
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychol., 08 July 2022
Sec. Health Psychology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.873885
 Richard D. Gettings1*
Richard D. Gettings1* Jenna Kirtley1
Jenna Kirtley1 Gemma Wilson-Menzfeld1
Gemma Wilson-Menzfeld1 Gavin E. Oxburgh1
Gavin E. Oxburgh1 Derek Farrell2
Derek Farrell2 Matthew D. Kiernan1
Matthew D. Kiernan1Background: It has been identified that military veterans have distinct experiences of loneliness and social isolation and, when comparing this community to other client groups with a PTSD diagnosis, veterans respond less favorably to treatment. However, the link between PTSD and loneliness for veterans remains insufficiently researched and it is unclear if there are effective interventions tackling this distinct experience of loneliness.
Aims: This systematic narrative review aimed to synthesize existing evidence incorporating elements of social connection, social isolation, and loneliness within interventions for military veterans with a diagnosis of PTSD, consequently aiming to examine the impact of such interventions upon this community.
Methods: Six databases were searched, utilizing relevant search criteria, with no date restrictions. Articles were included if they involved intervention or treatment for military veterans with PTSD and considered elements of social connection, social isolation, and/or loneliness. The initial search returned 202 papers. After exclusions, removal of duplications, and a reference/citation search, 28 papers remained and were included in this review.
Results: From the 28 studies, 11 directly addressed social isolation and two studies directly addressed loneliness. Six themes were generated: (i) rethinking the diagnosis of PTSD, (ii) holistic interventions, (iii) peer support, (iv) social reintegration, (v) empowerment through purpose and community, and (vi) building trust.
Conclusions: A direct focus upon social reintegration and engagement, psychosocial functioning, building trust, peer support, group cohesiveness and empowerment through a sense of purpose and learning new skills may mitigate experiential loneliness and social isolation for veterans with PTSD. Future research and practice should further explore the needs of the PTSD-diagnosed veteran community, seek to explore and identify potential common routes toward the development of PTSD within this community and consider bespoke interventions for tackling loneliness.
The effects of trauma upon the function of the human brain have been known for millennia, reported diversely across ancient Greek, Roman and Hebrew literature, to name a few. Wherever global armies battled the effects of trauma upon the combatants was later reported and recorded for posterity. Under the guise of many different monikers, Shell Shock, Battle Fatigue, Soldier's Heart to name three, the consequences of combat upon cognitive function have been laid bare. These studies became more formalized in the nineteenth Century, culminating in Post-Traumatic Stress Disorder (PTSD) becoming a diagnosable condition in 1980, when the American Psychological Association included it in the Diagnostic and Statistical Manual of mental disorders (DSM), 3rd Edition (American Psychiatric Association, 1980). Eight percent of the general population will be affected by PTSD, at some stage in their life, figures which do not take into account the inevitable consequences of COVID upon many emergency service and public-facing occupations, a rate which is doubled for active duty service members and veterans (Judkins et al., 2020). In comparison, 17% of UK troops who were deployed in combat roles, during the Iraq and Afghanistan conflicts, later developed symptoms of PTSD; compared with 6% for those who were not deployed (Stevelink et al., 2018). This juxtaposition of PTSD prevalence rates is perhaps indicative of both the disparate nature of trauma faced by active-duty service personnel and the potentially incongruous, outdated and non-sufferer centric diagnostic, support and therapeutic processes instituted for the PTSD diagnosed, military and veteran, communities? (Iversen et al., 2009; Ginzburg et al., 2010).
PTSD is a prevalent and debilitating disorder amongst military personnel (serving and veterans) globally, having a long-term impact and creating a significant public health challenge (Steenkamp et al., 2015). It has been found to be associated with transition out of the military, taking hold of an individual potentially once they enter the void of psychological inactivity and lack of direction that faces many whom leave with little, or no, planning and preparation. It is, furthermore, associated with social exclusion and higher rates of deprivation (Karstoft et al., 2015; Sayer et al., 2015; Murphy et al., 2016). There is a certain latency with the development of PTSD, sometimes many years after transition (Marmar et al., 2015). Since 2001, in excess of 280,000 UK Service personnel have been deployed to combat zones in Iraq and Afghanistan (Carlson et al., 1998), and ~11–15,000 UK service personnel currently make the transition into civilian life each year (Ministry of Defence, 2021b). Advances in the treatment and diagnosis of PTSD have led to the differentiation between PTSD and Complex PTSD (C-PTSD) (Powers et al., 2017), whereby it is now recognized that early life traumatisation, prolonged and multiple traumas, deep-seated and unresolved symptoms may prove to be the catalysts for the complex derivative of the disorder; significantly diagnosed within the military and veteran communities due, potentially, to the recruitment dynamic of those who join the military and the idiosyncratic nature of training, experience and culture (Wilson et al., 2018). Parallel advances in the identification, and detailed examination, of loneliness and its psychological correlates, such as feelings of shame and guilt, difficulty controlling emotions, dissociation, feeling cut off from family and friends and risky behavior (Walton et al., 1991) have led to an increasing awareness of the true experience of loneliness and social isolation. These symptoms are not captured in the existing PTSD diagnostic criteria in either the International Classification of Diseases (ICD), 11th edition or the DSM 5 (American Psychiatric Association, 2013; World Health Organization, 2020) (see Table 1). Amongst this panoply of additionally recognized symptoms and consequences are experiences that can be associated with loneliness and social isolation.
Loneliness is a subjective social and emotional experience, often traditionally characterized as the difference between the social relationships individuals actually have and those that they aspire to having (Walton et al., 1991). Conversely, social isolation is an objective experience which considers the integration of the individual into their social environment, the frequency of their social interactions and their integration within social networks (Cacioppo et al., 2006). Research shows that loneliness and social isolation are linked to poor physical health and wellbeing, including high blood pressure, cognitive decline, depression, and mortality (Cacioppo et al., 2006; Holt-Lunstad et al., 2010; Steptoe et al., 2013) and are global issues affecting individuals of all ages.
Evidence demonstrates the unique experiences and needs of military veterans in terms of social isolation and loneliness (Wilson et al., 2018). These unique experiences stem from both intrinsic and extrinsic factors related to military life, such as military-related trauma and PTSD. Transition, and losing touch with comrades was another factor which influenced experiences of loneliness and social isolation (Wilson et al., 2018). Further recent research from two of the largest UK military charities, Royal British Legion and the Soldiers, Sailors, Airmen and Families Association (Royal British Legion, 2014; SSAFA, 2017) indicates that 41% of veterans surveyed (over 2,000 veterans, aged 18–64, participated) had personally experienced loneliness or social isolation and 27% had experienced suicidal ideation, since transitioning from the military to civilian life.
Shepherd et al. (2020) highlight the many challenges of transition and throw light upon cultural and structural differences between the military and civilian communities which facilitate and aggravate these difficulties. A recent US military family lifestyle survey (Sonethavillay et al., 2018) reported that 47% of veteran families had a difficult or very difficult transition experience due to loss of connection and purpose, stress, depression and suicidal thoughts. It is argued that these were exacerbated by frequent relocations and disruption of the established friendship bonds and community links (Stapleton, 2018). Woodward and Jenkings (2011) encapsulated the term “fictive kinship” to describe the practice of considering the military as “family”. The potential loss of this military family becomes a catalyst for “experiential isolation”, the truly unique and extraordinary psychological circumstances that veterans find themselves in; suddenly unable to bond psychologically with members of their family and friends and being unable to share a common empathy or moral compass (Stein and Tuval-Mashiach, 2014, 2015). Previously accepted and established value-system goalposts are suddenly moved, and ethical and social signposts are taken away; leaving the transitioning veteran isolated and estranged.
It is argued that a comorbidity exists between loneliness and PTSD symptomology. Ypsilanti et al. (2020) concluded that self-disgust and loneliness simultaneously predict PTSD symptomology, and these two measures play a cooperative role in predicting anxiety and depression. Research affirms that loneliness and social isolation are uniquely linked to PTSD symptomology via the catalyst of Combat Stress Reaction (Solomon et al., 1986, 2013); idiosyncratic trigger points that relate to military culture, lived experience and the distinctive pressures exerted by transitioning from the military to civilian life (Keats, 2010). These issues are known to be aggravated by mental health stigmatization, denial and avoidance within the military and veteran communities (Rozanova et al., 2015). A comorbidity potentially exists between PTSD, loneliness, and suicide (Pietrzak et al., 2017; Yael and Yager, 2019). A systematic review and meta-analysis of the link between loneliness and suicidal ideation concluded that loneliness was indeed a significant predictor of suicidal ideation in select communities (McClelland et al., 2020). However, more focused research is now required to gain a better understanding of the unique veteran experience of loneliness, and to subsequently aid the design of interventions aimed at reducing loneliness, social isolation and the consequent rates of suicide and suicidal ideation amongst this community.
This systematic narrative review aims to synthesize existing evidence incorporating elements of social connection, social isolation, and loneliness within interventions for military veterans with a diagnosis of PTSD, consequently aiming to examine the impact of such interventions upon this community.
A systematic narrative literature review was conducted. Ethical approval was not required due to it being a review only. Six identified databases were searched (see Table 2; Popay et al., 2012; Snilstveit et al., 2012). Inclusion/exclusion criteria were applied that the accepted studies must involve intervention or treatment for military veterans with PTSD and consider elements of social connection, social isolation, and/or loneliness. Papers must have been written in English and, could not be review papers (see Table 2).
A total of 202 articles were identified from the title and abstract search (Figure 1; Moher et al., 2009). However, 162 were removed as they did not meet the inclusion criteria, i.e., they were not written in English, did not include any aspect of social connection within the intervention, or did not include military veterans diagnosed with PTSD. Fifteen papers were duplicates and thus, were removed. From the 25 remaining studies, a full-text search was conducted, and two further papers were excluded as it was found that they also did not fulfill the inclusion criteria. A reference and citation search was carried out on all included papers, and this resulted in five further papers being included. A total of 28 papers were included in this review (see Supplementary Material).
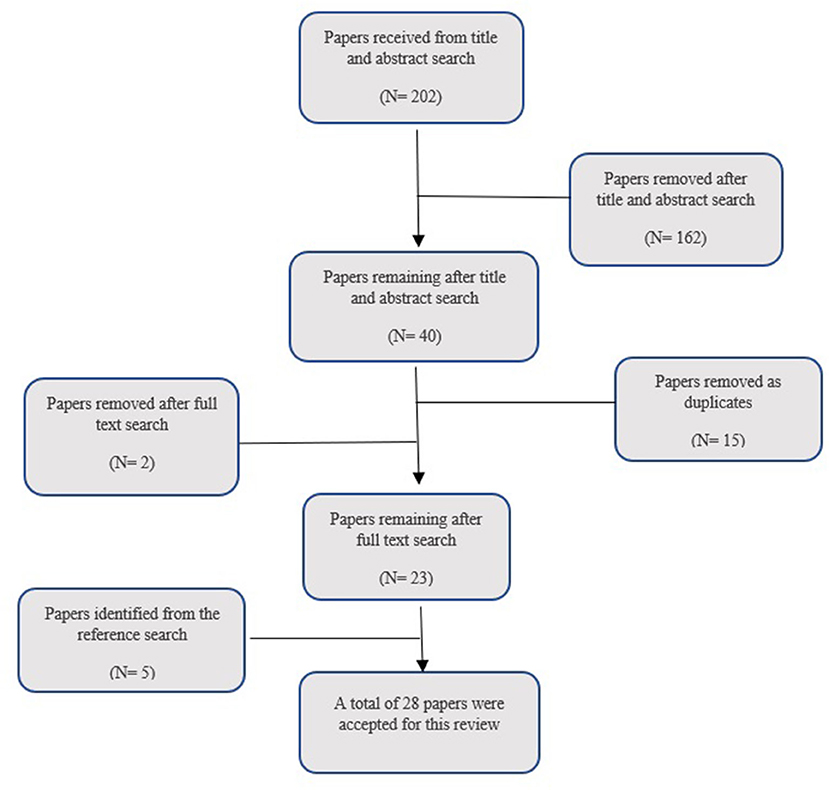
Figure 1. Search strategy used within the systematic search (Moher et al., 2009).
Data analysis was undertaken, using reflexive, deductive thematic synthesis (Braun and Clarke, 2006, 2014, 2019) to generate themes. Specifically, the six stages of Thematic Analysis were followed: generating initial codes; searching for themes; reviewing themes; defining and naming themes; and producing the report (Braun and Clarke, 2006). A collaborative approach to coding and data analysis was taken by members of the research team. Initial codes and were discussed between the research team and final themes/sub-themes were generated based on this collective analysis. Given that this is a review into a novel, and potentially pioneering, aspect of military veteran PTSD prognosis and support, it was decided not to utilize any quality assessment tool, such as CASP for this systematic literature review as it would have been counter-productive to exclude any of the identified papers based upon their conceived quality of contribution.
Six main themes were generated reflecting the findings of the 28 identified studies: (i) rethinking the diagnosis of PTSD; (ii) holistic interventions; (iii) peer support; (iv) social reintegration; (v) empowerment through purpose and community, and; (vi) building trust.
The age of veterans differed between the studies, most being non-specific with regards to age. Seventeen studies included veterans of all ages (Jones et al., 2000; Bensimon et al., 2008, 2012; Holliday et al., 2015; Azevedo et al., 2016; Beidel et al., 2017; Bergen-Cico et al., 2018; Crowe et al., 2018; Johnson et al., 2018; Lobban and Murphy, 2018, 2020; Pezzin et al., 2018; Weiss et al., 2018; Bolman, 2019; McLaughlin and Hamilton, 2019; Galsgaard and Eskelund, 2020; Bauer et al., 2021), whereas four studies were age-specific by virtue of the criteria that they sought veterans from the Vietnam War (1961-75) (Obenchain and Silver, 1991; Ragsdale et al., 1996; Johnson et al., 2004; Otter and Currie, 2004) or Post-9/11/Iraq and Afghanistan veterans (Beidel et al., 2016; Lawrence et al., 2017, 2019; Matthieu et al., 2017; Cushing et al., 2018). Three studies focused solely on female veterans, with two of these relating to rural female veterans who had suffered military sexual trauma (Azevedo et al., 2016; Weiss et al., 2018), and the other relating to a single case study (Trahan et al., 2016).
Eight studies utilized animal-focused interventions (Nevins et al., 2013; Trahan et al., 2016; Bergen-Cico et al., 2018; Crowe et al., 2018; Johnson et al., 2018; Bolman, 2019; McLaughlin and Hamilton, 2019; Galsgaard and Eskelund, 2020). Three studies investigated the efficacy of music related interventions (Bensimon et al., 2008, 2012; Pezzin et al., 2018). One study focused upon yoga as an intervention (Cushing et al., 2018), one upon an adventure-activity intervention (Ragsdale et al., 1996), whilst three studies examined the power of civic service to ameliorate PTSD symptomology (Lawrence et al., 2017, 2019; Matthieu et al., 2017). One study focused upon military museums and art therapy (Lobban and Murphy, 2020), another solely upon art therapy (Lobban and Murphy, 2018), whilst another investigated the efficacy of virtual reality exposure as a suitable medium for PTSD intervention (Beidel et al., 2016). One study involved exercise to mediate PTSD symptomology (Otter and Currie, 2004), whilst one (Johnson et al., 2004) sought to incorporate a veteran's family into the whole treatment and support process.
The vast majority of studies (n = 21) were carried out in the USA (Obenchain and Silver, 1991; Ragsdale et al., 1996; Jones et al., 2000; Johnson et al., 2004, 2018; Holliday et al., 2015; Azevedo et al., 2016; Beidel et al., 2016, 2017; Trahan et al., 2016; Lawrence et al., 2017, 2019; Matthieu et al., 2017; Bergen-Cico et al., 2018; Crowe et al., 2018; Cushing et al., 2018; Pezzin et al., 2018; Weiss et al., 2018; Bolman, 2019; Bauer et al., 2021) whilst two were conducted in Israel (Bensimon et al., 2008, 2012), two in the UK (Lobban and Murphy, 2018, 2020), one in Denmark (Galsgaard and Eskelund, 2020) and two in Australia (Otter and Currie, 2004; McLaughlin and Hamilton, 2019).
Seven studies used a mixed-methods approach (Johnson et al., 2004; Bensimon et al., 2008, 2012; Beidel et al., 2016, 2017; Bergen-Cico et al., 2018; Lobban and Murphy, 2020), 12 studies used a quantitative approach (Ragsdale et al., 1996; Holliday et al., 2015; Trahan et al., 2016; Lawrence et al., 2017, 2019; Matthieu et al., 2017; Johnson et al., 2018; Lobban and Murphy, 2018; Pezzin et al., 2018; Weiss et al., 2018; Bauer et al., 2021) and nine used a qualitative approach (Obenchain and Silver, 1991; Jones et al., 2000; Otter and Currie, 2004; Azevedo et al., 2016; Crowe et al., 2018; Cushing et al., 2018; Bolman, 2019; McLaughlin and Hamilton, 2019; Galsgaard and Eskelund, 2020). Within each broad methodological approach a variety of methods were employed; 11 studies employed focus groups or a group-centric approach (Obenchain and Silver, 1991; Ragsdale et al., 1996; Jones et al., 2000; Johnson et al., 2004; Otter and Currie, 2004; Bensimon et al., 2008, 2012; Crowe et al., 2018; Lobban and Murphy, 2018, 2020; Galsgaard and Eskelund, 2020), eight used semi-structured interviews (Johnson et al., 2004; Bensimon et al., 2008, 2012; Beidel et al., 2016, 2017; Crowe et al., 2018; Cushing et al., 2018; Galsgaard and Eskelund, 2020) and 16 utilized questionnaires (Holliday et al., 2015; Azevedo et al., 2016; Beidel et al., 2016, 2017; Trahan et al., 2016; Lawrence et al., 2017, 2019; Matthieu et al., 2017; Johnson et al., 2018; Lobban and Murphy, 2018, 2020; Weiss et al., 2018; McLaughlin and Hamilton, 2019; Bauer et al., 2021). Two studies were quasi-experimental (Ragsdale et al., 1996; Bergen-Cico et al., 2018), two studies utilized a randomized trial (Johnson et al., 2018; Pezzin et al., 2018) and two a controlled trial (Beidel et al., 2016, 2017). Five studies were pilot analyses (Bensimon et al., 2012; Beidel et al., 2017; Pezzin et al., 2018; Weiss et al., 2018; Galsgaard and Eskelund, 2020).
Of the studies using questionnaires, six specifically measured loneliness, using either the SELSA (Johnson et al., 2018) or UCLA loneliness self-report scales (Ragsdale et al., 1996; Lawrence et al., 2017, 2019; Matthieu et al., 2017; Lobban and Murphy, 2020).
A central banner that emanates from almost all of the identified studies, other than those focused on talking therapies such as Cognitive Processing Therapy (CPT; Holliday et al., 2015) and Cognitive Behavior Therapy (CBT; Trahan et al., 2016), is an acceptance that the current parameters of PTSD diagnoses and treatment are, perhaps, too narrow and restrictive. The strength of the interventions explored here emanates from their recognition of the need to tackle loneliness and social isolation. The diagnosis and treatment of PTSD has, potentially, been viewed in too reductionist a fashion, relying too heavily on the traditional views and approaches; rather than seeing the existential and moral dimensions of treating the whole person holistically (Walton et al., 1991; Iversen et al., 2009; Ginzburg et al., 2010; McFarlane, 2014).
Walton et al. (1991) and Cacioppo et al. (2006), assisted by Wilson et al. (2018) who provide the bespoke nature of military and veteran community, assist moving the dialogue, relating to what the true inherent ingredients of loneliness and social isolation really are, to where it needs to be to be current and relevant for military and veteran PTSD. Such red flags as depression, guilt, shame, psychosexual difficulties, betrayal, stigmatization, self-medication and addiction and increased vulnerability to re-traumatisation all contribute to the destructive cocktail that manifests in the loneliness and social isolation of those living with a PTSD diagnosis in these communities (Walton et al., 1991; Van Ommeren et al., 2002; Iversen et al., 2009; Ginzburg et al., 2010; Palic and Elklit, 2011). Any fit for purpose system, therefore, which seeks to diagnose, signpost and support these communities must acknowledge and accommodate these catalysts.
Studies within this review identify the use of animals (Matthieu et al., 2017; Bergen-Cico et al., 2018; Crowe et al., 2018; Johnson et al., 2018; Bolman, 2019; McLaughlin and Hamilton, 2019; Galsgaard and Eskelund, 2020), music (Bensimon et al., 2008, 2012; Pezzin et al., 2018), art and museums (Lobban and Murphy, 2018, 2020) and adventure training (Ragsdale et al., 1996) as holistic interventions, which seek to offer the PTSD diagnosed veteran meaningful engagement, social connections, and a sense of purpose, thus ameliorating the negative mindset maintained by loneliness and social isolation; holistic in as much as they offer a treatment of mind and body as a whole, via the conduit of addressing the often ignored social, emotional and personal catalysts. Four studies found that dogs offered a non-judgmental, unconditional, support and buffer, facilitating responsibility and a sense of purpose (Bergen-Cico et al., 2018; Crowe et al., 2018; McLaughlin and Hamilton, 2019; Galsgaard and Eskelund, 2020). The study that focused on caring for a traumatized parrot fostered a sense of “becoming well together” and mutually shared suffering and empathy (Bolman, 2019). The studies that explored horse riding therapy found that the veterans were able to build mastery, improve mindfulness skills, and were able to connect with the animal (Nevins et al., 2013; Johnson et al., 2018). These animal-centric studies assessed outcomes via a combination of PTSD, loneliness, and social isolation metrics and group interviews. One study (Obenchain and Silver, 1991) provided Vietnam veterans an opportunity to address social isolation and “alienation” via the affirmation provided through a “Welcoming Home” ceremony, which aided societal participation and reintegration. The efficacy of these interventions appears to be that they focus on improving the overall wellbeing of the veteran, considering the various social and personal contributors to their difficulties, rather than focusing on PTSD symptomology in isolation.
A dominant theme running through the identified studies was the power of peer support in fostering a suitable environment for an intervention to be effective; a significant number adopting a group focused delivery approach (Obenchain and Silver, 1991; Ragsdale et al., 1996; Jones et al., 2000; Johnson et al., 2004; Otter and Currie, 2004; Bensimon et al., 2008, 2012; Crowe et al., 2018; Lobban and Murphy, 2018, 2020; Galsgaard and Eskelund, 2020), and many others taking advantage of this group dynamic indirectly through the creation of a “team atmosphere”. The worth of creating an environment which is accepting, normalizing, and non-judgmental for PTSD diagnosed veterans is clear; an atmosphere of shared understanding empowering the healing process (Obenchain and Silver, 1991; Lobban and Murphy, 2018, 2020). This approach acknowledges and utilizes a strength of the military and veteran communities; its sense of brother/sisterhood, its “fictive kinship” (Woodward and Jenkings, 2011), that helps veterans re-engage and re-motivate each other and take a lead in their own respective recovery journeys.
Through the mitigation of a veteran's estrangement from their community, loved ones, friends and family, it is possible to cultivate an environment where mindfulness, self-awareness and motivation is developed; in contrast to an individual treatment that focuses solely on tackling PTSD symptoms. Within the veteran community, difficulties with social interaction predict lower reductions in PTSD symptomology after treatment interventions such as CPT, CBT and pharmacology (Holliday et al., 2015; Trahan et al., 2016). However, the holistic interventions, which address the disenfranchisement and estrangement experienced by a transitioning veteran and their family (Obenchain and Silver, 1991; Ragsdale et al., 1996; Jones et al., 2000; Johnson et al., 2004, 2018; Otter and Currie, 2004; Bensimon et al., 2008, 2012; Azevedo et al., 2016; Trahan et al., 2016; Lawrence et al., 2017, 2019; Matthieu et al., 2017; Bergen-Cico et al., 2018; Crowe et al., 2018; Cushing et al., 2018; Lobban and Murphy, 2018, 2020; Pezzin et al., 2018; Weiss et al., 2018; Bolman, 2019; McLaughlin and Hamilton, 2019; Galsgaard and Eskelund, 2020; Bauer et al., 2021), generally show either a direct reduction of PTSD symptomology (Ragsdale et al., 1996; Nevins et al., 2013; Beidel et al., 2016, 2017; Trahan et al., 2016; Lawrence et al., 2017, 2019; Matthieu et al., 2017; Bergen-Cico et al., 2018; Johnson et al., 2018; Lobban and Murphy, 2018; Pezzin et al., 2018; Weiss et al., 2018; Galsgaard and Eskelund, 2020; Bauer et al., 2021) or an indirect reduction of such via mitigation of social estrangement and isolation (Obenchain and Silver, 1991; Johnson et al., 2004, 2018; Nevins et al., 2013; Holliday et al., 2015; Beidel et al., 2017; Matthieu et al., 2017; Bergen-Cico et al., 2018; Lobban and Murphy, 2018; Weiss et al., 2018; Bauer et al., 2021). More inclusive interventions, which seek to target the panoply of social integration and quality of life issues, would appear to address the whole lifestyle and culture of symptomology that is endemic within veteran PTSD; taking account of the unique community that the veteran has emerged from, providing a bespoke alternative to focused talking therapy or medication, allowing the veteran to take control over their prognosis and empowering their drive to recovery. Some studies (Bensimon et al., 2008, 2012; Pezzin et al., 2018) targeted group cohesion, togetherness, and connectedness, empowering veterans to gain a sense of control and esteem through mastery of a new skill. Retention and attrition rates are improved through the distraction and mindfulness facilitated by learning a musical instrument (Pezzin et al., 2018). The art and museum interventions (Lobban and Murphy, 2018, 2020) developed a sense of belonging, group bonding and self-efficacy through targeting experiential avoidance and assessing this progress through workshops and interviews. “Sanctuary Trauma”, the internal conflict within veterans relating to the apparent deficiency of their home environment, once they transition from the military, was addressed by the application of a “Welcome Home” ceremony to Vietnam veterans in one of the studies (Obenchain and Silver, 1991); aiming to focus upon their sense of social isolation and “alienation” through a process of re-affirmation, reintegration, and societal participation. It is, perhaps, surprising that only one study (Johnson et al., 2004) sought to involve the family of diagnosed veterans within the treatment and support process. Family-centric preventive interventions have habitually manifested a high efficacy for promoting positive outcomes with the PTSD diagnosed veteran and supporting family unit, and for encouraging consistent engagement, retention and focus upon the recovery journey (Lester et al., 2016).
Empowerment of PTSD diagnosed veterans through the facilitation of hope, purpose, challenge, direction and community (Obenchain and Silver, 1991; Beidel et al., 2016, 2017; Lawrence et al., 2017; Cushing et al., 2018; Lobban and Murphy, 2018; Weiss et al., 2018; Bauer et al., 2021) creates motivation, self-efficacy and opportunity for the veteran, via skill-building interventions, increasing their employability (Azevedo et al., 2016; Weiss et al., 2018; Bauer et al., 2021) and enabling their enrolment in voluntary schemes that contribute to the good of the community; promoting pride, improved self-esteem, increased confidence, courage and resilience (Lawrence et al., 2017, 2019; Matthieu et al., 2017).
None of the above-mentioned themes would have any efficacy or power without the full investment, engagement and commitment of the PTSD diagnosed veterans who need support, guidance and signposting, many at the nadir of their respective journeys. Levels of veteran attrition and disengagement are high for the traditional PTSD therapies that they are directed toward (Haveman-Gould and Newman, 2018), this being contingent upon endemic levels of distrust amongst this community regarding the relevance and appropriacy of these measures and the disconnect they see between themselves and the “white coat” experts who tell them what is best for themselves. Effective interventions must, therefore, be able to empower and facilitate high levels of trust amongst the PTSD diagnosed veteran community. Holistic therapies succeed in fostering the required levels of trust by placing the veteran more centrally in the process, empowering them to feel as if they driving their own recovery, and not merely a passenger in someone else's vehicle (Obenchain and Silver, 1991; Johnson et al., 2004; Azevedo et al., 2016; Beidel et al., 2017; Lawrence et al., 2017, 2019; Matthieu et al., 2017; Weiss et al., 2018; Bauer et al., 2021).
The purpose of this review was to explore the effectiveness of interventions for tackling loneliness and social isolation in PTSD-diagnosed military veterans. Six themes were generated: (i) rethinking PTSD as a diagnosis; (ii) holistic intervention; (iii) peer support; (iv) social integration; (v) empowerment through purpose and community; and (vi) building trust. The papers highlighted that holistic interventions which can mitigate experiential loneliness and social isolation for veterans with PTSD include the following characteristics: a direct focus upon social reintegration and engagement, psychosocial functioning, building trust, peer support, group cohesiveness, empowerment through a sense of purpose and learning new skills. Peer and group-oriented holistic interventions were able to effectively target loneliness, and social isolation through improvements in the veterans' social and community engagement, self- efficacy, self-purpose, and through instilling hope and direction.
This review highlights the importance of socially reintegrating a PTSD-diagnosed veteran back within their community and with their loved ones. This social reintegration is a prerequisite of an effective treatment and a positive recovery journey; fostering growth and engagement through the conduit of group cohesion, togetherness, and connectedness. Linking the veteran back in with their vital support structures and, most importantly, empowering them to be able to communicate openly and honestly with that network, is paramount (Obenchain and Silver, 1991; Azevedo et al., 2016; Lawrence et al., 2017, 2019; Matthieu et al., 2017; Weiss et al., 2018; Bauer et al., 2021). As the studies suggest, the issues of alienation and stigmatization can be countered effectively, but also subtly (Ragsdale et al., 1996; Bensimon et al., 2008, 2012; Bergen-Cico et al., 2018; Crowe et al., 2018; Cushing et al., 2018; Johnson et al., 2018; Lobban and Murphy, 2018, 2020; Pezzin et al., 2018; Bolman, 2019; McLaughlin and Hamilton, 2019; Galsgaard and Eskelund, 2020). The panoply of issues, logistical and psychological, encountered by a veteran transitioning from the military to civilian life need to have been effectively identified, pre-empted and addressed (Obenchain and Silver, 1991; Johnson et al., 2004; Azevedo et al., 2016; Lawrence et al., 2017, 2019; Matthieu et al., 2017; Weiss et al., 2018; Bauer et al., 2021) as is highlighted in recent research and policy focused on understanding the needs of, and supporting, veterans through transition (Keats, 2010; Royal British Legion, 2014; SSAFA, 2017; Cooper et al., 2018; HM Government, 2018; Sonethavillay et al., 2018; National Health Service England, 2019; Shepherd et al., 2020; Ministry of Defence, 2021a).
A significant number of the studies also highlight the importance of trust (Obenchain and Silver, 1991; Johnson et al., 2004; Azevedo et al., 2016; Beidel et al., 2017; Lawrence et al., 2017, 2019; Matthieu et al., 2017; Weiss et al., 2018; Bauer et al., 2021). Engagement with any support and recovery mechanism is contingent upon the veteran trusting the process; trust of those involved in the process, trusting the agenda, and trusting the aspirations of the process. Trust takes time to build, especially within the PTSD-diagnosed veteran community which has become alienated and estranged from both their natural environment, the military community which it has now left, and from their new civilian environment, which it fails to identify or reconcile with. Awareness of the needs for interventions to “culturally adapt” to uniquely homogenous communities is evolving, even within the military and veteran worlds, but lessons learned need to be consolidated and cultivated further (Whealin et al., 2017). Transparency, openness and listening sincerely to the needs, aspirations and fears of the veteran community are key. As highlighted by recent UK Government strategies and NHS trusts, effective intervention should accommodate these needs, and seek to build the necessary trust (Whealin et al., 2017; HM Government, 2018; National Health Service England, 2019; Ministry of Defence, 2021a). Active involvement of the PTSD-diagnosed veteran community within care planning and transition (HM Government, 2018; National Health Service England, 2019) and within the design and construction stages of interventions through research (Bortoli, 2021) are some ways of effectively achieving this.
The power of peer-centered support and mutual understanding provides a sense of non-judgmental acceptance and normalization (Obenchain and Silver, 1991; Ragsdale et al., 1996; Jones et al., 2000; Johnson et al., 2004; Otter and Currie, 2004; Bensimon et al., 2008, 2012; Crowe et al., 2018; Lobban and Murphy, 2018, 2020; Galsgaard and Eskelund, 2020) and supports the mitigation of loneliness within PTSD. This camaraderie is especially important at the time of transition, when a serving member of the armed forces becomes a veteran. This is due to the potential sudden loss of social connectedness and intense bonds of friendship that they had during military service (Cooper et al., 2018; National Health Service England, 2019; Ministry of Defence, 2021a). A PTSD diagnosed veteran is more so able to normalize, accept, and consequently manage, their symptomology once they are around their similarly diagnosed comrades (Obenchain and Silver, 1991; Ragsdale et al., 1996; Jones et al., 2000; Johnson et al., 2004; Otter and Currie, 2004; Bensimon et al., 2008, 2012; Crowe et al., 2018; Lobban and Murphy, 2018, 2020; Galsgaard and Eskelund, 2020). The commonality of suffering and common language of military/veteran PTSD, built upon the forged “fictive kinship” (Woodward and Jenkings, 2011), is a powerful conduit to achieve these monumental and necessary steps toward normalization, acceptance, and management; and the fostering of the necessary purpose, meaning, and hope (Obenchain and Silver, 1991; Beidel et al., 2016, 2017; Lawrence et al., 2017; Cushing et al., 2018; Lobban and Murphy, 2018; Weiss et al., 2018; Bauer et al., 2021). In this manner, peer support becomes a complimentary mechanism for increasing treatment engagement and reducing negativity, pessimism, and dropout from veterans who are receiving ongoing support, through investing them in a process in which they feel central (Hundt et al., 2015).
Symptom-centric interventions tend to focus upon mental health professionals “doing” interventions to the veterans, but research indicates that patients are likely to drop out of treatment if they do not receive what it is they feel they need (Veeninga and Hafkenscheid, 2004). The findings of this review suggest that holistic, non-symptom focused, interventions have a productive role to play in the mitigation of veteran PTSD symptomology, its treatment and support, especially perhaps during the period of transition (Obenchain and Silver, 1991; Ragsdale et al., 1996; Jones et al., 2000; Johnson et al., 2004, 2018; Otter and Currie, 2004; Bensimon et al., 2008, 2012; Azevedo et al., 2016; Trahan et al., 2016; Lawrence et al., 2017, 2019; Matthieu et al., 2017; Bergen-Cico et al., 2018; Crowe et al., 2018; Cushing et al., 2018; Lobban and Murphy, 2018, 2020; Pezzin et al., 2018; Weiss et al., 2018; Bolman, 2019; McLaughlin and Hamilton, 2019; Galsgaard and Eskelund, 2020; Bauer et al., 2021); perhaps working in collaboration with, and sometimes working in place of, more traditional medical, psychological and pharmacological approaches. These interventions appear to be effective because they target the overall wellbeing of the veteran, rather than focusing on PTSD symptomology in isolation. The studies identified in the review broach this issue by fostering an atmosphere of trust, normalization, and mutual endeavor, which may facilitate the PTSD diagnosed veterans' investment in the whole process of “therapy” and taking personal ownership of their recovery pathways. Recent research developments, regarding holistic, non-trauma focused, interventions, coupled with the raising of awareness levels of what it is to be a transitioning veteran (Hundt et al., 2015; Cooper et al., 2018; HM Government, 2018; Wilson et al., 2018, 2020; McGill et al., 2019; National Health Service England, 2019; Ministry of Defence, 2021a), should include a focus on the effective mitigation of the loneliness and social isolation elements of veteran PTSD symptomology, in accordance with the Defense holistic transition policy (Ministry of Defence, 2021a).
The implementation of a holistic and personalized approach, and empowering veterans to be involved in their recovery, was a running theme within the studies included in the review. This is in line with the UK Government and the Ministry of Defense strategy, which addresses the needs, concerns and aspirations of the military and veteran communities with regards to their mental health and general wellbeing, especially during the period of transition (HM Government, 2018; National Health Service England, 2019; Ministry of Defence, 2021a). Levels of engagement and acceptance, within both the military and civilian worlds, of holistic, peer focused and delivered, interventions have accelerated in recent years, as well as a wider acceptance of the power of targeting both mind and body (Veeninga and Hafkenscheid, 2004; Hundt et al., 2015; McGill et al., 2019). By promoting, and securing, the effective transition of our military personnel we empower them to become the valuable, contributory, members of society that they have the potential to be; fully utilizing all the skills, abilities and positive characteristics of their military careers (HM Government, 2018; National Health Service England, 2019; Ministry of Defence, 2021a). To achieve this, however, requires the full collaboration, investment and coordination of organizations and charities within the sector, and the full endorsement of this ethos by the Government, Ministry of Defense, National Health Service and third sector organizations. This emerging, holistic, viewpoint has a strong synergy with the principles of Trauma-Informed Care (TIC) that are becoming more accepted and instrumental within the approach taken by the National Health Service when addressing the needs of the nation's mental health care and support (National Health Service Northern England, 2020). At the heart of TIC is a focus upon the causes of the presented malady and a move away from the previous focus on symptoms.
This review seeks to be pioneering and ground-breaking in it's proposal to re-assess and re-engage with a vulnerable population which has conceivably been ostracized and estranged by traditional and reductionist outlooks and values. The power and strength of this review, therefore, lies in it's desire and aspiration to remove the blinkers, throw away the rule book and begin to move the dialogue to where it needs to be; to be current, relevant, and authentic to the needs, concerns and hopes of this population. A conscious decision was made to not utilize any quality assessment tool, such as CASP, upon the identified papers and to cast as wide a net as possible, to gather and glean as much evidence of good practice and strategy, with regards to loneliness and isolation within the PTSD diagnosed veteran community, as is feasible. Only by the laying of such broad and diverse foundations can the true worth of holistic interventions be effectively gauged, and the direction of the journey forwards be charted.
That said, the review has it's limitations. Only papers written in English, from the selected sources and utilizing the chosen search terms, were examined. Therefore, any papers outside of these parameters were excluded. The chosen search terms, and sources selected from, could be viewed as subjective and biased perhaps, depending upon one's previous experience within the use of holistic, non-traditional, interventions to mitigate loneliness and social isolation within the PTSD diagnosed veteran community?
There are several limitations to the studies identified, and as a consequence, areas for further research are identified below. Global research which directly addresses loneliness and social isolation within veteran PTSD is both limited and localized. Only 2 out of 28 studies were UK-based (Lobban and Murphy, 2018, 2020), whereas 21 were US studies (Obenchain and Silver, 1991; Ragsdale et al., 1996; Jones et al., 2000; Johnson et al., 2004, 2018; Holliday et al., 2015; Azevedo et al., 2016; Beidel et al., 2016, 2017; Trahan et al., 2016; Lawrence et al., 2017, 2019; Matthieu et al., 2017; Bergen-Cico et al., 2018; Crowe et al., 2018; Cushing et al., 2018; Pezzin et al., 2018; Weiss et al., 2018; Bolman, 2019; Bauer et al., 2021), two were conducted in Israel (Bensimon et al., 2008, 2012), one in Denmark (Galsgaard and Eskelund, 2020) and two in Australia (Otter and Currie, 2004; McLaughlin and Hamilton, 2019). Endemic cultural differences exist between the UK and the other countries, extending to their respective armed forces and veteran communities, raising the need for more UK-centric veteran research to be carried out.
Service user/career involvement in the design of the identified studies was not mentioned. It is important that service user/careers are involved in the research process to ensure the design of interventions that the community can trust and invest in. Future research should embrace service user/career involvement in the design of appropriate interventions, in compliance with the National Institute for Health Research (NIHR) (Bortoli, 2021). From the 28 identified studies, 15 directly address loneliness and social isolation, via the conduits of promoting social engagement and functioning (Obenchain and Silver, 1991; Johnson et al., 2004, 2018; Bensimon et al., 2008, 2012; Azevedo et al., 2016; Beidel et al., 2017; Crowe et al., 2018; Pezzin et al., 2018; Weiss et al., 2018; Bauer et al., 2021) and psychosocial functioning (Holliday et al., 2015; Lawrence et al., 2017, 2019; Matthieu et al., 2017). This trend must be cultivated and developed further, in order to give consequent conclusions and recommendations more statistical power and authority.
A significant number of the studies utilized a small research cohort (Ragsdale et al., 1996; Johnson et al., 2004; Bensimon et al., 2012; Holliday et al., 2015; Matthieu et al., 2017; Bergen-Cico et al., 2018; Lobban and Murphy, 2018, 2020; Weiss et al., 2018; Lawrence et al., 2019; McLaughlin and Hamilton, 2019; Galsgaard and Eskelund, 2020) and, therefore, only have limited statistical power and moderate effect sizes. Many of the studies are novel in approach and are, therefore, potentially both logistically complex in nature and problematic to quantify regarding efficacy (Obenchain and Silver, 1991; Otter and Currie, 2004; Bensimon et al., 2008; Lobban and Murphy, 2018, 2020), as they are moving away from established research norms of medical and psychological protocol and classification. Furthermore, many are overly-representative of white males aged 30–50; albeit that the military does recruit more males than females and there is also an age criterion for service. It would be encouraging, nonetheless, to see more female veterans and people from BAME communities within research. There were only two studies which considered African American PTSD diagnosed veterans (Jones et al., 2000; Nevins et al., 2013). A number of studies also utilize self-reporting of PTSD symptomology, rather than the “gold standard”, clinically administered, assessment (Beidel et al., 2016; Cushing et al., 2018; Pezzin et al., 2018; Bolman, 2019). This perhaps compromises the reliability of the results because some people who identify as having PTSD may not actually meet the diagnostic criteria. Furthermore, few studies conducted a pre, post and 6 month follow up. This approach would have given a clearer understanding of whether the interventions were effective in the long term, and therefore follow ups should be considered in future research.
More dedicated consideration needs to be given to the mitigation of veteran PTSD through holistic and bespoke measures that directly address the loneliness and social isolation elements of a PTSD diagnosed veteran's symptomology; out of the 28 identified studies only 15 directly address these issues. Future research should investigate the order and combination that interventions are carried out; for example, whether being offered a holistic intervention prior to any other interventions, such as therapy or medication, empowers a veteran to engage more with PTSD focused interventions. The lived experience, and direct involvement, of PTSD diagnosed veterans should be given prominence in the process of designing effective interventions that better understand their loneliness and social isolation. Furthermore, future research should seek to examine the potential link between early years trauma and later diagnosis of PTSD within the military and veteran communities.
There has been some progress in recent years in the support offered to UK veterans, with an increasing focus on their mental health and wellbeing. Significant collaboration has been made between the Ministry of Defense, HM Government, the National Health Service and the third sector charities and support groups, capturing the synergy and clarity of focus that can be obtained when diverse organizations jointly own key decisions, share research for common aspirations and are committed to wholly altruistic ideals (Bortoli, 2021). This has resulted in a more coherent, targeted and joined up service for the veteran, PTSD-diagnosed, community and has begun to address previously identified shortcomings that existed with regards to the need to identify the unique position of the veteran community and their need for bespoke support and treatment, acknowledging the role that the community itself can take within their journey forwards (Hundt et al., 2015) and increasing receptiveness amongst the parties involved to raise awareness of the true etiology of veteran PTSD symptomology (Wilson et al., 2018, 2020; McGill et al., 2019) and the role that transition, from the military to civilian life, plays in experiences of loneliness and social isolation (HM Government, 2018; National Health Service England, 2019; Ministry of Defence, 2021a). This review highlights the instrumental position of loneliness and social isolation within the lives of the PTSD-diagnosed veteran community, and the mitigating role of holistic, non-clinical, non-trauma focused, interventions.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
RG contributed to the data analysis, was the primary author of the manuscript, and had overall responsibility. MK, JK, and GW-M contributed to the data analysis and co-authored the manuscript. DF and GO co-authored the manuscript. All authors contributed to the article and approved the submitted version.
The United Kingdom Armed Forces Covenant Fund Trust (AFCFT) has funded a 2 year research study, under their Tackling Loneliness Program. Submission fees for this manuscript are to be paid by Northumbria University Student, Library and Academic Services.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.873885/full#supplementary-material
American Psychiatric Association (1980). Diagnostic and Statistical Manual of Mental Disorders. 3rd Edn. Arlington, VA: American Psychiatric Association.
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders. 5th Edn. Arlington, VA: American Psychiatric Association.
Azevedo, K. J., Weiss, B. J., Webb, K., Gimeno, J., and Cloitre, M. (2016). Piloting specialized mental health care for rural women veterans using STAIR delivered via telemental health: IMPLICATIONS for reducing health disparities. J. Health Care Poor Underser. 27, 1–7. doi: 10.1353/hpu.2016.0189
Bauer, A., Amspoker, A. B., Fletcher, T. L., Jackson, C., Jacobs, A., Hogan, J., et al. (2021). A resource building virtual care programme: improving symptoms and social functioning among female and male rural veterans. Eur. J. Psychotraumatol. 12, 357. doi: 10.1080/20008198.2020.1860357
Beidel, D. C., Frueh, B. C., Neer, S. M., and Lejuez, C. W. (2017). The efficacy of Trauma Management Therapy: a controlled pilot investigation of a three-week intensive outpatient program for combat related PTSD. J. Anxiety Disord. 50, 23–32. doi: 10.1016/j.janxdis.2017.05.001
Beidel, D. C., Frueh, B. C., Neera, S. M., Bowers, C. A., Trachik, B., Uhde, T. W., et al. (2016). Trauma management therapy with virtual-reality augmented exposure therapy for combat-related PTSD: a randomized controlled trial. J. Anxiety Disord. 61, 64–74. doi: 10.1016/j.janxdis.2017.08.005
Bensimon, M., Amir, D. A., and Wolf, Y. (2008). Drumming through trauma: music therapy with post-traumatic soldiers. Arts Psychother. 35, 34–48. doi: 10.1016/j.aip.2007.09.002
Bensimon, M., Amir, D. A., and Wolf, Y. (2012). A pendulum between trauma and life: group music therapy with post-traumatized soldiers. Arts Psychother. 39, 223–233. doi: 10.1016/j.aip.2012.03.005
Bergen-Cico, D., Smith, Y., Wolford, K., Gooley, C., Hannon, K., Woodruff, R., et al. (2018). Dog ownership and training reduces post-traumatic stress symptoms and increases self-compassion among veterans: results of a longitudinal control study. J. Altern. Compl. Med. 24, 1166–1175. doi: 10.1089/acm.2018.0179
Bolman, B. (2019). Parroting patriots: interspecies trauma and becoming well-together. Med. Human. 45, 305–312. doi: 10.1136/medhum-2018-011630
Bortoli, S. (2021). NIHR Guidance on Co-producing a Research Project. National Institute for Health Research. Southampton: Involve.
Braun, V., and Clarke, V. (2006). Using thematic analysis in psychology. Qual. Res. Psychol. 3, 77–101 doi: 10.1191/1478088706qp063oa
Braun, V., and Clarke, V. (2014). What can ‘thematic analysis' offer health and wellbeing researchers? Int. J. Qualit. Stud. Health Well-being 9, 26152. doi: 10.3402/qhw.v9.26152
Braun, V., and Clarke, V. (2019). Reflecting on reflexive thematic analysis. Qualit. Res. Sport Exer. Health 11, 589–597. doi: 10.1080/2159676X.2019.1628806
Cacioppo, J. T., Hughes, M. E., Waite, L. J., Hawkley, L. C., and Thisted, R. A. (2006). Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol. Aging 21, 140–151. doi: 10.1037/0882-7974.21.1.140
Carlson, J., Chemtob, C. M., Rusnak, K., Hedlund, N. L., and Muraoka, M. Y. (1998). Eye movement desensitization and reprocessing (EDMR) treatment for combat-related posttraumatic stress disorder. J. Traum. Stress 11, 3–32. doi: 10.1023/A:1024448814268
Cooper, L., Caddick, N., Godier, L., Cooper, A., and Fossey, M. (2018). Transition from the military into civilian life: an exploration of cultural competence. Armed Forces Soc. 44, 156–177. doi: 10.1177/0095327X16675965
Crowe, T. K., Sánchez, V., Howard, A., Western, B., and Barger, S. (2018). Veterans transitioning from isolation to integration: a look at veteran/service dog partnerships. Disabil. Rehabil. 40, 2953–2961. doi: 10.1080/09638288.2017.1363301
Cushing, R. E., Braun, K. L., and Alden, S. (2018). A qualitative study exploring yoga in veterans with PTSD symptoms. Int. J. Yoga Ther. 28, 63–70. doi: 10.17761/2018-00020
Galsgaard, A., and Eskelund, K. (2020). An explorative clinical pilot study into the effect of service dogs on chronic posttraumatic stress disorder. Traumatology 26, 361–369. doi: 10.1037/trm0000278
Ginzburg, K., Ein-Dor, T., and Solomon, Z. (2010). Comorbidity of posttraumatic stress disorder, anxiety and depression: a 20-year longitudinal study of war veterans. J. Affect. Disord. 123, 249–257. doi: 10.1016/j.jad.2009.08.006
Haveman-Gould, B., and Newman, C. (2018). Post-traumatic stress disorder in veterans. JAAPA 31, 21–24. doi: 10.1097/01.JAA.0000546474.26324.05
Holliday, R., Williams, R., Bird, J., Mullen, K., and Suris, A. (2015). The role of cognitive processing therapy in improving psychosocial functioning, health, and quality of life in veterans with military sexual trauma related posttraumatic stress disorder. Psychol. Serv. 12, 428–434. doi: 10.1037/ser0000058
Holt-Lunstad, J., Smith, T. B., and Layton, J. B. (2010). Social relationships and mortality risk: a meta-analytic review. PLoS Medicine 7, e1000316. doi: 10.1371/journal.pmed.1000316
Hundt, N. E., Robinson, A., Arney, J., Stanley, M. A., and Cully, J. A. (2015). Veterans' perspectives on benefits and drawbacks of peer support for posttraumatic stress disorder. Military Med. 180, 851–856. doi: 10.7205/MILMED-D-14-00536
Iversen, A. C., van Staden, L., Hughes, J. H., Browne, T., Hull, L., Hall, J., et al. (2009). The prevalence of common mental disorders and PTSD in the UK military: using data from a clinical interview-based study. BMC Psychiatry 9, 1–12. doi: 10.1186/1471-244X-9-68
Johnson, D. R., Fontana, A., Lubin, H., Corn, B., and Rosenheck, R. (2004). Long-term course of treatment-seeking vietnam veterans with posttraumatic stress disorder; mortality, clinical condition, and life satisfaction. J. Nerv. Mental Dis. 192, 35–41. doi: 10.1097/01.nmd.0000105998.90425.6a
Johnson, R. A., Albright, D. L., Marzolf, J. R., Bibbo, J. L., Yaglom, H. D., Crowder, S. M., et al. (2018). Effects of therapeutic horseback riding on post-traumatic stress disorder in military veterans. Milit. Med. Res. 5, 3. doi: 10.1186/s40779-018-0149-6
Jones, L., Brazel, D., Peskind, E. R., Morelli, T., and Raskind, M. A. (2000). Group therapy program for African-American veterans with posttraumatic stress disorder. Psychiatr. Serv. 51, 1177–1179. doi: 10.1176/appi.ps.51.9.1177
Judkins, J., Moore, B., Collette, T., Hale, W., Peterson, A., and Morissette, S. (2020). Incidence rates of posttraumatic stress disorder over a 17-year period in active duty military service members: PTSD incidence rates in service members. J. Traum. Stress. 33, 558. doi: 10.1002/jts.22558
Karstoft, K., Armour, C., Andersen, S. B., Bertelsen, M., and Madsen, T. (2015). Community integration after deployment to Afghanistan: a longitudinal investigation of Danish soldiers. Soc. Psychiatry Psychiatr. Epidemiol. 50, 653–660. doi: 10.1007/s00127-014-0973-2
Keats, P. A. (2010). Soldiers working internationally: impacts of masculinity, military culture, and operational stress on cross-cultural adaptation. Int. J. Adv. Couns. 32, 290–303. doi: 10.1007/s10447-010-9107-z
Lawrence, K. A., Matthieu, M. M., and Robertson-Blackmore, E. (2017). Completion of a veteran-focused civic service program improves health and psychosocial outcomes in Iraq and Afghanistan veterans with a history of traumatic brain injury. J. Milit. Med. 182, 150. doi: 10.7205/MILMED-D-16-00150
Lawrence, K. A., Matthieu, M. M., and Robertson-Blackmore, E. (2019). Civic service as an intervention to promote psychosocial health and implications for mental health in post-9/11/01 era women veterans. J. Womens Health 28, 7338. doi: 10.1089/jwh.2018.7338
Lester, P., Liang, L.-J., Milburn, N., Magil, C., Woodward, K., Nash, W., et al. (2016). Evaluation of a family-centred preventive intervention for military families: parent and longitudinal outcomes. J. Am. Acad. Child Adoles. Psychiatry 55, 14–24. doi: 10.1016/j.jaac.2015.10.009
Lobban, J., and Murphy, D. (2018). Using art therapy to overcome avoidance in veterans with chronic post-traumatic stress disorder. Int. J. Art Ther. 23, 99–114. doi: 10.1080/17454832.2017.1397036
Lobban, J., and Murphy, D. (2020). Military museum collections and art therapy as mental health resources for veterans with PTSD. Int. J. Art Ther. 25, 172–182. doi: 10.1080/17454832.2020.1845220
Marmar, C. R., Schlenger, W., HennHaase, C., Qian, M., Purchia, E., and Li, M. (2015). Course of posttraumatic stress disorder 40 years after the Vietnam War: findings from the National Vietnam Veterans Longitudinal Study. JAMA Psychiatry 72, 875–881. doi: 10.1001/jamapsychiatry.2015.0803
Matthieu, M. M., Lawrence, K. A., and Robertson-Blackmore, E. (2017). The impact of a civic service program on biopsychosocial outcomes of post 9/11 U.S. military veterans. J. Psychiatry Res. 248, 111–116. doi: 10.1016/j.psychres.2016.12.028
McClelland, H., Evans, J. J., Nowland, R., Ferguson, E., and O'Connor, R. C. (2020). Loneliness as a predictor of suicidal ideation and behaviour: a systematic review and meta-analysis of prospective studies. J. Affect. Disord. 274, 880–896. doi: 10.1016/j.jad.2020.05.004
McFarlane, A. (2014). PTSD and DSM-5: unintended consequences of change. Lancet Psychiatry 1, 246–247. doi: 10.1016/S2215-0366(14)70321-9
McGill, G., Wilson, G., Hill, M., and Kiernan, M. (2019). Utilisation of the principles of the armed forces covenant in NHS trusts and clinical commissioning groups across england: a freedom of information investigation. Br. Med. J. Open 9, 53. doi: 10.1136/bmjopen-2018-022053
McLaughlin, K., and Hamilton, A. L. (2019). Exploring the influence of service dogs on participation in daily occupations by veterans with PTSD: A pilot study. Aust. Occup. Ther. J. 66, 648–655. doi: 10.1111/1440-1630.12606
Ministry of Defence (2021a). JSP100: Defence Holistic Transition Policy, Parts 1 and 2 Combined: Directive and Guidance. London: Ministry of Defence.
Ministry of Defence (2021b). Statistics at MOD. Available online at: https://www.gov.uk/government/organisations/ministry-of-defence/about/statistics (accessed January 2022).
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. (2009). PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Public Library Sci. Med. 3, 123–130. doi: 10.1371/journal.pmed.1000097
Murphy, D., Palmer, E., and Busuttil, W. (2016). Exploring indices of multiple deprivation within a sample of veterans seeking help for mental health difficulties residing in England. J Epidemiol Public Health Rev. 1, 6. doi: 10.16966/2471-8211.132
National Health Service England (2019). Armed Forces Personnel in Transition, Integrated Personal Commissioning for Veterans Framework (IPC4V). London: National Health Service.
National Health Service and Northern England (2020). Trauma Informed Community of Action; Brief Evaluation of the Community and Its Use of the Future NHS Platform. London: National Health Service.
Nevins, R., Finch, S., Hickling, E. J., and Barnett, S. D. (2013). The Saratoga WarHorse project: a case study of the treatment of psychological distress in a veteran of Operation Iraqi Freedom. Adv. Mind-Body Med. 27, 22–25.
Obenchain, J. V., and Silver, S. M. (1991). Symbolic recognition: ceremony in a treatment of posttraumatic stress disorder. J. Traum. Stress 5, 37–43. doi: 10.1002/jts.2490050105
Otter, L., and Currie, J. (2004). A long time getting home: Vietnam Veterans' experiences in a community exercise rehabilitation programme. Disabil. Rehabil. 26, 27–34. doi: 10.1080/09638280410001645067
Palic, S., and Elklit, A. (2011). Psychosocial treatment of posttraumatic stress disorder in adult refugees: a systematic review of prospective treatment outcome studies and a critique. J. Affect. Disord. 131, 8–23. doi: 10.1016/j.jad.2010.07.005
Pezzin, L. E., Larson, E. R., Lorber, W., McGinley, E. L., and Dillingham, T. R. (2018). Music-instruction intervention for treatment of post-traumatic stress disorder: a randomized pilot study. BMC Psychology 19, 60. doi: 10.1186/s40359-018-0274-8
Pietrzak, R. H., Pitts, B. L., Harpaz-Rotem, I., Southwick, S. M., and Whealin, J. M. (2017). Factors protecting against the development of suicidal ideation in military veterans. World Psychiatry 2016, 326–327. doi: 10.1002/wps.20467
Popay, J., Roberts, H., Sowden, A., and Petticrew, M. (2012). Guidance on the conduct of narrative synthesis in systematic reviews. ESRC Methods Program. 15, 047–071. doi: 10.13140/2.1.1018.4643
Powers, A., Fani, N., Carter, S., Cross, D., Cloitre, M., and Bradley, B. (2017). Differential predictors of DSM-5 PTSD and ICD-11 complex PTSD among African American women. Eur. J. Psychotraumatol. 8, 1338914. doi: 10.1080/20008198.2017.1338914
Ragsdale, K. G., Cox, R. D., Finn, P., and Eisles, R. M. (1996). Effectiveness of short-term specialized inpatient treatment for war-related posttraumatic stress disorder: a role for adventure-based counseling and psychodrama. J. Traum. Stress 9, 269–283. doi: 10.1002/jts.2490090209
Royal British Legion (2014). A UK Household Survey of the Ex-Service Community. London: The Royal British Legion.
Rozanova, J., Noulas, P., Smart, K., Roy, A., Southwick, S. M., Davidson, L., et al. (2015). ‘I'm coming home, tell the world I'm coming home' The Long Homecoming and Mental Health Treatment of Iraq and Afghanistan War Veterans. Psychiatric Quart. 87, 427–443. doi: 10.1007/s11126-015-9398-7
Sayer, N., Orazem, R. J., Noorbaloochi, S., Gravely, A., Frazier, P., Carlson, K. F., et al. (2015). Iraq and Afghanistan war veterans with reintegration problems: differences by Veterans Affairs healthcare user status. Admin. Policy Mental Health Health Serv. Res. 42, 493–503. doi: 10.1007/s10488-014-0564-2
Shepherd, S., Sherman, D. K., Maclean, A., and Kay, A. (2020). The challenges of Military Veterans in their transition to the workplace; a call for integrating basic and applied psychological science. Perspect. Psychol. Sci. 16, 590–613. doi: 10.1177/1745691620953096
Snilstveit, B., Oliver, S., and Vojtkova, M. (2012). Narrative approaches to systematic review and synthesis of evidence for international development policy and practice. J. Dev. Effects 4, 409–429. doi: 10.1080/19439342.2012.710641
Solomon, Z., Bensimon, M., Greene, T., Horesh, D., and Ein-Dor, T. (2013). Loneliness trajectories: the role of posttraumatic symptoms and social support. J. Loss Trauma 20, 1–21. doi: 10.1080/15325024.2013.815055
Solomon, Z., Mikulincer, M., and Hobfoll, S. E. (1986). Effects of social support and battle intensity on loneliness and breakdown during combat. J. Pers. Soc. Psychol. 51, 1269–1276. doi: 10.1037/0022-3514.51.6.1269
Sonethavillay, H., Maury, R. V., Hurwitz, J. L., Uvegas, R. L., Akin, J. L., De Coster, J. L., et al. (2018). Blue Star Families Military Family Lifestyle Survey Comprehensive Report. New York, NY: The Department of Applied Research, The Institute of Veterans and Military Families, Syracuse University.
SSAFA (2017). Available online at: https://www.ssafa.org.uk/latest/41-veteranshave-felt-isolated-research-reveals (accessed September 2021).
Stapleton, M. (2018). Loneliness and Social Isolation in the Armed Forces Community. London: Royal British Legion.
Steenkamp, M. M., Litz, B. T., Hoge, C. W., and Marmar, C. R. (2015). Psychotherapy for military-related ptsd: a review of randomized clinical trials. JAMA 314, 489–500. doi: 10.1001/jama.2015.8370
Stein, J. Y., and Tuval-Mashiach, R. (2014). Loneliness and isolation in life-stories of israeli veterans of combat and captivity. Psychol. Trauma: Theory Res. Pract. Policy. 7, 122–130. doi: 10.1037/a0036936
Stein, J. Y., and Tuval-Mashiach, R. (2015). The social construction of loneliness: an integrative conceptualization. J. Constr. Psychol. 28, 210–227. doi: 10.1080/10720537.2014.911129
Steptoe, A., Shankar, A., Demakakos, P., and Wardle, J. (2013). Social isolation, loneliness, and all-cause mortality in older men and women. Proc. Natl. Acad. Sci. USA 110, 5797–5801. doi: 10.1073/pnas.1219686110
Stevelink, S., Jones, M., Hull, L., Pernet, D., MacCrimmon, S., Goodwin, L., et al. (2018). Mental health outcomes at the end of the British involvement in the Iraq and Afghanistan conficts: a cohort study. Br. J. Psychiatry 213, 690–697. doi: 10.1192/bjp.2018.175
Trahan, L. H., Carges, E., Stanley, M. A., and Evans-Hudnall, G. (2016). Decreasing PTSD and depression symptom barriers to weight loss using an integrated CBT approach. Sage J. 15, 280–294. doi: 10.1177/1534650116637918
Van Ommeren, M., Sharma, B., Sharma, G. K., Komproe, I., Cardeña, E., and de Jong, J. T. (2002). The relationship between somatic and PTSD symptoms among Bhutanese refugee torture survivors: examination of comorbidity with anxiety and depression. J. Traum. Stress 15, 415–421. doi: 10.1023/A:1020141510005
Veeninga, A., and Hafkenscheid, A. J. P. M. (2004). Expectations of patients starting psychotherapy: predictors of drop-out? Tijdschrift voor Psychotherapie 30, 187–195. doi: 10.1007/BF03062079
Walton, C. G., Shultz, C. M., Beck, C. M., and Walls, R. C. (1991). Psychological correlates of loneliness in the older adult. Arch. Psychiatric Nurs. 5, 165–170. doi: 10.1016/0883-9417(91)90017-Y
Weiss, B. J., Azevedo, K., Webb, K., Gimeno, J., and Cloitre, M. (2018). Telemental health delivery of skills training in affective and interpersonal regulation (STAIR) for rural women veterans who have experienced military sexual trauma. J. Traumatic Stress 31, 305. doi: 10.1002/jts.22305
Whealin, J. M., Yoneda, A. C., Nelson, D., Hilmes, T. S., Kawasaki, M. M., and Yan, O. H. (2017). A culturally adapted family intervention for rural pacific island veterans with PTSD. J. Psychiatric Serv. 14, 295–306. doi: 10.1037/ser0000186
Wilson, G., Hill, M., and Kiernan, M. (2018). Loneliness and social isolation of military veterans: systematic narrative review. Occup. Med. 68, 600–609. doi: 10.1093/occmed/kqy160
Wilson, G., Leslie, C., McGill, G., and Kiernan, M. (2020). Understanding the Unique Factors of Social Isolation and Loneliness of Military Veterans: A Delphi Study. Newcastle: Northumbria University.
Woodward, R., and Jenkings, N. K. (2011). Military identities in the situated accounts of British military personnel. Sociology 45, 252–268. doi: 10.1177/0038038510394016
World Health Organization (2020). International Statistical Classification of Diseases and Related Health Problems. 11th Edn. Geneva: World Health Organization.
Yael, D., and Yager, J. (2019). Addressing loneliness in complex PTSD. J. Nerv. Mental Dis. 207, 433–439. doi: 10.1097/NMD.0000000000000992
Keywords: loneliness, mental health, military, Post-Traumatic Stress Disorder, psychosocial, social isolation, veteran
Citation: Gettings RD, Kirtley J, Wilson-Menzfeld G, Oxburgh GE, Farrell D and Kiernan MD (2022) Exploring the Role of Social Connection in Interventions With Military Veterans Diagnosed With Post-traumatic Stress Disorder: Systematic Narrative Review. Front. Psychol. 13:873885. doi: 10.3389/fpsyg.2022.873885
Received: 11 February 2022; Accepted: 03 June 2022;
Published: 08 July 2022.
Edited by:
Wai Kai Hou, The Education University of Hong Kong, Hong Kong SAR, ChinaReviewed by:
Hulya Cabadak, Marmara University, TurkeyCopyright © 2022 Gettings, Kirtley, Wilson-Menzfeld, Oxburgh, Farrell and Kiernan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Richard D. Gettings, cmljaGFyZC5nZXR0aW5nc0Bub3J0aHVtYnJpYS5hYy51aw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.