- 1Ningbo Key Laboratory of Sleep Medicine, Ningbo Kangning Hospital, Affiliated Tongyi Hospital of Medical College of Ningbo University, Ningbo, China
- 2Ningbo Municipal Center for Disease Control and Prevention, Ningbo, China
Objective: A quantitative synthesis of online psychotherapies' effectiveness in managing COVID-19 related distress is lacking. This study aimed to estimate online psychological interventions' effectiveness and associated factors on COVID-19 related psychological distress.
Methods: Multi-databases including PubMed, EBSCO, ProQuest, and Cochrane were searched repeatedly till the end of June 2022. Hand-picking was also utilized for relevant papers. Depression, anxiety, stress, and quality of sleep were evaluated as outcomes. The risk of bias was evaluated using the Cochrane tool. Data analyses were conducted through Review Manager (version 5.4.1).
Results: A total of 13 studies involving 1,897 participants were included for meta-analysis. Results showed that online psychotherapy significantly reduced the levels of depression [standard mean difference, SMD = −0.45, 95% CI (−0.69, −0.20)], anxiety [SMD = −0.67, 95% CI (−0.99, −0.36)], and stress [SMD = −0.73, 95% CI (−1.11, −0.34)], but not quality of sleep [SMD = −0.53, 95% CI (−1.23, 0.17)]. In addition, guided therapies were more effective than self-help ones on reducing levels of anxiety (χ2 = 5.58, p = 0.02, and I2 = 82.1%), and ≤ 2 weeks' daily interventions were more effective on treating depression than 2-month weekly interventions (χ2 = 7.97, p = 0.005, I2 = 87.5%).
Conclusion: Online psychological interventions effectively reduced COVID-19 related depression, anxiety, and stress levels, and the effectiveness was influenced by settings like guidance and duration and frequency.
Systematic review registration: https://inplasy.com/inplasy-2022-7-0081/, identifier: INPLASY202270081.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has affected every aspect of people's lives worldwide. There have been 553 million confirmed COVID-19 cases and more than 6.3 million deaths globally (World Health Organization, 2022). It raises a constellation of issues which challenges people's mental health, including social isolation, worries of infection of the self and significant others, financial difficulties, and uncertainties (Brooks et al., 2020). More psychosomatic problems or exacerbations of psychiatric symptoms were found in people with COVID-19 and preexisting mental illness, healthcare workers, and the general population (Vindegaard and Benros, 2020). Thus, effective mental health services are essential and urgent under such a circumstance. In the post-pandemic era, online psychological interventions have been boosted and broadly accepted, as it is more accessible and efficient than traditional onsite or face-to-face psychotherapy (Wind et al., 2020).
The COVID-19 related distress refers to a broad range of mental experiences and symptoms related with the COVID-19 pandemic, with or without clinical diagnoses. Among these COVID-19 related distress and psychiatric symptoms, depression, anxiety, sleeping disorder, and stress-related symptoms have been mostly reported (Brooks et al., 2020; Salari et al., 2020; Vindegaard and Benros, 2020). Due to the urgent and extensive need for online psychological interventions during the pandemic, online psychological interventions have been delivered in various forms and settings. Online interventions, for example, single-session mindfulness, 1-week psychoeducational support, 4-session weekly CBT, and 8-week daily mindfulness have been reported to be effective in treating COVID-19 related distress (Farris et al., 2021; Mahoney et al., 2021; Mirhosseini et al., 2021; Nourian et al., 2021). However, many of these studies were not conducted in randomized controlled trials (e.g., without control groups). The effectiveness and associated factors of online psychological interventions on COVID-19 related distress have yet to be clarified. Therefore, this meta-analysis aimed to estimate the effectiveness of online psychological intervention of COVID-19 related distress in randomized controlled trials and explore associated influential factors.
Materials and methods
This study was conducted according to the preferred reporting items for systematic review and meta-analyses (PRISMA, Moher et al., 2009).
Search strategy
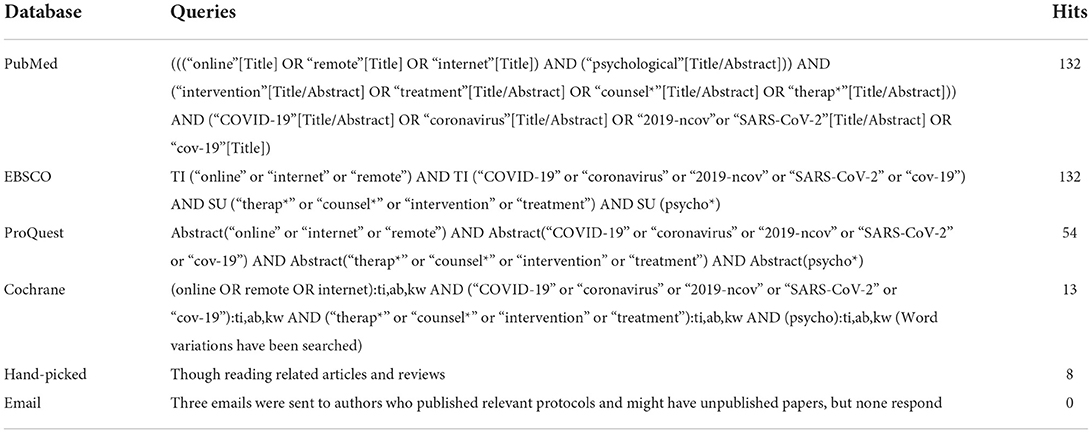
This review followed the established guidelines of evidence-based clinical review to ensure clarity and transparency. The topic was relevant and of common clinical interest. A systematic literature search was initially conducted in April 2022 and re-ran to identify newly published studies on 24 June 2022. Multi-databases were searched as suggested (Siwek et al., 2002), including PubMed, EBSCO, ProQuest, and Cochrane (Table 1). Hand-picked processes were also applied to find the references in relevant articles and reviews. In addition, emails were sent to authors who registered potentially relevant protocols to detect completed but not yet published papers.
Study selection
After the removal of studies of non-adult participants, not written in English, and duplicates, titles and abstracts were screened. Two authors (DC and YZ) independently screened the lists of titles/abstracts identified through database searching according to inclusion and exclusion criteria. Any discrepancies were resolved by discussions with a third member of the team (DZ). Then, the potentially relevant records were retrieved in full text for eligibility checking.
This study used relatively broad inclusion criteria as it had been only more than 2 years since the COVID-19 pandemic. We included studies that:
• used validated quantitative measures to examine the effects of the interventions on depression, anxiety, perceived psychological stress or distress, and quality of sleep;
• administered interventions to people aged 18 years old or above;
• delivered psychological interventions online through digital devices;
• used a randomized controlled design;
• administered to people who perceived distress related to COVID-19.
The exclusion criteria included:
• The intervention was not well-supported by empirical evidence;
• The intervention was not aimed at treating COVID-19 related psychological conditions;
• Participants in studies were patients with preexisting mental or severe physical illnesses;
• The article did not provide sufficient data to calculate the effect sizes.
Data extraction
Data extraction was conducted by the first author (DC) and checked by another author (DZ). Disagreements were resolved by discussion. Extracted data included: first author, year and country of publication, population, characteristics of populations (e.g., age and percentage of female), characteristics of intervention (type, guidance, delivery mode, sessions and durations), sample sizes of treated and control groups, and outcome measures (e.g., depression, anxiety, stress, and quality of sleep). Two authors were contacted and requested for extra data with regard to the data extraction. However, neither of them responded.
Risk of bias assessment
The risk of bias assessment was conducted by GX and GB independently based on Cochrane's suggestions (Higgins and Altman, 2008), and discrepancies were resolved through discussion. Criteria provided in Review Manager (version 5.4.1) were applied: random sequence generation and allocation concealment, blinding of participants and outcomes assessment, incomplete outcome data, selective reporting, and other biases. Each criterion was assessed as “low risk”, “unclear”, or “high risk”. The overall quality was considered as “high” if all criteria were assessed as low risk of bias, as “low” if one or more criteria were assessed as high risk of bias, and as “moderate” if they did not fit the first two situations.
Statistical analyses
Data were analyzed with Cochrane RevMan (version 5.4.1). The effect of online psychological intervention compared to inactive control was assessed using the standardized mean difference (SMD) at post-treatment as the outcome. For each comparison between a treated and a control group, effect sizes were calculated per outcome variable (i.e., depression, anxiety, stress, and quality of sleep). If more than one instrument were used to measure the same outcome, the more valid and commonly used one was adopted. One study used the total score rather than the subscales of DASS to measure general psychological distress (Brog et al., 2022), and thus, this total score was considered as a measure of stress. All outcomes were continuous variables in this meta-analysis, and SMD with a 95% confidence interval (CI) were used to present the pooled results. Heterogeneity was assessed with χ2 and I2 (Higgins and Thompson, 2002). The random-effects model was used as variations across studies are inevitable in real settings. Forest plots were used to assess variations in effects across studies. Sensitivity analyses were conducted to test the stability of the results by assessing whether study quality was related to outcome by comparing the low-risk studies in risk of bias assessment. Funnel plots were used to assess the publication bias. The level of significance in this study was set to p < 0.05.
Results
Study selection
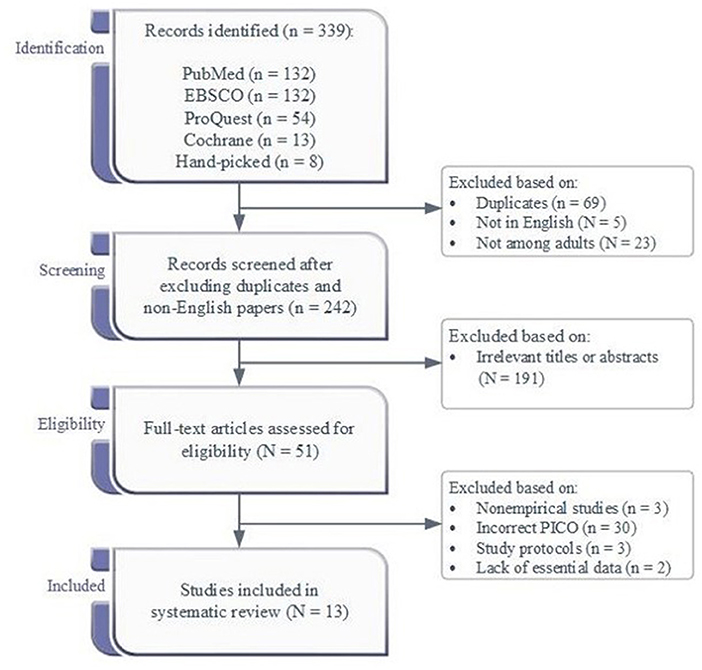
Figure 1 presented the flow diagram of the study selection process. The database searches and hand-picking produced 339 records. After excluding the duplicates and studies not written in English or conducted in adults, 242 records were screened, and 191 were excluded due to irrelevant titles or abstracts. Of the 51 full-text articles checked for eligibility, 15 fit the criteria. However, two of them were lack of essential data. Emails were sent to the authors to request relevant data, but the authors did not respond. In addition, no unpublished data were available after sending emails to three authors who had published potentially relevant protocols. Thus, 13 records were included.
Description of included studies
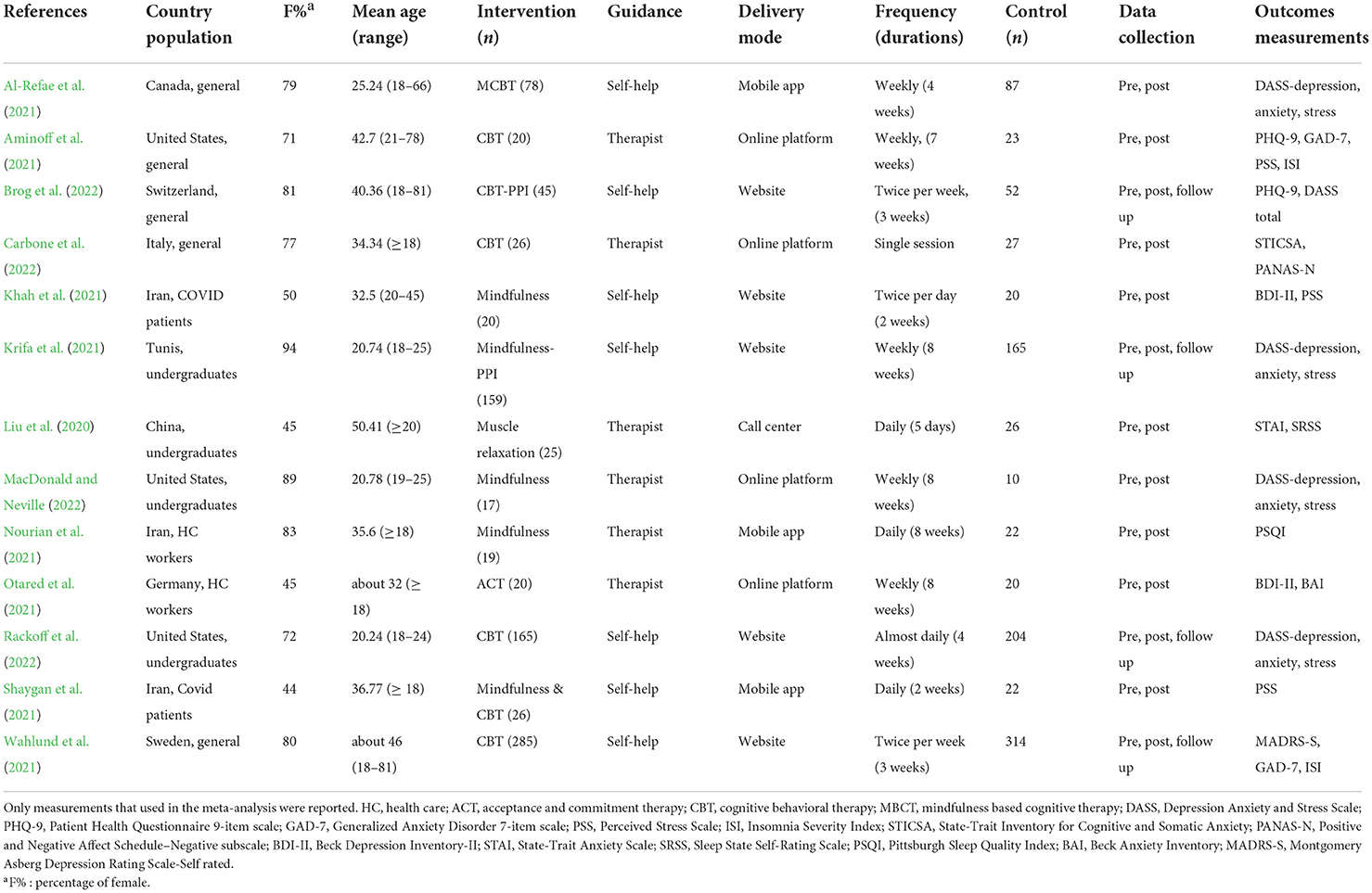
The included studies were conducted in many different countries, and Table 2 summarized their characteristics.
Population characteristics
The total population comprised 1,897 participants, of which 905 were in the treated groups and 992 were in the control groups. All participants were adults, with a mean age ranging from 20.24 to 50.41 years. The majority of the sample was female in nine of the included studies. The total sample size ranged from 27 (MacDonald and Neville, 2022) to 599 (Wahlund et al., 2021). All included studies were conducted in populations without previously identified mental or severe physical illnesses. Three studies were conducted among COVID-19 patients with mild symptoms (Liu et al., 2020; Khah et al., 2021; Shaygan et al., 2021), two were in health care workers (Nourian et al., 2021; Otared et al., 2021), three were in undergraduates (Krifa et al., 2021; MacDonald and Neville, 2022; Rackoff et al., 2022), and others were in the general population (Al-Refae et al., 2021; Aminoff et al., 2021; Brog et al., 2022; Carbone et al., 2022).
Intervention
The online interventions reviewed in this study aimed to reduce COVID-19 related psychological distress and/or promote participants' mental health. CBT (n = 5) and mindfulness (n = 4) were mostly adopted interventions, and two studies used integrated interventions of CBT and mindfulness, and the other two used ACT (Otared et al., 2021) and progressive muscle relaxation (Liu et al., 2020), respectively. The interventions were either therapist-guided (n = 6) or self-helped (n = 7) in which participants were provided with access to online materials. The interventions were delivered through online platforms like Zoom (n = 4), websites (n = 5), other mobile applications (n = 3), and hospital's call system (n = 1). Frequencies in these studies were daily (n = 5), twice per week (n = 2), weekly (n = 5), or a single session (n = 1), and the duration of interventions ranged from a single session to 8 weeks.
Comparison
Each of the 13 studies used an inactive control. Studies in COVID-19 patients provided routine care to control groups (Liu et al., 2020; Khah et al., 2021; Shaygan et al., 2021). Treated groups were compared with waitlist control groups (n = 10) or routine care groups (n = 3). One study provided music files and materials for caring to the control group, whereas the treated group was given guided mindfulness training (Nourian et al., 2021). Other studies used waitlist groups as inactive control.
Outcomes
All studies measured the outcomes pre- and post-intervention. Four studies reported follow-up data but were not analyzed in this study. The numbers of studies which measured depression, anxiety, stress, and quality of sleep were 9, 9, 9, and 4, respectively.
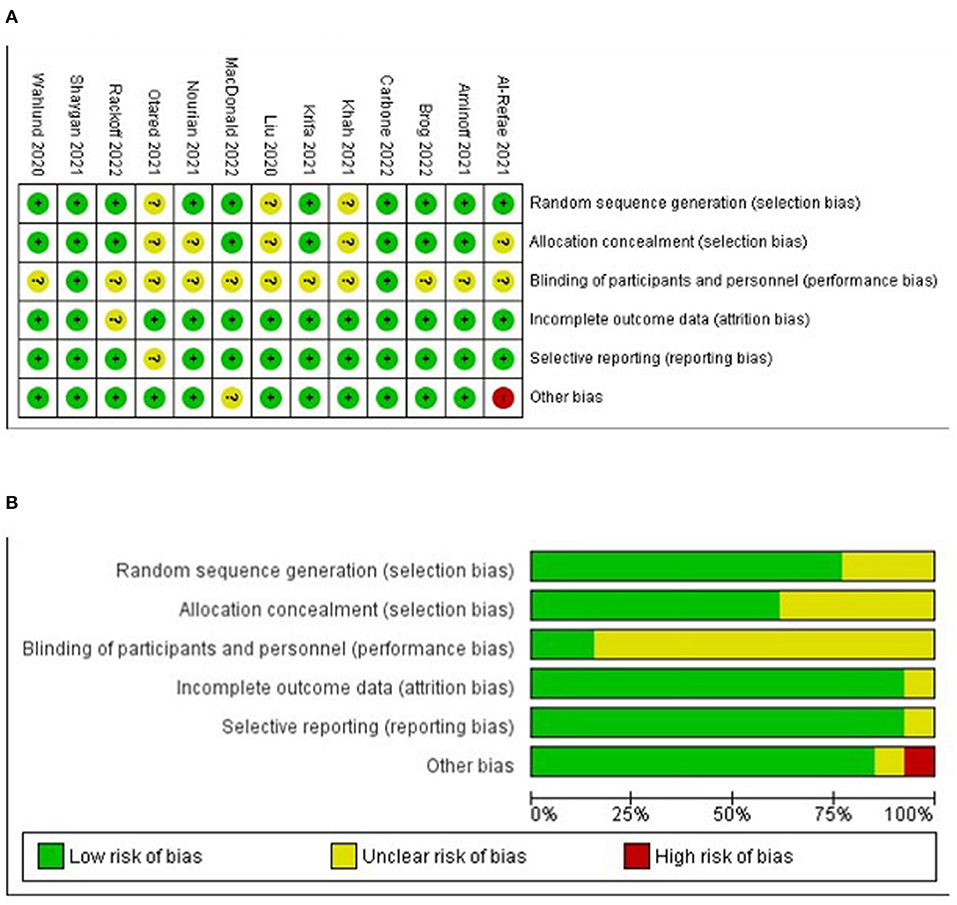
Risk of bias assessment
In studies that used self-reporting, the criterion of blinding outcomes assessment was not applicable. Therefore, six criteria rather than seven were utilized. Many studies used waitlist control, and the criterion of blinding intervention to participants was not met. The risk of bias assessment showed that most studies were of high (n = 2) or moderate (n = 11) quality. One study was assessed as low quality due to conflicts of interest: Two of the authors were the co-founders of the mobile application used in their study, and the application was going to be commercialized (Al-Refae et al., 2021). Figures 2A,B present the risk of bias summary and graph, respectively.
Meta-analysis
Overall effects
The between-group effects at post-intervention for depression, anxiety, stress, and sleep are presented in Table 3, and Forest plots are shown in Supplementary Figure S1.
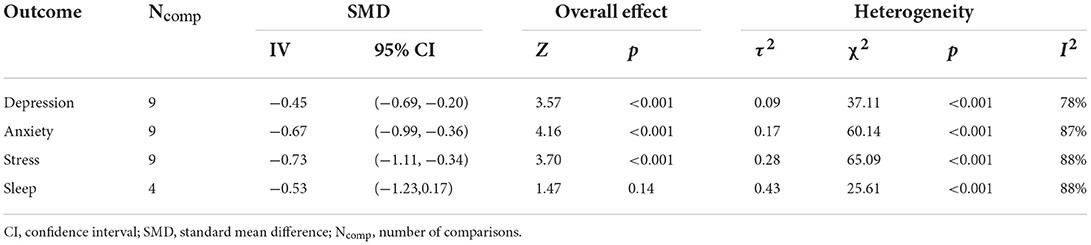
Table 3. Comparative effectiveness between treated and control group in terms of depression, anxiety, stress, and quality of sleep.
A total of nine studies reported levels of pre- and post-treatment depression. A significant effect of online psychotherapy on depression was observed: SMD = −0.45 and 95% CI = (−0.69, −0.20), and the heterogeneity was also significant: τ2 = 0.09, χ2 = 37.11, p < 0.001, and I2 = 78%.
Based on the nine comparisons, a significant effect of online psychological interventions on anxiety was observed: SMD = −0.67, 95% CI = (−0.99, −0.36). A significant heterogeneity was also observed: τ2 = 0.17, χ2 = 60.14, p < 0.001, and I2 = 87%.
The significant overall effect size for nine comparisons on perceived stress was observed: SMD = −0.73 and 95% CI = (−1.11, −0.34), with a significant level of heterogeneity (τ2 = 0.28, χ2 = 65.09, p < 0.001, and I2 = 88%).
Based on the four studies, the effect of online psychological interventions on quality of sleep was not significant, SMD = −0.53 and 95% CI = (−1.23, 0.17), with a significant heterogeneity (τ2 = 0.43, χ2 = 25.61, p < 0.001, and I2 = 88%).
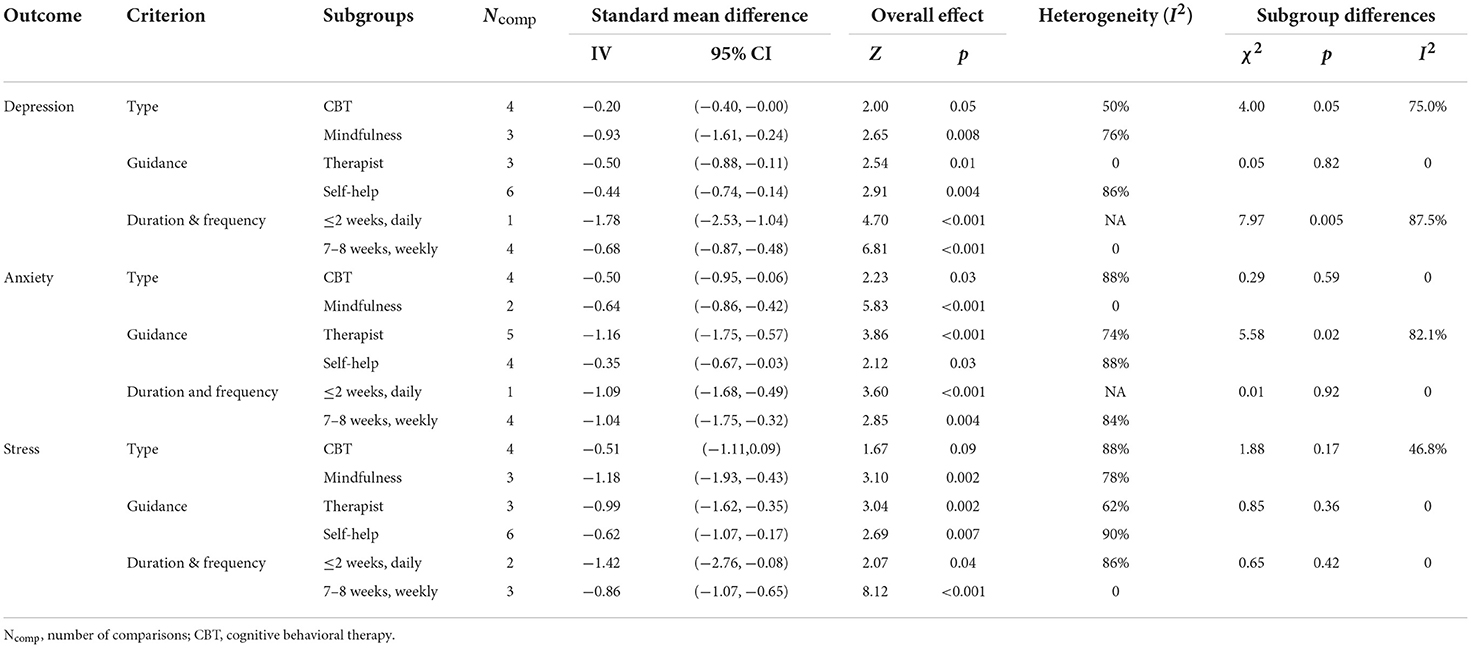
Subgroup analyses
Exploratory subgroup analyses were summarized in Table 4. Criterions included types of intervention (CBT or mindfulness), guidance (therapist-guided or self-help), and duration and frequency ( ≤2 weeks daily vs. 2-month weekly). Subgroup analyses were conducted to explore the effect differences of online psychological intervention on depression, anxiety, and stress, but not the quality of sleep due to limited studies (n = 4).
For depression, significant larger effect was found in shorter and intense sessions (i.e., daily and ≤ 2 weeks): χ2 = 7.97, p = 0.005, and I2 = 87.5%. Effect differences on depression among other subgroups were insignificant (Table 4). For anxiety, larger effect was found in therapist-guided interventions: χ2 = 5.58, p = 0.02, and I2 = 82.1%. None of the effect differences on stress between subgroups was significant (Table 4).
Publication bias and sensitivity analysis
Funnel plots for each outcome were presented in Supplementary Figure S2. No significant publication bias was identified. Leave-one-out sensitivity analysis was conducted, and no single study had a substantial influence on the overall effect sizes.
Discussion
Main findings
This meta-analysis included 13 studies and confirmed the overall effects of online psychological interventions in reducing COVID-19 related depression, anxiety, and stress, and explored associated factors that might influence the effectiveness, such as types of intervention (CBT or mindfulness), guidance (therapist involved or self-help), and duration and frequency ( ≤2 weeks daily or 2-month weekly).
This present study found that CBT and mindfulness were the most commonly used online interventions among the 13 included studies. The effectiveness of online mindfulness has also been well-supported in treating general mental conditions and COVID-19 related distress (Spijkerman et al., 2016; Wright et al., 2019; Yeun and Kim, 2022). Online guided CBT was found as effective as face-to-face CBT in treating mental and somatic conditions in a meta-analysis that reviewed 20 studies (Carlbring et al., 2018), though it is not specific to the pandemic. No published studies have compared the effectiveness between online CBT and mindfulness on COVID-19 related distress, and this present study found non-significant differences in effectiveness between them in treating COVID-related depression, anxiety, and stress.
The findings of this study suggested that both guided and online self-help interventions were effective in managing the pandemic related depression, anxiety, and stress, and that therapist-guided interventions were more effective than self-help ones in treating COVID-19 related anxiety, but not depression or stress. In partially consistent with the findings of this present study, a recent study found that though both therapist-guided and self-help online 6-week CBT treatment were effective in reducing COVID-19 related depression and anxiety levels, therapist-guided was more effective than the self-help one (Al-Alawi et al., 2021). Similarly, the superiority of guided online treatment (i.e., mindfulness-based interventions) in managing depression, anxiety, stress, and wellbeing in general and clinical populations was also reported in two meta-analyses (Spijkerman et al., 2016; Wright et al., 2019; Zhang et al., 2020). However, A four-session self-help CBT has been found to have similar effects to the clinician-guided CBT in reducing levels of depression and anxiety in young adults at post-treatment and 3- and 12-month follow-ups (Dear et al., 2018). It is possible that factors like patients' adherence and clinicians' estimation of treatment response influenced the effectiveness of online interventions (Salomonsson et al., 2020), but both of them compromised in self-help treatment, and so did the effectiveness.
The findings of this study suggested that intense and short-term interventions (i.e., ≤2 weeks' daily sessions) were more effective in reducing depression than weekly and longer ones (i.e., 7–8 weeks). Short-term daily sessions might be more effective and efficient than 2-month weekly ones in treating COVID-19 related depression, though the long-term effects of these two types of sessions were not clear. Though limited published studies investigated the impact of frequency and duration on the effectiveness of COVID-19 studies, studies have found that the number of total sessions moderated the effectiveness of online mindfulness-based interventions in treating stress (Spijkerman et al., 2016). However, as most studies reviewed in Spijkerman et al.'s meta-analysis were conducted weekly, and thus the potential moderator role of frequency as unable to explore.
Limitations and implications
In the post-pandemic era, enormous needs for psychological interventions are yet to be fulfilled. Online psychological intervention can benefit a broad range of people with lower costs and higher accessibility without worrying about exposure to the infection (Wind et al., 2020). However, few studies reviewed online psychological interventions of COVID-19 related distress, and the effective settings are yet to be clarified. This study is of the few (if not none) to confirm the effectiveness of online psychological interventions in reducing COVID-19 related distress (e.g., depression, anxiety, sleeping disorder, and stress) and identify associated factors. These findings can help practitioners and therapists set and deliver more effective and efficient online psychological interventions to people experiencing COVID-19 related distress.
There were some limitations of this study. Included studies used waitlist control or routine care control for COVID-19 patients, which means the effectiveness of online psychological interventions was based on comparisons with those who did not receive psychological support or interventions. It was unclear whether online psychological interventions were more effective than psychoeducation or psychological support groups. Considerable variability in online psychological settings existed, and the limited sample size constrained us from further exploring the interactions of these different settings.
Future studies need to use more active control (e.g., online psychoeducation or online psychological support) to investigate the effectiveness of online psychotherapy. Appropriate settings can promote effectiveness. As a relatively new mode of delivering psychological interventions, empirical studies on identifying more effective and efficient settings are needed. Future studies need to investigate the stability of online psychological interventions, and a more structured guideline can benefit people globally in the post-pandemic era.
Clinicians or psychotherapists can involve in the online psychological interventions or some of the sessions. Self-help interventions are better than no interventions at all, and the effectiveness can be enhanced with the involvement or guidance of therapists. Moreover, in treating with COVID-19 related psychological distress, people are more likely to benefit from daily and short-term sessions (i.e., ≤2 weeks) rather than weekly and longer treatment (i.e., 7–8 weeks). Therefore, clinicians and psychotherapists are encouraged to use online psychological interventions as an effective and accessible way to deliver service in the post-pandemic era.
Conclusion
This study estimated the effectiveness and explored the influential factors of online psychological interventions on COVID-19 related distress. The findings confirmed the effectiveness of online psychological interventions in relieving the COVID-19 related depression, anxiety, and perceived stress, but not in improving sleeping quality. Settings like with or without guidance and frequency and duration also influenced the effectiveness of the online psychological interventions. Online psychological interventions with appropriate settings are required to benefit more people in but not limited to the COVID-19 post-pandemic era.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
DC, YZ, and DZ designed the searching queries, searched the databases, screened the records, and checked the eligibility of the records. DC and DZ contributed to the data extraction, analyses, and draft writing. GX and GB contributed to the supervision of the process, assessing the bias, and reviewing and editing the draft. All authors contributed to the conceptualization of the study. All authors agree to be accountable for the content of the work and approved the submitted version.
Funding
The study was supported by the Ningbo Municipal Emergency Science and Technology Major Project (No. 2022Z034) and the Medical and Health Brand Discipline in Ningbo (No. PPXK2018-08).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.1045400/full#supplementary-material
References
Al-Alawi, M., McCall, R. K., Sultan, A., Al Balushi, N., Al-Mahrouqi, T., Al Ghailani, A., et al. (2021). Efficacy of a six-week-long therapist-guided online therapy versus self-help internet-based therapy for COVID-19-induced anxiety and depression: open-label, pragmatic, randomized controlled trial. JMIR Mental Health 8, e26683. doi: 10.2196/26683
Al-Refae, M., Al-Refae, A., Munroe, M., Sardella, N. A., and Ferrari, M. (2021). A self-compassion and mindfulness-based cognitive mobile intervention (Serene) for depression, anxiety, and stress: promoting adaptive emotional regulation and wisdom. Front. Psychol. 12, 648087. doi: 10.3389/fpsyg.2021.648087
Aminoff, V., Sellén, M., Sörliden, E., Ludvigsson, M., Berg, M., and Andersson, G. (2021). Internet-based cognitive behavioral therapy for psychological distress associated with the COVID-19 pandemic: a pilot randomized controlled trial. Front. Psychol. 12, 684540. doi: 10.3389/fpsyg.2021.684540
Brog, N. A., Hegy, J. K., Berger, T., and Znoj, H. (2022). Effects of an internet-based self-help intervention for psychological distress due to COVID-19: results of a randomized controlled trial. Int. Intervent. 27, 100492. doi: 10.1016/j.invent.2021.100492
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., et al. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395, 912–920. doi: 10.1016/S0140-6736(20)30460-8
Carbone, G. A., Zarfati, A., Nicoli, M. S., Paulis, A., Tourjansky, G., Valenti, G., et al. (2022). Online psychological counselling during lockdown reduces anxiety symptoms and negative affect: Insights from Italian framework. Clin. Psychol. Psychother. 29, 367–372. doi: 10.1002/cpp.2608
Carlbring, P., Andersson, G., Cuijpers, P., Riper, H., and Hedman-Lagerlöf, E. (2018). Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cogn. Behav. Therapy 47, 1–18. doi: 10.1080/16506073.2017.1401115
Dear, B. F., Fogliati, V. J., Fogliati, R., Johnson, B., Boyle, O., Karin, E., et al. (2018). Treating anxiety and depression in young adults: a randomised controlled trial comparing clinician-guided versus self-guided Internet-delivered cognitive behavioural therapy. Aust. N. Z. J. Psychiatry 52, 668–679. doi: 10.1177/0004867417738055
Farris, S. R., Grazzi, L., Holley, M., Dorsett, A., Xing, K., Pierce, C. R., et al. (2021). Online mindfulness may target psychological distress and mental health during COVID-19. Global Adv. Health Med. 9, 1–15. doi: 10.1177/21649561211002461
Higgins, J. P., and Altman, G. A., (eds.). (2008). “Assessing risk of bias in included studies,” in Cochrane Handbook for Systematic Reviews of Interventions. p. 187–241.
Higgins, J. P., and Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558. doi: 10.1002/sim.1186
Khah, A. S., Msc, S. M., Kateb, M. Y., and Niyazi, S. (2021). The effect of online mindfulness program on physical pain, stress and depression in the COVID-19 patients: a randomized control trail. J. Pain Manag. 14, 57–63.
Krifa, I., Hallez, Q., van Zyl, L. E., Braham, A., Sahli, J., and Ben Nasr, S. (2021). Effectiveness of an online positive psychology intervention among Tunisian healthcare students on mental health and study engagement during the COVID-19 pandemic. Appl. Psychol. Health Wellbeing. doi: 10.1111/aphw.12332. [Epub ahead of print].
Liu, K., Chen, Y., Wu, D., Lin, R., Wang, Z., and Pan, L. (2020). Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Comp. Ther. Clin. Pract. 39, 101132. doi: 10.1016/j.ctcp.2020.101132
MacDonald, H. Z., and Neville, T. (2022). Promoting college students' mindfulness, mental health, and self-compassion in the time of COVID-19: feasibility and efficacy of an online, interactive mindfulness-based stress reduction randomized trial. J. Coll. Student Psychotherapy. doi: 10.1080/87568225.2022.2028329. [Epub ahead of print].
Mahoney, A., Li, I., Haskelberg, H., Millard, M., and Newby, J. M. (2021). The uptake and effectiveness of online cognitive behaviour therapy for symptoms of anxiety and depression during COVID-19. J. Affect. Disord. 292, 197–203. doi: 10.1016/j.jad.2021.05.116
Mirhosseini, S., Vaghee, S., Nabavi, F., and Vashani, H. (2021). Effect of online psychoeducational support on caring burden in family caregivers of COVID-19 patients: a parallel randomized controlled trial. Fam. Med. Prim. Care Rev. 23, 323–329. doi: 10.5114/fmpcr.2021.108198
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339, b2535. doi: 10.1136/bmj.b2535
Nourian, M., Nikfarid, L., Khavari, A. M., Barati, M., and Allahgholipour, A. R. (2021). The impact of an online mindfulness-based stress reduction program on sleep quality of nurses working in COVID-19 care units: a clinical trial. Holist. Nurs. Pract. 35, 257–263. doi: 10.1097/HNP.0000000000000466
Otared, N., Moharrampour, N. G., Vojoudi, B., and Najafabadi, A. J. (2021). A group-based online acceptance and commitment therapy treatment for depression, anxiety symptoms and quality of life in healthcare workers during COVID-19 pandemic: a randomized controlled trial. Int. J. Psychol. Psychol. Therapy 21, 399–411.
Rackoff, G. N., Ellen Fitzsimmons-Craft, E., Barr Taylor, C., Daniel, E., Denise, W. E., and Michelle Newman, G. (2022). A randomized controlled trial of internet-based self-help for stress during the COVID-19 pandemic. J. Adolesc. Health. 71, 157–163. doi: 10.1016/j.jadohealth.2022.01.227
Salari, N., Hosseinian-Far, A., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, A., Mohammmadi, M., et al. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 16, 57. doi: 10.1186/s12992-020-00589-w
Salomonsson, S., Santoft, F., Lindsäter, E., Ejeby, K., Ingvar, M., Öst, L. G., et al. (2020). Predictors of outcome in guided self-help cognitive behavioural therapy for common mental disorders in primary care. Cogn. Behav. Ther. 49, 455–474. doi: 10.1080/16506073.2019.1669701
Shaygan, M., Yazdani, Z., and Valibeygi, A. (2021). The effect of online multimedia psychoeducational interventions on the resilience and perceived stress of hospitalized patients with COVID-19: a pilot cluster randomized parallel-controlled trial. BMC Psychiatry 21, 93. doi: 10.1186/s12888-021-03085-6
Siwek, J., Gourlay, M. L., Slawson, D. C., and Shaughnessy, A. F. (2002). How to write an evidence-based clinical review article. Am. Fam. Phys. 65, 251–258.
Spijkerman, M. P. J., Pots, W. T. M., and Bohlmeijer, E. T. (2016). Effectiveness of online mindfulness-based interventions in improving mental health: a review and meta-analysis of randomised controlled trials. Clin. Psychol. Rev. 45:102–114. doi: 10.1016/j.cpr.2016.03.009
Vindegaard, N., and Benros, M. E. (2020). COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 89:531–542. doi: 10.1016/j.bbi.2020.05.048
Wahlund, T., Mataix-Cols, D., Lauri, K. O., de Schipper, E., Ljótsson, B., and Aspvall, K. (2021). Brief online cognitive behavioural intervention for dysfunctional worry related to the COVID-19 pandemic: a randomised controlled trial. Psychother. Psychosom. 90, 191–199. doi: 10.1159/000512843
Wind, T. R., Rijkeboer, M., Andersson, G., and Riper, H. (2020). The COVID-19 pandemic: the ‘black swan' for mental health care and a turning point for e-health. Int. Intervent. 20, 100317. doi: 10.1016/j.invent.2020.100317
World Health Organization (2022). COVID-19 Weekly Epidemiological Update. Available form: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19-$-$13-july-2022 (accessed July 18, 2022).
Wright, J. H., Owen, J. J., Richards, D., Eells, T. D., Richardson, T., Brown, G. K., et al. (2019). Computer-assisted cognitive-behavior therapy for depression: A systematic review and meta-analysis. J. Clin. Psychiatry 80, 18r12188. doi: 10.4088/JCP.18r12188
Yeun, Y. R., and Kim, S. D. (2022). Psychological effects of online-based mindfulness programs during the COVID-19 pandemic: A systematic review of randomized controlled trials. Int. J. Environ. Res. Public Health 19, 1624. doi: 10.3390/ijerph19031624
Keywords: psychotherapy, COVID-19, online, effectiveness, setting, telepsychology, telepsychiatry
Citation: Chi D, Zhang Y, Zhou D, Xu G and Bian G (2022) The effectiveness and associated factors of online psychotherapy on COVID-19 related distress: A systematic review and meta-analysis. Front. Psychol. 13:1045400. doi: 10.3389/fpsyg.2022.1045400
Received: 15 September 2022; Accepted: 26 October 2022;
Published: 09 November 2022.
Edited by:
Pengfei Xu, Beijing Normal University, ChinaCopyright © 2022 Chi, Zhang, Zhou, Xu and Bian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dongsheng Zhou, d3l6aG91ZHNAc2luYS5jb20=; Guozhang Xu, eHVnekBuYmNkYy5vcmcuY24=; Guolin Bian, MjU4NDA4NkBxcS5jb20=
 Danni Chi
Danni Chi Yuanyuan Zhang
Yuanyuan Zhang Dongsheng Zhou
Dongsheng Zhou Guozhang Xu2*
Guozhang Xu2*