
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 04 July 2022
Sec. Health Psychology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.914183
 Teresa Fazia1*†
Teresa Fazia1*† Francesco Bubbico1†
Francesco Bubbico1† Andrea Nova1
Andrea Nova1 Emilia Riggi2
Emilia Riggi2 Giancarlo Caimi1
Giancarlo Caimi1 Beril Calgan1
Beril Calgan1 Gerardo Salvato1,3
Gerardo Salvato1,3 Salvatore Bruno4
Salvatore Bruno4 Gabriella Bottini1,3
Gabriella Bottini1,3 Luisa Bernardinelli1
Luisa Bernardinelli1To limit the first spread of COVID-19 in March 2020, the Italian government imposed strict lockdown measures to the population. Despite necessary to reduce the virus transmission and the burden to the hospitals, social isolation has caused detrimental effects on psychological wellbeing and mental health. Moreover, during this period, it was also difficult to deliver psychological treatments and psychiatric assistance. A short (a weekly session for 9 weeks) mindfulness-based meditation program, named Integral Meditation (IM), was administered entirely online to healthy adults from Italy. This is a two-groups pre–post-quasi-experimental study in which the two groups, treated and control, were not randomized. Through matching procedures aimed at overcoming the absence of randomization, we analyzed a sample of 84 subjects (42 for each group). By applying linear mixed effect models, we tested the hypothesis of a beneficial effect of IM on wellbeing, perceived stress, and state anxiety, as measured by three self-reported questionnaires (WEMWBS, PSS, and STAI-X1, respectively), assuming that this effect could be different according to the level of baseline trait anxiety, as measured by STAI-X2. The results showed a statistically significant effect of STAI-X1 (β = −8.24 [95%CI −15.39; −1.09], p = 0.02) and WEMWBS (β = 4.61 [95%CI 0.94; 8.29], p = 0.01) in the higher trait anxiety subgroup only. No statistically significant effect of IM was observed for PSS. These results suggest that our IM, delivered online, may increase mental wellbeing and decrease anxiety specifically in subjects with higher trait anxiety.
On 31 December 2019, the health authorities of Wuhan identified the cause of the recent cases of “pneumonia of unknown cause,” found since October 2019 (World Health Organization). The strain responsible for these infections has been designated as severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), and the related disease was named, on 11 February 2020, by the World Health Organization (WHO) [World Health Organization Coronavirus disease (COVID-19) pandemic, 2019; World Health Organization Listings of WHO's response to COVID-19, 2020] as COVID-19 (https://www.who.int/). COVID-19 is an infectious disease belonging to the coronavirus family with dramatic multisystemic consequences primarily on the respiratory system (Su et al., 2016; Zhu et al., 2020). On 11 March 2020, WHO declared a global pandemic since the virus has spread rapidly in a growing number of countries.
To limit the number of infections and to protect people, various preventive measures have been promoted worldwide since March 2020 (Ministero della Salute) and each country has adopted different strategies regarding lockdown measures and daily life restriction (https://ig.ft.com/coronavirus-lockdowns/). At that time, Italy was one of the hardest-hit countries in the European Union and it adopted one of the most rigid lockdowns with not negligible social and psychophysical effects on the population. Every individual responded differently to this situation, also based on his/her socioeconomic status. Some of the possible detrimental effects generated by this situation, as also listed in the Istituto Superiore di Sanità website (https://www.iss.it/), are as follows: (i) the fear of losing livelihoods, not being able to work during isolation and getting fired; (ii) the feeling of helplessness, boredom, frustration, loneliness, and depression due to isolation; (iii) the possible anger and aggression against children, spouses, partners, and family members (increased family and intimate violence by the partner); (iv) the relapses of people with developing or existing mental health and substance use problems and other negative outcomes because they avoid health facilities or are unable to access their care providers; and (v) the worries about the future (Brooks et al., 2020; Giallonardo et al., 2020; Sepúlveda-Loyola et al., 2020).
In Italy, early researches regarding the effects of COVID-19 on the population have brought out alarming data, with 40–50% of adults reporting some sorts of psychological distress (Marazziti et al., 2020; Moccia et al., 2020; Favieri et al., 2021) and 30% of children and adults reporting high risk of developing post-traumatic stress disorder (PTSD) symptoms (Marazziti et al., 2020; Davico et al., 2021). These data are consistent with previous research on the Chinese population (Huang and Zhao, 2020; Sun et al., 2020), on the psychological consequences of social isolation in different scenarios (Brooks et al., 2020), and on the exposure to life-threatening situations on the human psyche (Nickell et al., 2004; Holmes et al., 2020; Roy et al., 2020). Furthermore, the fear caused by the possibility of contracting COVID-19, despite has been proved useful in motivating people to comply with the preventive rules issued by the governments, is considered a possible risk factor in the development of anxiety (Roy et al., 2020) and depression (Holmes et al., 2020). In addition, the sense of not having control over the situation and the inability to predict its evolution, both emblematic elements of the pandemic emergency, are substantial factors that characterize stress (Koolhaas et al., 2011). Chief among these, there was the difficulty or impossibility, given quarantine, for most of those who need psychiatric assistance to come into direct contact with mental health professionals. Psychological wellbeing of some categories, such as women and healthcare workers, was more affected by COVID-19. Healthcare workers were systematically exposed to emotional distress, anxiety, and sense of isolation that might represent a risk factor for later psychological issues, and these considerations are common within countries (Saladino et al., 2022). The risk of burnout was higher for frontline headline personnel working in intensive care units who were much more likely to be infected, which has caused an increased fear of infection (Lewis and Zauskova, 2021; Phillips and Kucera, 2021). Detrimental effects have been reported to be more pronounced for women, which reported more severe depression, distress symptoms (Coleman, 2020; Connor et al., 2020; Duncan, 2020; Lai et al., 2020; Vloo et al., 2021), and higher state and trait anxiety levels (Karasu et al., 2021), than for men.
Despite these figures present a daunting picture, there is an equally vast pool of research that offers simple, effective, and inexpensive solutions with which to circumvent the various limitations that the health emergency has entailed. In this regard, technological advancement has allowed to administer therapeutic psychoeducational and psychological interventions even remotely (Ho et al., 2020). The use of remotely delivered psychological therapies is not new in the field of telehealth, and several studies have documented its effectiveness, for example, in the treatment of patients with Parkinson's disease (Swalwell et al., 2018), anxiety disorders (Théberge-Lapointe et al., 2015; Berryhill et al., 2019), PTSD (Germain et al., 2009; Bolton and Dorstyn, 2015), panic disorders (Bouchard et al., 2004), and obsessive-compulsive disorder (Fitt and Rees, 2012).
In the early stage of the COVID-19 epidemic, many researchers highlighted the importance of providing interventions aimed at aid people's mental health (Duan and Zhu, 2020; Pfefferbaum and North, 2020). Particularly, in a study carried out in Italy (Giallonardo et al., 2020), the authors have underlined the future negative effects of the lockdown on the mental health among healthcare workers at the beginning of COVID-19 pandemic. Isolation, loneliness, and trauma were determined as the risk factors whereas coping strategies, resilience, internet use, social network, and post-traumatic growth were listed as protective factors. It has been emphasized the need for immediate efforts for developing preventive strategies as well as direct interventions aiming to mitigate the impact of the outbreak on individual and population mental health (Giallonardo et al., 2020). In this context, online intervention groups can become a place of social aggregation to support the mental health during COVID-19 lockdown, especially for those who experienced a period of loneliness, with all the negative effects that it entails.
Some authors have proposed the use of mindfulness-based interventions (MBIs), which incorporate the practice of meditation, to serve this purpose of aiding people's mental health (Baiano et al., 2020; Behan, 2020; Bursky et al., 2021; Green et al., 2021). The term mindfulness is strictly connected to the awareness, and it involves the intentional attention of the present moment experience, and the acceptance and non-judgement of such experience as it is, allowing thoughts to come and go without attachment and reaching a state of calm and relaxation (Chiesa et al., 2017; Behan, 2020). Online MBIs have already been deployed for years, and their effectiveness in the treatment of stress, anxiety, and in increasing the individual's general wellbeing, even after few weeks, is well recognized (Lunn et al., 2020).
In this regard, during the first total lockdown in Italy, Accoto et al. (2021) conducted an 8-week online mindfulness-based stress reduction (MBSR) protocol with 6 weeks of video support for meditation practice. The results showed an improvement in the capacity to choose not to react to negative thoughts instead of accepting their existence, and the treatment was found to be a protective factor against stress among the treated compared to the control group. Another study carried out in Italy during COVID-19 pandemic found a positive and protective value of the mindfulness practice on mindfulness, positive affect, depression, and insomnia (Bossi et al., 2022).
Our study is framed in this context, and it aims at evaluating the beneficial effect in improving wellbeing, stress, and state anxiety of a 9-week online MBI, named Integral Meditation (IM), administered for the first time online, on non-clinical people from the general population during the first COVID-19 lockdown in a country like Italy, where there has been one of the most rigid lockdowns having probably the widest implications. Our IM intervention first described in the study of Fazia et al. (2020a) was developed to promote personal and spiritual growth, especially within the general non-clinical population.
Specifically, this study aims to test the hypotheses that our intervention: (i) decreases state anxiety as measured by State Trait Anxiety Inventory (STAI-X1); (ii) decreases stress as measured by Perceived Stress Score (PSS); and (iii) increases wellbeing as measured by Warwick-Edinburgh Mental wellbeing Scales (WEMWBS) and that these effects were more pronounced in subjects' with higher baseline levels of trait anxiety, as measured by STAI-X2 questionnaire, which means in statistical terms to assume a three-way interaction between trait anxiety, time, and treatment. The choice to investigate these three endpoints (i.e., state anxiety, stress, and wellbeing) and formulate the above reported hypotheses was driven by the fact that these endpoints, worsen following the pandemic course (Brooks et al., 2020), and they are reported to mainly benefit from MBIs (Eberth and Sedlmeier, 2012; Khoury et al., 2015). Furthermore, we assumed that subjects who at the beginning of the study had higher levels of trait anxiety and thus had the tendency to respond to the concerns, troubles, and worries to various situations (Gidron, 2013; Taoka et al., 2014; Saviola et al., 2020; Fino et al., 2021), presumably were more affected by COVID-19 pandemic, and were more likely to benefit from our short-term online intervention than those having lower score. In addition, empirical studies suggest an inverse relationship between trait mindfulness and trait anxiety, so that people with higher trait anxiety are more likely to have a lower trait mindfulness (Jaiswal et al., 2019a). Being our intervention built to be easy-to-learn and to produce quick benefits also via an increase of mindfulness, there may be a higher possibility to detect a stronger observable beneficial effect among those people with a more urgent need for support and with low level of mindfulness.
We planned this research to offer to non-clinical Italian adults a quick but still complete mindfulness-based training, during the first wave of infection by COVID-19 and the relative confinement imposed by the Italian government, and to study its effect on three psychological endpoints. Therefore, during April 2020, we opened a call for an application to join the study promoted through digital advertising, i.e., mailing lists and social media posting. Given the nature of our intervention, participation was voluntary-based. Given the challenging time due to the pandemic, we felt unethical to randomize people to intervention and non-intervention. People who were interested in participating to our program and met the inclusion criteria were admitted and allocated to the treated group. While as to the control group, who did not receive any intervention, subjects interested in contributing to this research and meeting the inclusion criteria but, for various logistical issues unable to attend the classes, served as passive control group by only filling out the same questionnaires as the treated group. The inclusion criteria were as follows: (i) the absence of any psychiatric record, assessed by asking straight questions about these conditions. So, subjects suffering from severe anxiety or depression, severe mental illness (e.g., hypomania or psychotic episode), or any other serious mental or physical health problem were excluded from the study; (ii) to be 18 or older; (iii) to have a digital device and an Internet connection to complete the assessment; (iv) to install a dedicated app and to participate to videoconferences; and (v) to understand Italian language. To join the study, we asked the participants to provide agreement with the privacy and informed consent form that was sent to them by email. The study was not registered at Clinicaltrials.gov.
Our intervention consists of nine mindfulness-based meditation classes, given one time a week and lasting ≈60 min each on the Zoom videoconferencing platform (Zoom Video Communications, Inc. Global Infrastructure and Security Guide Global Infastructure and Security Guide) from April to July 2020. Our mindfulness-based IM program, well accepted by both novice and experienced meditators, has strong evidence of efficacy in the general population as reported in our previous studies (Fazia et al., 2020a,b, 2021) in which the same program was instead provided one time a week on 12 face-to-face sessions. A detailed description of the IM is reported in the study of Fazia et al. (2020a). Briefly, it incorporates mindfulness and aspects from different traditional meditation techniques albeit it shared many features with the classical mindfulness-based program (MBP) it differs to them especially in the use of the imagery to power the concentration. IM was slightly adapted here to meet the need of the target population in this unprecedent historical moment, for example by (a) reducing the number of sessions from twelve to nine, to guarantee a better adherence and participation albeit non-neglecting the main research objectives, and (b) by administering it online given the impossibility of carrying face-to-face classes. As for the duration, mindfulness programs should be lasted at least 8 weeks, even if Gotink et al. (2016) assess how an 8-week MBI induces neurofucntional changes similar to those observed after a longer practice. Being a total of nine online instead of 12 face-to face sessions of the original version, each cycle is not repeated for three meditation sessions in a row as in the study of Fazia et al. (2020a), but it is structured as follows:
Cycle 1: aware diaphragmatic breathing, keeping the posture (repeated for two meditation sessions in a row).
Cycle 2: body scan and awareness of body sensations (repeated for two meditation sessions in a row).
Cycle 3: emotions and thoughts feeling and releasing (repeated for two meditation sessions in a row).
Cycle 4: imagery activity to change the state of consciousness (repeated for three meditation sessions in a row).
In each cycle, also the abilities acquired in the preceding cycle/s are still practiced and new one is introduced, and, as a result, the abilities evolve across cycles. IM simultaneously uses breathing, focusing attention, release of physical tensions, thoughts, and feeling sensations through internal senses and imagery, allowing a quick relaxation and more deeply a physical, energetic, and spiritual wellbeing. At the beginning and the end of the meditation classes, the participants had the opportunity to socialize (even if remotely) and share their thoughts, feelings, and emotions with the other participants.
Here, we assessed its efficacy in helping to reduce and managing stress, reducing anxiety, increasing, and balancing psychological well-being by administering it for the first time online during an unprecedented situation such as the COVID-19 quarantine.
Each participant, both in the treated and in the control groups, filled in three self-report psychological questionnaires, i.e., STAI-X1, PSS, and WEMWBS, at two different time points: at t0 (i.e., before the start of the study) and at t1 (i.e., at the end of the study). In addition, for each participant, we collected trait anxiety measures through STAI-X2 questionnaire, and sociodemographic information through a background questionnaire, at t0 only. Some information related to the impact of COVID-19 on participants' life was also collected at both t0 and t1, and the answers given at t0 are compared with those at t1 to obtain seven variables describing the impact of COVID-19 on participant's life during the studied time period. The seven COVID-related variables were used as covariates in the statistical analysis and provide information about the following: (i) if participants or (ii) someone in their inner circle (e.g., family, friends) or (iii) acquaintances have contracted the virus; (iv) if someone participants' inner circle or (v) acquaintances have died due to the virus; (vi) if participants have changed the people they lived with; and (vii) if participants have lost their job.
The participants completed the questionnaires online via Google Forms.
In detail, the psychological scales used were as follows:
STAI-X1 and STAI-X2 (State Trait Anxiety Inventory). The STAI questionnaire (Spielberger, 1970) is composed of two parts: the X1-scale assesses anxiety as a state to find out how the patient was feeling at the time of the assessment whereas the X2-scale assesses anxiety as a trait that reflects how a person generally feels. Each of them consists of 20 items, and responses are given in 4-point Likert scale. Participants are asked to classify themselves by given statements in the STAI-X1 scale as “not at all” (1) to “very much so” (4), while in the STAI-X2 scale as: “almost never” (1) to “almost always” (4). The values obtained in each of the scales range from 20 to 80 points, with the 20–40 range described as a low level of anxiety, 41–60 as moderate anxiety, and 61–80 as a high anxiety. We employed STAI-X1 as a dependent variable to measure the effect of the treatment on it. STAI-X2 was used to measure the baseline level of trait–anxiety before the intervention only and was used in the subsequent analysis as an explanatory interactor variable to test the hypothesis that the effect of treatment was different based on its value. The questionnaires have good psychometric properties in the English and Italian versions (Spielberger et al., 1983).
Perceived Stress Scale (PSS) (Cohen et al., 1983) is a 10-items questionnaire that measures the perception of stress and the degree to which situations in one's life are appraised as stressful during the last month. Answers were given on a 5-point scale and items were designed to tap how unpredictable, uncontrollable, and overloaded respondents find their lives. Higher scores are associated with a greater stress perception. The PSS has good psychometric properties in the English and Italian versions (Mondo et al., 2019). PSS scores were used as a dependent variable to evaluate the effect of the treatment on them.
Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS) (Tennant et al., 2007) is a 14-items questionnaire of mental wellbeing including subjective wellbeing and psychological functioning. All items in a 5-point scale are worded positively and addressed the aspects of positive mental health and measure the frequency of the subject's attitudes from “never” to “always.” Higher scores indicate mental wellbeing. This questionnaire has good psychometric properties valid also in its Italian version (Gremigni and Stewart-Brown, 2011). WEMWBS scores were used as a dependent variable to evaluate the effect of the treatment on them.
This is a two-group pre–post-quasi-experimental design, in which participants were not randomly assigned to the treatment or to the control group. So to reduce confounding bias due to the absence of randomization, we adopted a nearest neighbor matching on the propensity score (PS), using the matchit R function with method nearest, implemented in MatchIt R package (Ho et al., 2011). Conditionally on the PS, using the match.data R function, we matched the treated and control subjects with 1:1 ratio with respect to putative measured confounding variables included in the PS (i.e., nationality, marital status, number of children, dependent children/family members, unpaid loans, years of education, job, and type of employment agreement). Using this procedure, the control group will have nearly the same distribution of the included variables as the treated one, thus eliminating differences between the two groups and increasing comparability, thereby correcting for selection bias (Graham, 2010). To avoid a severe reduction in the sample size due to variables which are poorly represented in the whole sample, not all the collected background variables were included in the PS calculation. The variables that we did not included in the PS calculation, which resulted to be stastically significant different among the two groups, were added as covariates in the models to estimate the treatment effect adjusting and controlling for residual confounding. All the models were also corrected for sex, age, and location during the study period as well as for the seven COVID-19-related variables. So, despite the absence of randomization, in this way, we are confident to have controlled for all possible measured confounders.
On the matched sample (numbers reported in the RESULTS section), baseline differences in all the sociodemographic and COVID-19-related variables between the two groups were investigated using Wilcoxon rank-sum test for non-normally distributed age and chi-squared test for all the categorical variables.
Each outcome was collected at two time points (i.e., t0 and t1) and subjects who did not fill in the proposed questionnaires were excluded from the analysis. Questionnaires were scored following the provided guidelines and for each questionnaire, internal consistency was assessed via Cronbach's α coefficient (Cicchetti, 1994). Differences between groups at baseline were investigated for each outcome using non-parametric Wilcoxon rank-sum test.
Data were analyzed following an intention to treat approach, i.e., independent of the number of classes completed. This approach allows having a conservative estimation of the treatment effect and avoiding biases related to dropouts and participants' adherence.
For the purpose of the analysis, STAI-X2 was further categorized into two categories as above or below the median, chosen as cutoff value. Linear mixed model effects (LME) (Pinheiro and Bates) have been applied to test the hypothesis of a beneficial effect of our intervention on the investigated outcomes. A random intercept for subjects in the form of 1|subject had been used to adjust the models for intra-subject variability produced by the two repeated measurements at t0 and t1 carried out on the same subject. Since we hypothesized a different effect of treatment based on higher or lower baseline trait anxieiy, we first tested the statistically significance of the coefficient of the three-way interaction between time, treatment and the categorized STAI-X2 score (i.e., time * treatment * categorized STAI-X2). If the three-way interaction was statistically significant, which means that the effect of treatment is different in the two groups of baseline trait anxieiy, we further estimated the effect of the interaction between time and treatment (i.e., time * treatment) separately in the two groups of trait anxiety (within-group pre–post-treatment differences). Instead, if the three-way interaction was not statistically significant, we estimated the effect of the interaction between time and treatment in the whole sample without stratification. The coefficient of the interaction time * treatment measures the difference in slopes between the two treatment groups, indicating how much more the treatment group is improving over time with respect to the investigated endpoints, compared to the control group over the same period. Normality of residuals was assessed graphically through Q-Q plots and Shapiro–Wilk test.
In addition, for testing the possible dose–response effect of each endpoint in the treated group, a linear model was fitted by specifying as dependent variable, the post-intervention questionnaire's score, and as predictors, the number of classes attended by each participant, the baseline questionnaire's measure, sex, and age.
p-Value ≤ 0.05 was considered as statistically significant. Given the explanatory nature of our study, limited number of hypothesis tested (n = 3), and the need to avoid missing important findings, no multiple testing correction was applied (Rothman, 1990).
Descriptive statistics are reported for both groups as the means ± standard deviation (SD). All analyses were done using R 3.5.1 software (R Core Team).
During the recruitment phase, 95 voluntary participants were enrolled in the treated group, and simultaneously, the same numbers of participants were recruited in the control group. Among them, we excluded from the analysis those who did not fill in the post-treatment questionnaires, so that 102 participants (treated = 49, control = 53) were eligible for the study. Through the matching procedures, a final sample of 84 subjects (treated = 42, control = 42) were selected for the analysis. The sample consisted of 62 females and 22 males with a mean age±(SD) of 45.33 ± (15.04) ranging from 18 to 75. Participants' flow diagram is represented in Figure 1. To evaluate the effectiveness of the matching procedure, in Figure 2 the histogram of the density of PS distribution in the two groups before and after the matching procedure is plotted. Before matching (raw), treated groups have a different distribuition of PS than the control group; after matching, the density distributions of the two groups become somewhat more similar.
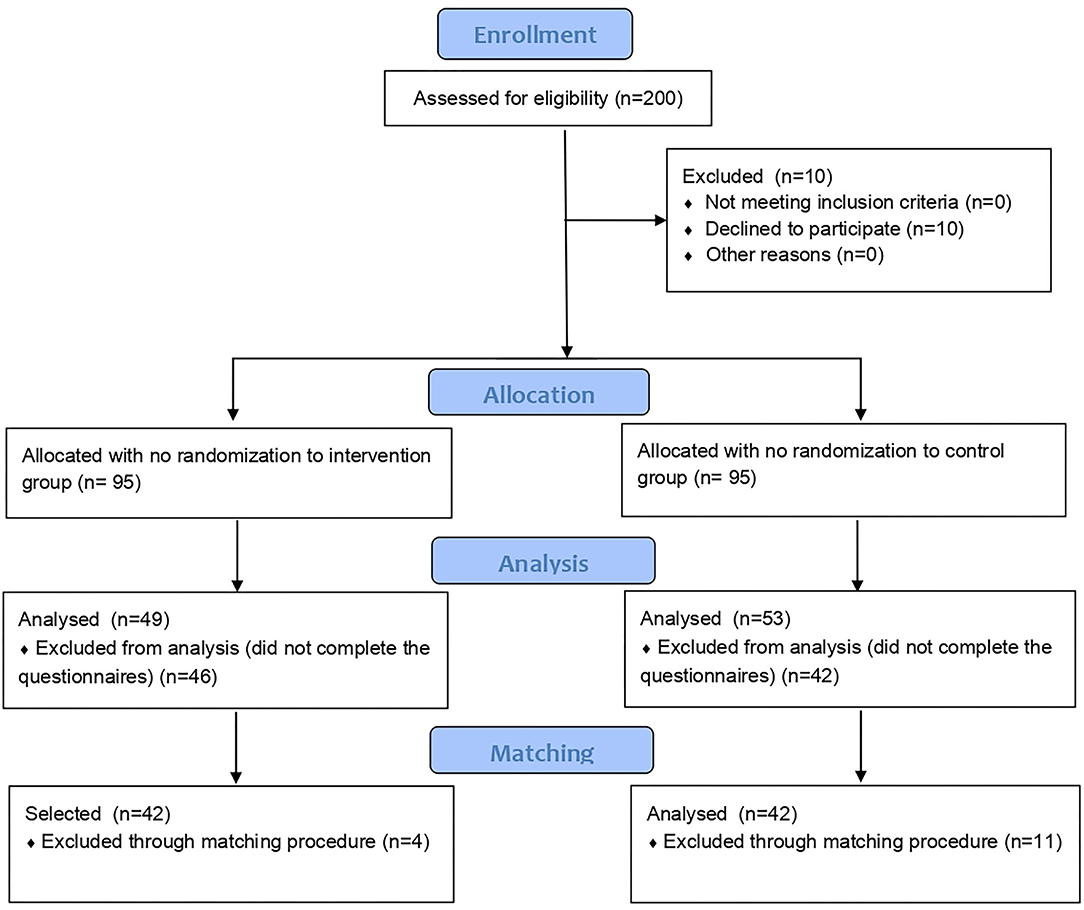
Figure 2. Histogram of the density of propensity score distribution in the two groups, i.e., treated and control, before (Raw) and after the matching procedure (Matched).
The sample size was determined by the feasibility of recruitment. For the analyzed sample size (n = 84 subjects) and for an expected medium effect size d = 0.50, power analysis was determined post-hoc and was equal to 0.80 with the alpha error equal to 0.05.
Study sample characteristics, including the COVID-related variables, are provided in Table 1. No differences were observed between the two groups at baseline characteristics except for the variables sport (p = 0.005), time spent on sport activities (p = 0.01), and previous meditation experience (p < 0.0001) as well as for having acquaintances who died for COVID-19 during the period of the study (p = 0.05) as illustrated in Table 1. These variables were included as covariates in the LME models to adjust the estimate of interest for confounding. Models were also adjusted for sex, age, and all the seven COVID-related variables, being variables not included in the matching procedure by PS.
Mean, SD, and internal consistency for each questionnaire at both t0 and t1 are reported separately in the control and in the treated groups in Table 2. In Table 2, the p-values of baseline differences for each questionnaire were also reported and no statistically significant differences were observed except for STAI-X2 that was used as an interactor in the model and so do not represent an endpoint.
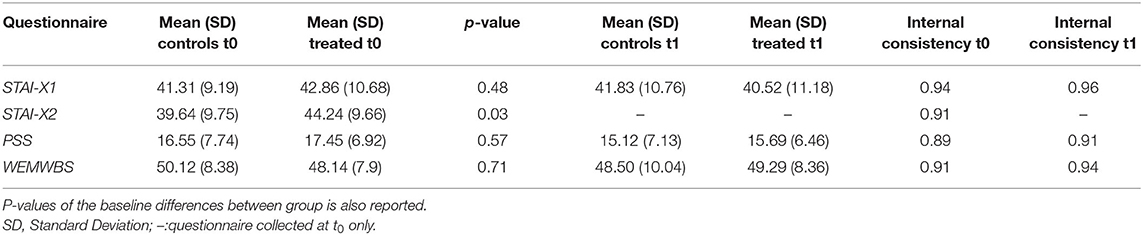
Table 2. Mean, Standard Deviation (SD) and internal consistency for each questionnaire and subscale in the two groups (controls and treated) at both time points (to and t1).
The continuous STAI-X2 score ranging from 22 to 63 was dichotomized using as cutoff its median value (=42). Thus, the sample was split into two categories: lower STAI-X2 with values ≤ 42 and higher STAI-X2 with values >42. A total of 43 subjects (24 controls and 19 treated) were assigned to the group with lower STAI-X2 whereas 41 subjects (18 controls and 23 treated) were assigned to the group with higher STAI-X2.
By testing the three-way interaction (time * treatment * categorized STAI-X2), we investigated whether the effect of our IM was different in the two groups (treated and control) at the two different levels of trait anxiety. A statistically significant three-way interaction, which means that there is a different effect of treatment in the two groups of trait anxiety, was found for STAI-X1 (β = −10.08 [95%CI −18.46; −1.70], p = 0.019) as well as for WEMWBS (β = 4.76 [95%CI 0.01; 9.50], p = 0.049) while not in PSS (β = 6.01 [96%CI −2.36; 14.38], p = 0.157). Full results are reported in Table 3.
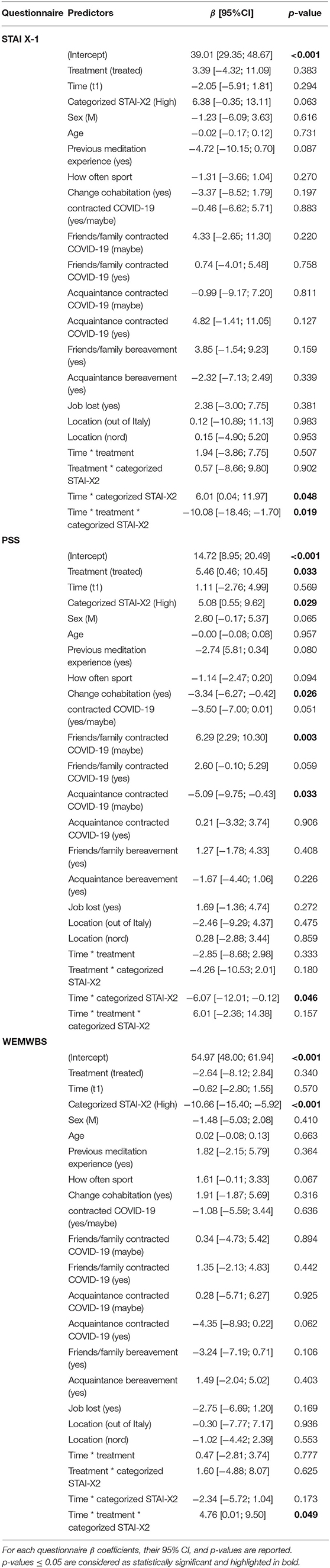
Table 3. Results of the linear mixed models for the effect of treatment and categorized STAI-X2 on the investigated outcomes.
When statistically significant three-way interaction was observed, that is for STAI-X1 and WEMWBS, a further analysis on these two endpoints was performed stratifying the data according to the trait anxiety groups and testing the effect of time * treatment separately within each group. No statistically significant results were found in the group with lower baseline value of STAI-X2 for both STAI-X1 and WEMWBS. While in the group with higher STAI-X2, a statistically significant time * treatment interaction was observed both in STAI-X1 (β = −8.24 [95%CI −15.39; −1.09], p = 0.02) and in WEMWBS (β = 4.61[95%CI 0.94; 8.29], p = 0.01). These latter results support the hypothesis of a beneficial effect of our intervention on decreasing state anxiety and increasing wellbeing in people having higher levels of baseline trait anxiety.
With regard to PSS in which no statistically significant three-way interaction was observed, a LME model on the whole sample was fitted for testing the interaction between time and treatment but no statistically significant difference between pre–post-changes in the two groups was found (β = −0.29 [95%CI −4.46; 3.87], p = 0.889), thus indicating that our intervention was not effecting in managing and reducing stress.
As for the number of IM session attendend, among the 42 treated subjects, 14 (33%) attended more than seven meditation classes, and 25 (60%) attended a number of classes between three and seven, whereas 3 (7%) attended <2 classes, with 5.43 mean number of classes attended. We did not find any statistically significant effect of the number of attended meditation classes on the investigated endpoint, Specifically, the estimate and the p-value of the effect of the number of attended meditation classes as from the fitted linear model were as follows: β = −0.96 with p = 0.22 for STAI-X1, β = −0.69 with p = 0.19 for PSS and, β = 0.56 with p = 0.22 for WEMWBS, which means that no dose–response relationship with the number of meditation classes was observed in our study.
The aim of this study was to investigate the efficacy of our IM program on improving stress, state anxiety, and wellbeing as measured by three self-reported questionnaires, i.e., PSS STAI-X1, and WEMWBS, respectively. Our IM may be classified as a MBP since it was created by adopting MBP fundamental parts and the variable features chosen according to the characteristics of our target population, i.e., healthy adults from Italy. This study took place during the first lockdown period during the COVID-19 pandemic in Italy; therefore, the intervention was administered via an online platform. The study has good ecological validity since it involved the participants while they were at their home and facing a new situation for a period of 9 weeks. Our intervention was aimed at providing them a tool to deal with the negative effects induced by the coronavirus pandemic on psychological health.
Being trait anxiety, as measured through STAI-X2 questionnaire, part of an individual's personality (Spielberger, 1972) and related to a tendency to respond with concerns, troubles, and worries to various situations (Saviola et al., 2020), we hypothesized that people with baseline higher levels of STAI-X2 scores were more likely to benefit from our short-term online intervention than those having lower scores. To verify this hypothesis, we considered the median-based categorization of the STAI-X2 scores (lower vs. high) to act as an interactor, thus modifying the effect of treatment. Statistically significant interaction implies that in a particular group, the effect of treatment could be more marked than in the other, and thus, analyzing the global sample, without considering this, a dilution of the treatment effect masking possible statistical significance could happen. In other words, people with lower levels of trait anxiety tend to have a better response to temporary stressful events (state anxiety); in contrast, individuals with higher levels of trait anxiety tend to have a worsen response to temporary stressful events (state anxiety) and could have a greater beneficial effect of our intervention. Furthermore, a growing body of evidence from literature has demonstrated the inverse relationship between mindfulness and trait anxiety: individuals with a higher predisposition to mindfulness will be those with lower levels of trait anxiety (Arch and Craske, 2010; Mankus et al., 2013; Jaiswal et al., 2018, 2019a,b). Interestingly, such inverse relationship also influences the cognitive functioning. For instance, Jaiswal et al. (2018) grouped participants based on their mindfulness and trait anxiety scores showing that the group with high mindfulness and low anxiety had higher efficiency of cognitive control. In a meta-analysis, it has been reported that the effect size of transcendental meditation technique on reducing trait anxiety depends on the patients' initial anxiety level (Orme-Johnson and Barnes, 2014). The principle that populations with elevated initial levels of an outcome will show larger effect sizes has been found also for other variables, such as depression and blood pressure. An EEG study also reported a differential effect of meditation based on participants' initial level of trait anxiety, suggesting that having lower trait anxiety more readily induces meditation with a predominance of an internalized attention while higher trait anxiety more readily induces meditation with a predominance of relaxation (Murata et al., 2004).
We found a statistically significant three-way interaction between time, group, and categorized STAI-X2, meaning that the effect of our intervention is different depending on having higher or lower levels of trait anxiety, both in STAI-X1 and in WEMWBS. In the subsequent stratified analysis, the results showed that in the group with higher trait anxiety, there was a statistically significant effect of treatment both in STAI-X1 and in WEMWBS. No statistically significant effect of treatment in the investigated outcomes was found in the group with lower STAI-X2 scores. The statistically significant results found in the high trait anxiety group but not in the low trait anxiety group confirm our hypothesis that a beneficial effect of our IM is more remarkable in this group of individuals. A possible explanation of these different effects could reside in the so-called well-known ceiling effect as it happens in the study of Matiz et al. (2020), where participants with low-resiliency obtained better results than those having higher resilience, since these latter had baseline healthy profiles. In our sample, the participants with higher trait anxiety vs. the participants with lower trait anxiety have higher baseline mean scores in PSS (18.46 vs. 15.60), STAI-X2 (46.29 vs. 38.07) and lower mean scores in WEMWBS (43.46 vs. 54.53). Another explanation could also be the probably higher motivation to attend mindfulness classes that may have subjects with psychological suffering as are those with higher trait anxiety in our study. Participants who are in a worse condition, in fact, could be more motivated to engage for their own recovery as described in other works (Hayes and Plumb, 2007; Matiz et al., 2018). As for PSS score, our intervention had no effect on this endpoint either globally or separately in the two groups of STAI-X2. This latter result is in contrast to our hypothesis about the beneficial effect of meditation on perceived stress during the quarantine period but even if not statistically significant, it is important to note that the direction of the effect observed in terms of reduction of stress, as also emerged from the CIs was that expected. The lack of significance may be probably due to the limited recruited sample size, further reduced due to the matching procedures necessary to face the lack of randomization.
During COVID-19 pandemic, research works were performed to investigate the effect of different MBI on psychological indicators of wellbeing in different target populations, even if, as far as we know, ours represent the first study performed during the first lockdown testing the hypotheses of a beneficial effect of a MBI on wellbeing, stress, and state anxiety different based on baseline levels of trait anxiety on general non-clinical population. For example, a cross-sectional study (Priyanka and Rasania, 2021) during COVID-19 pandemic on the general population reported higher mental wellbeing scores and lower risk of psychological distress and depression in subjects practicing yoga and meditation; The study of Nutting et al. (2022) conducted on family physicians showed a reduction of anxiety, stress, and an increasing in perceiving resilience and compassion after a brief mindfulness intervention. A positive effect of MBI was also observed in the study by González-García et al. (2021) where a brief online mindfulness and compassion-based intervention increase mental health on first-year psychology students from a university in Spain during COVID-19 pandemic, and in Desai et al. (2021) where an 8-week heartfulness meditation program showed a positive impact on stress and sleep quality.
To summarize, our intervention worked more efficiently on those people who tended to react in a more anxious manner to the events and therefore having more difficulties to cope with the stressful situations.
Our study suffers from some limitations: (i) the absence of monitoring of the number of meditations performed by the participants in their free time. Ideally, future research should add such measures, as the effect of meditation becomes more evident with frequency; (ii) the small sample size, which may be a possible cause for the non-significance of PSS; (iii) given the nature of our intervention, enrolment was obviously on voluntary basis and participants probably were people interested in the theme of meditation and willing to follow this practice, and this could represent only a problem of generalization, i.e., these results may be only applicable to people who are willing to meditate, but not a bias; (iv) given the difficult time due to pandemic, we felt unethical to randomize people to intervention and non-intervention, so this is a quasi-experimental study with its intrinsic limitation that was faced by adopting appropriate statistical method; (v) even if we used the PS to overcome possible non-comparability of the two treatment groups due to the absence of randomization, group differences could still be present due to on unmeasured variables, as it happens in all observational studies; (vi) furthermore, although we improved internal validity via covariate balancing, we have removed subjects with no match and in this way we could have introduced problem in generalizability; (vii) the control group was passive so not involved in any activity except to fulfill the questionnaires; for such reason, our study is not evaluating exclusively the effectiveness of the intervention, since the changes in the treated group can be promoted by the mere participation in a new activity; and (viii) finally, we did not collect information about use of medication and/or drug for decreasing stress and anxiety that could confound the effect of our treatment, but being a non-clinical population in consideration of the adopted inclusion criteria, we can assume the absence or at least limited use of drug with negligible effect.
Despite the above reported limitation, we contributed in some ways to understanding the emotional impact of the pandemic on the general non-clinical population living in Italy. The results obtained provide more insight into the understanding of the beneficial effect of our proposed free and easily accessible specific IM training, already tested in previous studies (Fazia et al., 2020a,b, 2021) to be effective for improving psychological wellbeing even in novice meditators. It should be noted that the intervention was administered online for the first time and investigated during the stressful and overwhelming period of COVID-19 quarantine.
As of 21 September 2021, more than 228 million people were infected with COVID-19, and more than 4 million and half deaths have been reported globally (World Health Organization).
The restrictions imposed by the Italian government due to COVID-19 pandemic have taken a great toll. The number of risk factors for an individual's mental wellbeing is manifold; ranging from being confined to a limited space for an extended period, not having certainties about the future, the possibility of losing one's job and being unable to reach a social environment are just the few examples. In this scenario, the possibility to engage in an activity designed to provide the tools to best cope with such stressors can be of enormous benefit to many individuals. Our project aimed at testing the efficacy of a particular mindfulness-based intervention in offering such help. Additionally, given the impossibility of gathering individuals in a face-to-face group, the intervention should have been held up in a virtual setting, in this case using videoconference meeting technologies.
Despite the impossibility to come in direct contact with the meditation group, participants showed improved outcomes on anxiety and mental wellbeing measures, even after a relatively short period of 9-week meditation training, and this happened in the high trait anxiety group.
Such results open a great possibility regarding public mental health services, offering a viable alternative to those services precluded to many individuals in remote areas or in time such as those lived in many areas of the world during the quarantine period. Future study on this topic should be performed to assess the longer-term impacts of the intervention, such as whether people have continued to meditate and how this has influenced their wellbeing. Additionally, further studies should investigate the generalizability capacity of a similar intervention in organizational contexts, such as schools, hospitals, and industries.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The study was approved by the Ethics Committee of Department of Brain and Behavioral Sciences (protocol code 49/2020 on 27 April 2020). The patients/participants provided their written informed consent to participate in this study.
Conceptualization: TF, SB, and LB. Data curation and writing—original draft: FB and TF. Formal analysis: FB, TF, AN, ER, and BC. Funding acquisition: LB. Methodology: TF and LB. Supervision: LB. Writing—reviewing and editing: TF, FB, AN, ER, GC, BC, GS, SB, GB, and LB. All authors have read and agreed to the published version of the manuscript. All authors contributed to the article and approved the submitted version.
We wish to thank the crowdfunding platform of the University of Pavia Universitiamo for helping us in the funding acquisition.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.914183/full#supplementary-material
Accoto, A., Chiarella, S. G., Raffone, A., Montano, A., Marco, A., de Mainiero, F., et al. (2021). Beneficial effects of mindfulness-based stress reduction training on the well-being of a female sample during the first total lockdown due to COVID-19 pandemic in Italy. Int. J. Environ. Res. Public Heal. 18, 5512. doi: 10.3390/IJERPH18115512
Arch, J., and Craske, M. (2010). Laboratory stressors in clinically anxious and non-anxious individuals: the moderating role of mindfulness. Behav. Res. Ther. 48, 495–505. doi: 10.1016/J.BRAT.2010.02.005
Baiano, C., Zappullo, I., Conson, M., Di Mauro, G., Petra, M., Piacenti, M., et al. (2020). Tendency to worry and fear of mental health during Italy's COVID-19 lockdown. Int. J. Environ. Res. Public Health 17, 1–8. doi: 10.3390/IJERPH17165928
Behan, C. (2020). The benefits of meditation and mindfulness practices during times of crisis such as COVID-19. Ir. J. Psychol. Med. 37, 1. doi: 10.1017/IPM.2020.38
Berryhill, M. B., Halli-Tierney, A., Culmer, N., Williams, N., Betancourt, A., King, M., et al. (2019). Videoconferencing psychological therapy and anxiety: a systematic review. Fam. Pract. 36, 53–63. doi: 10.1093/FAMPRA/CMY072
Bolton, A., and Dorstyn, D. (2015). Telepsychology for posttraumatic stress disorder: a systematic review. J. Telemed. Telecare 21, 254–267. doi: 10.1177/1357633X15571996
Bossi, F., Zaninotto, F., D'Arcangelo, S., Lattanzi, N., Malizia, A. P., and Ricciardi, E. (2022). Mindfulness-based online intervention increases well-being and decreases stress after Covid-19 lockdown. Sci. Rep. 12, 1–13. doi: 10.1038/s41598-022-10361-2
Bouchard, S., Paquin, B., Payeur, R., Allard, M., Rivard, V., Fournier, T., et al. (2004). Delivering cognitive-behavior therapy for panic disorder with agoraphobia in videoconference. Telemed. J. E. Health 10, 13–25. doi: 10.1089/153056204773644535
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., et al. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395, 912. doi: 10.1016/S0140-6736(20)30460-8
Bursky, M., Kosuri, M., Walsh Carson, K., Babad, S., Iskhakova, A., and Nikulina, V. (2021). The utility of meditation and mindfulness-based interventions in the time of COVID-19: a theoretical proposition and systematic review of the relevant prison, quarantine and lockdown literature. Psychol. Rep. 0, 196–44. doi: 10.1177/00332941211048734
Chiesa, A., Fazia, T., Bernardinelli, L., and Morandi, G. (2017). Citation patterns and trends of systematic reviews about mindfulness. Complement. Ther. Clin. Pract. 28, 26–37. doi: 10.1016/j.ctcp.2017.04.006
Cicchetti, D. V. (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess. 6, 284–290. doi: 10.1037/1040-3590.6.4.284
Cohen, S., Kamarck, T., and Mermelstein, R. (1983). A global measure of perceived stress. J. Health Soc. Behav. 24, 385–396. doi: 10.2307/2136404
Coleman, R. (2020). COVID-19 gender-based health worries, depressive symptoms, and extreme anxiety. J. Res. Gend. Stud. 10, 106. doi: 10.22381/JRGS10220206
Connor, J., Madhavan, S., Mokashi, M., Amanuel, H., Johnson, N. R., Pace, L. E., et al. (2020). Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: a review. Soc. Sci. Med. 266, 113364. doi: 10.1016/J.SOCSCIMED.2020.113364
Davico, C., Ghiggia, A., Marcotulli, D., Ricci, F., Amianto, F., and Vitiello, B. (2021). Psychological impact of the COVID-19 pandemic on adults and their children in Italy. Front. Psychiatry 12, 572997. doi: 10.3389/FPSYT.2021.572997
Desai, K., Gupta, P., Parikh, P., and Desai, A. (2021). Impact of virtual heartfulness meditation program on stress, quality of sleep, and psychological wellbeing during the COVID-19 pandemic: a mixed-method study. Int. J. Environ. Res. Public Health 18, 111114. doi: 10.3390/IJERPH182111114
Duan, L., and Zhu, G. (2020). Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry 7, 300. doi: 10.1016/S2215-0366(20)30073-0
Duncan, C. (2020). Gender-related depression, anxiety, and psychological stress experienced during the COVID-19 pandemic. J. Res. Gend. Stud. 10, 84. doi: 10.22381/JRGS10220204
Eberth, J., and Sedlmeier, P. (2012). The effects of mindfulness meditation: a meta-analysis. Mindfulness 3, 174–189. doi: 10.1007/s12671-012-0101-x
Favieri, F., Forte, G., Tambelli, R., and Casagrande, M. (2021). The Italians in the time of coronavirus: psychosocial aspects of the unexpected COVID-19 pandemic. Front. Psychiatry 12, 551924. doi: 10.3389/FPSYT.2021.551924
Fazia, T., Bubbico, F., Berzuini, G., Tezza, L. D., Cortellini, C., Bruno, S., et al. (2021). Mindfulness meditation training in an occupational setting: effects of a 12-weeks mindfulness-based intervention on wellbeing. Work 70, 1089–1099. doi: 10.3233/WOR-210510
Fazia, T., Bubbico, F., Iliakis, I., Salvato, G., Berzuini, G., Bruno, S., et al. (2020a). Short-term meditation training fosters mindfulness and emotion regulation: a pilot study. Front. Psychol. 11, 2828. doi: 10.3389/fpsyg.2020.558803
Fazia, T., Bubbico, F., Salvato, G., Berzuini, G., Bruno, S., Bottini, G., et al. (2020b). Boosting psychological well-being through a social mindfulness-based intervention in the general population. Int. J. Environ. Res. Public Health 17, 1–15. doi: 10.3390/ijerph17228404
Fino, E., Martoni, M., and Russo, P. M. (2021). Specific mindfulness traits protect against negative effects of trait anxiety on medical student wellbeing during high-pressure periods. Adv. Health Sci. Educ. Theory Pract. 26, 1095–1111. doi: 10.1007/S10459-021-10039-W
Fitt, S., and Rees, C. (2012). Metacognitive therapy for obsessive compulsive disorder by videoconference: a preliminary study. Behav. Chang. 29, 213–229. doi: 10.1017/BEC.2012.21
Germain, V., Marchand, A., Bouchard, S., Drouin, M., and Guay, S. (2009). Effectiveness of cognitive behavioural therapy administered by videoconference for posttraumatic stress disorder. Cogn. Behav. Ther. 38, 42–53. doi: 10.1080/16506070802473494
Giallonardo, V., Sampogna, G., Vecchio, V., Del L.uciano, M., Albert, U., Carmassi, C., et al. (2020). The impact of quarantine and physical distancing following COVID-19 on mental health: study protocol of a multicentric Italian population trial. Front. Psychiatry 11, 533. doi: 10.3389/FPSYT.2020.00533
Gidron, Y. (2013). “Trait Anxiety,” in Encyclopedia of Behavioral Medicine (New York, NY: Springer), 1989–1989. doi: 10.1007/978-1-4419-1005-9_1539
González-García, M., Álvarez, J. C., Pérez, E. Z., Fernandez-Carriba, S., and López, J. G. (2021). Feasibility of a brief online mindfulness and compassion-based intervention to promote mental health among university students during the COVID-19 pandemic. Mindfulness 12, 1685–1695. doi: 10.1007/S12671-021-01632-6
Gotink, R. A., Meijboom, R., Vernooij, M. W., Smits, M., and Hunink, M. G. M. (2016). 8-week mindfulness based stress reduction induces brain changes similar to traditional long-term meditation practice – a systematic review. Brain Cogn. 108, 32–41. doi: 10.1016/J.BANDC.2016.07.001
Graham, S. E. (2010). Using propensity scores to reduce selection bias in mathematics education research. J. Res. Math. Educ. 41, 147–168. Available online at: https://www.jstor.org/stable/20720129
Green, J., Huberty, J., Puzia, M., and Stecher, C. (2021). The effect of meditation and physical activity on the mental health impact of COVID-19-related stress and attention to news among mobile app users in the United States: cross-sectional survey. JMIR Ment. Heal. 8, e28479. doi: 10.2196/28479
Gremigni, P., and Stewart-Brown, S. (2011). Measuring mental well-being: Italian validation of the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS). G. Ital. di Psicol. 38, 485–505. doi: 10.1421/35174
Hayes, S. C., and Plumb, J. C. (2007). Mindfulness from the bottom up: providing an inductive framework for understanding mindfulness processes and their application to human suffering. Psychol. Inq. 18, 242–248. doi: 10.1080/10478400701598314
Ho, C. S., Chee, C. Y., and Ho, R. C. (2020). Mental health strategies to combat the psychological impact of coronavirus disease 2019 (COVID-19) beyond paranoia and panic. Ann. Acad. Med. Singap. 49, 155–160.
Ho, D., Imai, K., King, G., and Stuart, E. A. (2011). MatchIt: nonparametric preprocessing for parametric causal inference. J. Stat. Softw. 42, 1–28. doi: 10.18637/JSS.V042.I08
Holmes, E. A., O'Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., et al. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 7, 547. doi: 10.1016/S2215-0366(20)30168-1
Huang, Y., and Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 288, 112954. doi: 10.1016/J.PSYCHRES.2020.112954
Jaiswal, S., Muggleton, N., Juan, C., and Liang, W. (2019a). Indices of association between anxiety and mindfulness: a guide for future mindfulness studies. Personal. Neurosci. 2, e9. doi: 10.1017/PEN.2019.12
Jaiswal, S., Tsai, S. Y., Juan, C. H., Liang, W. K., and Muggleton, N. G. (2018). Better cognitive performance is associated with the combination of high trait mindfulness and low trait anxiety. Front. Psychol. 9, 627. doi: 10.3389/fpsyg.2018.00627
Jaiswal, S., Tsai, S. Y., Juan, C. H., Muggleton, N. G., and Liang, W. K. (2019b). Low delta and high alpha power are associated with better conflict control and working memory in high mindfulness, low anxiety individuals. Soc. Cogn. Affect. Neurosci. 14, 645–655. doi: 10.1093/scan/nsz038
Karasu, F., Öztürk Çopur, E., and Ayar, D. (2021). The impact of COVID-19 on healthcare workers' anxiety levels. Z. Gesundh. Wiss. 30, 1399–1409. doi: 10.1007/S10389-020-01466-X
Khoury, B., Sharma, M., Rush, S. E., and Fournier, C. (2015). Mindfulness-based stress reduction for healthy individuals: a meta-analysis. J. Psychosom. Res. 78, 519–528. doi: 10.1016/j.jpsychores.2015.03.009
Koolhaas, J. M., Bartolomucci, A., Buwalda, B., Boer, S. F., de Flügge, G., Korte, S. M., et al. (2011). Stress revisited: a critical evaluation of the stress concept. Neurosci. Biobehav. Rev. 35, 1291–1301. doi: 10.1016/J.NEUBIOREV.2011.02.003
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., et al. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 3, e203976. doi: 10.1001/JAMANETWORKOPEN.2020.3976
Lewis, E., and Zauskova, A. (2021). Prolonged stress, anxiety, and depression in medical staff during the COVID-19 crisis. Psychosociol. Issues Hum. Resour. Manag. 9, 21. doi: 10.22381/PIHRM9220212
Lunn, P. D., Belton, C. A., Lavin, C., McGowan, F. P., Timmons, S., and Robertson, D. A. (2020). Using behavioral science to help fight the coronavirus. J. Behav. Public Adm. 3, 1–15. doi: 10.30636/jbpa.31.147
Mankus, A., Aldao, A., Kerns, C., Mayville, E., and Mennin, D. (2013). Mindfulness and heart rate variability in individuals with high and low generalized anxiety symptoms. Behav. Res. Ther. 51, 386–391. doi: 10.1016/J.BRAT.2013.03.005
Marazziti, D., Pozza, A., Di Giuseppe, M., and Conversano, C. (2020). The psychosocial impact of COVID-19 pandemic in Italy: a lesson for mental health prevention in the first severely hit European country. Psychol. Trauma Theory, Res. Pract. Policy 12, 531–533. doi: 10.1037/TRA0000687
Matiz, A., Fabbro, F., and Crescentini, C. (2018). Single vs. group mindfulness meditation: effects on personality, religiousness/spirituality, and mindfulness skills. Mindfulness 9, 1236–1244. doi: 10.1007/s12671-017-0865-0
Matiz, A., Fabbro, F., Paschetto, A., Cantone, D., Paolone, A. R., and Crescentini, C. (2020). Positive impact of mindfulness meditation on mental health of female teachers during the COVID-19 outbreak in Italy. Int. J. Environ. Res. Public Health 17, 1–22. doi: 10.3390/IJERPH17186450
Ministero della Salute Norme circolari e ordinanze. Available online at: https://www.salute.gov.it/portale/nuovocoronavirus/archivioNormativaNuovoCoronavirus.jsp?lingua=italianoandiPageNo=55.
Moccia, L., Janiri, D., Pepe, M., Dattoli, L., Molinaro, M., Martin, V., et al. (2020). Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain. Behav. Immun. 87, 75. doi: 10.1016/J.BBI.2020.04.048
Mondo, M., Sechi, C., and Cabras, C. (2019). Psychometric evaluation of three versions of the Italian Perceived Stress Scale. Curr. Psychol. 40, 1–9. doi: 10.1007/s12144-019-0132-8
Murata, T., Takahashi, T., Hamada, T., Omori, M., Kosaka, H., Yoshida, H., et al. (2004). Individual trait anxiety levels characterizing the properties of zen meditation. Neuropsychobiology 50, 189–194.
Nickell, L. A., Crighton, E. J., Tracy, C. S., Al-Enazy, H., Bolaji, Y., Hanjrah, S., et al. (2004). Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. C. Can. Med. Assoc. J. 170, 793. doi: 10.1503/CMAJ.1031077
Nutting, R., Ofei-Dodoo, S., Rose-Borcherding, K., and Strella, G. (2022). Brief mindfulness intervention for emotional distress, resilience, and compassion in family physicians during COVID-19: a pilot study. Prim. Peer-Rev. Rep. Med. Educ. Res. 6, 3. doi: 10.22454/PRIMER.2022.746202
Orme-Johnson, D. W., and Barnes, V. A. (2014). Effects of the transcendental meditation technique on trait anxiety: a meta-analysis of randomized controlled trials. J. Altern. Complement. Med. 20, 330–341. doi: 10.1089/ACM.2013.0204
Pfefferbaum, B., and North, C. S. (2020). Mental health and the Covid-19 pandemic. N. Engl. J. Med. 383, 510–512. doi: 10.1056/NEJMP2008017
Phillips, A., and Kucera, J. (2021). Extreme anxiety, illness fears, and acute stress in COVID-19 Frontline healthcare professionals. Psychosociol. Issues Hum. Resour. Manag. 9, 35. doi: 10.22381/PIHRM9220213
Priyanka and Rasania, S. K. (2021). A cross–sectional study of mental wellbeing with practice of yoga and meditation during COVID-19 pandemic. J. Fam. Med. Prim. Care 10, 1576. doi: 10.4103/JFMPC.JFMPC_2367_20
R Core Team. (2017). R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria.
Rothman, K. J. (1990). No adjustments are needed for multiple comparisons. Epidemiology 1, 43–46. Available online at: http://www.ncbi.nlm.nih.gov/pubmed/2081237
Roy, D., Tripathy, S., Kar, S. K., Sharma, N., Verma, S. K., and Kaushal, V. (2020). Study of knowledge, attitude, anxiety and perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J. Psychiatr. 51, 102083. doi: 10.1016/J.AJP.2020.102083
Saladino, V., Auriemma, V., and Campinoti, V. (2022). Healthcare professionals, post-traumatic stress disorder, and COVID-19: a review of the literature. Front. Psychiatry 12, 2562. doi: 10.3389/FPSYT.2021.795221/BIBTEX
Saviola, F., Pappaianni, E., Monti, A., Grecucci, A., Jovicich, J., and De Pisapia, N. (2020). Trait and state anxiety are mapped differently in the human brain. Sci. Rep. 10, 11112. doi: 10.1038/s41598-020-68008-z
Sepúlveda-Loyola, W., Rodríguez-Sánchez, I., Pérez-Rodríguez, P., Ganz, F., Torralba, R., Oliveira, D., et al. (2020). Impact of social isolation due to COVID-19 on health in older people: mental and physical effects and recommendations. J. Nutr. Health Aging 24, 938–947. doi: 10.1007/S12603-020-1469-2
Spielberger, C. D. (1970). Manual for the State-trait Anxiety, Inventory. Palo Alto, CA: Consulting Psychologists.
Spielberger, C. D. (1972). Anxiety. Current Trends in Theory and Research. New York, NY: Academic Press.
Spielberger, C. D., Gorsuch, R. L., Lushene, R. E., Vagg, P., and Gerard, A. J. (1983). Manual for the State-trait Anxiety, Inventory. Palo Alto, CA: Consulting Psychologists.
Su, S., Wong, G., Shi, W., Liu, J., Lai, A. C. K., Zhou, J., et al. (2016). Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol. 24, 490–502. doi: 10.1016/j.tim.2016.03.003
Sun, L., Sun, Z., Wu, L., Zhu, Z., Zhang, F., Shang, Z., et al. (2020). Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China. medRxiv 2020.03.06.20032425. doi: 10.1101/2020.03.06.20032425
Swalwell, C., Pachana, N. A., and Dissanayaka, N. N. (2018). Remote delivery of psychological interventions for Parkinson's disease. Int. Psychogeriatrics 30, 1783–1795. doi: 10.1017/S1041610218000340
Taoka, R., Matsunaga, H., Kubo, T., Suzuki, T., and Yamamoto, S. (2014). Impact of trait anxiety on psychological well-being in men with prostate cancer. Int. Braz. J. Urol. 40, 620–626. doi: 10.1590/S1677-5538.IBJU.2014.05.06
Tennant, R., Hiller, L., Fishwick, R., Platt, S., Joseph, S., Weich, S., et al. (2007). The Warwick-Dinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual. Life Outcomes 5, 63. doi: 10.1186/1477-7525-5-63
Théberge-Lapointe, N., Marchand, A., Langlois, F., Gosselin, P., and Watts, S. (2015). Efficacy of a cognitive-behavioural therapy administered by videoconference for generalized anxiety disorder. Eur. Rev. Appl. Psychol. 65, 9–17. doi: 10.1016/J.ERAP.2014.10.001
Vloo, A., Alessie, R. J. M., Mierau, J. O., Boezen, M. H., Mierau, J. O., Franke, L., et al. (2021). Gender differences in the mental health impact of the COVID-19 lockdown: longitudinal evidence from the Netherlands. SSM – Popul. Heal. 15, 100878. doi: 10.1016/J.SSMPH.2021.100878
World Health Organization Coronavirus disease (COVID-19) pandemic. (2019). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019?gclid=Cj0KCQjwlvT8BRDeARIsAACRFiW_AoKe8cr7J7MyGq46ojb4LEDnznIAUBkEXISSPxIfKCLbfmxjYgUaAriBEALw_wcB
World Health Organization Listings of WHO's response to COVID-19. (2020). Available online at: https://www.who.int/news/item/29-06-2020-covidtimeline
Zhu, N., Zhang, D., Wang, W., Li, X., Yang, B., Song, J., et al. (2020). A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382, 727–733. doi: 10.1056/nejmoa2001017
Zoom Video Communications Inc. Global Infrastructure Security Guide Global Infastructure Security Guide . (2016). Available online at: https://zoom.us/
Keywords: mindfulness-based meditation, psychological wellbeing, COVID-19, lockdown, trait anxiety, state anxiety, stress
Citation: Fazia T, Bubbico F, Nova A, Riggi E, Caimi G, Calgan B, Salvato G, Bruno S, Bottini G and Bernardinelli L (2022) Online Short-Term Mindfulness-Based Intervention During COVID-19 Quarantine in Italy: Effects on Wellbeing, Stress, and Anxiety. Front. Psychol. 13:914183. doi: 10.3389/fpsyg.2022.914183
Received: 07 April 2022; Accepted: 10 June 2022;
Published: 04 July 2022.
Edited by:
Luca Simione, National Research Council (ISTC-CNR), ItalyReviewed by:
Hyochol Ahn, Florida State University, United StatesCopyright © 2022 Fazia, Bubbico, Nova, Riggi, Caimi, Calgan, Salvato, Bruno, Bottini and Bernardinelli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Teresa Fazia, VGVyZXNhLmZhemlhMDFAYXRlbmVvcHYuaXQ=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.