- 1Department of Geriatrics and National Clinical Research Center for Geriatrics, West China Hospital/West China School of Medicine, Sichuan University, Sichuan, China
- 2Health Management Center, General Practice Center, National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University, Sichuan, China
Objective: Early identification of delirium, which often occurs in older patients, can effectively reduce adverse prognoses. One way to increase the detection rate of delirium is to use an effective ultrabrief instrument for higher-frequency screening. The purpose of this review is to evaluate the diagnostic accuracy of ultrabrief screening tools for delirium.
Methods: The Cochrane Library, PubMed and EMBASE were searched from January 1, 1974, to November 31, 2022. We assessed the measurement properties of screening instruments using the consensus-based standards for selecting health measurement instruments (COSMIN) checklist and evaluated the risk bias of the included studies using the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool. The diagnostic test accuracy of instruments for delirium was reported using sensitivity, specificity, positive likelihood ratio (PLR) and negative likelihood ratio (NLR).
Result: Of the 4,914 items identified, 26 met the eligibility criteria, resulting in 5 different delirium identification tools. The overall study quality assessed by the QUADAS-2 tool was moderate to good. Of the five screening tools, two instruments had sensitivity ≥80% and specificities ≥80%: 4AT and UB-2. The most comprehensive is the 4AT scale, which has a sensitivity of 0.80 [95% confidence interval (CI):0.68, 0.88] and a specificity of 0.89 (95%CI: 0.83, 0.93) and contains 4 items. UB-2 has a sensitivity of 0.88 (95%CI: 0.72, 0.96) and a specificity of 0.64 (95%CI: 0.56, 0.70).
Conclusion: UB-2 and MOTYB had excellent sensitivity for delirium screening at an early stage. In terms of sensitivity and intentionality, the 4AT is the best recommended scale.
Introduction
Delirium is the clinical manifestation of acute encephalopathy, which is characterized by acute disorders of consciousness, attention, and cognition that fluctuate over time and are fundamental criteria in delirium diagnosis (Oh et al., 2017). It is a common disease that affects many hospitalized patients, especially those aged 65 and over. Prolonged hospitalization and decreased cognitive ability are considered risk factors for delirium, while delirium itself is a known complication of dementia and is associated with an increased risk of death (Breitbart et al., 2002). Many cases of delirium are not recognized, which means that the opportunity for prevention has been lost (MacLullich and Hall, 2011). Early detection is helpful for treatment and could reduce the duration and adverse effects of delirium. Although delirium screening is the standard procedure in many hospitals, up to 72% of delirium events have not been found or misdiagnosed (de la Cruz et al., 2015). The failure may be due to the fluctuation of delirium symptoms. The patient may not have developed delirium at routine screening. Therefore, it is particularly important to screen for delirium multiple times per day or every day, as well as obtain collateral history from a reliable caregiver, to detect its fluctuating nature.
At present, there are more than 40 delirium instruments for different purposes (e.g., screening, diagnosis and severity), for different clinical environments (e.g., intensive care units, emergency departments and medical wards), and for different users (e.g., psychiatrists, geriatricians, nurses, and caregivers; Helfand et al., 2021). Such a large number of instruments not only makes the direct comparison of evaluation results challenging but also increases the difficulty of selecting instruments for clinical staff. To detect delirium more efficiently, it is best to use a simple and rapid instrument to screen delirium. We named this rapid delirium screening instrument with an evaluation time ≤2 min and a number of items ≤4 the ultrabrief delirium screening instrument. This means that they can be routinely used 2–3 times a day in clinical situations. Thus, the recognition of delirium by clinical staff can be improved.
At present, many delirium screening scales are committed to simplifying and improving delirium detection. The MOTYB (the months of the year backwards test) is a commonly used attention test (Ryan et al., 2018). The 4 ‘A’s test or 4AT is a short delirium assessment tool intended for clinical use in general settings when delirium is suspected and was initially published on a dedicated website in 2011 (Bellelli et al., 2014). UB-2 (ultrabrief screen), consisting of the two most sensitive items in the 3 min diagnostic CAM (3D-CAM) (Fick et al., 2015), was used recently and shown to be useful in delirium screening. While many systematic reviews of delirium instruments exist, they all focus on a certain instrument or comprehensive evaluation (Wong et al., 2010; Morandi et al., 2012; LaMantia et al., 2014; De and Wand, 2015; Jeong et al., 2020; Helfand et al., 2021). However, to the best of our knowledge, no systematic reviews have comprehensively compared the diagnostic accuracy between those different ultrabrief delirium screening instruments.
The objective of this review is threefold. First, we assessed the measurement properties of screening instruments using the consensus-based standards for selecting consensus-based standards for the selection of health status measurement instruments (COSMIN) checklist (Mokkink et al., 2009). Second, we evaluated the risk bias of study quality using the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool. Third, we examined the diagnostic accuracy of ultrabrief delirium screening instruments in various care settings. The findings of this investigation provide recommendations for the choice of ultrabrief screening tools for delirium.
Materials and methods
Literature search strategy
Two authors conducted independent literature searches. The Cochrane Library, PubMed and EMBASE were searched from January 1, 1974, to November 31, 2022. Studies were included when they met the following criteria: (1) reported at least one delirium screening instrument; (2) examination of diagnostic accuracy against a widely accepted diagnostic criterion of delirium, such as the Diagnostic and Statistical Manual of Mental Disorders (DSM, Version III, IV or V), the International Classification of Diseases (ICD), or recognized instruments for delirium assessment, such as the confusion assessment method (CAM) and delirium rating scale (DRS). Exclusion criteria were: (1) case series, comments, letters, protocol, meeting reports; (2) non-English-language publications; (3) studies on delirium in children; (4) the scales involved in the study do not meet the requirements that the average use time is ≤2 min and the number of items is ≤4. The search terms included the keywords “delirium” and “instrument,” as well as their known synonyms. The detailed search strategy is shown in the Supplementary material (supplement 1).
Study selection and data extraction
Two independent authors (YaL and ZL) screened the relevant literature by title and abstract and then read the full text to select eligible articles. Any disagreement was resolved by consulting a third author (JY). We collected the following information: sample size, language, study design, study sites, country, application of reference standard and examiner specialty. We also calculated/extracted the sensitivity, specificity, area under the ROC curve (AUC), and other diagnostic accuracy indices of each study.
Risk of bias assessment
Two independent review authors (YaL and ZL) assessed the methodological quality of the studies using the Diagnostic Accuracy Study Quality Assessment (QUADAS-2) tool. This tool is available at https://www.bris.ac.uk/quadas. The QUADAS-2 tool assessed the study quality from four aspects: participant selection, index test, reference standards, flow and timing. Differences were resolved by a third author (JY).
Measurement property assessment
We used the COSMIN guidelines to rate the measurement properties for each delirium screening instrument. The COSMIN checklist is a tool for assessing the reliability and validity of the screening instrument, which is available at https://www.cosmin.nl. We evaluated the screening instrument from six aspects: (1) content validity; (2) structural validity; (3) reliability; (4) internal consistency; (5) cross-cultural validity; and (6) criterion validity. We reviewed all relevant articles about each instrument to make an accurate decision. The ratings on each of the COSMIN criteria were summed and reported as a 0 to 6 score (Appendix 2) using an adaptation of the COSMIN scoring procedure published previously (Helfand et al., 2021). For reporting on each of these categories, the instruments were given one point; failure to report on these categories resulted in no points. Two authors carefully extracted information from each article according to the COSMIN framework.
Statistical analysis
Meta-analyses were performed using the Stata (version 16.0, StataCorp, TX, United States) MIDAS module. Sensitivity, specificity, positive likelihood ratio (PLR), negative likelihood ratio (NLR), and area under the curve (AUC) were used to report diagnostic test accuracy for delirium instruments. Sensitivity, specificity, and likelihood ratios were calculated from the raw data and then rounded for display in the data tables. In general, larger PLRs and smaller NLRs indicate better diagnostic performance. AUC ≥0.9 indicates high diagnostic accuracy, 0.7–0.9 indicates moderate diagnostic capability, and 0.5–0.7 indicates low accuracy.
Heterogeneity was divided into low, moderate, and high with I2 values of 25%, 50%, and 75%, respectively. To explore the sources of heterogeneity, we performed a subgroup analysis for different sites (ICU or non-ICU). To investigate the robustness we found, we performed sensitivity analyses. We analysed only DSM standard studies. We evaluated the publication bias of all eligible studies using Deek’s funnel plot.
Results
Selection process
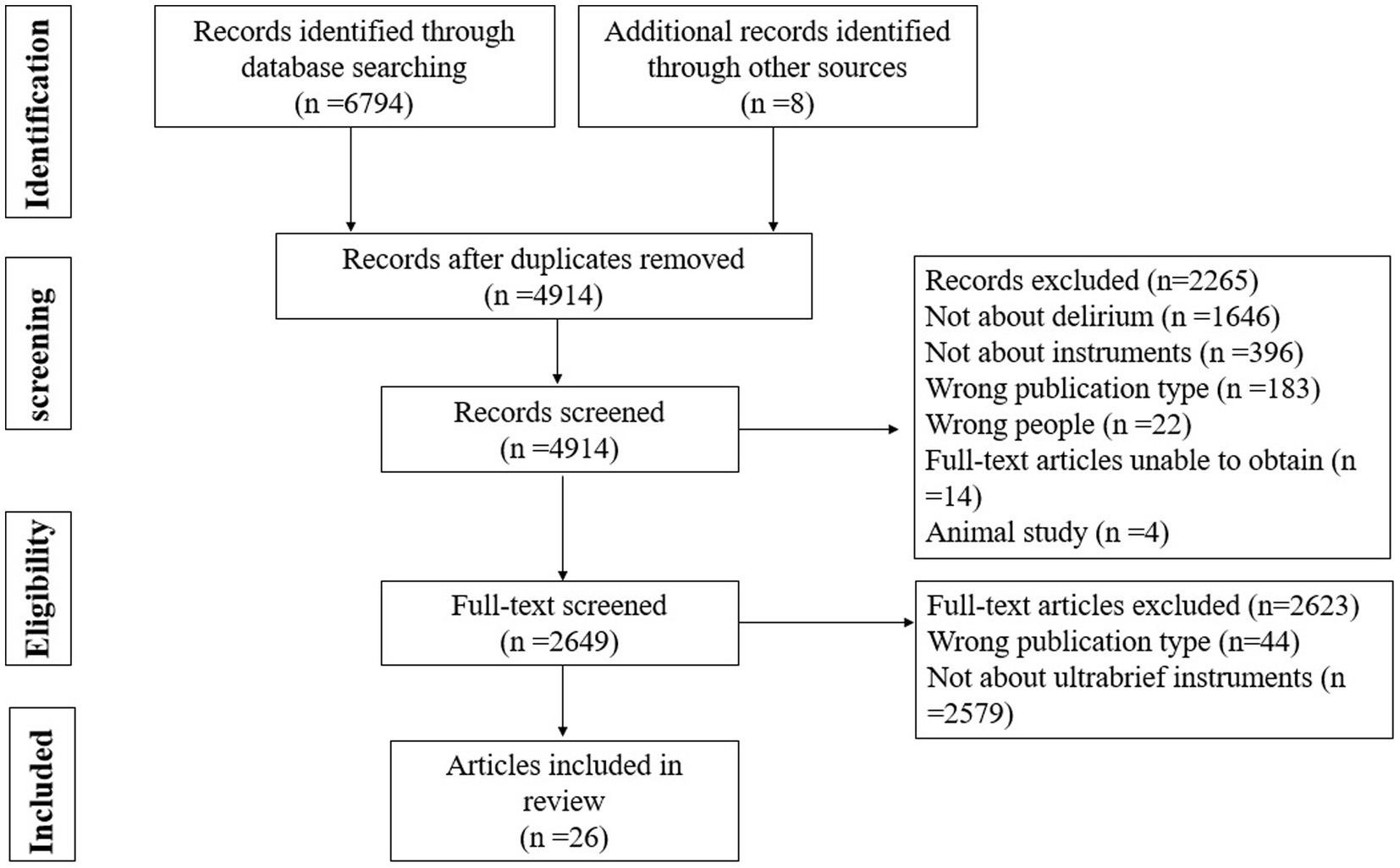
Figure 1 displays the PRISMA flowchart of the literature search and selection. We retrieved 4,914 potentially relevant records. A total of 2,265 records were excluded after title and abstract screening. Finally, 2,649 full texts were screened, of which 26 articles reporting five delirium screening instruments met the eligibility criteria and were included in this review. Five screening tools are 4AT (Robson et al., 2017), MOTYB (Marra et al., 2018), O3DY (Bédard et al., 2019), AMT-4 (Swain and Nightingale, 1997) and UB-2 (Fick et al., 2015).
Study characteristics
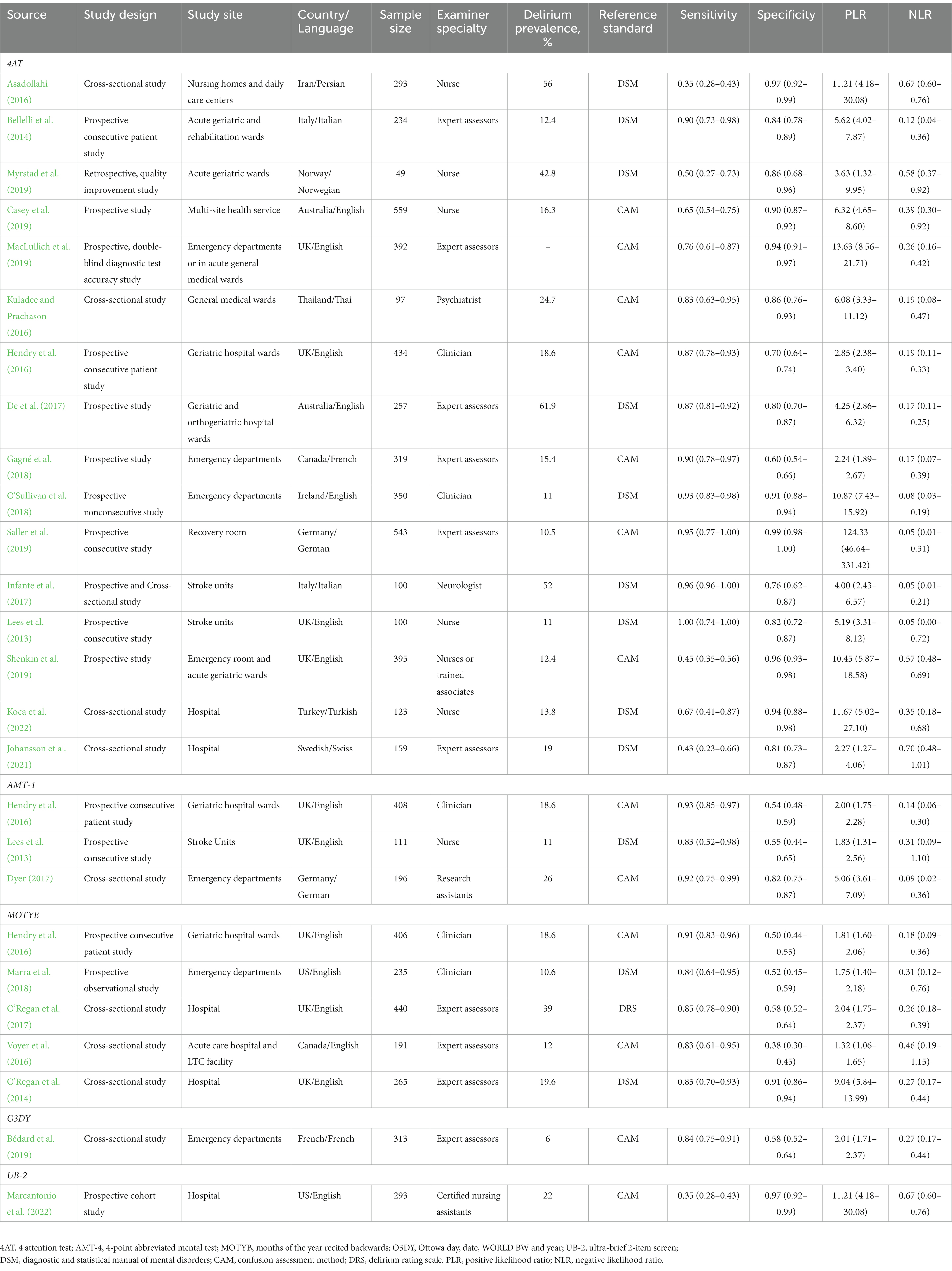
Table 1 shows the characteristics of all 26 included studies. A total of 7,262 participants were included. Eight studies (30.8%) were developed in ICUs, 3 studies (11.5%) were developed in stroke units, and 15 studies (57.7%) were conducted in non-ICUs. The gold standards used in each of the 26 articles include DSM (46.2%), CAM (50%), and DRS (3.8%).
Study quality assessed By The QUADAS-2 tool
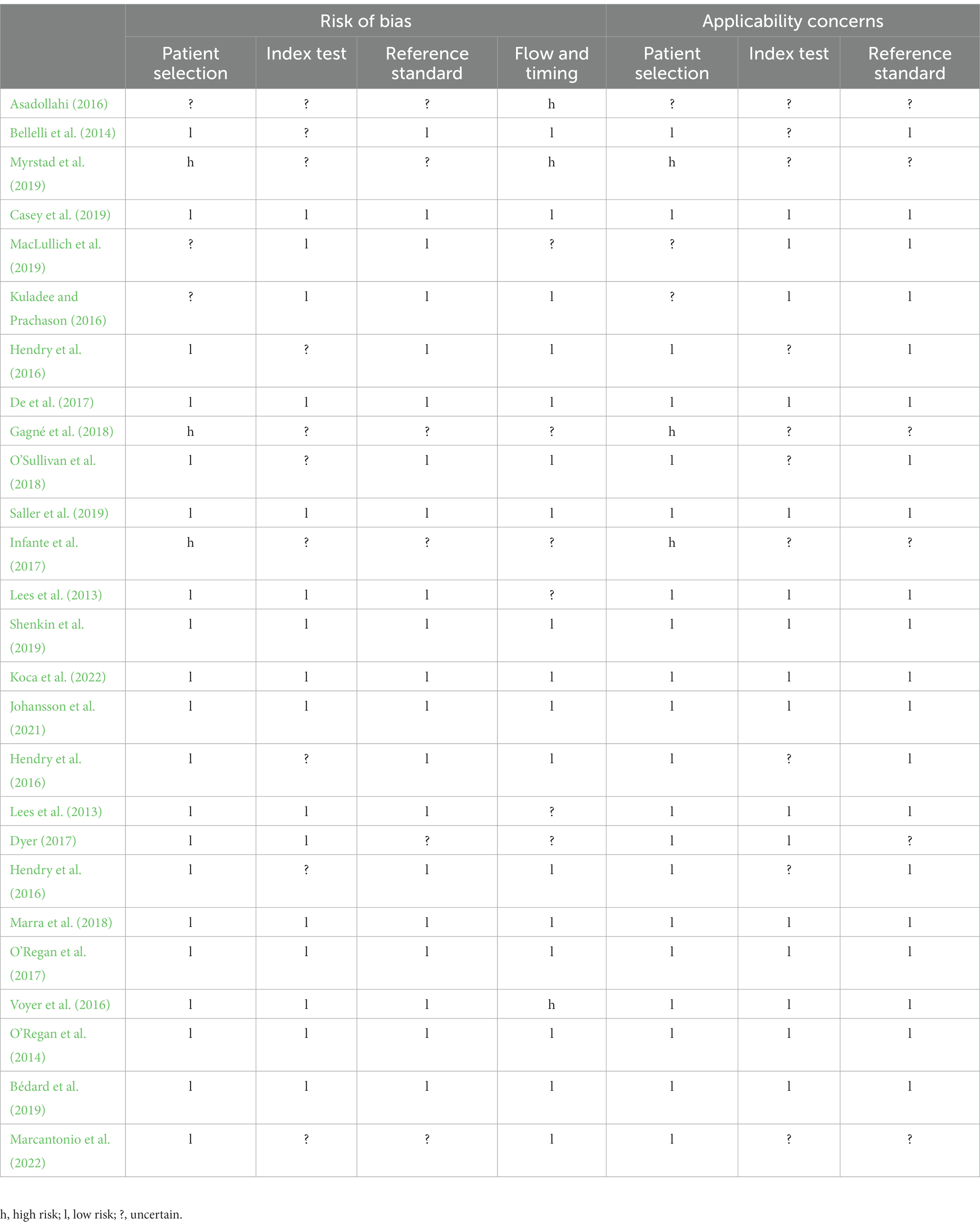
Table 2 summarizes the study quality risk biases assessed by the QUADAS-2 tool. The overall risk of bias was rated as low to moderate. Eight studies were considered to have low-risk bias. Fourteen studies were rated as having a high risk. Potential biases for our systematic review were listed as follows: (1) participant selection (e.g., ICU or non-ICU patients); (2) secondary analysis of retrospective studies was also considered high risk. The retrospective design may have introduced selection bias.
COSMIN assessment of screening instruments
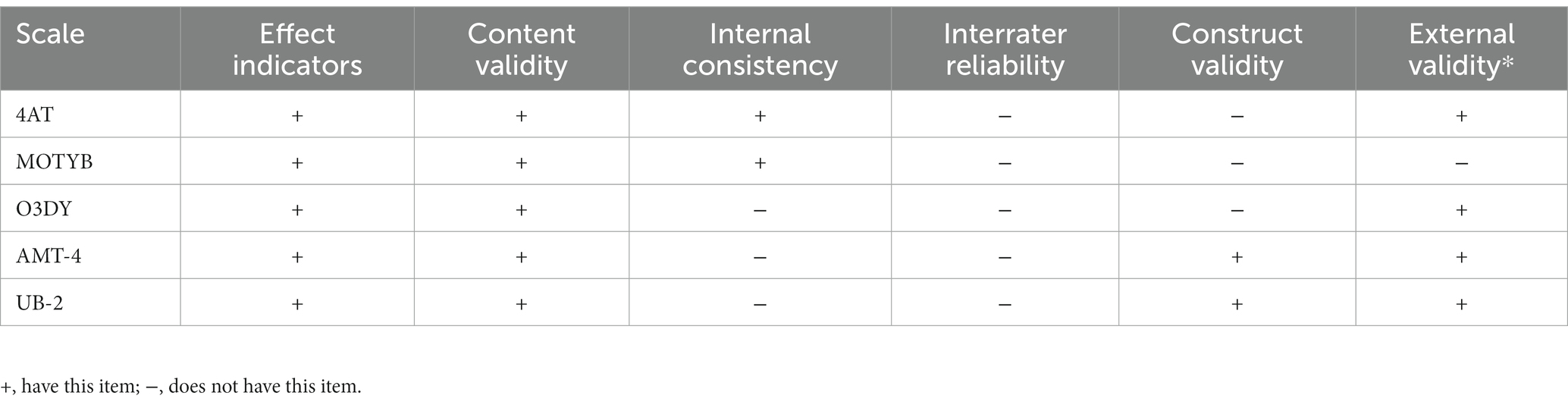
We used the COSMIN standards to assess the psychometric properties (reliability and validity) of five screening tools. We chose the single earliest publication for each instrument. The summarized COSMIN assessment results are shown in Table 3. None of the included studies reported internal reliability. All five instruments have internal consistency and effect indicators. The 4AT and MOTYB have good content validity. The AMT-4 and UB-2 have adequate construct validity. For external validity, the MOTYB is the only one that lacks it.
Diagnostic accuracy of screening tools
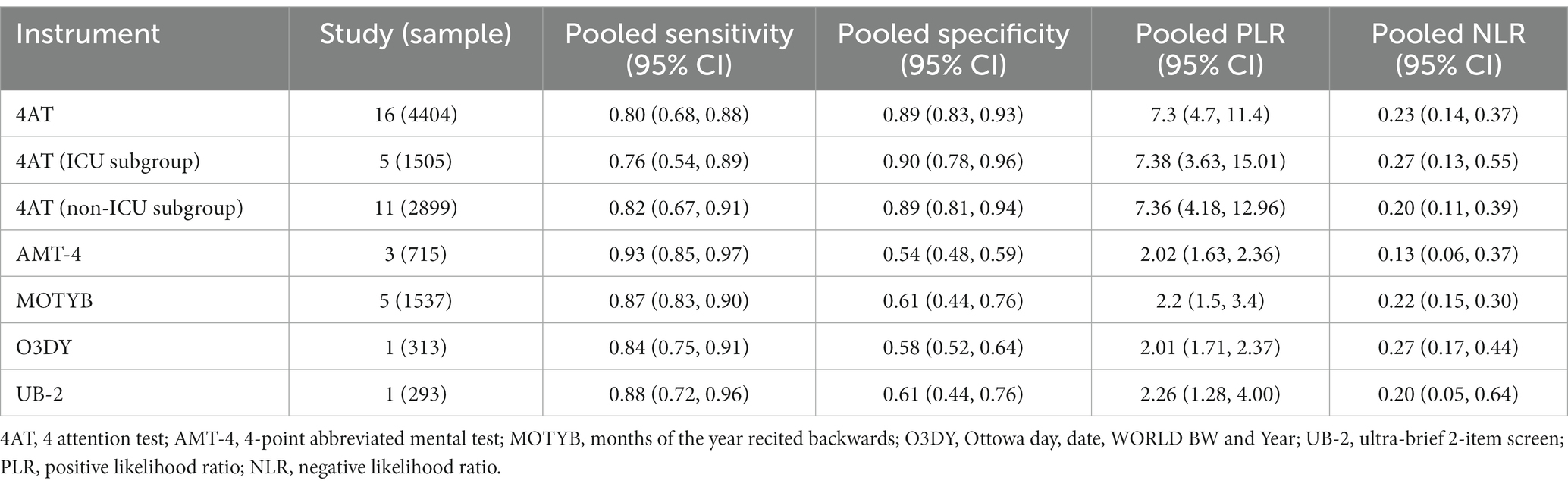
Studies have reported data on the diagnostic accuracy of all five screening tools for delirium: the 4AT, the MOTYB, the AMT-4, the O3DY, and the UB-2 (Table 3).
The 4AT (n = 16 studies) had a pooled sensitivity of 80% [95% confidence interval (CI): 68%–88%] and a pooled specificity of 89% (95% CI: 83%–93%); the pooled PLR and NLR were 7.3 (95% CI: 4.7–11.4) and 0.23 (95% CI: 0.14–0.37), respectively. The pooled estimates of sensitivity and specificity for the MOTYB (n = 5 studies) were 87% (95% CI: 83%–90%) and 61% (95% CI: 44%–76%), respectively; the pooled PLR and NLR were 2.2 (95% CI: 1.5–3.4) and 0.22 (95% CI: 0.15–0.30), respectively. The AMT-4 had a sensitivity of 93% [95% CI: 85%–97%] and a specificity of 54% (95% CI: 48%–59%); the O3DY had a sensitivity of 84% [95% CI: 75%–91%] and a specificity of 58% (95% CI: 52%–64%); and the UB-2 had a sensitivity of 88% [95% CI: 72%–96%] and a specificity of 61% (95% CI: 44%–76%). More details, such as the pooled PLR and NLR, are shown in Table 4.
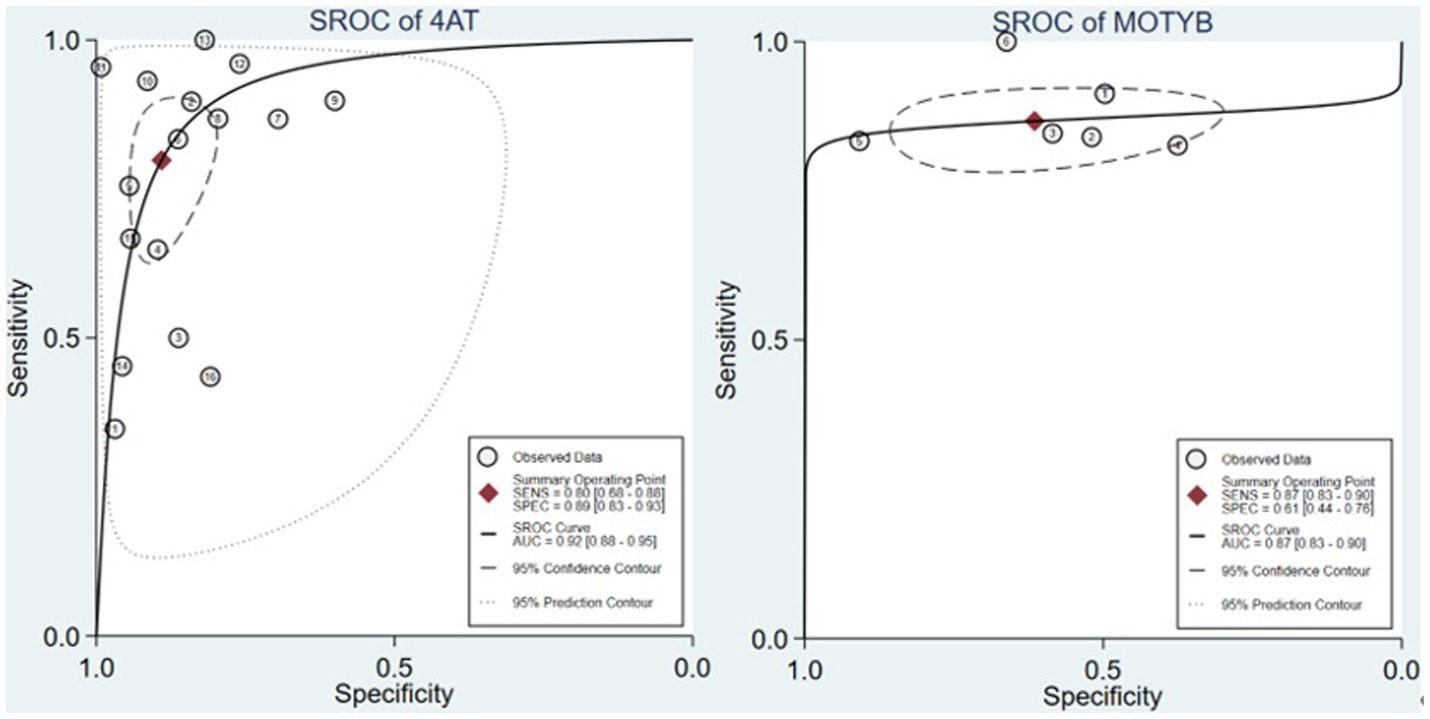
The summary receiver operating characteristic (SROC) curves can eliminate the threshold effects of the instrument to predict overall accuracy. By the SROC curves of Figure 2, the 4AT had a higher AUC (n = 16 studies, AUC = 0.92) than MOTYB (n = 5 studies, AUC = 0.87). AMT-4, O3DY and UB-2 did not conduct SROC due to the lack of relevant research.
Subgroup analysis
We performed a subgroup analysis of different sites (ICU or non-ICU) where 4AT was used. In the ICU, 4AT had a sensitivity of 76% (95% CI: 54%–89%) and a specificity of 90% (95% CI: 78%–96%); in the non-ICU, 4AT had a higher sensitivity of 82% (95% CI: 67%–91%) and a lower specificity of 89% (95% CI: 81%–94%). The PLR and NLR of the ICU were 7.4 (95% CI: 3.6–15.0) and 0.3 (95% CI: 0.1–0.6); those of the ICU were 7.4 (95% CI: 4.2–13.0) and 0.2 (95% CI: 0.1–0.4), respectively.
Sensitivity analysis and publication bias
After the exclusion of non-DSM standard studies, the pooled sensitivity, specificity, PLR, and NLR for the 4AT were 80% (95% CI: 61%–92%), 88% (95% CI: 82%–92%), 6.5 (95% CI: 4.5–9.2), and 0.22 (95% CI: 0.10–0.48), respectively. MOTYB, AMT-4, O3DY and UB-2 did not conduct sensitivity analysis due to the lack of enough studies.
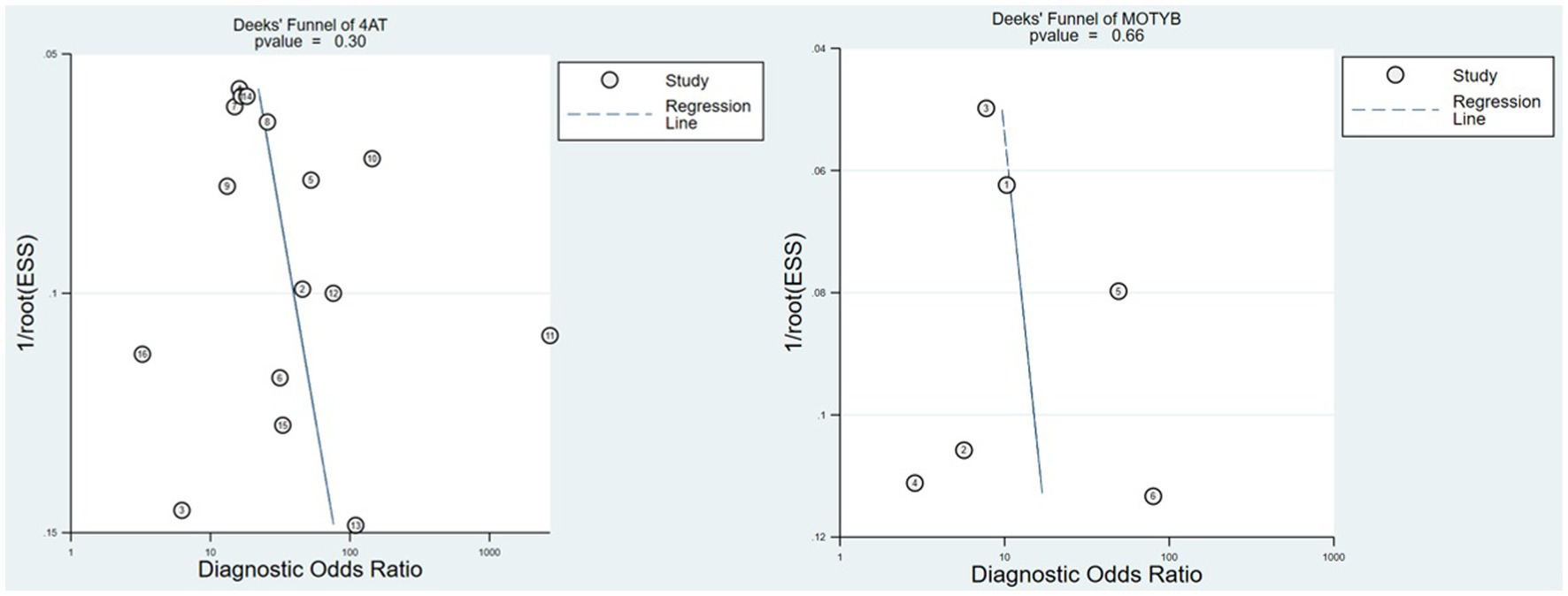
Deeks’ funnel plots revealed no evidence of publication bias, as shown in Figure 3 (4AT p = 0.3, MOTYB p = 0.66). We did not assess the publication bias of the AMT-4, O3DY and UB-2 because not enough studies were included.
Discussion
Accurate recognition of delirium is clinically important to effectively provide clinical care and reduce late complications. To promote the detection rate of delirium, it is important to select appropriate methods and use them at least twice a day. Five instruments were included in our systematic review and showed that they may be used for multiple rapid screenings of delirium in clinical practice. The study quality of this meta-analysis was moderate to good overall, according to the QUADAS-2 assessment. Of the five screening tools, two instruments had sensitivity ≥80% and specificities ≥80%: 4AT and UB-2. These two instruments have unique strengths and limitations, and several potential scenarios for their use are provided here. Based on our recommended principles, we recommend 4AT as a clinical daily multiple rapid screening instrument.
The 4AT test includes two simple cognitive screening items. It is short (only 4 items and generally <2 min; Tieges et al., 2021), does not need special training, is easy to manage (including people with visual or hearing impairment), does not need physical response, and allows the evaluation of patients who “cannot be tested” (those who cannot be tested or interviewed due to severe sleepiness or excitement). 4AT has experienced several pilot rounds and has been used in many hospitals in the United Kingdom and internationally. The 4AT had a sensitivity of 80% and specificity of 89%, with a PLR of 7.3 and an NLR of 0.22. Although the 4AT has high sensitivity and specificity, it has the longest use time among the five scales included. There is a dynamic balance between performance and simplicity. Fortunately, we limited the ultrabrief scale when we included the article and then chose the best performance from it.
At present, there are few relevant studies on UB-2, which has only been verified in the United States. UB-2 is extracted from 3D-CAM (Fick et al., 2015), but the author does not recommend using UB-2 alone to diagnose delirium but uses the UB-CAM framework. Even UB-2 had a sensitivity of 88% and specificity of 64%, with a PLR of 2.4 and an NLR of 0.34. Another important item excluded by the author is “Does the patient report feeling confused?” That is, if these three items are positive, delirium can be directly diagnosed. More evidence of this screening tool is needed in the future.
Among the remaining five scales, MOTYB is the most studied. However, MOTYB, as a scale with only one test item, is extremely simplified in operation, but it has a low specificity of 61%. The five scales involved do not involve delusion, while a scale involving delusion, Nu-DESC, does not meet the criteria of the ultrasimple scale. The remaining three scales involved in this study have a common problem: there are too few original studies directly related to delirium, of which UB-2 lacks relevant studies due to its late launch.
Notably, AMT-4 itself is a part of the 4AT. Although the number of entries in the strict sense of the word is more than 4, in the practical application of the 4AT, the four questions about the AMT-4 can be asked in one question in one book,1 and it is not necessary to count the scores of each question but only the number of wrong answers, so it can be regarded as one item. This is different from using the RASS to evaluate the level of consciousness. RASS cannot be simplified into one problem (Ely et al., 2003).
This study has several advantages. First, we evaluated all screening tools’ COSMIN quality and evaluated the QUADAS-2 risk bias of the included studies. Second, we also followed the principle of a double review process and developed an evidence-based process for quality assessment. The methodological quality of the included studies was moderate to good overall. There have been many systematic evaluations of delirium screening instruments before (Wong et al., 2010), and they are constantly updated; however, this paper focuses on simplifying the instrument and achieving the screening effect as efficiently as possible.
There are several limitations to this study. First, the description of the use duration in each study is different, which is different from the actual use duration in other institutions. For this reason, after the description of the original literature and the actual simulation of the expert team, we have comprehensively set the duration and set it as the interval value after discussion. Second, many scales were designed for different user groups at the beginning of the design when the scale was included, so some scales had design defects, which led to poor final results and were finally eliminated. For example, the Delirium Triage Screen (DTS)/Brief CAM (b-CAM) itself was a simple enough screening strategy (Rieck et al., 2020), but the combination of the two parts exceeded the limit of items and was eliminated. This part of the scale should be classified and discussed in detail. Then, the evaluation of consciousness level in many scales is unclear (such as BCS). After we replace RASS, the number of items and operation time will be exceeded, and we have to abandon it. If there is a simpler way to assess the level of awareness, this part of the scale should also be included in the discussion. Finally, the scale recommended in this study is the 4AT. Although there is no language restriction, the scale included in this study is all in English, which obviously limits the strength of evidence for the use of the scale in other language regions.
This article provides an overview of the delirium scale that can be used for daily multiple screening in clinical work. Different assessors will choose different scales for screening in different clinical environments, but these scales may not be suitable for multiple use every day. This paper recommends a comprehensive and ideal scale “4AT,” which has a very high coverage of standard diagnostic criteria, which means that under ideal conditions, it can be used as the final diagnostic scale without requiring a professional doctor to diagnose. Moreover, because of the ultrasimple characteristics of 4AT, it can be used in clinical practice many times a day, which can reduce the delirium ignored due to the fluctuation of delirium, improve the detection rate, and ensure a good prognosis through early prevention.
In view of the high specificity of 4AT in the subgroup of nondementia patients and the high sensitivity of the subgroup of dementia patients, an important area of future research may be to improve the scale to improve its ability to identify delirium in dementia patients. It is hoped that the work of this paper will help improve the detection rate of delirium in clinical work and lay a foundation for promoting research in the field of delirium.
This study comprehensively summarized delirium screening tools based on the COSMIN guidelines. Five screening instruments were available, and the methodological quality assessment of the included studies by the QUADAS-2 tool was moderate to good. UB-2 and MOTYB had excellent sensitivity for delirium screening at an early stage. In terms of sensitivity and intentionality, the 4AT is the best recommended scale according to the results of this study.
Author contributions
YaL and JY: study concept and design. YaL, ZL, and YiL: acquisition of data. YiL and YaL: analysis and interpretation of data. YaL and ZL: drafting of the manuscript. JY and NG: critical revision of the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Key Research and Development Program of China (no. 2020YFC2005300), Sichuan Science and Technology Program (2022ZDZX0021; 2021YFS0139), 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYJC21005).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1166392/full#supplementary-material
Footnotes
1. ^ www.the4AT.com
References
Asadollahi, A., and Fanisaberi, L. (2016). Iranian Version of 4AT, an Instrument for Rapid Delirium Screening for Later Life.
Bédard, C., Boucher, V., Voyer, P., Yadav, K., Eagles, D., Nadeau, A., et al. (2019). Validation of the O3DY French version (O3DY-F) for the screening of cognitive impairment in community seniors in the emergency department. J. Emerg. Med. 57, 59–65. doi: 10.1016/j.jemermed.2019.02.007
Bellelli, G., Morandi, A., Davis, D. H. J., Mazzola, P., Turco, R., Gentile, S., et al. (2014). Validation of the 4AT, a new instrument for rapid delirium screening: a study in 234 hospitalised older people. Age Ageing 43, 496–502. doi: 10.1093/ageing/afu021
Breitbart, W., Gibson, C., and Tremblay, A. (2002). The delirium experience: delirium recall and delirium-related distress in hospitalized patients with cancer, their spouses/caregivers, and their nurses. Psychosomatics 43, 183–194. doi: 10.1176/appi.psy.43.3.183
Casey, P., Dārziņš, P., Webb-St Mart, M., Baldwin, C., Riddell, K., Johnson, C., et al. (2019). Evaluation of a method to estimate the point prevalence of cognitive impairment and delirium in a multi-campus Australian health service. Australas. J. Ageing 38, 258–266. doi: 10.1111/ajag.12666
de la Cruz, M., Fan, J., Yennu, S., Tanco, K., Shin, S. H., Wu, J., et al. (2015). The frequency of missed delirium in patients referred to palliative care in a comprehensive cancer center. Support. Care Cancer 23, 2427–2433. doi: 10.1007/s00520-015-2610-3
De, J., and Wand, A. P. (2015). Delirium screening: a systematic review of delirium screening tools in hospitalized patients. Gerontologist 55, 1079–1099. doi: 10.1093/geront/gnv100
De, J., Wand, A. P. F., Smerdely, P. I., and Hunt, G. E. (2017). Validating the 4A's test in screening for delirium in a culturally diverse geriatric inpatient population. Int. J. Geriatr. Psychiatry 32, 1322–1329. doi: 10.1002/gps.4615
Dyer, A. H., Briggs, R., Nabeel, S., O’Neill, D., and Kennelly, S. P. (2017). The Abbreviated Mental Test 4 for cognitive screening of older adults presenting to the Emergency Department. Eur J Emerg Med. 24, 417–422. doi: 10.1097/MEJ.0000000000000394
Ely, E. W., Truman, B., Shintani, A., Thomason, J. W., Wheeler, A. P., Gordon, S., et al. (2003). Monitoring sedation status over time in ICU patients. JAMA 289, 2983–2991. doi: 10.1001/jama.289.22.2983
Fick, D. M., Inouye, S. K., Guess, J., Ngo, L. H., Jones, R. N., Saczynski, J. S., et al. (2015). Preliminary development of an ultrabrief two-item bedside test for delirium. J. Hosp. Med. 10, 645–650. doi: 10.1002/jhm.2418
Gagné, A. J., Voyer, P., Boucher, V., Nadeau, A., Carmichael, P. H., Pelletier, M., et al. (2018). Performance of the French version of the 4AT for screening the elderly for delirium in the emergency department. CJEM 20, 903–910. doi: 10.1017/cem.2018.367
Helfand, B. K. I., D’Aquila, M. L., Tabloski, P., Erickson, K., Yue, J., Fong, T. G., et al. (2021). Detecting delirium: a systematic review of identification instruments for non-ICU settings. J. Am. Geriatr. Soc. 69, 547–555. doi: 10.1111/jgs.16879
Hendry, K., Quinn, T. J., Evans, J., Scortichini, V., Miller, H., Burns, J., et al. (2016). Evaluation of delirium screening tools in geriatric medical inpatients: a diagnostic test accuracy study. Age Ageing 45, 832–837. doi: 10.1093/ageing/afw130
Infante, M. T., Pardini, M., Balestrino, M., Finocchi, C., Malfatto, L., Bellelli, G., et al. (2017). Delirium in the acute phase after stroke: comparison between methods of detection. Neurol. Sci. 38, 1101–1104. doi: 10.1007/s10072-017-2832-x
Jeong, E., Park, J., and Lee, J. (2020). Diagnostic test accuracy of the 4AT for delirium detection: a systematic review and Meta-analysis. Int. J. Environ. Res. Public Health 17:15. doi: 10.3390/ijerph17207515
Johansson, Y. A., Tsevis, T., Nasic, S., Gillsjö, C., Johansson, L., Bogdanovic, N., et al. (2021). Diagnostic accuracy and clinical applicability of the Swedish version of the 4AT assessment test for delirium detection, in a mixed patient population and setting. BMC Geriatr. 21:568. doi: 10.1186/s12877-021-02493-3
Koca, M., Öztürk, Y., Boğa, İ., Bürkük, S., Eşme, M., Akyürek, Y., et al. (2022). A quality improvement study on delirium awareness day: in pursuit of missed delirium diagnoses. J. Gerontol. Nurs. 48, 43–51. doi: 10.3928/00989134-20220630-03
Kuladee, S., and Prachason, T. (2016). Development and validation of the Thai version of the 4 'A's test for delirium screening in hospitalized elderly patients with acute medical illnesses. Neuropsychiatr. Dis. Treat. 12, 437–443. doi: 10.2147/ndt.s97228
LaMantia, M. A., Messina, F. C., Hobgood, C. D., and Miller, D. K. (2014). Screening for delirium in the emergency department: a systematic review. Ann. Emerg. Med. 4, S82–S83. doi: 10.1016/j.annemergmed.2013.11.010
Lees, R., Corbet, S., Johnston, C., Moffitt, E., Shaw, G., and Quinn, T. J. (2013). Test accuracy of short screening tests for diagnosis of delirium or cognitive impairment in an acute stroke unit setting. Stroke 44, 3078–3083. doi: 10.1161/strokeaha.113.001724
MacLullich, A. M., and Hall, R. J. (2011). Who understands delirium? Age Ageing 40, 412–414. doi: 10.1093/ageing/afr062
MacLullich, A. M., Shenkin, S. D., Goodacre, S., Godfrey, M., Hanley, J., Stíobhairt, A., et al. (2019). The 4 'A's test for detecting delirium in acute medical patients: a diagnostic accuracy study. Health Technol. Assess. 23, 1–194. doi: 10.3310/hta23400
Marcantonio, E. R., Fick, D. M., Jung, Y., Inouye, S. K., Boltz, M., Leslie, D. L., et al. (2022). Comparative implementation of a brief app-directed protocol for delirium identification by hospitalists, nurses, and nursing assistants: a cohort study. Ann. Intern. Med. 175, 65–73. doi: 10.7326/m21-1687
Marra, A., Jackson, J. C., Ely, E. W., Graves, A. J., Schnelle, J. F., Dittus, R. S., et al. (2018). Focusing on inattention: the diagnostic accuracy of brief measures of inattention for detecting delirium. J. Hosp. Med. 13, 551–557. doi: 10.12788/jhm.2943
Mokkink, L. B., Terwee, C. B., Stratford, P. W., Alonso, J., Patrick, D. L., Riphagen, I., et al. (2009). Evaluation of the methodological quality of systematic reviews of health status measurement instruments. Qual. Life Res. 18, 313–333. doi: 10.1007/s11136-009-9451-9
Morandi, A., McCurley, J., Vasilevskis, E. E., Fick, D. M., Bellelli, G., Lee, P., et al. (2012). Tools to detect delirium superimposed on dementia: a systematic review. J. Am. Geriatr. Soc. 60, 2005–2013. doi: 10.1111/j.1532-5415.2012.04199.x
Myrstad, M., Watne, L. O., Johnsen, N. T., Børs-Lind, E., and Neerland, B. E. (2019). Delirium screening in an acute geriatric ward by nurses using 4AT: results from a quality improvement project. Eur. Geriatr. Med. 10, 667–671. doi: 10.1007/s41999-019-00215-y
O’Regan, N. A., Maughan, K., Liddy, N., Fitzgerald, J., Adamis, D., Molloy, D. W., et al. (2017). Five short screening tests in the detection of prevalent delirium: diagnostic accuracy and performance in different neurocognitive subgroups. Int. J. Geriatr. Psychiatry 32, 1440–1449. doi: 10.1002/gps.4633
O’Regan, N. A., Ryan, D. J., Boland, E., Connolly, W., McGlade, C., Leonard, M., et al. (2014). Attention! A good bedside test for delirium? J. Neurol. Neurosurg. Psychiatry 85, 1122–1131. doi: 10.1136/jnnp-2013-307053
O’Sullivan, D., Brady, N., Manning, E., O’Shea, E., O’Grady, S., O’Regan, N., et al. (2018). Validation of the 6-item cognitive impairment test and the 4AT test for combined delirium and dementia screening in older emergency department attendees. Age Ageing 47, 61–68. doi: 10.1093/ageing/afx149
Oh, E. S., Fong, T. G., Hshieh, T. T., and Inouye, S. K. (2017). Delirium in older persons: advances in diagnosis and treatment. JAMA 318, 1161–1174. doi: 10.1001/jama.2017.12067
Rieck, K. M., Pagali, S., and Miller, D. M. (2020). Delirium in hospitalized older adults. Hosp Pract. 48, 3–16. doi: 10.1080/21548331.2019.1709359
Robson, C., Cheong, P., Walker, I., and Garbharran, U. (2017). 4AT vs CAM in diagnosis of delirium: a junior doctor’s view. Age Ageing 46:i41, –i43. doi: 10.1093/ageing/afx060.149
Ryan, S., Hayes, D., and Creedon, B. (2018). Use of "months of the year backwards" (MOTYB) as a screening tool for delirium in palliative care patients in the acute hospital setting. Ir. Med. J. 111:801.
Saller, T., MacLullich, A. M. J., Schäfer, S. T., Crispin, A., Neitzert, R., Schüle, C., et al. (2019). Screening for delirium after surgery: validation of the 4 A's test (4AT) in the post-anaesthesia care unit. Anaesthesia 74, 1260–1266. doi: 10.1111/anae.14682
Shenkin, S. D., Fox, C., Godfrey, M., Siddiqi, N., Goodacre, S., Young, J., et al. (2019). Delirium detection in older acute medical inpatients: a multicentre prospective comparative diagnostic test accuracy study of the 4AT and the confusion assessment method. BMC Med. 17:138. doi: 10.1186/s12916-019-1367-9
Swain, D. G., and Nightingale, P. G. (1997). Evaluation of a shortened version of the abbreviated mental test in a series of elderly patients. Clin. Rehabil. 11, 243–248. doi: 10.1177/026921559701100308
Tieges, Z., Maclullich, A. M. J., Anand, A., Brookes, C., Cassarino, M., O’connor, M., et al. (2021). Diagnostic accuracy of the 4AT for delirium detection in older adults: systematic review and meta-analysis. Age Ageing 50, 733–743. doi: 10.1093/ageing/afaa224
Voyer, P., Champoux, N., Desrosiers, J., Landreville, P., Monette, J., Savoie, M., et al. (2016). Assessment of inattention in the context of delirium screening: one size does not fit all! Int. Psychogeriatr. 28, 1293–1301. doi: 10.1017/s1041610216000533
Keywords: delirium, measurement, systematic review, psychometrics, older patients
Citation: Liu Y, Li Z, Li Y, Ge N and Yue J (2023) Detecting delirium: a systematic review of ultrabrief identification instruments for hospital patients. Front. Psychol. 14:1166392. doi: 10.3389/fpsyg.2023.1166392
Edited by:
Alexandra Wolf, RIKEN Center for Advanced Intelligence Project (AIP), JapanReviewed by:
Hany Ibrahim, Ain Shams University, EgyptEleonora Orena, IRCCS Carlo Besta Neurological Institute Foundation, Italy
Copyright © 2023 Liu, Li, Li, Ge and Yue. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jirong Yue, eXVlamlyb25nMTFAaG90bWFpbC5jb20=
†These authors have contributed equally to this work and share first authorship
 Yadong Liu
Yadong Liu Zhenzhen Li2†
Zhenzhen Li2† Ying Li
Ying Li Ning Ge
Ning Ge Jirong Yue
Jirong Yue