
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 11 April 2022
Sec. Psychology for Clinical Settings
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.861859
The current study was aimed to assess the reliability and validity of the Urdu version of the Psychosomatic Symptoms Scale (PSSS) in Pakistani patients. The PSSS is time-saving and easy to administer. The field experts drafted the translated version of PSSS. The Urdu version of PSSS, Patient Health Questionnaire- 9 (PHQ-9), and Symptom Checklist-90 (SCL-90) Urdu version were used for assessment. The translation procedure was comprised of three steps, namely forward translation, back translation, and expert panel discussion. A sample of 982 (men = 50.5% and women = 49.5%) was collected with a convenient sample technique from a general hospital and private clinic. The Cronbach’s alpha for PSSS was 0.974. The confirmatory factor analysis (CFA) revealed that all the items factor loading of PSSS were more than 0.35, the root mean square error of approximation (RMSEA) was = 0.062, the standardized root mean residual (SRMR) was = 0.043, and the comparative fit index (CFI) was = 0.97 with 90% CI. The results also showed that women (M = 72.08, SD = 6.79) are more likely to have psychosomatic symptoms than men (M = 51.21, SD = 13.36) on P < 0.001. The PSSS Urdu version is proven to be a useful and reliable instrument for screening, monitoring, and assessing Pakistani patients’ psychosomatics symptoms.
In 1818, a German psychiatrist named Heinroth, coined the word “Psychosomatic,” and Felix Deutsch then later coined the word with the extension “Psychosomatic medicine” in 1922. The word “Psychosomatic” is derived from Greek words “Psyche” and “soma,” which mean mind and body, respectively. The term psyche originally meant “soul or mind,” but it has subsequently been referred to as behavior. In contrast, soma denotes the organism’s body Psychosomatic refers to a wide range of concepts, from illnesses to biopsychosocial research and consultation-liaison work (Chandrashekar and Math, 2006; Shamim, 2012; Dhimole et al., 2016). According to the biopsychosocial model (Engel, 1977), it refers to the connection of psychological and biological factors that are associated with the concept of health and disease. This paradigm entails the idea that physical and psychological conditions are not separated in psychosomatic assessments. Moreover, individuals with psychosomatic diseases are focused on their somatic symptoms generally ignoring their psychological difficulties (Engel, 1977; Bauer et al., 2011; Bolton and Gillett, 2019). Clinicians only rely on the easily administered tool Psychosomatic Symptoms Scale (PSSS) to assess and diagnose the psychosomatic symptoms which was developed by Li et al. (2020). PSSS measures both the aspects of psychological and somatic problems, which provided adequate support to psychologists, clinicians, and psychiatrists in making precise diagnoses and characterizing other features affecting treatment. Moreover, the scale can convey a baseline for finding progress in illness during follow-up over a period in answer to a particular intervention (Shafique et al., 2017; Li et al., 2020).
In Pakistan, the national language is Urdu, and a massive fraction of the population cannot read, write, or speak English. There are few culturally adopted scales in the Urdu language used to diagnose and assess psychosomatics. In clinical settings and for research purposes, Symptoms Check List (SCL-90) is used widely, which is a multidisciplinary and lengthy scale with 90 items that is rather time-consuming. A short, reliable, and easily administered tool is required to assess the patients (Gaynes et al., 2008). Other than the SCL-90, the PSSS is very easy to administer in general hospitals and clinical setups. The PSSS is a shorter and valid scale with 26 items, which is time-saving for both the patients and doctors. However, the PSSS is only available in English and Chinese language. Therefore, the urge was felt to translate and adapt the PSSS in the Urdu language. The Urdu version of this scale will be filled by patients themselves without assistance for translation and will be handy for both clinicians and researchers. Moreover, the Urdu version of this scale will aid in avoiding misdiagnosis or inappropriate diagnosis. Therefore, the main objective of the current study was to provide a valid and reliable Urdu version of the PSSS scale to doctors, psychologists, and researchers.
Informed consent was received from patients before filling out the questionnaires. The present study was approved by the ethical committee of the hospital (2021ZDSYLL347-P01). In phase 1, the PSSS scale was translated into the Urdu language, and in phase II, the psychometric properties of the PSSS scale were calculated. The confirmatory factor analysis (CFA) was used to assess the factorial structure of two dimensions of PSSS. The correlation was inspected among the PSSS, SCL-90, and Patient Health Questionnaire- 9 (PHQ-9).
The PSSS was used to measure the symptoms of distress that occurred in the last 7 days. There scale has 26 total items, with each item rated and valued on a 4-point scale from not at all rated (0) to all the day rated (Shamim, 2012); the scale usually takes 15 min to complete. It was used to measure two main dimensions of symptoms, namely psychological and somatic complaints. The psychological symptoms were evaluated by 5, 10, 11, 12, 17, 21, and 25, while somatic symptoms were estimated by 1, 2, 3, 4, 6, 7, 8, 9, 13, 14, 15, 16, 18, 19, 20, 22, 23, 24, and 26 items of the scale (Li et al., 2020).
The Symptom Checklist-90 (SCL-90) has a 5-point Likert scale, with nine subscales of phobic anxiety, somatization, depression, obsessive-compulsive, paranoid ideation, interpersonal sensitivity, hostility, psychoticism, and anxiety. The reliability of SCL-90 is.98 (Shafique et al., 2017). This scale is used in many languages (Imperatori et al., 2020; Bianciardi et al., 2021). We used the subscale somatization Urdu version. The Urdu version of SCL-90 comprised of 90 items and used to determine criterion validity.
The Urdu version of Patient Health Questionnaire-9 (PHQ-9) was used in the present study as a standard measure. PHQ-9 has 9 items, and each item measures depression and starts from 0 to 3. The reliability of PHQ-9 is 0.91 (Ahmad et al., 2018).
The translation of PSSS was carried out in four main steps. The first step involved the translation of PSSS from the English language to the target language “Urdu,” with the help of four experts in the relevant fields (one psychiatry professor, one psychology professor, one Urdu literature Ph.D. scholar, and one English literature scholar). All the experts were requested to translate the PSSS questionnaire word by word without changing the meaning.
The second step involved determining the discrepancies, and assessment of the items was conducted under the supervision of the four subject experts (clinical psychologist, a professor, an associate professor, an assistant professor, and one senior researcher); each item was assessed thoroughly, with choosing the grammar and proper words near to the original one in Urdu.
The third step involved the Brislin method for back-translation. For that purpose, four experts (two English language professors, one psychology professor, and one Urdu professor) were requested to accurately translate the PSSS Urdu version into the English language. The scale was applied on 30 sample sizes with a mean age of 24.5 years (SD = 5.2). The results proved no ambiguity in the questionnaire and were ready for further validation (Tanku, 2013).
To quantify the psychometric properties of PSSS, the Cronbach’s alphas were calculated. CFA was used to accomplish the construct validity of PSSS in AMOS 23 (Arbuckle, 2014).
Participants were selected for research from the psychiatric clinic (Dr. A. Sadiq Psychiatric clinic, Peshawar, Khyber Pakhtunkhwa) and general hospital (Hayatabad Medical Complex, Peshawar Khyber Pakhtunkhwa) before COVID-19. The participants were asked to fill out the questionnaires manually. The inclusion criteria were the following: inpatients and outpatients from the general hospital and clinic, with age ranging from 20 to 65 years old.
The data were analyzed by using IBM SPSS version 22 and AMOS version 23 (IBM Corp, 2013; Arbuckle, 2014). The Cronbach’s alpha of PSSS was primarily measured. Spearman’s correlation test was applied to find the association of PSSS with PHQ-9 and SCL-90. P-value (P < 0.05) was considered significant for all the statistical analyses. Data from the sample of 982 patients were used to verify the item characteristics, factor and structure validities, and internal consistency of PSSS. Mean and SD, as well as corrected item-total correlation (CITCs), were measured for each item in the scale. CITCs values greater than 0.3 are considered good (Cristobal et al., 2007). Item number 20 of the PSSS measures different symptoms depending on genders, such as premature male ejaculation and female dysmenorrhea or irregular menstruation. Spearman’s correlation was used for the age factor. Construct validity was computed by using Spearman’s correlation between PSSS, SCL-90, and PHQ-9. CFA was used to find the factorial validity. The model, estimation of weighted least squares mean and variance (WLSMV), was used. The root mean square error of approximation (RMSEA) and comparative fit index (CFI) with 90% CI. For testing the model fit, the standardized root mean residual (SRMR) was used. The model fit indicated TLI > 0.95, CFI > 0.95, SRMR < 0.08, and RMSEA < 0.06.
The data were taken from 982 diagnosed patients with psychiatric disorders from different departments, as shown in Table 1. The questionnaires were filled in, and the basic demographic characteristics were obtained for the current study, including sex, education, age, employment status, financial status, marital status, and department.
Reliability coefficients and descriptive statistics (N = 982) were computed for PSSS. The results were tabulated and given in Table 2.
Table 2 shows the psychometric properties of the scale PSSS. The Cronbach’s α value for PSSS is 0.974, indicating the scale’s high reliability. The maximum range is 26, while the minimum range is 78. The mean for total participants (N = 982) is 6.54, and the SD is 14.89. The value of skewness = −0.684 and Kurtosis = −0.676 are negative. As far as skewness and kurtosis are concerned, the PSSS is in the range of ± 1. The scale as a whole has negative values. The negative values show that data has the highest values, while the positive shows that data has the lowest. According to Kim (2013), if values of skewness are less than 2 and the value of kurtosis are less than 7 for any sample (N > 300), it can be considered as the normal distribution (Kim, 2013) (shown in Table 2).
Table 3 shows all the items of PSSS, their mean, standard deviation, and corrected item- Total Correlations CITCs. Range of response options covered by the responses to each item. The mean CITCs of items ranged from 0.437 to 0.897. In the given table, most of the items have high Cronbach’s alpha, this high Cronbach’s alpha shows good and strong reliability.
Mean differences along gender were computed by independent t-test. The results were generated was then tabulated and displayed in Table 4.
Table 4 revealed significant differences of psychosomatic symptoms in men and women. The scores of women were higher on PSSS (M = 72.08, SD = 6.79) compared to men (M = 51.21, SD = 13.36) on p < 0.001.
The sum score of PSSS was significantly correlated with that of PHQ-9 (r = 0.589, P < 0.001) and SCL-90 subscale somatization (r = 0.635, P = 0.001), showing the good construct validity. Some items had moderate to high correlation of SCL-90.
Confirmatory factor analysis explained the underlying dimensions and the relationship between the observed and original factors. Exploratory factor analysis (EFA) was also used to find the validity of the scale. The Kaiser-Meyer-Okin (KMO) test of sphericity by component analysis was 0.98 and the Bartlett’s spherical test result was 325 (P < 0.000). These values showed that EFA could be accepted. CFA is a statistical technique used to verify the factor structure of a set of observed variables. In initial conditions, the standardized regression weights of all the observed factors that were high than 0.35 would be acceptable (Field, 2013). The model fit was good with RMSEA = 0.062, SRMR = 0.043 which is excellent, and the CFI = 0.97 which is also an excellent value. In the current study, all factors had higher CFA than standard value 0.35 except item no. 17 and 25. It proved that the factor models of the two subscales P and S. The factor loadings looked at the trail of observed pointers with covariance. All the values were greater than 0.35 as shown in Figure 1.
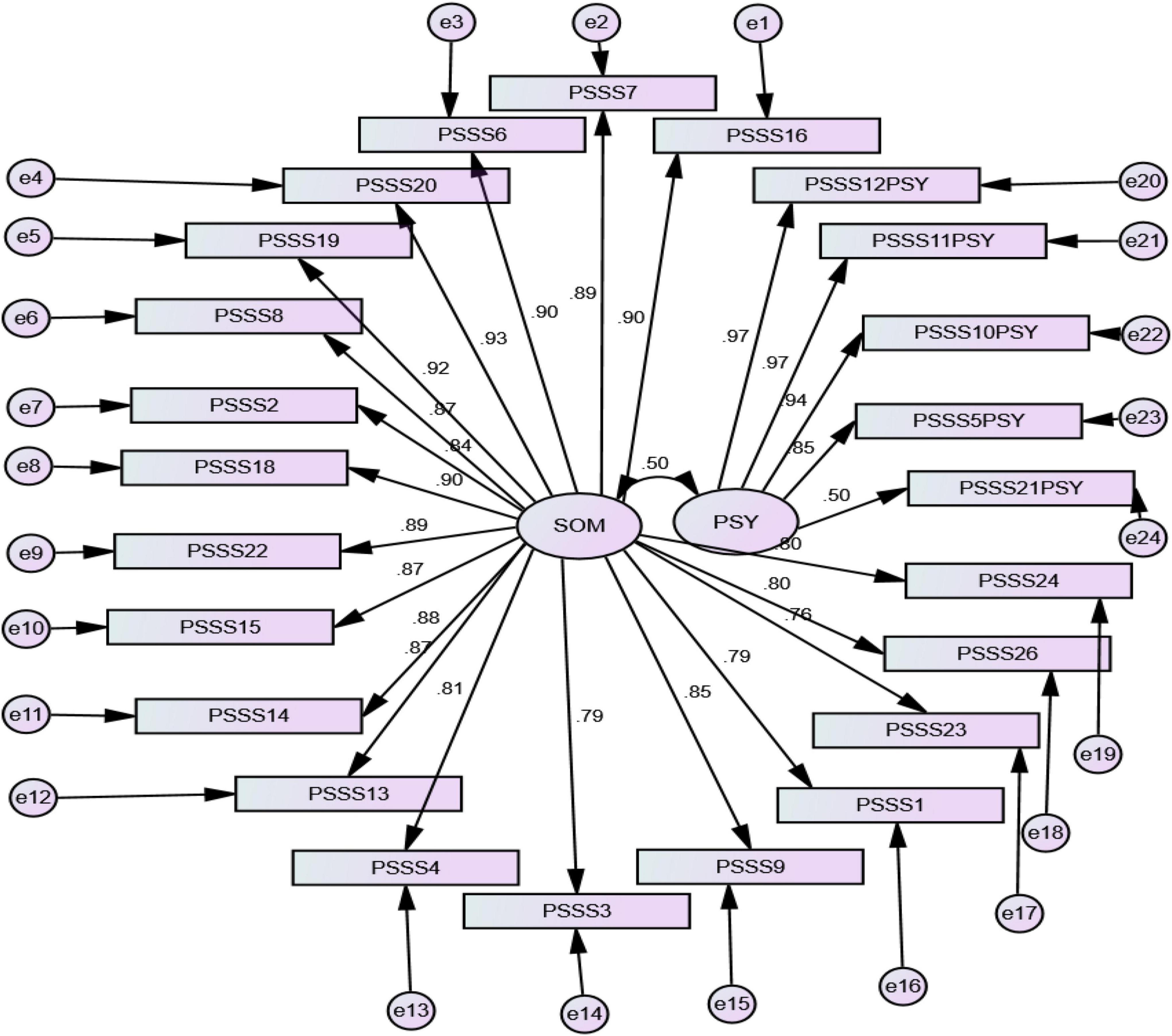
Figure 1. The confirmatory factor analysis of two subscales of Psychosomatic Symptoms Scale (PSSS). Som, somatic complaint; Psy, psychological complaints.
The current study was aimed to validate and translate the PSSS into the Urdu language. PSSS is the first scale for the assessment of patients measuring both psychological symptoms and physical complaints and their association because physical symptoms frequently occurred with psychological distress (Li et al., 2020).
Pakistan has more than 200 million human population, and the mental health is poorest but there are less than 500 psychiatrists serving this population. This low number of mental health professionals creates a big treatment gap, which is why more than 90% of the common mental disorders remain untreated (Bashir, 2018; Sikander, 2020). The needs for the care of individuals suffering from mental illnesses have been documented in this region for many centuries. Indigenous healthcare systems, such as Unani and Ayurveda treatment models, had a considerable influence on healthcare over the decades. The religious and cultural ideas about indigenous and traditional healthcare were always visible in local systems. They significantly impacted choices, awareness, and perception for several health-related treatments (World Health Organization [WHO], 2009).
Public health sectors are the key spots for mental health problems, but recently, private sectors have contributed to mental health treatment (Ali and Gul, 2018). Gender-based analysis for PSSS revealed that women score high on the P and S subscale of PSSS, wherein the score represents that women show severe symptoms compared to patients who are men. Previous studies reported that women rated higher for somatic symptoms than men (Bardel et al., 2019), supporting our results. However, in Pakistan, the literacy rate among women is relatively lower than men, which possibly be the cause of women scoring high on PSSS. Most of the patients are unaware of mental health, wherein they go to various clinics and hospitals for a checkup which diagnose them with various diseases. Due to a large number of patients, the psychiatrists cannot provide the deserving duration of time to diagnose or educate the patients about their illness. The patient’s attendants were unaware of the illness and frequently checked their patient with various medical professionals. Misdiagnosis of the patient, which leads to the wrong prescription of medicine, may progressively exacerbate the disease. Other reasons are additional responsibilities of women, such as caring for children and their housekeeping duties (Kishi et al., 2002; Scott et al., 2006; Bashir, 2018; Sikander, 2020). Also, the studies suggest a negative impact of conflict between the physical and mental wellbeing of women (Bourbonnais et al., 1999; Artazcoz et al., 2004). In this study, men have fewer psychosomatic complaints than women. Previous research reported that women have higher psychosomatic symptoms compared to men (Östberg et al., 2006; Brooks et al., 2021), which supports our results for translated versions of PSSS.
Therefore, the PSSS Urdu version is a valid and reliable tool for psychosomatics, and it could be used in Urdu-speaking communities for convenient and precise diagnosis.
In conclusion, our study demonstrated that the PSSS Urdu version is a useful and reliable instrument for screening, monitoring, and assessing Pakistani patients’ psychosomatics symptoms. The lower educational level of women compared to men, the reliance on spiritual healers, and the lack of health literacy might contribute to the gender difference in the prevalence of symptoms.
The current study will contribute to the convenient diagnosis of psychosomatic disorder. It is also easy to administer in general hospitals in Pakistan. This scale is short and time-saving and will aid further research.
The PSSS scale was applied only to the patients of province KP-Pakistan. To generalize its findings, it is mandatory to use this scale to various populations of Pakistan. Second, PHQ-9 was used instead of PHQ-12 and PHQ-15 because only PHQ-9 was available in the national language (Urdu language). Applying new and updated scale of PHQ-9 is therefore suggested.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
The studies involving human participants were reviewed and approved by the Ethical Committee of Zhongda Hospital, Southeast University, Nanjing, Jiangsu, China (2021ZDSYLL347-P01). The patients/participants provided their written informed consent to participate in this study.
SS and YY: conceptualization and methodology and data analysis. SS: writing original draft preparation. YY, WX, and MJ: review. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.861859/full#supplementary-material
Ahmad, S., Hussain, S., Akhtar, F., and Shah, F. S. (2018). Urdu translation and validation of PHQ-9, a reliable identification, severity and treatment outcome tool for depression. J. Pak. Med. Assoc. 68, 1166–1170.
Ali, T. M., and Gul, S. (2018). Mental health services in Pakistan. Psychol. Commun Health 7, 57–71. doi: 10.5964/pch.v7i1.224
Artazcoz, L., Artieda, L., Borrell, C., Cortès, I., Benach, J., and García, V. (2004). Combining job and family demands and being healthy: What are the differences between men and women? Eur. J. Public Health 14, 43–48. doi: 10.1093/eurpub/14.1.43
Bardel, A., Wallander, M. A., Wallman, T., Rosengren, A., Johansson, S., Eriksson, H., et al. (2019). Age and sex related self-reported symptoms in a general population across 30 years: patterns of reporting and secular trend. PLoS One 14:e0211532. doi: 10.1371/journal.pone.0211532
Bashir, A. (2018). The state of mental health care in Pakistan. Lancet Psychiatry 5:471. doi: 10.1016/S2215-0366(18)30191-3
Bauer, A. M., Bonilla, P., Grover, M. W., Meyer, F., Riselli, C., and White, L. (2011). The role of psychosomatic medicine in global health care. Curr. Psychiatry Rep. 13, 10–17. doi: 10.1007/s11920-010-0162-2
Bianciardi, E., Gentileschi, P., Niolu, C., Innamorati, M., Fabbricatore, M., Contini, L. M., et al. (2021). Assessing psychopathology in bariatric surgery candidates: discriminant validity of the SCL-90-R and SCL-K-9 in a large sample of patients. Eat. Weight Disord. 26, 2211–2218. doi: 10.1007/s40519-020-01068-2
Bolton, D., and Gillett, G. (2019). “Biopsychosocial Conditions of Health and Disease,” in The Biopsychosocial Model of Health and Disease (Cham: Palgrave Pivot), 109–145. doi: 10.1007/978-3-030-11899-0_4
Bourbonnais, R., Comeau, M., and Vézina, M. (1999). Job strain and evolution of mental health among nurses. J. Occup. Health Psychol. 4, 95–107. doi: 10.1037//1076-8998.4.2.95
Brooks, S. J., Feldman, I., Schiöth, H. B., and Titova, O. E. (2021). Important gender differences in psychosomatic and school-related complaints in relation to adolescent weight status. Sci. Rep. 11:14147.
Chandrashekar, C. R., and Math, S. B. (2006). Psychosomatic disorders in developing countries: current issues and future challenges. Curr. Opin. Psychiatry 19, 201–206. doi: 10.1097/01.yco.0000214349.46411.6a
Cristobal, E., Flavián, C., and Guinalíu, M. (2007). Perceived e-service quality (PeSQ). Manage. Serv. Qual. Int. J. 17, 317–340. doi: 10.1108/09604520710744326
Dhimole, A., Bhasin, N., Pandya, D., Dwivedi, N., and Nagarajappa, A. (2016). Psychosomatic disorders affecting the mouth: a critical review. Br. J. Med. Med. Res. 14, 1–9. doi: 10.9734/bjmmr/2016/24743
Engel, G. L. (1977). The need for a new medical model: a challenge for biomedicine. Science 196, 129–136. doi: 10.1126/science.847460
Field, A. (2013). Discovering Statistics using IBM SPSS Statistics. New York, NY: SAGE Publications.
Gaynes, B. N., Rush, A. J., Trivedi, M. H., Wisniewski, S. R., Balasubramani, G. K., McGrath, P. J., et al. (2008). Primary versus specialty care outcomes for depressed outpatients managed with measurement-based care: results from STAR*D. J. Gen. Intern. Med. 23, 551–560. doi: 10.1007/s11606-008-0522-3
Imperatori, C., Bianciardi, E., Niolu, C., Fabbricatore, M., Gentileschi, P., Di Lorenzo, G., et al. (2020). The symptom-checklist-K-9 (SCL-K-9) discriminates between overweight/obese patients with and without significant binge eating pathology: psychometric properties of an Italian version. Nutrients 12:674. doi: 10.3390/nu12030674
Kim, H.-Y. (2013). Statistical notes for clinical researchers: assessing normal distribution (2) using skewness and kurtosis. Restor. Dent. Endod. 38:52. doi: 10.5395/rde.2013.38.1.52
Kishi, R., Kitahara, T., Masuchi, A., and Kasai, S. (2002). Work-related reproductive, musculoskeletal and mental disorders among working women - History, current issues and future research directions. Indus. Health 40, 101–112. doi: 10.2486/indhealth.40.101
Li, L., Peng, T., Liu, R., Jiang, R., Liang, D., Li, X., et al. (2020). Development of the psychosomatic symptom scale (PSSS) and assessment of its reliability and validity in general hospital patients in China. Gen. Hosp. Psychiatry. 64, 1–8. doi: 10.1016/j.genhosppsych.2020.01.008
Östberg, V., Alfven, G., and Hjern, A. (2006). Living conditions and psychosomatic complaints in Swedish schoolchildren. Acta Paediatr. Int. J. Paediatr. 95, 929–934. doi: 10.1080/08035250600636545
Scott, L. D., Hwang, W. T., and Rogers, A. E. (2006). The impact of multiple care giving roles on fatigue, stress, and work performance among hospital staff nurses. J. Nurs. Adm. 36, 86–95. doi: 10.1097/00005110-200602000-00007
Shafique, N., Khalily, M. T., and Mchugh, L. (2017). Translation and validation of symptom checklist-90. Pak. J. Psychol. Res. 32, 545–561.
Shamim, T. A. (2012). Simple working type classification proposed for the psychosomatic disorders of the oral cavity. J. Coll. Phys. Surg. Pak. 22, 612–612.
Status, F. (2022). DAWN. Avilable online at: https://www.dawn.com/news/219652/defining-income-groups [accessed on November 20, 2006]
Tanku, P. (2013). Overview of translation process and equivalence in albanian literary translations. Acad. J. Interdiscip. Stud. 2:231. doi: 10.5901/ajis.2012.v2n4p231
Keywords: psychosomatic symptoms, Urdu, gender difference, PSSS scale, SCL scale, somatization
Citation: Shah SM, Jahangir M, Xu W and Yuan Y (2022) Reliability and Validity of the Urdu Version of Psychosomatic Symptoms Scale in Pakistani Patients. Front. Psychol. 13:861859. doi: 10.3389/fpsyg.2022.861859
Received: 25 January 2022; Accepted: 04 March 2022;
Published: 11 April 2022.
Edited by:
Gema T. Ruiz-Parraga, University of Malaga, SpainReviewed by:
Muhammad Aqeel, Foundation University Rawalpindi, PakistanCopyright © 2022 Shah, Jahangir, Xu and Yuan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yonggui Yuan, eXlnbGgyMDAwQHNpbmEuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.