- 1School of Marxism, Xi’an Jiaotong University, Xi’an, Shaanxi, China
- 2Department of Obstetrics and Gynecology, The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shaanxi, China
- 3Department of Gynecology, Shaanxi Provincial People's Hospital, Xi'an, Shaanxi, China
Introduction: The present study aimed to provide a more accurate representation of post-traumatic stress disorder (PTSD) in college students during COVID-19 by performing meta-analyses by continents, national income, and study majors, and comparing the results with estimated pooled prevalence.
Methods: Based on the guideline of PRISMA, literature was searched in PubMed, Web of Science, and Embase. The prevalence of PTSD was estimated through a random model based on the different continents and levels of national income, as well as study majors, and compared with the pooled prevalence of PTSD among college students.
Results: Totally 381 articles were retrieved from electronic databases and 38 articles were included in the present meta-analysis. The results showed that the pooled prevalence of college students’ PTSD was 25% (95% CI: 21–28%). Prevalence estimates of PTSD among college students were statistically significant (p < 0.00001) when stratified with geographical regions, income levels, and study majors. In comparison with the pooled prevalence of PTSD (25%), subgroups of Africa and Europe, lower-middle-income countries, and medical college students possessed higher prevalence estimates.
Discussion: The findings of the study showed that the prevalence of PTSD in college students worldwide during COVID-19 was relatively high and varied in different continents and countries with different income levels. Therefore, healthcare providers should pay attention to the psychologically healthy condition of college students during COVID-19.
1. Introduction
Around 16 years after the severe acute respiratory syndrome (SARS), another pathogenic coronavirus, the coronavirus disease-2019 (COVID-19) emerged in Wuhan City (Hubei Province, China) in 2019. Due to the serious situation, the World Health Organization (WHO) declared COVID-19 a global pandemic on March 11, 2020 (Si et al., 2021). Since the declaration of the outbreak, many countries adopted strict policies to control the spread of COVID-19, such as lockdowns, home isolation, and social distancing. Reports suggested that stressful events such as natural disasters and man-made traumas exerted significant mental health impacts and could result in conditions such as posttraumatic stress disorder (PTSD) and depression (Kopala-Sibley et al., 2016; Plexousakis et al., 2019; Schwartz et al., 2019). However, public health authorities and healthcare researchers had paid more attention to the biological and physical effects rather than to the mental health implications of COVID-19.
Post-traumatic stress disorder is a chronic impairment disorder that often occurs after exposure to severe stressors, like combat, nature disaster, or other events (White et al., 2015). It is characterized by re-experience and avoidance symptoms as well as negative alterations in cognition and arousal (Miao et al., 2018). PTSD was first noticed by public during and after the military of the United States in Afghanistan and Iraq, and then a large number of relevant studies occurred in this field. However, underlying mechanisms of PTSD and specific treatment for it remain unclear. Therefore, due to the significant medical, social and even financial problems, PTSD is remarkable both for individuals and society, people suffering from PTSD or under traumatic exposure need to know about the risk and effects of PTSD.
Previous studies based on the SARS outbreak indicated that mental health problems were common among SARS survivors and authors referred to SARS as a “mental health catastrophe” (Maunder, 2009). Mak et al. (2009) reported that among 90 residents of Hong Kong who were infected with SARS and survived, 25.6% had PTSD and 15.6% had depressive disorders 30 months after infection. Another study by Leung et al. showed the trend of the population’s anxiety followed the trend of the number of daily new cases (Leung et al., 2005). One prospective cohort study on college students indicated that the prevalence of anxiety increased markedly in the early phase of the SARS but gradually reduced over time (Cheng and Cheung, 2005). And for now, the COVID-19 pandemic has brought into focus the mental health of affected populations, such as patients, medical staff, children, and older adults (Fu et al., 2021). Mental health of college students during COVID-19 pandemic were gradually of particular interest, as they experienced nationwide school closures, sudden change in students’ learning environment, loss of internships, on-campus jobs, and other opportunities (J. Lee et al., 2021). Chi et.al conducted a study among college students in mainland China during the beginning of COVID-19 and indicated that 30.8% (95% CI: 28.8–32.8%) of the participants presented relevant PTSD symptoms (Chi et al., 2020). Another survey conducted in the US found that among 2031 participants, 48.14% showed a moderate-to-severe level of depression, 38.48% showed a moderate-to-severe level of anxiety, and 18.04% had suicidal thoughts, the majority of participants (71.26%) indicated that their stress/anxiety levels had increased during the COVID-19 pandemic (Wang et al., 2020).
A growing number of researchers investigated the prevalence of PTSD among college students, and the reported prevalence ranged from 2.7 to 66.7% (Tang et al., 2020; Abdel-Aziz et al., 2022). But the overall prevalence of college students worldwide was deficient for raising awareness and providing appropriate interventions. In addition, the findings of these researches converged on the uptick of mental health issues among college students, but the contributing factors might not be generalizable to populations worldwide. As we observed the prevalence of PTSD varied among college students from different countries, and the most significant difference existed between students in Egypt (Africa, 66.7%) and China (Asia,2.7%; Tang et al., 2020; Abdel-Aziz et al., 2022). Thus, we inferred that factor like continents and national income participated in the different outcome of studies. In addition, previous studies had reported several mental health problems were high prevalent among medical students (Pacheco et al., 2017). Therefore, there was an urgent need to comprehensively assess the effects of the COVID-19 pandemic on mental health especially the prevalence of PTSD among college students.
Collectively, the present study aimed to provide a more accurate representation of PTSD in college students during the COVID-19 pandemic by performing meta-analyses by continents, national income, and study majors and comparing the results with estimated pooled prevalence, to assist policymakers to develop relative policies and help clinical practitioners to provide services to the affected populations in time.
2. Materials and methods
The present study was conducted following the Preferred Reporting Item for Systematic Reviews and Meta-analyses (PRISMA) statement. And the study protocol was registered in the PROSPERO (CRD42022382828) before data extraction.
2.1. Search strategy
Electronic databases including PubMed, Embase, and Web of Science databases were used for systematically searching for related literature that was published in English from March 2020 to September 2022. The keywords used for search strategies were as follows: “COVID-19” OR “SARS-CoV-2” AND “college students” or “university students” or “undergraduate students” or “bachelor students” or “graduate students” or “doctorate students” or “higher education students” AND “post-traumatic stress disorder” OR “PTSD.” Combinations of the above keywords were modified to optimize the search results in the databases. All of the included literature were screened manually to identify potential articles.
2.2. Inclusion and exclusion criteria
The EndNote X7 program (Clarivate Analytics, Philadelphia) was used to import and document articles, and duplications were first excluded. The preliminary screening was conducted by reading the titles and abstracts of the articles. After that, the articles were further screened by two independent reviewers (BH and XY) according to the inclusion and exclusion criteria. A third researcher (XT) was consulted to assist in the judgment in case of disagreement.
The inclusion criteria were as follows: (a) studies related to COVID-19; (b) studies published in English; (c) the study design included cross-sectional studies; (d) the study population consisted of college or university students; (e) the presence of PTSD was measured with clinical interviews or questionnaires according to DSM diagnostic criteria; and (f) studies containing a clear description of the prevalence of PTSD. The exclusion criteria were as follows: (a) the college or university students with mental illness already; (b) articles that were inconsistent with the study aim, re-published, books, editorials, conference abstracts, letters to the editors, viewpoints, case presentations, and brief communications; and (c) lacking sufficient data required to conduct the basic analysis.
2.3. Data extraction
The extracted data were as follows: (1) the first author of the study; (2) publication year; (3) the country surveyed; (4) study design; (5) sample size; (6) the assessment tools; (7) prevalence and standard error (SE); (8) relevant subgroup data. SE could be calculated using the formula SE= when SE value was not presented in the article, and P was the proportions of cases reported in the article, N was the sample size of the prevalence estimate. For a longitudinal study in our meta-analysis, we chose the prevalence surveyed during the COVID-19 pandemic.
2.4. Data analysis
Review Manager 5.4 (RevMan 5.4, The Cochrane Collaboration, London) was used to conduct the meta-analytic calculations. The pooled prevalence of PTSD, 95% confidence intervals (CI), Z-value, and heterogeneity test values were calculated, respectively. Heterogeneity was estimated by Cochran’s Q-test (Chi-square) and I2 statistics, a value of p of Chi-square < 0.10 indicated heterogeneity of the estimates of the prevalence rates, and I2 of 25, 50 and 75% indicated low, moderate and high heterogeneity, respectively. The random effect mode was used to account for expected heterogeneity between studies. For the source of heterogeneity, we conducted the subgroup analysis divided by the economic level of countries, majors of college students, and the continents. Finally, we used funnel plots to explore whether publication bias existed.
2.5. Quality assessment
The Joanna Briggs Inventory (JBI) Checklist was used to evaluate study quality by two researchers (BH and XY) independently. The quality was evaluated based on the following items: (a) sample frame; (b) sampling; (c) sample size; (d) description of subjects and setting; (e) sample coverage of the data analysis; (f) validity of the methods to identify the condition; (g) standardization and reliability of the methods to measure the con by the edition of all participants; (h) statistical analysis; and (i) response rate (Table 1). An item was scored ‘0’ when it was rated ‘no’, ‘unclear’, or ‘not applicable’, and was scored ‘1’ when it was rated ‘yes’. The overall scores ranged from 0 to 9, and the quality of the included eligible studies was assessed as follows: 0–3, 4–6, and 7–9 indicated a high, moderate, and low risk of bias, respectively. And when disagreements occurred in the assessments, they were resolved by another author (XT).
3. Results
3.1. Search results
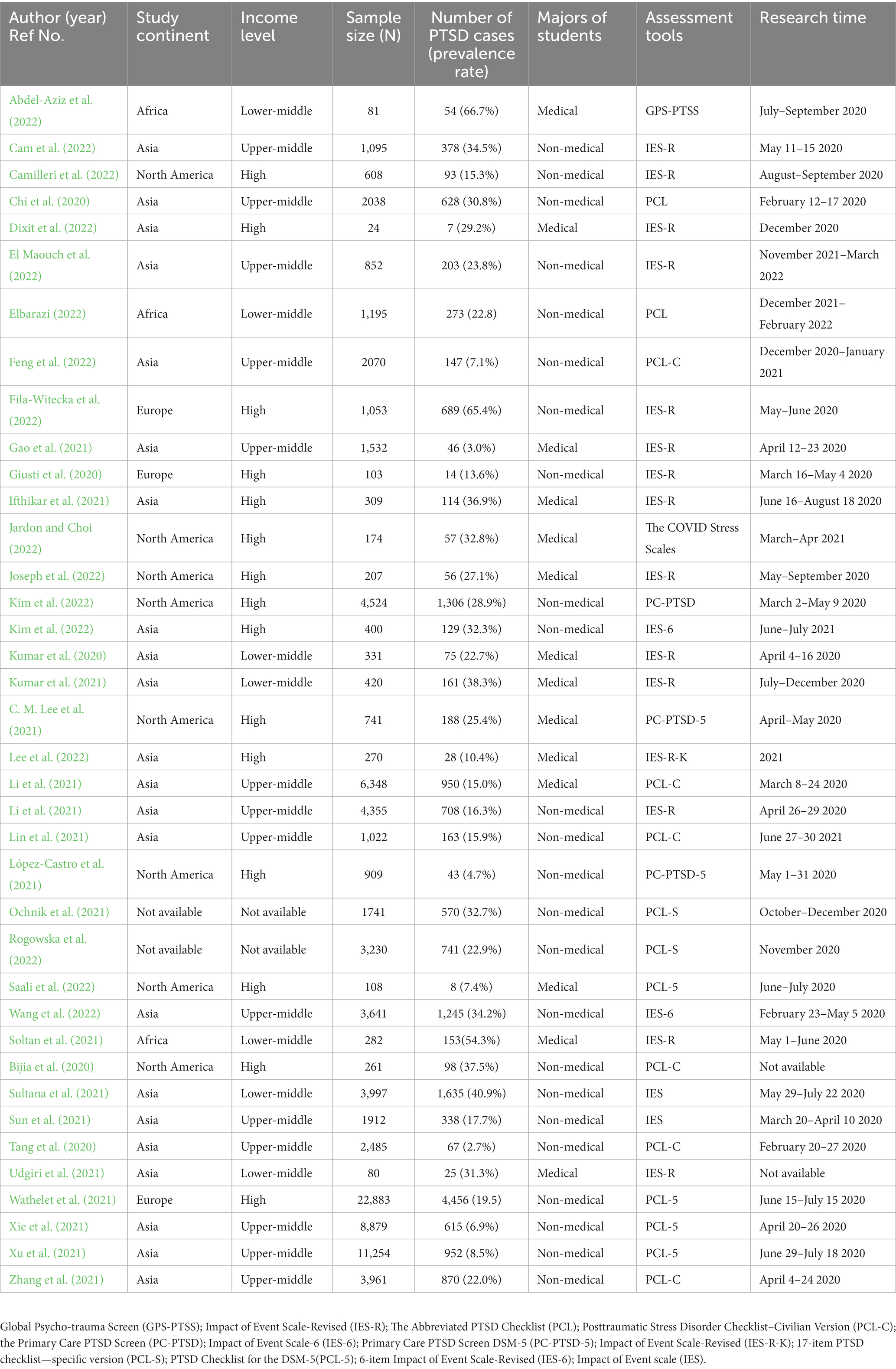
In total, 381 articles were retrieved from three electronic databases and then imported into the Endnote X7. After the removal of 146 duplications, 235 articles were next screened by two reviewers. By reading titles and abstracts, 137 articles were eliminated since they did not meet the inclusion criteria listed previously. Then 98 potential original articles were further screened by reading the full context and 60 articles were excluded because of the lack of detailed data mentioned in the inclusion criteria. Finally, 38 articles were included in the present meta-analysis (Figure 1).
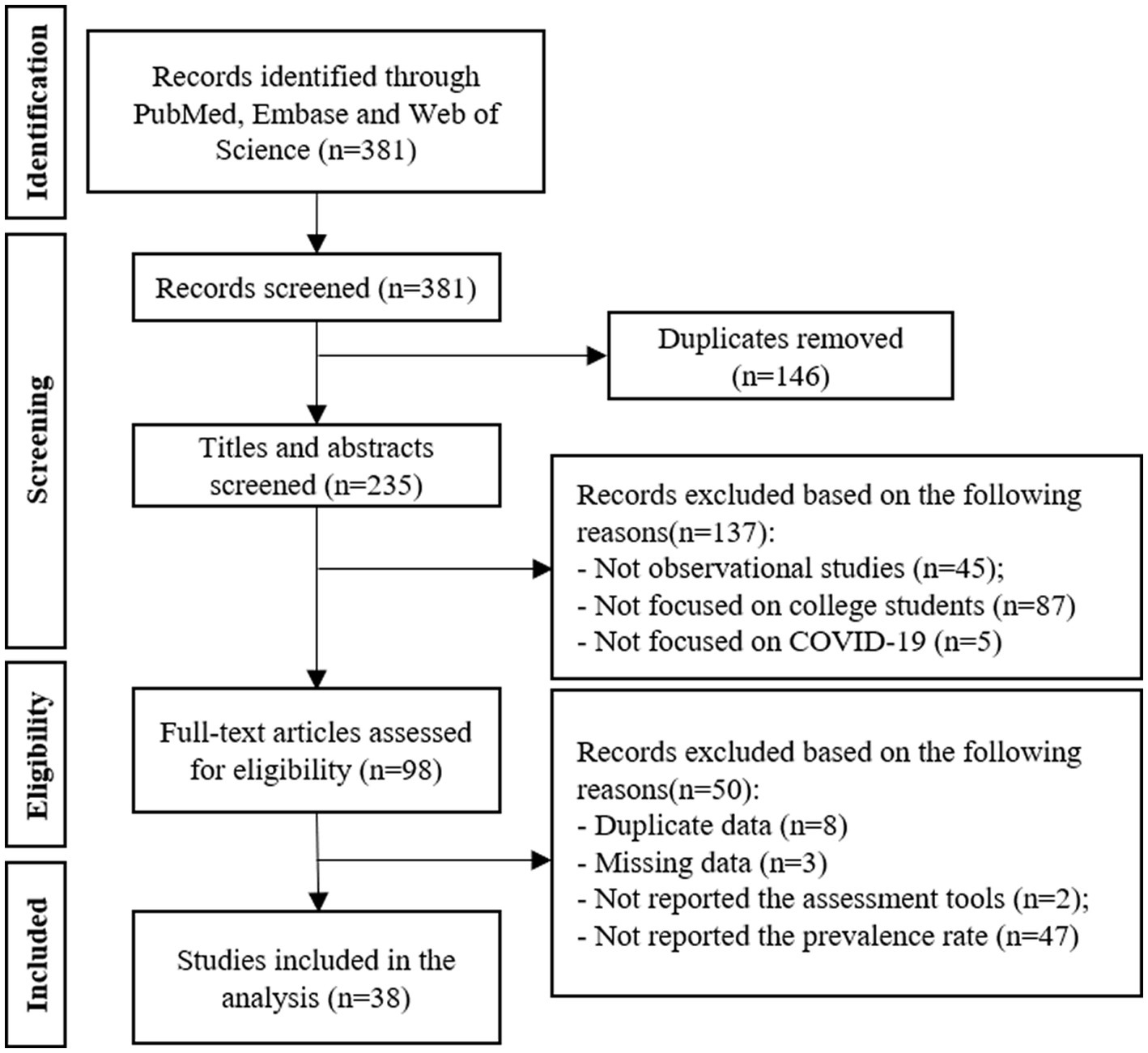
Figure 1. PRISMA flow diagram of the literature search strategy. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analyses. PTSD, post-traumatic stress disorders.
3.2. Study characteristics
The descriptive characteristics of the 38 included studies were presented in Table 2. Totally 95,375 college students were included in the present meta-analysis, and all of the included studies were cross-sectional studies. Included studies from 16 countries, that belonged to four continents (See Table 2). We extracted the information about mean age and standard deviation from all of the included studies if possible, and college students surveyed were at a similar age. For the assessment of PTSD, 14 studies used IES-R (Impact of Event Scale-Revised), six studies used PCL-C (Posttraumatic Stress Disorder Checklist—Civilian Version), four studies used PCL-5 (PTSD Checklist for the DSM-5), two studies used PCL (The Abbreviated PTSD Checklist), PC-PTSD (the Primary Care PTSD Screen), IES-6 (6-item Impact of Event Scale-Revised), PCL-S (17-item PTSD check list-specific version), and IES (Impact of Event scale) separately to assess PTSD. In addition, one study used GPS-PTSS (Global Psycho-trauma Screen), The COVID Stress Scale, PC-PTSD-5 (Primary Care PTSD Screen DSM-5), IES-R-K (Impact of Event Scale-Revised), respectively, to assess PTSD (See Table 2).
3.3. The pooled prevalence of PTSD
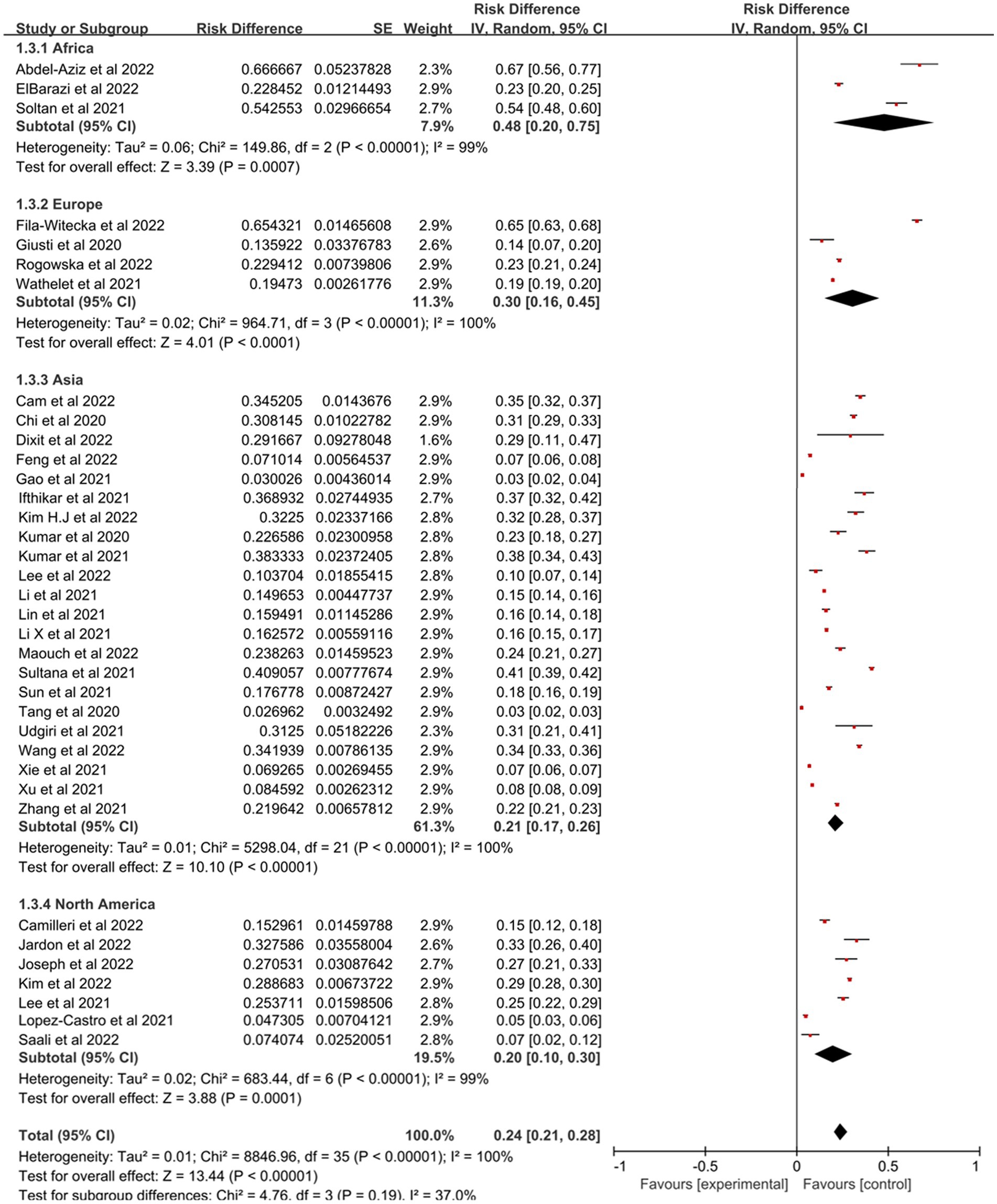
Figure 2 showed the forest plot for the complete dataset. Across the 38 studies with 95,375 college students, the pooled prevalence for all the students was 25% (N = 38, n = 95,375, 95% confidence interval: 21–28%) with high heterogeneity (I2 = 99.9%, p < 0.001).
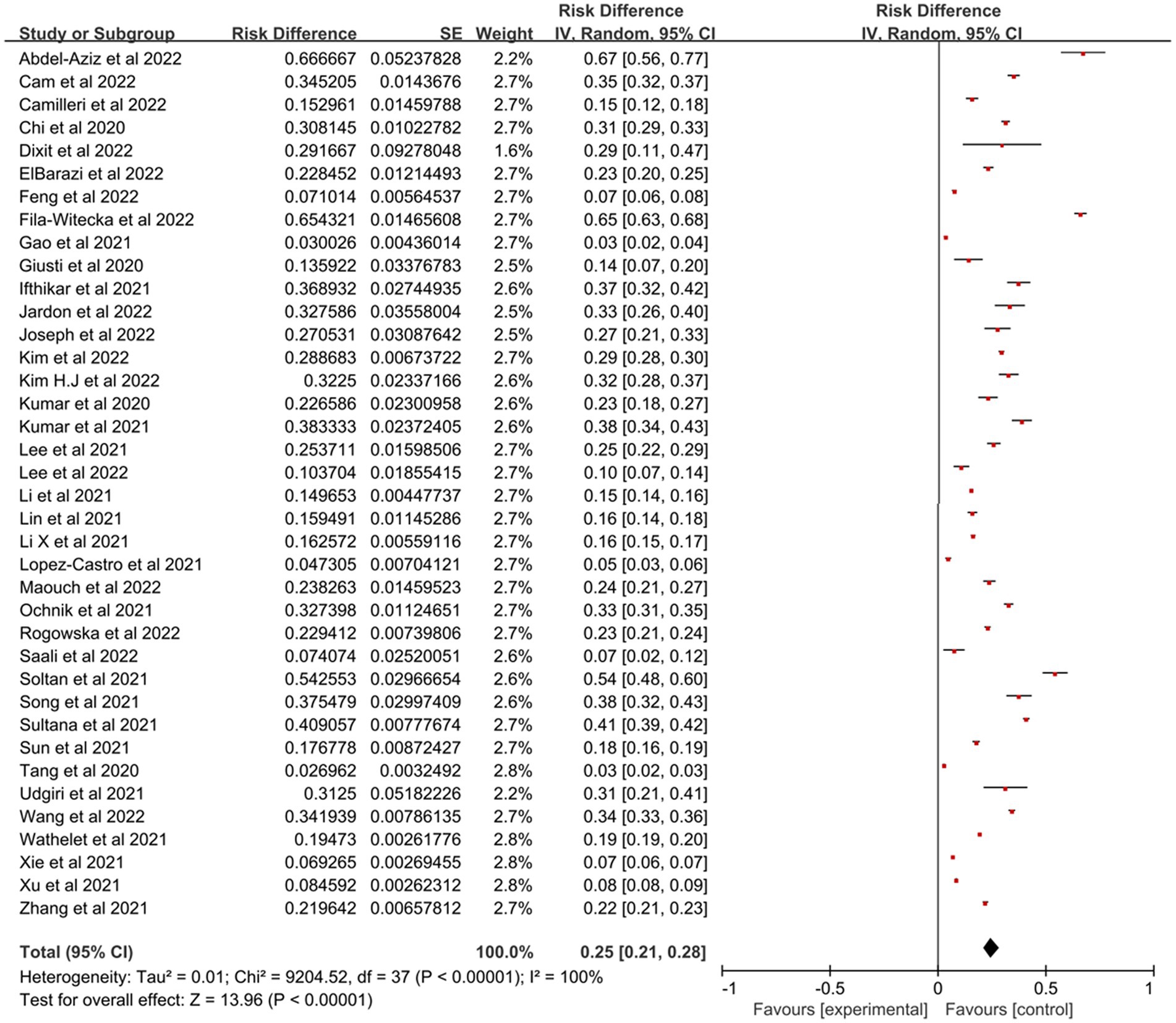
Figure 2. Forest plot showed the prevalence of PTSD among college students during the COVID-19 pandemic. CI, confidence intervals.
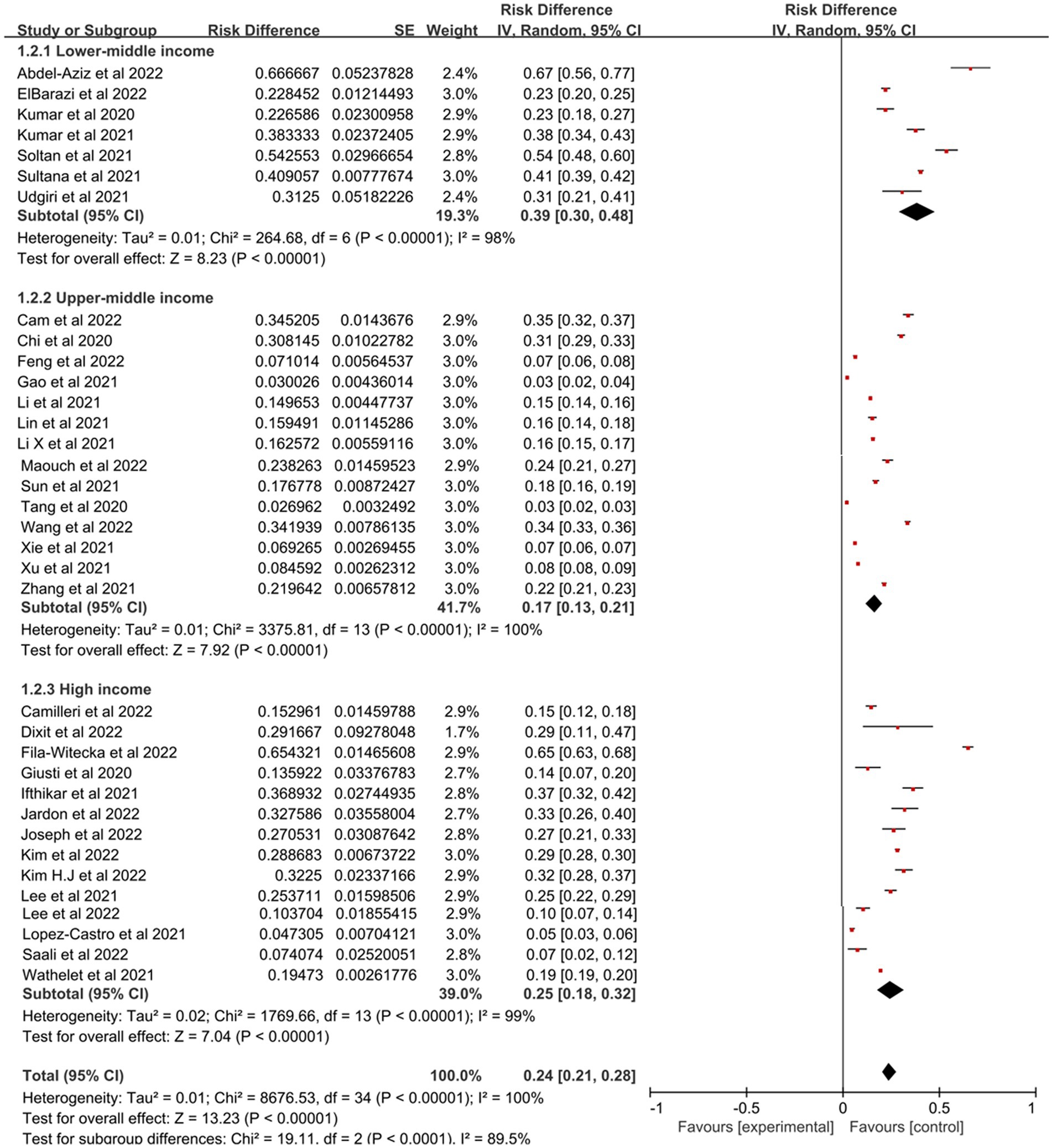
3.4. Subgroup analysis
Prevalence estimates of PTSD among college students were statistically significant (p < 0.00001) when stratified by geographical regions (Figure 3), with Africa having the highest prevalence (48, 95% CI: 20–75%), followed by Europe (30, 95% CI: 16–45%), Asia (21, 95% CI: 17–26%) and North America which was 20% (95% CI: 10–30%). Figure 4 represented the prevalence estimates of PTSD among college students were statistically significant (p < 0.00001) that were stratified by national income level, with lower-middle-income level having the highest prevalence (39, 95% CI:30–48%), followed by high-income level (25, 95% CI:18–32%) and upper-middle-income level which was 17% (95% CI:13–21%). Finally, in terms of study majors of college students, the prevalence estimates of PTSD among medical college students (28, 95% CI:21–35%) was higher than that of non-medical college students (23, 95% CI,19–28%; Figure 5). Collectively, in comparison with the pooled prevalence of PTSD (25%), subgroups of Africa and Europe, lower-middle-income countries and medical college students possessed higher prevalence estimates.
3.5. Quality assessment and publication bias
Assessment for the risk of bias ascertained for each article was listed in Table 1. Overall, the overall score ranged from 8 to 9 which indicated a low risk of bias. Publication bias was not observed among the analyses where it was possible to systematically assess publication bias using funnel plots (Supplementary Figure S1).
4. Discussion
To our knowledge, the present study is the first meta-analysis to investigate the prevalence of PTSD symptoms among college students worldwide during the COVID-19 pandemic. The pooled prevalence of PTSD during the COVID-19 pandemic is 25% (95%CI: 21–28%) in this study, compared with the prevalence in the general population ranging from 1 to 10%, and in college students ranging from 6 to 17% before the COVID-19 pandemic (Read et al., 2011). Higher prevalence can be explained by the decrease in face-to-face social interaction, long-time online learning, fear associated with the pandemic, and fewer opportunities to exercise for students during the COVID-19 pandemic (Feng et al., 2014; Nicola et al., 2020; Rogers et al., 2020). In all, the present study can be a great warning about the mental health of college students during the COVID-19 pandemic. Mental health care should not be, therefore, underestimated at present, especially for college students.
In this study, we observed that the prevalence of PTSD among college students on different continents varies from each other. The prevalence of PTSD among African college students is the highest (48%), while the prevalence among North American college students is the lowest (20%). With the rapidly increasing number of newly confirmed cases, three major factors are impacting the population and might lead to mental health problems: firstly, the direct impact of the disease, particularly near-death experiences during illness, and isolation from loved ones; secondly, restriction limits the social support and supply of food and medication; thirdly, uncertainty and stress resulting from loss of jobs and livelihoods (Semo and Frissa, 2020). Previous studies have reported significant differences in risk of acquiring COVID-19 between the continents, in which Asia and North America showed lower risks, and that lead to less direct or indirect impact of COVID-19 in North America and Asia (Sunjaya et al., 2022). Different social cultures, lifestyles, and political values in different continents might lead to the discrepant prevalence of PTSD among college students across continents. In addition, poor recognition of other outbreak-related epidemiologic terms might lead to passive attitudes to intervention strategies and measures (Zhang and Ba-Thein, 2022). It is also known that North America and Europe possess better medical condition than African, which partially interpret the difference of prevalence of PTSD among continents. Moreover, population density varies across continents, which also caused heterogeneity in the outcome. As Shuwiekh et al. (2022) have reported more densely populated countries like Egypt had a greater mental health impact than the countries with lower population density like Algeria and Saudi Arabia.
Factors like economic and income level also affect the spread of COVID-19 and its subsequent mental health impact like PTSD. Subgroup analyses based on the income levels (lower-middle income/upper-middle income/high-income) among countries indicate that the income levels of countries correlate with the prevalence of PTSD among college students. Lower-middle-income countries possess the highest prevalence since the reduction in household income is significantly associated with an increased risk of incident mental disorders (Sareen et al., 2011; Pieh et al., 2020). For example, it has been shown that lower socioeconomic status is linked to increased levels of PTSD and depression among people who have been exposed to trauma (Ochnik et al., 2021). Similarly, material assets are significantly related to mental health outcome, as the economic crises brought about by COVID-19 have markedly increased vulnerabilities to psychiatric symptomatology (Rudenstine et al., 2022). Moreover, the lower economic income can cause additional frustration due to incapable to cover the adequate need for supplies, medical attention and maintaining previous lifestyles, as indicated in previous studies on the consequences of quarantine (Alejandro-Salinas et al., 2022). A study based on family factors also has verified the relationship between the prevalence of PTSD and family background, which has shown university students from extremely poor families had the highest prevalence of PTSD, in contrast to the lowest level among students from wealthy families (Zhang et al., 2021). During the COVID-19 pandemic, some college students in developing countries like Pakistan, are unable to afford laptops because of electricity shortages and connectivity issues and may have apprehensions about their practical capabilities as a professional as they are unable to learn in hospitals through clinical rotations and internships (Gonzalo et al., 2009; Arima et al., 2020; Gallagher and Schleyer, 2020).
Finally, subgroup analysis that based on medical and non-medical students has shown, the prevalence of PTSD among medical college students during the COVID-19 pandemic is significantly higher than among non-medical college students. Related reasons are inferred as follows: first of all, medical students need to complete some on-site operation and internship courses in hospitals, but hospitals are key areas for epidemic control, which has caused more pressure on medical students. Then, in the process of fighting against COVID-19, the medical staff’s hard work and lack of corresponding supply guarantee in the early stage have made them go through a difficult period, which may have an impact on the medical students’ practice choice (Wang et al., 2022). Finally, during the period of isolation, separation from loved ones, loss of freedom, boredom and uncertainty about disease conditions may also bring psychological distress and disorder symptoms to medical staff.
The COVID-19 pandemic is one of the risk factors leading to college students’ psychological problems, which should be solved as an urgent matter of public health. Isolation and treatment of infected persons and possible expansion of the vaccination population are effective measures to control the COVID-19 pandemic (Frederiksen et al., 2020). Given that medical college students are more likely to suffer mental problems, we should give more attention to medical students and provide psychological support and material services to reduce their risk of developing PTSD and other mental problems. And for those who have suffered from PTSD, online and telephone support can be provided for help, since that has already been verified as an effective emergency measure in many countries. Popularizing medical knowledge about COVID-19 can also help reduce panic and the risk of mental problems among college students (Wang et al., 2020).
5. Conclusion
The objective of the meta-analysis was to assess the prevalence of PTSD in college students worldwide by continent and national income levels during the COVID-19 pandemic. The findings of our meta-analysis suggested that 25% of college students experienced PTSD during COVID-19, and the prevalence varied among different continents, different national income levels, and different study majors of college students. The highlighting of the high prevalence of college students’ PTSD, and comprehensive analysis of potential risk factors could help to raise caution among college students during COVID-19. To better understand the prevalence of PTSD among college students worldwide, future studies can use standard and reliable questionnaires to conduct surveys reasonably sampled from the world. Meanwhile, we should take measures to reduce the impact of the pandemic on people’s mental health urgently.
6. Limitation of the study and future direction
Limitations of our study must be noted to provide a better interpretation of the present study. Firstly, all of the included studies were cross-sectional studies, which might not provide sufficient evidence for the association between the COVID-19 pandemic and the increased prevalence of PTSD among college students. In addition, the heterogeneity of the studies included in our meta-analysis was relatively high, and heterogeneities of subgroup analysis based on the continents, national income and study major were also relatively high. However, the present study included 95,375 college students, which was quite a large sample for meta-analysis to assess the pooled prevalence of PTSD among college students worldwide, and might not affect the overall prevalence of PTSD among college students.
The results of the study highlighted the need for future research to pay attention to mental health of vulnerable population (such as patients, children, pregnant women and college students) after exposure to emergent events of public health. Additionally, further study is needed to determine the effects of the COVID-19 on college students’ mental health and well-being in its later phases rather than the peak period. Based on relative studies during the SARS outbreak, the effects of the COVID-19 on students might linger for a time beyond the peak of the COVID-19 itself (McAlonan et al., 2007).
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XT designed the methodology of the study, supervised and performed article screening, data extraction, statistical analyses, critically reviewed and revised the manuscript, and accepted responsibility for the integrity of the data analyzed. XY and BH performed article screening, data extraction, and statistical analyses and drafted the manuscript. All authors had read and approved the final version of the manuscript to be submitted.
Acknowledgments
We thank all authors of the eligible articles.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1129782/full#supplementary-material
References
Abdel-Aziz, S. B., Emadeldin, M., Al Hanafy, S. H., and Amin, T. T. (2022). Mental health outcomes and psychological support among university students during the COVID-19 pandemic in Egypt. Open Access Maced. J. Med. Sci. 10, 1248–1254. doi: 10.3889/oamjms.2022.6930
Alejandro-Salinas, R., Rojas-Cueva, A. C., Visconti-Lopez, F. J., Osorio-Martinez, M. L., and Toro-Huamanchumo, C. J. (2022). Factors associated with post-traumatic stress disorder symptoms in the post-quarantine context of the COVID-19 pandemic in Peruvian medical students. Heliyon 8:e09446. doi: 10.1016/j.heliyon.2022.e09446
Arima, M., Takamiya, Y., Furuta, A., Siriratsivawong, K., Tsuchiya, S., and Izumi, M. (2020). Factors associated with the mental health status of medical students during the COVID-19 pandemic: a cross-sectional study in Japan. BMJ Open 10:e043728. doi: 10.1136/bmjopen-2020-043728
Bijia, S., Yilin, Z., and Junchao, Z. (2020). COVID-19-related traumatic effects and psychological reactions among international students. J. Epidemiol. Global Health 11, 117–123. doi: 10.2991/jegh.k.201016.001
Cam, H. H., Ustuner Top, F., and Kuzlu Ayyildiz, T. (2022). Impact of the COVID-19 pandemic on mental health and health-related quality of life among university students in Turkey. Curr. Psychol. 41, 1033–1042. doi: 10.1007/s12144-021-01674-y
Camilleri, C., Fogle, C. S., O'Brien, K. G., and Sammut, S. (2022). The impact of COVID-19 and associated interventions on mental health: a cross-sectional study in a sample of university students. Front. Psychol. 12:801859. doi: 10.3389/fpsyt.2021.801859
Cheng, C., and Cheung, M. W. (2005). Psychological responses to outbreak of severe acute respiratory syndrome: a prospective, multiple time-point study. J. Pers. 73, 261–285. doi: 10.1111/j.1467-6494.2004.00310.x
Chi, X., Becker, B., Yu, Q., Willeit, P., Jiao, C., Huang, L., et al. (2020). Prevalence and psychosocial correlates of mental health outcomes among Chinese college students during the coronavirus disease (COVID-19) pandemic. Front. Psychol. 11:803. doi: 10.3389/fpsyt.2020.00803
Dixit, S., Musa, A., Sillva, A. B., Reddy, R. S., Abohashrh, M., Kakaraparthi, V. N., et al. (2022). The impact of post-traumatic stress of SARS-CoV-2 affliction on psychological and mental health of student survivors: cross sectional study. Front. Public Health 10:845741. doi: 10.3389/fpubh.2022.845741
El Maouch, M., Wang, Y., Jin, Z., Tamunang Tamutana, T., Zhao, K., and Liu, Y. (2022). Activity system, schizotypal personality, and mentalization: a study between halted activity and COVID-19 conducted in Henan, China. Front. Public Health 10:930842. doi: 10.3389/fpubh.2022.930842
Elbarazi, A. S. (2022). Post-traumatic stress disorder and difficulties in emotion regulation among university students under the COVID-19 condition. J. Evid.-Based Psychother. 22, 87–102. doi: 10.24193/jebp.2022.1.5
Feng, J., Lau, P. W. C., Shi, L., and Huang, W. Y. (2022). Movement behaviors and posttraumatic stress disorder during the COVID-19 pandemic: a retrospective study of Chinese university students. J. Exerc. Sci. Fit. 20, 263–268. doi: 10.1016/j.jesf.2022.05.002
Feng, Q., Zhang, Q. L., Du, Y., Ye, Y. L., and He, Q. Q. (2014). Associations of physical activity, screen time with depression, anxiety and sleep quality among Chinese college freshmen. PLoS One 9:e100914. doi: 10.1371/journal.pone.0100914
Fila-Witecka, K., Malecka, M., Senczyszyn, A., Wieczorek, T., Wieckiewicz, M., Szczesniak, D., et al. (2022). Sleepless in solitude-insomnia symptoms severity and psychopathological symptoms among university students during the COVID-19 pandemic in Poland. Int. J. Environ. Res. Public Health 19:2551. doi: 10.3390/ijerph19052551
Frederiksen, L. S. F., Zhang, Y., Foged, C., and Thakur, A. (2020). The long road toward COVID-19 herd immunity: vaccine platform technologies and mass immunization strategies. Front. Immunol. 11:1817. doi: 10.3389/fimmu.2020.01817
Fu, W., Yan, S., Zong, Q., Anderson-Luxford, D., Song, X., Lv, Z., et al. (2021). Mental health of college students during the COVID-19 epidemic in China. J. Affect. Disord. 280, 7–10. doi: 10.1016/j.jad.2020.11.032
Gallagher, T. H., and Schleyer, A. M. (2020). "we signed up for this!"–student and trainee responses to the Covid-19 pandemic. N. Engl. J. Med. 382:e96. doi: 10.1056/NEJMp2005234
Gao, J., Wang, F., Guo, S., and Hu, F. (2021). Mental health of nursing students amid coronavirus disease 2019 pandemic. Front. Psychol. 12:699558. doi: 10.3389/fpsyg.2021.699558
Giusti, L., Salza, A., Mammarella, S., Bianco, D., Ussorio, D., Casacchia, M., et al. (2020). #everything will be fine. Duration of home confinement and "all-or-nothing" cognitive thinking style as predictors of traumatic distress in young university students on a digital platform during the COVID-19 Italian lockdown. Front. Psychol. 11. doi: 10.3389/fpsyt.2020.574812
Gonzalo, J. D., Masters, P. A., Simons, R. J., and Chuang, C. H. (2009). Attending rounds and bedside case presentations: medical student and medicine resident experiences and attitudes. Teach. Learn. Med. 21, 105–110. doi: 10.1080/10401330902791156
Ifthikar, Z., Fakih, S. S., Johnson, S., and Alex, J. (2021). Post-traumatic stress disorder following COVID-19 pandemic among medical students in Riyadh: a cross-sectional study. Middle East Curr. Psychiatr. 28:44. doi: 10.1186/s43045-021-00127-3
Jardon, C., and Choi, K. R. (2022). COVID-19 experiences and mental health among graduate and undergraduate nursing students in Los Angeles. J. Am. Psychiatr. Nurses Assoc. :107839032110722. doi: 10.1177/10783903211072222
Joseph, R. A., Turner, T., Lee, C., Akers, S. W., Whorley, E., and Goodrich, C. (2022). Impact of COVID-19 on nursing students: factors associated with PTSD risk. J. Christ. Nurs. 39, 250–257. doi: 10.1097/cnj.0000000000000951
Kim, H., Rackoff, G. N., Fitzsimmons-Craft, E. E., Shin, K. E., Zainal, N. H., Schwob, J. T., et al. (2022). College mental health before and during the COVID-19 pandemic: results from a Nationwide survey. Cognit Ther. Res. 46, 1–10. doi: 10.1007/s10608-021-10241-5
Kopala-Sibley, D. C., Danzig, A. P., Kotov, R., Bromet, E. J., Carlson, G. A., Olino, T. M., et al. (2016). Negative emotionality and its facets moderate the effects of exposure to hurricane Sandy on children's postdisaster depression and anxiety symptoms. J. Abnorm. Psychol. 125, 471–481. doi: 10.1037/abn0000152
Kumar, R., Kumar, H., Kumari, R., Dars, J., Qureshi, S., Hamza, M. A., et al. (2021). The impact of covid-19 on medical students: a cross sectional survey. Pak. J. Med. Health Sci. 15, 2905–2909. doi: 10.53350/pjmhs2115112905
Kumar, A., Kumar, A., Shrama, D., Sharma, S., Bansal, R., Shukla, A., et al. (2020). The psychological impact of the Covid-19 lockdown on medical students of a College in North India. Indian J. Public Health Res. Dev. 11, 82–87. doi: 10.37506/ijphrd.v11i10.11118
Lee, C. M., Juarez, M., Rae, G., Jones, L., Rodriguez, R. M., Davis, J. A., et al. (2021). Anxiety, PTSD, and stressors in medical students during the initial peak of the COVID-19 pandemic. PLoS One 16:e0255013. doi: 10.1371/journal.pone.0255013
Lee, J., Lee, S. J., Chang, S. M., Won, S., Woo, J., and Kim, B. S. (2022). Association of Sociodemographic and Psychosocial Factors with COVID-19-related post-traumatic stress disorder risk group among medical students. Psychiatry Investig. 19, 676–686. doi: 10.30773/pi.2022.0080
Lee, J., Solomon, M., Stead, T., Kwon, B., and Ganti, L. (2021). Impact of COVID-19 on the mental health of US college students. BMC Psychol. 9:95. doi: 10.1186/s40359-021-00598-3
Leung, G. M., Ho, L. M., Chan, S. K., Ho, S. Y., Bacon-Shone, J., Choy, R. Y., et al. (2005). Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clin. Infect. Dis. 40, 1713–1720. doi: 10.1086/429923
Li, X., Fu, P., Fan, C., Zhu, M., and Li, M. (2021). COVID-19 stress and mental health of students in locked-down colleges. Int. J. Environ. Res. Public Health 18, 1–12. doi: 10.3390/ijerph18020771
Li, D., Zou, L., Zhang, Z., Zhang, P., Zhang, J., Fu, W., et al. (2021). The psychological effect of COVID-19 on home-quarantined nursing students in China. Front. Psychol. 12:652296. doi: 10.3389/fpsyt.2021.652296
Lin, Z., Zhang, X., Chen, L., Feng, D., Liu, N., and Chen, Z. (2021). Impact of middle- and long-distance running on mental health in college students in Guangzhou during COVID-19 outbreak. Nan Fang Yi Ke Da Xue Xue Bao 41, 1864–1869. doi: 10.12122/j.issn.1673-4254.2021.12.16
López-Castro, T., Brandt, L., Anthonipillai, N. J., Espinosa, A., and Melara, R. (2021). Experiences, impacts and mental health functioning during a COVID-19 outbreak and lockdown: data from a diverse New York City sample of college students. PLoS One 16:e0249768. doi: 10.1371/journal.pone.0249768
Mak, I. W., Chu, C. M., Pan, P. C., Yiu, M. G., and Chan, V. L. (2009). Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry 31, 318–326. doi: 10.1016/j.genhosppsych.2009.03.001
Maunder, R. G. (2009). Was SARS a mental health catastrophe? Gen. Hosp. Psychiatry 31, 316–317. doi: 10.1016/j.genhosppsych.2009.04.004
McAlonan, G. M., Lee, A. M., Cheung, V., Cheung, C., Tsang, K. W., Sham, P. C., et al. (2007). Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can. J. Psychiatr. 52, 241–247. doi: 10.1177/070674370705200406
Miao, X. R., Chen, Q. B., Wei, K., Tao, K. M., and Lu, Z. J. (2018). Posttraumatic stress disorder: from diagnosis to prevention. Mil. Med. Res. 5:32. doi: 10.1186/s40779-018-0179-0
Nicola, M., Alsafi, Z., Sohrabi, C., Kerwan, A., Al-Jabir, A., Iosifidis, C., et al. (2020). The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int. J. Surg. 78, 185–193. doi: 10.1016/j.ijsu.2020.04.018
Ochnik, D., Rogowska, A. M., Kuśnierz, C., Jakubiak, M., Wierzbik-Strońska, M., Schütz, A., et al. (2021). Exposure to COVID-19 during the first and the second wave of the pandemic and coronavirus-related PTSD risk among university students from six countries-a repeated cross-sectional study. J. Clin. Med. 10. doi: 10.3390/jcm10235564
Pacheco, J. P., Giacomin, H. T., Tam, W. W., Ribeiro, T. B., Arab, C., Bezerra, I. M., et al. (2017). Mental health problems among medical students in Brazil: a systematic review and meta-analysis. Braz. J. Psychiatr. 39, 369–378. doi: 10.1590/1516-4446-2017-2223
Pieh, C., Budimir, S., and Probst, T. (2020). The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 136:110186. doi: 10.1016/j.jpsychores.2020.110186
Plexousakis, S. S., Kourkoutas, E., Giovazolias, T., Chatira, K., and Nikolopoulos, D. (2019). School bullying and post-traumatic stress disorder symptoms: the role of parental bonding. Front. Public Health 7:75. doi: 10.3389/fpubh.2019.00075
Read, J. P., Ouimette, P., White, J., Colder, C., and Farrow, S. (2011). Rates of DSM-IV-TR trauma exposure and posttraumatic stress disorder among newly matriculated college students. Psychol. Trauma 3, 148–156. doi: 10.1037/a0021260
Rogers, J. P., Chesney, E., Oliver, D., Pollak, T. A., McGuire, P., Fusar-Poli, P., et al. (2020). Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 7, 611–627. doi: 10.1016/s2215-0366(20)30203-0
Rogowska, A. M., Kuśnierz, C., Pavlova, I., and Chilicka, K. (2022). A path model for subjective well-being during the second wave of the COVID-19 pandemic: a comparative study among polish and Ukrainian university students. J. Clin. Med. 11. doi: 10.3390/jcm11164726
Rudenstine, S., Bhatt, K., Schulder, T., McNeal, K., Ettman, C. K., and Galea, S. (2022). Examining the role of material and social assets on mental health in the context of COVID-19 among an urban public university sample. Psychol. Trauma 15, 483–492. doi: 10.1037/tra0001307
Saali, A., Stanislawski, E. R., Kumar, V., Chan, C., Hurtado, A., Pietrzak, R. H., et al. (2022). The psychiatric burden on medical students in New York City entering clinical clerkships during the COVID-19 pandemic. Psychiatr. Q. 93, 419–434. doi: 10.1007/s11126-021-09955-2
Sareen, J., Afifi, T. O., McMillan, K. A., and Asmundson, G. J. (2011). Relationship between household income and mental disorders: findings from a population-based longitudinal study. Arch. Gen. Psychiatry 68, 419–427. doi: 10.1001/archgenpsychiatry.2011.15
Schwartz, R. M., Rasul, R., Gargano, L. M., Lieberman-Cribbin, W., Brackbill, R. M., and Taioli, E. (2019). Examining associations between hurricane Sandy exposure and posttraumatic stress disorder by Community of Residence. J. Trauma. Stress. 32, 677–687. doi: 10.1002/jts.22445
Semo, B. W., and Frissa, S. M. (2020). The mental health impact of the COVID-19 pandemic: implications for sub-Saharan Africa. Psychol. Res. Behav. Manag. 13, 713–720. doi: 10.2147/prbm.s264286
Shuwiekh, H. A. M., Kira, I. A., Sous, M. S. F., Ashby, J. S., Alhuwailah, A., Baali, S. B. A., et al. (2022). The differential mental health impact of COVID-19 in Arab countries. Curr. Psychol. 41, 5678–5692. doi: 10.1007/s12144-020-01148-7
Si, M. Y., Su, X. Y., Jiang, Y., Wang, W. J., Gu, X. F., Ma, L., et al. (2021). Prevalence and predictors of PTSD during the initial stage of COVID-19 epidemic among female college students in China. Inquiry 58:469580211059953. doi: 10.1177/00469580211059953
Soltan, M. R., Soliman, S. S., and Dawoud, M. E. (2021). A study of anxiety, depression and stress symptoms among Fayoum medical students during COVID-19 lockdown, Egypt. Egypt J. Neurol. Psychiatr. Neurosurg. 57:123. doi: 10.1186/s41983-021-00377-2
Sultana, M. S., Khan, A. H., Hossain, S., Ansar, A., Sikder, M. T., and Hasan, M. T. (2021). Prevalence and predictors of post-traumatic stress symptoms and depressive symptoms among Bangladeshi students during COVID-19 mandatory home confinement: a nationwide cross-sectional survey. Child Youth Serv. Rev. 122:105880. doi: 10.1016/j.childyouth.2020.105880
Sun, S., Goldberg, S. B., Lin, D., Qiao, S., and Operario, D. (2021). Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Glob. Health 17:15. doi: 10.1186/s12992-021-00663-x
Sunjaya, A. P., Allida, S. M., Di Tanna, G. L., and Jenkins, C. R. (2022). Asthma and COVID-19 risk: a systematic review and meta-analysis. Eur. Respir. J. 59:2101209. doi: 10.1183/13993003.01209-2021
Tang, W., Hu, T., Hu, B., Jin, C., Wang, G., Xie, C., et al. (2020). Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 274, 1–7. doi: 10.1016/j.jad.2020.05.009
Udgiri, R. S., Biradar, S. G., and Shannawaz, M. (2021). Assessing impact event scale of post-traumatic stress disorder of covid-19 pandemic among postgraduates working at tertiary care hospital — a cross-sectional study. Journal of the Indian Medical Association, 119, 19–23.
Wang, X., Hegde, S., Son, C., Keller, B., Smith, A., and Sasangohar, F. (2020). Investigating mental health of US College students during the COVID-19 pandemic: cross-sectional survey study. J. Med. Internet Res. 22:e22817. doi: 10.2196/22817
Wang, H., Si, M. Y., Su, X. Y., Huang, Y. M., Xiao, W. J., Wang, W. J., et al. (2022). Mental health status and its influencing factors among college students during the epidemic of coronavirus disease 2019:a multi-center cross-sectional study. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 44, 30–39. doi: 10.3881/j.issn.1000-503X.14144
Wang, Z. H., Yang, H. L., Yang, Y. Q., Liu, D., Li, Z. H., Zhang, X. R., et al. (2020). Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: a large cross-sectional study. J. Affect. Disord. 275, 188–193. doi: 10.1016/j.jad.2020.06.034
Wathelet, M., Fovet, T., Jousset, A., Duhem, S., Habran, E., Horn, M., et al. (2021). Prevalence of and factors associated with post-traumatic stress disorder among French university students 1 month after the COVID-19 lockdown. Transl. Psychiatry 11:327. doi: 10.1038/s41398-021-01438-z
White, J., Pearce, J., Morrison, S., Dunstan, F., Bisson, J. I., and Fone, D. L. (2015). Risk of post-traumatic stress disorder following traumatic events in a community sample. Epidemiol. Psychiatr. Sci. 24, 249–257. doi: 10.1017/s2045796014000110
Xie, X., Zhu, K., Xue, Q., Zhou, Y., Liu, Q., Wu, H., et al. (2021). Problematic internet use was associated with psychological problems among university students during COVID-19 outbreak in China. Front. Public Health 9:675380. doi: 10.3389/fpubh.2021.675380
Xu, Y., Su, S., Jiang, Z., Guo, S., Lu, Q., Liu, L., et al. (2021). Prevalence and risk factors of mental health symptoms and suicidal behavior among university students in Wuhan, China during the COVID-19 pandemic. Front. Psychol. 12:695017. doi: 10.3389/fpsyt.2021.695017
Zhang, D., and Ba-Thein, W. (2022). COVID-19 epidemic and Chinese medical students: perception, emotions, attitudes, and conformity during domicile quarantine. J. Infect. Dev. Ctries. 16, 41–48. doi: 10.3855/jidc.14328
Keywords: PTSD, college students, mental health, COVID-19, meta-analysis
Citation: Hu B, Yang X and Tuo X (2023) The prevalence of post-traumatic stress disorder in college students by continents and national income during the COVID-19 pandemic: a meta-analysis. Front. Psychol. 14:1129782. doi: 10.3389/fpsyg.2023.1129782
Edited by:
Quan Zhuang, Central South University, ChinaReviewed by:
John Mark R. Asio, Gordon College, PhilippinesNaresh Poondla, Icahn School of Medicine at Mount Sinai, United States
Joanna Baj-Korpak, John Paul II University of Applied Sciences in Biala Podlaska, Poland
Copyright © 2023 Hu, Yang and Tuo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoqian Tuo, aXNsYW5kMTk5NDAzMzFAc3R1LnhqdHUuZWR1LmNu
 Biao Hu1
Biao Hu1 Xiaoqian Tuo
Xiaoqian Tuo