
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Psychol. , 05 September 2022
Sec. Health Psychology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.960373
This article is part of the Research Topic Psychosocial and Bioethical Challenges and Developments for The Future of Vascularized Composite Allotransplantations View all 11 articles
 Jessica Gacki-Smith1
Jessica Gacki-Smith1 Brianna R. Kuramitsu1
Brianna R. Kuramitsu1 Max Downey2
Max Downey2 Karen B. Vanterpool2
Karen B. Vanterpool2 Michelle J. Nordstrom3
Michelle J. Nordstrom3 Michelle Luken4
Michelle Luken4 Tiffany Riggleman4
Tiffany Riggleman4 Withney Altema4
Withney Altema4 Shannon Fichter4
Shannon Fichter4 Carisa M. Cooney5
Carisa M. Cooney5 Greg A. Dumanian6
Greg A. Dumanian6 Sally E. Jensen7
Sally E. Jensen7 Gerald Brandacher8
Gerald Brandacher8 Scott Tintle9
Scott Tintle9 Macey Levan10,11
Macey Levan10,11 Elisa J. Gordon12*
Elisa J. Gordon12*Background: People with upper extremity (UE) amputations report receiving insufficient information about treatment options. Furthermore, patients commonly report not knowing what questions to ask providers. A question prompt sheet (QPS), or list of questions, can support patient-centered care by empowering patients to ask questions important to them, promoting patient-provider communication, and increasing patient knowledge. This study assessed information needs among people with UE amputations about UE vascularized composite allotransplantation (VCA) and developed a UE VCA-QPS.
Methods: This multi-site, cross-sectional, mixed-methods study involved in-depth and semi-structured interviews with people with UE amputations to assess information needs and develop a UE VCA-QPS. Qualitative data were analyzed by thematic analysis; quantitative data were analyzed by descriptive statistics. The initial UE VCA-QPS included 130 items across 18 topics.
Results: Eighty-nine people with UE amputations participated. Most were male (73%), had a mean age of 46 years, and had a unilateral (84%) and below-elbow amputation (56%). Participants desired information about UE VCA eligibility, evaluation process, surgery, risks, rehabilitation, and functional outcomes. After refinement, the final UE VCA-QPS included 35 items, across 9 topics. All items were written at a ≤ 6th grade reading level. Most semi-structured interview participants (86%) reported being ‘completely’ or ‘very’ likely to use a UE VCA-QPS.
Conclusion: People with UE amputations have extensive information needs about UE VCA. The UE VCA-QPS aims to address patients’ information needs and foster patient-centered care. Future research should assess whether the UE VCA-QPS facilitates patient-provider discussion and informed decision-making for UE VCA.
Upper extremity (UE) vascularized composite allotransplantation (VCA) is a treatment option for people with hand and/or arm amputations that involves “transplantation of non-autologous vascularized tissues including skin, muscle, nerve, tendon and/or bone as a functional unit (e.g., a hand) to replace non-reconstructible tissue defects” (American Society of Transplant Surgeons, 2022). To date, 56 UE VCAs have been performed on 37 patients in the United States (OPTN, 2022), and more than 120 have been performed worldwide (Shores et al., 2017).
Upper extremity VCA is one of several treatment options (e.g., myoelectric and mechanical prostheses) for people with UE amputations. UE VCA is an innovative treatment modality that restores body wholeness and function for patients with complex reconstructive needs (Rose et al., 2019). Evidence suggests that people with UE amputations lack awareness and knowledge of UE VCA. People with UE limb loss report receiving insufficient information about their treatment options and report that healthcare providers do not engage in enough discussion about their condition (Nielsen, 1991; Pedlow et al., 2014; Pasquina et al., 2015; Bennett, 2016). Further, little is known about what information people with UE amputations need to know about UE VCA, which is necessary for optimizing their informed consent.
A patient-centered approach to care involves respecting and responding to patients’ needs and preferences, so they can make informed treatment decisions (Institute of Medicine, Committee on Quality of Health Care in America, 2001; Epstein and Street, 2011). Elements of patient-centered care include effective communication and information exchange. Effective communication entails a dialogue between provider and patient, and patient question-asking can increase patient engagement, empowerment, and the quality of provider information-giving (Barnlund, 1970; Shepherd et al., 2011; Barton et al., 2020). However, patients commonly do not know what questions to ask to guide decision making (Lopez-Vargas et al., 2014; Lederer et al., 2016; Schwarze et al., 2020). To date, no educational interventions have been developed to increase knowledge and understanding about UE VCA for people with UE amputations.
Communication tools, such as a question prompt sheet (QPS), can facilitate patient-provider communication and support patient-centered care (Belkora et al., 2009; Gordon and Ison, 2014; Brandes et al., 2015; Sansoni et al., 2015; Satteson et al., 2020). A QPS is a list of questions that can empower patients to ask questions about topics important to them and promote discussion between patients and their providers. QPSs have been shown to help patients obtain information, increase the number of questions asked, improve patient-provider communication, increase patient knowledge, increase patient satisfaction, and reduce or have no effect on consultation time across clinical settings (e.g., oncology, chronic kidney disease, palliative care) (Brown et al., 2001, 2011; Gaston and Mitchell, 2005; Brandes et al., 2015; Sansoni et al., 2015; Arthur et al., 2017; Miller and Rogers, 2018; Jayasekera et al., 2020). No QPS about UE VCA has been created for people with UE amputations.
This study assessed the information needs of people with UE amputations and developed a UE VCA-specific QPS to foster patient-centered care. Our UE VCA-QPS was designed to help people with UE amputations attain greater information about UE VCA and establish realistic expectations through patient-provider communication to make informed decisions about UE VCA.
In this cross-sectional study, we used a mixed-methods concurrent triangulation design (Greene et al., 1989; Creswell and Plano Clark, 2007), involving sequential in-depth and semi-structured interviews to develop and refine the UE VCA-QPS, as part of a larger study on decision making about UE VCA. Mixed-methods enabled elaboration and clarification of findings, increased validity of results, and informed subsequent data collection. We followed QPS development approaches used previously (Eggly et al., 2013; Ahmed et al., 2016; Lederer et al., 2016), and leveraged perspectives of patients and experts to ensure that the UE VCA-QPS is patient-centered.
The study was conducted at Northwestern University Feinberg School of Medicine (NU) in Chicago, IL, United States; Johns Hopkins University School of Medicine (JHU) in Baltimore, MD, United States; and Walter Reed National Military Medical Center (WRNMMC) in Bethesda, MD, United States from January 2020 through March 2022. Shirley Ryan AbilityLab in Chicago, IL, United States and David Rotter Prosthetics, LLC in Joliet, IL, United States supported recruitment for NU. The study was approved by the Institutional Review Boards at: NU (STU00209718), JHU (00225728), and WRNMMC (WRNMMC-EDO-2020-0432). NU served as the Institutional Review Board of record for WRNMMC. We used the Consolidated Criteria for Reporting Qualitative Research for quality reporting of qualitative studies (Tong et al., 2007).
Eligible participants were English-speaking adults age 18–65 years with acquired UE amputations who had not yet pursued UE VCA, UE VCA candidates (i.e., individuals who contacted a transplant center to express interest in pursuing UE VCA), UE VCA participants (i.e., individuals who began UE VCA evaluation), and UE VCA recipients. People who were cognitively impaired, and/or had congenital limb loss were excluded.
Multiple techniques were employed to increase sample size and ensure a representative sample (Patton, 2015). We recruited patients from study sites by mailing and/or emailing eligible individuals a letter describing the study, followed by a phone call a week later to screen for eligibility. Research team members did not have prior established relationships with study participants. We also recruited participants through support groups (n = 304) and social media websites (Facebook and Reddit) by emailing or posting study flyers online. Interested individuals contacting the team were screened by phone for eligibility. All participants provided verbal informed consent.
In Phase 1, we conducted telephone in-depth interviews from July 2020–March 2022 to assess study participants’ information needs and questions about UE VCA. We drew upon five open-ended questions from the in-depth interview guide, which assessed: UE VCA information needs (“If you were thinking about getting an upper limb transplant, what would you want to know about it?” and “If you were thinking about getting an upper limb transplant, what information would you need?); UE VCA-related questions (“If you were thinking about getting an upper limb transplant, what questions would you have about it?”); and perceptions about a UE VCA-QPS (“What do you think about the QPS idea?” and “Would [the QPS] be worthwhile?”). The subset of candidates, participants, and recipients were also asked what people seeking UE VCA should be informed about (“What questions should people seeking an upper limb transplant ask about it to become well informed?” and “Could you suggest some things about upper limb transplantation that people with amputations should be informed about?”).
Interviews assessed study participants’ likelihood of using a UE VCA-QPS (on a 5-point Likert scale anchored by “Not At All,” “A Little,” “Somewhat,” “A Lot,” and “Completely”); demographics (e.g., age, gender); clinical background (e.g., date of amputation, amputation level and type); and health literacy (“How often do you need to have someone help you when you read instructions, pamphlets, or other written material from your doctor or pharmacy?” anchored by “Never,” “Rarely,” “Sometimes,” “Often,” and “Always”; “Never” and “Rarely” responses reflected adequate health literacy) (Morris et al., 2006).
Interviews were conducted by female and male research team members (BK, KV, MD, MN) trained by the Principal Investigator (EJG), a seasoned qualitative researcher, to ensure consistent and high quality data collection. Telephone cognitive interviews were conducted (by BK) with five participants prior to in-depth interviews (January–March 2020) using standard “think aloud” procedures to ensure interview guide questions were interpreted as intended and improve question wording (Singleton and Straits, 2017). Research team members took field notes during and after interviews. Interviews lasted, on average, 78 (range: 37–140) minutes and were audio-recorded and transcribed. Participants were compensated with a $35 gift card.
To identify potential QPS items, two members of the research team at each study site reviewed each transcription and compiled participants’ responses about UE VCA information needs and questions into a single document using content analysis (Bernard and Ryan, 1998). Responses were grouped into topics organized in terms of a patient’s progress from initiating evaluation to rehabilitation. All interview transcripts were then re-examined by research team members as individual files (within-case) and as a list of all participant responses to each open-ended question (across-cases) (Ayres et al., 2003). The Principal Investigator then reviewed responses under each topic to derive draft QPS items that synthesized the information needs and questions raised by all participant responses. Thereafter, the research staff reviewed the draft QPS items to: (a) confirm that they fully represented all participants’ responses, (b) add or delete repetitive or idiosyncratic items, and (c) revise item wording for clarity. This iterative process ensured comprehensiveness. All items were compiled into a first QPS draft comprising 130 items organized into 18 topics.
To identify UE VCA information needs, all transcripts were analyzed for themes emergent from the data using constant comparison, inductive, and deductive coding methods (Lincoln and Guba, 1985; Bradley et al., 2007). The research team established an initial codebook by developing deductive codes based on questions asked in the interview guide (e.g., Information Needs). The team then developed inductive codes based on themes emergent from the data during open coding of six transcripts until reaching thematic saturation (Miles and Huberman, 1994; Giacomini and Cook, 2000). Thereafter, two research team members at each study site (JG-S, BK, MD, KV, MN, ML) independently coded transcripts from their site using the finalized codebook in NVivo (Release 1.6.1, QSR International) until reaching inter-rater reliability (Cohen’s Kappa > 0.80) (Guest et al., 2011). Then, all transcripts were re-coded. During this process, the two research team members at each site resolved coding discrepancies through discussion. Finally, research team members reviewed all text segments coded as “Information Needs” to identify patterns and themes in study participants’ UE VCA information needs and developed code summaries (Keith et al., 2017).
Upper extremity VCA-QPS item reduction was performed by three research team members (EJG, BK, JG-S) by identifying redundancy and combining or removing redundant items to retain items that best conveyed the ideas. We assessed the readability of each item using the Flesch-Kincaid grade level formula (Stossel et al., 2012; Centers for Medicare & Medicaid Services [CMS], 2010), and simplified complex words and long sentences in items above a 6th grade reading level (Houts et al., 2006; Brega et al., 2015). Some items remained above a 6th grade reading level because they included terms that could not be restated in a simpler way or included three or more syllables (e.g., transplantation, anti-rejection, recipient). Additionally, we assessed the understandability and actionability of the UE VCA-QPS by applying the Patient Education Materials Assessment Tool (PEMAT) (Shoemaker et al., 2013). Following item refinement and reduction, the draft QPS included 77 items categorized into 16 topics.
A 7-person multidisciplinary team of study collaborators comprised of researchers, UE VCA clinicians/surgeons, hand reconstructive surgeons, and occupational therapists reviewed the draft UE VCA-QPS and provided feedback on clinical accuracy, relevance to the UE VCA transplant evaluation process, clarity of question wording, and redundancy in question content. Based on the feedback, the research team revised item wording for clarity, moved items to different topic categories, combined items that addressed similar concepts, added items, and deleted items. Figure 1 includes examples of changes made to items and the rationale, based on multidisciplinary team feedback and research team review. Thereafter, the preliminary UE VCA-QPS included 52 items categorized into 12 topics.
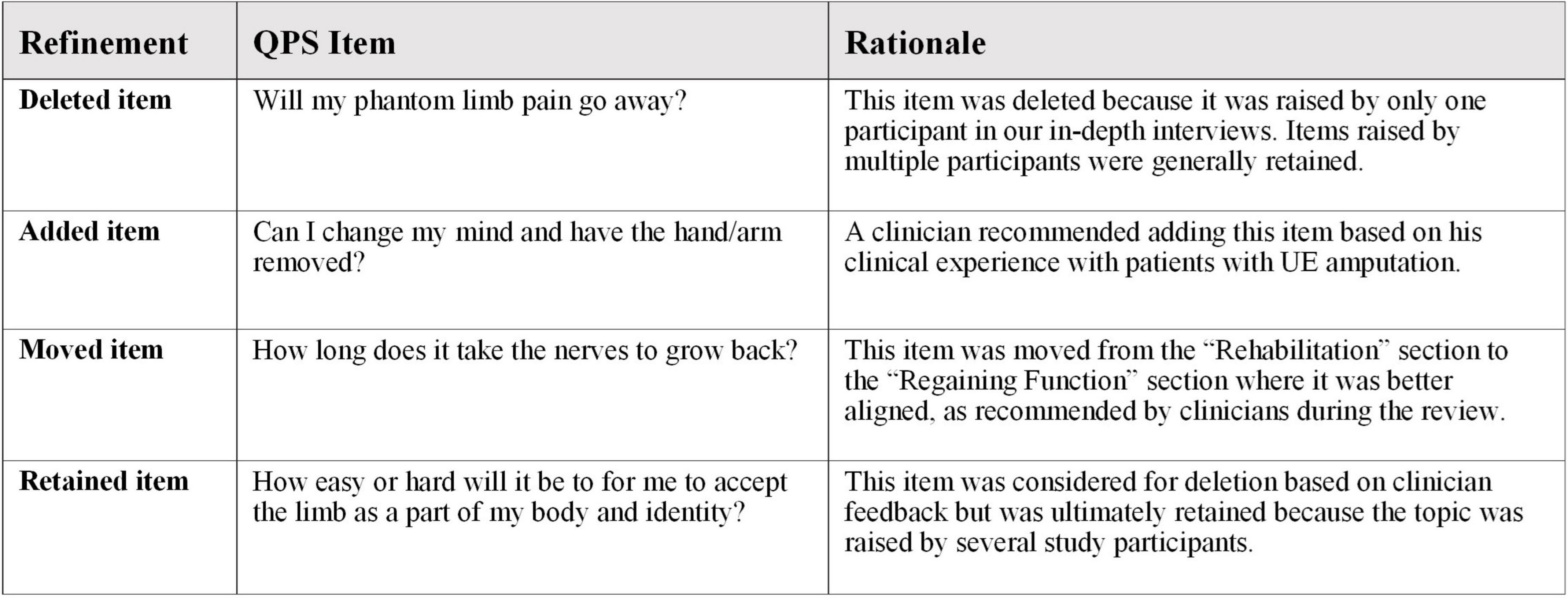
Figure 1. Examples of interim UE VCA-QPS refinement based on multidisciplinary feedback and research team review.
Semi-structured telephone interviews were conducted from September 2021– March 2022 by female and male research team members (BK, MD, WA, SF), trained by the Principal Investigator (EJG), to refine and reduce the 52-item preliminary UE VCA-QPS. Participants were asked to rate whether each question should be included in the UE VCA-QPS list on a 4-point Likert scale anchored by 4–“Definitely Keep,” 3–“Probably Keep,” 2–“Probably Cut,” and 1–“Definitely Cut.” Larger scores indicated a preference for item retention. When rating each question, participants were asked to consider how valuable each question and its answer would be to them if they were interested in the option of UE VCA. Closed-ended questions assessed participants’ likelihood of using the UE VCA-QPS if they were considering getting a UE VCA (on a 5-point Likert scale anchored by “Not At All,” “A Little,” “Somewhat,” “Very,” and “Completely”) and demographic and clinical characteristics (e.g., age, gender, amputation type and level, date of amputation). Open-ended questions assessed perceptions of the clarity of each item and suggestions for improving item wording, preferences between similar items, opinions about item order, and recommendations for adding or deleting questions. Interviews averaged 70 (range: 40–120) minutes and were audio-recorded, while research team members took field notes. Participants were compensated with a $35 gift card.
Frequencies and means for each item’s Likert score were generated and reviewed. All items with a mean score of 3.00 or smaller were eliminated, resulting in 11 items cut from the list. Remaining items’ scores and qualitative responses were analyzed together. Participants’ qualitative responses were reviewed by the research team (EJG, JG-S, BK) to identify QPS item changes (e.g., rewording items, combining items, moving items). After refining QPS items, the draft QPS included 38 items categorized into 12 topics.
We then sought feedback on this UE VCA-QPS draft from the study’s Scientific Advisory Board (SAB), comprised of four bioethicists, and from the research team’s Co-Investigators, who included two UE VCA clinicians/surgeons and two hand surgeons, for further refinement. The SAB and Co-Investigators provided feedback on improving item wording and identifying items to combine, delete, or add. Further, the SAB and Co-Investigators were asked to ensure that items covered perspectives of people with UE amputations, the military, VCA ethics, UE VCA clinical care, hand surgery, rehabilitation, prosthetics, and disability rights. These steps aimed to ensure that the UE VCA-QPS would be relevant and meaningful for patient-provider discussions about UE VCA. Demographics and clinical characteristics of participants in the in-depth and semi-structured interviews were analyzed through descriptive statistics using IBM SPSS Statistics (Version 27).
Overall, 89 people with UE amputations participated (63.9% participation rate) in in-depth interviews (n = 50, 61.7% participation rate) and semi-structured interviews (n = 56, 65.9% participation rate) (Supplementary Figure 1). Seventeen individuals participated in both the in-depth interview and the semi-structured interview (NU: n = 4, JHU: n = 8, WRNMMC: n = 5). Sixty refused to participate before or after providing consent because they were not interested, too busy, compensation was too low, or they did not show up for their scheduled interview. Study participants included people with UE amputations who had not pursued UE VCA (85%), UE VCA candidates and participants (9%), and UE VCA recipients (6%). Most participants were male (73%), White (74%), on average 46 years of age, and had a unilateral amputation (84%) and had a below elbow amputation (56%) (Table 1). Participants were interviewed, on average, 10 years after their amputation. One-third (34%) did not use a prosthesis(es).
When asked what information they would need if they were to pursue UE VCA, study participants reported different types of information that were organized into five major themes: broad and contextual information, information about the pre-UE VCA period, risks of UE VCA, the UE VCA procedure, and information about the post-UE VCA period. The major themes and subthemes are described below, with illustrative representative quotations presented in Table 2.
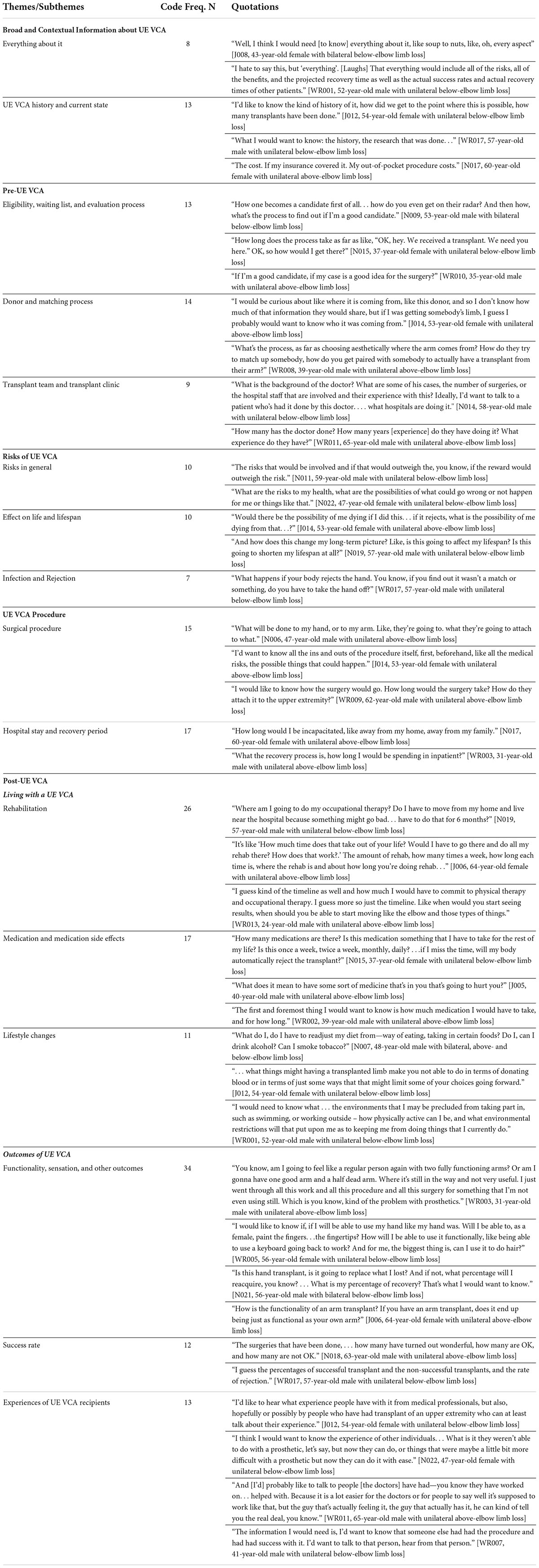
Table 2. Representative illustrative quotations about information needs by major theme and subtheme, with code frequency.
Participants desired broad and contextual information about UE VCA that included knowing “everything” about it as well as the historical context and present status of UE VCA. Knowing “everything” about UE VCA would enable participants to gain “a more in-depth understanding.” Participants desired historical information including “the research that was done,” and how the transplant field got “to the point where this is possible.” The current status of the UE VCA field pertained to “how many people have had the procedure done” and “the current state of technology.” Additionally, only participants at NU wanted to know about the “upfront and lifetime costs” of UE VCA and the insurance coverage and out-of-pocket expenses.
Several participants wanted information about the processes occurring prior to the UE VCA procedure. This information encompassed the eligibility criteria for UE VCA (e.g., “what would make a good qualified patient…”), the waiting list (e.g., “how long of a wait [would there be] on the waiting list for a set of arms to become available”), and the evaluation process (e.g., what does “the psychological review process… entail”). Participants also desired information about the donor process, such as “how long do you have to typically wait for a donor” and how well can they “match an arm to my body to make it look more realistic for myself.” Participants desired learning about the transplant team and clinic, such as the “doctors and clinicians [who have] done it and have had success,” “how many procedures they have done,” and “where it would be taking place.”
Participants wanted information about the risks of UE VCA, including general risks and the potential affect UE VCA could have on one’s life. General UE VCA risks included “the possibilities of what could go wrong” from receiving a UE VCA. Participants desired information on how UE VCA could potentially harm a person’s life and lifespan, including the “rate of life-threatening risks,” the risk of dying, infection, rejection, and whether recipients would “be more susceptible to cancers or other things like COVID.”
Participants desired information about the UE VCA surgical procedure, including the hospital stay and recovery period. Desired procedure details included “how they attach the bone,” the required number of surgeries, and the “length of time the surgery usually takes.” Others wanted information about the length of hospital stay post-transplant, and the recovery process: “how long [the UE VCA] is going to take to heal.”
Participants expressed interest in learning how UE VCA impacts a recipient’s life as it relates to medication and medication side effects, rehabilitation, function, success rate, lifestyle changes, and experiences of UE VCA recipients. Regarding medication and medication side effects, participants desired information on “how many drugs you have to be on for the rest of your life” and the “risk levels of life-time, consistent use of drugs and side effects of the drugs.” Study participants also desired information on what “the rehab process [would] be like,” how long they would do hand therapy, and “how much time [it would] take out of [their] life.”
Participants were interested in learning about the type and extent of functionality a UE VCA would provide, whether recipients would “experience the sensation of touch again,” and how long it would take “to get it working.” Some referred to their previous “natural hand” and wanted to know if a UE VCA would “work like my old arm worked.” Participants framed their interest in learning about the success rate in terms of “how many [UE VCAs] failed versus how many succeeded.” Others wanted to learn about required lifestyle changes, such as how long recipients might be “out of work” and any restrictions on diet, drinking alcohol, and smoking. Several participants reported interest in learning directly from UE VCA recipients about their experiences: “what kind of things can, and can’t they do.”
The final UE VCA-QPS has 35 items, organized into 9 main topics, and fits onto one double-sided page of paper. At the end of the list, patients can note additional questions. The UE VCA-QPS is available upon request.
Mean ratings of QPS items in the semi-structured interviews ranged from 2.70 to 3.93. Items ranked largest, reflecting preference for retention, were primarily about UE VCA risks. Items ranked moderately high were about UE VCA functional outcomes.
Among in-depth interview participants, most who were asked (n = 36/45, 80%) reported being “Completely” or “A Lot” likely to use a QPS (Table 3). Among all semi-structured interview participants, most (86%) reported being “Completely” or “Very” likely to use a QPS.
Through mixed-methods research, we developed a 35-item QPS specific to UE VCA to address the information needs of people with UE amputations and facilitate patient-centered care. Our study participants had extensive information needs, focusing on risks, the rehabilitation process, and expectations for functional and other outcomes of UE VCA. The UE VCA-QPS is intended for use in the UE VCA clinical context amongst candidates and participants undergoing UE VCA evaluation. Study participants reported a high likelihood of using the UE VCA-QPS in a clinic visit if they were to pursue UE VCA. The UE VCA-QPS supports patient-centered care by promoting patient-provider communication that addresses patients’ unique information needs and fosters information sharing so that patients can make informed treatment decisions.
People with UE amputations are typically healthy people, who generally have little need to know about transplantation. Our study participants had considerable information needs suggesting that they had limited knowledge of transplantation, rejection, and anti-rejection medications, which underscores the need to help people with UE amputations learn about the UE VCA option and establish realistic expectations so that they can make informed treatment decisions. The higher priority placed on risks and functional outcomes by participants in the semi-structured interviews indicates the relative importance that providers should emphasize in their discussions about UE VCA.
Our finding that only NU participants desired information about the costs of UE VCA makes sense considering that: (a) JHU participants included more UE VCA candidates, participants, and recipients and were thus more familiar with the insurance and out-of-pocket costs associated with UE VCA; and (b) all WRNMMC participants were military health system beneficiaries whose healthcare costs are covered by the federal government.
The UE VCA-QPS can be provided to patients in advance of their first visit to the VCA clinic, or it can be provided to them for review while waiting in the clinic to see their provider so that they can become more empowered to communicate with providers. Evidence shows a QPS may be more effective at increasing patient question-asking and provider information-giving when the QPS is provided to patients shortly before they meet with their provider (Sansoni et al., 2015). By reviewing the UE VCA-QPS prior to seeing the provider, the patient can identify questions they find important and become more engaged during their visit. Providers should ask patients for their QPS question list at the beginning of their visit given that other research has shown this provider practice of “endorsement” is effective at increasing the number of questions asked by patients and the amount of information provided by doctors during consultations (Sansoni et al., 2015).
In general, QPSs can vary in format and length. The number of items in other QPSs range from 3 to 169 items, with a mean of 33 items (Kinnersley et al., 2007; Brandes et al., 2015; Sansoni et al., 2015). Our 35-item UE VCA-QPS is comprehensive while also convenient in fitting onto a two-sided single page of paper for easy distribution, or may be viewed as an electronic document on a mobile phone, tablet, or computer.
Future research should assess the effectiveness of the UE VCA-QPS in facilitating communication between patients and providers in the UE VCA clinical context, as well as patients’ informed decision-making about UE VCA. Implementation science research should assess the most acceptable, appropriate, and feasible way of delivering and evaluating the UE VCA-QPS.
Strengths of our study include a multi-site study design conducted in geographically diverse locations in the US, and included individuals throughout the US. Our sample included civilian and military participants with unilateral and bilateral amputations that were above and/or below the elbow, which supports the transferability of findings, despite being a challenging population to recruit. Additionally, our sample is representative of the broader population of people with UE amputations in terms of gender, race, and age (Inkellis et al., 2018). Our mixed-methods design facilitated a patient-centered approach to QPS development by involving people with UE amputations in multiple phases of data collection, review, and feedback, and prioritizing their perspectives over other stakeholders’ feedback. Further, our multidisciplinary team of study collaborators included UE VCA clinicians/surgeons, hand reconstructive surgeons, and occupational therapists who helped to ensure that the UE VCA-QPS was clinically relevant for the target population. Designing the UE VCA-QPS at a low reading grade level and use of the PEMAT will foster a greater comprehensibility (Shoemaker et al., 2013).
Our study has limitations. Some (19%) participants completed both the in-depth and semi-structured interviews, which may reduce the transferability of study results. Although individuals motivated by the prospect of pursuing UE VCA may have been more inclined to participate in interviews, suggesting a selection bias, study participants’ views ranged broadly in their level of interest in pursuing UE VCA. As our study sample included disproportionately fewer Hispanic or Latino individuals compared to the U.S. population of people with UE amputations (10% versus 15%), future research should examine UE VCA information needs among more ethnically diverse participants. We produced the UE VCA-QPS in English; future research should prepare the UE VCA-QPS in other languages.
People with UE amputations desired extensive information about UE VCA, primarily on risks, the rehabilitation process, and functional outcomes. To empower people with UE amputations and foster patient-provider communication about UE VCA, we developed a 35-item UE VCA-QPS. Use of the UE VCA-QPS is designed to address information needs, facilitate patient-centered care, and enhance informed decision making among people with UE amputations undergoing evaluation for UE VCA.
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Institutional Review Boards at: Northwestern University (STU00209718), Johns Hopkins University (00225728), and Walter Reed National Military Medical Center (WRNMMC-EDO-2020-0432). Northwestern University served as the Institutional Review Board of record for Walter Reed National Military Medical Center. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements. All participants provided verbal informed consent.
EJG conceived and designed the research study and participated in performing the research, analyzing and interpreting the data, and writing the manuscript. JG-S and BK participated in performing the research, analyzing and interpreting the data, and writing the manuscript. MD, KV, MN, and ML participated in data collection and analyzing and interpreting the data. TR, WA, and SF participated in data collection. All authors reviewed and approved the final manuscript.
This study was supported by award #W81XWH-19-2-0033/RT180041 from the Department of Defense to EJG, Initiating Principal Investigator (PI); #W81XWH-19-2-0034/RT180041P1 to ML, Partnering PI; #W81XWH-19-2-0035/RT180041P2 to GB, Partnering PI; and #W81XWH-19-2-0036/RT180041P3 to ST, Partnering PI.
We would like to thank all study participants, as well as Peter Walsh, Hannah Nemeth, and Whitney Langlee for providing assistance with study procedures. We also thank the Scientific Advisory Board members for their helpful insights: Ana Iltis, Edmund Howe, and James DuBois. This study used Research Electronic Data Capture (REDCap), a secure online data capture application supported at the Feinberg School of Medicine by the Northwestern University Clinical and Translational Science Institute. Research reported in this publication was institutionally administratively supported in part by the NIH’s National Center for Advancing Translational Sciences. This work was also institutionally administratively supported in part by the Northwestern Medicine Enterprise Data Warehouse.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The views expressed in this paper are those of the authors and do not necessarily reflect the official policy of the Department of Defense or the U.S. Government.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.960373/full#supplementary-material
Supplementary Figure 1 | Consort diagrams for in-depth interviews and semi-structured interviews.
JHU, Johns Hopkins University; NU, Northwestern University; QPS, question prompt sheet; UE, upper extremity; VCA, vascularized composite allotransplantation; WRNMMC, Walter Reed National Military Medical Center.
Ahmed, R., McCaffery, K. J., and Aslani, P. (2016). Development and validation of a question prompt list for parents of children with attention-deficit/hyperactivity disorder: A Delphi study. Health Expect. 19, 234–252. doi: 10.1111/hex.12341
American Society of Transplant Surgeons (2022). Vascularized composite allograft Cmte. Available online at: https://members.asts.org/committees/Public-Committee-Details/?CommitteeId=f2e958f4-5e99-42a1-bdbc-baa1f36c4267 (accessed May 18, 2022).
Arthur, J., Yennu, S., Zapata, K. P., Cantu, H., Wu, J., Liu, D., et al. (2017). Perception of helpfulness of a question prompt sheet among cancer patients attending outpatient palliative care. J. Pain Symptom Manag. 53, 124–130.e1. doi: 10.1016/j.jpainsymman.2016.08.017
Ayres, L., Kavanaugh, K., and Knafl, K. A. (2003). Within-case and across-case approaches to qualitative data analysis. Qual. Health Res. 13, 871–883. doi: 10.1177/1049732303013006008
Barnlund, D. (1970). “A transactional model of communication,” in Foundations of communication theory, eds K. Sereno and C. Mortensen (New York, NY: Harper & Row).
Barton, E., Moore, T. F., Hamel, L., Penner, L., Albrecht, T., and Eggly, S. (2020). The influence of a question prompt list on patient-oncologist information exchange in an African-American population. Patient Educ. Couns. 103, 505–513. doi: 10.1016/j.pec.2019.09.020
Belkora, J. K., Loth, M. K., Volz, S., and Rugo, H. S. (2009). Implementing decision and communication aids to facilitate patient-centered care in breast cancer: A case study. Patient Educ. Couns. 77, 360–368. doi: 10.1016/j.pec.2009.09.012
Bennett, J. (2016). Limb loss: The unspoken psychological aspect. J. Vasc. Nurs. 34, 128–130. doi: 10.1016/j.jvn.2016.06.001
Bernard, H., and Ryan, G. (1998). “Text analysis: Qualitative and quantitative methods,” in Handbook of methods in cultural anthropology, ed. H. Bernard (Walnut Creek, CA: Altamira Press), 595–646.
Bradley, E. H., Curry, L. A., and Devers, K. J. (2007). Qualitative data analysis for health services research: Developing taxonomy, themes, and theory. Health Serv. Res. 42, 1758–1772. doi: 10.1111/j.1475-6773.2006.00684.x
Brandes, K., Linn, A. J., Butow, P. N., and Weert, J. C. (2015). The characteristics and effectiveness of question prompt list interventions in oncology: A systematic review of the literature. Psychooncology. 24, 245–252. doi: 10.1002/pon.3637
Brega, A. G., Barnard, J., Mabachi, N. M., Weiss, B. D., DeWalt, D. A., Brach, C., et al. (2015). AHRQ health literacy universal precautions toolkit, 2nd Edn. Rockville, MD: Agency for Healthcare Research and Quality.
Brown, R., Shuk, E., Leighl, N., Butow, P., Ostroff, J., Edgerson, S., et al. (2011). Enhancing decision making about participation in cancer clinical trials: Development of a question prompt list. Support Care Cancer 19, 1227–1238. doi: 10.1007/s00520-010-0942-6
Brown, R. F., Butow, P. N., Dunn, S. M., and Tattersall, M. H. (2001). Promoting patient participation and shortening cancer consultations: A randomised trial. Br. J. Cancer. 85, 1273–1279. doi: 10.1054/bjoc.2001.2073
Centers for Medicare & Medicaid Services [CMS] (2010). Toolkit for making written material clear and effective, part 7. Available online at: https://www.cms.gov/Outreach-and-Education/Outreach/WrittenMaterialsToolkit/Downloads/ToolkitPart07.pdf (accessed May 17, 2022).
Creswell, J., and Plano Clark, V. L. (2007). Designing and conducting mixed methods research, 3rd Edn. Thousand Oaks, CA: Sage Publications.
Eggly, S., Tkatch, R., Penner, L. A., Mabunda, L., Hudson, J., Chapman, R., et al. (2013). Development of a question prompt list as a communication intervention to reduce racial disparities in cancer treatment. J. Cancer Educ. 28, 282–289. doi: 10.1007/s13187-013-0456-2
Epstein, R. M., and Street, R. L. (2011). The values and value of patient-centered care. Ann. Fam. Med. 9, 100–103. doi: 10.1370/afm.1239
Gaston, C., and Mitchell, G. (2005). Information giving and decision-making in patients with advanced cancer: A systematic review. Soc. Sci. Med. 61, 2252–2264. doi: 10.1016/j.socscimed.2005.04.015
Giacomini, M. K., and Cook, D. J. (2000). Users’ guides to the medical literature: XXIII. Qualitative research in health care. A. Are the results of the study valid? Evidence-Based Medicine Working Group. JAMA. 284, 357–362. doi: 10.1001/jama.284.3.357
Gordon, E. J., and Ison, M. G. (2014). Decision aids for organ transplant candidates. Liver Transpl. 20, 753–755. doi: 10.1002/lt.23908
Greene, J. C., Caracelli, V., and Graham, W. F. (1989). Toward a conceptual framework for mixed-method evaluation designs. Educ. Eval. Policy Anal. 11, 255–274. doi: 10.3102/01623737011003255
Guest, G., MacQueen, K. M., and Namey, E. E. (2011). Applied thematic analysis. Los Angeles, CA: Sage Publishers.
Houts, P., Doak, C., Doak, L., and Loscalzo, M. (2006). The role of pictures in improving health communication: A review of research on attention, comprehension, recall, and adherence. Patient Educ. Couns. 61, 173–190. doi: 10.1016/j.pec.2005.05.004
Inkellis, E., Low, E. E., Langhammer, C., and Morshed, S. (2018). Incidence and characterization of major upper-extremity amputations in the National Trauma Data Bank. JB JS Open Access. 3:e0038. doi: 10.2106/JBJS.OA.17.00038
Institute of Medicine, Committee on Quality of Health Care in America (2001). Crossing the quality chasm: new health system for the 21st century. Washington, DC: National Academies Press.
Jayasekera, J., Vadaparampil, S. T., Eggly, S., Street, R. L. Jr., Foster Moore, T., Isaacs, C., et al. (2020). Question prompt list to support patient-provider communication in the use of the 21-gene recurrence test: Feasibility, acceptability, and outcomes. JCO Oncol. Pract. 16, e1085–e1097. doi: 10.1200/JOP.19.00661
Keith, R. E., Crosson, J. C., O’Malley, A. S., Cromp, D., and Taylor, E. F. (2017). Using the Consolidated Framework for Implementation Research (CFIR) to produce actionable findings: A rapid-cycle evaluation approach to improving implementation. Implement Sci. 12:15. doi: 10.1186/s13012-017-0550-7
Kinnersley, P., Edwards, A. G. K., Hood, K., Cadbury, N., Ryan, R., Prout, H., et al. (2007). Interventions before consultations for helping patients address their information needs. Cochrane Database Syst. Rev. 3:CD004565. doi: 10.1002/14651858.CD004565.pub2
Lederer, S., Fischer, M. J., Gordon, H. S., Wadhwa, A., Popli, S., and Gordon, E. J. (2016). A question prompt sheet for adult patients with chronic kidney disease. BMC Nephrol. 17:155. doi: 10.1186/s12882-016-0362-z
Lopez-Vargas, P. A., Tong, A., Phoon, R. K., Chadban, S. J., Shen, Y., and Craig, J. C. (2014). Knowledge deficit of patients with stage 1-4 CKD: A focus group study. Nephrology 19, 234–243. doi: 10.1111/nep.12206
Miles, M., and Huberman, A. (1994). Qualitative data analysis: An expanded sourcebook, 2nd Edn. Thousand Oaks, CA: Sage Publications.
Miller, N., and Rogers, S. N. (2018). A review of question prompt lists used in the oncology setting with comparison to the patient concerns inventory. Eur. J. Cancer Care 27:e12489. doi: 10.1111/ecc/12489
Morris, N. S., MacLean, C. D., Chew, L. D., and Littenberg, B. (2006). The single item literacy screener: Evaluation of a brief instrument to identify limited reading ability. BMC Fam. Pract. 7:21. doi: 10.1186/1471-2296-7-21
Nielsen, C. C. (1991). A survey of amputees: Functional level and life satisfaction, information needs, and the Prosthetist’s role. J. Prosthet. Orthot. 3, 125–129.
OPTN (2022). U.S. Department of health and human services, organ procurement and transplantation network. Transplants by Donor Type. U.S. transplants performed: January 1, 1988 – June 30, 2022, for organ = Upper Limb: Unilateral, and organ = Upper Limb: Bilateral. Based on OPTN data as of July 25, 2022. Available online at: https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/# (accessed July 27, 2022).
Pasquina, C. P., Carvalho, A. J., and Sheehan, T. P. (2015). Ethics in rehabilitation: Access to prosthetics and quality care following amputation. AMA J. Ethics 17, 535–546. doi: 10.1001/journalofethics.2015.17.6.stas1-1506
Patton, M. (2015). Qualitative research & evaluation methods, 4th Edn. Los Angeles, CA: Sage Publications.
Pedlow, H., Cormier, A., Provost, M., Bailey, S., Balboul, G., Councill, A., et al. (2014). Patient perspectives on information needs for amputation secondary to vascular surgery: What, when, why, and how much? J. Vasc. Nurs. 32, 88–98. doi: 10.1016/j.jvn.2014.01.002
Rose, J., Cooney, C. M., Kaufman, C., Talbot, S. G., Caplan, A., Kahn, J., et al. (2019). Evolving ethics, policy and reimbursement issues of vascularized composite allotransplantation: Symposium summary. SAGE Open Med. 7:2050312119866944. doi: 10.1177/2050312119866944
Sansoni, J. E., Grootemaat, P., and Duncan, C. (2015). Question prompt lists in health consultations: A review. Patient Educ. Couns. 98, 1454–1464. doi: 10.1016/j.pec.2015.05.015
Satteson, E. S., Roe, A. K., Eppler, S. L., Yao, J., Shapiro, L. M., and Kamal, R. N. (2020). Development and testing of a question prompt list for common hand conditions: An exploratory sequential mixed-methods study. J. Hand Surg. Am. 45, 1087. doi: 10.1016/j.jhsa.2020.05.015
Schwarze, M. L., Buffington, A., Tucholka, J. L., Hanlon, B., Rathouz, P. J., Marka, N., et al. (2020). Effectiveness of a question prompt list intervention for older patients considering major surgery: A multisite randomized clinical trial. JAMA Surg. 155, 6–13. doi: 10.1001/jamasurg.2019.3778
Shepherd, H. L., Barratt, A., Trevena, L. J., McGeechan, K., Carey, K., Epstein, R. M., et al. (2011). Three questions that patients can ask to improve the quality of information physicians give about treatment options: A cross-over trial. Patient Educ. 84, 379–385. doi: 10.1016/j.pec.2011.07.022
Shoemaker, S. J., Wolf, M. S., and Brach, C. (2013). The Patient Education Materials Assessment Tool (PEMAT) and user’s guide. Rockville, MD: Agency for Healthcare Research and Quality.
Shores, J. T., Malek, V., Lee, W. P. A., and Brandacher, G. (2017). Outcomes after hand and upper extremity transplantation. J. Mater. Sci. Mater. Med. 28, 1–8. doi: 10.1007/s10856-017-5880-0
Singleton, R. A., and Straits, B. C. (2017). Approaches to social research, 6th Edn. New York, NY: Oxford University Press.
Stossel, L. M., Segar, N., Gliatto, P., Fallar, R., and Karani, R. (2012). Readability of patient education materials available at the point of care. J. Gen. Intern. Med. 27, 1165–1170. doi: 10.1007/s11606-012-2046-0
Keywords: informed consent, patient–clinician communication, ethics, treatment decision making, patient-centered care, upper limb amputation, VCA
Citation: Gacki-Smith J, Kuramitsu BR, Downey M, Vanterpool KB, Nordstrom MJ, Luken M, Riggleman T, Altema W, Fichter S, Cooney CM, Dumanian GA, Jensen SE, Brandacher G, Tintle S, Levan M and Gordon EJ (2022) Information needs and development of a question prompt sheet for upper extremity vascularized composite allotransplantation: A mixed methods study. Front. Psychol. 13:960373. doi: 10.3389/fpsyg.2022.960373
Received: 02 June 2022; Accepted: 20 July 2022;
Published: 05 September 2022.
Edited by:
Martin Kumnig, Medical University of Innsbruck, AustriaReviewed by:
Fatih Zor, Wake Forest University School of Medicine, United StatesCopyright © 2022 Gacki-Smith, Kuramitsu, Downey, Vanterpool, Nordstrom, Luken, Riggleman, Altema, Fichter, Cooney, Dumanian, Jensen, Brandacher, Tintle, Levan and Gordon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elisa J. Gordon, ZS1nb3Jkb25Abm9ydGh3ZXN0ZXJuLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.