- 1Department of Chinese Medicine, Dalin Tzuchi Hospital, The Buddhist Tzuchi Medical Foundation, Chiayi, Taiwan
- 2Department of Biomedical Sciences, National Chung Cheng University, Chiayi, Taiwan
- 3Rehabilitation Counseling Program, Portland State University, Portland, OR, United States
- 4Department of Rehabilitation, Dalin Tzuchi Hospital, The Buddhist Tzuchi Medical Foundation, Chiayi, Taiwan
- 5Epigenomics and Human Diseases Research Center, National Chung Cheng University, Chiayi, Taiwan
- 6Division of Allergy, Immunology and Rheumatology, Dalin Tzuchi Hospital, The Buddhist Tzuchi Medical Foundation, Chiayi, Taiwan
- 7School of Medicine, Tzu Chi University, Hualien, Taiwan
- 8School of Post-Baccalaureate Chinese Medicine, Tzu Chi University, Hualien, Taiwan
- 9Department of General Surgery, Dalin Tzuchi Hospital, The Buddhist Tzuchi Medical Foundation, Chiayi, Taiwan
- 10Department of Environmental and Occupational Health, College of Medicine, National Cheng Kung University, Tainan, Taiwan
- 11Department of Nursing, Tzu Chi University of Science and Technology, Hualien, Taiwan
- 12Department of Medical Research, Dalin Tzuchi Hospital, The Buddhist Tzuchi Medical Foundation, Chiayi, Taiwan
Background: Breast cancer patients are at elevated risk of depression during treatment, thus provoking the chance of poor clinical outcomes. This retrospective cohort study aimed to investigate whether integrating Chinese herbal medicines citation(CHM) into conventional cancer therapy could decrease the risk of depression in the long-term breast cancer survivors.
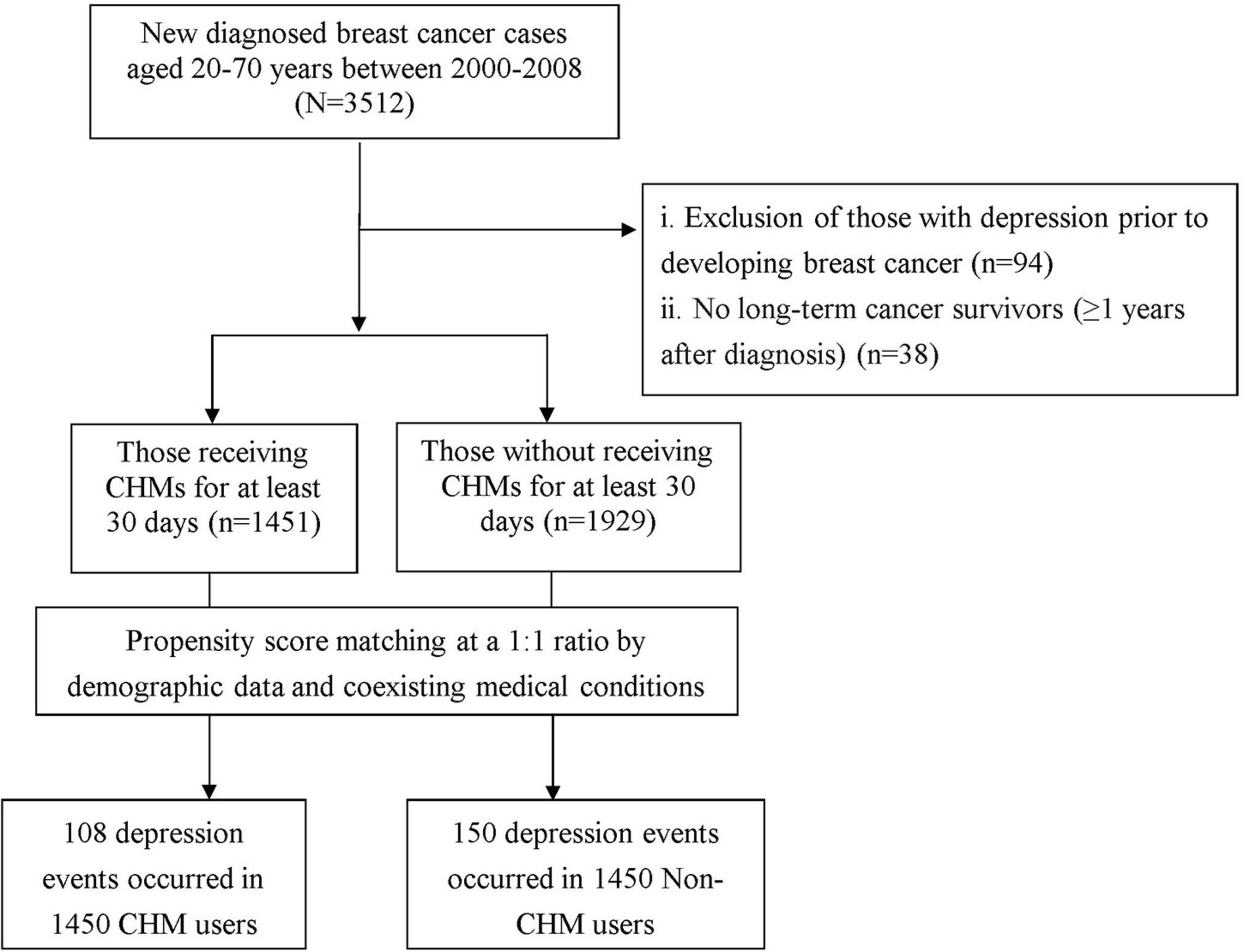
Methods: A cohort of patients aged 20–70 years and with newly diagnosed breast cancer during 2000–2008 was identified from a nationwide claims database. In this study, we focused solely on survivors of breast cancer at least1 year after diagnosis. After one-to-one matching for age, sex, and baseline comorbidities, breast cancer patients who received (n = 1,450) and did not receive (n = 1,450) CHM treatment were enrolled. The incidence rate and hazard ratio citation(HR) for depression between the two groups was estimated at the end of 2012. A Cox proportional hazard model was constructed to examine the impact of the CHM use on the risk of depression.
Results: During the study period, the incidence rate of depression was significantly lower in the treated cohort than in the untreated cohort [8.57 compared with 11.01 per 1,000 person-years citation(PYs)], and the adjusted HR remained significant at 0.74 (95% CI 0.58–0.94) in a Cox proportional hazards regression model. The corresponding risk further decreasing to 43% among those using CHM for more than 1 year.
Conclusion: Finding from this investigation indicated that the lower risk of depression observed in breast cancer patients treated with CHM, suggesting that CHM treatment should be considered for disease management toward breast cancer. Yet, the optimal administered dose should be determined in further clinical trials.
Introduction
Depression is a chronic medical condition that impacts the cognitive, affective and physical wellbeing of a person (Cui, 2015). Globally, depression affects approximately 350 million people (Cross et al., 2014), and is particularly common among people with chronic and life-threatening diseases, especially in patients affected by cancer (Delgado-Guay et al., 2009). Recently, the advances in treatment modalities have improved the survival for cancer survivors; nevertheless, the higher survival rate does not represent that they have successfully adapted or positively coped with the cancer. In contrast, the profound functional and visible changes resulting from such treatments, including surgery, chemotherapy, and radiation therapy, can insidiously lead to the onset of psychiatric disorders throughout the cancer experience (Chan et al., 2015).
Breast cancer is the most common form of malignancy in women, and affected patients are at a higher likelihood of experiencing depression, a condition aggravated by the necessity to undergo continuous life-saving treatments. After administering their cancer-related questionnaire to 179 women with breast cancer, Kamińska et al. (2015) found that breast cancer surgeries contributed to a higher prevalence of depression, reaching 64% for women who underwent mastectomy and 52.4% for women who had breast conserving treatment. Additionally, one recent meta-analysis of 18 studies, representing different countries, disclosed that estimated depression prevalence among these women ranged from 14 to 95.9%, with a pooled average of 46.83% (Ahmadi Gharaei et al., 2019). Notably, once individuals with breast cancer develop concomitant depression, their medical costs increased by nearly 200% (Mausbach et al., 2018). Worse yet, further aggravating these findings, their likelihood of mortality compared to patients with cancer alone was reported to more than double (Chan et al., 2015). These alarming data suggest that interventions geared toward minimizing the likelihood of depression are of utmost importance during cancer therapy.
Chinese herbal medicine citation(CHM) has shown promising results in improving the body’s ability to fight malignant disease. Several of these herbs were further proven to improve cognitive function through the suppression of monoamine oxidase activity and oxidative stress as well as the modulation of the hypothalamic-pituitary-adrenal axis activation (Zhang et al., 2018; Ahmadi Gharaei et al., 2019). Take use of Shao-Yao-Gan-Cao-Tang as an example, it has been found to have a beneficial effect on reducing emotional distress owing to its ingredients of Paeonia lactiflora Pall, and Glycyrrhiza uralensis (Liu C. T. et al., 2017; Chen et al., 2018). The latter ingredient even was proved to exert antidepressant effects on depressive rat model via regulating HPA Axis and the level of amino acids neurotransmitters (Wang et al., 2008). In this context, these biological activities of CHM may be of value for managing depression in patients with breast cancer. As of now, to the best of our knowledge, no study has so far investigated the long-term effects of CHM on depression prevention in breast cancer patients. To address this issue, we used administrative data to create an objective measure to determine if adding CHM into the conventional therapy could lower the incidence of depression among breast cancer patients.
Materials and methods
Data source and identification of patients with breast cancer
Taiwan’s NHI program, launched in 1995, is a single-payer government-operated compulsory health insurance program. As of 2015, up to 99.6% of Taiwan’s population was enrolled in the NHI program Research data for this retrospective cohort study were obtained from the Longitudinal Health Insurance Database citation(LHID) administered by the Ministry of Health and Welfare. The LHID contains data on one million beneficiaries randomly sampled from the Registry for Beneficiaries of the NHI Research Database. The use of multistage stratified systematic sampling ensures no significant deviations in the distribution of sex and age between the LHID enrollees and the general population (The National Health Research Institutes, 2002). The claim files include inpatient and outpatient demographics, primary and secondary diagnoses, procedures, prescriptions, and medical expenditures. The Ministry of Health and Welfare manages the claims data and provides scrambled random identification numbers for insured patients to protect their privacy. Accordingly, the Institutional Review Board and Ethics Committee of Buddhist Dalin Tzu Chi Hospital approved this study and waived informed consents for all the enrollees (No. B10004021-2).
In the present study, we used the ambulatory and inpatient data of LHID from 2000 to 2008 to identify subjects with breast cancer and being free of depression diagnosis at baseline. We used the International Classification of Diseases-Ninth Revision-Clinical Modification (ICD-9-CM) code for the identification of patients with breast cancer. Patients aged 20–70 years who were newly diagnosed with breast cancer (ICD-9-CM code: 174) were considered for enrollment in the study. To ensure the identification of new breast cancer cases, we employed a 4-year washout period (1996–1999) to exclude any patients who had been diagnosed with breast cancer before entering the cohort (n = 3,512). Meanwhile, to reduce the potential for disease misclassification, only those with catastrophic illness certification due to breast cancer were recruited. In Taiwan, insured persons with major chronic conditions can apply for catastrophic illness certification that grants exemption from co-payment. The date on which the patient gained approval for catastrophic illness registration due to breast cancer was considered the index date (Figure 1).
Outcome of interest
The study outcome was the first diagnosis of depression, which included major depressive disorder (ICD-9-CM codes: 296.2 and 296.3), dysthymic disorder (ICD-9-CM code: 300.4), and depressive disorder not elsewhere classified (ICD-9-CM code: 311). In this study, the diagnosis of depression was determined if patients were treated with ≧ 3 outpatient treatment claims or ≧1 hospitalization due to depression. We then excluded those who had a prior diagnosis of depression before the breast cancer onset (n = 94), and those followed up for less than 1 year after diagnosis of breast cancer (n = 38). Afterward, the final cohort included 3,380 patients.
Exposure of Chinese herbal medicines
Under the NHI program in Taiwan, only certified Chinese medicine physicians are allowed to provide CHM treatment. Based on the formerly established methods, CHM users were identified as those who ever received CHM due to breast cancer for more than 30 days, whereas those treated for 30 days or less were considered to be non-CHM users (Tsai et al., 2016; Li et al., 2019). After this algorithm, 1,451 subjects were classified as CHM users. A comparison cohort was randomly selected from the remaining enrollees who did not receive CHM. For each patient receiving CHM, one patient who did not receive CHM was selected via one-to-one propensity score matching. The propensity score value, the predicted probability of CHM exposure, was calculated using logistic regression on the basis of patients’ demographics as shown in Table 1, including age, sex, monthly income, residential area, and comorbidities. Every CHM user was randomly matched with a non-CHM user who had the nearest propensity score, where the difference in the score ranged between –0.1 and + 0.1 (Austin, 2011). Furthermore, to consider immortal time bias (Shariff et al., 2008), the index date for the follow-up period was the date of CHM treatment initiation or, for non-CHM users, the date of the initial breast cancer diagnosis. All patients were followed up to the end of 2012 to confirm depression status. The follow-up time, in PY, was determined by calculating the time interval from the index date to the earliest of the following end points: diagnosis of depression, date of withdrawal from the insurance citation(including death), or the date of December 31, 2012.
Definition of covariates
Covariates in the regression model contained the age, sex, insured amount, urbanization level of enrollee’s residential area, former comorbidities, and medication usage. Regarding insured amount, it was calculated from the patients’ average monthly income and thus, also served as an economic index. Insured income amounts were transformed to ordinal variables according to the ≤ New Taiwan Dollar citation(NTD) 17800, NTD 17,881–43,900, and ≥ NTD $43901. As to the urbanization level, it was calculated according to a published scheme that classified 359 communities in Taiwan into seven stratums, with a higher level indicating a higher degree of urbanization. The classification scheme included the population density, proportion of persons with a college-level education or higher, proportion of elderly residents, proportion of agricultural workers, and number of physicians per 100,000 population. In this work, the urbanization degree was grouped into three strata: urban (levels 1–2), suburban (levels 3–4), and rural (levels 5–7) (Liu et al., 2006). The influence of baseline comorbidities was considered according to medical records during the year preceding cohort entry, using the Charlson-Deyo Comorbidity Index (CCI) (Deyo et al., 1992). The sum of these scores was regarded as a continuous variable for the burden of comorbidities, with higher scores indicating a more severe impact of these comorbidities. To avoid duplicate counting, and possible over-adjustment in the regression model, the diagnoses of relevant tumor were excluded from the CCI score.
Statistical analysis
Data were analyzed using SAS version 9.3 software (SAS Institute Inc., Cary, NC, United States). Distributions of sociodemographic data and comorbidities between the CHM users and non-CHM users were compared by using the chi-square and Student’s t-test. Then we conducted a Cox proportional hazards regression analysis to compute the adjusted hazard ratio citation(HR) with 95% confidence interval citation(CI) of risk of depression in association with CHM use, after adjusting for age, sex, insurance premium (an indicator of income), urbanization level, and CCI simultaneously in the model. To test the robustness of the relationship between CHM use and depression risk, all CHM users were divided into two groups based on time of CHM use: (1) 31–365 days, and (2) ≥ 366 days. The Kaplan–Meier method was used to estimate the cumulative risk of depression in each group, and the difference between groups was assessed using the log-rank test. The proportional hazards assumption was examined by plotting the log [–log (survival function)] vs. the log citation(survival time). A P < 0.05 was considered statistically significant.
Results
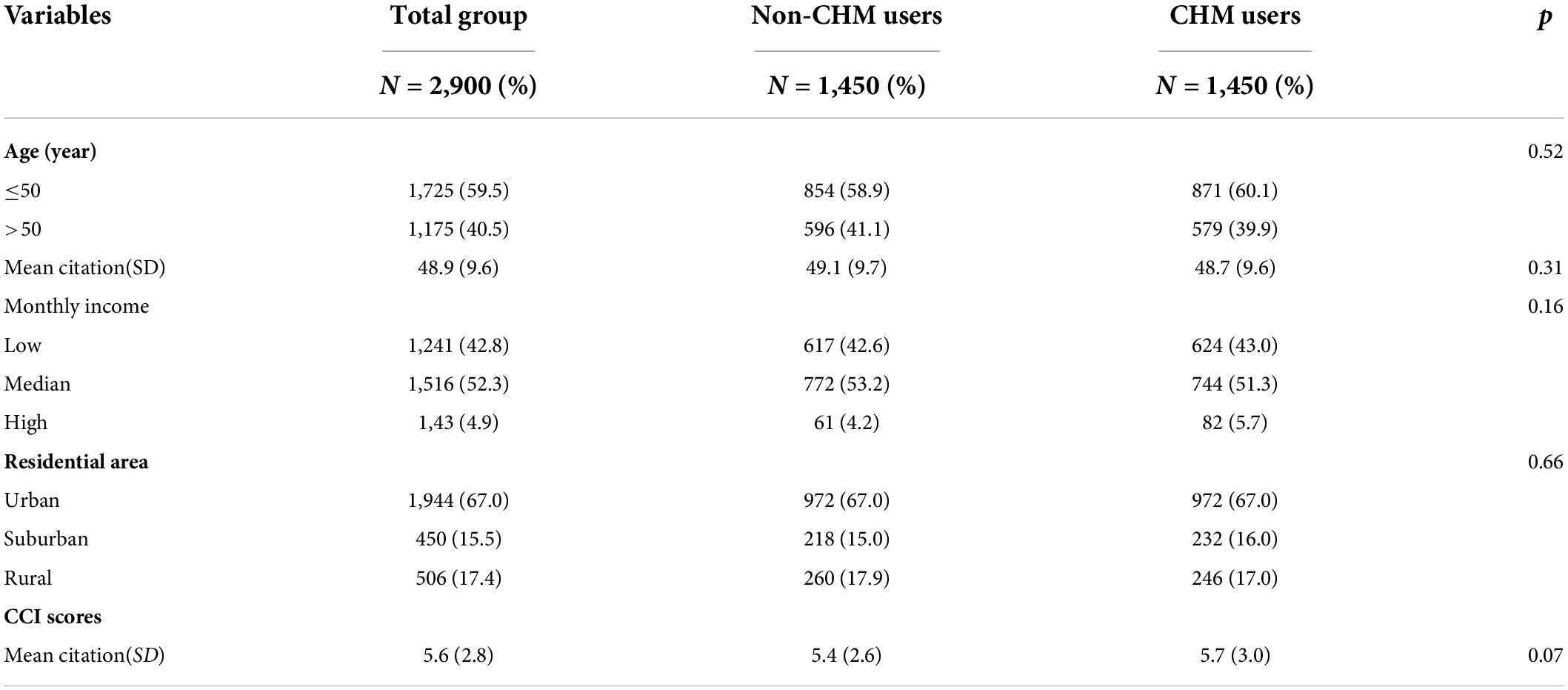
Data were analyzed for CHM users (n = 1,450) and non-CHM users (n = 1,450). Demographic data are shown in Table 1. The mean age of the enrollees was 48.9 ± 9.6 years. The majority of participants had monthly income level of NTD 17,881–43,900 (52.3%) and lived in urbanized areas (82.5%). Regarding comorbidities, the mean CCI score was 5.6 (± 2.8). No significant differences were found between two groups in relation to age, monthly income, residential area, or CCI score after PS matching, showing that the baseline characteristics between two groups were comparable.
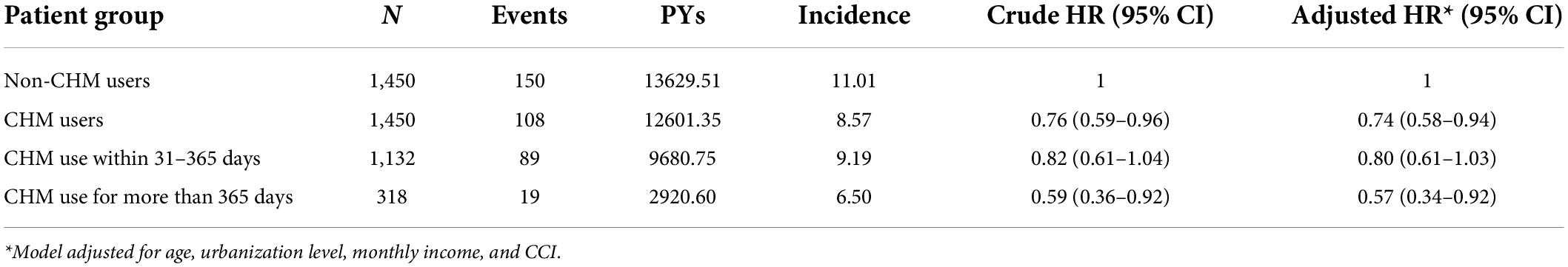
In the full cohort, 258 first episodes of depression were identified: 150 in non-CHM users and 108 in CHM users during the follow-up period of 13,629.51 and 12,601.35 person-years citation(PYs), respectively. The incidence of depression was significantly lower among CHM users than non-CHM users (8.57 vs. 11.01 per 1,000 PY, respectively) (adjusted HR = 0.76; 95% CI 0.59–0.96) (Table 2). The use of CHM for more than 1 year was associated with a 43% lower risk of depression. Kaplan–Meier survival curves and log-rank analysis showed a significant difference in survival rate free from depression across three groups during the follow-up period (P < 0.01) (Figure 2).
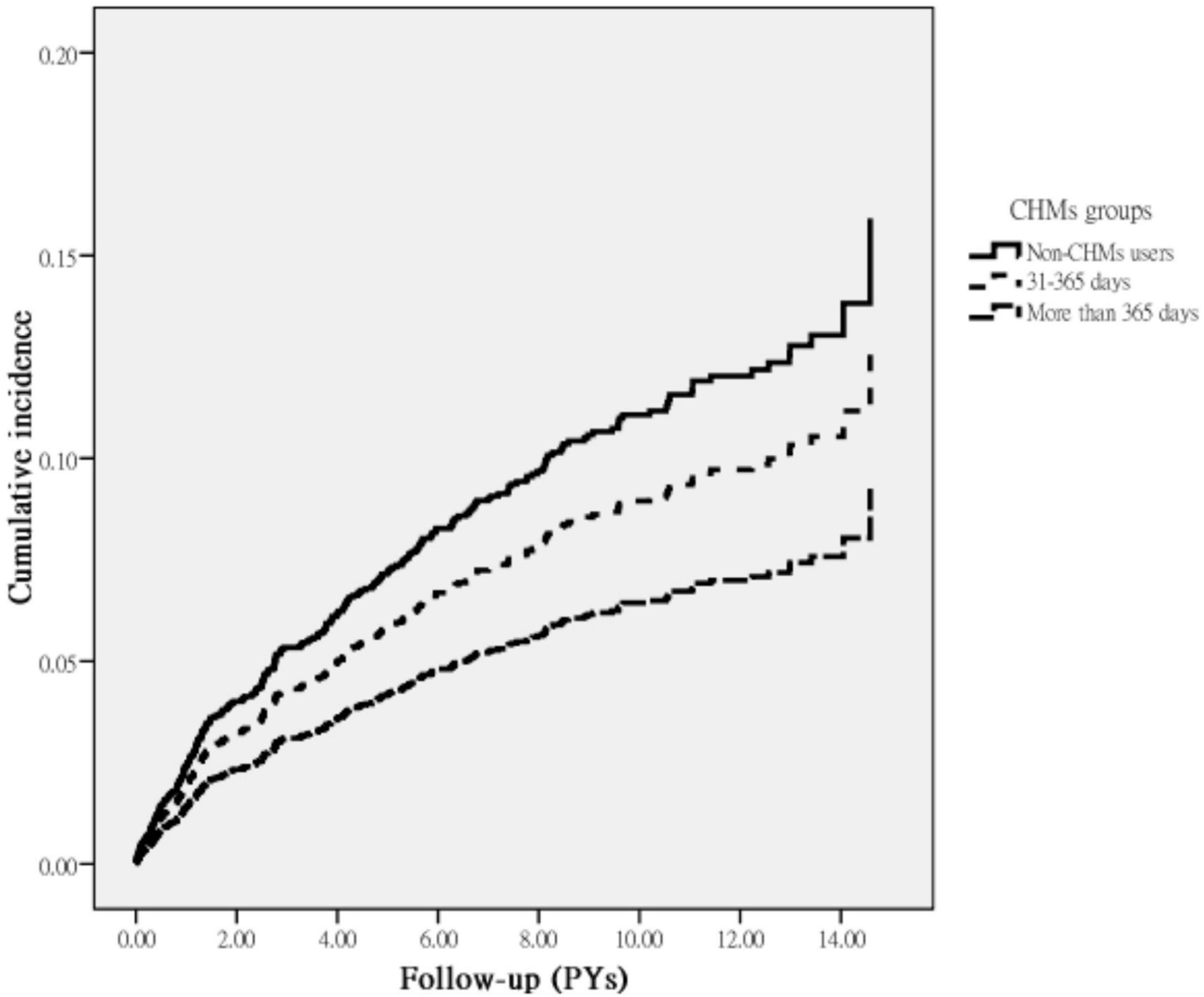
Figure 2. Cumulative incidence of depression in breast cancer patients with and without receiving CHM treatment during the study period (Log-rank test, P = 0.02).
The most commonly prescribed Chinese herbal products for breast cancer patients are summarized in Table 3. A total of five formulas for the breast cancer treatment were found to substantially lessen the subsequent risk of depression and summarized in Figure 3: Ge Gen citation(Puerariae Lobatae Radix), Xiang Fu citation(Cyperi Rhizoma), Bai-Hua-She-She-Cao citation(Hedyotidis Herba), Shao-Yao-Gan-Cao-Tang citation(Paeoniae Radix Alba, Glycyrrhizae Radix et Rhizoma), and Yin-Qiao-San (Forsythiae Fructus, Lonicerae Japonicae Flos, Platycodonis Radix, Menthae Haplocalycis Herba, Lophatheri Herba, Glycyrrhizae Radix et Rhizoma, Schizonepetae Herba, Sojae Semen Praeparatum, Arctii Fructus).

Table 3. Risk of depression in relation to the 10 most-used single-herb and multi-herb CHM products for participants.
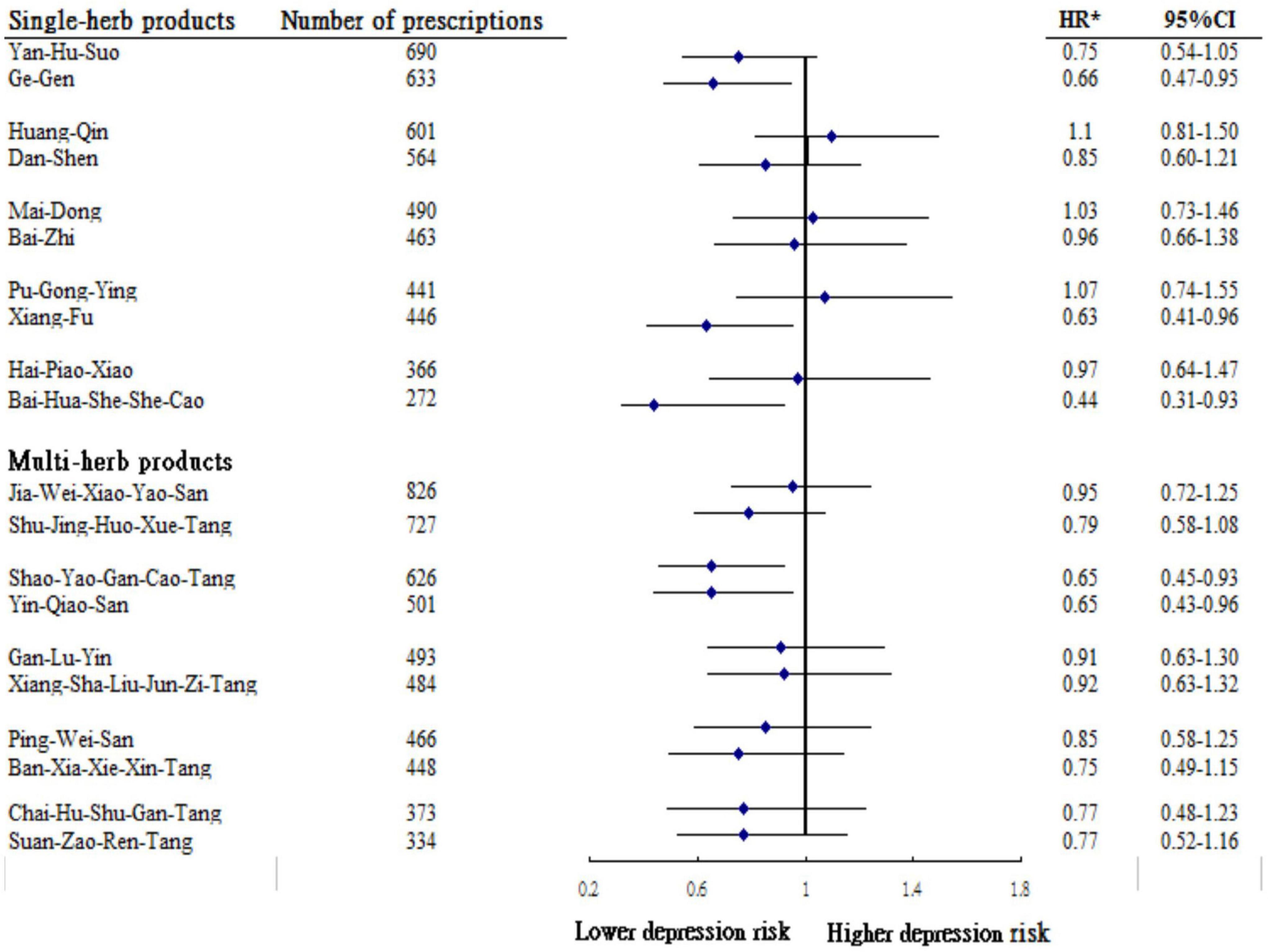
Figure 3. Risk of depression in relation to the top 10 most-used single-herb and multi-herb products among studying participants. *Model adjusted for age, urbanization level, monthly income and CCI.
Discussion
In this evidence-based cohort study exploring the relationship between CHM use and subsequent depression risk in breast cancer patients, we found that patients receiving CHM had a nearly 25% lower risk of depression than did those not using CHM. Furthermore, those receiving CHM for more than 365 days were found to have a significantly lower risk of depression by 43%. Through the determination of dose-response relation between an exposure citation(CHM use) and the risk of an outcome citation(depression incident), it may indeed support the causal association between the intensity of CHM use and the resultant lower risk for depression among breast cancer patients.
No previous studies have reported the long-term influence of CHM on depression risk in breast cancer patients, thus precluding comparison of results. Nevertheless, the positive therapeutic effect of CHM observed in this work adds to the accumulating evidence suggesting that CHM exerts antidepressant effects by modulating dysfunctional neurotransmission (So et al., 2015). Proposed mechanisms by which CHM use might decrease the risk of developing depression include the inhibition of the monoamine oxidase activity and oxidative stress, upregulation of neurotrophins, and modulation of hypothalamic-pituitary-adrenal axis function (Dowlati et al., 2010; Wang Y. et al., 2019).
A major contribution of this study is the identification of specific CHM products associated with the observed lower risk of depression in breast cancer patients. We found that three single-product CHM commonly used to treat breast cancer were associated with a lower sequent risk of depression, like use of Ge-gen, Xiang-fu, and Bai-hua-she-she-cao. A previous study using an animal model reports that Pueraria, the principal ingredient of Ge-gen, exerted marked anti-depressant effects by abating nuclear factor kappa beta (NF-κB) signaling (Chang et al., 2009). NF-κB is a critical transcriptional regulator of inflammatory response induction (Liu T. et al., 2017), and a decrease in such signaling thereby decreases the vulnerability to depression.
Xiang-fu is a cytotoxic herb that inhibits cell growth and promotes apoptosis of breast cancer cells (Park et al., 2014; Mannarreddy et al., 2017; Simorangkir et al., 2019; Suryavanshi et al., 2019; Wang F. et al., 2019). A recent in vivo study by Zhou et al. (2016) showed that two new cycloartane glycosides from the rhizomes of Xiang-fu were beneficial in modulating the function of brain-derived neurotrophic factor in the hippocampus, a compound known to promote synaptic efficacy, neuronal connectivity, and neuroplasticity, which in turn decrease the risk of depression.
Another commonly used single-herb product, Bai-Hua-She-She-Cao (Hedyotis diffusa), is commonly used to relieve heat and toxicity in cancer patients (Zhang et al., 2017). Recent animal experiments and human studies have shown that the administration of Bai-Hua-She-She-Cao may markedly suppress cancer cell proliferation and induced apoptosis by modulating pro-inflammatory cytokines (Ye et al., 2015; Zhang et al., 2017), which may account for its therapeutic effect of preventing the onset of psychiatric disorders, including depression.
With regard to multi-herb products, the use of Shao-Yao-Gan-Cao-Tang was observed to be associated with a decreased risk of depression in our cohort. A previous study reported that an active component of Shao-Yao-Gan-Cao-Tang decoction, such as glycyrrhizin, affected multiple biological processes and pathways that participate in neuron apoptosis and inflammatory responses (Chen et al., 2018), all of which play key roles in the pathogenesis of depression (Dowlati et al., 2010). Another commonly used CHM product, Yin-Qiao-San, is used to relieve external symptoms and clear pathogenic heat from the body in clinical practice. This herbal product was proven to prevent drug-induced pulmonary fibrosis in a mice model by decreasing the plasma levels of inflammatory cytokines, like TNF-α, interleukin citation(IL)-1, and IL-6 (Yeh et al., 2007); these mediators have been implicated in the development of depression (Dowlati et al., 2010).
As previously described in “Materials and methods” section, the database used in this study has several strengths, including its large sample size, the use of electronic records from a national health insurance registry, and a uniform approach to outcome assessment, all of which could strengthen validity of the study findings. On top of that, the selection bias ought to be minimized to a great extent by using data from the NHI database, which included over 99% of insured persons in Taiwan. Nonetheless, several limitations of this study merit attention. First, our findings were derived from analysis of retrospective cohort data based on ICD-9-CM diagnostic codes. Thus, relevant cases may have been misclassified. To improve diagnostic accuracy and avoid overestimation of the prevalence of cases of interests, we applied a 4-year washout period for breast cancer, where patients with a diagnosis of breast cancer during that period were considered prevalent and, therefore, excluded from analyses. Medical records were confirmed by requiring at least 3 outpatient service claims, or at least 1 inpatient hospitalization claim during the study period. Additionally, the diagnostic inclusion of breast cancer was further verified by the catastrophi illness certification. The NHI of Taiwan randomly reviews the charts and audits medical charges to verify the accuracy of claims. Despite this procedure, we recognize that the misclassification of cases is always a risk in database research, but this would be expected to occur at random which would likely serve to only bias the overall HR observed toward the null value and thus provide a more conservative estimate of effect. Second, data used in this study were drawn from a claim-based database and, accordingly, no detailed clinical information regarding laboratory data, family history, physical activity, and individual social network relationship was available. Thus, future studies that examine the influence of these variables are worthy of pursuit. Nevertheless, to carefully address the confounding by indication that may arise in this real-world comparative effectiveness study, we have capitalized on propensity score—matched analysis to analyze the association of CHM use with the attack of depression. For each breast cancer patient who received CHM, one control patient was selected by 1:1 matching, based on a propensity score. Additionally, to more robustly assess if other treatments may affect the finding herein, we reanalyzed the relationships between CHM use and subsequent risk of depression by adjusting for the utilization numbers of radiotherapy after breast cancer onset. The rational underlying this procedure was based on the assumption that radiotherapy for breast cancer patients is an obligatory component of a breast-conserving treatment modality and could cause deleterious psychological symptoms in such a group of patients (Almasri and Rimawi, 2020; Piroth et al., 2022). The re-analysis indicated that, as compared to breast cancer patients who did not receive CHM, the selected breast cancer patients who received CHM still had a significantly lower risk for depression (adjusted HR: 0.75; 95% CI = 0.59–0.89). Third, other indicators of comorbidities, aside from CCI score, deserve further investigation while examining the association of depression with CHM use, among such group. Fourth, a surveillance bias might arise with this type of exploration, as CHM users may be more likely than their control counterparts to seek medical care. To address this issue, we calculated the frequency of medical visits for each study subject and adjusted this variable in the multivariate regression model. After adjustment, findings from the reanalysis indicated that the positive effect of CHM still remained unchanged, with an adjusted HR of 0.79 (95% CI = 0.62–0.96), suggesting that the number of ambulatory care visits did not appreciably affect the conclusion herein. Fifth, due to the anonymity of identification numbers in the database, we were unable to directly contact the enrolled patients regarding their methods of taking CHM products. However, nearly 95% of the dose frequencies in Chinese herbal products are typically used for only 1 week in clinical practice, so those who continued to receive the same prescription for a longer period of time were, therefore, likely to have used the prescribed medications (Lai et al., 2010). Additionally, prescriptions for medications issued before NHI initiation were not reflected in the data analysis in the present study. This omission may result in underestimating the cumulative frequencies and may have weakened the effect of the specified CHM products. Last, although our study revealed a substantial association between CHM use and a decreased risk of depression among breast cancer patients, it must be recognized that participants were not initially randomly categorized into users and non-users and were recruited from a single country only. Therefore, a randomized controlled trial to test the effects of those commonly used herbal products in treating breast cancer patients is warranted, thus paving the way for further personalized therapies and clinical trials on the use of adjunctive therapy for the management of other types of malignancies.
Conclusion
Individuals with breast cancer suffer from the mood disorders more frequently than the general population, especially depression. This is the first population-based survey that rigorously evaluated the impact of CHM use on the prevention of depression among them. We found that integration of CHM into the conventional treatment regimen for breast cancer for more than 2 years may reduce the subsequent risk of depression by nearly 50%. This noteworthy finding can provide an impetus for further research venues, such as focusing on factors associated with utilization of CHM, as well as in vivo studies that attempt to uncover the main mechanisms of prescribed herbal formulae that may be beneficial for such groups.
Data availability statement
The data supporting the conclusion of this study are available from the authors, but the raw data (NHIRD) needs to be obtained from the National Health Research Institute of Taiwan through an application process upon approval, further inquiries should be directed to the corresponding author.
Ethics statement
This study was approved by the Research of Ethics Committee of Dalin Tzuchi Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
SY-Y, C-CY, C-KW, and T-YT: conception and design. M-CL and T-YT: provision of study material and patients. HL and T-YT: collection and assembly of data. SY-Y, HL, JS-J, S-WY, C-KW, and T-YT: data analysis and interpretation. SY-Y, HL, JS-J, S-WY, H-LH, MC, C-CY, C-KW, and T-YT: manuscript writing. SY-Y, HL, JS-J, S-WY, H-LH, MC, M-CL, C-CY, C-KW, and T-YT: final approval of manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
This study was based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by the National Health Research Institutes, Taiwan.
Author’s disclaimer
The interpretation and conclusions contained herein do not represent those of the Bureau of National Health Insurance, Department of Health, and National Health Research Institutes.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ahmadi Gharaei, H., Dianatinasab, M., Kouhestani, S. M., Fararouei, M., Moameri, H., Pakzad, R., et al. (2019). Meta-analysis of the prevalence of depression among breast cancer survivors in Iran: An urgent need for community supportive care programs. Epidemiol. Health 41:e2019030. doi: 10.4178/epih.e2019030
Almasri, H., and Rimawi, O. (2020). Assessment of depression and anxiety in breast cancer patients undergoing radiotherapy in palestine. SN Compr. Clin. Med. 2, 2787–2791. doi: 10.1007/s42399-020-00635-z
Austin, P. C. (2011). Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharmaceut. Stat. 10, 150–161. doi: 10.1002/pst.433
Chan, C. M., Wan Ahmad, W. A., Yusof, M. M., Ho, G. F., and Krupat, E. (2015). Effects of depression and anxiety on mortality in a mixed cancer group: A longitudinal approach using standardised diagnostic interviews. Psychooncology 24, 718–725. doi: 10.1002/pon.3714
Chang, Y., Hsieh, C. Y., Peng, Z. A., Yen, T. L., Hsiao, G., Chou, D. S., et al. (2009). Neuroprotective mechanisms of puerarin in middle cerebral artery occlusion-induced brain infarction in rats. J. Biomed. Sci. 16:9. doi: 10.1186/1423-0127-16-9
Chen, I. C., Lin, T. H., Hsieh, Y. H., Chao, C. Y., Wu, Y. R., Chang, K. H., et al. (2018). Formulated Chinese medicine shaoyao gancao tang reduces tau aggregation and exerts neuroprotection through anti-oxidation and anti-inflammation. Oxid. Med. Cell. Longev. 2018:9595741. doi: 10.1155/2018/9595741
Cross, M., Smith, E., Hoy, D., Carmona, L., Wolfe, F., Vos, T., et al. (2014). The global burden of rheumatoid arthritis: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 73, 1316–1322. doi: 10.1136/annrheumdis-2013-204627
Cui, R. (2015). Editorial: A systematic review of depression. Curr. Neuropharmacol. 13:480. doi: 10.2174/1570159x1304150831123535
Delgado-Guay, M., Parsons, H. A., Li, Z., Palmer, J. L., and Bruera, E. (2009). Symptom distress in advanced cancer patients with anxiety and depression in the palliative care setting. Support. Care Cancer 17, 573–579. doi: 10.1007/s00520-008-0529-7
Deyo, R. A., Cherkin, D. C., and Ciol, M. A. (1992). Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 45, 613–619. doi: 10.1016/0895-4356(92)90133-8
Dowlati, Y., Herrmann, N., Swardfager, W., Liu, H., Sham, L., Reim, E. K., et al. (2010). A meta-analysis of cytokines in major depression. Biol. Psychiatry 67, 446–457. doi: 10.1016/j.biopsych.2009.09.033
Kamińska, M., Kubiatowski, T., Ciszewski, T., Czarnocki, K. J., Makara-Studzińska, M., Bojar, I., et al. (2015). Evaluation of symptoms of anxiety and depression in women with breast cancer after breast amputation or conservation treated with adjuvant chemotherapy. Ann. Agric. Environ. Med. 22, 185–189. doi: 10.5604/12321966.1141392
Lai, M. N., Wang, S. M., Chen, P. C., Chen, Y. Y., and Wang, J. D. (2010). Population-based case-control study of Chinese herbal products containing aristolochic acid and urinary tract cancer risk. J. Natl. Cancer Inst. 102, 179–186.
Li, H. H., Livneh, H., Yeh, C. C., Guo, H. R., Lai, N. S., Lu, M. C., et al. (2019). Association between use of Chinese herbal medicine and depression risk in patients with rheumatoid arthritis: A nationwide retrospective cohort study. Int. J. Rheum. Dis. 22, 986–994. doi: 10.1111/1756-185X.13571
Liu, C. T., Wu, B. Y., Hung, Y. C., Wang, L. Y., Lee, Y. Y., Lin, T. K., et al. (2017). Decreased risk of dementia in migraine patients with traditional Chinese medicine use: A population-based cohort study. Oncotarget 8, 79680–79692. doi: 10.18632/oncotarget.19094
Liu, T., Zhang, L., Joo, D., and Sun, S. C. (2017). NF-κB signaling in inflammation. Signal Transduct. Target. Ther. 2:17023. doi: 10.1038/sigtrans.2017.23
Liu, C. Y., Hung, Y. T., Chuang, Y. L., Chen, Y. J., Weng, W. S., Liu, J. S., et al. (2006). Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J. Health Manage. 4, 1–22.
Mannarreddy, P., Denis, M., Munireddy, D., Pandurangan, R., Thangavelu, K. P., and Venkatesan, K. (2017). Cytotoxic effect of Cyperus rotundus rhizome extract on human cancer cell lines. Biomed. Pharmacother. 95, 1375–1387. doi: 10.1016/j.biopha.2017.09.051
Mausbach, B. T., Yeung, P., Bos, T., and Irwin, S. A. (2018). Health care costs of depression in patients diagnosed with cancer. Psychooncology 27, 1735–1741. doi: 10.1002/pon.4716
Park, S. E., Shin, W. T., Park, C., Hong, S. H., Kim, G. Y., Kim, S. O., et al. (2014). Induction of apoptosis in MDA-MB-231 human breast carcinoma cells with an ethanol extract of Cyperus rotundus L. by activating caspases. Oncol. Rep. 32, 2461–2470. doi: 10.3892/or.2014.3507
Piroth, M., Draia, S., Jawad, J., and Piefke, M. (2022). Anxiety and depression in patients with breast cancer undergoing radiotherapy: The role of intelligence, life history, and social support—preliminary results from a monocentric analysis. Strahlenther. Onkol. 198, 388–396. doi: 10.1007/s00066-022-01904-7
Shariff, S. Z., Cuerden, M. S., Jain, A. K., and Garg, A. X. (2008). The secret of immortal time bias in epidemiologic studies. J. Am. Soc. Nephrol. 19, 841–843. doi: 10.1681/asn.2007121354
Simorangkir, D., Masfria, M., Harahap, U., and Satria, D. (2019). Activity anticancer n-hexane fraction of Cyperus Rotundus l. rhizome to breast cancer MCF-7 cell line. Open Access Maced. J. Med. Sci. 7, 3904–3906. doi: 10.3889/oamjms.2019.530
So, R. W. L., Wong, H. S., and Ko, R. K. M. (2015). A traditional Chinese medicine approach in treating depression by promoting liver qi circulation: A Western medicine perspective. Chin. Med. 6, 187–195.
Suryavanshi, S., Choudhari, A., Raina, P., and Kaul-Ghanekar, R. (2019). A polyherbal formulation. HC9 regulated cell growth and expression of cell cycle and chromatin modulatory proteins in breast cancer cell lines. J. Ethnopharmacol. 242:112022. doi: 10.1016/j.jep.2019.112022
The National Health Research Institutes (2002). National Health Insurance Research Database. LHID 2000 [Online]. Available online at: https://nhird.nhri.org.tw/ (accessed June 15, 2017).
Tsai, T. Y., Li, C. Y., Livneh, H., Lin, I. H., Lu, M. C., and Yeh, C. C. (2016). Decreased risk of stroke in patients receiving traditional Chinese medicine for vertigo: A population-based cohort study. J. Ethnopharmacol. 184, 138–143. doi: 10.1016/j.jep.2016.03.008
Wang, Y., Shi, Y. H., Xu, Z., Fu, H., Zeng, H., and Zheng, G. Q. (2019). Efficacy and safety of Chinese herbal medicine for depression: A systematic review and meta-analysis of randomized controlled trials. J. Psychiatr. Res. 117, 74–91. doi: 10.1016/j.jpsychires.2019.07.003
Wang, F., Song, X., Ma, S., Liu, C., Sun, X., Wang, X., et al. (2019). The treatment role of Cyperus rotundus L. to triple-negative breast cancer cells. Biosci. Rep. 39:BSR20190502. doi: 10.1042/BSR20190502
Wang, W., Hu, X., Zhao, Z., Liu, P., Hu, Y., Zhou, J., et al. (2008). Antidepressant-like effects of liquiritin and isoliquiritin from Glycyrrhiza uralensis in the forced swimming test and tail suspension test in mice. Prog. Neuropsychopharmacol. Biol. Psychiatry 32, 1179–1184. doi: 10.1016/j.pnpbp.2007.12.021
Ye, J. H., Liu, M. H., Zhang, X. L., and He, J. Y. (2015). Chemical profiles and protective effect of Hedyotis diffusa willd in lipopolysaccharide-induced renal inflammation mice. Int. J. Mol. Sci. 16, 27252–27269. doi: 10.3390/ijms161126021
Yeh, C. C., Lin, C. C., Wang, S. D., Hung, C. M., Yeh, M. H., Liu, C. J., et al. (2007). Protective and immunomodulatory effect of Gingyo-san in a murine model of acute lung inflammation. J. Ethnopharmacol. 111, 418–426. doi: 10.1016/j.jep.2006.12.014
Zhang, S., Liu, X., Sun, M., Zhang, Q., Li, T., Li, X., et al. (2018). Reversal of reserpine-induced depression and cognitive disorder in zebrafish by sertraline and Traditional Chinese Medicine (TCM). Behav. Brain Funct. 14:13. doi: 10.1186/s12993-018-0145-8
Zhang, Y., Liang, Y., and He, C. (2017). Anticancer activities and mechanisms of heat-clearing and detoxicating traditional Chinese herbal medicine. Chin. Med. 12:20. doi: 10.1186/s13020-017-0140-2
Keywords: breast cancer, Chinese herbal medicines, depression, cohort study, risk
Citation: Yang S-Y, Livneh H, Jhang J-S, Yen S-W, Huang H-L, Chan MWY, Lu M-C, Yeh C-C, Wei C-K and Tsai T-Y (2022) Association of Chinese herbal medicine use with the depression risk among the long-term breast cancer survivors: A longitudinal follow-up study. Front. Psychol. 13:884337. doi: 10.3389/fpsyg.2022.884337
Received: 09 March 2022; Accepted: 15 July 2022;
Published: 18 August 2022.
Edited by:
Xinfeng Guo, Guangzhou University of Chinese Medicine, ChinaReviewed by:
Jiaying LI, The University of Hong Kong, Hong Kong SAR, ChinaMeaghan Coyle, RMIT University, Australia
Jian-Ping Liu, Beijing University of Chinese Medicine, China
Copyright © 2022 Yang, Livneh, Jhang, Yen, Huang, Chan, Lu, Yeh, Wei and Tsai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chia-Chou Yeh, eWVoY2MwNTMwQGdtYWlsLmNvbQ==; Chang-Kuo Wei, d2NrQHR6dWNoaS5jb20udHc=; Tzung-Yi Tsai, ZG03MzIwMjRAdHp1Y2hpLmNvbS50dw==
†These authors have contributed equally to this work
 Shu-Yi Yang1,2†
Shu-Yi Yang1,2† Hanoch Livneh
Hanoch Livneh Jing-Siang Jhang
Jing-Siang Jhang Ming-Chi Lu
Ming-Chi Lu Chia-Chou Yeh
Chia-Chou Yeh Tzung-Yi Tsai
Tzung-Yi Tsai