- 1Department of Psychology, The Ohio State University, Newark, OH, United States
- 2Department of Psychology, The Ohio State University, Mansfield, OH, United States
Previous research suggests a higher perceived risk associated with a risky behavior predicts a lower likelihood of involvement in that behavior; however, this relationship can vary based on personality characteristics such as impulsivity and behavioral activation. During the COVID-19 pandemic, individuals began to re-evaluate the level of risk associated with everyday behaviors. But what about risks associated with “typical” risk-taking behaviors? In the present study, 248 undergraduate student participants completed measures of impulsivity, behavioral activation and inhibition, propensity to take risks, numeracy, and perceptions of and involvement in both risk-taking behavior and health promoting behavior (e.g., blood donation, registering as an organ donor, vaccination). Our study revealed that higher behavioral inhibition and greater propensity to take risks predicted greater likelihood of involvement in COVID-19-related risk behaviors, even after accounting for perceived risks and benefits of the behavior. Greater likelihood of involvement in social risk behaviors was predicted by greater numeracy and risk-taking propensity. Identifying as male, a greater propensity to take risks, and greater impulsivity predicted increased health/safety risk behaviors. Younger age, lower risk-taking propensity, and lower impulsivity were associated with a greater likelihood of donating blood. For the likelihood of registering to become an organ donor, increasing risk perception, both before and during the pandemic, was associated with greater likelihood of registering, but greater risk-taking propensity was associated with a decreased likelihood of organ donation registration. For flu vaccination, a greater propensity to take risks was associated with a greater likelihood of flu vaccination during the 2020–2021 flu season. Both cognitive and personality factors can predict involvement in risk-taking and health-promotion behaviors, warranting their continued examination.
Introduction
Individuals often engage in risk-taking behaviors, behaviors with the potential for a negative outcome for one’s health or wellbeing. These behaviors include use or overuse of substances (alcohol, tobacco, illicit drugs), speeding, and involvement in risky sexual behaviors. The decision to engage in these activities can come from a focus on immediate, short-term outcomes (typically rewards) at the expense of consideration of long-term outcomes (typically losses/risks) (e.g., Steinberg, 2008). Involvement in risk-taking behaviors activates the nucleus accumbens and other portions of the mesocorticolimbic (reward) pathway (Galvan et al., 2007), increasing the likelihood the behavior is repeated. Significant correlations are frequently found between self-reported involvement in different risk-taking behaviors (e.g., risky driving and substance use; Arnett et al., 1997; Bina et al., 2006; Antonopoulos et al., 2011; Gilman et al., 2015; Sween et al., 2017), although some find differences across domains (e.g., Nicholson et al., 2005; Friedman et al., 2014).
Cognitive and personality factors predict the likelihood of involvement in risk-taking behaviors. One such factor is risk perception, or one’s assessment of how risky an uncertain/ambiguous situation could be (Bettman, 1973; Baird and Thomas, 1985). Greater perceived benefits (Galvan et al., 2007; Soane et al., 2010; Hanoch et al., 2018) and lower perceived risks (Galvan et al., 2007; Mills et al., 2008; Soane et al., 2010; Gilman et al., 2015; Hanoch et al., 2018) predict greater involvement in risk-taking behaviors. Lower levels of numeracy, or the ability to understand probabilities and use this information to make decisions (Peters and Levin, 2008; Lipkus and Peters, 2009), also predict greater risk-taking (Wright et al., 2009; Brand et al., 2014; López-Pérez et al., 2017; Hanoch et al., 2018). In terms of personality, impulsivity (e.g., Donohew et al., 1999; Carlson et al., 2010; Braddock et al., 2011; Gilman et al., 2015; Maher et al., 2015; Reniers et al., 2016), sensation seeking (Dissabandara et al., 2014; Khodarahimi, 2015; Zhang et al., 2016), behavioral inhibition (BIS) and activation (BAS) (Nelson et al., 2008; Gullo et al., 2010; Braddock et al., 2011; Dissabandara et al., 2014; Reniers et al., 2016; Kemp et al., 2019; Blankenstein et al., 2020), and risk-taking propensity (Lejuez et al., 2004; Szrek et al., 2012; Markiewicz and Weber, 2013) predict involvement in risk-taking behaviors. However, in many of these studies, just one predictor, or one category of predictors, is typically examined and it is less clear how these potential predictors collectively predict risk taking. A comprehensive assessment of both cognitive and personality predictors is warranted.
A related issue is that risk perception and risk taking has shifted during the COVID-19 pandemic. Behaviors that were previously taken for granted, such as shaking hands or going grocery shopping, were now perceived as riskier to one’s health, and cognitive, demographic, and environmental factors affected risk perception (e.g., Cannito et al., 2020; Dryhurst et al., 2020; Liu et al., 2020; Alqahtani et al., 2021; Attema et al., 2021; Birhanu et al., 2021). For some individuals, risk-taking behaviors increased during the pandemic, as reflected in greater rates of speeding and substance use (e.g., Czeisler et al., 2020; Doucette et al., 2021a,b). For others, risk aversion driven by pandemic-related concerns increased, leading to lowered involvement in risky and greater involvement in health-promoting behaviors (e.g., increased hand hygiene; Shilo and Mor, 2020; Starks et al., 2020; Khan et al., 2021; Magnan et al., 2021; Shachat et al., 2021). Perceived risk of COVID-19 was associated with greater involvement in health-promoting behaviors that supported COVID-19 prevention (e.g., hand hygiene, maintaining social distance; Wise et al., 2020; Qin et al., 2021; Rui et al., 2021; Sinclair et al., 2021). Non-pandemic related health-promoting behaviors, such as blood donation and vaccination, were encouraged throughout the COVID-19 pandemic because, despite an element of risk, the benefits of these health-promoting behaviors outweighed potential costs.
Relatedly, the need for transfusions to save lives or improve quality of life (e.g., for people with sickle cell disease) continued throughout the COVID-19 pandemic, and alarm due to an unusually low blood supply was raised (American Red Cross, 2021). Motivators of blood donation behavior include perceived need, self-efficacy, and incentives, while deterrents include fear, low self-efficacy, and inconvenience (Bednall and Bove, 2011). Similarly, routine vaccinations were encouraged throughout the pandemic, with seasonal influenza vaccination strongly encouraged due to public health concern of co-circulation of influenza A (H3N2) and SARS-CoV-2 delta and omicron variants (Centres fot Diesease Control Prevention, 2021). Although blood donation and vaccination are safe overall, a risk of adverse events is present. Both are needle-related procedures and thus share risks, such as bruising at the procedure site and pre-faint symptoms (Kamel et al., 2010; McMurtry, 2020). These health-promoting behaviors share some of the same predictors as those of risk-taking behaviors. Greater perceived risks lower involvement in blood/organ donation behaviors (Allen and Butler, 1993; Norvilitis and Riley, 2001; Cohen, 2010; Mostafa, 2010; Chen, 2017), but increase the intent to vaccinate (e.g., Ferguson and Gallagher, 2007). Perceived procedural risk interacts with health messaging to produce a beneficial impact on intention to vaccinate (Ferguson and Gallagher, 2007). More specifically, among people with greater perceived risks of vaccination, exposure to health promotion messaging highlighting the vaccine effectiveness and the benefits missed out on if the vaccine is not obtained was associated with greater intention to vaccinate compared to those with lower perceived procedural risk.
The present study examines cognitive and personality predictors of involvement in both risk-taking and health-promoting behaviors within the context of the COVID-19 pandemic. In addition, we extend the current knowledge of predictors of vaccination and blood donation behaviors by assessing whether perceived risks associated with the behavior, in addition to personality and cognitive variables, predict involvement in the behavior. Specifically, we test the following hypotheses: (1) greater risk perception and numeracy, but lower impulsivity and behavioral activation, will predict lowered involvement in risk-taking behaviors; (2) greater risk perception related to COVID-19 will be associated with greater risk perception for other behaviors and predict lowered involvement in all risk-taking domains assessed; (3) self-reported perceived risk associated with getting a flu vaccine, donating blood, or registering as an organ donor will be higher when rated during COVID-19 than when retrospectively rated pre-COVID-19, and predict involvement in the behaviors; and (4) greater risk-taking propensity will predict greater vaccination and donation behaviors.
Materials and Methods
Participants
We completed several waves of data collection during the COVID-19 pandemic, all among undergraduate students who received course credit for participation in research studies. Participants were invited to complete the surveys in October 2020 and January 2021, corresponding to the beginning of the Fall and Spring semesters. At those times, the COVID-19 vaccine was not readily available, mask and distancing mandates were in place on campus, and the average University positivity rate was 0.81–2.14%. We allowed as many students as were interested to complete the study, leading to an initial sample of 272 participants. Participants were excluded from analyses due to missing data on multiple measures (n = 16) or reporting being interrupted a lot (n = 2), distracted a lot (n = 3), influenced by others (n = 2), or a combination of those factors (n = 1). Because risk perception varies by age, four participants over age 35 were excluded per American Psychological Association guidelines (VandenBos, 2007). Our final sample included 244 participants [ages 18–35 (M = 19.14, SD = 2.12), 98 males, 64.2% White, 23.0% Black or African American]. We conducted power analyses (G*Power; Faul et al., 2007) to determine the maximum effect size we were adequately powered to detect. Using a two-tailed test, this sample size could detect an effect size of f2 = 0.12 (small-moderate) with a power of 0.95 and α = 0.05.
Measures and Procedure
The study protocol was determined exempt from IRB review due to the anonymous survey design. All ethical guidelines were followed. Participants completed all measures online via a Qualtrics survey. After informed consent, participants completed a series of questionnaires in a randomized order that included the measures detailed below.
Personality Variables
The Barratt Impulsiveness Scale (BIS-11; Patton et al., 1995) assesses impulsivity as a personality construct via a series of 30 questions. Participants respond on a 1 (Rarely/never) to 4 (Almost always/always) scale. Average scores were calculated for the overall impulsiveness score (α = 0.809), with higher scores indicating greater levels of impulsiveness.
The BIS/BAS (Carver and White, 1994) assesses two competing systems: behavioral inhibition (BIS) and behavioral activation (BAS). Individuals high in BIS experience risk-avoidant behaviors in response to threats whereas individuals high in BAS instead engage in risk-seeking behaviors in response to reward signals. Participants responded to the 24 items on a 1 (Very true for me) to 4 (Very false for me) scale. Average scores were calculated for overall BIS (α = 0.799) and BAS (α = 0.810) scores, with higher scores indicating greater risk-avoidance (BIS) or risk-seeking (BAS).
Risk Perception Variables
The General Risk Propensity Scale (GRiPS; Zhang et al., 2019) assesses an individuals’ likelihood of taking risks across different situations. Participants responded to eight items on a 1 (Strongly disagree) to 6 (Strongly agree) scale. Two versions were administered: the standard GRiPS, which uses the term “In general,” at the beginning of each item (α = 0.913) and a modified GRiPS that instead used “During COVID-19” at the beginning of each item (α = 0.949). For each, an average score was calculated with higher values indicating greater propensity to take risks.
Participants also responded to a single-item assessment of general risk-taking, “How willing are you to take risks, in general?” on a 0 (not at all willing) to 10 (very willing) scale (Dohmen et al., 2011).
The expanded Lipkus numeracy scale (Lipkus et al., 2001) was administered. The measure assesses understanding of numbers, percentages, and relative risks, with three items assessing general numeracy and eight assessing risk numeracy. Each response was scored as correct or incorrect, then summed total scores were calculated for both general and risk numeracy.
Health Promotion and Risk-Related Variables
The Domain-Specific Risk Taking Scale (DOSPERT; Blais and Weber, 2006) was administered. Due to study time constraints, only the Social and Health/Safety subscales were utilized. A third subscale was developed to assess risk-taking during COVID-19 (see Kowalsky, in preparation for development information). For each subscale, participants responded to a series of risky situations in terms of (1) likelihood of involvement (1 = Extremely unlikely, 7 = Extremely likely), (2) perceived risks (1 = Not at all risky, 7 = Extremely risky), and (3) perceived benefits (1 = No benefits at all, 7 = Great benefits). Higher average scores indicated greater likelihood of involvement, greater perceived risks, and greater perceived benefits. Internal consistency was moderate to strong across subscales for likelihood of involvement (α = 0.635-0.890), perceived risks (α = 0.7052-0.952), and perceived benefits (α = 0.631-0.894).
Participants responded to a series of questions regarding their history of vaccination and donation behaviors. Specifically, participants were asked to indicate (0 = no, 1 = yes) whether they were vaccinated against the flu for the 2020–2021 season, ever donated blood, or ever registered to be an organ donor. Participants also indicated their perceived level of risk associated with each behavior. They used a 1 (Not at all risky) to 7 (Extremely risky) scale to indicate how much risk was associated with donating blood, registering to be an organ donor, and getting vaccinated against the seasonal flu, prior to (i.e., using retrospective self-report) and during the COVID-19 pandemic.
Finally, participants completed a questionnaire assessing demographic and background information. They then were debriefed and course credit was assigned. A portion of the participants completed follow-up testing (Time 2) at the end of each semester. Given the small sample size, these analyses are presented in Supplemental Analysis 1.
Data Analysis
The hypotheses and analyses were registered at the Open Science Framework (OSF)1 following data collection but prior to analysis. To maximize power, we collapsed across the three BIS-11 subscale scores (Attentional Impulsivity, Motor Impulsivity, Non-planning Impulsivity) and the three BAS subscale scores (Drive, Fun Seeking, Reward Responsiveness) to create combined BIS-11 and BAS scores. This did not change the pattern of results, and the analyses by BIS-11 and BAS subscales can be found in Supplemental Analysis 2.
First, we assessed potential differences based on the time of data collection. The only significant differences emerged on behavioral inhibition, t(242) = 2.26, p = 0.012 (lower in Spring), and behavioral activation, t(242) = −2.99, p = 0.003 (higher in Spring). Therefore, a categorical variable for data collection time (1 = Fall, 2 = Spring) was added to the regression analyses. We also included age and gender as control variables, as risk perception can vary by these factors (e.g., Bonem et al., 2015; Brown et al., 2021), including during the COVID-19 pandemic (e.g., Alsharawy et al., 2021; Rosi et al., 2021).
Several blinded ex post analyses were conducted to assess the study hypotheses. First, Pearson correlations were examined to assess relationships between perceived risks and likelihood of involvement across DOSPERT risk-taking domains. Next, we conducted linear and logistic regressions examining whether risk and benefit perception, impulsivity, behavioral activation/inhibition, and numeracy predicted likelihood of involvement in risk-taking (DOSPERT domains) and health-promoting (blood donation, organ donation, vaccination) behaviors. Paired-samples t-tests were used to examine whether donating blood, registering to be an organ donor, or getting the flu vaccine were rated as riskier during COVID-19 than prior to COVID-19.
Results
Correlations
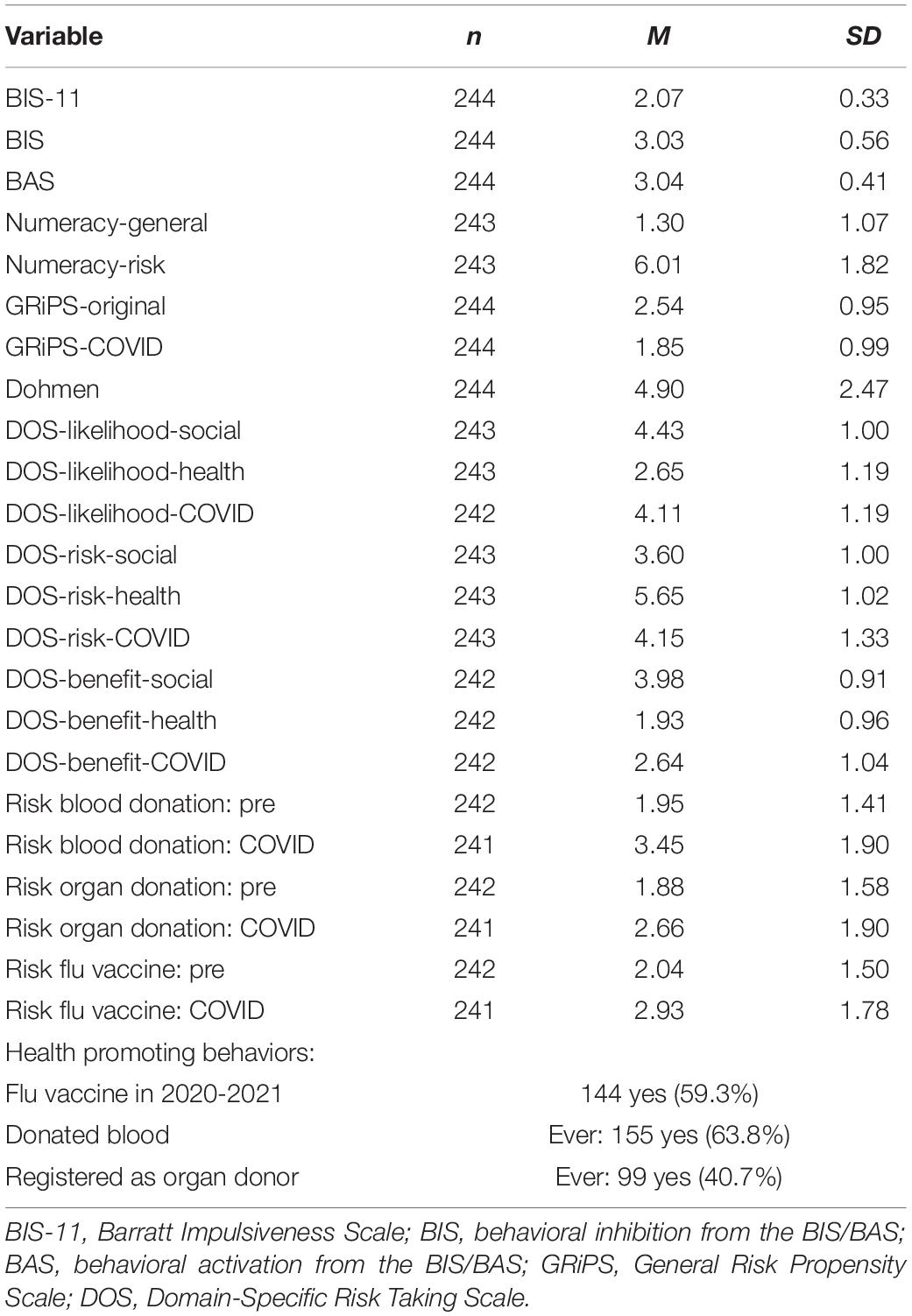
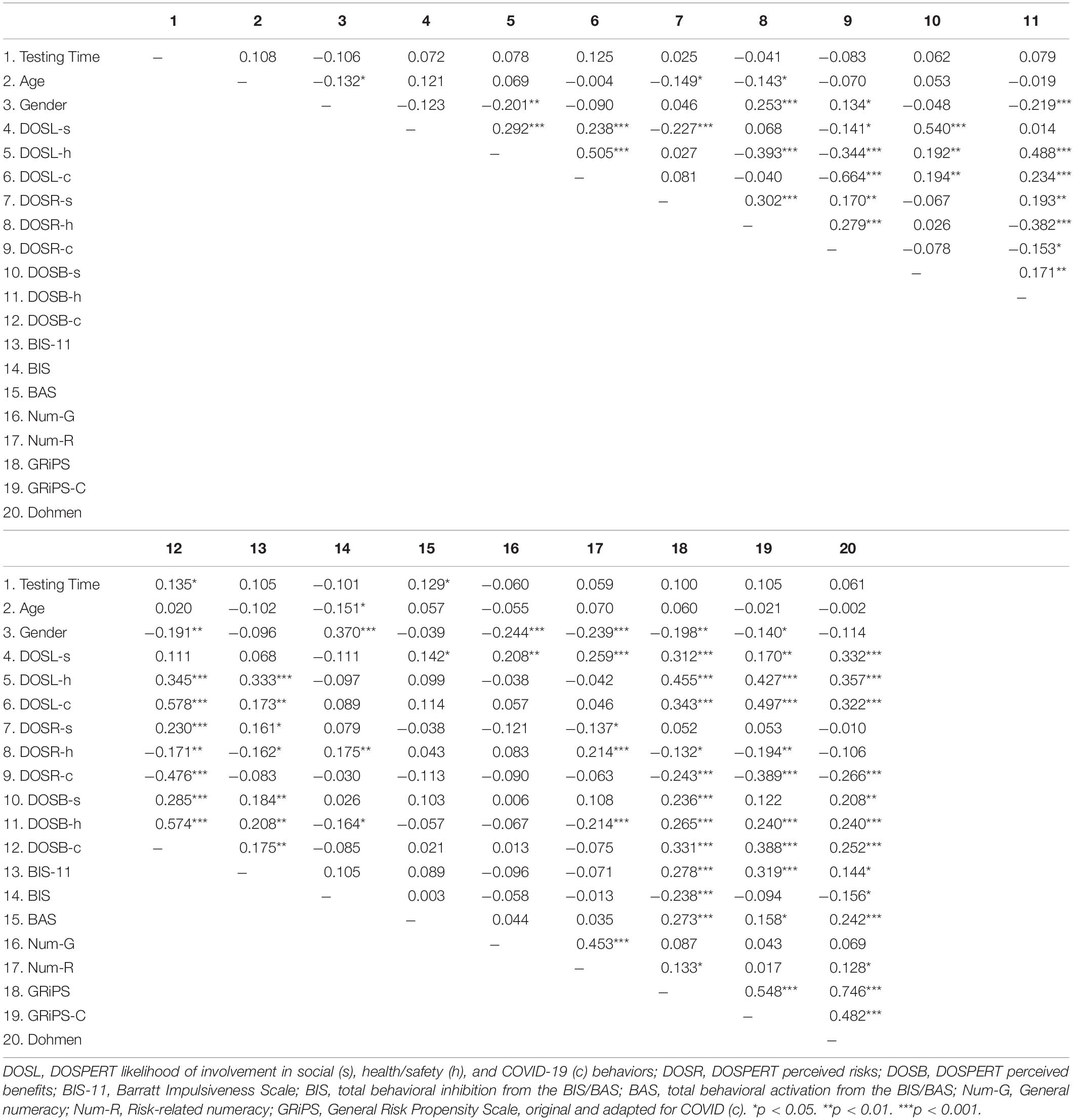
Means and standard deviations for all variables are included in Table 1. A correlation matrix (Table 2) indicated significant correlations between perceived risks, perceived benefits, and likelihood of involvement in different risk-taking behaviors. Specifically, positive correlations were found between perceived risks associated with social, health/safety, and COVID-19 behaviors (rs> 0.169, ps < 0.01). Positive correlations were also found between perceived benefits on the three DOSPERT subscales (rs > 0.170, ps < 0.01). Participants who reported a high likelihood of involvement in one DOSPERT risk-taking domain tended to also report a high likelihood of involvement in another DOSPERT domain (rs > 0.237, ps < 0.001). Thus, participants tended to interpret the risks and benefits of different types of risk-taking behaviors in a similar manner. Significant correlations were also found in the expected directions between impulsivity, BIS, BAS, and risk propensity (rs > 0.127, ps < 0.05), but not numeracy.
Predicting Risk-Taking Behaviors
We next assessed whether perceived risk on the DOSPERT COVID-19 subscale predicted likelihood of involvement in health/safety, social, and COVID-related risk behaviors. Lower perceived risks predicted a greater likelihood of involvement in COVID-19-related, F(1, 240) = 189.37, p < 0.001, R2 = 0.441, B = −0.594, β = −0.664, health/safety, F(1,241) = 32.24, p < 0.001, R2 = 0.118, B = −0.308, β = 0.344, and social, F(1, 241) = 4.86, p = 0.028, R2 = 0.020, B = −0.106, β = −0.141, risk behaviors.
Next, linear regression analyses were conducted to examine whether perceived risks and benefits predicted likelihood of risk-taking behavior (see Table 3). For each analysis, age, gender (1 = Male, 2 = Female), and time of testing were entered in Step 1 as controls. Next, perceived risks and benefits for the specific set of behaviors were entered in Step 2 (behavior-specific perceived risks and benefits). Scores on the GRiPS, Dohmen, and numeracy scales were included in Step 3 (more generalized risk taking). Of note, we conducted two sets of regressions: one with the original GRiPS and one with the GRiPS modified for COVID-19. Finally, scores on the BIS-11 and BIS/BAS were entered in Step 4 (personality characteristics associated with risk taking). Collinearity statistics were within the reasonable range (Tolerance > 0.361, VIF < 2.767). Females reported a lower likelihood of involvement in health/safety behaviors only. Collectively, lower risk perception and greater benefit perception for COVID-19-related, health/safety, and social risk behaviors predicted greater likelihood of involvement in the associated behavior. After accounting for perceived risks and benefits, higher behavioral inhibition and propensity to take risks (adapted for COVID-19) predicted greater likelihood of involvement in COVID-19 risk behaviors. Greater likelihood of involvement in social risk behaviors was predicted by greater numeracy and greater risk-taking propensity. Finally, increased health/safety risk behaviors were predicted by greater propensity to take risks (both original and adapted for COVID-19) and greater impulsivity.

Table 3. Results of linear regression analyses predicting likelihood of engaging in COVID-19-related, social, and health/safety risky behaviors.
Predicting Health-Promoting Behaviors
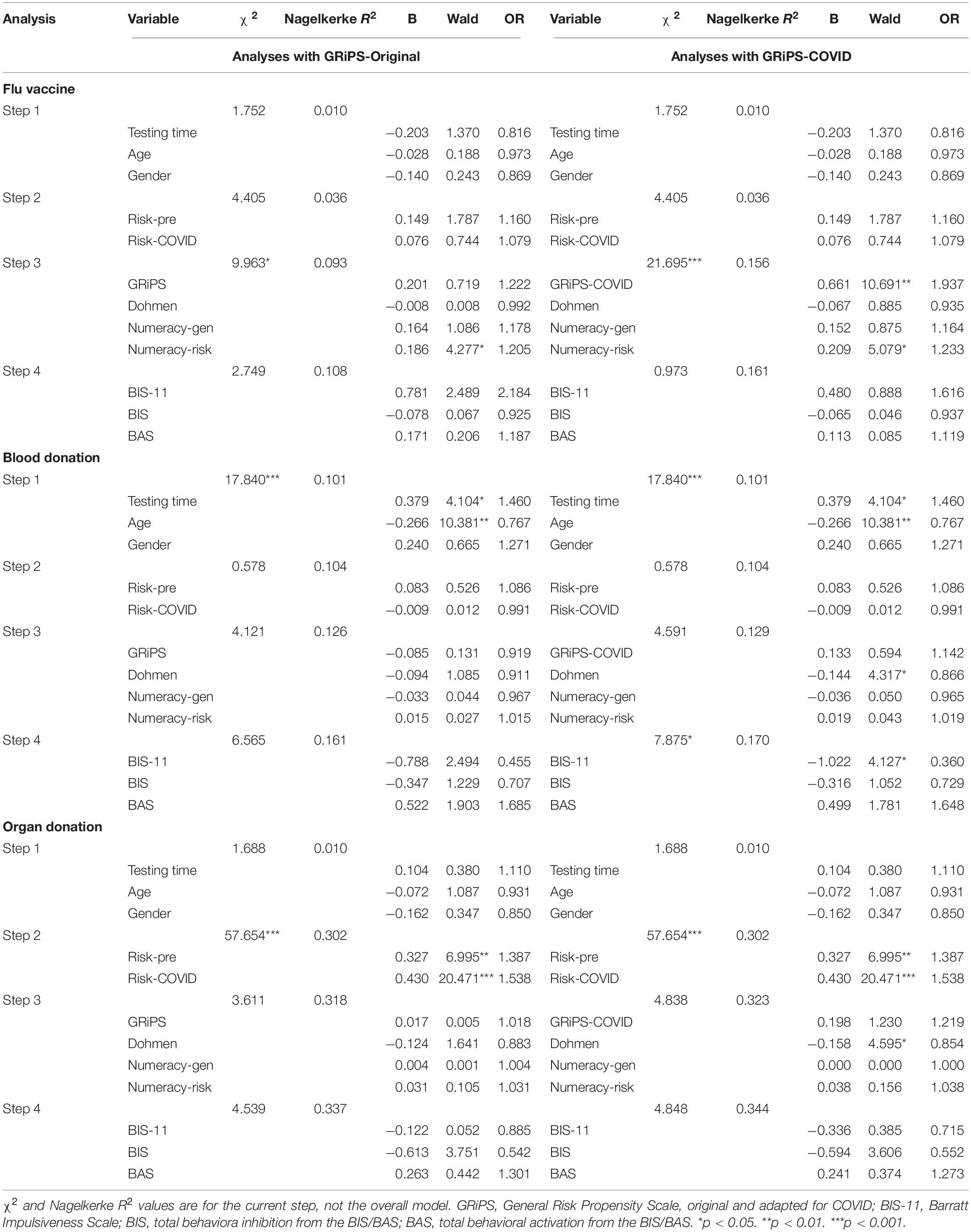
We next examined blood donation, organ donation, and vaccination behaviors. First, paired-samples t-tests assessed the extent to which participants perceived risks associated with these behaviors as different before vs. during COVID-19. Participants reported that donating blood, t(240) = −12.38, p < 0.001, Cohen’s d = 0.797; registering as an organ donor, t(240) = −7.15, p < 0.001, d = 0.460; and vaccinating against the seasonal flu, t(240) = −7.96, p < 0.001, d = 0.513; were all riskier during compared to before the COVID-19 pandemic. We used these perceived risk ratings, both pre- and during COVID-19, as predictors of self-reported involvement in these activities (Table 4). Self-reported history of blood donation, registering as an organ donor, or getting the seasonal flu vaccine were coded as 0 (No) and 1 (Yes). The logistic regressions followed the same format at the DOSPERT regressions, with control variables entered in Step 1, perceived risks of the behavior in Step 2, risk-taking propensity variables in Step 3, and personality variables in Step 4.
For a history of blood donation, the overall regression model, using the GRiPS adapted for COVID, was significant, χ2(12) = 30.885, p = 0.002, and explained 17.0% (Nagelkerke R2) of the variance while correctly classifying 67.5% of cases. Completing the survey in January, younger age, and lower risk propensity and impulsivity were associated with a greater likelihood of donating blood. Except for the Dohmen and impulsivity, these relationships held when the original GRiPS was included in the model.
The overall logistic regression model, using the GRiPS adapted for COVID, was significant for organ donation registration behavior, χ2(12) = 65.446, p < 0.001, and explained 33.5% (Nagelkerke R2) of the variance while correctly classifying 73.8% of cases. Increasing risk perception, both pre- and during COVID, was associated with a greater likelihood of registering to be an organ donor. In addition, greater risk-taking propensity (Dohmen) was associated with a decreased likelihood of registering to be an organ donor. Except for the Dohmen, these relationships held when the original GRiPS was included in the model.
The overall model for flu vaccination behaviors, when the original GRiPS was in the model, was not significant, χ2(12) = 18.868, p = 0.092, Nagelkerke R2 = 0.108. When the GRiPS-COVID-19 adaptation was utilized, the overall model was significant, χ2(12) = 28.825, p = 0.004, Nagelkerke R2 = 0.161, and correctly classified 65.9% of participants. A greater propensity to take risks, as assessed by the GRiPS adapted for COVID-19, and greater numeracy were associated with a greater likelihood of flu vaccination during the 2020–2021 season.
Discussion
This study examined cognitive and personality predictors of risk-taking and health-promoting behaviors during the COVID-19 pandemic. Other research demonstrated both increased risk-taking (e.g., Czeisler et al., 2020; Doucette et al., 2021a,b) and risk aversion (e.g., Shilo and Mor, 2020; Starks et al., 2020; Khan et al., 2021; Magnan et al., 2021; Shachat et al., 2021) during the pandemic, and we examined the extent to which previously identified predictors of risk predicted risk-taking during a pandemic.
First, we assessed whether greater risk perception and numeracy, but lower impulsivity and BAS, predicted lower involvement in risk-taking behaviors. Our results partially support this hypothesis. Perceived risks and benefits were the most consistent predictors of risk-taking. Across health/safety, social, and COVID-19-related behaviors, participants were more likely to take a risk if they endorsed low risk and high benefit perception, consistent with research prior to the pandemic (Galvan et al., 2007; Soane et al., 2010; Hanoch et al., 2018). After accounting for these factors, participants endorsing a high risk-taking propensity endorsed a greater likelihood of involvement in all risk-taking behaviors assessed. The influence of the other predictors depended on the type of behavior examined: (1) greater BIS predicted greater COVID-19-related risk-taking, (2) greater numeracy predicted greater social risk-taking, and (3) greater impulsivity predicted greater health/safety-related risk-taking. These results are consistent with some previous research indicating more impulsive individuals take more risks (Donohew et al., 1999; Carlson et al., 2010; Braddock et al., 2011; Gilman et al., 2015; Maher et al., 2015; Reniers et al., 2016), but counter those finding lower BIS (Braddock et al., 2011; Maher et al., 2015), lower numeracy (Brand et al., 2014; Hanoch et al., 2018), and greater BAS (Gullo et al., 2010; Dissabandara et al., 2014; Blankenstein et al., 2020) predict greater risk-taking behavior. Although further research is warranted to assess these relationships, it is possible that participants who experienced greater risk aversion (high BIS) but also a greater likelihood of COVID-19-related risk-taking behavior did not view the behaviors as particularly risky, or at least not risky enough to signal aversion to the behavior. The positive relationship between numeracy and social risk-taking runs counter to previous research and to expectation; however, examination of the specific DOSPERT items that make up this scale may play a role. While the health/safety and COVID-19-related DOSPERT items focus on behaviors that could be riskier during COVID-19 (e.g., unprotected sex, overuse of alcohol), the social subscale items do not rely on an in-person, physical interaction with someone (e.g., disagreeing with someone, speaking up in a meeting). It is possible that participants, including those who are knowledgeable about probabilities, recognized the low risk of COVID-19 in these situations. It is also possible that more numerate participants took greater risks due to how they weighed risks vs. benefits, in keeping with previous research indicating that the relative weighting of these factors changes the decision to take risks (e.g., Reyna and Farley, 2006; Maslowsky et al., 2011; Reyna et al., 2011). But in our findings, numeracy did not predict involvement in health/safety or COVID-19-related behaviors, and future research should investigate this anomaly.
We next examined relationships between COVID-19-related risk perception and involvement in different risk behaviors, and whether changing risk perception might affect both risk-taking and health-promoting behaviors. The results supported our hypothesis, as participants reporting greater COVID-19-related risk perception also rated social and health/safety behaviors as riskier. In terms of health-promoting behaviors, participants reported that donating blood, registering as an organ donor, and vaccinating against the seasonal flu were all riskier during vs. prior to the pandemic. Risk perception also affected the likelihood of registering as an organ donor but not of engaging in vaccination or blood donation behaviors. A greater risk-taking propensity predicted increased likelihood of vaccination but decreased likelihood of blood and organ donation. The only personality predictor to emerge was impulsivity, as less impulsivity was associated with greater likelihood of blood donation. Taken together, we find relatively little evidence that the personality variables previously shown to predict involvement in risk-taking behavior predict these health-promoting behaviors.
There are several limitations that could affect generalizability of the findings. Not all areas of risk-taking or health-promoting behavior were assessed. It is possible that personality and cognitive variables differentially predict involvement in other risk-taking behaviors. In addition, we did not conduct an exhaustive assessment of all cognitive or personality predictors; thus, future research should assess other facets that may affect risk perception. We utilized a convenience sample, and it is unclear if these same factors would predict behavior among older or more diverse individuals. As the relationship between factors is complex, future research should utilize structural equation modeling techniques in these larger and more diverse samples. Finally, we relied on self-report of both the predictors and of risk-taking behaviors. Although many previous studies have utilized the DOSPERT to assess risk, future studies should pair behavioral with self-report measures to assess the construct more fully.
Taken together, the present study provides evidence that cognitive and personality factors predict involvement in risk-taking and health-promoting behaviors, but the effect varies by the particular behavior studied. Future research examining risk-taking and health promotion should continue to assess different behaviors, as targets of interventions may depend on the particular behavior. Risk perception appears to differ based on the context of the behavior/situation, as can how cognitive and personality variables affect this relationship. From a health behavior perspective, individuals rated health behaviors with an interpersonal element, such as donating blood or receiving a vaccine, as more risky during COVID-19 vs. pre-pandemic. Although we relied on retrospective self-report of estimated risk, future research should examine longitudinally how risk perception changes as we emerge from the pandemic. During COVID-19, there has been an increased need for both blood donation and vaccination, as both behaviors support the individual and the community as a whole. Moving forward, there will likely be a need to address novel risk-related concerns within local medical settings (e.g., strategies in place to mitigate spread of a virus, how these strategies are communicated to reduce risk perception). Conveying important health-related information in a way that increases the likelihood of health-promoting and decreases the likelihood of risk-taking behaviors is vital to a healthy community.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://osf.io/aetfc/?view_only=20b3376236244f40a9a810303938dab3.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their informed consent to participate in this study.
Author Contributions
MB, JK, and AB designed the study and contributed to the drafting and revision of the manuscript. MB collected and analyzed the data. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.840284/full#supplementary-material
Footnotes
References
Allen, J., and Butler, D. D. (1993). Assessing the effects of donor knowledge and perceived risk on intentions to donate blood. J. Health Care Mark. 13, 26–33.
Alqahtani, M. M. J., Arnout, B. A., Fadhel, F. H., and Sufyan, N. S. S. (2021). Risk perceptions of COVID-19 and its impact on precautionary behavior: a qualitative study. Patient Educ. Couns. 104, 1860–1867. doi: 10.1016/j.pec.2021.02.025
Alsharawy, A., Spoon, R., Smith, A., and Ball, S. (2021). Gender differences in fear and risk perception during the COVID-19 pandemic. Front. Psychol. 12:689467. doi: 10.3389/fpsyg.2021.689467
Antonopoulos, C. N., Germeni, E., Bacopoulou, F., Kalampoki, V., Maltezos, S., Skalkidis, I., et al. (2011). Assessing the impact of risk-taking behavior on road crash involvement among University students residing in two Mediterranean countries. Saf. Sci. 49, 933–938. doi: 10.1016/j.ssci.2011.03.013
American Red Cross (2021). Blood Donors Urgently Needed This Fall as COVID-19 Pandemic Continues. Available online at: https://www.redcross.org/about-us/news-and-events/press-release/2021/blood-donors-urgently-needed-this-fall-as-covid-19-pandemic-continues.html (accessed December 9, 2021).
Arnett, J. J., Offer, D., and Fine, M. A. (1997). Reckless driving in adolescence: ‘state’ and ‘trait’ factors. Accid. Anal. Prev. 29, 57–63. doi: 10.1016/S00001-4575(97)97007-8
Attema, A. E., L’Haridon, O., Raude, J., Seror, V., and The Coconel Group (2021). Beliefs and risk perceptions about COVID-19: evidence from two successive French representative surveys during lockdown. Front. Psychol. 12:619145. doi: 10.3389/fpsyg.2021.619145
Baird, I. S., and Thomas, H. (1985). Toward a contingency model of strategic risk-taking. Acad. Manage. Rev. 10, 230–243. doi: 10.5465/amr.1985.4278108
Bednall, T. C., and Bove, L. L. (2011). Donating blood: a meta-analytic review of self-reported motivators and deterrents. Transfus. Med. Rev. 25, 317–334. doi: 10.1016/j.tmrv.2011.04.005
Bettman, J. R. (1973). Perceived risk and its components: a model and empirical test. J. Mark. Res. 10, 184–190. doi: 10.1177/002224377301000209
Bina, M., Graziano, F., and Bonino, S. (2006). Risky driving and lifestyles in adolescence. Accid. Anal. Prev. 38, 472–481. doi: 10.1016/j.aap.2005/11.003
Birhanu, Z., Ambelu, A., Fufa, D., Mecha, M., Zeynudin, A., Abafita, J., et al. (2021). Risk perceptions and attitudinal responses to COVID-19 pandemic: an online survey in Ethiopia. BMC Public Health 21:981. doi: 10.1186/s12889-021-10939-x
Blais, A. R., and Weber, E. U. (2006). A domain-specific risk-taking (DOSPERT) scale for adult populations. Judgm. Decis. Mak. 1, 33–47.
Blankenstein, N. E., Telzer, E. H., Do, K. T., van Duijvenvoorde, A. C. K., and Crone, E. A. (2020). Behavioral and neural pathways supporting the development of prosocial and risk-taking behavior across adolescence. Child Dev. 91, e665–e681. doi: 10.1111/cdev.13292
Bonem, E. M., Ellsworth, P. C., and Gonzalez, R. (2015). Age differences in risk: perceptions, intentions and domains. J. Behav. Decis. Mak. 28, 317–330. doi: 10.1002/bdm.1848
Braddock, K. H., Dillard, J. P., Voigt, D. C., Stephenson, M. T., Sopory, P., and Anderson, J. W. (2011). Impulsivity partially mediates the relationship between BIS/BAS and risky health behaviors. J. Pers. 79, 793–810. doi: 10.1111/j.1467-6494.2011.00699.x
Brand, M., Schiebener, J., Pertl, M.-T., and Delazer, M. (2014). Know the risk, take the win: how executive functions and probability processing influence advantageous decision making under risk conditions. J. Clin. Exp. Neuropsychol. 36, 914–929. doi: 10.1080/13803395.2014.955783
Brown, G. D., Largey, A., and McMullan, C. (2021). The impact of gender on risk perception: implications of EU member states’ national risk assessment processes. Int. J. Disaster Risk Reduct. 63:102452. doi: 10.1016/j.ijdrr.2021.102452
Cannito, L., Di Crosta, A., Palumbo, R., Ceccato, I., Anzani, S., La Malva, P., et al. (2020). Health anxiety and attentional bias toward virus-related stimuli during the COVID-19 pandemic. Sci. Rep. 10:16476. doi: 10.1038/s41598-020-73599-8
Carlson, S. R., Johnson, S. C., and Jacobs, P. C. (2010). Disinhibited characteristics and binge drinking among university student drinkers. Addict. Behav. 35, 242–251. doi: 10.1016/j.addbeh.2009.10.020
Carver, C. S., and White, T. L. (1994). Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: the BIS/BAS scales. J. Pers. Soc. Psychol. 67, 319–333. doi: 10.1037/0022-3514.67.2.319
Centres fot Diesease Control Prevention (2021). Increasing Seasonal Influenza A (H3n2) Activity, Especially Among Young Adults And In College And University Settings, During SARS-CoV-2 Co-Circulation. Available online at: https://emergency.cdc.gov/han/2021/han00458.asp (accesed December 9, 2021).
Chen, L. (2017). Applying the extended theory of planned behaviour to predict Chinese people’s non-remunerated blood donation intention and behaviour: the roles of perceived risk and trust in blood collection agencies. Asian J. Soc. Psychol. 20, 221–231. doi: 10.1111/ajsp.12190
Cohen, E. L. (2010). The role of message frame, perceived risk, and ambivalence in individuals’ decisions to become organ donors. Health Commun. 25, 758–769. doi: 10.1080/10410236.2010.521923
Czeisler, M. É, Lane, R. I., Petrosky, E., Wiley, J. F., Christensen, A., Rashid Njai, R., et al. (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24-30, 2020. MMWR Morb. Mortal. Wkly Rep. 69, 1049–1057. doi: 10.15585/mmwr.mm6932a1
Dissabandara, L. O., Loxton, N. J., Dias, S. R., Dodd, P. R., Daglish, M., and Stadlin, A. (2014). Dependent heroin use and associated risky behaviour: the role of rash impulsiveness and reward sensitivity. Addict. Behav. 39, 71–76. doi: 10.1016/j.addbeh.2013.06.009
Dohmen, T., Falk, A., Huffman, D., Sunde, U., Schupp, J., and Wagner, G. G. (2011). Individual risk attitudes: measurement, determinants, and behavioral consequences. J. Eur. Econ. Assoc. 9, 522–550. doi: 10.1111/j.1542-4774.2011.01015.x
Donohew, L., Hoyle, R., Clayton, R. R., Skinner, W., Colon, S., and Rice, R. E. (1999). Sensation-seeking and drug use by adolescents and their friends: models for marijuana and alcohol. J. Stud. Alcohol 60, 622–631. doi: 10.15288/jsa.1999.60.622
Doucette, M. L., Tucker, A., August, M. E., Gates, J. D., Shapiro, D., Ehsani, J. P., et al. (2021a). Evaluation of motor vehicle crash rates during and after the COVID-19-associated stay-at-home order in Connecticut. Accid. Anal. Prev. 162:106399. doi: 10.1016/j.aap.2021.106399
Doucette, M. L., Tucker, A., Auguste, M. E., Watkins, A., Green, C., Pereira, F. E., et al. (2021b). Initial impact of COVID-19’s stay-at-home order on motor vehicle traffic and crash patterns in Connecticut: an interrupted time series analysis. Inj. Prev. 27, 3–9. doi: 10.1136/injuryprev-2020-043945
Dryhurst, S., Schneider, C. R., Kerr, J., Freeman, A. L. J., Recchia, G., van der Bles, A. M., et al. (2020). Risk perceptions of COVID-19 around the world. J. Risk Res. 23, 994–1006. doi: 10.1080/13669877.2020.1758193
Faul, F., Erdfelder, E., Lang, A. G., and Buchner, A. (2007). G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39, 175–191. doi: 10.3758/bf03193146
Ferguson, E., and Gallagher, L. (2007). Message framing with respect to decisions about vaccination: the roles of frame valence, frame method, and perceived risk. Br. J. Psychol. 98, 667–680. doi: 10.1358/000712607X190692
Friedman, D., Isaac, R. M., James, D., and Sunder, S. (2014). Risky Curves: On the Empirical Failure of Expected Utility. (Abingdon: Routledge)
Galvan, A., Hare, T., Voss, H., Glover, G., and Casey, B. J. (2007). Risk-taking and the adolescent brain: who is at risk? Dev. Sci. 10, F8–F14. doi: 10.1111/j.1467-7687.2006.00579.x
Gilman, J. M., Calderon, V., Curran, M. T., and Evins, A. E. (2015). Young adult cannabis users report greater propensity for risk-taking only in non-monetary domains. Drug and Alcohol Depend. 147, 26–31. doi: 10.1016/j.drugalcdep.2014.12.020
Gullo, M. J., Ward, E., Dawe, S., Powell, J., and Jackson, C. J. (2010). Support for a two-factor model of impulsivity and hazardous substance use in British and Australian young adults. J. Res. Pers. 45, 10–18. doi: 10.1016/j.jrp.2010.11.002
Hanoch, Y., Rolison, J. J., and Freund, A. M. (2018). Does medical risk perception and risk taking change with age? Risk Anal. 38, 917–928. doi: 10.1111/risa.12692
Kamel, H., Tomasulo, P., Bravo, M., Wiltbank, T., Cusick, R., James, R. C., et al. (2010). Delayed adverse reactions to blood donation. Transfusion 50, 556–565. doi: 10.1111/j.1537-2995.2009.02397.x
Kemp, E., Sadeh, N., and Baskin-Sommers, A. (2019). A latent profile analysis of affective triggers for risky and impulsive behavior. Front. Psychol. 9:2651. doi: 10.3389/fpsyg.2018.02651
Khan, A. J., Nishimi, K., Tripp, P., Maven, D., Jiha, A., Woodward, E., et al. (2021). COVID-19 related moral injury: associations with pandemic-related perceived threat and risky and protective behaviors. J. Psychiatr. Res. 142, 80–88. doi: 10.1016/j.jpsychires.2021.07.037
Khodarahimi, S. (2015). Sensation-seeking and risk-taking behaviors: a study on young Iranian adults. Appl. Res. Qual. Life 10, 721–734. doi: 10.1007/s11482-014-9350-2
Lejuez, C. W., Simmons, B. L., Aklin, W. M., Daughters, S. B., and Dvir, S. (2004). Risk-taking propensity and risky sexual behavior of individuals in residential substance use treatment. Addict. Behav. 29, 1643–1647. doi: 10.1016/j.addbeh.2004.02.035
Lipkus, I., Samsa, G., and Rimer, B. K. (2001). General performance on a numeracy scale among highly educated samples. Med. Decis. Mak. 21, 37–44. doi: 10.1177/0272989X0102100105
Lipkus, I. M., and Peters, E. (2009). Understanding the role of numeracy in health: proposed theoretical framework and practical insights. Health Educ. Behav. 36, 1065–1081. doi: 10.1177/1090198109341533
Liu, M., Zhang, H., and Huang, H. (2020). Media exposure to COVID-19 information, risk perception, social and geographical proximity, and self-rated anxiety in China. BMC Public Health 20:1649. doi: 10.1186/s12889-020-09761-8
López-Pérez, B., Barnes, A., Frosch, D. L., and Hanoch, Y. (2017). Predicting prostate cancer treatment choices: the role of numeracy, time discounting, and risk attitudes. J. Health Psychol. 22, 788–797. doi: 10.1177/1359105315615931
Magnan, R. E., Gibson, L. P., and Bryan, A. D. (2021). Cognitive and affective risk beliefs and their association with protective health behavior in response to the novel health threat of COVID-19. J. Behav. Med. 44, 285–295. doi: 10.10007/s10865-021-00202-4
Maher, A. M., Thomson, C. J., and Carlson, S. R. (2015). Risk-taking and impulsive personality traits in proficient downhill sports enthusiasts. Pers. Individ. Differ. 79, 20–24. doi: 10.1016/j.paid.2015.01.041
Markiewicz, L., and Weber, E. U. (2013). DOSPERT’s gambling risk-taking propensity scale predicts excessive stock trading. J. Behav. Financ. 14, 65–78. doi: 10.1080/15427560.2013.762000
Maslowsky, J., Buvinger, E., Keating, D. P., Steinberg, L., and Cauffman, E. (2011). Cost-benefit analysis mediation of the relationship between sensation seeking and risk behavior. Pers. Indiv. Diff. 51, 802–806. doi: 10.1016/j.paid.2011.06.028
McMurtry, C. M. (2020). Managing immunization stress-related response: a contributor to sustaining trust in vaccines. Can. Commun. Dis. Rep. 46, 210–218. doi: 10.14745/ccdr.v46i06a10
Mills, B., Reyna, V. F., and Estrada, S. (2008). Explaining contradictory relations between risk perception and risk taking. Psychol. Sci. 19, 429–433. doi: 10.1111/j.1467-9280.2008.02104.x
Mostafa, M. M. (2010). Altruistic, cognitive, and attitudinal determinants of organ donation intention in Egypt: a social marketing perspective. Health Mark. Q. 27, 97–115. doi: 10.1080/07359680903519867
Nelson, M. C., Lust, K., Story, M., and Ehlinger, E. (2008). Credit card debt, stress and key health risk behaviors among college students. Am. J. Health Promot. 22, 400–406. doi: 10.4278/ajhp.22.6.400
Nicholson, N., Soane, E., Fenton-O’Creevy, M., and Willman, P. (2005). Personality and domain-specific risk taking. J. Risk Res. 8, 157–176. doi: 10.1080/1366987032000123856
Norvilitis, J. M., and Riley, T. M. (2001). Exploring the motivations of bone marrow typing donors. J. Psycho. Oncol. 19, 49–62. doi: 10.1300/J077v19n01_04
Patton, J. H., Stanford, M. S., and Barratt, E. S. (1995). Factor structure of the barratt impulsiveness scale. J. Clin. Psychol. 51, 768–774.
Peters, E., and Levin, I. P. (2008). Dissecting the risky-choice framing effect: numeracy as an individual-difference factor in weighting risky and riskless options. Judgm. Decis. Mak. 3, 435–448.
Qin, H., Sanders, C., Prasetyo, Y., Syukron, M., and Prentice, E. (2021). Exploring the dynamic relationships between risk perception and behavior in response to the Coronavirus disease 2019 (COVID-19) outbreak. Soc. Sci. Med. 285:114267. doi: 10.1016/j.socscimed.2021.114267
Reniers, R. L. E. P., Murphy, L., Lin, A., Bartolomé, S. P., and Wood, S. J. (2016). Risk perception and risk-taking behaviour during adolescence: the influence of personality and gender. PLoS One 11:e0153842. doi: 10.1371/journal.pone.0153842
Reyna, V. F., Estrada, S. M., DeMarinis, J. A., Ryers, R. M., Stanisz, J. M., and Mills, B. A. (2011). Neurobiological and memory models of risky decision making in adolescents versus young adults. J. Exp. Psychol. Learn., Mem. Cogn. 37, 1125–1142. doi: 10.1037/a0023943
Reyna, V. F., and Farley, F. (2006). Risk and rationality in adolescent decision making: implications for theory, practice, and public policy. Psychol. Sci. Pub. Interest 7, 1–44. doi: 10.1111/j.1529-1006.2006.00026.x
Rosi, A., van Vugt, F. T., Lecce, S., Ceccato, I., Vallarino, M., Rapisarda, F., et al. (2021). Risk perception in a real-world situation (COVID-19): how it changes from 18 to 87 years old. Front. Psychol. 12:646558. doi: 10.3389/fpsyg.2021.646558
Rui, J. R., Yang, K., and Chen, J. (2021). Information sources, risk perception, and efficacy appraisal’s prediction of engagement in protective behaviors against COVID-19 in China: repeated cross-sectional survey. JMIR Hum. Fact. 8, 1–23. doi: 10.2196/23232
Shachat, J., Walker, M. J., and Wei, L. (2021). How the onset of the COVID-19 pandemic impacted pro-social behaviour and individual preferences: experimental evidence from China. J. Econ. Behav. Organ. 190, 480–494. doi: 10.1016/j.jebo.2021.08.001
Shilo, G., and Mor, Z. (2020). COVID-19 and the changes in the sexual behavior of men who have sex with men: results of an online survey. J. Sex. Med. 17, 1827–1834. doi: 10.1016/j.jsxm.2020.07.085
Sinclair, A. H., Hakimi, S., Stanley, M. L., Adcock, R. A., and Samanez-Larkin, G. R. (2021). Pairing facts with imagined consequences improves pandemic-related risk perception. Proc. Natl. Acad. Sci. U.S.A. 118:e2100970118. doi: 10.1073/pnas.2100970118
Soane, E., Dewberry, C., and Narendran, S. (2010). The role of perceived costs and perceived benefits in the relationship between personality and risk-related choices. J. Risk Res. 13, 303–318. doi: 10.1080/13669870902987024
Starks, T. J., Jones, S. S., Sauermilch, D., Benedict, M., Adebayo, T., Cain, D., et al. (2020). Evaluating the impact of COVID-19: a cohort comparison study of drug use and risky sexual behavior among sexual minority men in the U.S.A. Drug Alcohol Depend. 216:108260. doi: 10.1016/j.drugalcdep.2020.108260
Steinberg, L. (2008). A social neuroscience perspective on adolescent risk-taking. Dev. Rev. 28, 78–106. doi: 10.1016/j.dr.2007.08.002
Sween, M., Ceschi, A., Tommasi, F., Sartori, R., and Weller, J. (2017). Who is a distracted driver? Associations between mobile phone use while driving, domain-specific risk taking, and personality. Risk Anal. 37, 2119–2131. doi: 10.1111/risa.12773
Szrek, H., Chao, L.-W., Ramlagan, S., and Peltzer, K. (2012). Predicting (un)healthy behavior: a comparison of risk-taking propensity measures. Judgm. Decis. Mak. 7, 716–727.
VandenBos, G. R. (ed.) (2007). APA Dictionary of Psychology. (Washington, DC: American Psychological Association)
Wise, T., Zbozinek, T. D., Michelini, G., Hagan, C. C., and Mobbs, D. (2020). Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States: COVID-19 risk perception and behavior. R. Soc. Open Sci. 7:200742. doi: 10.1098/rsos.200742
Wright, A. J., Whitwell, S. C. L., Takeichi, C., Hankins, M., and Marteau, T. M. (2009). The impact of numeracy on reactions to different graphic risk presentations formats: an experimental analogue study. Br. J. Health Psychol. 14, 107–125. doi: 10.1348/135910708X304432
Zhang, D. C., Highhouse, S., and Nye, C. D. (2019). Development and validation of the general risk propensity scale (GRiPS). J. Behav. Decis. Mak. 32, 152–167. doi: 10.1002/bdm.2102
Keywords: risk perception, decision making, risk taking, personality, behavioral activation and inhibition, COVID-19
Citation: Buelow MT, Kowalsky JM and Brunell AB (2022) Stability of Risk Perception Across Pandemic and Non-pandemic Situations Among Young Adults: Evaluating the Impact of Individual Differences. Front. Psychol. 13:840284. doi: 10.3389/fpsyg.2022.840284
Received: 21 December 2021; Accepted: 01 February 2022;
Published: 24 February 2022.
Edited by:
Melissa Cyders, Indiana University, Purdue University Indianapolis, United StatesReviewed by:
Loreta Cannito, University of Studies G. d’Annunzio Chieti and Pescara, ItalyDaniel Saul Levine, University of Texas at Arlington, United States
Jianbiao Li, Shandong University, China
Copyright © 2022 Buelow, Kowalsky and Brunell. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melissa T. Buelow, YnVlbG93LjExQG9zdS5lZHU=
 Melissa T. Buelow
Melissa T. Buelow Jennifer M. Kowalsky1
Jennifer M. Kowalsky1 Amy B. Brunell
Amy B. Brunell