
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 08 January 2024
Sec. Psychology for Clinical Settings
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1145229
This article is part of the Research Topic Coping with Life Stress, volume II View all 15 articles
Background: Fear of childbirth is one of the main causes of women’s emotional difficulty experienced in the perinatal period, especially those having their first child.
Objective: The aim of this study was to investigate the effect of emotional freedom technique (EFT) on the fear of childbirth among primiparous women in Ahvaz, Iran.
Materials and methods: This randomized clinical trial was conducted on 116 primiparous women. The participants were randomly divided into intervention (n = 58) or control (n = 58) groups. The intervention group received daily stimulation of certain points in their body for 12 weeks using EFT. The fear of childbirth was measured at the beginning of the study and 12 weeks after the intervention using the Wijma Delivery Expectancy/Experience Questionnaire (WDEQ-A) and at the first postpartum visit with WDEQ-B. Data were analyzed using independent t-test, paired t-test, Chi-square or Fisher’s exact test, and analysis of covariance (ANCOVA).
Results: After intervention, the mean score of fear of childbirth in the intervention group decreased from 49.39 ± 8.21 to 40.42 ± 13.43 (p < 0.0001), while the same rate in the control group increased from 49.47 ± 9.06 to 52.09 ± 7.73 (p = 0.002). The mean score of fear of childbirth after delivery in the control group (45.88 ± 7.10) was higher than that in the intervention group (27.13 ± 5.08) (p < 0.0001).
Conclusion: Based on the findings of this study, EFT can be considered as an effective method to reduce the fear of childbirth score in primiparous women.
Although pregnancy is associated with positive feelings about the baby, it is mostly accompanied with anxiety, stress and fear of childbirth (Wijma, 2003). According to a systematic review, the prevalence of intensive fear of childbirth in women around the world is 14%, with primiparous and multiparous women accounting for 16 and 12%, respectively (O’Connell et al., 2017). In Europe, the overall prevalence of intensive fear of childbirth is 11%, which is 11.4% for primiparous women and 11% for multiparous women (Lukasse et al., 2014). In Australia, the overall prevalence of intensive fear of childbirth is 24, and 31.5% of primiparous women report severe fear (Toohill et al., 2014). Fear of childbirth has been reported differently in developing countries. For example, a study in Malawi showed that 41 and 20% of pregnant women reported moderate and high fear of childbirth, respectively (Khwepeya et al., 2018). Another study in Southern Ethiopia showed that the prevalence of fear of childbirth is 24.2%, and women with the negative experience from previous pregnancy had a higher rate of fear (Aynalem and Eneye, 2021). A study in Iran showed that 77.2% of pregnant women had mild or moderate fear of childbirth, 18.5% had clinical and 4.3% had severe fear of childbirth (Alijani et al., 2019).
Mental stress during pregnancy and childbirth can be associated with adverse outcomes and consequences such as miscarriage, nausea and vomiting, pre-eclampsia, and premature birth. Furthermore, fear of childbirth may persist in the postpartum stage and leave an unpleasant experience of childbirth (Alehagen et al., 2001). According to a previous study, preterm birth almost is twice among women who experienced stress in their pregnancy in comparison to women who did not have (Lilliecreutz et al., 2016). A longitudinal study showed that higher maternal blood leptin was significantly associated with respiratory distress, low birth weight, lower head circumference, and low APGAR score in neonates (Rabiepoor et al., 2019). Another study showed that women with higher anxiety score during pregnancy had more uterine artery resistance index that in turn can deteriorate blood flow of uterus (Fisk and Glover, 1999). In addition, the hypoxia caused by the decrease in blood flow to the pelvic muscles in response to the fear-induced increase in serum catecholamine and cortisol levels can lead to increased pain in mothers. Women who experience excessive fear during pregnancy are at risk of emotional imbalance after giving birth, which can negatively affect their relationship with their baby (Areskog et al., 1983; Lederman, 1990). Also, fear of labor pains and feeling alone during pregnancy are predictive factors of pain and suffering during childbirth and may increase the risk of emergency cesarean section (Ryding et al., 1998) and elective cesarean section (Waldenström et al., 2006). In 1985, the World Health Organization (WHO) urged that there be no justification for a cesarean rate of higher than 10–15% in any region of the world (Chalmers, 1992). The reason why the WHO recommends to avoid unnecessary cesarean section is that, like any surgery, caesarean sections are associated with short- and long-term risks which can extend many years beyond the current delivery and affect the health of the woman, her child, and future pregnancies, and that these risks are higher in women with limited access to comprehensive obstetric care” (World Health Organization, 2023).
Studies have estimated the prevalence of cesarean section to be 50–60% in Iran, which is 3–4 times higher than that recommended by the WHO (Badiee et al., 2013). Negative experiences with last delivery may persuade pregnant women to resort to elective cesarean section (Størksen et al., 2015). However, there is evidence suggesting that fear of childbirth among primiparous women is higher than in multiparous women (Shakarami et al., 2021), and that such fear is the most common reason for having a cesarean section (Negahban and Ansari, 2009) even though complications of cesarean sections are far more frequent than those of natural childbirths.
Therefore, treatment of fear of childbirth should be a priority in order to reduce the risk of having an unpleasant experience of childbirth, reduce cesarean section rate, and improve the mental health of mothers (Delavar and Alizadeh, 2014). Several methods such as hypnosis, exercise, and cognitive-behavioral interventions with or without medications have been used to reduce the fear of childbirth (O’Connell et al., 2019).
Emotional freedom technique (EFT) is one of the alternative medicine treatments which is a combination of elements of cognitive-behavioral therapy, exposure therapy, and somatic stimulation of acupuncture points (Church, 2014; Stapleton et al., 2017). Physiological examination of the clinical effects of EFT has shown that this technique is associated with the regulation of cortisol, beneficial changes in gene expression, and regulation of the autonomic nervous system activity (Church et al., 2012, 2020).
The effect of EFT has been investigated in studies in different areas. For example, Church et al. found that EFT clearly reduced the level of cortisol, which in turns improved depression, anxiety and other psychological disorders (Church et al., 2018). According to Lane, the physiological mechanisms of the response to reduced stress and relaxation include a decrease in the secretion of stress hormones such as cortisol, an increase in the secretion of endogenous opioids, and as a result the decrease of fear in the amygdala (Lane, 2009). EFT has been reported to be effective in many other areas such as the treatment of disorders such as generalized or specific anxiety, morbid fears, depression, post-traumatic stress disorder, chronic pain, and addiction (Church, 2013). However, no research has so far been conducted on the effect of EFT on the fear of childbirth in Iran. Therefore, this research was conducted with the aim of investigating the effective of EFT on the fear of childbirth among primiparous women in Ahvaz, Iran. We hypothesized that EFT could reduce the fear of childbirth among primiparous women.
This study is a parallel randomized controlled trial on 116 primiparous pregnant women with fear of childbirth who were randomly divided into EFT and control (Sham therapy) groups. The study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (Ref. ID: IR.AJUMS.REC.1400.192). Also, the protocol of this study was registered in the Iranian Registry of Clinical Trials (Ref. ID: IRCT20210622051671N1). All participants provided written informed consent before data collection. The women were recruited in this study based on the following criteria: minimum elementary education, age 18 to 40 years, gestational age 28 to 30 weeks, primiparity, and obtaining a score greater than 37 from the Wijma Delivery Expectancy Questionnaire (WDEQ-A), which indicates moderate fear of childbirth. Women with the following criteria were excluded from the study: suffering from chronic diseases such as heart disease, high blood pressure, and diabetes, history of abortion, placenta previa, suffering from mental illnesses during the past year, taking psychoactive drugs, drug addiction, smoking, and pregnancy complications such as pre-eclampsia, hemorrhage, intrauterine death, and premature birth.
Data collection was started in November 2021 and completed in March 2022.
According to the objectives of the research and assuming a power of 80%, α = 0.05, s1 = s2 = 17.43 and d = 10, the sample size was determined using the following formula:
Assuming a 20% attrition rate, the number of participants in each group of intervention and Sham therapy was 58.
Participants who scored above 37 in the WDEQ-A were included in the study. The method of assigning women to the intervention or control groups was based on block randomization with a block size of 6 and an allocation ratio of 1:1. The randomization list was prepared by a statistician (EM). The codes assigned to the eligible women were placed in sealed envelopes by someone who was not involved in the study and was not aware of the research objectives. The envelops were then given to the clerk in health centers. In this way, neither the researcher nor the participants were aware of group allocation until the commencement of the study. This study was single blind, meaning that the researcher was aware of which group received the intervention, but participants were not aware of grouping.
The lead researcher visited two public health centers in Ahvaz city and screened pregnant women based on the inclusion/exclusion criteria. A total of 200 women were examined, of whom 116 who met the inclusion criteria were randomly assigned into EFT and control groups. Primiparous women who attended to Public Health Centers No. 2 and 3 in the west of Ahvaz were screened based on the inclusion criteria. Women who met inclusion criteria and received a score more than 37 from Wijma-A questionnaire were requested to fill-out the demographic questionnaire.
In this study, a demographic questionnaire and the Wijma Delivery Expectancy/Experience Questionnaire (W-DEQ) versions A and B were used to collect the data. The demographic questionnaire contained questions about age, gestational age, the woman’s and her husband’s educational attainment and occupation, and economic status.
W-DEQ-A is a questionnaire used to assess women’s fear of the childbirth. This questionnaire has 33 questions in six dimensions of “lack of positive anticipation (questions number 2, 19, 25 and 27),” “fear (questions number 3, 6, 7, 8, 11, 12 and 15),” “lack of self-efficacy (questions number 4, 5, 10, 13, 14, 16, 17, 20, 22, 23),” “loneliness (questions number 1, 9 and 29),” “concerns for the child (questions number 30, 32, 33),” and “negative appraisal (questions number 18, 21, 26, 28).” Questions 24 and 31 are not classified in any category, but they are taken into account when calculating the total score. The questions are scored based a six-point Likert scale (from 0 to 5). Some of the questions are affirmatively worded and some are negatively worded. The minimum total score obtained is 0 and the maximum score is 165. A score less than or equal to 37 means a mild fear level, a score of 38–65 suggest a moderate fear, and a score of 66–84 represents severe fear. The cut-off score is 85, which means that scores 85 and above prove clinical fear (Wjma et al., 1998).
The construct validity of this questionnaire and its reliability were confirmed in Abedi et al.’s study (Abedi et al., 2016). WDEQ-B has 33 questions in six sub-scales, and each question is scored from 0 to 5. It is similar to the A version in terms of scoring and cut-off point. They are different only in terms of the time point of assessment (the A version is used before delivery while the B version is used after delivery).
The EFT included the following steps:
1. Identifying the problem that caused the person to be upset (e.g., fear of childbirth) and scoring or measuring the severity of that problem.
2. Expressing an emphatic sentence (in relation to the person’s problem and self-acceptance) along with tapping the parts of the face and body with the tips of the fingers, which is known as correction (i.e., arrangement of the energy system).
These points include: the edge of the hand (the fleshy part of the outer edge of the hand that is used in karate to break objects), the beginning of the eyebrows (above the side of the nose), the side of the eyes (on the bone of the outer side of the eye), under the eyes (on the cheek and 2–3 cm below the eyeball), under the nose (in the short distance between the nose and the upper lip), chin (the distance between the depression of the chin and the lower lip), the beginning of the clavicle (at the intersection of the sternum, the clavicle and the first rib, 2.5 cm towards the navel from the U-shaped slit) and under the arm (10 cm from the armpit to the bottom), above the head (if an imaginary line is drawn from one ear to the other ear and another from the nose to the back of the neck, this point will be right at the intersection of these two lines; Figure 1).
In order to learn and master the principles of EFT, the lead researcher participated in a workshop held by an expert in EFT.
In groups of maximum 10 women, the participants in the intervention group received EFT training on how to manipulate the correct points in one session. In this training session, this technique was illustrated using a short training video, and the researcher ensured the correctness of manipulating the points (this training video was prepared by the training institute).1 Also, an approved educational brochure (to help the participants in the correctly use of this method) which was based on the standard instructions and EFT website was provided to the participants to use at home. Based on the initial research design, two face-to-face training sessions were supposed to be held, but due to the start of the COVID-19 pandemic and the subsequent home quarantine, only one face-to-face session was held for the participants.
The participants were recommended to do this technique every morning in order to improve their mood throughout the day. In addition, they were advised to use this technique during the day whenever they felt stressed out and afraid. While tapping, the women were asked to use positive statements and to accept themselves despite all the problems they had. In the next 10 weeks, the participants were followed up (on a weekly basis) by phone calls in order to check the regular implementation of this method (i.e., sending audio files on tapping techniques three times a week and answering the mothers’ questions) in accordance with the principles taught in the face-to-face training session. The participants’ questions were answered through phone calls and text messages. The women were asked to use affirmative sentences when tapping the EFT points.
Likewise, a face-to-face training session was held for the control group, but it included false points (i.e., elbow bumps, chin bumps, eye bumps, nose bumps, foreheads, and arms). All participants were asked to follow these instructions until the end of pregnancy. In order to abide by ethical consideration, women in the control group were given a pamphlet about right points at the end of the study.
We recruited women at 28–30 gestational age and followed them up for 10 weeks for measuring fear of childbirth before delivery. Women also followed up to 2 weeks after delivery for measuring fear of childbirth after delivery. Women in the intervention group received a phone call three times a week to ensure the correct use of EFT.
In the last prenatal visit (39–40 weeks), the fear of childbirth after intervention was assessed using WDEQ-A. For measuring fear of childbirth after delivery the WDEQ-B was given to the mothers (both as Google doc file and hard copy) to be completed at home after delivery. In the first postpartum visit (first 10 days after delivery) the completed questionnaires were checked by the lead researcher and in case of any unanswered question, the mothers were requested to provide answers to those questions.
• Fear of childbirth before delivery.
• Fear of childbirth after delivery.
Data analysis was done using SPSS version 20. The quantitative variables were reported using mean and standard deviation, and qualitative variables, using frequency (percentage). The normality of quantitative variables was assessed by the Shapiro–Wilk test. The comparison of qualitative variables in the two groups was done by Chi-square or Fisher’s exact tests. Comparison of the quantitative variables between two groups was performed using the independent samples t-test. Paired samples t-test was used for comparing the quantitative variables’ changes in each group. Effect of intervention on posttest outcome measures were examined using analysis of covariance (ANCOVA), adjusting for pretest scores. The significance level of the tests was considered as 0.05.
In this study, 58 women were included in each group (intervention and control) and all of them completed the study (Figure 2). The demographic characteristics of the participants are listed in Table 1. The mean age of the mothers was 22.11 ± 3.73 years, and their mean gestational age was 29.15 ± 0.77 weeks. According to the results of Table 1, the two groups had no statistically significant differences in terms of demographic factors (p > 0.05).
Table 2 shows the difference between the mean score of the components of WDEQ-A before and after intervention in the intervention and control groups. The mean score of lack of positive anticipation in the intervention group decreased from 7.72 ± 2.43 before the intervention to 6.86 ± 2.75 after intervention, which was not significantly different compared to the control group (p = 0.34). The mean score of fear in the intervention group fell from 13.60 ± 2.28 before the intervention to 10.95 ± 5.74 after intervention (p = 0.001), which was significantly different compared with the control group (p = 0.003). The mean score of lack of self-efficacy in both groups increased significantly. Results of independent t-test and ANCOVA did not show any significant difference between the two groups in this regard (p = 0.222). The mean score of loneliness in the intervention group rose from 3.08 ± 1.12 to 3.42 ± 2.51, which was not significantly different compared to the control group (p = 0.508). The mean score of concerns for the child in the intervention group increased from 1.36 ± 7.39 to 3.86 ± 1.46 (p < 0.0001), which showed a significant difference between the two groups based on independent t-test and ANCOVA (p < 0001). Finally, the mean score of negative appraisals before intervention in the control and intervention groups was 4.49 ± 3.95 and 3.31 ± 2.32, respectively (p = 0.001), which changed to 4.75 ± 1.61 and 3.13 ± 3.44, respectively after intervention (p = 0.001). Despite the lack of significant changes within the groups, the difference between the two groups was significant using ANCOVA test (p = 0.007). The mean overall score of fear of childbirth in the intervention group decreased from 49.39 ± 8.21 to 40.42 ± 13.43 (p < 0.0001), while the mean overall score of fear of childbirth in the control group increased from 49.47 ± 9.06 to 52.09 ± 7.73 (p = 0.002).
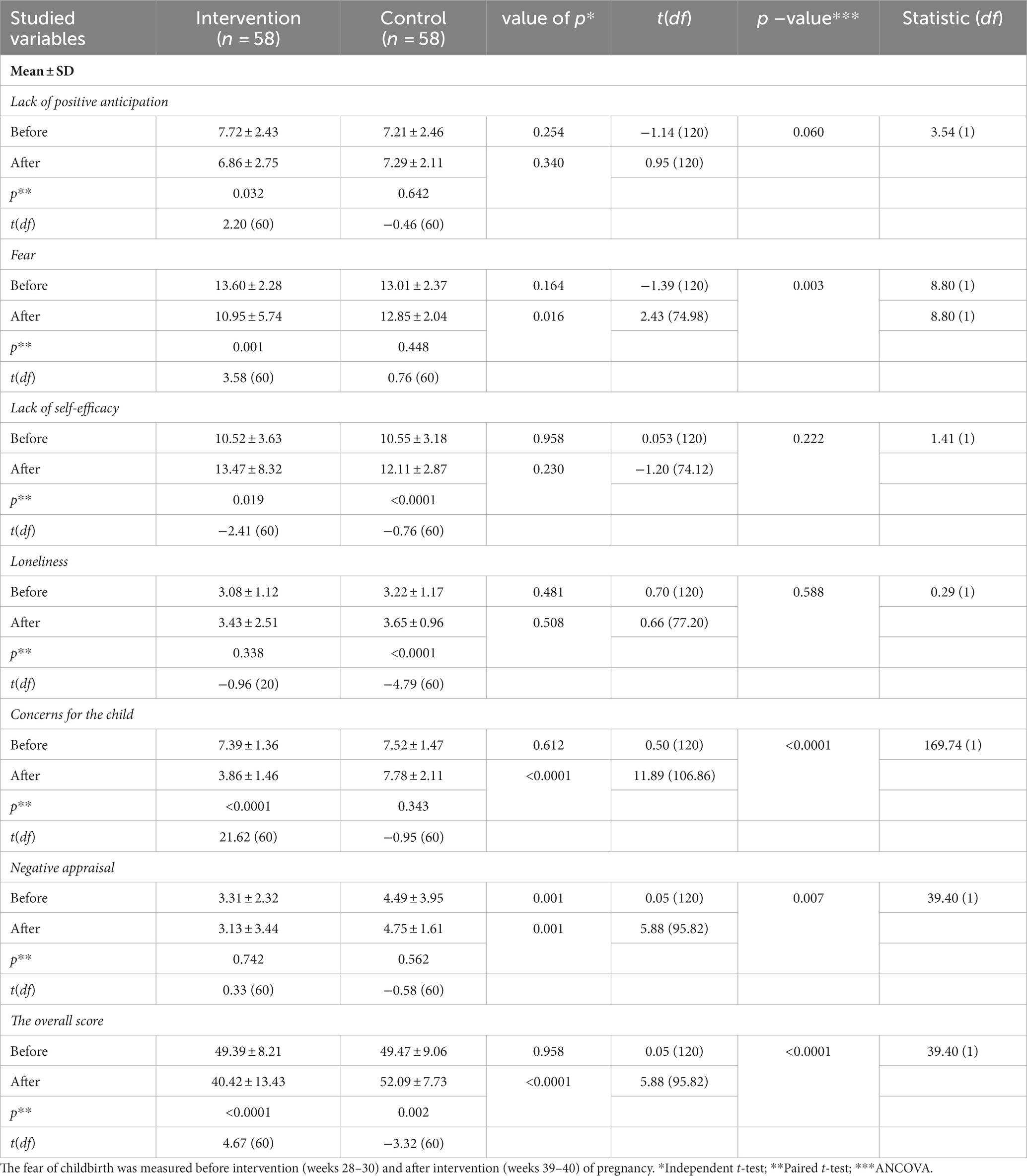
Table 2. Comparison of the mean score of the dimensions of WDEQ-A before and after intervention in the intervention and control groups.
Table 3 shows the difference in the mean score of the dimensions of WDEQ-B after delivery in the intervention and control groups. In all dimensions of fear of childbirth including lack of positive anticipation, fear, lack of self-efficacy, loneliness, concerns for the child, except negative appraisal, the score of the intervention group was significantly lower than that of the control group (p < 0.0001). The mean overall score of fear of childbirth after delivery in the control and intervention groups was 45.88 ± 7.10 and 27.13 ± 5.08, respectively, indicating a significant difference (p < 0.0001). No side effects were reported by participants in intervention or control groups.
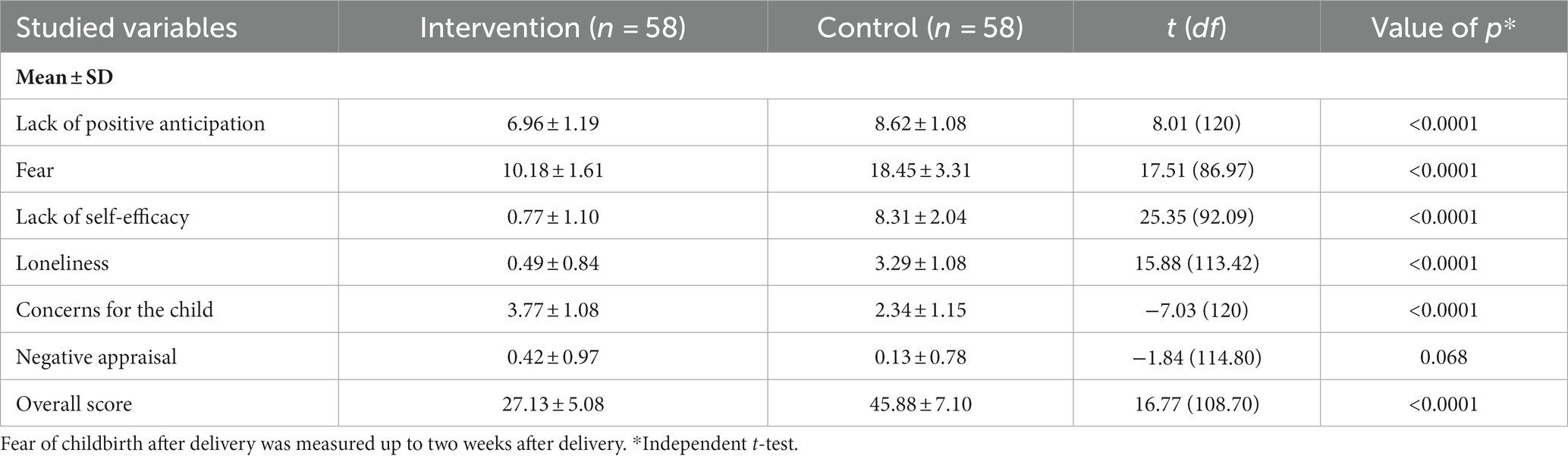
Table 3. Comparison of the mean score of the dimensions of WDEQ-B in the intervention and control groups.
This study was conducted to investigate the effect of EFT on the fear of childbirth in primiparous women. The results showed that the mean score of fear, concerns for the child, negative appraisal, and the overall score of Wijma-A were significantly improved in the intervention group compared to the control group. However, the two groups were not significantly different regarding lack of positive anticipation, lack of self-efficacy, and loneliness. The scores of all dimensions of Wijma-B except for negative appraisal were improved significantly in the intervention group compared to the control group.
EFT has been successfully used in treatment of various mental and physical disorders including depression, anxiety, phobias, post-traumatic stress disorder, irritable bowel syndrome, and obesity, proving to be effective usually within 1–10 sessions (Wells et al., 2003; Baker and Siegel, 2010). We could not find any study to investigate the effect of EFT on the dimensions of W-DEQ, but there are a number of studies that evaluated the effect of EFT on the stress, anxiety and fear of expectant mothers.
In a study on 120 pregnant women, for instance, Vural et al. investigated the role of EFT and conscious breathing in reducing fear of childbirth. They used the Subjective Units of Distress Scale and Wijma-B for measuring fear of childbirth. Their results showed that both types of intervention, namely EFT and conscious breathing, reduced the level of fear of childbirth, but the former had more profound and permanent effects (Vural and Aslan, 2019). Another study by Mardjan et al. was conducted in 2016 in Indonesia on 38 teenage pregnant women suffering from anxiety. Their study was aimed at investigating the effect of EFT on anxiety and cortisol levels, and they used Taylor Manifest Anxiety Scale (TMAS) and cortisol blood test for measuring anxiety level. Their results showed that EFT significantly contributes to the reduction of anxiety level and blood cortisol level by 57 and 43%, respectively, and that it indirectly affects the mother’s readiness for childbirth (Mardjan et al., 2018). In 2015, in a semi-quasi study with a pre-test-post-test design and control group in Tehran, Ghamsari et al. investigated the effect of EFT on perceived stress and tolerance of 30 pregnant women. They found that the experimental group’s scores on perceived stress significantly decreased while there was a significant increase in their scores of tolerance (Ghamsari and Lavasani, 2015). In Yuniarti et al. (2016) investigated the effect of EFT on the level of cortisol, immunoglobulin E, and the anxiety among pregnant women. Primiparous women who used this technique were more relaxed when facing childbirth (Yuniarti et al., 2016). Our results are in line with the above studies. The exact mechanism for stress and fear reduction of EFT is not clear, but evidence showed that improvement in physical parameters such as heart rate variability, hearth coherence, blood pressure, and level of cortisol, that all of them are predisposing factors for stress and anxiety, may play a main role in stress and fear reduction (Bach et al., 2019). Also, as EFT has almost similar mechanism to mindfulness, one of the underlying factors of stress reduction of both techniques is attention to present moments and monitor and acceptance (Lindsay et al., 2018).
Studies have shown that a high level of fear of childbirth before childbirth can persist for a long time after childbirth and that such fear is associated with the development of symptoms of post-traumatic stress disorder (Wijma et al., 1997). In their study on the fear of childbirth before, during and after childbirth, Alehagen et al. found that women with fear before childbirth are more likely to have fears during the active stage of labor and after childbirth (Alehagen et al., 2006). Screening to identify a high level of fear of childbirth during pregnancy can provide appropriate treatment for women with a high level of fear, possibly by reducing the risk of negative consequences in the future, both psychologically and obstetrically (Zar et al., 2001). Evidence from our study show that using EFT in the third trimester could reduce the fear of childbirth in postpartum women.
In Iran systematic efforts are being made in health centers to minimize the anxiety and fear of primiparous mothers, including counseling and pregnancy exercise under the supervision and guidance of an authorized midwife (Baker and Siegel, 2010). Of course, this sometimes makes it difficult for the mother to arrange her time to go to health centers and receive services (Roland-Price and Chamberlain, 2002). EFT enables mothers to do this technique either under the supervision of a teacher or independently at home without time limits and with the best possible results (Baker and Siegel, 2010).
Although, in the present study, the intervention based on EFT improved fear, concerns for the child, negative appraisal, and the overall score of Wijma-A, it failed to improve scores in the scales “lack of positive anticipation,” “lack of self-efficacy,” and “loneliness”. Satisfaction with childbirth is related to a variety of psychological factors which include, but are not limited to, sense of personal control and whether health providers and family are meeting the women’s expectations (Goodman et al., 2004). Therefore, it is likely that the EFT could not improve all these dimensions. Furthermore, the participants in the present study were primiparous and may had deeper fear of childbirth compared to women who already had other pregnancies, and this might have hindered their ability to overcome to any unanticipated situation happened around the time of labour and to experience a sense of self-efficacy making the improvement of the scales ‘lack of positive anticipation’ and ‘lack of self-efficacy difficult. Finally, physical and mental changes that occur during pregnancy might alienate a person from herself and the society around her (Rokach, 2004), and, although EFT could reduce feeling of loneliness to some extent, the changes did not reach a significant level.
The hypothesis of this study that EFT could significantly reduce the fear of childbirth was confirmed by our results. The results of this study can therefore be used by policy makers and health providers to improve the mental condition of primiparous women and to improve the quality of childbirth preparation classes.
This study has some strengths. First, it included a rigorous randomization of the sample in the two groups which eliminated selection bias and a design that allowed direct comparison between the two interventions. Second, a perspective design which assessed fear of childbirth before and after delivery (not only before it). Third, an adequate sample size was used in this study which was a priori calculated performing a power analysis. Finally, allocation to either group was not disclosed to participants, and interventions were similar (using sham therapy in the control group) enough to minimize the performance bias in women, and groups were comparable in terms of socio-demographic characteristics.
However, this study was not without limitations. First, we did not measure the cortisol level before and after the intervention. If we had, we could have come up with a better understanding of the role of EFT. Second, due to the spread of COVID-19 and the subsequent home quarantine, we were able to hold only one face-to-face training session. Third, the psychological effect of COVID-19 along with the home quarantine was not measured as a confounding factor affecting the women’s mental state and level of fear and anxiety. Fourth, recruitment was done only in two centers which might have created a selection bias in terms of participants’ education, age, and SES. Finally, the exclusion and inclusion criteria limited the study population. Therefore, future studies are recommended to replicate this study with a larger and more diverse population. Based on the strengths and limitations of the present study, further studies are advised to measure the cortisol level, rule out other causes of psychological disorders such as anxiety and depression, or be conducted in a multi-center design.
The results of this study showed that a 12-week EFT program can reduce the mean score of fear of childbirth in primiparous Iranian women, and this reduction is maintained even after delivery. It is recommended to use this technique in childbirth preparation classes to improve the mental health of these mothers.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ahvaz Jundishapur University of Medical Sciences. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
SE, KH, PA, and EM were contributed to design of the study, equally contributed to data analyzing, and interpretation. SE collected the data. SE and PA prepared the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
All expenses of this study were provided by Ahvaz Jundishapur University of Medical Sciences. The funder did not play any role in design, data collection, data analyzing and interpretation, or writing and submitting the manuscript to a journal.
This study was extracted from the master thesis of the lead investigator. We would like to thank all women who participated in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abedi, P., Hazeghi, N., Afshari, P., and Fakhri, A. (2016). The validity and reliability of Persian version of Wijma Delivery Expectancy/Experience Questionnaire (version a) among Iranian nulliparous women. Glob J Health Sci. 9:269. doi: 10.5539/gjhs.v9n2p269
Alehagen, S., Wijma, K., and Wijma, B. (2001). Fear during labor. Acta Obstet. Gynecol. Scand. 80, 315–320. doi: 10.1034/j.1600-0412.2001.080004315.x
Alehagen, S., Wijma, B., and Wijma, K. (2006). Fear of childbirth before, during, and after childbirth. Acta Obstet. Gynecol. Scand. 85, 56–62. doi: 10.1080/00016340500334844
Alijani, H., Borghei, N. S., and Behnampour, N. (2019). FOC in pregnancy and some of its effective factors. J Res Dev Nurs Midw. 16, 60–69. doi: 10.29252/jgbfnm.16.1.60
Areskog, B., Uddenberg, N., and Kjessler, B. (1983). Experience of delivery in women with and without antenatal fear of childbirth. Gynecol. Obstet. Investig. 16, 1–12. doi: 10.1159/000299205
Aynalem, Y., and Eneye, M. (2021). Fear of childbirth and associated factors among pregnant mothers who attend antenatal care service at Jinka public health facilities, Jinka town, southern Ethiopia. Int J Childbirth. 11, 101–111. doi: 10.1891/IJCBIRTH-D-20-00029
Bach, D., Groesbeck, G., Stapleton, P., Sims, R., Blickheuser, K., and Church, D. (2019). Clinical EFT (emotional freedom techniques) improves multiple physiological markers of health. J. Evid. Based Integ. Med. 24, 1–12. doi: 10.1177/2515690X18823691
Badiee, S., Ravanshad, Y., Azarfar, A., Dastfan, F., Babayi, S., and Mirzayi, N. (2013). Survey of cesarean deliveries and their causes in hospitals affiliated to Mashhad university of medical sciences, Iran, 2011. Iran J Obstet Gynecol Infertil. 16, 10–17. doi: 10.22038/IJOGI.2013.1899
Baker, A. H., and Siegel, M. (2010). Emotional freedom techniques (EFT) reduces intense fears: a partial replication and extension of Wells et al. Energy Psychol J. 2, 13–30. doi: 10.4236/psych.2019.107061
Chalmers, B. (1992). WHO appropriate technology for birth revisited. Br. J. Obstet. Gynaecol. 99, 709–710. doi: 10.1111/j.1471-0528.1992.tb13867.x
Church, D. (2013). Clinical EFT as an evidence-based practice for the treatment of psychological and physiological conditions. Psychology 4, 645–654. doi: 10.4236/psych.2013.48092
Church, D., Feinstein, D., Palmer-Hoffman, J., Stein, P. K., and Tranguch, A. (2020). Empirically supported psychological treatments: the challenge of evaluating clinical innovations. J. Nerv. Ment. Dis. 202, 699–709. doi: 10.1097/NMD.0000000000000188
Church, D., Yount, G., and Brooks, A. J. (2012). The effect of emotional freedom techniques on stress biochemistry: a randomized controlled trial. J. Nerv. Ment. Dis. 200, 891–896. doi: 10.1097/NMD.0b013e31826b9fc1
Church, D., Yount, G., Rachlin, K., Fox, L., and Nelms, J. (2018). Epigenetic effects of PTSD remediation in veterans using clinical emotional freedom techniques: a randomized controlled pilot study. Am. J. Health Promot. 32, 112–122. doi: 10.1177/0890117116661154
Delavar, G. S., and Alizadeh, G. J. (2014). The role of metacognitive beliefs and positive and negative affect in the fear of childbirth of pregnant women with first experience. IJNR 9, 10–18.
Fisk, N. M., and Glover, V. (1999). Association between maternal anxiety in pregnancy and increased uterine artery resistance index: cohort based study. BMJ 318, 153–157. doi: 10.1136/bmj.318.7177.153
Ghamsari, M. S., and Lavasani, M. G. (2015). Effectiveness of emotion freedom technique on pregnant women’s perceived stress and resilience. J. Educ. Sociol. 6, 118–122. doi: 10.7813/jes.2015/6-2/26
Goodman, P., Mackey, M. C., and Tavakoli, A. S. (2004). Factors related to childbirth satisfaction. J. Adv. Nurs. 46, 212–219. doi: 10.1111/j.1365-2648.2003.02981.x
Khwepeya, M., Lee, G. T., Chen, S. R., and Kuo, S. Y. (2018). Childbirth fear and related factors among pregnant and postpartum women in Malawi. BMC Pregnancy Childbirth 18:391. doi: 10.1186/s12884-018-2023-7
Lane, J. (2009). The neurochemistry of counterconditioning: acupressure desensitization in psychotherapy. Energy. Energy Psychology. 1, 31–44. doi: 10.9769/EPJ.2009.1.1.JRL
Lederman, R. (1990). Anxiety and stress in pregnancy: significance and nursing assessment. NAACOGS Clin. Issu. Perinat. Womens Health Nurs. 1, 279–288.
Lilliecreutz, C., Larén, J., Sydsjö, G., and Josefsson, A. (2016). Effect of maternal stress during pregnancy on the risk for preterm birth. BMC Pregnancy Childbirth 16:5. doi: 10.1186/s12884-015-0775-x
Lindsay, E. K., Young, S., Smyth, J. M., Brown, K. W., and Creswell, J. D. (2018). Acceptance lowers stress reactivity: dismantling mindfulness training in a randomized controlled trial. Psychoneuroendocrinology 87, 63–73. doi: 10.1016/j.psyneuen.2017.09.015
Lukasse, M., Schei, B., and Ryding, E. L., Group BS (2014). Prevalence and associated factors of fear of childbirth in six European countries. Sex Reprod. Healthc. 5, 99–106. doi: 10.1016/j.srhc.2014.06.007
Mardjan, M., Prabandari, Y. S., Hakimi, M., and Marchira, C. R. (2018). Emotional freedom techniques for reducing anxiety and cortisol level in pregnant adolescent primiparous. UJPH. 7, 1–6. doi: 10.15294/ujph.v7i1.19212
Negahban, T., and Ansari, A. (2009). Does fear of childbirth predict emergency cesarean section in Primiparous women? HAYAT 14, 73–81.
O’Connell, M. A., Leahy-Warren, P., Khashan, A. S., Kenny, L. C., and O’Neill, S. M. (2017). Worldwide prevalence of tocophobia in pregnant women: systematic review and meta-analysis. Acta Obstet. Gynecol. Scand. 96, 907–920. doi: 10.1111/aogs.13138
O’Connell, M. A., O’Neill, S. M., Dempsey, E., Khashan, A. S., Leahy-Warren, P., Smyth, R. M., et al. (2019). Interventions for fear of childbirth (tocophobia). Cochrane Database Syst. Rev. 2019:CD013321. doi: 10.1002/14651858.CD013321
Rabiepoor, S., Abedi, M., Saboory, E., and Khalkhali, H. R. (2019). Stress during pregnancy affected neonatal outcomes and changed cortisol and leptin levels both in mothers and newborns. J Neonatal Perinatal Med. 12, 209–219. doi: 10.3233/NPM-1818.
Rokach, A. (2004). Giving life: loneliness, pregnancy, and motherhood. Soc Behav Pers. Int. J. 32, 691–702. doi: 10.2224/sbp.2004.32.7.691
Roland-Price, A., and Chamberlain, Z. (2002). “Management of tocophobic women” in Preconceptional Medicine Paula and David Bloomer. ed. S. Arulkumaran, Oxford Academic, 281–288.
Ryding, E., Wijma, B., Wijma, K., and Rydhström, H. (1998). Fear of childbirth during pregnancy may increase the risk of emergency cesarean section. Acta Obstet. Gynecol. Scand. 77, 542–547. doi: 10.1034/j.1600-0412.1998.770512.x
Shakarami, A., Mirghafourvand, M., Abdolalipour, S., Jafarabadi, M. A., and Iravani, M. (2021). Comparison of fear, anxiety and self-efficacy of childbirth among primiparous and multiparous women. BMC Pregnancy Childbirth 21:642. doi: 10.1186/s12884-021-04114-8
Stapleton, P., Bannatyne, A., Chatwin, H., Urzi, K.-C., Porter, B., and Sheldon, T. (2017). Secondary psychological outcomes in a controlled trial of emotional freedom techniques and cognitive behaviour therapy in the treatment of food cravings. Complement. Ther. Clin. Pract. 28, 136–145. doi: 10.1016/j.ctcp.2017.06.004
Størksen, H. T., Garthus-Niegel, S., Adams, S. S., Vangen, S., and Eberhard-Gran, M. (2015). Fear of childbirth and elective caesarean section: a population-based study. BMC Pregnancy Childbirth 15:221. doi: 10.1186/s12884-015-0655-4
Toohill, J., Fenwick, J., Gamble, J., and Creedy, D. K. (2014). Prevalence of childbirth fear in an Australian sample of pregnant women. BMC Pregnancy Childbirth 14, 1–10. doi: 10.1186/1471-2393-14-275
Vural, P. I., and Aslan, E. (2019). Emotional freedom techniques and breathing awareness to reduce childbirth fear: a randomized controlled study. Complement. Ther. Clin. Pract. 35, 224–231. doi: 10.1016/j.ctcp.2019.02.011
Waldenström, U., Hildingsson, I., and Ryding, E.-L. (2006). Antenatal fear of childbirth and its association with subsequent caesarean section and experience of childbirth. BJOG 113, 638–646. doi: 10.1111/j.1471-0528.2006.00950.x
Wells, S., Polglase, K., Andrews, H. B., Carrington, P., and Baker, A. H. (2003). Evaluation of a meridian-based intervention, emotional freedom techniques (EFT), for reducing specific phobias of small animals. J. Clin. Psychol. 59, 943–966. doi: 10.1002/jclp.10189
Wijma, K. (2003). Why focus on ‘fear of childbirth’? J. Psychosom. Obstet. Gynecol. 24, 141–143. doi: 10.3109/01674820309039667
Wijma, K., Söderquist, J., and Wijma, B. (1997). Posttraumatic stress disorder after childbirth: a cross sectional study. J. Anxiety Disord. 11, 587–597. doi: 10.1016/S0887-6185(97)00041-8
Wjma, K., Wjma, B., and Zar, M. (1998). Psychometric aspects of the W-DEQ; a new questionnaire for the measurement of fear of childbirth. J Psychosom Obster Gynecol. 19, 84–97. doi: 10.3109/01674829809048501
World Health Organization. (2023). WHO Statement on Caesarean Section Rates. Available at: https://apps.who.int/iris/bitstream/handle/10665/161442/WHO_RHR_15.02_eng.pdf. (Accessed June 28, 2023)
Yuniarti, Y., Suwondo, A., Runjati, R., Maharani, S. I., Ofiwijayanti, H., and Anastasia, S.. (2016). Influence of Spiritual Therapy Emotional Freedom Technique (Seft) on Cortisol Levels and Immunoglobulin e (Study of Anxiety in Pregnant Women in Independent Practice Midwives SEMARANG). ASEAN/Asian Academic Society International Conference Proceeding Series.
Keywords: fear of childbirth, primiparous, emotional freedom technique (EFT), Wijma Delivery Expectancy/Experience, WDEQ-B
Citation: Emadi SF, Hekmat K, Abedi P and Maraghi E (2024) Effect of emotional freedom technique on the fear of childbirth in Iranian primiparous women: a randomized controlled trial. Front. Psychol. 14:1145229. doi: 10.3389/fpsyg.2023.1145229
Received: 15 January 2023; Accepted: 28 November 2023;
Published: 08 January 2024.
Edited by:
Alexander V. Libin, MedStar Health Research Institute (MHRI), United StatesReviewed by:
Laura Bozicevic, University of Liverpool, United KingdomCopyright © 2024 Emadi, Hekmat, Abedi and Maraghi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Khadijeh Hekmat, SGVrbWF0MTM0NkBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.