- 1Department of Health Sciences, University Magna Graecia of Catanzaro, Catanzaro, Italy
- 2Department of Clinical and Experimental Medicine, University Hospital of Messina, Messina, Italy
- 3Department of Cognitive Sciences, Psychology, Education and Cultural Studies, University of Messina, Messina, Italy
- 4Institute for Biomedical Research and Innovation (IRIB), National Research Council of Italy (CNR), Messina, Italy
- 5Department of Endocrinology, Research Centre for Ageing and Osteoporosis, Rigshospitalet-Glostrup Hospital, Copenhagen, Denmark
Growing evidence from scientific research elucidates the important role of alexithymia in chronic immune diseases. This Review aims to explore the presence of alexithymia in patients affected by asthma and clarify its associations with other involved psychological and physical factors. In January 2023, according to PRISMA guidelines, a systematic search using PubMed and Scopus was conducted. Twenty-six studies were eligible based on inclusion criteria. Alexithymia was significantly present in asthma patients, with most studies reporting a higher prevalence (from 9 to 62.8%) than in control groups (approximately 10%). The coexistence of asthma and alexithymia was associated with a worse quality of life, psychiatric comorbidity, poor symptom control, and difficulty in recognizing exacerbations of the disease. These results suggest that alexithymia can negatively impact the management of asthma. For this reason, we recommend an accuracy assessment in clinical settings and the implementation of psychological interventions to promote the emotional and physical wellbeing of asthmatic patients.
1. Introduction
Over time, researchers have shown increasing interest in the psychological factors that influence the onset, course, and outcomes of chronic illness (Cohen et al., 2015; Martino et al., 2019; Eikeseth et al., 2020; Bąk-Sosnowska et al., 2022). Psychological characteristics may influence the patient’s ability to manage chronic disease and contribute to determining variable health outcomes (Van Lieshout and MacQueen, 2008; Merlo, 2019; Conversano et al., 2020; Di Giuseppe and Conversano, 2022). On the other hand, the management of medical conditions represents a complex challenge and could increase the risk of developing psychopathology (Baiardini et al., 2015; Di Giuseppe et al., 2020; Isvoranu et al., 2021; Lin et al., 2022).
Asthma is a chronic respiratory disease characterized by persistent airway inflammation and represents one of the major public health issues worldwide (World Health Organization, 2019; Mortimer et al., 2022). It is characterized by heterogeneous symptoms, including shortness of breath, airway secretion, wheezing, chest pain, and coughing attacks, which are variable over time and in terms of intensity (Braido, 2013; Louis et al., 2023). For this reason, the Global Initiative for Asthma (GINA) guidelines classifies asthma, based on the frequency and severity of symptomatic manifestations, as intermittent and persistent, and the latter is subdivided into mild, moderate, or severe. In addition, a second classification criteria refers to the level of symptom control and allows differentiation between well-controlled, partially controlled, or uncontrolled asthma (Padem and Saltoun, 2019; Global Initiative for Asthma, 2022). According to epidemiological data provided by the “Global Burden of Disease Study,” it is estimated that 262 million people (cases: 3,416 per 100,000 people) presented with asthma in 2019 (GBD 2019 Diseases and Injuries Collaborators, 2020). Mortimer et al. (2022) analyzed the prevalence of asthma in adults in 17 countries and highlighted a rate of 4.4%; the authors provided results obtained from a study called “Global Asthma Network,” including a huge sample of adults showing a mean prevalence of 2.6% of asthma symptoms. According to the study, asthma represents a heavy burden for patients and relatives, impacting on quality of life and adaptation, as well as development. Hence, asthma as a complex medical condition causes significant social and economic burdens (Bahadori et al., 2009; Nunes et al., 2017; López-Tiro et al., 2022).
The control of asthma symptoms is complex and influenced by the presence and interaction of several factors (Braido, 2013), such as phenotypes (Hsiao et al., 2019), comorbidities (Boulet and Boulay, 2011), type of treatment (Papi et al., 2020), and patient characteristics, such as sociodemographic factors (Uchmanowicz et al., 2016), compliance (Baddar et al., 2014), adherence (Boulet et al., 2012), and behaviors (Horne et al., 2007). Moreover, different psychological aspects contribute to the process of asthma adaptation and management (Baiardini et al., 2015; Stanescu et al., 2019). Subjective perception of illness (Kaptein et al., 2010), coping strategies (Barton et al., 2003), presence of anxiety, and/or depression (Di Marco et al., 2011; Ye et al., 2021) strongly impact daily asthma management and consequently the main areas of life functioning, determining a poor perceived quality of life (Van Lieshout and MacQueen, 2008; Stanescu et al., 2019).
Alexithymia is a psychological factor reported in patients suffering from chronic respiratory diseases, such as asthma and chronic obstructive pulmonary disease (COPD), and is related to negative effects on quality of life and the exacerbation of symptoms (Braido, 2013). According to different studies, alexithymia has been described as impacting, complicating, and often directly affecting the psychological condition of subjects (Baiardini et al., 2015; Myles and Merlo, 2021). Selinheimo et al. (2022) and Zhang et al. (2023) highlighted a bidirectional influence between alexithymia and chronic respiratory diseases, and thus, reported that alexithymia increases the risk of developing chronic airway inflammation and vice versa. In the first study, subjects were followed for alexithymia for 11 years using binary logistic regressions to investigate the role of psychological factors in the onset and maintenance of physical conditions. In the second, a consistent decrease in quality of life in chronic respiratory diseases due to alexithymia was highlighted.
According to the literature, alexithymia is a multifactorial construct, defined as the difficulty in recognizing, processing, and expressing emotions and feelings, resulting in the inability to differentiate between physiological reactions to stimuli and affective dynamics (Sifneos, 2000; López-Muñoz and Pérez-Fernández, 2020). The term alexithymia was introduced by Nemiah and Sifneos (1970) to describe a lack of knowledge referring to affective dynamics in patients with psychosomatic disorders resistant to traditional treatments. Since then, this concept has undergone wide diffusion in the scientific literature, moving from its psychoanalytic origin to research fields on mechanisms of stress adaptation (Panayiotou, 2018; Myles and Merlo, 2021). In this regard, alexithymia has been described as a combination of different factors (Bagby et al., 1994; Hogeveen and Grafman, 2021), such as difficulty in identifying and describing affective states, difficulty in distinguishing kinesthetic sensations related to emotional arousal, reduced ability to imagine and fantasize, and an external event-oriented thinking style. These features have been frequently recognized in psychosomatic disorders, demonstrating that alexithymia is implicated in the alteration of the body–mind communication axis (Taylor et al., 1997; Kano and Fukudo, 2013). Moreover, in several chronic conditions, a high prevalence of alexithymia was observed among patients with negative health outcomes, also increasing the risk of developing anxiety and depression (Tselebis et al., 2010; Nekouei et al., 2014; Martino et al., 2020a,b; Zhang et al., 2023).
According to Tesio et al. (2019), alexithymia is clearly linked to precise medical domains, as in the case of dermatological diseases (Panasiti et al., 2020; Namdar and Kurtoglu, 2021; Holmes et al., 2022), cardiovascular conditions (Casagrande et al., 2019; Aluja et al., 2020; Kirchner et al., 2022), gastrointestinal disorders (Carrozzino and Porcelli, 2018; Kano et al., 2018), and chronic respiratory conditions such as asthma.
Currently, a range of studies have linked alexithymia to asthma; however, there has been no systematic synthesis of the available research examining this association. Probably because of this reason, there are several unanswered questions regarding this relationship, including whether alexithymia is frequently present in individuals with asthma and whether the characteristics of alexithymia can specifically interfere with asthma management.
The aim of this study was to perform a systematic literature review on alexithymia and asthma, offering new insights for application into clinical practice. Particularly, the present review was based on two main objectives: to provide a summary of the available evidence on the presence of alexithymia among individuals with asthma and the factors associated with alexithymia in asthmatic patients. A deeper understanding of this complexity may promote psychological adjustments, improve disease consciousness and management, and decrease the risks of adverse health outcomes.
2. Methods
This systematic review has been performed in accordance with the Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) guidelines (Liberati et al., 2009; Moher et al., 2009). The search methodology and related steps are presented as follows.
2.1. Search strategy
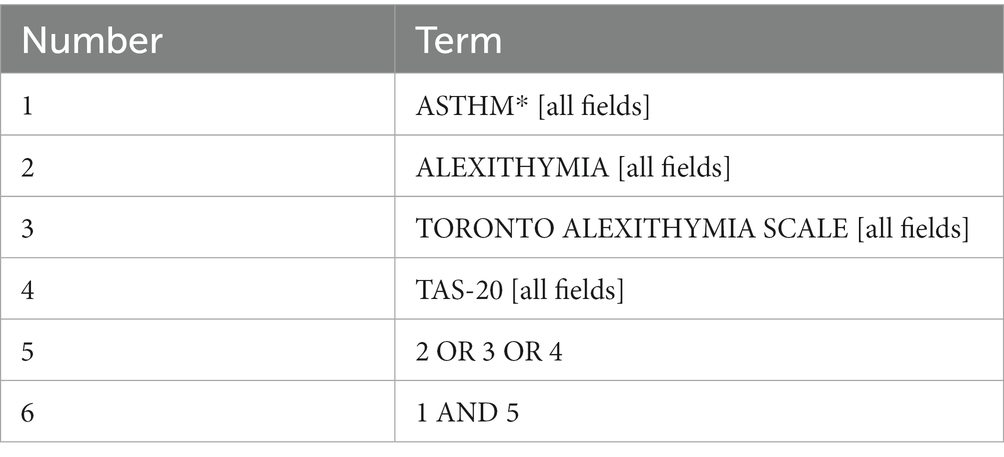
In January 2023, PubMed and Scopus databases were explored to select relevant publications. The terms searched were: “asthma” AND “alexithymia” [title, abstract, and keywords] (see Table 1 for the complete PubMed strategy). The same strategy was adopted for both databases without restrictions related to language and time. The reference lists of suitable studies from both databases were examined with the aim of identifying additional relevant articles to be added to previously selected items.
2.2. Inclusion and exclusion criteria
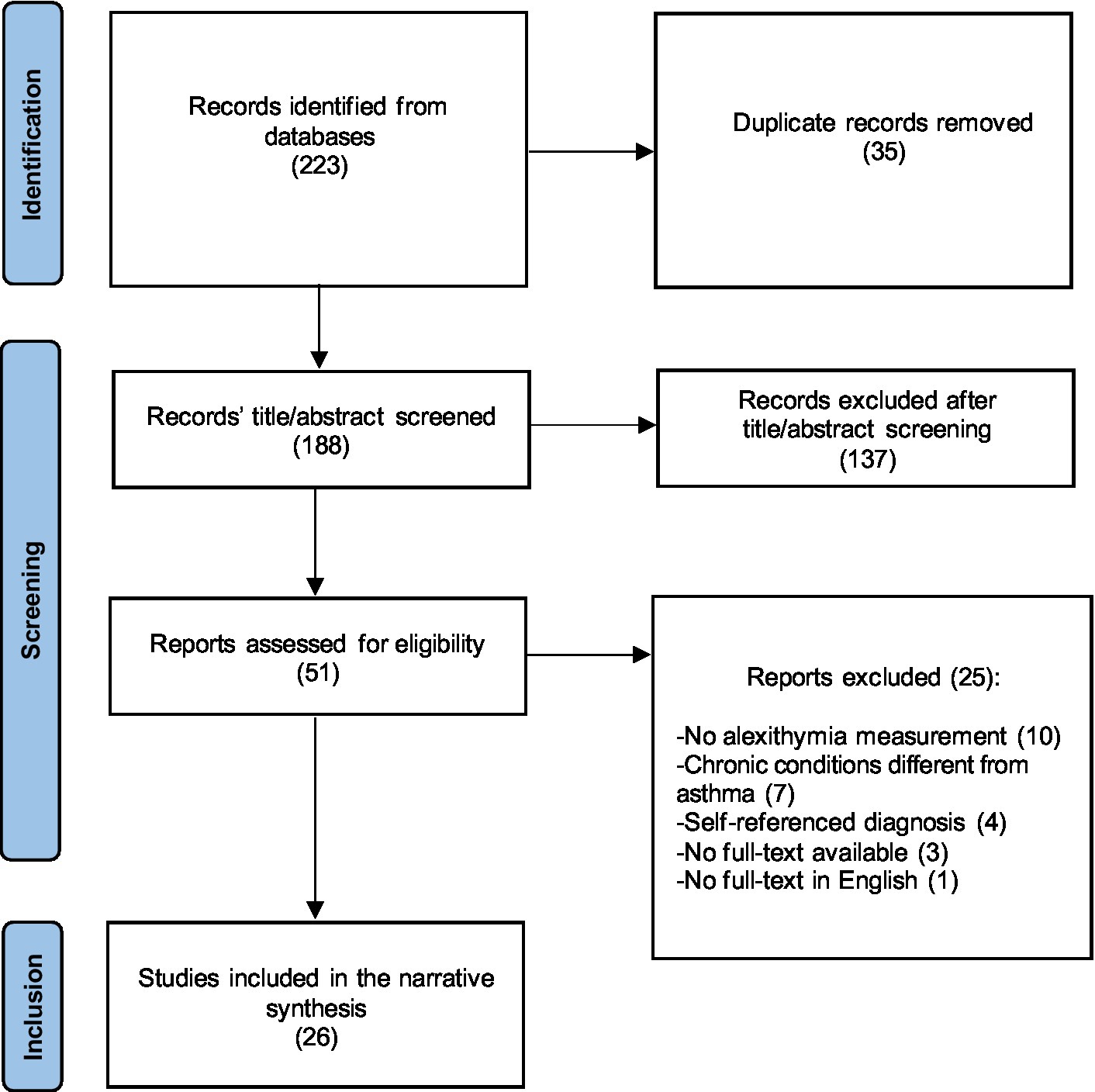
Once the PubMed and Scopus search was performed, the eligibility of the articles was based on the following criteria: (1) full-text available in English and published in peer-review journals to reduce the risk of including biased studies; (2) confirmed asthma diagnosis; and (3) use of standardized psychodiagnostic instruments measuring alexithymia to detect the variables of interest. In line with the purpose of this Review, the following publications were excluded: (1) conference abstracts, qualitative research, literature reviews, and case reports, selecting only comprehensive studies with adequate statistical methodology to link asthma to alexithymia; (2) studies in which the diagnosis was self-reported, ensuring accurate selection of the asthma population; and (3) articles in which the sample included respiratory chronic conditions other than asthma or mixed diagnosis, not being able to consider the direct relationship between asthma and alexithymia (see Figure 1, Prisma flowchart).
2.3. Screening and data extraction
After extracting results from databases, a thorough screening procedure was carried out to eliminate duplicates. In the first phase, all titles and abstracts were screened to identify potential pertinent articles. During the second phase, full-text manuscripts were examined and selected according to eligibility criteria. Data extracted from this research included author names, publication date, sample size and characteristics, main results, and tool used for alexithymia measurement.
2.4. Assessment of the methodological quality of the included studies
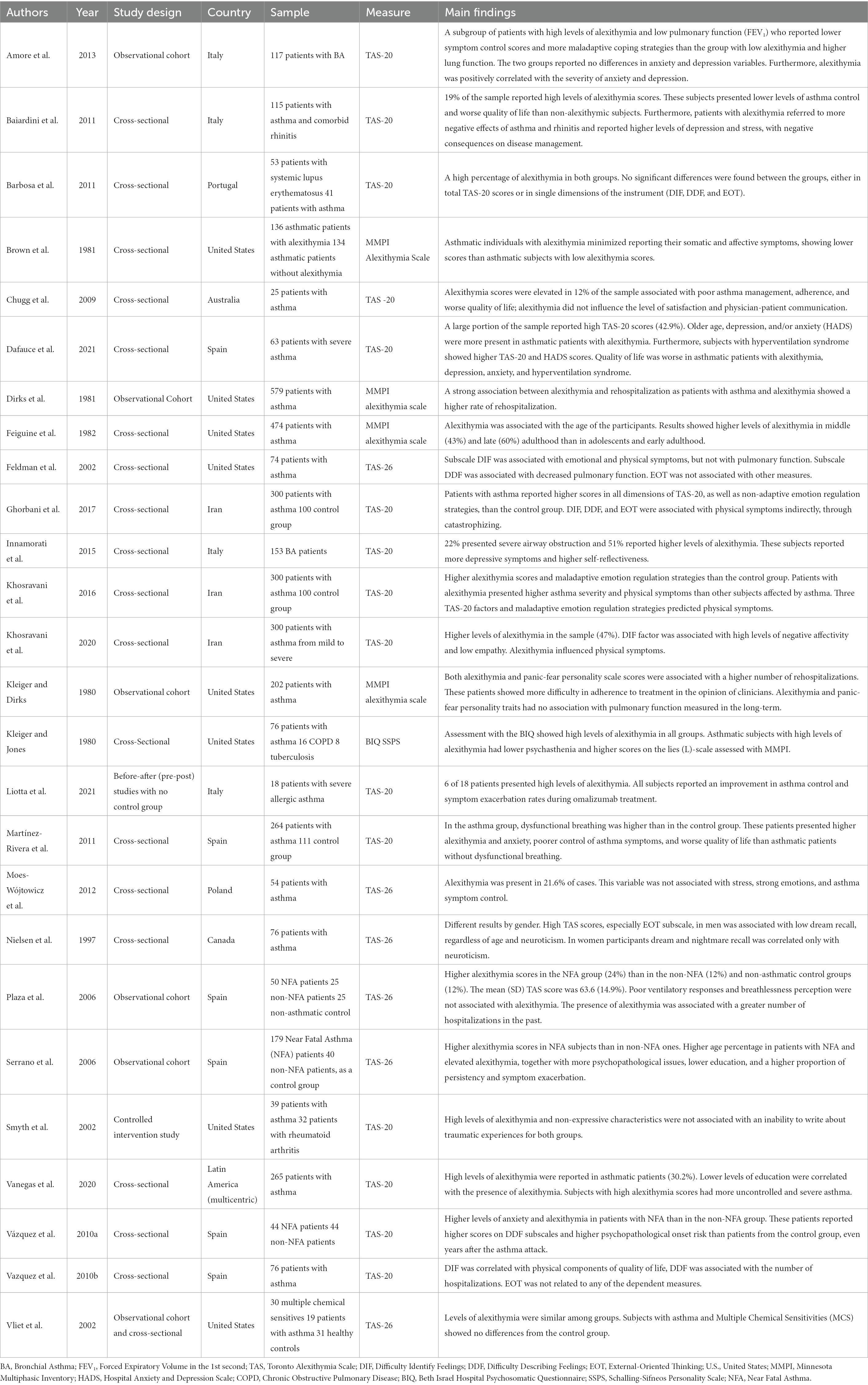
A complete evaluation of the studies was performed using the NIH Study Quality Assessment Tool. Each study was evaluated according to structure and study design by two independent reviewers, and two more reviewers were consulted when necessary. Specifically, the Quality Assessment Tool for Observational Cohort and Cross-sectional Studies, the Quality Assessment Tool for Before-After (Pre-Post) Studies with No Control Group, and the Quality Assessment of Controlled Intervention Studies were used. As shown in Table 2, this revision included 22 cross-sectional studies and six observational cohort studies evaluated with the first tool, one study assessing the effectiveness of a pharmacological intervention without a control group, and one randomized controlled trial. Finally, all the included studies were rated as “good” or “fair,” and outcomes were presented as Supplementary Table S1–S3.
3. Results
The PRISMA flowchart (Figure 1) illustrates the search strategy used for this systematic review. Through the databases search, 223 potentially eligible studies were identified and 35 were removed as duplicates. The remaining 188 records were reviewed with regard to title and abstract, and 137 were removed because of low accordance with the objectives of this Review or due to exclusion criteria. The process of recognizing valuable items through analysis of the reference lists produced no further results. Thus, 51 studies were comprehensively reviewed and 25 were excluded according to eligibility criteria. Finally, a total of 26 records were included in the current Review and analyzed with regard to three main domains (Table 2): the study characteristics and the tools used to assess alexithymia; the presence of alexithymia traits in subjects affected by asthma; and alexithymia correlation with psychological factors and physical components interfering with asthma.
3.1. Characteristics of the included studies
All 26 studies presented participants suffering from asthma, leading to a total of 4,282 subjects. Fifteen studies included adults (Feldman et al., 2002; Smyth et al., 2002; Vliet et al., 2002; Chugg et al., 2009; Vázquez et al., 2010a; Vazquez et al., 2010b; Baiardini et al., 2011; Barbosa et al., 2011; Martínez-Rivera et al., 2011; Innamorati et al., 2015; Khosravani et al., 2016, 2020; Vanegas et al., 2020; Dafauce et al., 2021; Liotta et al., 2021) and eight also included adolescents (Kleiger and Dirks, 1980; Kleiger and Jones, 1980; Dirks et al., 1981; Feiguine et al., 1982; Nielsen et al., 1997; Serrano et al., 2006; Amore et al., 2013; Ghorbani et al., 2017). Finally, three studies (Brown et al., 1981; Plaza et al., 2006; Moes-Wójtowicz et al., 2012) did not provide clear data on the age range of participants.
Asthma severity and intensity differed within the selected study. Specifically, eight studies (Brown et al., 1981; Feiguine et al., 1982; Nielsen et al., 1997; Feldman et al., 2002; Smyth et al., 2002; Vliet et al., 2002; Barbosa et al., 2011; Moes-Wójtowicz et al., 2012) selected subjects with asthma of varying degrees and did not report data on disease severity. Four studies (Khosravani et al., 2016; Ghorbani et al., 2017; Khosravani et al., 2020; Vanegas et al., 2020) analyzed patients affected by chronic asthma, with severity ranging from mild to severe. Additionally, Martínez-Rivera et al. (2011) included participants with intermittent asthma. Dirks et al. (1981), Kleiger and Dirks (1980), and Kleiger and Jones (1980) involved hospitalized patients receiving treatment. Chugg et al. (2009) and Vazquez et al. (2010b) analyzed subjects presenting moderate-to-severe persistent asthma. Two studies (Amore et al., 2013; Innamorati et al., 2015), conducted in Italy, included a sample of subjects diagnosed with bronchial asthma (BA). Three studies (Plaza et al., 2006; Serrano et al; 2006; Vázquez et al., 2010a) selected subjects affected by near-fatal asthma (NFA). Finally, Baiardini et al. (2011) analyzed 115 patients affected by asthma and comorbid rhinitis, Dafauce et al. (2021) conducted a study on 63 subjects with severe asthma, and Liotta et al. (2021) reported a small sample consisting of 18 patients with severe allergic asthma.
All studies used a standardized instrument to assess alexithymia. TAS-20 was used in more than half of the studies (Smyth et al., 2002; Chugg et al., 2009; Vázquez et al., 2010a; Vazquez et al., 2010b; Baiardini et al., 2011; Barbosa et al., 2011; Martínez-Rivera et al., 2011; Amore et al., 2013; Innamorati et al., 2015; Khosravani et al., 2016, 2020; Ghorbani et al., 2017; Vanegas et al., 2020; Dafauce et al., 2021; Liotta et al., 2021), followed by the previous 26-item version of the instrument (Nielsen et al., 1997; Feldman et al., 2002; Vliet et al., 2002; Plaza et al., 2006; Serrano et al., 2006; Moes-Wójtowicz et al., 2012). Four studies (Kleiger and Dirks, 1980; Brown et al., 1981; Dirks et al., 1981; Feiguine et al., 1982) measured alexithymia as a personality trait through the MMPI subscale. Only one single case (Kleiger and Jones, 1980) used a hetero-assessment interview (BIQ) and a self-report instrument (SPSS) to compare the homogeneity of the collected data.
Three studies included a group of asthma patients and a healthy control group (Martínez-Rivera et al., 2011; Khosravani et al., 2016; Ghorbani et al., 2017). Two studies compared patients with asthma with other chronic diseases, such as systemic lupus erythematosus (Barbosa et al., 2011) and rheumatoid arthritis (Smyth et al., 2002). Vliet et al. (2002) examined differences among subjects with multiple chemical sensitivities, asthma, and healthy controls. Regarding studies analyzing subjects with asthma and episodes of NFA, Serrano et al. (2006) and Vázquez et al. (2010a) included asthmatic subjects who presented no near-fatal exacerbations of disease as control groups, while Plaza et al. (2006) also included a third group of healthy subjects.
3.1.1. Instruments used for alexithymia assessment
Several instruments allow clinicians to measure alexithymia, but the TAS-20 (Bagby et al., 1994; Parker et al., 2003; Bagby et al., 2020) is regarded as the “gold standard.” This instrument analyzes three factors: difficulty identifying feelings (DIF); difficulty describing feelings (DDF); and externally oriented thinking (EOT). As known, DIF and DDF indicate an inability to become aware of affective states, denoting subjective experience of feelings (Goerlich, 2018), whereas EOT derives from the psychoanalytic literature, defined as “pensée opératoire” (Marty and de M'uzan, 1978), and indicates a way of thinking directed toward external objects, devoid of imagination and fantasy (Pirlot and Corcos, 2012; Schmid-Gloor, 2019; Mambou Nouemssi et al., 2021), as in the case of regression in the service of the ego (Kris, 1952).
Cross-validation studies demonstrated high consistency and validity of the TAS-20 scale, improving its scientific consideration and clinical-psychodiagnostic impact (Bach et al., 1996; Bressi et al., 1996; Franz et al., 2001; Torres et al., 2019; Bagby et al., 2020). It is derived from the previous version, the TAS-26, assessing alexithymia by dividing the construct into four factors (Taylor et al., 1985), presenting a scale for assessing the reduction in the ability to daydream. As the concept of reduced daydreaming revealed poor psychometric properties and little theoretical coherency with the alexithymia construct, it was substituted with the TAS-20 (Wise et al., 2000; Bagby et al., 2020).
As alexithymia has also been considered a maladaptive and stable personality trait, Kleiger and Kinsman (1980) developed a scale assessing this phenomenon in the MMPI personality test. This self-report instrument consists of 22 items and allows clinicians to assess the subject’s affective denial characteristics, depletion of imagination, and tendency to confound feelings derived from emotional activation. However, the MMPI-alexithymia scale has shown poor internal validity, generating the need to put in place new standardized instruments to detect this characteristic (Bagby et al., 1991). Two other instruments were introduced: BIQ and SPSS. BIQ is a semi-structured interview developed by Sifneos (1973) and is the first valid attempt to assess alexithymia. The core items cover the following domains: verbalizing emotions, emotion expression, fantasy, and external thinking (Bermond et al., 2015). The second instrument (SPSS) derived from BIQ was the first self-report instrument to measure alexithymia (Apfel and Sifneos, 1979). This instrument has no specific factorial scales and offers only a global score, although a division into three scales can be traced in the literature: the ability to identify and describe feelings, the ability to fantasize, and the presence of apathy (Martin et al., 1984).
3.2. Presence of alexithymia in asthmatic populations
Among the selected studies, 16 (Kleiger and Jones, 1980; Dirks et al., 1981; Smyth et al., 2002; Plaza et al., 2006; Serrano et al., 2006; Chugg et al., 2009; Vázquez et al., 2010a; Baiardini et al., 2011; Barbosa et al., 2011; Moes-Wójtowicz et al., 2012; Amore et al., 2013; Innamorati et al., 2015; Khosravani et al., 2016, 2020; Vanegas et al., 2020; Dafauce et al., 2021) provided data on prevalence estimation of alexithymia in asthma patients, reporting different results based on the instruments used and the populations considered. Seven studies (Kleiger and Dirks, 1980; Brown et al., 1981; Feiguine et al., 1982; Nielsen et al., 1997; Feldman et al., 2002; Vazquez et al., 2010b; Liotta et al., 2021) reported the presence of alexithymia among asthmatic patients, without providing prevalence estimates or comparisons on mean alexithymia scores among patients with asthma or other controls. Three studies (Vliet et al., 2002; Martínez-Rivera et al., 2011; Ghorbani et al., 2017) compared the mean alexithymia scores of subjects with control groups with or without asthma.
The highest percentage was reported by Khosravani et al. (2016) in a sample of 300 Iranian asthma patients (62.8%), using the TAS-20. However, the authors stated that subjects with asthma presented lower levels of education than the control group, and the sample consisted of subjects with severe (108), moderate (139), and mild asthma (53). In a second study, Khosravani et al. (2020) revealed an alexithymia prevalence of 47% in a sample of 300 subjects with asthma; additionally, in this case, the number of patients with severe asthma (n = 134) was greater than that with mild discomfort (n = 32). According to these data, a high percentage of alexithymia (42,9%) was also reported by Dafauce et al. (2021), involving only patients with severe asthma. Liotta et al. (2021), who analyzed patients with severe allergic asthma (SAA), found that six out of 18 had a TAS-20 score of ≥ 61, indicating high-pathological levels of alexithymia. Therefore, the severity of asthma symptoms seemed to have a significant influence on the presence of alexithymia in patients with such chronic conditions (Liotta et al., 2021).
Amore et al. (2013) and Innamorati et al. (2015) found that 15 and 13.7% of patients with BA presented high TAS-20 scores (≥ 61), and these subjects also showed worse physical and mental health outcomes than asthmatic patients. Baiardini et al. (2011) reported that 19% of patients with asthma and comorbid rhinitis showed high levels of alexithymia, accompanied by a worsening of symptoms and lower quality of life.
With reference to NFA, Plaza et al. (2006) and Serrano et al. (2006), using the TAS-26, found that, respectively, 24 and 36% of NFA patients displayed high levels of alexithymia. On the contrary, Vázquez et al. (2010a), using TAS-20, reported 9% of 44 subjects with NFA presented higher levels of alexithymia than non-alexithymic subjects in the control group consisting of patients with asthma without any experience of near-fatal crisis. These differences could be due to the use of different versions of the TAS for the assessment of alexithymia in asthmatic patients.
Chugg et al. (2009) administered the TAS-20 to a sample of 25 patients with moderate-to-severe asthma and revealed that 12% were high alexithymic subjects and 52% had borderline scores. Using the same instrument, Vanegas et al. (2020) found that in large samples of Latin American subjects with asthma, 30.2% had high alexithymia scores. Barbosa et al. (2011) highlighted a higher prevalence of alexithymia in systemic lupus erythematosus patients (51%) than in a group of asthmatic subjects (34%), but differences in the mean scores were not significant. The authors concluded that difficulty in recognizing and decoding feelings may be a common factor in these chronic medical conditions. Smyth et al. (2002) found that 13% of participants had a high TAS-20 score (≥ 61). However, this study used a group consisting of subjects with asthma and rheumatoid arthritis, and the authors did not analyze the TAS-20 score differences between groups. Moes-Wójtowicz et al. (2012) used the TAS-26 with a sample of Polish asthmatic patients and reported high levels of alexithymia (21.6%).
Dirks et al. (1981) used MPPI-alexithymia scales with a sample of 549 patients receiving intensive treatment for asthma and found that 33.7% of the sample had high alexithymia and 47.8% presented borderline levels. This study considered alexithymia as a stable personality trait that can influence the life functioning areas of the subjects.
Finally, Kleiger and Jones (1980) studied a heterogeneous sample of subjects with chronic respiratory diseases, consisting mostly of patients with asthma. In this study, the authors revealed that 47% of subjects had alexithymia using a hetero-assessment tool (BIQ).
Regarding the remaining results, Ghorbani et al. (2017) found that asthmatic patients exhibited higher mean scores on the three alexithymia subscales of the TAS-20 that healthy controls. Martínez-Rivera et al. (2011) reported similar results, again using the TAS-20. Only Vliet et al. (2002) found no statistically significant differences in mean scores of the TAS-26 when comparing three groups of subjects (multiple chemical sensitivities, asthma, and healthy controls). However, there were fewer participants with asthma than in other studies, and data on the severity of disease were not provided.
3.3. Association between alexithymia and other factors intervening in asthma
Twenty-four studies (Kleiger and Dirks, 1980; Kleiger and Jones, 1980; Brown et al., 1981; Dirks et al., 1981; Feiguine et al., 1982; Nielsen et al., 1997; Feldman et al., 2002; Smyth et al., 2002; Plaza et al., 2006; Serrano et al., 2006; Chugg et al., 2009; Vázquez et al., 2010a; Vazquez et al., 2010b; Baiardini et al., 2011; Martínez-Rivera et al., 2011; Moes-Wójtowicz et al., 2012; Amore et al., 2013; Innamorati et al., 2015; Khosravani et al., 2016, 2020; Ghorbani et al., 2017; Vanegas et al., 2020; Dafauce et al., 2021; Liotta et al., 2021) reported associations among alexithymia and other factors implicated in asthma. The analysis of these scientific contributions highlights some relevant issues, including quality of life, control of symptoms, psychiatric morbidity, pulmonary functioning, and hospitalization.
All studies in which clinicians administrated instruments to measure quality of life in asthmatic subjects (Chugg et al., 2009; Vazquez et al., 2010b; Baiardini et al., 2011; Martínez-Rivera et al., 2011; Dafauce et al., 2021; Liotta et al., 2021) showed that alexithymia presented a significant influence on this variable, leading to a lower perceived quality of life, despite adjusting for confounders (i.e., sociodemographic characteristics and the presence of anxiety or depression). Martínez-Rivera et al. (2011), analyzing subscales of TAS-20, found that DIF was associated with a low control of asthma symptoms, anxiety, worse affective quality of life, and a high probability of developing dysfunctional breathing. Vazquez et al. (2010b) reported that DDF was associated with a worse physical dimension of quality of life, and this relationship was maintained even after controlling for depressive and anxious symptoms. It has been hypothesized that asthmatic patients who manifested this found it difficult to encode and express emotions, confused simple bodily sensations with asthma symptoms, and had a lower adherence and worsening general health (Vazquez et al., 2010b; Martínez-Rivera et al., 2011).
Asthma control represents the main treatment goal that will increase positive health outcomes. Eight studies (Serrano et al., 2006; Chugg et al., 2009; Baiardini et al., 2011; Martínez-Rivera et al., 2011; Moes-Wójtowicz et al., 2012; Amore et al., 2013; Dafauce et al., 2021; Liotta et al., 2021) investigated this factor in relation to alexithymia in subjects affected by asthma. Except for Moes-Wójtowicz et al. (2012), all the authors (Chugg et al., 2009; Baiardini et al., 2011; Martínez-Rivera et al., 2011; Amore et al., 2013; Vanegas., 2020; Dafauce et al., 2021; Liotta et al., 2021) found that alexithymia was associated with poor symptom control, and this finding was not directly related to the severity of asthma (Baiardini et al., 2011). Therefore, if on the one hand the presence of alexithymia was high in subjects with severe asthma (Khosravani et al., 2020; Vanegas et al., 2020; Dafauce et al., 2021), on the other hand, this variable acted as an independent factor on asthma management and symptom control (Baiardini et al., 2011).
Moes-Wójtowicz et al. (2012) did not report significant associations between alexithymia and asthma control. This result contrasts with data from other studies (Serrano et al., 2006; Chugg et al., 2009; Baiardini et al., 2011; Martínez-Rivera et al., 2011; Amore et al., 2013; Vanegas et al., 2020; Dafauce et al., 2021; Liotta et al., 2021); however, the sample size was limited, and the authors declared that subjects had difficulties in filling out the Asthma Control Test.
Psychopathological morbidity was analyzed in ten studies (Feldman et al., 2002; Plaza et al., 2006; Serrano et al., 2006; Vázquez et al., 2010a; Baiardini et al., 2011; Martínez-Rivera et al., 2011; Amore et al., 2013; Innamorati et al., 2015; Khosravani et al., 2020; Dafauce et al., 2021), with particular reference to depression and anxiety. Amore et al. (2013) and Innamorati et al. (2015) administered the State–Trait Anxiety Inventory (STAI) and Beck Depression Inventory (BDI), reporting different results. Amore et al. (2013) divided samples in terms of pulmonary functioning (high-low) and TAS-20 score (cutoff of > 61) and did not reveal differences in the levels of depression and anxiety, despite highlighting a significant correlation between alexithymia, depression, and anxiety. Innamorati et al. (2015) found high levels of alexithymia and low pulmonary functioning in a small group of patients exhibiting moderate-to-severe depression compared with other clusters of patients, but did not report differences between the groups in terms of anxiety levels. Baiardini et al. (2011), using an instrument that generally assesses emotional distress (Profile of Mood States), reported that alexithymic participants with asthma showed higher levels of depression (p < 0.001), confusion (p > 0.001), and inertia (p < 0.001) than non-alexithymic subjects. Dafauce et al. (2021), referring to patients with severe asthma, highlighted a high rate of anxiety, depression, alexithymia, and hyperventilation syndrome, with negative effects on global quality of life.
Feldman et al. (2002), when analyzing relationships between TAS-26 factors and self-report symptoms, found that DIF was associated with increased emotions and physical self-reported symptoms, and this relationship was mediated by trait anxiety, which was evaluated using the Taylor Manifest Anxiety Scale (TMAS). Khosravani et al. (2020), when administering Depression Anxiety Stress Scales (DASS) in patients with asthma of varying degrees, revealed that participants with high scores in DIF, DDF, and EOT showed higher DASS global scores. Furthermore, anxiety, depression, and emotional distress (DASS) represented a mediation factor between DIF and physical symptoms.
Two studies (Plaza et al., 2006; Serrano et al., 2006) that used the General Health Questionnaire (GHQ) to measure psychological health, indicated that psychiatric morbidity (anxiety and depression) was more frequent in subjects with life-threatening asthma with high alexithymia assessment (TAS-26) scores. Vázquez et al. (2010a) did not find differences in total TAS-20 scores between patients with NFA and control groups; however, they highlighted that DDF and anxiety-trait (STAI-T) influenced different health outcomes in both groups. Furthermore, in this study, the associations between alexithymia, asthma severity, and depression cognitive factors were not disclosed (Cognitive Depression Index, CDI).
Pulmonary functioning was evaluated through different methods in seven studies (Kleiger and Dirks, 1980; Feldman et al., 2002; Plaza et al., 2006; Serrano et al., 2006; Martínez-Rivera et al., 2011; Amore et al., 2013; Innamorati et al., 2015). Among these studies, three (Kleiger and Dirks, 1980; Plaza et al., 2006; Serrano et al., 2006) did not report significant differences in pulmonary parameters according to levels of alexithymia observed in patients with asthma. On the opposite side, four studies (Feldman et al., 2002; Martínez-Rivera et al., 2011; Amore et al., 2013; Innamorati et al., 2015) highlighted a relationship between the severity of alexithymia and impaired pulmonary function in asthma. Particularly, Feldman et al. (2002), administering the TAS-26, found that DDF was correlated with decreased pulmonary function. It was suggested that alexithymia might alter the ability of patients to communicate their experience of disease to clinicians, confounding sensations, emotions, and feelings related to their chronic condition, possibly underestimating the exacerbation of symptoms and compromising adherence and disease management (Chugg et al., 2009; Vanegas et al., 2020).
With regard to hospitalization, Dirks et al. (1981), evaluating a group of patients for 6 months, revealed a higher frequency of asthma-related hospitalizations in patients with severe alexithymia (37.4% vs. 28.4%) and also found a significant difference in mean days spent in hospice care (18,92 vs. 13,70) between patients with high levels of alexithymia and subjects with only asthma. Kleiger and Dirks (1980) analyzed the association between panic-fear personality, which is understood as the tendency to be overwhelmed and feeling helpless in the face of illness and alexithymia. Results indicated that independently of panic-fear personality, subjects who showed alexithymic personality trait (MMPI) had a higher frequency of previous hospitalizations. These results are in line with more recent studies (Plaza et al., 2006; Serrano et al., 2006; Vazquez et al., 2010b) that highlighted the increased need for emergency care in asthmatic patients with alexithymic characteristics.
Feiguine et al. (1982) analyzed alexithymia in relation to the age of asthmatic patients and found that the highest levels of alexithymia were present in middle (40–59) and late adulthood (> 65). Other studies confirmed these associations (Kleiger and Jones, 1980; Plaza et al., 2006; Serrano et al., 2006; Dafauce et al., 2021), showing that as age increases, levels of alexithymia tend to rise. Another interesting relationship emerged in relation to educational levels, as three studies (Serrano et al., 2006; Chugg et al., 2009; Vanegas et al., 2020) reported that alexithymia was higher in patients with a poor school education. Therefore, age and educational level may represent factors that increase levels of alexithymia with unfavorable outcomes in asthma.
Two studies conducted in Iran (Khosravani et al., 2016; Ghorbani et al., 2017) confirmed a close association between alexithymia, maladaptive emotional regulation strategies, and physical symptoms, including those not directly related to typical asthma manifestations. Furthermore, Ghorbani et al. (2017) highlighted that catastrophizing tendency was associated with all TAS-20 dimensions (DIF, DDF, and EOT) and was a mediator between alexithymia and physical symptoms. According to these results, Amore et al. (2013) found a correlation between alexithymia and avoidance coping strategies, with reference to denial and behavioral disengagement. These data suggested that alexithymia alters the ability of asthmatic patients to process emotional stimuli, producing negative effects on the psychological, physical, and social sphere of the individual.
Brown et al. (1981) found that alexithymic patients reported lower Asthma Symptoms Checklist scores and hypothesized that these individuals underestimate both physical and emotional components of asthma exacerbations. Kleiger and Jones (1980) reported that patients with alexithymia had high scores on the L scale and low scores on the psychasthenia scale of the MMPI. Additionally, in this case, the authors interpreted results while assuming that alexithymic individuals have greater difficulty in recognizing and processing their emotions.
Finally, two studies (Nielsen et al., 1997; Smyth et al., 2002) examined the association between alexithymia and particular aspects in patients with asthma. Nielsen et al. (1997) analyzed dream and nightmare recall and highlighted that the EOT factor, for men only, is associated with a lower memory of both. A study by Smyth et al. (2002) attempted to analyze the effect of different variables related to emotional processing on writing about traumatic events. In this case, there was no association between alexithymia and the ability to write about traumatic life events.
4. Discussion
Starting from the analysis of the scientific literature that focused on psychological factors influencing the course and management of asthma, it was hypothesized that alexithymia might negatively affect the health of patients. Therefore, the current Review attempted to detect the frequency of severe alexithymia in asthmatic populations and investigate the relationships among alexithymia and other factors involved in disease management. Evidence could provide new insights into the affective dynamics of patients with asthma, facilitating implementation of a multidisciplinary approach to the disease, improving the health of patients.
The term alexithymia has been translated from Greek to mean “wordlessness for emotions” (López-Muñoz and Pérez-Fernández, 2020). Since its introduction, this complex phenomenon has been investigated in chronic conditions (Martino et al., 2020a,b; Tang et al., 2022), psychosomatic disorders (Nakao and Takeuchi, 2018), and psychopathology (De Berardis et al., 2008; Sagar et al., 2021). Research has widely demonstrated that alexithymia may contribute to the impairment of biological, psychological, and social domains in individuals, increasing the risk of comorbidity and mortality among subjects affected by chronic diseases (Kojima et al., 2010; Kojima, 2012; Vadini et al., 2019).
Regarding chronic respiratory diseases, our results showed a high presence of alexithymia in patients with asthma, indicating a meaningful impairment of affective capacities and a tendency to confuse disease symptoms with emotional stimuli. The prevalence of alexithymia among the general population is estimated to be approximately 10% (Franz et al., 2008; Wang et al., 2021), while the results of the current Review indicate higher rates in asthma patient samples (from 9 to 62.7%).
However, among the considered studies, significant differences emerged based on disease severity, target population, geographic localization, and the psychodiagnostic instruments used to assess alexithymia, making a comparison difficult but stimulating useful considerations. It is an unmet need to provide additional empirical evidence on this topic, using a scientific multidisciplinary integrated approach that allows physicians and clinical psychologists to evaluate patient needs from an interdisciplinary perspective. Future research could promote a deeper understanding of the interrelationship between alexithymia and asthma, leading to the early identification of signs and symptoms and promoting better self-awareness and disease management and providing a higher perceived quality of life.
Moreover, concerning interrelationships among alexithymia and other factors involved in asthma management, the current Review highlighted that alexithymia is associated with a lower quality of life, low control of symptoms, a high number of hospitalizations, cognitive avoidance, and psychopathology. In addition, although the results are not always aligned, some studies have also found a significant association between alexithymia and impaired pulmonary function. As such, alexithymia represents a vulnerability factor in the management of chronic asthma and in the long-term health of the subject (Braido, 2013; Baiardini et al., 2015).
Our results are in line with the initial hypothesis and implement knowledge regarding the role of alexithymia in patients with asthma. Axelsson et al. (2009), in a study involving young adults with asthma, found that alexithymia was associated with a lower adherence to therapies, and Chung et al. (2012) suggested that this variable influenced the psychological health of subjects who had experienced an asthma crisis. These studies were not included in our review because the patient diagnoses were self-reported, so they did not meet the inclusion criteria, even if they add further empirical evidence to our findings. With reference to the relationship between alexithymia and medical conditions, Carta et al. (2022) reported that this variable is associated with an increased risk of death in a long-term course of myocardial infarction. Such an association may be due to a delay in requesting help, depending on the difficulty of the early identification of the typical symptoms of a heart attack. In accordance with these findings, our results showed that asthmatic patients with alexithymia have poor symptom control. Additionally, a high prevalence of alexithymia has been found in dermatological diseases (Holmes et al., 2022). In psoriasis (Panasiti et al., 2020) and atopic dermatitis (Talamonti et al., 2021), alexithymia has been associated with the presence of depression, difficult emotional regulation, and negative coping strategies (Founta et al., 2019; Belugina, 2021). In gastroenterology domains, a recent review on inflammatory bowel disease (Martino et al., 2020a) elucidated that the presence of alexithymia was correlated with symptoms of anxiety and depression. Kano et al. (2018), investigating the literature on functional gastrointestinal disorders (i.e., irritable bowel syndrome), found that alexithymia is associated not only with the visceral hypersensitivity that characterizes these conditions but also with an altered psychological processing of symptoms. However, the mechanisms of interaction between alexithymia and impaired gut-brain communication are still unclear. Nevertheless, alexithymia showed a significant role in other relevant clinical conditions, such as fibromyalgia and type 2 diabetes mellitus (T2DM). In particular, it has been highlighted that alexithymia increases the risk of psychological disorders in fibromyalgic patients, modifying the subjective experience of pain (Tesio et al., 2018; Marchi et al., 2019); additionally, alexithymia has been associated with poor glycemic control, difficulty in disease management, anxiety, and depression in T2DM patients (Martino et al., 2020b; Celik et al., 2022).
Researchers also investigated the relationship between alexithymia and chronic obstructive pulmonary disease (COPD), noting that this variable is associated with anxiety, depression, and impaired quality of life (Tselebis et al., 2010; Zhang et al., 2023), thus confirming the relevance of analyzing alexithymia in clinical settings.
Finally, the difficulties in recognizing and describing inner dynamics, feelings, and a poor imaginative life associated with operative thinking represent potential characteristics involved in the onset, maintenance, and unfavorable disease course (Lumley et al., 2008). Research highlights the existence of a subgroup of asthma patients presenting clinically significative levels of alexithymia. Such individuals show an inability to get in touch with emotions and feelings and poor interoceptive awareness (Kano and Fukudo, 2013). Therefore, this complex phenomenon could explain the difficulty in distinguishing states of emotional arousal from typical asthma symptoms (i.e., dyspnea, breathlessness, and asthma attack), with negative repercussions on disease self-management. From a clinical perspective, the present Review suggests the early identification of asthmatic patients presenting alexithymia is important. The psychodiagnostic path provides a solid basis that is useful for the evaluation of a patient’s psychological status, personological characteristics, and patient-tailored interventions and treatments.
Chronic disease, and in the specific case of asthma, due its characteristics, requires continuous adjustment for patients to balance daily life tasks with the demand of the illness. In this context, awareness of emotions and feelings and reflective ability occupy a fundamental role in ensuring wellbeing and equilibrium between these factors. Consistently, data from the current Review suggest that the negative impact of alexithymia on health may be effectively controlled through clinical intervention programs (Nunes da Silva, 2021; Zhang and Zhang, 2022). This path would favor the improvement of emotional skills, promotion of patient self-disclosure, and therapeutic alliance, driving toward a multi-integrated approach allowing early diagnosis by clinicians and collaborative treatment.
5. Strengths and limitations
To the best of our knowledge, this is the first systematic Review exploring the phenomenon of alexithymia in association with asthma. The current Review has several limitations. First, most of the studies taken into consideration used convenience samples; therefore, the severity and type of asthma were not equally distributed in the population. Based on the established criteria, not many studies could be included, limiting the possibility of generalizing our results to a broader context. In the included studies, the assessment of alexithymia was carried out with different instruments (TAS-20, TAS-26, MMPI, and BIQ), leading to heterogeneity in the results and limiting the possibility of making a quantitative synthesis. Based on the findings, the present Review is a first step toward a greater understanding of the alexithymia burden in asthma management and offers clinicians valuable information regarding the treatment of asthma patients.
6. Conclusion
This Review highlights a significant presence of alexithymia in asthma patients, in association with anxiety, depression, lower quality of life, difficulty in identifying asthma symptoms, maladaptive emotion regulation strategies, exacerbation of disease, and hospitalization. Therefore, clinicians and psychologists could apply a multidisciplinary approach to early detect the presence of alexithymia and asthma, improving the diagnostic and therapeutic work-up in clinical settings and providing a better perceived quality of life.
Author contributions
GM and OS made significant contribution to the conception and design of the systematic review, to the acquisition, qualitative analysis, and synthesis of data by drafting both the first and revised versions of the manuscript. LR, AC, and CV contributed to the qualitative analysis and synthesis of data by drafting both the first and revised versions of the manuscript. FT, GP, GS, and PS gave significant contribution to draft part of the manuscript. PS, SG, and GM revised the manuscript for intellectual content and gave the final approval of the manuscript to be submitted. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1221648/full#supplementary-material
References
Aluja, A., Malas, O., Urieta, P., Worner, F., and Balada, F. (2020). Biological correlates of the Toronto alexithymia scale (TAS-20) in cardiovascular disease and healthy community subjects. Physiol. Behav. 227:113151. doi: 10.1016/j.physbeh.2020.113151
Amore, M., Antonucci, C., Bettini, E., Boracchia, L., Innamorati, M., Montali, A., et al. (2013). Disease control in patients with asthma is associated with alexithymia but not with depression or anxiety. Behav. Med. (Washington, DC) 39, 138–145. doi: 10.1080/08964289.2013.818931
Apfel, R. J., and Sifneos, P. E. (1979). Alexithymia: concept and measurement. Psychother. Psychosom. 32, 180–190. doi: 10.1159/000287386
Axelsson, M., Emilsson, M., Brink, E., Lundgren, J., Torén, K., and Lötvall, J. (2009). Personality, adherence, asthma control and health-related quality of life in young adult asthmatics. Respir. Med. 103, 1033–1040. doi: 10.1016/j.rmed.2009.01.013
Bach, M., Bach, D., De Zwaan, M., Serim, M., and Böhmer, F. (1996). Validation of the German version of the 20-item Toronto alexithymia scale in normal persons and psychiatric patients. Psychother. Psychosom. Med. Psychol. 46, 23–28.
Baddar, S., Jayakrishnan, B., and Al-Rawas, O. A. (2014). Asthma control: importance of compliance and inhaler technique assessments. J. Asthma 51, 429–434. doi: 10.3109/02770903.2013.871558
Bagby, R. M., Parker, J. D., and Taylor, G. J. (1991). Reassessing the validity and reliability of the MMPI alexithymia scale. J. Pers. Assess. 56, 238–253. doi: 10.1207/s15327752jpa5602_5
Bagby, R. M., Parker, J. D., and Taylor, G. J. (1994). The twenty-item Toronto alexithymia scale—I. Item selection and cross-validation of the factor structure. J. Psychosom. Res. 38, 23–32. doi: 10.1016/0022-3999(94)90005-1
Bagby, R. M., Parker, J. D. A., and Taylor, G. J. (2020). Twenty-five years with the 20-item Toronto alexithymia scale. J. Psychosom. Res. 131:109940. Advance online publication. doi: 10.1016/j.jpsychores.2020.109940
Bahadori, K., Doyle-Waters, M. M., Marra, C., Lynd, L., Alasaly, K., Swiston, J., et al. (2009). Economic burden of asthma: a systematic review. BMC Pulm. Med. 9:24. doi: 10.1186/1471-2466-9-24
Baiardini, I., Braido, F., Ferraioli, G., Menoni, S., Bruzzone, M., Conte, M. E., et al. (2011). Pitfalls in respiratory allergy management: alexithymia and its impact on patient-reported outcomes. J. Asthma 48, 25–32. doi: 10.3109/02770903.2010.535883
Baiardini, I., Sicuro, F., Balbi, F., Canonica, G. W., and Braido, F. (2015). Psychological aspects in asthma: do psychological factors affect asthma management? Asthma Res. Pract. 1:7. doi: 10.1186/s40733-015-0007-1
Bąk-Sosnowska, M., Gruszczyńska, M., Wyszomirska, J., and Daniel-Sielańczyk, A. (2022). The influence of selected psychological factors on medication adherence in patients with chronic diseases. Healthcare 10, 1–12. doi: 10.3390/healthcare10030426
Barbosa, F., Mota, C., Patrício, P., Alcântara, C., Ferreira, C., and Barbosa, A. (2011). The relationship between alexithymia and psychological factors in systemic lupus erythematosus. Compr. Psychiatry 52, 754–762. doi: 10.1016/j.comppsych.2010.11.004
Barton, C., Clarke, D., Sulaiman, N., and Abramson, M. (2003). Coping as a mediator of psychosocial impediments to optimal management and control of asthma. Respir. Med. 97, 747–761. doi: 10.1016/S0954-6111(03)00029-5
Belugina, O. (2021). Psychosomatic aspects of psoriasis and atopic dermatitis. BJPsych Open 7, S7–S8. doi: 10.1192/bjo.2021.80
Bermond, B., Oosterveld, P., and Vorst, H. C. M. (2015). “Measures of alexithymia” in Measures of Personality and Social Psychological Constructs. eds. G. J. Boyle, D. H. Saklofske, and G. Matthews (Cambridge, MA: Elsevier Academic Press), 227–256.
Boulet, L.-P., and Boulay, M.-È. (2011). Asthma-related comorbidities. Expert Rev. Respir. Med. 5, 377–393. doi: 10.1586/ers.11.34
Boulet, L.-P., Vervloet, D., Magar, Y., and Foster, J. M. (2012). Adherence: the goal to control asthma. Clin. Chest Med. 33, 405–417. doi: 10.1016/j.ccm.2012.06.002
Braido, F. (2013). Failure in asthma control: reasons and consequences. Scientifica 2013, 1–15. doi: 10.1155/2013/549252
Bressi, C., Taylor, G., Parker, J., Bressi, S., Brambilla, V., Aguglia, E., et al. (1996). Cross validation of the factor structure of the 20-item Toronto alexithymia scale: an Italian multicenter study. J. Psychosom. Res. 41, 551–559. doi: 10.1016/s0022-3999(96)00228-0
Brown, E. L., Fukuhara, J. T., and Feiguine, R. J. (1981). Alexithymic asthmatics: the miscommunication of affective and somatic states. Psychother. Psychosom. 36, 116–121. doi: 10.1159/000287534
Carrozzino, D., and Porcelli, P. (2018). Alexithymia in gastroenterology and hepatology: a systematic review. Front. Psychol. 9:470. doi: 10.3389/fpsyg.2018.00470
Carta, M. G., Sancassiani, F., Bina, D., Licciardi, M., Cossu, G., Nardi, A. E., et al. (2022). Alexithymia is a determinant of early death in the long-term course of post-myocardial infarction. J. Public Health Res. 11:2803. doi: 10.4081/jphr.2022.2803
Casagrande, M., Mingarelli, A., Guarino, A., Favieri, F., Boncompagni, I., Germanò, R., et al. (2019). Alexithymia: a facet of uncontrolled hypertension. Int. J. Psychophysiol. 146, 180–189. doi: 10.1016/j.ijpsycho.2019.09.006
Celik, S., Taskin Yilmaz, F., Yurtsever Celik, S., Anataca, G., and Bulbul, E. (2022). Alexithymia in diabetes patients: its relationship with perceived social support and glycaemic control. J. Clin. Nurs. 31, 2612–2620. doi: 10.1111/jocn.16088
Chugg, K., Barton, C., Antic, R., and Crockett, A. (2009). The impact of alexithymia on asthma patient management and communication with health care providers: a pilot study. J. Asthma 46, 126–129. doi: 10.1080/02770900802468525
Chung, M. C., Rudd, H., and Wall, N. (2012). Posttraumatic stress disorder following asthma attack (post-asthma attack PTSD) and psychiatric co-morbidity: the impact of alexithymia and coping. Psychiatry Res. 197, 246–252. doi: 10.1016/j.psychres.2012.01.008
Cohen, B. E., Edmondson, D., and Kronish, I. M. (2015). State of the art review: depression, stress, anxiety, and cardiovascular disease. Am. J. Hypertens. 28, 1295–1302. doi: 10.1093/ajh/hpv047
Conversano, C., Di Giuseppe, M., Miccoli, M., Ciacchini, R., Di Silvestre, A., Lo Sterzo, R., et al. (2020). Retrospective analyses of psychological distress and defense style among cancer patients. Clin. Neuropsychiatry 17, 217–224. doi: 10.36131/cnfioritieditore20200403
Dafauce, L., Romero, D., Carpio, C., Barga, P., Quirce, S., Villasante, C., et al. (2021). Psycho-demographic profile in severe asthma and effect of emotional mood disorders and hyperventilation syndrome on quality of life. BMC Psychol. 9:3. doi: 10.1186/s40359-020-00498-y
De Berardis, D., Campanella, D., Nicola, S., Gianna, S., Alessandro, C., Chiara, C., et al. (2008). The impact of alexithymia on anxiety disorders: a review of the literature. Curr. Psychiatr. Rev. 4, 80–86. doi: 10.2174/157340008784529287
Di Giuseppe, M., and Conversano, C. (2022). Psychological components of chronic diseases: the link between defense mechanisms and alexithymia. Mediterranean. J. Clin. Psychol. 10, 1–19. doi: 10.13129/2282-1619/mjcp-3602
Di Giuseppe, M., Prout, T. A., Fabiani, M., and Kui, T. (2020). Defensive profile of parents of children with externalizing problems receiving regulation-focused psychotherapy for children (RFP-C): a pilot study. Mediterranean J. Clin. Psychol. 8. doi: 10.6092/2282-1619/mjcp-2515
Di Marco, F., Santus, P., and Centanni, S. (2011). Anxiety and depression in asthma. Curr. Opin. Pulm. Med. 17, 39–44. doi: 10.1097/MCP.0b013e328341005f
Dirks, J. F., Robinson, S. K., and Dirks, D. L. (1981). Alexithymia and the psychomaintenance of bronchial asthma. Psychother. Psychosom. 36, 63–71. doi: 10.1159/000287527
Eikeseth, F. F., Sætren, S. S., Benjamin, B. R., Ulltveit-Moe Eikenæs, I., Sütterlin, S., and Hummelen, B. (2020). The test-retest reliability of heart rate variability and its association with personality functioning. Front. Psych. 11, 1–8. doi: 10.3389/fpsyt.2020.558145
Feiguine, R. J., Hulihan, D. M., and Kinsman, R. A. (1982). Alexithymic asthmatics: age and alexithymia across the life span. Psychother. Psychosom. 37, 185–188. doi: 10.1159/000287571
Feldman, J. M., Lehrer, P. M., and Hochron, S. M. (2002). The predictive value of the Toronto alexithymia scale among patients with asthma. J. Psychosom. Res. 53, 1049–1052. doi: 10.1016/s0022-3999(02)00452-x
Founta, O., Adamzik, K., Tobin, A. M., Kirby, B., and Hevey, D. (2019). Psychological distress, alexithymia and alcohol misuse in patients with psoriasis: a cross-sectional study. J. Clin. Psychol. Med. Settings 26, 200–219. doi: 10.1007/s10880-018-9580-9
Franz, M., Popp, K., Schaefer, R., Sitte, W., Schneider, C., Hardt, J., et al. (2008). Alexithymia in the German general population. Soc. Psychiatry Psychiatr. Epidemiol. 43, 54–62. doi: 10.1007/s00127-007-0265-1
Franz, M., Schneider, C., Schäfer, R., Schmitz, N., and Zweyer, K. (2001). Factoral structure and psychometric properties of the German version of the Toronto alexithymia scale (TAS-20) in psychosomatic patients. Psychother. Psychosom. Med. Psychol. 51, 48–55. doi: 10.1055/s-2001-10755
GBD 2019 Diseases and Injuries Collaborators (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet (London, England) 396, 1204–1222. doi: 10.1016/S0140-6736(20)30925-9
Ghorbani, F., Khosravani, V., Ardakani, R. J., Alvani, A., and Akbari, H. (2017). The mediating effects of cognitive emotion regulation strategies on the relationship between alexithymia and physical symptoms: evidence from Iranian asthmatic patients. Psychiatry Res. 247, 144–151. doi: 10.1016/j.psychres.2016.11.015
Global Initiative for Asthma . (2022). Global strategy for asthma management and prevention, (2022). Available at: https://www.ginasthma.org/
Goerlich, K. S. (2018). The multifaceted nature of alexithymia—a neuroscientific perspective. Front. Psychol. 9:1614. doi: 10.3389/fpsyg.2018.01614
Hogeveen, J., and Grafman, J. (2021). Alexithymia. Handb. Clin. Neurol. 183, 47–62. doi: 10.1016/B978-0-12-822290-4.00004-9
Holmes, A., Marella, P., Rodriguez, C., Glass Ii, D., and Goerlich, K. S. (2022). Alexithymia and cutaneous disease morbidity: a systematic review. Dermatology (Basel, Switzerland) 238, 1120–1129. doi: 10.1159/000524736
Horne, R., Price, D., Cleland, J., Costa, R., Covey, D., Gruffydd-Jones, K., et al. (2007). Can asthma control be improved by understanding the patient’s perspective? BMC Pulm. Med. 7:8. doi: 10.1186/1471-2466-7-8
Hsiao, H.-P., Lin, M.-C., Wu, C.-C., Wang, C.-C., and Wang, T.-N. (2019). Sex-specific asthma phenotypes, inflammatory patterns, and asthma control in a cluster analysis. The journal of allergy and clinical immunology. In Pract. 7, 556–567.e15. doi: 10.1016/j.jaip.2018.08.008
Innamorati, M., Chetta, A., Antonucci, C., Bettini, E., Aiello, M., Montali, A., et al. (2015). Alexithymia and self-reflectiveness in bronchial asthma. Riv. Psichiatr. 50, 245–252. doi: 10.1708/2040.22168
Isvoranu, A.-M., Abdin, E., Chong, S. A., Vaingankar, J., Borsboom, D., and Subramaniam, M. (2021). Extended network analysis: from psychopathology to chronic illness. BMC Psychiatry 21:119. doi: 10.1186/s12888-021-03128-y
Kano, M., Endo, Y., and Fukudo, S. (2018). Association between alexithymia and functional gastrointestinal disorders. Front. Psychol. 9:599. doi: 10.3389/fpsyg.2018.00599
Kano, M., and Fukudo, S. (2013). The alexithymic brain: the neural pathways linking alexithymia to physical disorders. BioPsychoSocial medicine 7:1. doi: 10.1186/1751-0759-7-1
Kaptein, A. A., Klok, T., Moss-Morris, R., and Brand, P. L. (2010). Illness perceptions: impact on self-management and control in asthma. Curr. Opin. Allergy Clin. Immunol. 10, 194–199. doi: 10.1097/ACI.0b013e32833950c1
Khosravani, V., Alvani, A., Sharifi Bastan, F., Jamaati Ardakani, R., and Akbari, H. (2016). The alexithymia, cognitive emotion regulation, and physical symptoms in Iranian asthmatic patients. Personal. Individ. Differ. 101, 214–219. Scopus. doi: 10.1016/j.paid.2016.05.364
Khosravani, V., Samimi Ardestani, S. M., Alvani, A., and Amirinezhad, A. (2020). Alexithymia, empathy, negative affect and physical symptoms in patients with asthma. Clin. Psychol. Psychother. 27, 736–748. doi: 10.1002/cpp.2458
Kirchner, K., Brauer, H., Van der Auwera, S., and Grabe, H. J. (2022). The impact of resilience, alexithymia and subjectively perceived helplessness of myocardial infarction on the risk of posttraumatic stress. J. Clin. Psychol. Med. Settings 29, 954–962. doi: 10.1007/s10880-022-09857-w
Kleiger, J. H., and Dirks, J. F. (1980). Psychomaintenance aspects of alexithymia: relationship to medical outcome variables in a chronic respiratory illness population. Psychother. Psychosom. 34, 25–33. doi: 10.1159/000287443
Kleiger, J. H., and Jones, N. F. (1980). Characteristics of alexithymic patients in a chronic respiratory illness population. J. Nerv. Ment. Dis. 168, 465–470. doi: 10.1097/00005053-198008000-00003
Kleiger, J. H., and Kinsman, R. A. (1980). The development of an MMPI alexithymia scale. Psychot. Psychos. 34, 17–24. doi: 10.1159/000287442
Kojima, M. (2012). Alexithymia as a prognostic risk factor for health problems: a brief review of epidemiological studies. BioPsychoSocial Med. 6, 21–29. doi: 10.1186/1751-0759-6-21
Kojima, M., Hayano, J., Suzuki, S., Seno, H., Kasuga, H., Takahashi, H., et al. (2010). Depression, alexithymia and long-term mortality in chronic hemodialysis patients. Psychother. Psychosom. 79, 303–311. doi: 10.1159/000319311
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P., et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann. Intern. Med. 151:W-65. doi: 10.1371/journal.pmed.1000100
Lin, P., Li, X., Liang, Z., and Wang, T. (2022). Association between depression and mortality in persons with asthma: a population-based cohort study. Allergy Asthma Clin. Immunol. 18, 29–27. doi: 10.1186/s13223-022-00672-4
Liotta, M., Liotta, M., Saitta, S., and Ricciardi, L. (2021). Severe allergic asthma: does alexithymia interfere with omalizumab treatment outcome? Asian Pacific J Allergy Immunol. doi: 10.12932/AP-040121-1031
López-Muñoz, F., and Pérez-Fernández, F. (2020). A history of the alexithymia concept and its explanatory models: an epistemological perspective. Front. Psych. 10:1026. doi: 10.3389/fpsyt.2019.01026
López-Tiro, J., Contreras-Contreras, A., Rodríguez-Arellano, M. E., and Costa-Urrutia, P. (2022). Economic burden of severe asthma treatment: a real-life study. World Allergy Organ. J. 15:100662. doi: 10.1016/j.waojou.2022.100662
Louis, G., Schleich, F., Louis, R., Guillaume, M., Sousa-Pinto, B., Bousquet, J., et al. (2023). How respiratory symptoms impact asthma-related quality of life in mild asthmatics. Respir. Med. 207:107098. doi: 10.1016/j.rmed.2022.107098
Lumley, M. A., Beyer, J., and Radcliffe, A. (2008). “Alexithymia and physical health problems: a critique of potential pathways and a research agenda” in Emotion Regulation: Conceptual and Clinical Issues. eds. A. Vingerhoets, I. Nyklíček, and J. Denollet (Berlin: Springer Science + Business Media), 43–68.
Mambou Nouemssi, J. P., Dumet, N., and Fotso Djemo, J. B. (2021). Operative thinking, alexithymia, feeling and expression of the theme of persecution. Mediterranean. J. Clin. Psychol. 9, 1–35. doi: 10.6092/2282-1619/mjcp-2920
Marchi, L., Marzetti, F., Orrù, G., Lemmetti, S., Miccoli, M., Ciacchini, R., et al. (2019). Alexithymia and psychological distress in patients with fibromyalgia and rheumatic disease. Front. Psychol. 10:1735. doi: 10.3389/fpsyg.2019.01735
Martin, J. B., Pihl, R. O., and Dobkin, P. (1984). Schalling-Sifneos personality scale: findings and recommendations. Psychother. Psychosom. 41, 145–152. doi: 10.1159/000287802
Martínez-Rivera, C., Vennera, M. d. C., Cañete, C., Bardagí, S., and Picado, C. (2011). Psychological profile of patients with bronchial asthma and functional dyspnea: a comparison with a non-asthmatic population and impact on the disease. Archivos De Bronconeumologia 47, 73–78. doi: 10.1016/j.arbres.2010.10.003
Martino, G., Caputo, A., Schwarz, P., Bellone, F., Fries, W., Quattropani, M. C., et al. (2020a). Alexithymia and inflammatory bowel disease: a systematic review. Front. Psychol. 11:1763. doi: 10.3389/fpsyg.2020.01763
Martino, G., Caputo, A., Vicario, C. M., Catalano, A., Schwarz, P., and Quattropani, M. C. (2020b). The relationship between alexithymia and type 2 diabetes: a systematic review. Front. Psychol. 11:2026. doi: 10.3389/fpsyg.2020.02026
Martino, G., Langher, V., Cazzato, V., and Vicario, C. M. (2019). Psychological factors as determinants of medical conditions. Front. Psychol. 10:2502. doi: 10.3389/fpsyg.2019.02502
Marty, P., and de M'uzan, M. (1978). Das operative Denken ("Pensée opératoire") [Operative thinking (pensée opératoire)]. Psyche 32, 974–984.
Merlo, E. M. (2019). Opinion article: the role of psychological features in chronic diseases, advancements and perspectives. Mediterranean J. Clin. Psychol. 7, 1–6. doi: 10.6092/2282-1619/2019.7.2341
Moes-Wójtowicz, A., Wójtowicz, P., Postek, M., and Domagała-Kulawik, J. (2012). Asthma as a psychosomatic disease. The causes, scale of the problem, connection with alexithymia and asthma control. Pneumonol. Alergol. Pol. 80, 13–19. doi: 10.5603/ARM.27612
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 151, 264–W64. doi: 10.7326/0003-4819-151-4-200908180-00135
Mortimer, K., Lesosky, M., García-Marcos, L., Asher, M. I., Pearce, N., Ellwood, E., et al. (2022). The burden of asthma, hay fever and eczema in adults in 17 countries: GAN phase I study. Eur. Respir. J. 60:2102865. doi: 10.1183/13993003.02865-2021
Myles, L. A. M., and Merlo, E. M. (2021). Alexithymia and physical outcomes in psychosomatic subjects: a cross-sectional study. J. Mind Med. Sci. 8, 86–93. doi: 10.22543/7674.81.P8693
Nakao, M., and Takeuchi, T. (2018). Alexithymia and somatosensory amplification link perceived psychosocial stress and somatic symptoms in outpatients with psychosomatic illness. J. Clin. Med. 7:112. doi: 10.3390/jcm7050112
Namdar, N. D., and Kurtoglu, Y. (2021). Alexithymia, anxiety, and depression in patients with vitiligo. Ann. Med. Res. 28, 663–667. doi: 10.5455/annalsmedres.2020.06.581
Nekouei, Z. K., Doost, H. T. N., Yousefy, A., Manshaee, G., and Sadeghei, M. (2014). The relationship of alexithymia with anxiety-depression-stress, quality of life, and social support in coronary heart disease (a psychological model). J. Educ. Health Promot. 3:68. doi: 10.4103/2277-9531.134816
Nemiah, J. C., and Sifneos, P. E. (1970). Psychosomatic illness: a problem in communication. Psychother. Psychosom. 18, 154–160. doi: 10.1159/000286074
Nielsen, T., Ouellet, L., Warnes, H., Cartier, A., Malo, J. L., and Montplaisir, J. (1997). Alexithymia and impoverished dream recall in asthmatic patients: evidence from self-report measures. J. Psychosom. Res. 42, 53–59. doi: 10.1016/s0022-3999(96)00230-9
Nunes da Silva, A. (2021). Developing emotional skills and the therapeutic Alliance in clients with alexithymia: intervention guidelines. Psychopathology 54, 282–290. doi: 10.1159/000519786
Nunes, C., Pereira, A. M., and Morais-Almeida, M. (2017). Asthma costs and social impact. Asthma Res. Pract. 3:1. doi: 10.1186/s40733-016-0029-3
Padem, N., and Saltoun, C. (2019). Classification of asthma. Allergy Asthma Proc. 40, 385–388. doi: 10.2500/aap.2019.40.4253
Panasiti, M. S., Ponsi, G., and Violani, C. (2020). Emotions, alexithymia, and emotion regulation in patients with psoriasis. Front. Psychol. 11:836. doi: 10.3389/fpsyg.2020.00836
Panayiotou, G. (2018). “Alexithymia as a Core trait in psychosomatic and other psychological disorders” in Somatoform and Other Psychosomatic Disorders. eds. C. Charis and G. Panayiotou (Cham: Springer)
Papi, A., Blasi, F., Canonica, G. W., Morandi, L., Richeldi, L., and Rossi, A. (2020). Treatment strategies for asthma: reshaping the concept of asthma management. Allergy, Asthma Clin. Immunol. 16:75. doi: 10.1186/s13223-020-00472-8
Parker, J. D. A., Taylor, G. J., and Bagby, R. M. (2003). The 20-item Toronto alexithymia scale. III. Reliability and factorial validity in a community population. J. Psychosom. Res. 55, 269–275. doi: 10.1016/s0022-3999(02)00578-0
Pirlot, G., and Corcos, M. (2012). Understanding alexithymia within a psychoanalytical framework (S. Leighton, Trans.). Int. J. Psychoanal. 93, 1403–1425. doi: 10.1111/j.1745-8315.2012.00657.x
Plaza, V., Giner, J., Picado, C., Sureda, B., Serrano, J., Casan, P., et al. (2006). Control of ventilation, breathlessness perception and alexithymia in near-fatal asthma. J. Asthma 43, 639–644. doi: 10.1080/02770900600878990
Sagar, R., Talwar, S., Desai, G., and Chaturvedi, S. K. (2021). Relationship between alexithymia and depression: a narrative review. Indian J. Psychiatry 63, 127–133. doi: 10.4103/psychiatry.IndianJPsychiatry_738_19
Schmid-Gloor, E. (2019). “Psychosomatic investigation and treatment” in Experiencing the Body (Oxfordshire: Routledge), 73–82.
Selinheimo, S., Jokela, M., Vasankari, T., Kanervisto, M., Pirkola, S., Suvisaari, J., et al. (2022). Poor respiratory health outcomes associated with high illness worry and alexithymia: eleven-year prospective cohort study among the working-age population. J. Psychosom. Res. 155:110751. doi: 10.1016/j.jpsychores.2022.110751
Serrano, J., Plaza, V., Sureda, B., de Pablo, J., Picado, C., Bardagí, S., et al. (2006). Alexithymia: a relevant psychological variable in near-fatal asthma. Eur. Respir. J. 28, 296–302. doi: 10.1183/09031936.06.00008105
Sifneos, P. E. (1973). The prevalence of ‘alexithymic’ characteristics in psychosomatic patients. Psychot. psychos. 22, 255–262. doi: 10.1159/000286529
Sifneos, P. E. (2000). Alexithymia, clinical issues, politics and crime. Psychother. Psychosom. 69, 113–116. doi: 10.1159/000012377
Smyth, J. M., Anderson, C. F., Hockemeyer, J. R., and Stone, A. A. (2002). Does emotional non-expressiveness or avoidance interfere with writing about stressful life events? An analysis in patients with chronic illness. Psychol. Health 17, 561–569. Scopus. doi: 10.1080/08870440290025777
Stanescu, S., Kirby, S. E., Thomas, M., Yardley, L., and Ainsworth, B. (2019). A systematic review of psychological, physical health factors, and quality of life in adult asthma. NPJ Primary Care Respir. Med. 29:1. doi: 10.1038/s41533-019-0149-3
Talamonti, M., Galluzzo, M., Silvaggio, D., Lombardo, P., Tartaglia, C., and Bianchi, L. (2021). Quality of life and psychological impact in patients with atopic dermatitis. J. Clin. Med. 10:1298. doi: 10.3390/jcm10061298
Tang, F.-Y., Xiong, Q., Gan, T., Yuan, L., Liao, Q., and Yu, Y.-F. (2022). The prevalence of alexithymia in psoriasis: a systematic review and meta-analysis. J. Psychosom. Res. 161:111017. doi: 10.1016/j.jpsychores.2022.111017
Taylor, G. J., Bagby, R. M., and Parker, J. D. A. (1997). Disorders of Affect Regulation: Alexithymia in Medical and Psychiatric Illness. Cambridge: Cambridge University Press.
Taylor, G. J., Ryan, D., and Bagby, R. M. (1985). Toward the development of a new self-report alexithymia scale. Psychother. Psychosom. 44, 191–199. doi: 10.1159/000287912
Tesio, V., Di Tella, M., Ghiggia, A., Romeo, A., Colonna, F., Fusaro, E., et al. (2018). Alexithymia and depression affect quality of life in patients with chronic pain: a study on 205 patients with fibromyalgia. Front. Psychol. 9:442. doi: 10.3389/fpsyg.2018.00442
Tesio, V., Goerlich, K. S., Hosoi, M., and Castelli, L. (2019). Editorial: alexithymia: state of the art and controversies. Clin. Neuroscientific Evidence Front. Psychol. 10, 1–3. doi: 10.3389/fpsyg.2019.01209
Torres, S., Guerra, M. P., Miller, K., Costa, P., Cruz, I., Vieira, F. M., et al. (2019). Factorial validity of the Toronto alexithymia scale (TAS-20) in clinical samples: a critical examination of the literature and a psychometric study in anorexia nervosa. J. Clin. Psychol. Med. Settings 26, 33–46. doi: 10.1007/s10880-018-9562-y
Tselebis, A., Kosmas, E., Bratis, D., Moussas, G., Karkanias, A., Ilias, I., et al. (2010). Prevalence of alexithymia and its association with anxiety and depression in a sample of Greek chronic obstructive pulmonary disease (COPD) outpatients. Ann. General Psychiatry 9:16. doi: 10.1186/1744-859X-9-16
Uchmanowicz, B., Panaszek, B., Uchmanowicz, I., and Rosińczuk, J. (2016). Sociodemographic factors affecting the quality of life of patients with asthma. Patient Prefer. Adherence 10, 345–354. doi: 10.2147/PPA.S101898
Vadini, F., Sozio, F., Madeddu, G., De Socio, G., Maggi, P., Nunnari, G., et al. (2019). Alexithymia predicts carotid atherosclerosis, vascular events, and all-cause mortality in human immunodeficiency virus-infected patients: an Italian multisite prospective cohort study. Open Forum Infect. Dis. 6:ofz331. doi: 10.1093/ofid/ofz331
Van Lieshout, R. J., and MacQueen, G. (2008). Psychological factors in asthma. Allergy Asthma Clin. Immunol. 4, 12–28. doi: 10.1186/1710-1492-4-1-12
Vanegas, E., Felix, M., Ramon, G. D., López Jove, O., Matos Benavides, E. E., Tinoco-Morán, I., et al. (2020). Influence of alexithymia on the management of Latin American patients with asthma: a cross-sectional study. SAGE Open Med. 8:2050312120930913. doi: 10.1177/2050312120930913
Vázquez, I., Romero-Frais, E., Blanco-Aparicio, M., Seoane, G., Otero, I., Rodríguez-Valcarcel, M. L., et al. (2010a). Psychological and self-management factors in near-fatal asthma. J. Psychosom. Res. 68, 175–181. doi: 10.1016/j.jpsychores.2009.04.012
Vazquez, I., Sández, E., González-Freire, B., Romero-Frais, E., Blanco-Aparicio, M., and Verea-Hernando, H. (2010b). The role of alexithymia in quality of life and health care use in asthma. J. Asthma 47, 797–804. doi: 10.3109/02770900903560217
Vliet, E. C.-V., Kelly-McNeil, K., Natelson, B., Kipen, H., and Fiedler, N. (2002). Anxiety sensitivity and depression in multiple chemical sensitivities and asthma. J. Occup. Environ. Med. 44, 890–901. doi: 10.1097/00043764-200210000-00006
Wang, X., Li, X., Guo, C., Hu, Y., Xia, L., Geng, F., et al. (2021). Prevalence and correlates of alexithymia and its relationship with life events in Chinese adolescents with depression during the COVID-19 pandemic. Front. Psych. 12:774952. doi: 10.3389/fpsyt.2021.774952
Wise, T. N., Simpson, N., and Sheridan, M. J. (2000). Comparison of 26-item and 20-item versions of the Toronto alexithymia scale for psychiatric outpatients. Psychol. Rep. 87, 127–132. doi: 10.2466/pr0.2000.87.1.127
World Health Organization . (2019). International statistical classification of diseases and related health problems (11th ed.). Available at: https://icd.who.int/
Ye, G., Baldwin, D. S., and Hou, R. (2021). Anxiety in asthma: a systematic review and meta-analysis. Psychol. Med. 51, 11–20. doi: 10.1017/S0033291720005097
Zhang, H., Wang, Y., Lou, H., Zhu, Y., Dong, Z., Dong, D., et al. (2023). Prevalence of and factors associated with alexithymia among patients with chronic obstructive pulmonary disease in China: a cross-sectional study. BMC Pulm. Med. 23:40. doi: 10.1186/s12890-023-02335-5
Keywords: alexithymia, asthma, psychosomatic disorders, psychological distress, chronic disease, clinical psychology
Citation: Silvestro O, Ricciardi L, Catalano A, Vicario CM, Tomaiuolo F, Pioggia G, Squadrito G, Schwarz P, Gangemi S and Martino G (2023) Alexithymia and asthma: a systematic review. Front. Psychol. 14:1221648. doi: 10.3389/fpsyg.2023.1221648
Edited by:
Mariagrazia Di Giuseppe, University of Rome Tor Vergata, ItalyReviewed by:
Alessandro Alberto Rossi, University of Padua, ItalyGiada Pietrabissa, Catholic University of the Sacred Heart, Italy
Copyright © 2023 Silvestro, Ricciardi, Catalano, Vicario, Tomaiuolo, Pioggia, Squadrito, Schwarz, Gangemi and Martino. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriella Martino, bWFydGlub2dAdW5pbWUuaXQ=
 Orlando Silvestro
Orlando Silvestro Luisa Ricciardi
Luisa Ricciardi Antonino Catalano
Antonino Catalano Carmelo Mario Vicario
Carmelo Mario Vicario Francesco Tomaiuolo
Francesco Tomaiuolo Giovanni Pioggia
Giovanni Pioggia Giovanni Squadrito2
Giovanni Squadrito2 Peter Schwarz
Peter Schwarz Sebastiano Gangemi
Sebastiano Gangemi Gabriella Martino
Gabriella Martino