- Institute of Medical Sociology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
Background: Health anxiety exists on a continuum ranging from the absence of health awareness to the obsessive fear of having a serious illness despite reassurance. Its pathological manifestation can be diagnosed as hypochondriacal or illness anxiety or somatic symptom disorder. Health anxiety is associated with psychological distress and adverse life events, among others, and leads to considerable economic burden. Compared to the majority population, migrants, and ethnic minorities often face major health inequalities. Several mental illnesses and psychosomatic complaints are more common among these groups. To date, potential ethnic and migration-related inequalities in health anxiety have not been clearly described. However, they are of high relevance for the provision of adequate health care of this diverse and potentially vulnerable group. Thus, we conducted a systematic review and meta-analysis of health anxiety in migrants and ethnic minorities.
Methods: A systematic literature search of PubMED, Web of Science, PsycINFO, and PSYNDEX was conducted, covering all studies published until 1st of December 2021. Studies were selected if they employed validated measurement tools of health anxiety and examined migrants and/or ethnic minorities in comparison with the majority population. Meta-analytic methods were applied by using a random-effect model. The study quality was assessed with the Effective Public Health Practice Project Quality Assessment Tool (EPHPP).
Results: We identified 18 studies from 445 studies initially screened. Of these, 14 studies conducted in North America with a total number of 5,082 study participants were included in the meta-analysis. The pooled effect size indicated a higher risk of health anxiety in migrants and ethnic minorities compared to the majority population (OR 1.39, 95%-CI 1.01–1.92). The results proved not to be robust according to publication bias (adjusted OR 1.18, 95%-CI 0.83–1.69) and fail-safe N (2/3 < benchmark N = 75) and are limited due to heterogeneity (I2 = 57%), small sample sizes and an overall low quality of included studies.
Conclusion: To address the diversity of migrants and ethnic minorities, inter-sectional approaches across different countries are needed in research to shed further light on social inequalities in health anxiety linked to migration.
Systematic review registration: PROSPERO, registration number CRD42022298458.
Introduction
In 2020, 281 million people or 3.6% of the world population were classified as migrants (McAuliffe and Triandafyllidou, 2021). Compared to 2.3% in 1970, there is a clear upward trend which also contributes to the diversity within countries. Globally, the United States are the number one destination for migrants, whereas India and Mexico are the number one countries to be left (McAuliffe and Triandafyllidou, 2021). Migration is understood as the temporary movement from the country of birth to the country of residence and immigration refers to a permanent movement. Reasons for migration are mostly due to work, family, or study. Refugees, however, are forced to leave their country due to e.g., political conflicts or disasters and are highly vulnerable. The term ethnicity (former race) ascribes people to a certain group by characteristics like origin, religion, or language (World Health Organization, 2010b; Bhopal, 2014). While the concepts of ethnicity and race are widely used in North America, migration background is frequently used in Europe. Since migration and ethnicity are related social constructs and often overlap, the World Health Organization calls for a joint consideration of both in research (World Health Organization, 2010b). Nevertheless, people with a migration background are a heterogeneous group regarding e.g., socio-demographic aspects, the immigrant generation or the length of stay (Rommel et al., 2015).
According to the concept of social determinants of health (Marmot and Wilkinson, 2011; World Health Organization, 2022b), experiences during migration process as well as discrimination are important for health and wellbeing. Hence, a major topic in public health research is the question to what extent health inequalities exist between migrants or ethnic minorities and the majority population (Davies et al., 2006; Chung and Griffiths, 2018). Since migrants are often not adequately represented in data on population health, and some groups are still not represented at all (World Health Organization, 2010b), research is limited. Until now, the findings tend to be quite heterogeneous. For example, migration is associated with higher rates of diabetes, specific infectious diseases, and post-traumatic stress disorder, the latter two especially occurring in refugees (Hunter and Schmidt, 2010; World Health Organization, 2010b). Whereas, e.g., allergies or alcohol misuse are less often detected in migrants (Rommel et al., 2015; World Health Organization, 2021). Migrants even tend to be among the healthiest in their home country, which is described as the healthy migrant effect (World Health Organization, 2010a; Bhopal, 2014). However, in the country of residence, refugees, migrants and several ethnic minority groups often face psychosocial, behavioral and material deprivation, like discrimination, poor living and working conditions, and inadequate access to health care services (World Health Organization, 2022a). Further, there is evidence that health services are used less in these groups (World Health Organization, 2010b; Klein and von dem Knesebeck, 2018). This might explain a frequently higher vulnerability of these groups regarding certain somatic or mental illnesses, e.g., stress-related and somatoform disorders which also includes (pathological) health anxiety.
Health anxiety is defined as the “preoccupation with the fear of having a serious disease, which persists in spite of appropriate medical reassurance” (Muse et al., 2010). Health anxiety exists on a continuum ranging from the absence of health awareness to excessive concerns about one's own health status (Ferguson, 2009; Bailer et al., 2016). Severe health anxiety in a pathological manner can be diagnosed as hypochondriacal disorder or hypochondriasis, illness anxiety disorder (IAD) or somatic symptom disorder (SSD) (Muse et al., 2010; American Psychiatric Association, 2013; World Health Organization, 2019). It is assessed either with diagnostic instruments or diagnostic interviews (Tyrer, 2018). However, appropriate cut-off scores to identify individuals with severe health anxiety are still under discussion (Creed and Barsky, 2004; Weck et al., 2014; Hedman et al., 2015). Health anxiety as a broader concept is present in about 10% of the general population and over 30% in mental health care settings (Weck et al., 2014). The prevalence for pathological health anxiety, primarily hypochondriasis, is <1% (Weck et al., 2014). To date, only few studies examine the newly defined diagnoses of IAD and SSD with prevalence rates of 7% for IAD in an Indian medical sample (Pandey et al., 2017) and almost 34% in case of SSD in Chinese patients (Cao et al., 2020). Health anxiety is associated with increased psychosomatic complaints and mental comorbidities, such as depression or anxiety disorders, (Newby et al., 2017) and leads to a reduction in health-related quality of life (Bleichhardt and Hiller, 2007). The economic burden of health anxiety is considerable, as it is associated with an increase in health care use (Barsky et al., 2001; Newby et al., 2017; Norbye et al., 2022), extended sick-leave (Eilenberg et al., 2015), and disability (Mykletun et al., 2009).
The etiology of health anxiety is explained in the cognitive-behavioral model of Barsky and Wyshak (1990) and the model of somatosensory amplification of Warwick and Salkovskis (1990). According to these models, negative and traumatic life events during childhood (e.g., a serious illness or abuse) can lead to dysfunctional illness responses and catastrophizing. Acute stressors which are often faced by refugees and certain migrant groups pre, during, and post migration process (e.g., the death of a relative, discrimination, or material deprivation) can activate these catastrophizing tendencies and lead to negative assumptions of the body (Hunter and Schmidt, 2010; World Health Organization, 2010a; Mölsä et al., 2014). Even slight symptoms or bodily sensations are then misinterpreted as a threatening illness (Sauer and Witthöft, 2020). Furthermore, negative treatment experiences like language barriers or cultural differences in illness perceptions can maintain or worsen the misinterpretation. As a result, (pathological) health anxiety can occur (Haasen, 2000; Arbisi et al., 2002; Ekblad, 2020), increasing inequalities in the particular vulnerable groups of migrants and ethnic minorities (World Health Organization, 2010b).
A meta-analysis by Barbek et al. (2021) found a higher risk of health anxiety in low socio-economic individuals, indicating social inequalities in health anxiety on a vertical level. Still, social inequalities in health anxiety according to migration background are not well studied and remain inconclusive (Mölsä et al., 2014; Weck et al., 2014; Akariya et al., 2021). Therefore, we examine differences in health anxiety between migrants and ethnic minorities compared to the majority population in the respective countries in a systematic review and meta-analysis. These findings may help to understand the specific needs and improve the health care of particular vulnerable groups of migrants and ethnic minorities.
Methods
Search strategy
According to the population, exposure and outcome criteria (PEO) (Pollock and Berge, 2018), the search strategy consisted of the following terms with closely related words: health anxiety, health worries, hypochondriasis, illness anxiety (disorder), somatic symptom disorder (as outcome) in combination with migration, immigrant, ethnicity, race, refugee, minority (as exposure in any adult population; for the full search strategy see Supplementary data 1). The following four databases were searched for relevant studies: PubMED, Web of Science, PsycINFO, and PSYNDEX. Additionally, the reference lists of included studies were screened.
Study selection
Review team consisted of three reviewers (RB; SH; JL). The results were processed in the Citavi reference management system. After removing duplicates, RB and JL independently screened all titles and abstracts and RB and SH independently reviewed all potential full-texts in concordance with pre-defined inclusion and exclusion criteria. Disagreement was solved via discussion in the review team. Inclusion criteria consisted of the following: (a) empirical studies published until 1st of December 2021; (b) full text in English or German; (c) adult population; (d) health anxiety assessed with a validated self-rating scale or diagnostic interview (criteria for validation were either the psychometric analysis of the assessment tool or a cross-reference to a validation study); (e) comparing a population of migrants, immigrants, refugees, or ethnic minority with the majority population in one country. The following exclusion criteria were defined: (a) qualitative studies, reviews or meta-analyses, and methodical studies on measurement invariance; (b) specific forms of health anxiety (e.g., fear of progression, modern health worries, COVID-related anxiety).
Extraction of study data and meta-analytical procedure
Two reviewers (RB; SH) independently extracted the following study characteristics: study design, country, setting/population, sample size, assessment of health anxiety, comparators, quality assessment, and summarized results. For the latter, univariate or adjusted results, if reported, were categorized as follows: significant or non-significant differences in health anxiety between migration or ethnic minority population and majority population. Since the majority of included studies were conducted in North America (USA and Canada), only these studies were pooled for the meta-analysis to reduce heterogeneity. To calculate the pooled effect size, prevalence rates were converted into log odds ratios (OR) with standard error (SE). In case of mean values, these were first transformed into standardized mean differences and second into log OR with SE (Lenhard and Lenhard, 2016; Borenstein et al., 2021). Since none of the studies reported adjusted models suitable for meta-analytical calculation, the meta-analysis includes only univariate results. Although study authors were contacted in case of missing data, none was able to provide the requested information. Hence, missing data was imputed by calculating the mean of the effect estimate and/or SE of the remaining studies. Due to great variety in observational study designs, the random effect model was chosen for meta-analysis (Hedges and Vevea, 1998). The standardized effect measures were weighted according to their SE. To assess the extent of heterogeneity, Cochran's Q and Higgins I2 were calculated (Higgins and Thompson, 2002; Harrer et al., 2021). Furthermore, a sensitivity analysis was conducted to examine pre-defined moderators of the pooled effect size (Aromataris and Munn, 2020). Stratified meta-analyses were conducted for each of the following moderators: assessment of health anxiety, comparators, study population, and study quality. To determine the risk of publication bias, Egger's regression test (no risk if p > 0.05) and the trim-and-fill method were applied (Egger et al., 1997; Duval and Tweedie, 2000). Further methods included the fail-safe N to test the stability of our meta-analysis. Therefore, fail-safe Ns with different preconditions were assumed (insignificant α 0.05 and 0.1; irrelevant OR 0.95; stable results if fail-safe N>5n+10) (Rosenthal, 1979; Orwin, 1983; Viechtbauer, 2021). The meta-analysis was calculated and visualized with the R packages “esc”, “meta”, “metafor", and “tidyverse”. Effect sizes were pre-calculated with the internet-based calculation tool Psychometrica (Lenhard and Lenhard, 2016; Harrer et al., 2021). For the R syntax see Supplementary data 2.
Quality assessment with the EPHPP
To determine the study quality, two reviewers (RB; SH) independently applied the Effective Public Health Practice Project Quality Assessment Tool (EPHPP) (Thomas et al., 2004). The EPHPP is a compact and validated tool suitable for interventional and observational studies. It consists of six categories: selection bias, study design, confounders, blinding, data collection method, and withdrawals/dropouts. Each category is rated as strong, moderate, or weak. The total score is calculated based on the number of weak categories (strong = 0 weak categories; moderate = 1 weak category; weak = more than 1 weak category) (Thomas et al., 2004). Since our systematic review consisted of observational studies only, the EPHPP was slightly adapted to the quality rating standards for observational studies as stated by the Cochrane Collaboration (Armijo-Olivo et al., 2012; Higgins et al., 2022). First, the category blinding was dropped because it refers to interventional studies only. Instead, the category statistical analysis was included. Second, cross-sectional studies were rated as moderate, as they are suitable for answering associative questions; cohort and case-control studies were rated as strong. Third, the focus of confounders was widened instead of rating pre-interventional group differences only. Fourth, withdrawals and dropouts were completed by loss to follow-up regarding cohort studies. The adapted tool has already proven its usefulness in a previous review of the research group (Barbek et al., 2021).
We conducted our systematic review and meta-analysis in concordance with the PRISMA standards (Moher et al., 2009) and MOOSE statement (Stroup et al., 2000) (see Supplementary Table 1). The review protocol was registered at PROSPERO under the number CRD42022298458.
Results
Screening and inclusion of studies
We identified 400 records through database screening and additional 45 records from citation searching, resulting in a total number of 445 records. After removing duplicates, we screened 316 titles and abstracts. From the remaining 70 full texts, we excluded 52 records due to our pre-defined inclusion and exclusion criteria. Main reasons for exclusion were: lack of the association of interest, outcome or exposure not like defined, wrong publication or study type, not written in English or German. Finally, we included 18 studies in our systematic review. Of these, we compiled a subsample of 14 studies from North America for our meta-analysis (see Figure 1). During the screening process, our inter-rater reliability reached 90%. For the remaining 10% of studies, we discussed their suitability until agreement. The details of excluded studies and the reason for exclusion can be found in the Supplementary Table 2.

Figure 1. PRISMA 2020 flow diagram. From: Page et al. (2021).
Table 1 presents the main study characteristics and summarized results of the 18 included studies with a total number of 5,914 study participants in our systematic review. The majority was of cross sectional design (n = 13), whereas case-control studies (n = 3) and cohort studies (n = 2) were less represented. More than three-quarters of studies were conducted in North America (n = 14), three studies in Europe and one study in Asia. In terms of the study population/setting, half of the studies investigated the general (or a specific) population (n = 9) and patients (either general or mental health care setting) (n = 9), respectively. Regarding the assessment of health anxiety, two-thirds of studies employed validated self-rating scales (n = 12), the remaining one-third used standardized diagnostic interviews (n = 6). Furthermore, the majority of included studies compared ethnic minority groups with the majority population (n = 14). Ethnic minorities were mainly of Black, Hispanic, or Asian background (according to race, ethnicity, or nationality as stated in the included studies). Only four studies explicitly investigated a population of immigrants (all of Hispanic or Asian background) or refugees (Somalis), who all had own migration experiences. Notably, at least one-quarter was of moderate study quality (n = 5) but three-quarters of weak quality (n = 13). Detailed results of the quality assessment can be found in Supplementary Table 3. The inter-rater reliability of the quality assessment reached 85%. The remaining 15% of disagreement were solved via discussion.
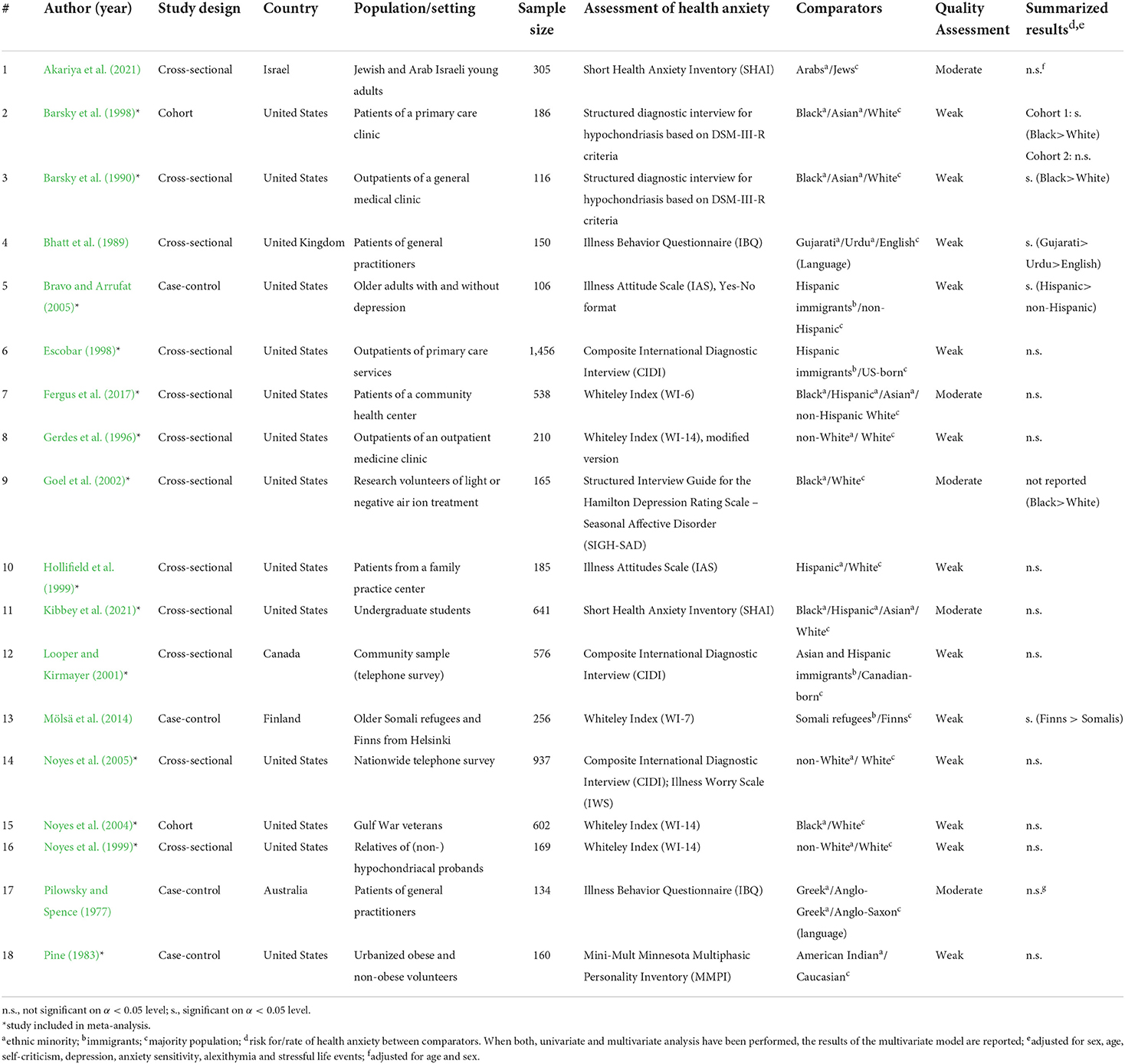
Table 1. Study characteristics and summarized results of included studies (n = 18 studies, with n = 5,914 study participants).
For a first overview, we summarized the data as reported in the included studies (Table 1). Four of the included studies reported a significantly higher risk or rate of health anxiety in migrants or ethnic minorities compared to the majority population. Another study also reported this difference, but the information on the level of significance was missing. Only one study stated a significant inverse association, whereas two-thirds of studies found no significant association (n = 12). Two studies presented results of multivariate models adjusted for age and gender, in one case, analyses additionally controlled for several psycho-social variables. The remaining 16 studies published only non-adjusted results.
Meta-analytical results
In our meta-analysis, we analyzed all 14 studies conducted in North America (USA n = 13; Canada n = 1) with a total number of 5,082 study participants. We calculated log ORs based on prevalence rates for nine studies and for four studies based on standardized mean differences. For the remaining study, we imputed values due to missing data. Since the standardized effect measure of one study proved oneself as an outlier, we only report the results of the remaining 13 studies. According to our model, migrants and ethnic minorities had a significant, almost 40% higher risk of health anxiety compared to the majority population (OR 1.39, 95%-CI 1.01–1.92; see Figure 2). However, results were significant in only three of the 13 studies. In seven studies, the risk was higher but insignificant and the remaining three studies found an insignificant inverse risk.
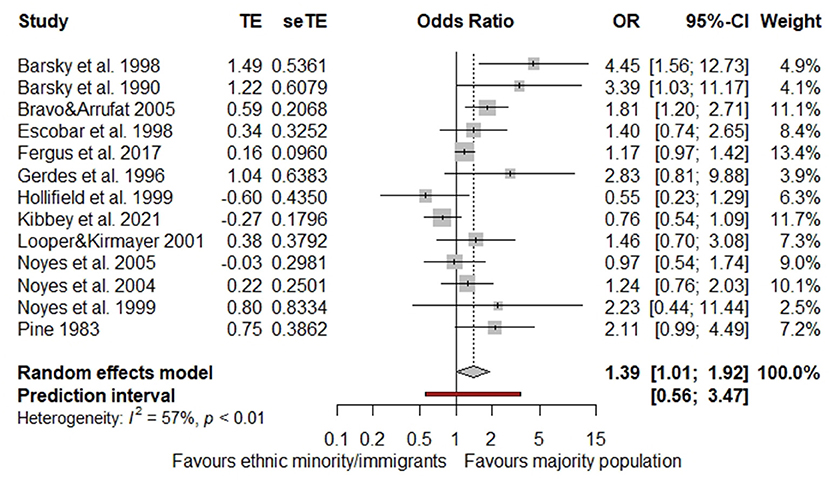
Figure 2. Pooled effect size of studies from North America (n = 13 studies, with n = 4,926 study participants, outlier-adjusted).
Sensitivity analysis
In the stratified analyses, we found no significant differences between the subgroups (Table 2; p of all subgroups > 0.05). This indicates that none of the pre-defined criteria are relevant moderators. Nonetheless, some indications can be drawn from our results. The risk of health anxiety in migrants and ethnic minorities was higher when assessed in patients (either general or mental health care setting) compared to population-based studies (OR 1.59, 95%-CI 0.89–2.84). Also, the risk of health anxiety in migrants and ethnic minorities was higher when assessed with a validated diagnostic interview compared to self-rating scales (OR 1.69, 95%-CI 0.80–3.59). Furthermore, immigrants formed a homogenous subsample with a slightly higher risk of health anxiety compared to the overall effect size (OR 1.57, 95%-CI 1.10–2.24).
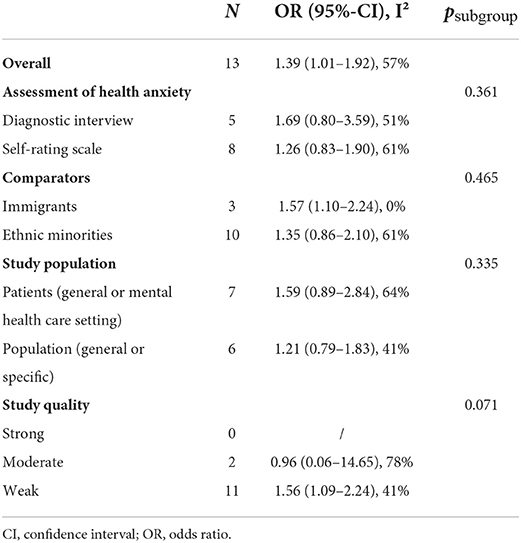
Table 2. Sensitivity analysis of studies from North America (n = 13 studies, with n = 4,926 study participants, outlier-adjusted).
Publication bias and stability of meta-analysis
The heterogeneity between studies was moderate, with Higgins I2 = 57%. Although stratification reduced heterogeneity in some cases, no clear trend emerged (Table 2). Only the subsample of immigrants was homogenous (I2 = 0%). Second, we evaluated potential publication bias. Egger's regression test gave no indication for biased results (intercept −0.03, t = 1.64, p = 0.130). Otherwise, after imputing studies to adjust for potential publication bias, the pooled OR decreased and became insignificant (studies trimmed n = 4, adjusted OR 1.18, 95%-CI 0.83–1.69). For visualization, the adjusted funnel plot is presented in the Supplementary Figure 1. Third, we calculated different fail-safe Ns to examine the effect of insignificant unpublished data on our meta-analysis. Two out of three fail-safe Ns did not reach the benchmark (α 0.05 fail-safe N = 57; α 0.1 fail-safe N = 103; OR 0.95 fail-safe N = 38; with benchmark 5x13+10 = 75). Taken together, results for publication bias and stability of our meta-analysis are inconclusive, questioning the robustness of the meta-analytical results.
Discussion
Summary and interpretation in context of literature
To the best of our knowledge, we conducted the first systematic review investigating ethnic and migration-related differences in health anxiety. Since migration and ethnic minority groups overlap, especially in the USA, we studied these groups together, as suggested (Haasen, 2000; World Health Organization, 2010b). To reduce heterogeneity, we included only the 14 studies conducted in North America with more than 5,000 individuals in our meta-analysis. The overall pooled effect size indicated a higher risk of health anxiety in migrants and ethnic minorities. However, summarizing Egger's regression test, the trim-and-fill method, and the fail-safe N, results on the robustness of our meta-analysis were inconclusive. Reason might be the small number and sample sizes of included studies. In our sensitivity analysis, none of the pre-defined moderators, namely assessment of health anxiety, comparators, study population, and study quality, revealed a significant influence on the association under study. Regarding the heterogeneity, only the three studies analyzing immigrants (all of Hispanic or Asian background) formed a homogeneous subgroup with a slightly increased risk of health anxiety. Overall, test for publication bias and sensitivity analysis revealed inconsistent results. Accordingly, further research is needed to shed light on migration-related differences in health anxiety with a focus on the diversity of the groups of migrants, refugees, and ethnic minorities.
Ethnic and migration-related inequalities in health anxiety can be explained following the concept of social determinants of health (Marmot and Wilkinson, 2011; World Health Organization, 2022b). According to this concept, migrants often face negative and traumatic life events pre, during and post-migration, acute psychosocial stressors, behavioral and material deprivation as well as negative treatment experience in the health care setting. Since the etiology of health anxiety, especially in its pathological extent, is strongly related to negative life events and acute stressors (Barsky and Wyshak, 1990), the possible onset or maintenance of health anxiety in some minority populations can be assumed. However, since our meta-analytical results were inconclusive and several included studies found no ethnic or migration-related disparities in health anxiety, further investigation is needed. Like stated e.g., by Kibbey et al. (2021), especially the high heterogeneity of people with migration background or of different ethnicities might not have been adequately represented in the included studies. This is in line with our sensitivity analysis, indicating a higher risk of health anxiety in the homogeneous group of Hispanic or Asian immigrants residing in the United States but not for the heterogeneous group of ethnic minorities including e.g., Black, Asian, Hispanic, Indian Americans, and other unspecified non-White residents in the United States and Canada. Accordingly, a generalization for all groups of migrants or ethnic minorities is not possible. To what extent health anxiety is present e.g., in Turkish migrants living in Germany, is still unknown. Hence, further research is needed which explicitly examines health anxiety in different migration populations and settings accounting for the heterogeneity of migration and ethnic minority populations as well as the contextual factors in the different countries of residence. Thereby, inter-sectional approaches and multivariate models can shed light on the potential interaction of different socio-demographic variables in the context of health anxiety (Crenshaw, 1989; Kibbey et al., 2021). Additionally, research is needed to shed light on the discrepancy of the generally lower health care utilization among migrants and the higher health care utilization in people with health anxiety. Overall, it remains an open question whether ethnic and migration-related inequalities in health anxiety exist in a systematic and consistent manner.
Limitations
The following methodological aspects should be considered when interpreting our results. First, our analyses are limited due to the small number of studies identified through the systematic literature search. This reflects the need for further research in the under-represented area of inequalities in mental health among migrants and minority groups. The small sample size also affects the sensitivity analysis, since subgroups should include n > 5 studies for reliable results (Borenstein et al., 2021). Accordingly, the results can only give indications which need further confirmation. Additionally, the small sample sizes of the respective study populations can be seen as one reason why the majority of included studies did not find significant ethnic or migration-related differences in health anxiety contrary to the overall effect size of our meta-analysis. Second, the overall low quality of the included studies limits our results. The studies were limited to answer our research question mainly due to the cross-sectional design and a lack of multivariate analysis. Future research in this field should provide adjusted models to increase the quality and reliability of results. Third, heterogeneity of included studies limits our findings which has several reasons: The included studies assessed migration and ethnic minority status with a variety of variables like migration/immigration, refugee status, ethnicity/race, nationality, or language. Based on this data, we were not able to satisfactorily differentiate between people with and without own migration experiences. Future research should collect both, migration background and ethnicity to reflect the high diversity of these groups. Together with a great variety of assessment tools for health anxiety, the included studies were even more heterogeneous. The heterogeneity also remained in the sensitivity analysis. Accordingly, other moderators besides the ones we assumed based on theoretical considerations could be of relevance to further modify the potential association between migration and health anxiety. Fourth, the inclusion of studies only written in English or German might have led to selection bias. However, we rated this risk as low, since most of the studies identified were conducted in English-speaking countries, mostly North America. The large number of studies conducted in North America might be explained by the fact that Mexico–United States is the number one country-to-country corridor worldwide (McAuliffe and Triandafyllidou, 2021). However, our results are not generalizable to other countries or cultures, since the situation of migrants, refugees and ethnic minorities is highly contextual (e.g., depending on the health care system, legal rights, or the integrational approaches made in the country of residence). Accordingly, further research in different countries with diverse cultural approaches is needed.
Conclusion
Research on mental health in migrant and ethnic minority populations is lacking, limited to certain countries and hence not generalizable. This is also the case for health anxiety, since our systematic review and meta-analysis found few suitable studies with high heterogeneity revealing no consistent ethnic and migration-related inequalities in health anxiety so far. However, clear insights are essential to adequately respond to the needs of these diverse groups. Since migration experiences are often related to high psychological stressors and behavioral as well as material deprivation, migrants and other minority groups might be particularly vulnerable to several mental illnesses, including (pathological) health anxiety. Health anxiety needs to be recognized early and appropriately treated in health care to reduce individual and economic burdens. Intersectional approaches and multivariate analysis can help to gain a deeper understanding of the associations between health anxiety, (psychological) distress, and all kinds of discrimination or deprivation due to migration, ethnicity and other social determinants like gender, age and socio-economic status. Additionally, since our sensitivity analysis indicated only specific immigrants as a homogeneous subgroup, future attempts should consider the heterogeneousness of migration and ethnic minority populations as well as the contextual factors in the country of residence (e.g., the health care system or legal aspects) to obtain reliable results.
Data availability statement
The datasets/overview of studies used and analyzed during the current study are available from the corresponding author on reasonable request.
Author contributions
RB developed the research question, performed the screening, quality assessment, analysis and interpretation of data, and was a major contributor in writing the manuscript. SH performed the screening, quality assessment, and analysis of data and was a contributor in writing the manuscript. JL performed the screening and was a contributor in writing the manuscript. OK developed the research question and was a contributor in writing the manuscript. All authors read and approved the final manuscript.
Funding
The analyses are part of the project Social Inequalities in Aggravating Factors of Somatic Symptom Persistence which is part of the Research Unit 5211 (RU 5211) Persistent SOMAtic Symptoms ACROSS Diseases: From Risk Factors to Modification (SOMACROSS), funded by the German Research Foundation (Deutsche Forschungsgemeinschaft, DFG, project number 445297796, speaker: Professor Bernd Löwe, MD); see also https://gepris.dfg.de/gepris/projekt/445297796.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.960256/full#supplementary-material
References
Akariya, O., Anholt, G. E., and Shahar, G. (2021). Is self-criticism uniquely associated with health anxiety among Jewish and Arab Israeli young adults? Int. J. Cogn. Ther. 15, 81–93. doi: 10.1007/s41811-021-00121-x
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th Edn. Arlington: American Psychiatric Publishing. doi: 10.1176/appi.books.9780890425596
Arbisi, P. A., Ben-Porath, Y. S., and McNulty, J. (2002). A comparison of MMPI-2 validity in African American and Caucasian psychiatric inpatients. Psychol. Assess. 14, 3–15. doi: 10.1037/1040-3590.14.1.3
Armijo-Olivo, S., Stiles, C. R., Hagen, N. A., Biondo, P. D., and Cummings, G. G. (2012). Assessment of study quality for systematic reviews: a comparison of the Cochrane collaboration risk of bias tool and the effective public health practice project quality assessment tool: methodological research. J. Eval. Clin. Pract. 18, 12–18. doi: 10.1111/j.1365-2753.2010.01516.x
Aromataris, E., and Munn, Z. (2020). JBI Manual for Evidence Synthesis. Available online at: https://synthesismanual.jbi.global/ (accessed February 22, 2022). doi: 10.46658/JBIMES-20-01
Bailer, J., Kerstner, T., Witthöft, M., Diener, C., Mier, D., and Rist, F. (2016). Health anxiety and hypochondriasis in the light of DSM-5. Anxiety Stress Coping 29, 219–239. doi: 10.1080/10615806.2015.1036243
Barbek, R., Makowski, A. C., and von dem Knesebeck, O. (2021). Social inequalities in health anxiety: a systematic review and meta-analysis. J. Psychosom. Res. 153:110706. doi: 10.1016/j.jpsychores.2021.110706
Barsky, A. J., Ettner, S. L., Horsky, J., and Bates, D. W. (2001). Resource utilization of patients with hypochondriacal health anxiety and somatization. Med. Care 39, 705–715. doi: 10.1097/00005650-200107000-00007
Barsky, A. J., Fama, J. M., Bailey, E. D., and Ahern, D. K. (1998). A prospective 4- to 5-year study of DSM-III-R hypochondriasis. Arch. Gen. Psychiatry 55, 737–744. doi: 10.1001/archpsyc.55.8.737
Barsky, A. J., and Wyshak, G. (1990). Hypochondriasis and somatosensory amplification. Br. J. Psychiatry 157, 404–409. doi: 10.1192/bjp.157.3.404
Barsky, A. J., Wyshak, G., Klerman, G. L., and Latham, K. S. (1990). The prevalence of hypochondriasis in medical outpatients. Soc. Psychiatry Psychiatr. Epidemiol. 25, 89–94. doi: 10.1007/BF00794988
Bhatt, A., Tomenson, B., and Benjamin, S. (1989). Transcultural patterns of somatization in primary care: a preliminary report. J. Psychosom. Res. 33, 671–680. doi: 10.1016/0022-3999(89)90082-2
Bhopal, R. S. (2014). Migration, Ethnicity, Race, and Health in Multicultural Societies. Oxford: Oxford University Press. doi: 10.1093/med/9780199667864.001.0001
Bleichhardt, G., and Hiller, W. (2007). Hypochondriasis and health anxiety in the German population. Br. J. Health Psychol. 12, 511–523. doi: 10.1348/135910706X146034
Borenstein, M., Hedges, L. V., Higgins, J. P. T., and Rothstein, H. R. (2021). Introduction to Meta-analysis. Chichester: Wiley. doi: 10.1002/9781119558378
Bravo, I. M., and Arrufat, O. (2005). The illness attitude scales: adaptation and translation into Spanish for use with older adults. J. Appl. Gerontol. 24, 355–371. doi: 10.1177/0733464805278133
Cao, J., Wei, J., Fritzsche, K., Toussaint, A. C., Li, T., Jiang, Y., et al. (2020). Prevalence of DSM-5 somatic symptom disorder in Chinese outpatients from general hospital care. Gen. Hosp. Psychiatry 62, 63–71. doi: 10.1016/j.genhosppsych.2019.11.010
Chung, R. Y., and Griffiths, S. M. (2018). Migration and health in the world: a global public health perspective. Public Health 158, 64–65. doi: 10.1016/j.puhe.2018.04.005
Creed, F., and Barsky, A. (2004). A systematic review of the epidemiology of somatisation disorder and hypochondriasis. J. Psychosom. Res. 56, 391–408. doi: 10.1016/S0022-3999(03)00622-6
Crenshaw, K. (1989). Demarginalizing the Intersection of Race and Sex: A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory and Antiracist Politics. University of Chicago Legal Forum, Chicago, IL, United States. p. 139–167.
Davies, A., Basten, A., and Frattini, C. (2006). Migration: A Social Determinant of the Health of Migrants. International Organization for Migration.
Duval, S., and Tweedie, R. (2000). Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56, 455–463. doi: 10.1111/j.0006-341X.2000.00455.x
Egger, M., Davey Smith, G., Schneider, M., and Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634. doi: 10.1136/bmj.315.7109.629
Eilenberg, T., Frostholm, L., Schroder, A., Jensen, J. S., and Fink, P. (2015). Long-term consequences of severe health anxiety on sick leave in treated and untreated patients: analysis alongside a randomised controlled trial. J. Anxiety Disord. 32, 95–102. doi: 10.1016/j.janxdis.2015.04.001
Ekblad, S. (2020). To increase mental health literacy and human rights among new-coming, low-educated mothers with experience of war: a culturally, tailor-made group health promotion intervention with participatory methodology addressing indirectly the children. Front Psychiatry 11:611. doi: 10.3389/fpsyt.2020.00611
Escobar, J. (1998). DSM-IV hypochondriasis in primary care. Gen. Hosp. Psychiatry. 20, 155–159. doi: 10.1016/s0163-8343(98)00018-8
Fergus, T. A., Griggs, J. O., Cunningham, S. C., and Kelley, L. P. (2017). Health anxiety and medical utilization: the moderating effect of age among patients in primary care. J. Anxiety Disord. 51, 79–85. doi: 10.1016/j.janxdis.2017.06.002
Ferguson, E. (2009). A taxometric analysis of health anxiety. Psychol. Med. 39, 277–285. doi: 10.1017/S0033291708003322
Gerdes, T. T., Noyes, R., Kathol, R. G., Phillips, B. M., Fisher, M. M., Morcuende, M. A., et al. (1996). Physician recognition of hypochondriacal patients. Gen. Hosp. Psychiatry 18, 106–112. doi: 10.1016/0163-8343(95)00122-0
Goel, N., Terman, M., and Terman, J. S. (2002). Depressive symptomatology differentiates subgroups of patients with seasonal affective disorder. Depress Anxiety 15, 34–41. doi: 10.1002/da.1083
Haasen, C. (2000). “Kultur und Psychopathologie [Culture and psychopathology],” in Beurteilung psychischer Störungen in einer multikulturellen Gesellschaft [Assessment of mental disorders in a multicultural society], eds C. Haasen and O. Yagdiran (Freiburg i. Br.: Lambertus), 13–28.
Harrer, M., Cuijpers, P., Furukawa, T. A., and Ebert, D. D. (2021). Doing Meta-analysis with R: A Hands-on Guide. Boca Raton, FL and London: Chapman and Hall/CRC Press. doi: 10.1201/9781003107347
Hedges, L. V., and Vevea, J. L. (1998). Fixed- and random-effects models in meta-analysis. Psychol. Methods 3, 486–504. doi: 10.1037/1082-989X.3.4.486
Hedman, E., Lekander, M., Ljótsson, B., Lindefors, N., Rück, C., Andersson, G., et al. (2015). Optimal cut-off points on the health anxiety inventory, illness attitude scales and whiteley index to identify severe health anxiety. PLoS ONE10:e0123412. doi: 10.1371/journal.pone.0123412
Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., et al. (2022). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane. Available online at: www.training.cochrane.org/handbook
Higgins, J. P. T., and Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558. doi: 10.1002/sim.1186
Hollifield, M., Paine, S., Tuttle, L., and Kellner, R. (1999). Hypochondriasis, somatization, and perceived health and utilization of health care services. Psychosomatics 40, 380–386. doi: 10.1016/S0033-3182(99)71202-8
Hunter, L. R., and Schmidt, N. B. (2010). Anxiety psychopathology in African American adults: literature review and development of an empirically informed sociocultural model. Psychol. Bull. 136, 211–235. doi: 10.1037/a0018133
Kibbey, M. M., Fedorenko, E. J., and Farris, S. G. (2021). Anxiety, depression, and health anxiety in undergraduate students living in initial US outbreak “hotspot” during COVID-19 pandemic. Cogn. Behav. Ther. 50, 409–421. doi: 10.1080/16506073.2020.1853805
Klein, J., and von dem Knesebeck, O. (2018). Inequalities in health care utilization among migrants and non-migrants in Germany: a systematic review. Int. J. Equity Health 17:160. doi: 10.1186/s12939-018-0876-z
Lenhard, W., and Lenhard, A. (2016). Computation of Effect Sizes. Available online at: https://www.psychometrica.de/effect_size.html (accessed March 23, 2022).
Looper, K. J., and Kirmayer, L. J. (2001). Hypochondriacal concerns in a community population. Psychol. Med. 31, 577–584. doi: 10.1017/s0033291701003737
Marmot, M. G., and Wilkinson, R. G, . eds. (2011). Social Determinants of Health, 2 Edn. Oxford: Oxford Univ. Press.
McAuliffe, M., and Triandafyllidou, A., eds. (2021). World Migration Report 2022. Geneva: International Organization for Migration. doi: 10.1002/wom3.25
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. doi: 10.1371/journal.pmed.1000097
Mölsä, M., Punamäki, R. L., Saarni, S. I., Tiilikainen, M., Kuittinen, S., and Honkasalo, M. L. (2014). Mental and somatic health and pre- and post-migration factors among older Somali refugees in Finland. Transcult. Psychiatry 51, 499–525. doi: 10.1177/1363461514526630
Muse, K., McManus, F., Hackmann, A., Williams, M., and Williams, M. (2010). Intrusive imagery in severe health anxiety: prevalence, nature and links with memories and maintenance cycles. Behav. Res. Ther. 48, 792–798. doi: 10.1016/j.brat.2010.05.008
Mykletun, A., Heradstveit, O., Eriksen, K., Glozier, N., Øverland, S., Maeland, J. G., et al. (2009). Health anxiety and disability pension award: the HUSK Study. Psychosom. Med. 71, 353–360. doi: 10.1097/PSY.0b013e31819cc772
Newby, J. M., Hobbs, M. J., Mahoney, A. E. J., Wong, S. K., and Andrews, G. (2017). DSM-5 illness anxiety disorder and somatic symptom disorder: comorbidity, correlates, and overlap with DSM-IV hypochondriasis. J. Psychosom. Res. 101, 31–37. doi: 10.1016/j.jpsychores.2017.07.010
Norbye, A. D., Abelsen, B., Førde, O. H., and Ringberg, U. (2022). Health anxiety is an important driver of healthcare use. BMC Health Serv. Res. 22:138. doi: 10.1186/s12913-022-07529-x
Noyes, R., Carney, C. P., Hillis, S. L., Jones, L. E., and Langbehn, D. R. (2005). Prevalence and correlates of illness worry in the general population. Psychosomatics 46, 529–539. doi: 10.1176/appi.psy.46.6.529
Noyes, R., Happel, R. L., and Yagla, S. J. (1999). Correlates of hypochondriasis in a nonclinical population. Psychosomatics 40, 461–469. doi: 10.1016/S0033-3182(99)71183-7
Noyes, R., Watson, D. B., Carney, C. P., Letuchy, E. M., Peloso, P. M., Black, D. W., et al. (2004). Risk factors for hypochondriacal concerns in a sample of military veterans. J. Psychosom. Res. 57, 529–539. doi: 10.1016/j.jpsychores.2004.05.006
Orwin, R. G. (1983). A fail-safe N for effect size in meta-analysis. J. Educ. Stat. 8, 157–159. doi: 10.2307/1164923
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 372:n71. doi: 10.1136/bmj.n71
Pandey, S., Parikh, M., Brahmbhatt, M., and Vankar, G. K. (2017). Clinical study of illness anxiety disorder in medical outpatients. Arch. Psychiatry Psychother 19, 32–41. doi: 10.12740/APP/76932
Pilowsky, I., and Spence, N. D. (1977). Ethnicity and illness behaviour. Psychol. Med. 7, 447–452. doi: 10.1017/s0033291700004426
Pine, C. J. (1983). Obese and non-obese American Indian and Caucasian performance on the mini-mult MMPI and I-E scale. J. Clin. Psychol. 39, 251–256. doi: 10.1002/1097-4679(198303)39:2<251:aid-jclp2270390219>3.0.co;2-h
Pollock, A., and Berge, E. (2018). How to do a systematic review. Int. J. Stroke 13, 138–156. doi: 10.1177/1747493017743796
Rommel, A., Saß, A. C., Born, S., and Ellert, U. (2015). Die gesundheitliche Lage von Menschen mit Migrationshintergrund und die Bedeutung des sozioökonomischen Status: erste Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1) [Health status of people with a migrant background and impact of socio-economic factors: first results of the German health interview and examination survey for adults (DEGS1)]. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz 58, 543–552. doi: 10.1007/s00103-015-2145-2
Rosenthal, R. (1979). The file drawer problem and tolerance for null results. Psychol. Bull. 86, 638–641. doi: 10.1037/0033-2909.86.3.638
Sauer, K. S., and Witthöft, M. (2020). Krankheitsängste und Hypochondrische Störung. [Illness anxiety and hypochondriacal disorder]. Fortschr Neurol Psychiatr 88, 730–744. doi: 10.1055/a-1165-7461
Stroup, D. F., Berlin, J. A., Morton, S. C., Olkin, I., Williamson, G. D., Rennie, D., et al. (2000). Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. Jama 283, 2008–2012. doi: 10.1001/jama.283.15.2008
Thomas, B. H., Ciliska, D., Dobbins, M., and Micucci, S. (2004). A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid. Based Nurs. 1, 176–184. doi: 10.1111/j.1524-475X.2004.04006.x
Tyrer, P. (2018). Recent advances in the understanding and treatment of health anxiety. Curr. Psychiatry Rep. 20:49. doi: 10.1007/s11920-018-0912-0
Viechtbauer, W. (2021). Fail-safe N Analysis (File Drawer Analysis). In Metafor: Meta-analysis Package for R. Available online at: https://rdrr.io/cran/metafor/man/fsn.html (accessed February 22, 2022).
Warwick, H. M., and Salkovskis, P. M. (1990). Hypochondriasis. Behav. Res. Ther. 28, 105–117. doi: 10.1016/0005-7967(90)90023-C
Weck, F., Richtberg, S., and Neng, J. (2014). Epidemiology of hypochondriasis and health anxiety: comparison of different diagnostic criteria. Curr. Psychiatry Rev. 10, 14–23. doi: 10.2174/1573400509666131119004444
World Health Organization (2010a). A Conceptual Framework for Action on the Social Determinants of Health. Social Determinats of Health Discussion Paper 2. Geneva: World Health Organization.
World Health Organization (2010b). How Health Systems Can Address Health Inequaities Linked to Migration and Ethnicity. Copenhagen: World Health OrganizationRegional Office for Europe.
World Health Organization (2019). International Classification of Diseases. 11th Rev. Geneva: World Health Organization.
World Health Organization (2021). Mental Health and Forced Displacement. Available online at: https://www.who.int/news-room/fact-sheets/detail/mental-health-and-forced-displacement (accessed June 30, 2022).
World Health Organization (2022a). Refugee and Migrant Health. Available online at: https://www.who.int/health-topics/refugee-and-migrant-health#tab=tab_1 (accessed June 30, 2022).
World Health Organization (2022b). Social Determinants of Health. Available online at: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 (accessed July 04, 2022).
Keywords: migration, ethnicity, ethnic minority, health anxiety, hypochondriasis, health inequalities, systematic review, meta-analysis
Citation: Barbek R, Henning S, Ludwig J and von dem Knesebeck O (2022) Ethnic and migration-related inequalities in health anxiety: A systematic review and meta-analysis. Front. Psychol. 13:960256. doi: 10.3389/fpsyg.2022.960256
Received: 02 June 2022; Accepted: 08 August 2022;
Published: 26 August 2022.
Edited by:
Tina Cartwright, University of Westminster, United KingdomReviewed by:
Kerstin Spanhel, University of Freiburg, GermanyLambert Zixin Li, Stanford University, United States
Tingting Liu, National Institute on Drug Abuse (NIH), United States
Copyright © 2022 Barbek, Henning, Ludwig and von dem Knesebeck. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rieke Barbek, ci5icmJla0B1a2UuZGU=
 Rieke Barbek
Rieke Barbek Sinje Henning
Sinje Henning Olaf von dem Knesebeck
Olaf von dem Knesebeck