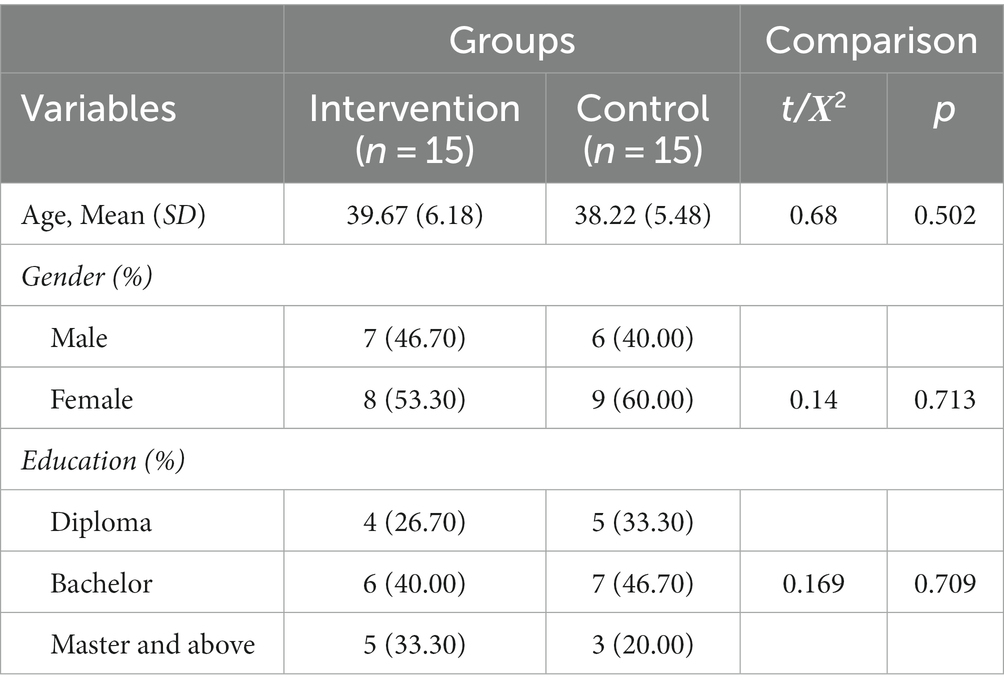
As shown in Table 1 groups did not differ significantly on demographic variables, including age, gender distribution, and level of education. Thus, the groups were matched in these variables. Table 2 also presents the means and standard deviations of study variables across assessment steps in each group.
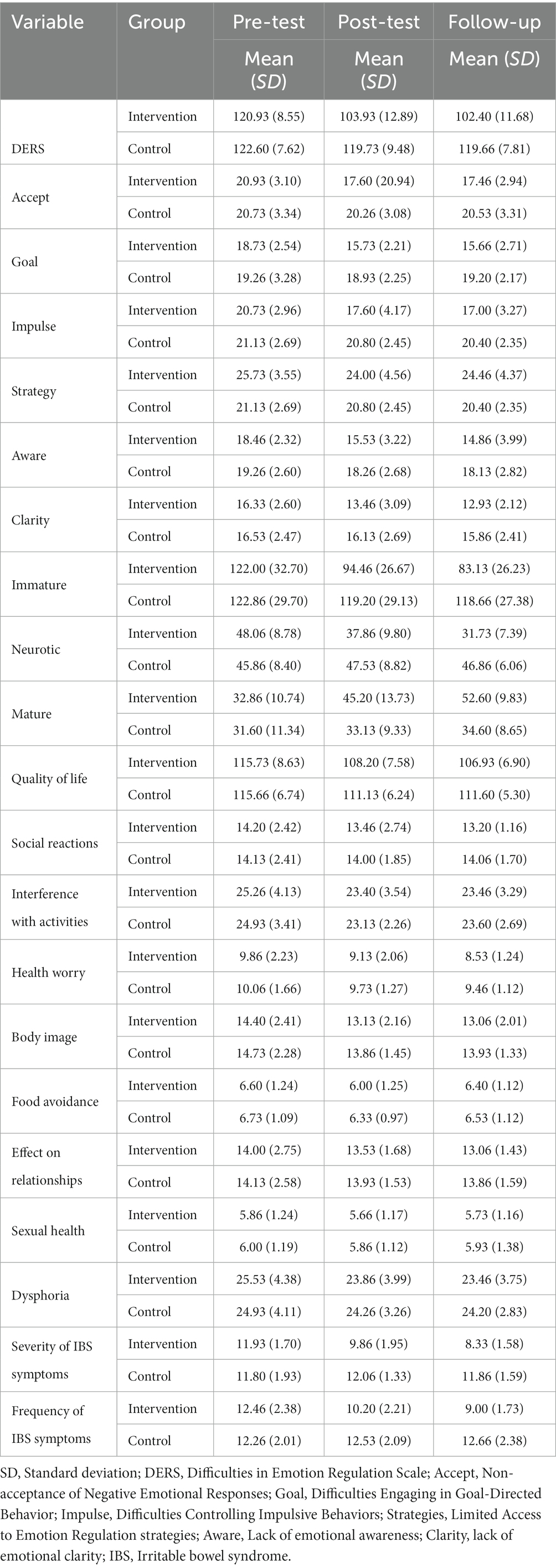
Table 2. Descriptive statistics of study variables across pre-test, post-test, and follow-up assessments.
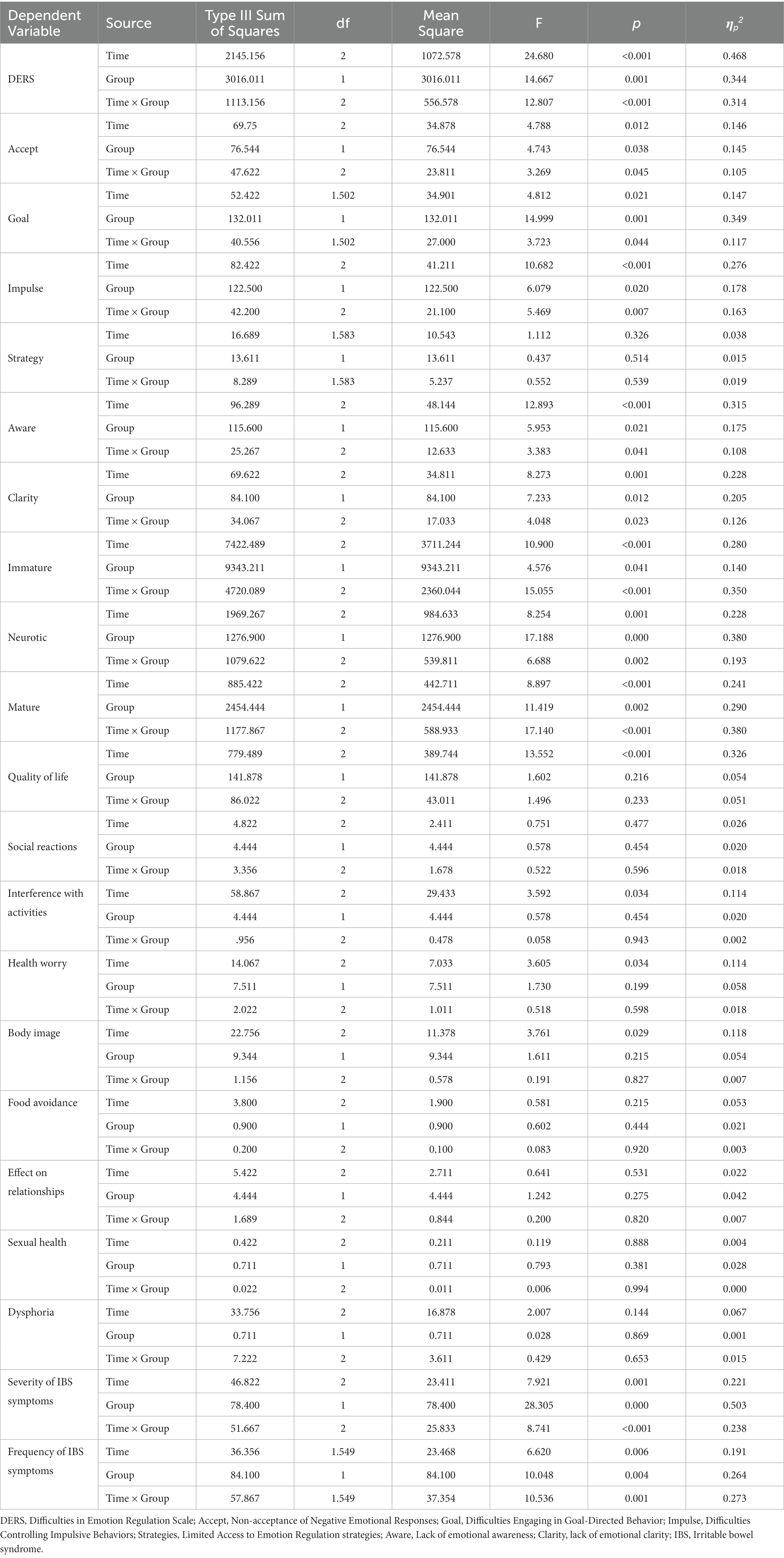
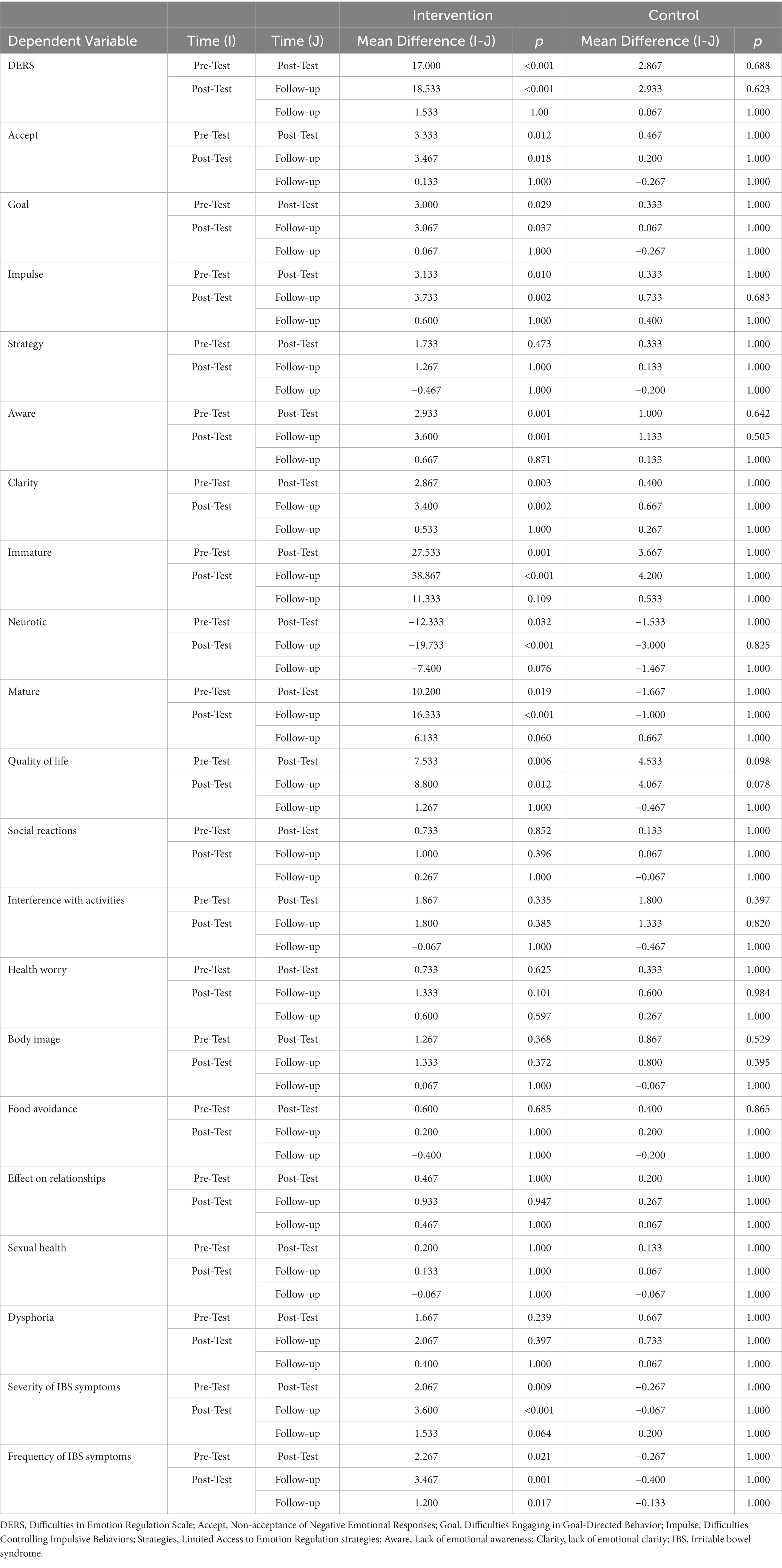
Repeated measures ANOVAs were conducted to examine the effectiveness of ISTDP on emotion regulation difficulties. As shown in Table 3, the results demonstrated a significant main effect of time for the DERS total score [F (2, 56) = 24.68, p < 0.001, ηp2 = 0.47] and subscales of Nonacceptance of Negative Emotional Responses [F (2, 56) = 4.79, p < 0.01, ηp2 = 0.15], Difficulties Engaging in Goal-Directed Behavior When Distressed [F (2, 56) = 4.81, p < 0.02, ηp2 = 0.15], Difficulties Controlling Impulsive Behaviors When Distressed [F (2, 56) = 10.68, p < 0.001, ηp2 = 0.28], Lack of Emotional Awareness [F (2, 56) = 12.89, p < 0.001, ηp2 = 0.31], and Lack of Emotional Clarity [F (2, 56) = 8.27, p < 0.001, ηp2 = 0.23] indicating that there are significant differences between the assessment steps in these scores. The results also showed significant between-subject effect of group on the DERS total score [F (1, 28) = 14.66, p < 0.001, ηp2 = 0.34] and subscales of Nonacceptance of Negative Emotional Responses [F (1, 28) = 4.74, p < 0.04, ηp2 = 0.15], Difficulties Engaging in Goal-Directed Behavior When Distressed [F (1, 28) = 14.99, p < 0.001, ηp2 = 0.35], Difficulties Controlling Impulsive Behaviors When Distressed [F (1, 28) = 6.08, p < 0.02, ηp2 = 0.18], Lack of Emotional Awareness [F (1, 28) = 5.95, p < 0.02, ηp2 = 0.17], and Lack of Emotional Clarity [F (1, 28) = 7.23, p < 0.01, ηp2 = 0.20], indicating significant overall differences between groups in these scores (Table 3). In addition, there was a significant time × group interaction for the DERS total score [F (2, 56) = 12.80, p < 0.001, ηp2 = 0.34] and subscales of Nonacceptance of Negative Emotional Responses [F (2, 56) = 3.27, p < 0.04, ηp2 = 0.10], Difficulties Engaging in Goal-Directed Behavior When Distressed [F (2, 56) = 3.72, p < 0.04, ηp2 = 0.12], Difficulties Controlling Impulsive Behaviors When Distressed [F (2, 56) = 5.47, p < 0.007, ηp2 = 0.16], Lack of Emotional Awareness [F (2, 56) = 3.38, p < 0.04, ηp2 = 0.11], and Lack of Emotional Clarity [F (2, 56) = 4.05, p < 0.02, ηp2 = 0.13], showing that the changes in the dependent variables across the assessment steps were statistically different between the groups. Post-hoc Tukey test comparisons were performed across the three assessment scores and separately for each group with Bonferroni’s correction for multiple comparisons. As shown in Table 4, our results indicated significant differences from pre-test to post-test and pre-test to follow-up in DERS total and subscales scores of Nonacceptance of Negative Emotional Responses, Difficulties Engaging in Goal-Directed Behavior When Distressed, Difficulties Controlling Impulsive Behaviors When Distressed, Lack of Emotional Awareness, and Lack of Emotional Clarity (p < 0.001 to 0.037) only in the intervention group (Table 4).
We conducted three sets of repeated measures ANOVAs to examine the effectiveness of ISTDP on defense mechanisms, and the results showed a significant main effect of time for the immature [F (2, 56) = 10.90, p < 0.001, ηp2 = 0.28], neurotic [F (2, 56) = 8.25, p < 0.01, ηp2 = 0.23], and mature [F (2, 56) = 8.90, p < 0.001, ηp2 = 0.24] defenses. Also, as shown in table, results indicated the significant between-subject effect of group on the immature [F (1, 28) = 4.58, p < 0.04, ηp2 = 0.14], neurotic [F (1, 28) = 17.19, p < 0.001, ηp2 = 0.38], and mature [F (1, 28) = 11.42, p < 0.002, ηp2 = 0.29] defenses. The results were also indicative of significant time × treatment interaction for the immature [F (2, 56) = 15.05, p < 0.001, ηp2 = 0.35], neurotic [F (2, 56) = 6.69, p < 0.002, ηp2 = 0.19], and mature [F (2, 56) = 17.14, p < 0.001, ηp2 = 0.38] defenses (Table 3). In addition, as could be retrieved from Table 4, post-hoc Tukey test comparisons showed significant differences from pre-test to post-test and pre-test to follow-up in immature, neurotic, and mature defenses (p < 0.001 to 0.032) in the intervention group.
We also conducted repeated measures ANOVAs to test the effectiveness of ISTDP on QOL. As Table 3 shows, the results indicated the significant main effect of time for the IBS-QOL total score [F (2, 56) = 13.55, p < 0.001, ηp2 = 0.33] and subscales of interference with activities [F (2, 56) = 3.59, p < 0.03, ηp2 = 0.11], health worry [F (2, 56) = 3.60, p < 0.03, ηp2 = 0.11], and body image [F (2, 56) = 3.76, p < 0.03, ηp2 = 0.12]. No significant between-subject effect of group and time × treatment interaction was observed for the IBS-QOL scores. Post-hoc Tukey test comparisons showed significant differences from pre-test to post-test and pre-test to follow up for only the IBS-QOL total score in the intervention group (Table 4).
Finally, two sets of repeated measures ANOVAs were conducted to examine the effectiveness of ISTDP on the severity and frequency of IBS symptoms. Table 3 shows the significant main effect of time on the severity [F (2, 56) = 7.92, p < 0.001, ηp2 = 0.22] and frequency [F (2, 56) = 6.62, p < 0.006, ηp2 = 0.19] of IBS symptoms. Also, as shown in table, results indicated the significant between-subject effect of the group on the severity [F (1, 28) = 28.30, p < 0.001, ηp2 = 0.50], and frequency [F (1, 28) = 10.05, p < 0.004, ηp2 = 0.26] of IBS symptoms. The results were also supportive of significant time × treatment interaction for the severity [F (2, 56) = 8.74, p < 0.001, ηp2 = 0.24] and frequency [F (2, 56) = 10.54, p < 0.001, ηp2 = 0.27] of IBS symptoms. In addition, as could be retrieved from Table 4, post-hoc Tukey test comparisons showed significant differences from pre-test to post-test and pre-test to follow up for the severity and frequency of IBS symptoms (p < 0.001 to 0.02) in the intervention group (Table 4).
Discussion
This study aimed to examine the effectiveness of ISTDP in improving ER, defense mechanisms, quality of life, and IBS symptoms in individuals with IBS. The results indicated that ISTDP was significantly effective in improving emotion regulation, defense mechanisms, and quality of life, and reducing the frequency/severity of IBS symptoms.
Overall, research indicates that ED problems among patients with IBS could exacerbate the severity/frequency of the IBS symptoms (e.g., Kano et al., 2007; Phillips et al., 2013; Lee et al., 2017; Sibelli et al., 2018; Selvi and Bozo Özen, 2022). In this vein, our findings provide evidence that ISTDP is effective in significantly improving ER abilities in individuals with IBS which is in line with theory and prior research on the effectiveness of the ISTDP on ER (e.g., Frederickson et al., 2018; Town et al., 2019; Malda Castillo et al., 2022). ISTDP facilitates the development of a deeper understanding of emotional experiences, triggers, and patterns. By gaining insight into their emotions, individuals enhance their awareness of emotional states, enabling them to recognize and respond to them more effectively. Additionally, ISTDP supports the processing and integration of unresolved emotional experiences and conflicts (Cooper et al., 2017). This therapeutic process encourages individuals to explore and express their emotions in a safe and supportive environment, leading to a reduction in emotional distress and an enhancement in their capacity to regulate emotions (e.g., Town et al., 2019; Malda Castillo et al., 2022). In this vein, a study on the effectiveness of ISTDP for dissociative seizures showed that participants gained increased control over their seizures and experienced fewer and less frequent episodes, partially due to their improved recognition and ability to address triggers. Participants also mentioned acquiring skills and techniques from ISTDP to manage their emotions and bodily sensations, reducing the likelihood of seizures (Malda Castillo et al., 2022). Furthermore, our study revealed that ISTDP led to a significant increase in the utilization of mature defenses, while simultaneously resulting in a significant reduction in the employment of neurotic and immature defenses. In accordance with our findings, Mehboodi et al. (2022) observed a significant increase in mature defense mechanisms and a concurrent decrease in immature defenses among individuals with social anxiety disorder following the application of ISTDP. Theoretically, ISTDP assists individuals in recognizing their defense mechanisms. It enables them to identify and acknowledge the ineffective defenses that are employed in inappropriate contexts, subsequently helping them reduce their reliance on such defenses. Simultaneously, individuals learn to cultivate and utilize mature and appropriate defenses in various situations. Moreover, as individuals in ISTDP engage with their emotions and gain insight into the behaviors and defenses that contribute to the suppression of their feelings, they gradually recognize the diminishing necessity to conceal their emotions using immature defenses (Frederickson et al., 2018).
In addition, our study demonstrated a significant improvement in the QOL of individuals with IBS following the implementation of ISTDP. ISTDP has the potential to assist individuals in effectively managing their IBS symptoms. This leads to a reduction in symptom severity, frequency, and related distress, resulting in an overall enhancement of QOL. ISTDP also aids in the reduction of anxiety, depression, and stress levels commonly experienced by individuals with IBS, thereby contributing to an improved QOL. Moreover, ISTDP facilitates the development of healthier communication patterns, enhances relationship skills, and fosters a more supportive social network. These improved interpersonal dynamics contribute to a higher quality of life by promoting social support and reducing feelings of isolation or alienation (Malda Castillo et al., 2022; Pakdel et al., 2022; Farzadkia et al., 2023). Furthermore, ISTDP was found to positively impact participants’ relationships with both themselves and others (Malda Castillo et al., 2022). Finally, our study found a significant decrease in the severity and frequency of IBS symptoms following ISTDP. These findings are in line with prior research suggesting that short-term psychodynamic psychotherapy is effective in the treatment of MUS (Lilliengren, 2017; Abbass et al., 2021). More specifically, in a review of 11 randomized controlled trials, two control trials, and ten case series studies, Russell et al. (2022) found that the ISTDP hold promises as a treatment modality for MUS. Psychodynamic treatments such as ISTDP propose that somatic symptoms are primarily caused by implicit emotional processing and distorted bodily awareness. According to ISTDP, these symptoms are manifestations of a patient’s automatic, unconscious, and habitual avoidance of emotions, leading to physiological states in the body (Russell et al., 2016, 2017). ISTDP aims to enhance patients’ self-understanding, including recognizing triggers, warning signs, and emotions associated with their symptoms (Town et al., 2019; Malda Castillo et al., 2022). By fostering the articulation and recognition of emotions, ISTDP empowers individuals to gain a deeper understanding of their life experiences. Moreover, the constructive impact of ISTDP on ER and defense mechanisms which was demonstrated in this study may elucidate why the treatment group experienced a notable reduction in both the severity and frequency of their IBS symptoms.
The findings of this study should be interpreted in light of several limitations. Firstly, the study did not differentiate between subtypes of IBS. Future research could benefit from addressing this aspect to provide a more nuanced understanding of IBS management. Secondly, the employment of self-report measures to evaluate outcome variables introduces the potential for biased data due to inaccuracies, social desirability bias, and shared method variance. Finally, the study’s sample size was constrained, emphasizing the need for future research with larger and more diverse samples to improve the generalizability and robustness of the findings.
Conclusion
This RCT furnishes compelling empirical support for the effectiveness of ISTDP in treating individuals with IBS. The results demonstrated the substantial promise of ISTDP as a pivotal intervention in alleviating IBS symptoms. Meanwhile, rigorous inquiry into the change mechanisms of the ISTDP specifically with a qualitative approach is imperative for refining the clinical application of ISTDP, ensuring its optimal integration within the broader framework of IBS care.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Research Deputy of Iran University of Medical Sciences. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
FS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Writing – original draft, Writing – review & editing. MD: Conceptualization, Project administration, Supervision, Writing – review & editing. FL: Conceptualization, Project administration, Supervision, Writing – review & editing. MeM: Project administration, Supervision, Writing – review & editing. MaM: Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors appreciate all individuals who voluntarily participated in this study. The authors also appreciate Mojtaba Elhami Athar for reviewing and revising the final draft of the current study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abbass, A., Lumley, M. A., Town, J., Holmes, H., Luyten, P., Cooper, A., et al. (2021). Short-term psychodynamic psychotherapy for functional somatic disorders: a systematic review and meta-analysis of within-treatment effects. J. Psychosom. Res. 145:110473. doi: 10.1016/j.jpsychores.2021.110473
Abbass, A., Town, J., and Driessen, E. (2012). Intensive short-term dynamic psychotherapy: a systematic review and Meta-analysis of outcome research. Harv. Rev. Psychiatry 20, 97–108. doi: 10.3109/10673229.2012.677347
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th). New York: American Psychiatric Pub.
Andrews, G., Singh, M., and Bond, M. (1993). The defense style questionnaire. J. Nerv. Ment. Dis. 181, 246–256. doi: 10.1097/00005053-199304000-00006
Begley, T. M. (1994). Expressed and suppressed anger as predictors of health complaints. J. Organ. Behav. 15, 503–516. doi: 10.1002/job.4030150603
Besharat, M. A., and Bazzazian, S. (2013). Psychometri properties of the cognitive emotion regulation questionnaire in a sample of Iranian population. Nurs. Midwif. J. 24, 61–70.
Bokic, T., Storr, M., and Schicho, R. (2015). Potential causes and present pharmacotherapy of irritable bowel syndrome: an overview. Pharmacology 96, 76–85. doi: 10.1159/000435816
Brandão, T., Tavares, R., Schulz, M. S., and Matos, P. M. (2016). Measuring emotion regulation and emotional expression in breast cancer patients: a systematic review. Clin. Psychol. Rev. 43, 114–127. doi: 10.1016/j.cpr.2015.10.002
Chang, L., Lacy, B. E., and Spiegel, B. M. (2010). An evidence-based approach to therapy in IBS-D: a case study compendium. Gastroenterol. Hepatol. 6, 1–12.
Chey, W. D., Kurlander, J., and Eswaran, S. (2015). Irritable bowel syndrome: a clinical review. JAMA 313, 949–958. doi: 10.1001/jama.2015.0954
Cooper, A., Abbass, A., and Town, J. (2017). Implementing a psychotherapy Service for Medically Unexplained Symptoms in a primary care setting. J. Clin. Med. 6:109. doi: 10.3390/jcm6120109
Craske, M. G., Wolitzky-Taylor, K. B., Labus, J., Wu, S., Frese, M., Mayer, E. A., et al. (2011). A cognitive-behavioral treatment for irritable bowel syndrome using interoceptive exposure to visceral sensations. Behav. Res. Ther. 49, 413–421. doi: 10.1016/j.brat.2011.04.001
Cretton, A., Brown, R. J., Curt LaFrance, W. J., and Aybek, S. (2020). What does neuroscience tell us about the conversion model of functional neurological disorders? J. Neuropsychiatry Clin. Neurosci. 32, 24–32. doi: 10.1176/appi.neuropsych.19040089
Eijsbouts, C., Zheng, T., Kennedy, N. A., Bonfiglio, F., Anderson, C. A., Moutsianas, L., et al. (2021). Genome-wide analysis of 53,400 people with irritable bowel syndrome highlights shared genetic pathways with mood and anxiety disorders. Nat. Genet. 53, 1543–1552. doi: 10.1038/s41588-021-00950-8
Farzadkia, M., Farhangi, A., and Abolghasemi, S. (2023). Effectiveness of mindfulness-based stress reduction and intensive short-term dynamic psychotherapy in improving mental health and mitigating alexithymia in fibromyalgia patients. Int. J. Musculosk. Pain Prevent. 8, 836–845.
First, M. B., and Gibbon, M. (2004). “The structured clinical interview for DSM-IV Axis I disorders (SCID-I) and the structured clinical interview for DSM-IV Axis II disorders (SCID-II)” in Comprehensive handbook of psychological assessment, Vol. 2: Personality assessment. eds. M. J. Hilsenroth and D. L. Segal (Hoboken: John Wiley & Sons, Inc)
Frederickson, J. (2013). Co-creating change: effective dynamic therapy techniques. California: Seven Leaves Press.
Frederickson, J. J., Messina, I., and Grecucci, A. (2018). Dysregulated anxiety and dysregulating defenses: toward an emotion regulation informed dynamic psychotherapy [perspective]. Front. Psychol. 9:2054. doi: 10.3389/fpsyg.2018.02054
Gratz, K. L., and Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assess. 26, 41–54. doi: 10.1023/B:JOBA.0000007455.08539.94
Gross, J. J., and Jazaieri, H. (2014). Emotion, emotion regulation, and psychopathology: an affective science perspective. Clin. Psychol. Sci. 2, 387–401. doi: 10.1177/2167702614536164
Gross, J. J., and Muñoz, R. F. (1995). Emotion regulation and mental health. Clin. Psychol. Sci. Pract. 2, 151–164. doi: 10.1111/j.1468-2850.1995.tb00036.x
Guan, Q. (2019). A comprehensive review and update on the pathogenesis of inflammatory bowel disease. J Immunol Res 2019, 7247238–7247216. doi: 10.1155/2019/7247238
Guthrie, E., Creed, F., Dawson, D., and Tomenson, B. (1993). A randomised controlled trial of psychotherapy in patients with refractory irritable bowel syndrome. Br. J. Psychiatry 163, 315–321. doi: 10.1192/bjp.163.3.315
Heidari Nasab, L., Mansouri, M., Azadfallah, P., and Shaieeri, M. R. (2007). Validity and reliability of Defens style Questionaire (DSQ-40) in Iranian samples. Clin. Psychol. Pers. 5, 11–27.
Hetterich, L., and Stengel, A. (2020). Psychotherapeutic interventions in irritable bowel syndrome. Front. Psych. 11:286. doi: 10.3389/fpsyt.2020.00286
Ihilevich, D., and Gleser, G. C. (1986). Defense mechanisms: their classification, correlates, and measurement with the defense mechanisms inventory. Lyon: DMI Associates.
Jung, H. K., Kim, Y. H., Park, J. Y., Jang, B. H., Park, S. Y., Nam, M. H., et al. (2014). Estimating the burden of irritable bowel syndrome: analysis of a nationwide korean database. J. Neurogastroenterol. Motil. 20, 242–252. doi: 10.5056/jnm.2014.20.2.242
Kano, M., Hamaguchi, T., Itoh, M., Yanai, K., and Fukudo, S. (2007). Correlation between alexithymia and hypersensitivity to visceral stimulation in human. Pain 132, 252–263. doi: 10.1016/j.pain.2007.01.032
Keough, M. E., Timpano, K. R., Zawilinski, L. L., and Schmidt, N. B. (2011). The association between irritable bowel syndrome and the anxiety vulnerability factors:body vigilance and discomfort intolerance. J. Health Psychol. 16, 91–98. doi: 10.1177/1359105310367689
Knowles, S. R., Austin, D. W., Sivanesan, S., Tye-Din, J., Leung, C., Wilson, J., et al. (2017). Relations between symptom severity, illness perceptions, visceral sensitivity, coping strategies and well-being in irritable bowel syndrome guided by the common sense model of illness. Psychol. Health Med. 22, 524–534. doi: 10.1080/13548506.2016.1168932
Koechlin, H., Coakley, R., Schechter, N., Werner, C., and Kossowsky, J. (2018). The role of emotion regulation in chronic pain: a systematic literature review. J. Psychosom. Res. 107, 38–45. doi: 10.1016/j.jpsychores.2018.02.002
Kopczyńska, M., Mokros, Ł., Pietras, T., and Małecka-Panas, E. (2018). Quality of life and depression in patients with irritable bowel syndrome. Prz. Gastroenterol. 13, 102–108. doi: 10.5114/pg.2018.75819
Laird, K. T., Tanner-Smith, E. E., Russell, A. C., Hollon, S. D., and Walker, L. S. (2016). Short-term and long-term efficacy of psychological therapies for irritable bowel syndrome: a systematic review and Meta-analysis. Clin. Gastroenterol. Hepatol. 14, 937–947.e4. doi: 10.1016/j.cgh.2015.11.020
Laird, K. T., Tanner-Smith, E. E., Russell, A. C., Hollon, S. D., and Walker, L. S. (2017). Comparative efficacy of psychological therapies for improving mental health and daily functioning in irritable bowel syndrome: a systematic review and meta-analysis. Clin. Psychol. Rev. 51, 142–152. doi: 10.1016/j.cpr.2016.11.001
Lee, C., Doo, E., Choi, J. M., Jang, S. H., Ryu, H. S., Lee, J. Y., et al. (2017). The increased level of depression and anxiety in irritable bowel syndrome patients compared with healthy controls: systematic review and Meta-analysis. J. Neurogastroenterol. Motil. 23, 349–362. doi: 10.5056/jnm16220
Lilliengren, P. (2017). Comprehensive compilation of randomized controlled trials (RCTs) involving psychodynamic treatments and interventions.
Loddo, I., and Romano, C. (2015). Inflammatory bowel disease: genetics, epigenetics, and pathogenesis [Mini review]. Front. Immunol. 6:551. doi: 10.3389/fimmu.2015.00551
Malda Castillo, J., Beton, E., Coman, C., Howell, B., Burness, C., Martlew, J., et al. (2022). Three sessions of intensive short-term dynamic psychotherapy (ISTDP) for patients with dissociative seizures: a pilot study. Psychoanal. Psychother. 36, 81–104. doi: 10.1080/02668734.2021.2018623
Masaeli, N., Kheirabadi, G. R., Afshar, H., Daghaghzadeh, H., Maracy, M. R., Assadolahi, F., et al. (2013). Validity, reliability, and factor analysis of Persian version of quality of life questionnaire for irritable bowel syndrome (IBS-QOL-34). J. Res. Med. Sci. 18, 492–496.
Mazaheri, M. (2015). Difficulties in emotion regulation and mindfulness in psychological and somatic symptoms of functional gastrointestinal disorders. Iran J. Psych. Behav. Sci. 9:e954. doi: 10.17795/ijpbs-954
Mehboodi, K., Mohammadi, N., Rahimi, C., and Sarafraz, M. R. (2022). The efficacy of intensive short-term dynamic psychotherapy (ISTDP) on self-esteem, emotion regulation, and defense mechanisms in men with social anxiety disorder [اثربخشی رواندرمانی پویشی فشرده کوتاهمدت بر حرمت خود، نظمجویی هیجان و مکانیسمهای دفاعی در مردان مبتلا به اختلال اضطراب اجتماعی]. Psychol. Sci. 21, 461–474. doi: 10.52547/JPS.21.111.461
Pakdel, H., Shorabi, F., and Haji Alizade, K. (2022). The efficacy of intensive short-term dynamic psychotherapy on job stress coping strategies, health-related quality of life, and self-efficacy of Iran air traffic controler staff [applicable]. J. Psychol. Sci. 21, 543–558. doi: 10.52547/jps.21.111.543
Patrick, D. L., Drossman, D. A., Frederick, I. O., Dicesare, J., and Puder, K. L. (1998). Quality of life in persons with irritable bowel syndrome (development and validation of a new measure). Dig. Dis. Sci. 43, 400–411. doi: 10.1023/A:1018831127942
Pellissier, S., and Bonaz, B. (2017). “Chapter eleven - The place of stress and emotions in the irritable bowel syndrome” in Vitamins and hormones. ed. G. Litwack (New York: Academic Press)
Phillips, K., Wright, B. J., and Kent, S. (2013). Psychosocial predictors of irritable bowel syndrome diagnosis and symptom severity. J. Psychosom. Res. 75, 467–474. doi: 10.1016/j.jpsychores.2013.08.002
Pokroy, R., Mayer, A., Stuart, A. D., and Pretorius, H. G. (1999). Coping styles and defense mechanisms utilised by patients suffering from irritable bowel syndrome. Health SA Gesondheid 4:7. doi: 10.4102/hsag.v4i1.8
Prat, F., Malak, N. A., Pelletier, G., Buffet, C., Fritsch, J., Choury, A. D., et al. (1996). Biliary symptoms and complications more than 8 years after endoscopic sphincterotomy for choledocholithiasis. Gastroenterology 110, 894–899. doi: 10.1053/gast.1996.v110.pm8608900
Russell, L., Abbass, A., and Allder, S. (2022). A review of the treatment of functional neurological disorder with intensive short-term dynamic psychotherapy. Epilepsy Behav. 130:108657. doi: 10.1016/j.yebeh.2022.108657
Russell, L. A., Abbass, A. A., Allder, S. J., Kisely, S., Pohlmann-Eden, B., and Town, J. M. (2016). A pilot study of reduction in healthcare costs following the application of intensive short-term dynamic psychotherapy for psychogenic nonepileptic seizures. Epilepsy Behav. 63, 17–19. doi: 10.1016/j.yebeh.2016.07.017
Russell, L., Turner, A., and Yates, P. (2017). A preliminary evaluation of intensive short-term dynamic psychotherapy within a functional neurological symptoms service. Neuropsychologist 1, 25–32. doi: 10.53841/bpsneur.2017.1.4.25
Saeed, F., Salehi, M., Alavi, K., Ajdarkosh, H., Kashaninasab, F., and Nasr Esfahani, F. (2019). Defense mechanisms in patients with irritable bowel syndrome and their relationship with symptom severity and quality of life. Middle East J. Dig. Dis. 11, 158–165. doi: 10.15171/mejdd.2019.143
Saha, L. (2014). Irritable bowel syndrome: pathogenesis, diagnosis, treatment, and evidence-based medicine. World J. Gastroenterol. 20, 6759–6773. doi: 10.3748/wjg.v20.i22.6759
Selvi, K., and Bozo Özen, Ö. (2022). Group comparison of individuals with and without irritable bowel syndrome in terms of psychological and lifestyle-related factors. J. Psych. Neurol. Sci. 35, 13–23. doi: 10.14744/DAJPNS.2022.00167
Shah, K., Ramos-Garcia, M., Bhavsar, J., and Lehrer, P. (2020). Mind-body treatments of irritable bowel syndrome symptoms: an updated meta-analysis. Behav. Res. Ther. 128:103462. doi: 10.1016/j.brat.2019.103462
Sibelli, A., Chalder, T., Everitt, H., Chilcot, J., and Moss-Morris, R. (2018). Positive and negative affect mediate the bidirectional relationship between emotional processing and symptom severity and impact in irritable bowel syndrome. J. Psychosom. Res. 105, 1–13. doi: 10.1016/j.jpsychores.2017.11.016
Stanculete, M. F., Căpățînă, O., Pojoga, C., and Surdea-Blaga, T. (2019). Anger mediates the relationship between pain and depression in irritable bowel syndrome [article]. J. Gastrointest. Liver Dis. 28, 415–419. doi: 10.15403/jgld-533
Town, J. M., Lomax, V., Abbass, A. A., and Hardy, G. (2019). The role of emotion in psychotherapeutic change for medically unexplained symptoms. Psychother. Res. 29, 86–98. doi: 10.1080/10503307.2017.1300353
Trindade, I. A., Melchior, C., Törnblom, H., and Simrén, M. (2022). Quality of life in irritable bowel syndrome: exploring mediating factors through structural equation modelling. J. Psychosom. Res. 159:110809. doi: 10.1016/j.jpsychores.2022.110809
Vafa, Z., Azizi, M., and Elhami Athar, M. (2021). Predicting academic alienation from emotion dysregulation, social competence, and peer relationships in school-attending girls: a multiple-regression approach. Front. Psychol. 12:755952. doi: 10.3389/fpsyg.2021.755952
van Middendorp, H., Geenen, R., Sorbi, M. J., Hox, J. J., Vingerhoets, A. J. J. M., van Doornen, L. J. P., et al. (2005). Styles of emotion regulation and their associations with perceived health in patients with rheumatoid arthritis. Ann. Behav. Med. 30, 44–53. doi: 10.1207/s15324796abm3001_6
Weibert, E., and Stengel, A. (2019). The role of psychotherapy in the treatment of irritable bowel syndrome. Psychother. Psychosom. Med. Psychol. 69, 360–371. doi: 10.1055/a-0829-6990 (Die Rolle Der Psychotherapie Beim Reizdarmsyndrom.)
Yıldız, M. A., and Duy, B. (2019). The predictive role of emotion regulation strategies on depressive and psychosomatic symptoms in adolescents. Curr. Psychol. 38, 387–396. doi: 10.1007/s12144-017-9616-6
Keywords: IBS, ISTDP, psychodynamic psychotherapy, emotion regulation, defense mechanisms, quality of life
Citation: Shafiei F, Dehghani M, Lavasani FF, Manouchehri M and Mokhtare M (2024) Intensive short-term dynamic psychotherapy for irritable bowel syndrome: a randomized controlled trial examining improvements in emotion regulation, defense mechanisms, quality of life, and IBS symptoms. Front. Psychol. 15:1293150. doi: 10.3389/fpsyg.2024.1293150
Edited by:
Annikka Polster, University of Oslo, NorwayReviewed by:
Donald R. Marks, Kean University, United StatesCiro Conversano, University of Pisa, Italy
Copyright © 2024 Shafiei, Dehghani, Lavasani, Manouchehri and Mokhtare. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mahmood Dehghani, ZGVoZ2hhbmkubTEzOTlAZ21haWwuY29t
 Faezeh Shafiei
Faezeh Shafiei Mahmood Dehghani1*
Mahmood Dehghani1* Marjan Mokhtare
Marjan Mokhtare