
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 13 May 2022
Sec. Perception Science
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.872619
This article is part of the Research Topic Meaningful Participation and Sensory Processing View all 15 articles
A correction has been applied to this article in:
Corrigendum: Construct Validity of the Sensory Profile Interoception Scale: Measuring Sensory Processing in Everyday Life
Scholars and providers are coming to realize that one’s ability to notice and respond to internal body sensations (i.e., interoception) contributes to an overall sense of wellbeing. Research has demonstrated a relationship between interoceptive awareness and anxiety, for example. Currently, however, tools for evaluating one’s interoception lack the conceptual foundation and clarity necessary to identify everyday behaviors that specifically reflect interoceptive awareness. Unlike existing interoceptive measures, the Sensory Profile Interoception (SPI) scale is participation-based and grounded in Dunn’s Sensory Processing framework. In this study we investigated concurrent validity by correlating the SPI with the Adolescent/Adult Sensory Profile (A/ASP); we investigated construct validity by correlating the SPI with the Perth Alexithymia Scale (PAS), the Body Awareness Scale (BAS), and the State-Trait Anxiety Inventory (STAI). Using the REDCAP online platform, 74 college-aged participants completed the measures. Using Spearman rank order correlations there were statistically significant relationships between the corresponding sensory pattern subscales on SPI and A/ASP (r = 0.277 to r = 0.582). The PAS was only weakly related to the registration subscale of the SPI (r = 0.260). The BAS had significant relationships with seeking and avoiding on the SPI (r = 0.496 and r = 0.385). The STAI had significant relationships with sensitivity and registrations of the SPI (r = 0.266 and r = 0.361 for state; r = 0.403 and r = 0.321 for trait). Taken together, these findings provide evidence of construct validity of the SPI to identify participation patterns associated with both high and low interoception. With the more precise information the SPI provides, professionals can design tailored interventions to support everyday life goals and researchers can study interoception within authentic activities.
There are many bodily functions that we take for granted because they operate outside of our momentary awareness unless something is awry. Although neuroscientists have studied the internal body sensations systems (i.e., interoception) many decades ago (Kandel et al., 2013; Ceuhen et al., 2016), applied scientists have only more recently paid attention to the relationship between one’s awareness of internal body sensations and various conditions like autism, anxiety, hypochondria, suicide attempts, and anorexia, to name a few (Engel-Yeger et al., 2013; Forrest et al., 2015; Longarzo et al., 2015; Critchley and Garfinkel, 2017; Fiene et al., 2018; Khoury et al., 2018; Abdulhamid et al., 2021).
An understanding of interoception and related conditions provides insight into how both interoceptive awareness and unawareness manifests as symptoms. Many studies have established that alexithymia (the inability to identify and describe one’s emotions) is associated with lower levels of interoception, and there is also evidence that atypical interoceptive perception might result in compromised ability to regulate body functions such as breathing (Abdulhamid et al., 2021). Similarly, adults with autism have high rates of interoceptive confusion (74%), and this lack of awareness of bodily states is associated with alexithymia (Fiene et al., 2018). Anxiety is naturally associated with interoception as many of the symptoms include bodily reactions such as shortness of breath and racing heartbeat. One model suggests that people with anxiety have poor predictive ability at interpreting interoceptive input to determine if it signals a true threat (Paulus and Stein, 2010). This poor predictive ability brings about a constant state of uncertainty for the future. A review of interoception and anxiety highlights the role that body awareness plays in learning and the exertion of a behavioral response (Van Diest, 2019). In panic disorder, interoceptive awareness in the form of feelings of breathlessness results in a conditioned response of cardiorespiratory fear and arousal. In yet another example, eating disorders are associated with a mistrust of bodily sensations (Martini et al., 2021).
Existing interoceptive measures use both physiological and self-report approaches. Garfinkel et al. (2015) suggest there are three dimensions of interoception that must be distinguished. First “interoceptive accuracy” refers to one’s ability to report about internal body sensations when compared to physiological measures. Secondly, “interoceptive sensibility” includes one’s self-perceived ability to notice internally body sensations. Finally, “interoceptive awareness” describes one’s metacognitive ability to recognize the synchrony of one’s reporting with physiological readings of internal sensations. For example, physiological measures, such as heartbeat tasks, quantify how accurately a person can detect their own heartbeat at rest (Schandry, 1981). Other measures use self-report as a means of capturing an individual’s self-perception of acuity or attention to interoception. Some self-report interoception measures focus on physiological observations (e.g., “I have an extra strong heartbeat” I feel when my bowels contract; e.g., Longarzo et al., 2015; Cabrera et al., 2018; Vlemincx et al., 2021). Others link attention to interoception as part of interoceptive sensibility (e.g., “When I’m short of breath, I focus on this”; Bogaerts et al., 2021; “I can return awareness to my body if I am distracted,” Mehling et al., 2018). Desmedt et al. (2022) examined current interoception questionnaires to examine whether they were testing a common interoceptive construct. They found that the most frequently used assessments each tested a different aspect of interoceptive sensibility. They call for additional work on both conceptualization of interoception and on clearly articulating these conceptualizations within assessments.
Yet, interoception has an impact on the person that goes beyond physiological responses, awareness of internal sensations, emotions, cognition, and symptoms. The experience of bodily sensations influences participation in daily life. The International Classification of Functioning, Disability and Health (ICF) (World Health Organization [WHO], 2001) includes physiological responses and internal body awareness as “body functions and structures.” The ICF also includes “participation” as a key factor in health; the ICF defines participation as “involvement in life situations.” For example, if someone is feeling breathless at work, they may choose to step outside for some fresh air. If someone lacks an awareness of the need to empty their bladder, they may experience accidents that could affect the ways they socialize with others. A person who notices the effect of caffeine on their body, may choose to avoid coffee later in the day so that they can get to sleep at a reasonable time. For a comprehensive conceptualization to evolve, researchers must also consider the influence of interoception on everyday life (i.e., “interoceptive impact”). Perhaps this current study extends Garfinkel et al.’s (2015) model to include this fourth dimension.
A greater appreciation for the role of interoception and symptoms has led to the development of interventions targeting interoception. There is evidence suggesting that mindfulness-based interventions can lead to increased noticing of interoception input, resulting in decreased stress and increased wellbeing (Fazia et al., 2021). In another study, women in treatment for substance use disorder experienced improvements in interoceptive awareness, emotion regulation and days abstinent after participating in a mindfulness intervention centered on body-awareness (Price et al., 2019). A systematic review of cognitive-behavior therapy for panic disorder found that the most effective interventions were those that were administered face-to-face and included interoceptive exposure (Pompoli et al., 2018). However, many practitioners are also interested in interventions with outcomes related to activities of daily living, instrumental activities of daily living, work, leisure, and socialization. Targeting participation as an outcome is best when the assessment addresses the link between interoception and participation. For example, a participation-based interoceptive measure may alert the practitioner to potential leisure restrictions because the individual is concerned with getting hurt.
When using an interoception measure for intervention planning with outcomes focused on participation, it is important that the measure link internal awareness to activities people do in their daily lives. For example, if a person fails to notice hunger or thirst (low registration of interoceptive cues) which interferes with concentration, we can collaborate to design reminders throughout the day.
The Adolescent/Adult Sensory Profile (A/ASP; Brown and Dunn, 2002) is widely accepted as an important measure for assessing sensory processing in daily life. The assessment is used for both research and clinical practice (e.g., Pfeiffer et al., 2005; Rieke and Anderson, 2009; Chung and Song, 2016; Howe and Stagg, 2016; Bijlenga et al., 2017). The A/ASP is built on an evidence-based conceptual framework (Dunn, 2014) to characterize four sensory processing preferences: sensitivity, avoiding, registration, and seeking. When the A/ASP was developed, seven senses were included: seeing, hearing, tasting, smelling, touching, moving (vestibular), and posturing (proprioception). The availability of an interoceptive measure based on Dunn (2014) provides a conceptual structure for intervention planning. Providers can obtain more details about interoceptive awareness from the four sensory processing preferences (seeking, avoiding, sensitivity, registration) to improve participation. Those who seek interoceptive input require interventions which facilitate more interoceptive activity (e.g., increasing the strenuousness of an activity), while those who are sensitive to interoceptive input require individualized plans that limit interoceptive input (e.g., planning controlled episodes of strenuousness).
In pilot studies focused on item development, researchers clarified wording, evaluated consistency with a conceptual framework (Dunn’s Sensory Processing Framework) using item to scale correlations, internal consistency tests (Chronbach’s alpha) and scale to scale correlations [A/ASP to Sensory Profile Interoception (SPI)], and edited the items based on feedback (Brown and Dunn, 2020). The current version of the SPI will benefit from further psychometric analysis that considers the relationship of the SPI with measures that capture related information already associated with interoception (anxiety, alexithymia, body awareness). If relationships are identified, this would support the construct validity of the SPI. Similarly, construct validity can be examined by determining the relationship between the SPI and Dunn (2014); the A/ASP contains subscales for the sensory patterns in DSPF, i.e., seeking, avoiding, sensitivity, and registration.
The purpose of this study was to evaluate the concurrent (A/ASP) and construct validity (other measures) of the Sensory Profile Interoception (SPI) scale, a participation-focused measure of internal body sensations. We expected that there would be positive correlations between low threshold sensory patterns (Sensitivity and Avoiding) and measures of body awareness and anxiety based on prior literature about interoception (Forrest et al., 2015; Longarzo et al., 2015; Critchley and Garfinkel, 2017; Fiene et al., 2018; Khoury et al., 2018; Abdulhamid et al., 2021). Similar to other researchers, we expected that alexithymia would be related to registration since both of these constructs reflect a failure to detect stimuli (Dunn, 2014; Fiene et al., 2018), and we hypothesized that the SPI sensory patterns would correlate most strongly with the corresponding sensory patterns of the A/ASP (Brown and Dunn, 2002) since we built items for the SPI using the same conceptual framework (DSPF; Dunn, 2014). Additionally, the SPI has the potential to expand the interoceptive framework of Desmedt et al. (2022) to include “interoceptive impact” based on the ICF model (World Health Organization [WHO], 2001) of function, disability and health.
We conducted a correlational analysis to evaluate the construct validity of the SPI.
We recruited a convenience sample of students from occupational therapy programs at three universities and a behavioral science program at one of these universities. We sent emails to students inviting them to participate and provided a link to the secured server. We accepted all students who chose to participate because we believed this sample would have an adequate range of scores on the various measures.
After obtaining IRB approval from each university and permission from chairs of each department, we sent emails to the students asking them to participate. The email included a description of what they would be doing and a link to a REDCAP survey, which held all the demographic and test items. We told participants that completing the REDCAP questions would serve as their permission to participate. Every participant received a code to track their answers; no personally identifiable information was collected.
The SPI is a newly developed scale to evaluate how interoception manifests itself in everyday life behaviors, particularly related to self-care (activities of daily living, ADL) (n = 29 items), eating (n = 25 items) and daily routines (instrumental activities of daily living, IADL) (n = 37 items). We designed the SPI for adolescents, young and older adults to align with the Adolescent/Adult Sensory Profile (A/ASP).
In pilot studies focused on item development, researchers clarified wording, evaluated consistency with a conceptual framework (Dunn, 2014), and edited the items based on feedback (Brown and Dunn, 2020). In the first study, we identified items from the literature, wrote items using the A/ASP as a guide to sensory pattern language, and solicited items from colleagues. We held focus groups with colleagues to obtain their feedback about clarity of items. Then we edited items and recruited a convenience sample of adults to take the SPI. We revised items to improve internal consistency. We used findings from this second pilot study to revise the SPI so that its structure reflects DSPF.
There are currently 91 items on the SPI, and respondents indicate the frequency with which they engage in the behaviors described in each item on a 5-point Likert scale (1 = almost never to 5 = almost always). The SPI is divided into four subscales, that mirror and are theoretically consistent with the sensory patterns of the Adolescent/Adult Sensory Profile described below. The sensitivity subscale (n-30 items) indicates a heightened awareness of interoception, the avoiding subscale (n = 25 items) is an assessment of active behaviors to avoid interoceptive sensations, the (low) registration subscale (n = 20 items) reveals a lack of awareness of interoceptive input, and the seeking subscale (n = 16 items) signals active behaviors to increase interoceptive input. These items have been tested in pilot studies (Brown and Dunn, 2020) to: a. clarify wording of items, and b. to evaluate consistency with DSPF using the Adolescent/Adult Sensory Profile. In the prior study we used item to subscale correlations, Chronbach’s alpha within subscales to test for consistency and correlations between the SPI and the A/ASP to determine which items were strongest. There was good internal consistency (α = 0.63–0.88) and significant/moderate correlations with sensory patterns on the A/ASP (Seeking r = 0.311, p = 0.032; Registration r = 0.378, p = 0.009; Sensitive r = 0.448, p = 0.002, Avoiding r = 0.323, p = 0.031), suggesting both convergent and divergent validity of the scale. Table 1 provides examples of the SPI items.
The A/ASP (Brown and Dunn, 2002) is widely accepted within and outside of occupational therapy as an important participation-based measure for assessing sensory processing. The A/ASP uses Dunn’s (2014) Sensory Processing Framework to characterize four sensory processing preferences: sensitivity, avoiding, registration, and seeking. In addition, the measure includes items representing seven different sensory modalities: vision, hearing, taste, smell, touch, vestibular (body movement), and proprioception (body position). Respondents record how frequently they engage in the behaviors described on 60 items using a 5-point Likert scale (1 = almost never to 5 = almost always). The A/ASP has good internal consistency (0.66–0.82), and validity has been established in the literature over the past two decades (e.g., Pfeiffer et al., 2005; Rieke and Anderson, 2009; Chung and Song, 2016; Gonthier et al., 2016; Howe and Stagg, 2016; Bijlenga et al., 2017; Mayer, 2017; Gándara-Gafo et al., 2019; Zaree et al., 2021).
The Perth Alexithymia Questionnaire measures difficulty attending to and assessing one’s own feelings. This scale was chosen because many studies find alexithymia is associated with poor interoception (Abdulhamid et al., 2021). The PAQ is a 24-item questionnaire, and respondents mark on a 7-point scale (1 = not at all true of me to 7 = very true of me). The scale is divided into 5 scales: (1) negative and (2) positive difficulty identifying feelings, (3) negative, and (4) positive difficulty describing feelings, and (5) a general external oriented thinking scale. There is support for the measure’s concurrent and discriminant validity and internal consistency, i.e., α ≥ 0.80 for all PAQ subscales (Preece et al., 2018, 2020), and it has an advantage over some other measures in that it assesses both positive and negative emotions (Preece et al., 2020).
The State-Trait Anxiety Inventory for adults is a well-established and widely used assessment of anxiety symptoms (STAI; Spielberger et al., 1983). This scale was chosen because anxiety is considered by many to include a heightened sensitivity to interoception (Mallorquí-Bagué et al., 2016). There are 20 items related to anxiety and 20 items related to general state. Respondents mark on a 7-point scale (1 = strongly disagree, 4 = neither agree nor disagree, 7 = strongly agree). The measure has excellent test-retest reliability (average r = 0.88), excellent internal consistency (average α > 0.89), and good discriminate validity (Metzger, 1976; Barnes et al., 2002).
The Body Awareness Questionnaire (Shields et al., 1989) is an assessment of interoception that does not include emotional body processes. Although the scale is not divided into subscales, some of the items are more reflective of awareness of bodily reactions (consistent with sensitivity in the interoception scale), while others address the impact of habit or routine on body functions (consistent with avoiding on the interoception scale). There are 18 items, and respondents rate them on 7-point scale (1 = not at all true of me to 7 = very true of me). There is support for the measure’s convergent and discriminant validity (Shields et al., 1989), test-retest reliability (r = 0.80), internal consistency (α range of 0.77–0.83; Shields et al., 1989), and concurrent validity (Unal et al., 2020).
We conducted a set of descriptive analyses to describe our participants. We used correlations to examine the relationships among the SPI and other benchmark measures. Specifically, we completed Spearman Rank Order Correlations between summary scores on the SPI and summary scores on the other measures. We used Spearman Rank Order Correlations because this calculation does not assume linearity.
We describe our results based on our hypotheses. Seventy-four students participated in the study. Eighty-five percent (n = 63) were White, 1.5% (n = 1) was black or African American, 4% (n = 3) were Hispanic or Latinx, 4% (n = 3) were Pacific Islanders, and 5.4% (n = 4) reported “other”; 90% were female (n = 67). They ranged in age from 21 to 45 years, with a mean of 26 years old and a standard deviation of 4.6 years. Eleven participants were 30 years of age or older. Table 2 provides the means and standard deviations for the other measures in the study. There were no differences between age groups (21–23 years, n = 22, 24–29 years, n = 41, 30 years and older, n = 11) on the measures in the study based on an Analysis of Variance by age (Hotelling’s Trace = 0.752, F = 1.128, significance = 0.338). We did not collect any additional information about the participant demographics.
Table 3 provides the correlations between the subscales of the A/ASP and the SPI. Supplementary Appendix 1 contains scatterplots of significant correlations. The constructs of Dunn’s Sensory Processing Framework (DSPF) were correlated across the A/ASP and the SPI. All of the SPI subscales correlated most strongly with their corresponding A/ASP subscale except for the avoiding subscale, with its highest correlation with the A/ASP sensitivity subscale (r = 0.366), but only a slightly lower correlation with the A/ASP avoiding subscale (r = 0.338). These findings support the SPI’s concurrent validity in terms of the measure’s consistency with its theoretical basis (the DSPF) (see Table 1 for examples), and a participation-based sensory processing measure. As outlined in Table 3, seeking is only correlated with the corresponding subscale between the 2 scales (seeking = 0.523). Registration and sensitivity have their highest correlations with their corresponding subscales (registration = 0.552; sensitivity = 0.582), although these scales also have significant correlations with other subscales.
Consistent with our hypotheses, we found that alexithymia had a small but significant correlation with the registration score on the SPI. Body awareness had moderate correlations with avoiding and seeking and a small but significant correlation with the sensitivity scores on the SPI. The State/Trait Anxiety measure had moderate correlations with sensitivity and registration on the SPI. Table 4 provides the correlations. Supplementary Appendix 1 provides scatterplots of significant correlations.
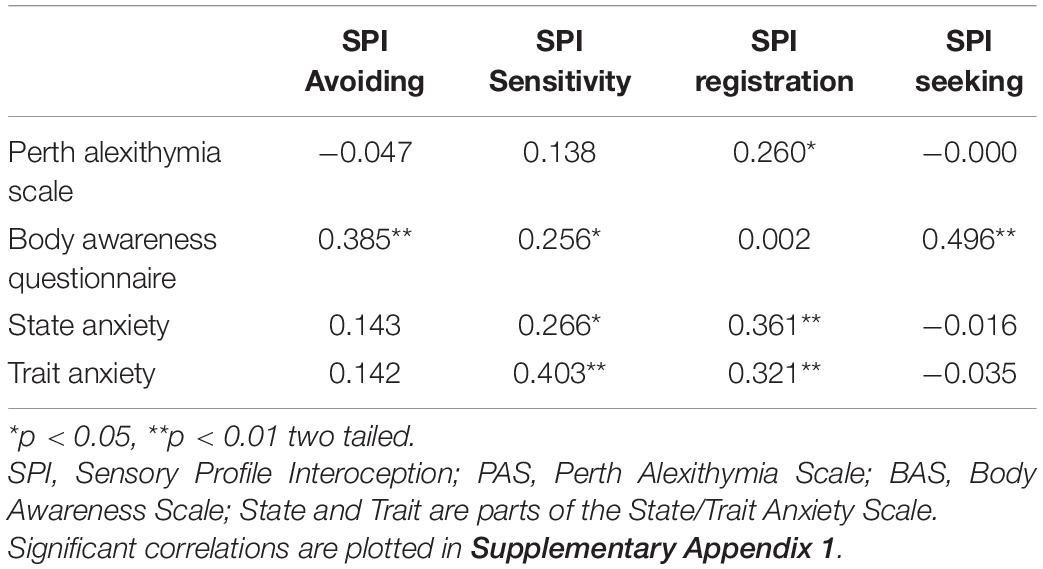
Table 4. Correlations between alexithymia, body awareness, and anxiety to the Sensory Profile Interoception scale (n = 74).
In this study, we examined the validity of the newly developed SPI in two ways. First, we examined the relationship between the SPI and the A/ASP to determine whether the SPI has a strong conceptual foundation, specifically Dunn’s Sensory Processing Framework (DSPF), with an established participation-based measure of sensory processing (i.e., the A/ASP) (concurrent validity). Secondly, we examined the relationship between the SPI and related mental health measures to determine whether the SPI reflects known relationships between interoception and psychological factors (construct validity). We provide examples of the SPI items in Table 1.
Knowing more precisely how interoceptive awareness will affect every day routines provides knowledge for effective intervention planning at the participation level. The State Anxiety scale includes “I feel tense” and “I feel upset”; the Trait Anxiety scale includes “I feel nervous and restless.” The SPI provides more detail about how “tense,” “nervous,” and “upset” might affect one’s daily routine, such as “I worry about stomach/digestive processes” and “I select hobbies that are orderly and predictable so I can stay calm” which indicate possible focus for intervention planning (e.g., in these examples, eating, or hobbies). Additionally, by also reflecting the four sensory patterns from DSPF, more precision is possible. For example, “I stay away from activities where I think I could get hurt” (avoiding), “I get bruises or other injuries, and I do not remember how the injury happened” (registration), “I enjoy activities that make my heart beat faster (e.g., vigorous physical activity, amusement park rides, scary movies)” (seeking), and “I try to control my heartbeat when it becomes too fast (e.g., by slowing down, meditating)” (sensitivity) suggest different approaches to supporting participation.
The SPI seems to reflect DSPF. All corresponding sensory pattern subscales (i.e., seeking, avoiding, sensitivity, registration) had significant correlations between the SPI and the A/ASP, and, in all cases but avoiding, these subscales correlated most strongly with their corresponding subscale (for example, the A/ASP seeking subscale and the SPI seeking subscale). As an illustration, “I find a razor cut later in the day” from the SPI is significantly correlated with several low registration items on the A/ASP: “I trip or bump into things,” “I am unsure of footing when walking on stairs,” and “I miss the street, building or room signs when trying to go somewhere new,” while being unrelated to A/ASP items reflecting other sensory patterns. Additionally, the correlations were moderate, suggesting the SPI is assessing some additional information not covered by the A/ASP. The SPI seems to reflect the strong conceptual base of DSPF seen across many studies of the Child and Adult Sensory Profiles (e.g., Little et al., 2018; Nesayan et al., 2018; Tomchek et al., 2018; Zaree et al., 2021). This foundation gives providers and researchers a clear structure for discussing findings about interoception and linking to other systems that might be relevant to a specific research question or intervention planning.
The seeking subscales only correlated with each other, suggesting that seeking has some distinct characteristics that are present on both the SPI and the A/ASP. As reported in prior literature, the low threshold sensory patterns (avoiding and sensitivity) correlate with their corresponding pattern (i.e., avoiding with avoiding, sensitivity with sensitivity), and with each other. This trend is also consistent with prior literature, which suggests there is a continuum of high responsiveness to sensory input (low sensory thresholds). Finally, registration, which reveals missing cues in the environment, is most highly correlated with its counterpart as well.
We examined construct validity with psychological factors by correlating the SPI with alexithymia, body awareness and anxiety measures. The SPI differs from other interoception measures because the quadrants allow for consideration of level of awareness of interoception (sensitivity and registration) as well as active efforts to regulate interoceptive input (avoiding and seeking quadrants).
As anticipated, the Perth Alexithymia Scale was correlated with the registration score on the SPI, which was the only significant correlation. Alexithymia is an inability to detect and describe one’s emotions; registration scores (as it is tested on the SPI and the A/ASP) indicate the amount that a person misses cues in the environment. This finding is consistent with other studies indicating a relationship between poor interoception and alexithymia (e.g., Abdulhamid et al., 2021).
The Body Awareness Questionnaire related to all the subscales except registration. As expected, the Body Awareness Questionnaire was associated with the SPI sensitivity scale, which assesses interoceptive awareness. However, the highest correlations were with the seeking and avoiding scales. Both seeking and avoiding are measuring active self-regulation patterns; perhaps active self-regulation patterns contribute to knowing about one’s body. Since registration on the SPI evaluates how frequently people miss cues in their everyday lives, it is not surprising that with our sample from a general population, registration on the SPI would not be correlated to body awareness as tested on the BAQ.
State and trait anxiety were related to sensitivity and registration. Patterns of both noticing and missing input is consistent with other studies examining anxiety and sensory processing. In the second edition of the Toddler Sensory Profile (Dunn, 2014) and in other studies with adults (Engel-Yeger and Dunn, 2011; Engel-Yeger et al., 2016, 2018; Brown et al., 2020), there is a small but significant relationship between registration and conditions such as anxiety, hypochondria, anorexia, and pain catastrophizing (Forrest et al., 2015; Longarzo et al., 2015; Critchley and Garfinkel, 2017; Fiene et al., 2018; Khoury et al., 2018; Abdulhamid et al., 2021). We believe that people with registration tendencies do miss cues as we originally believed. However, at some point, bystanders (people with low registration) do notice a possible catastrophe, but it is so late in the situation that a big response is necessary (Little et al., 2016). This big response looks remarkably like a sensor’s responses; it is the timing that is different. In addition, Clark et al. (2018) found high sensitivity and registration from the A/ASP and high trait anxiety in people with chronic low back pain. However, they also found high sensation avoiding. They hypothesize that premorbid trait anxiety and sensory processing patterns contribute to pain experiences.
It is unclear as to why avoiding on the SPI was not correlated with trait or state anxiety, but it may be that this relationship is more detectable in a clinical population. Alternatively, the regulation through avoiding may be different for interoceptive input. People with avoiding tendencies are more likely to anticipate difficult situations and stop them, for instance not attending a party or turning down an invitation to a public event. However, with the SPI, avoiding is characterized as an active behavioral response that can be adaptive in terms of managing unpleasant sensations. Anxiety is associated with passive coping strategies, which can include a general lack of engagement in life (LeDoux and Gorman, 2001). People with sensitivity try to participate and then find themselves overwhelmed, which is consistent with anxiety laden behaviors and thoughts (Dunn et al., 2016a,b).
We recruited a convenience sample of students for this study, which introduces sampling bias. It is possible that students in occupational therapy and behavioral sciences would be more aware of interoception and behavior, although participants had not completed their professional education at the time of participation. We also had a majority of white female participants, which could also bias our outcomes. Future studies must expand the demographics to learn how these data fit into the bigger picture.
The concurrent validity of the four-quadrant model of the SPI was supported by the correlation of the SPI with the Adolescent/Adult Sensory Profile. The low to moderate correlations with the psychological factors (construct validity) already related to interoception suggest that the SPI reflects related concepts while being a distinct assessment of interoception. As the first participation-based interoception assessment, the SPI may be particularly useful for clinical use when intervention goals focus on participation-oriented outcomes.
The datasets presented in this article are not readily available because the measure described by the authors is under development and we would want to approve of any use of the data before offering it to others. Requests to access the datasets should be directed to Y2Jyb3duMkBtaWR3ZXN0ZXJuLmVkdQ==.
The studies involving human participants were reviewed and approved by Midwestern University Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
WD and CB contributed to the conceptualization and design of the study, data analysis, and writing and editing of the manuscript. AB contributed by assisting with the selection of relevant assessment and editing of the manuscript. AS contributed by assisting with data collection and editing of the manuscript. All authors contributed to the article and approved the submitted version.
WD and CB were authors of the Adolescent/Adult Sensory Profile, a measure that was used in this study. We receive royalties for the assessment.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.872619/full#supplementary-material
Abdulhamid, H., Jäger, N., Schnädelbach, H., and Smith, A. D. (2021). Room to breathe: using adaptive architecture to examine the relationship between alexithymia and interoception. J. Psychosom. Res. 153:110708. doi: 10.1016/j.jpsychores.2021.110708
Barnes, L. L. B., Harp, D., and Jung, W. S. (2002). Reliability correlations of scores on the spielberger state-trait anxiety inventory. Educ. Psychol. Meas. 62, 603–618. doi: 10.1177/0013164402062004005
Bijlenga, D., Tjon-Ka-Jie, J. Y. M., Schuijers, F., and Kooij, J. J. S. (2017). Atypical sensory profiles as core features of adult ADHD, irrespective of autistic symptoms. Eur. Psychiatry 43, 51–57. doi: 10.1016/j.eurpsy.2017.02.481
Bogaerts, K., Walentynowicz, M., Van Den Houte, M., Constantinou, E., and Van den Bergh, O. (2021). The interoceptive sensitivity and attention questionnaire: evaluating aspects of self-reported interoception in patients with persistent somatic symptoms, stress-related syndromes and healthy controls. Psychosom. Med. 84, 251–260. doi: 10.1097/PSY.0000000000001038
Brown, C., and Dunn, W. (2002). Adolescent/Adult Sensory Profile. San Antonio, TX: Psychological Corporation.
Brown, C., and Dunn, W. (2020). Development of a participation-focused measure of interoception. Occup. Ther. J. Res. 74:7411500038.
Brown, C., Karim, R., and Steuter, M. (2020). Retrospective analysis of studies examining sensory processing preferences in people with a psychiatric condition. Am. J. Occup. Ther. 74, 7404205130p1–7404205130p11. doi: 10.5014/ajot.2020.038463
Cabrera, A., Kolacz, J., Pailhez, G., Bulbena-Cabre, A., Bulbena, A., and Porges, W. (2018). Assessing body awareness and autonomic reactivity: factor structure and psychometric properties of the Body Perception Questionnaire-Short Form (BPQ-SF). Int. J. Methods Psychiatr. Res. 27:e1596. doi: 10.1002/mpr.1596
Ceuhen, E., Vlaeyen, J. W. S., and Van Diest, I. (2016). On the origin of interoception. Front. Psychol. 7:743. doi: 10.3389/fpsyg.2016.00743
Chung, S. M., and Song, B. K. (2016). Evaluation of sensory processing abilities following stroke using the adolescent/adult sensory profile: implications for individualized intervention. J. Phys. Ther. Sci. 28, 2852–2856. doi: 10.1589/jpts.28.2852
Clark, J. R., Yeowell, G., and Goodwin, P. C. (2018). Trait anxiety and sensory processing profile characteristics in patients with non-specific chronic low back pain and central sensitisation - A pilot observational study. J. Body Mov. Ther. 22, 909–916. doi: 10.1016/j.jbmt.2017.11.007
Critchley, H. D., and Garfinkel, S. N. (2017). Interoception and emotion. Curr. Opin. Psychol. 17, 7–14. doi: 10.1016/j.copsyc.2017.04.020
Desmedt, O., Heeren, A., Corneille, O., and Luminet, O. (2022). What do measures of self-report interoception measure? Insights from a systematic review, latent factor analysis, and network approach. Biol. Psychol. 169:108289. doi: 10.1016/j.biopsycho.2022.108289
Dunn, W. (2014). Sensory Profile 2: Strengths-Based Approach to Assessment and Planning. San Antonio: Pearson, Inc.
Dunn, W., Little, L., Dean, E., Robertson, S., and Evans, B. (2016a). The state of the science on sensory factors and their impact on daily life for children: a scoping review. OTJR 36(Suppl. 2), 3S–26S. doi: 10.1177/1539449215617923
Dunn, W., Tomchek, S., Little, L., and Dean, E. (2016b). Prevalence of sensory characteristics in the general population: a person-centered approach. Am. J. Occup. Ther. 70(4 Suppl. 1):7011500001. doi: 10.5014/ajot.2016.70S1-RP202A
Engel-Yeger, B., Bloch, B., Gonda, X., Canepa, G., Pompili, M., Sher, L., et al. (2018). Sensory profiles in unipolar and bipolar affective disorders: possible predictors of response to antidepressant medications? A prospective follow-up study. J. Affect. Disord. 240, 237–246. doi: 10.1016/j.jad.2018.07.032
Engel-Yeger, B., and Dunn, W. (2011). Relationship between pain catastrophizing level and sensory processing patterns in typical adults. Am. J. Occup. Ther. 65, e1–e10. doi: 10.5014/AJOT.2011.09004
Engel-Yeger, B., Gonda, X., Muzio, C., Rinosi, G., Pompili, M., Amore, M., et al. (2016). Sensory processing patterns, coping strategies, and quality of life among patients with unipolar and bipolar disorders. Rev. Bras. Psiquiatr. 38, 207–215. doi: 10.1590/1516-4446-2015-1785
Engel-Yeger, B., Palgy-Levin, D., and Lev-Wiesel, R. (2013). The sensory profile of people with post-traumatic stress symptoms. Occup. Ther. Ment. Health 29, 266–278. doi: 10.1080/0164212X.2013.819466
Fazia, T., Bubbico, F., Berzuini, G., Tezza, L. D., Cortellini, C., Bruno, S., et al. (2021). Mindfulness meditation training in an occupational setting: effects of a 12-weeks mindfulness-based intervention on wellbeing. Work 70, 1089–1099. doi: 10.3233/WOR-210510
Fiene, L., Ireland, M. J., and Brownlow, C. (2018). The Interoception Sensory Questionnaire (ISQ): a scale to measure interoceptive challenges in adults. J. Autism Dev. Disord. 48, 3354–3366. doi: 10.1007/s10803-018-3600-3
Forrest, L. N., Smith, A. R., White, R. D., and Joiner, T. E. (2015). (Dis)connected: an examination of interoception in individuals with suicidality. J. Abnorm. Psychol. 124, 754–763. doi: 10.1037/abn0000074
Gándara-Gafo, B., Sntos-Del Riego, S., Viana-Moldes, I., and Muñiz, J. (2019). Cultural adaptation of the adolescent/adult sensory profile for Spain. Am. J. Occup. Ther. 73, 7306205070p1–7306205070p9. doi: 10.5014/ajot.2019.031815
Garfinkel, S. N., Seth, A. K., Barrett, A. B., Suzuki, K., and Critchley, H. D. (2015). Knowing your own heart: distinguishing interoceptive accuracy from interoceptive awareness. Biol. Psychol. 104, 65–74. doi: 10.1016/j.biopsycho.2014.11.004
Gonthier, C., Longuépée, L., and Bouvard, M. (2016). Sensory processing in low-functioning adults with autism spectrum disorder: distinct sensory profiles and their relationships with behavioral dysfunction. J. Autism Dev. Disord. 46, 3078–3089. doi: 10.1007/s10803-016-2850-1
Howe, F. E., and Stagg, S. D. (2016). How sensory experiences affect adolescents with an autistic spectrum condition within the classroom. J. Autism Dev. Disord. 46, 1656–1668. doi: 10.1007/s10803-015-2693-1
Kandel, E., Schwartz, J., Jessell, T., Siegelbaum, S., and Hudspeth, A. (Eds). (2013). Principles of Neural Science, 5th Edn. New York, NY: McGraw Hill.
Khoury, N. M., Lutz, J., and Schuman-Olivier, Z. (2018). Interoception in psychiatric disorders: a review of randomized, controlled trials with interoception-based interventions. Harv. Rev. Psychiatry 26, 250–263. doi: 10.1097/HRP.0000000000000170
LeDoux, J. E., and Gorman, J. M. (2001). A call to action: overcoming anxiety through active coping. Am. J. Psychiatry 158, 1953–1955. doi: 10.1176/appi.ajp.158.12.1953
Little, L., Dean, E., Tomcheck, S., and Dunn, W. (2018). Sensory processing in autism, attention deficit hyperactivity disorder and typical development. Phys. Occup. Ther. Pediatr. 38, 243–254. doi: 10.1080/01942638.2017.1390809
Little, L., Dean, E., Tomchek, S., and Dunn, W. (2016). Classifying sensory profiles of children in the general population. Child Care Health Dev. 43, 81–88. doi: 10.1111/cch.12391
Longarzo, M., D’Olimpio, F., Chiarazzo, A., Santangelo, G., Trojano, L., and Grossi, D. (2015). The relationship between interoception and alexithymic trait. The Self Awareness Questionnaire in healthy subjects. Front. Psychol. 6:1149. doi: 10.3399/fpsyg.2015.01149
Mallorquí-Bagué, N., Bulbena, A., Pailhez, G., Garfinkel, S. N., and Critchley, H. D. (2016). Mind-body interactions in anxiety and somatic symptoms. Harv. Rev. Psychiatry 24, 53–60. doi: 10.1097/HRP.0000000000000085
Martini, M., Marzola, E., Brustolin, A., and Abbate-Daga, G. (2021). Feeling imperfect and imperfectly feeling: a network analysis on perfectionism, interoceptive sensibility, and eating symptomatology in anorexia nervosa. Eur. Eat. Disord. Rev. 29, 893–909. doi: 10.1002/erv.2863
Mayer, J. L. (2017). The relationship between autistic traits and atypical sensory functioning in neurotypical and ASD adults: a spectrum approach. J. Autism Dev. Disord. 47, 316–327. doi: 10.1007/s10803-016-2948-5
Mehling, W. E., Acree, M., Stewart, A., Silas, J., and Jones, A. (2018). The Multidimensional Assessment of Interoceptive Awareness, Version 2 (MAIA-2). PLoS One 13:e0208034. doi: 10.1371/journal.pone.0208034
Metzger, R. L. (1976). A reliability and validity study of the State-Trait Anxiety Inventory. J. Clin. Psychol. 32, 276–278. doi: 10.1002/1097-4679(197604)32:2<276::aid-jclp2270320215>3.0.co;2-g
Nesayan, A., Gandomani, R. A., Movallali, G., and Dunn, W. (2018). The relationship between sensory processing patterns and behavioral patterns in children. J. Occup. Ther. Sch. Early Interv. 11, 124–132. doi: 10.1080/19411243.2018.1432447
Paulus, M. P., and Stein, M. B. (2010). Interoception in anxiety and depression. Brain Struct. Funct. 214, 451–463. doi: 10.1007/s00429-010-0258-9
Pfeiffer, B., Kinnealey, M., Reed, C., and Herzberg, G. (2005). Sensory modulation and affective disorders in children and adolescents with Asperger’s disorder. Am. J. Occup. Ther. 59, 335–345. doi: 10.5014/ajot.59.3.335
Pompoli, A., Furukawa, T. A., Efthimiou, O., Imai, H., Tajika, A., and Salanti, G. (2018). Dismantling cognitive-behaviour therapy for panic disorder: a systematic review and component network meta-analysis. Psychol. Med. 48, 1945–1953. doi: 10.1017/S0033291717003919
Preece, D., Becerra, R., Allan, A., Robinson, K., Chen, W., Hasking, P., et al. (2020). Assessing alexithymia: psychometric properties of the Perth Alexithymia Questionnaire and the 20-item Toronto Alexithymia Scale in United States adults. Pers. Individ. Differ. 166:110138. doi: 10.1016/j.paid.2020.110138
Preece, D., Becerra, R., Robinson, K., Dandy, J., and Allan, A. (2018). The psychometric assessment of alexithymia: development and validation of the Perth Alexithymia Questionnaire. Pers. Individ. Differ. 132, 32–44. doi: 10.1016/j.paid.2018.05.011
Price, C. J., Thompson, E. A., Crowell, S. E., Pike, K., Cheng, S. C., Parent, S., et al. (2019). Immediate effects of interoceptive awareness training through Mindful Awareness in Body-oriented Therapy (MABT) for women in substance use disorder treatment. Subst. Abus. 40, 102–115. doi: 10.1080/08897077.2018.1488335
Rieke, E. F., and Anderson, D. (2009). Adolescent/Adult Sensory Profile and obsessive-compulsive disorder. Am. J. Occup. Ther. 63, 138–145. doi: 10.5014/ajot.63.2.138
Schandry, R. (1981). Heart beat perception and emotional experience. Psychophysiology 18, 483–488. doi: 10.1111/j.1469-1981.tb2486.x
Shields, S. A., Mallory, M. E., and Simon, A. (1989). The body awareness questionnaire: reliability and validity. J. Pers. Assess. 53, 802–815. doi: 10.1207/s15327752jpa5304_16
Spielberger, C. D., Gorsuch, R. L., Lushene, R., Vagg, P. R., and Jacobs, G. A. (1983). State-Trait Anxiety Inventory STAI. Palo Alto, CA: Consulting Psychologists Press.
Tomchek, S. D., Little, L. M., Myers, J., and Dunn, W. (2018). Sensory subtypes in preschool aged children with autism spectrum disorder. J. Autism Dev. Disord. 48, 2139–2147. doi: 10.1007/s10803-018-3468-2
Unal, A., Altug, F., Erden, A., Cavlak, U., and Senol, H. (2020). Validity and reliability of the Body Awareness Questionnaire in patients with non-specific chronic low back pain. Acta Neurol. Belig. 121, 701–705. doi: 10.1007/s13760-020-01399-y
Van Diest, I. (2019). Interoception, conditioning, and fear: the panic threesome. Psychophysiology 56:e13421. doi: 10.1111/psyp.13421
Vlemincx, E., Walentynowicz, M., Zamariola, G., Van oudenhove, L., and Luminet, O. (2021). A novel self-report scale of interoception: the three domain interoceptive sensations questionnaire (THISQ). Psychol. Health 7, 1–20. doi: 10.1080/08870446.2021.2009479
World Health Organization [WHO] (2001). International Classification of Functioning, Disability and Health: ICF. Geneva: World Health Organization [WHO].
Keywords: interoception, measurement, construct validity, participation, sensory processing, occupational therapy, interoceptive impact
Citation: Dunn W, Brown C, Breitmeyer A and Salwei A (2022) Construct Validity of the Sensory Profile Interoception Scale: Measuring Sensory Processing in Everyday Life. Front. Psychol. 13:872619. doi: 10.3389/fpsyg.2022.872619
Received: 09 February 2022; Accepted: 11 April 2022;
Published: 13 May 2022.
Edited by:
Emily R. Stern, NYU Grossman School of Medicine, United StatesReviewed by:
Eleanor R. Palser, University of California, San Francisco, United StatesCopyright © 2022 Dunn, Brown, Breitmeyer and Salwei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Winnie Dunn, ZHVubndpQGhlYWx0aC5taXNzb3VyaS5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.