
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychol. , 19 January 2023
Sec. Psychopathology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.968638
This article is part of the Research Topic Methods and Applications in Psychopathology: New Methods and Trends for the Understanding of Neuropsychiatric Disorders View all 12 articles
Objects: This study aimed to elucidate the effect of cognitive bias modification on depression.
Methods: This research included 10 randomized studies searching four major databases: PubMed, Embase, PsycINFO, and Cochrane Library, with a total sample size of 467. Moreover, they were examined for quality and possible publication bias.
Results: Cognitive bias modification (CBM) had statistically significant results, g = −0.64, 95% CI = [−0.97–0.32]. The interpretation of cognitive bias modification shows the highest effect size, g = −1.45, 95% CI = [−2.05–0.88]. When the training place is located in the laboratory, the training effect is significant, g = −1.11, 95% CI = [−1.62–0.61]. The difference is statistically significant when the training environment was changed to home, g = −0.28, 95% CI = [−0.51–0.05]. CBM has a statistical effect on moderate-to-severe depression, g = −0.70, 95% CI = [−1.04–0.36].
Conclusion: We found that CBM had a moderate therapeutic effect on depression, whether the setting was at home or in the lab. Especially when the interpretation of cognitive bias modification (CBM-I) was used, we got the highest effect value. Furthermore, CBM has a statistical effect on moderate-to-severe depression.
Depression is a common mental disorder, accounting for 5% prevalence in adults worldwide (WHO, 2021). It is a costly and disabling illness that reduces life expectancy and affects people of all ages. It is well-established that there are many symptoms of depression, such as loss of interest and anhedonia, persistent depression, insomnia, fatigue, attention deficit, problems with low self-esteem, hopelessness, and suicide (Hasin et al., 2018).
According to the cognitive theory of depression, Cognitive theory holds that different psychopathological conditions are associated with specific biases that influence how an individual incorporates and responds to new information (Beck and Dozois, 2011). Negative attentional bias plays a significant role in developing and maintaining depression (Beck, 2008). A large body of literature has documented that depressed people selectively pay attention to negative information (Gotlib and Joormann, 2010). Furthermore, depressed individuals tend to interpret ambiguous situations negatively (Orchard et al., 2016). Some theories also suggest that attentional bias and explanatory bias jointly affect depression (Everaert et al., 2012). These attentional patterns are associated with persistent rumination of negative value information and impaired emotional regulation due to difficulty in dissociating from negative stimuli (Yaroslavsky et al., 2019). When adverse circumstances activate potential negative patterns, depressed people’s belief that they are unlovable and bad will be highlighted, so that individuals may selectively pay attention to information and opinions consistent with this negative self. It is a pessimistic view not only for yourself but also for others and the world (Roiser et al., 2012).
Among them, the persistent negative effects of cognitive dysfunction, attention deviation, and MDD can be understood as partly due to the dysfunction of prefrontal cortex circuits and related obstacles in emotional cognitive control (Murrough et al., 2011). There is a lot of research on the neural structure and function of negative cognitive bias. The two basic types of cognitive dysfunction observed in MDD are cognitive bias, including information processing or attention distribution distortion of negative stimuli, and cognitive deficits, including impaired attention, short-term memory, and executive function (Darcet et al., 2016). Based on cognitive defects such as impaired attention, some intervention strategies of implicit attention training can be explored. As mentioned later in this article, the attention deviation correction program is used to intervene in depression and anxiety (Jonassen et al., 2019).
Ochsner found that depressed adults’ perception bias toward negative stimulation was related to the dysfunction of the amygdala and ventromedial prefrontal lobe. These brain regions are involved in bottom-up emotional processing (Ochsner et al., 2004). Dai found in the event-related unit that depressed adults are more likely to be aroused by negative sad faces (Dai and Feng, 2012). The above two studies are based on neuroimaging and EEG techniques, respectively, which make us realize that negative cognitive bias is not only a kind of psychological bias or thinking distortion but also corresponds to the defect of neurocognitive function. In addition, Fritzsche found that the attention bias of depressed adults toward negative stimuli, especially sad stimuli, will last until the recovery period of depression (Fritzsche et al., 2010). The attention bias to negative stimuli will cause further difficulties in the life of depressed adults, such as interpersonal dysfunction, thus aggravating the development and maintenance of depression (Geerts and Bouhuys, 1998). Besides, it is more difficult for depressed adults than non-depressed adults to exclude irrelevant negative information from working memory, and when working memory shows competition for resources, depressed adults will also suffer damage in selecting relevant positive content (Levens and Gotlib, 2009).
About one-third of adults with depression receive traditional antidepressant treatment [e.g., selective 5-hydroxytryptamine reuptake inhibitors (SSRI)] but respond poorly (Aguglia et al., 2014). Another study also showed that SSRIs are usually used as the first-line treatment for MDD. However, only 42–53% of patients treated with SSRIs have improved their condition, and medication for treatment-resistant depression remains a challenge (Tanaka et al., 2022). Biased cognition and maladaptive behavior patterns are considered to be the key factors leading to the development and persistence of depression. Given the safety of cognitive-behavioral therapy (CBT) and the important role of cognitive bias in the occurrence and maintenance of depression, CBT is the most commonly sought alternative therapy (Sudak, 2012). The selective efficacy of CBT combined with antidepressants has been previously reported (Ironside et al., 2016). However, the World Health Organization has listed it as the main cause of the burden of all diseases in middle- and high-income countries. This has led to increasing demands for innovative treatments that can be delivered by computer or telephone (Simon and Ludman, 2009).
Cognitive bias modification (CBM) is an application based on computer-intervention programs and cognitive theory. The intermediary hypothesis of cognitive theory is that the way individuals think and explain events affects their emotional and behavioral responses. Cognitive change assumes that individuals can become more functional and adaptable by intentionally changing their cognitive and behavioral responses to the environment they face (Beck and Dozois, 2011). CBM aims to directly change the process of prejudice in the cognitive process, such as biased attention to threatening stimuli and biased interpretation of vague stimuli as threats (Joormann et al., 2015).
These programs aim to modify information processing through cognitive tasks, which use basic learning principles and repeated exercises to encourage a healthier way of thinking. Researchers pointed out the practical benefits provided by CBM, such as scalability and easy dissemination, which can enhance the effect of CBT (Beard and Amir, 2008). Among them, CBMI usually aims at allowing individuals to explain ambiguous situations in a benign way, to encourage more flexible thinking, and be less rigid and negative (Joormann et al., 2015). CBM technology does not need to consider the quality and cost of the individual therapist. The role of the therapist is handed over to a relatively automated process. On the other hand, patients can even do it themselves at home (Pictet et al., 2016).
A growing number of studies and reviews have reported the promise of CBM as an alternative or complementary intervention to anxiety and depression. A study reports that the interpretation of Cognitive bias modification (CBM-I) can significantly correct the negative explanations to reduce depressive symptoms and provide evidence for supporting a clinical application, particularly in mild-to-moderate depression (Nejati et al., 2018). Another study shows that attention to Cognitive bias modification (CBM-A) showed effectiveness in reducing attentional bias to negative information, increasing attention allocation to positive stimuli, and reducing depressive symptoms (LeMoult et al., 2016). Furthermore, a pilot study provides preliminary evidence that imagery and interpretation of cognitive bias modification (i-CBMI) could provide positive clinical outcomes in an Iranian psychiatric setting, showing that i-CBMI led to significant improvements in depressive symptoms (Torkan et al., 2014). However, there are some inconsistent results. Study shows that CBM had just a small effect on anxiety and depression (g = 0.13); when anxiety and depression were examined separately, CBM significantly modified anxiety but not depression (Hallion and Ruscio, 2011). A meta-analysis shows that the intervention effect of CBM on depression is insufficient (Fodor et al., 2020).
The results of these studies are in contrast. We found that some studies have included both depression and anxiety, which may have confounding factors because of comorbidity (Bowler et al., 2012). Furthermore, the study shows some differences in symptoms between adolescent depression and adult depression. Studies show that the differences in how depression presents in adolescents and adults may be consistent with different pathophysiological mechanisms. For adolescents, they found that physical disturbances were common (loss of energy, appetite, and sleep changes). For adults, anhedonia, loss of interest, and concentration difficulties were more common (Rice et al., 2019). At the same time, studies have shown that attentional bias was positively associated with anhedonia. Assessing biases in multiple domains increased sensitivity to uncover relationships between emotional processing biases and anhedonia symptoms (Salem et al., 2018). Therefore, we pay more attention to the cognitive bias modification of adult depression, which may reduce the mixing factors to expect purer and more targeted results.
The purpose of this study is to explore the effectiveness of cognitive bias modification in the intervention of depression patients with different severity; Second, to explore the effect of cognitive bias modification used by depressed adults in different training places; Finally, we want to know the intervention effect of three cognitive bias modification paradigms on depression.
This meta-analysis was entirely guided by the PRISMA tool (Stovold et al., 2014). This study was conducted to explore the effect of CBM on depression symptoms. Two authors (JL and HY) conducted a systematic search independently in PubMed, PsycINFO, Embase, and Cochrane Library on September 17, 2021. We searched four databases and used the same search strategy “((Cognitive bias modification) OR (attention* bias modification) OR (interpret* bias modification) OR (attention training) OR (bias training) AND (depression [Mesh Terms]) OR (depressive disorder) OR (depress*)).” In case of missing any research that may not be randomized controlled trials, the reference lists within published reviews on CBM for depression were also searched.
Studies were identified using the following inclusion criteria: (1) randomized controlled trials; (2) using CBM intervention, alone or in combination with another treatment (i.e., CBM-I, CBM-A, and imagery CBM-I); (3) adult depression participants were included; and (4) clinically relevant outcomes. Exclusion criteria included the following: (1) healthy control group; (2) children or adolescent participants; and (3) conference abstracts and non-English articles were excluded.
Two authors (JL and HY) examined the literature obtained through the search strategy. Differences were resolved through discussion, and they will be consulted by the senior author (MH) if they still exist.
The quality of the included studies was assessed using criteria for seven “Risk of Bias” assessment tools developed by the Cochrane Collaboration (Higgins et al., 2011): (1) random sequence generation (selection bias), (2) allocation concealment (selection bias), (3) blinding of participants and personnel (performance bias), (4) blinding of outcome assessment (detection bias), (5) incomplete outcome data (attrition bias), (6) selective reporting (reporting bias), and (7) other bias.
The content of data extraction includes the following dimensions: author, publication date, sample type, sample size, female sample size, mean age, CBM training location, training session, CBM process alone or in combination, CBM type (i.e., CBM-A, CBM-I, or imagery CBM-I) outcome measures, type of control group (i.e., sham training or waiting list), and follow-up study.
For each study, the correlation values of the post-test in the control group were compared [mean and standard deviations (SD)]. Considering that different samples used different self-assessment questionnaires and several studies had small sample sizes, we used hedges’ g-value to represent the effect size (Borenstein et al., 2009).
Most of the included studies were measured using self-rated questionnaires. The Beck depression inventory-II is a self-reported measure used to assess depressive symptoms. Depression was measured by BDI-II. The self-rating depression scale is a 20-item self-report inventory that assesses depressive symptoms in both clinical and non-clinical populations and can distinguish between different levels of severity in depression symptoms (Zung, 1973). The PHQ-9 is a nine-question instrument given to patients in a primary care setting to screen for the presence and severity of depression. It is the nine-question depression scale from the Patient Health Questionnaire (PHQ). The Center for Epidemiologic Studies Depression Scale (CES-D) is a brief self-report questionnaire developed in 1977 by Laurie Radloff to measure the severity of depressive symptoms in the general population.
RevMan5 and STATA software were used to analyze the results. If data are insufficient, try contacting the author of the original article. Considering the CBM was divided into three similar interventions: CBM-A, CBM-I, and i-CBMI, specific methods are introduced in Table 1. The random effect model is considered to calculate the effect value, and this model assumes that the included studies are from different research groups (Riley et al., 2011). Moreover, we can easily guess the heterogeneity between studies for they use three different similar interventions. We also need to calculate the Q statistic and I2 index to assess heterogeneity. In addition, sensitivity analysis was used for the robustness of the study. How do you analyze sensitivity? The main approach used is a step-by-step elimination method, in which one study at a time is removed and the effect size (ES) of the remaining studies is calculated to see if heterogeneity changes. If an outlier occurs, the reason behind the anomaly literature needs to be explored. Subgroup meta-analyses can also help identify the sources of heterogeneity and understand the effects of experimental interventions in different subgroups. For assessment of publication bias, the Funnel plot can be used by looking at the symmetry of the Funnel plot. Egger’s test is used to test the symmetry of the funnel plot.
We searched a total of 1,884 articles in four databases, one of them was obtained through manual retrieval of references. There are 1,885 articles; 385 duplicating papers were first removed, leaving 1,500, and then a selection of titles and abstracts was done which excluded 1,287 articles. Therefore, 213 relevant literature pieces were left for the final full-test screening, from which 203 articles were excluded. The details of full-text screening are shown in Figure 1.
Table 2 shows the characteristics of the 10 studies included. Sample sizes ranged from 18 to 114, with a total sample size of 467. This meta-analysis included studies of six moderate, three mild, and one severe depression samples. CBM’s session ranges from 3 to 20 times. Four of the trials used CBM-A as an independent treatment, and the last one used CBM-A and CBM-I in combination. Another five items were divided into three items of i-CBMI and two items of CBM-I intervention methods.
There are few studies on the best quality. Three studies met five of the criteria and two studies met four criteria; two studies met three criteria, and three studies met only two criteria. In general, the randomization of the studies was good. However, almost all of the studies did not elaborate on how they hid the allocation, which could lead to a risk that the estimates would deviate from the true clinical outcomes. Three other studies had no follow-up and lacked complete outcome reports. Finally, some bias in other aspects mainly comes from the small sample size of the experiment, and the selection of subclinical samples is not precise enough and relatively broad, which is determined by the characteristics of mild symptoms themselves. Figure 2 is the bias diagram. In addition, there is a certain dropout rate in some studies, which may lead to inconsistency with the number of people who just started to be included, and the dropout rate may affect the reliability of outcome indicators. In addition, most of the included studies use self-assessment questionnaires, which may also lead to bias. In addition, considering that some interventions are made by patients themselves at home, there may be uncontrollable related factors, which will affect the quality of research.
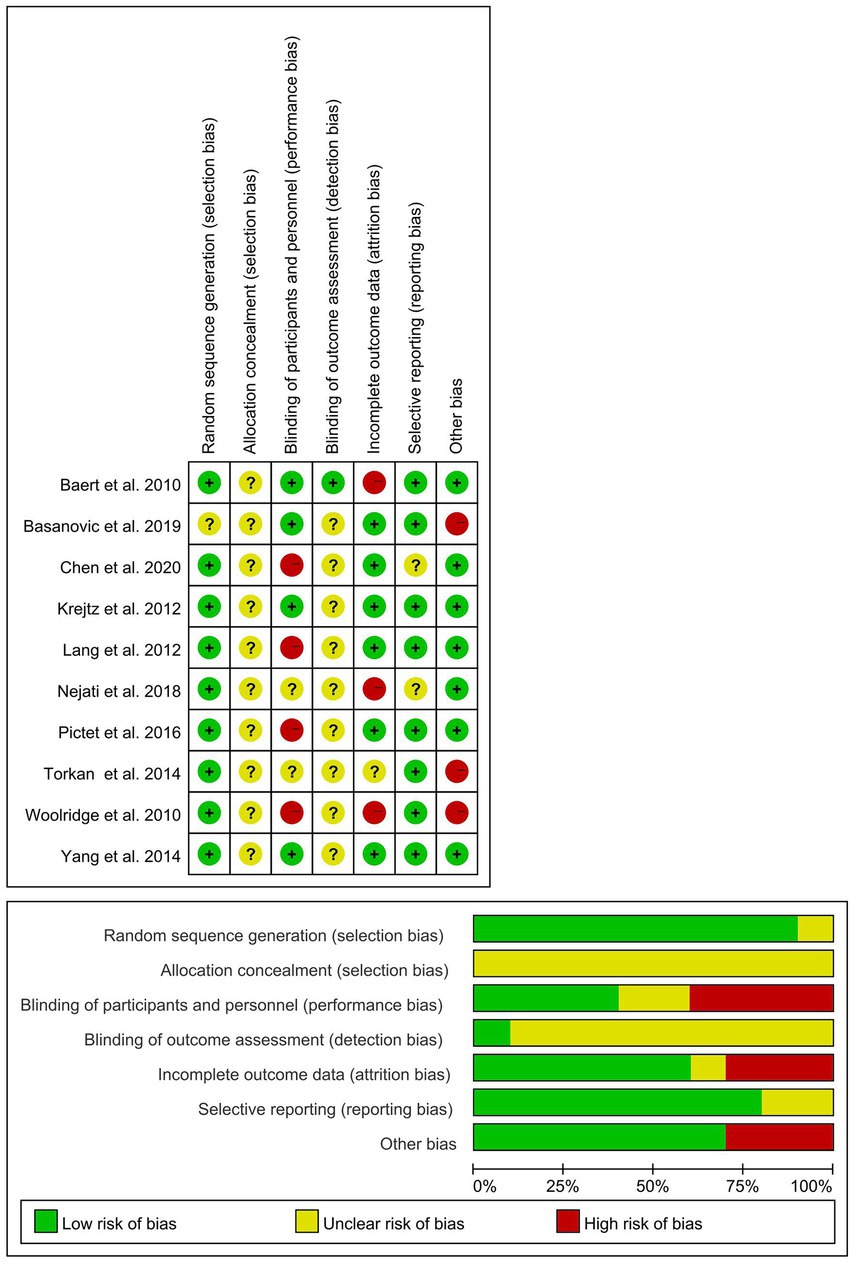
Figure 2. Risk of bias graph. Review authors’ judgments about each risk of bias item presented as percentages across all included studies.
Our study found that the analysis results of 10 studies reported the effect of CBM intervention on depression, the 95% CI (expressed numerically) of the meta-analysis results did not cross the invalid value, and both CBM significantly reduced the symptom score of depression. The total effect size was (g = −0.64, 95% CI = [−0.97–0.32], N = 10, z = −3.84, p < 0.001) and the research of heterogeneity was [Q (9) = 24.05, p = 0.004, I2 (%) = 62.6; Figure 3].
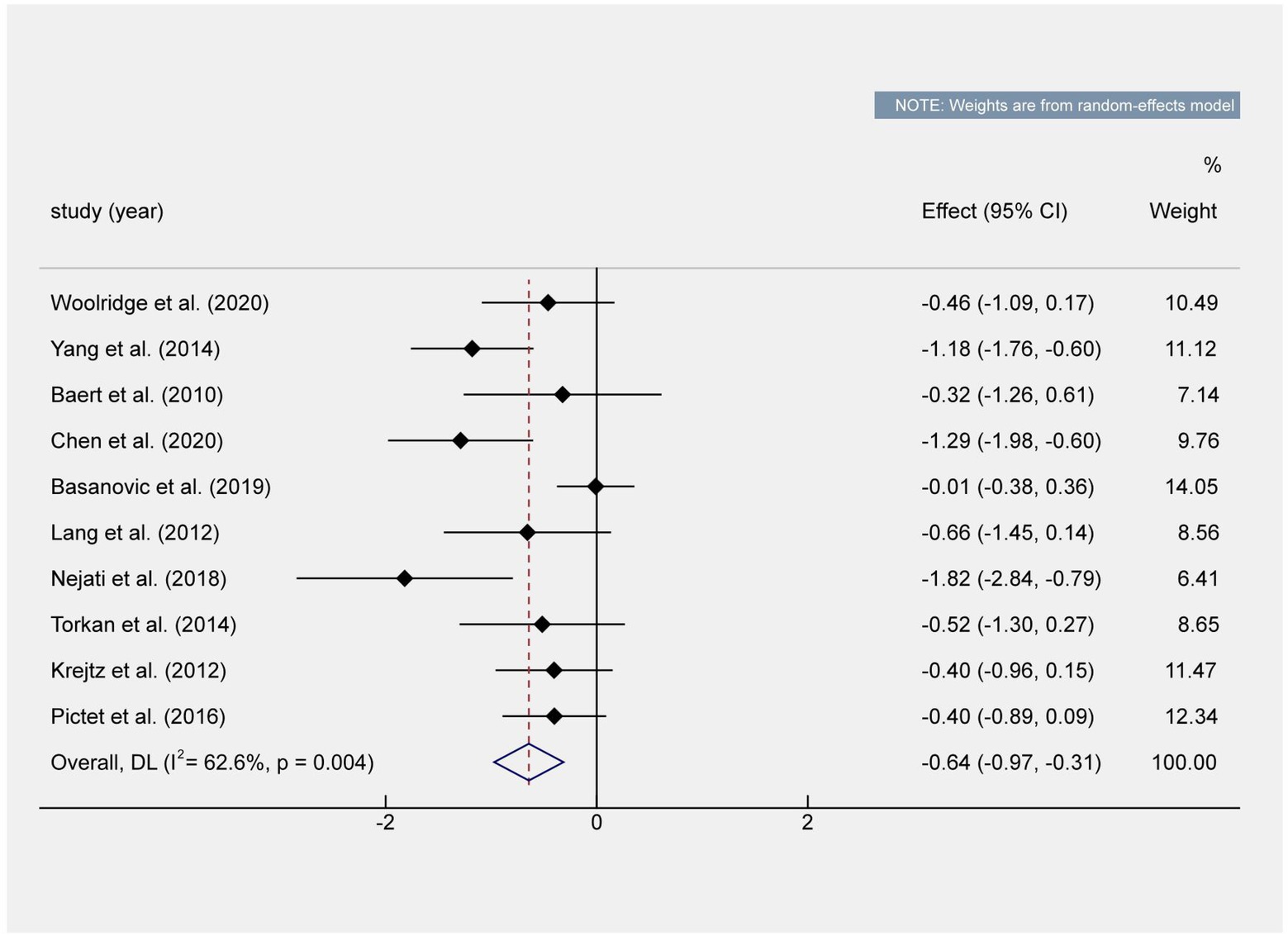
Figure 3. Overall effect shown in a forest plot. The total effect value shows that there are statistically significant differences. The effect value of the meta-analysis did not cross the invalid value.
Subgroup analyses revealed that the three training methods and CBM training setting show significant statistical differences (Table 3). For different severity of depression, the results of subjects with severe depression had statistical significance. The intervention results of subjects with mild depression did not reach statistical differences. Compared to the experimental group, both the sham training and the waiting list showed significant differences. As we can see in Table 4, the meta-regressions revealed that the mean age of participants significantly moderated the post-test effect size. But there is no significant correlation between the publication year, the proportion of women, the session, and the effect value. The study found that the mean age significantly moderated the post-test effect size with younger participants benefiting more from CBM.
Although most of the included studies were small sample studies, sensitivity analysis showed that the results of the random-effects model and the fixed-effects model were not significantly different; however, we decided to use the random utility model because we knew the heterogeneity of the research methods. Moreover, we found that sensitivity analysis and stepwise elimination showed no significant change in the final combined effect size. It is also proved that the result is robust.
We use review management to find out that the funnel plot is roughly asymmetric. Stata was used for trim-and-fill analysis, but we found that no trimming performed; and data unchanged. The Funnel asymmetry may be due to heterogeneity among studies. Continuity-corrected Begg’s test shows marginal publication bias (p = 0.049) but egger’s test shows publication bias (p = 0.038; Figure 4).
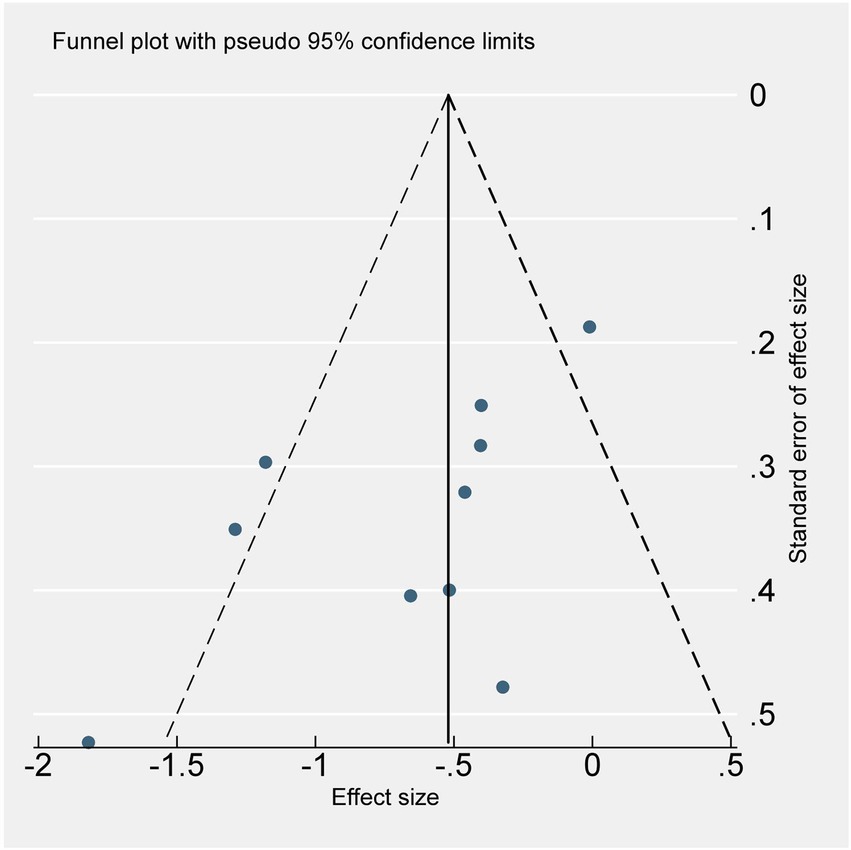
Figure 4. Funnel plot shows the publication bias and the heterogeneity. Scatter distribution suggests that there may be publication bias. Three studies fall outside the funnel chart, suggesting that there may be heterogeneity.
This is the first meta-analysis that includes three different cognitive bias modifications (CBM-A, CBM-I, and i-CBMI), and we only include depression participants. Considering the difference in cognitive symptoms between children’s symptoms and depressive symptoms in adults (Rice et al., 2019), we included only adult depression studies. Heterogeneity and publication bias of the included literature was further explored. A total of 10 studies were included with a total sample size of 467 subjects. The results show that CBM has a significant effect on depression. This is different from previous studies of CBM on depression (Fodor et al., 2020).
We found that the heterogeneity of this research is high. However, the subgroup analysis we conducted later found that the different intervention mainly causes the reason. We have estimated the high heterogeneity before the analysis of this research. The experimental methods used between groups are not the same. In the subgroup analysis, we found that the heterogeneity within the three methods was very low, while the effect values and results were stable. This study shows that the combined effect size of subjects in the CBM-I group is the largest, higher than that in the CBM-A and i-CBMI groups. But we only included three CBM-I studies, one of which combined CBM-I and CBM-A. Thus, only two studies were included in the analysis, which may lead to bias. Among the three different methods, the effect size of the CBM-A value is larger than that of the i-CBMI group. The reason may be that i-CBMI requires imagination to intervene. There is a study that shows that different people may have different abilities for imagination, which will lead to confusion about this intervention (Lang et al., 2009). The method may not take into account individual differences. Some people’s imagination is not prominent, thus, it may be difficult to ensure that the imagined scene is as clear as we think. However, considering the small sample size of this study, there are differences in the statistical data of the three methods, representing the efficacy of the three methods in alleviating depressive symptoms. Maybe we should arrange CBM paradigm according to the individual differences of subjects. We can refer to future research that may focus on which method is the most suitable way for individuals. If the patients have a great imagination, we can recommend i-CBMI intervention; if the patient has good language ability, we can recommend CBM-I intervention; and we can arrange CBM-A intervention for the patient who has great facial recognition and emotional vocabulary recognition. Therefore, we can conclude that both CBM-I and CBM-A and i-CBMI can be used as potential alternative therapies for depression.
In the laboratory, CBM intervention will produce a larger experimental effect size, enabling CBM tests and intervention to be more serious in the laboratory. We speculated that low compliance at home might be the reason (Enock et al., 2014). Interventions at home may be more dependent on the patient’s initiative, and the level of conscientiousness and concentration is less easily assured. In addition, the motivation of depressed adults, affected by symptoms (such as loss of interest, loss of pleasure, and energy exhaustion), is difficult for ensuring the full effect of the intervention. From this point of view, it may be a good plan to design a computer laboratory specifically for cognitive intervention in the future.
This study found that CBM was only effective in moderate-to-severe patients and did not achieve good results in mild patients. Nevertheless, Baert et al. found that CBM could only decrease symptom scores for those with mild depressive symptoms, while symptom scores increased for those with moderate-to-severe depression (Baert et al., 2010). Subjects with moderate-to-severe depression may have more room to lower their scores.
This research found that CBM (CBM-A, CBM-I, and i-CBMI) can significantly reduce depression symptom scores at post-test in adults. The CBM-I might be the best intervention training among the three methods. This may be because CBM-A and i-CBMI involve neurocognitive interventions, such as expression of emotion, positive/negative attention, and imagination, while CBM-I involves more top-down psychological explanation interventions. There may be some differences between them. We usually think that the neurocognitive level is the more basic part, which of course means the more difficult part to change. Moderate-to-severe depression participants and young adults tend to predict a larger effect size. It may be due to the decline of cognitive functions such as processing speed, working memory, and executive cognitive function of the elderly (Murman, 2015). CBM, as an independent treatment method, is not limited by space and can be easily intervened in homes and laboratories. Compared with other psychotherapy, it requires less effort and money, and saves a lot of resources. It can be considered as a potential complementary therapy for depression.
There are several limitations to this study. First, this study was not pre-registered, which may result in some potential bias. However, we have strictly followed the common procedures of systematic reviews. Second, there was no follow-up in some studies, and the follow-up intervals were different, which was not conducive to testing the long-term effects of CBM. Third, there are three methods of CBM, which cause heterogeneity among studies. Perhaps we need to devote all of our attention to one specific intervention paradigm in the future. Fourth, the total number of included studies is small and the sample size is relatively small, making the results of subgroup analysis less reliable, although we have used the Hedges’ g as the effect value. Fifth, we only included studies published in English journals so we may have missed some studies. We hope there will be more studies with more accuracy and larger sample sizes in the future, not limited to English studies. Finally, we found that publication bias exists. This study shows that the effect of meta-analysis calculation may overestimate the efficacy of intervention measures, suggesting that we should draw conclusions cautiously. In future studies, we need to be more rigorous, ensure that the groups are masked, and reduce the experimenter effect.
Our research results of CBM on depression show that the intervention effect of CBM-I is the most obvious, so we can devote ourselves to further improving CBM-I, for example, considering individual differences and improving the training materials. The boring experimental procedure may easily lead to psychological conflict, and the training may be affected, thus affecting the effectiveness of the intervention. Maybe we should arrange intervention exercises according to the uniqueness of the subjects. Different subjects may be suitable for different training methods. In addition, cognitive bias correction is a training method that changes cognitive bias and then emotional response. However, these changed methods will not lead to people forgetting about fear or the original related situational events but will establish a new event background. When new fear clues appear, the original automatic response mode, namely negative deviation mode, may be restored. Thus, how to promote the generalization of cognitive bias correction is very important. It can be tried that the training materials should contain as many kinds of situational clues as possible, and these life situations usually reappear in reality and cause negative prejudice. The more types of situation simulation, the more helpful it is for the subjects to learn and cope. In addition, considering the individual specificity, the subjects can recognize their negative emotional reactions and record the situation and coping style at that time, such as the negative explanation of encountering vague situations. Feedback on the recorded content was provided to scientists or psychologists in the laboratory so that the cognitive deviation correction program can be iterated and updated, and become a training version more suitable for patients themselves. In addition, some studies have shown that the fuzziness of information is an important adjustment factor for the correction of interpretation bias. If the fuzziness of information is insufficient, then no matter whether it is positive or negative stimulation, the subjects’ interpretation mode can be affected (Hoppitt et al., 2010). And ambiguity of information is an important adjustment factor to correct for interpretation bias. If the ambiguity of the information is not sufficient, then it will affect the training results. (Brosan et al., 2011). On the one hand, the laboratory encourages the subjects to strictly follow the task instructions, actively pay attention to the screen, and try to respond accurately, but more consideration should also be given to how to make the cognitive deviation correction program more participatory and interactive, even by increasing the interest, reducing the subjects’ conflict, and enhancing the popularization of cognitive deviation correction training, such as developing a program that combines cognitive bias modification with animation and games. Even virtual reality technology.
Because this study is based on the theoretical basis of cognitive therapy. It represents a shortcoming, which is restricted by the theory of cognitive therapy. Therefore, it may be a better way to integrate CBM with other therapies. In view of the relatively low clinical effect of cognitive bias correction therapy, while affirming its value, we also see its limitations. On the one hand, we need to further explore the improvement and perfection of cognitive bias correction programs as an independent training technique, and at the same time, we need to pay attention to the value of combining it with other therapies. For example, the explanation deviation correction training with a relatively large experimental effect amount is combined with behavior training, considering that the former is more based on the correction of thinking and explanation, while the latter is more about adjusting the emotional state of patients. The advantages of the combination of the two may be even greater, which of course needs further research to verify. However, previous studies have shown that the combination of online cognitive behavior therapy and cognitive deviation correction training can significantly improve the symptoms of patients (Yiend et al., 2005).
However, the integration alone may not be enough, if the effect of integration does not meet our expectations. Then, it may be necessary to re-examine the theoretical paradigm of depression. This study supports that cognitive processes and disease symptoms can be changed by correcting cognitive bias, and it is concluded that the effect value of cognitive bias correction training based on explanation is higher than that of the other two cognitive bias correction training methods. Studies have shown that the effect of cognitive bias correction based on interpretation can last for more than 24 h, and it is not easily affected by the individual’s environment (Lang et al., 2012). But on the whole, the experimental effect of cognitive deviation correction training is only low-to-moderate. This has made us think about where the future of cognitive bias correction technology will develop. We feel that this kind of program or technology seems to have some limitations. A basic assumption of cognitive therapy and cognitive assessment of emotional disorders is that cognition plays an important role in emotional resilience and vulnerability, which is confirmed by cognitive bias correction training. However, more and more experimental studies have found that the cognitive bias correction of mental disorders is a very complicated cognitive process. For example, behind some psychological symptoms, there may be many cognitive biases. Additionally, although perception or attention is the lower part of the neural mechanism, and thinking or explanation is the higher cognitive content, they are actually closely interactive processes, and some studies also show that there are common potential mechanisms among cognitive processing systems (Mathews and MacLeod, 2005). In this regard, the ideological trend of embodied concepts sweeping the cognitive building in recent years is challenging the traditional symbolic operation or processing theory. The former closely embeds the body and cognition, emphasizing the great roles of the experience and state of the body and perceptual movement in cognition. Perhaps, in the absence of complete analysis and understanding of the pathological mechanism of depression, we can partially expand the clinical treatment of depression and enrich the cognitive theory of depression by changing theoretical paradigms, such as the treatment method of combining cognitive deviation correction procedures with physical activation training mentioned earlier and the combination of cognitive deviation correction with vivid scenes by using virtual reality technology. We hope that more effective training paradigms will appear in future, to improve the well-being of patients with clinical depression.
In our research, we found that CBM has a moderate effect on depression, whether at home or in the laboratory. The effect of CBM-I paradigm training is relatively the best. In addition, CBM has statistically significant effect on adults with moderate to severe depression. Based on the effect of CBM, the core effect of human cognitive correction on emotion is further affirmed. People can try to use such a convenient computer program to help correct their biased cognition and improve their emotional symptoms, which is an economical and effective method.
The original contributions presented in the study are included in the article/Supplementary material; further inquiries can be directed to the corresponding author.
JL: data curation, conceptualization, data analysis, and writing an original draft. HM: supervision, method, and conceptualization. HYa: data curation. NZ: supervision. HYu: manuscript editing and word correction. All authors contributed to the article and approved the submitted version.
This work was supported by Jiangsu Provincial key research and development program (Grant No. BE2015609).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.968638/full#supplementary-material
Aguglia, E., Biggio, G., Signorelli, M. S., and Mencacci, C., Steering Committee on behalf of the STIMA-D Investigators (2014). Italian study on depressive disorders (STudio Italiano MAlattia Depressiva, or STIMA-D): a nationwide snapshot of the status of treatment for major depression. Pharmacopsychiatry 47, 105–110. doi: 10.1055/s-0034-1375628
Baert, S., De Raedt, R., Schacht, R., and Koster, E. H. W. (2010). Attentional bias training in depression: therapeutic effects depend on depression severity [J]. J. Behav. Ther. Exp. Psychiatry 41, 265–274. doi: 10.1016/j.jbtep.2010.02.004
Basanovic, J., Grafton, B., Ford, A., Hirani, V., Glance, D., MacLeod, C., et al. (2019). Cognitive bias modification to prevent depression (COPE): results of a randomised controlled trial. Psychol. Med. 1–12.
Beard, C., and Amir, N. (2008). A multi-session interpretation modification program: changes in interpretation and social anxiety symptoms. Behav. Res. Ther. 46, 1135–1141. doi: 10.1016/j.brat.2008.05.012
Beck, A. T. (2008). The evolution of the cognitive model of depression and its neurobiological correlates. Am. J. Psychiatry 165, 969–977. doi: 10.1176/appi.ajp.2008.08050721
Beck, A. T., and Dozois, D. J. A. (2011). Cognitive therapy: current status and future directions. Annu. Rev. Med. 62, 397–409. doi: 10.1146/annurev-med-052209-100032
Borenstein, M., Hedges, L V., Higgins, J P. T., and Rothstein, H R. (2009). Introduction to Meta-Analysis UK: John Wiley & Sons Ltd, 478–479
Bowler, J. O., Mackintosh, B., Dunn, B. D., Mathews, A., Dalgleish, T., and Hoppitt, L. (2012). A comparison of cognitive bias modification for interpretation and computerized cognitive behavior therapy: effects on anxiety, depression, attentional control, and interpretive bias. J. Consult. Clin. Psychol. 80, 1021–1033. doi: 10.1037/a0029932
Brosan, L., Hoppitt, L., Shelfer, L., Sillence, A., and Mackintosh, B. (2011). Cognitive bias modification for attention and interpretation reduces trait and state anxiety in anxious patients referred to an out-patient service: results from a pilot study. J. Behav. Ther. Exp. Psychiatry 42, 258–264. doi: 10.1016/j.jbtep.2010.12.006
Chen, R., Zheng, J., Li, T., Zhang, Q., Li, C., and Cui, L. (2022). Cognitive bias modification of interpretation training for Chinese undergraduates with depressive symptoms. Curr. Psychol. 41, 6024–6037. doi: 10.1007/s12144-020-01094-4
Dai, Q., and Feng, Z. (2012). More excited for negative facial expressions in depression: evidence from an event-related potential study. Clin. Neurophysiol. 123, 2172–2179. doi: 10.1016/j.clinph.2012.04.018
Darcet, F., Gardier, A. M., Gaillard, R., David, D. J., and Guilloux, J.-P. (2016). Cognitive dysfunction in major depressive disorder. A translational review in animal models of the disease. Pharmaceuticals 9, 2–42. doi: 10.3390/ph9010009
Enock, P. M., Hofmann, S. G., and McNally, R. J. (2014). Attention bias modification training via smartphone to reduce social anxiety: a randomized, controlled multi-session experiment. Cogn. Ther. Res. 38, 200–216. doi: 10.1007/s10608-014-9606-z
Everaert, J., Koster, E. H. W., and Derakshan, N. (2012). The combined cognitive bias hypothesis in depression. Clin. Psychol. Rev. 32, 413–424. doi: 10.1016/j.cpr.2012.04.003
Fodor, L. A., Georgescu, R., Cuijpers, P., Szamoskozi, S., David, D., Furukawa, T. A., et al. (2020). Efficacy of cognitive bias modification interventions in anxiety and depressive disorders: a systematic review and network meta-analysis. Lancet Psychiatry 7, 506–514. doi: 10.1016/s2215-0366(20)30130-9
Fritzsche, A., Dahme, B., Gotlib, I. H., Joorman, J., Magnussen, H., Watz, H., et al. (2010). Specificity of cognitive biases in patients with current depression and remitted depression and in patients with asthma. Psychol. Med. 40, 815–826. doi: 10.1017/s0033291709990948
Geerts, E., and Bouhuys, N. (1998). Multi-level prediction of short-term outcome of depression: non-verbal interpersonal processes, cognitions and personality traits. Psychiatry Res. 79, 59–72. doi: 10.1016/s0165-1781(98)00021-3
Gotlib, I. H., and Joormann, J. (2010). Cognition and depression: current status and future directions. Annu. Rev. Clin. Psychol. 6, 285–312. doi: 10.1146/annurev.clinpsy.121208.131305
Hallion, L. S., and Ruscio, A. M. (2011). A meta-analysis of the effect of cognitive bias modification on anxiety and depression. Psychol. Bull. 137, 940–958. doi: 10.1037/a0024355
Hasin, D. S., Sarvet, A. L., Meyers, J. L., Saha, T. D., Ruan, W. J., Stohl, M., et al. (2018). Epidemiology of adult DSM-5 major depressive disorder and its Specifiers in the United States. JAMA Psychiat. 75, 336–346. doi: 10.1001/jamapsychiatry.2017.4602
Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The cochrane collaboration’s tool for assessing risk of bias in randomised trials. Bmj 343. doi: 10.1136/bmj.d5928
Hoppitt, L., Mathews, A., Yiend, J., and Mackintosh, B. (2010). Cognitive mechanisms underlying the emotional effects of bias modification. Appl. Cogn. Psychol. 24, 312–325. doi: 10.1002/acp.1678
Ironside, M., O'Shea, J., Cowen, P. J., and Harmer, C. J. (2016). Frontal cortex stimulation reduces vigilance to threat: implications for the treatment of depression and anxiety. Biol. Psychiatry 79, 823–830. doi: 10.1016/j.biopsych.2015.06.012
Jonassen, R., Harmer, C. J., Hilland, E., Maglanoc, L. A., Kraft, B., Browning, M., et al. (2019). Effects of Attentional bias modification on residual symptoms in depression: a randomized controlled trial. BMC Psychiatry 19:141. doi: 10.1186/s12888-019-2105-8
Joormann, J., Waugh, C. E., and Gotlib, I. H. (2015). Cognitive bias modification for interpretation in major depression: effects on memory and stress reactivity. Clin. Psychol. Sci. 3, 126–139. doi: 10.1177/2167702614560748
Krejtz, I., Holas, P., Rusanowska, M., and Nezlek, J. B. (2018). Positive online attentional training as a means of modifying attentional and interpretational biases among the clinically depressed: an experimental study using eye-tracking. J. Clin. Psychol. 74, 1594–1606. doi: 10.1002/jclp.22617
Lang, T. J., Blackwell, S. E., Harmer, C. J., Davison, P., and Holmes, E. A. (2012). Cognitive bias modification using mental imagery for depression: developing a novel computerized intervention to change negative thinking styles. Eur. J. Personal. 26, 145–157. doi: 10.1002/per.855
Lang, T. J., Moulds, M. L., and Holmes, E. A. (2009). Reducing depressive intrusions via a computerized cognitive bias modification of appraisals task: developing a cognitive vaccine. Behav. Res. Ther. 47, 139–145. doi: 10.1016/j.brat.2008.11.002
LeMoult, J., Joormann, J., Kircanski, K., and Gotlib, I. H. (2016). Attentional bias training in girls at risk for depression. J. Child Psychol. Psychiatry 57, 1326–1333. doi: 10.1111/jcpp.12587
Levens, S. M., and Gotlib, I. H. (2009). Impaired selection of relevant positive information in depression. Depress. Anxiety 26, 403–410. doi: 10.1002/da.20565
Mathews, A., and MacLeod, C. (2005). Cognitive vulnerability to emotional disorders. Annu. Rev. Clin. Psychol. 1, 167–195. doi: 10.1146/annurev.clinpsy.1.102803.143916
Murman, D. L. (2015). The impact of age on cognition [J]. Semin. Hear. 36, 111–121. doi: 10.1055/s-0035-1555115
Murrough, J. W., Iacoviello, B., Neumeister, A., Charney, D. S., and Iosifescu, D. V. (2011). Cognitive dysfunction in depression: neurocircuitry and new therapeutic strategies. Neurobiol. Learn. Mem. 96, 553–563. doi: 10.1016/j.nlm.2011.06.006
Nejati, V., Fathi, E., Shahidi, S., and Salehinejad, M. A. (2018). Cognitive training for modifying interpretation and attention bias in depression: relevance to mood improvement and implications for cognitive intervention in depression. Asian J. Psychiatr. 39, 23–28. doi: 10.1016/j.ajp.2018.11.012
Ochsner, K. N., Ray, R. D., Cooper, J. C., Robertson, E. R., Chopra, S., et al. (2004). For better or for worse: neural systems supporting the cognitive down and up regulation of negative emotion. NeuroImage 23, 483–499. doi: 10.1016/j.neuroimage.2004.06.030
Orchard, F., Pass, L., and Reynolds, S. (2016). 'It was all my Fault'; negative interpretation bias in depressed adolescents. J. Abnorm. Child Psychol. 44, 991–998. doi: 10.1007/s10802-015-0092-x
Pictet, A., Jermann, F., and Ceschi, G. (2016). When less could be more: investigating the effects of a brief internet-based imagery cognitive bias modification intervention in depression. Behav. Res. Ther. 84, 45–51. doi: 10.1016/j.brat.2016.07.008
Rice, F., Riglin, L., Lomax, T., Souter, E., Potter, R., Smith, D. J., et al. (2019). Adolescent and adult differences in major depression symptom profiles. J. Affect. Disord. 243, 175–181. doi: 10.1016/j.jad.2018.09.015
Riley, R. D., Higgins, J. P. T., and Deeks, J. J. (2011). Interpretation of random effects meta-analyses. BMJ 342:d549. doi: 10.1136/bmj.d549
Roiser, J. P., Elliott, R., and Sahakian, B. J. (2012). Cognitive mechanisms of treatment in depression. Neuropsychopharmacology 37, 117–136. doi: 10.1038/npp.2011.183
Salem, T., Winer, E. S., and Nadorff, M. R. (2018). Combined behavioural markers of cognitive biases are associated with anhedonia. Cognit. Emot. 32, 422–430. doi: 10.1080/02699931.2017.1307808
Simon, G. E., and Ludman, E. J. (2009). It's time for disruptive innovation in psychotherapy. Lancet 374, 594–596. doi: 10.1016/s0140-6736(09)61415-x
Stovold, E., Beecher, D., Foxlee, R., and Noel-Storr, A. (2014). Study flow diagrams in Cochrane systematic review updates: an adapted PRISMA flow diagram. Syst. Rev. 3:54. doi: 10.1186/2046-4053-3-54
Sudak, D. M. (2012). Cognitive behavioral therapy for depression. Psychiatr. Clin. North Am. 35, 99–110. doi: 10.1016/j.psc.2011.10.001
Tanaka, M., Szabó, A., Spekker, E., Polyák, H., Tóth, F., and Vécsei, L. (2022). Mitochondrial impairment: a common motif in neuropsychiatric presentation? The link to the tryptophan–Kynurenine metabolic system. Cells 11:2607. doi: 10.3390/cells11162607
Torkan, H., Blackwell, S., Holmes, E. A., Kalantari, M., Neshat-Doost, H. T., Maroufi, M., et al. (2014). Positive imagery cognitive bias modification in treatment-seeking patients with major depression in Iran: a pilot study. Cogn. Ther. Res. 38, 132–145. doi: 10.1007/s10608-014-9598-8
WHO (2021). Depression. Available at: https://www.who.int/news-room/fact-sheets/detail/depression
Woolridge, S. M., Harrison, G. W., Best, M. W., and Bowie, C. R. (2022). Attention bias modification in depression: A randomized trial using a novel, reward-based, eye-tracking approach. J. Behav. Ther. Exp. Psychiatry doi: 10.1016/j.jbtep.2020.101621
Yang, W., Ding, Z., Dai, T., Peng, F., and Zhang, J. X. (2015). Attention bias modification training in individuals with depressive symptoms: A randomized controlled trial. J. Behav. Ther. Exp. Psychiatry 49, 101–111. doi: 10.1016/j.jbtep.2014.08.005
Yaroslavsky, I., Allard, E. S., and Sanchez-Lopez, A. (2019). Can't look away: attention control deficits predict rumination, depression symptoms and depressive affect in daily life. J. Affect. Disord. 245, 1061–1069. doi: 10.1016/j.jad.2018.11.036
Yiend, J., Mackintosh, B., and Mathews, A. (2005). Enduring consequences of experimentally induced biases in interpretation [J]. Behav. Res. Ther. 43, 779–797. doi: 10.1016/j.brat.2004.06.007
Keywords: depression, review, meta-analysis, cognitive bias modification, cognitive bias
Citation: Li J, Ma H, Yang H, Yu H and Zhang N (2023) Cognitive bias modification for adult’s depression: A systematic review and meta-analysis. Front. Psychol. 13:968638. doi: 10.3389/fpsyg.2022.968638
Received: 14 June 2022; Accepted: 07 December 2022;
Published: 19 January 2023.
Edited by:
Gabriele Nibbio, University of Brescia, ItalyReviewed by:
Masaru Tanaka, University of Szeged (ELKH-SZTE), HungaryCopyright © 2023 Li, Ma, Yang, Yu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Ma,  bWFodWlfbmptdUAxMjYuY29t
bWFodWlfbmptdUAxMjYuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.