- 1Clinical Epidemiology Unit, IDI-IRCCS, Rome, Italy
- 2Clinical Psychology Unit, IDI-IRCCS, Rome, Italy
- 3Department of Human Science, European University of Rome, Rome, Italy
- 4Dermatology Unit, IDI-IRCSS, Rome, Italy
Objectives: Non-melanoma skin cancers (NMSC) include two main types: basal cell carcinoma (BCC) and cutaneous squamous cell carcinoma (cSCC). Generic Health-Related Quality of Life (HRQoL) instruments revealed little to no HRQoL impairment in NMSC patients. Instead, the use of specific skin disease HRQoL tools contradicted those observations. For example, the Skin Cancer Index (SCI) was suggested as a validated instrument for the evaluation of the impact of skin cancers on HRQoL, and has already been validated in several languages, but not in Italian. The aim of this study is to testing some psychometric properties of the Italian version of the SCI questionnaire in a large sample of NMSC patients.
Methods: This is a cross-sectional, single-center, observational study. Firstly, different factor models proposed in the literature were compared and the model with the best fit was identified. Secondly, the psychometric properties of the SCI, convergent validity and reliability, were evaluated.
Results: The sample was composed of 371 NMSC patients. The factor analysis revealed that a revised version of the original model had the best fit [χ2(df = 85) = 354.53, p < 0.001, RMSEA = 0.09, CFI = 0.98, TLI = 0.97, SRMR = 0.03]. The SCI had satisfactory internal consistency for all subscales (Emotional subscale: ordinal alpha = 0.95; Social subscale: ordinal alpha = 0.94; Appearance subscale: ordinal alpha = 0.94). The convergent validity with Skindex-17 psychosocial subscale was adequate for all the SCI subscales (Emotional Subscale: rho = −0.50; Social Subscale: rho = −0.54; Appearance subscale: rho = −0.44; Total Skin Cancer Index: rho = −0.56; and p < 0.001).
Conclusion: The tested psychometric properties of the Italian version of the SCI may suggest that it is an appropriate tool to measure the HRQoL in NMSC patients, however, further studies are needed in order to confirm and tested other psychometric features of this tool.
Introduction
Non-melanoma skin cancers (NMSC) include two main types: basal cell carcinoma (BCC) and cutaneous squamous cell carcinoma (cSCC). Their incidence has been estimated to be 18–20 times higher than that of melanoma (Fania et al., 2021b). NMSC are an important health issue worldwide due to the aging population and the widespread sun exposure (Fania et al., 2020, 2021a). Even if the mortality from BCC is negligible, and even if the cSCC (whether in situ or as an invasive form) prognosis is good (with a 5-year survival ≥90%), these cancers can be associated with relevant morbidity (Miller and Weinstock, 1994; Skulsky et al., 2017) and a significant impact on people’s health related quality of life (HRQoL) (Chernyshov et al., 2015; Alam et al., 2018). Furthermore, recurrences and subsequent NMSC lesions occur often (Trakatelli et al., 2007) and temporary or permanent scars caused by treatment sequelae could be associated with functional and esthetic issues (Kauvar et al., 2015) that may considerably affect HRQoL (van der Geer et al., 2010).
Even though one of the first published studies addressing the effect of BCC on HRQoL demonstrated little impact with only minimal differences before and after treatment (Blackford et al., 1996), and a review by Gibbons et al. (2013) concluded that generic HRQoL instruments revealed little to no HRQoL impairment in NMSC patients (Gibbons et al., 2013), the use of specific skin disease HRQoL tools contradicted those observations.
As it is stressed by Sampogna et al. (2019), comparing HRQoL of melanoma and NMSC patients using Skindex-17, the symptomatic component of HRQoL was more affected in patients with NMSC than in those with melanoma (Sampogna et al., 2019), and even the impact on the psychosocial component was not negligible (Gaulin et al., 2015). Moreover, the Skindex (both in its extended version and in its 17-item version) is a widely recognized tool that has been used for many years to measure the quality of life of people with different skin disorders (Sampogna et al., 2012), has good psychometric properties and is adequately sensitive and reliable (Nijsten et al., 2006). In addition, this instrument contains a total score and a subscale score called “psychosocial subscale” that is well suited to comparison with SCI. For these reason, among others, we have chosen this tool for comparison.
The Skindex-17 and SCI both measure constructs such as psychological and social functioning, but only SCI contains three specific items related to patients’ appearance perception. Both questionnaires included a total HRQoL scale, so we hypothesized that the SCI and Skindex-17 would be highly correlated, but not overlapping, in their general HRQoL measurement.
As stated in a position paper of the European Academy of Dermatology and Venereology Task Force on Quality of Life (Chernyshov et al., 2019), the generic or even the dermatology-specific instruments may not be sensitive enough to measure the total impact of skin cancer on patient’s lives. The Skin Cancer Index (SCI; Rhee et al., 2006) was suggested as a validated instrument for the assessment of the impact of skin cancer on HRQoL, and has already been validated in several languages (i.e., English by Rhee et al., 2006; in Spanish by De Troya-Martín et al., 2015; and Canadian French by Moran et al., 2021).
A tool assessing HRQoL of NMSC patients is also needed for the Italian population, given their high life expectancy, the frequent occupational and leisure-time UV exposure, and the ever-increasing intensity of UV radiation. Therefore, the aim of the present study was to validate some psychometric properties of the Italian version of the SCI questionnaire in a large sample of NMSC patients. Specifically, the first aim was to compare different factor models proposed in the literature (Rhee et al., 2006; De Troya-Martín et al., 2015; Moran et al., 2021) and to identify the model with the best fit. The second aim was to investigate the convergent validity, and reliability of the SCI.
Materials and methods
Setting, study design, and sample
This is a cross-sectional, single-center, observational study. The research has been conducted in accordance with the Declaration of Helsinki (64th WMA General Assembly, Fortaleza, Brazil, October 2013) and was approved by the Institutional Ethical Committee (protocol number n°608/1, 17th September 2019). All studies are registered by the Institutional Ethical Committee, which in turn, every year, transfers relevant information (e.g., enrolment open or close, number of enrolled patients during the past year, etc.) to the Italian Ministry of Health.
Data were collected from October 10, 2019 to December 14, 2021 at the dedicated NMSC outpatients clinic of the dermatological research hospital IDI-IRCCS, Rome, Italy.
Being a registry-based study, no sample size or power calculation was performed, however, we have reached an adequate number of participants, considering a sample size of at least 50 patients adequate for the assessment as asserted by Terwee et al. (2007). Consecutive patients were enrolled within the framework of the IDI-IRCCS NMSC Registry. Included patients had to satisfy the following inclusion criteria: (i) history or clinical suspicion of NMSC diagnosed by expert dermatologists assigned to the specific NMSC outpatients clinic and following NCCN guidelines for NMSC (NCCN Guidelines® for Basal Cell Skin Cancer, Version. 1.2022, 2021; Schmults et al., 2021); (ii) a good fluency of spoken and written Italian, and (iii) the obtainment of the written informed consent, signed by the patient if 18-and-over years old or by a parent/guardian for patients younger than 18 years of age. Exclusion criteria were: (i) any diagnosed major psychiatric disorders or cognitive impairment.
Data collection procedures
Data collected included demographic and clinical information. Demographic variables included sex, age, weight, and height in order to calculate Body Mass Index (BMI), educational level, marital status, and job status (employment), alcohol and tobacco intake, and number of hours of sun exposure. Clinical variables included type of NMSC, family history of cancer, patient global assessment (PtGA), and physician global assessment (PGA). The PGA was ranked for each participant by the dermatologist during the medical examination. It is a frequently used measure to assess clinical severity in dermatology (Pascoe et al., 2015). The SCI and Skindex-17 questionnaires were handed out to the patients who agreed to complete them. The Skindex-17 (Nijsten et al., 2006) is a dermatological self-report HRQoL instrument composed by 17 items. Answers are given on a three-point Likert scale (i.e., “never” to “often/always”). It measures the burden of dermatologic conditions on two scales: psychosocial and symptoms. Higher scores correspond to a worst condition experienced by patients. In this sample the total and Skindex-17 subscale scores had an adequate reliability (i.e., Skindex-17 total score Cronbach alpha = 0.93; Symptoms subscale score: α = 0.82; Psychosocial subscale score: α = 0.92).
The research questionnaires and the clinical case report forms are then processed by trained personnel in the clinical epidemiology unit (i.e., NMS, SM, and RF) who perform data management, data entry, and quality control.
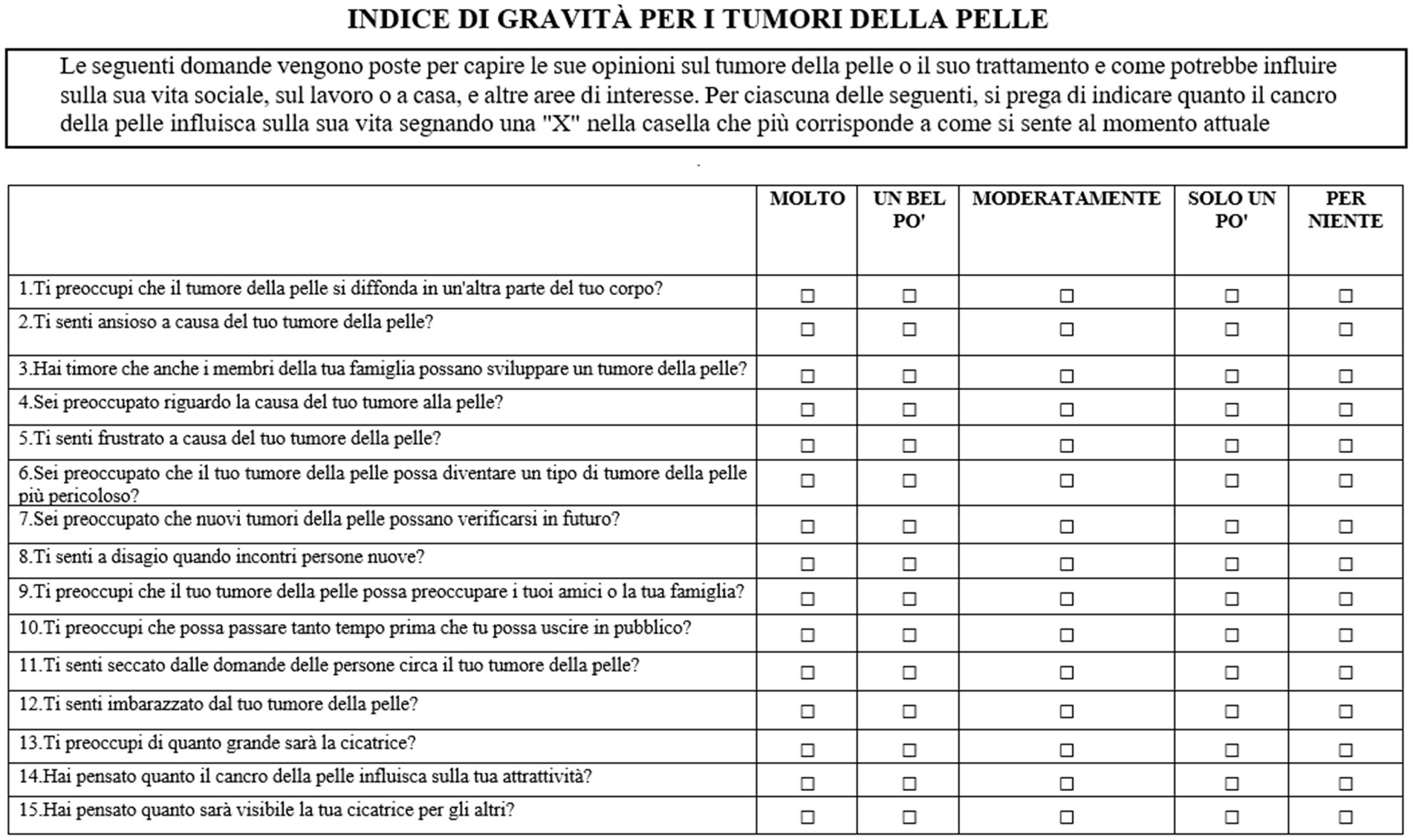
The skin cancer index
The skin cancer index (SCI; Rhee et al., 2007) is a 15-item self-report measure that so far has demonstrated the best evidence of its usefulness in patients with BCC and SCC (Lee et al., 2013). The SCI assesses HRQoL on three subscales: Emotional Subscale (i.e., anxiety, worry, and frustration), Social Subscale (i.e., meeting new people and going out in public), and Appearance Subscale (i.e., worry about dimension and noticeability of the scars). The scales are constituted by seven, four, and four items, respectively. Each item is rated on a five-point Likert scale, and the raw scores are transformed from a 0 (worst) to 100 (best) standardized score. Subscales total scores are obtained by summing the standardized scores and dividing by the number of items of each subscale. The total Skin Cancer Index score is computed by summing the subscale total scores and dividing by 3 (Rhee et al., 2006).
Differently from the original validation study (Rhee et al., 2006), De Troya-Martín et al. (2015) found evidence for a two-factor structure, combining the social and appearance subscales, which reported satisfactory Cronbach’s alpha (i.e., both of 0.87), with 12 items (items #2, #9, and #13 were removed because of low factor loadings). Also Moran et al. (2021) reported results for a two-factor structure, with no item removed, however, the model did not fit the data well [χ2(df = 89) = 326.44, p < 0.001, RMSEA = 0.12, 90% CI [0.11, 0.14], CFI = 0.96, TLI = 0.96]. Also, a one-factor model and a hierarchical model were tested, but both these models did not fit the data (Moran et al., 2021).
Study phases
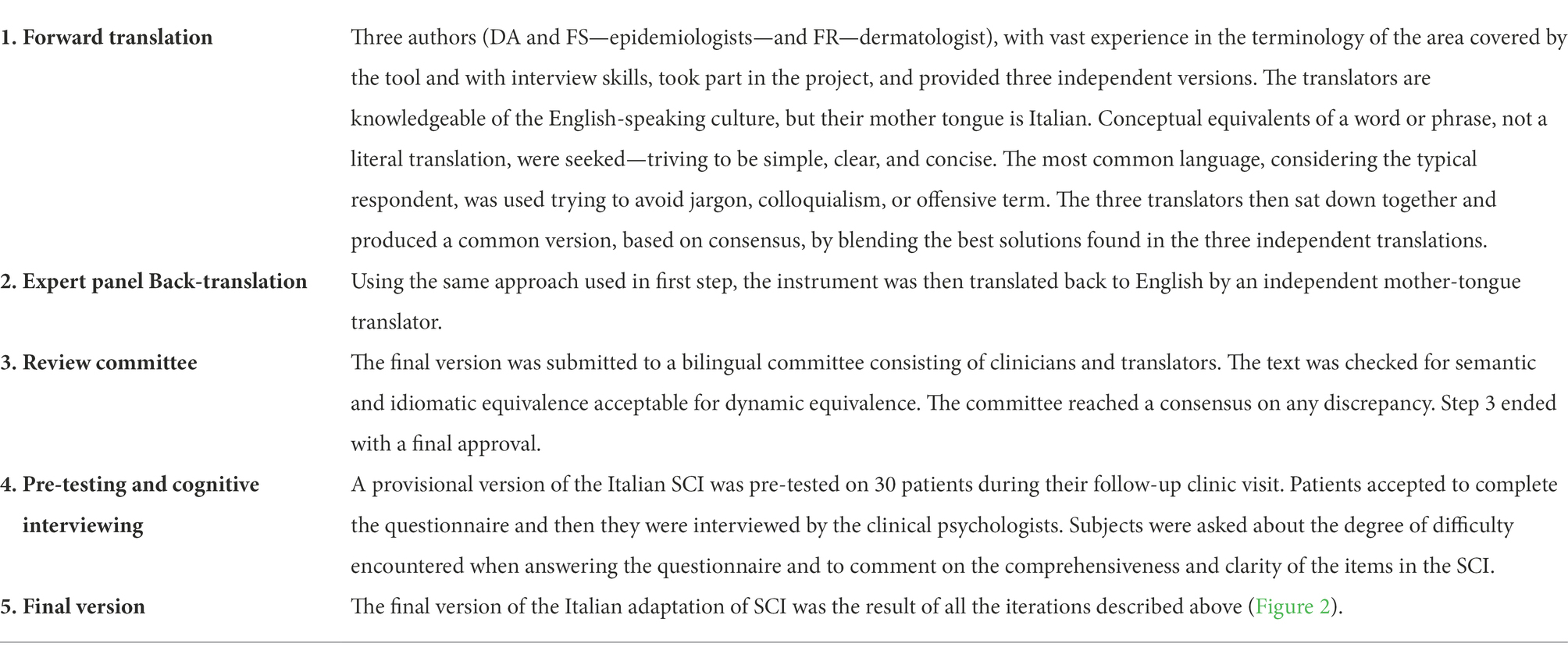
To adapt and validate the original SCI scale, a study with two consecutive phases was designed. The first phase, summarized in Table 1, referred to the Italian translation and adaptation of the SCI, and was carried out according to Beaton’s guidelines (Beaton et al., 2000). The second phase referred to the evaluation of the psychometric properties of the questionnaire. To assess the questionnaire’s factorial structure and reliability, exploratory factor analysis, and ordinal alpha were conducted, respectively. To indicate the convergent validity (i.e., the measurement of theoretically similar constructs that should be highly inter-correlated, that can be estimated using correlation coefficients), Spearman’s correlation analysis was performed with the Skindex-17 for which reliability and validity studies have been conducted in the Italian-speaking population (Nijsten et al., 2006).
Statistical analysis
All the analyses were performed with Mplus 8.3 (Los Angeles, CA: Muthén & Muthén; Muthén and Muthén, 2017), R Core Team (2021), and the Statistical Package for the Social Sciences (SPSS, 2013), and G power (Faul et al., 2007).
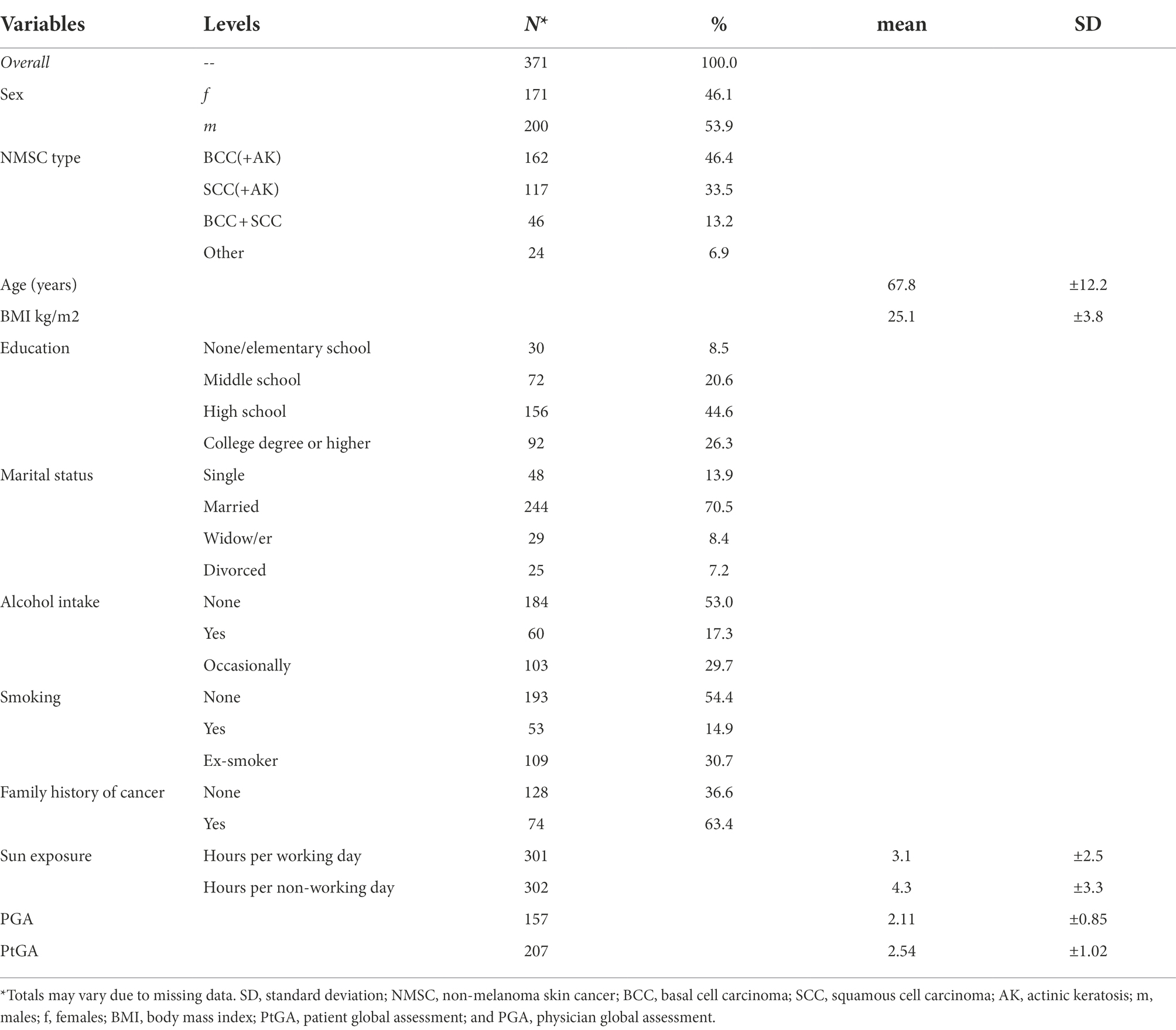
All patients who reported missing data in SCI and/or Skindex-17 questionnaire were excluded from the analyses. Instead, it was not possible to achieve the same in the socio-demographic variables; indeed, the exact frequencies of the available data are shown in Table 2. For the purpose of describing sociodemographic and clinical features of the sample, descriptive statistics were obtained through the computation of mean and standard deviation (SD) for the quantitative variables and through the frequency distribution for the qualitative ones.
To test whether the data were suitable for factor analysis, the Bartlett’s test of sphericity and the Kaiser–Meyer–Olkin (KMO) test were performed. Adequacy of the correlation matrix is suggested by a significant Bartlett’s test (p < 0.05) and a KMO index >0.70. Multiple Confirmatory Factor Analyses (CFAs) testing the different models proposed in the literature were conducted using a mean-and variance-adjusted weighted least square (WLSMV) estimator, given the categorical nature of the variables, with a polychoric correlation matrix. To perform a factor analysis a large sample size is required. The usually recommended minimum number of individuals is 200 (Kyriazos, 2018). Models fit were evaluated using the following indices: (1) the root mean square error of approximation (RMSEA), with values below 0.05 indicating evidence of absolute fit, values between 0.05 and 0.09 indicating the adequacy of the model, and values above or equal to 0.10 indicating the poor fit of the model (Browne and Cudeck, 1992; Hu and Bentler, 1999); (2) the Tucker–Lewis Index (TLI), with values >0.95 indicating the good fit of the model and values of 0.90 and higher an acceptable fit; (3) the Comparative Fit Index (CFI), with values >0.95 indicating good model fit and values of 0.90 and higher an acceptable fit; (4) the standardized root mean square residual (SRMR), with values <0.08 indicating good fit (Yu, 2002); and (5) the chi-square (χ2) test, with p values greater than 0.05 indicating an adequate fit to the data. However, χ2 is sensitive to sample size, and so p values might become significant for large samples (Schumacker and Lomax, 2012). In case of suboptimal fit of all the models tested, a parallel analysis (PAs; Horn, 1965) was performed to determine the number of factors to retain.
Eventually, if the model suggested in PA did not report a satisfactory fit, large modification indexes (>10) of the model with the most acceptable fit were inspected to look for refinements to add to the model. Modification indices (MIs) may suggest the need to add a path between variables or constraint/free one or more parameters. Values greater than 10 indicate that the model would be improved if a MI is applied, and the p value for the new parameter would be <0.001. However, since refinement of the factor model based on MIs is a data driven approach, modification indices should be considered one by one, and the model should be tested each time. A final CFA, based on the results from the MIs was performed, and model fit was evaluated with the same indices reported above.
Moreover, indices of internal consistency [i.e., ordinal alpha, the Molenaar Sijtsma statistic (MS), and latent class reliability coefficient (LCRC)] of the SCI were calculated. Ordinal alpha was used as a reliability estimations method, rather than Cronbach’s alpha, because the SCI is an ordinal type scale, which cannot be considered as continuous (Gadermann et al., 2012).
Convergent validity of SCI was assessed with Skindex-17 by examining the correlation between individual scores in SCI and in Skindex-17 subscales and total score. Factor scores of each SCI subscales were calculated and used to compute the correlation analyses. Finally, to assess the adequacy of our sample size for convergent validity, a G Power analysis (Faul et al., 2007) was conducted. A minimum of 64 participants was required to provide adequate statistical power (1-β = 80%) in order to detect a moderate effect size (ES = 0.30) with α =0.05.
Results
Three hundred and seventy-one patients diagnosed with NMSC, 53.90% males, with a mean age of 67.80 (±12.25) years, completed all questionnaires without any missing data. Mean PGA and PtGA scores for the present sample were attested at 2.11 (±0.85) and 2.54 (±1.02) respectively. We compared the patients included in this study (i.e., patients with complete answers to the SCI and the Skindex-17) with those who are in the registry but were excluded because of missing values, and we found no differences in age (t-test = 1.408, p = 0.993), gender [χ2(df = 1) = 0.799, p = 0.371], Physician Global Assessment (t-test = 1.439, p = 0.917), and Patient Global Assessment (t-test = 0.679, p = 0.408). Demographic and clinical data related to the patients are reported in Table 2.Totals of some variables in Table 2 may vary due to missing data (i.e., 22 missing for “NMSC type”; 21 missing data for “Education”; 25 missing item for “Marital status”; 24 missing data for “Alcohol intake”; 16 missing data for “Smoking”; 169 missing data for “Family history of cancer”; 214 missing data for “PGA”; and 164 missing data for “PtGA”; Table 2).
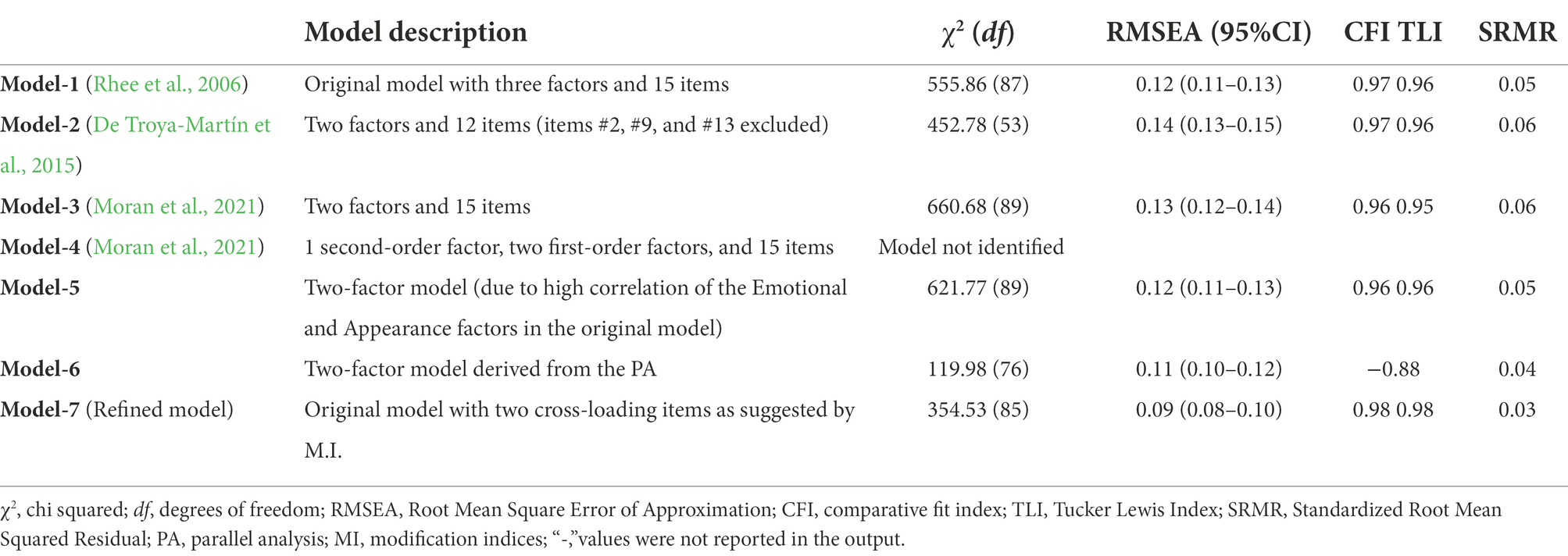
The correlation matrix was adequate for factor analysis (Bartlett’s test of sphericity = 4640.05; df = 105; p < 0.001; KMO = 0.93). Table 3 reports the fit of the competing models tested. The CFAs of the models proposed in the literature (Model-1, Model-2, and Model-3) did not fit the data well, while Model-4 was not identified. For all the models tested, all items reported high factor loadings (≥ 0.71), which did not identify the problematic items. Since the CFA of the original model indicated a high correlation between the Emotional and Appearance factors (r = 0.90), a two-factor model combining these two factors was tested (Model-5). However, it did not show a good fit. The PA suggested the presence of three factors, however, since only the third factor had an eigenvalue <1 (= 0.21) and reported low factor loadings (< 0.35) for all items, only a two-factor solution (Model-6) was retained, but it still did not yield a good fit.
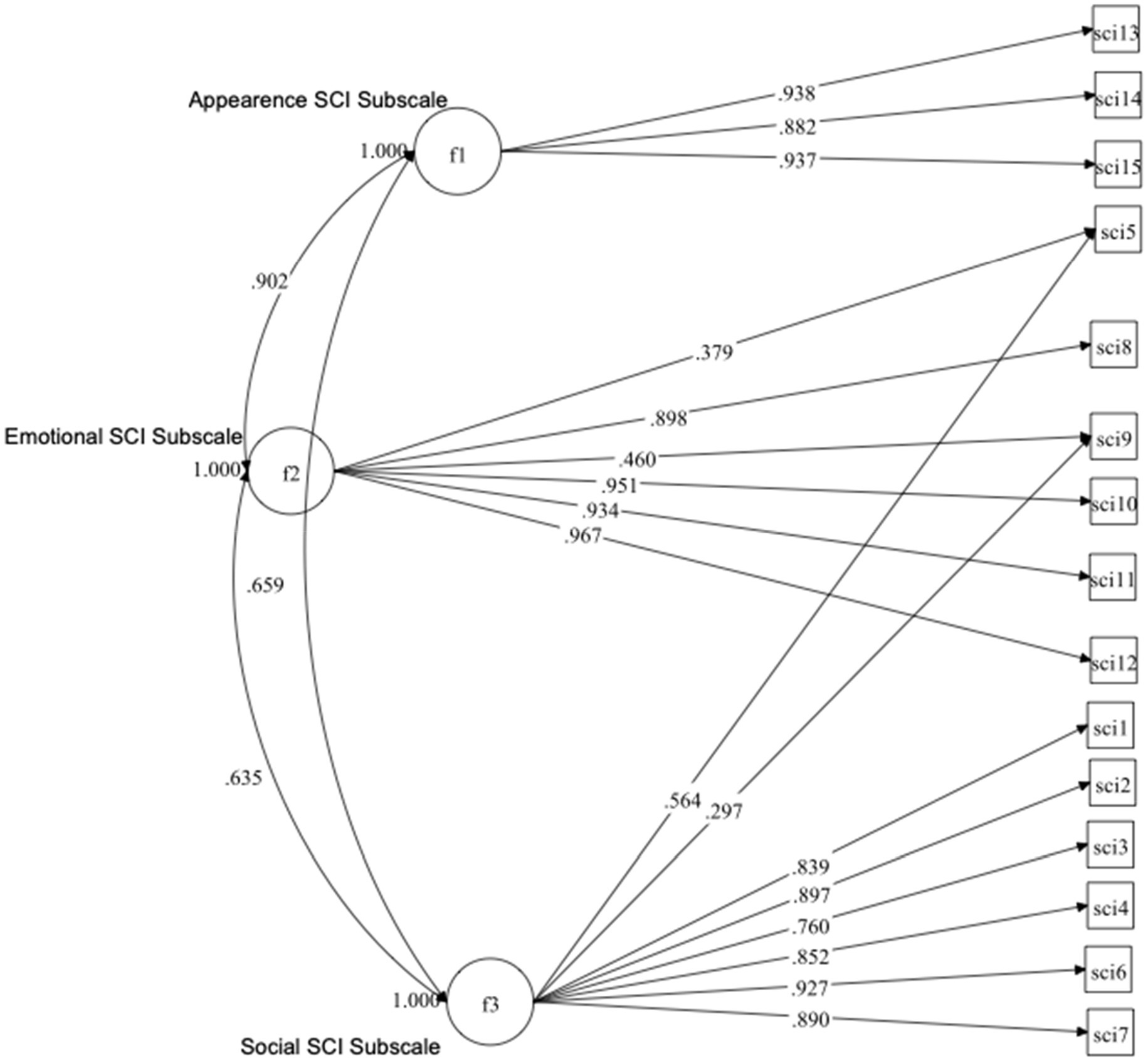
Since the original model (Model-1) showed the most acceptable fit, the MI of this model was looked-for. MIs suggested the cross-loadings of two items (item #5 and #9), which were associated with the highest estimated parameter change (0.49 and 0.50, respectively), and significant (p < 0.001) changes in the value of the χ2 statistic. Specifically, item #5, which belongs to the Social subscale, was suggested to cross-load in the Emotional subscale, and item #9, which belongs to the Emotional subscale, was suggested to cross-load in the Social subscale. The decision to add these two cross-loadings was also supported theoretically, since the meaning of these items fits both the Emotional and Social subscales (item #5, “Felt frustrated about your skin cancer?” and #9, “Felt concerned that your skin cancer may worry friends or family?”). The refined model (Model-7) had an acceptable fit to the data [χ2(df = 85) = 354.53, p < 0.001, RMSEA = 0.09, CFI = 0.98, TLI = 0.97, SRMR = 0.03; Figure 1].
The whole SCI scale had satisfactory internal consistency (ordinal alpha = 0.96, MS = 0.94, and LCRC = 0.95), as well as each subscale (Emotional: ordinal alpha = 0.95, MS = 0.91, and LCRC = 0.92; Social: ordinal alpha = 0.94, MS = 0.92, and LCRC = 0.92; Appearance: ordinal alpha = 0.94, MS = 0.90, and LCRC = 0.91). It is relevant to know that the reliability of each subscale was computed by including the fifth item in the Emotional subscale, and the ninth item in the Social subscale.
In Table 4, we reported the Spearman correlation coefficients between SCI subscales, SCI Total Skin Cancer Index, and Skindex-17 subscales. The scores of the Skindex-17 and SCI subscales (i.e., SCI Emotional subscale; SCI Social subscale; SCI Appearance subscale; Total Skin Cancer Index; Skindex-17 Psychosocial subscale; and Skindex-17 Symptoms subscale) were satisfactorily and significantly related to each other (p < 0.001).
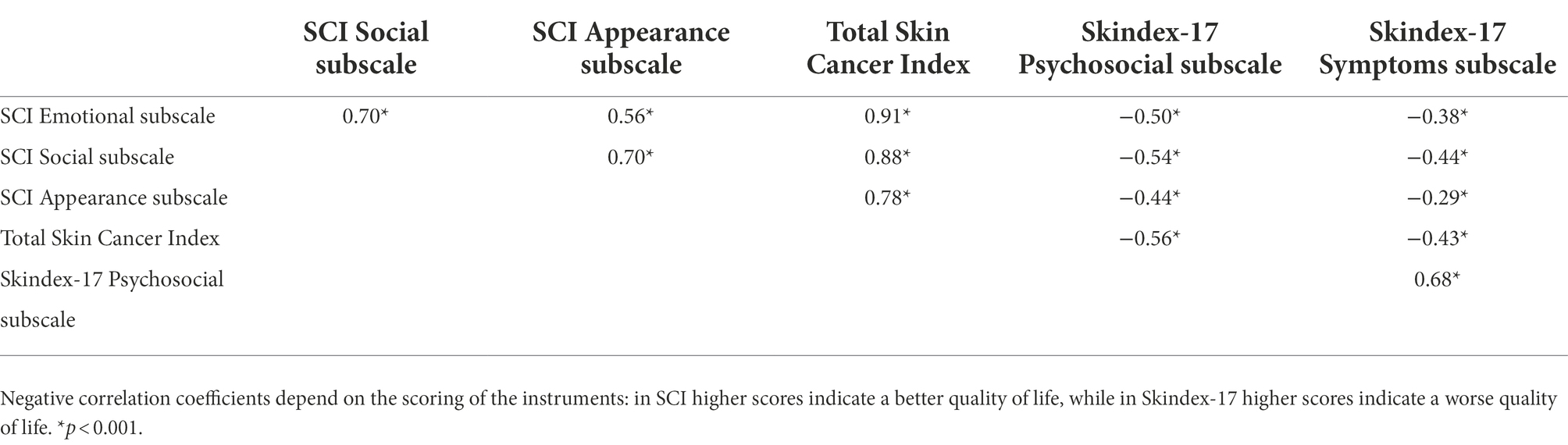
Table 4. Spearman correlation between SCI subscales, SCI Total Skin Cancer Index, and Skindex-17 subscales (N 371).
Discussion
This paper describes the adaptation and validation of some psychometric properties of the Italian version of the SCI, with the intent to achieve a linguistic and semantic equivalence with the original questionnaire proposed in English (Rhee et al., 2006). Our results supported the model originally proposed by Rhee et al., (2006), with three factors (corresponding to Appearance, Emotion, and Social subscales) and 15 items. As in the original instrument, our analysis identified two separate subscales for the evaluation of appearance and emotions. In fact, the first construct refers to worry about physical appearance, while the second focuses on worry, anxiety, and frustration due to the clinical characteristics of the condition. However, in the present study, we had to revise the original three-factor model by including two cross-loadings for items #5 and #9, as suggested by the MI. Specifically, item #5 (“Felt frustrated about your skin cancer?”), which loaded on the social subscale in the original model, was also loaded on the emotional subscale and item #9 (“Felt concerned that your skin cancer may worry friends or family?”), which loaded on the emotional subscale in the original model, was also loaded on the social subscale. This decision was also supported by considering the meaning of these items, which seem to assess both the social and emotional aspects at the same time. Perhaps this result was not found in other studies because of cultural differences, which can also explain why other studies reported findings for different numbers of factors and also had to remove some items. On the basis of this interpretation, we have decided to include the two cross-loadings to compute the subscales scores by using the factor scores. Therefore, both item #5 and item #9 were used to compute both Social and Emotional subscales scores. Moreover, these cross-loadings items seem to explain different aspects of each subscale, which would be missing if we did not include them to compute the subscales scores. Finally, the SCI index, as well as each subscale, showed satisfactory internal consistency.
This Italian adaptation was created following the current recommendations for the cultural adaptation and validation of patient-reported outcome measures (PROMs; Guillemin et al., 1993; Herdman et al., 1998; Beaton et al., 2000). As concerns manageability, the Italian adaptation of the SCI achieved a high degree of acceptability and patients did not require assistance to complete the questionnaire, managing to respond to all items in a self-administered way, through a Likert-scale evaluation. Moreover, the total and subscale scores are easy to obtain (i.e., summing each item score), and then it is possible to convert the total score to a scale from 0 to 100. None of these procedures require specific software.
Concerning field practice, SCI could be a particularly specific and useful tool that allows clinicians and researchers to analyze the psychological and emotional impact of NMSC on patients’ lives. This information allow to operationalize and compare the psychological impact of NMSC in the evaluation of potential therapeutic alternatives to invasive surgery for BCC. On the other side, SCI could help clinicians to recognize patients who need a more in-depth psychological assessment, in order to provide a specific psycho-oncological counseling to patients and/or their caregivers. From this perspective the SCI could also be considered as a screening tool useful to investigate the psychological well-being of patients suffering from NMSC.
The Italian version of the SCI showed good convergent validity with the Skindex-17, especially for the psychosocial scale.
As hypothesized, the SCI and the Skindex-17, despite being correlated, were not overlapping. This result confirms that dermatology-specific and NMSC-specific questionnaires do not measure the same aspects of HRQoL impairment. As stated in the position paper by Chernyshov et al. (2019), the dermatological component may not be the main source of problems in patients with skin cancer. Especially at a late stage of the disease, the psychological burden may overcome the skin problems and thus cancer-specific or disease-specific questionnaires may be more appropriate. The items of the SCI are particularly focused on worry, which is a component of anxiety and a frequent emotion in people with cancer in general, and in particular in NMSC (Khoshab et al., 2020). In fact, it has been observed that even after surgery, patients with facial NMSC report cancer worry (van Hensbergen et al., 2022), and such emotion has a strong impact on patients’ quality of life and wellbeing (Radiotis et al., 2014). In this sample, the SCI had satisfactory internal consistency for all subscales. For this reason, it could be possible to assert that SCI has a good possibility in proving that the different test-items who belong to the same construct produce similar results. So, the three constructs assessed by SCI are consistent and related but only partially overlapping. From this evidence, it is possible to hypothesize that a low level of self-appearance acceptance could have repercussions in psychological or social well-being, or it may also be possible that people with better levels of social and psychological life could better accommodate appearance issues resulting from NMSC sequelae.
The current study and the Italian version of the SCI have various strengths. As for the study: (i) we used an up-to-date statistical approach which also considered the categorical nature of the variables analyzed; (ii) we were also able to investigate the validity of the SCI; (iii) this Italian adaptation has demonstrated a high structural similarity with the original model (Rhee et al., 2006); and (iv) the women/men ratio in our sample was well balanced.
However, some limitations of this study affecting the generalizability of the results should also be noted. First, we did not investigate the stability of the factor structure of the SCI over time. Second, given the cross-sectional nature of the data, test–retest validity could not be assessed. Future studies will be needed to investigate and confirm our results on the factorial structure of SCI. Moreover, multi-group CFA for measurement invariance of the SCI are needed to compare the results across different language versions of the questionnaire and cultures. In the current study, we were not able to perform a measurement of invariance analysis due to not adequate sample size (< 200 subjects for the female group; Meade, 2005). Third, the presence of cross-loadings suggests that the SCI needs to be extensively revised. This is also supported by the fact that the results of the PA did not match the ones reported by the CFA (Li et al., 2020) and, also, by the fact that the other studies that tried to validate the SCI in other languages reported different findings in matter of its factor structure.
Finally, it was not possible to quantitatively depict the clinical or demographic features of participants who refused to took part to the research, because no systematic data collection was performed. This could be a limit in considering the tool manageability. However, from a qualitative point of view, the reasons that led the participants to refuse were: advanced age, contextual or chronic sensory, and/or motor deficits (due to the advanced age, a typical feature of the population affected by NMSC), and difficulties in getting space and time that are due to the setting in which the study was carried out.
In conclusion, the SCI could be a promising tool for assessing the quality of life, self-acceptance, social and psychological problems of people with NMSC, also in the Italian context. However, other research is needed to test in different contexts the features of this tool.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Istituto Dermopatico dell’Immacolata Ethical Committee, IDI-IRCCS. The patients/participants provided their written informed consent to participate in this study.
Author contributions
TS, FR, FS, and DA: conceptualization. SM, RF, NMS, AD, EP, TS, and LF: enrollment and data curation. GR, TS, and DA: methodology and formal analysis. FS, FR, and DA: project administration and supervision..TS and GR: writing—original draft. All authors contributed to the article and approved the submitted version.
Funding
This study was supported in part by “Progetto Ricerca Corrente 2021–2022” of the Italian Ministry of Health.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alam, M., Armstrong, A., Baum, C., Bordeaux, J. S., Brown, M., Busam, K. J., et al. (2018). Guidelines of care for the management of cutaneous squamous cell carcinoma. J. Am. Acad. Dermatol. 78, 560–578. doi: 10.1016/j.jaad.2017.10.007
Beaton, D. E., Bombardier, C., Guillemin, F., and Ferraz, M. B. (2000). Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 25, 3186–3191. doi: 10.1097/00007632-200012150-00014
Blackford, S., Roberts, D., Salek, M. S., and Finlay, A. (1996). Basal cell carcinomas cause little handicap. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehab. 5, 191–194. doi: 10.1007/BF00434740
Browne, M. W., and Cudeck, R. (1992). Alternative ways of assessing model fit. Sociol. Methods Res. 21, 230–258. doi: 10.1177/0049124192021002005
Chernyshov, P. V., Lallas, A., Tomas-Aragones, L., Arenbergerova, M., Samimi, M., Manolache, L., et al. (2015). Quality of life in non-melanoma skin cancer. Br. J. Dermatol. 33, 816–827. doi: 10.1111/jdv.15487
Chernyshov, P. V., Lallas, A., Tomas-Aragones, L., Arenbergerova, M., Samimi, M., Manolache, L., et al. (2019). Quality of life measurement in skin cancer patients: literature review and position paper of the European academy of dermatology and venereology task forces on quality of life and patient oriented outcomes, melanoma and non-melanoma skin cancer. J. Eur. Acad. Dermatol. Venereol. 33, 816–827. doi: 10.1111/jdv.15487
De Troya-Martín, M., Rivas-Ruiz, F., Blázquez-Sánchez, N., Fernández-Canedo, I., Aguilar-Bernier, M., Repiso-Jiménez, J. B., et al. (2015). A Spanish version of the skin cancer index: a questionnaire for measuring quality of life in patients with cervicofacial nonmelanoma skin cancer. Br. J. Dermatol. 172, 160–168. doi: 10.1111/bjd.13173
Fania, L., Didona, D., Di Pietro, F. R., Verkhovskaia, S., Morese, R., Paolino, G., et al. (2021a). Cutaneous squamous cell carcinoma: from pathophysiology to novel therapeutic approaches. Biomedicine 9. doi: 10.3390/biomedicines9020171
Fania, L., Didona, D., Morese, R., Campana, I., Coco, V., Di Pietro, F. R. F. R. F. R., et al. (2020). Basal cell carcinoma: from pathophysiology to novel therapeutic approaches. Biomedicine 8, 488. doi: 10.3390/biomedicines8110449
Fania, L., Samela, T., Moretta, G., Ricci, F., Dellambra, E., Mancini, M., et al. (2021b). Attitudes among dermatologists regarding non-melanoma skin cancer treatment options. Discov. Oncol. 12:31. doi: 10.1007/s12672-021-00421-w
Faul, F., Erdfelder, E., Lang, A. G., and Buchner, A. G. (2007). G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior research methods 39, 175–191.
Gadermann, A. M., Guhn, M., and Zumb, B. D. (2012). Estimating ordinal reliability for Likert-type and ordinal item response data: A conceptual, empirical, and practical guide. Practical Assessment, Research, and Evaluation 17, 3.
Gaulin, C., Sebaratnam, D. F., and Fernández-Peñas, P. (2015). Quality of life in non-melanoma skin cancer. Australas. J. Dermatol. 56, 70–76. doi: 10.1111/ajd.12205
Gibbons, E., Comabella, C, C. I., and Fitzpatrick, R. (2013). A structured review of patient-reported outcome measures for patients with skin cancer, 2013. Br. J. Dermatol. 168, 1176–1186. doi: 10.1111/bjd.12310
Guillemin, F., Bombardier, C., and Beaton, D. (1993). Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J. Clin. Epidemiol. 46, 1417–1432. doi: 10.1016/0895-4356(93)90142-N
Herdman, M., Fox-Rushby, J., and Badia, X. (1998). A model of equivalence in the cultural adaptation of HRQoL instruments: the universalist approach. Qual. Life Res. 7, 323–335. doi: 10.1023/A:1024985930536
Horn, J. L. (1965). A rationale and test for the number of factors in factor analysis. Psychometrika 30, 179–185. doi: 10.1007/BF02289447
Hu, L. T., and Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model. 6, 1–55. doi: 10.1080/10705519909540118
Kauvar, A. N. B., Cronin, T. Jr., Roenigk, R., Hruza, G., and Bennett, R. (2015). Consensus for nonmelanoma skin cancer treatment: basal cell carcinoma, including a cost analysis of treatment methods. Dermatol. Surg. 41, 550–571. doi: 10.1097/DSS.0000000000000296
Khoshab, N., Vaidya, T. S., Dusza, S., Nehal, K. S., and Lee, E. H. (2020). Factors contributing to cancer worry in the skin cancer population. J. Am. Acad. Dermatol. 83, 626–628. doi: 10.1016/j.jaad.2019.09.068
Lee, E. H., Klassen, A. F., Nehal, K. S., Cano, S. J., Waters, J., and Pusic, A. L. (2013). A systematic review of patient-reported outcome instruments of nonmelanoma skin cancer in the dermatologic population. J. Am. Acad. Dermatol. 69, e59–e67. doi: 10.1016/j.jaad.2012.09.017
Kyriazos, T. A. (2018). Applied psychometrics: sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology, 9, 2207.
Li, Y., Wen, Z., Hau, K.-T., Yuan, K.-H., and Peng, Y. (2020). Effects of cross-loadings on determining the number of factors to retain. Struct. Equ. Model. Multidiscip. J. 27, 841–863. doi: 10.1080/10705511.2020.1745075
Meade, A. W. (2005). “Sample size and tests of measurement invariance.” in Paper presented at the 20 th Annual Conference of the Society for Industrial and Organizational Psychology. Los Angeles, CA.
Miller, D. L., and Weinstock, M. A. (1994). Nonmelanoma skin cancer in the United States: incidence. J. Am. Acad. Dermatol. 30, 774–778. doi: 10.1016/S0190-9622(08)81509-5
Moran, C., Coroiu, A., and Körner, A. (2021). Psychosocial distress in patients with cutaneous melanoma: validation of the skin cancer index (SCI). Support Care Cancer 29, 1005–1014. doi: 10.1007/s00520-020-05568-w
Muthén, L. K., and Muthén, B. (2017). Mplus User's Guide: Statistical Analysis With Latent Variables, User's Guide, Los Angeles, CA: Muthén & Muthén.
Nijsten, T. E. C., Sampogna, F., Chren, M. M., and Abeni, D. D. (2006). Testing and reducing Skindex-29 using rasch analysis: Skindex-17. J. Investig. Dermatol. 126, 1244–1250. doi: 10.1038/sj.jid.5700212
Pascoe, V. L., Enamandram, M., and Corey, K. C. (2015). Using the Physician Global Assessment in a Clinical Setting to Measure and Track Patient Outcomes. JAMA Dermatol 151, 375–381. doi: 10.1001/jamadermatol.2014.3513
R Core Team (2021). "R: A language and enviroment for statistical computing". (Vienna: R Foundation for Statistical Computing).
Radiotis, G., Roberts, N., Czajkowska, Z., Khanna, M., and Körner, A. (2014). Nonmelanoma skin cancer: disease-specific quality-of-life concerns and distress. Oncol. Nurs. Forum 41, 57–65. doi: 10.1188/14.onf.57-65
Rhee, J. S., Matthews, B. A., Neuburg, M., Logan, B. R., Burzynski, M., and Nattinger, A. B. (2006). Validation of a quality-of-life instrument for patients with nonmelanoma skin cancer. Arch. Facial Plast. Surg. 8, 314–318. doi: 10.1001/archfaci.8.5.314
Rhee, J. S., Matthews, B. A., Neuburg, M., Logan, B. R., Burzynski, M., and Nattinger, A. B. (2007). The skin cancer index: clinical responsiveness and predictors of quality of life. Laryngoscope 117, 399–405. doi: 10.1097/MLG.0b013e31802e2d88
Sampogna, F., Paradisi, A., Iemboli, M. L., Ricci, F., Sonego, G., and Abeni, D. (2019). Comparison of quality of life between melanoma and non-melanoma skin cancer patients. Eur. J. Dermatol. 29, 185–191. doi: 10.1684/ejd.2019.3523
Sampogna, F., Tabolli, S., Abeni, D., and Abeni, D. (2012). Living with psoriasis: prevalence of shame, anger, worry, and problems in daily activities and social life. Acta dermato-venereologica, 92.
Schmults, C. D., Blitzblau, R., Aasi, S. Z., Alam, M., Andersen, J. S., Baumann, B. C., and Nguyen, M. Q. (2021). NCCN Guidelines® insights: squamous cell skin cancer, version 1.2022: Featured updates to the NCCN guidelines. Journal of the National Comprehensive Cancer Network, 19, 1382–1394.
Schumacker, R. E., and Lomax, R. G. (2012). A Beginner's Guide to Structural Equation Modeling. 3rd Edn.
Skulsky, S. L., O'Sullivan, B., McArdle, O., Leader, M., Roche, M., Conlon, P. J., et al. (2017). Review of high-risk features of cutaneous squamous cell carcinoma and discrepancies between the American joint committee on cancer and NCCN clinical practice guidelines in oncology. Head Neck 39, 578–594. doi: 10.1002/hed.24580
Terwee, C. B., Bot, S. D., de Boer, M. R., van der Windt, D. A., Knol, D. L., Dekker, J., et al. (2007). Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 60, 34–42. doi: 10.1016/j.jclinepi.2006.03.012
Trakatelli, M., Ulrich, C., Del Marmol, V., Euvard, S., Stockfleth, E., and Abeni, D. (2007). Epidemiology of nonmelanoma skin cancer (NMSC) in Europe: accurate and comparable data are needed for effective public health monitoring and interventions. Br. J. Dermatol. 156, 1–7. doi: 10.1111/j.1365-2133.2007.07861.x
van der Geer, S., Reijers, H. A., van Tuijl, H. F. J. M., de Vries, H., and Krekels, G. A. M. (2010). Need for a new skin cancer management strategy. Arch. Dermatol. 146, 332–336. doi: 10.1001/archdermatol.2010.1
van Hensbergen, L. J., Veldhuizen, I. J., Lee, E. H., Houterman, S., Brinkhuizen, T., van der Hulst, R. R. W. J., et al. (2022). Cancer worry after facial nonmelanoma skin cancer resection and reconstruction: a 1-year prospective study. Psycho-Oncology 31, 238–244. doi: 10.1002/pon.5810
Keywords: keratinocytes, outcome measure (healthcare), psychodermatology, skin disease, italian preliminary validation
Citation: Samela T, Raimondi G, Sampogna F, Ricci F, Fania L, Mastroeni S, Fusari R, Melo Salcedo N, Dattolo A, Papanikolaou ES and Abeni D (2022) Testing some psychometric properties of the Italian version of the Skin Cancer Index: A questionnaire for measuring quality of life in patients with non-melanoma skin cancer. Front. Psychol. 13:991080. doi: 10.3389/fpsyg.2022.991080
Edited by:
Semira Tagliabue, Catholic University of the Sacred Heart, Brescia, ItalyReviewed by:
Joan Trujols, Hospital de la Santa Creu i Sant Pau, SpainLucia C. Pérez-Herrera, Unimeq-Orl, Colombia
Songlin He, Chongqing Medical University, China
Copyright © 2022 Samela, Raimondi, Sampogna, Ricci, Fania, Mastroeni, Fusari, Melo Salcedo, Dattolo, Papanikolaou and Abeni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tonia Samela, t.samela@idi.it
 Tonia Samela
Tonia Samela