Addendum: Exposure to unpredictability and mental health: Validation of the brief version of the Questionnaire of Unpredictability in Childhood (QUIC-5) in English and Spanish
- 1Department of Psychology, Chapman University, Orange, CA, United States
- 2Department of Statistics, University of California, Irvine, Irvine, CA, United States
- 3Department of Anatomy/Neurobiology, University of California, Irvine, Irvine, CA, United States
- 4Department of Pediatrics, University of California, Irvine, Irvine, CA, United States
- 5Department of Neurology, University of California, Irvine, Irvine, CA, United States
- 6Department of Psychology, University of Denver, Denver, CO, United States
- 7Department of Psychiatry and Human Behavior, University of California, Irvine, Irvine, CA, United States
- 8Center of Excellence for Stress and Mental Health, Veterans Affairs, San Diego, CA, United States
- 9Department of Psychiatry, University of California, San Diego, San Diego, CA, United States
Unpredictability is increasingly recognized as a primary dimension of early life adversity affecting lifespan mental health trajectories; screening for these experiences is therefore vital. The Questionnaire of Unpredictability in Childhood (QUIC) is a 38-item tool that measures unpredictability in childhood in social, emotional and physical domains. The available evidence indicates that exposure to unpredictable experiences measured with the QUIC predicts internalizing symptoms including depression and anxiety. The purpose of the present study was to validate English and Spanish brief versions (QUIC-5) suitable for administration in time-limited settings (e.g., clinical care settings, large-scale epidemiological studies). Five representative items were identified from the QUIC and their psychometric properties examined. The predictive validity of the QUIC-5 was then compared to the QUIC by examining mental health in four cohorts: (1) English-speaking adult women assessed at 6-months postpartum (N = 116), (2) English-speaking male veterans (N = 95), (3) English-speaking male and female adolescents (N = 155), and (4) Spanish-speaking male and female adults (N = 285). The QUIC-5 demonstrated substantial variance in distributions in each of the cohorts and is correlated on average 0.84 (r’s = 0.81–0.87) with the full 38-item version. Furthermore, the QUIC-5 predicted internalizing symptoms (anxiety and depression) in all cohorts with similar effect sizes (r’s = 0.16–0.39; all p’s < 0.05) to the full versions (r’s = 0.19–0.42; all p’s < 0.05). In sum, the QUIC-5 exhibits good psychometric properties and is a valid alternative to the full QUIC. These findings support the future use of the QUIC-5 in clinical and research settings as a concise way to measure unpredictability, identify risk of psychopathology, and intervene accordingly.
Introduction
There is little dispute that early life experience imparts a lasting imprint on trajectories of health and development across the lifespan. A rapidly accumulating body of evidence has shown poverty, neglect and abuse as well as other adverse experiences in childhood influence morbidity and mortality, including increased risk for psychopathology (LeMoult et al., 2020; Luby et al., 2020; McLaughlin et al., 2020). Unfortunately, exposure to childhood adversity is common – it is estimated that in developed nations 40–60% of adults have experienced at least one adverse childhood experience and 15–25% have been exposed to 2 or more (Green et al., 2010; Kessler et al., 2010; Merrick et al., 2018; Hughes et al., 2021). Although global estimates are less well described, projections indicate that one billion children ages 2–17 (more than 50%) are the victims of physical, sexual or emotional abuse each year (Hillis et al., 2016). Not surprisingly, due to its widespread prevalence, the global impacts on human and fiscal capital are significant. For example, as many as 20–30% of mental health disorders are attributable to childhood adversity (Green et al., 2010; Kessler et al., 2010). Similarly, the total annual burden of adversity exposures in Europe and North America total over $1.3 billion, roughly equating to 3.5% of North America’s and 2.7% of Europe’s regional gross domestic products (Bellis et al., 2019).
Although childhood adversity has been widely studied, much of this work has focused on a canonical set of adverse childhood experiences or ACEs (Felitti et al., 1998; Hughes et al., 2017) and employs a cumulative risk approach in which these adverse experiences are summed to create a composite risk score without regard for type of exposure. This model, while playing a pivotal role in documenting the pervasive and persisting influences of adversity exposures, is limited in that although it successfully identifies risk at the population level, it is unable to identify risk at the level of the individual (Baldwin et al., 2021). This observation, coupled with a need to advance conceptual models focused on the developmental consequences of early life adversity, has spurred calls for a more nuanced approach in which childhood adversity is characterized in terms of multiple dimensions or underlying factors (Ellis et al., 2009; McLaughlin and Sheridan, 2016). These dimensional models do converge on core components including threat/harshness and deprivation (Ellis et al., 2009; Sheridan and McLaughlin, 2014; Berman et al., 2022). Increasing consensus also includes a focus on unpredictability as a distinct dimension worthy of investigation (Ellis et al., 2009; Baram et al., 2012; Glynn and Baram, 2019; McLaughlin et al., 2021; Liu and Fisher, 2022).
There are studies that have characterized unpredictability in a number of ways including parental behaviors (Ainsworth and Bowlby, 1991; Bernard et al., 2013; Davis et al., 2017, 2019), parental mood lability (Glynn et al., 2018; Howland et al., 2021), residential transitions, changes in parental cohabitation and employment status (Doom et al., 2016) and there are instruments that quantify specific components of unpredictability such as family routines and household chaos (Jensen et al., 1983; Matheny et al., 1995). However, until recently there did not exist a tool to assess the broad dimension of childhood unpredictability. To meet this need, we developed and validated the Questionnaire of Unpredictability in Childhood, or QUIC (Glynn et al., 2019), a 38-item self-report instrument which comprehensively assesses exposures to unpredictability in social, emotional and physical environments. The psychometric properties were originally examined in four independent cohorts and include excellent reliability for both the English and Spanish versions (Glynn et al., 2019; Liu et al., under review). Importantly, retrospective reports on the QUIC were linked to prospectively gathered measures of unpredictability in childhood validating the retrospective recall on this instrument. For example, 83% of adolescents who endorsed the item “I moved frequently” had in fact moved 3 or more times during their lifetimes. It also is the case that self-reports of more unpredictability assessed with the QUIC were associated with two prospectively measured observational measures of parental inputs – unpredictable sensory signals in infancy (Davis et al., 2017), and unpredictable maternal mood in infancy and childhood (Glynn et al., 2018) – providing support for the construct validity of the instrument.
Growing evidence also demonstrates the predictive validity of the QUIC as a tool to measure the associations between unpredictability and mental health risk. In our initial validation paper, the QUIC predicted anxiety and depression in three independent cohorts: adult females, male veterans and male and female adolescents (Glynn et al., 2019). Importantly, these associations persisted after accounting for other indicators of early life adversity including both threat and deprivation. The subsequent QUIC Spanish language validation study then also associated unpredictability assessed via the QUIC-SP to anxiety and depressive symptoms in adulthood (as well as anhedonia and poorer physical health; Liu et al., under review). Building upon these findings, the QUIC has now also been linked to posttraumatic stress, anhedonic, depressive and anxiety symptoms as well as suicidal ideation in trauma-exposed male veterans (Spadoni et al., 2022). Further, Gillespie and Rao (2022) recently documented associations between increased childhood unpredictability assessed with the QUIC with higher rates of depressive symptoms and compromised executive function in adolescents. Thus, increasing evidence suggests that childhood unpredictability is a distinct dimension of early life adversity that deserves additional consideration and that the QUIC is a valid tool to further these investigations.
While the QUIC is emerging as a comprehensive and valid tool to measure unpredictability in early life, a measure of this length may not be feasible in time-limited research and clinical contexts. Therefore, this study aimed to validate a brief version of the QUIC and QUIC-SP for use in these settings (QUIC-5 and QUIC-SP-5). We did this by examining the psychometric properties of these measures in four independent cohorts.
Methods
Procedure
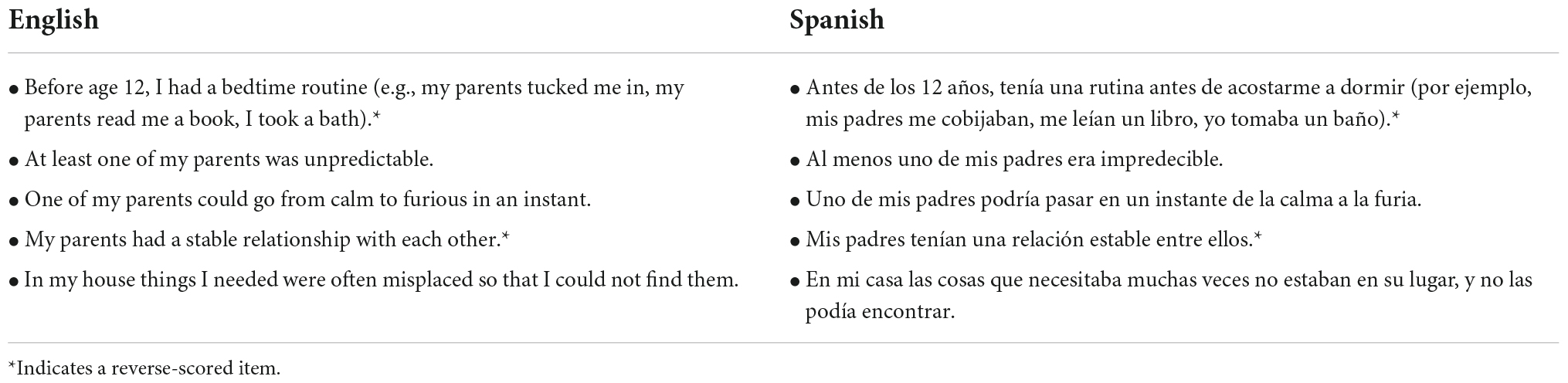
The Questionnaire of Unpredictability in Childhood, which is validated in English (QUIC; Glynn et al., 2019) and Spanish (QUIC-SP; Liu et al., under review), is a 38-item questionnaire that measures unpredictability in childhood. The QUIC broadly assesses social, emotional, and physical environments and answers are given as yes/no responses. To create brief versions of this measure, five items were identified from the QUIC to form the QUIC-5 and QUIC-SP-5 (Table 1). These five items were selected by expert consensus to include experiences that represent different domains of unpredictability and that are applicable to children from birth to 18 years of age. Scores on the full QUICs range from 0 to 38, while scores on the QUIC-5 and QUIC-SP-5 range from 0 to 5. For all versions, a higher score indicates greater exposure to unpredictability in childhood. In this study, the QUIC-5 and QUIC-SP-5 scores were compared to the QUIC and QUIC-SP scores, respectively, to characterize the performance of the brief versions. Additionally, the correlation between mental health outcomes and the full QUICs and short QUICs were compared to assess the predictive validity of the brief version.
Participants
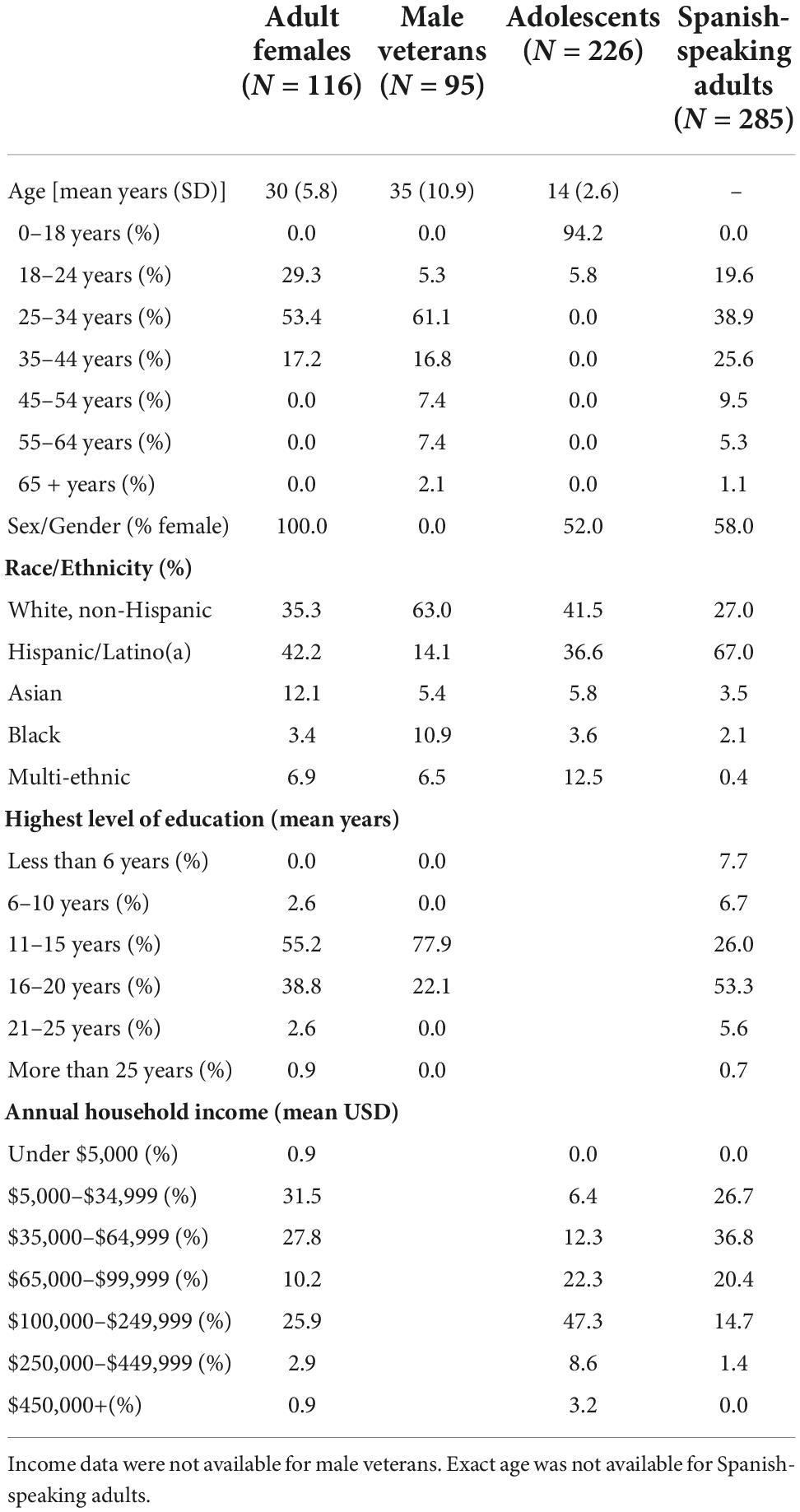
The utility and predictive validity of the QUIC-5 was assessed in four independent cohorts: (1) adult females, (2) male military veterans, (3) adolescents, and (4) Spanish-speaking adults. See Table 2 for demographics for each cohort.
Cohort 1: Adult females assessed postpartum
Cohort 1 consisted of 116 adult females (age: 18–44 years) participating in an ongoing longitudinal study on maternal and child health. These participants completed the QUIC and the 10-item Edinburgh Postnatal Depression Scale (EPDS), which is a widely used and validated measure of depressive symptoms (Cox et al., 1987). The EPDS was administered at 6 months postpartum.
Cohort 2: Male military veterans
Cohort 2 consisted of 95 male veterans (age: 24–70 years) participating in either a follow-up assessment from a prospective, longitudinal study of deployment trauma or the Center of Excellence for Stress and Mental Health TBI/PTSD biorepository data archives. Participants completed the QUIC and Patient Health Questionnaire-9 (PHQ-9), which is a well validated 9-item questionnaire assessing severity of depressive symptoms (Löwe et al., 2004).
Cohort 3: Adolescents
Cohort 3 comprised 226 adolescents (52% female; age: 10–23 years) participating in a longitudinal study of maternal and child health. Adolescent participants completed the QUIC, the 12-item Children’s Depression Inventory (CDI; Kovacs, 2011), and the 20-item State-Trait Anxiety Inventory for Children (STAIC; Spielberger et al., 1973).
Cohort 4: Spanish-speaking adults
Cohort 4 consisted of 285 Spanish-speaking adults (58% female) recruited for an online validation study of the QUIC-SP. In addition to the QUIC-SP, these participants completed the Beck Depression Inventory (BDI; Beck et al., 1996; Sanz et al., 2003), which is a widely-used 21-item questionnaire quantifying depressive symptoms in adults. Participants also reported on their anxiety symptoms using the 10-item State-Trait Anxiety Inventory (STAI; Spielberger et al., 1982, 1983).
Data analyses
The distribution of QUIC-5 scores were first compared to examine variability in scores among the four cohorts. Next, Pearson correlations were used to determine the strength of the associations between the full and brief versions within each cohort. Last, the predictive validity of the QUIC-5 was compared to that of the full QUIC by examining bivariate correlations between the two versions of the QUIC and measures of anxiety and depressive symptoms.
Results
Distribution of scores
The distributions, means, medians, and standard deviations of QUIC-5 scores for each cohort are shown in Figure 1. Compared to the adult females, adolescents, and Spanish-speaking adults, the male veterans had the highest QUIC-5 scores, which was consistent with the pattern of results observed with the full-length QUIC (Glynn et al., 2019).
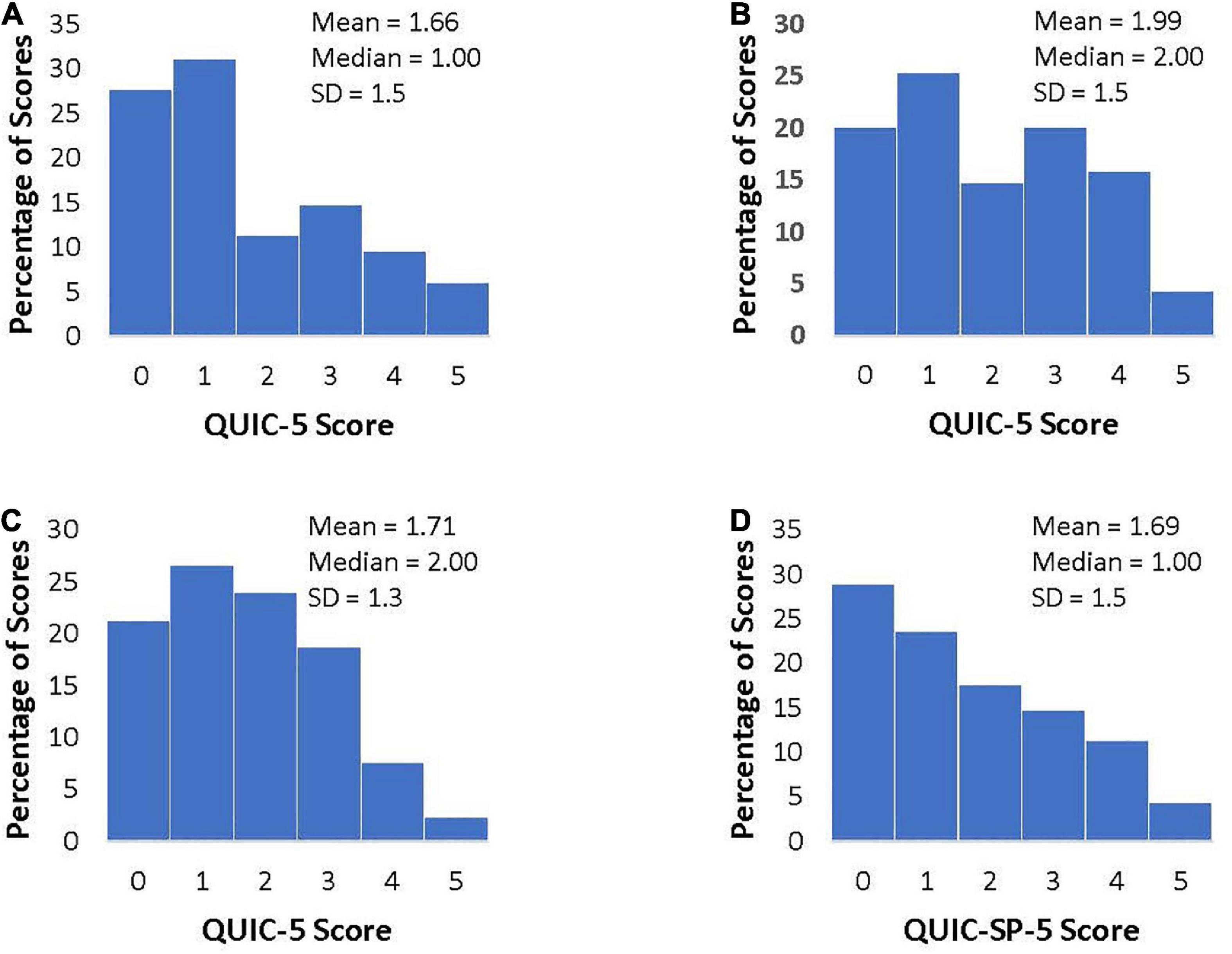
Figure 1. Distributions of QUIC-5 and QUIC-SP-5 Scores. (A) Adult females (N = 116), (B) male veterans (N = 95), (C) adolescents (N = 226), and (D) Spanish-speaking adults (N = 285).
Endorsement rates and associations between brief and full versions
For each cohort, QUIC-5 scores were strongly correlated with full-length QUIC scores (all r’s > 0.81; all p’s < 0.001). Among the adult females, the QUIC-5 was correlated 0.82 (95% CI [0.75, 0.87]) with the QUIC, 0.85 (95% CI [0.78, 0.90]) among male veterans, and 0.81 (95% CI [0.76, 0.85]) among adolescents. Among Cohort 4 (Spanish-speaking adults), the QUIC-SP-5 and QUIC-SP were correlated 0.87 (95% CI [0.84, 0.90]).
Predictive validity
The QUIC-5 and QUIC-SP-5 predicted internalizing symptoms (anxiety and depression) in each of the four cohorts (r’s = 0.16–0.39; all p’s < 0.05). Critically, the effect sizes were not substantively different from the association between the full-length QUIC and these same mental health indicators (r’s = 0.19–0.42; all p’s < 0.05; see Figure 2).
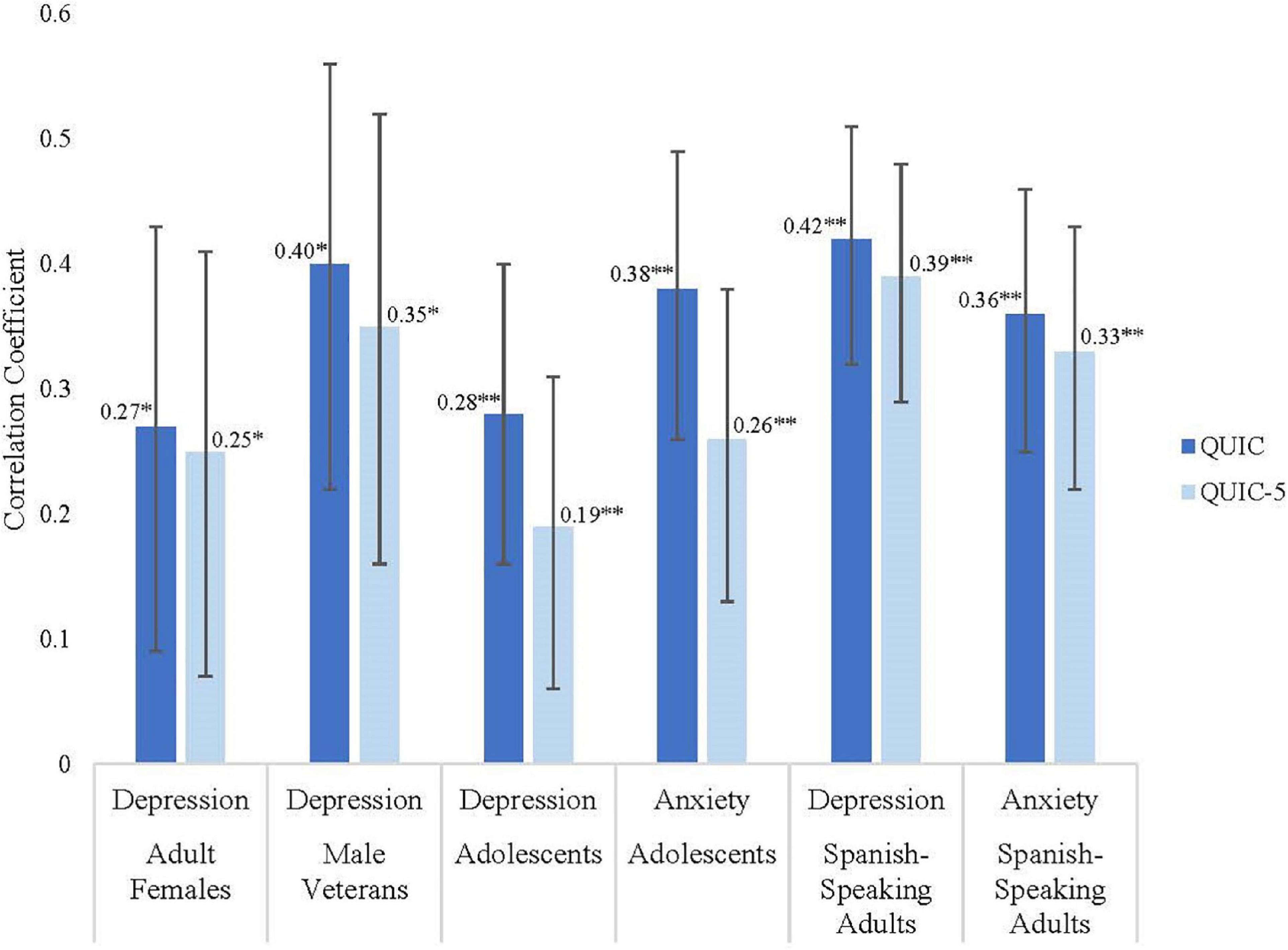
Figure 2. Predictive validity for mental health outcomes of the QUIC-5 compared to the QUIC (*p < 0.05; **p < 0.01). Dark bars indicate the size of the correlation coefficient for the 38-item QUIC, and the light bars are the correlation for the QUIC-5. Bars indicate 95% confidence intervals.
Discussion
Here we show that both the English and Spanish language versions of the QUIC-5 demonstrate excellent promise as brief assessments of unpredictability in childhood. These 5-item versions are associated on average 0.84 with the full-length version across four independent cohorts that span sex/gender, socioeconomic, and cultural groups and range in age from adolescence through 70 years. This high correlation is especially promising given that the full version was validated against prospective assessments of early life unpredictability and exhibits strong content and discriminant validity (Glynn et al., 2019). Perhaps an even stronger indicator of the brief version’s promise is that among four diverse cohorts, the QUIC-5 predicts mental health outcomes with virtually identical effect sizes to the full-length QUIC.
Progress has been made in documenting the role of adversity in shaping health and development. However, a significant barrier that remains is the relative lack of neurobiological models testing biologically plausible mechanistic processes linking early life adversity to developmental and mental health outcomes (Smith and Pollak, 2021) – a gap that further investigations of unpredictability may help address (Birnie and Baram, 2022). Foundational studies on the formation of sensory circuits, such as vision and hearing established that modality-specific sequences of sensory signals at a moment-to-moment timescale are required for the maturation of these neural circuits and further that disrupted sequences of sensory signals (e.g., visual or auditory) during sensitive developmental periods disturb the sculpting and maturation of visual, somatosensory and auditory brain circuits, leading to commensurate functional deficits (Wiesel and Hubel, 1963; Khazipov et al., 2004; Hackett et al., 2011; Espinosa and Stryker, 2012). The mechanisms involve altered synaptic pruning by microglia (Bolton et al., 2022) as well as maturation and maintenance in brain circuits subserving cognitive and emotional functions (Avishai-Eliner et al., 2001; Brunson et al., 2005; Ivy et al., 2010; Singh-Taylor et al., 2015; Molet et al., 2016a,b; Bolton et al., 2022). These preclinical studies provide mechanistic insight into the processes by which sequences of signals shape the organization of the developing brain and are complemented by research in human infants characterizing the importance of moment-to-moment signals (Yu and Smith, 2013). Building upon these principles and working with human infants, a translational model was developed to test the hypothesis that sequences of parental signals on a moment-to-moment timescale influence the maturation of human brain circuits underlying cognitive and emotion functions (Davis et al., 2017). These investigations do indicate that exposure to unpredictable parental signals is associated with poorer memory, compromised self-regulation and altered brain development of circuits related to cognitive and emotion function in infants and children (Davis et al., 2017, 2019; Granger et al., 2021).
Given that unpredictability is emerging as a core dimension in multiple conceptual models of childhood adversity (Ellis et al., 2009; Baram et al., 2012; Glynn and Baram, 2019; McLaughlin et al., 2021), the brevity of and predictive validity of the QUIC-5 has the potential to further facilitate the investigation of this dimension in a wider range of research studies. In addition to its increased utility in research settings, the QUIC-5 has potential as a brief and feasible tool for implementation in clinical contexts. A growing number of leading health care organizations now advocate for universal screening for childhood adversity in primary care resulting in increased implementation (AAP, 2017; Dube, 2018; Centers for Disease Control and Prevention, 2019; Hetherington, 2020). However, there are barriers to this implementation on the part of the clinical care providers, including time constraints, discomfort related to querying about sensitive items, uncertainty regarding appropriate referrals and potential iatrogenic effects (Maunder et al., 2020; Thompson et al., 2020). One potential advantage of screening for unpredictability is that the questions are relatively innocuous and many of these aspects of the family environment are amenable to change without requiring significant resources.
Research thus far indicates that the effect sizes for the associations between unpredictability with mental health outcomes are similar to those of previously established adverse childhood experiences such as poverty and abuse (Lawson et al., 2018; LeMoult et al., 2020), underscoring the neccessity of continuing to work on this crucial aspect of the early environment. It has been estimated that a 10% reduction in childhood adversity exposures in Europe and North America could equate to a savings of $105 billion or 3 million disability-adjusted life-years annually (Bellis et al., 2019). Multiple aspects of unpredictability (e.g., bedtime or mealtime routines, consistency in parenting practices) are sensitive to intervention and do not require significant monetary resources nor change to societal structural inequalities for remedy, unlike many other sources of childhood adversity. This is not to suggest that efforts should not be made to address the glaring disparities in adversity exposures arising from structural inequalities or other more intractable adversities, but rather that addressing unpredictability is an additional avenue to support the health of children. To this end, the QUIC and QUIC-5 can aid in endeavors to mitigate the deleterious influences of exposure to adversity in early life, with the potential to reduce the associated burdens on both monetary and human capital and improve public health.
Data availability statement
The data presented in the study are available upon request to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by University of California, Irvine IRB; San Diego, VA IRB. Written informed consent to participate in this study was provided by all adult study participants. Written informed consent for minors to participate in this study was provided by the participants’ legal guardian/next of kin. Additionally, children provided assent to participate in this study.
Author contributions
LG, TB, and HS developed the QUIC-5. LG and NL conducted the statistical analyses. LG, NL, MM, and SL drafted the manuscript. LG, EP, TB, HS, VR, DB, and CN participated in study conception and design and contributed funding. All authors provided editorial feedback and approved the submitted version.
Funding
This research was supported by National Institutes of Health MH096889, California Initiative to Advance Precision Medicine, Veterans Affairs Center of Excellence for Stress and Mental Health, and Department of Defense CDMRP award MR141217. VR is funded by a BLR&D VA Research Scientist Award.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.971350/full#supplementary-material
References
Ainsworth, M. S., and Bowlby, J. (1991). An ethological approach to personality development. Am. Psychol. 46:333. doi: 10.1037/0003-066X.46.4.333
AAP Committee on Practice and Ambulatory Medicine and AAP Bright Futures Periodicity Schedule Workgroup (2017). Recommendations for preventive pediatric health care. Pediatrics 139:e20170254.
Avishai-Eliner, S., Eghbal-Ahmadi, M., Tabachnik, E., Brunson, K. L., and Baram, T. Z. (2001). Down-regulation of hypothalamic corticotropin-releasing hormone messenger ribonucleic acid (mRNA) precedes early-life experience-induced changes in hippocampal glucocorticoid receptor mRNA. Endocrinology 142, 89–97. doi: 10.1210/endo.142.1.7917
Baldwin, J. R., Caspi, A., Meehan, A. J., Ambler, A., Arseneault, L., Fisher, H. L., et al. (2021). Population vs individual prediction of poor health from results of adverse childhood experiences screening. JAMA Pediatr. 175, 385–393. doi: 10.1001/jamapediatrics.2020.5602
Baram, T. Z., Davis, E. P., Obenaus, A., Sandman, C. A., Small, S. L., Solodkin, A., et al. (2012). Fragmentation and unpredictability of early-life experience in mental disorders. Am. J. Psychiatry 169, 907–915. doi: 10.1176/appi.ajp.2012.11091347
Beck, A. T., Steer, R. A., and Brown, G. K. (1996). Beck depression inventory (BDI-II). London: Pearson.
Bellis, M. A., Hughes, K., Ford, K., Rodriguez, G. R., Sethi, D., and Passmore, J. (2019). Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: A systematic review and meta-analysis. Lancet Public Health 4:e517–e528. doi: 10.1016/S2468-2667(19)30145-8
Berman, I. S., McLaughlin, K. A., Tottenham, N., Godfrey, K., Seeman, T., Loucks, E., et al. (2022). Measuring early life adversity: A dimensional approach. Dev. Psychopathol. 34, 499–511. doi: 10.1017/S0954579421001826
Bernard, K., Meade, E., and Dozier, M. (2013). Parental synchrony and nurturance as targets in an attachment based intervention: Building upon mary ainsworth’s insights about mother–infant interaction. Attach. Hum. Dev. 15, 507–523. doi: 10.1080/14616734.2013.820920
Birnie, M. T., and Baram, T. Z. (2022). Principles of emotional brain circuit maturation. Science 376, 1055–1056. doi: 10.1126/science.abn4016
Bolton, J. L., Short, A. K., Othy, S., Kooiker, C. L., Shao, M., Gunn, B. G., et al. (2022). Early stress-induced impaired microglial pruning of excitatory synapses on immature CRH-expressing neurons provokes aberrant adult stress responses. Cell Rep. 38:110600. doi: 10.1016/j.celrep.2022.110600
Brunson, K. L., Kramar, E., Lin, B., Chen, Y., Colgin, L. L., Yanagihara, T. K., et al. (2005). Mechanisms of late-onset cognitive decline after early-life stress. J. Neurosci. 25, 9328–9338. doi: 10.1523/JNEUROSCI.2281-05.2005
Centers for Disease Control and Prevention (2019). Preventing adverse childhood experiences: Leveraging the Best Available Evidence. Atlanta, GA: Centers for Disease Control and Prevention.
Cox, J. L., Holden, J. M., and Sagovsky, R. (1987). Detection of postnatal depression. Br. J. Psychiatry 150, 782–786. doi: 10.1192/bjp.150.6.782
Davis, E. P., Korja, R., Karlsson, L., Glynn, L. M., Sandman, C. A., Vegetabile, B., et al. (2019). Across continents and demographics, unpredictable maternal signals are associated with children’s cognitive function. EBioMedicine 46, 256–263. doi: 10.1016/j.ebiom.2019.07.025
Davis, E. P., Stout, S. A., Molet, J., Vegetabile, B., Glynn, L. M., Sandman, C. A., et al. (2017). Exposure to unpredictable maternal sensory signals influences cognitive development across species. Proc. Natl. Acad. Sci. U.S.A. 114, 10390–10395. doi: 10.1073/pnas.1703444114
Doom, J. R., Vanzomeren-Dohm, A. A., and Simpson, J. A. (2016). Early unpredictability predicts increased adolescent externalizing behaviors and substance use: A life history perspective. Dev. Psychopathol. 28, 1505–1516. doi: 10.1017/S0954579415001169
Dube, S. R. (2018). Continuing conversations about adverse childhood experiences (ACEs) screening: A public health perspective. Child Abuse Negl. 85, 180–184. doi: 10.1016/j.chiabu.2018.03.007
Ellis, B. J., Figueredo, A. J., Brumbach, B. H., and Schlomer, G. L. (2009). Fundamental dimensions of environmental risk. Hum. Nat. 20, 204–268. doi: 10.1007/s12110-009-9063-7
Espinosa, J. S., and Stryker, M. P. (2012). Development and plasticity of the primary visual cortex. Neuron 75, 230–249. doi: 10.1016/j.neuron.2012.06.009
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. Am. J. Prev. Med. 14, 245–258. doi: 10.1016/S0749-3797(98)00017-8
Gillespie, M. L., and Rao, U. (2022). Relationships between depression and executive functioning in adolescents: The moderating role of unpredictable home environment. J. Child Fam. Stud. 31, 1–17. doi: 10.1007/s10826-022-02296-z
Glynn, L. M., and Baram, T. Z. (2019). The influence of unpredictable, fragmented parental signals on the developing brain. Front. Neuroendocrinol. 53:100736. doi: 10.1016/j.yfrne.2019.01.002
Glynn, L. M., Howland, M. A., Sandman, C. A., Davis, E. P., Phelan, M., Baram, T. Z., et al. (2018). Prenatal maternal mood patterns predict child temperament and adolescent mental health. J. Affect. Disord. 228, 83–90. doi: 10.1016/j.jad.2017.11.065
Glynn, L. M., Stern, H. S., Howland, M. A., Risbrough, V. B., Baker, D. G., Nievergelt, C. M., et al. (2019). Measuring novel antecedents of mental illness: The questionnaire of unpredictability in childhood. Neuropsychopharmacology 44, 876–882. doi: 10.1038/s41386-018-0280-9
Granger, S. J., Glynn, L. M., Sandman, C. A., Small, S. L., Obenaus, A., Keator, D. B., et al. (2021). Aberrant maturation of the uncinate fasciculus follows exposure to unpredictable patterns of maternal signals. J. Neurosci. 41, 1242–1250. doi: 10.1523/JNEUROSCI.0374-20.2020
Green, J. G., McLaughlin, K. A., Berglund, P. A., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., et al. (2010). Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: Associations with first onset of DSM-IV disorders. Arch. Gen. Psychiatry 67, 113–123. doi: 10.1001/archgenpsychiatry.2009.186
Hackett, T. A., Barkat, T. R., O’Brien, B. M., Hensch, T. K., and Polley, D. B. (2011). Linking topography to tonotopy in the mouse auditory thalamocortical circuit. J. Neurosci. 31, 2983–2995. doi: 10.1523/JNEUROSCI.5333-10.2011
Hetherington, K. (2020). Ending Childhood Adversity: a Public Health Approach. Edinburgh: Public Health Scotland.
Hillis, S., Mercy, J., Amobi, A., and Kress, H. (2016). Global prevalence of past-year violence against children: A systematic review and minimum estimates. Pediatrics 137:e20154079. doi: 10.1542/peds.2015-4079
Howland, M. A., Sandman, C. A., Davis, E. P., Stern, H. S., Phelan, M., Baram, T. Z., et al. (2021). Prenatal maternal mood entropy is associated with child neurodevelopment. Emotion 21:489. doi: 10.1037/emo0000726
Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C., et al. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health 2:e356–e366. doi: 10.1016/S2468-2667(17)30118-4
Hughes, K., Ford, K., Bellis, M. A., Glendinning, F., Harrison, E., and Passmore, J. (2021). Health and financial costs of adverse childhood experiences in 28 European countries: A systematic review and meta-analysis. Lancet Public Health 6:e848–e857. doi: 10.1016/S2468-2667(21)00232-2
Ivy, A. S., Rex, C. S., Chen, Y., Dube, C., Maras, P. M., Grigoriadis, D. E., et al. (2010). Hippocampal dysfunction and cognitive impairments provoked by chronic early-life stress involve excessive activation of CRH receptors. J. Neurosci. 30, 13005–13015. doi: 10.1523/JNEUROSCI.1784-10.2010
Jensen, E. W., James, S. A., Boyce, W. T., and Hartnett, S. A. (1983). The family routines inventory: Development and validation. Soc. Sci. Med. 17, 201–211. doi: 10.1016/0277-9536(83)90117-X
Kessler, R. C., McLaughlin, K. A., Green, J. G., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., et al. (2010). Childhood adversities and adult psychopathology in the WHO World mental health surveys. Br. J. Psychiatry 197, 378–385. doi: 10.1192/bjp.bp.110.080499
Khazipov, R., Sirota, A., Leinekugel, X., Holmes, G. L., Ben-Ari, Y., and Buzsaki, G. (2004). Early motor activity drives spindle bursts in the developing somatosensory cortex. Nature 432, 758–761. doi: 10.1038/nature03132
Kovacs, M. (2011). Children’s Depression Inventory 2nd edition (CDI 2): Technical manual. Toronto, ON: Multi-Health Systems.
Lawson, G. M., Hook, C. J., and Farah, M. J. (2018). A meta-analysis of the relationship between socioeconomic status and executive function performance among children. Dev. Sci. 21:e12529. doi: 10.1111/desc.12529
LeMoult, J., Humphreys, K. L., Tracy, A., Hoffmeister, J.-A., Ip, E., and Gotlib, I. H. (2020). Meta-analysis: Exposure to early life stress and risk for depression in childhood and adolescence. J. Am. Acad. Child Adolesc. Psychiatry 59, 842–855. doi: 10.1016/j.jaac.2019.10.011
Liu, S., and Fisher, P. A. (2022). Early Experience unpredictability in child development as a model for understanding the impact of the COVID-19 pandemic: A translational neuroscience perspective. Dev. Cogn. Neurosci. 54:101091. doi: 10.1016/j.dcn.2022.101091
Liu, S., Bailey, N., Romero-González, S., Moors, A., Campos, B., Davis, E. P., et al. (under review). *The QUIC-SP: a Spanish language tool assessing unpredictability in early life is linked to physical and mental Health.
Löwe, B., Kroenke, K., Herzog, W., and Gräfe, K. (2004). Measuring depression outcome with a brief self-report instrument: Sensitivity to change of the Patient Health Questionnaire (PHQ-9). J. Affect. Disord. 81, 61–66. doi: 10.1016/S0165-0327(03)00198-8
Luby, J. L., Baram, T. Z., Rogers, C. E., and Barch, D. M. (2020). Neurodevelopmental optimization after early-life adversity: Cross-species studies to elucidate sensitive periods and brain mechanisms to inform early intervention. Trends Neurosci. 43, 744–751. doi: 10.1016/j.tins.2020.08.001
Matheny, A. P. Jr., Wachs, T. D., Ludwig, J. L., and Phillips, K. (1995). Bringing order out of chaos: Psychometric characteristics of the confusion, hubbub, and order scale. J. Appl. Dev. Psychol. 16, 429–444. doi: 10.1016/0193-3973(95)90028-4
Maunder, R. G., Hunter, J. J., Tannenbaum, D. W., Le, T. L., and Lay, C. (2020). Physicians’ knowledge and practices regarding screening adult patients for adverse childhood experiences: A survey. BMC Health Serv. Res. 20:314. doi: 10.1186/s12913-020-05124-6
McLaughlin, K. A., and Sheridan, M. A. (2016). Beyond cumulative risk: A dimensional approach to childhood adversity. Curr. Dir. Psychol. Sci. 25, 239–245. doi: 10.1177/0963721416655883
McLaughlin, K. A., Colich, N. L., Rodman, A. M., and Weissman, D. G. (2020). Mechanisms linking childhood trauma exposure and psychopathology: A transdiagnostic model of risk and resilience. BMC Med. 18:96. doi: 10.1186/s12916-020-01561-6
McLaughlin, K. A., Sheridan, M. A., Humphreys, K. L., Belsky, J., and Ellis, B. J. (2021). The value of dimensional models of early experience: Thinking clearly about concepts and categories. Perspect. Psychol. Sci. 16, 1463–1472. doi: 10.1177/1745691621992346
Merrick, M. T., Ford, D. C., Ports, K. A., and Guinn, A. S. (2018). Prevalence of adverse childhood experiences from the 2011-2014 behavioral risk factor surveillance system in 23 states. JAMA Pediatr. 172, 1038–1044. doi: 10.1001/jamapediatrics.2018.2537
Molet, J., Heins, K., Zhuo, X., Mei, Y. T., Regev, L., Baram, T. Z., et al. (2016a). Fragmentation and high entropy of neonatal experience predict adolescent emotional outcome. Transl. Psychiatry 6:e702. doi: 10.1038/tp.2015.200
Molet, J., Maras, P. M., Kinney-Lang, E., Harris, N. G., Rashid, F., Ivy, A. S., et al. (2016b). MRI uncovers disrupted hippocampal microstructure that underlies memory impairments after early-life adversity. Hippocampus 26, 1618–1632. doi: 10.1002/hipo.22661
Sanz, J., Perdigón, A. L., and Vázquez, C. (2003). Adaptación española del inventario para la depresión de beck-II (BDI-II): 2. Propiedades psicométricas en población general. Clin. Salud 14, 249–280.
Sheridan, M. A., and McLaughlin, K. A. (2014). Dimensions of early experience and neural development: Deprivation and threat. Trends Cogn. Sci. 18, 580–585. doi: 10.1016/j.tics.2014.09.001
Singh-Taylor, A., Korosi, A., Molet, J., Gunn, B. G., and Baram, T. Z. (2015). Synaptic rewiring of stress-sensitive neurons by early-life experience: A mechanism for resilience? Neurobiol. Stress 1, 109–115. doi: 10.1016/j.ynstr.2014.10.007
Smith, K. E., and Pollak, S. D. (2021). Rethinking concepts and categories for understanding the neurodevelopmental effects of childhood adversity. Perspect. Psychol. Sci. 16, 67–93. doi: 10.1177/1745691620920725
Spadoni, A. D., Vinograd, M., Cuccurazzu, B., Torres, K., Glynn, L. M., Davis, E. P., et al. (2022). Contribution of early-life unpredictability to neuropsychiatric symptom patterns in adulthood. Depress. Anxiety 39, 706–717.
Spielberger, C. D., Gorsuch, R. L., and Lushene, R. E. (1982). Cuestionario De Ansiedad Estado-Rasgo, Madrid: TEA publishers.
Spielberger, C., Edwards, C., Montuori, J., and Lushene, R. (1973). Children’s State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press.
Spielberger, C., Gorsuch, R., Lushene, R., Vagg, P., and Jacobs, G. (1983). Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press.
Thompson, L. A., Filipp, S. L., Mack, J. A., Mercado, R. E., Barnes, A., Bright, M., et al. (2020). Specific adverse childhood experiences and their association with other adverse childhood experiences, asthma and emotional, developmental and behavioral problems in childhood. Pediatr. Res. 88, 100–109. doi: 10.1038/s41390-020-0784-y
Wiesel, T. N., and Hubel, D. H. (1963). Single-cell responses in striate cortex of kittens deprived of vision in one eye. J. Neurophysiol. 26, 1003–1017. doi: 10.1152/jn.1963.26.6.1003
Keywords: early life adversity, unpredictability, mental health, anxiety, depression
Citation: Lindert NG, Maxwell MY, Liu SR, Stern HS, Baram TZ, Poggi Davis E, Risbrough VB, Baker DG, Nievergelt CM and Glynn LM (2022) Exposure to unpredictability and mental health: Validation of the brief version of the Questionnaire of Unpredictability in Childhood (QUIC-5) in English and Spanish. Front. Psychol. 13:971350. doi: 10.3389/fpsyg.2022.971350
Received: 21 June 2022; Accepted: 17 October 2022;
Published: 09 November 2022.
Edited by:
Daniel Rodriguez, La Salle University, United StatesReviewed by:
Caitlin S. M. Cowan, The University of Sydney, AustraliaJohn Taylor, La Salle University, United States
Copyright © 2022 Lindert, Maxwell, Liu, Stern, Baram, Poggi Davis, Risbrough, Baker, Nievergelt and Glynn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Laura M. Glynn, lglynn@chapman.edu
 Natasha G. Lindert
Natasha G. Lindert Megan Y. Maxwell
Megan Y. Maxwell Sabrina R. Liu1
Sabrina R. Liu1 Hal S. Stern
Hal S. Stern Tallie Z. Baram
Tallie Z. Baram Elysia Poggi Davis
Elysia Poggi Davis Victoria B. Risbrough
Victoria B. Risbrough Laura M. Glynn
Laura M. Glynn