
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 02 June 2023
Sec. Psychology of Aging
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1172552
This article is part of the Research Topic Highlights in Psychology of Aging: Impact of the Covid-19 Pandemic on Older Adults View all 9 articles
Objectives: Loneliness is a major public health concern. Duration of loneliness is associated with severity of health outcomes, and further research is needed to direct interventions and social policy. This study aimed to identify predictors of the onset vs. the maintenance of loneliness in older adults before and during the pandemic using longitudinal data from the Survey of Health, Age, and Retirement in Europe (SHARE).
Methods: Groupings of persistent, situational, and no loneliness were based on self-reports from an ordinary pre-pandemic SHARE wave and a peri-pandemic telephone interview. Predictors were identified and compared in three hierarchical binary regression analyses, with independent variables added in blocks of geographic region, demographics, pre-pandemic social network, pre-pandemic health, pandemic-related individual, and country level variables.
Results: Self-reported loneliness levels for the persistent, situational, and no loneliness groups were stable and distinct through 7 years preceding the pre-pandemic baseline measure. Shared predictors were chronic diseases, female sex, depression, and no cohabitant partner. Persistent loneliness was uniquely predicted by low network satisfaction (OR: 2.04), functional limitations (OR: 1.40), and a longer country-level isolation period for older adults (OR: 1.24).
Conclusion: Interventions may target persons with depression, functional limitations, chronic health issues, and no cohabitant partner. The added burden of the length of isolation on those who are already lonely should be taken into account when employing social policies that target older adults. Further research should distinguish between situational and persistent loneliness, and seek to identify predictors of chronic loneliness onset.
As lockdowns and social distancing measures were employed in order to contain the spread of COVID-19, the alarm of a potential “loneliness pandemic” was raised (Armitage and Nellums, 2020; Killgore et al., 2020; Wu, 2020; Laranjeira, 2021). Pandemic-related restrictions have a direct effect on social isolation, defined as the objectively measured absence of social contacts, relationships, or activities (e.g., Davies et al., 2021). Loneliness is a related but distinct construct referring to the subjective experience stemming from the actual or perceived absence of social relationships that serve to meet basic emotional needs (Park et al., 2020; Quadt et al., 2020). While social isolation and loneliness do not necessarily co-occur (Park et al., 2020), a recent meta-analysis of 24 longitudinal studies found a small but significant increase in loneliness since before the outbreak of COVID-19 (Ernst et al., 2022). Loneliness is a unique risk factor for heightened mortality risk (Holt-Lunstad et al., 2015; Rico-Uribe et al., 2018) and is associated with a number of adverse health outcomes including depression (Quadt et al., 2020), cardiovascular disease (Lim et al., 2020; Park et al., 2020), and dementia (Rawtaer et al., 2017; Lara et al., 2019; Lee et al., 2022; Salinas et al., 2022). The older adult population, being simultaneously vulnerable to COVID-19 infection, subjective loneliness, and cognitive decline, has been identified as a particular risk group (Lara et al., 2019; Luchetti et al., 2020; Atzendorf and Gruber, 2021; Piolatto et al., 2022).
Identification of concomitants and modifiable risk factors of loneliness is an important step toward developing effective interventions targeting relevant risk groups. In cross-sectional and longitudinal research, a large number of variables have been identified as correlates or risk factors of loneliness. Among adults over 50 years of age, higher prevalence of loneliness has been found with advancing age (Yang and Victor, 2011). Lower education level, migrant status, and living in a nursing home or a rural rather than an urban area have also been associated with higher levels of loneliness (Cohen-Mansfield et al., 2016; Vozikaki et al., 2018; Lim et al., 2020), and a larger incidence of loneliness has been found among individuals suffering from physical and mental conditions (Cacioppo and Hawkley, 2009; Kim et al., 2020; Park et al., 2020), including alcohol abuse (Åkerlind and Hörnquist, 1992). While loneliness is a known risk factor for, or prodrome of, cognitive impairment (Rawtaer et al., 2017; Lara et al., 2019; Lee et al., 2022; Salinas et al., 2022), cognitive decline may simultaneously increase the risk of social isolation and loneliness over time (Hackett et al., 2019). So far, cognitive impairment has been understudied as a risk factor for loneliness (Dahlberg et al., 2022).
Despite the large number of correlates and risk factors identified, a recent review of longitudinal studies by Dahlberg et al. (2022) found that only a few risk factors have been consistently related to loneliness in multivariate analyses in older adult samples, describing the evidence base as “broad but shallow.” Consistent associations were found for not being married or partnered, having a limited social network, low social activity level, poor self-rated health, and depression. While representing distinct entities, depression and loneliness often co-occur and may exacerbate each other over time (Luanaigh and Lawlor, 2008). Dahlberg et al. (2022) found that female sex was only significant in bivariate analyses, and concluded that this relationship may be mediated by other factors more commonly seen in females, such as widowhood.
Crucially, loneliness has been characterized as equally state–and trait-like (Mund et al., 2020a,b). The short-term, state-dependent, dynamic component of loneliness has been termed situational or transient loneliness, while the temporally stable trait component has been referred to as chronic or persistent loneliness. To date, clear definitions and distinctions between the terms situational and transient, as well as chronic and persistent, are lacking, and we will therefore use them interchangeably. The differentiation of persistent from transient loneliness is important because chronic loneliness is associated with worse health outcomes compared to short-term loneliness (Cacioppo and Hawkley, 2009; Cacioppo and Cacioppo, 2018; Martín-María et al., 2020). For older adults, persistent loneliness is associated with greater cognitive decline (Zhong et al., 2016), higher risk of dementia onset (Akhter-Khan et al., 2021), more frailty (Chu and Zhang, 2022), and higher mortality rates (Shiovitz-Ezra and Ayalon, 2010). This is in line with conceptual models portraying loneliness as a complex biopsychosocial process (Qualter et al., 2015; Cacioppo and Cacioppo, 2018). While state loneliness is common and may be adaptive by preventing damage to the “social body,” these models link duration of loneliness to severity of health outcomes through “wear and tear” by hypervigilance to social threats, avoidance, and maladaptive thought patterns leading to an allostatic overload (Quadt et al., 2020). In 2022, the Tackling Loneliness Evidence Group of the United Kingdom Department for Digital, Culture, Media and Sport (DCMS) published a report stating the need for a clear distinction between transient and chronic loneliness (McDaid et al., 2022), highlighting the need for further research into whether the predictors of transient and chronic loneliness are shared or distinct. Although one paper (Yang, 2018) reported largely similar risk factors for situational and persistent loneliness, research on this topic has been sparse.
While studies of general loneliness in the COVID-19 pandemic have not identified any pandemic-specific risk or protective factors (Buecker and Horstmann, 2021), they do not control for the fact that a portion of participants likely experienced chronic loneliness already before the pandemic. In addition, studying the effects of country-level pandemic-related factors, such as social policies, requires large surveys with cross-country data, perhaps explaining why this has not been widely done. In one paper by Atzendorf and Gruber (2021), self-rated increase of depression and sadness, but not loneliness, was more common in countries with a higher number of COVID-19 related deaths per million inhabitants, as well as more stringent socially restrictive measures.
To date, many studies have focused on general levels of loneliness in response to the COVID-19 pandemic, as reviewed by Buecker and Horstmann (2021), Ernst et al. (2022), and Lazzari and Rabottini (2022). We extend this research by focusing on duration of loneliness, distinguishing between the risk and protective factors for developing, or maintaining, feelings of loneliness. We hypothesize that loneliness measured during the pandemic captures both recent onset (situational) and long-term (persistent) loneliness, and that there are distinct predictors for loneliness onset and maintenance. Using longitudinal interview data from the cross-national Survey of Health, Aging and Retirement in Europe (Börsch-Supan et al., 2013), we aim to identify pre-pandemic and pandemic-specific predictors of peri-pandemic loneliness onset and maintenance in older adults. We account for the simultaneous measurement of both state and trait loneliness by dividing the sample into groups based on pre-pandemic loneliness levels. Using weighted hierarchical logistic regression analyses, we investigate effects of commonly studied factors added in blocks. The design allows us to evaluate unique first order effects of each predictor candidate, while controlling for other potentially influential factors including geographic region and residential area, age, sex, cohabitation, widowhood, education, cognitive and mental health, social isolation, and network satisfaction. We also include national and individual pandemic-specific measures, such as COVID-19 deaths per million inhabitants, length of recommended or required self-isolation period for older adults, frequency of personal contact with others, and leaving home since the start of the pandemic.
The sample comprised older adults from 26 European countries and Israel, participating in SHARE before and during the COVID-19 pandemic. The sample was limited to participants taking part in the 8th regular SHARE wave interview, between October 2019 and March 2020 (Bergmann and Börsch-Supan, 2021; Börsch-Supan, 2022g), and a peri-pandemic telephone interview (SHARE Corona Survey; SCS) conducted 3–10 months later, between June and August 2020 (Scherpenzeel et al., 2020; Börsch-Supan, 2022h), N = 56 689. Participants were included if they also had cognitive test data from at least two waves including Wave 8 (N = 32 321), were above 50 years of age upon entering SHARE (N = 31 236), and had no missing pre–and peri-pandemic loneliness data (N = 31 148). Participants with an interval of more than 10 months between Wave 8 and the SCS (N = 1), who reported having been hospitalized or tested positive for COVID-19 (N = 155), and/or did not have a calibrated inverse probability weight for being part of the SCS subsample (N = 4) were excluded. Weights are provided as part of the SCS dataset (Scherpenzeel et al., 2020; Börsch-Supan, 2022h) and detailed information about the weights can be found in the SHARE Wave 8 and Corona Survey methodology documentation (De Luca et al., 2022; De Luca and Li Donni, 2022). The final sample consisted of participants who also fit into any of the three longitudinal loneliness groups of interest defined: (1) onset of loneliness from before to after the outbreak of COVID-19, (2) stable loneliness levels at both time points, and (3) no peri-pandemic loneliness (N = 30 245). Data from the same sample in SHARE waves 1–2 and 4–7 (Gruber et al., 2014; Bergmann et al., 2019; Börsch-Supan, 2022a,b,c,d,e,f), and a second SCS, conducted in June–August 2021 (Börsch-Supan, 2022i), was also used. For an overview of the SHARE time points, loneliness measures and groupings used in this study, see Figure 1.

Figure 1. Timeline with overview of time points, available loneliness measures, and definition of loneliness groups used in the study. Three assessments of loneliness are available: 1. A single-item question asking about current loneliness, 2. A three item loneliness rating scale, 3. A single-item retrospective change question. Loneliness groupings were derived from the single-item current loneliness because it was asked at every wave and the SCSs. *Wave 6 data collection in Netherlands ended in 2016.
SHARE data was supplemented with country-level pandemic-related data from the Oxford Coronavirus Government Response Tracker (OxCGRT; Hale et al., 2021, retrieved on 7th December 2021) and the COVID-19 Data Repository by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (Dong et al., 2020, retrieved on 2nd Feburary 2022).
Loneliness was measured using a single item asking participants to rate the general frequency with which they experienced feelings of loneliness on a three-point scale (often / some of the time / hardly ever or never), and defined as reporting feeling lonely at least some of the time. Based on this dichotomous loneliness measure, three groups were defined based on loneliness levels before (Wave 8) and during the pandemic (in the SCS): situational loneliness, persistent loneliness, and no loneliness. Situational loneliness (onset) was defined as no loneliness before the pandemic (in Wave 8), and loneliness during the pandemic (in the SCS). Note, due to the lack of a follow-up measure, we refer to this as situational rather than transient loneliness. Persistent loneliness (maintenance) was defined as identical loneliness ratings before and during the pandemic. Due to the relatively short time in between the measures, this is referred to as persistent rather than chronic loneliness. The third group did not report feeling lonely during the pandemic. Groups defined using the single-item measure were validated using scores on the Three-Item Loneliness Scale (Hughes et al., 2004), a short version of the Revised UCLA Loneliness Scale (Russell et al., 1980) that was used in SHARE waves 5–8. Both measures have been shown to be reliable and valid measures of loneliness and show good convergent validity (Mund et al., 2022).
In the SCS, participants who reported feeling lonely at least some of the time were asked to rate loneliness change since the outbreak of COVID-19 (“Has that been more so, less so or about the same as before the outbreak of Corona?”), and this data was used to compare self-rated retrospective loneliness increase to single-item longitudinal loneliness increase from Wave 8 to the SCS.
European countries were grouped into regions according to the United Nations geoscheme for Europe (United Nations, 2021), and Israel was treated as a distinct region. Western European countries were Austria, Belgium, France, Germany, Luxembourg, Netherlands, and Switzerland. Northern European countries were Denmark, Estonia, Finland, and Sweden. Eastern European countries were Bulgaria, Czech Republic, Hungary, Latvia, Lithuania, Poland, Romania, and Slovakia. Southern Europe countries were Cyprus, Croatia, Greece, Italy, Malta, Slovenia, and Spain. For all participants, country of residence stayed the same from Wave 8 to the SCS.
Demographic variables included age in years, sex, migrant status, and nursing home residence. The 1997 International Standard Classification of Education (ISCED-97; United Nations Educational, Scientific and Cultural Organization [UNESCO], 2003) education level was trichotomized into less than upper secondary education, upper secondary including post-secondary non-tertiary education, and tertiary education. Area of residence was also trichotomized, comprising big city, large town or suburb, and small town or village. All demographic variables were measured at Wave 8, except for education level which was measures in each participant’s baseline wave, and age which was determined from the timepoint of the SCS, measured between March 3rd and July 31st 2020.
Network size was defined as the number of persons that the participant listed in response to the interviewer asking who they have most often discussed important things during the past year (range 0–7), trichotomized into small network (0–1), medium network (2–3), and large network (4–7). Network satisfaction was measured by a single item asking participants how satisfied they were with their reported social network, on a scale from 0 to 10 (completely dissatisfied to completely satisfied). Low network satisfaction was defined as a rating below 8, capturing the bottom quartile of the population. Engagement in social activities was measured by four questions asking the participant how often they had done voluntary/charity work, attended an educational or training course, gone to a sport/social/other kind of club, or taken part in a political/community-related organization during the past year (almost daily, almost every week, almost every month, or less often). Not partaking in social activities was defined as not engaging in any of the activities with a frequency of at least “almost every week” during the past year. Further social network variables of interest were cohabiting with a partner (yes/no), widower status (yes/no), and having children (yes/no). All social network variables were measured or updated in Wave 8.
Self-reported dichotomous health measures were two or more chronic diseases, limitations with at least one of seven Instrumental Activities of Daily Living (IADL; Lawton and Brody, 1969; Steel et al., 2002), engaging in vigorous activities such as sports, heavy housework, or a job that involves physical labor less than once a month, and having six or more alcoholic drinks at least three times per week. Body Mass Index (Quetelet, 1832) was trichotomized using the standard categories defined by the World Health Organization (World Health Organization [WHO], 1995): underweight (< 18.5), normal, and overweight (≥25). Depression was defined as a score above the cut off on the EURO-D depression scale (Prince et al., 1999; ≥4 points). A cognitive function sum score was computed using immediate and delayed word recall tests of verbal learning and memory, and a serial sevens subtraction test of working memory. Cognitive impairment was defined as a cognitive function sum score at least one standard deviation below the country mean at Wave 8, in combination with longitudinal decline (negative word recall slope across at least two time points, measured in Wave 8, and at least one previous wave). All other health variables were measured at Wave 8. Computation and validation of the cognitive impairment variable is detailed in Supplementary material.
Pandemic-related country-level variables were the number of COVID-19 attributed deaths per million inhabitants, and number of months where extensive restrictions were in place in long term care facilities, and/or all older individuals were required to stay at home and not leave the home with minimal exceptions, and receive no external visitors (Phillips and Tatlow, 2021). Individual-level pandemic variables were reporting seldom having personal contact with others, defined as less than once a week, and reporting not having left one’s home since the start of the pandemic. Individual-level pandemic-related variables were measured at the SCS, and country-level variables were determined from the period of the SCS data collection, between March 3rd and July 31st 2020.
The proportion of missingness was 8.8% for the full dataset, with 4.16% for area of residence, 1.74% for BMI, and less than 1% for each of the other variables. Imputation of missing values was performed using predictive mean matching, prior to dichotomization or categorization of variables. Analyses were weighted using the cross-sectional calibrated inverse probability weights provided as part of the SCS dataset (Scherpenzeel et al., 2020; Börsch-Supan, 2022h). Individual weights reflect each responder’s probability of being part of the 2020 SCS sample, based on characteristics of the national target population, and weighted data results in more representative estimates. The weight calibration procedure in SHARE is described in detail by De Luca et al. (2022) and De Luca and Li Donni (2022).
In order to partially validate the groupings that were defined by combining the single-item current loneliness scores from before and during the pandemic, mean scores on the Three-Item Loneliness Scale for the three groups were compared across the time points where this measure was also available (i.e., SHARE waves 5–8, not the SCSs), using a two-way mixed ANOVA for repeated measures. In addition, the longitudinal loneliness increase from Wave 8 to the SCS based on current reports was compared to the self-rated retrospective loneliness change from the SCS using a Chi-Square test of Independence.
Three weighted hierarchical binary logistic regression analyses were performed. In Analysis 1, the outcome was situational over no loneliness (coded as 1 and 0, respectively). In Analysis 2, the outcome was persistent (1) over no loneliness (0), and in Analysis 3, the outcome was persistent (1) over situational loneliness (0).
Predictor candidates and control variables were identical across the analyses and were grouped in five blocks added one at a time: 1–geographic region, 2–demographic variables, 3–pre-pandemic social network, 4–pre-pandemic health, and 5–pandemic variables. Block 1 contained categorial Northern, Southern, and Eastern Europe, Israel, and Western Europe as reference. Block 2 comprised continuous age in years, sex with male as reference, categorical education level with upper secondary as reference, dichotomous migrant status and nursing home residence, and categorical residential area consisting of big city, rural area or small town, and large town or suburb as reference. Block 3 included dichotomous cohabitant partner, widow/-er status, having no children, engaging in no social activities, and having low network satisfaction. It also contained categorical network size, comprising small, large, and medium as reference. Block 4 contained dichotomous two or more chronic diseases, one or more IADL limitations, not engaging in any vigorous physical activities, alcohol consumption, cognitive impairment, and depression, as well as categorical BMI (underweight, overweight, and normal as reference). Block 5 included continuous deaths per million inhabitants, and number of older population isolation months, as well as dichotomous staying home, and seldom having personal contact with others, since the pandemic started. In order to account for practice effects (i.e., responses that might change as a function of exposure), control variables of no interest were categorical ordinary SHARE wave appearances (range 2–7, mode: 5, and including Wave 8), and continuous months between Wave 8 and SCS (range 3–10, M: 5.92, and SD: 1.45).
This procedure resulted in five regression models for each of the three analyses. For every block added, the aggregated model was compared to the previous model using the Rao-Scott Likelihood Ratio Chi-Squared Test. Model fit was assessed by the percentage of residuals falling within error bounds of ± 2 standard deviations (Gelman and Hill, 2006). Results are presented with robust standard errors, as returned by the “svyglm” function of the Survey package for R (Lumley, 2020), allowing for the identification of first order trends in the data. The Area Under the Receiver Operating Characteristic (AUC) was used to measure discriminative capacity.
Analyses were computed using RStudio version 1.4.1717, running on Mac OS X 12.3.1. Imputation of missing values was done using the Mice package (van Buuren and Groothuis-Oudshoorn, 2011), and regression analyses were done using the Survey package (Lumley, 2020).
The final sample consisted of 30 245 older adults, 56.5% female, between 52 and 104 years of age (M: 70.33 and SD: 8.64). Sample characteristics for SHARE variables are presented in Table 1. Across countries, the average older population isolation period lasted for 2.17 months (SD: 1.16, median: 3.80, and range: 0–5.03), and the mean number of COVID-19 deaths per million inhabitants was 184.65 (SD: 233.74, median: 35.53, and range: 5.32–846). Figure 2A shows longitudinal loneliness incidence based on the single-item cut off, defined between Wave 8 and SCS 1, for all waves.
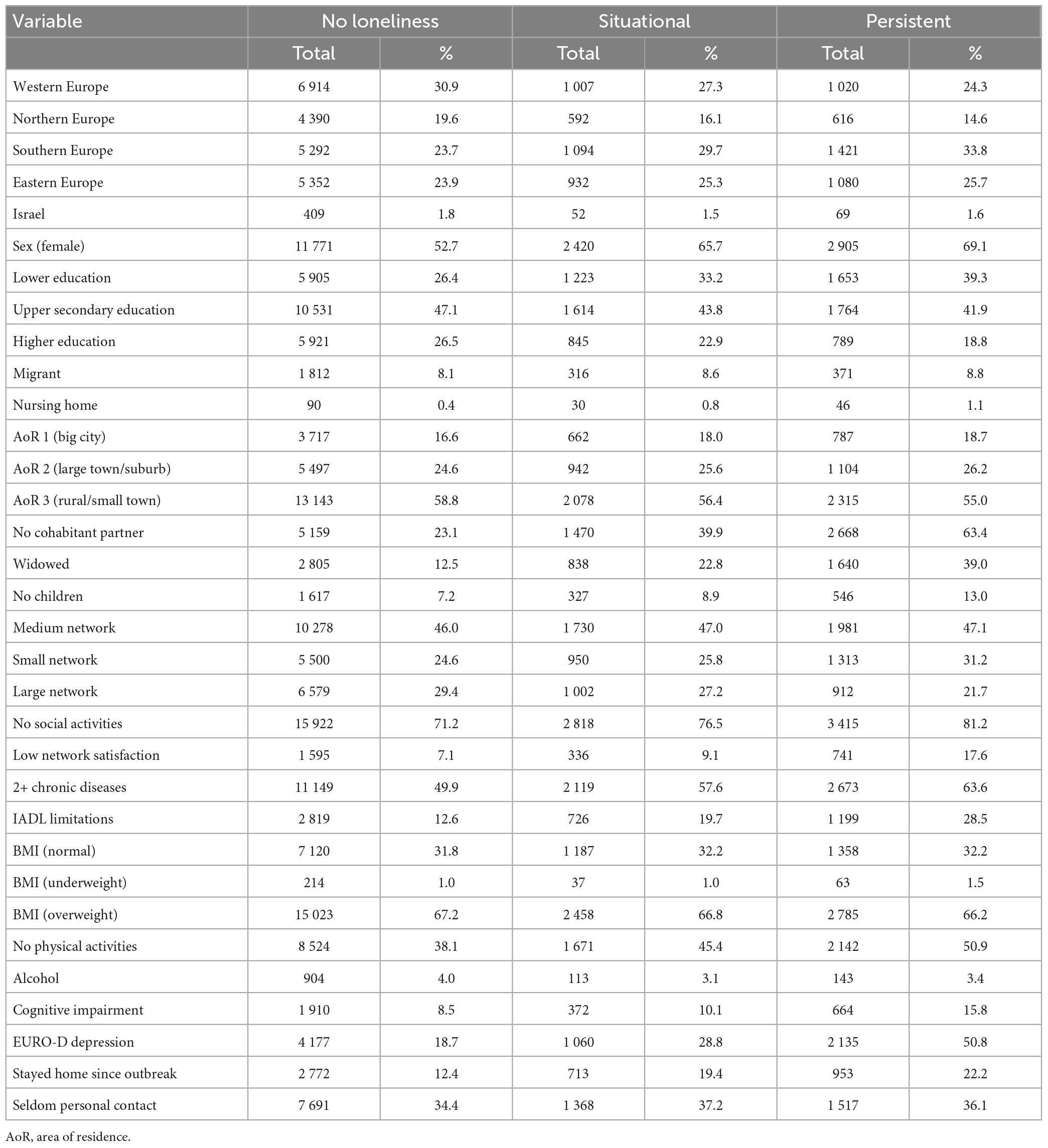
Table 1. Sample characteristics for categorical and dichotomous SHARE variables, by loneliness group.
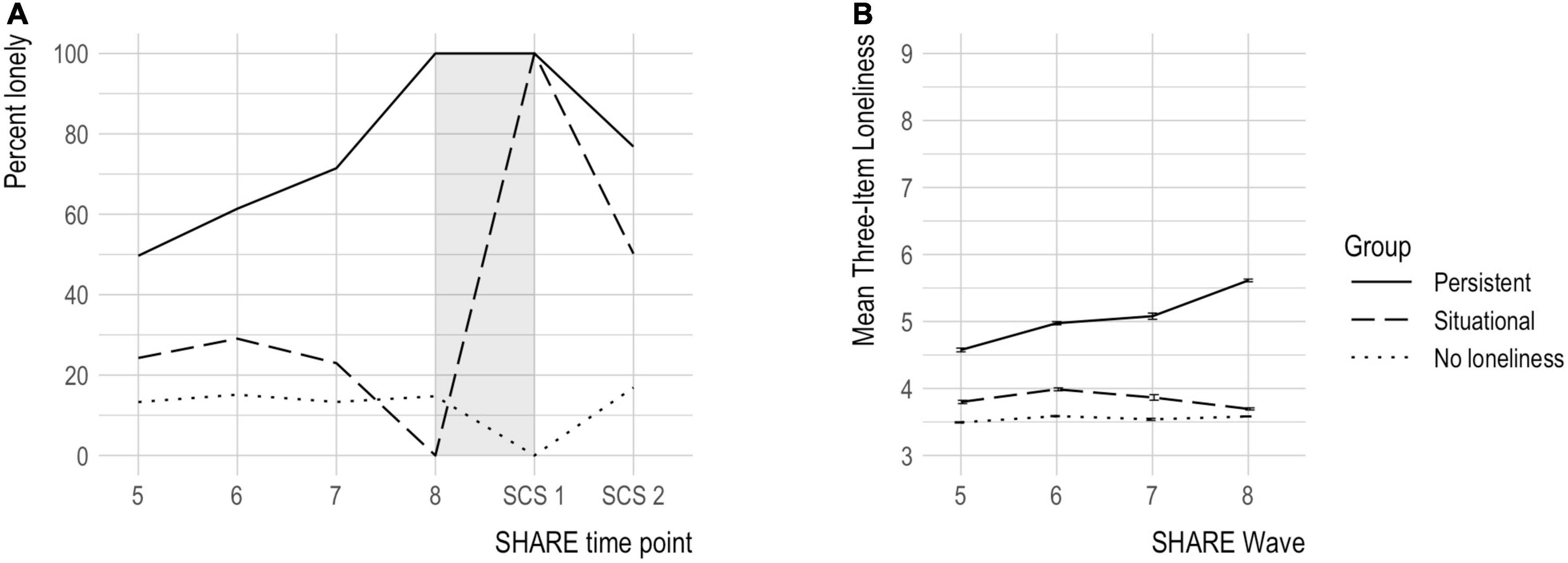
Figure 2. Loneliness in three groups over all available time points. (A) Percentage of groups reporting feeling lonely at ordinary SHARE wave 5 (N = 17 246), 6 (N = 21 508), 7 (N = 5 458), and 8 (N = 30 245), the first SHARE Corona Survey (SCS; SCS 1, N = 30 245), and the second SCS conducted 1 year later (SCS 2, N = 26 438). The gray band represents the period used to define the groups (Wave 8–SCS 1). (B) Mean Three-Item Loneliness Scale score (min = 3 and max = 9) and standard error for loneliness groups at ordinary SHARE wave 5 (N = 17 213), 6 (N = 21 487), 7 (N = 5 433), and 8 (N = 30 176).
There was a statistically significant interaction between loneliness group and wave number for the Three-Item Loneliness Scale score, F(6, 11 700) = 77.59, p = < 0.0001. The main effect of loneliness group was significant at all-time points [p = < 0.0001 (Wave 5), p = < 0.0001 (Wave 6), p = < 0.0001 (Wave 7), and p = < 0.0001 (Wave 8)], and pairwise comparisons showed that the mean Three-Item Loneliness Scale score was significantly different between all groups at all-time points (all p = < 0.0001; for details, see Supplementary Table 5). Figure 2B shows longitudinal mean scores on the Three-Item Loneliness Scale for all available time points (SHARE waves 5–8) for the three loneliness groups.
Interestingly, the single-item self-rated retrospective loneliness increase at the SCS did not correspond to longitudinal single-item loneliness increase from Wave 8 to the SCS, χ2 (1, N = 7 888) = 34.64, p < 0.001, with loneliness increase being reported by 42.5% of the situational loneliness group, characterized by an increase in longitudinal loneliness, and 36.0% of the persistent loneliness group characterized by stable longitudinal loneliness levels.
The first hierarchical regression analysis identified predictors of situational loneliness, i.e., onset, compared to no loneliness. Essential results of Analysis 1 are presented in Table 2, and full results including data for variables that were non-significant in all models can be found in Supplementary Table 6. Consistent predictors across all blocks were female sex, no cohabitant partner, two or more chronic diseases, and depression. Staying home and seldom having personal contact with others since the outbreak of COVID-19 were both associated with higher, while frequent alcohol use was associated with lower odds of situational loneliness. Chronological age was significant when adding the second block (Model 2) but rendered insignificant after social network variables were added. Eastern and Southern Europe predicted situational loneliness until pandemic variables were added, suggesting that these relationships may have been mediated by pandemic-related factors. Living in Northern Europe was a protective factor in the final model. For the full model, 96% of binned residuals were within error bounds, and discriminative ability was poor (AUC = 0.65).
The second analysis identified predictors of persistent loneliness, i.e., maintenance, compared to no loneliness. Essential results of Analysis 2 are presented in Table 3, and full results including data for variables that were non-significant in all models can be found in Supplementary Table 7. Consistent predictors of loneliness maintenance across all blocks were female sex, low education, no cohabitant partner, low network satisfaction, one or more IADL limitations, depression, and widowhood. Living in a country with a longer isolation period for older individuals, and a lower number of deaths attributed to COVID-19 per million inhabitants, also predicted persistent loneliness. Residing in a nursing home or small town/rural area, both protective, became significant after the inclusion of health and pandemic variables, respectively. Chronic diseases predicted persistent loneliness after the inclusion of pandemic variables, and chronological age was rendered insignificant when health variables were added. Living in Eastern Europe was a consistent predictor of persistent loneliness, while Southern Europe was significant until pandemic variables were added. Living in Northern Europe or Israel were protective factors in the final model. For the full model, 93% of binned residuals fell within error bounds, and discriminative ability was excellent (AUC = 0.81).
The third analysis identified predictors of persistent loneliness compared to situational loneliness, and the essential results of Analysis 3 are presented in Table 4. Full results including data for variables that were non-significant in all models can be found in Supplementary Table 8. Consistent predictors of persistent over situational loneliness across all blocks were no cohabitant partner, low network satisfaction, one or more IADL limitations, frequent alcohol use, depression, and living in a country with a longer isolation period for older individuals. Chronological age and low education were significant when adding the second block (Model 2), but rendered insignificant when social network variables were added. For the full model, 97% of binned residuals fell within error bounds, and discriminative ability was acceptable (AUC = 0.70).
Results of all model comparisons are presented in Table 5. For all analyses, the addition of each covariate block resulted in a significant model improvement, except for the addition of demographic variables to the intercept and control variables model in Analysis 3. Frequency, significance, and direction of association for all significant variables in the full models from Analysis 1, 2, and 3 are shown in Figure 3.
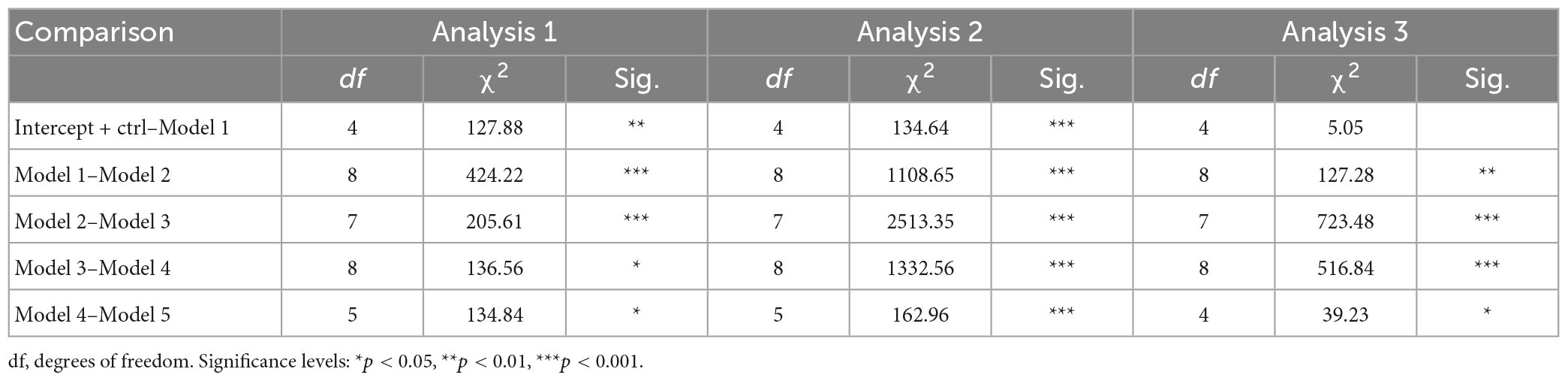
Table 5. Results of Rao-Scott Likelihood Ratio Chi-Squared Tests for stepwise comparisons of the models when adding one additional block of covariates in analyses 1 (situational over no loneliness), 2 (persistent over no loneliness), and 3 (persistent over situational loneliness).
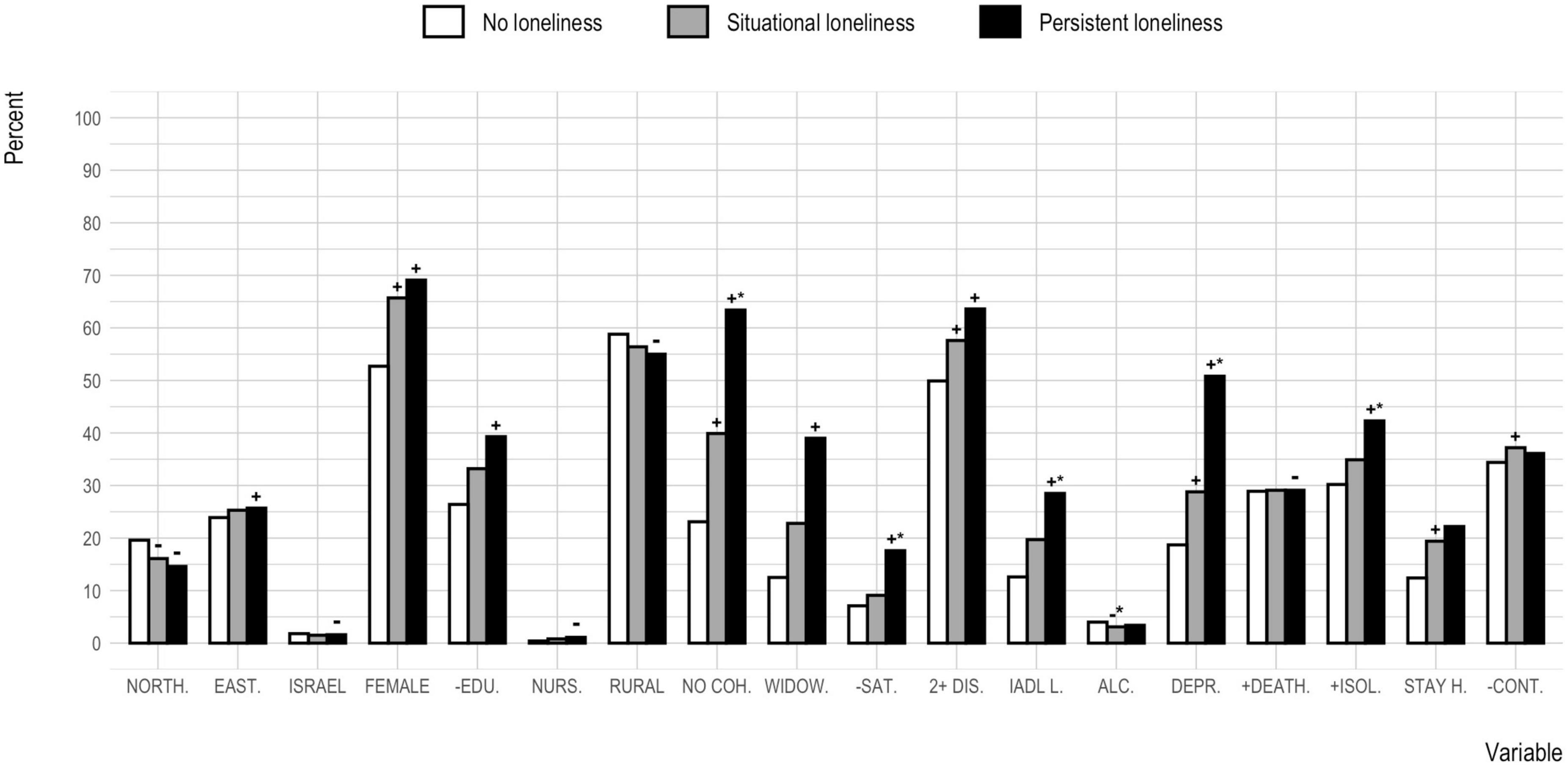
Figure 3. Frequency, significance, and direction of association for all significant variables in the full model from analyses 1, 2, and 3, per loneliness group. The continuous country-level variables deaths per million and number of older population isolation months have been dichotomized to reflect frequency of above average observations. NORTH., Northern Europe; EAST., Eastern Europe; FEMALE, female sex; -EDU, less than upper secondary education; NURS., residing in nursing home; RURAL, residing in rural area or small town; NO COH., no cohabitant partner; WIDOW, widowed; -SAT., low network satisfaction; 2 + DIS., two or more chronic diseases; IADL L., one or more IADL limitations; ALC., having six or more alcoholic drinks at least three times per week; DEPR., above cut-off on the EURO-D Depression Scale; + DEATH., above average COVID-19 attributed deaths per million inhabitants; + ISOL., above average number of older population isolation months; STAY H., stayed home since the beginning of the pandemic; -CONT., seldom personal contact. +Significantly higher odds for situational or persistent loneliness, as compared to the no loneliness group (in Analysis 1 or 2). –Significantly lower odds for situational or persistent loneliness, as compared to the no loneliness group (in Analysis 1 or 2). *Significantly higher or lower (±) odds for persistent/situational loneliness, as compared to situational/persistent loneliness (in Analysis 3).
Predictors of loneliness onset and maintenance among older adults in the COVID-19 pandemic were investigated among frequently studied candidate variables. Here, those individuals who reported feeling frequently lonely during the pandemic were further divided into groups of situational and persistent loneliness according to their reports of loneliness obtained before the pandemic. As hypothesized, hierarchical logistic regression analyses identified unique, shared, and pandemic-specific predictors of loneliness during the pandemic for those different groups.
This is in line with research showing that cross-sectional measures of loneliness capture both a remarkably stable trait and a more dynamic state component (Mund et al., 2020a,b). Indeed, the model for situational analysis showed worse discriminative ability than that for persistent loneliness, possibly reflecting the difficulty of predicting a state as compared to a trait. Comparing the persons with situational and persistent loneliness on other measures of loneliness, we found that a three-item loneliness measure obtained before the pandemic confirmed differences in loneliness as far back as 7 years prior to the pandemic. However, retrospective reports of subjective increases in loneliness at the time of the pandemic did not relate to longitudinal reports at each wave. Based on these and previous findings, and in line with our hypothesis, we argue that the group reporting cross-sectional loneliness is heterogeneous, containing both transient and chronic loneliness which should be treated as different constructs, at least until their similarities and differences have been fully established.
In contrast to prior work by Yang (2018), three unique predictors for persistent, and one for situational, loneliness were found. Among these was the country-level length of recommended or enforced isolation for older adults, uniquely predicting persistent loneliness. This variable has, to our knowledge, not been studied in relation to loneliness before. Extending previous findings (Atzendorf and Gruber, 2021; Buecker and Horstmann, 2021), this result indicates that pre-and peri-pandemic loneliness predictors were not identical when considering situational and persistent loneliness separately, and that restrictions and social policy had an impact on maintenance of loneliness in the older adult population during this time. Low network satisfaction and functional limitations were also unique predictors of persistent loneliness. While self-rated quality of social relationships has consistently been identified as a risk factor for loneliness in older adults, evidence regarding functional limitations has been ambiguous (Dahlberg et al., 2022). Functional limitations may have been more closely related to loneliness maintenance during the COVID-19 pandemic, or, alternatively, the disparity of previous findings may be due to the grouping together of persistent and situational loneliness.
Out of the five shared predictors of situational and persistent loneliness, two were also associated with significantly higher odds of loneliness maintenance rather than onset. These were depression and no cohabitant partner, each more than doubling the odds of experiencing persistent over both situational and no loneliness, with the largest effect sizes (small to medium) of any predictors in the study. Depression has consistently been associated with loneliness in longitudinal studies of older adults (Dahlberg et al., 2022), and the mutually aggravating relationship between loneliness and depression over time described by Luanaigh and Lawlor (2008) could possibly account for the stronger association to persistent loneliness found in this study. Marital status and cohabitation have also been consistent predictors of loneliness before and during the pandemic (Bu et al., 2020; Groarke et al., 2020; Hansen et al., 2021; O’Shea et al., 2021; van Tilburg et al., 2021; Dahlberg et al., 2022), although a greater influence of quality over quantity of social relationships has been argued (Pinquart and Sörensen, 2003). In this study, however, quality of relationships (network satisfaction) was only a significant predictor alongside quantity (cohabitant partner, but not network size) in the case of persistent loneliness. While lending further weight to partnership as a protective factor against loneliness in general, our findings point to the absence of a cohabiting partner as a particularly strong predictor of long-term loneliness. This is consistent with theoretical models of chronic loneliness as a self-sustaining, vicious circle of social withdrawal (Qualter et al., 2015), minimizing opportunities for meeting and engaging with potential partners.
Both situational and persistent loneliness were predicted by geographical region, physical health, and sex. The results for geographical regions were largely similar to findings from a pre-pandemic meta-analysis by Surkalim et al. (2022), with residents of Northern Europe being less likely than those of Western Europe to report feeling lonely. Since the evidence for chronic illness as a risk factor for loneliness was not found to be consistent in the review by Dahlberg et al. (2022), the relationship we found may be unique to the pandemic context, e.g., through belonging to a COVID-19 risk group. The sex difference found in this study is consistent with previous research using a direct single-item measure of loneliness (von Soest et al., 2018), with females being significantly more likely than males to report feeling lonely when asking the participant directly about how lonely they feel. However, females were also found to experience a significantly larger increase in loneliness from before to during the COVID-19 pandemic in a study by Entringer and Gosling (2022), using an indirect multi-item loneliness measure, not excluding the possibility of female sex being a pandemic-specific risk factor.
Inconsistently, two predictors of loneliness onset, and seven predictors of loneliness maintenance, were significant when compared to the non-loneliness group, but non-significant in the third comparison analysis. Further research is required in order to establish whether, or through which mechanisms, factors such as pandemic behavior, education, residential area, and widowhood act upon transient and chronic loneliness. In addition, the results showed that frequent alcohol consumption (having six or more alcoholic drinks at least three times per week during the past 3 months) was more common among both the persistent and no loneliness groups as compared to the situational loneliness group. This is a counter-intuitive finding that may be further studied in samples with a higher frequency of alcohol abuse, or including a more refined measure that distinguishes types of alcohol, multi-item scales, and structured interview instruments.
To our knowledge, it is the first study to separately investigate predictors of situational and persistent loneliness during the COVID-19 pandemic from longitudinal data. We used a large sample from a longitudinal cross-country survey and were able to control for a large number of previously studied variables. Combining ordinary SHARE waves and the peri-pandemic SCS, we were able to rely on longitudinal self-reports rather than retrospective self-reported change which may introduce bias (Blome and Augustin, 2015; Hipp et al., 2020), e.g., if self-assessments are collectively impacted by changes in societal norms (Jaspers et al., 2009), and which did not correspond to longitudinal change in this sample. However, the single-item loneliness measure used in this study, while being adequate and comparable to more complex multi-item measures (Mund et al., 2022), does not allow for the distinction of social and emotional loneliness. Originally described by Weiss (1973), emotional loneliness refers to the lack of a close, intimate attachment to another person, while social loneliness denotes a perceived lack of social networks that provide a wider sense of belonging and community (Russell et al., 1984; de Jong Gierveld et al., 2006). These two facets of loneliness have different correlates (Dahlberg and McKee, 2014; Lee et al., 2022), and a need for further research distinguishing between predictors of emotional and social loneliness, respectively, has been pointed out (Dahlberg et al., 2022). In addition, these facets of loneliness may have been differently impacted by the pandemic, and a larger pandemic-related increase in emotional rather than social loneliness has been found by van Tilburg (2022). Future research should investigate facets of loneliness within the context of situational and persistent loneliness.
In-depth analysis of higher-order relationships, interactions, and mediation among predictor candidates was also outside the scope of this study. Given the investigation of loneliness onset and maintenance during a pandemic, our results may be either general or specific to these circumstances, and generalization of the findings requires corroboration outside of the pandemic context. Further, onset of loneliness in the COVID-19 pandemic likely represents the start of persistent feelings for some, and a passing state for others. The specific identification of predictors for onset of persistent loneliness would have required the use of more time points. This is, however, an important avenue for future research, as the development of chronic loneliness, leading to worse health outcomes than transient loneliness, is an important target for intervention.
In our study, persistent loneliness in older adults was predicted by length of isolation during the first months of the COVID-19 pandemic. Under social contact restrictions, persistently lonely older adults may be seen as a particularly vulnerable group, and may also lack the internal and external resources to “bounce back” and attain social reconnection after a period of mandated social isolation. Therefore, future lockdowns and social contact restrictions should be followed up with efforts put in place in order to minimize their long-term negative consequences for this particular group. While severe circumstances such as the COVID-19 pandemic may increase the risk of loneliness maintenance among persistently lonely individuals, it remains imperative to target chronic loneliness during times when no restrictions are in place. Since the United Kingdom launched a national strategy to combat loneliness and became the first European country to appoint a Minister for Loneliness in 2018 (United Kingdom Department for Digital Culture, Media, and Sport, 2018), more light has been shed on loneliness as a major public health concern, and more national and European efforts have been directed toward combating loneliness in the aftermath of the COVID-19 pandemic [e.g., the 2021 Policy Brief titled “Addressing loneliness and social isolation among older people in Europe” (European Centre for Social Welfare Policy and Research, 2021), the 2022 German Strategy Against Loneliness (Federal Ministry for Family Affairs, Senior Citizens, Women and Youth, 2023), and the special focus on loneliness announced by the Swedish Minister for Social Affairs and Public Health as part of the Swedish 6 month presidency of the Council of the European Union in early 2023 (Swedish Presidency of the Council of the European Union, 2023)]. National strategies may seek to address loneliness risk factors on a country or municipality level, e.g., by instituting policies recommending screening for loneliness and specialized treatment of late-life depression in public health settings, shared housing developments for older citizens, and promoting research on, and dissemination of, effective treatment protocols specifically targeting the thoughts and behaviors that work to maintain chronic loneliness on an individual level.
Loneliness and its negative consequences for mental and physical wellbeing is an important facet of the impact of the COVID-19 pandemic on older adults. Our study shows that a distinction of situational and persistent loneliness is warranted. The sensitivity of persistent loneliness to length of isolation should be taken into account when employing social policies affecting older adults. Interventions aimed at preventing or addressing loneliness may target persons with symptoms of depression, functional limitations, chronic health issues, and no cohabitant partner. Future research should aim to develop a standard classification of transient and chronic loneliness, and to further the understanding of their unique or shared risk factors and outcomes. Where the temporal relationship is unclear, efforts should be made to understand the mechanisms by which persistent loneliness and its predictors are associated, e.g., whether these factors maintain chronic loneliness independently, or whether they mediate the relationship between prior and future loneliness. Apart from identifying risk groups, the characterization of such mechanisms may direct intervention targets, e.g., environmental circumstances, or individual patterns of thought and behavior.
Publicly available datasets were analyzed in this study. This data can be found here: https://share-eric.eu/data/data-documentation/share-data-releases.
The studies involving human participants were reviewed and approved by the Ethics Committee of the University of Mannheim (SHARE waves 1 to 3) and the Ethics Council of the Max Planck Society (SHARE waves 4 onward). For more details please see: https://share-eric.eu/fileadmin/user_upload/Ethics_Documentation/SHARE_ethics_approvals.pdf. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
VPL and AR designed the research. VPL and MJ analyzed the data. VPL wrote the manuscript. AR and MJ contributed to the writing. All authors contributed to the article and approved the submitted version.
AR and VPL were supported by funding from the European Commission under Horizon 2020 (SHARE-COVID-19: GA No. 101015924). The SHARE data collection has been funded by the European Commission, DG RTD through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, and SHARELIFE: CIT4-CT-2006-028812), FP7 (SHARE-PREP: GA No. 211909, SHARE-LEAP: GA No. 227822, SHARE M4: GA No. 261982, and DASISH: GA No. 283646) and Horizon 2020 (SHARE-DEV3: GA No. 676536, SHARE-COHESION: GA No. 870628, SERISS: GA No. 654221, SSHOC: GA No. 823782, and SHARE-COVID19: GA No. 101015924) and by the DG Employment, Social Affairs and Inclusion through VS 2015/0195, VS 2016/0135, VS 2018/0285, VS 2019/0332, and VS 2020/0313. Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C, and RAG052527A) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1172552/full#supplementary-material
Åkerlind, I., and Hörnquist, J. O. (1992). Loneliness and alcohol abuse: A review of evidences of an interplay. Soc. Sci. Med. 34, 405–414. doi: 10.1016/0277-9536(92)90300-f
Akhter-Khan, S. C., Tao, Q., Ang, T. F. A., Itchapurapu, I. S., Alosco, M. L., Mez, J., et al. (2021). Associations of loneliness with risk of Alzheimer’s disease dementia in the Framingham Heart Study. Alzheimers Dement. 17, 1619–1627. doi: 10.1002/alz.12327
Armitage, R., and Nellums, L. B. (2020). COVID-19 and the consequences of isolating the elderly. Lancet Public Health 5:e256. doi: 10.1016/S2468-2667(20)30061-X
Atzendorf, J., and Gruber, S. (2021). Depression and loneliness of older adults in Europe and Israel after the first wave of covid-19. Eur. J. Ageing 19, 849–861. doi: 10.1007/s10433-021-00640-8
Bergmann, M., and Börsch-Supan, A. (2021). SHARE wave 8 methodology: Collecting cross-national survey data in times of COVID-19. Munich: MEA, Max Planck Institute for Social Law and Social Policy.
Bergmann, M., Kneip, T., de Luca, G., and Scherpenzeel, A. (2019). Survey participation in the survey of health, ageing and retirement in Europe (SHARE), wave 1-7. Based on release 7.0.0. SHARE working paper series 41-2019. Munich: MEA, Max Planck Institute for Social Law and Social Policy.
Blome, C., and Augustin, M. (2015). Measuring change in quality of life: Bias in prospective and retrospective evaluation. Value Health 18, 110–115. doi: 10.1016/j.jval.2014.10.007
Börsch-Supan, A. (2022a). Survey of health, ageing and retirement in Europe (SHARE) wave 1. Release version: 8.0.0. SHARE-ERIC. Data Set doi: 10.6103/SHARE.w1.800
Börsch-Supan, A. (2022b). Survey of health, ageing and retirement in Europe (SHARE) wave 2. Release version: 8.0.0. SHARE-ERIC. Data Set doi: 10.6103/SHARE.w2.800
Börsch-Supan, A. (2022c). Survey of health, ageing and retirement in Europe (SHARE) wave 4. Release version: 8.0.0. SHARE-ERIC. Data Set doi: 10.6103/SHARE.w4.800
Börsch-Supan, A. (2022d). Survey of health, ageing and retirement in Europe (SHARE) wave 5. Release version: 8.0.0. SHARE-ERIC. Data Set doi: 10.6103/SHARE.w5.800
Börsch-Supan, A. (2022e). Survey of health, ageing and retirement in Europe (SHARE) wave 6. Release version: 8.0.0. SHARE-ERIC. Data Set doi: 10.6103/SHARE.w6.800
Börsch-Supan, A. (2022f). Survey of health, ageing and retirement in Europe (SHARE) wave 7. Release version: 8.0.0. SHARE-ERIC. Data Set doi: 10.6103/SHARE.w7.800
Börsch-Supan, A. (2022g). Survey of health, ageing and retirement in Europe (SHARE) wave 8. Release version: 8.0.0. SHARE-ERIC. Data Set doi: 10.6103/SHARE.w8.800
Börsch-Supan, A. (2022h). Survey of health, ageing and retirement in Europe (SHARE) wave 8. COVID-19 survey 1. Release version: 8.0.0. SHARE-ERIC. Data Set doi: 10.6103/SHARE.w8ca.800
Börsch-Supan, A. (2022i). Survey of health, ageing and retirement in Europe (SHARE) wave 9. COVID-19 survey 2. Release version: 8.0.0. SHARE-ERIC. Data Set doi: 10.6103/SHARE.w9ca.800
Börsch-Supan, A., Brandt, M., Hunkler, C., Kneip, T., Korbmacher, J., Malter, F., et al. (2013). Data resource profile: The survey of health, ageing and retirement in Europe (share). Int. J. Epidemiol. 42, 992–1001. doi: 10.1093/ije/dyt088
Börsch-Supan, A., and Gruber, S. (2022). easySHARE. Release version: 8.0.0. SHARE-ERIC. Data Set doi: 10.6103/SHARE.easy.800
Bu, F., Steptoe, A., and Fancourt, D. (2020). Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health 186, 31–34. doi: 10.1016/j.puhe.2020.06.036
Buecker, S., and Horstmann, K. T. (2021). Loneliness and social isolation during the COVID-19 pandemic: A systematic review enriched with empirical evidence from a large-scale diary study. Eur. Psychol. 26, 272–284. doi: 10.1027/1016-9040/a000453
Cacioppo, J. T., and Cacioppo, S. (2018). “Loneliness in the modern age: An evolutionary theory of loneliness (ETL),” in Advances in experimental social psychology, ed. J. M. Olson (Cambridge, MA: Academic Press Inc.), 127–197. doi: 10.1016/bs.aesp.2018.03.003
Cacioppo, J. T., and Hawkley, L. C. (2009). Perceived social isolation and cognition. Trends Cogn. Sci. 13, 447–454. doi: 10.1016/j.tics.2009.06.005
Chu, B. L., and Zhang, W. (2022). Impact of transient and chronic loneliness on progression and reversion of frailty in community-dwelling older adults: Four-year follow-up. BMC Geriatr. 22:642. doi: 10.1186/s12877-022-03283-1
Cohen-Mansfield, J., Hazan, H., Lerman, Y., and Shalom, V. (2016). Correlates and predictors of loneliness in older-adults: A review of quantitative results informed by qualitative insights. Int. Psychogeriatr. 28, 557–576. doi: 10.1017/S1041610215001532
Dahlberg, L., and McKee, K. J. (2014). Correlates of social and emotional loneliness in older people: Evidence from an English community study. Aging Ment. Health 18, 504–514. doi: 10.1080/13607863.2013.856863
Dahlberg, L., McKee, K. J., Frank, A., and Naseer, M. (2022). A systematic review of longitudinal risk factors for loneliness in older adults. Aging Ment. Health 26, 225–249. doi: 10.1080/13607863.2021.1876638
Davies, K., Maharani, A., Chandola, T., Todd, C., and Pendleton, N. (2021). The longitudinal relationship between loneliness, social isolation, and frailty in older adults in England: A prospective analysis. Lancet Healthy Longev. 2, e70–e77. doi: 10.1016/S2666-7568(20)30038-6
de Jong Gierveld, J., van Tilburg, T., and Dykstra, P. A. (2006). “Loneliness and social isolation,” in The Cambridge handbook of personal relationships Cambridge handbooks in psychology, eds A. L. Vangelisti and D. Perlman (Cambridge, MA: Cambridge University Press), 485–500. doi: 10.1017/CBO9780511606632.027
De Luca, G., and Li Donni, P. (2022). “Weights,” in SHARE corona survey release guide. Available online at: https://share-eric.eu/fileadmin/user_upload/Release_Guides/SHARE_Corona_Survey_Release_Guide.pdf (accessed April 5, 2023).
De Luca, G., Li Donni, P., and Rashidi, M. (2022). “Weights and imputations in SHARE wave 8,” in Share wave 8 methodology: Collecting cross-national survey data in times of COVID-19, eds M. Bergmann and A. Börsch-Supan (Munich: MEA, Max Planck Institute for Social Law and Social Policy), 133–145.
Dong, E., Du, H., and Gardner, L. (2020). An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 20, 533–534. doi: 10.1016/S1473-3099(20)30120-1
Entringer, T. M., and Gosling, S. D. (2022). Loneliness during a nationwide lockdown and the moderating effect of extroversion. Soc. Psychol. Personal. Sci. 13:194855062110378. doi: 10.1080/13548506.2022.2058030
Ernst, M., Niederer, D., Werner, A. M., Czaja, S. J., Mikton, C., Ong, A. D., et al. (2022). Loneliness before and during the COVID-19 pandemic: A systematic review with meta-analysis. Am. Psychol. 77, 660–677. doi: 10.1037/amp0001005
European Centre for Social Welfare Policy and Research (2021). Addressing loneliness and social isolation among older people in Europe. Available online at: https://www.euro.centre.org/downloads/detail/4126 (accessed April 5, 2023).
Federal Ministry for Family Affairs, Senior Citizens, Women and Youth (2023). Strategie gegen Einsamkeit. Available online at: https://www.bmfsfj.de/bmfsfj/themen/engagement-und-gesellschaft/strategie-gegen-einsamkeit (accessed April 5, 2023).
Gelman, A., and Hill, J. (2006). Data analysis using regression and multilevel/hierarchical models. Cambridge, MA: Cambridge University Press. doi: 10.1017/CBO9780511790942
Groarke, J. M., Berry, E., Graham-Wisener, L., McKenna-Plumley, P. E., McGlinchey, E., and Armour, C. (2020). Loneliness in the UK during the COVID-19 pandemic: Cross-sectional results from the COVID-19 psychological wellbeing study. PLoS One 15:e0239698. doi: 10.1371/journal.pone.0239698
Gruber, S., Hunkler, C., and Stuck, S. (2014). Generating easySHARE: Guidelines, structure, content and programming. SHARE working paper series 17-2014. Munich: MEA, Max Planck Institute for Social Law and Social Policy.
Hackett, R. A., Steptoe, A., Cadar, D., and Fancourt, D. (2019). Social engagement before and after dementia diagnosis in the English longitudinal study of ageing. PLoS One 14:e0220195. doi: 10.1371/journal.pone.0220195
Hale, T., Angrist, N., Goldszmidt, R., Kira, B., Petherick, A., Phillips, T., et al. (2021). A global panel database of pandemic policies (Oxford COVID-19 government response tracker). Nat. Hum. Behav. 5, 529–538. doi: 10.1038/s41562-021-01079-8
Hansen, T., Nilsen, T. S., Yu, B., Knapstad, M., Skogen, J. C., Vedaa, Ø., et al. (2021). Locked and lonely? A longitudinal assessment of loneliness before and during the COVID-19 pandemic in Norway. Scand. J. Public Health 49, 766–773. doi: 10.1177/1403494821993711
Hipp, L., Bünning, M., Munnes, S., and Sauermann, A. (2020). Problems and pitfalls of retrospective survey questions in COVID-19 studies. Surv. Res. Methods 14, 109–114.
Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T., and Stephenson, D. (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect. Psychol. Sci. 10, 227–237. doi: 10.1177/1745691614568352
Hughes, M. E., Waite, L. J., Hawkley, L. C., and Cacioppo, J. T. (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Res. Aging 26, 655–672. doi: 10.1177/0164027504268574
Jaspers, E., Lubbers, M., and de Graaf, N. D. (2009). Measuring once twice: An evaluation of recalling attitudes in survey research. Eur. Sociol. Rev. 25, 287–301.
Killgore, W. D. S., Cloonan, S. A., Taylor, E. C., and Dailey, N. S. (2020). Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Res. 290:113117. doi: 10.1016/j.psychres.2020.113117
Kim, A. J., Beam, C. R., Greenberg, N. E., and Burke, S. L. (2020). Health factors as potential mediators of the longitudinal effect of loneliness on general cognitive ability. Am. J. Geriatr. Psychiatry 28, 1272–1283. doi: 10.1016/j.jagp.2020.07.017
Lara, E., Martín-María, N., de la Torre-Luque, A., Koyanagi, A., Vancampfort, D., Izquierdo, A., et al. (2019). Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Res. Rev. 52, 7–16. doi: 10.1016/j.arr.2019.03.002
Laranjeira, C. (2021). The ‘loneliness pandemic’: Implications for gerontological nursing. Br. J. Nurs. 30, 652–655. doi: 10.12968/bjon.2021.30.11.652
Lawton, M. P., and Brody, E. M. (1969). Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 3, 179–186.
Lazzari, C., and Rabottini, M. (2022). COVID-19, loneliness, social isolation and risk of dementia in older people: A systematic review and meta-analysis of the relevant literature. Int. J. Psychiatry Clin. Pract. 26, 196–207. doi: 10.1080/13651501.2021.1959616
Lee, J. H., Luchetti, M., Aschwanden, D., Sesker, A. A., Strickhouser, J. E., Terracciano, A., et al. (2022). Cognitive impairment and the trajectory of loneliness in older adulthood: Evidence from the health and retirement study. J. Aging Health 34, 3–13. doi: 10.1177/08982643211019500
Lim, M. H., Eres, R., and Vasan, S. (2020). Understanding loneliness in the twenty-first century: An update on correlates, risk factors, and potential solutions. Soc. Psychiatry Psychiatr. Epidemiol. 55, 793–810. doi: 10.1007/s00127-020-01889-7
Luanaigh, C. Ó., and Lawlor, B. A. (2008). Loneliness and the health of older people. Int. J. Geriatr. Psychiatry 23, 1213–1221. doi: 10.1002/gps.2054
Luchetti, M., Lee, J. H., Aschwanden, D., Sesker, A., Strickhouser, J. E., Terracciano, A., et al. (2020). The trajectory of loneliness in response to COVID-19. Am. Psychol. 75, 897–908. doi: 10.1037/amp0000690
Martín-María, N., Caballero, F. F., Miret, M., Tyrovolas, S., Haro, J. M., Ayuso-Mateos, J. L., et al. (2020). Differential impact of transient and chronic loneliness on health status. A longitudinal study. Psychol. Health 35, 177–195. doi: 10.1080/08870446.2019.1632312
McDaid, D., Qualter, P., Arsenault, L., Barreto, M., Fett, A.-K., Hey, N., et al. (2022). Tackling loneliness evidence review. Available online at: https://www.gov.uk/government/publications/tackling-loneliness-evidence-review/tackling-loneliness-evidence-review-full-report (accessed March 17, 2023).
Mund, M., Freuding, M. M., Möbius, K., Horn, N., and Neyer, F. J. (2020a). The stability and change of loneliness across the life span: A meta-analysis of longitudinal studies. Pers. Soc. Psychol. Rev. 24, 24–52. doi: 10.1177/1088868319850738
Mund, M., Lüdtke, O., and Neyer, F. J. (2020b). Owner of a lonely heart: The stability of loneliness across the life span. J. Pers. Soc. Psychol. 119, 497–516. doi: 10.1037/pspp0000262
Mund, M., Maes, M., Drewke, P. M., Gutzeit, A., Jaki, I., and Qualter, P. (2022). Would the real loneliness please stand up? The validity of loneliness scores and the reliability of single-item scores. Assessment doi: 10.1177/10731911221077227 [Epub ahead of print].
O’Shea, B. Q., Finlay, J. M., Kler, J., Joseph, C. A., and Kobayashi, L. C. (2021). Loneliness among us adults aged =55 early in the COVID-19 pandemic: Findings from the COVID-19 coping study. Public Health Rep. 136, 754–764.
Park, C., Majeed, A., Gill, H., Tamura, J., Ho, R. C., Mansur, R. B., et al. (2020). The effect of loneliness on distinct health outcomes: A comprehensive review and meta-analysis. Psychiatry Res. 294:113514. doi: 10.1016/j.psychres.2020.113514
Phillips, T., and Tatlow, H. (2021). Codebook for the Oxford Covid-19 government response tracker. Available online at: https://github.com/OxCGRT/covid-policy-tracker/blob/master/documentation/codebook.md#codebook-for-the-oxford-covid-19-government-response-tracker (accessed December 7, 2021).
Pinquart, M., and Sörensen, S. (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychol. Aging 18, 250–267. doi: 10.1037/0882-7974.18.2.250
Piolatto, M., Bianchi, F., Rota, M., Marengoni, A., Akbaritabar, A., and Squazzoni, F. (2022). The effect of social relationships on cognitive decline in older adults: An updated systematic review and meta-analysis of longitudinal cohort studies. BMC Public Health 22:278. doi: 10.1186/s12889-022-12567-5
Prince, M. J., Reischies, F., Beekman, A. T. F., Fuhrer, R., Jonker, C., Kivela, S. L., et al. (1999). Development of the EURO-D scale - A European union initiative to compare symptoms of depression in 14 European centres. Br. J. Psychiatry 174, 330–338. doi: 10.1192/bjp.174.4.330
Quadt, L., Esposito, G., Critchley, H. D., and Garfinkel, S. N. (2020). Brain-body interactions underlying the association of loneliness with mental and physical health. Neurosci. Biobehav. Rev. 116, 283–300. doi: 10.1016/j.neubiorev.2020.06.015
Qualter, P., Vanhalst, J., Harris, R., van Roekel, E., Lodder, G., Bangee, M., et al. (2015). Loneliness across the life span. Perspect. Psychol. Sci. 10, 250–264. doi: 10.1177/1745691615568999
Quetelet, A. (1832). Recherches sur le poids de l’homme aux différens âges. Nouveaux Mém. Acad. R. Sci. Belles Lett. Bruxelles 7:1.
Rawtaer, I., Gao, Q., Nyunt, M. S. Z., Feng, L., Chong, M. S., Lim, W. S., et al. (2017). Psychosocial risk and protective factors and incident mild cognitive impairment and dementia in community dwelling elderly: Findings from the Singapore longitudinal ageing study. J. Alzheimers Dis. 57, 603–611. doi: 10.3233/JAD-160862
Rico-Uribe, L. A., Caballero, F. F., Martín-María, N., Cabello, M., Ayuso-Mateos, J. L., and Miret, M. (2018). Association of loneliness with all-cause mortality: A meta-analysis. PLoS One 13:e0190033. doi: 10.1371/journal.pone.0190033
Russell, D., Cutrona, C. E., Rose, J., and Yurko, K. (1984). Social and emotional loneliness: An examination of Weiss’s typology of loneliness. J. Pers. Soc. Psychol. 46, 1313–1321. doi: 10.1037/0022-3514.46.6.1313
Russell, D., Peplau, L. A., and Cutrona, C. E. (1980). The revised UCLA loneliness scale: Concurrent and discriminant validity evidence. J. Pers. Soc. Psychol. 39, 472–480. doi: 10.1037//0022-3514.39.3.472
Salinas, J., Beiser, A. S., Samra, J. K., Odonnell, A., Decarli, C. S., Gonzales, M. M., et al. (2022). Association of loneliness with 10-year dementia risk and early markers of vulnerability for neurocognitive decline. Neurology 98, E1337–E1348. doi: 10.1212/WNL.0000000000200039
Scherpenzeel, A., Axt, K., Bergmann, M., Douhou, S., Oepen, A., Sand, G., et al. (2020). Collecting survey data among the 50+ population during the COVID-19 outbreak: The survey of health, ageing and retirement in Europe (SHARE). Surv. Res. Methods 14, 217–221.
Shiovitz-Ezra, S., and Ayalon, L. (2010). Situational versus chronic loneliness as risk factors for all-cause mortality. Int. Psychogeriatr. 22, 455–462. doi: 10.1017/S1041610209991426
Steel, N., Huppert, F. A., McWilliams, B., and Melzer, D. (2002). “Physical and cognitive function,” in Health, wealth and lifestyles of the older population in England: The 2002 English longitudinal study of ageing, eds M. Marmot, J. Banks, R. Blundell, C. Lessof, and J. Nazroo (London: The Institute for Fiscal Studies), 249–300.
Surkalim, D. L., Luo, M., Eres, R., Gebel, K., van Buskirk, J., Bauman, A., et al. (2022). The prevalence of loneliness across 113 countries: Systematic review and meta-analysis. BMJ 376:e067068. doi: 10.1136/bmj-2021-067068
Swedish Presidency of the Council of the European Union (2023). “Health care,” in Swedish presidency programme. Available online at: https://swedish-presidency.consilium.europa.eu/media/ntkerqpw/the-swedish-presidency-programme.pdf (accessed April 5, 2023).
United Kingdom Department for Digital Culture, Media, and Sport (2018). PM launches government’s first loneliness strategy. Available online at: https://www.gov.uk/government/news/pm-launches-governments-first-loneliness-strategy/ (accessed April 5, 2023).
United Nations (2021). Standard country or area codes for statistical use (M49). New York, NY: United Nations. Available online at: https://unstats.un.org/unsd/methodology/m49/overview/ (accessed December 7, 2021).
United Nations Educational, Scientific and Cultural Organization [UNESCO] (2003). International standard classification of education, ISCED 1997. Berlin: Springer.
van Buuren, S., and Groothuis-Oudshoorn, K. (2011). mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 45, 1–67.
van Tilburg, T. G. (2022). Emotional, social, and existential loneliness before and during the COVID-19 pandemic: Prevalence and risk factors among Dutch older adults. J. Gerontol. Ser B 77, e179–e184. doi: 10.1093/geronb/gbab101
van Tilburg, T. G., Steinmetz, S., Stolte, E., van der Roest, H., and de Vries, D. H. (2021). Loneliness and mental health during the COVID-19 pandemic: A study among Dutch older adults. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 76, E249–E255. doi: 10.1093/geronb/gbaa111
von Soest, T., Luhmann, M., Hansen, T., and Gerstorf, D. (2018). Development of loneliness in midlife and old age: Its nature and correlates. J. Pers. Soc. Psychol. 118, 388–406. doi: 10.1037/pspp0000219
Vozikaki, M., Papadaki, A., Linardakis, M., and Philalithis, A. (2018). Loneliness among older European adults: Results from the survey of health, aging and retirement in Europe. J. Public Health 26, 613–624. doi: 10.1007/s10389-018-0916-6
Weiss, R. (1973). Loneliness: The experience of emotional and social isolation. Cambridge, MA: MIT press.
World Health Organization [WHO] (1995). Physical status: The use of and interpretation of anthropometry, report of a WHO expert committee. Geneva: World Health Organization.
Wu, B. (2020). Social isolation and loneliness among older adults in the context of COVID-19: A global challenge. Glob. Health Res. Policy 5:27. doi: 10.1186/s41256-020-00154-3
Yang, K. (2018). Longitudinal loneliness and its risk factors among older people in England. Can. J. Aging 37, 12–21. doi: 10.1017/S0714980817000526
Yang, K., and Victor, C. (2011). Age and loneliness in 25 European nations. Ageing Soc. 31, 1368–1388. doi: 10.1017/S0144686X1000139X
Keywords: longitudinal, predictors, loneliness, transient loneliness, persistent loneliness, chronic loneliness, COVID-19, pandemic
Citation: Panes Lundmark V, Josefsson M and Rieckmann A (2023) Predictors of loneliness onset and maintenance in European older adults during the COVID-19 pandemic. Front. Psychol. 14:1172552. doi: 10.3389/fpsyg.2023.1172552
Received: 23 February 2023; Accepted: 17 April 2023;
Published: 02 June 2023.
Edited by:
Alessia Rosi, The University of Pavia, ItalyReviewed by:
Elena Rolandi, Fondazione Golgi Cenci, ItalyCopyright © 2023 Panes Lundmark, Josefsson and Rieckmann. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vania Panes Lundmark, dmFuaWEucGFuZXMtbHVuZG1hcmtAdW11LnNl; Anna Rieckmann, YW5uYS5yaWVja21hbm5AdW5pYncuZGU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.