
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CONCEPTUAL ANALYSIS article
Front. Psychol. , 03 October 2022
Sec. Psycho-Oncology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.973640
This article is part of the Research Topic Psychosocial Rehabilitation for Cancer Patients View all 13 articles
Background: In extant literature, the concept of social isolation has been explored primarily in the context of older adults. However, people with cancer may also experience social isolation, and there is a need for increased clarity regarding this phenomenon in this population.
Objective: To conceptualize social isolation in adult cancer care.
Methods: PubMed, Web of Science, PsycINFO, CINAHL, China National Knowledge Infrastructure, Wanfang Data, and the Chinese Biomedical Literature Database were systematically searched using the key terms “cancer,” “social isolation,” “social alienation,” and “social exclusion” for studies (from the earliest date available to June 2022). The main disciplines involved were psychology, nursing, medicine, and public health. Rodgers’ evolutionary concept analysis was employed to clarify the antecedents, attributes, and consequences of social isolation in adults with cancer.
Results: A total of 60 eligible articles were reviewed entirely and the main findings were categorized into antecedents, attributes, and consequences. The antecedents of social isolation were classified into six categories: cancer-related physiological changes, cognitive beliefs, psychological wellbeing, unsatisfactory social supports or relationships, restrictions associated with receiving treatments, and social-level barriers. Attributes were characterized according to behavior or social avoidance and negative affective experiences, while consequences were attributed to low therapeutic compliance, poor health conditions and mental health problems, and low quality of life. White’s heuristic model is a potential theoretical context applicable to social isolation in adults with cancer.
Conclusion: This concept analysis provides a basis for developing multidimensional assessment tools and measures to alleviate social isolation in adults with cancer, a complex and varied phenomenon. However, while this review contributes to the current knowledge on social isolation in people with cancer, studies should further investigate the relationships among attributes associated with social isolation.
Globally, over 19 million individuals are diagnosed with cancer annually (Sung et al., 2021). Cancer diagnosis and treatment can cause severe adversity, resulting in varying psychological distress levels (Sender et al., 2020). However, with advances in healthcare, survival rates are also higher, and there is now increased advocacy to enhance the quality of survivorship care. Consequently, treatment goals include improving patients’ quality of life, symptom management, and psychosocial effects (Bray et al., 2018; Nekhlyudov et al., 2019). Despite this, limited attention has been paid to severe psychosocial issues, among which social isolation is one.
The term “social isolation” was introduced in Berkman and Syme’s (1979) seminal study. Initially, it referred to individuals who lacked social networks or had limited social supports. Thereafter, it was developed concurrently across multiple disciplines including public health, medicine, and nursing (Nicholson, 2009). In public health literature, the definition of social isolation evolved from “…irreversible loss of social bonds” (Berkman, 1983) to “lack of attachments within a person’s social network” (LaVeist et al., 1997). In the context of nursing, the subjective feeling of the unmet needs for social connections or supports and experiences of loneliness have been emphasized (Lien-Gieschen, 1993; Biordi, 1998; Ackley and Ladwig, 2004), while medicine views it as an objective indicator of social contact (Havens et al., 2004). The final definition of this concept incorporates both subjective and objective measures. Specifically, social isolation is characterized by minimal contact with other people and limited involvement in community affairs (Iredell et al., 2004).
The aforementioned definitions of social isolation have generally been developed with reference to older adults. Thus, an oncology-specific multidimensional definition of social isolation is yet to be clarified. The experience of social isolation and its associated attributes may differ among various age groups and by health conditions. Furthermore, social isolation is a phenomenon associated with severe health consequences and has been expanded to cancer. Specifically, in the context of oncology, social isolation has been analyzed primarily in patients with breast, prostate, head and neck, and lung cancers (Ettridge et al., 2018; Ashi et al., 2020; Dornan et al., 2021; Kudjawu and Agyeman-Yeboah, 2021).
Several studies underscore the impact of social isolation. Research indicates that social isolation is linked with the increased risk of tumor recurrence and mortality among patients with breast cancer (Kroenke et al., 2017). Friedler et al. (2015) summarized several studies on the pathophysiological mechanisms of social isolation, revealing that it affects the immune system, autonomic nervous system, and neuroendocrine axis. Moreover, long-term social isolation may increase the risk of mental illness (Yuan et al., 2020), reduce patient compliance with treatment, and increase cancer care costs (de Souza et al., 2017). Despite a lack of in-depth explorations, there is increasing evidence to suggest that social isolation could impact health in adults with cancer. This may be attributed to the different implications of social isolation between adults with cancer and older adults. The concept of social isolation in adults with cancer remains unclear. Therefore, this study aimed to clarify the meaning of social isolation in adults with cancer and examine its antecedents, attributes, and consequences by conducting a concept analysis.
Rodgers’ concept analysis method is an inductive process (Rodgers, 2000). In Rodgers’ view, concepts evolve and are shaped by the context in which they are used. Therefore, they are constantly developed and redefined. There have been studies on social isolation across various fields. Furthermore, the meaning of the associated terms has been established over the years. Thus, we applied Rodgers’ evolutionary concept analysis method and reviewed the literature on social isolation focusing on people with cancer to understand social isolation in the cancer context (Table 1; Rodgers, 2000).
We conducted systematic electronic searches (from the earliest date available to June 2022) of PubMed, Web of Science, PsycINFO, CINAHL, China National Knowledge Infrastructure, Wanfang Data, and the Chinese Biomedical Literature Database using combinations of the terms “cancer,” “social isolation,” “social alienation,” and “social exclusion” in the abstract or title. The inclusion criteria were articles that were published in English or Chinese; had undergone peer review (excluding dissertations, theses, or comments); and underscored social isolation in people with cancer, specifically concepts, antecedents, attributes, and consequences. Searches were conducted without any time and discipline constraints to ensure the identification of as many relevant articles as possible and to provide an overview of the concept’s use over time. The exclusion criteria were published abstracts of studies that did not contain specific information on social isolation and studies conducted on non-cancer populations.
The original search resulted in 711 articles after deleting duplicates using the NoteExpress 3.5.0.9054 software (Figure 1). Upon performing further screening based on the exclusion criteria by reading the titles and abstracts of the articles, a sample size of 312 was obtained. There was no consensus on the criteria for evaluation of the data sources included in the concept analysis; only articles that mentioned social isolation in people with cancer were included. Duplicate studies that were not recognized by the software were manually deleted. Studies with insufficient information regarding the characteristics of social isolation in people with cancer, making attribute identification difficult, were also removed. This resulted in the removal of 252 of the 312 studies. Rodgers (2000) recommends that the total number of references per discipline included in a study should be approximately 20% of the total. This was not feasible in the current study. To gain a deeper insight into social isolation, the remaining 60 selected studies were included in this concept analysis. Finally, the disciplines involved were psychology (n = 12), nursing (n = 24), medicine (n = 19), public health (n = 3), medical informatics (n = 1), and epidemiology (n = 1).
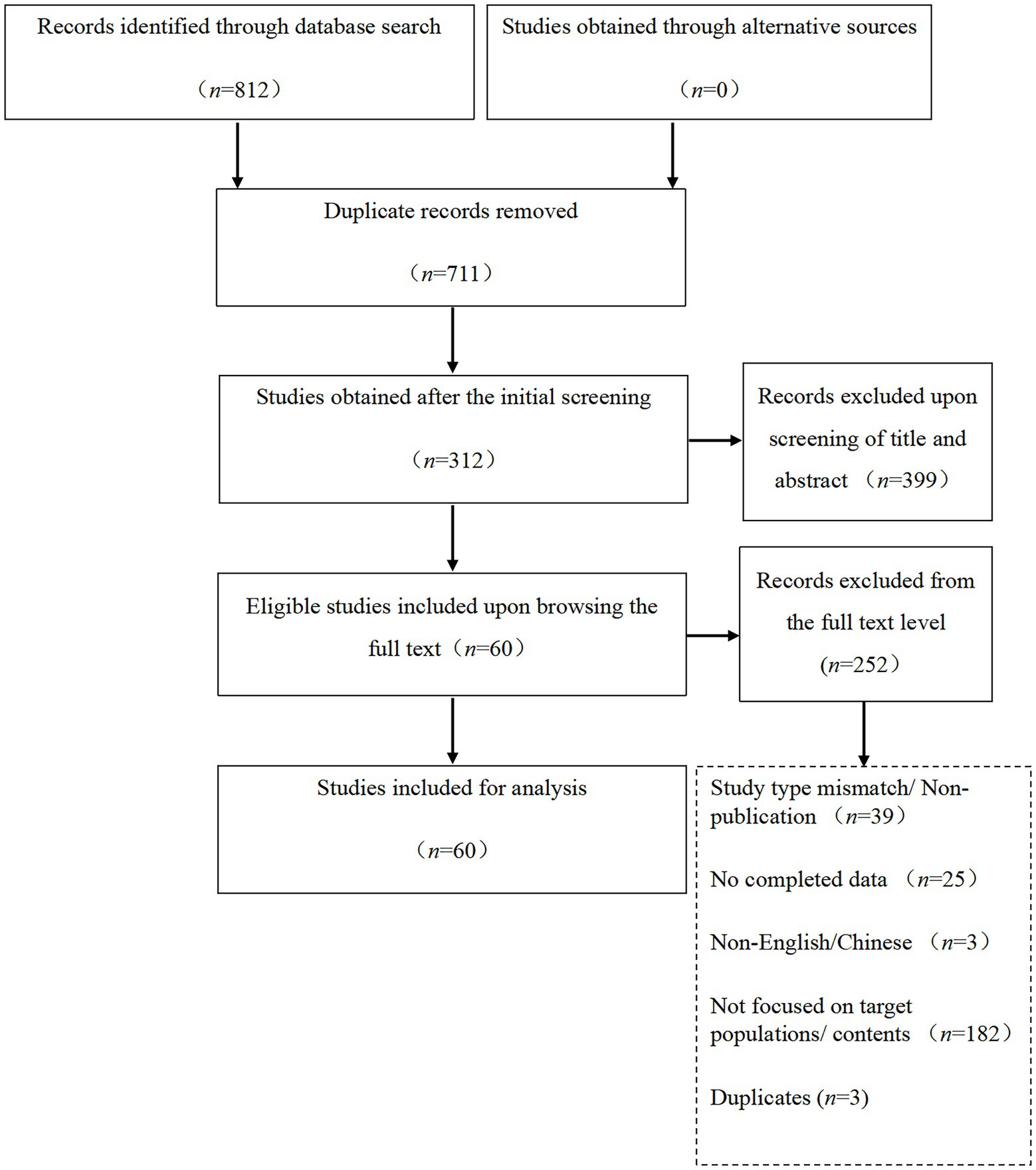
Figure 1. Flow chart of the study screening process. The studies obtained from each database are as follows: PubMed (n = 16), Web of Science (n = 5), PsycINFO (n = 22), CINAHL (n = 12), China National Knowledge Infrastructure (n = 3), Wanfang Data (n = 2), and the Chinese Biomedical Literature Database (n = 0).
Based on Rodgers’ method, the articles were studied for the identification of surrogate terms and related concepts. Furthermore, they were reviewed for systematic data collection and management in terms of attributes, antecedents, and consequences of the concept. The aforementioned information was extracted and tabulated. Among the 60 articles reviewed, an explicit definition of social isolation was rare. Thus, not all articles were extracted for their attributes of the concept. The data sources were reviewed by two of the researchers and checked by a third (Zhu et al., 2018). The matrix was developed by YL and MW.
The included articles were coded according to antecedents, attributes, consequences, surrogate terms, contextual basis, and theoretical and practical definitions. The coding was conducted using the standard procedure of thematic analysis underscored in Rodgers’ evolutionary method (Rodgers, 2000). Independently, two reviewers partially completed the work before discussing it with a third to reach a cohesive and comprehensive consensus to minimize bias as much as possible. Finally, the review team developed the conceptual definition of social isolation in people with cancer (Zhu et al., 2018).
The studies included in this analysis were published between 1980 and 2022; 55 were in English and five were in Chinese. Most employed cross-sectional and qualitative research designs. Patients with various types of cancer such as those affecting the lung, breast, head and neck, and prostate were included. The sample sizes ranged from three to 25,382. Only some studies included all the definitions, antecedents, attributes, and consequences of social isolation.
Multiple terms have been used interchangeably with social isolation. For example, social alienation has been used in place of social isolation (Yang et al., 2021). While the term “social exclusion” is distinct from “social isolation,” it has been used to describe social isolation in some studies (Dahill et al., 2020). There are two main concepts—alienation and loneliness—that need to be differentiated from social isolation. According to Seeman (1959), alienation encompasses powerlessness, isolation, normlessness, self-estrangement, and meaninglessness. Thus, isolation is only one psychological state of alienation. Some researchers use “loneliness” to express “social isolation.” However, we did not use “loneliness” as a surrogate term in our search; using “social isolation” and “loneliness” interchangeably can be confusing, as we found loneliness to be an attribute of social isolation (Raque-Bogdan, 2019; Raque-Bogdan et al., 2019).
Definitions of social isolation in adults with cancer have been presented in several studies with varying emphasis. Reduced social networks and loneliness are the most prevalent aspects of these definitions. Changing social health contexts, as influenced by factors such as coronavirus disease 2019 (COVID-19), have led to a spate of studies related to social isolation (Table 2).
A concept is defined by distinct meanings, referred to as attributes. Attributes comprise a set of characteristics that can be used to categorize similar situations related to a certain concept (Rodgers, 2000). During the analysis, two attributes underscored by succinct generalizations of social isolation in people with cancer emerged. These attributes recurred in the description of social isolation in data sources, and included behaviors and states of social avoidance as well as negative affective experiences. Studies supporting each attribute are shown in Table 3. Notably, there is a significant difference between external social isolation and perceived or internal social isolation. However, some patients experiencing the former (i.e., behaviors and states of social isolation) may not experience negative affective experiences. It is imprudent to classify all the behaviors and states of social avoidance simply as social isolation and ignore emotional isolation.
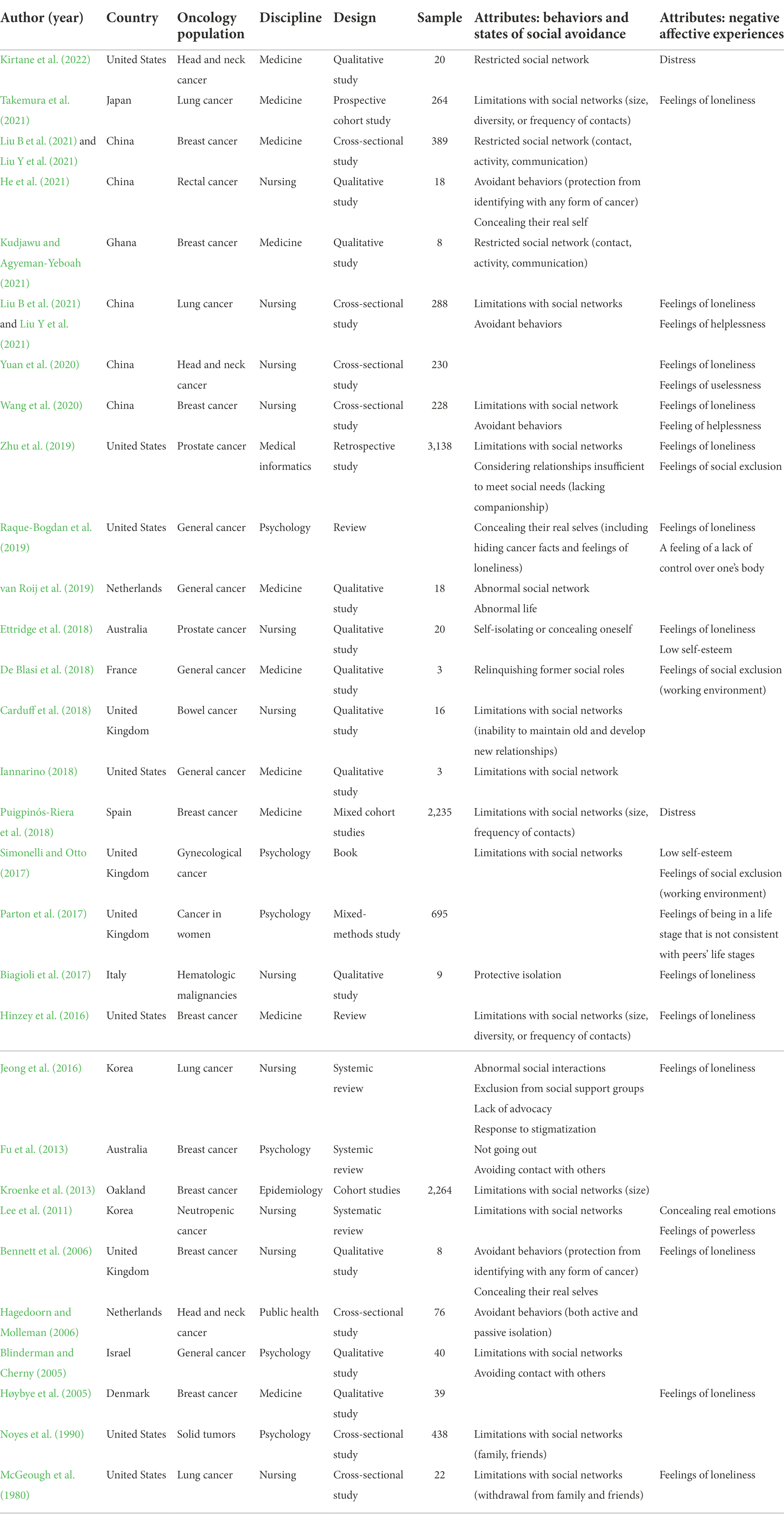
Table 3. Overview of the characteristics and attributes of social isolation defined in the studies included in the concept analysis.
States of social avoidance include limitations regarding social networks, which are determined by the frequency of social contact, activity, communication, size, and diversity (Liu B et al., 2021; Liu Y et al., 2021; Takemura et al., 2021). Discontinuing work after cancer diagnosis or treatment and relinquishing social roles are common for patients, and exacerbate feelings of isolation (De Blasi et al., 2018). To some extent, the choices of discontinuing work or relinquishing social roles belong to the social avoidance behavior attribute.
Some cancer survivors choose to self-isolate (Ettridge et al., 2018; He et al., 2021). They are often reluctant to communicate with others, specifically concerning details of their illness. Social avoidance behaviors are more common among patients with prostate and rectal cancer (Ettridge et al., 2018; Zhu et al., 2019; He et al., 2021). Social isolation can be a passive choice induced by the inability to socialize like before due to medical conditions, surgery, and treatment effects. Notably, some cancer survivors conceal their identities and emotions (including hiding cancer-related information and feelings of loneliness) to protect themselves or their loved ones. This paradoxical behavior, aiming to eliminate negative emotions such as loneliness while hiding critical health-related facts from medical staff, patients, and their loved ones, requires increased prioritization (Raque-Bogdan, 2019).
Loneliness has been reported as a negative effect among patients for several reasons. Cancer survivors experience distress, as they cannot speak about their illness with anyone except their intimate partners and medical specialists (Ettridge et al., 2018; Zhu et al., 2019).
Furthermore, low self-esteem, generally linked to self-discrimination, has been identified as a negative affective experience. Some patients may experience negative self-perception or self-denial due to cancer-related physiological changes, and thus avoid contact with people around them (Blinderman and Cherny, 2005; Ettridge et al., 2018). Behaviors and states of social avoidance and negative affective experiences are closely related. Another manifestation of low self-esteem is the fear of being humiliated in front of others (Johansson et al., 2005).
Feelings of social exclusion are common negative experiences resulting from the incapability to perform family or work roles owing to illness and result in survivors feeling excluded from society (Rhoten et al., 2013; Simonelli and Otto, 2017; De Blasi et al., 2018; Puigpinós-Riera et al., 2018). For some women and young adults, the feeling of being in a life stage that is not consistent with peers is also an attribute of social isolation (Parton et al., 2017; De Blasi et al., 2018; Iannarino, 2018).
Antecedents are events or phenomena that precede the concept (Rodgers, 2000). Six antecedents of social isolation were identified in adults with cancer. These included cancer-related physiological changes, cognitive beliefs, psychological wellbeing, unsatisfactory social supports or relationships, restrictions on receiving treatments, and social-level barriers.
Physiological change is the most common antecedent of social isolation among cancer survivors. Cancer survivors may experience physical and functional impairments caused by their illness and treatment, thus resulting in limited social integration (Noyes et al., 1990; Sandén and Hydén, 2002; Johansson et al., 2005; Lund-Nielsen et al., 2005; Bennett et al., 2006; Simonelli and Otto, 2017; De Blasi et al., 2018; Abdollahimohammad et al., 2019; Borgi et al., 2020; Stolley et al., 2020; Yuan et al., 2020; He et al., 2021; Kudjawu and Agyeman-Yeboah, 2021; Tsui and Huang, 2021). For instance, the complications associated with head and neck cancer, such as disfigurement, dysphagia, and speech impairment, can impair social functioning among survivors, exacerbating social isolation (Rogers et al., 2016; Moore et al., 2018; Kirtane et al., 2022). For gastrointestinal cancer survivors, gastrointestinal-specific morbidities such as ostomy leakage and incontinence deter them from an active social life (Martopullo et al., 2020; He et al., 2021). Other cancers (e.g., prostate, breast, and gynecological cancer) can impact survivors’ sexual life, as they may consider it an embarrassing topic to raise with friends and partners. These individuals need support, such as from peer groups, to express their challenges and share experiences (Sandén and Hydén, 2002; Power and Hegarty, 2010; Campo et al., 2017; Ettridge et al., 2018; Iannarino, 2018). Thus, as their physical health deteriorates, cancer survivors become weaker, more dependent, and socially isolated, resulting in their inability to socialize as well as maintain and form relationships (Schapmire et al., 2012; Carduff et al., 2018).
Cognitive beliefs are also an important antecedent of social isolation. These refer to a set of habitual pattern recognitions that one is used to, which is “fundamental to a person’s world view” (Charles et al., 2006). According to White’s heuristic cognitive behavioral model (White, 2000), false beliefs may lead to negative behavior (e.g., social avoidance). Regarding patients with rectal cancer tolerating stomas, two extreme attitudes can arise and prevent them from engaging in social activities. Stomas are sometimes treated inappropriately by patients who think their stomas are infectious and should quarantine themselves, while other times patients overprotect them, believing that they are fragile and thus should not be exposed (He et al., 2021). Recently, cognitive and psychological influencing factors such as body image, which can lead to social avoidance in people with head and neck cancer, have become research hotspots in the tumor population (Rhoten et al., 2013). While the underlying mechanism of social isolation in people with cancer is unclear, several theories can improve the understanding of the process that leads to it. The fear-avoidance model (Newell, 1999) explains cancer-related changes from a cognitive-behavioral perspective. Social avoidance behavior among cancer survivors is caused by the fear of changing appearances and functions. Fear and avoidance are conditioned reflexes maintained by learned thinking that constantly reminds individuals of their flaws. Individuals who are unable to adapt to physical deficiencies often continue to avoid society. Regarding nursing practice, social isolation can be guided by assessing the potential factors through understanding the avoidance behaviors demonstrated by patients based on this model.
Psychological wellbeing is integral to holistic health. Psychological discomfort serves as an antecedent of social isolation in people with cancer. It has been suggested that social isolation correlates positively with symptoms of anxiety and depression in patients with breast cancer (Liu B et al., 2021; Liu Y et al., 2021). Studies have shown that people with cancer with impaired psychological status demonstrate higher social isolation levels (Im and Chee, 2021). Furthermore, anxiety and depressive symptoms have been identified as common predictors in patients with oral cancer who exhibit increased social isolation levels due to stigma (Yuan et al., 2020). A qualitative study conducted in Ireland found that cancer survivors experience persistent symptoms of fatigue, anxiety, depression, and pain after receiving treatment, which increases their social isolation and reduces their activity levels. Notably, the first year after treatment involves managing the transition to survivorship and returning to daily life; survivors often feel isolated during this time (Boland et al., 2019).
Unsatisfactory social support is also an important antecedent of social isolation among cancer survivors. First, it may arise from not having someone with whom to discuss cancer-related matters (D’Agostino and Edelstein, 2013; Ettridge et al., 2018; Zhu et al., 2019). According to cancer survivors, their loneliness results from external avoidance and misunderstandings from others and cancer’s long-lasting impact (Fu et al., 2013; Hinzey et al., 2016; Raque-Bogdan et al., 2019; Kirtane et al., 2022). Second, the need for special attention for individuals with several intersecting identities might be unnoticed. It has been underscored that having several intersecting identities (e.g., lesbianism) may perpetuate a sense of isolation among individuals after a cancer diagnosis owing to previous experiences with societal oppression or marginalization. Thus, it is imperative to analyze individuals’ underlying identities and life experiences before the illness to provide tailored social supports (Raque-Bogdan, 2019). Moreover, individuals who live alone and do not have family or friends nearby may be more likely to experience social isolation (Fu et al., 2013; Ettridge et al., 2018; Leung et al., 2021). Some cancer survivors have reported that support from physicians and family members declines upon receiving treatment. This often leaves them feeling powerless and isolated because they still require care and support (Power and Hegarty, 2010; Kirtane et al., 2022).
Patients with neutropenic cancer are sometimes placed in protective isolation at the hospital, enhancing their sense of security during treatment. Patients often practice self-isolation by refusing to interact with people, both emotionally and physically, to protect both themselves and others. Specifically, these patients often feel powerless (Lee et al., 2011). Similarly, several patients with head and neck cancer required isolation for radiochemotherapy during the COVID-19 pandemic, which exacerbated social isolation (Kirtane et al., 2022).
Research has indicated that the public health events associated with COVID-19 social distancing measures imposed more loneliness and social isolation, which are both stress-inducing factors (Miaskowski et al., 2020; Kirtane et al., 2022). Several lung cancer survivors reported that they were excluded from social activities. Consequently, experiences of exclusion increased their reluctance to engage with society (Liu et al., 2016). In Syria, cancer is not sufficiently understood and accepted by the public, and people with cancer often fear that chemotherapy will prevent them from marrying owing to effects that may impact their social functioning (Nizamli et al., 2011).
Consequences refer to the results of corresponding events or phenomena (Rodgers, 2000). The literature suggests that social isolation is generally accompanied by three consequences, namely, low therapeutic compliance, poor health conditions and mental health status, and low quality of life.
The first consequence of social isolation is low therapeutic compliance. Healthcare professionals often emphasize treatment compliance to patients. However, perceived social isolation among patients with cancer negatively impacts their treatment compliance (de Souza et al., 2017; Iannarino, 2018; Martopullo et al., 2020; Stolley et al., 2020). The second consequence is poor health conditions and mental health status. A systematic review has indicated that social isolation and loneliness can increase mortality rates, regardless of their link to underlying medical conditions (Kroenke et al., 2013; Holt-Lunstad et al., 2015; Zhu et al., 2019). Furthermore, a high symptom burden is associated with loneliness and social isolation (Adams et al., 2018). Social isolation also has effects, as low emotional support and social isolation are clear risk factors for increased anxiety and depression (Puigpinós-Riera et al., 2018; Alcaraz et al., 2020). Furthermore, social isolation in people with cancer is a significant issue that could aggravate depressive symptoms and increase tumor activity owing to the decreased expression of brain-derived neurotrophic factors (Borgi et al., 2020). Moreover, it can potentially contribute to the development of breast cancer through hormonal, angiogenic, and inflammatory markers and mediators (Hinzey et al., 2016). Low or impaired quality of life is a major consequence of social isolation, and health-related quality of life may be negatively affected by social isolation (Simonelli and Otto, 2017; Iannarino, 2018; Dahill et al., 2020; Martopullo et al., 2020; Dornan et al., 2021; Leung et al., 2021; Takemura et al., 2021).
Based on the attributes, antecedents, and consequences identified in this analysis, we propose the following definition of social isolation in people with cancer:
Social isolation in adults with cancer refers to individuals demonstrating behaviors and states of social avoidance (e.g., avoiding contact with others and concealing one’s emotions) and experiencing specific negative affective experiences (e.g., feelings of loneliness). Social isolation can result from cancer-related physiological changes, cognitive beliefs, psychological well-being, unsatisfactory social supports or relationships, restrictions associated with receiving treatments, and social-level barriers. Social isolation can result in low therapeutic compliance, poor health conditions, mental health problems, and low quality of life.
Figure 2 illustrates the negative antecedents, attributes, and consequences associated with social isolation in people with cancer.
Clear and precise conceptual systems play a significant role in the development of nursing knowledge (Tofthagen and Fagerstrom, 2010). Based on current knowledge, this is the first study to conceptualize social isolation in adults with cancer. Previous studies have only provided an in-depth analysis of issues related to social isolation in older adults (Nicholson, 2009). Furthermore, studies have underscored the effects of social isolation at the physiological level (Friedler et al., 2015). However, limited studies in this regard focus on people with cancer, who are also affected severely by social isolation. This may be why social isolation in people with cancer has not been explained adequately using the social isolation concepts from other populations. Therefore, it is necessary to clarify this concept in the cancer population. This concept analysis has established a set of attributes to define social isolation in adults living with cancer. Using standardized language developed using the concept analysis procedure, nurses and physicians can assess social isolation among cancer survivors and differentiate it from that among older adults and non-cancer survivors. It is crucial to recognize that social isolation in cancer survivors is a multidimensional experience influenced by several factors, particularly cancer-related physiological changes.
In this analysis, the attributes of social isolation were classified into two categories, namely, behaviors and states of social avoidance and negative affective experiences. Insufficient social networks and feelings of loneliness were the most frequent characteristics of social isolation among the two categories. Table 3 indicates that only some of the included studies covered both categories. This may be owing to the varying cancer populations present in the included studies. Hence, the focus on social isolation in this analysis also differed.
No consensus was reached on the definition of social isolation in cancer populations. Compared to the behaviors and states of social avoidance, the negative affective experience attributes were more challenging to identify. Studies indicate that the latter attribute, which includes perceived social isolation and feelings of loneliness, is more harmful to mental health than the former (Liu B et al., 2021; Liu Y et al., 2021). Several patients were not aware that they were socially isolated despite having restricted social networks (Blinderman and Cherny, 2005; Tomaka et al., 2006). However, individuals can still feel lonely even if they are well-supported socially (Tomaka et al., 2006). Thus, it can be suggested that subjective or perceived social isolation warrants increased priority. During follow-up, nurses and physicians should pay close attention to the patient’s psychological changes and identify social isolation early.
White’s heuristic model stipulates that individuals will reshape their ideal self-image when their appearance and/or physical function are damaged (White, 2000). However, excessive expectations regarding their external image can lead to persistent and unpleasant emotions as well as social avoidance behaviors. Thus, people living with cancer may rebuild their ideal self-image after perceiving changes in appearance and physical function. However, owing to stigma, among other reasons, they could demonstrate compensatory behaviors to avoid social activities.
Notably, White’s heuristic model suggests that social isolation could result from incorrect self-perception, such as negative self-evaluation and unrealistic expectations. Furthermore, this model can enable nurses and physicians to analyze the internal influencing factors of social isolation among patients. Moreover, it suggests that nurses and physicians ought to predictably guide the establishment of improved self-cognition while providing psychological care to patients with cancer. It is imperative to address negative self-assessments among patients as soon as they exhibit social isolation behavior. Social isolation is a multidimensional experience, and its antecedents may comprise the aforementioned attributes; thus, future studies must provide an in-depth examination of the relationships among these attributes.
Identifying the attributes of social isolation in adults with cancer has profound implications. Along with the common attributes (i.e., limitations in social networks and feelings of loneliness), living an abnormal life and concealing individual emotions have been identified as characteristics of behaviors and states of social avoidance. The findings from this analysis illustrate the unique aspect of social isolation associated with cancer. Upon our review (Miaskowski et al., 2020; Morreale et al., 2020; Takemura et al., 2021), we also found that the measurement tools used to assess social isolation vary across studies. This confirms a lack of consensus on the concept of social isolation regarding cancer populations. Furthermore, it suggests that future research ought to explore and implement social isolation assessment tools that can perform standardized scoring to facilitate nursing assessment, as well as increase the comparability of this indicator in the cancer population. In future research, antecedent social health factors such as COVID-19 could enhance the complexity associated with the concept of social isolation. Thus, researchers should consider the issue more comprehensively.
Several limitations and biases have been identified in this analysis, including the interpretations of the results and the possibility of an incomplete search of sources. Despite following the guidance of the inductive process underscored in Rodgers’ evolutionary method (Rodgers, 2000), this analysis might contain bias. In an attempt to mitigate this, the process of data extraction was performed independently by two reviewers, and a third reviewer was consulted in case of a disagreement. While a systematic search was conducted, it is unlikely that it was comprehensive. Moreover, this concept analysis only included literature published in English and Chinese, as there is a more extensive volume of articles in these two languages.
The findings from this concept analysis contribute to the understanding and clarity of social isolation regarding adults with cancer. This analysis could be applied to developing cancer-specific assessment tools and measures that can facilitate early recognition of the requirements underlying psychosocial support and establish a conceptual foundation to mitigate social isolation regarding clinical practice and research. Subjective, perceived social isolation is of specific concern. Further studies are required to examine the relationships among attributes. Moreover, research mitigating social isolation is needed to assist people living with cancer to improve ways of adapting to adversity throughout their experience.
YL: conceptualization, methodology–data collection, methodology–data analysis, writing–original draft preparation, and writing–reviewing and editing. GH: resources and revision. MW: methodology–data collection and methodology–data analysis. LH: writing–review and editing and supervision. All authors contributed to the article and approved the submitted version.
This work was supported by the Shanghai Association For Science and Tech (21002411300) and Innovation research team of high-level local universities in Shanghai (SHSMU-ZDCX20212802).
We would like to thank Editage (www.editage.cn) for English language editing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abdollahimohammad, A., Firouzkouhi, M., and Naderifar, M. (2019). Lived experiences of Iranian cancer patients after survival: a phenomenological research. J. Patient Exp. 6, 164–168. doi: 10.1177/2374373518800783
Ackley, B. J., and Ladwig, G. B. (2004). Nursing diagnosis handbook: A guide to planning care. St. Louis: Mosby.
Adams, R. N., Mosher, C. E., Winger, J. G., Abonour, R., and Kroenke, K. (2018). Cancer-related loneliness mediates the relationships between social constraints and symptoms among cancer patients. J. Behav. Med. 41, 243–252. doi: 10.1007/s10865-017-9892-5
Alcaraz, K. I., Wiedt, T. L., Daniels, E. C., Yabroff, K. R., Guerra, C. E., and Wender, R. C. (2020). Understanding and addressing social determinants to advance cancer health equity in the United States: a blueprint for practice, research, and policy. CA Cancer J. Clin. 70, 31–46. doi: 10.3322/caac.21586
Ashi, N., Kataoka, Y., Takemura, T., Shirakawa, C., Okazaki, K., Sakurai, A., et al. (2020). Factors influencing social isolation and loneliness among lung cancer patients: a cross-sectional study. Anticancer Res 40, 7141–7145. doi: 10.21873/anticanres.14744
Bennett, B. M., Laidlaw, T. M., Dwivedi, P., Naito, A., and Gruzelier, J. H. (2006). A qualitative study of the experience of self-hypnosis or Johrei in metastatic breast cancer using interpretative phenomenological analysis. Contemp. Hypn. 23, 127–140. doi: 10.1002/ch.318
Berkman, L. F. (1983). The assessment of social networks and social support in the elderly. J. Am. Geriatr. Soc. 31, 743–749. doi: 10.1111/j.1532-5415.1983.tb03393.x
Berkman, L. F., and Syme, S. L. (1979). Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am. J. Epidemiol. 109, 186–204. doi: 10.1093/oxfordjournals.aje.a112674
Biagioli, V., Piredda, M., Annibali, O., Iacorossi, L., D’Angelo, D., Matarese, M., et al. (2017). Being in protective isolation following autologous haematopoietic stem cell transplantation: a phenomenological study. J. Clin. Nurs. 26, 4467–4478. doi: 10.1111/jocn.13777
Biordi, D. L. (1998). “Social isolation,” in Chronic illness: impact and interventions. eds. I. Lubkin and P. Larsen (Boston, MA: Jones and Bartlett), 181–203.
Blinderman, C. D., and Cherny, N. I. (2005). Existential issues do not necessarily result in existential suffering: lessons from cancer patients in Israel. Palliat. Med. 19, 371–380. doi: 10.1191/0269216305pm1038oa
Boland, L., Bennett, K., Cuffe, S., Gleeson, N., Grant, C., Kennedy, J., et al. (2019). Cancer survivors’ experience of Opti mal, a 6-week, occupation-based, self-management intervention. Br. J. Occup. Ther. 82, 90–100. doi: 10.1177/0308022618804704
Borgi, M., Collacchi, B., Ortona, E., and Cirulli, F. (2020). Stress and coping in women with breast cancer: unravelling the mechanisms to improve resilience. Neurosci. Biobehav. Rev. 119, 406–421. doi: 10.1016/j.neubiorev.2020.10.011
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., and Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424. doi: 10.3322/caac.21492
Campo, R., Bluth, K., Santacroce, S., Knapik, S., Tan, J., Gold, S., et al. (2017). A mindful self-compassion videoconference intervention for nationally recruited posttreatment young adult cancer survivors: feasibility, acceptability, and psychosocial outcomes. Support. Care Cancer 25, 1759–1768. doi: 10.1007/s00520-017-3586-y
Carduff, E., Kendall, M., and Murray, S. A. (2018). Living and dying with metastatic bowel cancer: serial in-depth interviews with patients. Eur. J. Cancer Care 27, 1–8. doi: 10.1111/ecc.12653
Charles, C., Gafni, A., Whelan, T., and O’Brien, M. A. (2006). Cultural influences on the physician-patient encounter: the case of shared treatment decision-making. Patient Educ. Couns. 63, 262–267. doi: 10.1016/j.pec.2006.06.018
D’Agostino, N. M., and Edelstein, K. (2013). Psychosocial challenges and resource needs of young adult cancer survivors: implications for program development. J. Psychosoc. Oncol. 31, 585–600. doi: 10.1080/07347332.2013.835018
Dahill, A., Al-Nakishbandi, H., Cunningham, K. B., Humphris, G. M., Lowe, D., and Rogers, S. N. (2020). Loneliness and quality of life after head and neck cancer. Br. J. Oral Maxillofac. Surg. 58, 959–965. doi: 10.1016/j.bjoms.2020.04.041
De Blasi, G., Bouteyre, E., and Rollin, L. (2018). Giving up work after cancer: an exploratory qualitative study of three clinical cases. Work 60, 105–115. doi: 10.3233/WOR-182712
de Souza, J. A., Kung, S., O’Connor, J., and Yap, B. J. (2017). Determinants of patient-centered financial stress in patients with locally advanced head and neck cancer. J. Oncol. Pract. 13, e310–e318. doi: 10.1200/JOP.2016.016337
Dornan, M., Semple, C., Moorhead, A., and McCaughan, E. (2021). A qualitative systematic review of the social eating and drinking experiences of patients following treatment for head and neck cancer. Support. Care Cancer 29, 4899–4909. doi: 10.1007/s00520-021-06062-7
Ettridge, K. A., Bowden, J. A., Chambers, S. K., Smith, D. P., Murphy, M., Evans, S. M., et al. (2018). Prostate cancer is far more hidden: perceptions of stigma, social isolation and help-seeking among men with prostate cancer. Eur. J. Cancer Care 27:e12790. doi: 10.1111/ecc.12790
Friedler, B., Crapser, J., and McCullough, L. (2015). One is the deadliest number: the detrimental effects of social isolation on cerebrovascular diseases and cognition. Acta Neuropathol. 129, 493–509. doi: 10.1007/s00401-014-1377-9
Fu, M. R., Ridner, S. H., Hu, S. H., Stewart, B. R., Cormier, J. N., and Armer, J. M. (2013). Psychosocial impact of lymphedema: a systematic review of literature from 2004 to 2011. Psychooncology 22, 1466–1484. doi: 10.1002/pon.3201
Hagedoorn, M., and Molleman, E. (2006). Facial disfigurement in patients with head and neck cancer: the role of social self-efficacy. Health Psychol. 25, 643–647. doi: 10.1037/0278-6133.25.5.643
Havens, B., Hall, M., Sylvestre, G., and Jivan, T. (2004). Social isolation and loneliness: differences between older rural and urban Manitobans. Can. J. Aging 23, 129–140. doi: 10.1353/cja.2004.0022
He, L. J., Zheng, M. C., Yuet Wong, F. K., Ying, J., and Zhang, J. E. (2021). Immediate postoperative experiences before discharge among patients with rectal cancer and a permanent colostomy: a qualitative study. Eur. J. Oncol. Nurs. 51:101911. doi: 10.1016/j.ejon.2021.101911
Hinzey, A., Gaudier-Diaz, M. M., Lustberg, M. B., and DeVries, A. C. (2016). Breast cancer and social environment: getting by with a little help from our friends. Breast Cancer Res. 18:54. doi: 10.1186/s13058-016-0700-x
Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T., and Stephenson, D. (2015). Loneliness and social isolation as risk factors for mortality. Perspect. Psychol. Sci. 10, 227–237. doi: 10.1177/1745691614568352
Høybye, M. T., Johansen, C., and Tjørnhøj-Thomsen, T. (2005). Online interaction effects of storytelling in an internet breast cancer support group. Psychooncology 14, 211–220. doi: 10.1002/pon.837
Iannarino, N. T. (2018). ‘My insides feel like Keith Richards’ face’: a narrative analysis of humor and biographical disruption in young adults’ cancer blogs. Health Commun. 33, 1233–1242. doi: 10.1080/10410236.2017.1350909
Im, E. O., and Chee, W. (2021). Clusters by menopausal symptoms: Asian American breast cancer survivors. West. J. Nurs. Res. 44:1990966708, 854–862. doi: 10.1177/01939459211018828
Iredell, H., Grenade, L., Nedwetzky, A., Collins, J., and Howat, P. (2004). Reducing social isolation amongst older people - implications for health professionals. Geriaction 22, 13–20. doi: 10.3316/informit.450291051229816
Jeong, J. Y., Jeong, G., and So, H. S. (2016). How do lung cancer patients experience stigma? A meta-synthesis of qualitative studies. Korean J. Adult Nurs. 28, 116–126. doi: 10.7475/kjan.2016.28.1.116
Johansson, Å., Svensson, E., and Axelsson, L. (2005). Social isolation -- a nursing problem in cancer patients with fatigue. Nordic J. Nurs. Res. Clin. Stud./Vård I Norden 25, 60–63. doi: 10.1177/010740830502500414
Kirtane, K., Geiss, C., Arredondo, B., Hoogland, A. I., Chung, C. H., and Muzaffar, J. (2022). “I have cancer during COVID; that’s a special category”: a qualitative study of head and neck cancer patient and provider experiences during the COVID-19 pandemic. Support. Care Cancer 30, 4337–4344. doi: 10.1007/s00520-021-06773-x
Kroenke, C. H., Michael, Y. L., Poole, E. M., Kwan, M. L., Nechuta, S., Leas, E., et al. (2017). Postdiagnosis social networks and breast cancer mortality in the after breast cancer pooling project. Cancer 123, 1228–1237. doi: 10.1002/cncr.30440
Kroenke, C. H., Quesenberry, C., Kwan, M. L., Sweeney, C., Castillo, A., and Caan, B. J. (2013). Social networks, social support, and burden in relationships, and mortality after breast cancer diagnosis in the life after breast cancer epidemiology (LACE) study. Breast Cancer Res. Treat. 137, 261–271. doi: 10.1007/s10549-012-2253-8
Kudjawu, S., and Agyeman-Yeboah, J. (2021). Experiences of women with breast cancer undergoing chemotherapy: a study at Ho teaching hospital. Ghana. Nurs. Open 8, 3161–3169. doi: 10.1002/nop2.1029
LaVeist, T. A., Sellers, R. M., Brown, K. A., and Nickerson, K. J. (1997). Extreme social isolation, use of community-based senior support services, and mortality among African American elderly women. Am. J. Community Psychol. 25, 721–732. doi: 10.1023/a:1024643118894
Lee, M. Y., Lang, D., and Tho, C. P. (2011). The experience of being a neutropenic cancer patient in an acute care isolation room: a systematic review of qualitative evidence. JBI Libr. Syst. Rev. 9, 400–416. doi: 10.11124/jbisrir-2011-118
Leung, B., Shokoohi, A., Bates, A., and Ho, C. (2021). Patient-reported psychosocial needs and psychological distress predict survival in geriatric oncology patients. J. Geriatr. Oncol. 12, 612–617. doi: 10.1016/j.jgo.2020.10.001
Lien-Gieschen, T. (1993). Validation of social isolation related to maturational age: elderly. Nurs. Diagn. 4, 37–44. doi: 10.1111/j.1744-618x.1993.tb00082.x
Liu, Y., Weng, L., Zhang, X., Wei, J., Li, Y., and Huang, Q. (2021). Status of social isolation among lung cancer survivors: the influencing factors. J. Nurs. Sci. 36, 63–66. doi: 10.3870/j.issn.1001-4152.2021.15.063
Liu, B., Wu, X., Shi, L., Li, H., Wu, D., Lai, X., et al. (2021). Correlations of social isolation and anxiety and depression symptoms among patients with breast cancer of Heilongjiang province in China: the mediating role of social support. Nurs. Open 8, 1981–1989. doi: 10.1002/nop2.876
Liu, H., Yang, Q., Narsavage, G. L., Yang, C., Chen, Y., Xu, G., et al. (2016). Coping with stigma: the experiences of Chinese patients living with lung cancer. Springerplus 5:1790. doi: 10.1186/s40064-016-3486-5
Lund-Nielsen, B., Müller, K., and Adamsen, L. (2005). Malignant wounds in women with breast cancer: feminine and sexual perspectives. J. Clin. Nurs. 14, 56–64. doi: 10.1111/j.1365-2702.2004.01022.x
Martopullo, C., Oberoi, D., Levin, G., Qureshi, M., Morgan-Maver, E., Korzeniewski, O., et al. (2020). ‘In the same boat’—a mixed-methods exploration of reasons why male gastrointestinal cancer patients joined a professionally led men-only cancer support group. J. Cancer Surviv. 14, 261–272. doi: 10.1007/s11764-019-00838-x
McGeough, A., Edwards, J., Chamberlain, R. M., and Nogeire, C. (1980). Social isolation in lung cancer patients. Soc. Work Health Care 5, 433–436. doi: 10.1300/J010v05n04_08
Miaskowski, C., Paul, S. M., Snowberg, K., Abbott, M., Borno, H., Chang, S., et al. (2020). Stress and symptom burden in oncology patients during the COVID-19 pandemic. J. Pain Symptom Manage. 60, e25–e34. doi: 10.1016/j.jpainsymman.2020.08.037
Moore, S., Leung, B., Bates, A., and Ho, C. (2018). Social isolation: impact on treatment and survival in patients with advanced cancer. J. Clin. Oncol. 36:156. doi: 10.1200/JCO.2018.36.34_suppl.156
Morreale, M. K., Moore, T. F., Kim, S., Uphold, H. S., Mabunda, L. M., and Harper, F. W. K. (2020). Preferences for notification of imaging results in patients with metastatic cancer. Patient Educ. Couns. 103, 392–397. doi: 10.1016/j.pec.2019.08.032
Nekhlyudov, L., Mollica, M. A., Jacobsen, P. B., Mayer, D. K., Shulman, L. N., and Geiger, A. M. (2019). Developing a quality of cancer survivorship care framework: implications for clinical care, research, and policy. J. Natl. Cancer Inst. 111, 1120–1130. doi: 10.1093/jnci/djz089
Newell, R. J. (1999). Altered body image: a fear-avoidance model of psycho-social difficulties following disfigurement. J. Adv. Nurs. 30, 1230–1238. doi: 10.1046/j.1365-2648.1999.01185.x
Nicholson, N. R. Jr. (2009). Social isolation in older adults: an evolutionary concept analysis. J. Adv. Nurs. 65, 1342–1352. doi: 10.1111/j.1365-2648.2008.04959.x
Nizamli, F., Anoosheh, M., and Mohammadi, E. (2011). Experiences of Syrian women with breast cancer regarding chemotherapy: a qualitative study. Nurs. Health Sci. 13, 481–487. doi: 10.1111/j.1442-2018.2011.00644.x
Noyes, R., Kathol, R. G., Debelius-Enemark, P., Williams, J., Mutgi, A., Suelzer, M. T., et al. (1990). Distress associated with cancer as measured by the illness distress scale. Psychosomatics 31, 321–330. doi: 10.1016/S0033-3182(90)72170-6
Parton, C., Ussher, J. M., and Perz, J. (2017). Experiencing menopause in the context of cancer: women’s constructions of gendered subjectivities. Psychol. Health 32, 1109–1126. doi: 10.1080/08870446.2017.1320799
Power, S., and Hegarty, J. (2010). Facilitated peer support in breast cancer: a pre-and post-program evaluation of women’s expectations and experiences of a facilitated peer support program. Cancer Nurs. 33, E9–E16. doi: 10.1097/NCC.0b013e3181ba9296
Puigpinós-Riera, R., Graells-Sans, A., Serral, G., Continente, X., Bargalló, X., Domenech, M., et al. (2018). Anxiety and depression in women with breast cancer: social and clinical determinants and influence of the social network and social support (DAMA cohort). Cancer Epidemiol. 55, 123–129. doi: 10.1016/j.canep.2018.06.002
Raque-Bogdan, T. L. (2019). Relational cultural theory and cancer: addressing the social well-being of a growing population. Pract. Innov. 4, 99–111. doi: 10.1037/pri0000087
Raque-Bogdan, T. L., Lamphere, B., Kostiuk, M., Gissen, M., and Beranek, M. (2019). Unpacking the layers: a meta-ethnography of cancer survivors’ loneliness. J. Cancer Surviv. 13, 21–33. doi: 10.1007/s11764-018-0724-6
Rhoten, B. A., Murphy, B., and Ridner, S. H. (2013). Body image in patients with head and neck cancer: a review of the literature. Oral Oncol. 49, 753–760. doi: 10.1016/j.oraloncology.2013.04.005
Rodgers, B. L. (2000). “Concept analysis: An evolutionary view,” in Concept development in nursing: foundation, techniques, and applications. eds. B. L. Rodgers and K. Knafl (Philadelphia, PA: Saunders), 77–102.
Rogers, S. N., Heseltine, N., Flexen, J., Winstanley, H. R., Cole-Hawkins, H., and Kanatas, A. (2016). Structured review of papers reporting specific functions in patients with cancer of the head and neck: 2006-2013. Br. J. Oral Maxillofac. Surg. 54, e45–e51. doi: 10.1016/j.bjoms.2016.02.012
Sandén, I., and Hydén, L. (2002). How everyday life is affected: an interview study of relatives of men suffering from testicular cancer. J. Psychosoc. Oncol. 20, 27–44. doi: 10.1300/J077v20n02_02
Schapmire, T. J., Head, B. A., and Faul, A. C. (2012). Just give me hope: lived experiences of Medicaid patients with advanced cancer. J. Soc. Work End Life Palliat. Care 8, 29–52. doi: 10.1080/15524256.2012.650672
Sender, A., Friedrich, M., Schmidt, R., and Geue, K. (2020). Cancer-specific distress, supportive care needs and satisfaction with psychosocial care in young adult cancer survivors. Eur. J. Oncol. Nurs. 44:101708. doi: 10.1016/j.ejon.2019.101708
Simonelli, L. E., and Otto, A. K. (2017). “Biopsychosocial factors in gynaecological cancer,” in Biopsychosocial factors in obstetrics and Gynaecology. eds. L. C. Edozien and P. M. S. O'Brien (New York, NY: Cambridge University Press), 169–177.
Stolley, M. R., Sheean, P., Matthews, L., Banerjee, A., Visotcky, A., Papanek, P., et al. (2020). Exploring health behaviors, quality of life, and support needs in African-American prostate cancer survivors: a pilot study to support future interventions. Support. Care Cancer 28, 3135–3143. doi: 10.1007/s00520-019-05092-6
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., et al. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. doi: 10.3322/caac.21660
Takemura, T., Kataoka, Y., Shirakawa, C., Okazaki, K., Sakurai, A., Imakita, T., et al. (2021). Influence of loneliness and social isolation on the diagnosis and treatment of Japanese patients with advanced lung cancer: a prospective cohort study. Ann. Palliat. Med. 10, 6236–6246. doi: 10.21037/apm-21-402
Tofthagen, R., and Fagerstrom, L. M. (2010). Rodgers’ evolutionary concept analysis--a valid method for developing knowledge in nursing science. Scand. J. Caring Sci. 24, 21–31. doi: 10.1111/j.1471-6712.2010.00845.x
Tomaka, J., Thompson, S., and Palacios, R. (2006). The relation of social isolation, loneliness, and social support to disease outcomes among the elderly. J. Aging Health 18, 359–384. doi: 10.1177/0898264305280993
Tsui, H., and Huang, X. Y. (2021). Experiences of losing bowel control after lower anterior resection with sphincter saving surgery for rectal cancer: a qualitative study. Cancer Nurs. doi: 10.1097/NCC.0000000000001036 [Epub ahead of print].
van Roij, J., Brom, L., Youssef-El Soud, M., van de Poll-Franse, L., and Raijmakers, N. J. H. (2019). Social consequences of advanced cancer in patients and their informal caregivers: a qualitative study. Support. Care Cancer 27, 1187–1195. doi: 10.1007/s00520-018-4437-1
Wang, S., Liu, P., and Lv, L. (2020). Social isolation and influencing factors among breast cancer survivors. Nurs. J. Chin. Peoples Liber. Army 37, 5–9. doi: 10.3969/j.issn.1008-9993.2020.12.002
White, C. A. (2000). Body image dimensions and cancer: a heuristic cognitive behavioural model. Psychooncology 9, 183–192. doi: 10.1002/1099-1611(200005/06)9:3<183::aid-pon446>3.0.co;2-l
Yang, Y., Kang, F., Wu, D., Zhang, X., and Tian, C. (2021). Social alienation and the influencing factors in old and middle-aged patients after radical prostatectomy. Modern Clin. Nurs. 20, 22–26. doi: 10.3969/j.issn.1671-8283.2021.03.004
Yuan, L., Pan, B., Wang, W., Wang, L., Zhang, X., and Gao, Y. (2020). Prevalence and predictors of anxiety and depressive symptoms among patients diagnosed with oral cancer in China: a cross-sectional study. BMC Psychiatry 20:394. doi: 10.1186/s12888-020-02796-6
Zhu, V. J., Lenert, L. A., Bunnell, B. E., Obeid, J. S., Jefferson, M., and Hughes, C. (2019). Automatically identifying social isolation from clinical narratives for patients with prostate cancer. BMC Med. Inform. Decis. Mak. 19:43. doi: 10.1186/s12911-019-0795-y
Keywords: social isolation, cancer, psychological nursing, psychosocial behavior, concept analysis
Citation: Liang Y, Hao G, Wu M and Hou L (2022) Social isolation in adults with cancer: An evolutionary concept analysis. Front. Psychol. 13:973640. doi: 10.3389/fpsyg.2022.973640
Received: 20 June 2022; Accepted: 31 August 2022;
Published: 03 October 2022.
Edited by:
Xu Tian, University of Rovira i Virgili, SpainReviewed by:
Xuchun Ye, Naval Medical Center, ChinaCopyright © 2022 Liang, Hao, Wu and Hou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lili Hou, cGlzY2VzX2xpekAxNjMuY29t
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.