- 1Zhejiang Rehabilitation Medical Center, Hangzhou, Zhejiang, China
- 2School of Teacher Education, Taizhou University, Taizhou, Zhejiang, China
Objective: The psychological problems among Chinese parents of special children (mental retardation, limb disorder, hearing impairment, autism, cerebral palsy and other types) should be paid more attention. The aim of this study was to investigate the association between anxiety, social support, coping style and sleep quality among Chinese parents of special children during the early COVID-19 epidemic, so as to provide more help for the mental health of parents of special children scientifically and effectively.
Method: A total of 305 Chinese parents of special children were invited to accomplish four questionnaires. Anxiety was measured by the Self-Rating Anxiety Scale, social support was evaluated by the Perceived Social Support Scale, sleep quality was assessed by the Pittsburgh Sleep Quality Index, and coping style was measured by the Simplified Coping Style Questionnaire.
Results: This study revealed that anxiety was positively correlated with sleep quality (p < 0.01) and negatively correlated with social support (p < 0.01) and coping style (p < 0.01). Sleep quality was negatively correlated with social support (p < 0.01), but not significantly correlated with coping style (p > 0.05). Social support was positively correlated with coping style (p < 0.01). The study confirmed that social support had a partial mediating effect on the relationship between anxiety and sleep quality.
Conclusion: The anxiety of parents of special children not only directly affects sleep quality, but also indirectly affects sleep quality through social support. Social support can alleviate the impact of anxiety on sleep quality through the mediating role.
Introduction
Sleep quality which is always recognized as a very important physical and mental health index has been widely discussed (American Psychiatric Association, 2013). For example, studies found that lower sleep quality and sleep duration increase the risk of being overweight and obese (Parvaneh et al., 2016). Sleep disturbance is strongly associated with periodontitis, cardiovascular diseases and some cancers (Alqaderi et al., 2020). Lack of sleep leads to decreased work efficiency (Morgan, 1974), and poor sleep quality impairs emotion regulation and contributes depression symptoms (O'Leary et al., 2016). There are intertwined relationships discussed among sleep quality, physiological and psychological factors (Mohammadkhani et al., 2019; Taheri et al., 2019). Many studies have shown that parents of special children (mentally disabled children) have sleep problems. Parents of children with ASDs (autism spectrum disorders) reported poorer sleep quality compared to the TD (typically developing) group (Meltzer, 2008). Parents of children with developmental disabilities reported poorer sleep quality than parents of normal children (Gallagher et al., 2010). Children with neurodevelopmental disorders and their parents reported more severe sleep disturbances (sleep quality, insomnia symptoms and sleep efficiency) than typically developing children and their parents (Varma et al., 2021). Therefore, the quality of sleep has a big impact on body and mental health, and it is necessary to carry out further study for clarifying sleep quality related to mental health among parents of special children.
Which psychological factors affect sleep quality? Studies have shown that anxiety affects sleep quality. Most of studies have found a significant correlation between anxiety and sleep quality, and anxiety is a significant predictor of sleep quality (Augner, 2011; Liu et al., 2021; Simonetti et al., 2021; Yin et al., 2021). Many studies also have shown that social support is related to sleep quality (Brummett et al., 2006; Nordin et al., 2012; Guo et al., 2014; Marini et al., 2020; Mitchell et al., 2022). Some Studies have found positive coping style was negatively correlated with sleep quality (Kong et al., 2021) or not (Zhao et al., 2006), while negative coping style was positively correlated with sleep quality (Kong et al., 2021; Xue et al., 2012) or not (Zhou et al., 2013). In addition, studies have shown a correlation between anxiety and social support, coping style (Wu, 2010; Ma, 2013; Chen et al., 2016; Taş, 2019).
So, previous studies have found that anxiety, social support, coping style and sleep quality are related to each other. In addition, many studies have shown that the COVID-19 epidemic will affect individual sleep, anxiety and other mental health (Stanton et al., 2020; Qiu et al., 2021; Chatterjee, 2022). Studies have explored the psychometric relationship among these related variables, but the mediating role of social support and coping style between anxiety and sleep quality has been explored very rarely. How social support and coping style mediate the association between anxiety and sleep quality? Besides, selecting subjects of previous relevant studies mainly focus on college students.
Based on existing theories and researches, this study speculated that social support and coping style mediate the relationship between anxiety and sleep quality, and selected Chinese parents of special children as the psychological measurement subjects. The purpose of this study was to investigate the deep relationship among anxiety, social support, sleep quality and coping style of parents with special children, so as to provide some theoretical and practical proofs for the mental health of parents with special children during the COVID-19 epidemic period.
Methods
Participants
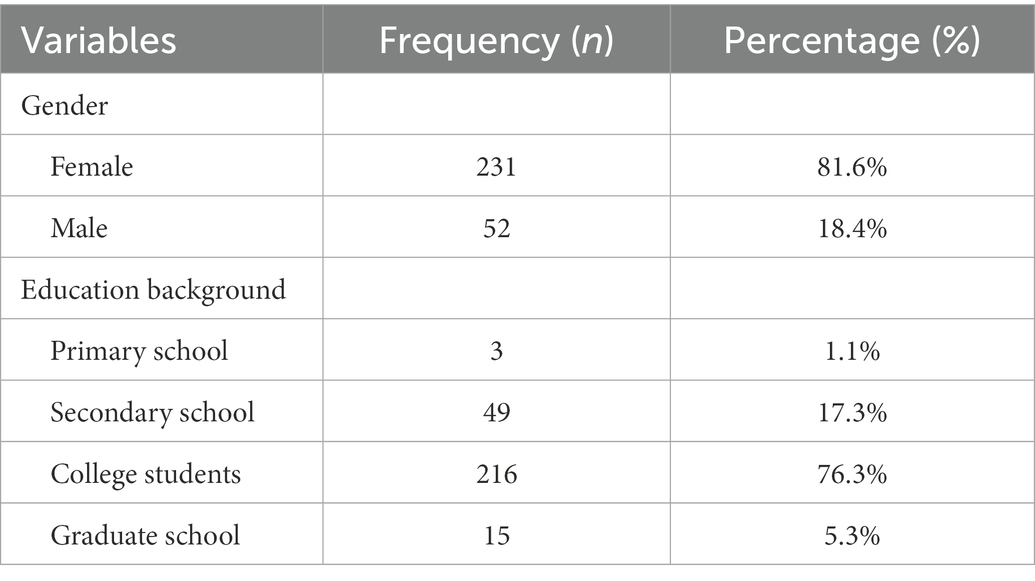
The Participants of this survey study were Chinese parents of special children refer to mental retardation, limb disorder, hearing impairment, autism, cerebral palsy and other types. This study conducted an online questionnaire to parents of special children in Hangzhou Green Apple Kindergarten in March 2020. A total of 305 questionnaires were distributed. After excluding missing data, a total of 283 questionnaires were included in this study. Two hundred eighty-three participants information see Table 1, and the study flow chart see Figure 1.
Measurement tools
Self-rating anxiety scale
Anxiety was assessed with a 20-item Self-Rating Anxiety Scale by Zung (the scale derived from handbook: Wang et al., 1999). Ratings were made a 4-point Scale. Cronbach’s α of the scale in this study was 0.817. Confirmatory factor analysis indicated that the validity of this scale was good (χ2 =376.244; χ2/df = 2.650; p < 0.001; GFI=0.874; NFI=0.803; IFI=0.867; TLI = 0.817; CFI = 0.864; RMSEA = 0.076).
Perceived social support scale
Social support was assessed with a Chinese revised version of Perceived Social Support Scale by Qianjin Jiang (the scale derived from handbook: Wang et al., 1999). The 12 items were rated on a 7-point Likert scale, ranging from 1 for strongly disagree to 7 for strongly agree with higher scores indicating greater social support. The Perceived Social Support Scale consists of three subscales: family support, friend support and significant others support. Cronbach’s α of the scale in this study was 0.932. Confirmatory factor analysis indicated that the validity of this scale was good (χ2 =122.376; χ2/df = 2.781; p < 0.001; GFI=0.935; NFI=0.949; IFI=0.966; TLI = 0.949; CFI = 0.966; RMSEA = 0.079).
Simplified coping style questionnaire
Coping style in this study was assessed with a 20-item Simplified Coping Style Questionnaire developed by Yaning Xie (the scale derived from handbook: Wang et al., 1999). Ratings were made on a 4-point scale. The Simplified Coping Style Questionnaire consists of two subscales: positive and negative coping style. Cronbach’s α of the scale in this study was 0.875. Confirmatory factor analysis indicated that the validity of this scale was good (χ2 =396.742; χ2 /df = 2.681; p < 0.001; GFI=0.875; NFI=0.828; IFI=0.885; TLI = 0.849; CFI = 0.883; RMSEA = 0.077).
Pittsburgh sleep quality index
Sleep quality was assessed with a Chinese revised version of Pittsburgh Sleep Quality Index by Xianchen Liu (the scale derived from handbook: Wang et al., 1999). This Scale had 24 items. The total score (without item 19 and 5 other evaluation items) ranged from 0 to 21, with higher scores indicating poorer sleep quality. Cronbach’s α of the scale in this study was 0.742. Confirmatory factor analysis indicated that the validity of this scale was good (χ2 =16.824; χ2/df = 2.103; p < 0.05; GFI=0.984; NFI=0.984; IFI=0.992; TLI = 0.978; CFI = 0.992; RMSEA = 0.063).
Test of common method bias
Harman’s one-factor test was used to check Common Method Bias by exploratory factor analysis. As the results showed that characteristic values of 14 factors were greater than 1. The variation explained for the first factor of 14 factors was 19.015%, indicating that the variance interpretation of the maximum factor was below the upper limit standard of 40% (Podsakoff et al., 2003). Thus, there were no serious Common Method Bias of data in this study and further analysis can be used.
Statistical method
Data statistics were implemented by SPSS (version 22.0). Applicable statistical methods were chosen to analyze the relationship among anxiety, social support, coping style and sleep quality in parents of special children.
Results
Descriptive analysis
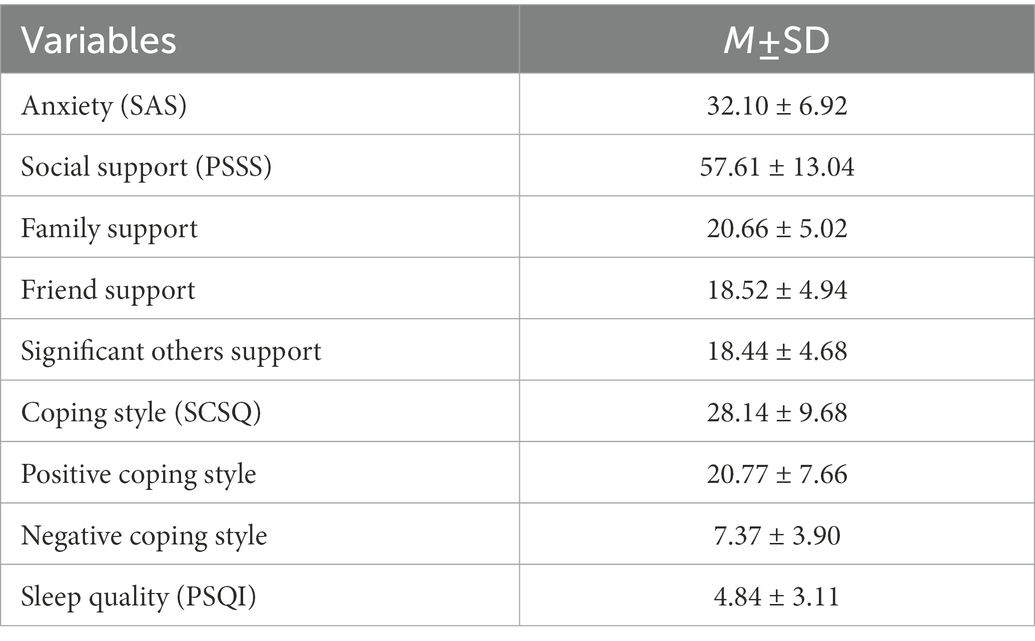
Descriptive analysis results based on the questionnaire of 283 parents of special children are presented in Table 2. The average score of anxiety (SAS) was 32.10 (standard deviation: 6.92). For social support (PSSS), the average score was 57.61(standard deviation: 13.04). For sleep quality (PSQI), the average score was 4.84(standard deviation: 3.11). For coping style (SCSQ), the average score was 28.14(standard deviation: 9.68). Subscale average scores of the four variables are also presented in Table 2.
Correlation analysis
The results of correlation analysis (Pearson) are presented in Table 3. Sleep quality had significant positive correlation with anxiety (p < 0.01) and significant negative correlation with social support (included its three subscales “family, friend and significant others support”) (p < 0.01). There was nonsignificant correlation between sleep quality and coping style (included its subscale “positive coping style”) (p < 0.05), but the subscale “negative coping style” was positively correlated with sleep quality (p < 0.01). Anxiety had significant negative correlation with social support and coping style (p < 0.01). Social support and coping style had significant positive correlation (p < 0.01).
Mediation analysis
Stepwise analysis method
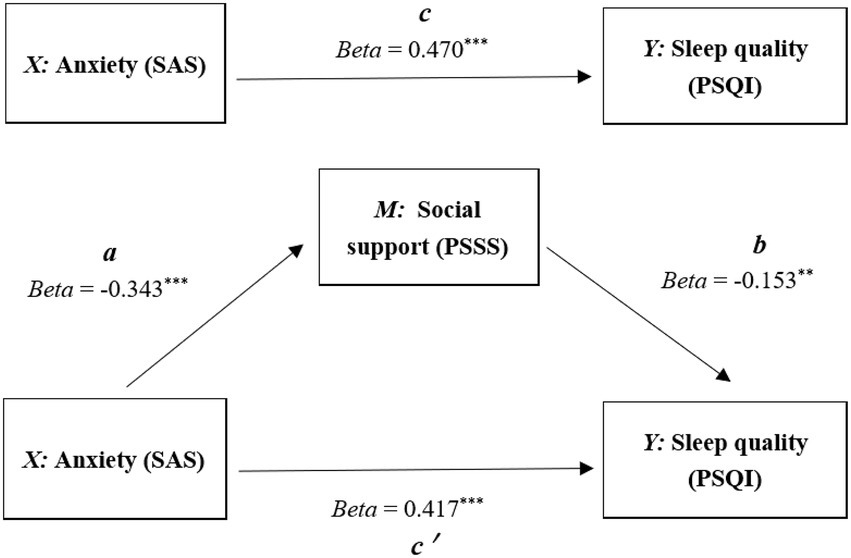
The mediation effect was analyzed by using the stepwise analysis method (Baron and Kenny, 1986; Wen and Ye, 2014). In Figure 2, results indicated that anxiety played significant prediction on sleep quality (total effect coefficient “c”, t = 8.924, p < 0.001) and social support (indirect effect coefficient “a,” t = −6.128, p < 0.001); After bring into the mediation variable (social support), social support played significant prediction on sleep quality (indirect effect coefficient “b,” t = −2.769, p < 0.01), anxiety also played significant prediction on sleep quality (direct effect coefficient “cʹ”, t = 7.529, p < 0.001). Therefore, social support partially mediated the relationship between anxiety and sleep quality.
Table 4 showed that in the stepwise regression equation, the direct effect (cʹ) had allocated 88.72% explanatory effect, and the indirect effect (a × b) had allocated 11.17% explanatory effect. Obviously, social support as the mediating role leaded to this indirect effect producing.
Bootstrap analysis method
Beside the method of Stepwise, Bootstrap method (Hayes, 2013) was also made to test the mediating effect. According to the mediating effect test procedure proposed by Zhao et al. (2010), indirect effect “a × b” (confidence interval: LLCI = 0.0059, ULCI = 0.0503) was significant, and the direct effect “cʹ,” (confidence interval: LLCI = 0.1382, ULCI = 0.2361) was also significant. So, bootstrap method suggested that social support partially mediated the relationship between anxiety and sleep quality as same as the stepwise method.
Discussion
The aim of this study was to investigate the association between anxiety, social support, coping style and sleep quality among Chinese parents of special children during the early COVID-19 epidemic. The result found anxiety was significantly positively correlated with sleep quality, which was consistent with previous studies (Augner, 2011; Liu et al., 2021; Simonetti et al., 2021; Yin et al., 2021), and showed that social support also related to sleep quality closely, which was consistent with previous studies (Brummett et al., 2006; Nordin et al., 2012; Marini et al., 2020; Mitchell et al., 2022). This study found that coping style and its subscale “positive coping style” were not correlated with sleep quality, but the subscale “negative coping style” was positively correlated with sleep quality, which was partially consistent with previous studies (Zhao et al., 2006; Xue et al., 2012; Gao and Hu, 2021; Luo et al., 2022; Yu et al., 2022). So, we did not consider the coping style as the mediating role in the following analysis.
In this study, both stepwise and bootstrap analysis methods result suggested that social support partially mediated the relationship between anxiety and sleep quality. That means if parents of special children who have more anxiety will get worse sleep quality, while more social support can alleviate the impact of anxiety on sleep quality (Pittsburgh Sleep Quality Index with higher scores indicating poorer sleep quality) between anxiety and sleep quality. Like other studies with different subjects, the more social support was received or perceived, the better sleep quality was, and the social support could improve sleep quality (Guo et al., 2014; Wang et al., 2021; Xu et al., 2022). On the other hand, this study results suggest that the anxiety of parents of special children not only directly affects sleep quality, but also indirectly affects sleep quality through social support. The mediating role of social support can alleviate the impact of anxiety on sleep quality, and play a buffer role.
During early COVID-19 epidemic period (March 2020, also the time when parents answered the questionnaires), the Hangzhou Green Apple Kindergarten had delayed the start of school for a while. For parents of special children, they had to take care and train children at home themselves, without professional help of rehabilitation institute (the kindergarten) and without adequate outdoor physical activity. In this situation, as common mental health influence factors, anxiety and sleep problems may occur more obviously (Qiu et al., 2021; Blasco-Lafarga et al., 2022). We have seen that social support will be the key point for solving anxiety and sleep disorders through their logical relationship in this study. Therefore, increasing social support of parents of special children for reducing the impact of anxiety on their sleep quality is very necessary during COVID-19 epidemic with the prevention and control policy of school. Relevant organizations and charities should offer social psychological service and lead the society to give more understanding and support to these parents of special children.
Conclusion
(1) Sleep quality had a significant positive correlation with anxiety and significant negative correlation with social support, but nonsignificant correlation with coping style; (2) Social support had a partial mediating effect on the relationship between anxiety and sleep quality. The anxiety of parents of special children not only directly affects sleep quality, but also indirectly affects sleep quality through social support. The mediating role of social support can alleviate the impact of anxiety on sleep quality through a buffer role.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Zhejiang Rehabilitation Medical Center. All participants gave informed consent before be investigated.
Author contributions
JT and JX designed the study. JX recruited the participants, distributed and collected the questionnaire. JX and JT analyzed the data, wrote the manuscript. JT and JX revised the manuscript. JT replied the office. JX submit for publication. All authors approved the final manuscript for publication.
Funding
This work was supported by Taizhou Philosophy and Social Science Planning Project (22GHB24), and General Project of Zhejiang Provincial Education Department (Y201941753).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alqaderi, H., Goodson, J. M., and Agaku, I. (2020). Association between sleep and severe periodontitis in a nationally representative adult US population. J. Periodontol. 91, 767–774. doi: 10.1002/JPER.19-0105
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM-5, Arlington: American Psychiatric Association, 361–422.
Augner, C. (2011). Associations of subjective sleep quality with depression score, anxiety, physical symptoms and sleep onset latency in students. Cent. Eur. J. Public Health. 19, 115–117. doi: 10.21101/cejph.a3647
Baron, R. M., and Kenny, D. A. (1986). The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 51, 1173–1182. doi: 10.1037/0022-3514.51.6.1173
Blasco-Lafarga, C., Roldán, A., Cordellat, A., and Monteagudo, P. (2022). Acute high-intensity exercise reduces performance anxiety: a pilot study in wind musicians. Ann. Appl. Sport Sci. 10:e1094. doi: 10.52547/aassjournal.1094
Brummett, B. H., Babyak, M. A., Siegler, I. C., Vitaliano, P. P., Ballard, E. L., Gwyther, L. P., et al. (2006). Associations among perceptions of social support, negative affect, and quality of sleep in caregivers and noncaregivers. Health Psychol. 25, 220–225. doi: 10.1037/0278-6133.25.2.220
Chatterjee, A. B. (2022). COVID-19, critical illness, and sleep. Crit. Care Med. 50, 1021–1023. doi: 10.1097/CCM.0000000000005519
Chen, C. C., Du, X. X., Su, S. H., and Yang, Y. R. (2016). The relationship between mindfulness and anxiety in parents of special children: the mediating role of coping style. Chin. J. Spec. Educ. 07, 70–75. doi: 10.3969/j.issn.1007-3728.2016.07.011
Gallagher, S., Phillips, A. C., and Carroll, D. (2010). Parental stress is associated with poor sleep quality in parents caring for children with developmental disabilities. J. Pediatr. Psychol. 35, 728–737. doi: 10.1093/jpepsy/jsp093
Gao, J., and Hu, L. J. (2021). Study on the relationship between sleep quality, coping style and social support of pediatric medical staff in 5 hospitals in Jiangxi Province. Occup. Health 16, 2211–2215. doi: 10.13329/j.cnki.zyyjk.2021.0539
Guo, S. R., Wu, S. W., and Feng, X. W. (2014). The effect of social support on sleep quality in college students: a multiple mediation model test. Psychol. Sci. 6, 1404–1408. doi: 10.16719/j.cnki.1671-6981.2014.06.020
Hayes, A. F. (2013). An Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-based Approach. New York: Guilford Press.
Kong, H., Huang, H. X., Wang, M. H., Cheng, F., and Song, Y. P. (2021). Mediation between coping style and sleep quality of vocational high school students with anxiety. The Modern Chinese Physician 14, 160–163.
Liu, B. L., Qiao, K., and Lu, Y. F. (2021). The relationship between perceived stress, state-trait anxiety, and sleep quality among university graduates in China during the COVID-19 pandemic. Front. Psychol. 12:664780. doi: 10.3389/fpsyg.2021.664780
Luo, Y. F., Lu, G. Y., Zhang, H. Y., and Li, Q. H. (2022). The correlation analysis of alert fatigue, coping style and sleep quality among medical staff in the critical care department of 5 third class first class hospitals in Sichuan Province. Occup. Health. 9, 1237–1242. doi: 10.13329/j.cnki.zyyjk.2022.0230
Ma, Y. (2013). A study on the relationship among locus of control, anxiety and coping style of college students. J. Henan Univ. Sci. Technol. 6, 78–80. doi: 10.3969/j.issn.1673-6060.2013.06.025
Marini, C., Wilson, S., Nah, S., Martire, L., and Sliwinski, M. (2020). Links between rumination and sleep quality among older adults: an examination of the role of social support. Innov. Aging. 4:562. doi: 10.1093/geroni/igaa057.1853
Meltzer, L. J. (2008). Brief report: sleep in parents of children with autism spectrum disorders. J. Pediatr. Psychol. 33, 380–386. doi: 10.1093/jpesy/jsn005
Mitchell, A. M., Kowalsky, J. M., Christian, L. M., Belury, M. A., and Cole, R. M. (2022). Perceived social support predicts self-reported and objective health and health behaviors among pregnant women. J. Behav. Med. 45, 589–602. doi: 10.1007/s10865-022-00306-5
Mohammadkhani, P. G., Irandoust, K., Taheri, M., Mirmoezzi, M., and Baić, M. (2019). Effects of eight weeks of aerobic exercise and taking caraway supplement on C-reactive protein and sleep quality in obese women. Biol. Rhythm. Res. 52, 218–226. doi: 10.1080/09291016.2019.1587837
Morgan, B. B. (1974). Effects of continuous work and sleep loss in the reduction and recovery of work efficiency. Am. Ind. Hyg. Assoc. J. 35, 13–20. doi: 10.1080/0002889748507001
Nordin, M., Westerholm, P., Alfredsson, L., and Akerstedt, T. (2012). Social support and sleep. Longitudinal relationships from the wolf-study. Psychology. 03, 1223–1230. doi: 10.4236/psych.2012.312A181
O'Leary, K., Bylsma, L. M., and Rottenberg, J. (2016). Why might poor sleep quality lead to depression? A role for emotion regulation. Cognit. Emot. 31, 1698–1706. doi: 10.1080/02699931.2016.1247035
Parvaneh, K., Poh, B., Hajifaraji, M., and Ismail, M. (2016). Less sleep duration and poor sleep quality Lead to obesity. Proc. Nutr. Soc. 75:E19. doi: 10.1017/S0029665115004528
Podsakoff, P. M., Mackenzie, S. B., Lee, J. Y., and Podsakoff, N. P. (2003). Common method biases in behavioral research: a critical review of the literature and recommended remedies. J. Appl. Psychol. 88, 879–903. doi: 10.1037/0021-9010.88.5.879
Qiu, Y., Huang, J., Sun, J. H., Zhao, J. X., Chen, A., Chen, J. D., et al. (2021). Prevalence of risk factors associated with mental health symptoms among the outpatient psychiatric patients and their family members in China during the coronavirus disease 2019 pandemic. Front. Psychol. 12:622339. doi: 10.3389/fpsyg.2021.622339
Simonetti, V., Durante, A., Ambrosca, R., Arcadi, P., and Cicolini, G. (2021). Anxiety, sleep disorders and self-efficacy among nurses during COVID-19 pandemic: a large cross-sectional study. J. Clin. Nurs. 30, 1360–1371. doi: 10.1111/jocn.15685
Stanton, R., To, Q. G., Khalesi, S., Williams, S. L., Alley, S. J., Thwaite, T. L., et al. (2020). Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health. 17:4065. doi: 10.3390/ijerph17114065
Taheri, M., Irandost, K., Mirmoezzi, M., and Ramshini, M. (2019). Effect of aerobic exercise and Omega-3 supplementation on psychological aspects and sleep quality in Prediabetes elderly women. Sleep Hypnosis. 21, 170–174. doi: 10.5350/Sleep.Hypn.2019.21.0185
Taş, I. (2019). Association between depression, anxiety, stress, social support, resilience and internet addiction: a structural equation modelling. Malays. Online J. Educ. Technol. 7, 1–10. doi: 10.17220/mojet.2019.03.001
Varma, P., Conduit, R., Junge, M., Lee, V. V., and Jackson, M. L. (2021). A systematic review of sleep associations in parents and children. J. Child Fam. Stud. 30, 2276–2288. doi: 10.1007/s10826-021-02002-5
Wang, Q., Mu, Y. L., and Qiu, R. Y. (2021). Social support mediates stress and sleep quality. Chin. Contemp. Med. 28, 208–211. doi: 10.3969/j.issn.1674-4721.202.25.057
Wang, X. D., Wang, X. L., and Ma, H. (1999). Handbook of Mental Health Rating Scale. Beijing: Chinese Journal of Mental Health.
Wen, Z. L., and Ye, B. J. (2014). Mediation effect analysis: method and model development. Adv. Psychol. Sci. 22, 731–745. doi: 10.3724/SP.J.1042.2014.00731
Wu, M. (2010). A study on the relationship between social support and anxiety of parents of autistic children. J. Gannan Norm. Univ. 2, 100–102. doi: 10.13698/j.cnki.cn36-1037/c.2010.02.013
Xu, R. Z., Ma, Y., and Dai, Q. (2022). The relationship between expectant sadness and sleep disorder in parents of children with acute leukemia -- mediated by social support. Chin. J. Pract. Nurs. 34, 2691–2697. doi: 10.3760/cma.j.cn211501-20220217-00429
Xue, F., Zhang, Q. X., Wang, J. N., Luo, S. F., and Yang, L. H. (2012). The relationship between life events, coping styles and sleep quality of college students. Neuropathy and Mental Health 12, 275–278. doi: 10.3969/j.issn.1009-6574.2012.03.019
Yin, H. Z., Zhang, L., Li, D., Xiao, L., and Cheng, M. (2021). The gray matter volume of the right insula mediates the relationship between symptoms of depression/anxiety and sleep quality among college students. J. Health Psychol. 26, 1073–1084. doi: 10.1177/1359105319869977
Yu, H., Li, X. Y., Wen, F., and Li, H. M. (2022). The influence of social support and coping style on sleep quality of medical staff in grade a hospitals. Occup. Health. 13, 1812–1816. doi: 10.13329/j.cnki.zyyjk.2022.0373
Zhao, J. B., Xie, Y. N., Ren, Z. W., and Shi, M. C. (2006). Sleep quality of Plateau soldiers and its influencing factors. Chinese J. Neuropsychiatric Disorders 2, 154–156. doi: 10.3969/j.issn.1002-0152.2006.02.016
Zhao, X., Lynch, J. G. Jr., and Chen, Q. (2010). Reconsidering Baron and Kenny: myths and truths about mediation analysis. J. Consum. Res. 37, 197–206. doi: 10.1086/651257
Keywords: anxiety, social support, sleep quality, coping style, Chinese parents of special children
Citation: Xu J and Tang J (2023) Social support as a mediator between anxiety and quality of sleep among Chinese parents of special children. Front. Psychol. 14:1077596. doi: 10.3389/fpsyg.2023.1077596
Edited by:
Amy Chan Hyung Kim, Florida State University, United StatesReviewed by:
Morteza Taheri, Imam Khomeini International University, IranKhadijeh Irandoust, Imam Khomeini International University, Iran
Copyright © 2023 Xu and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiliang Tang, ✉ Mzk0OTA4NjkzQHFxLmNvbQ==
 Junda Xu
Junda Xu Jiliang Tang
Jiliang Tang