- 1College of Education, Charles Darwin University, Darwin, NT, Australia
- 2Northern Institute, College of Indigenous Futures, Arts and Society, Charles Darwin University, Darwin, NT, Australia
- 3We Al-li Pty Ltd, Goolmangar, NSW, Australia
- 4Green River Aboriginal Corporation, Nauiyu Nambiyu, Daly River, NT, Australia
The COVID-19 pandemic represents the most significant global challenge in a generation. Based on extant data from previous pandemics, demographic, occupational, and psychological factors have been linked to distress and for some vulnerable members of society. COVID-19 has added to the layers of grief and distress of existing trauma. Evidence-based frameworks exist to guide our individual and collective response to reduce the trauma associated with the experience of a pandemic. Pandemic and post-pandemic measures to ameliorate impacts require a multi-disciplined approach, central to which is community connectedness, resilience, and access to support. We advocate for the acceptance and broader application of Dadirri, a healing practice held by the Ngan'gikurunggurr and Ngen'giwumirri Aboriginal people of the Daly River region in the Northern Territory, Australia. This modality engages therapeutic phases that are comparable with other practiced trauma therapies. The demonstrated therapeutic outcomes from Dadirri can be attained through an individualistic or in a relational engagement context. This practice is accessible to all ages, is non-specific to gender and is suitable for people constrained in their mobility or limited by resources, pertinent in pandemic affected settings.
Introduction
The effects of a global pandemic can be profound on individuals and communities. Previous epidemics have induced widespread fear, loneliness, and psychological sequelae; COVID-19 has induced similar effects (Alradhawi et al., 2020). Empirical studies have shown that people who tested positive for COVID-19 had experienced poorer mental health outcomes. Individuals with a COVID-19 diagnosis have been found to have major psychological distress, anxiety, depression, and other mental health problems compared to people without infection (Guo et al., 2020; Hao et al., 2020; Huang and Zhao, 2020; Rogers, 2020; Hossain et al., 2020b). Psychological risk factors have been identified that predict for poorer mental health outcomes during the pandemic, these include psychological inflexibility (Li et al., 2020; Sultana et al., 2020), limited social support (Wang et al., 2020b), lack of cognitive control over emotions (Chirico et al., 2020), worry (Rogers, 2020; Hossain et al., 2020b), ineffective or maladaptive use of emotion regulation and coping strategies (Patel et al., 2018; Ehrlich et al., 2020; Pappa et al., 2020). Consequently, the lockdowns imposed throughout the pandemic, albeit crucial to reduce COVID-19 infection rates, have apparently exacerbated existing mental health issues. Social interaction is broadly linked with psychological health, social opportunities, and employment; thus, restricting these measures is evidenced to be profoundly distressing to those experiencing strict isolation.
Since the pandemic, research has explored the insulating factors that have supported the mental health of individuals impacted by the pandemic. Studies on psychological resilience, found a negative relationship between resilience and mental health problems such as depression, anxiety, and somatization (Goyal et al., 2020; Huang and Zhao, 2020; Walton et al., 2020) during the pandemic. Empirical studies demonstrate that greater social support, increased levels of mindfulness, cognitive control over emotions, and greater psychological flexibility, predicts the relationship between illness perceptions, resilience, and mental health problems (Chirico et al., 2020; Kavoor, 2020; Li et al., 2020; Mamun and Griffiths, 2020). This suggests that people who accessed more social support, and who were able to flexibly adapt their coping strategies in the event of distress, showed the most positive mental health outcomes during the pandemic (Hossain et al., 2020a). Additionally, research found social cohesion, measured in terms of sense of belonging, to be associated with mental wellbeing during lockdowns (Mamun and Ullah, 2020; Hossain et al., 2020a; Wang et al., 2020a). On this premise, we describe a culturally appropriate praxis that enables greater access by distressed peoples to increase their sense of belonging and connectedness during a pandemic (Atkinson et al., 2010; Morris, 2019).
What Is Dadirri?
Dadirri is a healing framework of the Ngan'gikurunggurr and Ngen'giwumirri Aboriginal people of the Daly River region in the Northern Territory, Australia. Dadirri involves listening to the inner self (feelings, thoughts, reactions) and taking responsibility for internal responses (Ungunmerr-Baumann, 2002). It is the “self” that yearns for connection with all others and its environment, and that strives for spiritual reconnection with the cosmos (Atkinson, 2001; Delauney, 2013). Despite slight variations in meaning, it seems many (if not all) Aboriginal languages have words for listening, wanting to listen, needing to listen. In Australia there are more than 250 Indigenous languages including 800 dialects. Each language is specific to a particular place and people. For example, Bundjalung people have a similar word which is ninganah meaning “shush” with an emphasis on listening; in Wiradjuri language, the equivalent is Winhangadhurinya, a word describing meditation, deep listening, knowing, and reflecting.
The practice of Dadirri aims to lessen the effects of trauma and provide a pathway of empowerment and resilience for individuals and community. The diverse manifestations of trauma in this remote Aboriginal community necessitated an urgent and Indigenous-led response (Atkinson, 2002; Morris, 2019). Some commonalities experienced by the community align with the psychological distress observed during national emergencies, mostly stemming from uncertainty and fear, but also from the grief of separation, loss, and shame—a pain that is deep and unresolved. Similarly, where COVID-19 has revealed and exacerbated uncertainties and fears, Dadirri as a practice of listening and being seen during painful lockdowns and ongoing unresolved situations, can partially transcend separation by the sharing supported by online communities.
Principles of Dadirri
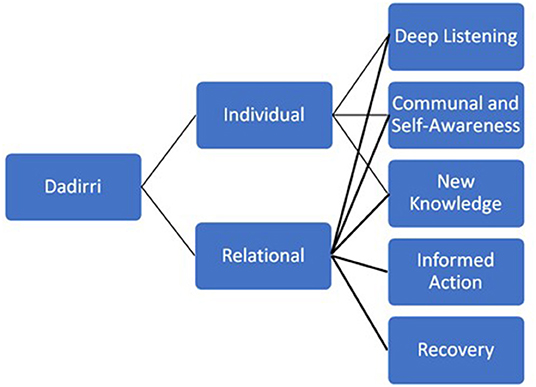
At its core, Dadirri enables a cyclical process of deep, heart-based listening, which witnesses, and empathizes via an individualistic or relational pathway (Figure 1). The great strength of Dadirri in this context is two-fold. Firstly, the cyclical, deep listening and reflection promoted through dialogue; Dadirri encourages relationships built on trust and respect, providing an opportunity to create the co-directional sharing of knowledge (Atkinson, 2002; West et al., 2012); that effectively attends to oppression and marginalization. The principle of reciprocity and connection are fundamental tenets to Dadirri and will shape the way stories and information are shared. Collectively, Dadirri is informed by the concept of community—all people matter, all people belong (Atkinson, 2001; Ungunmerr-Baumann, 2002; Morris, 2019). Secondly, it places recognition on community care and practice, valuing the contribution people make in their activities of relating, defining, and narrating their life experiences. There is a need to honor the integrity and fidelity of community in both its dynamic diversity and its interconnected unity (Atkinson, 2002).
Healing Through Dadirri
The pandemic and the measures to mitigate it, have resulted in widespread restrictions placed on all aspects of people's everyday life. Attending to the pressures of society (e.g., social commitments, employment) is a daily concern for many and restricting people from leaving their home, for example, has caused great anguish and despair. In Dadirri, you are grounded in the present, time stands still. As Ngan'gikurunggurr Elders assert, “we are the river people—we cannot hurry the river, we need to move with the current and understand its ways.” During lockdown, people could no longer fill their life with “busyness” they were forced to stop, to be present, a scenario rarely experienced by many. Indeed, people yearn for this “busyness” as it distracts us from the silence, and the thoughts which can consume us while being grounded in the “present” (Morris, 2019).
Comparison With Eastern and Western Approaches
Widely regarded in contemporary terms as “mindfulness”, a practice of deep awareness in the present moment and what is going on within and around oneself (Hanh, 1976) can be characterized by openness, curiosity, and acceptance (Bishop et al., 2004). There are multiple therapeutic modalities for trauma that incorporate techniques analogous to mindfulness as a critical first phase, these include Empowerment and Resilience Therapy, Acceptance and Commitment Therapy and Mindfulness-Based Cognitive Therapy. Chodron (2001) explained that there are four aspects that are fostered when people meditate: commitment, awareness, willingness to experience emotional distress, and attention to the present moment. Similarly, Dadirri integrates deep-listening and self-awareness, these phases are regarded as key for true connection and the dissolution of self-object dualism. Transformative learning theorists describe a state from which transformation is born. According to McWhinney and Markos (2003), that state is attained when one withdraws from the world to an inner place from which new insights and frames of reference emerge. This was observed as the “aha” moment in participants enduring the final stages of Dadirri practice: new knowledge, informed action, and recovery. Participants described a sense of overwhelming peace (Morris, 2019).
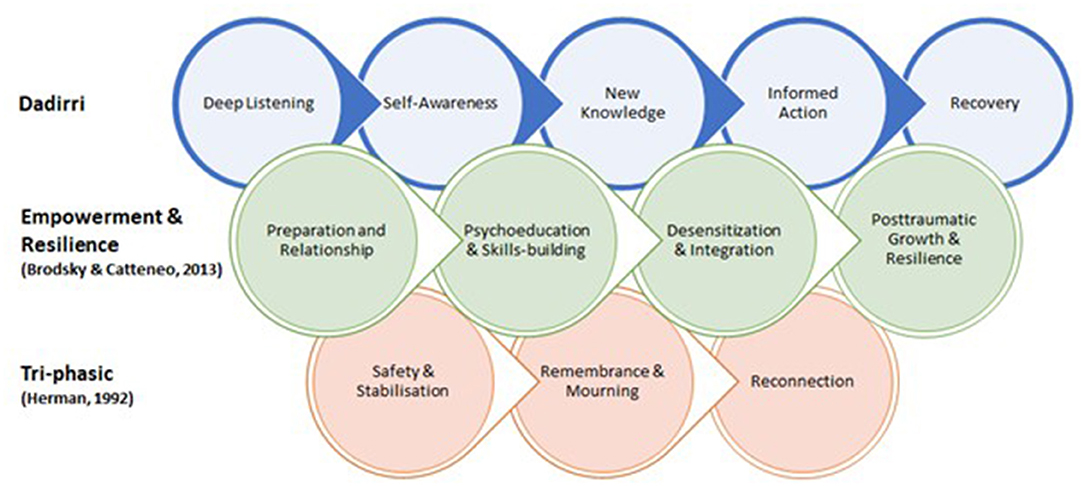
Dadirri as a practice has been used to endure painful emotions in ways that are not typical of Western approaches but broadly aligns with eastern Buddhist philosophies. While there are important similarities between Dadirri, Buddhist thought and some schools of Western psychology, there is value in recognizing their common objectives. The varied perspectives have parallel goals where they seek to foster growth, understanding, and freedom from suffering (Figure 2). Herman (1992) constructs a tri-phasic model that moves toward reconnection, while Brodsky and Cattaneo (2013) present stages of empowerment and resilience that build cumulatively. Dadirri aligns with these Western models of recovery such as in similar preparatory techniques, collective shifts during deep listening and self-awareness that supports the process to build toward re-integration of conscious knowing and doing. Furthermore, these varied perspectives share a fundamental assumption that there is an inherent potential within each person toward continual growth (Kumar, 2002). Practicing these behaviors as interventions in both pleasant and unpleasant circumstances, such as the COVID-19 pandemic and its after-effects, helps people consciously recognize themselves. This recognition of self is part of a greater context, not as good or bad, but as part of a changing universe and within a community.
Dadirri as Healing From Trauma and Colonization
The importance of Dadirri as an Indigenous healing practice was articulated in a recent study on the impact of colonization in Daly River (Morris, 2019). Participants recognized the contemplative process of listening and learning from the stories of others and it allowed for healing to occur and increased their sense of community and connection (Morris, 2019). As illustrated in Figure 1, the therapeutic phases have both individual and relational aspects, and to fully appreciate Dadirri, one needs to move from the individualistic, to a collective perspective. By way of example, one participant stated that “it was this feeling of belonging and community which allows stories to be shared without fear of judgment”. Dadirri permeates every aspect of life, continually renewing the spirit, bringing peace and contemplation. As the recounts of trauma were repeated over time, another participant revealed “your story eventually changes, and the pain of trauma is released and replaced with love and acceptance as the healing process begins”.
Utilizing Dadirri within a local Nauiyu community context provides an opportunity for members to re-engage, trust and value their own cultural practices. Rather than a quick fix or the need to fix and change what arises, Dadirri asks of us to allow each moment, each breath, each story to unfold naturally. Giving us the opportunity to accept what is arising for us, or in us, at each successive moment of experience, without the need to fix, fight or avert what is arising. Empowering people through the learning and application of their traditional healing practices and knowledge is demonstrated to increase their individual and collective health, strength, and wellbeing (Atkinson et al., 2010; Barnabe, 2021).
For non-Indigenous people Dadirri allows engagement in a practice that has been shared across thousands of generations attributing equity to an accessible and beneficial therapy. Emerging research suggests that mainstream perceptions and subsequent policy implementations of Indigenous healing practices reflect the attitudes formed during the decline of Indigenous healing practice throughout colonization (Gone, 2013; Dudgeon et al., 2017). Dadirri offers a treatment option for practitioners in trauma therapy.
Relevance to COVID-19 and Post-Pandemic Futures
The persistent trauma from COVID-19 requires a spectrum of resilience from individual and community-level acts to shift paradigms and policy, to combat the inequities of complex trauma through a foundation for collective healing. Public health challenges necessitate mobilizing resources available within and between contexts. In COVID-19, biopsychosocial challenges such as anxiety, fear and isolation experienced by individuals may be addressed by local and regional organizations through enhancing collaboration and extending social capital. Chen and Bonanno (2020) offer a spectrum of temporal elements of resilience that demonstrate multifactor social capital aspects contributing to resilience and recovery. Dadirri similarly draws on individual and collective community responses that support healing from trauma, such as in this case, COVID-19 effects. Supporting healing from COVID-19 adversity and building resilience by maintaining a sense of equilibrium can be achieved through connectedness to community and/or resilience resources; this is a key protective factor during times of hardship. Access to regular treatment and support during a pandemic is a major challenge but is necessary for limiting long-term consequences for mental health (Moreno et al., 2020; Pfefferbaum and North, 2020). Factors underlying the concept of Western mental health should also be addressed, such as expectations around lifestyle and sets of rigid strategies that prove insufficient in pandemic times. Dadirri is a flexible and accessible technique, demonstrated to be an appropriate and supportive treatment for people who have experienced trauma (Atkinson, 2002; Morris, 2019). Addressing the trauma in the current pandemic cultivates fertile ground for trauma-informed healing and recovery in our communities, beyond the COVID-19 aftermath.
Trauma Aftermaths
The American Psychological Association (2016) defines trauma as events that pose a significant threat (physical, emotional, or psychological) to the safety of the victim or loved ones and are overwhelming and shocking. Current events, such as a pandemic, may aggravate past wounds for individuals who have experienced trauma in other areas of their life, requiring additional support measures. Persistent trauma that is not buffered by early intervention can permanently alter our DNA, promote vulnerability to future stressors (Youssef et al., 2018; Thumfart et al., 2022), and may be transmitted to future generations (Atkinson, 2002; Lavallée et al., 2015; Yehuda et al., 2016). As the challenges arising from the COVID-19 pandemic continue to evolve, so too have the significant and varying psychosocial demands on the global population (Ho et al., 2020; Xiang et al., 2020; Ammar et al., 2020); Psychosocial shifts can occur due to confinement, economic shutdown, financial pressure, and social distancing.
With access to psychosocial services being restricted within the pandemic, alternative frameworks for healing justify consideration. Within a community, an individual can take steps to disrupt negative responses to trauma and community collective action can also be enabled. Successful community-based programs for the treatment of trauma are implemented in diverse contexts throughout the world (Ertl et al., 2011; Konanur et al., 2015; López-Zerón and Parra-Cardona, 2015).
Intersections of Resilience
COVID-19 has impacted the population in an unequal manner. Haase (2020) highlights the inequality and justice challenges arising from the COVID-19 crisis and how exposure and vulnerability to COVID-19 emerges at the intersection between different dimensions of disadvantage and marginalization. The degree to which the pandemic impacts a place and exposes its people to health risk is without doubt related to the socio-spatial inequalities and socio-economic status or lack thereof (Simon, 2020; Haase, 2020) resilience. As was the case in previous pandemics, the trauma associated with COVID-19 has disproportionately impacted vulnerable population groups, particularly those who have experienced past trauma and have pre-existing differences in health status (Gaynor and Wilson, 2020).
Recommendations and Future Directions
Dadirri works by influencing behavioral change through developing deep acceptance and prompting holistic behavior. It is integral to the community healing program in several remote communities in Australia with complex trauma. The healing capacity of Dadirri has been successfully applied in a range of national and international contexts. It is a profoundly important healing practice to the Nauiyu community and whilst it is important to acknowledge the place-based significance of Dadirri, hundreds of people from across the world have traveled to Nauiyu to practice Dadirri over many years. There are an increasing number of evidence-based programs that have used Dadirri “off Country” to establish respectful healing environments to address symptoms of trauma (Bevis et al., 2020; Coombes et al., 2020).
Although studies are still emerging from the COVID-19 pandemic, Dadirri as an ancient application that can be transferred into multimodal contexts may be compared with similar holistic practices studied during the pandemic, such as yoga and mindfulness-based online interventions (Godara et al., 2021; Verma et al., 2021). Dadirri has also been applied to broader organizational and service-level systems of care to build community healing networks through educational settings, primary health care providers and other government and non-government organizations (Bevis et al., 2020; Woodland, 2021). Training in Dadirri offers professionals and service providers a way of engaging and responding to clients who are triggered by authority figures and procedures that trigger trauma. As psychological, medical, and community health practitioners continue to deal with the aftermath of COVID-19 procedures and authority figures, Dadirri may be applied to create safe healing spaces. Developing a posture of awareness and deep listening through Dadirri counters the dismissive and insensitive “expert” and instead creates gentle and co-invitational healing spaces. Dadirri is adaptable in a range of social contexts, with its therapeutic capacity proven in solitary settings, small groups in face-to-face environments and devices with online platforms (Sunderland et al., 2020) which also reduce feelings of isolation for affected patients, their families and members of the public (Xiang et al., 2020).
The importance of Dadirri as part of a broader body of Indigenous healing practices has been recognized as significant by national peak-body mental health organizations including, the Psychotherapy and Counseling Federation of Australia (PACFA1)- the national peak body for counselors and psychotherapists and for professional associations in the counseling and psychotherapy field in Australia. PACFA has recently launched an Indigenous led college within its organization to accredit Indigenous Healing Practices and training standards. The College of Aboriginal and Torres Strait Healing Practices (CATSIHP) has developed training standards which encompass “traditional contemporary, and emerging healing modalities created by and founded in Indigenous wisdom, systems of knowledge and ways of being” (https://www.pacfa.org.au/). The association acknowledges Indigenous healing practices in its constitution and is working to accredit and validate Indigenous healing practices, such as Dadirri, as equal with traditional Western and Eurocentric counterparts. Indeed, such has been the emergence of Indigenous Healing practices in Western health settings, CATSIHP has been approached by large Australian private health insurers to explore the potential of including traditional healing practices in their mainstream insurance packages.
The uncertainty of the COVID-19 pandemic; the confinement, isolation, physical distancing, and other confinement strategies which have resulted in societal breakdown and economic collapse has seen a profound decline in mental health. Trauma is a multisensory experience; therefore, we need multisensory interventions—whole of body interventions which not only involve the individual but also the collective. Dadirri is an adaptable Indigenous healing practice, proven in a range of contexts to offer therapeutic responses to trauma, healing the wounds of separation and restoring our living flow.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Charles Darwin University Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GM, RG, ES, JA, CA, and M-RU-B wrote the manuscript. GM gathered and analyzed the data. All authors have read and approved the final manuscript.
Conflict of Interest
CA was employed by the company We Al-li Pty Ltd. Author Emeritus Professor JA is an advisor for the company We Al-li Pty Ltd without any financial interests in this company.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We extend our sincere gratitude to all the participants of the Nauiyu community, Daly River who have given their time and trust in this study. We also would like to express our gratitude to the College of Indigenous Futures, Arts and Society at Charles Darwin University which supported this research.
Footnotes
1. ^Psychotherapy and Counselling Federation of Australia. Available online at: https://www.pacfa.org.au/ (accessed March 04, 2022).
References
Alradhawi, M., Shubber, N., Sheppard, J., and Ali, Y. (2020). Effects of the COVID-19 pandemic on mental well-being amongst individuals in society- A letter to the editor on “The socio-economic implications of the coronavirus and COVID-19 pandemic: A review”. Int. J. Surg. 78, 147–148. doi: 10.1016/j.ijsu.2020.04.070
American Psychological Association (2016). Revision of Ethical Standard 3.04 of the “Ethical Principles of Psychologists and Code of Conduct” (2002, as amended 2010). Am. Psychol. 71, 900.
Ammar, A., Mueller, P., Trabelsi, K., Chtourou, H., Boukhris, O., Masmoudi, L., et al. (2020). Psychological consequences of COVID-19 home confinement: the ECLB-COVID19 multicenter study. PLoS ONE 15,e0240204. doi: 10.1371/journal.pone.0240204
Atkinson, J.. (2001). Lifting the blankets: the transgenerational effects of trauma in Indigenous Australia (Ph.D.). Queensland University of Technology, Brisbane, QLD, Australia.
Atkinson, J.. (2002). Trauma Trails, Recreating Song Lines: The Transgenerational Effects of Trauma in Indigenous Australia. Melbourne, VIC: Spinifex Press.
Atkinson, J., Nelson, J., and Atkinson, C. (2010). “Trauma transgenerational transfer and effects on community wellbeing,” in Working Together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice, eds N. Purdie, P. Dudgeon, and R. Walker (Canberra, ACT: Australian Institute of Health and Welfare), 135–144.
Barnabe, C.. (2021). Towards attainment of Indigenous health through empowerment: resetting health systems, services and provider approaches. BMJ Global Health 6, e004052. doi: 10.1136/bmjgh-2020-004052
Bevis, M., Atkinson, J., McCarthy, L., and Sweet, M. (2020). Kungas' Trauma Experiences and Effects on Behaviour in Central Australia. Sydney, NSW: ANROWS.
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., et al. (2004). Mindfulness: a proposed operational definition. Clin. Psychol. Sci. Pract. 11, 230–241. doi: 10.1093/clipsy.bph077
Brodsky, A., and Cattaneo, L. (2013). A transconceptual model of empowerment and resilience: divergence, convergence and interactions in kindred community concepts. Am. J. Commun. Psychol. 52, 333–346. doi: 10.1007/s10464-013-9599-x
Chen, S., and Bonanno, G. (2020). Psychological adjustment during the global outbreak of COVID-19: a resilience perspective. Psychol. Trauma Theory Res. Pract. Policy 12, S51–S54. doi: 10.1037/tra0000685
Chirico, F., Nucera, G., and Magnavita, N. (2020). COVID-19: protecting healthcare workers is a priority Infection control and hospital epidemiology. Infect. Control Hosp. Epidemiol. 41, 1117. doi: 10.1017/ice.2020.148
Chodron, P.. (2001). The Places That Scare You: A Guide to Fearlessness in Difficult Times. Boston, MA: Shambhala Publications.
Coombes, J., Hunter, K., Mackean, T., and Ivers, R. (2020). The journey of aftercare for Australia's First Nations families whose child had sustained a burn injury: a qualitative study. BMC Health Serv. Res. 20, 536. doi: 10.1186/s12913-020-05404-1
Delauney, T.. (2013). Fractured culture: educare as a healing approach to indigenous trauma. Int. J. Sci. Soc. 4, 53–62. doi: 10.18848/1836-6236/CGP/v04i01/59279
Dudgeon, P., Bray, A., D'Costa, B., and Walker, R. (2017). Decolonising psychology: validating social and emotional wellbeing. Austral. Psychol. 52, 316–325. doi: 10.1111/ap.12294
Ehrlich, H., McKenney, M., and Elkbuli, A. (2020). Protecting our healthcare workers during the COVID-19 pandemic. Am. J. Emerg. Med. 38, 1527–1528. doi: 10.1016/j.ajem.2020.04.024
Ertl, V., Pfeiffer, A., Schauer, E., Elbert, T., and Neuner, F. (2011). Community-implemented trauma therapy for former child soldiers in Northern Uganda: a randomized controlled trial. JAMA 306, 503–512. doi: 10.1001/jama.2011.1060
Gaynor, T. S., and Wilson, M. E. (2020). Social vulnerability and equity: the disproportionate impact of COVID-19. Public Admin. Rev. 80, 832–838. doi: 10.1111/puar.13264
Godara, M., Silveira, S., Matthäus, H., Heim, C., Voelkle, M. al., et al. (2021). Investigating differential effects of socio-emotional and mindfulness-based online interventions on mental health, resilience and social capacities during the COVID-19 pandemic: the study protocol. PLOS ONE 16, e0256323. doi: 10.1371/journal.pone.0256323
Gone, J. P.. (2013). Redressing First Nations historical trauma: theorizing mechanisms for indigenous culture as mental health treatment. Transcult. Psychiatry 50, 683–706. doi: 10.1177/1363461513487669
Goyal, K., Chauhan, P., Chhikara, K., Gupta, P., and Singh, M. P. (2020). Fear of COVID 2019: First suicidal case in India! Asian J. Psychiatry 49, 101989. doi: 10.1016/j.ajp.2020.101989
Guo, Q., Zheng, Y., Shi, J., Wang, J., Guanjun, L., Li, C., et al. (2020). Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav. Immun. 88, 17–27. doi: 10.1016/j.bbi.2020.05.038
Haase, A.. (2020). Covid-19 as a social crisis and justice challenge for cities. Front. Sociol. 5, 583638. doi: 10.3389/fsoc.2020.583638
Hao, F., Tan, W., Jiang, L., Zhang, L., Zhao, X., Zou, Y., et al. (2020). Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 87, 100–106. doi: 10.1016/j.bbi.2020.04.069
Ho, C. S., Chee, C. Y., and Ho, R. C. (2020). Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann. Acad. Med. Singap. 49, 155–160. doi: 10.47102/annals-acadmedsg.202043
Hossain, M., Tasnim, S., Sultana, A., Faizah, F., Mazumder, H., Zou, L., et al. (2020a). Epidemiology of mental health problems in COVID-19: a review. F1000Res. 9, 636. doi: 10.12688/f1000research.24457.1
Hossain, M., Tasnim, S., Sultana, A., McKyer, E. L. J., and Ma, P. (2020b). COVID-19 and suicide of an army soldier in India: perspectives on psychosocial epidemiology of suicidal behavior. SocarXiv. 1–6. doi: 10.31235/osf.io/k2jgf
Huang, Y., and Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 288, 112954. doi: 10.1016/j.psychres.2020.112954
Kavoor, A. R.. (2020). COVID-19 in people with mental illness: challenges and vulnerabilities. Asian J. Psychiatry 51, 102051. doi: 10.1016/j.ajp.2020.102051
Konanur, S., Muller, R. T., Cinamon, J. S., Thornback, K., and Zorzella, K. P. M. (2015). Effectiveness of trauma-focused cognitive behavioral therapy in a community-based program. Child Abuse Neglect 50, 159–170. doi: 10.1016/j.chiabu.2015.07.013
Kumar, S. M.. (2002). An introduction to Buddhism for the cognitive-behavioral therapist. Cogn. Behav. Pract. 9, 40–43. doi: 10.1016/S1077-7229(02)80038-4
Lavallée, L., Menzies, P., Harper, V., and Centre for Addiction Mental Health Mental, H. (2015). Journey to Healing: Aboriginal People With Addiction and Mental Health Issues: What Health, Social Service and Justice Workers Need to Know. Toronto, ON: Centre for Addiction and Mental Health
Li, G., Miao, J., Wang, H., Xu, S., Sun, W., Fan, Y., et al. (2020). Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: a cross-sectional study. J. Neurol. Neurosurg. Psychiatry 91, 895–897. doi: 10.1136/jnnp-2020-323134
López-Zerón, G., and Parra-Cardona, J. R. (2015). Elements of change across community-based trauma interventions. J. Syst. Therap. 34, 60–76. doi: 10.1521/jsyt.2015.34.3.60
Mamun, M. A., and Griffiths, M. D. (2020). First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: possible suicide prevention strategies. Asian J. Psychiatry 51, 102073. doi: 10.1016/j.ajp.2020.102073
Mamun, M. A., and Ullah, I. (2020). COVID-19 suicides in Pakistan, dying off not COVID-19 fear but poverty? - The forthcoming economic challenges for a developing country. Brain Behav. Immun. 87, 163–166. doi: 10.1016/j.bbi.2020.05.028
McWhinney, W., and Markos, L. (2003). Transformative education:across the threshold. J. Transform. Educ. 1, 16–37. doi: 10.1177/1541344603252098
Moreno, C., Wykes, T., Galderisi, S., Nordentoft, M., Crossley, N., Jones, N., et al. (2020). How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry 7, 813–824. doi: 10.1016/S2215-0366(20)30307-2
Morris, G.. (2019). Edge of sacred - exploring the life stories of the Nauiyu community. An investigation into trauma and the traditional healing practices of a remote Aboriginal community (Ph.D.). Charles Darwin University, Casuarina, NT, Australia.
Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V. G., Papoutsi, E., and Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 88, 901–907. doi: 10.1016/j.bbi.2020.05.026
Patel, R. S., Bachu, R., Adikey, A., Malik, M., and Shah, M. (2018). Factors related to physician burnout and its consequences: a review. Behav. Sci. 8, 98. doi: 10.3390/bs8110098
Pfefferbaum, B., and North, C. S. (2020). Mental health and the Covid-19 pandemic. N. Engl. J. Med. 383, 510–512. doi: 10.1056/NEJMp2008017
Rogers, J.. (2020). Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 7, 611–627. doi: 10.1016/S2215-0366(20)30203-0
Simon, D. A.. (2020). Cities Are at Centre of Coronavirus Pandemic - Understanding This Can Help Build a Sustainable, Equal Future. The Conversation. Available online at: https://theconversation.com/cities-are-at-centre-of-coronavirus-pandemic-understanding-this-can-help-build-a-sustainable-equal-future-136440 (accessed November 14, 2020).
Sultana, A., Sharma, R., Hossain, M., Bhattacharya, S., and Purohit, N. (2020). Burnout among healthcare providers during COVID-19 pandemic: challenges and evidence-based interventions. SocarXiv. doi: 10.31235/osf.io/4hxga
Sunderland, N., Woods, G., and Dorsett, P. (2020). Making the invisible visible: applying digital storytelling for immersive, transformative and anti-colonial learning. Brit. J. Soc. Work 50, 483–505. doi: 10.1093/bjsw/bcz161
Thumfart, K. M., Jawaid, A., Bright, K., Flachsmann, M., and Mansuy, I. M. (2022). Epigenetics of childhood trauma: long term sequelae and potential for treatment. Neurosci. Biobehav. Rev. 132, 1049–1066. doi: 10.1016/j.neubiorev.2021.10.042
Ungunmerr-Baumann, M. R.. (2002). Dadirri: Inner Deep Listening and Quiet Still Awareness. Port Macquarie, NSW: Emmaus.
Verma, S., Donovan, J., Tunuguntla, H. S., Tunuguntla, R., Gupta, B. V., Nandi, A., et al. (2021). Yoga of immortals intervention reduces symptoms of depression, insomnia and anxiety. Front. Psychiatry 12, 648029. doi: 10.3389/fpsyt.2021.648029
Walton, M., Murray, E., and Christian, M. D. (2020). Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J. 9, 241–247. doi: 10.1177/2048872620922795
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., et al. (2020a). Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 17, 1729. doi: 10.3390/ijerph17051729
Wang, J., Zhou, M., and Liu, F. (2020b). Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J. Hosp. Infect. 105, 100–101. doi: 10.1016/j.jhin.2020.03.002
West, R., Stewart, L., Foster, K., and Usher, K. (2012). Through a critical lens: indigenist research and the Dadirri method. Qual. Health Res. 22, 1582–1590. doi: 10.1177/1049732312457596
Woodland, S.. (2021). “Creating audio drama with incarcerated women,” in The Routledge Companion to Applied Performance: Volume One - Mainland Europe, North and Latin America, Southern Africa, and Australia and New Zealand, 1st Edn., eds T. Prentki and A. Breed (New York, NY: Routledge). 150–171.
Xiang, Y.-T., Yang, Y., Li, W., Zhang, L., Zhang, Q., Cheung, T., et al. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7, 228–229. doi: 10.1016/S2215-0366(20)30046-8
Yehuda, R., Daskalakis, N. P., Bierer, L. M., Bader, H. N., Klengel, T., Holsboer, F., et al. (2016). Holocaust exposure induced intergenerational effects on FKBP5 methylation. Biol. Psychiatry 80, 372–380. doi: 10.1016/j.biopsych.2015.08.005
Keywords: trauma, Dadirri, COVID-19, indigenous practice, traditional healing
Citation: Morris G, Groom R, Schuberg E, Atkinson J, Atkinson C and Ungunmerr-Baumann M-R (2022) Mitigating Contemporary Trauma Impacts Using Ancient Applications. Front. Psychol. 13:645397. doi: 10.3389/fpsyg.2022.645397
Received: 23 December 2020; Accepted: 21 June 2022;
Published: 02 August 2022.
Edited by:
Cyrille Kossigan Kokou-Kpolou, Laval University, CanadaReviewed by:
Belinda Jayne Liddell, University of New South Wales, AustraliaJucier Gonçalves Júnior, University of São Paulo, Brazil
Copyright © 2022 Morris, Groom, Schuberg, Atkinson, Atkinson and Ungunmerr-Baumann. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gavin Morris, Z2F2aW4ubW9ycmlzQGNkdS5lZHUuYXU=
 Gavin Morris
Gavin Morris Rachel Groom
Rachel Groom Emma Schuberg2
Emma Schuberg2