
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Psychol., 28 September 2022
Sec. Psychology for Clinical Settings
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.940088
This article is part of the Research TopicThe Bio-Psycho-Social Approach to Understanding Mental DisordersView all 7 articles
 Izabella Uchmanowicz1,2
Izabella Uchmanowicz1,2 Marta Wleklik1,2
Marta Wleklik1,2 Marva Foster3,4
Marva Foster3,4 Agnieszka Olchowska-Kotala5
Agnieszka Olchowska-Kotala5 Ercole Vellone1,6
Ercole Vellone1,6 Marta Kaluzna-Oleksy7
Marta Kaluzna-Oleksy7 Remigiusz Szczepanowski8
Remigiusz Szczepanowski8 Bartosz Uchmanowicz9*
Bartosz Uchmanowicz9* Krzysztof Reczuch2,10
Krzysztof Reczuch2,10 Ewa Anita Jankowska2,10
Ewa Anita Jankowska2,10Despite advances in the treatment of heart failure (HF), the physical symptoms and stress of the disease continue to negatively impact patients’ health outcomes. Technology now offers promising ways to integrate personalized support from health care professionals via a variety of platforms. Digital health technology solutions using mobile devices or those that allow remote patient monitoring are potentially more cost effective and may replace in-person interaction. Notably, digital health methods may not only improve clinical outcomes but may also improve the psycho-social status of HF patients. Using digital health to address biopsychosocial variables, including elements of the person and their context is valuable when considering chronic illness and HF in particular, given the multiple, cross-level factors affecting chronic illness clinical management needed for HF self-care.
The search for technological solutions to support HF patients in managing their physical and psychological well-being is important because self-management has been shown to decrease hospitalizations and improve survival (Meng et al., 2021). As digital technologies will play an increasing role in the management of HF patients, it is important to assess their impact on both physical and psychosocial support and identify those most effective to incorporate in daily clinical practice. This review discusses the use of digital health and modern technologies that can be used to support psychosocial well-being in patients with HF. The review will follow the pattern as seen in Figure 1.
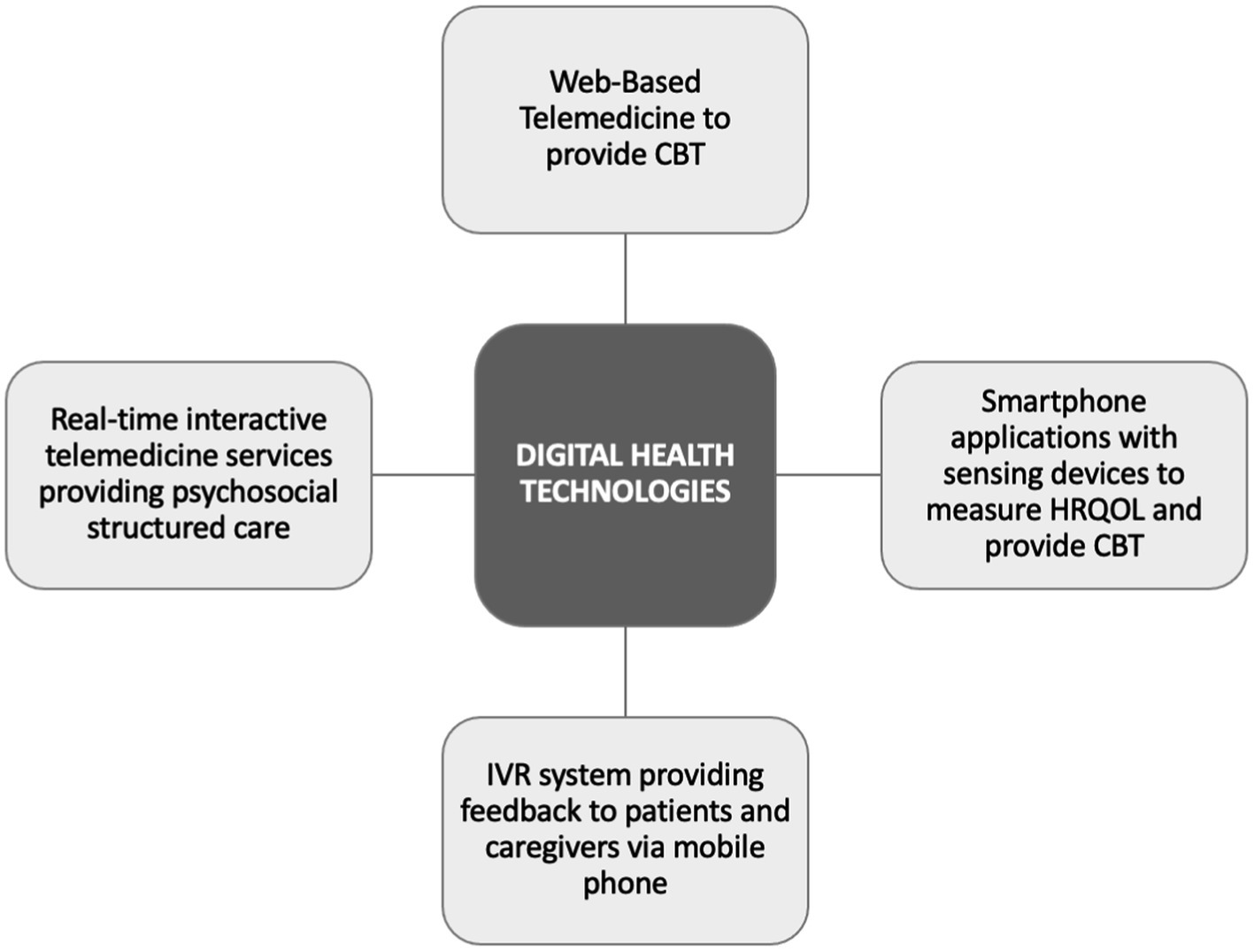
Figure 1. Scheme of main applications of digital health technologies in heart failure for biopsychosocial support.
The current global prevalence of heart failure (HF) is estimated at 64.3 million cases (Lippi and Sanchis-Gomar, 2020). This is expected to rise due to population growth, increasing numbers of older adults and improved survival after cardiovascular events (Obiegło et al., 2016, 2017). Research increasingly shows how selective and targeted use of digital health technologies—mobile health, remote patient monitoring, telemedicine and telehealth—can have several advantages in improving psychosocial support (De Witte et al., 2021; Farwati et al., 2021). Ideally, such strategies should be components of HF transition of care programs and include individualized interventions (Ong et al., 2016).
Interactive voice response, or IVR, allows patients to communicate with clinicians asynchronously using a mobile or landline telephone (Piette et al., 2013). Based on their responses, the patients can receive tailored feedback during the same call, and clinicians can receive alerts identifying patients who need additional assistance (Piette, 2000; Skolarus et al., 2017). Interactive voice response has also been used to facilitate telephone peer-to-peer support among older adults with HF (Heisler et al., 2007). Participants were paired with another patient who had HF who they contacted weekly using a toll-free IVR phone system. The study noted positive effects on participants’ HF social support and an improvement in depressive symptoms. In another IVR HF study (Zan et al., 2015), it was found that almost all participants reported feeling more connected to their health care team and their HF-related quality of life scores improved from baseline. Thus, indicating the efficacy of increased engagement and support with patients may alleviate loneliness and social isolation. The results from Clark et al. (2007) support the rationale for using IVR and telemonitoring as part of a comprehensive chronic HF management program. They show a high acceptability rate of 78% for such methods. As the study involved elderly patients, it can be considered that this vulnerable audience will be able to adapt to such solutions and accept them as part of the healthcare routine (Clark et al., 2007). The effectiveness of digital health solutions is dependent on the context in which they are applied. It has been suggested that interventions with more contact between clinicians and patients could be more effective (Chaudhry et al., 2010).
Real-time telemedicine, or interactive telemedicine, uses real-time interaction between patients and health professionals (Segato and Masella, 2017; Sasikala et al., 2018). Using real-time interactive services to address biopsychosocial variables, including elements of the person and their context is useful when considering chronic illness and HF in particular, given the multiple, cross-level factors affecting chronic illness clinical management and HF self-care (Holden et al., 2015a,b, 2017). In a study of a group-based HF telerehabilitation program found that participants liked the health benefits, access to care and social support (Hwang et al., 2017). The Better Effectiveness After Transition–Heart Failure (BEAT-HF) study found that telephone support improved the quality of life for patients 180 days after hospital discharge. The study offered: HF patient education before hospital discharge, regularly scheduled telephone coaching, and home telemonitoring of symptoms (Ong et al., 2016). Individuals participating in the intervention experienced improvements in their quality of life over the course of the study (Cordeiro et al., 2022). Research has shown that telephone contact to a trained nurse with access to a family physician, can prevent hospitalization in a quarter of HF patients (Kolasa et al., 2020). Therefore, patients with low social support or feelings of loneliness may therefore benefit from the support provided by telephone interventions (Blumenthal et al., 2019).
In a multisite randomized clinical trial (RCT) of the Collaborative Care to Alleviate Symptoms and Adjust to Illness (CASA) intervention, it was found that although HF-specific health status did not improve, secondary outcomes of depression and fatigue, both difficult symptoms to treat in HF, did improve (Bekelman et al., 2018). In yet another RCT comparing telemedicine versus a comprehensive outpatient management program, there was a demonstrated reduction in both anxiety and depression over the study period of 90 days (Pekmezaris et al., 2019). The Telemedical Interventional Management in Patients with Heart Failure (TIM-HF2) study suggests that a structured remote patient management intervention, can improve quality of life, while reducing the rate of lost days due to unplanned hospital admissions for cardiovascular causes and mortality from any cause (Koehler et al., 2018). Another study found that HF patients who received diet, medication and lifestyle teaching via real-time interactive services with nurses improved their mental health status, quality of life and an associated decrease in rehospitalization over a 1-year period (Mo et al., 2021).
Mobile health (m-Health) is defined as medical and public health practice supported by mobile devices, such as smartphones, software apps on mobile devices, wireless sensors, etc. (WHO Global Observatory for eHealth, 2011; Sohn et al., 2020). The ubiquity of smartphones makes them a unique tool to use for providing psychosocial support. mHealth technology is increasingly being proposed for cardiovascular disease management (Lewis et al., 2016). Studies using mHealth interventions have shown to improve psychosocial functioning in those with noncardiac chronic medical conditions (Mlynarska et al., 2018; Sevilla-Cazes et al., 2018; Mansouri et al., 2019). This clear therapeutic potential indicates the possibility of mHealth as tool to improve the psychosocial status of those with HF. In a study using smartphones with wireless sensors, patient-reported outcome measures indicated improvement in fatigue, anxiety, depression, sleep disturbance, and social isolation (Sohn et al., 2020). The improvement persisted through the 180-day follow-up of the study. The HeartMan study, an RCT of HF patients, used a mHealth system that included a psychological support component. The psychological component included personalized messages based on cognitive behavioral therapy (CBT) and a weekly mindfulness games and exercises for relaxation and general psychological wellbeing. The findings suggest that psychological support has an important impact on patients, relieving their symptoms of depression, as well as their state and trait signs of anxiety (Toukhsati et al., 2015; Clays et al., 2021). This is in line with the growing evidence showing the ability of mindfulness to improve psychological well-being in chronic disease overall (Toback and Clark, 2017), and specifically in CHF (Löfvenmark et al., 2009). The results of HeartMan were similar to the home-based self-management psychosocial education intervention (HOM-HEMP) RCT (Jiang et al., 2021). In another study (Hägglund et al., 2019), using an mHealth system, participants reported that the system not only helped them better manage their heart failure but offered them psychological support, comfort, and a feeling of not being alone in their situation.
Web-based or internet-based cognitive behavioral therapy (ICBT) is therapy provided through a computer or a mobile device (Lear et al., 2021). In ICBT, patients become active participants in their treatment and perform tasks to become aware of and to modify negative thoughts, emotions and unhelpful behaviors (Lundgren et al., 2016). A randomized clinical trial (RCT) of 230 participants compared the effect of an internet-based self-management and symptom monitoring program targeted (that included ICBT) to patients with HF and other chronic diseases (internet chronic disease management [CDM]) with usual care on hospitalizations over a 2-year period. The findings showed that self-management improved as well as social support as measured by the Medical Outcomes Study Social Support Scale (Sherbourne and Stewart, 1991). There was a significant change in favor of the internet CDM intervention in 2 of the 5 domains: emotional and informational support and overall support. In addition, fewer participants in the internet CDM vs. usual care group had at least 1 hospitalization and had a lower risk of time to first hospitalization.
An RCT investigating of 62 participants compared the effect of an ICBT program compared and an online moderated discussion forum in patients with HF (Lundgren et al., 2016). The study found a statistically significant improvement in depressive symptoms among patients in the ICBT group (Lundgren et al., 2016). In a follow-up qualitative study conducted with participants from this same RCT, findings revealed that participants perceived the support from the program as confirmative and motivating (Lundgren et al., 2018). Thus, the efficacy of using ICBT to improve psychosocial status remains a valid digital tool.
In this review, we looked at several inter/intra-disciplinary digital health interventions that incorporated elements of psychosocial support. Among patients with HF, lack of emotional support has been shown to be a significant predictor of fatal and nonfatal cardiovascular outcomes within 1 year of hospital admission (Krumholz et al., 1998). Psychosocial support is therefore essential for maintaining physical and emotional well-being, supporting effective coping with HF symptoms, and improving patients’ life quality. Identifying the availability of social support should become an integral part of HF care, especially since in just over half of HF patients, having a partner does not translate into receiving high levels of support (Barutcu and Mert, 2013; Albert et al., 2015). Digital health technology now offers promising ways to integrate personalized support from health care professionals and improve the psychosocial status of HF patients (Van Spall et al., 2019) In conclusion, while there is no clear consensus on the type of digital technology and the optimal timing of its use in HF self-care, it is clear that these technologies have the ability to improve psychosocial wellbeing.
IU, MW, MF, AO-K, EV, MK-O, RS, BU, KR, and EJ participated equally in this paper and were responsible for the paper conception, data collection, literature review as well as drafting and reviewing the manuscript. All authors contributed to the article and approved the submitted version.
This review paper was supported by the Ministry of Health subventions according to the number of SUBZ.E250.22.095 from the IT Simple system of the Wroclaw Medical University in Poland.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
CBT, Cognitive behavioral therapy; HRQOL, Health-related quality of life; IVR, Interactive voice response.
Albert, N. M., Barnason, S., Deswal, A., Hernandez, A., Kociol, R., Lee, E., et al. (2015). Transitions of care in heart failure: a scientific statement from the American Heart Association. Circ. Heart Fail. 8, 384–409. doi: 10.1161/HHF.0000000000000006
Barutcu, C. D., and Mert, H. (2013). The relationship between social support and quality of life in patients with heart failure. J. Pak. Med. Assoc. 63, 463–467.
Bekelman, D. B., Allen, L. A., McBryde, C. F., Hattler, B., Fairclough, D. L., Havranek, E. P., et al. (2018). Effect of a Collaborative Care Intervention vs Usual Care on Health Status of Patients With Chronic Heart Failure. JAMA Intern. Med. 178, 511–519. doi: 10.1001/jamainternmed.2017.8667
Blumenthal, J. A., Zhu, Y., Koch, G. G., Smith, P. J., Watkins, L. L., Hinderliter, A. L., et al. (2019). The modifying effects of social support on psychological outcomes in patients with heart failure. Health Psychol. 38, 502–508. doi: 10.1037/hea0000716
Chaudhry, S. I., Mattera, J. A., Curtis, J. P., Spertus, J. A., Herrin, J., Lin, Z., et al. (2010). Telemonitoring in Patients with Heart Failure. N. Engl. J. Med. 363, 2301–2309. doi: 10.1056/NEJMoa1010029
Clark, R. A., Yallop, J. J., Piterman, L., Croucher, J., Tonkin, A., Stewart, S., et al. (2007). Adherence, adaptation and acceptance of elderly chronic heart failure patients to receiving healthcare via telephone-monitoring. Eur. J. Heart Fail. 9, 1104–1111. doi: 10.1016/j.ejheart.2007.07.018
Clays, E., Puddu, P. E., Luštrek, M., Pioggia, G., Derboven, J., Vrana, M., et al. (2021). Proof-of-concept trial results of the HeartMan mobile personal health system for self-management in congestive heart failure. Sci. Rep. 11:5663. doi: 10.1038/s41598-021-84920-4
Cordeiro, A. L. L., da Silva Miranda, A., de Almeida, H. M., and Santos, P. (2022). Quality of life in patients with heart failure assisted by telerehabilitation: a systematic review and meta-analysis. Int. J. Telerehabil. 14:e6456. doi: 10.5195/ijt.2022.6456
De Witte, N. A. J., Joris, S., Van Assche, E., and Van Daele, T. (2021). Technological and Digital Interventions for Mental Health and Wellbeing: An Overview of Systematic Reviews. Front. Digit. Health 3:754337. doi: 10.3389/fdgth.2021.754337
Farwati, M., Riaz, H., and Tang, W. H. W. (2021). Digital Health Applications in Heart Failure: a Critical Appraisal of Literature. Curr. Treat. Options Cardiovasc. Med. 23:12. doi: 10.1007/s11936-020-00885-z
Hägglund, E., Strömberg, A., Hagerman, I., and Lyngå, P. (2019). Theory Testing of Patient Perspectives Using a Mobile Health Technology System in Heart Failure Self-care. J. Cardiovasc. Nurs. 34, 448–453. doi: 10.1097/JCN.0000000000000595
Heisler, M., Halasyamani, L., Resnicow, K., Neaton, M., Shanahan, J., Brown, S., et al. (2007). “I am not alone”: the feasibility and acceptability of interactive voice response-facilitated telephone peer support among older adults with heart failure. Congest. Heart Fail. 13, 149–157. doi: 10.1111/j.1527-5299.2007.06412.x
Holden, R. J., Schubert, C. C., Eiland, E. C., Storrow, A. B., Miller, K. F., and Collins, S. P. (2015a). Self-care Barriers Reported by Emergency Department Patients With Acute Heart Failure: A Sociotechnical Systems-Based Approach. Ann. Emerg. Med. 66, 12e.1–12e.2. doi: 10.1016/j.annemergmed.2014.12.031
Holden, R. J., Schubert, C. C., and Mickelson, R. S. (2015b). The patient work system: an analysis of self-care performance barriers among elderly heart failure patients and their informal caregivers. Appl. Ergon. 47, 133–150. doi: 10.1016/j.apergo.2014.09.009
Holden, R. J., Valdez, R. S., Schubert, C. C., Thompson, M. J., and Hundt, A. S. (2017). Macroergonomic factors in the patient work system: examining the context of patients with chronic illness. Ergonomics 60, 26–43. doi: 10.1080/00140139.2016.1168529
Hwang, R., Mandrusiak, A., Morris, N. R., Peters, R., Korczyk, D., Bruning, J., et al. (2017). Exploring patient experiences and perspectives of a heart failure telerehabilitation program: A mixed methods approach. Heart Lung J. Crit. Care 46, 320–327. doi: 10.1016/j.hrtlng.2017.03.004
Jiang, Y., Koh, K. W. L., Ramachandran, H. J., Nguyen, H. D., Lim, D. S., Tay, Y. K., et al. (2021). The effectiveness of a nurse-led home-based heart failure self-management programme (the HOM-HEMP) for patients with chronic heart failure: A three-arm stratified randomized controlled trial. Int. J. Nurs. Stud. 122:104026. doi: 10.1016/j.ijnurstu.2021.104026
Koehler, F., Koehler, K., Deckwart, O., Prescher, S., Wegscheider, K., Kirwan, B.-A., et al. (2018). Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet 392, 1047–1057. doi: 10.1016/S0140-6736(18)31880-4
Kolasa, J., Uchmanowicz, I., Wleklik, M., Lisiak, M., Lelonek, M., Pawlak, A., et al. (2020). “The Weak Heart” as an educational model for patients hospitalised due to decompensation of heart failure with reduced ejection fraction. Folia Cardiol. 15, 99–106. doi: 10.5603/FC.a2020.0014
Krumholz, H. M., Butler, J., Miller, J., Vaccarino, V., Williams, C. S., Mendes de Leon, C. F., et al. (1998). Prognostic importance of emotional support for elderly patients hospitalized with heart failure. Circulation 97, 958–964. doi: 10.1161/01.cir.97.10.958
Lear, S. A., Norena, M., Banner, D., Whitehurst, D. G. T., Gill, S., Burns, J., et al. (2021). Assessment of an Interactive Digital Health-Based Self-management Program to Reduce Hospitalizations Among Patients With Multiple Chronic Diseases: A Randomized Clinical Trial. JAMA Netw. Open 4:e2140591. doi: 10.1001/jamanetworkopen.2021.40591
Lewis, J., Ray, P., and Liaw, S.-T. (2016). Recent Worldwide Developments in eHealth and mHealth to more Effectively Manage Cancer and other Chronic Diseases - A Systematic Review. Yearb. Med. Inform. 1, 93–108. doi: 10.15265/IY-2016-020
Lippi, G., and Sanchis-Gomar, F. (2020). Global epidemiology and future trends of heart failure. AME Med. J. 5:15. doi: 10.21037/amj.2020.03.03
Löfvenmark, C., Mattiasson, A.-C., Billing, E., and Edner, M. (2009). Perceived loneliness and social support in patients with chronic heart failure. Eur. J. Cardiovasc. Nurs. 8, 251–258. doi: 10.1016/j.ejcnurse.2009.05.001
Lundgren, J. G., Dahlström, Ö., Andersson, G., Jaarsma, T., Kärner Köhler, A., and Johansson, P. (2016). The Effect of Guided Web-Based Cognitive Behavioral Therapy on Patients With Depressive Symptoms and Heart Failure: a Pilot Randomized Controlled Trial. J. Med. Internet Res. 18:e194. doi: 10.2196/jmir.5556
Lundgren, J., Johansson, P., Jaarsma, T., Andersson, G., and Kärner Köhler, A. (2018). Patient Experiences of Web-Based Cognitive Behavioral Therapy for Heart Failure and Depression: Qualitative Study. J. Med. Internet Res. 20:e10302. doi: 10.2196/10302
Mansouri, A., Baraz, S., Elahi, N., Malehi, A. S., and Saberipour, B. (2019). The effect of an educational program based on Roy’s adaptation model on the quality of life of patients suffering from heart failure: A clinical trial study. Jpn. J. Nurs. Sci. 16, 459–467. doi: 10.1111/jjns.12255
Meng, X., Wang, Y., Tang, X., Gu, J., and Fu, Y. (2021). Self-management on heart failure: A meta-analysis. Diabetes Metab. Syndr. 15:102176. doi: 10.1016/j.dsx.2021.06.013
Mlynarska, A., Golba, K. S., and Mlynarski, R. (2018). Capability for self-care of patients with heart failure. Clin. Interv. Aging 13, 1919–1927. doi: 10.2147/CIA.S178393
Mo, Y., Chu, M., Hu, W., and Wang, H. (2021). Association between the nurse-led program with mental health status, quality of life, and heart failure rehospitalization in chronic heart failure patients. Medicine 100:e25052. doi: 10.1097/MD.0000000000025052
Obiegło, M., Siennicka, A., Jankowska, E. A., and Danel, D. P. (2017). Direction of the Relationship Between Acceptance of Illness and Health-Related Quality of Life in Chronic Heart Failure Patients. J. Cardiovasc. Nurs. 32, 348–356. doi: 10.1097/JCN.0000000000000365
Obiegło, M., Uchmanowicz, I., Wleklik, M., Jankowska-Polańska, B., and Kuśmierz, M. (2016). The effect of acceptance of illness on the quality of life in patients with chronic heart failure. Eur. J. Cardiovasc. Nurs. 15, 241–247. doi: 10.1177/1474515114564929
Ong, M. K., Romano, P. S., Edgington, S., Aronow, H. U., Auerbach, A. D., Black, J. T., et al. (2016). Effectiveness of Remote Patient Monitoring After Discharge of Hospitalized Patients With Heart Failure: The Better Effectiveness After Transition -- Heart Failure (BEAT-HF) Randomized Clinical Trial. JAMA Intern. Med. 176, 310–318. doi: 10.1001/jamainternmed.2015.7712
Pekmezaris, R., Nouryan, C. N., Schwartz, R., Castillo, S., Makaryus, A. N., Ahern, D., et al. (2019). A Randomized Controlled Trial Comparing Telehealth Self-Management to Standard Outpatient Management in Underserved Black and Hispanic Patients Living with Heart Failure. Telemed. J. E-Health 25, 917–925. doi: 10.1089/tmj.2018.0219
Piette, J. D. (2000). Interactive voice response systems in the diagnosis and management of chronic disease. Am. J. Manag. Care 6, 817–827.
Piette, J. D., Rosland, A.-M., Marinec, N. S., Striplin, D., Bernstein, S. J., and Silveira, M. J. (2013). Engagement with automated patient monitoring and self-management support calls: experience with a thousand chronically ill patients. Med. Care 51, 216–223. doi: 10.1097/MLR.0b013e318277ebf8
Sasikala, S., Indhira, K., and Chandrasekaran, V. M. (2018). Performance prediction of interactive telemedicine. Inform. Med. Unlocked 11, 87–94. doi: 10.1016/j.imu.2018.03.003
Segato, F., and Masella, C. (2017). Telemedicine services: How to make them last over time. Health Policy Technol. 6, 268–278. doi: 10.1016/j.hlpt.2017.07.003
Sevilla-Cazes, J., Ahmad, F. S., Bowles, K. H., Jaskowiak, A., Gallagher, T., Goldberg, L. R., et al. (2018). Heart Failure Home Management Challenges and Reasons for Readmission: a Qualitative Study to Understand the Patient’s Perspective. J. Gen. Intern. Med. 33, 1700–1707. doi: 10.1007/s11606-018-4542-3
Sherbourne, C. D., and Stewart, A. L. (1991). The MOS social support survey. Soc. Sci. Med. 1982, 705–714. doi: 10.1016/0277-9536(91)90150-b
Skolarus, L. E., Piette, J. D., Pfeiffer, P. N., Williams, L. S., Mackey, J., Hughes, R., et al. (2017). Interactive Voice Response-An Innovative Approach to Post-Stroke Depression Self-Management Support. Transl. Stroke Res. 8, 77–82. doi: 10.1007/s12975-016-0481-7
Sohn, A., Speier, W., Lan, E., Aoki, K., Fonarow, G. C., Ong, M. K., et al. (2020). Integrating remote monitoring into heart failure patients’ care regimen: A pilot study. PLoS One 15:e0242210. doi: 10.1371/journal.pone.0242210
Toback, M., and Clark, N. (2017). Strategies to improve self-management in heart failure patients. Contemp. Nurse 53, 105–120. doi: 10.1080/10376178.2017.1290537
Toukhsati, S. R., Driscoll, A., and Hare, D. L. (2015). Patient Self-management in Chronic Heart Failure-Establishing Concordance Between Guidelines and Practice. Card. Fail. Rev. 1, 128–131. doi: 10.15420/cfr.2015.1.2.128
Van Spall, H. G. C., Lee, S. F., Xie, F., Oz, U. E., Perez, R., Mitoff, P. R., et al. (2019). Effect of Patient-Centered Transitional Care Services on Clinical Outcomes in Patients Hospitalized for Heart Failure. JAMA 321, 753–761. doi: 10.1001/jama.2019.0710
WHO Global Observatory for eHealth (2011). mHealth: new horizons for health through mobile technologies: second global survey on eHealth. Geneva 27, Switzerland: World Health Organization.
Keywords: digital health, heart failure, modern technologies, patient-centered outcomes, telemedicine
Citation: Uchmanowicz I, Wleklik M, Foster M, Olchowska-Kotala A, Vellone E, Kaluzna-Oleksy M, Szczepanowski R, Uchmanowicz B, Reczuch K and Jankowska EA (2022) Digital health and modern technologies applied in patients with heart failure: Can we support patients’ psychosocial well-being? Front. Psychol. 13:940088. doi: 10.3389/fpsyg.2022.940088
Received: 17 May 2022; Accepted: 09 September 2022;
Published: 28 September 2022.
Edited by:
Emmanuel Andrès, Hôpitaux Universitaires de Strasbourg, FranceReviewed by:
Sara Marelli, San Raffaele Hospital (IRCCS), ItalyCopyright © 2022 Uchmanowicz, Wleklik, Foster, Olchowska-Kotala, Vellone, Kaluzna-Oleksy, Szczepanowski, Uchmanowicz, Reczuch and Jankowska. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bartosz Uchmanowicz, YmFydG9zei51Y2htYW5vd2ljekB1bXcuZWR1LnBs
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.