- 1Faculty of Biomedical Sciences, Università della Svizzera Italiana, Lugano, Switzerland
- 2Neuropsychological and Speech Therapy Unit, Neurocenter of Southern Switzerland, Ente Ospedaliero Cantonale (EOC), Lugano, Switzerland
The purpose of this study was to investigate emotion recognition and processing in patients with mild cognitive impairment (MCI) in order to update the state of current literature on this important but undervalued topic. We identified 15 papers published between 2012 and 2022 that meet the inclusion criteria. Paper search, selection, and extraction followed the PRISMA guidelines. We used a narrative synthesis approach in order to report a summary of the main findings taken from all papers. The results collected are still ambiguous: some studies did not find any differences between MCI and healthy controls (HC) groups in emotion recognition and processing, and other results reported emotion-specific deficits in emotion recognition regarding MCI patients (both regarding negative and neutral emotions). It is essential to underline that these findings could not be generalized to the whole MCI population due to the heterogeneous use of measures and composition of the sample. This does not allow us to make a comprehensive comparison between the results. Our suggestion for future research is to align the results using the same type of tests and emotion recognition assessment.
Introduction
Emotion recognition and processing are considered the first abilities to establish social interactions (that go through three processes: social perception, social understanding, and social decision-making) (Morese and Palermo, 2020, 2022). Social perception is a fundamental skill of social cognition because the analysis of facial expressions, gestures, posture, language, and voice allows us to recognize others as “living people” (Arioli et al., 2018; Morellini et al., 2022).
In particular, emotion recognition plays an important role in interpersonal communication (Ferretti and Papaleo, 2019). Thanks to the facial expressions of others, it is possible to make inferences about their emotional states. The understanding of emotional cues might lead to a relevant empathic response in emotional situations (Adolphs, 2002; Balconi and Pozzoli, 2009). This ability permits one to anticipate situations, have an adequate response, avoid conflict, and self-regulate emotions (Brüne and Brüne-Cohrs, 2006). Deficits in this domain could contribute to several problems in daily life, such as difficulties in interpersonal relationships (Palermo et al., 2020); they can also predict psychiatric or neurodegenerative disorders (Ferretti and Papaleo, 2019). As an example, weaker emotion recognition might influence social behavior (Mueser et al., 1996) that could become inappropriate. Also, this type of impairment is correlated with higher levels of depression (Chiu et al., 2006), interpersonal difficulties, social isolation, and psychobehavioral disturbances (Shimokawa et al., 2001) that could lead to an increased risk of institutionalization (Brodaty, 1996).
Till present, we do not know how old people’s pathologies affect emotional processing and social cognition in general (Cárdenas et al., 2021).
However, the vulnerability in social cognition mechanisms is age-related, as reported in the literature (Williams et al., 2009); in particular, evidence shows that younger adults have better performance than older adults in recognizing basic emotions (McCade et al., 2011). In addition, emotion recognition can be more impaired in older adults with disorders that involve social cognition’s brain structure, such as MCI or other dementias (Amlerova et al., 2022).
Mild cognitive impairment is considered a prodromal phase of dementia, a transitional stage between healthy aging and dementia (Anderson, 2019; Breton et al., 2019). The risk of developing dementia in the following years is higher in this specific phase, but their daily functioning is still mainly preserved (Petersen, 1996; Smith et al., 1996). The first definition of MCI belongs to Petersen et al. (1997), which describes a moment of transition where patients, as reported before, do not meet the dementia’s criteria.
In this regard, MCI is also described by the DSM 5 (American Psychiatric Association, 2013) through a diagnostic category named “mild cognitive disorder (mild-NCD),” which fits with Petersen et al. (1997) and Albert et al. (2011) criteria. These diagnostic criteria highlight a mild cognitive decline in one or more domains (for example, language and memory); it also reports that the decline does not interfere with daily routine and cannot be explicated by mental disorders or delirium (for example, schizophrenia or depression) (American Psychiatric Association, 2013).
Petersen (2016) delineated an important distinction between two different types of MCI, namely, amnestic MCI (aMCI) and non-amnestic MCI (naMCI). The first one considers deficits only in the memory domain. In contrast, the naMCI is related to single or multiple cognitive domain impairments, such as visuospatial abilities, language, memory, and executive functions.
Currently, there are several studies on the topic, but the last review performed refers to 10 years ago (McCade et al., 2011), and their results were ambiguous. Based on that, we decided to present a new systematic review describing the literature of last decade.
The aim of this study was to investigate emotion recognition and processing in MCI patients to update the state of current literature on this crucial but underestimated topic.
We took into account only results about this social cognition domain because our purpose was to understand the strengths and weaknesses of this argument in the current literature. To achieve this goal, considering that the selected articles were enough/adequate to conduct a systematic review, we found it necessary to focus on a single domain.
The goal of this study review
The aim of this study is led by the need to understand and update the state of the current literature regarding emotion recognition and processing in MCI. To date, the last review on this topic was made by McCade et al. (2011), and their results are ambiguous; that is the reason behind the choice to collect and analyze the previous findings on this field.
Based on the past research on social cognition in neurodegenerative disorders (Morese and Palermo, 2020; Palermo et al., 2020; Morellini et al., 2022), we could expect that emotion recognition and processing might be impaired in the MCI population.
Method
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA, Moher et al., 2009). The method is currently available in the Open Science Framework (OSF).1
Eligibility criteria
The aim of this systematic review was to gather studies that analyze the functionality of emotion recognition and processing in patients with mild cognitive impairments (MCI).
The inclusion criteria were the following:
• Studies with a population with a diagnosis of mild cognitive impairment (MCI), evaluated by standardized diagnostic criteria of Petersen (1996, 2004), Petersen and Negash (2008), Petersen (2016) or DMS 5—DSM IV—DSM IV-TR criteria (American Psychiatric Association, 1994, 2000, 2013) or Winblad et al. (2004) or Albert (PD-MCI—Albert et al., 2011) or every cognitive impairment—without dementia—diagnosed with a validated cognitive test; for example, Dementia Rating Scale (DSR) (Mattis, 1988) or PD-MCI (Litvan et al., 2011).
• Study sample must be over 60 years old, either male or female.
• All types of MCI: amnesic MCI (aMCI), non-amnesic MCI (naMCI), Parkinson MCI (PD-MCI), Alzheimer MCI (AD-MCI), and Vascular MCI (VaMCI).
• Studies that evaluated the domains of social cognition, “emotion recognition and processing.”
• Studies must include at least one clinical cognitive measurement for the social cognition domain analyzed (emotion recognition and processing).
The exclusion criteria were the following:
• Articles not in English were excluded.
• Meta-analysis, systematic reviews, single case studies or other studies with a small sample (i.e., studies with less than 10 participants) or only qualitative measurements, comments, books, conference papers, letters, theses, and all other studies not peer-reviewed were excluded.
Information sources
Search strategy
The search for this study was conducted across PubMed and Medline databases. For the MCI search strategy, we used the terms “MCI” OR “mild cognitive impairment.” The keywords were combined with the domain of social cognition “emotion recognition and processing,” to produce the results.
Study selection
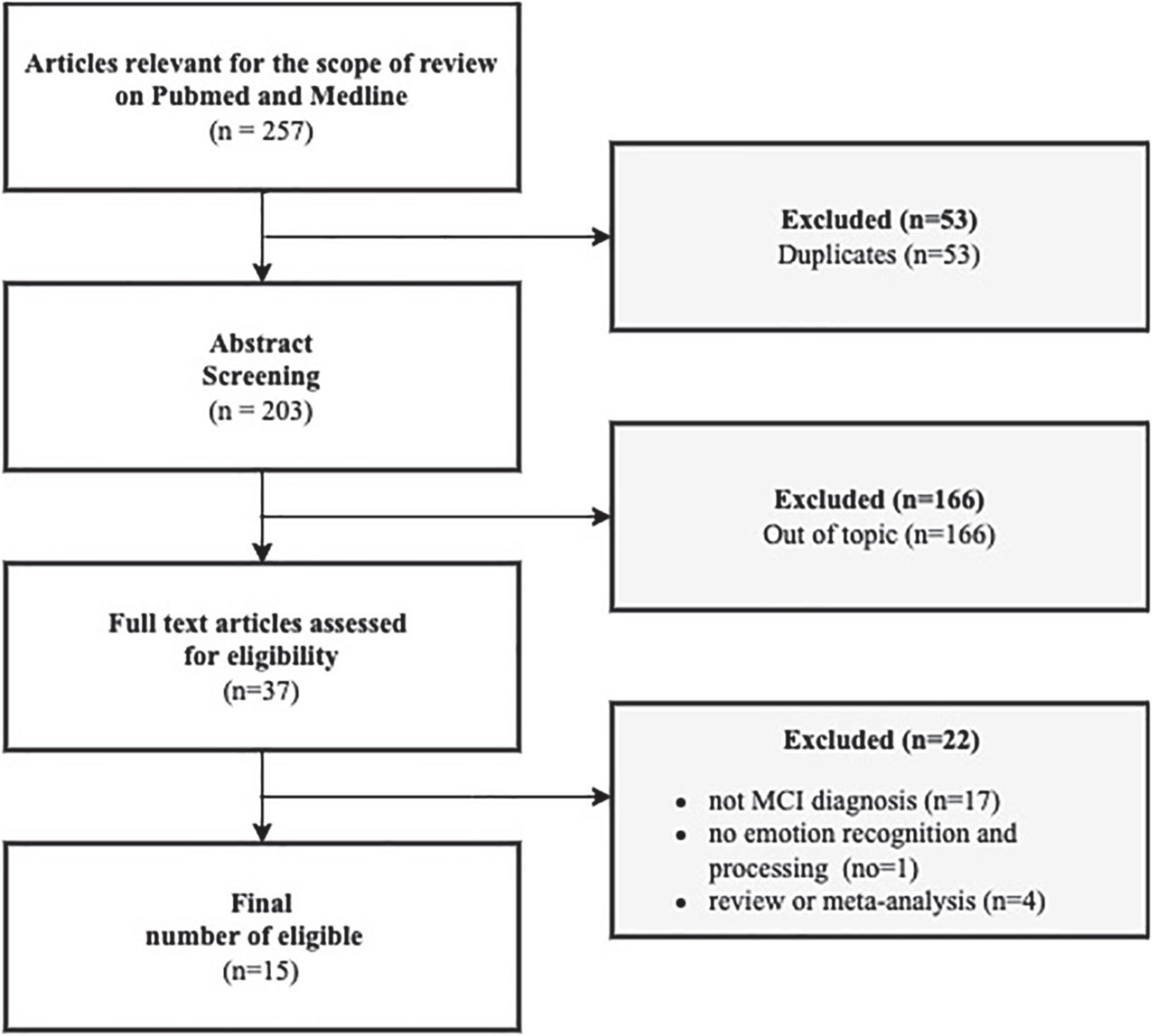
We only considered studies that are limited to humans, with a limited range of periods from January 2012 to May 2022. We considered the studies in the past 10 years because of the number of papers and because they are appropriate for our time and resources. Moreover, meta-analysis, other systematic reviews, case studies, qualitative studies, or every study with a very small sample without quantitative measurements were excluded from this review. Initially, 256 papers were included in the selection and then 53 duplicates were excluded. Reading the title and abstract of 203 articles, we excluded 166 other articles from the topic. Only 37 papers were considered eligible for the scope of this review. Those 37 papers were further analyzed by reading the complete text to discover if they met the inclusion criteria. At this point, the other 22 articles were excluded because 17 did not have an MCI diagnosis (in line with inclusion criteria), one did not investigate the domain of social cognition elected for this review, and the last 4 were reviews or meta-analyses (as described previously in the inclusion criteria).
In the end, 15 articles were included in our review.
Despite the age range (2012–2022), we found only eligible articles until 2020 (Figure 1).
Results
Overall, 15 studies were included in our review. Those studies examine the domain of social cognition and emotion recognition and processing. We examined articles from 2012 to 2022, but we found eligible articles only until 2020.
Participant characteristics
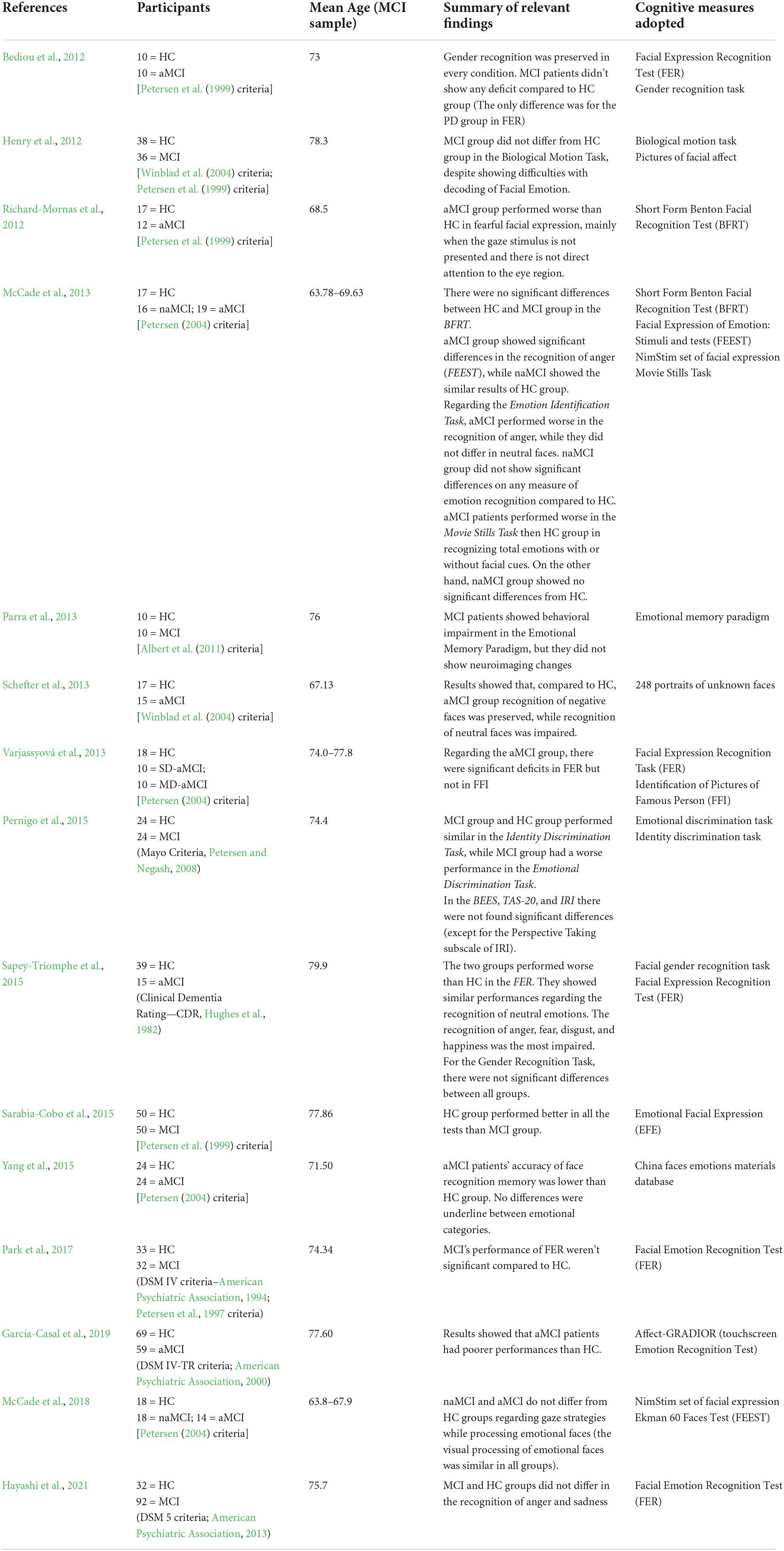
In the 15 studies included in our review, participant ages ranged from 63.70 (McCade et al., 2013) to 79.9 (Sapey-Triomphe et al., 2015).
The sample size varied from a minimum of 10 MCI (Bediou et al., 2012; Parra et al., 2013) to a maximum of 92 MCI (Hayashi et al., 2021); most of the studies differentiated MCI types (for example, aMCI, naMCI, single/multiple domain MCI) (Bediou et al., 2012; Richard-Mornas et al., 2012; McCade et al., 2013, 2018; Sapey-Triomphe et al., 2015; Schefter et al., 2013; Varjassyová et al., 2013; Yang et al., 2015; García-Casal et al., 2019).
Diagnostic criteria
The main diagnostic criteria adopted to assess MCI patients were described by Petersen et al. (1997, 1999), Petersen (2004) and Petersen and Negash (2008), which were used in most of the studies in this review (Bediou et al., 2012; Henry et al., 2012; Richard-Mornas et al., 2012; McCade et al., 2013, 2018; Varjassyová et al., 2013; Pernigo et al., 2015; Sarabia-Cobo et al., 2015; Yang et al., 2015; Park et al., 2017).
Other studies adopted Winblad et al. (2004) criteria (Henry et al., 2012; Schefter et al., 2013), Albert et al. (2011) criteria were used by Parra et al. (2013), the Clinical Dementia Rating (CDR, Hughes et al., 1982) was used by Sapey-Triomphe et al. (2015), and DSM-IV/DSM-IV-TR/DSM-5 (American Psychiatric Association, 1994, 2000, 2013) was adopted by Park et al. (2017), García-Casal et al. (2019), and Hayashi et al. (2021).
Emotion recognition and processing measures
The methodologies used to assess emotion recognition and processing were various. All the studies adopted different types of tasks.
The Facial Expression Recognition Task (FER; Ekman and Friesen, 1976) was the test most used by the authors (Bediou et al., 2012; Richard-Mornas et al., 2012; Varjassyová et al., 2013; Sapey-Triomphe et al., 2015; Hayashi et al., 2021), and the Gender Recognition Task (Bediou et al., 2009) was endorsed by Bediou et al. (2012) and Sapey-Triomphe et al. (2015).
Measures adopted by the other authors are described in Table 1 due to the large number of methodologies selected for each study included in our review.
It is necessary to point out that two studies out of 15 (Parra et al., 2013; Yang et al., 2015) included neuroimaging measures: fMRI was used to investigate the emotional memory associated with emotion recognition, which could be deteriorated in patients with MCI. EEG was registered to investigate the features of emotional face processing using event-related potentials (ERPs).
Summary of relevant findings
All the articles described in our review investigated emotion recognition and processing in patients with MCI; it’s necessary to underline that the results obtained differ due to the variety of tasks adopted by the authors and the sample’s composition.
In this review, eight studies out of 15 reported homogeneous results (Bediou et al., 2012; Richard-Mornas et al., 2012; Sarabia-Cobo et al., 2015; Yang et al., 2015; Park et al., 2017; McCade et al., 2018; García-Casal et al., 2019; Hayashi et al., 2021). Specifically, 4 of them showed similar performances in emotion recognition and processing between MCI patients and healthy subjects: Bediou et al. (2012) found out that patients with aMCI (N = 10) showed no deficits compared with the HC group in either of the two tests adopted (refer to Table 2). Correspondingly, Park et al. (2017) reported that the performance of MCI patients (N = 32) was not significantly different compared to the HC group. On the same line, McCade et al. (2018), who evaluated the visual processing of emotional faces by using two different tests (refer to Table 2), obtained the same results: the performances of aMCI (N = 14) and naMCI (N = 18) were similar to the HC group. The most recent study, conducted by Hayashi et al. (2021), followed the same line and found that the MCI participants (n = 92) did not differ in feelings of anger and sadness in comparison with the HC group.
On the contrary, four further studies underline the worse performance of MCI patients compared to the HC group in emotion recognition tasks. For example, Richard-Mornas et al. (2012) reported worse performances in fearful facial expressions in patients with aMCI (N = 12) compared to the control group. In line with this finding, a study by Sarabia-Cobo et al. (2015) showed the same results (refer to Table 2). Finally, two studies (Yang et al., 2015; García-Casal et al., 2019) reported lower accuracy and poorer performance in face recognition in patients with aMCI (N = 24).
The remaining studies reported ambiguous results. For instance, Henry et al. (2012) discovered that MCI patients did not report performance differences in the Biological Motion Tasks (Vanrie and Verfaillie, 2004), while there were remarkable difficulties with decoding facial emotions (Ekman and Friesen, 1976). Likely, Schefter et al. (2013) adopted only one test (refer to Table 2), from which they obtained two different results: aMCI group (N = 15) displayed deteriorated performance in the recognition of neutral faces, while the recognition of negative faces was preserved.
Another study (Pernigo et al., 2015) assessed emotion recognition and processing with two different tasks [Emotional Discrimination Task (Pernigo et al., 2015), and Identity Discrimination Task (Pernigo et al., 2015)] on a sample of 24 patients with MCI. Identity Discrimination Task obtained similar results between the two groups. Meanwhile, the Emotional Discrimination Task showed a worse performance for MCI patients.
The research of Varjassyová et al. (2013) compared MCI single and cognitive domains (SD-aMCI, N = 10; MD-aMCI, N = 10) and adopted two different tasks to assess emotion recognition (FER and FFI, refer to Table 2). Both aMCI groups reported significant deficits in FER but not in FFI, and the impairment was more significant for MD-aMCI.
Two studies reported emotion-specific deficits (McCade et al., 2013; Sapey-Triomphe et al., 2015); in particular, Sapey-Triomphe et al. (2015) used a large battery of tests (refer to Table 2) and found that aMCI group (N = 15) performed worse than healthy subjects in the FER (Ekman and Friesen, 1976). The group showed similar performances regarding the recognition of neutral emotions, while the recognition of anger, fear, disgust, and happiness was the most impaired. At the same time, there were no significant differences for the Gender Recognition Task (Bediou et al., 2009), in line with the results mentioned before, reported by Bediou et al. (2012).
On the equal line, McCade et al. (2013), using an extensive battery of tests, showed that patients with aMCI (N = 19) performed worse in emotion recognition, especially regarding the recognition of anger, while they did not report significant differences in neutral faces. On the contrary, naMCI (N = 50) group did not reveal any deficit compared to HC.
In the end, the neuropsychological studies underline more accurate results: Yang et al. (2015) investigated the time course of emotional face recognition in patients with aMCI (N = 24) through the use of EEG and ERP data. The results showed that the aMCI and HC groups obtained similar results in visual processing (ERP P100). Nonetheless, in accordance with the cognitive results, the face structural encoding (ERP N170) was delayed in patients with aMCI.
In Parra et al.’s (2013) study, cognitive results showed impairment in the recognition of emotion in MCI patients (N = 10), but there were no neuroimaging changes.
Discussion
This review had the aim of investigating emotion recognition and processing in patients with MCI in order to update the state of current literature on this important but undervalued topic.
There is another important consequence of these studies’ analysis to highlight: knowing which types of cognitive impairments are associated with neurodegenerative disorders could have an important predictive role. Also, knowing the emotional situation (in this case, emotion recognition and processing) could help to lay out a more detailed cognitive profile, which might permit clinicians to determine effective strategies and programs of prevention.
Nevertheless, from the results reported previously, we did not find aligned outcomes. In this section, we try to explore the reasons behind them. The ambiguous results make it difficult to conclude: most of the studies reported cross-over results (Henry et al., 2012; McCade et al., 2013; Parra et al., 2013; Schefter et al., 2013; Varjassyová et al., 2013; Pernigo et al., 2015; Sapey-Triomphe et al., 2015). On the contrary, some of the studies obtained homogeneous results: a part of them showed MCI’s worse performances on emotion recognition and processing tasks (Richard-Mornas et al., 2012; Sarabia-Cobo et al., 2015; Yang et al., 2015; García-Casal et al., 2019). Meanwhile, the remaining studies reported similar performances between the MCI and HC groups (Bediou et al., 2012; Park et al., 2017; McCade et al., 2018; Hayashi et al., 2021).
Those results could have several underlying reasons. First, the wide selection of the tasks adopted by the authors makes it difficult to compare and overlap the results obtained. This heterogeneity could also be considered a strength because it allows us to explore the emotion recognition domain comprehensively. However, the recommendations for the future research are to achieve unanimity regarding the use of all the tests in order to give more validity to the results.
Despite the various methodologies, we underline a common ground: Some studies reported an emotion-specific deficit in MCI patients (those results concern every type of MCI). The emotion-specific deficits regard the recognition of negative emotions (especially for fear and anger), as shown by Richard-Mornas et al. (2012), McCade et al. (2013), and Sapey-Triomphe et al. (2015), while the recognition of neutral emotions seems to be unimpaired, except for the findings of Schefter et al. (2013), which reported opposing results.
Another aspect to highlight is the sample composition that, in the studies included in our review, varied from a minimum of 10 (Bediou et al., 2012; Parra et al., 2013) to a maximum of 92 (Hayashi et al., 2021). This might be why it has been arduous to overlap the full results and, at the same time, could involve a wrong generalization and overestimation of the findings. Despite everything, we decided anyway to include studies with a small sample because the research was limited and we wanted to get a complete picture of this topic.
In addition, studies had a different sample composition based on the ways to diagnose MCI (i.e., DSM IV; American Psychiatric Association, 1994 or Petersen, 1996). For instance, some studies have a sample of patients with aMCI only (Bediou et al., 2012; Richard-Mornas et al., 2012; Schefter et al., 2013; Varjassyová et al., 2013; Sapey-Triomphe et al., 2015; Yang et al., 2015; García-Casal et al., 2019); others have included both types of aMCI and naMCI subjects (McCade et al., 2013, 2018).
Against this background, a good suggestion for future research could be to divide MCI patients based on their categorization in order to make an equal comparison of their results.
Finally, it would be empowering to conduct longitudinal studies to investigate the association between the impairment of emotion recognition and neurodegeneration.
For instance, it could be interesting to see if social cognition deficits, in particular in emotion recognition, deepen simultaneously with the MCI course. This hypothetic exploration could lead to many scenarios, such as the deterioration of this ability over time, the impact of the etiology on this ability impairment (for example, AD-MCI or PD-MCI) or if social cognition impairment could be predictive of major neurodegenerative disorders.
Finally, regarding the neuropsychological studies, the current findings on this topic are very poor.
We highlight the necessity to adopt more of this methodology because it provides more accuracy and precision in results. For example, thanks to the study by Yang et al. (2015), we know that the time course of emotional face recognition (assessed with EEG and ERP data) could lend different results depending on the stage considered (i.e., in MCI patients, the results in the visual processing are similar compared to those in HC, instead of the results in the structural encoding of the face that are worse).
It would be helpful and functional to adopt a combined analysis (cognitive and neuropsychologic assessment) that could better equip the scientific community with more objective and accurate data. These latter might have a more predicting power to assess MCI and address future diagnoses.
Conclusion
This systematic review analyzed the literature of last decade on emotion recognition and processing in MCI population. On the database, there is another review on the topic (McCade et al., 2011), but it dates from 2011, so that is the reason behind the choice to explore this field and obtain new findings.
Regarding 2011, the papers eligible for this work were more than twice (6 in 2015 in 2022), but the results are still ambiguous: heterogeneity measures, different size samples, and ways to diagnose MCI patients do not allow us to align and compare the studies in order to widen the results. At the same time, we could highlight a common point: some studies showed that negative emotions are the most difficult to recognize and process, so there is an emotion-specific deficit (Richard-Mornas et al., 2012; McCade et al., 2013; Sapey-Triomphe et al., 2015). Schefter et al. (2013) underlined that there is also an emotion-specific deficit, but in recognizing neutral emotions.
As mentioned before, different samples and measurements could be a limit to generalizing, while this wide range of options could permit the scientific community to understand and address toward the most suitable methodology design.
In conclusion, neuropsychological approach is still almost unexplored (just 2 studies out of 15), so this might be an encouragement to further explore this path.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
LS carried out part of the literature search, collected part of the studies, and reviewed the final version manuscript. LM had the main contribution in the literature search and selection, created the draft, two tables, and flow diagram, dealt with defining and writing the method, wrote the abstract, introduction, part of the results, discussion, conclusion, reviewed the references, and final version of the manuscript. AI elaborated Table 1, wrote part of the introduction, results, discussion, and conclusion, wrote the abstract, reviewed the references, and final version of the manuscript. SR, GZ, and EB contributed to the collected part of the literature search. MC and LR-C contributed to the collection and selection of the literature. All authors contributed to the article and approved the submitted version.
Funding
Open access funding was provided by Università Della Svizzera Italiana.
Acknowledgments
We thank Ilaria Minio for her valuable support in the review.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
Adolphs, R. (2002). Recognizing emotion from facial expressions: Psychological and neurological mechanisms. Behav. Cogn. Neurosci. Rev. 1, 21–62. doi: 10.1177/1534582302001001003
Albert, M. S., DeKosky, S. T., Dickson, D., Dubois, B., Feldman, H. H., Fox, N. C., et al. (2011). The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 7, 270–279. doi: 10.1016/j.jalz.2011.03.008
American Psychiatric Association (1994). DSM IV. Diagnostic and statistical manual of mental disorders fourth edition. Milano: Masson.
American Psychiatric Association (2000). DSM IV-TR. Diagnostic and statistical manual of mental disorders fourth edition (text revision). Barcelona: Masson.
American Psychiatric Association (2013). Cautionary statement for forensic use of DSM-5. In Diagnostic and statistical manual of mental disorders, 5th Edn. Washington, DC: Author. Cautionary Statement.
Amlerova, J., Laczó, J., Nedelska, Z., Laczó, M., Vyhnálek, M., Zhang, B., et al. (2022). Emotional prosody recognition is impaired in Alzheimer’s disease. Alzheimers Res. Ther. 14:50. doi: 10.1186/s13195-022-00989-7
Anderson, N. D. (2019). State of the science on mild cognitive impairment (MCI). CNS Spectrums 24, 78–87. doi: 10.1017/S1092852918001347
Arioli, M., Crespi, C., and Canessa, N. (2018). Social Cognition through the Lens of Cognitive and Clinical Neuroscience. Biomed. Res. Int. 2018:4283427. doi: 10.1155/2018/4283427
Balconi, M., and Pozzoli, U. (2009). Arousal effect on emotional face comprehension: Frequency band changes in different time intervals. Physiol. Behav. 97, 455–462. doi: 10.1016/j.physbeh.2009.03.023
Bechyně, K., Varjassyová, A., Lodinská, D., Vyhnálek, M., Bojar, M., Brabec, J., et al. (2008). The relation between amygdala atrophy and other selected brain structures and emotional agnosia in Alzheimer disease. Cesk. Slov. Neurol. Neurochir. 71, 675–681.
Bediou, B., Brunelin, J., d’Amato, T., Fecteau, S., Saoud, M., Hénaff, M. A., et al. (2012). A comparison of facial emotion processing in neurological and psychiatric conditions. Front. Psychol. 3:98. doi: 10.3389/fpsyg.2012.00098
Bediou, B., Ryff, I., Mercier, B., Milliery, M., Henaff, M. A., D’amato, T., et al. (2009). Impaired socialcognition in mild Alzheimer dis-ease. J. Geriatr. Psychiatry Neurol. 22, 130–140.
Benton, A. L., Sivan, A. B., Hamsher, K. S., Varney, N. R., and Spreen, O. (1994). Contributions to neuropsychological assessment, 2nd Edn. New York, NY: Oxford University Press.
Breton, A., Casey, D., and Arnaoutoglou, N. A. (2019). Cognitive tests for the detection of mild cognitive impairment (MCI), the prodromal stage of dementia: Meta-analysis of diagnostic accuracy studies. Int. J. Geriatr. Psychiatry 34, 233–242. doi: 10.1002/gps.5016
Brodaty, H. (1996). Caregivers and behavioral disturbances: Effects and interventions. Int. Psychogeriatr. 8, 455–458. doi: 10.1017/s1041610297003840
Brüne, M., and Brüne-Cohrs, U. (2006). Theory of mind–evolution, ontogeny, brain mechanisms and psychopathology. Neurosci. Biobehav. Rev. 30, 437–455. doi: 10.1016/j.neubiorev.2005.08.001
Cárdenas, J., Blanca, M. J., Carvajal, F., Rubio, S., and Pedraza, C. (2021). Emotional Processing in Healthy Ageing, Mild Cognitive Impairment, and Alzheimer’s Disease. Int. J. Environ. Res. Public Health 18:2770. doi: 10.3390/ijerph18052770
Chiu, M. J., Chen, T. F., Yip, P. K., Hua, M. S., and Tang, L. Y. (2006). Behavioral and psychologic symptoms in different types of dementia. J. Formos. Med. Assoc. 105, 556–562. doi: 10.1016/S0929-6646(09)60150-9
Ekman, P., and Friesen, W. V. (1978). Manual for the facial action code. Palo Alto, CA: Consulting Psychologist Press.
Ekman, P., and Friesen, W. V. (1976). Pictures of facial affect. Palo Alto, CA: Consulting Psychologists Press.
Ferretti, V., and Papaleo, F. (2019). Understanding others: Emotion recognition in humans and other animals. Genes Brain Behav. 18:e12544. doi: 10.1111/gbb.12544
García-Casal, J. A., Martínez-Abad, F., Cid-Bartolomé, T., Smith, S. J., Llano-Ordóñez, K., Perea-Bartolomé, M. V., et al. (2019). Usability study and pilot validation of a computer-based emotion recognition test for older adults with Alzheimer’s disease and amnestic mild cognitive impairment. Aging Ment. Health 23, 365–375. doi: 10.1080/13607863.2017.1423033
Hayashi, S., Terada, S., Takenoshita, S., Kawano, Y., Yabe, M., Imai, N., et al. (2021). Facial expression recognition in mild cognitive impairment and dementia: Is the preservation of happiness recognition hypothesis true? Psychogeriatrics 21, 54–61. doi: 10.1111/psyg.12622
Henry, J. D., Thompson, C., Rendell, P. G., Phillips, L. H., Carbert, J., Sachdev, P., et al. (2012). Perception of biological motion and emotion in mild cognitive impairment and dementia. J. Int. Neuropsychol. Soc. 18, 866–873. doi: 10.1017/S1355617712000665
Hughes, C. P., Berg, L., Danziger, W., Coben, L. A., and Martin, R. L. (1982). A new clinical scale for the staging of dementia. Br. J. Psychiatry 140, 566–572. doi: 10.1192/bjp.140.6.566
Keane, J., Calder, A. J., Hodges, J. R., and Young, A. W. (2002). Face and emotion processing in frontal variant frontotemporal dementia. Neuropsychologia 40, 655–665. doi: 10.1016/s0028-3932(01)00156-7
Lang, P. J., Ohman, A., and Vaitl, D. (1988). The International Affective Picture System(photographic slides). Gainesville: The Center for Research inPsychophysiology, University of Florida.
Litvan, I., Aarsland, D., Adler, C. H., Goldman, J. G., Kulisevsky, J., Mollenhauer, B., et al. (2011). MDS Task Force on mild cognitive impairment in Parkinson’s disease: Critical review of PD-MCI. Mov. Disord. 26, 1814–1824. doi: 10.1002/mds.23823
Losh, M., Adolphs, R., Poe, M. D., Couture, S., Penn, D., Baranek, G. T., et al. (2009). Neuropsychological profile of autism and the broadautism phenotype. Arch. Gener. Psychiatry 66, 518–526. doi: 10.1001/archgenpsychiatry.2009.34
Lundqvist, D., Flykt, A., and Öhman, A. (1998). The Karolinska Directed Emotional Faces –KDEF[CD Rom]. Sweden: Department of Clinical Neuroscience.
Martinez, A. M., and Benavente, R. (1998). The AR Face Database. CVC Technical Report, no. 24. West Lafayette, IN: Purdue University.
Matsumoto, D., and Ekman, P. (1988). Japanese and Caucasian Facial Expressions of Emotion(JACFEE) and Neutral Faces (JACNeuF). San Francisco, CA: Intercultural and EmotionResearch Laboratory.
Mattis, S. (1988). Dementia rating scale: Professional manual. Odessa: Psychological Assessment Resources.
McCade, D., Savage, G., Guastella, A., Lewis, S., and Naismith, S. L. (2013). Emotion recognition deficits exist in mild cognitive impairment, but only in the amnestic subtype. Psychol. Aging 28, 840–852. doi: 10.1037/a0033077
McCade, D., Savage, G., and Naismith, S. L. (2011). Review of emotion recognition in mild cognitive impairment. Dement. Geriatr. Cogn. Disord. 32, 257–266. doi: 10.1159/000335009
McCade, D. L., Guastella, A. J., Chen, N., Lewis, S., and Naismith, S. L. (2018). Visual Processing of Emotional Faces is Preserved in Mild Cognitive Impairment. J. Alzheimers Dis. 66, 397–405. doi: 10.3233/JAD-170175
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. Prisma Group. (2009). Reprint-preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Phys. Therapy 89, 873–880. doi: 10.1136/bmj.b2535
Morellini, L., Ceroni, M., Rossi, S., Zerboni, G., Rege-Colet, L., Biglia, E., et al. (2022). Social Cognition in Adult ADHD: A Systematic Review. Front. Psychol. 13:940445. doi: 10.3389/fpsyg.2022.940445
Morese, R., and Palermo, S. (2020). Altruistic Punishment and Impulsivity in Parkinson’s Disease: A Social Neuroscience Perspective. Front. Behav. Neurosci. 14:102. doi: 10.3389/fnbeh.2020.00102
Morese, R., and Palermo, S. (2022). Feelings of loneliness and isolation: Social brain and social cognition in the elderly and Alzheimer’s disease. Front. Aging Neurosci. 14:896218. doi: 10.3389/fnagi.2022.896218
Mueser, K. T., Doonan, R., Penn, D. L., Blanchard, J. J., Bellack, A. S., Nishith, P., et al. (1996). Emotion recognition and social competence in chronic schizophrenia. J. Abnorm. Psychol. 105, 271–275. doi: 10.1037//0021-843x.105.2.271
Palermo, S., Carassa, A., and Morese, R. (2020). Editorial: Perspective-Taking, Self-Awareness and Social Cognition in Neurodegenerative Disorders, Cerebral Abnormalities and Acquired Brain Injuries (ABI): A Neurocognitive Approach. Front. Psychol. 11:614609. doi: 10.3389/fpsyg.2020.614609
Park, S., Kim, T., Shin, S. A., Kim, Y. K., Sohn, B. K., Park, H. J., et al. (2017). Behavioral and Neuroimaging Evidence for Facial Emotion Recognition in Elderly Korean Adults with Mild Cognitive Impairment, Alzheimer’s Disease, and Frontotemporal Dementia. Front. Aging Neurosci. 9:389. doi: 10.3389/fnagi.2017.00389
Parra, M. A., Pattan, V., Wong, D., Beaglehole, A., Lonie, J., Wan, H. I., et al. (2013). Medial temporal lobe function during emotional memory in early Alzheimer’s disease, mild cognitive impairment and healthy ageing: An fMRI study. BMC Psychiatry 13:76. doi: 10.1186/1471-244X-13-76
Pernigo, S., Gambina, G., Valbusa, V., Condoleo, M. T., Broggio, E., Beltramello, A., et al. (2015). Behavioral and neural correlates of visual emotion discrimination and empathy in mild cognitive impairment. Behav. Brain Res. 294, 111–122. doi: 10.1016/j.bbr.2015.07.047
Petersen, R., and Negash, S. (2008). Mild Cognitive Impairment: An Overview. CNS Spectrums 13, 45–53. doi: 10.1017/S1092852900016151
Petersen, R. C. (1996). “Disorders of memory,” in Office practice in neurology, Vol. 138, eds M. A. Samuels and S. Feske (New York, NY: Churchill Livingstone), 728–736.
Petersen, R. C. (2004). Mild cognitive impairment as a diagnostic entity. J. Int. Med. 256, 183–194. doi: 10.1111/j.1365-2796.2004.01388.x
Petersen, R. C. (2016). Mild cognitive impairment. Continuum (Minneapolis, Minn.) 22, 404–418. doi: 10.1212/CON.0000000000000313
Petersen, R. C., Smith, G. E., Waring, S. C., Ivnik, R. J., Kokmen, E., and Tangelos, E. G. (1997). Aging, memory, and mild cognitive impairment. Int. Psychogeriatr. 9, 65–69. doi: 10.1017/s1041610297004717
Petersen, R. C., Smith, G. E., Waring, S. C., Ivnik, R. J., Tangalos, E. G., and Kokmen, E. (1999). Mild cognitive impairment: Clinical characterization and outcome. Arch. Neurol. 56, 303–308. doi: 10.1001/archneur.56.3.303
Richard-Mornas, A., Borg, C., Klein-Koerkamp, Y., Paignon, A., Hot, P., and Thomas-Antérion, C. (2012). Perceived eye region and the processing of fearful expressions in mild cognitive impairment patients. Dement. Geriatr. Cogn. Disord. 33, 43–49. doi: 10.1159/000336599
Sapey-Triomphe, L. A., Heckemann, R. A., Boublay, N., Dorey, J. M., Hénaff, M. A., Rouch, I., et al. (2015). Neuroanatomical Correlates of Recognizing Face Expressions in Mild Stages of Alzheimer’s Disease. PLoS One 10:e0143586. doi: 10.1371/journal.pone.0143586
Sarabia-Cobo, C. M., García-Rodríguez, B., Navas, M. J., and Ellgring, H. (2015). Emotional processing in patients with mild cognitive impairment: The influence of the valence and intensity of emotional stimuli: The valence and intensity of emotional stimuli influence emotional processing in patients with mild cognitive impairment. J. Neurol. Sci. 357, 222–228. doi: 10.1016/j.jns.2015.07.034
Schefter, M., Werheid, K., Almkvist, O., Lönnqvist-Akenine, U., Kathmann, N., and Winblad, B. (2013). Recognition memory for emotional faces in amnestic mild cognitive impairment: An event-related potential study. Neuropsychol. Dev. Cogn. Sec. B Aging Neuropsychol. Cogn. 20, 49–79. doi: 10.1080/13825585.2012.665021
Shimokawa, A., Yatomi, N., Anamizu, S., Torii, S., Isono, H., Sugai, Y., et al. (2001). Influence of deteriorating ability of emotional comprehension on interpersonal behavior in Alzheimer-type dementia. Brain Cogn. 47, 423–433. doi: 10.1006/brcg.2001.1318
Smith, G. E., Petersen, R. C., Parisi, J. E., Ivnik, R. J., Kokmen, E., Tangalos, E. G., et al. (1996). Definition, course, and outcome of mild cognitive impairment. Aging Neuropsychol. Cogn. 3, 141–147. doi: 10.1080/13825589608256619
Tottenham, N., Tanaka, J. W., Leon, A. C., McCarry, T., Nurse, M., Hare, T. A., et al. (2009). The NimStim set of facial expressions:Judgments from untrained research participants. Psychiatry Res. 168, 242–249. doi: 10.1016/j.psychres.2008.05.006
Vanrie, J., and Verfaillie, K. (2004). Perception of biological motion:A stimulus set of human point-light actions. Behav. Res. Methods Instr. Comput. 36, 625–629.
Varjassyová, A., Hořínek, D., Andel, R., Amlerova, J., Laczó, J., Sheardová, K., et al. (2013). Recognition of facial emotional expression in amnestic mild cognitive impairment. J. Alzheimers Dis. 33, 273–280. doi: 10.3233/JAD-2012-120148
Wang, Y., and Luo, Y. J. (2005). Standardization and assessment of college students’ facial expression of emotion. Chin. J. Clin. Psychol. 13, 396–398.
Williams, L. M., Mathersul, D., Palmer, D. M., Gur, R. C., Gur, R. E., and Gordon, E. (2009). Explicit identification and implicit recognition of facial emotions: I. Age effects in males and females across 10 decades. J. Clin. Exp. Neuropsychol. 31, 257–277. doi: 10.1080/13803390802255635
Winblad, B., Palmer, K., Kivipelto, M., Jelic, V., Fratiglioni, L., Wahlund, L. O., et al. (2004). Mild cognitive impairment–beyond controversies, towards a consensus: Report of the International Working Group on Mild Cognitive Impairment. J. Int. Med. 256, 240–246. doi: 10.1111/j.1365-2796.2004.01380.x
Yang, L., Zhao, X., Wang, L., Yu, L., Song, M., and Wang, X. (2015). Emotional face recognition deficit in amnestic patients with mild cognitive impairment: Behavioral and electrophysiological evidence. Neuropsychiatr. Dis. Treat. 11, 1973–1987. doi: 10.2147/NDT.S85169
Keywords: mild cognitive impairment, social cognition, systematic review, tasks, emotion recognition and processing
Citation: Morellini L, Izzo A, Rossi S, Zerboni G, Rege-Colet L, Ceroni M, Biglia E and Sacco L (2022) Emotion recognition and processing in patients with mild cognitive impairment: A systematic review. Front. Psychol. 13:1044385. doi: 10.3389/fpsyg.2022.1044385
Received: 14 September 2022; Accepted: 28 September 2022;
Published: 28 October 2022.
Edited by:
Sara Palermo, University of Turin, ItalyReviewed by:
Chiara Fante, National Research Council (CNR), Genova, ItalyMarghertia Luciani, University of Applied Sciences and Arts of Southern Switzerland (SUPSI), Switzerland
Copyright © 2022 Morellini, Izzo, Rossi, Zerboni, Rege-Colet, Ceroni, Biglia and Sacco. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lucia Morellini, bHVjaWEubW9yZWxsaW5pQHVzaS5jaA==
†These authors have contributed equally to this work and share first authorship
 Lucia Morellini
Lucia Morellini Alessia Izzo
Alessia Izzo Stefania Rossi
Stefania Rossi Giorgia Zerboni2
Giorgia Zerboni2 Martino Ceroni
Martino Ceroni Leonardo Sacco
Leonardo Sacco