- 1Department of Gastroenterology, Shenzhen Hospital, Southern Medical University, Shenzhen, Guangdong, China
- 2Hunan Key Laboratory of Oral Health Research & Xiangya Stomatological Hospital & Xiangya School of Stomatology, Central South University, Changsha, Hunan, China
- 3Department of Nursing Research, Affiliated Hospital of Guangdong Medical University, Zhanjiang, Guangdong, China
- 4Clinical Nursing Teaching and Research Section, The Second Xiangya Hospital of Central South University, Changsha, Hunan, China
- 5Department of Pediatrics, The Second Xiangya Hospital of Central South University, Changsha, Hunan, China
Objective: This study aimed to compare the effects of robot-assisted thoracic surgery (RATS), video-assisted thoracic surgery (VATS), and thoracotomy on the psychological status, medical coping mode, and quality of life of patients with lung cancer.
Methods: A total of 158 patients with lung cancer were selected from the thoracic surgery center of a third-grade hospital in Hunan Province, China, from September to November 2020. The Self-Rating Anxiety Scale (SAS), Self-Rating Depression Scale (SDS), Medical Coping Modes Questionnaire (MCMQ), and Medical Outcomes Study (MOS) 36-item Short Form Health Survey (SF-36) were used to assess the effects of the surgical approaches on the study parameters before and 48–96 h after surgery. The t-test and analysis of variance were used to analyze the data.
Results: The results revealed that the patients’ depression increased, their short-term quality of life decreased, and they tended to adopt a positive coping mode after surgery (p < 0.05). The RATS and VATS groups differed in avoidance dimension of medical coping modes (p < 0.05). The VATS and thoracotomy groups differed in the body pain dimension of quality of life (p < 0.05). Different surgical approaches had no effect on the psychological status, medical coping modes except the avoidance dimension, and quality of life except the body pain dimension.
Conclusion: Surgical approaches have little effect on the psychological status, medical coping modes, and quality of life of patients with lung cancer; however, their depression increased and quality of life decreased after the surgery.
1. Introduction
Lung cancer is one of the prevalent malignant tumors and major causes of death worldwide (Patricia et al., 2018). Surgical resection with curative intent remains the gold standard for treating patients with lung cancer. (Deffebach and Humphrey, 2015; Ettinger et al., 2022). Surgery is the preferred treatment of choice for stage I, stage II, and some stage III non-small cell lung cancers and stage I and some stage IIA small cell lung cancers. It can effectively remove diseased tissues and improve patient survival rates (Zhi et al., 2015; Suzuki et al., 2019; Saji et al., 2022). Current surgical approaches include robot-assisted thoracic surgery (RATS), video-assisted thoracic surgery (VATS), and thoracotomy, and each has specific advantages and disadvantages. Thoracotomy has a short operation time, but involves large incision and trauma, and difficulty in recovery. VATS has the advantages of less trauma and easy recovery, but involves a long and complex operation (Wang et al., 2015; Huang et al., 2016). Compared with VATS, RATS has a shorter hospital stay, less bleeding, more radical lymph node dissection, and more accurate surgical incisions (Louie et al., 2012; Farivar et al., 2014; Wilson et al., 2014).
Studies have reported a high incidence of anxiety and depression (33–44%) in patients with lung cancer during diagnosis and treatment (Shimizu et al., 2012; Gu et al., 2018). Moreover, patients may experience psychological problems such as anger, feelings of isolation, anxiety, depression, and lower self-esteem after surgery. Coping is the process through which a person adopts different strategies to deal with a problem (Darabos et al., 2021). Patients with lung cancer adopt a more positive coping mode after the surgery compared with that in the preoperative stage; however, the specific medical coping modes corresponding to different surgical methods are unknown. Perioperative quality of life is an important factor and prognostic indicator of the survival and recovery of patients with lung cancer (Morrison et al., 2017; Mederos et al., 2020; Zheng et al., 2020), and it is also the ultimate goal of patient treatment (Buitron et al., 2018). Previous studies have shown that the quality of life of patients with lung cancer was associated with their depression and anxiety (Jung et al., 2018; Polański et al., 2018).
Existing studies have focused on comparing the effects of the three surgical approaches on surgical complications and oncological outcomes for patients regarding survival or recurrence after the surgical treatment (Jiang et al., 2019; Meng, 2020). Psychological status and quality of life after surgery are equally or even more important for patients. However, previous studies have shown no statistically significant difference in quality of life of patients with lung cancer in the thoracotomy and VATS groups (Hopkins et al., 2017). With increasing medical innovation in the field of surgical intervention, new evidence is needed to confirm the reliability of the results. Accordingly, we aimed to compare the effects of surgical approaches on the psychological status, medical coping mode, and quality of life of patients with lung cancer, providing a basis for prevention and intervention to help the patients improve their psychological health and quality of life.
2. Materials and methods
2.1. Patient enrollment
We included all patients with lung cancer who underwent surgery at the thoracic surgery center of a hospital in Hunan Province, China, from September to November 2020.
The inclusion criteria were as follows: (a) diagnosed with lung cancer, (b) underwent surgery, and (c) volunteered for the study. Correspondingly, the exclusion criteria were: (a) inadequate literacy level, (b) severe mental disorders, and (c) inadequate communication ability.
The ethics approval was obtained from the ethics committee of Central South University [No: E2020178]. Written informed consent to participate in this study was provided by the participants.
2.2. Measures
Health-related quality of life was measured using the Medical Outcomes Study (MOS) 36-item Short Form Health Survey (SF-36) compiled by Stewart et al. (1988). The scale comprises 36 items and eight dimensions, including physical function, role-physical function, and body pain. The scores for the SF-36 were converted to a range from 0 to 100 using the formula (raw sum – possible minimum score) ÷ (possible maximum score – possible minimum score). This scale is one of the commonly used health measurement tools worldwide. The Cronbach’s alpha for the SF-36 was 0.899.
Anxiety was determined using the Self-Rating Anxiety Scale (SAS) compiled by Zung (1971). The scale consists of 20 items, and each item is ranked from 1 to 4, with higher scores indicating higher levels of anxiety. According to the Chinese norm (Dai, 2010), the criteria for severity were as follows: no anxiety (score < 50), mild anxiety (score 50–59), moderate anxiety (score 60–68) and severe anxiety (score ≥ 69). The Cronbach’s alpha for the SAS was 0.864.
Depression was determined using the Self-Rating Depression Scale (SDS) compiled by Zung (1965). The scale consists of 20 items, and each item is ranked from 1 to 4, with higher scores indicating higher levels of depression. The criteria for severity were as follows: no depression (score < 53), mild depression (score 53–62), moderate depression (score 63–72), and severe depression (score ≥ 73) (18). The Cronbach’s alpha for the SDS was 0.873.
The coping mode was measured using the Medical Coping Modes Questionnaire (MCMQ) compiled by Feifel et al. (1987) and translated into Chinese by Shen (2000). The scale comprises 20 items and three dimensions: confrontation (8 items), avoidance (7 items), and acceptance-resignation (5 items). Each item is ranked from 1 to 4. The dimension with the highest cumulative score indicated the particular coping strategy that patients were most likely to use (Zeng et al., 2021). Cronbach’s alpha of the three dimensions were 0.69, 0.60, and 0.76, respectively.
2.3. Statistical analysis
Data were analyzed using SPSS 18.0. Descriptive data were summarized as frequencies and percentages. The scores were expressed as mean ± standard deviation (X ± S). Differences between groups were analyzed using the paired-sample t-test or analysis of variance, and p-values of less than 0.05 were considered statistically significant.
3. Results
3.1. Patient characteristics
In total, 158 patients enrolled in this study. The cohort consisted of 73 men (46.2%) and 85 women (53.8%); 11 (7.0%), 44 (27.8%), and 103 (65.2%) were < 30 years, 30–50 years, and > 50 years of age.
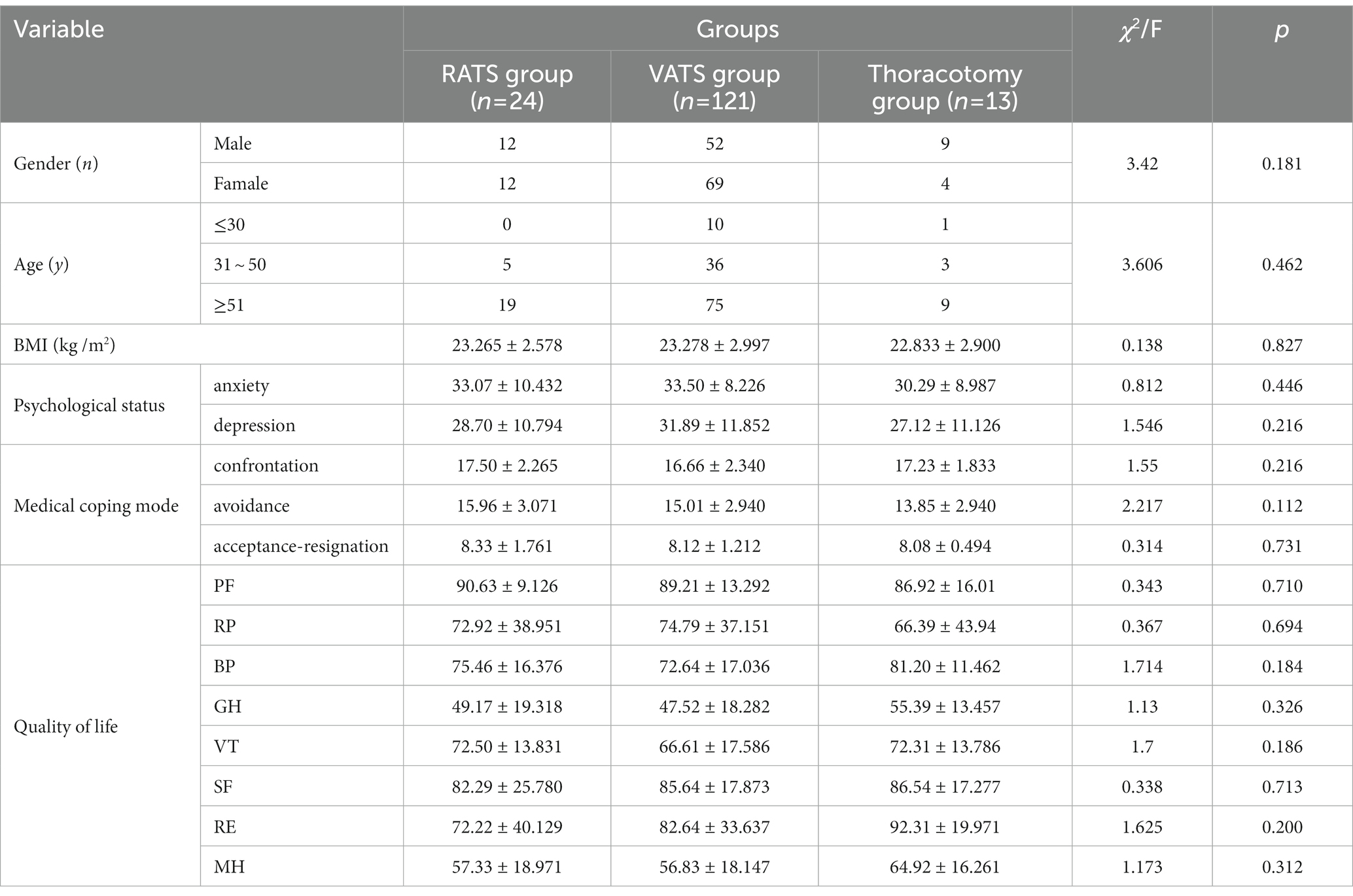
According to the surgical method, the participants were categorized in three groups, 24, 121, and 13 in the RATS, VATS, thoracotomy groups, respectively. As shown in Table 1, there was no statistically significant difference in gender, age, body mass index (BMI), psychological status, medical coping mode, and quality of life among the three groups (p > 0.05), and they were comparable.
3.2. Comparison of psychological status, medical coping modes, and quality of life before and after surgery
As shown in Table 2, surgery had no effect on the anxiety scores of patients with lung cancer (p > 0.05), however, it increased their depression scores (p < 0.05). In terms of medical coping modes, the score of the confrontation and acceptance-resignation dimensions increased, and that of avoidance dimension decreased after surgery (p < 0.05). Regarding quality of life, there was no statistically significant difference between the changes in general health and mental health scores at 48–96 h after surgery (p > 0.05), while the scores of other dimensions decreased (p < 0.05).
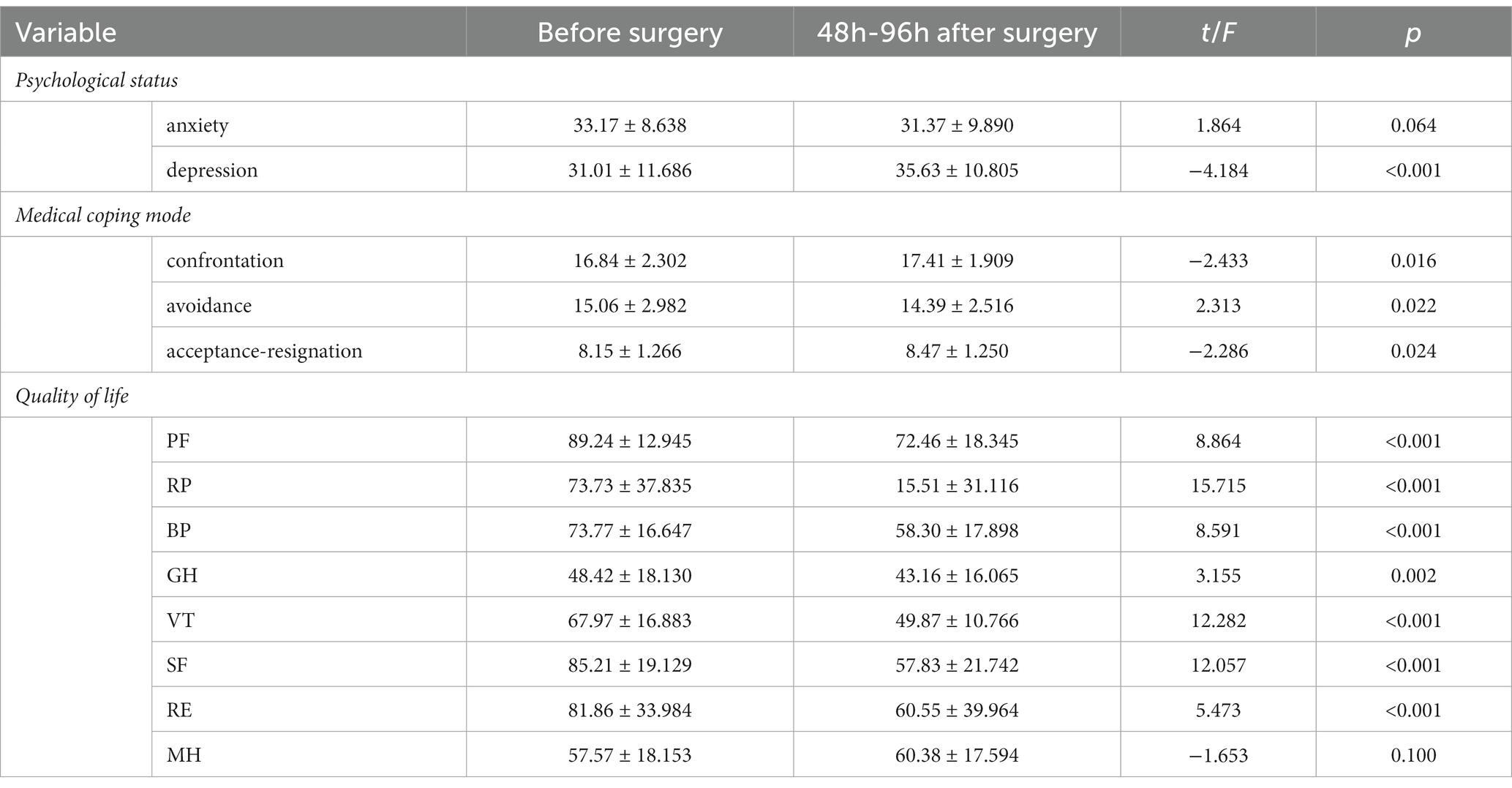
Table 2. Comparison of psychological status, medical coping mode and quality of life of lung cancer patients before and after surgery.
3.3. Comparison between the effects of surgical approaches on the psychological status, medical coping modes, and quality of life
As shown in Table 3, the avoidance dimension score of medical coping modes for the RATS group was higher than that for the VATS group (p < 0.05), and the body pain dimension score of quality of life for the thoracotomy group was higher than that for the VATS group (p < 0.05). Different surgical approaches had no effect on the total scores of psychological status, medical coping modes except for the avoidance dimension, and quality of life except for the body pain dimension of patients with lung cancer (p > 0.05).
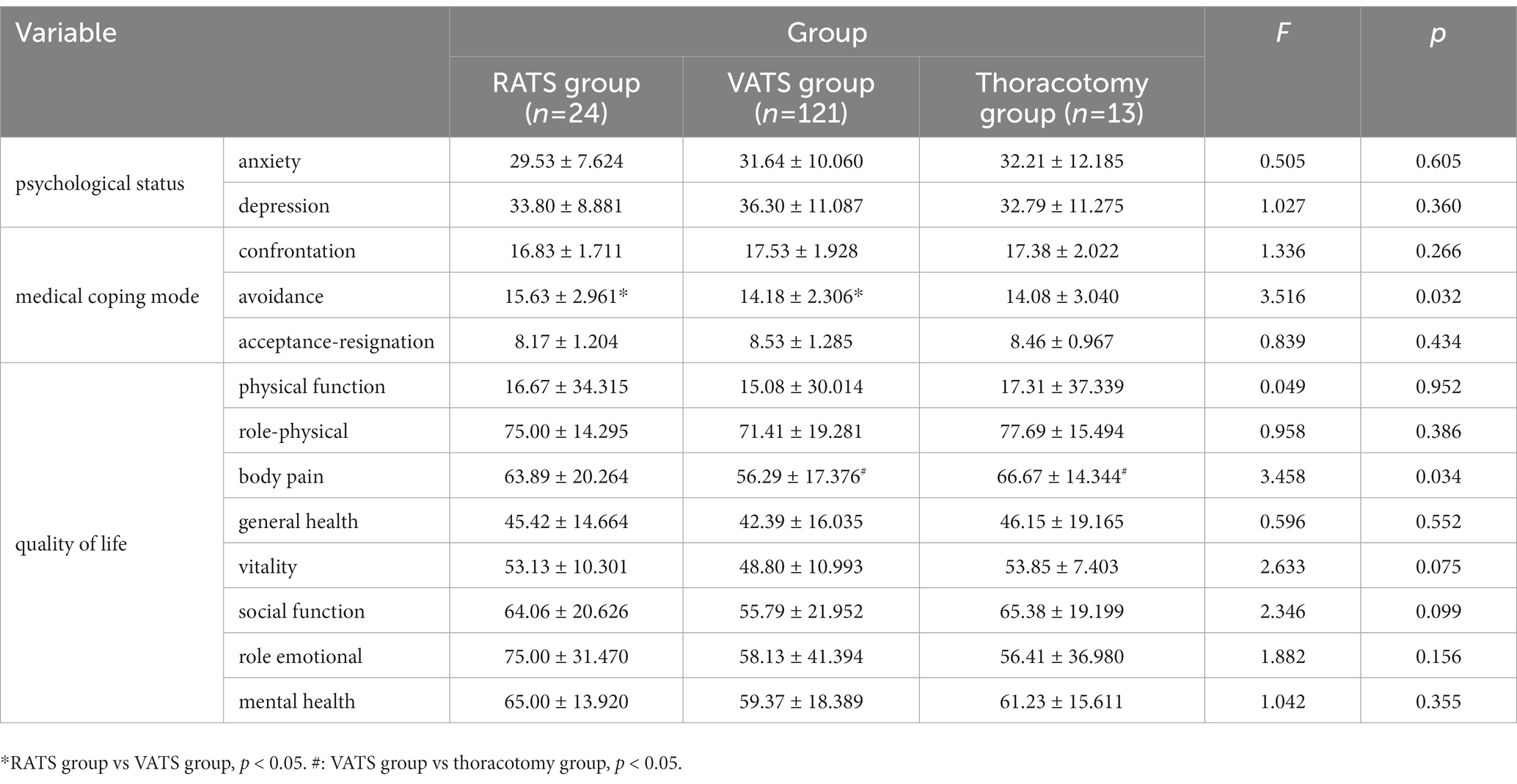
Table 3. Comparison of the effects of different surgical approaches on the psychological status, medical coping modes and quality of life of patients with lung cancer.
4. Discussion
4.1. Patients’ depression scores increased and quality of life scores decreased post-surgery
Our study found an increase in patients’ postoperative depression scores and a decrease in quality of life scores compared to those in the pre-operative period. This is consistent with the study by Zhu et al. (2019) and may be related to the significant postoperative physical changes of patients (Jian et al., 2016). Depression is a common complication of surgical trauma and stress. Previous studies have indicated that patients with cancer complicated by depression have a 19% higher fatality rate than those with cancer alone (Pinquart and Duberstein, 2010). Moreover, long-term experience of depression and other mental disorders can activate the neuroendocrine immune regulatory network, leading to destruction of the body’s cellular immunity and resulting in a decline in the immune function of patients with cancer. This can induce tumors or lead to aggravation and deterioration of patients with tumor. In addition, negative emotions can easily cause patients not to cooperate with treatment or even to discontinue it. Patients may experience loss of appetite, sleep disorders, etc. which may reduce their quality of life (Wang et al., 2016). Li et al. (2014) formulated a group psychotherapy plan for patients with lung cancer. The main techniques used include psychoeducation, rational-emotional behavior therapy, support-expression, confidence therapy, painting, meditation relaxation training, and abdominal breathing training. The results of this study found that group psychotherapy based on psychoeducation and supportive expression could improve the social function and emotional state of patients and reduce depression in patients with lung cancer. Therefore, medical staff should pay attention to the depressive symptoms of patients with lung cancer after surgery and promptly detect and provide individualized psychological care to improve treatment compliance, quality of life, and achieve the best treatment effect.
4.2. Patients with lung cancer were more inclined to adopt positive coping modes after surgery
Among the three dimensions of the MCMQ, “confrontation” is regarded as a positive and effective coping mode, and “avoidance” and “acceptance-resignation” are regarded as negative coping modes. The results showed the participants’ confrontation and acceptance-resignation dimension scores increased, and the avoidance dimension score decreased. The score of the confrontation dimension was much higher than that of the avoidance and acceptance-resignation dimensions, which implies that patients tend to adopt a more active coping mode to confront diseases after surgery. Coping mode is an important intermediary variable of psychological stress. Individuals may adopt completely different coping modes when facing the same stress, which causes different psychological effects (Ju and Xu, 2019). Therefore, strengthening the education of coping modes and helping patients actively face surgery and illness are important ways to improve their quality of life. Wang (2019) found that the quality of life of patients with lung cancer was significantly related to social support and self-efficacy. Social support can improve the psychological status of patients with cancer by reducing negative emotions and regulating coping mechanisms (Li et al., 2016; Hajek et al., 2017). Self-efficacy is a predictor of patients’ ability to cope with the disease and adopt healthy behaviors. Self-efficacy affects health outcomes by influencing patients’ attitudes toward difficulties (Hellström et al., 2009). Yeung and Lu (2014) found that high levels of self-efficacy play an important role in optimizing the quality of life of patients with cancer. Therefore, medical staff can take relevant measures to enhance confidence and self-efficacy of patients to help them overcome the disease to improve their quality of life.
4.3. Different surgical methods have little effect on the patient’s psychological status and short-term quality of life after surgery
Our research showed that the RATS and VATS groups differed only in the avoidance dimension of medical coping modes, and that the VATS and thoracotomy groups differed in the body pain dimension of quality of life, which may be related to the different sizes of wounds caused by different surgical methods. Previous studies have shown that other factors affecting the mental health of patients with lung cancer include the type of lung cancer (Zeilinger et al., 2022), type of resection of the surgery (Hao et al., 2016), pathological stage (Yan et al., 2019), postoperative dyspnea, and severe pain (Morrison et al., 2017). There is moderate-quality evidence that preoperative exercise significantly reduces postoperative complication rates (Steffens et al., 2018). Therefore, it is essential that physicians make a reasonable preoperative assessment of these influencing factors, select a suitable surgical method, and assist patients with early protective rehabilitation programs, including pre-pulmonary surgery aerobic exercise and respiratory muscle training (Barğı et al., 2021). In addition, special attention should be paid to pain care of patients with major surgical wounds.
Different surgical methods have no effect on the psychological status, and little effect on medical coping modes (except avoidance dimension) and quality of life (except the body pain dimension) of patients with lung tumors, which suggests that the three surgical methods have equivalent effects on the short-term psychological status and quality of life after surgery. This highlights that the surgical method should be chosen based on the patient’s condition.
4.4. Research implications and clinical practice
This study revealed the changes in psychological status, medical coping modes, and quality of life of patients with lung cancer before and after surgery, as well as the differences in these parameters for the patients who underwent RATS, VATS, and thoracotomy. It provides a reference and theoretical basis for medical professionals to pay timely attention to the changes and formulate interventions for patients with lung cancer to improve their psychological status and quality of life after surgery.
According to the results of this study, the depression of patients increased and their short-term quality of life decreased after surgery. It is difficult for surgeons to evaluate patients’ psychological status, and the actual incidence of psychological distress may be underestimated. Therefore, patients should be carefully screened for psychological status by physicians using appropriate methods throughout the treatment process, and those with psychological distress should be managed by psychiatrists who can provide appropriate professional mental health care. In addition, our research showed that the different surgical methods had little effect on the psychological status, medical coping modes, and short-term quality of life of patients with lung cancer after surgery. This suggests that the surgical approach for patients with lung cancer is not universal and should be individualized; that is, the focus of surgery should be to make a holistic and comprehensive assessment to select the most appropriate procedure considering the patient’s physical condition. This reminds healthcare professionals of the need to pay attention to the psychological condition of patients when treating lung cancer and to use individualized treatment and care with the ultimate goal of improving the patient’s quality of life.
4.5. Study limitations
Our study has some limitations. First, it only focused on the impact of different surgical approaches on patients with lung cancer, and other factors such as types of lung cancer, pathological stage, postoperative dyspnea, severe pain, or comorbidities were not considered. This should be considered in future prospective cohort studies. Second, the formal sample size was not calculated beforehand, and we included all patients with lung cancer who met the selection criteria in a specific time period. It is necessary to expand the scope to include more patients. Finally, we did not follow up the discharged patients for a long time; therefore, a longer follow-up tis necessary to update the state of patients’ health in the future.
5. Conclusion
There is little difference in the effects of various surgical approaches on the psychological status, medical coping modes, and quality of life after 48–96 h of surgery of patients with lung cancer. However, their depression increased and quality of life decreased after surgery; therefore, it is necessary to focus on the psychological status of the patients and improve their quality of life after surgery.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The ethics approval was obtained from the ethics committee of Central South University [No: E2020178]. The patients/participants provided their written informed consent to participate in this study.
Author contributions
YL and GX are the primary investigator of the study. Y-pC and YZ conducted the study, data analysis, and drafted the manuscript. XC, ZC, JL, LZ, GX, and XC helped conduct the study and proof reading the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Hunan Province Disabled Rehabilitation Scientific Research Project, China (fund number: 2019XK007) and Clinical Nursing and Management Perso-nnel Research Start-up Foundation of the Xiangya Stomatological Hospital of Central South University (No. HG202303).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Barğı, G., Baytok, E., Çelik, Z., Türk, M. Ş., Çelik, A., Kurul, İ. C., et al. (2021). Exercise capacity, muscle strength, dyspnea, physical activity, and quality of life in preoperative patients with lung cancer. Turk. J. Med. Sci. 51, 2621–2630. doi: 10.3906/sag-2102-55
Buitron, D. L. V. P., Coe, C., Paasche-Orlow, M. K., Clark, J. A., Waite, K., Sanchez, M. J., et al. (2018). “It’s like a mirror image of my illness”: exploring patient perceptions about illness using health mind mapping-a qualitative study. J. Gen. Intern. Med. 33, 1692–1699. doi: 10.1007/s11606-018-4557-9
Dai, X. Y. (2010). Common Psychological Assessment Mannual. Beijing: People’s Military Medical Press.
Darabos, K., Renna, M. E., Wang, A. W., Zimmermann, C. F., and Hoyt, M. A. (2021). Emotional approach coping among young adults with cancer: relationships with psychological distress, posttraumatic growth, and resilience. Psychooncology 30, 728–735. doi: 10.1002/pon.5621
Deffebach, M. E., and Humphrey, L. (2015). Lung cancer screening. Surg. Clin. North Am. 95, 967–978. doi: 10.1016/j.suc.2015.05.006
Ettinger, D. S., Wood, D. E., Aisner, D. L., Akerley, W., Bauman, J. R., Bharat, A., et al. (2022). Non-small cell lung cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 20, 497–530. doi: 10.6004/jnccn.2022.0025
Farivar, A. S., Cerfolio, R. J., Vallières, E., Knight, A. W., Bryant, A., Lingala, V., et al. (2014). Comparing robotic lung resection with thoracotomy and video-assisted thoracoscopic surgery cases entered into the Society of Thoracic Surgeons database. Innovations (Phila) 9, 10–15. doi: 10.1097/IMI.0000000000000043
Feifel, H., Strack, S., and Nagy, V. T. (1987). Coping strategies and associated features of medically ill patients. Psychosom. Med. 49, 616–625. doi: 10.1097/00006842-198711000-00007
Gu, W., Xu, Y. M., and Zhong, B. L. (2018). Health-related quality of life in Chinese inpatients with lung cancer treatedin large general hospitals: across-sectional study. BMJ Open 8:e019873. doi: 10.1136/bmjopen-2017-019873
Hajek, A., Brettschneider, C., Mallon, T., van der Leeden, C., Mamone, S., Wiese, B., et al. (2017). How does social support affect functional impairment in late life? Findings of a multicenter prospective cohort study in Germany. Age Ageing 46, 813–820. doi: 10.1093/ageing/afx012
Hao, Z., Cai, Y., Fu, S., Zhang, N., and Fu, X. (2016). Comparison study of post-operative pain and short-term quality of life between Uniportal and three portal video-assisted thoracic surgery for radical lung cancer resection. Zhongguo Fei Ai Za Zhi 19, 122–128. doi: 10.3779/j.issn.1009-3419.2016.03.02
Hellström, K., Vahlberg, B., Urell, C., and Emtner, M. (2009). Fear of falling, fall-related self-efficacy, anxiety and depression in individuals with chronic obstructive pulmonary disease. Clin. Rehabil. 23, 1136–1144. doi: 10.1177/0269215509342329
Hopkins, K. G., Ferson, P. F., Shende, M. R., Christie, N. A., Schuchert, M. J., and Pennathur, A. (2017). Prospective study of quality of life after lung cancer resection. Ann. Transl. Med. 5:204. doi: 10.21037/atm.2017.04.34
Huang, J., Li, S., Hao, Z., Chen, H., He, J., Xu, X., et al. (2016). Complete video-assisted thoracoscopic surgery (VATS) bronchial sleeve lobectomy. J. Thorac. Dis. 8, 553–574. doi: 10.21037/jtd.2016.01.63
Jian, G., Jun, X. U., and Song, X. (2016). Research on anxiety and depression mood, coping style and quality of life of patients with breast cancer undergoing modified radical mastectomy during perioperative period and chemotherapy period. J. int. Psych. 43, 1046–1048.
Jiang, B., Kang, P., Tao, S., Shen, C., Deng, B., Wang, R., et al. (2019). Short-term efficacy of robot-assisted surgery versus video-assisted thoracoscopic surgery for anterior mediastinal mass. J. Third Mil. Med. Univ. 41, 1578–1582. doi: 10.16016/j.1000-5404.201904181
Ju, Q., and Xu, L. (2019). Clinical curative effect of hysteroscopy-laparoscopy combined with supportive psychotherapy in the treatment of oviduct obstructive infertility and the influence on anxiety, depression, coping style and quality of life. China. J. Health Psychol. 27, 523–527. doi: 10.13342/j.cnki.cjhp.2019.04.010
Jung, J. Y., Lee, J. M., Kim, M. S., Shim, Y. M., Zo, J. I., and Yun, Y. H. (2018). Comparison of fatigue, depression, and anxiety as factors affecting posttreatment health-related quality of life in lung cancer survivors. Psychooncology 27, 465–470. doi: 10.1002/pon.4513
Li, J. J., Pang, Y., and Tang, L. L., and Institute (2014). An open controlled study of group psychotherapy on quality of life and mood in patients with lung cancer. Chin. Ment. Health J. 28, 657–662.
Li, M. Y., Yang, Y. L., Liu, L., and Wang, L. (2016). Effects of social support, hope and resilience on quality of life among Chinese bladder cancer patients: a cross-sectional study. Health Qual. Life Outcomes 14:73. doi: 10.1186/s12955-016-0481-z
Louie, B. E., Farivar, A. S., Aye, R. W., and Vallières, E. (2012). Early experience with robotic lung resection results in similar operative outcomes and morbidity when compared with matched video-assisted thoracoscopic surgery cases. Ann. Thorac. Surg. 93, 1598–1605. discussion 1604-5. doi: 10.1016/j.athoracsur.2012.01.067
Mederos, N., Friedlaender, A., Peters, S., and Addeo, A. (2020). Gender-specific aspects of epidemiology, molecular genetics and outcome: lung cancer. ESMO Open 5:e000796. doi: 10.1136/esmoopen-2020-000796
Meng, C. (2020). “Evaluation of short-term curative effect of Da Vinci robot, thoracoscope and thoracotomy in treating mediastinal tumor ”, in. Gansu University of Chinese Medcine). Lanzhou
Morrison, E. J., Novotny, P. J., Sloan, J. A., Yang, P., Patten, C. A., Ruddy, K. J., et al. (2017). Emotional problems, quality of life, and symptom burden in patients with lung cancer. Clin. Lung Cancer 18, 497–503. doi: 10.1016/j.cllc.2017.02.008
Patricia, M., De, G., Carol, C., and Wu, B., W, and Carter (2018). The epidemiology of lung cancer Trans. Lung Cancer Res. 7, 220–233. doi: 10.21037/tlcr.2018.05.06
Pinquart, M., and Duberstein, P. R. (2010). Depression and cancer mortality: a meta-analysis. Psychol. Med. 40, 1797–1810. doi: 10.1017/S0033291709992285
Polański, J., Chabowski, M., Chudiak, A., Uchmanowicz, B., Janczak, D., Rosińczuk, J., et al. (2018). Intensity of anxiety and depression in patients with lung cancer in relation to quality of life. Adv. Exp. Med. Biol. 1023, 29–36. doi: 10.1007/5584_2017_50
Saji, H., Okada, M., Tsuboi, M., Nakajima, R., Suzuki, K., Aokage, K., et al. (2022). Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet 399, 1607–1617. doi: 10.1016/S0140-6736(21)02333-3
Shen, X. (2000). Report on application of Chinese version of MCMQ in 701 patients. chinese J. Behav. Med. Sci. 01, 22–24.
Shimizu, K., Nakaya, N., Saito-Nakaya, K., Akechi, T., Yamada, Y., Fujimori, M., et al. (2012). Clinical biopsychosocial risk factors for depression in lung cancer patients: a comprehensive analysis using data from the lung cancer database project. Ann. Oncol. 23, 1973–1979. doi: 10.1093/annonc/mds061
Steffens, D., Beckenkamp, P. R., Hancock, M., Solomon, M., and Young, J. (2018). Preoperative exercise halves the postoperative complication rate in patients with lung cancer: a systematic review of the effect of exercise on complications, length of stay and quality of life in patients with cancer. Br. J. Sports Med. 52:344. doi: 10.1136/bjsports-2017-098032
Stewart, A. L., Hays, R. D., and Ware, J. J. (1988). The MOS short-form general health survey. Reliability and validity in a patient population. Med. Care 26, 724–735. doi: 10.1097/00005650-198807000-00007
Suzuki, K., Saji, H., Aokage, K., Watanabe, S. I., Okada, M., Mizusawa, J., et al. (2019). Comparison of pulmonary segmentectomy and lobectomy: safety results of a randomized trial. J. Thorac. Cardiovasc. Surg. 158, 895–907. doi: 10.1016/j.jtcvs.2019.03.090
Wang, C. (2019). “The Relationship Between Social support, self-efficacy and Quality of Life in Patients with Lung Cancer ”, China: Shandong University).
Wang, X., Huang, Y. Q., Huang, Y. Q., Wang, J., Liu, J., Jin, L. M., et al. (2016). Comorbidity and risk factors of depressive and anxious symptoms in postoperative patients with lung tumor. Chin. Ment. Health J. 30, 401–405.
Wang, G. S., Wang, J., Rao, Z. P., Ding, G. G., and Wang, Z. (2015). Uniportal complete video-assisted thoracoscopic surgery lobectomy with partial pulmonary arterioplasty for lung cancer with calcified lymph node. J. Thorac. Dis. 7, 2366–2370. doi: 10.3978/j.issn.2072-1439.2015.12.50
Wilson, J. L., Louie, B. E., Cerfolio, R. J., Park, B. J., Vallières, E., Aye, R. W., et al. (2014). The prevalence of nodal upstaging during robotic lung resection in early stage non-small cell lung cancer. Ann. Thorac. Surg. 97, 1901–1907. discussion 1906-7. doi: 10.1016/j.athoracsur.2014.01.064
Yan, X., Chen, X., Li, M., and Zhang, P. (2019). Prevalence and risk factors of anxiety and depression in Chinese patients with lung cancer:a cross-sectional study. Cancer Manag. Res. 11, 4347–4356. doi: 10.2147/CMAR.S202119
Yeung, N. C., and Lu, Q. (2014). Affect as a mediator between self-efficacy and quality of life among Chinese cancer survivors in China. Eur J Cancer Care (Engl) 23, 149–155. doi: 10.1111/ecc.12123
Zeilinger, E. L., Oppenauer, C., Knefel, M., Kantor, V., Schneckenreiter, C., Lubowitzki, S., et al. (2022). Prevalence of anxiety and depression in people with different types of cancer or haematologic malignancies: a cross-sectional study. Epidemiol. Psychiatr. Sci. 31:e74. doi: 10.1017/S2045796022000592
Zeng, Q., Cao, H., Ma, Q., Chen, J., Shi, H., and Li, J. (2021). Appetite loss, death anxiety and medical coping modes in COVID-19 patients: a cross-sectional study. Nurs. Open 8, 3242–3250. doi: 10.1002/nop2.1037
Zheng, Y., Mao, M., Ji, M., Zheng, Q., Liu, L., Zhao, Z., et al. (2020). Does a pulmonary rehabilitation based ERAS program (PREP) affect pulmonary complication incidence, pulmonary function and quality of life after lung cancer surgery? Study protocol for a multicenter randomized controlled trial. BMC Pulm. Med. 20:44. doi: 10.1186/s12890-020-1073-6
Zhi, X. Y., Yu, J. M., and Shi, Y. K. (2015). Chinese guidelines on the diagnosis and treatment of primary lung cancer (2015 version). Cancer-Am. Cancer Soc. 121, 3165–3181. doi: 10.1002/cncr.29550
Zhu, Y., Chen, J., and Kou, H. T. (2019). Clinical observation of the effect of thoracoscopic radical esophagectomy on postoperative pulmonary function and quality of life. Journal of laparoscopic. Surgery, 24, 37–40. doi: 10.13499/j.cnki.fqjwkzz.2019.01.037
Zung, W. W. (1965). A SELF-RATING DEPRESSION SCALE. Arch. Gen. Psychiatry 12, 63–70. doi: 10.1001/archpsyc.1965.01720310065008
Keywords: anxiety, depression, medical coping mode, psychological status, lung cancer, surgery
Citation: Chen Y-p, Zhang Y, Chen X, Luo J, Chen Z, Zhao L, Xia G, Sui X and Li Y (2023) The effects of different surgical approaches on the psychological status, medical coping mode and quality of life of patients with lung cancer. Front. Psychol. 14:1039501. doi: 10.3389/fpsyg.2023.1039501
Edited by:
Clelia Madeddu, University of Cagliari, ItalyReviewed by:
Clizia Cincidda, University of Milan, ItalyHuiyuan Li, The Chinese University of Hong Kong, China
Copyright © 2023 Chen, Zhang, Chen, Luo, Chen, Zhao, Xia, Sui and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yunchen Li, bGhsaWh1YW5AY3N1LmVkdS5jbg==; Guili Xia, MzU0OTk2NDU0QHFxLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Yi-ping Chen
Yi-ping Chen Yi Zhang
Yi Zhang Xing Chen3
Xing Chen3 Guili Xia
Guili Xia Yunchen Li
Yunchen Li