- 1Department of Physical Therapy, Federal University of Rio Grande do Norte, Natal, Brazil
- 2Graduation Program in Sciences of Rehabilitation, University of Brasilia (UNB), Brasília, Distrito Federal, Brazil
- 3Research Directory, Catholic University of Temuco, Temuco, Chile
Introduction: Early intervention and parental education for preemies are limited in some low-income countries. Thus, this study aimed to assess whether daily tummy time (TT) associated with usual care (UC) enhances motor and cognitive development in preemies from low-income countries. The main and secondary aim was to assess prone head elevation (PHE) and motor and cognitive functions, respectively.
Methods: Thirty-one preemies with a mean gestational age at birth of 33.3 ± 1.6 weeks and weighing <2,500 g were included and 18 completed all assessments. Parents from the TT group were asked to perform TT with their preemies for at least 20 min during daily activities and playtime. Motor and cognitive functions were assessed by a blinded examiner using the motor and cognitive composite scores of Bayley-III after two and four months of corrected age. PHE was given by the angle from the tragus of the ear to the supporting surface of the infant; measurements were obtained using the Kinovea® software at baseline, after two, three, and four months of corrected age.
Results: The Bayley-III motor composite score of the TT group was higher than the UC group after two and four months of corrected age. The PHE angle increased over time but did not differ between groups.
Discussion: Nevertheless, TT expanded the perspective of preemies to explore their bodies and environment, favoring the stimuli for motor and cognitive patterns. The loss of participants (31%) was one of the limitations of the study, illustrating the challenge of providing continued early interventions to preemies from low-income countries. In this sense, TT practice is a home intervention that may improve motor and cognitive function of preemies immediately after hospital discharge.
Introduction
Tummy time (TT) is a crucial intervention that enhances motor skills in infants (World Health Organization, 2023). TT was formerly recommended to combat musculoskeletal complications from the campaign Safe to Sleep and involves placing the infant in the prone position for some time under the supervision of an adult (World Health Organization, 2019). Infants during TT are exposed to new experiences that develop motor, cognitive, and sensory abilities needed to explore and perceive the environment and their bodies. Thus, TT may enhance the development of infants, especially in the first months (Adolph and Hoch, 2019). In this way, new experiences provide a wide primary and secondary variability in the development (Hadders-Algra, 2018), which may be useful for developing problem-solving expertise. For instance, the infant is encouraged to lift the head, strengthening several muscular groups (e.g., cervical extensor, paravertebral, and scapular stabilizing muscles) and increasing cervical mobility. Moreover, the weight-bearing experience in the arms favors the development of manual and manipulative skills since it improves mobility and strengthens the muscles of the arms. Thus, TT develops muscle synergy needed for movement control and the acquisition of new abilities. In addition, the required visual adjustments improve the visual function, enhancing visual accuracy, focus, and attention (Adolph and Hoch, 2019; Kretch et al., 2014; Lee and Galloway, 2012; Soska and Adolph, 2014). In this sense, Kretch et al. (2014) presented that the changed visual experience may lead infants to have divergent experiences and different opportunities for learning. In their study, 13 infants experienced different postures wearing a head-mounted eye-tracker recording gaze direction and head-centered field of view.
Besides the biomechanical and functional changes, the new visual fields develop new spatial and movement concepts, as well as cause-effect associations. Consequently, preemies are exposed to new learning experiences and exploration of the environment. Hence, improved perception and movement planning increase movement possibilities based on decision-making and problem-solving approaches, refining cognitive abilities (Adolph and Hoch, 2019). In this sense, TT is an important intervention that improves the neurodevelopment of preemies and is highly recommended for infants up to six months of age by World Health Organization (2019). Additionally, TT fosters bonding between baby and parents and does not require special equipment, representing an accessible and feasible intervention for daily life. Thus, TT may be effective as a preterm follow-up intervention, especially in low-income settings, in which many families present difficulties in health assessment due to socioeconomic or transportation problems (Sampaio et al., 2023).
Brazil is a low-income country that presents a large socioeconomic diversity (Brazil, 2024), and about 70% of the neonatal care services and early intervention programs are concentrated in metropolitan areas (Ministério da Saúde, 2024). Moreover, most health services for outpatient follow-up of preemies currently use the watchful waiting approach, which only refers the preemie to an early intervention service when a neurodevelopment delay is detected (Lyne et al., 2022). The Brazilian northeast is the second poorest Brazilian region, characterized by low educational attainment and poor social support. Thus, preemies with neurodevelopmental delays from this region are not referred for early intervention service. Therefore, the literature shows that the interventions during this critical developmental window are inadequate due to the lack of knowledge of what, how, or when to stimulate a preemie (Baggett et al., 2020; Novak et al., 2020; Rosenberg et al., 2013; Twardzik et al., 2017; Watson, 2013). Thus, challenges in the current practice hindered the follow-up of infants with high risk for developmental delays (Lyne et al., 2022). Furthermore, the specialized care followed by caregivers is affected by barriers, such as difficulties in transport access, poor social support, limited time at home, and medical concerns regarding the mother or the preemie (Smith et al., 2017). The impact of this issue is enhanced after hospital discharge, as caregivers are challenged to keep the same level of care provided by the multiprofessional team while coping with anxiety, isolation, and financial constraints.
Although TT is important for the neurodevelopment during early childhood (Boutot and DiGangi, 2018; Clark and Kingsley, 2020; Hewitt et al., 2017; World Health Organization, 2019), literature still lacks evidence regarding its effects on motor and cognitive functions in preemies. Thus, this study aimed to verify whether TT improve motor and cognitive development of preterm infants, assessing prone head elevation (PHE), and motor and cognitive functions after TT.
Materials and methods
Study setting and participants
This single-blinded, randomized clinical trial was conducted at the Januario Cicco maternity School of the Federal University of Rio Grande do Norte (Natal, Rio Grande do Norte, Brazil) and was approved by the research ethics committee of the Federal University of Rio Grande do Norte (CAAE: 44712221.5.0000.5537). This study was registered in the Brazilian Registry of Clinical Trials (REBEC; RBR-2nwkr47), and the protocol was previously reported (Sampaio et al., 2023). Written informed consent and the authorization of the image use were obtained from the caregivers of the preemies on behalf of both before the start of the study.
Participants and recruitment
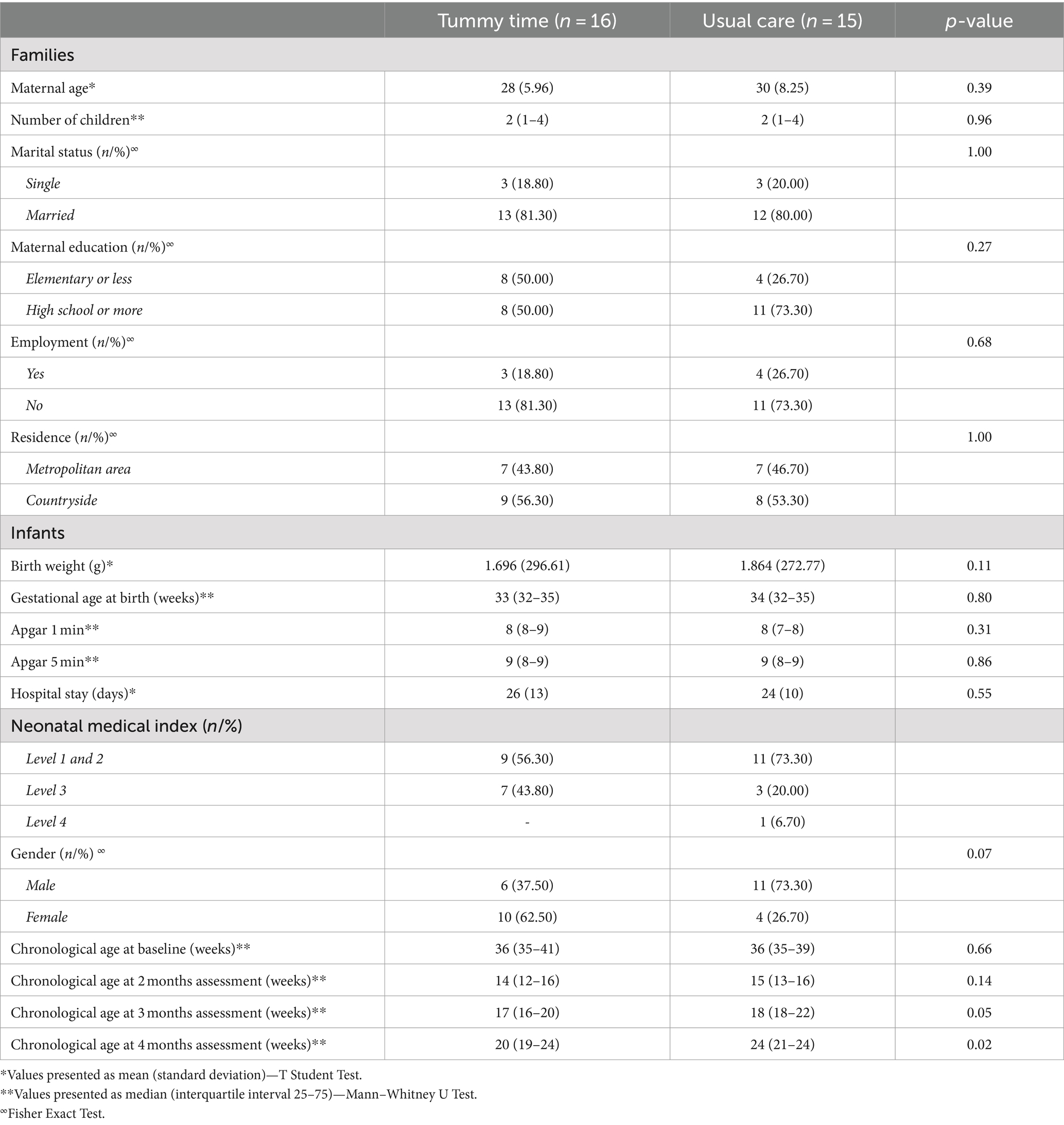
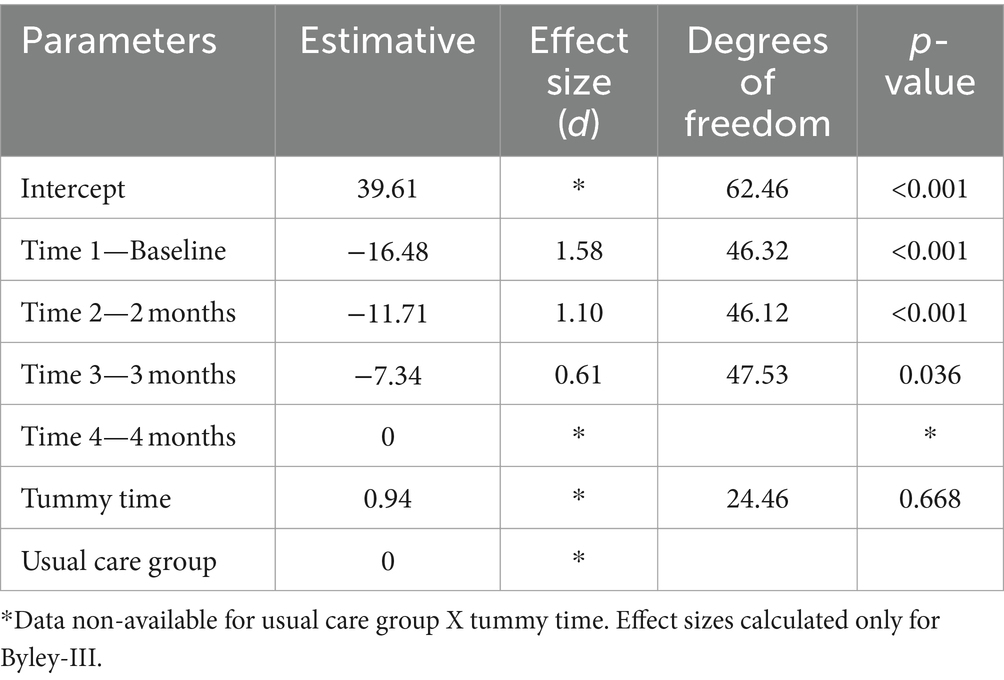
The families were recruited at the Januario Cicco pediatrics and childcare ambulatory care maternity school 48 h after hospital discharge (corresponding to the first outpatient consultation); recruitment occurred on spontaneous demand. Table 1 summarizes the characteristics of the participants.
The gestational age of the preemies, but not the age at hospital discharge, was controlled according to the inclusion criteria: caregivers with preemies born between 30 and 36 weeks and six days confirmed by ultrasound, adequate gestational age with a normal or poor repertoire in the general movements assessment. Exclusion criteria included brain injuries (e.g., intraventricular hemorrhage [grade 3 or 4], periventricular white matter injury, or hypoxic–ischemic encephalopathy), genetic syndrome (e.g., trisomy 21), or musculoskeletal deformity (e.g., limb deficiency). Medical complications and the neonatal medical index (ranges from 0 to 5; high scores indicate a higher risk of comorbidities) were extracted from the medical records of the preemies (Korner et al., 1993). After randomization, preemies who experienced any decline in health requiring hospitalization, who were relocated out of the state, or whose caregivers did not answer the contact were also excluded.
Retention and attrition
Forty preemies were eligible among the 60 enrolled during the study period; 31 provided their informed consent to participate in the study and completed the baseline assessment. Afterward, 26 and 18 preemies completed the assessment after two months and four months of corrected age, respectively (eight from the TT group and 10 from the usual care [UC] group). Three preemies from the TT group required hospitalization, and 10 caregivers (five from each group) did not reply to the contact attempts. Figure 1 illustrates the recruitment and retention of participants.
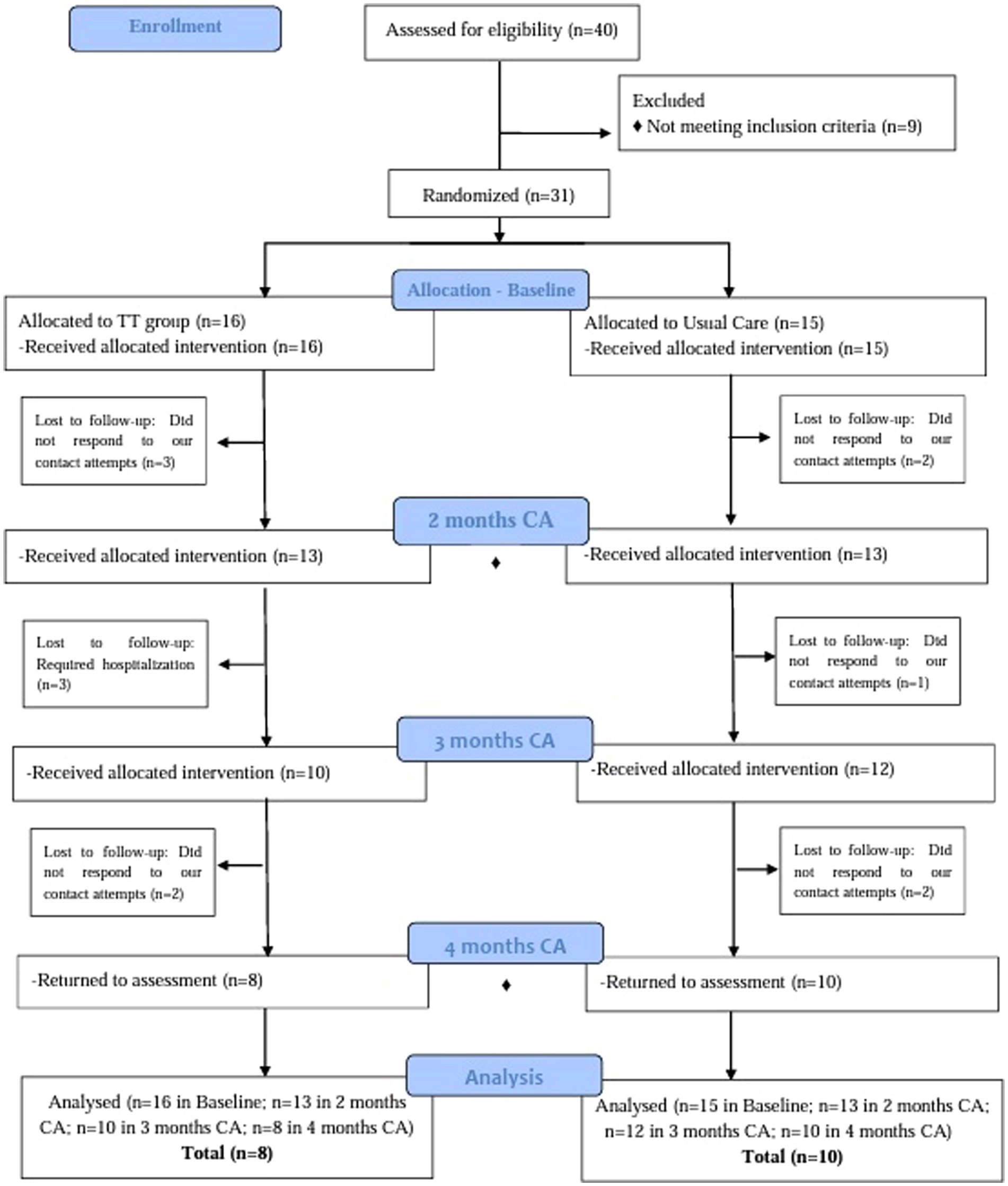
Figure 1. CONSORT flow chart. This flow chart showing the recruitment and retention of participants in each arm of the clinical trial. The kinematic analysis in the Kinovea® software was used in all assessments. ♦ Scale Bayley was administered at 2 and 4 months of corrected age.
Randomization and blinding
Preemies were randomized to TT or UC groups after baseline assessment using a computer-generated randomization sequence (Dallal, 2013). Both groups received UC as it would be unethical to withhold routine care. UC comprised the kangaroo mother care (KMC) (Brazil, 2017), a well-established practice known for its proven short- and mid-term effectiveness and safety that engages parents as the primary caregivers to meet the biological needs of the preemie (Dhage et al., 2023).
The KMC was implemented in Brazil by the Ministry of Health to guide the care of low-birth-weight preemies as part of policies for humanizing maternal and child care (Brazil, 2017). During hospitalization, KMC constitutes UC according to two components: (1) the kangaroo position that provides continuous skin-to-skin contact between mother and infant, resulting in thermal regulation and other benefits, and (2) exclusive breastfeeding. After hospital discharge, as part of the ambulatory care routine, physicians also verify the nutritional status based on weight, height, and body mass index-for-age and refer preemies to specialized services if needed (e.g., physiotherapy, psychology, nutritionist, phono audiology, and others). Furthermore, parents and caregivers were encouraged to increase the family interaction with the preemies using toys and active verbal communication (Brazil, 2017).
Caregivers from both groups received orientation about each protocol. Parents from the TT group were asked to place the preemies in the prone position for at least 20 min during daily life and playtime. During TT, parents were encouraged to stimulate their preemies using toys, sit or lie in front of them, maintain eye contact, engage in verbal communication, or sing (Figure 2A); illustrative examples for the TT were provided in a booklet (available in Supplementary material). The parents received these instructions during the first ambulatory care consultation on the same day they were invited to participate in the study.
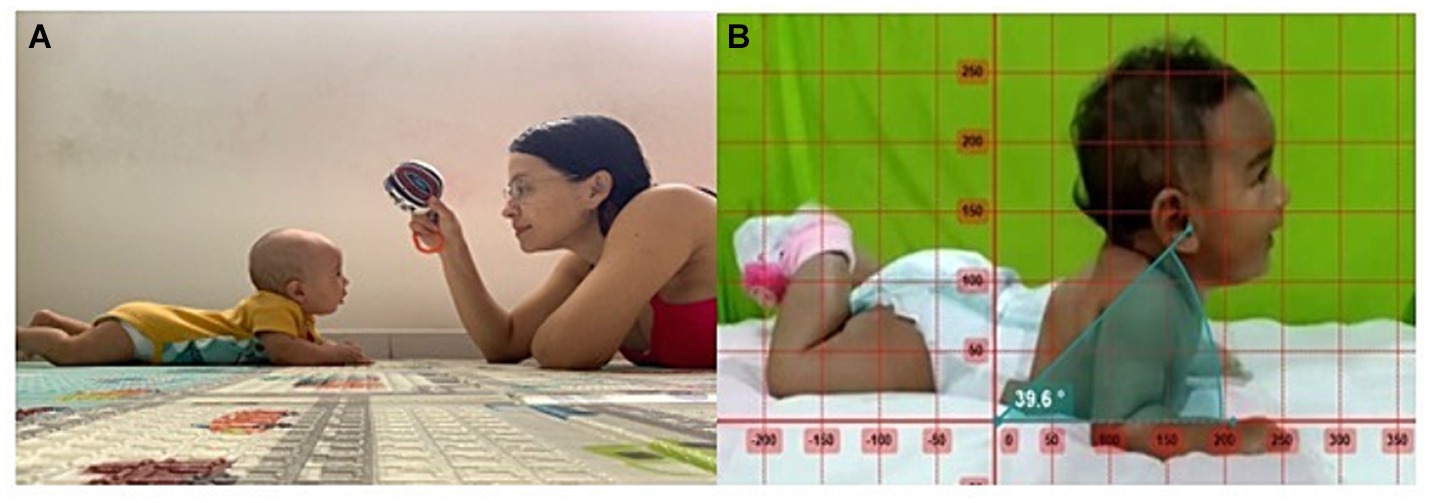
Figure 2. (A) Tummy time practice carried out by mother according to the handout. (B) The kinematic analysis in the Kinovea® software was performed using a 2D.
Telemonitoring visits were conducted at least once a week for all parents until their preemies reached three months of corrected age. During these visits, the interventionist reinforced the UC guidelines for all parents and provided additional guidance for TT. Parents were encouraged to register in a booklet the number of minutes the preemie remained in the prone position each day to ensure adherence to TT (available in the Supplementary material). The study interventionist (SSSS) was a board-certified pediatric physical therapist with experience in providing intervention in neonatal care and the first months of life. Moreover, SSSS received training and attended regular meetings to discuss intervention strategies with the researchers SAP and CDLA.
All assessments were blinded. Two researchers not involved in the study (NAAR and TLGS) conducted the assessments, and data were tabulated using predetermined encoding by another blinded researcher (IAG). The results were not disclosed to the study interventionist, and parents were instructed not to reveal the intervention they were performing.
Outcomes and follow-up
All preemies were assessed in person on the same schedule by a researcher blinded to the group assignment. However, the PHE assessment after three months of corrected age was recorded by the parents and sent via WhatsApp® to the interventionist. This evaluation was online to ensure the continuity of assessments even in financial and transportation difficulties. The PHE was assessed at baseline, two months (eight weeks after baseline), three months (end of follow-up), and four months (one month after the end of follow-up) of corrected age. Motor and cognitive development were assessed after two and four months of corrected age since they needed to be performed in person.
Primary outcomes
Prone head elevation (PHE)
PHE was measured using the Kinovea® software version 0.9.5 (Joan Charmant & Contributors, Bordeaux, France). The kinematic analysis was performed using a 2D measurement of movements recorded during the prone position, which considered the angle from the tragus of the ear to the supporting surface of the preemie (Bentzley et al., 2015; Figure 2B). This software presents adequate reliability, validity, and reproducibility for analyzing dynamic movements (Fernández-González et al., 2020; Puig-divı et al., 2019). All assessments were performed individually in the presence of caregivers. The PHE was recorded for 2 min for all preemies. During the recording, they were encouraged to focus on a toy displayed between 4 and 6 in. above the eye line.
Secondary outcome measures
Motor and cognitive development
Bayley Scales of Infant and Toddler Development, third edition (Bayley-III) was used to assess the motor and cognitive development at two and four months of corrected age. This scale was translated, validated, and adapted for Brazilian children (Madaschi et al., 2016). Normative values on the Bayley-III include composite scores for cognitive and motor outcomes with a mean of 100 and a standard deviation of 15. All assessments were performed individually in the presence of caregivers at the pediatrics and childcare ambulatory care. An interventionist trained in the Bayley-III scale conducted all the assessments following the guidelines (Bayley, 2006).
At two and four months, the motor assessment using the Bayley-III primarily focused on the head control in the vertical, ventral suspension, and prone position, as well as their duration. On the other hand, the cognitive assessment encompassed items related to the interaction of the baby with the environment, such as object observation, exploration, and visual preference (Bayley, 2006).
The reversal rule was considered in the assessments, as the infant scored 1 on the first three items from the starting point compatible with their age. The age-corrected score was considered in the case of a preemie. However, the assessment returned to the corresponding starting point for the previous age if the preemie scored zero in any of the first three items, and was interrupted if the preemie scored zero in five consecutive items (Bayley, 2006).
Statistical analysis
The a priori statistical analysis considered that data collection from 14 preemies (seven per group) provided the statistical power needed to detect differences between groups in the primary outcomes with an alpha of 5 and 80% power (29). Data normality was assessed using the Shapiro–Wilk test. Bayley motor composite and cognitive composite scores were expressed as mean and standard deviation.
Frequency distribution and percentages described categorical variables. The Mann–Whitney U test was used to compare medians (number of infants, Apgar, and chronological age). The chi-square test or Fisher exact test (for the categories with less than five cases) was applied for gender, marital status, educational level, familiar income, and housing between TT and UC groups.
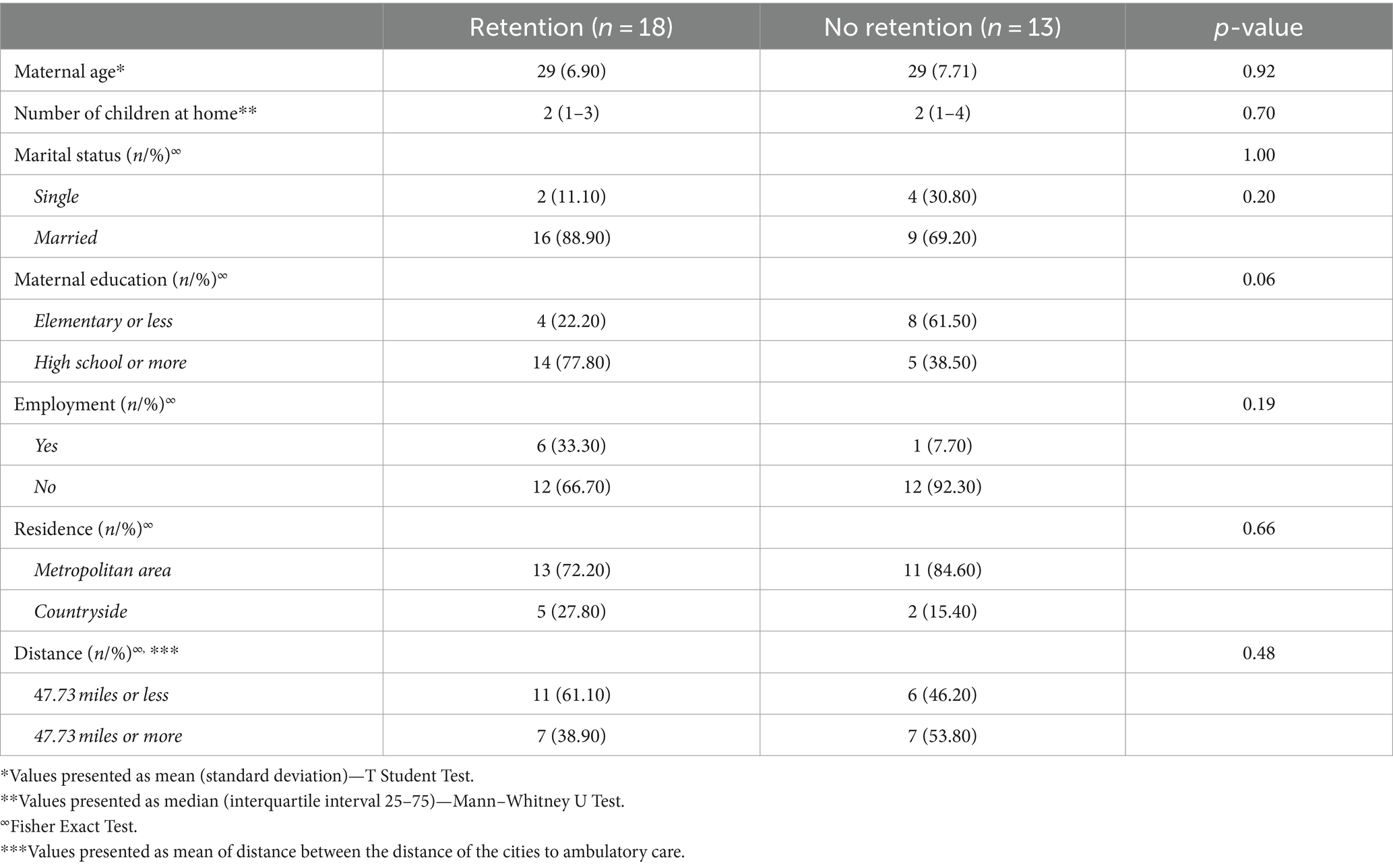
PHE was assessed using the linear mixed model according to the group (TT and UC) and time (i.e., baseline, two months, three months, and four months).
Bayley-III composite scores were compared using the Student’s t-test for unpaired samples from both groups at two and four months of corrected age. Additionally, effect sizes were calculated to verify the differences between the Bayley-III composite scores (motor and cognitive components) after two and four months of corrected age. The significance level adopted was 5%. All analyses were conducted using the Statistical Package for Social Science (SPSS) software, version 25 (IBM Corp., USA).
Results
All families were from the Brazilian northeast, self-declared brown, completed prenatal care, and presented poor socioeconomic conditions. Most mothers (77.4%) reported no household income, and seven (22.6%) lived in rural areas. Among the 31 preemies, 10 were delivered via cesarean section, and three required mechanical ventilation during hospitalization. None of the preemies received sedation medication, and the hospital length of stay ranged from 8 to 54 days. Based on the neonatal medical index, 20 preemies were classified at level 1 or 2, 10 at level 3, 1 at level 4, and no preemie ranked at level 5 (Table 1).
Description of UC group
All caregivers performed KMC daily at home and maintained exclusive breastfeeding. The nutritional status percentiles for all preemies were between the 5th and 95th curves (WHO Multicentre Growth Reference Study Group, 2006), and none were referred to specialized infant rehabilitation services. The mean duration of telemonitoring visits ranged from five to 15 min (mean of 9 min) twice a week, and the intervals between meetings ranged from two to three days. Caregivers usually presented no doubts about the routine care.
Description of TT group
The mean time for TT was 17 min, ranging from 10 to 30 min per day. All caregivers self-declared enjoying having playtime with their preemies during TT. The mean duration of telemonitoring meetings ranged from 10 to 20 min (mean of 13 ± 3 min) twice a week with intervals ranging from two to three days. Caregivers usually presented no doubts regarding the positions illustrated in the booklet. Moreover, three preemies from the TT group were hospitalized with respiratory infections.
Primary outcomes
Prone head elevation (PHE)
PHE was 23.59 ± 7.67 degrees in both groups at baseline and increased up to 39.77 ± 2.73 degrees at four months of correct age. The comparison of the degrees between groups over the timeline is shown in Figure 3. The PHE presented significant interaction between time and the increase in the PHE angle (p = 0.001). However, no significant group-time interactions were observed between groups (p = 0.668; Table 2). The calculated effect sizes are shown in Table 2. The PHE degrees increased to 4.77 degrees after two months (d = 1.58), 9.14 degrees after three months (effect size = 1.10), and 16.48 degrees after four months (effect size = 0.61) compared with baseline (evaluation 1) (Table 2).
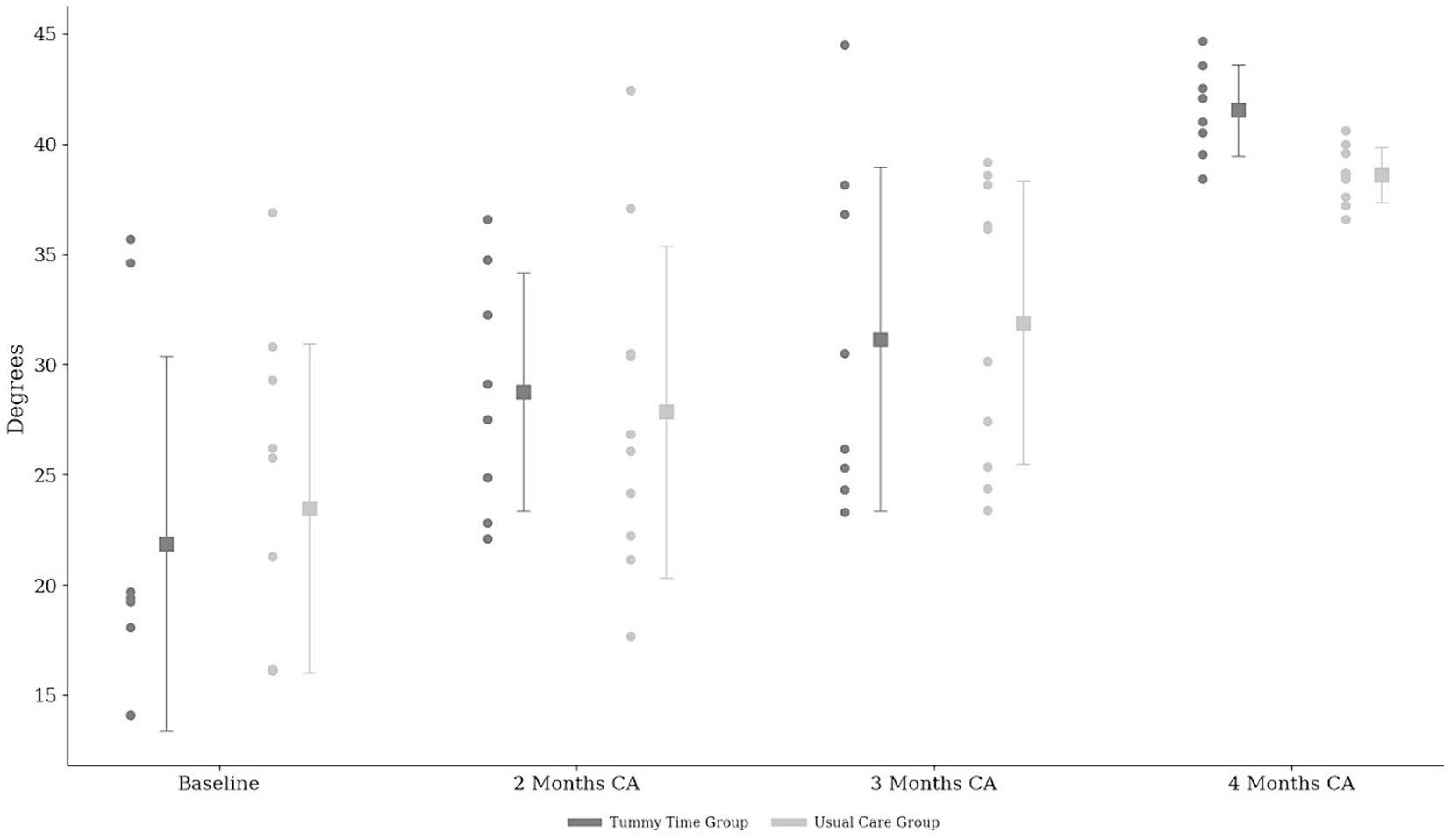
Figure 3. The angles for prone head elevation between groups over a timeline and the individual trajectories of each subject. Values presented as mean and the individual trajectories of each subject throughout the assessments. ▪ Mean values for each group and time period and the standard deviation; CA, corrected age.
Secondary outcomes
Developmental outcomes
During the study period (October 2021 to September 2022), 26 Bayley-III assessments were administered at two months, and 18 after four months of corrected age. The Bayley-III motor composite score was significantly different between TT (117.85 ± 9.67) and UC (85.91 ± 13.81) groups after two months (t [6.71] = 19.27, p < 0.001), with effect size d = 2.81. This component was also different between TT (126.62 ± 16.15) and UC (87.80 ± 18.54) groups after four months of corrected age (t [4.74] = 15.84, p < 0.001); effect size of d = 1.46 (Figure 4).
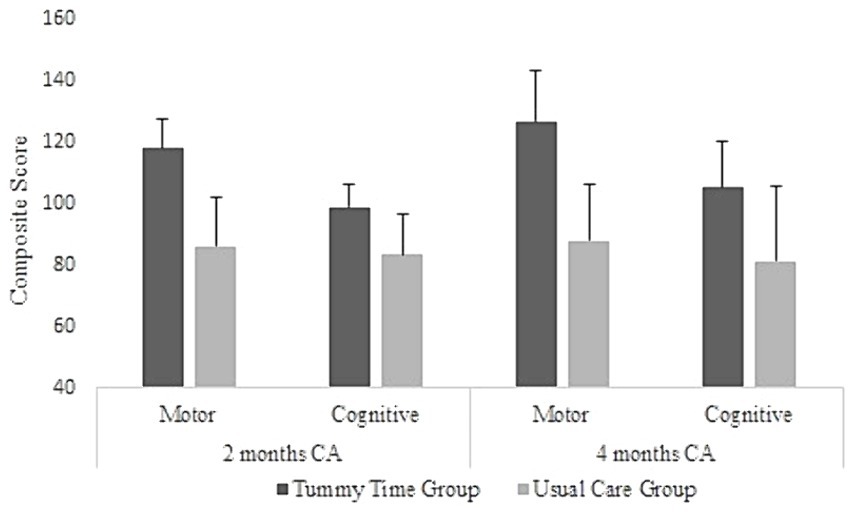
Figure 4. Bayley composite scores for motor and cognitive components and groups. Values presented as mean and the standard deviation; CA, corrected age.
The Bayley-III cognitive composite score of the TT group was increased (98.57 ± 7.44) compared with the UC (83.33 ± 13.37) group after two months (t [3.50] = 16.63, p = 0.003), presenting an effect size of d = 2.30. Importantly, two preemies from the UC group presented results below the mean. Furthermore, the TT group presented an increased cognitive composite score (105.00 ± 14.88) compared with the UC group (81.00 ± 24.24) after four months of corrected age (t [2.58] = 15.15, p = 0.021); effect size of d = 1.20 (Figure 4). The UC group presented scores that were one standard deviation below the mean on the composite cognitive scale at both ages assessed. All preemies scoring below one standard deviation on the composite score of the Bayley Scale in both motor and cognitive skills were referred to specialized infant rehabilitation services.
Participants who dropped out
Thirty-one preemies were assessed at baseline, and 18 were reassessed after four months of corrected age. Sixteen preemies were included in the TT group: two withdrew at two months of corrected age and six at three months. Fifteen preemies were included in the UC group: three withdrew at two months, two at three months, and two at four months of corrected age. Among those who dropped out, two (15.4%) lived in rural areas. The distance between the residences to the pediatrics and childcare ambulatory ranged from 12.42 to 152.85 miles. Table 3 describes the socioeconomic conditions of the families of the remaining and dropped preemies. No significant differences were observed between groups.
Discussion
This randomized clinical trial was the first study to assess the effect of daily TT on the PHE and motor and cognitive development of preemies. Considering that previous studies discussed how different stimuli in environmental exploration trigger a developmental cascade that improves motor and cognitive development (Adolph and Hoch, 2019; Kretch et al., 2014; Lee and Galloway, 2012; Soska and Adolph, 2014), this study hypothesized whether daily TT could improve motor and cognitive development in preemies compared with those not engaged in this practice.
The present study showed that TT may increase PHE degree over time, confirming the first hypothesis. This position contributes to early development by strengthening head, neck, and trunk muscles, enhancing mobility and motor control (Adolph and Hoch, 2019; Lee and Galloway, 2012; Wentz, 2017).
The preemies from the TT group presented improved motor and cognitive scores compared with those from the UC group. Furthermore, these findings were associated with enhanced PHE angle, corroborating the second hypothesis of this study. The TT stimulates preemies to develop motor, cognitive, and sensory skills by presenting new environmental challenges. Moreover, TT enhances manual dexterity and visual function, improving accuracy and attention. These physical and sensory experiences contribute to varied developmental paths, enhancing problem-solving skills and cognitive abilities in infants (Adolph and Hoch, 2019; Hadders-Algra, 2018; Kretch et al., 2014).
A longitudinal study addressing the benefits of TT on motor and cognitive outcomes showed that healthy full-term infants presented improved motor development between one and six months of life (Silva et al., 2023). Therefore, infants who practiced the prone position were more likely to achieve motor skills expected for their age. Furthermore, a systematic review showed that daily parent-delivered interventions were more effective in improving cognitive and motor outcomes in preemies than other interventions in the short and possibly long term (Khurana et al., 2020), corroborating the positive association between TT and improved cognitive performance observed in the present study.
Although the PHE angle increased over time, its values were not different between groups. This finding is possibly related to the UC associated with the KMC performed by both groups (Brazil, 2017). This method involves positioning infants in a kangaroo position on the chest of the parent to maximize skin-to-skin contact. This positioning supports physiological benefits, such as temperature regulation, bonding, and breastfeeding (Akbari et al., 2018; Dhage et al., 2023; Durmaz et al., 2023), and also facilitates neck muscle activation and head training (Wang et al., 2021). Since isolating the effects of the two interventions is unfeasible as it would be unethical, further studies could assess the existence of a cumulative effect.
The effects of TT may also be extended to preemies at risk of developmental delays due to immature neurological (Altimier and Phillips, 2018) or musculoskeletal (Drzał-grabie, 2019) systems. Although TT is already recommended for preemies (Clark and Kingsley, 2020), previous studies did not investigate its effects in this population. Therefore, encouraging TT may be a supportive strategy for parents of preemies to enhance their movements. Active involvement and empowerment of families are crucial factors in improving the environment and the development of preemies (Ferreira et al., 2020).
Early stimulation by family members promotes daily stimuli that improve the development of preemies, as well as the development of knowledge, capacity, and ability of the parents to identify the needs of their preemies (Ferreira et al., 2020). The best motor and cognitive results associated with early stimulation are related to the environmental setup that supports the self-regulatory mechanisms of the preemie and opportunities for exploration, promoting the development of primary and secondary variability. All these aspects are facilitated by direct interaction with their parents (Hadders-Algra, 2018). In addition, this type of intervention provides opportunities for early stimulation in low-income countries, where part of the population faces socioeconomic barriers and difficult access to specialized health centers (Nanyunja et al., 2022). The TT promotes family participation in a cost-effective intervention starting after hospital discharge, empowering the care of parents for their preemies.
Although this study stands as the first clinical trial examining the impacts of TT in preemies, the interpretation of the results may be limited due to the number of dropouts during the study. Notably, the Northeast region of Brazil ranks among the areas with the highest levels of vulnerability to poverty. This circumstance often leads to financial constraints to access transportation and specialized healthcare facilities (Brazil, 2024).
In this sense, strategies must be implemented to ensure access to interventions that reduce the risk of developmental delays in vulnerable infants, including preemies. Therefore, the TT is a feasible strategy to facilitate early intervention in low- and middle-income countries by empowering parents to establish a daily routine with their preemies. This intervention may be encouraged during hospitalization and reinforced during outpatient follow-up. Thus, healthcare professionals must be stimulated to disclose information using educational approaches (e.g., illustrative booklets).
Conclusion
The PHE increased over time but it was not significantly different between groups. Nevertheless, the results suggest that the TT possibly improves the motor and cognitive development of preemies. This finding may be a feasible strategy in early stimulation to reduce barriers to access in low- and middle-income countries.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics and Research Committee of the Federal University of Rio Grande do Norte, CAAE:44712221.5.0000.5537, (number: 4.699.000) and by the Brazilian Clinical Trials Registry (protocol RBR-2nwkr47). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any identifiable images or data included in this article.
Author contributions
SS: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Writing – original draft, Writing – review & editing. NA: Conceptualization, Investigation, Methodology, Resources, Writing – review & editing. TS: Conceptualization, Methodology, Resources, Writing – review & editing. JM: Conceptualization, Methodology, Resources, Writing – review & editing. IA: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Writing – review & editing. CL-A: Conceptualization, Formal analysis, Methodology, Resources, Supervision, Writing – review & editing. SP: Conceptualization, Formal analysis, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Coordination of Superior Level Staff Improvement, (CAPES) Grant/Award Number: Code 001.
Acknowledgments
CAPES—code 001, CNPQ—Public Notice PIBIC, and the families who agreed to participate in the study, Maternidade Escola Januário Cicco and Empresa Brasileira de Serviços Hospitalares.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1289446/full#supplementary-material
References
Adolph, K. E., and Hoch, J. E. (2019). Motor development: embodied, embedded, enculturated, and enabling. Annu. Rev. Psychol. 70, 141–164. doi: 10.1146/annurev-psych-010418-102836
Akbari, E., Binnoon-erez, N., Rodrigues, M., Ricci, A., Schneider, J., Madigan, S., et al. (2018). Kangaroo mother care and infant biopsychosocial outcomes in the first year: a meta-analysis. Early Hum. Dev. 122, 22–31. doi: 10.1016/j.earlhumdev.2018.05.004
Altimier, L., and Phillips, R. (2018). Neuroprotective care of extremely preterm infants in the first 72 hours after birth. Crit. Care Nurs. Clin. North Am. 30, 563–583. doi: 10.1016/j.cnc.2018.07.010
Baggett, K. M., Davis, B., Landry, S. H., Feil, E. G., Whaley, A., Schnitz, A., et al. (2020). Understanding the steps toward Mobile early intervention for mothers and their infants exiting the neonatal intensive care unit: descriptive examination. J. Med. Internet Res. 22, e18519–e18511. doi: 10.2196/18519
Bayley, N. (2006). Bayley scales of infant and toddler development. 3rd Edn. San Antonio, TX: Pearson.
Bentzley, J. P., Coker-Bolt, P., Moreau, N. G., Hope, K., Ramakrishnan, V., Brown, T., et al. (2015). Kinematic measurement of 12-week head control correlates with 12-month neurodevelopment in preterm infants. Early Hum. Dev. 91, 159–164. doi: 10.1016/j.earlhumdev.2015.01.001
Boutot, E. A., and DiGangi, S. A. (2018). Effects of activation of preferred stimulus on tummy time behavior of an infant with down syndrome and associated Hypotonia. Behav. Anal. Pract. 11, 144–147. doi: 10.1007/s40617-018-0212-5
Brazil, M. D. S. (2017). Atenção Humanizada ao Recém – Nascido – Método Canguru. 3rd Edn. Brasília, DF.
Brazil . (2024). Atlas of human development. Available at: http://www.atlasbrasil.org.br (Accessed June 22, 2024).
Clark, G. F., and Kingsley, K. L. (2020). Occupational therapy practice guidelines for early childhood: birth-5 years. Am. J. Occup. Ther. 74, 7403397010p1–7403397010p42. doi: 10.5014/ajot.2020.743001
Dallal, G. (2013). Randomization.com. Available at: http://www.randomization.com (Accessed April 1, 2021).
Dhage, V. D., Rannaware, A., and Choudhari, S. G. (2023). Kangaroo mother Care for low-Birth-Weight Babies in low and middle-income countries: a narrative review. Cureus 15:e38355. doi: 10.7759/cureus.38355
Drzał-grabie, J. (2019). Parameters characterizing the posture of preterm children in standing and sitting position un corrected proof version correct. J. Back Musculoskelet. Rehabil. 33, 455–462. doi: 10.3233/BMR-170882
Durmaz, A., Sezici, E., and Akkaya, D. D. (2023). The effect of kangaroo mother care or skin-to-skin contact on infant vital signs: a systematic review and meta-analysis. Midwifery 125:103771. doi: 10.1016/j.midw.2023.103771
Fernández-González, P., Koutsou, A., Cuesta-Gómez, A., Carratalá-Tejada, M., Miangolarra-Page, J., and Molina-Rueda, F. (2020). Reliability of Kinovea ® software and agreement with a three-dimensional motion system for gait. Sensors 20:3154. doi: 10.3390/s20113154
Ferreira, R. D. C., Alves, C. R. L., Guimarães, M. A. P., Menezes, K. K. P., and Magalhães, L. C. (2020). Effects of early interventions focused on the family in the development of children born preterm and/or at social risk: a meta-analysis. J. Pediatr. 96, 20–38. doi: 10.1016/j.jped.2019.05.002
Hadders-Algra, M. (2018). Early human motor development: from variation to the ability to vary and adapt. Neurosci. Biobehav. Rev. 90, 411–427. doi: 10.1016/j.neubiorev.2018.05.009
Hewitt, L., Stanley, R., and Okely, A. (2017). Correlates of tummy time in infants aged 0–12 months old: a systematic review. Infant Behav. Dev. 49, 88–97. doi: 10.1016/j.infbeh.2017.11.008.Child
Khurana, S., Kane, A. E., Brown, S. E., Tarver, T., and Dusing, S. C. (2020). Effect of neonatal therapy on the motor, cognitive, and behavioral development of infants born preterm: a systematic review. Dev. Med. Child Neurol. 62, 684–692. doi: 10.1111/dmcn.14485
Korner, A. F., Steverson, D. K., Kraemer, H. C., Spiker, D., and Scott, D. T. (1993). Prediction of the development of low birth weight preterm infants by a new neonatal medical index. J. Dev. Behav. Pediatr. 14, 106–111. doi: 10.1097/00004703-199304000-00005
Kretch, K. S., Franchak, J. M., and Adolph, K. E. (2014). Crawling and walking infants see the world differently. Child Dev. 85, 1503–1518. doi: 10.1111/cdev.12206
Lee, H., and Galloway, J. C. (2012). Early intensive postural and MovementTraining advances head control in very young infants. Phys. Ther. 92, 935–947. doi: 10.2522/ptj.20110196
Lyne, H., Burgoine, K., Ogara, C., Ditai, J., and Gladstone, M. (2022). ‘They said, let's teach you how you are going to care for the child at home…’: caregivers' and healthcare worker's perceptions and experiences of post-discharge preterm care in eastern Uganda. BMC Health Serv. Res. 22:1521. doi: 10.1186/s12913-022-08894-3
Madaschi, V., Mecca, T. P., Macedo, E. C., and Paula, C. (2016). Bayley-III scales of infant and toddler development: transcultural adaptation and psychometric properties. Paidéia (Ribeirão Preto) 26, 189–197. doi: 10.1590/1982-43272664201606
Ministério da Saúde . (2024). Cadastro Nacional de Estabelecimentos de Saúde – Datasus. Available at: https://datasus.saude.gov.br/cnes-estabelecimentos (Accessed June 16, 2024).
Nanyunja, C., Sadoo, S., Kohli-Lynch, M., Nalugya, R., Nyonyintono, J., Muhumuza, A., et al. (2022). Early care and support for young children with developmental disabilities and their caregivers in Uganda: the baby Ubuntu feasibility trial. Front. Pediatr. 10, 1–16. doi: 10.3389/fped.2022.981976
Novak, I., Morgan, C., Fahey, M., Finch-edmondson, M., Galea, C., Hines, A., et al. (2020). State of the evidence traffic lights 2019: systematic review of interventions for preventing and treating children with cerebral palsy. Curr. Neurol. Neurosci. Rep. 20, 3–21. doi: 10.1007/s11910-020-1022-z
Puig-divı, A., Escalona-Marfil, C., Padulles-Riu, J., Busquets, A., Padulles-Chando, X., and Marcos-Ruiz, D. (2019). Validity and reliability of the Kinovea program in obtaining angles and distances using coordinates in 4 perspectives. PLoS One 14, 1–14. doi: 10.5281/zenodo.2843847
Rosenberg, S. A., Robinson, C. C., Shaw, E. F., and Ellison, M. C. (2013). Part C early intervention for infants and toddlers: percentage eligible versus served. Pediatrics 131, 38–46. doi: 10.1542/peds.2012-1662
Sampaio, S. S. S., de Amorim Rodrigues, N. A., Moura, J. R., de Lima-Alvarez, C. D., and Pereira, S. A. (2023). Effects of prone positioning on head control in preterm infants: randomized and controlled clinical trial protocol. Int. J. Environ. Res. Public Health 20:2375. doi: 10.3390/ijerph20032375
Silva, B. F. V. E., Sampaio, S. S. S., Moura, J. R., De Medeiros, C. E. B., De Lima-Alvarez, C. D., Simão, C. R., et al. (2023). “I am afraid of positioning my baby in prone”: beliefs and knowledge about tummy time practice. Int. J. Pediatr. 2023, 1–7. doi: 10.1155/2023/4153523
Smith, E. R., Bergelson, I., Constantian, S., Valsangkar, B., and Chan, G. J. (2017). Barriers and enablers of health system adoption of kangaroo mother care: a systematic review of caregiver perspectives. BMC Pediatr. 17, 1–16. doi: 10.1186/s12887-016-0769-5
Soska, K. C., and Adolph, K. E. (2014). Postural position constrains multimodal object exploration in infants. Infancy 19, 138–161. doi: 10.1111/infa.12039
Twardzik, E., Cotto-negr, C., and Macdonald, M. (2017). Factors related to early intervention part C enrollment: a systematic review. Disabil. Health J. 10, 467–474. doi: 10.1016/j.dhjo.2017.01.009
Wang, Y., Zhao, T., Zhang, Y., Li, S., and Cong, X. (2021). Positive effects of kangaroo mother care on long-term breastfeeding rates, growth, and neurodevelopment in preterm infants. Breastfeed. Med. 16, 282–291. doi: 10.1089/bfm.2020.0358
Watson, A. (2013). Understanding neurodevelopmental outcomes of prematurity. Adv. Neonatal Care 10, 188–193. doi: 10.1097/ANC.0b013e3181e9414b
Wentz, E. E. (2017). Importance of initiating a tummy time intervention early in infants with down syndrome. Pediatr. Phys. Ther. 29, 68–75. doi: 10.1097/PEP.0000000000000335
WHO Multicentre Growth Reference Study Group (2006). WHO child growth standards 528 based on length/height, weight and age. Acta Paediatr. 450, 76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x
World Health Organization . (2019). Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. Geneva: World Health Organization.
Keywords: motor skill, premature birth, tummy time, prone position, infant development, low-income countries, intervention
Citation: Sampaio SSS, Amorim Rodrigues NA, Souza TLG, Moura JR, Azevedo IG, Lima-Alvarez CD and Pereira SA (2024) Cognitive and motor improvement by tummy time practice in preemies from low-income settings: a randomized clinical trial. Front. Psychol. 15:1289446. doi: 10.3389/fpsyg.2024.1289446
Edited by:
Pamela Bryden, Wilfrid Laurier University, CanadaReviewed by:
Marie Martel, University of Surrey, United KingdomShaziela Ishak, Ramapo College, United States
Copyright © 2024 Sampaio, Amorim Rodrigues, Souza, Moura, Azevedo, Lima-Alvarez and Pereira. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Silvana Alves Pereira, c2lsdmFuYS5hbHZlc0B1ZnJuLmJy
†These authors have contributed equally to this work
 Sabrinne Suelen Santos Sampaio
Sabrinne Suelen Santos Sampaio Nathalia Allana Amorim Rodrigues
Nathalia Allana Amorim Rodrigues Thalyson Luiz Gomes Souza1†
Thalyson Luiz Gomes Souza1† Julia Raffin Moura
Julia Raffin Moura Ingrid Guerra Azevedo
Ingrid Guerra Azevedo Carolina Daniel Lima-Alvarez
Carolina Daniel Lima-Alvarez Silvana Alves Pereira
Silvana Alves Pereira