
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychol., 29 September 2022
Sec. Psycho-Oncology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.926383
Posttraumatic growth (PTG) has been correlated with coping style among patients with breast cancer. However, to date, there is no consensus on the extent to which coping style is associated with PTG in patients with breast cancer. Therefore, we performed a meta-analysis to quantitatively synthesize previous findings. Based on the PRISMA method, this study employed a random effects model using the Stata software (version 16.0) to calculate the pooled correlation coefficient and examined a range of moderators: cancer stage, publication type, participants’ age, and coping style measurement tools. Relevant studies, published from inception to 9 March 2022, were identified through a systematic search in PubMed, Embase, Web of Science, PsycINFO, WANFANG DATA, Chinese National Knowledge Infrastructure (CNKI), and China Science and Technology Journal Database (VIP) databases. Finally, 20 studies involving 3,571 breast cancer patients were included in this investigation. The results showed a high positive relation between confrontation coping and PTG and a moderate positive relation between avoidance coping and PTG (confrontation: r = 0.456; avoidance: r = 0.291). Additionally, a moderate negative relation was identified between acceptance–resignation coping and PTG (r = –0.289). Publication type and coping style measurement tools moderated the relation between coping style and PTG among breast cancer patients. The findings indicated that breast cancer patients should either confront the disease or avoid coping with it according to their disease state, which would facilitate better growth. More studies, especially, large prospective studies, are warranted to verify our findings.
Systematic review registration: [https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022319107], identifier [CRD42022319107].
Breast cancer is amongst the most common malignant tumors in women worldwide (Ghoncheh et al., 2016). According to global cancer statistics, breast cancer was the most commonly diagnosed cancer in 2020, with an incidence rate of 11.7% and a mortality rate of 6.9% (Sung et al., 2021). With the improvement of medical technology, the breast cancer survival rate has gradually increased (Maajani et al., 2019). However, breast loss (mastectomy), surgical chest scars, hair loss, and sexual dysfunction caused by chemotherapy sometimes result in anxiety, depression, despair, fear, etc., which severely impact cancer survivors’ quality of life (Schmid-Büchi et al., 2011; Denieffe et al., 2014; Soriano et al., 2021). In contrast, a few studies have reported that patients with cancer often experience positive psychological changes in the course of their cancer trajectory, known as posttraumatic growth (PTG) (Ýnan and Üstün, 2014; Casellas-Grau et al., 2017; Mostarac and Brajković, 2022).
Posttraumatic growth is defined as the result of an individual’s struggle with a traumatic event (Tedeschi and Calhoun, 2004). Unlike responses to minor or everyday stressors and normal growth and developmental processes (Linley and Joseph, 2004), PTG is an individual’s effort to control the impact of trauma on their lives and attempts to cope with the trauma related experiences and consequences (Tedeschi and Calhoun, 2004). A common used assessment tool is the Posttraumatic Growth Inventory (PTGI) (Tedeschi and Calhoun, 1996), which includes the five dimensions of relating to others, new possibilities, personal strength, spiritual change, and appreciation of life. It comprises 21 items rated on a 6-point Likert-type scale ranging from 0 (I did not experience this change as a result of my crisis) to 5 (I experienced this change to a very great degree). The score ranges from 0 to 105, with high scores indicating positive growth.
In the past few years, many breast cancer patients have reported experiencing PTG (Lelorain et al., 2010; Paredes and Pereira, 2018; Karimzadeh et al., 2021). Furthermore, breast cancer patients have higher PTG levels than healthy people (Bourdon et al., 2019). Researchers have explored potential growth promoters and identified diverse coping styles as a significant psychological adjustment factor to promote faster PTG among breast cancer patients (Buyukasik-Colak et al., 2012; Li et al., 2016; Bellur et al., 2018).
Coping style, or coping strategy, refers to behavioral and cognitive efforts of individuals in response to the environment, adverse life events, or internal needs to manage the internal and external requirements produced by people–situation interactions (Folkman et al., 1986). Feifel et al. (1987) declared that individuals mainly adopt three types of coping methods: confrontation coping, acceptance–resignation coping, and avoidance coping when encountering traumatic events. Among them, confrontation coping is a positive coping style, which implies that the individual is optimistic, rational, non-evasive, prudent, and considers effective methods and strategies to adjust the body and mind to promote health (Kroemeke et al., 2017; Liu, 2018). Acceptance–resignation coping is a negative coping style, which implies that in the face of traumatic events, individuals often feel helpless, disheartened, and negative and lose confidence in treatment and recovery. As for avoidance coping, different research results have different conclusions. A few studies have shown that through avoidance coping style, individuals can divert attention from the disease, suspend conflicts, reduce psychological barriers, and maintain emotional stability to obtain positive results and better quality of life (Ando et al., 2011; Lee et al., 2017); therefore, avoidance coping is considered a positive coping style. However, certain researchers believe that individuals adopt avoidance coping deliberately or even to avoid the impact of traumatic events, which is not conducive to treatment and recovery (Tong et al., 2013); thus, avoidance coping is considered a negative coping mechanism.
Many researchers have investigated the relation between coping style and PTG among patients with breast cancer, and the coping style–PTG relation is still in literature a controversial topic. A few studies have shown a close relation between the two (Ma, 2014; Cheng and Zhang, 2015), several researchers have identified a moderate relation between them (Lisica et al., 2019; Tu et al., 2020), and a few others have suggested a weak relation (Svetina and Nastran, 2012; Romeo et al., 2019). According to Zhang et al. (2017) and Zhao (2021), there is no significant relation between coping style and PTG. One of the reasons for this debate is the small sample size of individual studies; thus, this study used a meta-analysis to integrate previous empirical studies on the relation between coping style and PTG to evaluate the magnitude of the relation between the two factors, providing evidence for whether coping style is associated with PTG.
Additionally, we examined whether the coping style–PTG relation in patients with breast cancer was moderated by certain factors, such as cancer stage, publication type, participants’ age, and coping style measurement tools. First, based on the psychological theory proposed by Janoff-Bulman (2006), patients with advanced cancer experience a greater degree of disruption and psychological stress than those with early stage cancer because of treatment side effects. With the increase in psychological distress, they often adopt a negative coping mechanism, which is not conducive to PTG. Therefore, this relation may vary based on the cancer stage. Second, studies with significant results are more likely to be published, which may tempt authors to exaggerate the true relation between variables (Sterne et al., 2000). To this end, we included dissertations that were not officially published in journals and divided the publication types into two categories, journal and dissertation, to examine the moderating effect of publication type on the relation between coping style and PTG. Third, previous studies have identified that younger breast cancer survivors experience a deeper impact from cancer, reporting greater emotional distress and poorer psychological adjustment than older survivors (Kroenke et al., 2004; Howard-Anderson et al., 2012). Thus, the relation between coping style and PTG in patients with breast cancer may differ based on age. Finally, in terms of the measurement of coping style, the Medical Coping Modes Questionnaire (MCMQ) (Feifel et al., 1987), the abbreviated situational version of the COPE Inventory (Brief COPE) (Carver, 1997), and the Mini-Mental Adaptation to Cancer Scale (Mini-MAC) (Watson et al., 1994) are widely used. As the number of items and dimensions of each scale are different, coping style measurement tools may be a factor that could moderate the relation between coping style and PTG in patients with breast cancer.
To sum up, this study conducted a meta-analysis to deeply investigated the relation between coping style and PTG in patients with breast cancer and examined whether this relation was moderated by (a) cancer stage, (b) publication type, (c) participants’ age, and (d) coping style measurement tools.
The current systematic review and meta-analysis was conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) 2020 guidelines (Page et al., 2021). Moreover, the protocol has been registered in PROSPERO (ID: CRD 42022319107)—a prospective international registry of systematic reviews.
Relevant literature was retrieved by systematically searching PubMed, Embase, Web of Science, PsycINFO, WANFANG DATA, Chinese National Knowledge Infrastructure (CNKI), and China Science and Technology Journal Database (VIP) databases for studies from inception to 9 March 2022. Search terms used for breast cancer primarily included: “Breast Neoplasms,” “Breast Tumor,” “Breast Tumors,” “Breast Carcinoma,” and “Breast Carcinomas.” Search terms used for PTG primarily included: “Posttraumatic Growth, Psychological,” “Psychological Posttraumatic Growth,” and “Post-traumatic Growth, Psychological.” Search terms employed for coping style mainly included: “Coping Styles,” “Coping Mode,” “Coping Strategy,” “Coping Strategies,” “Coping Behaviors,” and “Coping Skills.” Thereafter, those search terms were combined using appropriate Boolean operators. A detailed search strategy for PubMed is available in the Supplementary material. Furthermore, the reference lists of retrieved articles were manually scrutinized to identify potentially relevant studies.
Two reviewers independently screened the literature, applying the following selection criteria for articles. (1) It reported either the Pearson correlation coefficient r, or F, t, χ2, and β values that could be converted to r values. (2) PTG measurement instruments were limited to the PTGI or a revised scale based on the PTGI. (3) Coping style measurement tools were limited to scales that could distinguish one or more of the coping strategies of confrontation coping, avoidance coping, and acceptance–resignation coping, such as the MCMQ, the Brief COPE, and the Mini-MAC. (4) Participants were patients with histopathologically diagnosed breast cancer. (5) When duplicate publications reporting on the same participants were identified, the primary study was selected.
The exclusion criteria were (1) articles not written in English or Chinese language; (2) conference reports; (3) low-quality studies as assessed using the 9-item Joanna Briggs Institution Critical Appraisal Checklist (Munn et al., 2015); (4) studies with obvious data errors.
Two researchers independently collected the data using a purpose-designed form, and in case of disagreements, a consensus was achieved through discussion. We coded the collected studies for the following information: author information, publication year, country, publication type, cancer stages 1–4, participant characteristics, sample size, correlation coefficients between coping style and PTG, and instruments used to measure coping-style level. For the correlation coefficient entry, if studies did not report correlation coefficients r but reported F, t, χ2, and β values, according to corresponding formula, they were transformed to r values: r = , r = , r = r = β × 0.98 + 0.05 (β ≥ 0); r = β × 0.98 – 0.05 (β < 0) [–0.5 < β < 0.5] (Card, 2012).
The methodological quality of all included studies was independently assessed by two researchers using the 9-item Joanna Briggs Institution Critical Appraisal Checklist (Munn et al., 2015). These items are mainly described from nine aspects, including target population, sampling method, sample size, response rate, etc. Relevant details are provided in Supplementary material. “Yes,” “no,” “unclear,” and “not applicable” were the answer options for each item, with 1 point for “yes” and 0 points for the rest. Higher scores reported better methodological quality. Furthermore, any doubt or disagreement was resolved through centralized discussion (among at least three people) or by soliciting the opinions of third-party experts. We considered all included studies to be of moderate to high quality (total score of ≥ 6) (Table 1).
The pooled correlation coefficients and their corresponding 95% confidence intervals (CIs) between PTG and confrontation coping, avoidance coping, and acceptance–resignation coping were calculated using the inverse variance method (Moles, 2009). Specifically, we applied Fisher’s z-transformation to r, weighted based on the sample size with 95% CIs: Z=0.5 × ln [(1 + r)/(1 – r)], where the variance of Z is VZ = 1/n – 3, and the standard deviation of Z is SEZ=. As suggested by Lipsey and Wilson (2001), effect size r values of 0.10, 0.25, and 0.40 correspond to low, moderate, and high correlations, respectively. Heterogeneity across studies was assessed using Cochran’s Q and I2 statistics (Higgins et al., 2003). A p of <0.05 or I2 of >75% indicated that the between-study heterogeneity was statistically significant. Finally, a random effects model was used to calculate the summary correlation coefficient. Otherwise, the fixed effects model would be used.
Meanwhile, a significant degree of heterogeneity suggested potential moderation effects. The moderating effect analysis involved two forms. (1) When the moderating variable was a continuous variable, we used meta-regression analysis to check whether the result was significant. (2) When the moderating variable was a categorical variable, we used subgroup analysis to test whether the result was significant. Moreover, we performed a sensitivity analysis by sequentially omitting one study for each turn to evaluate the influence of individual studies on the summary correlation coefficients and to test the robustness of the relation between PTG and confrontation coping, avoidance coping, and acceptance–resignation coping. Potential publication bias was detected using funnel plots. Additionally, Begg’s test was performed to help judge publication bias (Begg and Mazumdar, 1994). All statistical analyses were conducted using Stata software (version 16.0).
Our search strategy identified 701 studies without duplicates (Figure 1 is the PRISMA flow diagram of the study screening process). After reading titles and abstracts, full texts of 63 articles were reviewed for eligibility. Of these, 43 studies were excluded because they were conference reports (n = 17), in other language (n = 7), repeated the samples (n = 2), had poor quality (n = 1), or had insufficient data (n = 16). Finally, 20 studies were included in the meta-analysis, with a total sample size of 3,571 participants. All 20 studies reported correlation coefficients between confrontation coping and PTG. Sixteen studies reported correlation coefficients between avoidance coping and PTG. Thirteen studies reported correlation coefficients between acceptance–resignation coping and PTG. The characteristics of the included studies are summarized in Table 1. The sample size ranged from 60 to 325, and the samples included patients with breast cancer. Among the 20 studies, 2 were from Turkey and Japan each, 11 were form China, and 5 were from Slovenia, the US, Poland, Bosnia and Herzegovina, and Italy each.
As shown in Table 2, random effects models were used for the summary of three different outcomes (heterogeneity for confrontation coping: I2 = 92.5%, p < 0.001; heterogeneity for avoidance coping: I2 = 94.8%, p < 0.001; heterogeneity for acceptance–resignation coping: I2 = 97.3%, p < 0.001). The random effects model showed a high positive relation of 0.456 (95% CI [0.354, 0.548], p < 0.001) between confrontation coping and PTG, a moderate positive relation of 0.291 (95% CI [0.139, 0.429], p < 0.001) between avoidance coping and PTG, and a moderate negative relation of –0.289 (95% CI [–0.486, –0.064], p < 0.001) between acceptance–resignation coping and PTG. Moreover, the relation between coping style and PTG was stable, as the Z-value of PTG and confrontation coping, avoidance coping, and acceptance–resignation coping was 7.846 (p < 0.001), 3.677 (p < 0.001), –2.502 (p < 0.05), respectively.
First, the meta-analysis was tested by funnel plot for publication bias. Figure 2 shows that the effect sizes of the relation between PTG and confrontation coping, avoidance coping, and acceptance–resignation coping of patients with breast cancer were basically evenly distributed on both sides of the overall effect sizes, implying little publication bias. We used Begg’s test to verify this further. Begg’s rank correlation test also showed little significant bias (confrontation coping: p = 0.581; avoidance coping: p = 0.892; acceptance–resignation coping: p = 0.076). Thus, the published research articles included in this study could systematically and comprehensively represent the research population in this field. Additionally, by sequentially removing one individual study for each turn and then recalculating the summary correlation coefficients, we found that the summary correlation coefficients between coping style (confrontation coping, avoidance coping, and acceptance–resignation coping) and PTG revealed minor changes, suggesting that our results were stable.
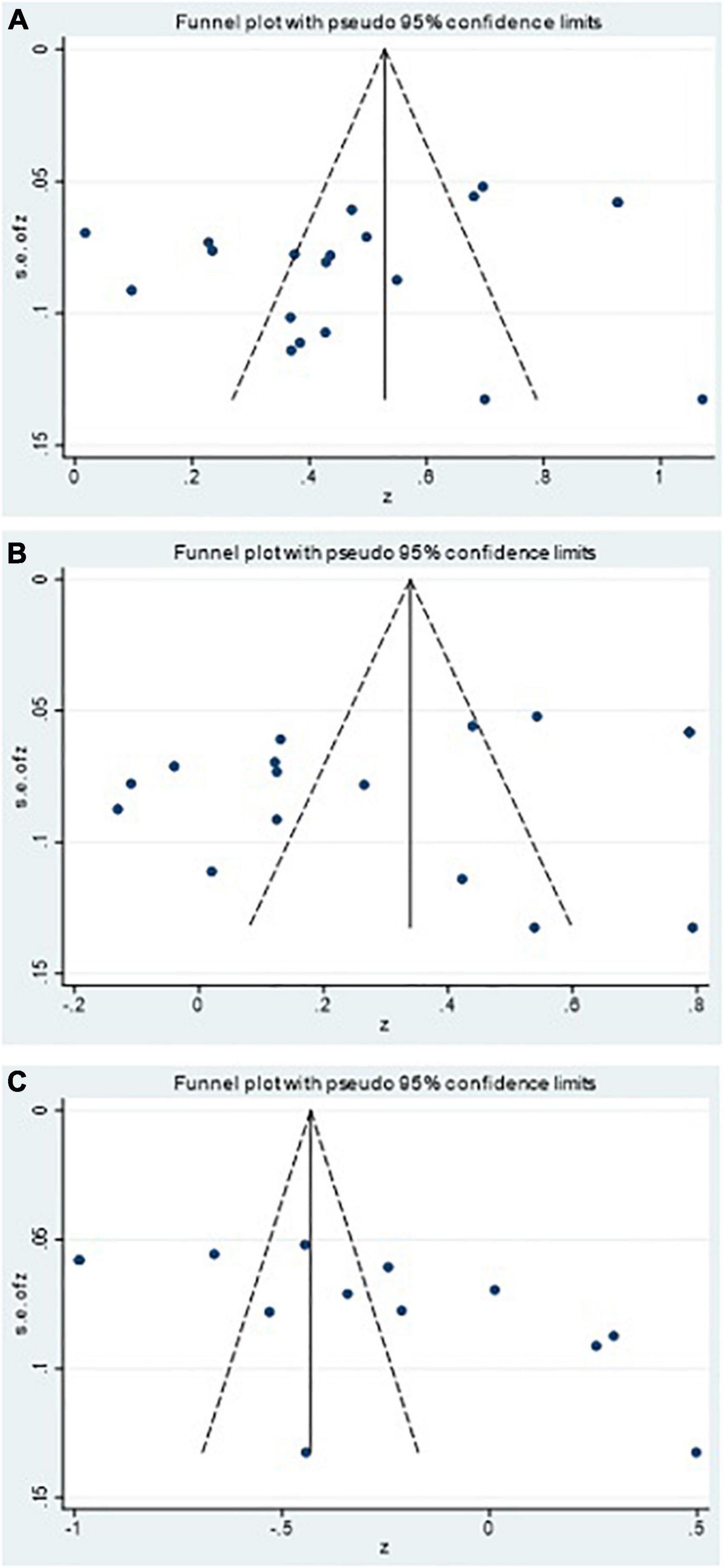
Figure 2. Funnel plots of the relation of posttraumatic growth and (A) confrontation, (B) avoidance, and (C) acceptance-resignation.
In this study, the moderating effect of four variables was tested: cancer stage, publication type, participant’s age, and tool for measuring coping style (Tables 3, 4). For the publication type, the effect of dissertation (confrontation: r = 0.666, 95% CI [0.510, 0.779]; acceptance–resignation: r = –0.678, 95% CI [–0.816, –0.468]) on PTG and confrontation coping and acceptance–resignation coping among breast cancer patients was significantly larger than that of journal articles (confrontation: r = 0.427, 95% CI [0.320, 0.523]; acceptance–resignation: r = –0.197, 95% CI [–0.416, 0.043]). Regarding the tool for measuring coping style, the MCMQ had the largest effect on breast cancer patients’ PTG and confrontation coping (r = 0.555, 95% CI [0.414, 0.669]) in comparison to the Brief COPE (r = 0.280, 95% CI [0.146, 0.403]) and the Mini-MAC (r = 0.292, 95% CI [–0.092, 0.600]). The MCMQ (r = 0.402, 95% CI [0.228, 0.551]) had a larger effect on breast cancer patients’ avoidance coping and PTG than the Mini-MAC (r = 0.032, 95% CI [–0.127, 0.190]). However, the moderating effects of cancer stage and age on coping style and PTG were not significant (all p > 0.05).
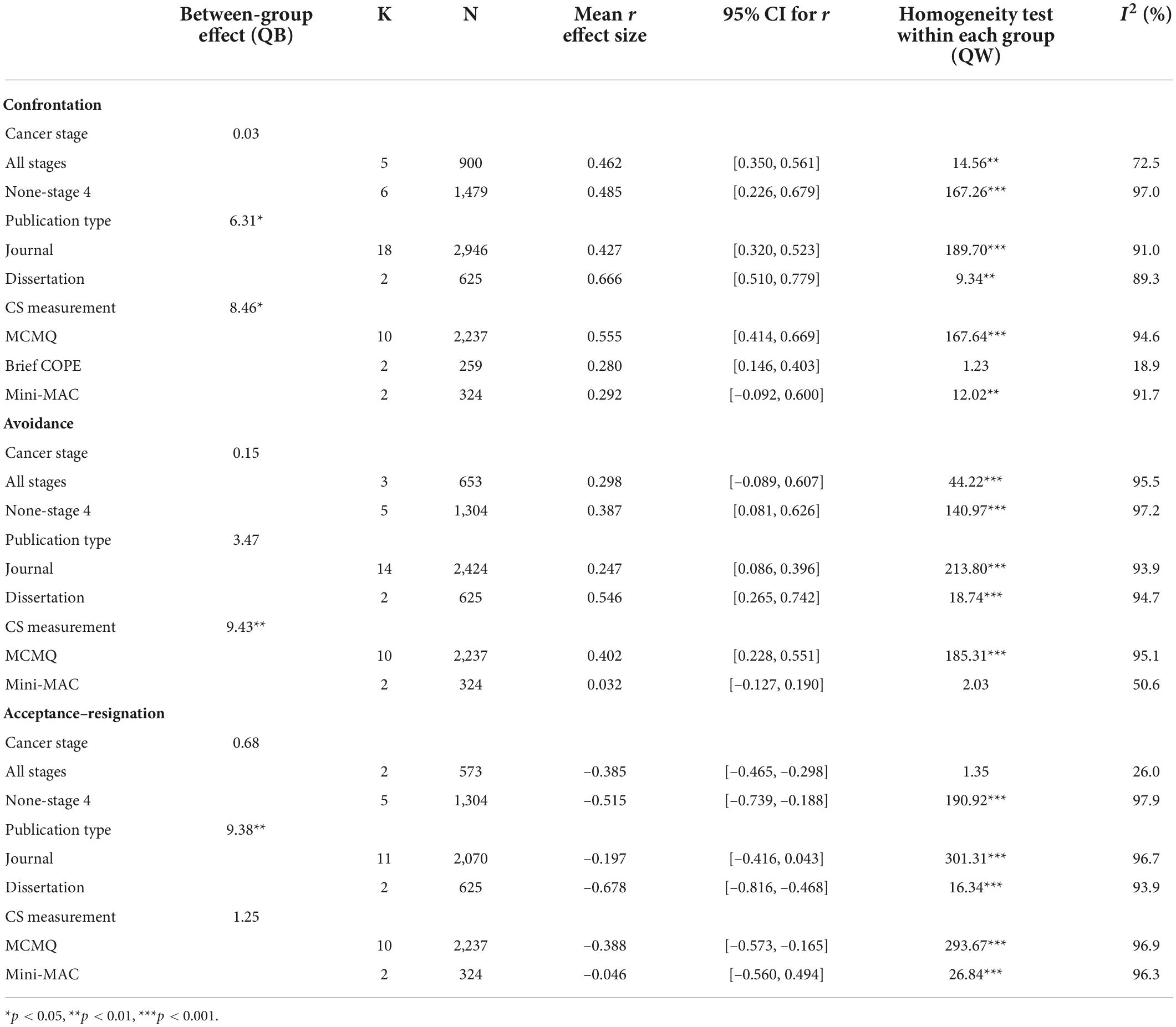
Table 3. Coping styles and posttraumatic growth (PTG): Univariate analysis of variance for moderators.
This systematic review and meta-analyses clarified for the first time the scientific discussion on the magnitude of the relation between confrontation coping and PTG and the magnitude and direction of the relation between PTG and avoidance coping and acceptance–resignation coping. The results showed a highly positive relation between confrontation coping and PTG among breast cancer patients, which was consistent with the findings of most researchers (Tomita et al., 2017; Hu et al., 2018; Liu et al., 2019). It indicated that confronting the disease positively helps boost PTG in patients with breast cancer. The results also showed a moderate positive relation between avoidance coping and PTG in patients with breast cancer, which was in line with the studies by Wang et al. (2020) and Fujimoto and Okamura (2021). It showed that avoidance coping could be seen as a positive coping style, and the process of growth after trauma in patients with breast cancer may require temporary avoidance coping. However, a few studies have suggested that avoidance coping is detrimental to long-term psychological health or attainment of a high level of PTG is unfavorable (Tong et al., 2013; Wilski and Tasiemski, 2016). Thus, more empirical research on the relation between avoidance coping and PTG among breast cancer patients is needed to verify this result. Moreover, the results of our study showed a negative relation between acceptance–resignation coping and PTG in patients with breast cancer, which was consistent with literature (Li et al., 2016; Liu, 2018; Tu et al., 2020). This result indicated that when breast cancer patients adopt acceptance–resignation coping mechanisms to cope with the disease, it is likely to have a negative physical impact. Taken together, these findings demonstrate that coping style is an important variable influencing breast cancer patients’ PTG.
Furthermore, these results showed that PTG was more strongly associated with confrontation and avoidance coping than acceptance–resignation coping was associated with PTG. In other words, positive coping styles are significantly related to breast cancer patients’ PTG. Patients generally do not immediately accept the diagnosis of breast cancer, which is a malignant tumor (Early and Moon, 2021). Thus, they can avoid a sudden mental shock and maintain emotional stability by adopting avoidance coping methods, which divert their attention from the illness (Joseph et al., 2012). However, when patients accept the cancer treatment, numerous avoidance coping methods are adopted, which may be detrimental to the treatment of the disease and the recovery of health. Patients need to actively confront the disease at this time, which can improve their chances of survival and quality of life. Therefore, psychotherapy interventions may focus on coping styles and adopt appropriate and effective coping methods according to the different stages of breast cancer patients to support their PTG.
For cancer stage, comparing studies based on stages 1–3 patients (non-stage 4 patients) to studies of only stage 4 patients, we identified that the relation between coping style (confrontation coping, avoidance coping, and acceptance–resignation coping) and PTG among breast cancer patients was not moderated by cancer stage, which was inconsistent with our previous hypothesis. This might be explained by the inclusion of an equal number of studies for stage 4 or no–stage 4. Additionally, patients at different stages of breast cancer bear different levels of psychological distress, but there might be patients with similar educational and family environments and personal character traits adopting the same coping methods (Soo and Sherman, 2015; Yeung and Lu, 2018); thus, the difference is not significant.
Meta-analyses should include unpublished studies to reduce publication bias (Sterne et al., 2000). Our study included two master’s dissertations not officially published in journals, and the results showed that publication type significantly moderated the relation between PTG and confrontation coping and acceptance–resignation coping among patients with breast cancer. However, the moderating effect on the relation between avoidance coping and PTG was not significant. The correlation coefficients between breast cancer patients’ coping style (confrontation coping and acceptance–resignation coping) and PTG reported in different types of articles were dissimilar, and the degree of correlation reported in dissertations was higher than that reported in journal articles. This difference might be due to the quality of the studies and the rigor of the review. Additionally, as we only included two master’s dissertations, the difference between the number of journal articles and the number of unpublished studies was relatively large, leading to a stronger relation between breast cancer patients’ coping style (confrontation coping and acceptance–resignation coping) and PTG in dissertations.
Meta-regression revealed that the moderating effect of age on the relation between the three coping styles and PTG in breast cancer patients was not significant, which was not consistent with the result of a previous study (Boyle et al., 2017). The reason for this result might be that the majority of the study population we included were middle-aged breast cancer patients, with a small age span. Hence, the relation between the two was not significantly different. Additionally, breast cancer comprises multiple chronic traumas rather than a single event. For different age stages of patients, the diagnosis of cancer may be the trauma or difficult cancer treatment may be the trauma (Tomita et al., 2017). Thus, in an individual case of fighting cancer, breast cancer patients at different age stages may adopt the same coping strategies according to different types of trauma, thereby leading to less variation in the relation between these two variables.
The relation between coping style (confrontation coping and avoidance coping) and PTG in patients with breast cancer was moderated by coping style measurement tools. However, the moderating effect on the relation between acceptance-resignation coping and PTG was not significant. The relation between confrontation coping and PTG was higher when the coping style was measured with the MCMQ than with the Mini-MAC and Brief COPE. The relation between avoidance coping and PTG was higher when the coping style was measured with the MCMQ than with the Mini-MAC. The reason for the difference might be that, on the one hand, each scale is divided into different dimensions and items, and on the other hand, the reliability and validity of each scale are different (Cronbach’s α of the MCMQ, Brief COPE, and Mini-MAC are 0.660–0.700, 0.500–0.900, and 0.620–0.870, respectively) (Feifel et al., 1987; Watson et al., 1994; Carver, 1997). Thus, the MCMQ was stable and balanced to a certain extent, whereas the Mini-MAC and Brief COPE had problems, such as unstable and unbalanced factor attribution of certain items. Therefore, the MCMQ can better reflect the relation between breast cancer patients’ coping style (confrontation coping and avoidance coping) and PTG compared to other scales.
Unlike previous studies on the relation between coping style and PTG among patients with breast cancer, this study adopted the method of meta-analysis to investigate the relation between breast cancer patients’ coping style and PTG, clarifying the controversy about the magnitude and direction of the relation between them in empirical studies. Nevertheless, a few limitations of the current meta-analysis should be considered. First, PTG measurement instruments were restricted to the PTGI or a revised scale based on the PTGI to minimize the potential source of heterogeneity. Similarly, measurement instruments for coping style were restricted to scales that can distinguish one or more of the coping strategies of confrontation coping, avoidance coping, and acceptance–resignation coping. Consequently, only 20 studies were included in the current meta-analysis. Thus, attention should be paid to the interpretation of our findings, as these could be underpowered. Second, given the inclusion of a small number of studies in certain subgroups, the subgroup analyses based on certain moderators should be interpreted with caution. Third, this study focused on the influence of certain moderator variables on the relation between breast cancer patients’ coping style and PTG. Other potential moderator variables, such as gender, time since diagnosis, and PTG measurement tools, should also be analyzed in the future. Fourth, as a few of the included articles did not report effect size directly, and we used a transformed method to calculate the effect size, there might be some bias. Therefore, the search for source material in articles should be expanded in future research.
Clinicians and nurses who engage in the assessment and treatment of breast cancer patients and survivors should be aware of these possible relations between coping styles and PTG and understand that each situation is unique. On the one hand, because different stages of breast cancer have different degrees of psychological distress and different psychological problems, clinical medical staff should promote PTG according to the different stages of breast cancer. On the other hand, considering that there are differences in individual characteristics of breast cancer patients, their PTG levels may also be different and affected by various factors. Therefore, clinical medical staff should help breast cancer patients choose appropriate coping methods based on their unique PTG experience and apply them in daily life to promote their physical and mental recovery.
A significantly positive relation between coping style (confrontation coping and avoidance coping) and PTG and a significantly negative relation between acceptance–resignation coping and PTG have been identified. Both cancer stage and age did not have a moderating effect on the relation between coping style and PTG among patients with breast cancer. Publication type significantly moderated the relation between breast cancer patients’ coping style (confrontation coping and acceptance–resignation coping) and PTG. Coping style measurement tools significantly moderated the relation between breast cancer patients’ coping style (confrontation coping and avoidance coping) and PTG. In the future, more studies, especially, large prospective studies, are warranted to verify our findings.
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
XW and HH: conceptualization, methodology, formal analysis, and writing—original draft preparation. QP, YZ, and JH: software. XW and GL: validation and data curation. XW and CC: writing—review and editing. GL and CC: supervision. CC: project administration and funding acquisition. All authors contributed to the article and approved the submitted version.
This work was supported by the Henan Graduate Education Reform and Quality Improvement Project (Grant No. YJS2021AL074).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.926383/full#supplementary-material
Ando, M., Morita, T., Hirai, K., Akechi, T., Kira, H., Ogasawara, E., et al. (2011). Development of a Japanese benefit finding scale (JBFS) for patients with cancer. Am. J. Hosp. Palliat. Care 28, 171–175. doi: 10.1177/1049909110382102
Begg, C. B., and Mazumdar, M. (1994). Operating characteristics of a rank correlation test for publication bias. Biometrics 50, 1088–1101.
Bellur, Z., Aydyn, A., and Alpay, E. H. (2018). Mediating role of coping styles in personal, environmental and event related factors and posttraumatic growth relationships in women with breast cancer. J. Clin. Psychiat. 21, 38–51. doi: 10.5505/kpd.2018.65365
Bourdon, M., Blanchin, M., Campone, M., Quéreux, G., Dravet, F., Sébille, V., et al. (2019). A comparison of posttraumatic growth changes in breast cancer and melanoma. Health Psychol. 38, 878–887. doi: 10.1037/hea0000766
Boyle, C. C., Stanton, A. L., Ganz, P. A., and Bower, J. E. (2017). Posttraumatic growth in breast cancer survivors: Does age matter? Psychooncology 26, 800–807. doi: 10.1002/pon.4091
Buyukasik-Colak, C., Gundogdu-Akturk, E., and Bozo, O. (2012). Mediating role of coping in the dispositional optimism-posttraumatic growth relation in breast cancer patients. J. Psychol. 146, 471–483. doi: 10.1080/00223980.2012.654520
Card, N. A. (2012). Applied meta-analysis for social science research. New York, NY: Guilford Press.
Carver, C. S. (1997). You want to measure coping but your protocol’s too long: Consider the brief COPE. Int. J. Behav. Med. 4, 92–100. doi: 10.1207/s15327558ijbm0401_6
Casellas-Grau, A., Ochoa, C., and Ruini, C. (2017). Psychological and clinical correlates of posttraumatic growth in cancer: A systematic and critical review. Psychooncology 26, 2007–2018. doi: 10.1002/pon.4426
Cheng, H., and Zhang, A. (2015). Correlation between posttraumatic growth, coping styles and quality of life in breast cancer patients. J. Nurs. Sci. 30, 84–86. doi: 10.3870/hlxzz.2015.14.084
Denieffe, S., Cowman, S., and Gooney, M. (2014). Symptoms, clusters and quality of life prior to surgery for breast cancer. J. Clin. Nurs. 23, 2491–2502. doi: 10.1111/jocn.12430
Early, A. P., and Moon, W. (2021). Breast cancer and secondary cancer recurrences after autologous tissue reconstruction. Clin. Breast Cancer 21, e96–e101. doi: 10.1016/j.clbc.2020.07.015
Feifel, H., Strack, S., and Nagy, V. T. (1987). Coping strategies and associated features of medically ill patients. Psychosom. Med. 49, 616–625. doi: 10.1097/00006842-198711000-00007
Folkman, S., Lazarus, R. S., Dunkel-Schetter, C., DeLongis, A., and Gruen, R. J. (1986). Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. J. Pers. Soc. Psychol. 50, 992–1003. doi: 10.1037//0022-3514.50.5.992
Fujimoto, T., and Okamura, H. (2021). The influence of coping types on post-traumatic growth in patients with primary breast cancer. Jpn. J. Clin. Oncol. 51, 85–91. doi: 10.1093/jjco/hyaa159
Ghoncheh, M., Pournamdar, Z., and Salehiniya, H. (2016). Incidence and mortality and epidemiology of breast cancer in the world. Asian Pac. J. Cancer Prev. 17, 43–46. doi: 10.7314/apjcp.2016.17.s3.43
Higgins, J., Thompson, S. G., Decks, J. J., and Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ 327, 557–560. doi: 10.1136/bmj.327.7414.557
Howard-Anderson, J., Ganz, P. A., Bower, J. E., and Stanton, A. L. (2012). Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: A systematic review. J. Natl. Cancer Inst. 104, 386–405. doi: 10.1093/jnci/djr541
Hu, J., Dong, X., and Cheng, W. (2018). Posttraumatic growth in breast cancer patients and its relationship with coping style and quality of life. Zhejiang J. Trauma. Surg. 23, 572–574. doi: 10.3969/j.issn.1009-7147.2018.03.081
Ýnan, F., and Üstün, B. (2014). Breast cancer and posttraumatic growth. J. Breast Health 10, 75–78. doi: 10.5152/tjbh.2014.1778
Janoff-Bulman, R. (2006). “Schema-change perspectives on posttraumatic growth,” in Handbook of posttraumatic growth: Research and practice, eds L. G. Calhoun and R. G. Tedeschi (Mahwah, NJ: Erlbaum).
Joseph, S., Murphy, D., and Regel, S. (2012). An affective-cognitive processing model of post-traumatic growth. Clin. Psychol. Psychother. 19, 316–325. doi: 10.1002/cpp.1798
Karimzadeh, Y., Rahimi, M., Goodarzi, M. A., Tahmasebi, S., and Talei, A. (2021). Posttraumatic growth in women with breast cancer: Emotional regulation mediates satisfaction with basic needs and maladaptive schemas. Eur. J. Psychotraumatol. 12:1943871. doi: 10.1080/20008198.2021.1943871
Kroemeke, A., Bargiel-Matusiewicz, K., and Kalamarz, M. (2017). Mixed psychological changes following mastectomy: Unique predictors and heterogeneity of post-traumatic growth and post-traumatic depreciation. Front. Psychol. 8:1245. doi: 10.3389/fpsyg.2017.01245
Kroenke, C. H., Rosner, B., Chen, W. Y., Kawachi, I., Colditz, G. A., and Holmes, M. D. (2004). Functional impact of breast cancer by age at diagnosis. J. Clin. Oncol. 22, 1849–1856. doi: 10.1200/JCO.2004.04.173
Lee, M., Song, Y., Zhu, L., and Ma, G. X. (2017). Coping strategies and benefit-finding in the relationship between non-disclosure and depressive symptoms among breast cancer survivors in China. Am. J. Health Behav. 41, 368–377. doi: 10.5993/AJHB.41.4.1
Lelorain, S., Bonnaud-Antignac, A., and Florin, A. (2010). Long term posttraumatic growth after breast cancer: Prevalence, predictors and relationships with psychological health. J. Clin. Psychol. Med. Settings 17, 14–22. doi: 10.1007/s10880-009-9183-6
Li, H., Yang, H., Sun, D., Mei, Y., and Dou, W. (2016). The mediation role of coping modes between illness perceptionand posttraumatic growthamong patients with breast cance. Chin. J. Behav. Med. Brain Sci. 25, 698–702.
Linley, P. A., and Joseph, S. (2004). Positive change following trauma and adversity: A review. J. Trauma. Stress 17, 11–21. doi: 10.1023/B:JOTS.0000014671.27856.7e
Lipsey, M. W., and Wilson, D. B. (2001). The way in which intervention studies have “personality” and why it is important to meta-analysis. Eval. Health Prof. 24, 236–254. doi: 10.1177/016327870102400302
Lisica, D., Kolenović-Ðapo, J., Džubur, A., Abdulahović, D., and Ejubović, M. (2019). The relationship between protective factors and a measure of psychological resistance in women diagnosed with breast cancer. Med. Glas. (Zenica) 16, 317–322. doi: 10.17392/1034-19
Liu, C., Luo, H., Chang, R., and Cui, J. (2019). Correlation between cognitive appraisal and coping styles and posttraumatic growth in breast cancerpatients. Chin. J. Clin. Oncol. Rehabil. 26, 751–753. doi: 10.13455/j.cnki.cjcor.2019.06.30
Liu, X. (2018). The mediating role of cognitive evaluation and coping style in social support and post-traumatic growth of breast cancer patients. Master’s dissertation. Hefei: Anhui Medical University.
Ma, L. (2014). The influencing factors of posttraumatic growth in breast cancer patients. Master’s dissertation. Hefei: Anhui Medical University.
Maajani, K., Jalali, A., Alipour, S., Khodadost, M., Tohidinik, H. R., and Yazdani, K. (2019). The global and regional survival rate of women with breast cancer: A systematic review and meta-analysis. Clin. Breast Cancer 19, 165–177. doi: 10.1016/j.clbc.2019.01.006
Mostarac, I., and Brajkovic, L. (2022). Life after facing cancer: Posttraumatic growth, meaning in life and life satisfaction. J. Clin. Psychol. Med. Settings 29, 92–102. doi: 10.1007/s10880-021-09786-0
Munn, Z., Moola, S., Lisy, K., Riitano, D., and Tufanaru, C. (2015). Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int. J. Evid. Based Healthc. 13, 147–153. doi: 10.1097/XEB.0000000000000054
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372:n71. doi: 10.1136/bmj.n71
Paredes, A. C., and Pereira, M. G. (2018). Spirituality, distress and posttraumatic growth in breast cancer patients. J. Relig. Health 57, 1606–1617. doi: 10.1007/s10943-017-0452-7
Romeo, A., Di Tella, M., Ghiggia, A., Tesio, V., Gasparetto, E., Stanizzo, M. R., et al. (2019). The traumatic experience of breast cancer: Which factors can relate to the post-traumatic outcomes? Front. Psychol. 10:891. doi: 10.3389/fpsyg.2019.00891
Schmid-Büchi, S., van den Borne, B., Dassen, T., and Halfens, R. J. (2011). Factors associated with psychosocial needs of close relatives of women under treatment for breast cancer. J. Clin. Nurs. 20, 1115–1124. doi: 10.1111/j.1365-2702.2010.03376.x
Soo, H., and Sherman, K. A. (2015). Rumination, psychological distress and post-traumatic growth in women diagnosed with breast cancer. Psychooncology 24, 70–79. doi: 10.1002/pon.3596
Soriano, E. C., Otto, A. K., LoSavio, S. T., Perndorfer, C., Siegel, S. D., and Laurenceau, J. P. (2021). Fear of cancer recurrence and inhibited disclosure: Testing the social-cognitive processing model in couples coping with breast cancer. Ann. Behav. Med. 55, 192–202. doi: 10.1093/abm/kaaa043
Sterne, J. A., Gavaghan, D., and Egger, M. (2000). Publication and related bias in meta-analysis: Power of statistical tests and prevalence in the literature. J. Clin. Epidemiol. 53, 1119–1129. doi: 10.1016/s0895-4356(00)00242-0
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., et al. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. doi: 10.3322/caac.21660
Svetina, M., and Nastran, K. (2012). Family relationships and post-traumatic growth in breast cancer patients. Psychiatr. Danub. 24, 298–306.
Tedeschi, R. G., and Calhoun, L. G. (1996). The posttraumatic growth inventory: Measuring the positive legacy of trauma. J. Trauma. Stress 9, 455–471. doi: 10.1007/bf02103658
Tedeschi, R. G., and Calhoun, L. G. (2004). Tedeschi RG, Calhoun LGPosttraumatic growth: Conceptual foundations and empirical evidence. Psychol. Inq. 15, 1–18.
Tomita, M., Takahashi, M., Tagaya, N., Kakuta, M., Kai, I., and Muto, T. (2017). Structural equation modeling of the relationship between posttraumatic growth and psychosocial factors in women with breast cancer. Psychooncology 26, 1198–1204. doi: 10.1002/pon.4298
Tong, X., Zhang, P., and Song, X. (2013). Study on correlation between postoperative social support, coping styleand posttraumatic growth of patients with breast cance. Chin. Nurs. Res. 27, 3215–3217.
Tu, P. C., Yeh, D. C., and Hsieh, H. C. (2020). Positive psychological changes after breast cancer diagnosis and treatment: The role of trait resilience and coping styles. J. Psychosoc. Oncol. 38, 156–170. doi: 10.1080/07347332.2019.1649337
Wang, J., Zhou, Y., Xia, L., and Wang, X. (2020). Coping modes and post-traumatic growth in the postoperative breast cancer patients: A longitudinal research. Chin. J. Pract. Nerv. Dis. 23, 1344–1348. doi: 10.12083/SYSJ.2020.15.029
Watson, M., Law, M. G., Santos, M., Greer, S., Baruch, J., and Bliss, J. (1994). The mini-MAC: Further development of the mental adjustment to cancer scale. J. Psychosoc. Oncol. 12, 33–46. doi: 10.1300/J077V12N03_03
Wilski, M., and Tasiemski, T. (2016). Illness perception, treatment beliefs, self-esteem, and self-efficacy as correlates of self-management in multiple sclerosis. Acta. Neurol. Scand. 133, 338–345. doi: 10.1111/ane.1246
Yeung, N., and Lu, Q. (2018). Perceived stress as a mediator between social support and posttraumatic growth among Chinese American breast cancer survivors. Cancer Nurs. 41, 53–61. doi: 10.1097/NCC.0000000000000422
Zhang, Q., Zhuang, Y., Huang, H., Yao, D., and Cui, Y. (2017). Study on post-traumatic growth related factors in patients with breast cancer during chemotherapy. Med. J. Chin. Peoples Health 29, 1–3+35. doi: 10.3969/j.issn.1672-0369.2017.11.001
Keywords: breast cancer, coping style, posttraumatic growth, meta-analysis, review
Citation: Wan X, Huang H, Peng Q, Zhang Y, Hao J, Lu G and Chen C (2022) The relation between coping style and posttraumatic growth among patients with breast cancer: A meta-analysis. Front. Psychol. 13:926383. doi: 10.3389/fpsyg.2022.926383
Received: 22 April 2022; Accepted: 12 September 2022;
Published: 29 September 2022.
Edited by:
Norbert Schäffeler, Tübingen University Hospital, GermanyReviewed by:
Caroline Rometsch-Ogioun El Sount, University of Tübingen, GermanyCopyright © 2022 Wan, Huang, Peng, Zhang, Hao, Lu and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiwei Hao, NzI5Mjk4Njg4QHFxLmNvbQ==; Guangli Lu, a2Z3YW5nbGkwOTE1QDEyNi5jb20=; Chaoran Chen, a2ZjY3JAMTI2LmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.