
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
OPINION article
Front. Psychol., 21 June 2022
Sec. Eating Behavior
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.926415
Autism Spectrum Disorder (ASD) is a lifelong neurodevelopmental condition characterized by anomalies in two domains: social interactions and communication, and restricted/repetitive patterns of behaviors (American Psychiatric Association [APA], 2013). Cognitive-behavioral processes (e.g., central coherence, set shifting) associated with autism have further been linked with eating disorders (EDs) (Huke et al., 2013): life-threatening psychiatric conditions that affect psychological, physical and social well-being (American Psychiatric Association [APA], 2013; Schmidt et al., 2016). As such, research has established several commonalities in underlying cognitive and neural phenotypes in autism and anorexia nervosa (AN) (characterized by restrictive food intake, disproportionate fear of weight gain and weight and shape concerns; American Psychiatric Association [APA], 2013; Westwood and Tchanturia, 2017). More specifically, evidence suggests autistic traits, such as differing cognitive-behavioral and/or body-sensory processing, increases the risk of developing disordered body and eating pathology (Tchanturia et al., 2013; Vuillier et al., 2020). Extant ED research has, however, approached autism as a co-occurrence with EDs: an afterthought to a primary ED symptom profile. Thus, what remains is the exploration into the opposite and increasingly isolated phenomenon – EDs in people with autism (and related neurodiverse markers). Consequently, present screening tools and interventions for EDs lack adaptation and translation to neurodivergent populations (Huke et al., 2013; Tchanturia et al., 2020). Current research and practice therefore inaccurately capture and/or target how constructs are experienced in this population, negatively impacting the rigor and validity of ED intervention development and their application(s) (Nicolaidis et al., 2020).
As part of developing screening tools and interventions, researchers are encouraged to refer to theoretical models to guide their content, design, and administration (Campbell et al., 2000; Skivington et al., 2021). A systematic review identified twenty-three theoretical models for disordered eating, most of which refer to cognitive-behavioral approaches and have helped inform the development of screening tools and interventions for disordered eating (Pennesi and Wade, 2016). Conceptual ambiguity in current theory is, however, maintained by relying on cognitive-behavioral features that often differ in presentation (observed from others) and phenomenology (ones' felt experience) among autistic individuals, including: (i) body self-schema, (ii) cognitive biases, (iii) compensatory behaviors, and (iv) psychological risk factors for developing and/or maintaining disordered body and eating pathology (see Williamson et al., 2004). As a result, this perpetuates an axis of contention regarding limited generalisability among individuals with cognitive-behavioral variances, such as autistic individuals (Pennesi and Wade, 2016). Furthermore, existing models lack reference to other EDs commonly associated with autism – in particular, avoidant/restrictive food intake disorder (ARFID) (persistent avoidance/disturbance in feeding or eating due to sensory concerns and/or lack of interest; American Psychiatric Association [APA], 2013; Farag et al., 2021). For a more inclusive conceptualization of EDs, existing models should be adapted, or a parallel explanatory framework should be developed alongside existing practice, to better serve neurodivergent populations.
Here, we synthesize transdisciplinary autism research to better account for presentations distinctive to the neurodiverse population. While it is beyond the scope of this Opinion to yield a simple, concrete model, it will illustrate an actionable opportunity to develop an integrative framework which addresses current limitations in the ED literature by integrating the autistic experience into existing models for EDs.
Within autism research, the autistic personality (AP) consists of behaviors denoting an underlying neurobiological endophenotype identified within the diagnostic profile for autism (Landry and Chouinard, 2016; Sarovic, 2021). The AP conceptualizes autism as being manifold (see Sarovic, 2021), in contrast to the Autism Quotient Questionnaire (AQ) (Baron-Cohen et al., 2001), which originally quantified autistic traits as being unidimensional – that is, the “continuum from ASD to normality” (Murray et al., 2014, p. 56). This notion of normality has, in effect, led to current research and practice to compare – and inherently pathologize – AP features against behaviors which are traditionally considered ‘typical' (Sucksmith et al., 2011). The AP, however, shifts the autistic experience away from this reductionist, nosographic sphere by considering primary phenomenon, rather than behavioral epiphenomenon – specifically, it is contextual and idiosyncratic in its approach. Differentiating the “disorder” (ASD) to the AP in the context of EDs is therefore foundational to understanding the unique sequalae of EDs from a neurodiverse perspective, rather than through “normative” observation – for instance, acknowledging adaptive eating behaviors to be autism-specific (e.g., avoiding certain food groups to manage sensory difficulties; Kinnaird et al., 2019), rather than inherently being maladaptive (e.g., avoiding food for weight-loss).
While the AP and AQ both recognize phenotypic issues – in particular, presentations of a maladaptive behavioral phenotype (Sarovic, 2021) – the AP is more complex by accounting for the accumulative effect of behavioral difficulties (e.g., altered sensory processing) subsequent to cognitive compensation (CC): the cognitive ability to compensate for, and overcome, maladaptive AP features through learning and carrying out adaptive responses (see Pugliese et al., 2015, 2016; Livingston and Happé, 2017). Although relatively temporally stable, CC is dependent on internal (e.g., heritability, executive function) and external factors (e.g., day-to-day cognitive demands; Happé and Frith, 2006; Livingston and Happé, 2017). CC is therefore associated with a multitude of risk factors, implying diverse potential pathways which may generate impairment and contribute to AP maladaptation (Lenroot and Yeung, 2013). As a result, CC is highly individualized : two individuals may present equal cognitive deficits, however present differences in behavior due to varying in amount of CC; AP features may also lessen over time in one individual, to the extent they no longer fulfill the ASD diagnostic profile (Livingston and Happé, 2017). In other words, the AP presents heterogeneity across dynamic psychic facets, influencing disorder developmental trajectory and outcomes (Uljarevic et al., 2017) – which should be accounted for within ED theory and practice. Moreover, impaired CC increases the probability of the AP to become both pronounced and maladaptive, giving rise to complex mental health difficulties (Geurts et al., 2014; Ullman and Pullman, 2015; Lever and Geurts, 2016). Overall, rather than applying a diagnosis of AN across all samples presenting restrictive eating and/or body dissatisfaction, we argue additional investigation to determine whether such symptomatology is simply features of the AP (e.g., lower interoceptive awareness) or inadequate CC/maladaptive AP (Sarovic, 2021).
Brede et al. (2020) developed a model of restrictive eating in autism, which proposes autistic-specific mechanisms to induce ED development and/or maintenance. This model presents underlying mechanisms and/or presentations through an “autistic” lens, including sensory sensitivities (e.g., altered interoceptive awareness); social interactions and relationships; impaired self and identity; emotional difficulties; and alternative thinking styles. Whilst these features are general risk factors for EDs among the neurotypical population, they disproportionately affect autistic individuals in terms of severity and frequency (Westwood and Tchanturia, 2017). Therefore, it is plausible that beneath the surface of “typical” risk-factors (e.g., appearance internalization) lies autism-specific risk factors (e.g., social camouflaging/masking; Brede et al., 2020).
Features of the (non-pathological) AP acts as a “first-hit” for precipitating ED-like behavior (e.g., missing meals/overeating by accident), as an individual reports differences in cognitive and body-sensory processes, such as altered interoceptive awareness (e.g., differing awareness of hunger, satiation or thirst; see Hatfield et al., 2019; Kinnaird et al., 2019). However, research considers these body-sensory processes as typically “innate,” moderating both positive (e.g., intuitive eating) and negative outcomes (e.g., disordered eating) (Tribole and Resch, 2003). Subsequently, existing models associate these processes with the ED etiology and/or target of intervention. For example, the multidimensional model of AN proposes biogenetic and personality factors (e.g., low interoceptive awareness) to predict ED onset (Lyon et al., 1997), while the acceptance model of intuitive eating posits intuitive and/or adaptive eating to prevent and/or reduce ED symptomatology (Augustus-Horvath and Tylka, 2011; Babbott et al., 2022). Furthermore, the AP and its features can be broadly categorized into two domains: social (e.g., communicative/relational difficulties) and non-social (e.g., repetitive/restrictive behaviors, intense/obsessive interests; see Happé et al., 2006). Yet, current ED practice is predominantly informed by theory, such as the cognitive-interpersonal maintenance model of AN (Schmidt and Treasure, 2006; Treasure and Schmidt, 2013), which again asserts that AP features – particularly, obsessive-compulsive and interpersonal difficulties – act as predisposing and/or maintenance factors for EDs. Overall, existing ED theory and practice assume features of the AP to inherently underlie ED pathology (Table 1 presents a non-exhaustive list which highlights these current conceptual ambiguities). Yet, the incidence of mental health difficulties amongst autistic individuals “might [alternatively] speak to the demanding and taxing nature of [CC]” (Livingston and Happé, 2017, p. 736). Current theory and practice should therefore accommodate – rather than pathologize – the AP, and alternatively focus on the “second-hit” of impaired CC, which precipitates maladaptive responses to AP challenges, such as sensory sensitivities, and manifests ED symptomatology. For example, (re)conceptualizing restrictive eating to include rationales like avoiding sensations of digestion due to sensory sensitivities (Trevisan et al., 2012).
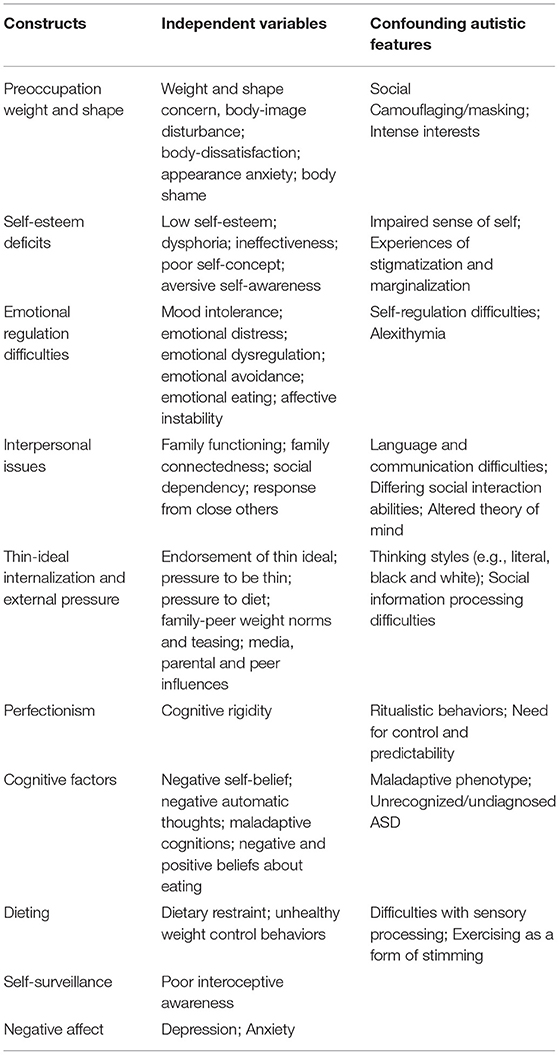
Table 1. A list of the main existing constructs and independent variables of disordered eating as summarized by Pennesi and Wade (2016, p. 184) and confounding autistic features.
Existing models are, however, restricted in variances of cognitive processes and related maladaptive behavioral outcomes. This is despite the role of inadequate CC for maladaptive AP, and its plausible influence on the onset of ED-related beliefs and/or behaviors (e.g., appearance investment). For instance, autistic individuals report differing social interaction and communication abilities (the AP) and, when met with the lower ability to adaptively learn from social interactions (lower CC), present secondary disordered body and eating pathology as a maladaptive resource (e.g., changing ones' appearance to “fit in”; Brede et al., 2020). Whilst this might resemble maladaptive behaviors presented in neurotypical groups, such as difficulties with social functioning precipitates a negative sense of self and disordered eating as proposed by the interpersonal model of binge eating (Wifley et al., 2000), CC serves as a “scaffold” for social behavior (socially adapted behaviors which are achieved through conscious CC strategies; Ullman and Pullman, 2015; Livingston and Happé, 2017). For example, autistic individuals may engage in masking/social camouflaging (suppressing AP behaviors) in an attempt to appear neurotypical (Lai et al., 2016; Hull et al., 2017). Although these strategies potentially facilitate social navigation, they are susceptible to rapid decline and/or maladaptation when faced with stressors (e.g., mental fatigue), and are inflexible to novel or ambiguous situations (Hull et al., 2017; Livingston and Happé, 2017). As a result, an individual may “mask” in way which adopts external, socio-cultural influences (e.g., copying anorexic values; Brede et al., 2020). This potentially contextualizes the subtle differences in the ways in which autistic individuals understand and/or experience relevant constructs, such as dieting and self-surveillance (see Kinnaird et al., 2019).
As such, it is conceivable that existing models are limited in experiential and/or construct equivalence among autistic individuals, subsequent to the lack of divergence in neurocognitive mechanisms associated with lower CC – namely, executive function (cognitive abilities in planning, inhibition and cognitive flexibility; see Hill, 2004). For instance, the dual-pathway model for bulimia nervosa (BN) suggests socio-cultural processes (e.g., thin internalization) and environmental factors (e.g., harmful media messaging) promote body dissatisfaction, manifesting ED pathology (Stice, 2001). Whilst this may be the case among autistic individuals, it is, instead, subsequent to presenting deficits in executive function and theory of mind which alters social information processing (e.g., difficulties with interpreting societal messaging) and thinking styles (e.g., literal, black and white thinking; Hill, 2004; Mazza et al., 2017; Kalandadze et al., 2018), manifesting disordered body and eating beliefs – “She takes things as absolutely true and cannot cope with nuances – ‘If I'm not thin then I'm fat and horrible', with nothing in between” (Brede et al., 2020, p. 4289).
Both internal and external sources therefore moderate CC processes and AP maladaptation (Livingston and Happé, 2017), similar to the tripartite influence model of body dissatisfaction and disordered eating (van den Berg et al., 2002; Keery et al., 2004; Yamamiya et al., 2008) which proposes external/environmental factors (e.g., media, family) to promote maladaptation (e.g., thin internationalization), manifesting negative outcomes (e.g., body dissatisfaction, disordered eating). However, what is unique to the autistic experience is environmental accommodation, where one's immediate environment may facilitate or impede CC, thereby moderate AP maladaptation (Johnson et al., 2015). More specifically, autistic individuals experience certain environments negatively, as they contain increasing demands (e.g., requires social interaction, sensory overload) which directly induces lower CC and, therefore, AP maladaptation (Livingston and Happé, 2017; Kerr-Gaffney et al., 2020). In turn, this potentially elicits negative emotional consequences (e.g., impacted sense of self, emotional dysregulation) which, as a result, reinforces ED-related behaviors/coping strategies (Mansour et al., 2016; Brede et al., 2020). For example, Kinnaird et al. (2019) found autistic individuals presented ED behaviors as a way of dealing with communication difficulties during social interactions, as well as sensory issues during mealtimes. Although these findings are preliminary, we argue that this highlights nuances in current correlates, predictors and consequences for EDs.
An impetus for defining and subsequently describe the confounding autistic experience of EDs was to illuminate current gaps in the ED literature. Existing theory remains to lack conceptual variation in cognition and behavior and focuses on a pathological rather an inclusive view of autism, making it difficult to explore the influence of ED-related independent variables (e.g., weight and shape concerns) within this population. We hypothesize that autistic individuals will understand and/or experience theoretical constructs, such as body dissatisfaction and internalization, differently to neurotypical groups. Taken together, this suggests testing the applicability and acceptability of existing models using a mixed methods design. We therefore propose a current, actionable, and accessible framework which enhances inclusive ED theory and practice and follows guidelines for conducting research with the autism community (see Gowen et al., 2019).
As a contextual factor, researchers may test the Acceptance Model of Intuitive Eating (Augustus-Horvath and Tylka, 2011) through four stages. First, scholars may investigate how constructs within a model (e.g., intuitive eating) are experienced among autistic individuals using a qualitative design, both in non-clinical (e.g., Kinnaird et al., 2019) and clinical settings (e.g., Barraclough et al., 2019). Second, translate and validate an existing measure (e.g., Intuitive Eating Scale-2; Tylka and Kroon van Diest, 2013) through psychometric testing (e.g., exploratory to confirmatory factor analysis) among both autistic and neurotypical samples (see Swami and Baron, 2019). This is with the aim to determine reliability and validity – in particular, its idiomatic and experiential equivalence – within this population. In doing so, this addresses the lack of validated measures for autistic individuals and may promote positive outcomes (e.g., reduce mis- or under-diagnosis). As recommended in the MRC framework (Campbell et al., 2000; Skivington et al., 2021), development should be carried out prior to systematically developing an intervention. Thus, the third stage involves identifying or developing theory through examining modeling processes and outcomes using structural equation modeling (e.g., Oh et al., 2012). This informs the fourth and final stage, which involves evaluating the efficacy of an existing programme which has been previously found to improve ED outcomes (e.g., Eat for Life; Bush et al., 2014). Alternatively, researchers may develop an adapted intervention which responds to ASD literature. For example, incorporating intuitive eating with enhancing interoceptive task performance among autistic individuals (e.g., ADIE; see Quadt et al., 2021). This should include testing their (i) feasibility (piloting), (ii) efficacy (evaluation), and (iii) effectiveness (implementation) (see Campbell et al., 2000; Skivington et al., 2021). We call for developments to be made with an approach which is sensitive to the autistic experience, by adequately promoting community research involvement (see Pickard et al., 2021) and responding to the ASD literature (e.g., Brede et al., 2020). Overall, we argue this will determine whether current screening tools and interventions effectively translate to this population, however considering cognitive and behavioral variances; and/or developments specific to this population are necessary.
The autistic experience of EDs receives little theoretical or empirical investigation, despite autistic individuals presenting poorer and long-enduring outcomes (Westwood and Tchanturia, 2017). Autism-ED research is limited in acknowledging the nuances of the autistic experience in two ways: first, research lacks accounting for its heterogenic nature more generally and/or its entirety (e.g., development, presentation); second, despite it not being limited to a specific ED diagnostic category and/or severity level, research predominantly refers to restrictive eating pathology (Brede et al., 2020). Furthermore, existing ED theory has yet to be extended to feeding disorders such as ARFID, despite its prevalence among both neurotypical and neurodiverse groups – particularly children and adolescents (Nicely et al., 2014; Farag et al., 2021). Consequently, current understanding limits engagement and advancement of neurodiverse detection and intervention practices. By drawing inferences from autism-ED literature, this Opinion highlights how the autistic experience confounds existing models of EDs: the AP is be expressed in a way which resembles typical ED symptom profile; however, it is, instead, maladaptive AP features and impaired CC (or cognitive ability) which manifest ED pathology. As this is likely to be relevant to other neurodiverse phenotypes (e.g., ADHD), the potential utility of reframing existing models for EDs from a neurodiverse perspective may ultimately advance research and clinical practice concerning heterogeneity, and enhance inclusive assessment, prevention and treatment applications. This Opinion therefore aims to serve as a catalyst for future development, as we call for research and practice to integrate the autistic experience into existing models for EDs through an integrating framework.
PL and LC contributed to writing and editing the manuscript. Both authors contributed to the article and approved the submitted version.
PL was employed by the British Association for Counselling and Psychotherapists.
The remaining author declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
American Psychiatric Association [APA]. (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edn. American Psychiatric Publishing, Inc. doi: 10.1176/appi.books.9780890425596
Augustus-Horvath, C. L., and Tylka, T. L. (2011). The acceptance model of intuitive eating: a comparison of women in emerging adulthood, and middle adulthood. J. Couns. Psychol. 58, 110–125. doi: 10.1037/a0022129
Babbott, K. M., Cavadino, A., Brenton-Peters, J., Consedine, N. S., and Roberts, M. (2022). Outcomes of intuitive eating interventions: a systematic review and meta-analysis. Eat. Disord. 1–31. doi: 10.1080/10640266.2022.2030124
Baron-Cohen, S., Wheelwright, S., Skinner, R., Martin, J., and Clubley, E. (2001). The autism-spectrum quotient (AQ): evidence from asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. J. Autism Dev. Disord. 31, 5–17. doi: 10.1023/A:1005653411471
Barraclough, E. L., Hay-Smith, J. C., Boucher, S. E., Tylka, T. L., and Horwath, C. C. (2019). Learning to eat intuitively: a qualitative exploration of the experience of mid-age women. Health Psychol. Open 6, 1–8. doi: 10.1177/2055102918824064
Brede, J., Babb, C., Jones, C., Elliott, M., Zanker, C., Tchanturia, K., et al. (2020). “For Me, the Anorexia is Just a Symptom, and the Cause is the Autism”: Investigating Restrictive Eating Disorders in Autistic Women. J. Autism Dev. Disord. 50, 4280–4296. doi: 10.1007/s10803-020-04479-3
Bush, H. E., Rossy, L., Mintz, L. B., and Schopp, L. (2014). Eat for life: a work site feasibility study for a novel mindfulness-based intuitive eating intervention. Am. J. Health Promot. 28, 380–388. doi: 10.4278/ajhp.120404-QUAN-186
Campbell, M., Fitzpatrick, R., Haines, A., Kinmonth, A. L., Sandercock, P., Spiegelhalter, D., et al. (2000). Framework for the design and evaluation of complex interventions to improve health. Br. Med. J. 321, 694–696. doi: 10.1136/bmj.321.7262.694
Farag, F., Sims, A., Strudqick, K., Carrasco, J., Waters, A., Ford, V., et al. (2021). Avoidant/restrictive food intake disorder and autism spectrum disorder: clinical implications for assessment and management. Dev. Med. Child Neurol. 64, 176–182. doi: 10.1111/dmcn.14977
Geurts, H. M., Sinzig, J., Booth, R., and Happ,é, F. (2014). Neurophysiological heterogeneity in executive functioning in autism spectrum disorders. Int. J. Dev. Disabil. 60, 155–162. doi: 10.1179/2047387714Y.0000000047
Gowen, E., Taylor, R., Bleazard, T., Greenstein, A., Baimbridge, P., and Poole, D. (2019). Guidelines for conducting research studies with the autism community. Autism Policy Pract. 2, 29–45.
Happé, F., and Frith, U. (2006). The weak coherence account: detail-focused cognitive style in autism spectrum disorders. J. Autism Dev. Disord. 36, 5–25. doi: 10.1007/s10803-005-0039-0
Happé, F., Ronald, A., and Plomin, R. (2006). Time to give up on a single explanation for autism. Nat. Neurosci. 9, 1218–1220. doi: 10.1038/nn1770
Hatfield, T. R., Brown, R. F., Giummarra, M. J., and Lenggenhager, B. (2019). Autism spectrum disorder and interoception: Abnormalities in global integration? Autism 23, 212–222. doi: 10.1177/1362361317738392
Hill, E (2004). Executive dysfunction in autism. Trends Cogn. Sci. 8, 26–32. doi: 10.1016/j.tics.2003.11.003
Huke, V., Turk, J., Saeidi, S., Kent, A., and Morgan, J. F. (2013). Autism spectrum disorders in eating disorder populations: a systematic review. Eur. Eat. Disord. Rev. 21, 345–351. doi: 10.1002/erv.2244
Hull, L., Petrides, K. V., Allison, C., Smith, P., Baron-Cohen, S., Lai, M.-C., et al. (2017). “Putting on my best normal”: Social camouflaging in adults with autism spectrum conditions. J. Autism Dev. Disord. 47, 2519–2534. doi: 10.1007/s10803-017-3166-5
Johnson, M. H., Jones, E. J. H., and Gliga, T. (2015). Brain adaptation and alternative developmental trajectories. Dev. Psychopathol. 27, 425–442. doi: 10.1017/S0954579415000073
Kalandadze, T., Norbury, C., Naerland, T., and Naess, K. B. (2018). Figurative language comprehension in individuals with autism spectrum disorder: a meta-analytic review. Autism 22, 99–117. doi: 10.1177/1362361316668652
Keery, H., van den Berg, P., and Thompson, J. K. (2004). An evaluation of the tripartite model influence model of body dissatisfaction and eating disturbance with adolescent girls. Body Image 1, 237–251. doi: 10.1016/j.bodyim.2004.03.001
Kerr-Gaffney, J., Halls, D., Harrison, A., and Tchanturia, K. (2020) 11. Exploring relationships between autism spectrum disorder symptoms eating disorder symptoms in adults with anorexia nervosa: a network approach. Front. Psychiatry. 1–11. doi: 10.3389/fpsyt.2020.00401
Kinnaird, E., Norton, C., Pimblett, C., Stewart, C., and Tchanturia, K. (2019). Eating as an autistic adult: An exploratory qualitative study. PLoS ONE 14, 1–17. doi: 10.1371/journal.pone.0221937
Lai, M.-C., Lombardo, M. V., Ruigrok, A. N. V., Chakrabarti, B., Auyeung, B., Szatmari, P., et al. (2016). Quantifying and exploring camouflaging in men and women with autism. Autism 21, 690–702. doi: 10.1177/1362361316671012
Landry, O., and Chouinard, P. A. (2016). Why we should study the broader autism phenotype in typically developing populations. J. Cogn. Dev. 17, 584–595. doi: 10.1080/15248372.2016.1200046
Lenroot, R. K., and Yeung, P. K. (2013). Heterogeneity within autism spectrum disorders: what have we learned from neuroimaging studies? Front. Hum. Neurosci. 7, 1–16. doi: 10.3389/fnhum.2013.00733
Lever, A. G., and Geurts, H. M. (2016). Psychiatric co-occuring symptoms and disorders in young, middle-aged and older adults with autism spectrum disorder. J. Autism Dev. Disord. 46, 1916–1930. doi: 10.1007/s10803-016-2722-8
Livingston, L. A., and Happé, F. (2017). Conceptualising compensation in neurodevelopmental disorders: reflections from autism spectrum disorder. Neurosci. Biobehav. Rev. 80, 729–742. doi: 10.1016/j.neubiorev.2017.06.005
Lyon, M. E., Chatoor, I., Atkins, D., Silber, T., Mosimann, J., and Gray, J. (1997). Testing the hypothesis of a multidimensional model of anorexia nervosa in adolescents. Adolescence 32, 101–111.
Mansour, S., Rozenblat, V., Fuller-Tyszkiewicz, M., Paganini, C., Treasure, J., and Krug, I. (2016). Emotions mediate the relationship between autistic traits and disordered eating: a new autistic-emotional model for eating pathology. Psychiatry Res. 245, 119–126. doi: 10.1016/j.psychres.2016.08.021
Mazza, M., Mariano, M., Peretti, S., Masedu, F., Pino, M. C., and Valenti, M. (2017). The role of theory of mind on social information in children with autism spectrum disorders: a mediation analysis. J. Autism Dev. Disord. 47, 1369–1379. doi: 10.1007/s10803-017-3069-5
Murray, A. L., Booth, T., McKenzie, K., Kuenssberg, R., and O'Donnell, M. (2014). Are autistic traits measures equivalently in individuals with and without an autism spectrum disorder: An invariance analysis of the autism spectrum quotient short form. J. Autism Dev. Disorders 44, 55–64. doi: 10.1007/s10803-013-1851-6
Nicely, T. A., Lane-Loney Masciulli, E., Hollenbeak, C. S., and Ornstein, R. M. (2014). Prevalence and characteristics of avoidant/restrictive food intake disorder in a cohort of young patients in day treatment for eating disorders. J. Eat. Disord. 2, 21. doi: 10.1186/s40337-014-0021-3
Nicolaidis, C., Raymaker, D. M., McDonald, K. E., Lund, E. M., Leotti, S., Kapp, S. K., et al. (2020). Creating accessible survey instruments for use with autistic adults and people with intellectual disability: lessons learned and recommendations. Autism Adulthood, 2, 61-76. doi: 10.1089/aut.2019.0074
Oh, K. H., Wiseman, M. C., Hendrickson, J., Phillips, J. C., and Hayden, E. W. (2012). Testing the acceptance model of intuitive eating with college women athletes. Psychol. Women Q. 36, 88–89. doi: 10.1177/0361684311433282
Pennesi, J.-L., and Wade, T. D. (2016). A systematic review of the existing models of disordered eating: Do they inform the development of effective interventions. Clin. Psychol. Rev. 43, 175–192. doi: 10.1016/j.cpr.2015.12.004
Pickard, H., Pellicano, E., den Houting, J., and Crane, L. (2021). Participatory autism research: early career and established researchers' views and experiences. Autism 26, 75–87. doi: 10.1177/13623613211019594
Pugliese, C. E., Anthony, L., Strang, J. F., Dudley, J., Wallace, G. L., and Kenworthy, L. (2015). Increasing adaptive behaviour skill deficits from childhood to adolescence in autism spectrum disorder: role of exective function. J. Autism Dev. Disord. 45, 1579–1587. doi: 10.1007/s10803-014-2309-1
Pugliese, C. E., Anthony, L. G., Strang, J. F., Dudley, K., Wallace, G. L., Naiman, D. Q., et al. (2016). Longitudinal examination of adaptive behaviour in autism spectrum disorders: influence of executive function. J. Autism Dev. Disord. 46, 467–477. doi: 10.1007/s10803-015-2584-5
Quadt, L., Garfinkel, S. N., Mulcahy, J. S., Larsson, D. E., Silva, M., Jones, A., et al. (2021). Interoceptive training to target anxiety in autistic adults (ADIE): A single-centre, superiority randomised controlled trial. E-Clin. Med. 39, 101042. doi: 10.1016/j.eclinm.2021.101042
Sarovic, D (2021). A unifying theory for autism: The pathogenetic triad as a theoretical framework. Front. Psychiatry. 12:767075. doi: 10.3389/fpsyt.2021.767075
Schmidt, U., Adan, R., Bohm, I., Campbell, I. C., Dingemans, A., Ehrlich, S., et al. (2016). Eating disorders: the big issue. Lancet Psychiatry 3, 313–315. doi: 10.1016/S2215-0366(16)00081-X
Schmidt, U., and Treasure, J. (2006). Anorexia nervosa: valued and visible. a cognitive-interpersonal maintenance model and its implications for research and practice. Br. J. Clin. Psychol. 45, 343–266. doi: 10.1348/014466505X53902
Skivington, K., Matthews, L., Simpson, S. A., Craig, P., Baird, J., Blazby, J. M., et al. (2021). A new framework for developing and evaluating complex interventions: update of medical research council guidance. BMJ 374, 1–11. doi: 10.1136/bmj.n2061
Stice, E (2001). A prospective test of the dual-pathway model of bulimic pathology: mediating effects of dieting and negative effect. J. Abnorm. Psychol. 110, 124–135. doi: 10.1037/0021-843X.110.1.124
Sucksmith, E., Roth, I., and Hoekstra, R. A. (2011). Autistic traits below the clinical threshold: re-examining the broader autistic phenotype in the 21st century. Neuropsychol. Rev. 21, 360–389. doi: 10.1007/s11065-011-9183-9
Swami, V., and Baron, D. (2019). Translation and validation of body image instruments: challenges, good practice guidelines, and reporting recommendations for test adaptation. Body Image 31, 204–220. doi: 10.1016/j.bodyim.2018.08.014
Tchanturia, K., Smith, E., Weineck, F., Fidanboylu, E., Kern, N., Treasure, J., et al. (2013). Exploring autistic trats in anorexia: a clinical study. Mol. Autism 4, 44. doi: 10.1186/2040-2392-4-44
Tchanturia, K., Smith, K., Glennon, D., and Burhouse, A. (2020). Towards an improved understanding of the anorexia nervosa and autism spectrum comorbidity: PEACE pathway implementation. Front. Psychiatry. 11, 1–7. doi: 10.3389/fpsyt.2020.00640
Treasure, J., and Schmidt, U. (2013). The cognitive-interpersonal maintenance model of anorexia nervosa revisited: a summary of the evidence for cognitive, socio-emotional and interpersonal predisposing and perpetuating factors. J. Eat. Disord. 1, 13. doi: 10.1186/2050-2974-1-13
Trevisan, D. A., Parker, T., and McPartland, J. C. (2012). First-hand accounts of interoceptive difficulties in autistic adults. J. Autism Dev. Disord. 51, 3483–3491. doi: 10.1007/s10803-020-04811-x
Tribole, E., and Resch, E. (2003). Intuitive Eating: A Revolutionary Program that Works. New York, NY: St. Martin's Griffin.
Tylka, T. L., and Kroon van Diest, A. M. (2013). The intuitive eating scale-2: item refinement and psychometric evaluation with college women and men. J. Counsel. Psychol. 60, 137–153. doi: 10.1037/a0030893
Uljarevic, M., Baranek, G., Vivanti, G., Hedley, D., Hudry, K., and Lane, A. (2017). Heterogeneity of sensory features in autism spectrum disorder: challenges and perspectives for future research. Autism Res. 10, 703–710. s doi: 10.1002/aur.1747
Ullman, M. T., and Pullman, M. Y. (2015). A compensatory role for declarative memory in neurodevelopmental disorders. Neurosci. Biobehav. Rev. 51, 205–222. doi: 10.1016/j.neubiorev.2015.01.008
van den Berg, P., Thompson, J. K., Obremski-Brandon, K., and Coovert, M. (2002). The tripartite influence model of body image and eating disturbance: a covariance structure modeling investigation testing the mediational role of appearance comparison. J. Psychosom. Res. 53, 1007–1020. doi: 10.1016/S0022-3999(02)00499-3
Vuillier, L., Carter, Z., Teizeira, A. R., and Moseley, R. L. (2020). Alexithymia may explain the relationship between autistic traits and eating disorder psychopathology. Mol. Autism 11, 63. doi: 10.1186/s13229-020-00364-z
Westwood, H., and Tchanturia, K. (2017). Autism spectrum disorder in anorexia nervosa: an updated literature review. Curr. Psychiatry Rep. 19, 41. doi: 10.1007/s11920-017-0791-9
Wifley, D. E., MacKenzie, K. R., Welch, R., Ayers, V. E., and Weissman, M. M. (2000). Interpersonal Psychotherapy for Group. New York, NY: Basic Books.
Williamson, D. A., White, M. A., York-Crowe, E., and Stewart, T. M. (2004). Cognitive-behavioural theories of eating disorders. Behav. Modif. 28, 711–738. doi: 10.1177/0145445503259853
Keywords: Autism Spectrum Disorder (ASD), eating behaviour and eating disorder (ED), cognitive-behavioural theory, theoretical model, framework, neurodiversity
Citation: Longhurst P and Clark L (2022) Integrating the Autistic Experience Into Existing Models for Disordered Eating. Front. Psychol. 13:926415. doi: 10.3389/fpsyg.2022.926415
Received: 22 April 2022; Accepted: 24 May 2022;
Published: 21 June 2022.
Edited by:
Edward A. Selby, Rutgers, The State University of New Jersey, United StatesReviewed by:
Gennaro Catone, Suor Orsola Benincasa University, ItalyCopyright © 2022 Longhurst and Clark. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Phaedra Longhurst, cGhhZWRyYS5sb25naHVyc3RAYmFjcC5jby51aw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.