
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 06 February 2024
Sec. Quantitative Psychology and Measurement
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1339902
 Issaku Kawashima1*
Issaku Kawashima1* Tomoko Hinuma1
Tomoko Hinuma1 Masatoshi Nagata2
Masatoshi Nagata2 Akio Yoneyama2
Akio Yoneyama2 Masaru Honjo3
Masaru Honjo3 Hiroaki Kumano4
Hiroaki Kumano4 Saori C. Tanaka1,5*
Saori C. Tanaka1,5*This study was undertaken to translate the Standardised Assessment of Personality – Abbreviated Scale (SAPAS) into Japanese and to evaluate its validity and reliability. SAPAS is one of the most rapid tools for assessing personality disorder (PD) and has excellent sensitivity and good specificity, whereas other PD assessment tools require such a significant investment of time that they are infeasible for large surveys or routine clinical practice. Customary assessment in clinical practice ideally incorporates screening for PD, as it is associated with a substantial public health burden, including premature mortality and increased health service utilization. Furthermore, PD’s status as a key prognostic variable of mental disorders also drives PD screening. While SAPAS has been translated into several languages, there has been no Japanese version. Therefore, we translated SAPAS into Japanese (SAPAS-J) and evaluated its reliability and validity. Study 1 recruited undergraduates to reveal its test–retest reliability. Although its internal consistency was not high, since the intent of the original SAPAS was to assess the broad character of personality disorder with the fewest possible items, minimal correlations between items were reasonable. We tested two factorial models, the single-factor model and the higher-order-single-factor model, and the latter offered better fitting. This higher-order model contained a three-factor structure corresponding to clusters described in DSM-5. It measures general PD traits as a common higher-order latent variable comprising those factors. Correlations of SAPAS-J with the much longer PD screening questionnaire in Study 1 and depressive and anxiety symptoms in Study 2 from the general population support its validity. Although validation for the clinical use of SAPAS-J is limited, our research with non-clinical populations demonstrated sufficient validity to justify its use in the context of psychopathological analog research. Since PD is understood as a continuum, the severity of which is distributed dimensionally, the analog study recruiting from the general population and attempting to reveal psychopathological mechanisms of PD is meaningful.
The purpose of this study was to translate the Standardised Assessment of Personality – Abbreviated Scale (SAPAS; Moran et al., 2003) into Japanese and to evaluate its validity and reliability. SAPAS is one of the most efficient screening tools for personality disorder (PD), the mental disorder characterized by pervasive, inflexible, and enduring experiential/behavioral patterns that deviate from the expectations of the individual’s culture and cause distress and impairment of functioning (American Psychiatric Association, 2013b). SAPAS has excellent sensitivity and good specificity to screen patients with PD (Moran et al., 2003) and captures variance specifically associated with PD rather than variance of general personality traits (Ball et al., 2017). The SAPAS score also correlates with several PD-related symptoms, including depression, anxiety, and impairment of social function (Goddard et al., 2015). While it was originally developed as a structured interview, it was also validated as a questionnaire (Germans et al., 2008) in clinical populations. Moreover, SAPAS is one of the most rapid tools for assessing PD since it has only eight items, whereas other PD assessment tools, including structured interviews (1–2 h to complete) and questionnaires (85–390 items) are infeasible for routine clinical practice or large surveys (Tyrer et al., 2015).
Routine assessment in clinical practice ideally incorporates screening of PD (Moran et al., 2003; Fok et al., 2015), given that PD constitutes a major mental health burden. Life expectancy at birth among patients with PD is 18.7 years less for women and 17.7 years less for men than for the general population (Fok et al., 2012). Reported quality-of-life scores of patients with PD are lower than those of patients with major depressive disorder (Laurenssen et al., 2016). The economic cost of PD was estimated as €16,879 per year (Laurenssen et al., 2016) and it is reported that PD increases health service costs not only in psychiatry but also in non-mental health services (Kavanagh et al., 2021). One of the reasons for this is treatment-seeking motivated by difficulties in accessing appropriate care (Kavanagh et al., 2021). Routine PD screening in non-mental health services would help to overcome this problem.
Furthermore, the fact that PD is a key prognostic variable of mental disorders motivates PD screening. The comorbidity of PD decreases the remission rate of main symptoms in several mental disorders, including anxiety disorders (Massion et al., 2002; Carlier et al., 2014), body dysmorphic disorder (Phillips et al., 2005), depression, and somatoform disorder (Carlier et al., 2014). While the global prevalence of PD is estimated at 7.8% (Winsper et al., 2020), the comorbidity rate among mental disorders is much higher. For example, 45–77% of patients with major depressive disorder exhibit PD comorbidity (Friborg et al., 2014; Wongpakaran et al., 2015). Hence, screening tools for PD help formulate prognoses for treatment. The SAPAS score predicts the dropout rate (Goddard et al., 2015) and suboptimal responses from psychotherapy (Goddard et al., 2015; Mars et al., 2021) and antidepressants (Gorwood et al., 2010). Furthermore, SAPAS items contribute to personalized psychotherapy recommendations based on machine learning (Delgadillo et al., 2017, 2022).
In brief, SAPAS is the most efficient screening tool for PD. It helps to introduce patients to appropriate treatment and predicts prognoses of comorbid mental disorders. While SAPAS has now been translated into several languages, including Spanish, French, Danish, and Bengali (Sen et al., 2021), there has been no Japanese version. Therefore, we translated SAPAS into Japanese (SAPAS-J) and evaluated its reliability and validity.
To establish the validity and reliability of the SAPAS, we performed two studies. The first study investigated internal consistency, test–retest reliability, and convergent and structural validity. The second study compensated for some limitations of Study 1 and supported its convergent validity.
Study protocols were approved by an ethics committee and were not preregistered. To perform these analyses, we used Python (version 3.10.6), R (version 4.2.2), Pingouin-stats (version 0.5.3; Vallat, 2018), and Lavaan (version 0.6.13; Rosseel, 2012).
In the first study, 110 (31 men) undergraduates at a university in Japan provided valid answers. The average age was 23.27 years (SD = 6.77). Among participants, 58 responded to the Depression and Anxiety Mood Scale (DAMS; Fukui, 1997) and 97 to the Personality Diagnostic Questionnaire-Revised (PDQ-R; Hyler et al., 1992). Two weeks after the first survey, we retested using SAPAS-J, and 33 participants responded.
SAPAS-J, the questionnaire translated in the current study, is an eight-item assessment of PD tendency. The authors, including a medical doctor of psychosomatic medicine, translated the original SAPAS into Japanese. While the original SAPAS and the self-reporting version of SAPAS (Germans et al., 2008) used dichotomous (yes/no) questions, SAPAS-J employs a 4-response Likert-scale (1. False for me; 2. Somewhat false for me; 3. Somewhat true for me; 4. True for me). Binary questions can be completed more quickly; however, nuanced answers are forced into “yes” or “no” and tend to be “yes” (Rivera-Garrido et al., 2022). Therefore, we adopted a scaled rating in order to capture more subtle psychopathology to improve its specificity. The author of the original SAPAS checked the back-translated SAPAS-J and confirmed that the meanings of the original questions were retained. SAPAS-J is available in the Supplementary material and is available for anyone to use for research purposes.
PDQ-R is a self-report assessment tool for PD. The original (Hyler et al., 1992) and the Japanese version (Uehara et al., 1997) of PDQ-R show sufficient validity and reliability. Diagnostic comparisons with semi-structured interview assessments revealed that PDQ-R has low specificity, but fairly high sensitivity (Hyler et al., 1992). However, we used this questionnaire to validate SAPAS because a high-sensitivity/low-specificity assessment tool may produce sufficient variation among non-clinical populations. PDQ-R was also employed among non-clinical populations to assess general PD traits using its total score (Trull et al., 1993), although it was originally developed to detect patients with PD. We abbreviated the 31 duplicated items and items in a dummy factor and used 121 items.
DAMS, a 7-point Likert 9-item questionnaire having high validity and reliability, assesses depressive and anxious moods in the preceding two or 3 days (Fukui, 1997; Takahashi et al., 2021). DAMS has three factors: positive mood, negative mood, and anxious mood.
We performed two patterns of confirmatory factorial analyses. As in the original SAPAS, we assumed that the SAPAS-J total score measures transdiagnostic general PD traits, and prepared a single-factor model in which all items were explained by one factor. Additionally, we tested the higher-order model in which items were classified into three factors, corresponding to clusters described in the Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-5; American Psychiatric Association, 2013b). Since PD includes a wide range of symptoms and SAPAS was developed based on the cluster model of DSM, we considered that the three-factor model would explain the structure of SAPAS better than a single-factor model. However, SAPAS was originally developed as a scale for measuring only one construct, i.e., general PD trait. Furthermore, considering the brevity of SAPAS, the interpretation of each subscale is not informative. Hence, in the model, we devised one higher-order factor that included those three factors. We calculated CFI, RMSEA, and SRMR as indices of goodness-of-fit. Considering the model’s simplicity and the relatively small dataset (< 500), we defined acceptable cutoffs as CFI > 0.90, RMSEA < 0.10, and SRMR < 0.10 (Weston and Gore, 2006).
To investigate the reliability of SAPAS-J, we calculated Cronbach’s alpha αCronbach, McDonald’s omega ωMcDonald, and interclass correlation (ICC) between the test and retest scores. To validate SAPAS-J, we investigated correlations between the SAPAS-J score and the subscale and total score of PDQ-R and DAMS. p values of correlations were adjusted with Holm’s method.
We collected answers from 2,004 people (1,000 men), and their average age was 49.3 years (SD = 17.0). We calculated correlations between SAPAS-J scores and tendencies toward symptoms of depression, general anxiety, social anxiety, and obsessive compulsiveness. These symptoms frequently co-occur with personality disorder, and we hypothesized that they also correlate with the SAPAS-J score. p values of correlations were adjusted using Holm’s method.
The CES-D is a 20-item scale assessing the depressive symptom level in the general population (Radloff, 1977). Its adequate reliability and validity were maintained in the Japanese version (Shima et al., 1985). A meta-analysis reported the comorbid rate of depressive disorder in PD as 44% (Friborg et al., 2014).
The STAI-Y is a widely used tool for distinguishing and assessing state and trait anxiety (Spielberger, 1983). The reliability of the Japanese version was investigated (Iwata et al., 1998). From this questionnaire, we only used the second part (STAI-Y2) to measure trait anxiety.
The original LSAS (Liebowitz, 1987) is a 24-item clinical rating scale for social anxiety disorder (SAD) that has good reliability and validity (Heimberg et al., 1999). As its reliability and validity were also demonstrated in a self-rating Japanese version (Asakura et al., 2002), we used the self-rating LSAS. A meta-analysis summarizing comorbidities of anxiety disorders reported that 48% of patients with social anxiety disorder exhibit some cluster of PD (Friborg et al., 2013).
The OCI is a 42-item assessment tool for the diagnosis and severity assessment of obsessive-compulsive disorder (OCD) with satisfactory reliability and validity (Foa et al., 1998). Its Japanese version also reported satisfactory reliability and validity among both undergraduate students and clinical participants (Ishikawa et al., 2014). A study reported that 52% of patients with OCD had comorbid PD (Friborg et al., 2013).
Descriptive values and results of the Shapiro–Wilk test are provided in Table 1. The average score of SAPAS in Study 1 was 20.47 (SD = 4.03). There were no ceiling or floor effects. While the result of the Shapiro–Wilk test of SAPAS was not significant (W = 0.99, p = 0.274), other scores yielded a significant result (PDQ-R Cluster-A: W = 0.96; PDQ-R Cluster-B: W = 0.96; PDQ-R Cluster-C: W = 0.97; PDQ-R Total: W = 0.97; DAMS Depressive: W = 0.96; DAMS Anxious: W = 0.93; DAMS Positive: W = 0.96.). To investigate structural validity, we performed the CFA, assuming one-factor and higher-order structures (Figures 1, 2 and Tables 2, 3). Goodness-of-fit scores are reported in Table 4. The CFI of the first-order model was 0.80, RMSEA was 0.10, and SRMR was 0.08. The CFI of the higher-order model was 0.94. RMSEA was 0.06, and SRMR was 0.06.
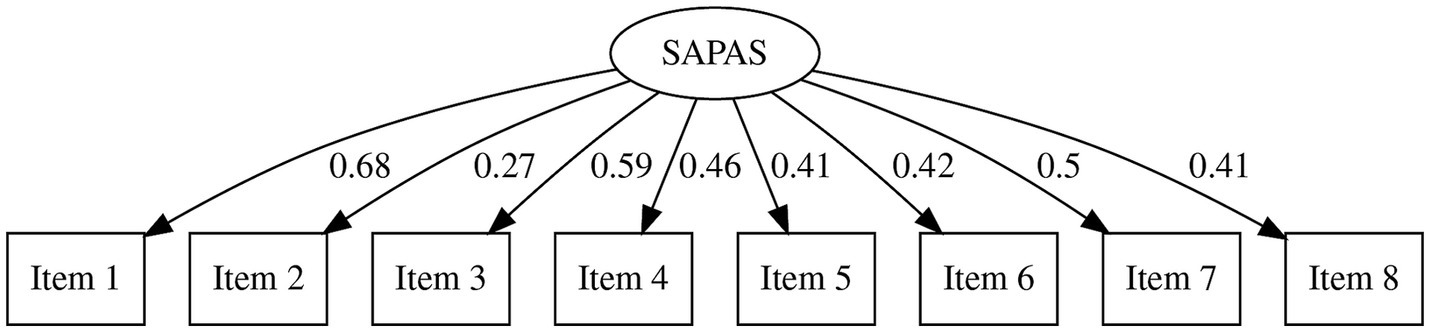
Figure 1. Results of confirmatory factor analysis (first-order model) SAPAS, the Japanese version of Standardised Assessment of Personality - Abbreviated Scale.
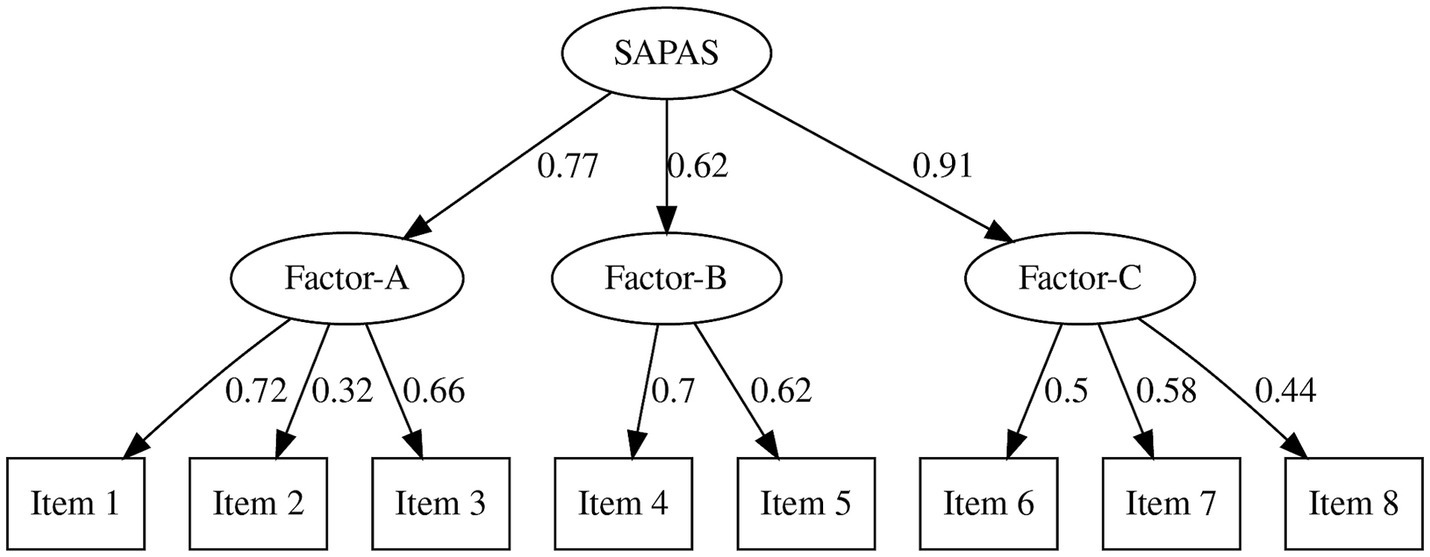
Figure 2. Results of confirmatory factor analysis (higher-order model) SAPAS, the Japanese version of Standardised Assessment of Personality - Abbreviated Scale.
As indices of internal consistency, we reported αCronbach and ωMcDonald (Table 5) to indicate reliability. The overall αCronbach was 0.69 and ωMcDonald was 0.70. We checked test–retest reliability using recollected answers, and the result was reliable (ICC = 0.85, F = 12.63, p < 0.001).
In order to establish the convergent validity, we calculated Spearman’s correlations (Table 6) since the Shapiro–Wilk test indicated that scores were not normally distributed. All correlations were significant and moderate (PDQ-R Cluster-A: ρ = 0.60; PDQ-R Cluster-B: ρ = 0.69; PDQ-R Cluster-C: ρ = 0.58; PDQ-R Total: ρ = 0.73; DAMS Depressive: ρ = 0.60; DAMS Anxious: ρ = 0.46; DAMS Positive: ρ = −0.40.)
Descriptive values are provided in Table 7. The average score of SAPAS in Study 2 was 19.22 (SD = 3.84). There were no ceiling or floor effects. To support the convergent validity, we calculated correlations with SAPAS, and the results are shown in Table 8. Since scores were not normally distributed (Figure 3), we calculated Spearman’s ρ. All correlations were significant and moderate (CES-D: ρ = 0.50; STAI-Y2: ρ = 0.58; LSAS: ρ = 0.40; OCI: ρ = 0.40.)
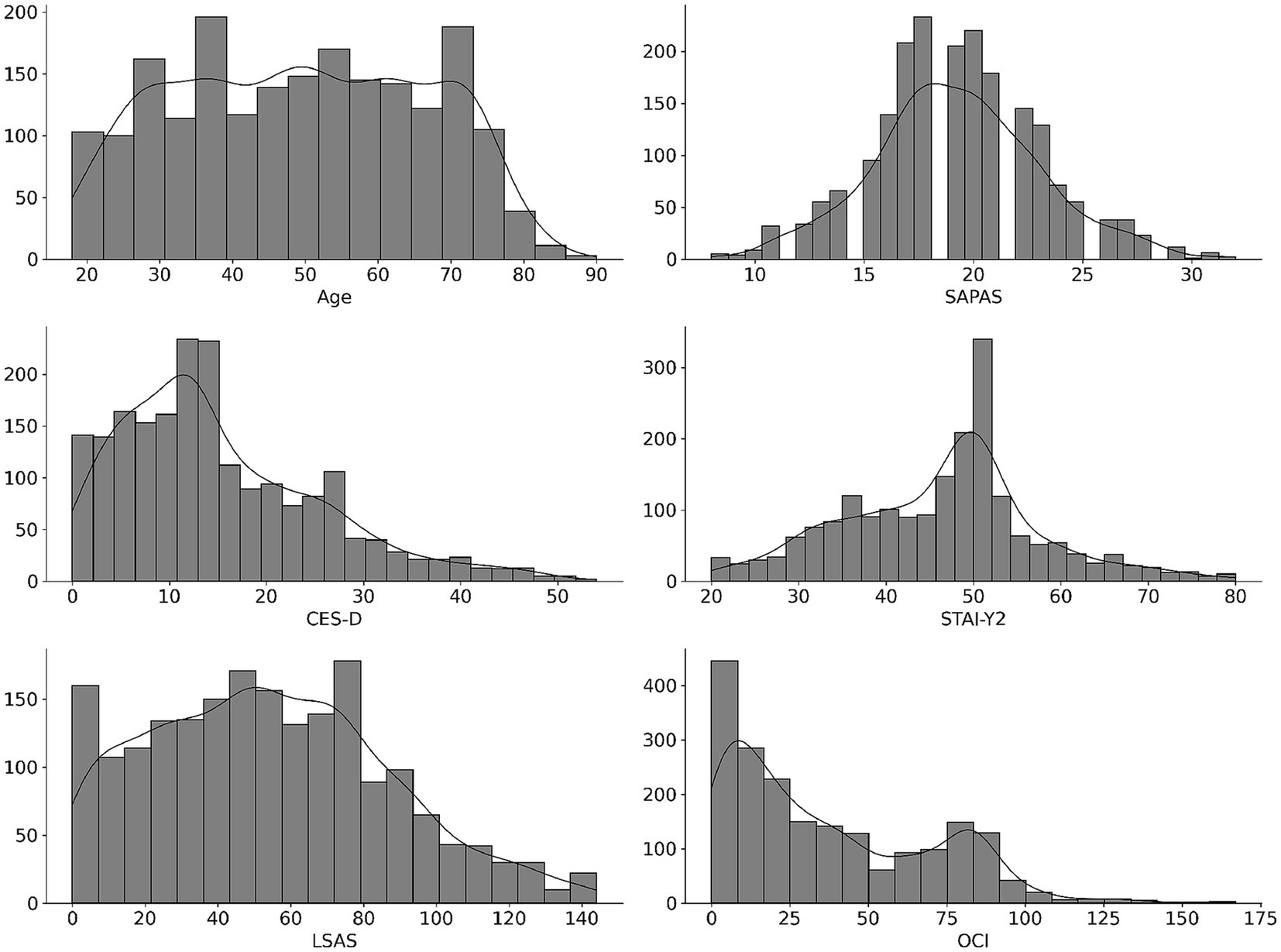
Figure 3. Distributions of scores in Study 2.SAPAS, the Japanese version of Standardised Assessment of Personality - Abbreviated Scale CES-D, Center for Epidemiologic Studies Depression Scale STAI-Y2, State–Trait Anxiety Inventory Form-Y2LSAS, Leibowitz Social Anxiety Scale OCI, Obsessive-Compulsive Inventory.
In Study 1, we confirmed the factorial structure, reliability, and validity of SAPAS-J. We tested two factorial models. One was a single-factor model based on the assumption that SAPAS-J simply measures the transdiagnostic general PD traits. The other was a higher-order model reflecting the three-factor structure of SAPAS-J, corresponding to clusters described in DSM-5. This second model measures general PD traits as a common higher-order latent variable including them. Considering that SAPAS was developed based on the cluster model of DSM, we expected that this model would better explain SAPAS structure. While the single-factor model indicated acceptable SRMR and not quite sufficient CFI and RMSEA, all indices in the high-order model were good or acceptable. Hence, we consider the SAPAS-J to be a higher-order, single-factor scale containing three factors. Although this result did not suggest an alternative use of SAPAS-J, it supposes that SAPAS is a scale measuring the common feature of three clusters of PD, and helps future discussions about results using this questionnaire.
Although its internal consistency was not high, it was equal to or better than that of the original version (αCronbach = 0.68; Moran et al., 2003). The original SAPAS intended to capture the broad character of personality disorder with the fewest possible items. The low correlations between items were reasonable. Because the test–retest reliability of SAPAS-J was very good, overall, the reliability of SAPAS-J was demonstrated.
With our two studies, we demonstrated its validity. We showed sufficiently strong correlations between PDQ-R and SAPAS-J. Almost half of the information of PDQ-R, the 121-item questionnaire, was explained by this 8-item questionnaire, confirming the effectiveness of SAPAS-J. SAPAS-J also indicated adequate correlations between depressive, anxious, and positive moods among undergraduates. Furthermore, by expanding the survey to the general population, we demonstrated correlations with more pathological symptoms than depressive and anxious moods in the preceding days. Moderate correlation with depressive symptoms, trait anxiety, and scales relating to two anxiety disorders, i.e., OCD and SAD, in people with a broad range of ages and characteristics was indicated. Though disorders tend to occur depending on the category (i.e., schizotypal, borderline, etc.) of PD, the validity of SAPAS-J as a screening tool for general PD traits is supported.
SAPAS-J demonstrated sufficient reliability, and the results support its convergent and structural validity. Considering that it is a translation of a widely used screening tool, its content validity is guaranteed. However, the current validation had some limitations. First, our samples were collected only from a non-clinical population, and further validation with clinical samples is needed. Nevertheless, we demonstrated that its reliability and factorial structure correspond to DSM-5 clusters in a non-clinical population. The present research supports proceeding to validate SAPAS-J with clinical samples. Future studies should validate SAPAS-J, with the Structured Clinical Interview for DSM (SCID; First et al., 2015) as a candidate reference standard, as the original (Moran et al., 2003) and other language versions (Germans et al., 2008; Merlhiot et al., 2014) used it. We used PDQ-R to validate SAPAS, as it produces adequate variance in scores among the general population (Trull et al., 1993). However, semi-structured interviews such as SCID or the International Personality Disorder Examination (Loranger, 1994) are required to demonstrate concurrent validity, since the false-positive rate of PDQ-R tends to be high (Hyler et al., 1992).
While validation for the clinical use of SAPAS-J is limited, sufficient validity was demonstrated for its use in the context of psychopathological analog research. As a recent trend in research and clinical understanding, the model of PD is shifting from the conventional categorical/cluster model to a dimensional model (American Psychiatric Association, 2013a). Since PD is understood as a continuum, the severity of which distributes dimensionally (Bagge and Trull, 2003; Brud and Cieciuch, 2022), the analog study, recruiting members of the general population and attempting to reveal psychopathological mechanisms of PD, is meaningful (Carr and Francis, 2010). While SAPAS was developed based on the cluster model, and we found that its structure includes three factors, we think it is compatible with the dimensional model. The three factors in SAPAS converged on the higher-order single factor, and this is considered to be the common feature of PD. Although further research is necessary to validate this hypothesis, we postulate that the common factor identified in our study is likely to be preserved even in the dimensional model. Therefore, we argue that SAPAS can be effectively utilized in future research adopting the dimensional approach to PDs. It would also be beneficial to clarify the relationship between elements of PD dimensions and SAPAS score. Correlation between SAPAS and some questionnaires measuring personality functioning, e.g., DSM-5 Levels of Personality Functioning Questionnaire; Huprich et al. (2018), and pathological personality traits, e.g., Personality Inventory for DSM-5; Krueger et al. (2012), would better clarify the concept that SAPAS assesses. Furthermore, considering that some previous research reported evidence suggesting substantial variation in psychopathology when the same mental disorder co-occurs with a personality disorder (Richman and Unoka, 2015; Chechko et al., 2016), assessing PD traits can also be worthwhile in analog studies seeking to investigate the pathology of psychological disorders other than PD. SAPAS-J requires so little time that researchers can assess PD traits with little burden on participants. Moreover, it can handle the heterogeneity raised by the comorbidity of PD in various mental disorder analog studies. Although there are other self-reporting questionnaires for PD traits besides SAPAS-J, its brevity is a significant advantage.
The datasets presented in this article are not readily available for the following reasons: The data from Study 1 cannot be shared publicly as consent for its dissemination was not obtained from the participants. The data used in Study 2 is subject to ongoing research; however, it is planned to be shared after the research concludes. Requests to access the datasets should be directed to the corresponding author.
The studies involving humans were approved by ATR Review Board Ethics Committee, Ethics Review Committee on Research with Human Subjects at the Waseda University. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because the participants were instructed that their participation in the study would be considered as consenting to respond to the survey, and the study was conducted accordingly.
IK: Conceptualization, Formal analysis, Methodology, Writing – original draft, Funding acquisition. TH: Conceptualization, Data curation, Formal analysis, Investigation, Writing – review & editing, Methodology. MN: Investigation, Writing – review & editing, Data curation. AY: Investigation, Writing – review & editing, Data curation. MH: Investigation, Writing – review & editing, Funding acquisition, Data curation. HK: Methodology, Project administration, Supervision, Writing – review & editing, Conceptualization. ST: Funding acquisition, Project administration, Supervision, Writing – review & editing, Investigation.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by JST Moonshot R&D (Grant Number JPMJMS2291).
The authors are grateful to Paul Moran, Population Health Sciences, University of Bristol, who supported our study and gave us constructive comments and suggestions. Additionally, we thank Steven D. Aird (www.sda-technical-editor.org) for English language editing.
IK, TH, and ST were employed by Advanced Telecommunications Research Institute International (ATR). MN, AY, and MH were employed by KDDI Research, Inc.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1339902/full#supplementary-material
American Psychiatric Association (2013a). “Alternative DSM-5 model for personality disorders” in Diagnostic and statistical manual of mental disorders (Washington DC: American Psychiatric Association Publishing), 761–781.
American Psychiatric Association (2013b). “Personality disorders” in Diagnostic and statistical manual of mental disorders (Washington DC: American Psychiatric Association Publishing), 645–684.
Asakura, S., Inoue, S., Sasaki, T., Sasaki, Y., Kitagawa, N., Inoue, T., et al. (2002). Investigation of the reliability and validity of the Japanese version of Liebowitz social anxiety scale (LSAS). Jpn. J. Psychiatry 44, 1077–1084. doi: 10.11477/mf.1405902721
Bagge, C. L., and Trull, T. J. (2003). DAPP-BQ: factor structure and relations to personality disorder symptoms in a non-clinical sample. J. Personal. Disord. 17, 19–32. doi: 10.1521/pedi.17.1.19.24055
Ball, L., Tully, R. J., and Egan, V. (2017). The SAPAS, personality traits, and personality disorder. J. Personal. Disord. 31, 385–398. doi: 10.1521/pedi_2016_30_259
Brud, P., and Cieciuch, J. (2022). Polish adaptation of self-report instruments for studying borderline personality traits – FFBI and FFBI-SF. Psychiatr. Pol. 1–16, 1–16. doi: 10.12740/pp/onlinefirst/150420
Carlier, I. V. E., Colijn, S., van Rood, Y. R., Streevelaar, M. F., van Vliet, I. M., and van Veen, T. (2014). A comparative analysis of personality pathology profiles among patients with pure depressive-, pure anxiety-, and pure somatoform disorders. J. Affect. Disord. 168, 322–330. doi: 10.1016/j.jad.2014.07.012
Carr, S. N., and Francis, A. J. P. (2010). Early maladaptive schemas and personality disorder symptoms: an examination in a non-clinical sample. Psychol. Psychother. Theory Res. Pract. 83, 333–349. doi: 10.1348/147608309x481351
Chechko, N., Kellermann, T., Augustin, M., Zvyagintsev, M., Schneider, F., and Habel, U. (2016). Disorder-specific characteristics of borderline personality disorder with co-occurring depression and its comparison with major depression: an fMRI study with emotional interference task. NeuroImage Clin. 12, 517–525. doi: 10.1016/j.nicl.2016.08.015
Delgadillo, J., Ali, S., Fleck, K., Agnew, C., Southgate, A., Parkhouse, L., et al. (2022). Stratified care vs stepped care for depression. JAMA Psychiatry 79, 101–108. doi: 10.1001/jamapsychiatry.2021.3539
Delgadillo, J., Huey, D., Bennett, H., and McMillan, D. (2017). Case complexity as a guide for psychological treatment selection. J. Consult. Clin. Psychol. 85, 835–853. doi: 10.1037/ccp0000231
First, M. B., Williams, J. B. W., Karg, R. S., and Spitzer, R. L. (2015). User’s guide for the SCID-5-PD (structured clinical interview for DSM-5 personality disorder). Arlington, VA: American Psychiatric Association.
Foa, E. B., Kozak, M. J., Salkovskis, P. M., Coles, M. E., and Amir, N. (1998). The validation of a new obsessive–compulsive disorder scale: the obsessive–compulsive inventory. Psychol. Assess. 10, 206–214. doi: 10.1037/1040-3590.10.3.206
Fok, M. L.-Y., Hayes, R. D., Chang, C.-K., Stewart, R., Callard, F. J., and Moran, P. (2012). Life expectancy at birth and all-cause mortality among people with personality disorder. J. Psychosom. Res. 73, 104–107. doi: 10.1016/j.jpsychores.2012.05.001
Fok, M. L.-Y., Seegobin, S., Frissa, S., Hatch, S. L., Hotopf, M., Hayes, R. D., et al. (2015). Validation of the standardised assessment of personality - abbreviated scale in a general population sample. Personal. Ment. Health 9, 250–257. doi: 10.1002/pmh.1307
Friborg, O., Martinsen, E. W., Martinussen, M., Kaiser, S., Øvergård, K. T., and Rosenvinge, J. H. (2014). Comorbidity of personality disorders in mood disorders: a meta-analytic review of 122 studies from 1988 to 2010. J. Affect. Disord. 152-154, 1–11. doi: 10.1016/j.jad.2013.08.023
Friborg, O., Martinussen, M., Kaiser, S., Øvergård, K. T., and Rosenvinge, J. H. (2013). Comorbidity of personality disorders in anxiety disorders: a meta-analysis of 30 years of research. J. Affect. Disord. 145, 143–155. doi: 10.1016/j.jad.2012.07.004
Fukui, I. (1997). The depression and anxiety mood scale (DAMS): scale development and validation. Jpn. J. Behav. Ther. 23, 83–93. doi: 10.24468/jjbt.23.2_83
Germans, S., Heck, G. L. V., Moran, P., and Hodiamont, P. P. G. (2008). The self-report standardized assessment of personality-abbreviated scale: preliminary results of a brief screening test for personality disorders. Personal. Ment. Health 2, 70–76. doi: 10.1002/pmh.34
Goddard, E., Wingrove, J., and Moran, P. (2015). The impact of comorbid personality difficulties on response to IAPT treatment for depression and anxiety. Behav. Res. Ther. 73, 1–7. doi: 10.1016/j.brat.2015.07.006
Gorwood, P., Rouillon, F., Even, C., Falissard, B., Corruble, E., and Moran, P. (2010). Treatment response in major depression: effects of personality dysfunction and prior depression. Br. J. Psychiatry 196, 139–142. doi: 10.1192/bjp.bp.109.067058
Heimberg, R. G., Horner, K. J., Juster, H. R., Safren, S. A., Brown, E. J., Schneier, F. R., et al. (1999). Psychometric properties of the liebowitz social anxiety scale. Psychol. Med. 29, 199–212. doi: 10.1017/s0033291798007879
Huprich, S. K., Nelson, S. M., Meehan, K. B., Siefert, C. J., Haggerty, G., Sexton, J., et al. (2018). Introduction of the DSM-5 levels of personality functioning questionnaire. Personal. Disord. Theory Res. Treat. 9, 553–563. doi: 10.1037/per0000264
Hyler, S. E., Skodol, A. E., Oldham, J. M., Kellman, H. D., and Doidge, N. (1992). Validity of the personality diagnostic questionnaire-revised: a replication in an outpatient sample. Compr. Psychiatry 33, 73–77. doi: 10.1016/0010-440x(92)90001-7
Ishikawa, R., Kobori, O., and Shimizu, E. (2014). Development and validation of the Japanese version of the obsessive-compulsive inventory. BMC. Res. Notes 7:306. doi: 10.1186/1756-0500-7-306
Iwata, N., Mishima, N., Shimizu, T., Mizoue, T., Fukuhara, M., Hidano, T., et al. (1998). The Japanese adaptation of the STAI form Y in Japanese working adults. The presence or absence of anxiety. Ind. Health 36, 8–13. doi: 10.2486/indhealth.36.8
Kavanagh, B. E., Gwini, S. M., Pasco, J. A., Stuart, A. L., Quirk, S. E., Gaston, J., et al. (2021). The added burden of personality disorder on subsidized australian health service utilization among women with mental state disorder. Front. Glob. Women’s Health 2:615057. doi: 10.3389/fgwh.2021.615057
Krueger, R. F., Derringer, J., Markon, K. E., Watson, D., and Skodol, A. E. (2012). Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychol. Med. 42, 1879–1890. doi: 10.1017/s0033291711002674
Laurenssen, E. M. P., Eeren, H. V., Kikkert, M. J., Peen, J., Westra, D., Dekker, J. J. M., et al. (2016). The burden of disease in patients eligible for mentalization-based treatment (MBT): quality of life and costs. Health Qual. Life Outcomes 14:145. doi: 10.1186/s12955-016-0538-z
Liebowitz, M. R. (1987). Social phobia. Mod. Probl. Pharmacopsyhiatry 22, 141–173. doi: 10.1159/000414022
Loranger, A. W. (1994). The international personality disorder examination. Arch. Gen. Psychiatry 51:215. doi: 10.1001/archpsyc.1994.03950030051005
Mars, B., Gibson, J., Dunn, B. D., Gordon, C., Heron, J., Kessler, D., et al. (2021). Personality difficulties and response to community-based psychological treatment for anxiety and depression. J. Affect. Disord. 279, 266–273. doi: 10.1016/j.jad.2020.09.115
Massion, A. O., Dyck, I. R., Shea, M. T., Phillips, K. A., Warshaw, M. G., and Keller, M. B. (2002). Personality disorders and time to remission in generalized anxiety disorder, social phobia, and panic disorder. Arch. Gen. Psychiatry 59, 434–440. doi: 10.1001/archpsyc.59.5.434
Merlhiot, G., Mondillon, L., Vermeulen, N., Basu, A., and Mermillod, M. (2014). Adaptation and validation of the standardized assessment of personality – abbreviated scale as a self-administered screening test (SA-SAPAS). J. Psychol. Psychotherapy 4:6. doi: 10.4172/2161-0487.1000164
Moran, P., Leese, M., Lee, T., Walters, P., Thornicroft, G., and Mann, A. (2003). Standardised assessment of personality – abbreviated scale (SAPAS): preliminary validation of a brief screen for personality disorder. Br. J. Psychiatry 183, 228–232. doi: 10.1192/bjp.183.3.228
Phillips, K. A., Pagano, M. E., Menard, W., Fay, C., and Stout, R. L. (2005). Predictors of remission from body dysmorphic disorder. J. Nerv. Ment. Dis. 193, 564–567. doi: 10.1097/01.nmd.0000172681.51661.54
Radloff, L. S. (1977). The CES-D scale. Appl. Psychol. Meas. 1, 385–401. doi: 10.1177/014662167700100306
Richman, M. J., and Unoka, Z. (2015). Mental state decoding impairment in major depression and borderline personality disorder: Meta-analysis. Br. J. Psychiatry 207, 483–489. doi: 10.1192/bjp.bp.114.152108
Rivera-Garrido, N., Ramos-Sosa, M. P., Accerenzi, M., and Brañas-Garza, P. (2022). Continuous and binary sets of responses differ in the field. Sci. Rep. 12:14376. doi: 10.1038/s41598-022-17907-4
Rosseel, Y. (2012). Lavaan an R package for structural equation modeling. J. Stat. Softw. 48, 1–36. doi: 10.18637/jss.v048.i02
Sen, P., Barnicot, K., Podder, P., Dasgupta, I., and Gormley, M. (2021). Exploring the prevalence of personality disorder and the feasibility of using the SAPAS as a screening tool for personality disorder in an emergency department in India. Med. Sci. Law 62, 8–16. doi: 10.1177/00258024211011387
Shima, S., Shikano, T., Kitamura, T., and Asai, M. (1985). A novel self-rating scale for depression. Jpn. J. Psychiatry 27, 713–723.
Spielberger, C. D. (1983). Manual for the state-trait anxiety inventory: STAI (form Y). Palo Alto, CA: Consulting Psychologists Press.
Takahashi, Y., Yamagata, S., Ritchie, S. J., Barker, E. D., and Ando, J. (2021). Etiological pathways of depressive and anxiety symptoms linked to personality traits: a genetically-informative longitudinal study. J. Affect. Disord. 291, 261–269. doi: 10.1016/j.jad.2021.05.004
Trull, T. J., Goodwin, A. H., Schopp, L. H., Hillenbrand, T. L., and Schuster, T. (1993). Psychometric properties of a cognitive measure of personality disorders. J. Pers. Assess. 61, 536–546. doi: 10.1207/s15327752jpa6103_10
Tyrer, P., Reed, G. M., and Crawford, M. J. (2015). Classification, assessment, prevalence, and effect of personality disorder. Lancet 385, 717–726. doi: 10.1016/s0140-6736(14)61995-4
Uehara, T., Sakado, K., and Sato, T. (1997). Test—retest reliability of the personality diagnostic questionnaire: revised. Psychiatry Clin. Neurosci. 51, 369–372. doi: 10.1111/j.1440-1819.1997.tb02601.x
Vallat, R. (2018). Pingouin: statistics in python. J. Open Source Softw. 3:1026. doi: 10.21105/joss.01026
Weston, R., and Gore, P. A. (2006). A brief guide to structural equation modeling. Couns. Psychol. 34, 719–751. doi: 10.1177/0011000006286345
Winsper, C., Bilgin, A., Thompson, A., Marwaha, S., Chanen, A. M., Singh, S. P., et al. (2020). The prevalence of personality disorders in the community: a global systematic review and meta-analysis. Br. J. Psychiatry 216, 69–78. doi: 10.1192/bjp.2019.166
Keywords: personality disorder, analog study, questionnaire, assessment tool, validity and reliability, standardised assessment of personality abbreviated scale
Citation: Kawashima I, Hinuma T, Nagata M, Yoneyama A, Honjo M, Kumano H and Tanaka SC (2024) Psychometric properties of the Japanese version of the standardised assessment of personality abbreviated scale. Front. Psychol. 14:1339902. doi: 10.3389/fpsyg.2023.1339902
Received: 17 November 2023; Accepted: 26 December 2023;
Published: 06 February 2024.
Edited by:
Kee-Hong Choi, Korea University, Republic of KoreaReviewed by:
Eunsil Cho, Korea University, Republic of KoreaCopyright © 2024 Kawashima, Hinuma, Nagata, Yoneyama, Honjo, Kumano and Tanaka. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Issaku Kawashima, aXNzYWt1c3NAZ21haWwuY29t; Saori C. Tanaka, eHNhb3JpQGF0ci5qcA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.