
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 27 June 2023
Sec. Quantitative Psychology and Measurement
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1157636
 Liliana Dell’Osso†
Liliana Dell’Osso† Benedetta Nardi*†
Benedetta Nardi*† Chiara Bonelli
Chiara Bonelli Davide Gravina
Davide Gravina Francesca Benedetti
Francesca Benedetti Luca Del Prete
Luca Del Prete Gabriele Massimetti
Gabriele Massimetti Giulia Amatori
Giulia Amatori Barbara Carpita
Barbara Carpita Ivan Mirko Cremone
Ivan Mirko CremoneAim: In the recent years, a rising amount of research has stressed the importance of a dimensional perspective on mental disorders. In particular, the conceptualization of an obsessive–compulsive spectrum appears to be in line with the very first descriptions of Obsessive–Compulsive Disorder and has been partially acknowledged by the inclusion of the “OCD-spectrum related syndromes and disorders” section in the DSM-5. The goal of the current study is to ascertain the psychometric characteristics of the Obsessive–Compulsive Spectrum–Short Version (OBS-SV), a novel questionnaire designed to measure the complete range of obsessive–compulsive symptoms, from severe full blown to subthreshold ones.
Methods: Forty three subjects with a clinical diagnosis of OCD according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5); 42 subjects with a clinical diagnosis of social anxiety disorder (SAD), and 60 individuals without current or lifetime mental disorders (HC) were recruited from the Psychiatric Clinic of the University of Pisa. Subjects were assessed with the SCID-5, the Yale Brown Obsessive Compulsive Scale (Y-BOCS) and the OBS-SV.
Results: OBS-SV showed strong test–retest reliability for both the total and the domains scores, as well as a high level of internal consistency. The Pearson’s coefficients for the OBS-SV domain scores ranged from 0.771 to 0.943, and they were positively and strongly linked with one another (p < 0.001). The OBS-SV total score had a strong correlation with each of the OBS-SV domain scores. All correlation coefficients between OBS-SV and additional measures of OCS were observed to be strong, significant and positive. Both OBS-SV domain and overall score differences between diagnostic groups were found to be statistically significant. From HCs, to the SAD, up to the OC group, which had the highest values, the OBS-SV total score grew dramatically and progressively.
Conclusion: The OBS-SV demonstrated significant convergent validity with other dimensional OCD measures, excellent internal consistency, and test–retest reliability. Across the three diagnostic categories, the questionnaire functioned differently, with a rising score gradient from healthy controls through SAD patients to OCD subjects.
The Obsessive–Compulsive Disorder (OCD) is a severe chronic illness that affects a significant portion of the world’s population and, also due its limited response to pharmacological treatments, often represent one of the major management challenges for clinical psychiatrists (Karno et al., 1988). OCD is characterized by the presence of obsessions and compulsions; although the presence of only one of these two symptoms is sufficient for receiving an OCD diagnosis, patients typically display both of them (American Psychiatric Association, 2013, 2023). Obsessions are persistent and recurrent thoughts, impulses, or urges that makes the individual feel uncomfortable or anxious. These can be differentiated from delusions since they are frequently perceived as intrusive or ego-dystonic, and they are typically recognized as unrealistic or exaggerated, although the difference can become hazy in some circumstances. Compulsions, on the other hand, are repetitive behaviors or mental acts carried out with the aim to prevent dreaded events or reduce anxiety and distress, frequently in response to obsessions (American Psychiatric Association, 2013, 2023). A recent national survey highlighted that OCD has a lifetime prevalence of 2–3% and it is often associated with other comorbid mental disorders, although prevalence rates may vary depending on specific regional areas (Fontenelle et al., 2006; Kessler et al., 2012). Despite the majority clinical researches on OCD have focused on the full-blown condition (Grant et al., 2012), the literature is stressing how, like many other psychiatric disorders, OCD can also occur in a milder subsyndromal form: in light of a dimensional approach to psychopathology, subthreshold obsessive–compulsive (OC) traits can be found continuously distributed in the general population (Chamberlain et al., 2005; Grant and Chamberlain, 2019). In addition, OC traits have been observed in clinical population of patients with different psychiatric conditions, such as autism spectrum disorder (Postorino et al., 2017; Pazuniak and Pekrul, 2020), mood disorders (Tonna et al., 2021), feeding and eating disorders (Amianto et al., 2022; Reilly et al., 2022), personality disorders (McKay et al., 2000) and even catatonic manifestations (Mukai et al., 2011).
The main international classifications of mental disorders, the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Classification of Diseases (ICD), in their most recent version successfully focused on increasing the specificity of psychiatric nomenclature. However, due the rigidity of the categorical system failed to adequately represent the full spectrum of potentially distressing psychopathological symptoms with which the patient may come to clinical attention. This spectrum of manifestation comprehends a wide range of subclinical, atypical, prodromal or residual symptoms and traits that may have an impact on subject’s quality of life although not being sufficient for receiving a full-blown diagnosis (Angst et al., 1997; Pincus et al., 1999; Helmchen and Linden, 2000).
A spectrum model of psychopathology is more useful for identifying the broad sub-threshold conditions that may coexist with the main psychiatric diseases (Frank et al., 1998). Traditionally, in this framework the word “spectrum” has been employed to emphasize the connection between different symptomatic clusters or between different levels of severity of a same disorder (Akiskal and Akiskal, 1992) or different disorders (Hollander and Wong, 1995). Starting from these considerations, at the beginning of the current century was developed the “Collaborative Spectrum Project” with the aim to describe and better characterize the subtle and atypical signs linked to numerous DSM disorders (Cassano et al., 1997, 1998, 1999; Dell’Osso et al., 2003, 2016a,b, 2017, 2022, 2023; Carmassi et al., 2023). According to the spectrum project conceptualization (Cassano et al., 1997, 1998, 1999; Dell’Osso et al., 2003, 2016b, 2017, 2022, 2023, Carmassi et al., 2023), the spectrum of a disorder encompasses both full-blown and prototypical presentations along with sub-clinical and non-typical ones. It also comprises discrete signs and symptoms, symptom clusters, behavioral patterns, temperamental and/or personality qualities, and symptoms that are assumed to be related to the primary symptoms of the disorder. These last manifestations—signs, symptoms, and behavioral patterns—might be regarded as prodromes of a condition that has not yet fully manifested, or as aftereffects of a previously experienced, full-blown disorder, furthermore, they may also persist throughout life without fully manifesting clinically (Dell’Osso et al., 2000). In particular, the conceptualization of an OC spectrum appears to be in line even with some of the first conceptualizations of the disorder, when Janet described, under the term of psychasthenia, a picture that ranged from subthreshold obsessive features to the “obsessional personality” and “obsessional neurosis” (Gardiner, 1904) concept later resumed by Hollander et al. with the elaboration of the “OCD-spectrum related syndromes and disorders” (Hollander and Wong, 1995). Moreover, currently, the clinical evidence of OC-related disorders and the recognition of over-threshold and subthreshold OC comorbidity are compatible with the spectrum model of OC spectrum symptoms along an obsessive–compulsive component (Dell’Osso et al., 2000).
In the context of the spectrum project, together with other spectrum based psychometric instruments, the “Obsessive–Compulsive Spectrum Self-report” (OBS-SR) questionnaire was developed and validated with the aim to assess not only the prototypic symptoms of OCD but also unusual manifestations, temperamental traits, and other noteworthy clinical and sub-clinical aspects linked to the main symptoms (Dell’Osso et al., 2000, 2002). The questionnaire demonstrated a moderate internal consistency and a good inter-rater reliability along with a good discriminant validity; however, its use in the daily clinical practice remained quite difficult due to the long time needed to fill out it, which is around 50 min. In addition, the instrument, being developed in the early 2000s, still includes dated and redundant items.
As the main authors of the OBS-SR, we aimed to develop a new revised and shortened version of the questionnaire, the Obsessive–Compulsive Spectrum – Short Version (OBS-SV), which should be characterized by a reduced compilation time, but also by a greater internal consistency, inter-rater reliability and discriminant validity, also excluding dated items and including more modern ones, useful for the clinical practice and the investigation of both the full-blown and the milder subsyndromal form and OCD traits. In particular, the OBS-SV evaluates not only the typical OCD symptoms but also uncommon presentations, temperamental characteristics, and other notable clinical features related to the primary symptoms. Moreover, compared to the other commonly available measures of OCD, the OBS-SV is able to detect and evaluate the presence of obsessive traits in patients suffering from other mental disorder and in the non-clinical population, allowing the clinician to better assess the clinical picture and to recognize possible risk factor for the development of a concomitant disorder. In this study we sought to validate the OBS-SV questionnaire in a clinical population of subjects with OCS, Social Anxiety Disorder (SAD) and in healthy controls (HC). In particular, considering the reported presence of sub-threshold OCD traits in subjects with SAD and the overlapping features between OCD and SAD spectra, the SAD group was recruited as a potential intermediate group for OCD traits between OCD patients and HC (Carpita et al., 2020). We chose to recruit this kind of sample, with SAD subjects as an intermediate group, guided by evidences from numerous research that showed a substantial correlation between SAD and OCD. In fact, not only the comorbidity between OCD and SAD is reported to range from 12 to 42% in clinical samples and from 15 to 43.5% in the general population (Baldwin et al., 2008; Assunção et al., 2012), but also SAD is the most frequent co-occurring anxiety disorder among OCD patients (43.5%) as well as OCD has been noted to frequently co-occur with anxiety disorders (Bartz and Hollander, 2006; Ruscio et al., 2010). Despite that, OCD has been separated from anxiety disorders both in the DSM-5 and in the ICD-11 and is now included in a different category that also includes related conditions like body dysmorphic disorder (BDD), trichotillomania, hoarding disorder, and skin-picking disorder. This approach, while emphasizing the distinctive characteristics of the obsessive–compulsive spectrum, ignores the characteristics that OCD and anxiety disorders have in common, which are instead shown by both the responsiveness to similar therapies and the commonly observed comorbidity between these diseases (Carrasco et al., 1992; Baldwin et al., 2008; Assunção et al., 2012). According to the dimensional approach, identifying potential transnosographic symptoms among psychiatric disorders may help us better understand psychopathology and eventually get past the drawbacks of the existing nosological classification, like the high rates of comorbidity. In particular, the choice of SAD as an intermediate group for obsessive traits between OCD and HC was in line with a previous study from Dell’Osso et al., which highlighted intermediate levels of OCD traits among subjects with SAD (Carpita et al., 2020).
In this framework, the aim of the study was to validate the OBS-SV questionnaire in a clinical population of subjects with OCS, SAD, HC, and to evaluate its psychometric properties, expecting the questionnaire not only to report a significant convergent validity with other dimensional OCD measures, great internal consistency, and test–retest reliability, but also to perform differently in the three diagnostic categories.
Data have been collected between September 2022 and December 2023 at the Psychiatric clinic of the University of Pisa.
The sample was composed of 145 subjects which comprised into three diagnostic categories and assessed using DSM-5 diagnostic criteria. Ages under 18, language or intellectual disabilities that made it difficult to complete the examinations, mental disabilities, a lack of collaboration skills, and persistent psychotic symptoms were considered exclusion grounds. All groups were individuated as follows: 43 subjects with a clinical diagnosis of OCD; 42 subjects with a clinical diagnosis of SAD and 60 members of the medical and paramedical workforce who do not currently have or have ever had mental disorders (HC). All subjects in order to be recruited must be aged between 18 and 70 and willing to sign an informed consent. Diagnosis of OCD and SAD, and the lack of mental disorders among HC, were confirmed using the Structured Clinical Interview for DSM-5, Research Version (SCID-5-RV) (First et al., 2015). The test–retest reliability of the OBS-SV was assessed using 30 subjects randomly selected, 10 belonging to the OCD group, 10 from the SAD group and 10 HC.
A second evaluation conducted over a period of 21 days following the original assessment in order to give evidence for the temporal stability of the scores. The study was conducted in accordance with the Declaration of Helsinki. The study was fully explained to the eligible individuals, who then gave their written informed permission after having a chance to ask any questions. The subjects received no compensation for taking part.
Assessment procedures included the SCID-5-RV (First et al., 2015), the Yale Brown Obsessive Compulsive Scale (Y-BOCS) (Goodman et al., 1989), and the Obsessive–Compulsive Spectrum – Short Version questionnaire (OBS-SV).
The diagnostic assessment was carried out by four trained psychiatry of the university department of Psychiatry of Pisa. Raters received instruction on the obsessive compulsive spectrum and were given an extensive description of the OBS-SV. A separate group of raters was recruited to test the test–retest reliability. Raters who administered the SCID were formally certified.
The Y-BOCS is a clinician-rated scale that is considered by many investigators to be the gold-standard for measuring OCD symptoms severity (Pato et al., 1994; Melli et al., 2015). It consists in two sections: the first 67 items are a symptoms inventory, organized by category: the first 29 items investigate the obsessions, the second 29 the compulsions and the last 9 the presence of avoidant behavior. The next section, which consists of 10 items, is the severity scale. Its goal is to gather all the data on time spent, distress, resistance, interference, and level of control for both obsessions and compulsions. Finally, the last 4 items consider the indices of insight, reliability, global severity and global improvement. The Y-BOCS showed an overall strong internal consistency (α = 0.89), high inter-rater (ICC = 0.96) and 1-week test–retest reliability (ICC = 0.85) (Storch et al., 2010).
The OBS-SV consist of 139 items, organized in 6 domains (104 items) and 2 appendices (35 items). The answers to the different items are dichotomously coded (yes/no) and the scores for the individual domains and appendices are calculated by counting the number of positive responses. The Doubt domain (10 items) explore the areas of insecurity, uncertainty and indecisions related to personal feelings, emotions and behaviors. The Hypercontrol domain (37 items) investigates the propensity to exert control by exploring area of caution, personal accountability, checking, emotional control, other-directed control, conformity, conventional values and magical thinking. The Temporal dimension domain (7 items) study different ways to use time, such as compulsive slowness and hyper- or anti-economic time management. The Perfectionism domain (16 items) investigates the propensity of accuracy, exactness, orderliness or symmetry. The Repetition and automation domain (8 items) concerns the sensation of feeling forced to repeat actions, or performing repetitive gestures, albeit inconvenient and inappropriate to the context. The Obsessive themes domain (26 items) examines seven themes of attitudes and behaviors toward contamination, cleansing, sexuality, spirituality, existentialism and aggressiveness.
The first appendix, Childhood and adolescence, refers to various obsessive–compulsive characteristics emerged during infancy or adolescence, particularly at school, in ones’ free time and in the family environment. The second appendix, Impulsivity and loss of control, explores atypical manifestations which concern the loss of control in various context, including eating, drinking alcohol, taking drugs, and exercising excessively. As the previous version of the instrument, the OBS-SV was simultaneously developed in English and Italian language.
The scale items were created by the same authors of the already validated OBS-SR, based on the items of the previous scale. Five trained clinicians (LDO, BC, BN, DG, BC) screened the items for inclusion and disagreements were resolved by discussion. The selection of the items was based on the affinity with the clinical description given by the DMS and the recent literature; the exclusion regarded items deemed dated, not applicable to the general population due to cultural or historical factors, ambiguous or easily misunderstood or non-discriminatory for the OC spectrum. More information about the development of the previous scale, from which the final items were taken are reported elsewhere (Dell’Osso et al., 2000, 2002). Of the 183 items present in the previous version, after a process of clinical selection, only 139 items were selected. Compared to the previous version, the Doubt domain went from 13 to 10 items; the Hypercontrol domain went from 55 to 37 items; the Temporal dimension domain passed from 9 to 7 items; the Perfectionism domain went from18 to 16 items; the Repetition and automation domain went from 12 to 8 items and the Obsessive themes domain went from 33 to 26 items. The Childhood and adolescence and the Impulsivity and loss of control domains were transformed into appendix and, respectively, reduced from 23 to 18 items and from 20 to 17 items.
The Cronbach’s alpha was determined for each domain and the questionnaire’s overall score in order to estimate the internal consistency of the OBS-SV. To ascertain how each item affected the instrument’s accuracy, the variations in alpha with removed items were evaluated. Computing bivariate Pearson’s correlation coefficients between the six domain scores and between each domain score and the overall score allowed researchers to examine the validity of the instrument’s internal structure. By calculating the intra-class correlation coefficient (ICC) on a subgroup of 30 participants randomly selected from the original database and re-evaluated after a gap of 3 weeks, the test–retest reliability of the questionnaire was examined. By measuring the Pearson’s correlation coefficients between the OBS-SV domains and total scores as well as the Y-BOCS total score as an alternate measure of OCD, the convergent validity was examined. The mean total and domain scores recorded in the three diagnostic groups were compared by a One-way analysis of variance to examine the instrument’s discriminatory ability (Known-groups validity) (ANOVA). Post-hoc comparisons were made using the Bonferroni Test. With SPSS version 26.0, all statistical analyses were carried out (IBM Corp, 2019).
The OC sample reported a mean age of 40.95 years (± 11.48) and consisted of 19 (44.2%) males and 24 (55.8%) females. The SAD sample reported a mean age of 40.95 years (± 13.22) and consisted of 21 (50%) males and 21 (50%) females. The HC group reported a mean age of 37.25 years (± 13.48) and consisted in 27 (45%) males and 33 (55%) females (see Table 1). Regarding the educational level, 13 (9%) subjects reported to have a master degree, 42 (29%) subjects reported to have a degree, 41 (28.3%) subjects referred to have graduated, 12 (8.3%) subjects had a middle school certificate, 1 (0.7) subject did not finish the elementary school and 1 subject preferred not to disclose. Regarding the occupational role, 19 (13.1%) subjects were students, 21 (4.5%) subjects were unoccupied, 16 (11%) subjects were housewives, 39 (26.9%) subjects were employed, 4 (2.8%) subjects were retired and 13 (9%) subjects preferred not to disclose. Regarding the marital status 21 (14.5) subjects referred to live with their parents, 31 (21.4%) subjects were married, 36 (24.8%) subjects were unmarried, 10 (6.9%) subjects were divorced, 1 (0.7%) subject was a widower and 13 (9%) subjects preferred not to disclose.
The OBS-SV was reported to have a compilation time of circa 30 min, proving to be a more time efficient and manageable tool compared to the previous version that reported a compilation time around 50 min.
The Cronbach alphas and ICCs for the individual domains and the total score calculated for the entire sample are displayed in Table 2. A high level of internal consistency was shown by the OBS-SV scale. All of the OBS domains’ Cronbach alpha values are good (above the value of 0.7), and the value for the scale’s overall score is excellent (α = 0.964). As evidenced by the alpha value dropping when each item was removed individually, each item had a substantial correlation with the total and contributed in some way to the scale. With all ICCs above the value of 0.90, the test–retest reliability for total and domain scores was outstanding.
The Pearson’s coefficients for the OBS-SV domain scores ranged from 0.771 to 0.943, and they were all significantly, positively and strongly linked with one another (p < 0.01). The OBS overall score and each OBS-SV domain score showed strong correlation (see Table 3).
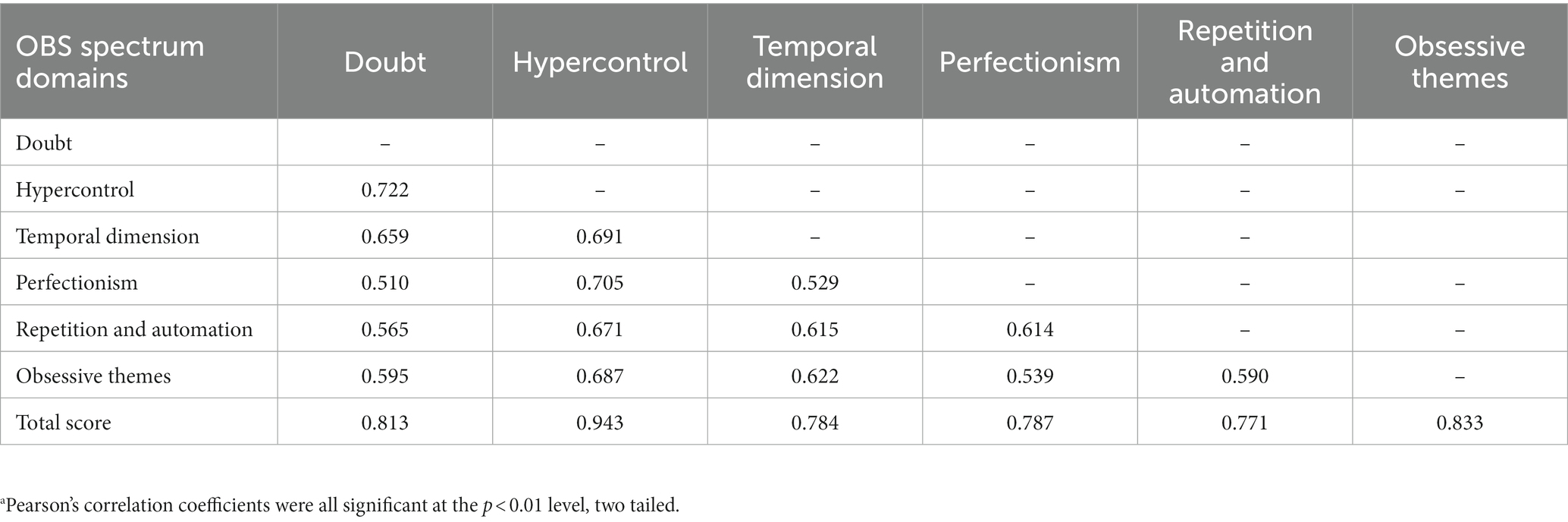
Table 3. Correlations among the OBS-SV domains.a
Table 4 shows Pearson’s correlation coefficients for the correlation of OBS-SV total and domain scores with the Y-BOCS global severity item and total score. All the correlation coefficients appeared strong, statistically significant and positive.
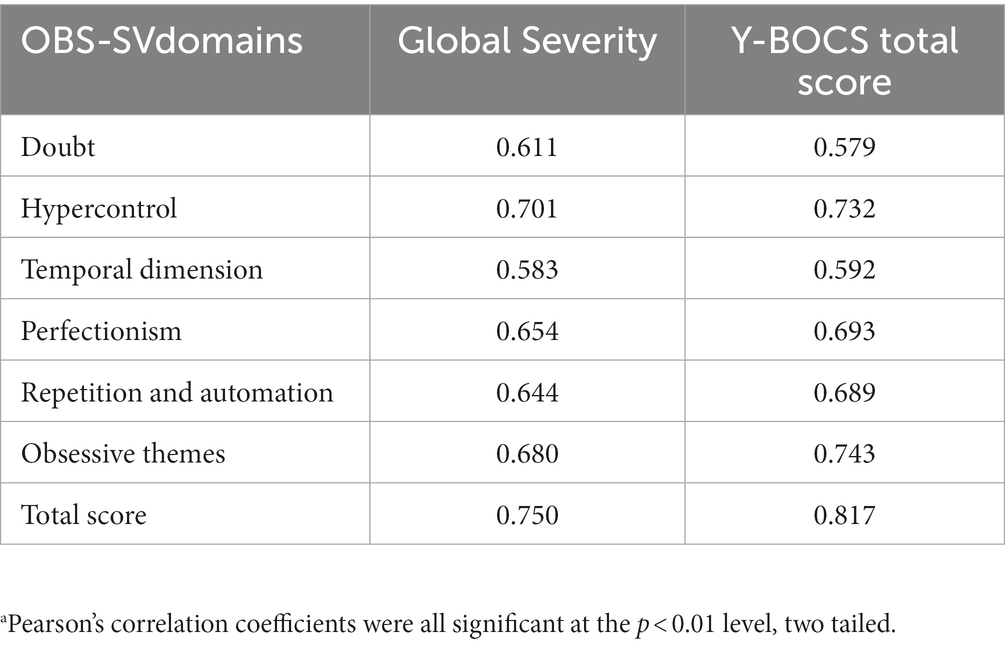
Table 4. Correlations between the OBS-SV domains and Y-BOCS total score.a
The ANOVA analysis revealed that there were significant differences between diagnostic groups for all OBS-SV domain and total scores (see Table 5). The OBS-SV total score was seen to rise dramatically and steadily from the HC, through the SAD, and up to the OC group, which reported the highest value. The OC group scored significantly higher in all domains than the SAD group, which in turn scored significantly higher than the HC group in all domains, with the exception of the Repetition and automation domain thus proving a good discriminant validity. Figure 1 illustrates the increasing trend of the OCD domain scores across groups. When comparing among groups the scores reported to the Y-BOCS, which is tailored to assess full-blown symptoms, OCD patients showed significantly higher scores than the other two groups. The SAD group reported higher scores than HCs but the difference was not statistically significant (see Figure 2).
The goal of this work was to introduce the OBS-SV, a clinical tool inspired by a dimensional approach to psychopathology, in light of the spectrum model (Cassano et al., 1997, 1998, 1999; Dell’Osso et al., 2003, 2016a,b, 2017, 2022). The OBS-SV investigates not only the prototypic symptoms of OCD but also unusual manifestations, temperamental traits, and other noteworthy clinical aspects linked to the main symptoms. For example, the OBS-SV allows to investigate the pervasive perfectionism (that although being a key factor in obsessive–compulsive personality disorder, is not necessarily present in OCD) thoughts of hurting someone else or themselves, moral absolutism, emotional control such as being unspontaneous, cold or detached toward others or being hypercritical, umorless or unimaginative. Results provided evidence of the validity and reliability of the OBS-SV administered to participants with a clinical diagnosis of OCD and SAD as well as HC. Using various dimensional measures of OCD, we discovered strong convergent validity, great internal consistency, and test–retest reliability. As expected, the questionnaire functioned differently among the three groups studied, with a progressive increase of the OBS-SV score going from healthy controls to SAD patients up to OCD participants.
The OBS–SV scores displayed positive, strong and significant correlations with the YBOCS, one of the most utilized instruments currently adopted to assess OC symptoms and features (Greeven et al., 2009; Anagnostou et al., 2011; Boyette et al., 2011; Ji et al., 2020). Compared to the previous version of the questionnaire that reported an internal consistency for all domains that ranged from moderate to substantial (0.60–0.90), the results from the new version confirmed its superiority showing all domains’ Cronbach alpha values above the value of 0.7 and an overall score of the scale (α = 0.964). Moreover, the OBS-SV exceeded the results reported from the previous scale both for the correlation between the domains (0.472–0.758 versus 0.771–0.943), and for the correlation with the alternative measure analyzed (0.58–9.82 versus 0.49–0.70).
Interestingly, the OBS–SV questionnaire seemed to be a useful tool for identifying subthreshold OC traits also in the healthy population and in SAD group, showing an increasing gradient of obsessive traits from the HC, passing through SAD subjects up to the OCD group. The different grades of OC spectrum among group seemed instead to be less clearly identified by the YBOCS, as highlighted by the comparison of the graphs of normalized OBS–SV and Y-BOCS scores among groups (Figures 1, 2). However, the presence of intermediate levels of OC traits in the SAD group is line with previous literature in the field, which frequently highlighted several OC traits among SAD patients, as well as overlapping features between the two disorders, and further support the spectrum model of psychopathology (Lochner and Stein, 2010; Egan et al., 2011; Dell’Osso et al., 2014, 2015; Marazziti et al., 2014; de Vries et al., 2018; Carpita et al., 2020).
Globally, our findings support the ability of the OBS-SV to properly detect the whole spectrum of OCD, from the subthreshold manifestations to the full-blown clinical picture. These results should be considered in light of some limitations. The principal limit of this work is the relatively limited sample size, which may, limit the extensibility of our data. Secondly, the OBS-SV, being a self-report questionnaire, may be at risk of underestimating or overestimating symptoms depending on the subjects’ judgment, and thus could be considered less precise when compared to the evaluation of the clinician. Additionally, we did not perform any inter-rater reliability tests nor the OBS-SV was administered to any pilot sample. Moreover, given the presence of a SAD group and the associations of SAD and OCD symptoms, it could have been interesting to examine the discriminant validity with a SAD measure. Likelywise, it would have also been interesting to assess the convergent validity of the OBS-SV with the OBS-SR, however, during the recruitment, the sample was only assessed with the OBS-SV and the Y-BOCS as an alternative measure of OCD.
The OBS-SV demonstrated good psychometric properties within the context of the aforementioned restrictions, and our findings offer a coherent construct of the OBS-SV with high internal consistency, strong test–retest reliability, and significant and positive convergent validity with alternative dimensional measures of OCD, such as the Y-BOCS. When compared with the previous version of the instrument and, the OBS-SV has the advantage of being more time efficient and more in line with the current conceptualization of OCD. Moreover, its use in the clinical setting, before the clinical interview could allow the clinician to have a general assessment of the symptomatologic profile of the subject and consent a faster and deeper investigation on some relevant symptomatologic domains. In this framework, it should be noted that, besides SAD, OC features have been also reported in a wide range of psychiatric conditions, ranging from neurodevelopmental disorders, to mood disorders, feeding and eating disorders and personality disorders, often worsening the clinical picture and response to treatments (McKay et al., 2000; Mukai et al., 2011; Postorino et al., 2017; Pazuniak and Pekrul, 2020; Tonna et al., 2021; Amianto et al., 2022; Reilly et al., 2022).
In conclusion, the OBS-SV not only demonstrated a significant convergent validity with other dimensional OCD measures, excellent internal consistency, and test–retest reliability but also, unlike the other commonly used measures, show the added value to be able to assess the wide spectrum of OCD manifestation, from the full-blown disorder to the subclinical manifestation, uncommon presentations, temperamental characteristics and other features related to the primary symptoms. Indeed, when evaluated with the Y-BOCS – a instrument designed to assess only full-blown manifestation – OCD patients scored significantly higher than the other two groups, but the latter had no significant differences with each other (Figure 2). On the contrary, the OBS-SV showed to have the specific value to be able to distinguish the presence of obsessive compulsive traits even in the SAD and HC groups, reporting a significant difference between them (Figure 1). The availability of an instrument able to detect sub-syndromic and atypical manifestations of this condition in both the general population and in clinical samples of patients with other mental disorders, may undoubtedly help in improving the diagnostic assessment and the treatment project of the patients, as well as support preventive and screening strategies in the general population.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Comitato Etico Regionale per la Sperimentazione Clinica della Regione Toscana. The patients/participants provided their written informed consent to participate in this study.
LD’O conceived the work. All authors collected the data processed in the study. GM did statistical analysis. BN, CB, and LD’O drafted the manuscript. BC and LD’O revised the work. All authors provided approval of the version to be published.
The authors thank the participants for their continued support and participation in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1157636/full#supplementary-material
Akiskal, H. S., and Akiskal, K. (1992). Cyclothymic, hyperthymic, and depressive temperaments as subaffective variants of mood disorders. Am. Press. Rev. Psychiatry. 11, 43–62.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. 5th. Washington, DC: American Psychiatric Association.
American Psychiatric Association. (2023) Diagnostic and statistical manual of mental disorders, fifth edition, text revision. Washington: American Psychiatric Association.
Amianto, F., Secci, I., Arletti, L., Davico, C., Abbate Daga, G., and Vitiello, B. (2022). Obsessive-compulsive symptoms in young women affected with anorexia nervosa, and their relationship with personality, psychopathology, and attachment style. Eat. Weight Disord. 27, 1193–1207. doi: 10.1007/s40519-021-01252-y
Anagnostou, E., Chaplin, W., Watner, D., Silverman, J. M., Smith, C. J., Zagursky, K., et al. (2011). Factor analysis of repetitive behaviors in autism as measured by the Y-BOCS. J. Neuropsychiatry Clin. Neurosci. 23, 332–339. doi: 10.1176/jnp.23.3.jnp332
Angst, J., Merikangas, K. R., and Preisig, M. (1997). Subthreshold syndromes of depression and anxiety in the community. J. Clin. Psychiatry 58, 6–10.
Assunção, M. C., Costa, D. L., de Mathis, M. A., Shavitt, R. G., Ferrão, Y. A., do Rosário, M. C., et al. (2012). Social phobia in obsessive-compulsive disorder: prevalence and correlates. J. Affect. Disord. 143, 138–147. doi: 10.1016/j.jad.2012.05.044
Baldwin, D. S., Brandish, E. K., and Meron, D. (2008). The overlap of obsessive-compulsive disorder and social phobia and its treatment. CNS Spectr. 13, 47–53. doi: 10.1017/S1092852900026936
Bartz, J. A., and Hollander, E. (2006). Is obsessive-compulsive disorder an anxiety disorder? Neuro-Psychopharmacol Biol. Psychiatry 30, 338–352. doi: 10.1016/j.pnpbp.2005.11.003
Boyette, L., Swets, M., Meijer, C., and Wouters, L., GROUP Authors (2011). Factor structure of the Yale-Brown obsessive-compulsive scale (Y-BOCS) in a large sample of patients with schizophrenia or related disorders and comorbid obsessive-compulsive symptoms. Psychiatry Res. 186, 409–413. doi: 10.1016/j.psychres.2010.07.048
Carmassi, C., Pedrinelli, V., Antonini, C., Dell’Oste, V., Gravina, D., Nardi, B., et al. (2023). Validation of the Spanish version of the trauma and loss Spectrum self-report (TALS-SR): a study on healthcare workers facing the COVID-19 pandemic. Neuropsychiatr. Dis. Treat. 19, 495–506. doi: 10.2147/NDT.S396540
Carpita, B., Muti, D., Petrucci, A., Romeo, F., Gesi, C., Marazziti, D., et al. (2020). Overlapping features between social anxiety and obsessive-compulsive spectrum in a clinical sample and in healthy controls: toward an integrative model. CNS Spectr. 25, 527–534. doi: 10.1017/S109285291900138X
Carrasco, J. L., Hollander, E., Schneier, F. R., and Liebowitz, M. R. (1992). Treatment outcome of obsessive compulsive disorder with comorbid social phobia. J. Clin. Psychiatry 53, 387–391.
Cassano, G. B., Dell’Osso, L., Frank, E., Miniati, M., Fagiolini, A., Shear, K., et al. (1999). The bipolar spectrum: a clinical reality in search of diagnostic criteria and an assessment methodology. J. Affect. Disord. 54, 319–328. doi: 10.1016/s0165-0327(98)00158-x
Cassano, G. B., Michelini, S., Shear, M. K., Coli, E., Maser, J. D., and Frank, E. (1997). The panic-agoraphobic spectrum: a descriptive approach to the assessment and treatment of subtle symptoms. Am. J. Psychiatry 154, 27–38. doi: 10.1176/ajp.154.6.27
Cassano, G., Rotondo, A., Maser, J., Shear, M., Frank, E., Mauri, M., et al. (1998). The panic-agoraphobic Spectrum: rationale, assessment, and clinical usefulness. CNS Spectr. 3, 35–48. doi: 10.1017/S1092852900005848
Chamberlain, S. R., Blackwell, A. D., Fineberg, N. A., Robbins, T. W., and Sahakian, B. J. (2005). The neuropsychology of obsessive compulsive disorder: the importance of failures in cognitive and behavioural inhibition as candidate endophenotypic markers. Neurosci. Biobehav. Rev. 29, 399–419. doi: 10.1016/j.neubiorev.2004.11.006
de Vries, H. T., Nakamae, T., Fukui, K., Denys, D., and Narumoto, J. (2018). Problematic internet use and psychiatric co-morbidity in a population of Japanese adult psychiatric patients. BMC Psychiatry 18:9. doi: 10.1186/s12888-018-1588-z
Dell’Osso, L., Abelli, M., Pini, S., Carlini, M., Carpita, B., Macchi, E., et al. (2014). Dimensional assessment of DSM-5 social anxiety symptoms among university students and its relationship with functional impairment. Neuropsychiatr. Dis. Treat. 10, 1325–1332. doi: 10.2147/NDT.S59348
Dell’Osso, L., Abelli, M., Pini, S., Carpita, B., Carlini, M., Mengali, F., et al. (2015). The influence of gender on social anxiety spectrum symptoms in a sample of university students. Riv. Psichiatr. 50, 295–301. doi: 10.1708/2098.22688
Dell’Osso, L., Amatori, G., Cappelli, A., Cremone, I. M., Massimetti, G., Gravina, D., et al. (2022). Catatonia Spectrum: validation of a questionnaire investigating catatonia Spectrum. Front. Psych. 13:913286. doi: 10.3389/fpsyt.2022.913286
Dell’Osso, L., Amatori, G., Nardi, B., Bonelli, C., Gravina, D., Benedetti, F., et al. (2023). Validation of the short version of the panic agoraphobic Spectrum (PAS-SV) questionnaire. Clin. Neuropsychiatry 20, 151–156. doi: 10.36131/cnfioritieditore20230207
Dell’Osso, L., Cassano, G. B., Sarno, N., Millanfranchi, A., Pfanner, C., Gemignani, A., et al. (2000). Validity and reliability of the structured clinical interview for obsessive-compulsive Spectrum (SCI-OBS) and of the structured clinical interview for social phobia Spectrum (SCI-SHY). Int. J. Methods Psychiatric. Res. 9, 11–24. doi: 10.1002/mpr.76
Dell’Osso, L., Dalle Luche, R., and Maj, M. (2016a). Adult autism spectrum as a transnosographic dimension. CNS Spectr. 21, 131–133. doi: 10.1017/S1092852915000450
Dell’Osso, L., Gesi, C., Massimetti, E., Cremone, I. M., Barbuti, M., Maccariello, G., et al. (2017). Adult autism subthreshold Spectrum (AdAS Spectrum): validation of a questionnaire investigating subthreshold autism spectrum. Compr. Psychiatry 73, 61–83. doi: 10.1016/j.comppsych.2016.11.001
Dell’Osso, L., Luche, R. D., Gesi, C., Moroni, I., Carmassi, C., and Maj, M. (2016b). From Asperger’s Autistischen Psychopathen to DSM-5 autism Spectrum disorder and beyond: a subthreshold autism Spectrum model. Clin. Pract. Epidemiol. Ment. Health 12, 120–131. doi: 10.2174/1745017901612010120
Dell’Osso, L., Rucci, P., Cassano, G. B., Maser, J. D., Endicott, J., Shear, M. K., et al. (2002). Measuring social anxiety and obsessive-compulsive spectra: comparison of interviews and self-report instruments. Compr. Psychiatry 43, 81–87. doi: 10.1053/comp.2002.30795
Dell’Osso, L., Rucci, P., Ducci, F., Ciapparelli, A., Vivarelli, L., Carlini, M., et al. (2003). Social anxiety spectrum. Eur. Arch. Psychiatry Clin. Neurosci. 253, 286–291. doi: 10.1007/s00406-003-0442-5
Egan, S. J., Wade, T. D., and Shafran, R. (2011). Perfectionism as a transdiagnostic process: a clinical review. Clin. Psychol. Rev. 31, 203–212. doi: 10.1016/j.cpr.2010.04.009
First, M. B., Williams, J. B. W., Karg, R. S., and Spitzer, R. L. (2015) Structured clinical interview for DSM-5—Research version (SCID-5 for DSM-5, research version; SCID-5-RV). Arlington: VA, American Psychiatric Association.
Fontenelle, L. F., Mendlowicz, M. V., and Versiani, M. (2006). The descriptive epidemiology of obsessive-compulsive disorder. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 30, 327–337. doi: 10.1016/j.pnpbp.2005.11.001
Frank, E., Cassano, G., Shear, M., Rotondo, A., Dell’Osso, L., Mauri, M., et al. (1998). The Spectrum model: a more coherent approach to the complexity of psychiatric symptomatology. CNS Spectr. 3, 23–34. doi: 10.1017/S1092852900005836
Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleischmann, R. L., Hill, C. L., et al. (1989). The Yale-Brown obsessive compulsive scale. I. Development, use, and reliability. Arch. Gen. Psychiatry 46, 1006–1011. doi: 10.1001/archpsyc.1989.01810110048007
Grant, J. E., and Chamberlain, S. R. (2019). Obsessive compulsive personality traits: Understanding the chain of pathogenesis from health to disease. J. Psychiatr. Res. 116, 69–73. doi: 10.1016/j.jpsychires.2019.06.003
Grant, J. E., Mooney, M. E., and Kushner, M. G. (2012). Prevalence, correlates, and comorbidity of DSM-IV obsessive-compulsive personality disorder: results from the National Epidemiologic Survey on alcohol and related conditions. J. Psychiatr. Res. 46, 469–475. doi: 10.1016/j.jpsychires.2012.01.009
Greeven, A., Spinhoven, P., and van Balkom, A. J. (2009). Hypochondriasis Y-BOCS: a study of the psychometric properties of a clinician-administered semi-structured interview to assess hypochondriacal thoughts and behaviours. Clin. Psychol. Psychother. 16, 431–43. doi: 10.1002/cpp.634
Helmchen, H., and Linden, M. (2000). Subthreshold disorders in psychiatry: clinical reality, methodological artifact, and the double-threshold problem. Compr. Psychiatry 41, 1–7. doi: 10.1016/s0010-440x(00)80001-2
Hollander, E., and Wong, C. M. (1995). Obsessive-compulsive spectrum disorders. J. Clin. Psychiatry 56, 1–5.
Ji, G., Wei, W., Yue, K. C., Li, H., Shi, L. J., Ma, J. D., et al. (2020). Effects of the COVID-19 pandemic on obsessive-compulsive symptoms among university students: prospective cohort survey study. J. Med. Internet Res. 22:e21915. doi: 10.2196/21915
Karno, M., Golding, J. M., Sorenson, S. B., and Burnam, M. A. (1988). The epidemiology of obsessive-compulsive disorder in five US communities. Arch. Gen. Psychiatry 45, 1094–1099. doi: 10.1001/archpsyc.1988.01800360042006
Kessler, R. C., Petukhova, M., Sampson, N. A., Zaslavsky, A. M., and Wittchen, H. U. (2012). Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int. J. Methods Psychiatr. Res. 21, 169–184. doi: 10.1002/mpr.1359
Lochner, C., and Stein, D. J. (2010). Obsessive-compulsive spectrum disorders in obsessive-compulsive disorder and other anxiety disorders. Psychopathology 43, 389–396. doi: 10.1159/000321070
Marazziti, D., Abelli, M., Baroni, S., Carpita, B., Piccinni, A., and Dell’Osso, L. (2014). Recent findings on the pathophysiology of social anxiety disorder. Clin. Neuropsychiatry 11, 91–100.
McKay, D., Kulchycky, S., and Danyko, S. (2000). Borderline personality and obsessive-compulsive symptoms. J. Personal. Disord. 14, 57–63. doi: 10.1521/pedi.2000.14.1.57
Melli, G., Avallone, E., Moulding, R., Pinto, A., Micheli, E., and Carraresi, C. (2015). Validation of the Italian version of the Yale-Brown obsessive compulsive scale-second edition (Y-BOCS-II) in a clinical sample. Compr. Psychiatry 60, 86–92. doi: 10.1016/j.comppsych.2015.03.005
Mukai, Y., Two, A., and Jean-Baptiste, M. (2011). Chronic catatonia with obsessive compulsive disorder symptoms treated with lorazepam, memantine, aripiprazole, fluvoxamine and neurosurgery. BMJ Case Rep. 2011:bcr0220113858. doi: 10.1136/bcr.02.2011.3858
Pato, M. T., Eisen, J., and Pato, C. N. (1994). Rating scales for obsessive compulsive behavior. Curr. Insights Obsess. Compul. Disor., 77–91.
Pazuniak, M., and Pekrul, S. R. (2020). Obsessive-compulsive disorder in autism Spectrum disorder across the lifespan. Child Adolesc. Psychiatr. Clin. N. Am. 29, 419–432. doi: 10.1016/j.chc.2019.12.003
Pincus, H. A., Davis, W. W., and McQueen, L. E. (1999). ’Subthreshold’ mental disorders. A review and synthesis of studies on minor depression and other ‘brand names’. Br. J. Psychiatry 174, 288–296. doi: 10.1192/bjp.174.4.288
Postorino, V., Kerns, C. M., Vivanti, G., Bradshaw, J., Siracusano, M., and Mazzone, L. (2017). Anxiety disorders and obsessive-compulsive disorder in individuals with Autism Spectrum disorder. Curr. Psychiatry Rep. 19:92. doi: 10.1007/s11920-017-0846-y
Reilly, E. E., Gorrell, S., Brosof, L., Lock, J., and Le Grange, D. (2022). Characterizing changes in obsessive-compulsive symptoms over the course of treatment for adolescent bulimia nervosa. Int. J. Eat. Disord. 55, 1342–1351. doi: 10.1002/eat.23782
Ruscio, A. M., Stein, D. J., Chiu, W. T., and Kessler, R. C. (2010). The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol. Psychiatry 53, 53–63. doi: 10.1038/mp.2008.94
Storch, E. A., Rasmussen, S. A., Price, L. H., Larson, M. J., Murphy, T. K., and Goodman, W. K. (2010). Development and psychometric evaluation of the Yale–Brown obsessive-compulsive scale—second edition. Psychol. Assess. 22, 223–232. doi: 10.1037/a0018492
Keywords: obsessive–compulsive spectrum, OCD, spectrum model, questionnaire, Obsessing-compulsive disorder
Citation: Dell’Osso L, Nardi B, Bonelli C, Gravina D, Benedetti F, Del Prete L, Massimetti G, Amatori G, Carpita B and Cremone IM (2023) Validation of the short version of the obsessive compulsive spectrum questionnaire. Front. Psychol. 14:1157636. doi: 10.3389/fpsyg.2023.1157636
Received: 02 February 2023; Accepted: 05 June 2023;
Published: 27 June 2023.
Edited by:
Sara Giovagnoli, University of Bologna, ItalyReviewed by:
Jean-Sébastien Audet, Montreal University, CanadaCopyright © 2023 Dell’Osso, Nardi, Bonelli, Gravina, Benedetti, Del Prete, Massimetti, Amatori, Carpita and Cremone. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Benedetta Nardi, YmVuZWRldHRhLm5hcmRpQGxpdmUuaXQ=
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.