- 1School of Nursing, Chengdu Medical College, Chengdu, Sichuan, China
- 2Department of Nursing, Suining Central Hospital, Suining, Sichuan, China
- 3Department of Oncology, Chengdu Pidu District People’s Hospital, Chengdu, Sichuan, China
Introduction: In recent years, fear of disease progression (FoP) has become one of the most common psychological problems in cancer patients. However, there are fewer studies on the FoP in patients with gastrointestinal tumors. We aimed to assess the level of FoP in patients with gastrointestinal tumors and analyze the factors related to FoP. We also aimed to examine the relationship among loneliness, hope and FoP in patients with gastrointestinal cancer.
Methods: A cross-sectional survey was conducted on three Grade A hospitals in southwestern China from November 2021 to July 2022. The demographic and clinical characteristics questionnaire, Fear of Disease Progression Scale (FoP-Q-SF), Cancer Loneliness Scale (CLS), and Herth Hope Index (HHI) were included in this study. Data analysis included descriptive statistics, independent samples t-tests, one-way analysis of variance, and multiple linear regression analysis.
Results: In total, 245 gastrointestinal cancer patients participated in this study. The average (standard deviation) FoP score in patients was 32.94 ± 10.64. In total, 245 gastrointestinal cancer patients participated in this study. The average (standard deviation) FoP score in patients was 32.94 ± 10.64. The average score of CLS was 17.65 ± 6.71, and that for the HHI was 31.27 ± 7.73. Pearson correlation analysis showed that FoP was negatively significant correlated with hope level (r = −0.522) and FoP was positively significant correlated with loneliness (r = 0.545). Linear regression analysis showed that educational level, age, living condition, hope, and loneliness were the significant predictors of FoP and explained 53.10% of the variability in FoP (F = 16.372).
Conclusion: Findings highlight the need to strengthen attention to FoP in gastrointestinal cancer patients. Our study showed that gastrointestinal cancer patients who have a high school education, are age 45 to 59, live alone, high level of loneliness, and low level of hope have higher FoP. Medical staff should enhance clinical screening of FoP and consider the formulation of relevant interventions for high-risk groups to reduce loneliness among patients, raise their hope level, and reduce their FoP.
Introduction
According to the 2020 Global Cancer Statistical Report, the number of new cases and deaths owing gastrointestinal neoplasms ranks among the highest worldwide (Sung et al., 2021). Gastrointestinal neoplasms have the characteristics of a short course, rapid development, early metastasis, and generally poor prognosis; thus, these cancers have become a serious global public health problem (Hamashima, 2014). According to different stages of gastrointestinal neoplasms, a series of treatments are available, such as surgery, radiotherapy, and chemotherapy, but all these have adverse effects on patients (Numico et al., 2015). Due to the special physiological characteristics of patients with gastrointestinal tumors, they are more likely to have adverse reactions such as nausea, vomiting, renal insufficiency, and radiation enteritis during cancer treatment (van den Boorn et al., 2020). Moreover, the long-term sequelae associated with cancer treatments can affect the social life of patients with gastrointestinal tumors, resulting in substantial psychosocial pressure and distress (Kim and Yoo, 2021). Research has shown that fear of progression (FoP) is one of the most frequent distress symptoms in people with cancer (Herschbach and Dinkel, 2014).
FoP has been proposed by Dankert et al. (2003), as referring to an individual’s fear of everything related to his or her real-life disease, specifically defined as the various biopsychosocial consequences of the fear of disease progression or the fear of disease recurrence. It is reported that 33 to 96% of cancer patients worldwide have FoP, and the proportion with severe fear reaches 87% (Lebel et al., 2016). FoP has become one of the most common psychological problems in patients with cancer, and FoP is now included in the international definition of fear of cancer recurrence (FCR; Youssef et al., 2021). FCR is fear or apprehension in cancer survivors about the possibility of cancer recurrence, progression, or metastasis at the primary site or elsewhere (Barrows et al., 2020). It is clear that the relevant defining features of the two concepts are comparable and identical in nature Herschbach and Dinkel (2014). In the present paper, we treat FoP and FCR as equivalent from the perspective of tumor psychology.
Many scholars have interpreted the influencing factors of FoP from different perspectives. Some studies have shown that FoP in cancer patients is related to sex or gender (Pang and Humphris, 2021), age (Lim and Humphris, 2020), educational level (Thewes et al., 2018), and marital status (Thewes et al., 2016). In a cross-sectional study, high levels of FoP in Korean survivors of gastric cancer were associated with poor social support, functional decline, fatigue, pain, sleep problems, anxiety, and depression, regardless of sex, type of cancer treatment, duration, or disease stage (Shin et al., 2022). Previous studies have found that colorectal cancer patients with high levels of FoP may face higher levels of psychological distress, post-traumatic stress symptoms, and lower quality of life (Custers et al., 2016). FoP is therefore affected by many factors and can seriously affect the physical and mental health of patients with cancer. Based on this, we aimed to explore multiple perspectives to determine the influence of various factors on FoP in patients with gastrointestinal neoplasms in China.
Loneliness is another important negative emotion that is common in cancer patients. As a common chronic stressor, loneliness accelerates the progression of cancer (Dai et al., 2020). Loneliness refers to the emotional experience of social isolation due to a subjective desire for social interactions that are higher than the actual level of socialization (Ross et al., 2020). Loneliness in cancer patients is related to the specific cancer experience of patients. Studies have shown that patients with cancer have a greater risk of loneliness (Gray et al., 2020). Research on loneliness in cancer patients has been conducted for many years. A 5-year follow-up study confirmed that high levels of loneliness can cause patients great distress (Drageset et al., 2013). Cancer patients with high levels of loneliness also have more severe depressive symptoms, often accompanied by higher mortality. A cross-sectional descriptive correlation study found that adult patients with cancer felt moderate levels of loneliness (Kavalal and Koc, 2021). A population-based national study showed that the average age at diagnosis of digestive tract tumors in China is 55.20 years, and most patients were adults (Xu et al., 2021). Meanwhile, it has been shown that there is an association between loneliness and FoP in breast cancer patients, with patients with high levels of loneliness having a higher risk of psychological problems (Li et al., 2022). Therefore, the relationship between the level of loneliness and FoP in patients with gastrointestinal tumors deserves further exploration. In this study, we investigated the correlation between loneliness and FoP among patients with gastrointestinal tumors in China.
Hope plays a significant role in the field of positive psychology. Hope can help cancer patients better cope with the disease, promote healthy behaviors, and reduce the occurrence of depression (Corn et al., 2020). Previous research demonstrated that maintaining a positive and optimistic mood helps alleviate patients’ fear of disease progression (Otto et al., 2016). Research indicated that even patients with advanced cancer can possess substantial levels of hope, predominantly related to a potential cure and expectations regarding quality of life (Daneault et al., 2016). An observational cross-sectional study showed that when cancer patients have high levels of hope, they have a positive attitude toward treatment and a high degree of subjective cooperation (Ozen et al., 2020). Additionally, a study of long-term survivors of colorectal cancer showed that patients with enterostomy experienced different levels of psycho-emotional conditions, decreased levels of hope, and increased levels of anxiety and depression (Kunitake et al., 2017).
The Herth’s theory of hope holds that the essence of hope is belief, centered on positive goals, which gives patients sustained motivation. As a common psychological state in cancer patients coping with the disease, FoP can also affect levels of hope (Starreveld et al., 2018). Loneliness is thought to be an important psychosocial factor associated with cancer severity (Dai et al., 2020). Therefore, the research questions addressed were: (a) What is the FoP level in patients with gastrointestinal tumors? (b) How does the level of FoP vary according to demographic and disease-related variables? (c) What is the relationship between FoP, loneliness, and hope?
Materials and methods
Study setting and participants
A cross-sectional relational design was used in this study. The study was conducted between November 2021 and July 2022 in the oncology departments of three Grade A hospitals in southwest China. We guaranteed patient confidentiality and the right to withdraw from the study at any time. The STROBE guidelines for cross-sectional studies were adhered to in this study (Supplementary Table S1). Study participants were recruited from the oncology departments of three Grade A hospitals in southwest China using a convenience sampling method. The inclusion criteria were as follows: (a) diagnosed with gastrointestinal tumors in clinicopathological imaging and hospitalized for cancer treatment; (b) aged 18–80 years; and (c) provided informed consent. The exclusion criteria were as follows: (a) other types of cancer; (b) lacking the ability to communicate effectively with others; or (c) current participation in other studies. G*Power Version 3.1 for multiple linear regression was utilized to calculate the sample size (Faul et al., 2007). Based on a medium effect size of 0.15, alpha of 0.05, power of 0.95 and 23 predictors, the sample size was determined 234. The sample of 245 met the criteria of this study.
Ethical consideration
An informed consent was signed and that the study was approved by the hospital’s ethics committee (approval number: 2021CYFYIRB-BA-60-01).
Data collection
Study recruitment information was posted by the research staff at the time of admission. The investigators screened inpatients with digestive system cancer who met the eligibility requirements in person on the hospital ward. Before the formal survey, we fully explained the purpose and content of the study to patients again and then distributed questionnaires. The data collection method was a combination of electronic medical record review and a paper questionnaire survey. Approximately 20 min were required to complete the questionnaire. After completing the questionnaire, the investigators checked the quality of the questionnaire promptly, asked patients about missing or unclear items, and corrected and completed the information to ensure the quality of the questionnaire. We made sure to avoid any inductive language during questioning. Research team members then extracted demographic and disease-related data from patients’ electronic medical records. A total of 250 questionnaires were distributed. Five patients had to stop the survey because of physical discomfort. Ultimately, 245 completed questionnaires were collected.
Measures
Demographic and disease-related characteristics
In the present study, we collected sociodemographic data using 12 items, including sex, age, educational level, marital status, geographic area, living condition (living alone or with family members), the number of escorts, insurance type, occupational status, income (RMB/month), family history of cancer, and religious beliefs. Four items were used to investigate disease-related features, including tumor stage, time of diagnosis (month), disease type, and type of treatment.
Fear of Progression Questionnaire-Short Form
FoP was measured using the Chinese version of the Fear of Progression Questionnaire-Short Form (FoP-Q-SF). This short-form questionnaire was translated into Chinese by Wu et al. (2015). The short-form questionnaire includes a total of 12 items in two dimensions, the physiological dimension (6 items) and social dimension (6 items), based on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree), for a total score ranging from 12 to 60. Higher scores indicate higher levels of FoP. A score of 20–31 indicates mild fear, 32–38 moderate fear, and 39–60 indicates severe fear (Zhang et al., 2022a). The total Cronbach’s α for the Chinese version of the FoP-Q-SF was 0.883. In the current study, the Cronbach’ s α was 0.905 in total for the short-form questionnaire.
Cancer Loneliness Scale
The Chinese version of the Cancer Loneliness Scale (CLS) was translated by Cui and Sun (2020). The scale is used to evaluate loneliness among Chinese patients with gastrointestinal neoplasms. This scale has seven items across a single dimension graded on a 6-point Likert scale (1 = strongly disagree, 6 = strongly agree), for a total score of 7–35. A higher score on the CLS indicates more serious loneliness. The Cronbach’s α coefficient of the Chinese version of CLS was 0.912 (Cui and Sun, 2020). In the current study, the Cronbach’s α was 0.881, indicating good reliability and validity.
Herth Hope Index
Hope was measured using the Chinese version of the Herth Hope Index (HHI) by Zhao and Wang (2000). This instrument includes 12 items in three dimensions: temporality and future, positive readiness and expectancy, and interconnectedness. Each item on the HHI is scored on a scale from 1 to 4, with 1 being “strongly disagree” and 4 being “strongly agree,” for a total score of 12–48. A score of 12–23 indicates a low level of hope, 24–35 a moderate level of hope, and 36–48 indicates a high level of hope. The total Cronbach’s α for the Chinese version of the HHI was 0.85 (Zhao and Wang, 2000). In the current study, the Cronbach’s α for the overall HHI was 0.910.
Data analysis
All analyses were performed using IBM SPSS version 26 (IBM Corp., Armonk, NY, United States). Descriptive statistics are presented as frequencies and scores. The t-test and analysis of variance (ANOVA) were used to test differences in FoP between patients with different demographic and clinical variables. Pearson’s correlation was used to analyze the correlation among three variables: FoP, loneliness, and hope. At the same time, we set up virtual coding (Supplementary Table S2), and all dummy variables were entered into the regression equation using the input method; the other variables were entered into the regression equation using the stepwise method. Multiple linear regression analysis was used to identify important predictors of FoP among patients with gastrointestinal tumors. p < 0.05 was considered statistically significant.
Results
Descriptive analysis
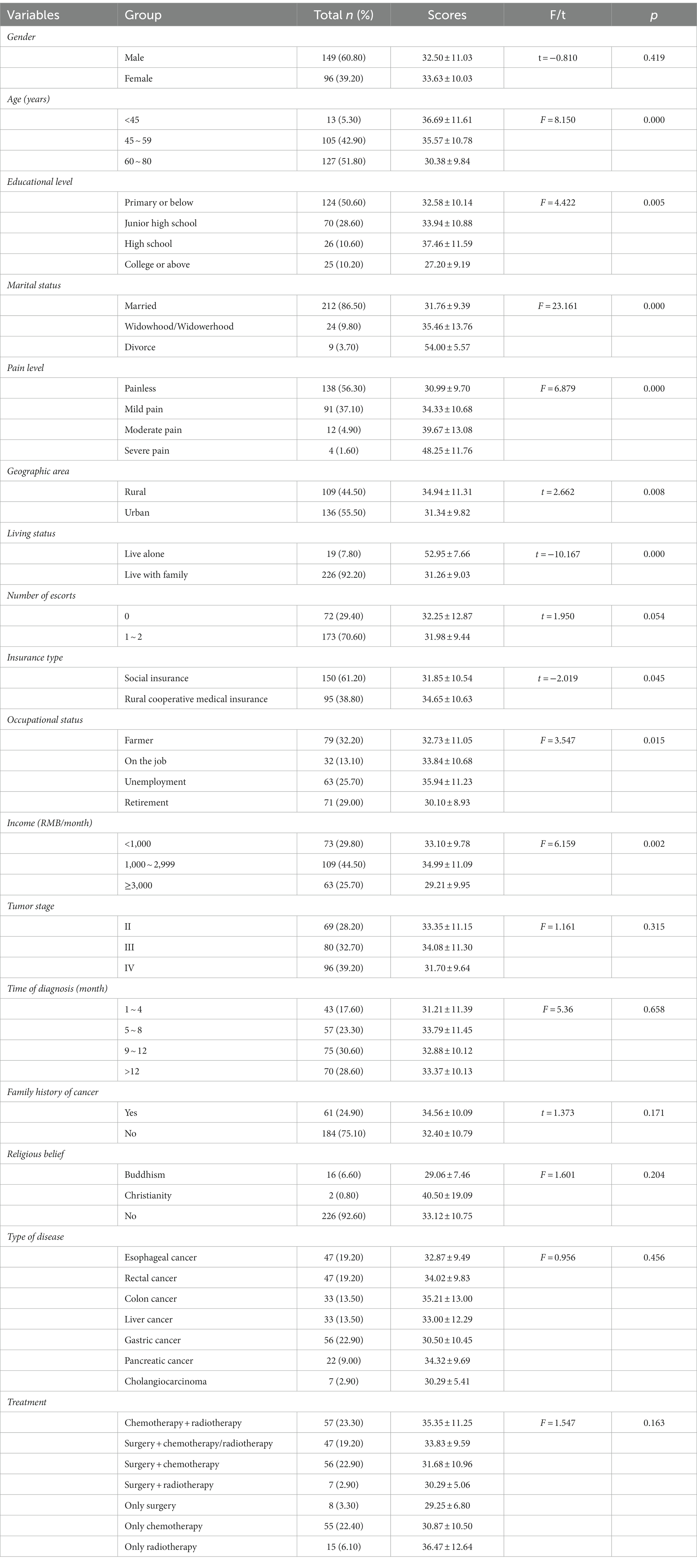
The main characteristics of participants can be seen in Table 1. A total of 245 patients were recruited for this study. Most participants (n = 149, 60.8%) were men. In addition, 127 participants (51.80%) were aged 60–80 years, and 105 (42.90%) were aged 45–59 years. Furthermore, most participants (n = 212, 86.50%) were married; 109 patients (44.50%) lived in a rural area and 136 (55.50%) lived in an urban area. Regarding disease-related characteristics, most patients (n = 75, 30.60%) had been diagnosed between 9 and 12 months earlier. In addition, 39.2% of patients (n = 96) had stage IV tumors, and most patients (n = 57, 22.90%) were treated with concurrent chemoradiotherapy. The most common cancer (n = 80, 32.70%) was colorectal cancer, followed by gastric (n = 56, 22.90%), esophageal (n = 47, 19.20%), and liver cancer (n = 33, 13.50%).
Univariate analysis
FoP varied significantly according to age, education level, marital status, pain score, geographic area, living condition, type of insurance, occupational status, and average monthly income. However, there were no significant differences for FoP among participants by sex, tumor stage, tumor type, and family history of cancer (Table 1).
Correlation analysis
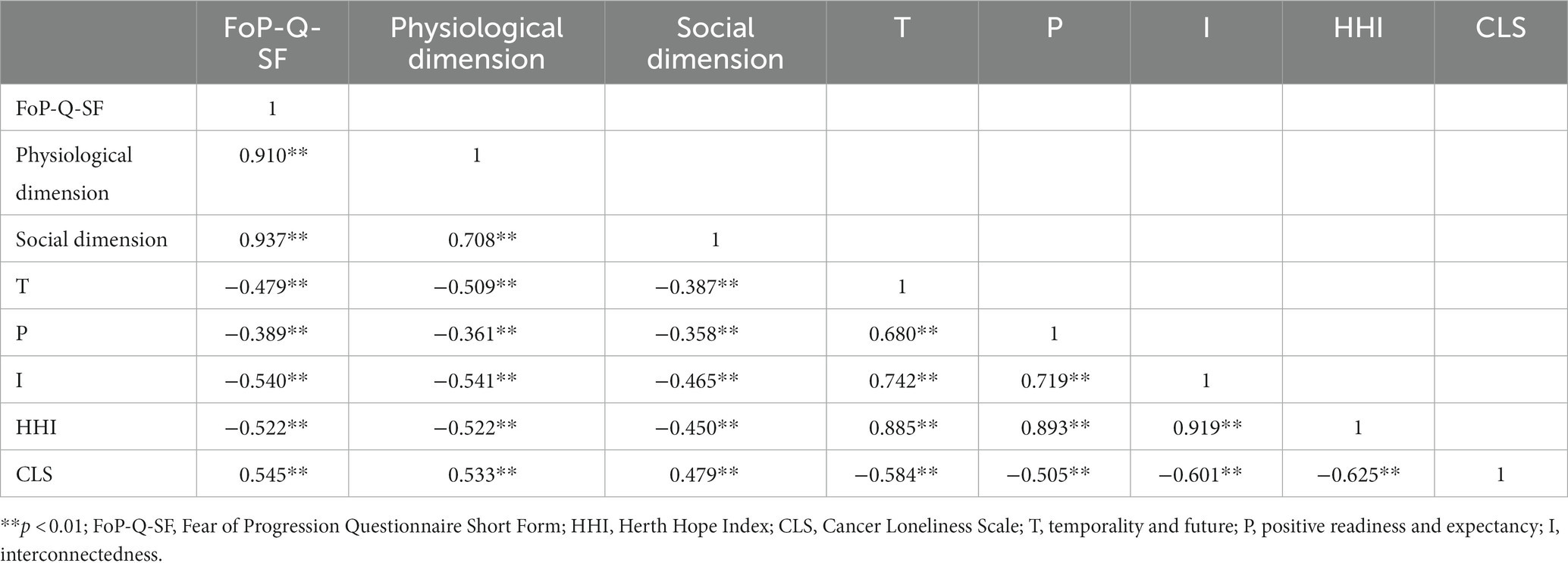
As presented in Table 2, the average score for FoP was 32.94 ± 10.64, which indicated a moderate level of FoP. The average score for the CLS was 17.65 ± 6.71, and HHI showed an average score of 31.27 ± 7.73. Furthermore, Table 3 showed that FoP was negatively significant correlated with the level of hope (r = −0.522, p < 0.01) and positively significant correlated with loneliness (r = 0.545, p < 0.01). Hope was inversely correlated with loneliness (r = −0.625, p < 0.01). This further suggested that the higher the patient’s level of hope, the lower their level of FoP, as well as the higher the level of loneliness, the higher the patient’s degree of FoP.

Table 2. Scores of the Fear of Progression Questionnaire-Short Form, Cancer Loneliness Scale, Herth Hope Index (N = 245).
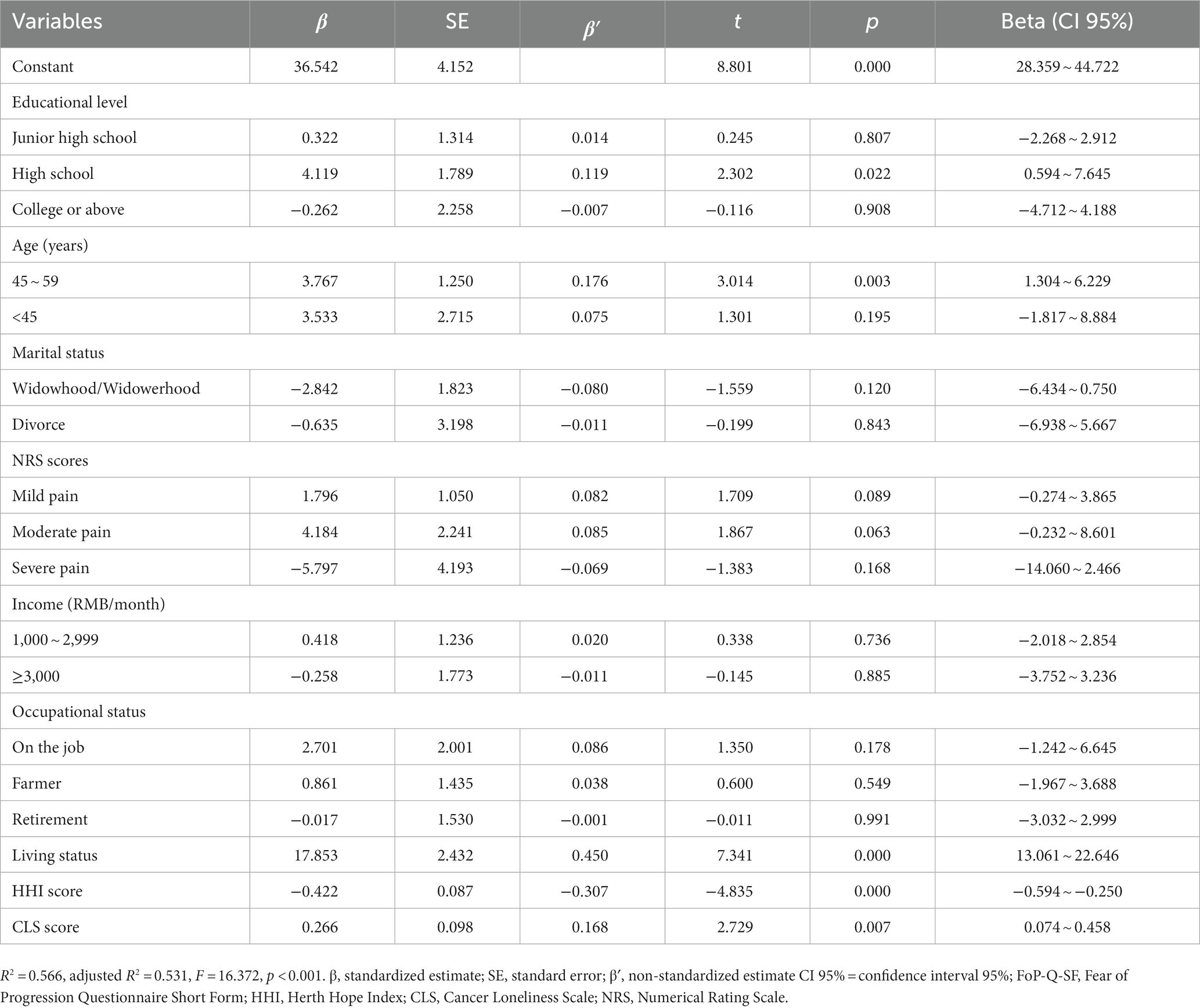
Regression analysis
Based on the ANOVA, t-test, and Pearson correlation analysis results, we entered the significant variables into the regression equation model. As shown in Table 4, education level, age, living status, level of hope, and loneliness were important predictors of FoP in patients with gastrointestinal tumors. Among them, five variables, high school education level, 45–59 years old, living alone, low level of hope, and high level of loneliness, were statistically significant in the regression model, explaining 53.10% of the variance in FoP (F = 16.372).
Discussion
In this study, we measured the levels of FoP in patients with gastrointestinal tumors, analyzed the influencing factors of FOP, and explored the relationship between hope, loneliness, and FoP. The findings confirmed that patients with gastrointestinal tumors had moderate levels of FoP, that hope levels and loneliness were significantly associated with FoP, and that patients’ FoP levels were also influenced by a variety of other factors.
Current status of FoP among gastrointestinal cancer patients
In our study, the average score (standard deviation) for FoP among patients with gastrointestinal tumors was 32.94 ± 10.64. However, it is worth mentioning that a previous study reported 335 patients with mixed cancer diagnosis with a lower FOP score (16.70 ± 0.46) than our study (Sarkar et al., 2015). The reason for this may be that 71.50% of patients had received a cancer diagnosis less than 1 year earlier in our study, and newly diagnosed patients had greater fear and worry about the disease. In addition, patients with gastrointestinal tumors have a high symptom burden, which also increases patients’ FoP. We also found that on the physical dimension, the patients’ greatest fear was that the treatment and medication would damage my body (mean score, 3.65), which was similar to the findings of other studies (Hong et al., 2020). Patients with gastrointestinal tumors mainly rely on surgical treatment, chemotherapy, and radiation therapy. Postoperative complications and the toxic side effects of radiotherapy and chemotherapy can exacerbate patients’ fear of disease treatment and medication. Therefore, although the effects of time to cancer diagnosis and treatment modality on FoP were not statistically significant in the univariate analysis of this study, we should still pay attention to the effects of these clinically relevant variables on FoP in patients with gastrointestinal tumors. Moreover, clinical staff should provide tailored psychosocial care to patients with gastrointestinal cancers, especially close to the time of diagnosis. For example, patients should be educated about disease treatment and preventive measures for the adverse effects of radiotherapy to reduce their fear level and psychological burden.
Influencing factors of FoP for gastrointestinal cancer patients
Family is an important factor influencing FoP in patients with gastrointestinal tumors. We found that in the social dimension, the item with the highest score was worrying about what would happen to the patient’s family (average score, 3.40). In a survey of Chinese patients with lung cancer (Kuang et al., 2022), the highest score was also for worry about the family, with an average score of 3.31, which is similar to our research results. A possible explanation for this phenomenon is that FoP is influenced by the concept of family in the traditional culture of Confucianism in China. Today, there is still a strong family concept in Chinese society, and families are closely linked. There are often two or three generations living together in the same household (Yiu et al., 2021). On the one hand, patients with cancer worry that treatment of the disease will increase the financial burden on family members; on the other hand, patients worry that disease progression or death will bring irreparable psychological trauma to their family members (Kang et al., 2022). Therefore, this item has the highest score. Interestingly, a study of leukemia patients in Germany (Thiele et al., 2020) and another study of cervical cancer patients in Thailand (Hanprasertpong et al., 2017). Also showed that “worrying about my family” was the highest scoring entry on the FoP. This illustrates that in Asian as well as European countries, the family is of great concern to cancer patients, who may be as worried about their family as they are about themselves. As an important ethical standard in traditional Chinese culture, filial piety is considered the most important cultural foundation for regulating intergenerational relationships in Chinese families. Through the process and function of socialization, filial piety is internalized in people’s conscious awareness, guiding and constraining obedience and respect toward parents and elders (Bedford and Yeh, 2019). In addition, in terms of the residential situation, patients who lived alone had higher FoP levels than those who lived with family members. Patients who live alone usually receive less social support from family and friends and have a greater FoP (Zhong et al., 2022). Patients living alone must also bear the physical and psychological pain caused by cancer alone, so they pay greater attention to progression or recurrence of the disease. On the contrary, patients who live with their family members can communicate with family when they encounter problems owing to disease progression, which will help reduce the patient’s psychological pain and pressure and reduce their fear levels (Yeung and Lu, 2022). Therefore, medical staff should encourage patients to communicate with their family and friends to improve loneliness, help patients obtain more sources of social support, and help them deal with negative emotions.
Age is an influencing factor in FoP among patients with gastrointestinal tumors. In this study, the FoP score of patients aged less than 45 years (36.69 ± 11.61), 45–59 years (35.57 ± 10.78), and 60–80 years (30.38 ± 9.84) gradually decreased with age. The FoP scores of young and middle-aged patients in our study were lower than the FoP scores in a survey among adult cancer patients in Germany (Richter et al., 2022). The possible reason for this could be differences in the age group divisions of participants in the different studies. Richter limited the age range of the survey participants to 15–39 years old; in the current study, we considered young cancer patients to be those less than 45 years old. Our study results showed that compared with patients aged 45–59 years, those aged 60–80 years had less FoP. This may be related to coping strategies adopted by patients of different ages (Hernandez et al., 2019). The older the patient and the richer their social experience, the better at regulating their emotions and the more actively and calmly they can face a disease diagnosis, leading to lower FoP scores (Richter et al., 2022). However, the reason for the higher levels of FoP in young and middle-aged patients may be related to earlier incidence of gastrointestinal tumors (Arnold et al., 2020). Alternatively, these results may also be because young and middle-aged patients take on more professional and family responsibilities. After a cancer diagnosis, these responsibilities do not diminish, leading to great psychological pressure as people may lose their job due to cancer treatment, which can increase their financial burden (Maheu et al., 2021). This can ultimately lead to higher FoP levels in this population. Therefore, clinical medical staff should pay greater attention to the economic situation of middle-aged and young patients with gastrointestinal cancer and guide them in easily accessing medical resources. For example, hospitals can work with relevant departments to provide financial assistance (such as reducing prescription drug costs or non-medical daily expenses) and conduct educational lectures (such as improving financial literacy, debt planning, and registering and optimizing health insurance; Smith et al., 2022).
This study also found that compared to patients who had elementary education levels, patients with high school education levels had a higher FoP level in relation to gastrointestinal cancer. This is consistent with the conclusion of a study conducted by Mahendran et al. (2021) and may be because patients with high literacy levels actively seek information about a disease, treatment, and prognosis, thereby increasing their awareness about cancer recurrence and risk factors; this, in turn, can lead to more catastrophic thinking and increase the patient’s level of fear.
The relationship between loneliness and FoP
Loneliness in patients with gastrointestinal tumors is positively significant correlated with FoP, that is, the higher the level of loneliness, the higher the patient’s degree of FoP. This finding aligns with the conclusions of a study conducted among patients diagnosed with head and neck cancer and their caregivers (Maguire et al., 2017). In both the Western and Chinese cultural contexts, lonely patients develop emotional expression disorders when they are unable to freely express their emotions owing to a lack of social contact with others, leading to increased levels of phobia disorders (Barracliffe et al., 2018). The cognitive theory of loneliness states that loneliness can harm an individual’s cognition and behavior (Cacioppo and Hawkley, 2009). Patients with greater degrees of loneliness will focus on the progression and prognosis of their own disease and are prone to having more negative perceptions about the disease, resulting in an increased FoP. In a qualitative study including patients with breast cancer in Türkiye (Şengün İnan and Üstün, 2019) and mixed tumors in Canada (Mutsaers et al., 2016), patients with FoP stated that despite the support of their family, friends, and medical team, it was difficult for others to understand their FoP or FCR, which exacerbated the sense of loneliness. This highlights that in clinical work, attention is needed for not only the patient’s FoP but also their experience of loneliness, and the patient’s family environment and social environment should be evaluated. Medical staff can regularly organize communication between patients as patients with the same cancer experiences can better understand each other’s feelings, and staff can provide patients with a social environment that can promote their expression of emotions and ability to communicate ideas, which will help reduce patients’ loneliness and FoP.
The relationship between hope and FoP
The level of hope in patients with gastrointestinal tumors is inversely correlated with FoP, that is, the higher the patient’s level of hope, the lower their level of FoP. Previous studies have pointed out that the hope level of cancer patients is correlated with their psychological resilience (Ye et al., 2017). In the Chinese cultural context, hope is regarded as an inner force that can energize patients in the face of adversity or difficulties, helping patients to establish positive goals and mobilize resources to actively respond to challenges and difficulties (Wu et al., 2016). A survey of breast cancer patients. Showed that patients with higher levels of hope had a lower burden of symptoms from cancer (Li et al., 2021). In addition, studies have shown that hope is an important factor in patient survival, which is related to patients’ quality of life, survival well-being, and psychological suffering (Manor-Binyamini, 2020; Shen et al., 2020). Hope includes an individual’s positive attitude toward the future, which is related to the patient’s positive attitude toward their disease. A greater level of hope can lead to the patient developing greater strength, confidence, and courage to overcome disease and can reduce the patient’s fear of the disease (Bovero et al., 2021). As a traumatic stressful event, cancer development can cause physical and psychological harm to patients that is difficult to overcome. When patients believe that disease progression is a threat, an increase in negative emotions such as anxiety and depression can weaken their confidence and hope in actively treating the disease (Kim and Kim, 2022; Yang et al., 2022). Therefore, we suggest that health care staff develop targeted interventions based on positive psychology theories to increase patients’ level of hope and reduce patients’ FoP to improve their quality of life and subjective well-being. One study showed that dignity therapy can improve the hope level of cancer patients (Zhang et al., 2022b). Clinical medical staff should evaluate and identify patients with high levels of FoP early and provide psychological counseling referral services for these patients when necessary.
Strengths and limitations
The advantages of this research are as follows: First, by investigating the level of fear of disease in patients with gastrointestinal tumors, exploring its influencing factors, and providing a basis for research related to fear of disease progression. This can draw the attention of clinical medical staff and patients’ families to the fear of disease progression in patients with gastrointestinal tumors, and clinical caregivers can also use FOP as a screening index for patients with gastrointestinal tumors. Second, this study found that patients with high school education level, 45–59 years old, and living alone had higher levels of FOP, which is conducive to the timely detection of the high-risk group of FOP by healthcare personnel and the early adoption of intervention measures for such patients. Third, this study found a relationship between lower levels of hope, higher levels of loneliness, and high levels of fear of disease progression, which provides new ideas for subsequent research. It is suggested that other researchers may also introduce new variables to explore the relationship between them.
Nevertheless, this research has certain limitations that need to be acknowledged: First, the sample size was relatively small, which could compromise the generalizability of the research findings. Other psychological variables that might influence fear of progression have not been investigated. It should also be included that there is great variability in the time since diagnosis (as well as specific types of gastrointestinal cancer) that could affect FoP levels, leading to different periods in the treatment pathway of patients. Future studies should be based on large samples, including specific tumor types. Second, the FoP levels in patients with gastrointestinal tumors may fluctuate, and the influencing factors may also vary. Therefore, longitudinal research is needed to explore the FoP trajectory of patients with gastrointestinal tumors or to gain a deeper understanding of their true experience of fear of disease progression through qualitative research. Lastly, to ensure the quality of the questionnaire, the researchers reviewed returned questionnaires and queried patients regarding missing items; the researchers then filled in the missing items on the questionnaire. This could lead to subjectivity among researchers in some questionnaire responses.
Conclusion
In summary, FoP is common in patients with gastrointestinal tumors. In this study, loneliness in patients with gastrointestinal tumors was found to be positively significant correlated with FoP and hope among patients with gastrointestinal tumors was inversely correlated with FoP. Education level, age, living situation, level of hope, and loneliness were independent predictors of FoP. Medical staff should assess the degree of FoP in patients with digestive tract tumors and provide more health education and social support for these patients. Targeted interventions can be formulated, such as the development of measures such as financial education and dignity therapy, to improve the hope level of patients, enhance their confidence in overcoming disease, and reduce their loneliness and FoP.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
YL: Conceptualization, Data curation, Supervision, Writing – original draft. TX: Methodology, Project administration, Writing – original draft. HL: Funding acquisition, Investigation, Validation, Writing – original draft. HQ: Project administration, Conceptualization, Formal analysis, Writing – review & editing. PR: Project administration, Investigation, Resources, Validation, Visualization, Writing – review & editing. XC: Conceptualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the joint project of Chengdu Medical College and Chengdu Pidu District People’s Hospital (grant number 2021LHHL-05); the project of Applied Psychology Research Center of Sichuan Province (grant number CSXL-22211).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1279561/full#supplementary-material
References
Arnold, M., Abnet, C. C., Neale, R. E., Vignat, J., GiovannucciI, E. L., Mcglynn, K. A., et al. (2020). Global burden of 5 major types of gastrointestinal cancer. Gastroenterology 159, 335–349.e15. doi: 10.1053/j.gastro.2020.02.068
Barracliffe, L., Yang, Y., Cameron, J., Bedi, C., and Humphris, G. (2018). Does emotional talk vary with fears of cancer recurrence trajectory? A content analysis of interactions between women with breast cancer and their therapeutic radiographers. J. Psychosom. Res. 106, 41–48. doi: 10.1016/j.jpsychores.2018.01.004
Barrows, C. E., Belle, J. M., Fleishman, A., Lubitz, C. C., and James, B. C. (2020). Financial burden of thyroid cancer in the United States: an estimate of economic and psychological hardship among thyroid cancer survivors. Surgery 167, 378–384. doi: 10.1016/j.surg.2019.09.010
Bedford, O., and Yeh, K. H. (2019). The history and the future of the psychology of filial piety: chinese norms to contextualized personality construct. Front. Psychol. 10:100. doi: 10.3389/fpsyg.2019.00100
Bovero, A., Opezzo, M., Botto, R., Gottardo, F., and Torta, R. (2021). Hope in end-of-life cancer patients: a cross-sectional analysis. Palliat. Support Care. 19, 563–569. doi: 10.1017/S1478951520001388
Cacioppo, J. T., and Hawkley, L. C. (2009). Perceived social isolation and cognition. Trends Cogn. Sci. 13, 447–454. doi: 10.1016/j.tics.2009.06.005
Corn, B. W., Feldman, D. B., and Wexler, I. (2020). The science of hope. Lancet Oncol. 21, e452–e459. doi: 10.1016/S1470-2045(20)30210-2
Cui, H., and Sun, Z. (2020). Chinese version of cancer loneliness scale and cancer-related negative social expectations scale and its reliability and validity test. Chin. Nurs. Res. 34, 2676–2679. doi: 10.12102/j.issn.1009-6493.2020.15.011
Custers, J. A. E., Gielissen, M. F. M., JanssenA, S. H. V., de Wilt, J. H. W., and Prins, J. B. (2016). Fear of cancer recurrence in colorectal cancer survivors. Support Care Cancer 24, 555–562. doi: 10.1007/s00520-015-2808-4
Dai, S., Mo, Y., Wang, Y., Xiang, B., Liao, Q., Zhou, M., et al. (2020). Chronic stress promotes cancer development. Front. Oncol. 10:1492. doi: 10.3389/fonc.2020.01492
Daneault, S., Lussier, V., Mongeau, S., Yelle, L., Cote, A., Sicotte, C., et al. (2016). Ultimate journey of the terminally ill: ways and pathways of hope. Can. Fam. Physician 62, 648–656.
Dankert, A., Duran, G., Engst-Hastreiter, U., Keller, M., Waadt, S., Henrich, G., et al. (2003). Fear of progression in patients with cancer, diabetes mellitus and chronic arthritis. Rehabilitation (Stuttg) 42, 155–163. doi: 10.1055/s-2003-40094
Drageset, J., Eide, G. E., Kirkevold, M., and Ranhoff, A. H. (2013). Emotional loneliness is associated with mortality among mentally intact nursing home residents with and without cancer: a five-year follow-up study. J. Clin. Nurs. 22, 106–114. doi: 10.1111/j.1365-2702.2012.04209.x
Faul, F., Erdfelder, E., Lang, A. G., and Buchner, A. (2007). G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39, 175–191. doi: 10.3758/bf03193146
Gray, T. F., Azizoddin, D. R., and Nersesian, P. V. (2020). Loneliness among cancer caregivers: a narrative review. Palliat. Support Care. 18, 359–367. doi: 10.1017/S1478951519000804
Hamashima, C. (2014). Current issues and future perspectives of gastric cancer screening. World J. Gastroenterol. 20, 13767–13774. doi: 10.3748/wjg.v20.i38.13767
Hanprasertpong, J., Geater, A., Jiamset, I., Padungkul, L., Hirunkajonpan, P., and Songhong, N. (2017). Fear of cancer recurrence and its predictors among cervical cancer survivors. J. Gynecol. Oncol. 28:e27. doi: 10.3802/jgo.2017.28.e72
Hernandez, R., Calderon, C., Carmona, B. A., Rodriguez, C. A., Jara, C., Padilla, Á. A., et al. (2019). Differences in coping strategies among young adults and the elderly with cancer. Psychogeriatrics 19, 426–434. doi: 10.1111/psyg.12420
Herschbach, P., and Dinkel, A. (2014). Fear of progression. Recent Results Cancer Res. 197, 11–29. doi: 10.1007/978-3-642-40187-9_2
Hong, S. J., Shin, N., and Jung, S. (2020). A predictive model of fear of cancer recurrence for patients undergoing chemotherapy. Support Care Cancer 28, 4173–4181. doi: 10.1007/s00520-019-05245-7
Kang, D., Bae, K. R., Lim, J., Kim, N., Shim, S., Kweon, S. S., et al. (2022). Impact of objective financial burden and subjective financial distress on spiritual well-being and quality of life among working-age cancer survivors. Support Care Cancer 30, 4917–4926. doi: 10.1007/s00520-022-06906-w
Kavalal, E. T., and Koc, Z. (2021). Loneliness, death perception, and spiritual well-being in adult oncology patients. Cancer Nurs. 44, E503–E512. doi: 10.1097/NCC.0000000000000930
Kim, S. Y., and Kim, S. (2022). Do COVID-19-related treatment changes influence fear of cancer recurrence, anxiety, and depression in breast cancer patients. Cancer Nurs. 45, E628–E638. doi: 10.1097/NCC.0000000000000937
Kim, H., and Yoo, Y. (2021). Factors influencing supportive care needs of colorectal cancer survivors. Asian Nurs Res (Korean Soc Nurs Sci). 15, 60–66. doi: 10.1016/j.anr.2020.11.003
Kuang, X., Long, F., Chen, H., Huang, Y., He, L., Chen, L., et al. (2022). Correlation research between fear of disease progression and quality of life in patients with lung cancer. Ann Palliat Med. 11, 35–44. doi: 10.21037/apm-21-2821
Kunitake, H., Russell, M. M., Zheng, P., Yothers, G., Land, S. R., Petersen, L., et al. (2017). Quality of life and symptoms in long-term survivors of colorectal cancer: results from NSABP protocol LTS-01. J. Cancer Surviv. 11, 111–118. doi: 10.1007/s11764-016-0567-y
Lebel, S., Ozakinci, G., Humphris, G., Mutsaers, B., Thewes, B., Prins, J., et al. (2016). From normal response to clinical problem: definition and clinical features of fear of cancer recurrence. Support Care Cancer 24, 3265–3268. doi: 10.1007/s00520-016-3272-5
Li, Y., Ni, N., Zhou, Z., Dong, J., Fu, Y., Li, J., et al. (2021). Hope and symptom burden of women with breast cancer undergoing chemotherapy: a cross sectional study. J. Clin. Nurs. 30, 2293–2300. doi: 10.1111/jocn.15759
Li, J., Zhu, S., and Gao, W. (2022). The psychological impact of COVID-19 among newly diagnosed patients with breast cancer when cancer care was returning to normal. Eur J Cancer Care (Engl). 31:e13762. doi: 10.1111/ecc.13762
Lim, E., and Humphris, G. (2020). The relationship between fears of cancer recurrence and patient age: a systematic review and meta-analysis. Cancer Rep (Hoboken). 3:e1235. doi: 10.1002/cnr2.1235
Maguire, R., Hanly, P., Balfe, M., Timmons, A., Hyland, P., O’Sullivan, E., et al. (2017). Worry in head and neck cancer caregivers: the role of survivor factors, care-related stressors, and loneliness in predicting fear of recurrence. Nurs. Res. 66, 295–303. doi: 10.1097/NNR.0000000000000223
Mahendran, R., Liu, J. L., Kuparasundram, S., Simard, S., Chan, Y. H., Kua, E. H., et al. (2021). Fear of cancer recurrence among cancer survivors in Singapore. Singap. Med. J. 62, 305–310. doi: 10.11622/smedj.2020007
Maheu, C., Singh, M., Tock, W. L., Eyrenci, A., Galica, J., Hebert, M., et al. (2021). Fear of cancer recurrence, health anxiety, worry, and uncertainty: a scoping review about their conceptualization and measurement within breast cancer survivorship research. Front. Psychol. 12:644932. doi: 10.3389/fpsyg.2021.644932
Manor-Binyamini, I. (2020). Internalized stigma among bedouin and jews with mental illness: comparing self-esteem, hope, and quality of life. Psychiatry Q. 91, 1381–1393. doi: 10.1007/s11126-020-09758-x
Mutsaers, B., Jones, G., Rutkowski, N., Tomei, C., Seguin, L. C., Petriconr, W. D., et al. (2016). When fear of cancer recurrence becomes a clinical issue: a qualitative analysis of features associated with clinical fear of cancer recurrence. Support Care Cancer 24, 4207–4218. doi: 10.1007/s00520-016-3248-5
Numico, G., Longo, V., Courthod, G., and Silvestris, N. (2015). Cancer survivorship: long-term side-effects of anticancer treatments of gastrointestinal cance. Curr. Opin. Oncol. 27, 351–357. doi: 10.1097/CCO.0000000000000203
Otto, A. K., Szczesny, E. C., Soriano, E. C., Laurencrau, J., and Siegel, S. D. (2016). Effects of a randomized gratitude intervention on death-related fear of recurrence in breast cancer survivors. Health Psychol. 35, 1320–1328. doi: 10.1037/hea0000400
Ozen, B., Ceyhan, O., and Buyukcelik, A. (2020). Hope and perspective on death in patients with cancer. Death Stud. 44, 412–418. doi: 10.1080/07481187.2019.1626942
Pang, C., and Humphris, G. (2021). The relationship between fears of cancer recurrence and patient gender: a systematic review and meta-analysis. Front. Psychol. 12:640866. doi: 10.3389/fpsyg.2021.640866
Richter, D., Clever, K., Mehnert, T. A., and Schonfelder, A. (2022). Fear of recurrence in young adult cancer patients—a network analysis. Cancers (Basel). 14:2092. doi: 10.3390/cancers14092092
Ross, A., Perez, A., Wehrlen, L., Lee, L. J., Yang, L., Cox, R., et al. (2020). Factors influencing loneliness in cancer caregivers: a longitudinal study. Psycho-Oncology 29, 1794–1801. doi: 10.1002/pon.5477
Sarkar, S., Sautier, L., Schilling, G., Bokemeyer, C., Koch, U., and Mehnert, A. (2015). Anxiety and fear of cancer recurrence and its association with supportive care needs and health-care service utilization in cancer patients. J. Cancer Surviv. 9, 567–575. doi: 10.1007/s11764-015-0434-2
Şengün İnan, F., and Üstün, B. (2019). Fear of recurrence in Turkish breast cancer survivors: a qualitative study. J. Transcult. Nurs. 30, 146–153. doi: 10.1177/1043659618771142
Shen, A., Qiang, W., Wang, Y., and Chen, Y. (2020). Quality of life among breast cancer survivors with triple negative breast cancer--role of hope, self-efficacy and social support. Eur. J. Oncol. Nurs. 46:101771. doi: 10.1016/j.ejon.2020.101771
Shin, J., Shin, D. W., Lee, J., Hwang, J., Lee, J. E., Cho, B., et al. (2022). Exploring socio-demographic, physical, psychological, and quality of life-related factors related with fear of cancer recurrence in stomach cancer survivors: a cross-sectional study. BMC Cancer 22:414. doi: 10.1186/s12885-022-09507-2
Smith, G. L., Banegas, M. P., Acquati, C., Chang, S., Chino, F., Conti, R. M., et al. (2022). Navigating financial toxicity in patients with cancer: a multidisciplinary management approach. CA Cancer J. Clin. 72, 437–453. doi: 10.3322/caac.21730
Starreveld, D. E. J., Markovitz, S. E., Breukelen, G., and Peters, M. L. (2018). The course of fear of cancer recurrence: different patterns by age in breast cancer survivors. Psychooncology 27, 295–301. doi: 10.1002/pon.4505
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., et al. (2021). Global cancer statistics 2020: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. doi: 10.3322/caac.21660
Thewes, B., Kaal, S. E. J., Custers, J. A. E., Manten, H. E., Jansen, R., Servaes, P., et al. (2018). Prevalence and correlates of high fear of cancer recurrence in late adolescents and young adults consulting a specialist adolescent and young adult (AYA) cancer service. Support Care Cancer 26, 1479–1487. doi: 10.1007/s00520-017-3975-2
Thewes, B., Lebel, S., Seguin, L. C., and Butow, P. (2016). A qualitative exploration of fear of cancer recurrence (FCR) amongst Australian and Canadian breast cancer survivors. Support Care Cancer 24, 2269–2276. doi: 10.1007/s00520-015-3025-x
Thiele, S., Goebel, S., Kroger, N., and Pedersen, A. (2020). Fear of disease progression and relevant correlates in acute leukemia patients prior to allogeneic hematopoietic stem cell transplantation. Psychooncology 29, 1248–1254. doi: 10.1002/pon.5397
van den Boorn, H. G., Stroes, C. I., Zwinderman, A. H., Eshuis, W. J., Hulshof, M. C. C. M., Etten, J. F. S., et al. (2020). Health-related quality of life in curatively-treated patients with esophageal or gastric cancer: a systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 154:103069. doi: 10.1016/j.critrevonc.2020.103069
Wu, Q., Ye, Z., Li, L., and Liu, P. (2015). Reliability and validity of Chinese version of fear of progression questionnaire-short for cancer patients. Chin. J Nurs. 50, 1515–1519. doi: 10.3761/j.issn.0254-1769.2015.12.021
Wu, Z., Liu, Y., Li, X., and Li, X. (2016). Resilience and associated factors among mainland Chinese women newly diagnosed with breast cancer. PLoS One 11:e0167976. doi: 10.1371/journal.pone.0167976
Xu, L., Ma, Y., Wang, S., Feng, J., Liu, L., Wang, J., et al. (2021). Incidence of gastrointestinal stromal tumor in Chinese urban population: a national population based study. Cancer Med. 10, 737–744. doi: 10.1002/cam4.3644
Yang, Y., Sun, H., Luo, X., Li, W., Yang, F., Xu, W., et al. (2022). Network connectivity between fear of cancer recurrence, anxiety, and depression in breast cancer patients. J. Affect. Disord. 309, 358–367. doi: 10.1016/j.jad.2022.04.119
Ye, Z. J., Qiu, H. Z., Li, P. F., Liang, M. Z., Zhu, Y. F., Zeng, Z., et al. (2017). Predicting changes in quality of life and emotional distress in Chinese patients with lung, gastric, and colon-rectal cancer diagnoses: the role of psychological resilience. Psychooncology 26, 829–835. doi: 10.1002/pon.4237
Yeung, N. C. Y., and Lu, Q. (2022). Social constraints and fear of recurrence among Chinese American breast cancer survivors: an exploration of psychosocial mediators. Psychooncology 31, 98–106. doi: 10.1002/pon.5784
Yiu, H. C., Zang, Y., Chew, J. H. S., and Chau, J. P. C. (2021). The influence of confucianism on the perceptions and process of caring among family caregivers of persons with dementia: a qualitative study. J. Transcult. Nurs. 32, 153–160. doi: 10.1177/1043659620905891
Youssef, Y., Mehnert Theuerkauf, A., Gotze, H., Friedrich, M., and Esser, P. (2021). Rapid screener for the assessment of fear of progression in cancer survivors: the fear of progression questionnaire rapid screener. Eur J Cancer (Engl). 30:e13400. doi: 10.1111/ecc.13400
Zhang, Y., Li, J., and Hu, X. (2022a). The effectiveness of dignity therapy on hope, quality of life, anxiety, and depression in cancer patients: a meta-analysis of randomized controlled trials. Int. J. Nurs. Stud. 132:104273. doi: 10.1016/j.ijnurstu.2022.104273
Zhang, Y., Zhou, F., Yang, H., Gong, X., and Gao, J. (2022b). Current status of fear of disease progression in patients with advanced cancer and usefulness of dignity therapy intervention. J Healthc Eng. 2022:6069060. doi: 10.1155/2022/6069060
Zhao, H., and Wang, J. (2000). Social support and hope for hemodialysis patients. Chin. J. Nurs. 5, 49–51. doi: 10.3321/j.issn:0254-1769.2000.05.024
Keywords: gastrointestinal neoplasms, fear of progression, hope, loneliness, cancer nursing
Citation: Li Y, Xiao T, Liao H, Qu H, Ren P and Chen X (2024) Fear of progression, loneliness, and hope in patients with gastrointestinal cancer: a cross-sectional relational study. Front. Psychol. 14:1279561. doi: 10.3389/fpsyg.2023.1279561
Edited by:
Marialaura Di Tella, University of Turin, ItalyReviewed by:
Agata Benfante, University of Turin, ItalySara Veggi, University of Turin, Italy
Nuri Türk, Siirt University, Türkiye
Copyright © 2024 Li, Xiao, Liao, Qu, Ren and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoju Chen, Y2hlbnhpYW9qdUBjbWMuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
 Yanjun Li1,2†
Yanjun Li1,2† Xiaoju Chen
Xiaoju Chen