
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 31 May 2023
Sec. Psycho-Oncology
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1138070
Objective: Cognitive-behavioral stress management (CBSM) is a psychotherapy that helps patients cognize and manage stress to improve mental health and quality of life. This study aimed to explore the influence of CBSM on anxiety, depression, and quality of life in non-small cell lung cancer (NSCLC) patients.
Methods: In total, 172 NSCLC patients who received tumor resection were randomized 1:1 into the usual care (UC) group (N = 86) and CBSM group (N = 86) to receive 10-week UC and CBSM interventions. Moreover, all participants attended a 6-month follow-up.
Results: Hospital Anxiety and Depression Scales (HADS)-anxiety score at 3rd month (M3) (P = 0.015) and 6th month (M6) (P = 0.018), HADS-depression score at M3 (P = 0.040) and M6 (P = 0.028), and depression rate at M6 (P = 0.035) were descended in CBSM group compared to UC group. Besides, depression severity was reduced at M6 (P = 0.041) in CBSM group compared to UC group, but anxiety severity only showed a decreased trend (P = 0.051). Additionally, Quality of Life Questionnaire-Core 30 (QLQ-C30) global health status score and QLQ-C30 function score at 1st month (M1), M3, and M6 were elevated (all P < 0.05), while QLQ-C30 symptoms score was declined at M1 (P = 0.031) and M3 (P = 0.014) in CBSM group compared to UC group. Notably, the efficacy of CBSM was impressive in patients with baseline depression or undergoing adjuvant therapy.
Conclusion: CBSM is a feasible intervention that effectively improves mental health and quality of life in postoperative NSCLC patients.
Non-small cell lung cancer (NSCLC) is responsible for about 80–85% of lung cancer, which is one of the leading causes of cancer-related deaths around the whole world (Sung et al., 2021; Chen P. et al., 2022). Generally, the treatment methods for NSCLC include surgery, radiotherapy, chemotherapy, immunotherapy, targeted therapy, etc., which have developed to some extent in recent years (Alexander et al., 2020; Mithoowani and Febbraro, 2022). However, NSCLC patients still suffer burdens of symptoms (such as pain, dyspnea, etc.), recurrence, and economics, which all further cause negative influences on their mental health and quality of life (Vijayvergia et al., 2015; Buja et al., 2021; Bowes et al., 2022; Kroll et al., 2022; Merlo et al., 2022). Notably, 30.1–49.6% of postoperative NSCLC patients experience anxiety or depression, and 6–52% of postoperative NSCLC patients experience a decrease in quality of life, which may reduce the treatment adherence of patients and even negatively affect their clinical outcomes (Moller and Sartipy, 2012; Arrieta et al., 2013; Lowery et al., 2014; Huang et al., 2020; Iovoli et al., 2022). Therefore, it is crucial to find a feasible management to improve the mental health and quality of life in NSCLC patients.
Cognitive-behavioral stress management (CBSM) is a psychotherapy that helps patients prevent maladaptive cognitions and improve their ability to cope with stress (Hofmann et al., 2012; Francis and Kumar, 2013; Nakao et al., 2021). Unlike other common psychological interventions such as reminiscence therapy which increases happiness by recalling past memories or music therapy which improves emotions and quality of life through distraction, CBSM focuses on direct stress management of patients, which helps them establish coping strategies early on to ameliorate mental health and quality of life (Kasl-Godley and Gatz, 2000; Francis and Kumar, 2013; Chirico et al., 2020). One previous study suggests that CBSM reduces the Center for Epidemiologic Studies-Depression scale score in females with non-metastatic breast cancer (Stagl et al., 2015a). In addition, another study reveals that CBSM can effectively enhance the Functional Assessment of Cancer Therapy-General (FACT-G) score in prostate cancer patients after surgery (Penedo et al., 2004). Furthermore, one research reports that an intervention involving CBSM declines the hospital anxiety and depression scale (HADS) score and increases the Short-Form Health Surveys score in cancer survivors (Borosund et al., 2020). These studies reveal that CBSM is a beneficial intervention mode to relieve patients' mental health as well as improve their quality of life. Notably, NSCLC patients may suffer from similar or even more serious mental stress and worse quality of life than the above cancer patients due to the high incidence rate and mortality (Pitman et al., 2018). Therefore, we suppose that CBSM may also be a good fit for NSCLC patients. However, there is no study reporting the effect of CBSM on NSCLC patients.
Therefore, this study aimed at investigating the influence of CBSM on ameliorating mental health and enhancing the quality of life in postoperative NSCLC patients.
In this randomized, controlled research, a total of 172 NSCLC patients who received tumor resection were continuously enrolled from August 2019 to November 2021. The inclusion criteria were: (a) diagnosis with NSCLC by pathology; (b) aged more than 18 years; (c) the expected survival time over 1 year; (d) received tumor resection; (e) could complete assessments in this study. The exclusion criteria were: (a) complicated with other primary carcinomas or malignancies; (b) incapable of normal communication; (c) had a severe mental disorder or cognitive impairment. This research protocol was reviewed and approved by the Ethics Committee of Harbin Medical University Cancer Hospital, approval number [2018-164-IIT]. All patients provided written informed consent.
The included patients were randomized into two groups after receiving baseline assessments, one group received the CBSM intervention (n = 86) and the other group received the usual care (UC) intervention (n = 86). Survival status and health information were updated weekly by the charge nurses. Patients in both groups received routine follow-up for 6 months, with the first 10 weeks of intervention or education at the rehabilitation center of our hospital. The assessment scales for this study included the HADS and quality of life questionnaire-core 30 (QLQ-C30), which patients self-completed at discharge (M0), 1st month (M1), 3rd month (M3), and 6th month (M6) after discharge. All study procedures were approved by the Ethics Committee of Harbin Medical University Cancer Hospital.
Demographics, concomitant disease, disease-related information, and therapy-related information of patients were collected, which were screened from the Electronic Medical Record System, entered by one investigator, and re-checked by another investigator.
Random assignment (1:1) was carried out by designated investigators who were blinded to patient information using the CLEANWEB® software. Blocks size was selected as 4. After randomization, the patients were told which group they were assigned to. As a result, eighty-six patients were assigned to the CBSM group, and eighty-six patients were assigned to the UC group.
UC was carried out for NSCLC patients in the UC group once a week for 10 weeks by trained nurses. Usual care was conducted in a group-based form (5–6 patients per group). Each weekly group training lasted about 90 min including 60-min didactic portion and 30-min free time, in which didactic portion mainly contained health education, rehabilitation care education, and answering questions.
CBSM was applied to NSCLC patients in the CBSM group once a week for 10 weeks. CBSM was conducted in a group-based form (5-6 patients per group) by trained nurses. Each weekly group training lasted about 90 min, including a didactic portion for 60 min (the same content as the UC group plus special interventions) and relaxation training for 30 min. The additional special interventions of didactic portion contained: (a) stress management, including stress awareness, cognitive adjustment, anger management, and assertiveness establishment; (b) information associated with NSCLC: including bodily changes, fears over progression, coping with symptoms, and frustration with health care; (c) pain care: including the management of surgical pain, rehabilitation pain, and cancer-related pain. The relaxation training contained deep breathing, muscle relaxation, and meditation (Penedo et al., 2008). The study sessions were shown in Supplementary Table 1. All study procedures were approved by the Ethics Committee of Harbin Medical University Cancer Hospital.
The self-assessment scale questionnaires used in this study were distributed to patients at appropriate times by their charge nurses. For all patients, the HADS and QLQ-C30 scores were evaluated at M0, M1, M3, and M6. The HADS score was conducted to evaluate anxiety and depression, and the severity was classified as no (0~7), mild (8~10), moderate (11~14), and severe (15~21) (Zigmond and Snaith, 1983). The QLQ-C30 score was performed to evaluate the quality of life, in which the dimension of QLQ-C30 included pain, functions, symptoms, fatigue, etc. (Aaronson et al., 1993). Those self-assessment score results were entered by one investigator and re-checked by another investigator.
The sample size calculation was performed per the hypothesis that the mean M6 QLQ-C30 global health status in the CBSM group was 75, while the mean M6 QLQ-C30 global health status in the US group was 70. The standard deviation (SD) was supposed as 10. With the significance (α) level of 0.05 and the power of 85%, the minimum sample size was 72 for each group and then adjusted to 86 considering the drop-out possibility of 20%. Comparisons between the two groups were determined by the χ2 test, Student t-test, and Wilcoxon rank-sum test. P < 0.05 indicated significance. SPSS v.22.0 was used for data processing and GraphPad Prism v.7.0 was used for figure plotting.
The study flow of our study was shown in the Consort Diagram (Figure 1). The UC group consisted of 66 (76.7%) males and 20 (23.3%) females, whose mean age was 59.4 ± 10.1 years. Meanwhile, the CBSM group consisted of 70 (81.4%) males and 16 (18.6%) females, whose mean age was 60.8 ± 9.3 years. Additionally, no difference was found in clinical characteristics between UC group and CBSM group, including demographics, medical histories, tumor characteristics, treatment, as well as HADS and QLQ-C30 scores at M0 (all P > 0.05) (Table 1).
HADS-A score was declined at M3 (6.1 ± 2.3 vs. 7.1 ± 2.8) (P = 0.015) and M6 (5.9 ± 2.4 vs. 6.9 ± 2.6) (P = 0.018) in CBSM group compared to UC group (Figure 2A). Besides, HADS-D score was also reduced at M3 (6.2 ± 2.8 vs. 7.2 ± 2.8) (P = 0.040) and M6 (6.0 ± 2.6 vs. 7.0 ± 2.7) (P = 0.028) in CBSM group compared to UC group (Figure 2B).
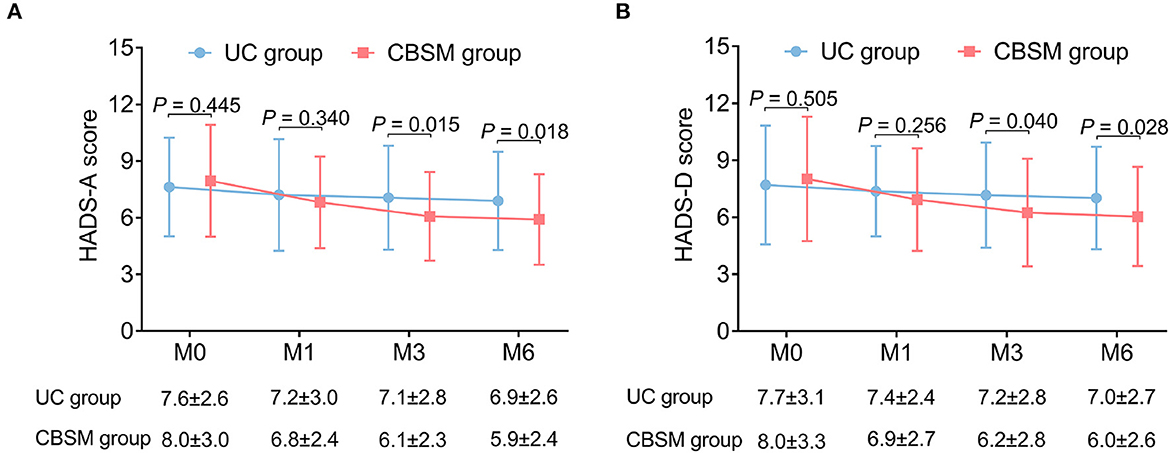
Figure 2. Comparison of HADS scores between groups. HADS-A score (A) and HADS-D score (B) were decreased at M3 and M6 in CBSM group compared with UC group.
In terms of anxiety rate, there was no discrepancy between groups at any assessment time points (all P > 0.05), however, anxiety rate showed a decreasing trend at M6 in CBSM group compared with UC group although it did not reach statistical significance (20.3 vs. 34.2%) (P = 0.057) (Figure 3A). Furthermore, depression rate was descended at M6 (18.9 vs. 34.2%) (P = 0.035) in CBSM group compared to UC group (Figure 3B).
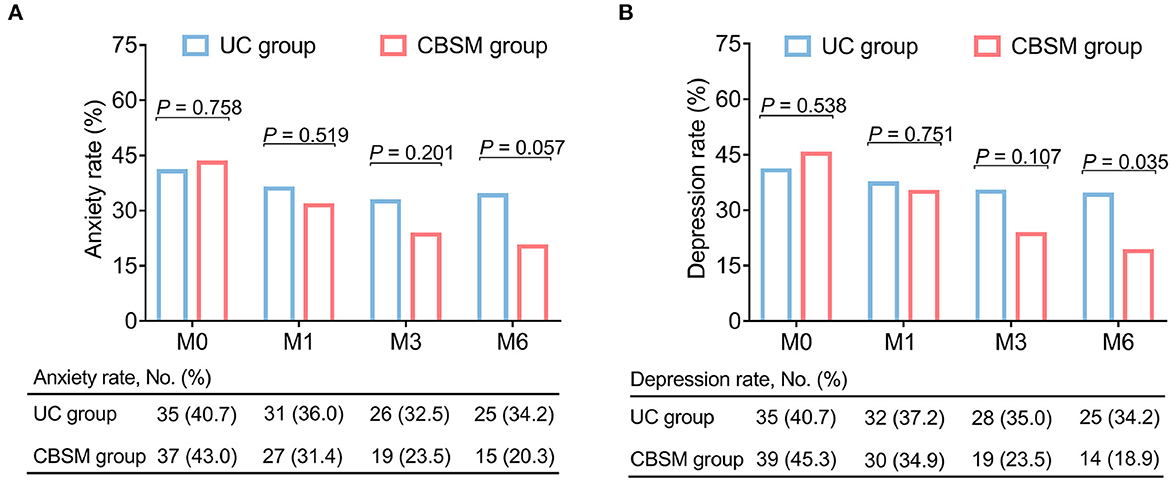
Figure 3. Comparison of anxiety rate and depression rate between groups. Anxiety rate showed a decreasing trend at M6 in CBSM group compared with UC group (A), depression rate was reduced at M6 in CBSM group compared with UC group (B).
In general, no discrepancy was found in anxiety severity between groups at any assessment time points (all P > 0.05), but anxiety severity tended to decrease at M6 in CBSM group compared to UC group without statistical significance (P = 0.051). Notably, depression severity declined at M6 (P = 0.041) in CBSM group compared with UC group (Table 2).
QLQ-C30 global health status score was increased at M1 (72.6 ± 10.8 vs. 68.0 ± 12.7) (P = 0.013), M3 (76.4 ± 13.6 vs. 70.4 ± 15.6) (P = 0.010), and M6 (78.8 ± 12.4 vs. 72.9 ± 13.5) (P = 0.006) in CBSM group compared to UC group (Figure 4A). Moreover, QLQ-C30 function score was ascended at M1 (68.9 ± 15.7 vs. 63.9 ± 14.2) (P = 0.032), M3 (73.2 ± 14.7 vs. 68.1 ± 13.5) (P = 0.024), and M6 (76.1 ± 13.2 vs. 70.1 ± 14.8) (P = 0.010) in CBSM group compared to UC group (Figure 4B). Regarding QLQ-C30 symptoms score, it was declined at M1 (27.3 ± 13.8 vs. 32.3 ± 16.1) (P = 0.031) and M3 (24.3 ± 13.7 vs. 30.1 ± 15.5) (P = 0.014) in CBSM group compared to UC group (Figure 4C).
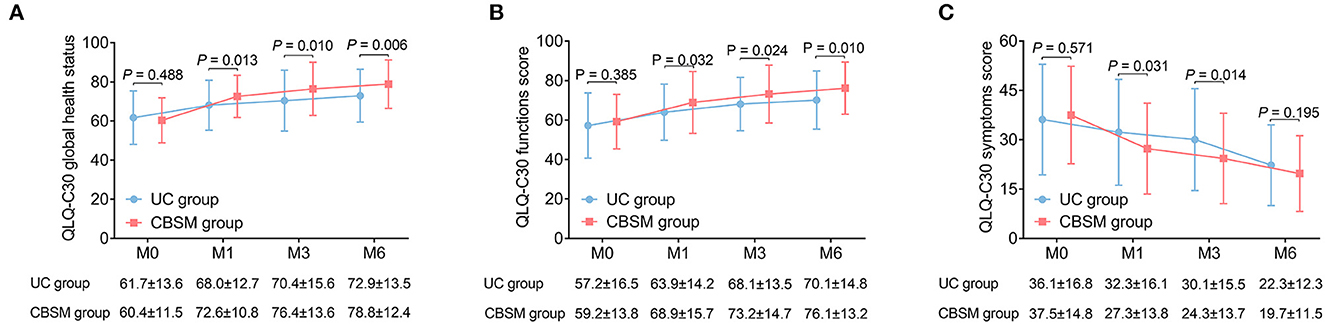
Figure 4. Comparison of QLQ-C30 scores between groups. QLQ-C30 global health status score was increased at M1, M3, and M6 (A), QLQ-C30 function score was elevated at M1, M3, and M6 (B), while QLQ-C30 symptoms score was declined at M1 and M3 (C) in CBSM group compared to UC group.
In NSCLC patients without baseline anxiety, QLQ-C30 global health status was elevated at M6 in CBSM group compared to UC group (P = 0.010). In NSCLC patients with baseline anxiety, QLQ-C30 functions score was ascended at M6 in CBSM group compared to UC group (P = 0.026) (Table 3). Moreover, in NSCLC patients without baseline depression, HADS-A score was declined at M6 in CBSM group compared to UC group (P = 0.027). In NSCLC patients with baseline depression, HADS-D score (P = 0.006) was descended at M6, but QLQ-C30 global health status (P = 0.017) and QLQ-C30 functions score (P = 0.002) increased at M6 in CBSM group compared to UC group.
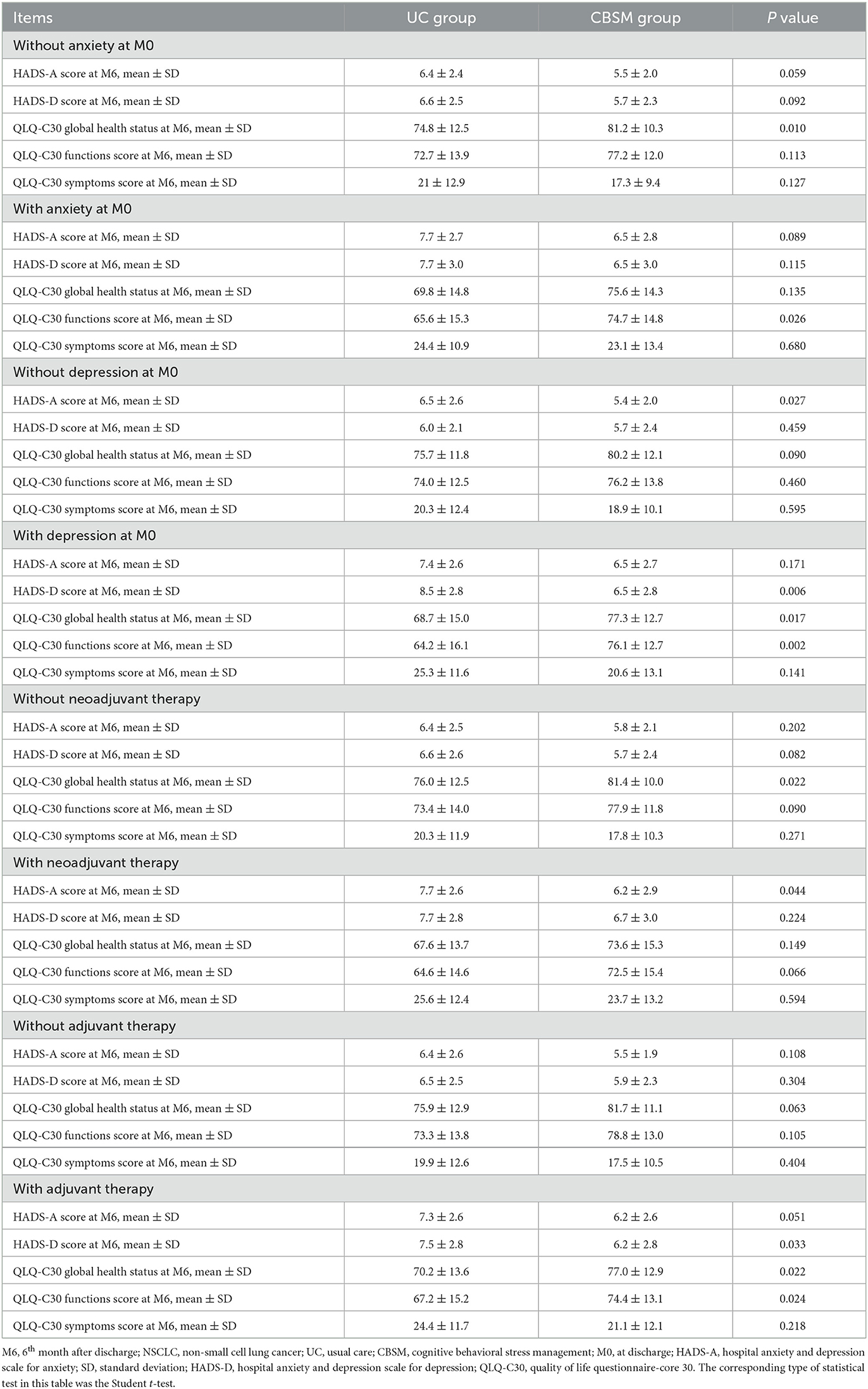
Table 3. Subgroup analysis of outcomes at M6 based on anxiety at baseline, depression at baseline, neoadjuvant therapy, and adjuvant therapy among the NSCLC patients.
In NSCLC patients without neoadjuvant therapy, QLQ-C30 global health status (P = 0.022) was elevated at M6 in CBSM group compared to UC group. In NSCLC patients with neoadjuvant therapy, HADS-A score (P = 0.044) decreased at M6 in CBSM group compared to UC group (Table 3). In addition, in NSCLC patients without adjuvant therapy, there was no discrepancy in HADS scores or QLQ-C30 scores between groups at M6 (all P > 0.05). In NSCLC patients with adjuvant therapy, HADS-D score (P = 0.033) was descended at M6, whereas QLQ-C30 global health status (P = 0.022) and QLQ-C30 functions score (P = 0.024) were both elevated at M6 in CBSM group compared to UC group.
Additionally, by subgroup analyses based on age, gender, and TNM stage, it was revealed that the efficacy of CBSM in NSCLC patients with age <60 years, males, and NSCLC patients with TNM stage II or III was better (Supplementary Table 2).
Previous studies exhibit that CBSM improves anxiety and depression in many cancer patients (Bouchard et al., 2019; Tang et al., 2020). For example, one meta-analysis shows that CBSM reduces anxiety and depression in breast cancer patients (Tang et al., 2020). Moreover, another research indicates that CBSM also relieves anxiety in men with advanced prostate cancer (Bouchard et al., 2019). Similar to previous studies, our study found that CBSM decreased anxiety and depression reflected by HADS to some degree compared to UC in NSCLC patients. The possible explanations were as follows: (1) CBSM helped patients deal with negative emotions, release stress, and promoted stress management, thus alleviated anxiety and depression in patients (Nakao et al., 2021). (2) CBSM clarified the patients' knowledge of the disease, which decreased their fear of the disease and increased their confidence in the current medical level, thus relieving the patients' anxiety and depression (Chen J. et al., 2022). (3) Through relaxation training, CBSM fully alleviated the patients' physical and mental pressure, reduced their mental burden, and thus alleviated their anxiety and depression (Stagl et al., 2015b; Chen J. et al., 2022). Notably, CBSM did not reduce anxiety severity at any assessment time points and only decreased depression severity at M6 compared to UC in NSCLC patients. The possible reason was as follows: Most NSCLC patients were in the status of no/mild anxiety or depression, while the number of NSCLC patients who were in the status of moderate/severe anxiety or depression was small, resulting in a less significant effect of CBSM.
In addition to improving mental health, enhancing the quality of life in NSCLC patients is a noteworthy issue. CBSM is believed to increase the quality of life in some cancer patients (Penedo et al., 2007; Acevedo-Ibarra et al., 2019). For example, one study suggests that CBSM effectively elevates the quality of life in colorectal cancer patients (Acevedo-Ibarra et al., 2019). Another study also observes that CBSM enhances the FACT-G score in patients with postoperative prostate cancer patients (Penedo et al., 2007). Similarly, our study revealed that CBSM enhanced quality of life reflected by QLQ-C30 compared to UC in NSCLC patients. This might be because: (1) CBSM reduced the pressure and psychological burden of patients, enabling them to adjust their emotions timely and face treatment actively, thus improving their quality of life (Ghazavi et al., 2016). (2) CBSM was a skill that continuously benefited patients through 10-week interventions. Through this skill, patients could elevate their own life index in a timely and dynamic manner for continuous improvement of quality of life.
Furthermore, according to the subgroup analysis, our study found that CBSM had a better effect on patients with depression at baseline or adjuvant therapy than those without. The possible reasons were as follows: (1) Compared with the patients without depression at baseline, those with depression at baseline were more emotionally unstable. When receiving CBSM, those patients might release more pressure and negative emotions than patients without depression at baseline, so as to get a better treatment impact (Wu et al., 2021; Yu, 2021). (2) Adjuvant treatment imposed a certain burden on patients, whose side effects might negatively influence their quality of life (Fallowfield, 2005; Bezjak et al., 2008; Poghosyan et al., 2013). Therefore, patients with adjuvant therapy might benefit more from pain care and relaxation training than those without, but further exploration was needed. Meanwhile, our study also found that CBSM was more effective in patients with age <60 years, males, and patients with TNM stage II or III. These findings might be because: (1) Patients with age ≥60 years might have poor cognitive abilities and were not sensitive to CBSM care (Lovden et al., 2020). (2) The sample size of female patients in our study was relatively small. (3) Patients with TNM stage I had milder disease symptoms, better survival, and their own symptoms of anxiety and depression might be relatively mild, thus benefiting less from CBSM (Huang et al., 2020; Deng and Chen, 2023).
There were some limitations in this study: (1) Our study was a single-center study, which might lead to the bias of selection. (2) Our study only recruited postoperative NSCLC patients. While the effect of CBSM in NSCLC patients who were unable to receive surgery was unknown. (3) The assessment scale used to assess anxiety and depression was single in our study, only HADS. Therefore, future research should consider using more assessment scales. (4) It was reported that a short-term CBSM intervention would have a long-term effect on breast cancer patients (Stagl et al., 2015b). Therefore, further studies should explore the effect of long-term influence of CBSM in NSCLC patients. (5) Our study did not set blinding due to the fact that patients were easily aware of their grouping during the nursing process.
In conclusion, CBSM relieves anxiety and depression, as well as improves the quality of life in postoperative NSCLC patients, particularly in those having baseline depression symptom or adjuvant therapy. Our findings indicate that CBSM may be an effective intervention for postoperative NSCLC patients. However, further multi-center studies are required for confirmation, and the effect of CBSM in NSCLC patients who are unable to receive surgery should be also investigated in future studies.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Harbin Medical University Cancer Hospital. The patients/participants provided their written informed consent to participate in this study.
FW and YH conceived and designed the study. FW, SZ, and YH collected and analyzed the data. FW and SZ wrote the manuscript. BS and YH revised the manuscript. All authors read and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1138070/full#supplementary-material
Aaronson, N. K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N. J., et al. (1993). The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 85, 365–376. doi: 10.1093/jnci/85.5.365
Acevedo-Ibarra, J. N., Juarez-Garcia, D. M., Espinoza-Velazco, A., and Buenaventura-Cisneros, S. (2019). Cognitive Behavioral Stress Management intervention in Mexican colorectal cancer patients: Pilot study. Psychooncology 28, 1445–1452. doi: 10.1002/pon.5094
Alexander, M., Kim, S. Y., and Cheng, H. (2020). Update 2020: Management of non-small cell lung cancer. Lung 198, 897–907. doi: 10.1007/s00408-020-00407-5
Arrieta, O., Angulo, L. P., Nunez-Valencia, C., Dorantes-Gallareta, Y., Macedo, E. O., Martinez-Lopez, D., et al. (2013). Association of depression and anxiety on quality of life, treatment adherence, and prognosis in patients with advanced non-small cell lung cancer. Ann. Surg. Oncol. 20, 1941–1948. doi: 10.1245/s10434-012-2793-5
Bezjak, A., Lee, C. W., Ding, K., Brundage, M., Winton, T., Graham, B., et al. (2008). Quality-of-life outcomes for adjuvant chemotherapy in early-stage non-small-cell lung cancer: results from a randomized trial, JBR.10. J. Clin. Oncol. 26, 5052–5059. doi: 10.1200/JCO.2007.12.6094
Borosund, E., Ehlers, S. L., Varsi, C., Clark, M. M., Andrykowski, M. A., Cvancarova, M., et al. (2020). Results from a randomized controlled trial testing StressProffen; an application-based stress-management intervention for cancer survivors. Cancer Med. 9, 3775–3785. doi: 10.1002/cam4.3000
Bouchard, L. C., Yanez, B., Dahn, J. R., Flury, S. C., Perry, K. T., Mohr, D. C., et al. (2019). Brief report of a tablet-delivered psychosocial intervention for men with advanced prostate cancer: Acceptability and efficacy by race. Transl. Behav. Med. 9, 629–637. doi: 10.1093/tbm/iby089
Bowes, K., Jovanoski, N., Brown, A. E., Di Maio, D., Belleli, R., Chadda, S., et al. (2022). Treatment patterns and survival of patients with locoregional recurrence in early-stage NSCLC: a literature review of real-world evidence. Med. Oncol. 40, 4. doi: 10.1007/s12032-022-01790-0
Buja, A., Pasello, G., De Luca, G., Bortolami, A., Zorzi, M., Rea, F., et al. (2021). Non-Small-Cell Lung Cancer: Real-World Cost Consequence Analysis. JCO Oncol. Pract.17, e1085–e1093. doi: 10.1200/OP.20.00863
Chen, J., Qian, L., Chen, C., and Wang, X. (2022). The characteristics of fear of recurrence and the effect of cognitive-behavioral stress management intervention in patients after radiofrequency ablation of atrial fibrillation. Evid Based Complement Alternat. Med. 2022, 6916302. doi: 10.1155/2022/6916302
Chen, P., Liu, Y., Wen, Y., and Zhou, C. (2022). Non-small cell lung cancer in China. Cancer Commun. 42, 937–970. doi: 10.1002/cac2.12359
Chirico, A., Maiorano, P., Indovina, P., Milanese, C., Giordano, G. G., Alivernini, F., et al. (2020). Virtual reality and music therapy as distraction interventions to alleviate anxiety and improve mood states in breast cancer patients during chemotherapy. J. Cell Physiol. 235, 5353–5362. doi: 10.1002/jcp.29422
Deng, L., and Chen, B. (2023). Two-scale assessment of anxiety and depression in postoperative non-small cell lung cancer patients: their prevalence, risk factors, and prognostic potency. Ir. J. Med. Sci. doi: 10.1007/s11845-023-03321-w. [Epub ahead of print].
Fallowfield, L. (2005). Acceptance of adjuvant therapy and quality of life issues. Breast 14, 612–616. doi: 10.1016/j.breast.2005.08.012
Francis, J. L., and Kumar, A. (2013). Psychological treatment of late-life depression. Psychiatr. Clin. North Am. 36, 561–575. doi: 10.1016/j.psc.2013.08.005
Ghazavi, Z., Rahimi, E., Yazdani, M., and Afshar, H. (2016). Effect of cognitive behavioral stress management program on psychosomatic patients' quality of life. Iran J. Nurs. Midwifery Res. 21, 510–515. doi: 10.4103/1735-9066.193415
Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., and Fang, A. (2012). The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit. Ther. Res. 36, 427–440. doi: 10.1007/s10608-012-9476-1
Huang, X., Zhang, T. Z., Li, G. H., Liu, L., and Xu, G. Q. (2020). Prevalence and correlation of anxiety and depression on the prognosis of postoperative non-small-cell lung cancer patients in North China. Medicine (Baltimore) 99, e19087. doi: 10.1097/MD.0000000000019087
Iovoli, A. J., Yu, B., Ma, S. J., Farrugia, M. K., Dexter, E. U., Yendamuri, S., et al. (2022). Quality of life after stereotactic body radiation therapy or surgery for early-stage NSCLC: a systematic review. JTO Clin. Res. Rep. 3, 100417. doi: 10.1016/j.jtocrr.2022.100417
Kasl-Godley, J., and Gatz, M. (2000). Psychosocial interventions for individuals with dementia: an integration of theory, therapy, and a clinical understanding of dementia. Clin. Psychol. Rev. 20, 755–782. doi: 10.1016/S0272-7358(99)00062-8
Kroll, J. L., Kim, S., Cho, D., Weathers, S. P., Chen, A. B., Smith, G., et al. (2022). Financial distress and its associated burden in couples coping with an advanced cancer. Support Care Cancer 30, 4485–4495. doi: 10.1007/s00520-021-06758-w
Lovden, M., Fratiglioni, L., Glymour, M. M., Lindenberger, U., and Tucker-Drob, E. M. (2020). Education and cognitive functioning across the life span. Psychol. Sci. Public Interest. 21, 6–41. doi: 10.1177/1529100620920576
Lowery, A. E., Krebs, P., Coups, E. J., Feinstein, M. B., Burkhalter, J. E., Park, B. J., et al. (2014). Impact of symptom burden in post-surgical non-small cell lung cancer survivors. Support Care Cancer 22, 173–180. doi: 10.1007/s00520-013-1968-3
Merlo, A., Carlson, R., Espey, J., Williams, B. M., Balakrishnan, P., Chen, S., et al. (2022). Postoperative Symptom Burden in Patients Undergoing Lung Cancer Surgery. J. Pain Symptom. Manage. 64, 254–267. doi: 10.1016/j.jpainsymman.2022.05.016
Mithoowani, H., and Febbraro, M. (2022). Non-small-cell lung cancer in 2022: a review for general practitioners in oncology. Curr. Oncol. 29, 1828–1839. doi: 10.3390/curroncol29030150
Moller, A., and Sartipy, U. (2012). Predictors of postoperative quality of life after surgery for lung cancer. J. Thorac. Oncol. 7, 406–411. doi: 10.1097/JTO.0b013e3182398e82
Nakao, M., Shirotsuki, K., and Sugaya, N. (2021). Cognitive-behavioral therapy for management of mental health and stress-related disorders: Recent advances in techniques and technologies. Biopsychosoc. Med. 15, 16. doi: 10.1186/s13030-021-00219-w
Penedo, F. J., Antoni, M. H., and Schneiderman, N. (2008). Cognitive-Behavioral Stress Management for Prostate Cancer Recovery: Facilitator Guide. New York: Oxford University Press. doi: 10.1093/med:psych/9780195336979.001.0001
Penedo, F. J., Dahn, J. R., Molton, I., Gonzalez, J. S., Kinsinger, D., Roos, B. A., et al. (2004). Cognitive-behavioral stress management improves stress-management skills and quality of life in men recovering from treatment of prostate carcinoma. Cancer 100, 192–200. doi: 10.1002/cncr.11894
Penedo, F. J., Traeger, L., Dahn, J., Molton, I., Gonzalez, J. S., Schneiderman, N., et al. (2007). Cognitive behavioral stress management intervention improves quality of life in Spanish monolingual hispanic men treated for localized prostate cancer: results of a randomized controlled trial. Int. J. Behav. Med. 14, 164–172. doi: 10.1007/BF03000188
Pitman, A., Suleman, S., Hyde, N., and Hodgkiss, A. (2018). Depression and anxiety in patients with cancer. BMJ 361, k1415. doi: 10.1136/bmj.k1415
Poghosyan, H., Sheldon, L. K., Leveille, S. G., and Cooley, M. E. (2013). Health-related quality of life after surgical treatment in patients with non-small cell lung cancer: a systematic review. Lung. Cancer 81, 11–26. doi: 10.1016/j.lungcan.2013.03.013
Stagl, J. M., Antoni, M. H., Lechner, S. C., Bouchard, L. C., Blomberg, B. B., Gluck, S., et al. (2015a). Randomized controlled trial of cognitive behavioral stress management in breast cancer: a brief report of effects on 5-year depressive symptoms. Health Psychol. 34, 176–180. doi: 10.1037/hea0000125
Stagl, J. M., Bouchard, L. C., Lechner, S. C., Blomberg, B. B., Gudenkauf, L. M., Jutagir, D. R., et al. (2015b). Long-term psychological benefits of cognitive-behavioral stress management for women with breast cancer: 11-year follow-up of a randomized controlled trial. Cancer 121, 1873–1881. doi: 10.1002/cncr.29076
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., et al. (2021). Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 71, 209–249. doi: 10.3322/caac.21660
Tang, M., Liu, X., Wu, Q., and Shi, Y. (2020). The effects of cognitive-behavioral stress management for breast cancer patients: a systematic review and meta-analysis of randomized controlled trials. Cancer Nurs. 43, 222–237. doi: 10.1097/NCC.0000000000000804
Vijayvergia, N., Shah, P. C., and Denlinger, C. S. (2015). Survivorship in Non-Small Cell Lung Cancer: Challenges Faced and Steps Forward. J. Natl. Compr. Canc. Netw. 13, 1151–1161. doi: 10.6004/jnccn.2015.0140
Wu, Z., Xiao, L., Wang, H., and Wang, G. (2021). Neurogenic hypothesis of positive psychology in stress-induced depression: Adult hippocampal neurogenesis, neuroinflammation, and stress resilience. Int. Immunopharmacol. 97, 107653. doi: 10.1016/j.intimp.2021.107653
Yu, D. (2021). Effect of cognitive behaviour therapy on the improvement of psychological stress. Work 69, 515–529. doi: 10.3233/WOR-213496
Keywords: non-small cell lung cancer, cognitive behavioral therapy, anxiety, depression, quality of life
Citation: Wang F, Zhang S, Song B and Han Y (2023) Anxiety, depression, and quality of life in postoperative non-small cell lung cancer patients under the intervention of cognitive-behavioral stress management. Front. Psychol. 14:1138070. doi: 10.3389/fpsyg.2023.1138070
Received: 05 January 2023; Accepted: 02 May 2023;
Published: 31 May 2023.
Edited by:
Antonio Macciò, Ospedale Oncologico Armando Businco, ItalyReviewed by:
Simin Jahani, Ahvaz Jundishapur University of Medical Sciences, IranCopyright © 2023 Wang, Zhang, Song and Han. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuxiang Han, aGFuX195dXhpYW5nQDEyNi5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.