
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 05 June 2023
Sec. Health Psychology
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1132154
This article is part of the Research TopicPost COVID-19: Analysing and Addressing the Challenges Faced by Patients Following Intensive Care Treatment for COVID-19View all 16 articles
A correction has been applied to this article in:
Corrigendum: Construct validity of the General Health Questionnaire (GHQ-12) in patients with COVID-19 and its demographic and medical correlates
 Mojtaba Habibi Asgarabad1,2,3,4,5*†
Mojtaba Habibi Asgarabad1,2,3,4,5*† Farnaz Etesam6,7†
Farnaz Etesam6,7† Pardis Salehi Yegaei1†
Pardis Salehi Yegaei1† Zahra Vahabi6,8*†
Zahra Vahabi6,8*† Niusha Akbari Saneh9
Niusha Akbari Saneh9 Fatemeh Fathi10
Fatemeh Fathi10 Fatemeh Ghosi11
Fatemeh Ghosi11 Nora Wiium12
Nora Wiium12Introduction: The present cross sectional study aimed to evaluate the construct and criterion validity, reliability, and gender and age differences of the 12-item General Health Questionnaire (GHQ-12) among hospitalized patients with COVID-19 in 2020. The criterion validity was assessed via its link with perceived stress, sleep quality, daily life activities, and demographic and medical characteristics.
Methods: A total of 328 COVID-19 patients (55.8% men; Mage = 50.49, SD = 14.96) completed the GHQ-12, the Perceived Stress Scale (PSS), the Pittsburgh Sleep Quality Index (PSQI), the Activities of Daily Life (ADL)-Katz Scale, and the Lawton Instrumental Activities of Daily Living Scale (IADL).
Results: Among 13 factorial models, the three-factor model (successful coping, self-esteem, and stress) was shown to have the best fit. GHQ-12 was positively associated with PSQI, PSS, Hyperlipidemia, psychiatry disorders, hospitalization duration, the change in sleep time, and use of sleeping pills, and negatively correlated with educational level, and the number of family members. The GHQ-12 also had a negative correlation with ADL and IADL in over 60 years of age group. Females scored higher on total GHQ-12 scores, compared to males. Finally, the hospitalization duration was longer for patients over 60 (mean = 8.8 days, SD = 5.9) than patients under 60 (mean = 6.35 days, SD = 5.87).
Discussion: Overall, the findings provided evidence that mental distress in patients with COVID-19 is correlated with high perceived stress, low sleep quality, low ADL and IADL, and a range of demographic features and medical conditions. Designing psychological interventions for these patients that target the aforementioned correlates of mental distress is warranted.
New measures of the COVID-19 pandemic (e.g., self-isolation and quarantine) have led to an increase in mental distress, such as anxiety, insomnia, and suicidal attempt (WHO, 2020; Santomauro et al., 2021). Review studies after the COVID-19 pandemic showed high prevalence rate of anxiety (27–41.3%) and depression (27 to 34.1%) in Eastern Europe (Zhang et al., 2022), Southeast Asia (Pappa et al., 2022) and South Asia (Hossain et al., 2021).
To capture changes in mental health in both general and clinical populations, the self-administered General Health Questionnaire (GHQ; Goldberg, 1988) was developed. The 12-item short-form of GHQ (GHQ-12; Goldberg et al., 1997) was derived from the original 60-item questionnaire for fast administration in busy clinical settings. This questionnaire screens those with common psychological problems, such as poor self-esteem, stress, and sleep loss (del Pilar Sánchez-López and Dresch, 2008).
Although GHQ-12 was originally designed as a unidimensional measure (Goldberg, 1972), several exploratory factor analyses indicated that a two-factor (Zhong et al., 2021) or three-factor model (del Pilar Sánchez-López and Dresch, 2008) is the most common model (full information of these factorial models and their reliabilities are presented in Table 1). However, considering the study of Liang et al. (2016) for instance, they failed to find the best fitting model among ten existing factorial models, highlighting that there is a need for further research on the factor structure of GHQ-12.
Mental health is reciprocally linked to sleep quality, specifically in patients with COVID-19 who are commonly susceptible to sleep disturbances (Deng et al., 2021; Marvaldi et al., 2021). Perceived stress, referring to the extent to which a person perceives their daily life situations as stressful, was also found to be positively associated with GHQ-12 in a large cross-national sample of COVID-19 patients (Bonsaksen et al., 2022). Patients infected with COVID-19 experienced the burden of job loss (Crayne, 2020), death anxiety (Korkut, 2022), and may react with heightened stress (Bonsaksen et al., 2022).
Coronavirus may severely impair the subsequent physical functioning in some patients, especially the elderly (Carfì et al., 2020; Halpin et al., 2020). The Activities of daily living (ADL) and the Instrumental Activities of Daily Living (IADL; Katz et al., 1970; Lawton, 2000) are basic skills necessary for independently taking care of oneself (Edemekong et al., 2017) and environmental adaptation (Roehrig et al., 2007). Although few in number, some studies have shown the link of mental health to ADL and IADL scores (de Castroe Costa et al., 2008).
Due to the negative effect of COVID-19 on several aspects of people’s lives (Santomauro et al., 2021), research should document the association of mental health status in COVID-19 patients with demographics and medical features. Previous studies have suggested the positive link of mental health status with medical features, such as change in sleep time before and after COVID-19 and use of sleeping pills (Becker et al., 2018), hospitalization duration (Liao et al., 2020), psychiatry disorders (Kaufman et al., 2020), hyperlipidemia (HLP; Chang et al., 2021), diabetes (Moradian et al., 2021), cardiovascular disease (CVD; de Paiva Teixeira et al., 2020), substance use history (Czeisler et al., 2020), as well as demographics characteristics, namely, educational level (Dalgard et al., 2007), unemployment (Achdut and Refaeli, 2020), and the number of family members (Hendriksen et al., 2021). COVID-19 pandemic was shown to result in greater mental distress in women (Giorgi et al., 2014; Bucciarelli et al., 2021). As an example, in a study on large data of 49,156 participants, Proto and Quintana-Domeque (2021) found that after the COVID-19 pandemic, women manifested higher elevation in GHQ-12 scores (higher psychological distress) than men. Aging is believed to be associated with decrease in mental distress (Hoeymans et al., 2004), while COVID-19 pandemic have led to greater mental distress in younger patients (Bruine de Bruin, 2021).
Iran is among the worst-hit countries by Coronavirus, with heavy death tolls (more than 19,000 deaths until August 2020; Shahriarirad et al., 2021). Challenging factors, namely, the shortage of hygiene and medical supplies and equipment (i.e., masks and disinfectants), economic constraints (Zandifar and Badrfam, 2020), and the incapacity of government to formulate and enforce effectual social distancing and lockdown measures have led to the mental distress in the Iranian general population (Moghanibashi-Mansourieh, 2020; Zandifar and Badrfam, 2020; Shahriarirad et al., 2021). The Iranian population has been no exception to the global trend of increased mental issues. In a group of 5,328 individuals from the general population of Iran, the prevalence rates of anxiety, depression, and comorbid depression-anxiety were determined to be 30.1, 33.4, and 22.1%, respectively (Nakhostin-Ansari et al., 2020). Moreover, in another recent study by Maroufizadeh et al. (2022), the prevalence of mild-to-severe anxiety and depression in Iranian medical students was found to be 38.1 and 27.6%, showing a significant impact on sleep patterns.
In Iran, two studies have assessed the psychometric properties of GHQ-12. In a study on emerging adults, Montazeri et al. (2003) findings confirmed the two-factor model, comprising “depression” and “social dysfunction.” Their study showed the negative association of GHQ-12 with global quality of life, supporting its satisfactory convergent validity. Similarly, the results of Najarkolaei et al. (2014) study supported a two-factor model including “distress” and “social dysfunction” in freshmen university students. Nevertheless, participants of these two studies had limited age range (18–26 years of age) and were recruited from university students, which prevent their results from being generalized to the general or clinical Iranian population.
The present study was first-of-its-kind that aimed to examine the psychometric properties of the GHQ-12 in Iranian patients with COVID-19. In specific, we aimed to examine: (1) the factor structure by conducting Confirmatory Factor Analysis (CFA) based on 13 empirically-derived factorial models, (2) the internal consistency, (3) the criterion validity through the relationship of GHQ with perceived stress, sleep quality, ADL/IADL, and demographic and medical variables, and (4) the comparison of the average GHQ-12 scores among age and gender groups (if any). We hypothesized that higher GHQ-12 score—that reflects lower mental health—has a positive relationship with: (1) poor sleep quality, (2) higher perceived stress, and (3) lower level of ADL/IADL functions.
Participants comprised a total of 328 patients with COVID-19 (55.8% men), aged 21 to 92 (Meanage (SD) = 50.49 (14.96); 73.6% 60 years old or younger). As for educational level, 19.8% of participants were illiterate, 22.9% had primary education, 16.5% had secondary education, 23.5% had diploma level, and 17.3% had higher education. Their job status included 15.3% employee, 6.7% skill-worker, 20.7% self-employed, 39.6% unemployed, and 13.1% retired. Most patients (88.6%) were living with their spouse and/or their children, while 10.5% were living alone. A majority of 86.6% had no history of smoking, while 10.1 and 2.4% reported smoking in the past and at the present time. In addition, 93.9 and 96.6% reported no history of alcohol and drug use, respectively. Among participants, 4.6% reported using sleeping pills—mostly Alprazolam, Chlordiazepoxide, and Asentra. Patients under and over 60 reported underlying diseases, including Diabetes (13 and 44.6%), High Blood Pressure (HTN; 15.2 and 28.9%), HLP (11.7 and 31.3%), psychiatry disorders (4.8 and 3.6%), immune deficiency disease (IDD; 1.3 and 4.8%), and Cardiovascular disease (9.1 and 28.9%), each. Finally, the mean of hospitalization duration was 6.35 days (SD = 5.87) for patients under 60 and 8.8 days (SD = 5.9) for patients over 60.
The self-report GHQ-12 was developed to screen global mental state (Goldberg et al., 1997). Among two common scoring methods of the bi-modal (0–0–1-1) and Likert scoring (0–1–2-3) types, the Likert method is preferable since it measures the symptom severity on a continuum (Hystad and Johnsen, 2020). In this study, the scoring based on the 4-point Likert-scale (0–1–2-3) was used, in which: 0 = “not at all,” 1 = “no more than usual,” 2 = “rather more than usual,” and 3 = “much more than usual,” where a higher score indicated lower mental health (Goldberg et al., 1997).
This 19-item self-administered tool (Buysse et al., 1989) was designed for brief assessment of seven components: (1) subjective sleep quality (e.g., “how would you rate your sleep quality overall?”), (2) sleep latency (e.g., “cannot get to sleep within 30 min”), (3) sleep duration (e.g., “how many hours of actual sleep do you get at night?”), (4) sleep efficiency (e.g., “when have you usually gone to bed?”), (5) sleep disturbances (e.g., “wake up in the middle of the night or early morning”), (6) use of sleeping medication (e.g., “how often have you taken medicine to help you sleep?”), and (7) daytime dysfunction (e.g., “how often have you had trouble staying awake while driving,…”). Each component was weighted on a Likert scale from 0 to 3, with higher scores indicating poorer sleep quality. Cronbach’s alpha in the current study was.77 for the total score. The Persian version of PSQI that showed adequate psychometric properties (Farrahi Moghaddam et al., 2012) was used in the current study.
PSS is a 10-item unidimensional scale (Cohen et al., 1983) that measures how much patients appraise the situations in their life as stressful during the preceding month. Items were coded based on a 5-point Likert-type scale: 0 (never), 1 (almost never), 2 (once in a while), 3 (often), and 4 (very often). Higher scores indicated higher perceived stress (e.g., “unable to control the important things in your life”). Cronbach’s α for the Persian version of PSS was.84 for the total score (Maroufizadeh et al., 2018), while an alpha value of.68 was obtained in our study.
The 6-item ADL-Katz Scale (Katz et al., 1970) assessed the ability of bathing, transferring, dressing and grooming, walking, toileting, and feeding in people over 60 years of age. The Lawton Instrumental Activities of Daily Living Scale (Lawton, 2000) measured instrumental functioning, namely, using the phone, doing housework, doing laundry, managing transportation, shopping, cooking, managing medications, and managing finances. Items for both ADL and IADL were scored based on 0 (no) and 1 (yes). Cronbach’s alphas for the Persian versions of ADL and IADL were 0.80 (Sharifi et al., 2018) and between 0.72 and 0.76 (Mehraban et al., 2014), respectively. In this study, alphas were 0.66 and 0.82 for ADL and IADL, respectively.
In order to evaluate the patients’ demographics and medical characteristics, a questionnaire constructed by researchers was used. The medical features included: (a) the history of underlying diseases (Diabetes, HTN, HLP, Myocardial Infarction (MI), Cerebrovascular Accident (CVA), Pulmonary Disease (PD), Kidney failure, Psychiatry disorders, Obesity, IDD, and CVD) (yes/no), (b) cigarette, alcohol, and drug history (yes/no), (c) hospitalization duration (days), (d) use of downer or sleeping pills (yes/no), and (e) the change in sleep time before and after COVID-19 (hours). The demographic characteristics included: (a) gender (male/female), (b) age (years), (c) job status (employed/unemployed), (d) educational level (illiterate, primary education, secondary education, diploma level, and higher education), and (e) the number of family members.
The current cross-sectional study was carried out on patients hospitalized due to Coronavirus infection at the Baharloo and Ziaeian Hospitals from March to October 2020 in Tehran, Iran. After being discharged from the hospital, those who accepted to take part in the current study were asked to sign the consent form. The demographic information of those who consented to take part and their contact number was collected in a registration form. Then, three psychologists collected the data (demographic and medical variables, GHQ-12, PSS-10, PSQI, ADL and IADL), using telephone survey. Patients were informed about their optional participation in the current research and that they can leave the research any time they wish. This study received ethic approval from the Review Board of Tehran University of Medical Sciences (Ethical Code: IR.TUMS.VCR.REC.1399.156).
Data screening was performed via IBM SPSS Statistics (Version 28). CFA tests of the GHQ-12 were conducted using Mplus version 8.8. Evaluating the assumption of normality revealed a mostly positive but non-substantial skewness in all items; thus, transformation was not required (Gravetter et al., 2020). We applied CFA using the Weighted Least Square Mean and Variance Adjusted (WLSMV) estimator. Statistical strategies were as follows: First, we used the following statistical tests and indices (MacCallum et al., 1996; Hu and Bentler, 1999; Hooper and Coughlan, 2008) to assess the models’ “goodness-of-fit” (acceptable values in parenthesis): the Chi-square (χ2; desired p > 0.05), the Comparative Fit Index (CFI > 0.95), the Tucker–Lewis Index (TLI > 0.95), the Standardized Root Mean Square Residual (SRMR <0.08), the Normal Chi-square (χ2/df < 5), the Root Mean Square Error of Approximation (RMSEA <0.10), and its 90% Confidence Interval (Bentler and Bonett, 1980; MacCallum et al., 1996; Loehlin, 2004; Miles and Shevlin, 2007). The exact fit is defensible when the Chi-square is not significant, regardless of the SRMR value. Approximate fit is tenable when Chi-square is significant, SRMR ≤0.08, and standard residuals are all small (|rres| < 0.1), and finally poor fit is concluded if Chi-square is significant, and SRMR >0.08 (Satorra and Bentler, 2010).
Second, for internal consistency—as recommended for ordinal Likert-type scales, the equivalents of Cronbach’s alpha coefficient (Ordinal Theta and Omega reliability coefficients) using R version 4.1.2 (Team, R. C, 2013; Revelle, 2017) were conducted, which instead of the Pearson correlation matrix, apply the poly-choric correlation matrix (Zumbo et al., 2007; Gadermann et al., 2012). A reliability coefficient of 0.70 or higher was considered an acceptable level (Cicchetti, 1994).
Third, the criterion validity was evaluated by the Spearman coefficient of rank correlation of GHQ-12 with PSQI, PSS-10, and ADL/IADL, since the data showed evidence of non-normality. Correlation coefficients were interpreted based on the effect size classification of Cohen (1988): 0.10 = small, 0.30 = medium, 0.50 = large, and 0.70 = very large.
Forth, Multivariate Analysis of Variance (MANOVA) and effect size (Hedge’s g) were used to compare the mean and standard deviation of the GHQ-12 scores across gender. According to a rule of thumb suggested by Cohen (1988), effect sizes were classified into small (<0.20), medium (0.21–0.50), large (0.51–0.80), and very large (>0.80).
To test the GHQ-12 factor structure, CFA was conducted and the goodness of fit for 13 models was examined (Table 2). Model 1 (M1) examined a general factor, in which, the total of the 12 items were loaded on a single common factor of general mental health (Goldberg et al., 1997; Romppel et al., 2013; Gnambs and Staufenbiel, 2018; Hystad and Johnsen, 2020; Alaminos-Torres et al., 2021) to test the unidimensional model of assumed latent factor and included just random measurement error and indicator-specific variance (Gustafsson and Åberg-Bengtsson, 2010). If the general factor model fitted the data well, it meant that the assumption of the multidimensionality of the measurement tool was violated. Models two to seven (M2 to M7) consisted of a the first-order two-factor oblique models that suggested two subscales measuring two distinct dimensions (Politi et al., 1994; Schrnitz et al., 1999; Montazeri et al., 2003; Kalliath et al., 2004; Najarkolaei et al., 2014; Zhong et al., 2021; Hamad, 2022). Models 8–13 (M8 to M13) examined first-order three-factor oblique models, resembling the Exploratory Factor Analysis (EFA) according to the literature (Graetz, 1991; Farrell, 1998; Martin, 1999; Daradkeh et al., 2001; Gao et al., 2004; del Pilar Sánchez-López and Dresch, 2008; Liang et al., 2016; Lee and Kim, 2020). Model 8 (M8) included general dysphoria, lack of enjoyment, and social dysfunction (Daradkeh et al., 2001). Model 9 (M9) consisted of anxiety, depression, and social dysfunction (Farrell, 1998). Model 10 (M10) was loaded by all three first-order factors, which included social dysfunction, anxiety and depression, and loss of confidence (Graetz, 1991; Gao et al., 2004; Lee and Kim, 2020). Model 11 (M11) included cope, stress, and low self-esteem (Martin, 1999). Model 12 (M12) comprised low level of social function, anxiety/depression, and poor self-confidence (Liang et al., 2016). Finally, Model 13 (M13) included successful coping, self-esteem, and stress (del Pilar Sánchez-López and Dresch, 2008).
In Table 2, all two-factor models (Politi et al., 1994; Schrnitz et al., 1999; Montazeri et al., 2003; Kalliath et al., 2004; Najarkolaei et al., 2014; Zhong et al., 2021; Hamad, 2022) are inadmissible, due to factors correlate greater than 1.00 between two latent factors. The correlation between the two latent factors in two out of six models for the three-factor model also exceeded 1.00, as shown in Table 2 (M9 and M12; Farrell, 1998; Liang et al., 2016). The fit indices of the three-factor oblique model for remaining four models (Table 2; M8, M10, M11, and M13) met some of the specified fit criteria, as prior, and based on the theory-derived models (Graetz, 1991; Martin, 1999; Daradkeh et al., 2001; Gao et al., 2004; del Pilar Sánchez-López and Dresch, 2008; Lee and Kim, 2020). Then, the parsimonious principle (Bollen, 1989) was used to compare the fit indices of the three-factor first-order oblique models (Table 2; M8 [Δχ2 = 357.62, Δdf = 3, p < 0.001], M10[Δχ2 = 500.20, Δdf = 3, p < 0.001], M11[Δχ2 = 278.87, Δdf = 7, p < 0.001], and M13[Δχ2 = 528.49, Δdf = 4, p < 0.001]) with those of the unidimensional first-order model (M1) as the baseline/null model. For three-factor models, four out of six models exhibited similar fitness, though with poor goodness-of-fit (Table 2). To determine the most efficient parsimonious model, the nesting and equivalence testing (NET) methodology was implemented via Mplus 8.8 (Bentler and Satorra, 2010; Asparouhov and Muthén, 2019). Since all models are non-tested and/or non-equivalent, as was expected (the NET value = 0.0000001), it can be concluded that model 13 showed the best fit, due to its low Chi-square value in comparison with the others (χ2/df = 10.04; CFI = 0.96; TLI = 0.94; RMSEA = 0.17; 90% CI = 0.16 to 0.18; SRMR = 0.08). More information on confirmatory factor analysis of models 1, 8, 10, 11, and 13 is presented in supporting information file (Supplementary Figures S1–S5).
The Ordinal Theta and the Omega reliability coefficients for the subscales of GHQ-12 are presented in Table 3. The means of inter-item correlation were 0.10, 0.53, 0.48, and 0.58 for the total score, successful coping, self-esteem, and stress, respectively. Almost all items within the three subscales had a moderate positive relationship with each other (based on the corrected item-total correlation for subscale’s items), with values ranging from 0.34 to 0.83, 0.23 to 0.78., and 0.53 to 0.66 for successful coping, self-esteem, and stress, respectively.
Table 4 demonstrates that the inter-correlation between GHQ-12 total score and subscales ranged from 0.40 to 0.83 (p < 0.01). Criterion validity was estimated by the correlation of GHQ-12 total score and its subscales with PSQI and PSS (Table 4). PSQI had significant positive correlations with total GHQ-12 (r = 0.28, p < 0.01), successful coping (r = 0.24, p < 0.01), self-esteem (r = 0.21, p < 0.01), and stress (r = 0.20, p < 0.01). Also, PSS had significant positive correlations with the total score of GHQ-12 and its subscales (r = 0.31 to 0.58, p < 0.01). In the over 60 years of age group, negative correlations of the total GHQ-12 score were found with the ADL (r = −0.34, p < 0.01; r = −0.37, p < 0.01) and IADL scores (r = −0.42, p < 0.01, r = −0.46, p < 0.01) before and after the infection of COVID-19, respectively (Table 4).
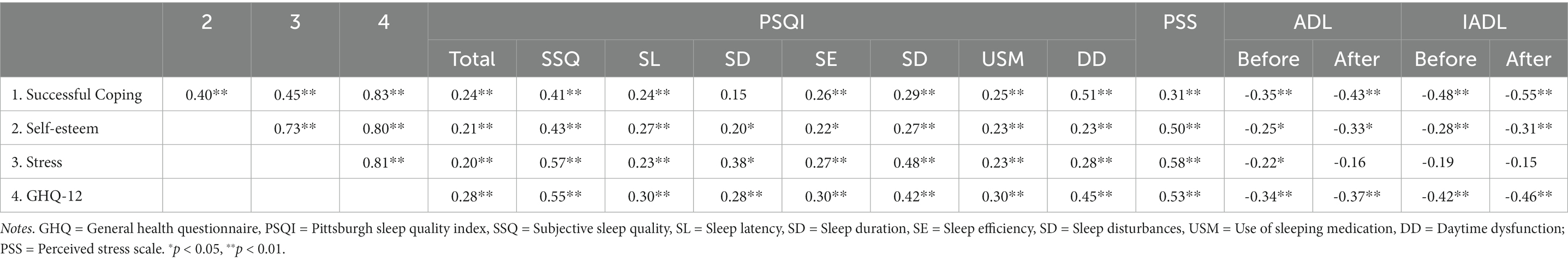
Table 4. The correlation between GHQ-12 subscales and their correlations with sleep quality, perceived stress, and daily functioning.
As depicted in Table 5 for demographic and medical variables, the total score of GHQ-12 was significantly correlated with HLP (r = 0.16, p < 0.01), kidney failure (r = 0.12, p < 0.05), psychiatry disorders (r = 0.18, p < 0.01), the hospitalization duration (r = 0.15, p < 0.01), the change in sleep time (r = 0.31, p < 0.01), use of sleeping pills (r = 0.30, p < 0.01), educational level (r = −0.26, p < 0.01), and the number of family members (r = −0.12, p < 0.05). The correlation of the total score of GHQ-12 with Diabetes, HTN, MI, CVA, PD, obesity, IDD, CVD, and drug, alcohol, and cigarette history were non-significant (p > 0.01). Information for the correlation of GHQ-12 subscales is presented in Table 5.
Table 3 presents the mean and Standard Deviations (SD) of the GHQ-12 total score and subscales across gender and age groups. The female patients scored significantly higher than the males on total GHQ-12 scores [t (310) = −4.77, p < 0.001, Cohen’s d = −0.65, mean difference bootstrap 95% CI = −4.46 to-1.92]. The patients above 60 also scored slightly higher than patents under 60 on their total GHQ-12 scores [t (312) = −1.45, p = 0.08, Cohen’s d = −0.19, mean difference bootstrap 95% CI = −2.94 to 0.55]. A Multivariate Analysis of Variance (MANOVA) showed significant group differences by gender [F (3–308) = 10.80, p < 0.001, η2 = 0.095] and age groups [F (3–310) = 7.27, p < 0.001, η2 = 0.066] on mean scores of the subscales (see Table 3 for Mean scores). Subsequent tests of between-subjects’ effects showed that females scored significantly higher on successful coping [F (1–310) = 5.68, p < 0.05, η2 = 0.018], self-esteem [F (1–310) = 28.11, p < 0.001, η2 = 0.083], and stress [F (1–310) = 27.38, p < 0.081, η2 = 0.081] than males. The patients over 60 scored significantly higher on successful coping [F (1–312) = 9.41, p < 0.01, ns, η2 = 0.029], than patients under 60. However, non-significant differences in mean score were found for self-esteem [F (1–312) = 0.31, p = 0.58, ns, η2 = 0.001] = and stress [F (1–312) = 1.60, p = 0.21, ns, η2 = 0.005] across age.
The present study aimed to assess the psychometric properties of the General Health Questionnaire-12 in patients hospitalized with a diagnosis of COVID-19. Overall, our results offer support for the construct validity, criterion validity, and internal consistency of GHQ-12. Therefore, this questionnaire demonstrates its applicability in Iranian COVID-19 patients.
Among 13 theoretically and empirically emerged models of the GHQ-12 tested in this study, the current data fitted better with the three-factor model of del Pilar Sánchez-López and Dresch (2008), including successful coping, self-esteem, and stress. The factor loading of all items was adequate (Ford et al., 1986). This result is contrary to Liang et al. (2016) study that showed equal model fit (CFI = 0.98, RMSEA = 0.03) for 11 previously emerged factorial models. The unidimensional model (Goldberg et al., 1997) was not supported in our study, suggesting that GHQ-12 may not be a homogeneous tool that measures only one construct of mental health, or rather, it may cover several constructs instead of concentrating on “narrow aspects” of mental health (Gustafsson and Åberg-Bengtsson, 2010). The established factorial model manifested good reliabilities. Indeed, the overall results of the Cronbach’s alpha, Theta, and Omega coefficients were satisfactory, with the adequate means of inter-item correlations for subscales. These results are in line with a bulk of studies on the psychometric features of GHQ-12 in different contexts (Liang et al., 2016; Elovanio et al., 2020).
To test how accurately the GHQ-12 can correlate the expected outcomes, the criterion validity was conducted as our third objective through the relationship of GHQ with perceived stress, sleep quality, ADL/IADL, and demographic and medical variables. First, GHQ-12 total score and subscales showed significant weak to strong correlations with the sleep quality total score and all subscales, where the subscale of subjective sleep quality had the strongest correlation coefficients. These findings are supported by previous research (Xiong et al., 2019; Aquil et al., 2021; Thielmann et al., 2021). Oh et al. (2019), for instance, found that adults with higher psychological distress had higher difficulty falling asleep. Second, perceived stress showed moderate to high positive correlations with the GHQ-12 total score and three subscales, further supporting the criterion validity of GHQ-12. These findings were consistent with previous studies (Örücü and Demir, 2009; Gajula et al., 2021). It is thought that psychosocial stressors, such as living alone, social restrictions and isolation, financial burden, and loss of family members, that lead to heightened anxiety, fear, and anger, made a significant contribution to the higher level of stress experienced by patients with COVID-19 (Torales et al., 2020; Matalon et al., 2021; Varman et al., 2022).
The GHQ-12 in patients over 60 demonstrated negative correlations with ADL and IADL-as the third criterion variable. A similar result was found by earlier studies (Albanese et al., 2020). Our finding suggested that lack of autonomy in daily life can seriously damage a person’s self-esteem, increase their conflicts with others, and make them more vulnerable to symptoms of anxiety and depression.
The forth variable used to evaluate the criterion validity of GHQ-12 was medical variables, that manifested a set of significant associations. This questionnaire had significant positive correlation with HLP, in line with the study of Wang et al. (2016) that found the GHQ-12 scores was significantly higher in patients with HLP. This association seems bidirectional, given that on the one hand, the empirical evidence suggested that HLP triggers the onset of depression (Chuang et al., 2014), and on the other hand, patients with depression experience a higher incidence of HLP, compared to the general population (Chien et al., 2013). Chang et al. (2021) also showed positive correlation of high blood fat and stress. Kidney failure was shown to be positively correlated with GHQ-12, consistent with two systematic reviews that found a high rate of depression in patients with Kidney failure (Bautovich et al., 2014; Kondo et al., 2020). One explanation for this link might be the impact of difficulties the patients with kidney failure face, such as the psychological and social burden of the disease, comorbid diseases, and the experience of dialysis, which may lead to depression/anxiety (Ozcan et al., 2015). These symptoms are, in turn, associated with negative outcomes including poor quality of life, poor treatment compliance, and elevated mortality rates (Bautovich et al., 2014; Butt et al., 2022). Furthermore, GHQ-12 was significantly correlated with psychiatry disorders. This association is expected because mental illnesses decrease the quality of life and severely impair patients’ ability to communicate and form social relationships. Therefore, it is likely that they are more affected by a pandemic than those with no psychiatric conditions (Kaufman et al., 2020). GHQ-12 was positively correlated with the hospitalization duration. This is another expected result, because at hospitals, patients experience a loss of dignity as a result of their physical conditions, elevating their senses of powerlessness, embarrassment, and being violated. Consequently, these debilitating experiences may lead to mental distress (Liao et al., 2020). Finally, GHQ-12 showed positive correlations with change in sleep time and use of sleeping pills. The change in the sleep–wake cycle might be explained by a third mechanism like anxiety symptoms (Becker et al., 2018). Tang et al. (2017) suggested that higher score of GHQ-12 was strongly predicted by the reduced sleep duration and use of sleeping pills, and vice versa. They argued that extremely long or short sleep duration and excessive use of sleeping pills lead to difficulty in daytime function, which result in adverse outcomes. However, it should be noted that all of these correlations in the current study were weak to moderate and should be interpreted cautiously.
Finally, the criterion validity of GHQ-12 was examined via its link with demographic characteristics. GHQ-12 showed negative correlations with educational level and the number of family members. Consistent with our finding, Dalgard et al. (2007) study have shown a significant association between lower educational level and psychological distress in both Norwegian males and female. Additionally, people who live alone may be especially dependent on others for social connection and support, making them more vulnerable to social distancing (Hendriksen et al., 2021). Hence, larger number of family members may be a protective factor against the sense of loneliness and act as a means for social support.
Due to some clues that showed the gender and age differences in the level of GHQ-12, we investigated these group mean differences to be considered in the future use of the questionnaire. In the present study, consistent with previous evidence (Giorgi et al., 2014), lower average of general health in women (higher GHQ-12 total scores and subscales) was observed. Previous evidence have shown that the prevalence of factors thought to be intensified during a pandemic (such as preceding anxiety and depression, chronic environmental exposure, and domestic violence) is higher among women (Bucciarelli et al., 2021). This could increase women’s odds of developing mental health issues. As for age differences, higher level of the GHQ-12 total score and successful coping subscale in patients older than 60 years was found in the present study. This result contradicted previous findings that indicated the association of aging with an intrinsic reduction in susceptibility to psychological distress (Hoeymans et al., 2004). However, losing social contacts in the elderly (e.g., the death of family members), becoming prohibited from engagement in common social interactions due to social distancing order, and receiving limited access to social support and services may increase their susceptibility to mental health problems (Stuart et al., 2022).
The current study results provide insight into the general mental health status in patients with COVID-19. However, this study is not without limitations. First, GHQ-12 is a screening tool and was not designed for diagnosis objectives and distinguishing among mental disorders (Goldberg, 1986; Schrnitz et al., 1999). Researchers in future work can use semi-structured interviews to provide more in-depth information regarding high scored items of GHQ-12 and compare yielded scores of GHQ-12 with the additional probe questions (i.e., regarding symptom severity and duration) to evaluate the accuracy of GHQ-12. Second, the cross-sectional design of the current study has prevented causal inferences. It restricts our knowledge on the direction of the correlation of GHQ-12 with perceived stress and sleep quality. It also prevents us from measuring the stability of mental health scores over time. Longitudinal studies are recommended to explore the predictive role of the abovementioned variables on each other, and evaluate the stability of GHQ-12 scores over time. Finally, the present study did not perform the measurement invariance analyses across gender or age, because the sample sizes would start to become small when we divided the sample into age and gender subgroups. In the age case, sample size would be down to 87 for the younger segment. Such small sample sizes lacked sufficient power to detect any invariance.
Given the positive link of poor mental health with perceived stress, sleep disturbances, and impaired independent daily activities among Iranian COVID-19 patients, an important clinical implication for physicians, psychologists, and psychiatrists is to design psychological interventional courses for COVID-19 hospitalized patients that specifically target these problems. Access to such services via social media may be beneficial not only for their mental health, but also for their ability to improve their physical and mental functioning and independency (Shojaei and Masoumi, 2020).
The current study was undertaken to evaluate the psychometric properties of GHQ-12 among Iranian COVID-19 patients. The results of construct validity analyses supported the three-factor model of successful coping, self-esteem, and stress, which showed satisfactory reliability. The criterion validity of GHQ-12 was confirmed through its positive relationship with perceived stress and sleep quality, as well as its negative relationships with activities and instrumental activities of daily living in patients with over 60 years of age. Women and patients above 60 manifested higher GHQ-12 scores, compared to men and patients under 60.
The raw data supporting the conclusions of this article can be provided by the corresponding author upon reasonable request.
The studies involving human participants were reviewed and approved by the Review Board of Tehran University of Medical Sciences (ethical code: IR.TUMS.VCR.REC.1399.156). The patients/participants provided their written informed consent to participate in this study.
MHA, FE, and ZV: conceptualization, design, methodology, and investigation and project administration. FF and FG: data collection. MHA: formal analysis and supervision. PSY, NAS, and MHA: writing the original draft. PSY, NW, and MHA: revising the draft. All authors have contributed to the conception and design of the study, drafted or revised this manuscript, reviewed the final version of this manuscript before submission, and agreed to be accountable for all aspects of the work.
This research was supported by grant number 99-1-101-47,395 from the Tehran University of Medical sciences.
The authors would like to thank all patients who participated in the study and the Baharloo and Ziaeian Hospitals’ staff who assisted in data collection.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1132154/full#supplementary-material
GHQ, General Health Questionnaire; PSS, Perceived Stress Scale; PSQI, Pittsburgh Sleep Quality Index; ADL, activities of daily life; IADL, instrumental activities of daily living; HTN, high blood pressure; HLP, hyperlipidemia; CVA, cerebrovascular accident; HPA, hypothalamic pituitary adrenal; PD, pulmonary disease; IDD, immune deficiency disease; MI, myocardial infarction; CVD, cardiovascular disease.
Achdut, N., and Refaeli, T. (2020). Unemployment and psychological distress among young people during the COVID-19 pandemic: psychological resources and risk factors. Int. J. Environ. Res. Public Health 17:7163. doi: 10.3390/ijerph17197163
Alaminos-Torres, A., Martinez-Lorca, M., Sifre De Sola, I., López-Ejeda, N., and Dolores Marrodán, M. (2021). Psychological distress in Spanish airline pilots during the aviation crisis caused by the COVID-19 pandemic and psychometric analysis of the 12-item general health questionnaire. Ergonomics 65, 741–752. doi: 10.1080/00140139.2021.1984587
Albanese, A. M., Bartz-Overman, C., Parikh, M. T., and Thielke, S. M. (2020). Associations between activities of daily living independence and mental health status among medicare managed care patients. J. Am. Geriatr. Soc. 68, 1301–1306. doi: 10.1111/jgs.16423
Aquil, A., El Kherchi, O., El Azmaoui, N., Mouallif, M., Guerroumi, M., Chokri, A., et al. (2021). Body image dissatisfaction and lower self-esteem as major predictors of poor sleep quality in gynecological cancer patients after surgery: cross-sectional study. BMC Womens Health 21, 229–211. doi: 10.1186/s12905-021-01375-5
Asparouhov, T., and Muthén, B. (2019). Nesting and equivalence testing for structural equation models. Struct. Equ. Model. Multidiscip. J. 26, 302–309. doi: 10.1080/10705511.2018.1513795
Bautovich, A., Katz, I., Smith, M., Loo, C. K., and Harvey, S. B. (2014). Depression and chronic kidney disease: a review for clinicians. Aust N Z J Psychiatry 48, 530–541. doi: 10.1177/0004867414528589
Becker, S. P., Jarrett, M. A., Luebbe, A. M., Garner, A. A., Burns, G. L., and Kofler, M. J. (2018). Sleep in a large, multi-university sample of college students: sleep problem prevalence, sex differences, and mental health correlates. Sleep Health 4, 174–181. doi: 10.1016/j.sleh.2018.01.001
Bentler, P. M., and Bonett, D. G. (1980). Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 88, 588–606. doi: 10.1037/0033-2909.88.3.588
Bentler, P. M., and Satorra, A. (2010). Testing model nesting and equivalence. Psychol. Methods 15, 111–123. doi: 10.1037/a0019625
Bonsaksen, T., Leung, J., Price, D., Ruffolo, M., Lamph, G., Kabelenga, I., et al. (2022). Self-reported Long COVID in the general population: sociodemographic and health correlates in a cross-national sample. Life 12:901. doi: 10.3390/life12060901
Bruine de Bruin, W. (2021). Age differences in COVID-19 risk perceptions and mental health: evidence from a national US survey conducted in March 2020. J Gerontol Ser B 76, e24–e29. doi: 10.1093/geronb/gbaa074
Bucciarelli, V., Nasi, M., Bianco, F., Seferovic, J., Ivkovic, V., Gallina, S., et al. (2021). Depression pandemic and cardiovascular risk in the COVID-19 era and long COVID syndrome: gender makes a difference. Trends Cardiovasc. Med. 32, 12–17. doi: 10.1016/j.tcm.2021.09.009
Butt, M. D., Ong, S. C., Butt, F. Z., Sajjad, A., Rasool, M. F., Imran, I., et al. (2022). Assessment of health-related quality of life, medication adherence, and prevalence of depression in kidney failure patients. Int. J. Environ. Res. Public Health 19:15266. doi: 10.3390/ijerph192215266
Buysse, D. J., Reynolds, C. F. III, Monk, T. H., Berman, S. R., and Kupfer, D. J. (1989). The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213. doi: 10.1016/0165-1781(89)90047-4
Carfì, A., Bernabei, R., and Landi, F. (2020). Persistent symptoms in patients after acute COVID-19. JAMA 324, 603–605. doi: 10.1001/jama.2020.12603
Chang, P.-Y., Chiou, S.-T., Lo, W.-Y., Huang, N., and Chien, L.-Y. (2021). Stressors and level of stress among different nursing positions and the associations with hyperlipidemia, hyperglycemia, and hypertension: a national questionnaire survey. BMC Nurs. 20, 250–210. doi: 10.1186/s12912-021-00777-y
Chien, I.-C., Lin, C.-H., Chou, Y.-J., and Chou, P. (2013). Increased risk of hyperlipidemia in patients with major depressive disorder: a population-based study. J. Psychosom. Res. 75, 270–274. doi: 10.1016/j.jpsychores.2013.06.003
Chuang, C.-S., Yang, T.-Y., Muo, C.-H., Su, H.-L., Sung, F.-C., and Kao, C.-H. (2014). Hyperlipidemia, statin use and the risk of developing depression: a nationwide retrospective cohort study. Gen. Hosp. Psychiatry 36, 497–501. doi: 10.1016/j.genhosppsych.2014.05.00
Cicchetti, D. V. (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess. 6, 284–290. doi: 10.1037/1040-3590.6.4.284
Cohen, J. (1988). Statistical Power Analysis for the Behavioral Sciences. Abingdon-on-Thames: Routledge Academic.
Cohen, S., Kamarck, T., and Mermelstein, R. (1983). A global measure of perceived stress. J. Health Soc. Behav. 24:385. doi: 10.2307/2136404
Crayne, M. P. (2020). The traumatic impact of job loss and job search in the aftermath of COVID-19. Psychol. Trauma Theory Res. Pract. Policy 12, S180–S182. doi: 10.1037/tra0000852
Czeisler, M. É., Lane, R. I., Petrosky, E., Wiley, J. F., Christensen, A., Njai, R., et al. (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morb. Mortal. Wkly Rep. 69, 1049–1057. doi: 10.15585/mmwr.mm6932a1
Dalgard, O. S., Mykletun, A., Rognerud, M., Johansen, R., and Zahl, P. H. (2007). Education, sense of mastery and mental health: results from a nation wide health monitoring study in Norway. BMC Psychiatry 7, 1–9. doi: 10.1186/1471-244x-7-20
Daradkeh, T. K., Ghubash, R., and El-Rufaie, O. E. (2001). Reliability, validity, and factor structure of the Arabic version of the 12-item general health questionnaire. Psychol. Rep. 89, 85–94. doi: 10.2466/pr0.2001.89.1.85
de Castroe Costa, E., Uchoa, E., Oliveira Araújo Firmo, J., Lima-Costa, M. F., and Prince, M. (2008). Association of cognitive impairment, activity limitation with latent traits in the GHQ-12 in the older elderly. The Bambui health and aging study (BHAS). Aging Clin. Exp. Res. 20, 562–568. doi: 10.1007/bf03324885
de Paiva Teixeira, L. E. P., de Freitas, R. L., Abad, A., da Silva, J. A., Antonelli-Ponti, M., Bastos, S., et al. (2020). Psychological impacts related to stress and fear during the COVID-19 pandemic: cardiovascular diseases, diabetes and psychological disorders as risk factors. World J Neurosci 10, 191–205. doi: 10.4236/wjns.2020.104019
del Pilar Sánchez-López, M., and Dresch, V. (2008). The 12-item general health questionnaire (GHQ-12): reliability, external validity and factor structure in the Spanish population. Psicothema 20, 839–843.
Deng, J., Zhou, F., Hou, W., Silver, Z., Wong, C. Y., Chang, O., et al. (2021). The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann. N. Y. Acad. Sci. 1486, 90–111. doi: 10.1111/nyas.14506
Edemekong, P.F., Bomgaars, D.L., and Levy, S.B. (2017). Activities of daily living (ADLs). Treasure Island (FL): StatPearls Publishing.
Elovanio, M., Hakulinen, C., Pulkki-Råback, L., Aalto, A.-M., Virtanen, M., Partonen, T., et al. (2020). General health questionnaire (GHQ-12), Beck depression inventory (BDI-6), and mental health index (MHI-5): psychometric and predictive properties in a Finnish population-based sample. Psychiatry Res. 289:112973. doi: 10.1016/j.psychres.2020.112973
Farrahi Moghaddam, J., Nakhaee, N., Sheibani, V., Garrusi, B., and Amirkafi, A. (2012). Reliability and validity of the Persian version of the Pittsburgh sleep quality index (PSQI-P). Sleep Breath 16, 79–82. doi: 10.1007/s11325-010-0478-5
Farrell, G. A. (1998). The mental health of hospital nurses in Tasmania as measured by the 12-item general health questionnaire. J. Adv. Nurs. 28, 707–712. doi: 10.1046/j.1365-2648.1998.00735.x
Ford, J. K., MacCallum, R. C., and Tait, M. (1986). The application of exploratory factor analysis in applied psychology: a critical review and analysis. Pers. Psychol. 39, 291–314. doi: 10.1111/j.1744-6570.1986.tb00583.x
Gadermann, A. M., Guhn, M., and Zumbo, B. D. (2012). Estimating ordinal reliability for Likert-type and ordinal item response data: a conceptual, empirical, and practical guide. Pract Assess Res Eval 17:3. doi: 10.7275/n560-j767
Gajula, M., Bant, D., and Bathija, G. V. (2021). Perceived stress among adolescent school students in Hubli: a cross-sectional study. Natl J Community Med 12, 169–174. doi: 10.5455/njcm.20210625054326
Gao, F., Luo, N., Thumboo, J., Fones, C., Li, S.-C., and Cheung, Y.-B. (2004). Does the 12-item general health questionnaire contain multiple factors and do we need them? Health Qual. Life Outcomes 2, 1–7. doi: 10.1186/1477-7525-2-63
Giorgi, G., Perez, J. M. L., D’Antonio, A. C., Perez, F. J. F., Arcangeli, G., Cupelli, V., et al. (2014). The General Health Questionaire (GHQ-12) in a sample of Italian workers: mental health at individual and organizational level. World J Med Sci 11, 47–56. doi: 10.5829/idosi.wjms.2014.11.1.83295
Gnambs, T., and Staufenbiel, T. (2018). The structure of the general health questionnaire (GHQ-12): two meta-analytic factor analyses. Health Psychol. Rev. 12, 179–194. doi: 10.1080/17437199.2018.1426484
Goldberg, D. P. (1972). The detection of psychiatric illness by questionnaire. Maudsley Monogr. Windsor, UK: Nfer-Nelson Publisher, 21:483.
Goldberg, D. (1986). Use of the general health questionnaire in clinical work. Br. Med. J. (Clin. Res. Ed.) 293, 1188–1189. doi: 10.1136/bmj.293.6556.1188
Goldberg, D. P., Gater, R., Sartorius, N., Ustun, T. B., Piccinelli, M., Gureje, O., et al. (1997). The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 27, 191–197. doi: 10.1017/s0033291796004242
Graetz, B. (1991). Multidimensional properties of the general health questionnaire. Soc. Psychiatry Psychiatr. Epidemiol. 26, 132–138. doi: 10.1007/bf00782952
Gravetter, F. J., Wallnau, L. B., Forzano, L.-A. B., and Witnauer, J. E. (2020). Essentials of Statistics for the Behavioral Sciences. Boston, MA: Cengage Learning.
Gustafsson, J.-E., and Åberg-Bengtsson, L. (2010). “Unidimensionality and interpretability of psychological instruments,” in Measuring Psychological Constructs: Advances in Model-Based Approaches. ed. S. E. Embretson (Washington, DC, US: American Psychological Association), 97–121.
Halpin, D. M., Singh, D., and Hadfield, R. M. (2020). Inhaled corticosteroids and COVID-19: a systematic review and clinical perspective. Eur. Respir. J. 55:2001009. doi: 10.1183/13993003.01009-2020
Hamad, E. O. (2022). Psychological well-being among Saudi adults during the context of COVID-19 lockdown: a psychometric analysis of the 12-item General Health Questionnaire. BMC Psychol. 10:319. doi: 10.21203/rs.3.rs-1591586/v1
Hendriksen, P. A., Kiani, P., Garssen, J., Bruce, G., and Verster, J. C. (2021). Living alone or together during lockdown: association with mood, immune fitness and experiencing COVID-19 symptoms. Psychol. Res. Behav. Manag. 14, 1947–1957. doi: 10.2147/prbm.s332853
Hoeymans, N., Garssen, A. A., Westert, G. P., and Verhaak, P. F. (2004). Measuring mental health of the Dutch population: a comparison of the GHQ-12 and the MHI-5. Health Qual. Life Outcomes 2, 1–6. doi: 10.1186/1477-7525-2-23
Hooper, D., and Coughlan, J. (2008). Structural equation modelling: guidelines for determining model fit. Electron. J. Bus. Res. Methods 6, 53–60. doi: 10.21427/D7CF7R
Hossain, M. M., Rahman, M., Trisha, N. F., Tasnim, S., Nuzhath, T., Hasan, N. T., et al. (2021). Prevalence of anxiety and depression in South Asia during COVID-19: a systematic review and meta-analysis. Heliyon 7:e06677. doi: 10.31234/osf.io/q4k5b
Hu, L. T., and Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 6, 1–55. doi: 10.1080/10705519909540118
Hystad, S. W., and Johnsen, B. H. (2020). The dimensionality of the 12-item general health questionnaire (GHQ-12): comparisons of factor structures and invariance across samples and time. Front. Psychol. 11:1300. doi: 10.3389/fpsyg.2020.01300
Kalliath, T. J., O'Driscoll, M. P., and Brough, P. (2004). A confirmatory factor analysis of the General Health Questionnaire-12. Stress Health 20, 11–20. doi: 10.1002/smi.993
Katz, S., Downs, T. D., Cash, H. R., and Grotz, R. C. (1970). Progress in development of the index of ADL. Gerontologist 10, 20–30. doi: 10.1093/geront/10.1_part_1.20
Kaufman, K. R., Petkova, E., Bhui, K. S., and Schulze, T. G. (2020). A global needs assessment in times of a global crisis: world psychiatry response to the COVID-19 pandemic. BJPsych Open 6:e48. doi: 10.1192/bjo.2020.25
Kondo, K., Antick, J. R., Ayers, C. K., Kansagara, D., and Chopra, P. (2020). Depression screening tools for patients with kidney failure: a systematic review. Clin. J. Am. Soc. Nephrol. 15, 1785–1795. doi: 10.2215/CJN.05540420
Korkut, S. (2022). Evaluation of Psychopathological Conditions, Corona Anxiety, Death Anxiety and Suicide Risk in Hemodialysis Patients during the COVID-19 Pandemic. doi: 10.21203/rs.3.rs-1211968/v1
Lawton, M. (2000). Lawton instrumental activities of daily living scale. Merck Manual Geriatr 108, 52–62. doi: 10.1097/01.naj.0000314810.46029.74
Lee, B., and Kim, Y. E. (2020). Factor structure of the 12-item general health questionnaire (GHQ-12) among Korean university students. Psychiatry Clin. Psychopharmacol 30, 248–253. doi: 10.5455/pcp.20200518112914
Liang, Y., Wang, L., and Yin, X. (2016). The factor structure of the 12-item general health questionnaire (GHQ-12) in young Chinese civil servants. Health Qual. Life Outcomes 14, 136–139. doi: 10.1186/s12955-016-0539-y
Liao, K.-M., Ho, C.-H., Lai, C.-C., Chao, C.-M., Chiu, C.-C., Chiang, S.-R., et al. (2020). The association between depression and length of stay in the intensive care unit. Medicine 99:e20514. doi: 10.1097/md.0000000000020514
Loehlin, J.C. (2004). Latent Variable Models: An introduction to Factor, Path, and Structural Equation Analysis. 4th. New Jersey: Lawrence Erlbaum Associates Publishers.
MacCallum, R. C., Browne, M. W., and Sugawara, H. M. (1996). Power analysis and determination of sample size for covariance structure modeling. Psychol. Methods 1, 130–149. doi: 10.1037/1082-989X.1.2.130
Maroufizadeh, S., Foroudifard, F., Navid, B., Ezabadi, Z., Sobati, B., and Omani-Samani, R. (2018). The perceived stress scale (PSS-10) in women experiencing infertility: a reliability and validity study. Middle East Fertil Soc J 23, 456–459. doi: 10.1016/j.mefs.2018.02.003
Maroufizadeh, S., Pourshaikhian, M., Pourramzani, A., Sheikholeslami, F., Moghadamnia, M.T., and Alavi, S.A. (2022). Prevalence of Anxiety and Depression in General Population of Iran during the COVID-19 Pandemic: A Web-Based Cross-Sectional Study. Iran. J. Psychiatry 17, 230–239. doi: 10.21203/rs.3.rs-39082/v1
Martin, A. J. (1999). Assessing the multidimensionality of the 12-item general health questionnaire. Psychol. Rep. 84, 927–935. doi: 10.2466/pr0.1999.84.3.927
Marvaldi, M., Mallet, J., Dubertret, C., Moro, M. R., and Guessoum, S. B. (2021). Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 126, 252–264. doi: 10.1016/j.neubiorev.2021.03.024
Matalon, N., Dorman-Ilan, S., Hasson-Ohayon, I., Hertz-Palmor, N., Shani, S., Basel, D., et al. (2021). Trajectories of post-traumatic stress symptoms, anxiety, and depression in hospitalized COVID-19 patients: a one-month follow-up. J. Psychosom. Res. 143:110399. doi: 10.1016/j.jpsychores.2021.110399
Mehraban, A. H., Soltanmohamadi, Y., Akbarfahimi, M., and Taghizadeh, G. (2014). Validity and reliability of the Persian version of Lawton instrumental activities of daily living scale in patients with dementia. Med. J. Islam Repub. Iran 28:25.
Miles, J., and Shevlin, M. (2007). A time and a place for incremental fit indices. Personal. Individ. Differ. 42, 869–874. doi: 10.1016/j.paid.2006.09.022
Moghanibashi-Mansourieh, A. (2020). Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatr. 51:102076. doi: 10.1016/j.ajp.2020.102076
Montazeri, A., Harirchi, A. M., Shariati, M., Garmaroudi, G., Ebadi, M., and Fateh, A. (2003). The 12-item general health questionnaire (GHQ-12): translation and validation study of the Iranian version. Health Qual. Life Outcomes 1, 1–4. doi: 10.1186/1477-7525-1-66
Moradian, S., Teufel, M., Jahre, L., Musche, V., Fink, M., Dinse, H., et al. (2021). Mental health burden of patients with diabetes before and after the initial outbreak of COVID-19: predictors of mental health impairment. BMC Public Health 21, 2068–2011. doi: 10.1186/s12889-021-12101-z
Najarkolaei, F. R., Raiisi, F., Rahnama, P., Fesharaki, M. G., Zamani, O., Jafari, M. R., et al. (2014). Factor structure of the Iranian version of 12-item general health questionnaire. Iran Red Crescent Med J 16:e11794. doi: 10.5812/ircmj.11794
Nakhostin-Ansari, A., Sherafati, A., Aghajani, F., Khonji, M. S., Aghajani, R., and Shahmansouri, N. (2020). Depression and anxiety among Iranian medical students during COVID-19 pandemic. Iran. J. Psychiatry 15, 228–235. doi: 10.18502/ijps.v15i3.3815
Oh, C.-M., Kim, H. Y., Na, H. K., Cho, K. H., and Chu, M. K. (2019). The effect of anxiety and depression on sleep quality of individuals with high risk for insomnia: a population-based study. Front. Neurol. 10:849. doi: 10.3389/fneur.2019.00849
Örücü, M. Ç., and Demir, A. (2009). Psychometric evaluation of perceived stress scale for Turkish university students. Stress Health 25, 103–109. doi: 10.1080/09638237.2017.1417566
Ozcan, H., Yucel, A., Avşar, U., Çankaya, E., Yucel, N., Gözübüyük, H., et al. (2015). Kidney transplantation is superior to hemodialysis and peritoneal dialysis in terms of cognitive function, anxiety, and depression symptoms in chronic kidney disease. Transplant Proc 47, 1348–1351. doi: 10.1016/j.transproceed.2015.04.032
Pappa, S., Chen, J., Barnett, J., Chang, A., Dong, R. K., Xu, W., et al. (2022). A systematic review and meta-analysis of the mental health symptoms during the Covid-19 pandemic in S outheast a sia. Psychiatry Clin. Neurosci. 76, 41–50. doi: 10.1111/pcn.13306
Politi, P., Piccinelli, M., and Wilkinson, G. (1994). Reliability, validity and factor structure of the 12-item general health questionnaire among young males in Italy. Acta Psychiatr. Scand. 90, 432–437. doi: 10.1111/j.1600-0447.1994.tb01620.x
Proto, E., and Quintana-Domeque, C. (2021). COVID-19 and mental health deterioration by ethnicity and gender in the UK. PLoS One 16:e0244419. doi: 10.1371/journal.pone.0244419
Revelle, W. R. (2017). Psych: Procedures for Personality and Psychological Research [Computer software]. Comprehensive R Archive Network.
Roehrig, B., Hoeffken, K., Pientka, L., and Wedding, U. (2007). How many and which items of activities of daily living (ADL) and instrumental activities of daily living (IADL) are necessary for screening. Crit. Rev. Oncol. Hematol. 62, 164–171. doi: 10.1016/j.critrevonc.2006.10.001
Romppel, M., Braehler, E., Roth, M., and Glaesmer, H. (2013). What is the general health Questionnaire-12 assessing?: dimensionality and psychometric properties of the general health Questionnaire-12 in a large scale German population sample. Compr. Psychiatry 54, 406–413. doi: 10.1016/j.comppsych.2012.10.010
Santomauro, D. F., Herrera, A. M. M., Shadid, J., Zheng, P., Ashbaugh, C., Pigott, D. M., et al. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 398, 1700–1712. doi: 10.1016/S0140-6736(21)02143-7
Satorra, A., and Bentler, P. M. (2010). Ensuring Positiveness of the scaled difference chi-square test statistic. Psychometrika 75, 243–248. doi: 10.1007/s11336-009-9135-y
Schrnitz, N., Kruse, J., and Tress, W. (1999). Psychometric properties of the general health questionnaire (GHQ-12) in a German primary care sample. Acta Psychiatr. Scand. 100, 462–468. doi: 10.1111/j.1600-0447.1999.tb10898.x
Shahriarirad, R., Erfani, A., Ranjbar, K., Bazrafshan, A., and Mirahmadizadeh, A. (2021). The mental health impact of COVID-19 outbreak: a Nationwide survey in Iran. Int. J. Ment. Heal. Syst. 15:19. doi: 10.1186/s13033-021-00445-3
Sharifi, F., Alizadeh-Khoei, M., Saghebi, H., Angooti-Oshnari, L., Fadaee, S., Hormozi, S., et al. (2018). Validation study of ADL-Katz scale in the Iranian elderly nursing homes. Ageing Int. 43, 508–523. doi: 10.1007/s12126-017-9314-6
Shojaei, S. F., and Masoumi, R. (2020). The importance of mental health training for psychologists in COVID-19 outbreak. Middle East J Rehabil Health Stud 7:e102846. doi: 10.5812/mejrh.102846
Stuart, A., Katz, D., Stevenson, C., Gooch, D., Harkin, L., Bennasar, M., et al. (2022). Loneliness in older people and COVID-19: applying the social identity approach to digital intervention design. Comput Hum Behav Rep 6:100179. doi: 10.31234/osf.io/qk9hb
Tang, N. K., Fiecas, M., Afolalu, E. F., and Wolke, D. (2017). Changes in sleep duration, quality, and medication use are prospectively associated with health and well-being: analysis of the UK household longitudinal study. Sleep 40. doi: 10.1093/sleep/zsw079
Team, R. C. (2013). R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. Available at: http://www.R-project.org/ (Accessed April 23, 2022).
Thielmann, B., Schierholz, R. S., and Böckelmann, I. (2021). Subjective and objective consequences of stress in subjects with subjectively different sleep quality—a cross-sectional study. Int. J. Environ. Res. Public Health 18:9990. doi: 10.3390/ijerph18199990
Torales, J., Ríos-González, C., Barrios, I., O'Higgins, M., González, I., García, O., et al. (2020). Self-perceived stress during the quarantine of COVID-19 pandemic in Paraguay: an exploratory survey. Front. Psych. 11:558691. doi: 10.3389/fpsyt.2020.558691
Varman, P. A., Ananthi, P., and Sugirda, P. (2022). Evaluation of perceived stress and coronavirus-specific anxiety among hospitalized COVID-19 patients–a cross-sectional study. Asian J Med Sci 13, 18–22. doi: 10.3126/ajms.v13i4.42132
Wang, S., Li, B., Ungvari, G. S., Ng, C. H., Chiu, H. F., Kou, C., et al. (2016). Poor mental health status and its associations with demographic characteristics and chronic diseases in Chinese elderly. Soc. Psychiatry Psychiatr. Epidemiol. 51, 1449–1455. doi: 10.1007/s00127-016-1271-y
WHO (2020). Mental Health and Psychosocial Considerations during the COVID-19 Outbreak, 18 March 2020. World Health Organization. Available at: https://apps.who.int/iris/handle/10665/331490
Xiong, W., Liu, H., Gong, P., Wang, Q., Ren, Z., He, M., et al. (2019). Relationships of coping styles and sleep quality with anxiety symptoms among Chinese adolescents: a cross-sectional study. J. Affect. Disord. 257, 108–115. doi: 10.1016/j.jad.2019.07.032
Zandifar, A., and Badrfam, R. (2020). Fighting COVID-19 in Iran; economic challenges ahead. Arch. Iran. Med. 23:284. doi: 10.34172/aim.2020.14
Zhang, S. X., Miller, S. O., Xu, W., Yin, A., Chen, B. Z., Delios, A., et al. (2022). Meta-analytic evidence of depression and anxiety in Eastern Europe during the COVID-19 pandemic. Eur. J. Psychotraumatol. 13:2000132. doi: 10.1080/20008198.2021.2000132
Zhong, X., Jin, X., Yan, L., Yang, L., Long, H., Wang, J., et al. (2021). Reliability and validity of General Health Questionnaire-12 in Chinese dental healthcare workers during the COVID-19 pandemic. Front. Psych. 12:792838. doi: 10.3389/fpsyt.2021.792838
Keywords: COVID-19, concurrent validity, general health, medical condition, reliability, sleep, activities of daily life, stress
Citation: Habibi Asgarabad M, Etesam F, Salehi Yegaei P, Vahabi Z, Akbari Saneh N, Fathi F, Ghosi F and Wiium N (2023) Construct validity of the General Health Questionnaire (GHQ-12) in patients with COVID-19 and its demographic and medical correlates. Front. Psychol. 14:1132154. doi: 10.3389/fpsyg.2023.1132154
Received: 26 December 2022; Accepted: 30 March 2023;
Published: 05 June 2023.
Edited by:
Vincenzo Auriemma, University of Salerno, ItalyCopyright © 2023 Habibi Asgarabad, Etesam, Salehi Yegaei, Vahabi, Akbari Saneh, Fathi, Ghosi and Wiium. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mojtaba Habibi Asgarabad, TW9qdGFiYS5oLmFzZ2FyYWJhZEBudG51Lm5v; Zahra Vahabi, enZhaGFiaUBzaW5hLnR1bXMuYWMuaXI=
†ORCID: Mojtaba Habibi Asgarabad, https://orcid.org/0000-0002-5011-2823
Farnaz Etesam, https://orcid.org/0000-0002-4083-4216
Pardis Salehi Yegaei, https://orcid.org/0000-0002-0773-650X
Zahra Vahabi, https://orcid.org/0000-0001-5057-8028
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.