- 1Department of Rehabilitation Medicine, Beijing Friendship Hospital, Capital Medical University, Beijing, China
- 2UCL Great Ormond Street Institute of Child Health, Faculty of Population Health Science, London, United Kingdom
This cross-sectional study examines the association between coffee and caffeine consumption and depressive symptoms in postpartum women. In total, 821 postpartum women who met the study’s inclusion criteria were interviewed. Data were extracted from the 2007–2018 National Health and Nutrition Examination Survey. Coffee consumption and 11 confounding variables were considered and analyzed as baseline data. Weighted logistic regression models were constructed by adjusting the variables, and the odds ratios of total coffee, caffeinated coffee, and decaffeinated coffee were assessed for their impact on depression status. In addition, subgroup analyses were conducted according to race, breastfeeding status, and postpartum period. The results show that generic coffee and caffeinated coffee intake have a potentially protective effect in postpartum women. Drinking more than three cups of caffeinated coffee may lower the risk of postpartum depression, particularly in the 1–2 year postpartum period and in non-breastfeeding women. The association between decaffeinated coffee consumption and postpartum depression remains unclear.
Introduction
Postpartum depression (PPD) is one of the most prevalent postpartum complications and affects approximately 8–26% of postpartum women every year (Shorey et al., 2018; Wang and Shan, 2022). Notably, a recent survey has demonstrated that the incidence rate of PPD has increased since the global COVID-19 pandemic (Alsabi et al., 2022; Perez et al., 2021). PPD can hit a woman between 3 and 18 months after giving birth, depending on hormonal changes in the mother’s body (Slomian et al., 2019). Moreover, recent studies have observed that 5% of postpartum women experienced continuously PPD symptoms for even three years after giving delivery (Kolomanska-Bogucka and Mazur-Bialy, 2019; Wan et al., 2021). Meanwhile, PPD is also known to have a long-lasting impact on the mother as well as her newborn and can influence the economic well-being and financial stability of mothers up to 15 years later (Rokicki et al., 2022). The economic burden of PPD is significant and estimated at approximately $14.2 billion annually in the United States (Luca et al., 2019). Therefore, there is an urgent need to investigate protective factors associated with PPD.
Coffee is one of the most popular beverages worldwide, and its primary component, caffeine, is recognized as the most widely used psychoactive substance. According to a survey conducted by the National Coffee Association (NCA), 62% of Americans consume coffee on a daily basis, and the average American coffee drinker consumes more than three cups per day. Generic coffee consumption in the United States has increased by 5% since 2015, prompting academics to conduct more studies on the effects of coffee on generic health (Shehaj and Morina, 2022). Coffee has been shown to lower the risk of cardiovascular disease (Surma et al., 2023), colorectal cancer (Deng et al., 2022), liver cirrhosis (Barre et al., 2022), and other illnesses, but it may also increase the risk of sleep problems (Riera-Sampol et al., 2022), anxiety disorders (Pan et al., 2022), and bone fractures (Webster et al., 2022).
The association between coffee consumption and depression remains debatable. Caffeine can reverse the dopaminergic system impairments observed in depression; for example, inhibiting the A1 adenosine receptor subunit may boost catecholamines and serotonin (5-HT) levels in the central nervous system (CNS) (Fredholm, 1995; Lopez-Cruz et al., 2018), besides, it is also worth noting that Caffeine increases the release of 5-HT in the limbic system and dopamine (DA) in the prefrontal cortex, producing effects similar to those of antidepressants (Acquas et al., 2002; Szopa et al., 2016). A longitudinal study of 50,776 women in the United States observed a negative correlation between coffee consumption and depressive behaviors after adjusting for age. A daily coffee intake of 2–3 cups and 4 cups was related to a 45 and 53% reduction in the risk of suicide, respectively; however, this effect was not observed in the decaffeinated population (Lucas et al., 2011). More recently, Grosso et al. (2016) conducted a meta-analysis that included 23 observational studies. Their results suggested that coffee consumption has a protective effect on the risk of depression, with a peak protective effect of 400 ml/day (Grosso et al., 2016). However, randomized clinical trials on coffee and depression produced contradictory results. In a prospective, randomized crossover trial by Quinlan et al. (2000), tea and coffee were found to exert similar mood and cognitive effects, which could not be explained by the caffeine content and rather the potential effects of other factors, such as flavonoids.
Multiple subpopulations, including college students (Yang et al., 2022), schoolchildren (Richards and Smith, 2015), and older adults (Guo et al., 2014), have been the focus of recent studies exploring the connection between coffee and depression. The data suggest that coffee has a favorable effect on adolescents but a detrimental effect on older adults in terms of depression. Although postpartum women are at an increased risk of depression, there are insufficient data on coffee and postpartum depression. Using the National Health and Nutrition Examination Survey (NHANES) database, we performed a large-scale, nationally representative study between 2007 and 2018 to learn more about the association between coffee consumption and PPD.
The remainder of the paper is structured as follows: Section “Materials and methods” presents the materials and methods used in the study. Section “Results” elaborates on the results of the study. Section “Discussion” presents the findings in the light of previous knowledge as well as the limitations and directions for future research.
Materials and methods
Data source and population
This analysis was based on NHANES data from 2007 to 2018. The NHANES is a nationally representative database comprising interviews, examinations, and laboratory data obtained from a multistage, stratified sample of adults and children in the United States, which may reflect the physical and mental well-being status of the total population. The data gathered by the NHANES are accessible to the public and are primarily used by public health researchers, policymakers, and physicians to estimate the prevalence of diseases and risk factors, and to promote the design of appropriate public health policies. The study was authorized by the National Center for Health Statistics Institutional Ethics Review Board, and all participants involved in NHANES study provided written consent.
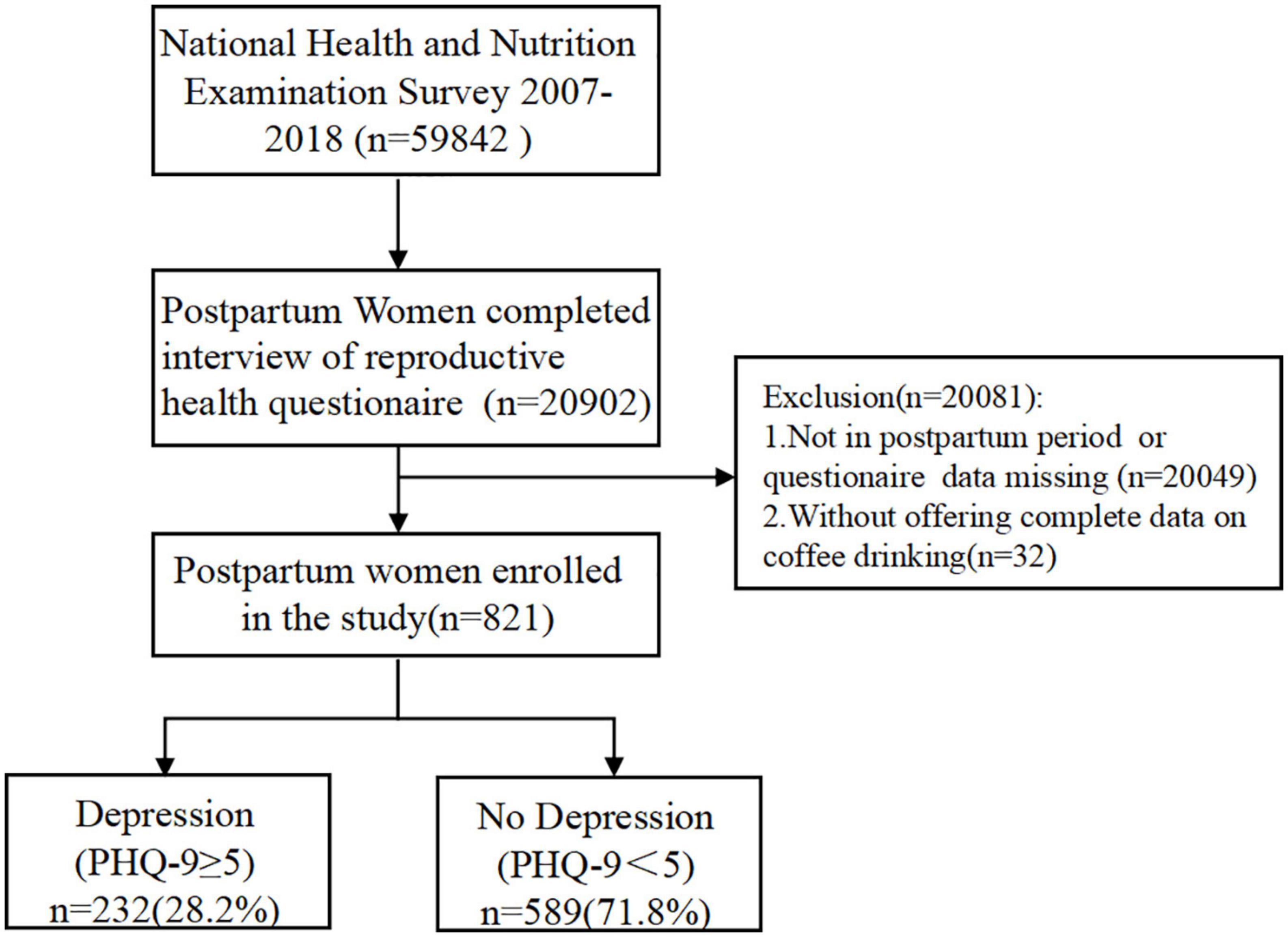
A total of 59,842 individuals from six successive NHANES cycles (2007–2008, 2009–2010, 2011–2012, 2013–2014, 2015–2016, and 2017–2018) were selected, of which 20,902 individuals had completed the reproductive health questionnaire. After excluding 20,049 women who were not in postpartum stage or had missing data, as well as two women who did not offer dietary information on their coffee consumption, 821 individuals were included in our investigation. Patient Health Questionnaire-9 items (PHQ-9) scores were simultaneously obtained to evaluate depression. Referring to recent evidence, postpartum depression can still occur up to 2 years postpartum (Kolomanska-Bogucka and Mazur-Bialy, 2019; Wan et al., 2021). Therefore, we included participants several months, 1 year and 2 years after delivery. According to Huyen et al. (2021), a cut-off value of >5 could predict 70% of cases of mild postpartum depression. We used a binarized interval score of 0–4 and more than 5 as the benchmarks for depression diagnosis. Ultimately, 232 cases (28.2%) were classified into the depression group, and 586 cases (71.8%) were classified into the non-depression group (Figure 1). According to the official sampling ratio and weight design, the 821 participants extracted from the NHANES represented 5.87 million noninstitutionalized residents of the United States.
Coffee and caffeine intake calculation
Two 24-h dietary recall interviews were used to gather data on NHANES participants’ coffee intake. The first dietary recall interview was conducted at a mobile examination center (MEC), while the second interview was conducted one week later via telephone. The NHANES data on coffee consumption included several types of coffee and coffee drinks. This survey detailedly collected the meals and beverages participants consumed in the past day (from midnight that day to midnight the day before) or in the previous 24 h, and synthesizes nutritive information of ingredients according to formula obtained from various sources, including the manufacturer or retailer, Internet or company catalogs. Hence, this method is widely recognized as an effective strategy for evaluating the coffee intake in population (Chen et al., 2022; Geng et al., 2022; Wang et al., 2022; Zheng et al., 2022). Caffeine intake was calculated based on the overall quantity of caffeinated meals and beverages consumed. This study examined coffee, decaffeinated coffee, sugar-sweetened coffee, and total caffeine consumption to analyze the correlation between coffee and its components, and depressive symptoms.
Covariables
Based on past research on the relationship between coffee and caffeine intake and depression, the following characteristics were added as covariables: age (year), body mass index (BMI, kg/m2), and postpartum time (within 1 year/1–2 years/More than 2 years). Race and socioeconomic factors that could influence incidences of PPD were also included: education level (less than high school, high school or equivalent, and above high school), family income-to-poverty ratio (PIR), covered by insurance (yes/no), and marital status (married/living with a partner, widowed/separated/divorced, and never married). In addition, smoking status (never, ever, and currently) and breastfeeding status (yes/no) were included as variables in this investigation.
Statistical analysis
The MEC sample weight was considered and allocated to each participant in accordance with the NCHS recommendations. Categorical data were presented as frequencies or percentages, while continuous variables were represented as mean ± standard deviation (SD). To quantify the differences between the groups, a weighted analysis of variance (ANOVA) or chi-square test (for categorical variables) was used. In accordance with the guidelines provided by the Reporting on Observational Studies in Strengthening Epidemiology, three weighted logistic regression models were used to calculate the odds ratios (ORs) and 95% confidence intervals (CIs) for PPD in each coffee drinking group. Model 1 was crude and untouched; Model 2 was adjusted for age and race/ethnicity; and Model 3 accounted for all the confounders. In addition, we performed subgroup analyses based on race, postpartum duration, and smoking status to further evaluate the association between coffee intake and PPD. R1 and StataSE 15.1 were used for all the statistical analyses (StataCorp LLC, College Station, TX, USA). Statistical significance was set at p < 0.05.
Results
Description of the study’s baseline characteristics
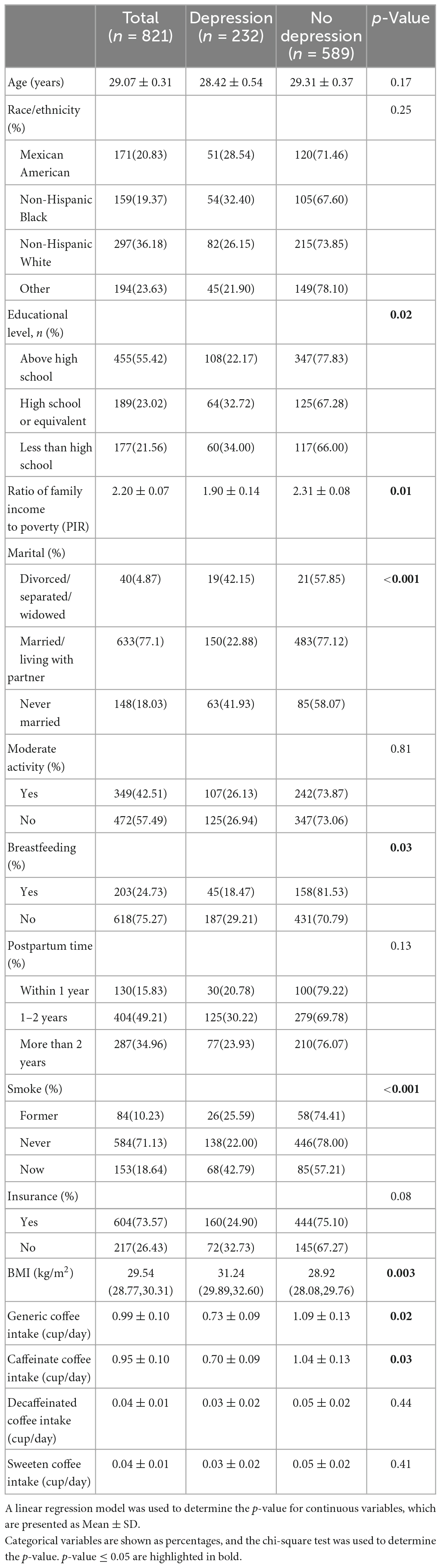
Table 1 shows the overall weighted characteristics of the study sample. Of the 821 postpartum women, 232 had depressive symptoms, and 589 had no obvious depressive symptoms. There was a significant difference in coffee intake between the depressed and non-depressed groups. The total intake of coffee in the depressed group was 0.73 ± 0.09 cups/day vs. 1.09 ± 0.13 cups/day in the non-depressed group (p = 0.02). A statistical difference was also observed for caffeinated coffee consumption: 0.70 ± 0.09 cups per day in the depressed group versus 1.04 ± 0.13 cups per day in the non-depressed group (p = 0.03). However, there was no statistically significant difference between the two groups in terms of decaffeinated coffee and sweetened coffee intake. In addition, there were statistical differences in education, household income, poverty rates, breastfeeding status, BMI, and smoking status, although differences in insurance coverage were marginal (p = 0.08). No statistically significant differences were observed in terms of race or ethnicity, moderate activity level, or postpartum period. The mean age of the depression group was 28.42 ± 8.62 years old, and the mean age of the non-depressive women was 34.42 ± 8.84 years old, with no statistical significance.
Association between coffee, caffeine intake, and risk of PPD
The association between generic coffee, decaffeinated coffee, and caffeinated coffee and the risk of PPD is shown in Table 2.

Table 2. Generic coffee, caffeinated coffee, and decaffeinated coffee intake (cup/day) and the risk of PPD.
Three weighted logistic regression models were established. Model 1 was established without adjustments (crude model). The results indicated that each increment of one cup in generic coffee and caffeinated coffee consumption was associated with an OR (95%) of 0.882 (0.786, 0.989) and 0.888 (0.794, 0.993), respectively, indicating a reduced risk of PPD of 11.2 and 11.1%, respectively. The trend in decaffeinated coffee consumption was not statistically significant. Model 2 was adjusted for age and race; however, the results were not statistically significant. Model 3 included all the relative covariates: age, BMI, race, educational level, ratio of family income to poverty, marital status, moderate activity status, breastfeeding status, postpartum time, smoking status, and insurance. The ORs (95% CIs) for per-cup increments of daily intake of generic coffee and caffeinated coffee were associated with a decrease in the risk of PPD of 11.1% (0.15–19.8%) and 11.3% (0.18–19.9%), respectively.
Stratified analysis
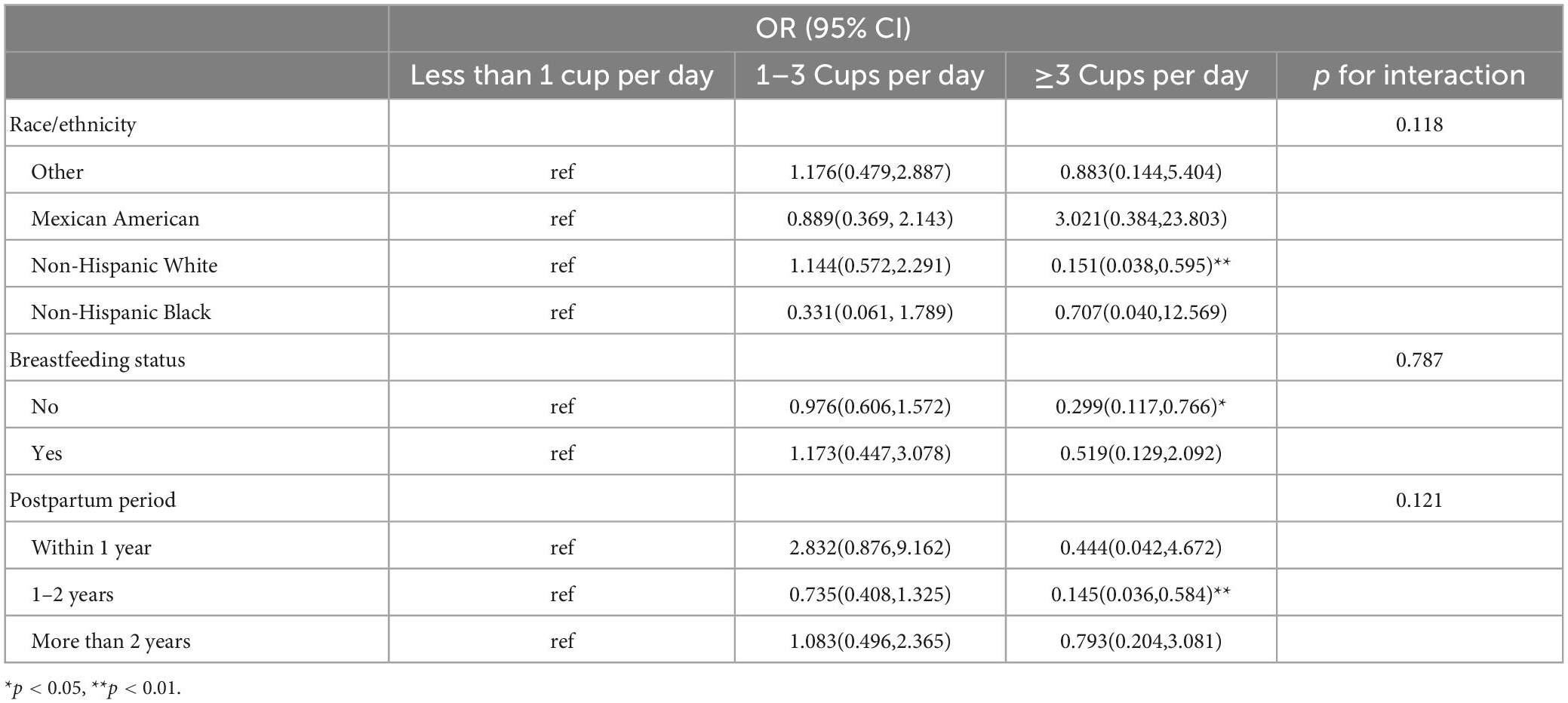
Based on the above analysis, we speculated that there may be a negative association between coffee consumption and PPD. To further explore and verify the factors that affect this association, we performed a stratified analysis by race, breastfeeding status, and postpartum period, and quantified coffee consumption at three levels. Table 3 presents the subgroup analyses of the results of the fully adjusted model (Model 3). Overall, the group that consumed more than three cups of caffeinated coffee daily had a declining trend in PPD risk compared with the group that consumed less than one cup per day. In non-Hispanic white people, the ORs (95% CIs) of PPD for the group drinking three cups of caffeinated coffee per day against the group consuming less than one cup per day was 0.151 (0.038, 0.595) with a p < 0.001 significance level, which indicated a reduced PPD risk of 84.9%. In terms of breastfeeding status, women who were not breastfeeding benefitted from drinking more than three cups of caffeinated coffee per day with ORs (95% CIs) of 0.299 (0.117, 0.766) compared with mothers who drank less than one cup per day, with a significant difference. Women who were breastfeeding also had a reduced risk of PPD when drinking more than three cups of caffeinated coffee per day, although no statistical significance was observed.
Previous research has indicated that the pathophysiology and pathogenesis of PPD may vary during various postpartum periods (Batt et al., 2020). In this study, the postpartum period was stratified as 1 year, 1–2 years, and more than 2 years. In the group of 1–2 years, the ORs (95% CIs) of PPD in the population drinking three cups of caffeinated coffee per day versus the group consuming less than one cup per day were 0.145 (0.036, 0.584) with a p < 0.001 significance level. Although there was a negative association between drinking more than three cups of caffeinated coffee and PPD in other time period subgroups (within 1 year or more than 2 years), no statistical difference was found. In addition, the interaction effect was evaluated to clarify the potential association between the stratifying variables and coffee consumption, but no statistically meaningful interaction effect was found.
Discussion
The popularity of coffee and coffee beverages is increasing worldwide, and their effects on human physical and mental health have been extensively studied. Although numerous studies have demonstrated a potential negative association between coffee consumption and depression (Grosso et al., 2016; Navarro et al., 2018; Wang et al., 2016), evidence on postpartum women is sparse. PPD is often unrecognized and left untreated and it can have a profound impact on children’s parenting and development (Goodman, 2004; Psychosocial Paediatrics Committee, 2004; Ko et al., 2017). Therefore, we conducted this exhaustive, representative, cross-sectional study using the NHANES database from 2007 to 2018 and analyzed a representative sample of 821 postpartum women.
We found a negative independent association between coffee intake and postpartum depression. The results of the cross-study indicated that this negative correlation is statistically significant in generic and caffeinated coffee consumption, but not in decaffeinated coffee consumption. This suggests that the protective effect of coffee against PPD is most likely mediated by caffeine. Correspondingly, this beneficial association was found to be significant in multiple subgroups, including white individuals and women who were not breastfeeding. We concluded that women who are 1–2 years postpartum are more likely to benefit from this protective effect of coffee.
The main finding of this study is consistent with the conclusions of previous studies (Lucas et al., 2011; Lahortiga-Ramos et al., 2018; Kimura et al., 2020; Ma et al., 2022; Wang et al., 2023). In a 10-year follow-up study that included 14,413 male and female participants with a mean age of 36 years, the hazard ratio of depression in participants who consumed ≥ 4 cups of coffee daily was 0.37 compared with participants who drank less than one cup of coffee daily (Navarro et al., 2019). For older women, Lucas et al. (2011) established a prospective United States cohort of 50,739 women with a mean age of 63. After a 10-year follow-up, they found that consuming two to three cups or ≥4 cups per day could lower the risk of depression by approximately 10 and 15%, respectively. A similar effect was also observed in older Asian women (Kimura et al., 2020) with a more marked impact. In a recent meta-analysis of 11 publications and 330,677 individuals, a linear association between coffee consumption and depression was observed, with a decline of 8% in depression for each increment of one cup of coffee (Wang et al., 2016). Current studies have also provided some insights into the molecular interactions between caffeine and human neuro-activities (Fang et al., 2021).
Despite extensive evidence supporting the antidepressant benefits of coffee and caffeine, evidence involving postpartum women is still lacking. Possible reasons may include ethical and legal issues related to postpartum mental disorder screening (Gilbert et al., 2017; Vemuri, 2012), sparse demographic distribution, and low self-reporting rates (Simmons et al., 2007). Moreover, evidence recommending caffeine consumption guidelines for postpartum women is scarce, of poor quality, and equivocal (McCreedy et al., 2018). To the best of our knowledge, this is the first study to investigate the associations between coffee consumption, caffeine intake, and depression in postpartum women. The first benefit of our study is that we used 821 samples from the NHANES between 2007 and 2018, which is representative of 5.86 million United States residents, and offered a strong and trustworthy result with minimized sample bias. Second, we chose covariables based on the characteristics of the postpartum population and adjusted them based on outcome- and exposure-related factors, which strengthened the generalizability of the results. The findings of this study may therefore provide practical and instructional evidence for future research on the prevention of postpartum depression.
This study has several limitations that need to be clarified. First, this was a cross-sectional study, and the data on coffee drinking were obtained from 24-h dietary recall in MEC, which cannot reflect the dynamic changes in diet before and after pregnancy. Second, this study was unable to incorporate individual’s prepartum mental disorder and family history as covariables due to the inaccessibility of complete medical history. Last, although the results indicate that consuming three or more cups of caffeinated coffee per day can reduce risk of PPD, it is notable that no statistically significant results were found in the currently breastfeeding population. Thus, the results of this study should be interpreted with caution and should not be regarded as a recommendation for increased coffee consumption in whole-population during lactation.
As a result of the COVID-19 pandemic, the global incidence of PPD has climbed from 13 to 19% to 23 to 27% (Nisar et al., 2020). This dismal trend prompts more focus on the prevention and treatment of PPD. In addition to genetic and social variables, lifestyle factors, such as diverse diets that may contain moderate psychoactive substances, may have an impact on PPD (Gow et al., 2022). The discovery of these associations and the recommendation of a specific diet for postpartum populations will contribute to the reduction of PPD risk. Consequently, based on the findings of this study, we recommend that in future questionnaire surveys and cohort studies of postpartum populations, appropriate consideration should be given to enhancing the screening of dietary characteristics and evaluating their impact on the pathogenesis and treatment of PPD.
In conclusion, the results suggest that generic and caffeinated coffee consumption could have protective effects in PPD, and that consuming more than three cups of caffeinated coffee could lower risk of PPD. The subgroup analyses indicate that this tendency is more prominent in white people, women 1–2 years postpartum, and non-breastfeeding groups with statistical significance. A protective effect was not observed in decaffeinated coffee.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.cdc.gov/nchs/nhanes/index.htm.
Ethics statement
The studies involving human participants were reviewed and approved by NCHS Research Ethics Review Board. The patients/participants provided their written informed consent to participate in this study.
Author contributions
YW collected the data and drafted the manuscript. ZW revised the manuscript. YX designed the study. BZ and PG analyzed the data. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by Beijing Hospital Authority Youth Program (grant number: QML20200109).
Acknowledgments
We thank Zhang Jing for his contribution on the NHANES database and nhanesR package, which made it easier for us to explore NHANES database.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
Acquas, E., Tanda, G., and Di Chiara, G. (2002). Differential effects of caffeine on dopamine and acetylcholine transmission in brain areas of drug-naive and caffeine-pretreated rats. Neuropsychopharmacology 27, 182–193. doi: 10.1016/S0893-133X(02)00290-7
Alsabi, R., Zaimi, A., Sivalingam, T., Ishak, N., Alimuddin, A., Dasrilsyah, R., et al. (2022). Improving knowledge, attitudes and beliefs: A cross-sectional study of postpartum depression awareness among social support networks during COVID-19 pandemic in Malaysia. BMC Womens Health 22:221. doi: 10.1186/s12905-022-01795-x
Barre, T., Fontaine, H., Ramier, C., Di Beo, V., Pol, S., Carrieri, P., et al. (2022). Elevated coffee consumption is associated with a lower risk of elevated liver fibrosis biomarkers in patients treated for chronic hepatitis B (ANRS CO22 Hepather cohort). Clin. Nutr. 41, 610–619. doi: 10.1016/j.clnu.2022.01.016
Batt, M., Duffy, K., Novick, A., Metcalf, C., and Epperson, C. (2020). Is postpartum depression different from depression occurring outside of the perinatal period? A review of the evidence. Focus (Am Psychiatr Publ) 18, 106–119. doi: 10.1176/appi.focus.20190045
Chen, S., Li, J., Gao, M., Li, D., Shen, R., Lyu, L., et al. (2022). Association of caffeine intake with all-cause and cardiovascular mortality in elderly patients with hypertension. Front. Nutr. 9:1023345. doi: 10.3389/fnut.2022.1023345
Deng, Y., Huang, J., and Wong, M. (2022). Associations of alcohol and coffee with colorectal cancer risk in East Asian populations: A Mendelian randomization study. Eur. J. Nutr. doi: 10.1007/s00394-022-03002-x [Epub ahead of print].
Fang, C., Hayashi, S., Du, X., Cai, X., Deng, B., Zheng, H., et al. (2021). Caffeine protects against stress-induced murine depression through activation of PPARgammaC1alpha-mediated restoration of the kynurenine pathway in the skeletal muscle. Sci. Rep. 11:7287. doi: 10.1038/s41598-021-86659-4
Fredholm, B. (1995). Astra award lecture. Adenosine, adenosine receptors and the actions of caffeine. Pharmacol. Toxicol. 76, 93–101. doi: 10.1111/j.1600-0773.1995.tb00111.x
Geng, J., Qiu, Y., Kang, Z., Li, Y., Li, J., Liao, R., et al. (2022). The association between caffeine intake and risk of kidney stones: A population-based study. Front. Nutr. 9:935820. doi: 10.3389/fnut.2022.935820
Gilbert, A. L., Balio, C., and Bauer, N. S. (2017). Making the legal and ethical case for universal screening for postpartum mood and anxiety disorders in pediatric primary care. Curr. Probl. Pediatr. Adolesc. Health Care 47, 267–277. doi: 10.1016/j.cppeds.2017.08.001
Goodman, J. H. (2004). Paternal postpartum depression, its relationship to maternal postpartum depression, and implications for family health. J. Adv. Nurs. 45, 26–35. doi: 10.1046/j.1365-2648.2003.02857.x
Gow, M., Rossiter, C., Roberts, L., Henderson, M., Yang, L., Roche, J., et al. (2022). COVID-19, lifestyle behaviors and mental health: A mixed methods study of women 6 months following a hypertensive pregnancy. Front. Public Health 10:1000371. doi: 10.3389/fpubh.2022.1000371
Grosso, G., Micek, A., Castellano, S., Pajak, A., and Galvano, F. (2016). Coffee, tea, caffeine and risk of depression: A systematic review and dose-response meta-analysis of observational studies. Mol. Nutr. Food Res. 60, 223–234. doi: 10.1002/mnfr.201500620
Guo, X., Park, Y., Freedman, N. D., Sinha, R., Hollenbeck, A., Blair, A., et al. (2014). Sweetened beverages, coffee, and tea and depression risk among older US adults. PLoS One 9:e94715. doi: 10.1371/journal.pone.0094715
Huyen, D. P., Thang, V. V., Bao-Yen, L. T., Nguyen, L., Valdebenito, S., Eisner, M., et al. (2021). 728Comparative performance of WHO-5, PHQ-9 and PSS Scale for screening antenatal depression and suicide risk. Int. J. Epidemiol. 50(Suppl. 1):1.
Kimura, Y., Suga, H., Kobayashi, S., and Sasaki, S. (2020). Three-generation study of women on diets and health study group. Intake of coffee associated with decreased depressive symptoms among elderly japanese women: A multi-center cross-sectional study. J. Epidemiol. 30, 338–344. doi: 10.2188/jea.JE20190010
Ko, J., Rockhill, K., Tong, V., Morrow, B., and Farr, S. (2017). Trends in postpartum depressive symptoms – 27 states, 2004, 2008, and 2012. MMWR Morb. Mortal. Wkly. Rep. 66, 153–158. doi: 10.15585/mmwr.mm6606a1
Kolomanska-Bogucka, D., and Mazur-Bialy, A. I. (2019). Physical activity and the occurrence of postnatal depression-a systematic review. Medicina (Kaunas) 55:560. doi: 10.3390/medicina55090560
Lahortiga-Ramos, F., Unzueta, C., Zazpe, I., Santiago, S., Molero, P., Sánchez-Villegas, A., et al. (2018). Self-perceived level of competitiveness, tension and dependency and depression risk in the SUN cohort. BMC Psychiatry 18:241. doi: 10.1186/s12888-018-1804-x
Lopez-Cruz, L., Salamone, J. D., and Correa, M. (2018). Caffeine and selective adenosine receptor antagonists as new therapeutic tools for the motivational symptoms of depression. Front. Pharmacol. 9:526. doi: 10.3389/fphar.2018.00526
Luca, D. L., Garlow, N., Staatz, C., Margiotta, C., and Zivin, K. (2019). Societal costs of untreated perinatal mood and anxiety disorders in the united states. Mathematica policy research reports. Cambridge, MA: Mathematica Policy Research.
Lucas, M., Mirzaei, F., Pan, A., Okereke, O., Willett, W., O’Reilly, É, et al. (2011). Coffee, caffeine, and risk of depression among women. Arch. Intern. Med. 171, 1571–1578. doi: 10.1001/archinternmed.2011.393
Ma, Y., Li, R., Zhan, W., Huang, X., Zhang, L., and Liu, Z. (2022). The joint association between multiple dietary patterns and depressive symptoms in adults aged 55 and over in northern china. Front. Nutr. 9:849384. doi: 10.3389/fnut.2022.849384
McCreedy, A., Bird, S., Brown, L. J., Shaw-Stewart, J., and Chen, Y. (2018). Effects of maternal caffeine consumption on the breastfed child: A systematic review. Swiss Med. Wkly. 148:w14665. doi: 10.4414/smw.2018.14665
Navarro, A., Abasheva, D., Martínez-González, M., Ruiz-Estigarribia, L., Martín-Calvo, N., Sánchez-Villegas, A., et al. (2018). Coffee consumption and the risk of depression in a middle-aged cohort: The SUN project. Nutrients 10:1333. doi: 10.3390/nu10091333
Navarro, A., Martinez-Gonzalez, M., Gea, A., Ramallal, R., Ruiz-Canela, M., and Toledo, E. (2019). Coffee consumption and risk of hypertension in the SUN Project. Clin. Nutr. 38, 389–397. doi: 10.1016/j.clnu.2017.12.009
Nisar, A., Yin, J., Waqas, A., Bai, X., Wang, D., Rahman, A., et al. (2020). Prevalence of perinatal depression and its determinants in Mainland China: A systematic review and meta-analysis. J. Affect. Disord. 277, 1022–1037. doi: 10.1016/j.jad.2020.07.046
Pan, C., Ye, J., Wen, Y., Chu, X., Jia, Y., Cheng, B., et al. (2022). The associations between sleep behaviors, lifestyle factors, genetic risk and mental disorders: A cohort study of 402 290 UK Biobank participants. Psychiatry Res. 311:114488. doi: 10.1016/j.psychres.2022.114488
Perez, A., Gobel, A., Stuhrmann, L. Y., Schepanski, S., Singer, D., Bindt, C., et al. (2021). Born under COVID-19 pandemic conditions: infant regulatory problems and maternal mental health at 7 months postpartum. Front. Psychol. 12:805543. doi: 10.3389/fpsyg.2021.805543
Psychosocial Paediatrics Committee (2004). Maternal depression and child development. Paediatr. Child Health 9, 575–598. doi: 10.1093/pch/9.8.575
Quinlan, P. T., Lane, J., Moore, K. L., Aspen, J., Rycroft, J., and O’Brien, D. (2000). The acute physiological and mood effects of tea and coffee: The role of caffeine level. Pharmacol. Biochem. Behav. 66, 19–28. doi: 10.1016/s0091-3057(00)00192-1
Richards, G., and Smith, A. (2015). Caffeine consumption and self-assessed stress, anxiety, and depression in secondary school children. J. Psychopharmacol. 29, 1236–1247. doi: 10.1177/0269881115612404
Riera-Sampol, A., Rodas, L., Martínez, S., Moir, H. J., and Tauler, P. (2022). Caffeine intake among undergraduate students: Sex differences, sources, motivations, and associations with smoking status and self-reported sleep quality. Nutrients 14:1661. doi: 10.3390/nu14081661
Rokicki, S., McGovern, M., Von Jaglinsky, A., and Reichman, N. (2022). Depression in the postpartum year and life course economic trajectories. Am. J. Prev. Med. 62, 165–173. doi: 10.1016/j.amepre.2021.08.011
Shehaj, A., and Morina, A. (2022). Evaluation of some physical, chemical and sensorial parameter of turkish coffee trade in the Albanian market. J. Biol. Stud. 5, 396–404.
Shorey, S., Chee, C., Ng, E. D., Chan, Y., Tam, W., and Chong, Y. (2018). Prevalence and incidence of postpartum depression among healthy mothers: A systematic review and meta-analysis. J. Psychiatr. Res. 104, 235–248. doi: 10.1016/j.jpsychires.2018.08.001
Simmons, L. A., Huddleston-Casas, C., and Berry, A. (2007). Low-income rural women and depression: Factors associated with self-reporting. Am. J. Health Behav. 31, 657–666. doi: 10.5555/ajhb.2007.31.6.657
Slomian, J., Honvo, G., Emonts, P., Reginster, J., and Bruyère, O. (2019). Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Womens Health (Lond) 15, 1745978572. doi: 10.1177/1745506519844044
Surma, S., Sahebkar, A., and Banach, M. (2023). Coffee or tea: Anti-inflammatory properties in the context of atherosclerotic cardiovascular disease prevention. Pharmacol. Res. 187:106596. doi: 10.1016/j.phrs.2022.106596
Szopa, A., Poleszak, E., Wyska, E., Serefko, A., Wośko, S., Wlaź, A., et al. (2016). Caffeine enhances the antidepressant-like activity of common antidepressant drugs in the forced swim test in mice. Naunyn Schmiedebergs Arch. Pharmacol. 389, 211–221. doi: 10.1007/s00210-015-1189-z
Vemuri, M. (2012). Ethics commentary: Ethical considerations in treating women with mental illness during pregnancy. Focus J. Lifelong Learn. Psychiatry 10, 36–40.
Wan, M. R., Salarzadeh, J. H., and Samsudin, N. (2021). Postpartum depression symptoms in survey-based research: A structural equation analysis. BMC Public Health 21:27. doi: 10.1186/s12889-020-09999-2
Wang, H., Jin, M., Xie, M., Yang, Y., Xue, F., Li, W., et al. (2023). Protective role of antioxidant supplementation for depression and anxiety: A meta-analysis of randomized clinical trials. J. Affect. Disord. 323, 264–279. doi: 10.1016/j.jad.2022.11.072
Wang, L., Shen, X., Wu, Y., and Zhang, D. (2016). Coffee and caffeine consumption and depression: A meta-analysis of observational studies. Aust. N. Z. J. Psychiatry 50, 228–242. doi: 10.1177/0004867415603131
Wang, R., and Shan, Y. (2022). Hot spots and frontiers of postpartum depression research in the past 5 years: A bibliometric analysis. Front. Psychol. 13:901668. doi: 10.3389/fpsyg.2022.901668
Wang, S., Han, Y., Zhao, H., Han, X., Yin, Y., Wu, J., et al. (2022). Association between coffee consumption, caffeine intake, and metabolic syndrome severity in patients with self-reported rheumatoid arthritis: National health and nutrition examination survey 2003-2018. Nutrients 15:107. doi: 10.3390/nu15010107
Webster, J., Greenwood, D. C., and Cade, J. E. (2022). Foods, nutrients and hip fracture risk: A prospective study of middle-aged women. Clin. Nutr. 41, 2825–2832. doi: 10.1016/j.clnu.2022.11.008
Yang, B. W., Zou, P., Chen, Q., Sun, L., Ling, X., Yang, H., et al. (2022). Lifestyle-related risk factors correlated with mental health problems: A longitudinal observational study among 686 male college students in Chongqing, China. Front Public Health 10:1040410. doi: 10.3389/fpubh.2022.1040410
Keywords: depression, coffee, caffeine, postpartum population, postpartum rehabilitation
Citation: Wang Y, Wang Z, Gui P, Zhang B and Xie Y (2023) Coffee and caffeine intake and depression in postpartum women: A cross-sectional study from the National Health and Nutrition Examination Survey 2007–2018. Front. Psychol. 14:1134522. doi: 10.3389/fpsyg.2023.1134522
Received: 30 December 2022; Accepted: 06 February 2023;
Published: 17 February 2023.
Edited by:
Sayyed Mohsen Fatemi, York University, CanadaReviewed by:
Kingston Pal Thamburaj, Sultan Idris University of Education, MalaysiaChutima Roomruangwong, Chulalongkorn University, Thailand
Copyright © 2023 Wang, Wang, Gui, Zhang and Xie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ying Xie,  eGlleWluZ0BjY211LmVkdS5jbg==
eGlleWluZ0BjY211LmVkdS5jbg==
 Yinuo Wang
Yinuo Wang Zhuangfu Wang2
Zhuangfu Wang2