
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 26 October 2022
Sec. Positive Psychology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.1036564
This article is part of the Research TopicAn Integrated Positive Psychology Approach Into Counseling in Different SettingsView all 12 articles
The aim of this study is to evaluate “ReStress Mindset,” an internet-delivered intervention that combines the Stress Mindset Training Program (SMTP) with Acceptance and Commitment Therapy (ACT). To that end, the current study determined whether the pilot study’s findings on the intervention’s effectiveness on stress mindset and stress response among university students in the midst of the COVID-19 pandemic, remained for 3 months following the completion of “ReStress Mindset” intervention. Twenty-six participants were randomly assigned to an intervention (N = 12) and a control (N = 14) group. Participants in the intervention group attended 5 weekly sessions online, between the second and third waves of the COVID-19 pandemic. All participants completed self-report questionnaires (Stress Mindset Measure, Satisfaction With Life Scale, Depression Anxiety and Stress Scale-9, Perceived Stress Scale, Scale of Positive, and Negative Experience) before, at the end of the intervention and 3 months after the completion of the program. The “ReStress Mindset” intervention resulted in a statistically significant increase in “stress-is-enhancing” mindset (SIEM), life satisfaction, and self-efficacy against stress, as well as a statistically significant decrease in “stress-is-debilitating” mindset (SIDM), with these effects lasting 3 months after the program’s completion. The findings of this study suggest that university students could benefit from the “ReStress Mindset” intervention in order to cultivate and maintain a positive stress mindset and increase their life satisfaction and self-efficacy against stress, even during the COVID-19 pandemic or any other highly stressful period or crisis.
On March 2020, World Health Organization [WHO] (2020) has declared the COVID-19 as a pandemic. Coronavirus disease (COVID-19), which is thought to have originated in Wuhan, China, in December 2019, has had a significant global impact on people’s mental health (Holmes et al., 2020). A systematic review and meta-analysis, during the early period of the COVID-19 crisis in China, found that stress was the most prevalent (48.1%) mental health consequence of the COVID-19 pandemic, followed by depression (26.9%) and anxiety (21.8%; Bareeqa et al., 2021). According to a review study, stress can have a direct and indirect impact on health through changes in health behaviors, which can result in a variety of negative mental and physical health effects, including an increased risk of infectious diseases like COVID-19 (O’Connor et al., 2021). Moreover, a systematic review and meta-analysis showed that 28.6% of people worldwide reported low levels of wellbeing during the COVID-19 outbreak (Nochaiwong et al., 2021).
University students’ mental health is a growing public health concern (Bewick et al., 2010; Gallagher, 2012). Many studies show that students experience higher levels of distress, depression, and anxiety than the general population at their age (Eisenberg et al., 2007; Bayram and Bilgel, 2008; Lipson et al., 2018). A systematic review and meta-analysis found that during the COVID-19 pandemic anxiety symptoms were more prevalent among university students compare to similar populations prior to the pandemic (Deng et al., 2021). Moreover, the detrimental effects of the COVID-19 outbreak have been associated to higher stress levels and lower self-rated health among university students (Zurlo et al., 2020; Ryerson, 2022). Also, it is well documented that during the COVID-19 pandemic, university students and young adults worldwide experienced severe lifestyle and mental health disruptions, with serious consequences for their wellbeing (Cao et al., 2020; Li et al., 2020; Liu et al., 2020; McGinty et al., 2020; Tang et al., 2020; Giuntella et al., 2021).
A study in China found that during the coronavirus disease outbreak, the prevalence rates of stress among 746,217 university students was 34.9%, while anxiety symptoms were 11.0% (Ma et al., 2020). In a survey study conducted in the United Kingdom during the COVID-19 pandemic, university students reported significant levels of anxiety and depression, with more than half reporting levels above clinical cutoffs, as well as low levels of resilience (Chen and Lucock, 2022). Also, a study conducted among Polish university students found that self-reported physical health and life satisfaction decreased significantly during three waves of the COVID-19 pandemic (Rogowska et al., 2021b). Moreover, university students who reported high levels of perceived stress were seven times more likely to indicate high anxiety disorder risk. Low life satisfaction was also found to be a predictor of higher anxiety levels (Rogowska et al., 2021b). In Greece, a survey study among 1,018 undergraduates during the COVID-19 quarantine, found significantly increased levels of depression, anxiety, stress, and negative affect, while life disruption and perceived threat of the disease were risk factors in all psychological distress measures (Kornilaki, 2022).
Furthermore, the COVID-19 pandemic has exacerbated known mental health risk factors and other health concerns among university students, while also compromising students’ academic outcomes and future prospects (Lederer et al., 2021). As a result of campus closures and strict social isolation and physical distancing measures enacted in response to the COVID-19 pandemic, tertiary education institutions have shifted to online learning platforms. This transition is likely to exacerbate academic and other stressors for university students, such as mounting financial problems, a lack of social relationships, housing and food insecurity, uncertainty about the future, insufficient computer skills, poor quality of online classes, online exams, academic performance, and future studies (Byrnes et al., 2020; Kapasia et al., 2020; Aristovnik et al., 2021; Lederer et al., 2021; Chen and Lucock, 2022).
Previous research has clearly demonstrated that university students are experiencing unprecedented disruption and uncertainty, demanding immediate action to mitigate the pandemic’s negative academic and psychosocial impact (Grubic et al., 2020; Kornilaki, 2022). To that end, developing and implementing adequate prevention and intervention programs at universities should be a top priority in the fight against the COVID-19 pandemic, both during and after this global crisis (Grubic et al., 2020; Cénat et al., 2021; Rogowska et al., 2021b; Kornilaki, 2022).
There is mounting evidence that mindset influences not only intelligence (Dweck, 2008) and aging (Levy and Myers, 2004), but also the stress response (Crum et al., 2013). According to a growing body of research on mindset, changing individual’s mindset toward stress can have a significant impact on stress response (Crum et al., 2017). Stress mindset is conceptualized as one’s belief that stress itself has either enhancing or debilitating consequences for outcomes such as performance and productivity, health and wellbeing, learning and growth (Crum et al., 2013). Moreover, “stress-is-enhancing” (SIEM) and “stress-is-debilitating” (SIDM) mindsets can have a different impact on physiological and behavioral responses to stress (Crum et al., 2013). Furthermore, research suggests that stress mindset is related to perceived health and life satisfaction over and above the effects of amounts of stress, stress appraisals, and coping strategies (Crum et al., 2013).
Acceptance and Commitment Therapy (ACT; Hayes et al., 2011) is a transdiagnostic psychological intervention that aims to increase psychological flexibility through six core processes (cognitive defusion, acceptance, committed action, values, contact with the present moment, and self-as-context), all of which are important for improving mental health (Hayes et al., 2011). Psychological flexibility is defined as the ability to be mindful of experiences in the present moment, in an accepting and non-judgmental manner, as well as to take action guided by values in order to move toward who or what is important, even in the face of adversity (Hayes et al., 2006; Polk and Schoendorff, 2014; Levin et al., 2017). According to ACT, human suffering derives from psychological inflexibility, a core process in which behavior is rigidly guided by immediate psychological experiences rather than by the individual’s values or goals (Levin et al., 2017). Experiential avoidance is a major component of psychological inflexibility, in which individuals avoid negative internal experiences such as thoughts, emotions, bodily sensations, and memories (Kocovski et al., 2013). Previous research found that university students who received ACT intervention reported less stress, reduced anxiety and depressive symptoms, increased psychological flexibility and general mental health, as well as improved mindful acceptance (Levin et al., 2017; Grégoire et al., 2018).
A meta-analysis of internet-delivered interventions for mental health and wellbeing in university students found that these types of interventions can be effective and improve the functioning of university students (Harrer et al., 2019). The “ReStress Mindset” is an internet-delivered intervention program designed to change the stress mindset and stress response of Greek university students in the midst of the COVID-19 pandemic (Karampas et al., 2022). The modules of this program were formed by combining the Stress Mindset Training Program (SMTP; Crum, 2011; Crum et al., 2013) and the ACT matrix protocol (Polk and Schoendorff, 2014) into a unified psycho-educational intervention. The pilot study of the “ReStress Mindset” intervention demonstrated that combining both models in a single intervention benefited university students by providing them with a broader repertoire of strategies and tools to deal with their challenges (Karampas et al., 2022). Research also suggests that providing university students with a variety of coping strategies during this period of extreme uncertainty can help them deal with stress and improve their overall wellbeing (Rogowska et al., 2021a). Moreover, Hayes et al. (2019) argue that we must tailor interventions to specific people in specific contexts. In this regard, the “ReStress Mindset” intervention is a context-oriented program that acknowledges that psychological flexibility contains the ability to shift mindsets (Kashdan and Rottenberg, 2010). Furthermore, the “ReStress Mindset” intervention is built within the framework of evidence-based processes of change and intervention elements that move them forward (Hayes and Hofmann, 2018; Hofmann et al., 2021). Processes of change are defined as theory-based, dynamic, progressive, contextually bound, modifiable, and multilevel change mechanisms that occur in predictable, empirically established sequences oriented toward desirable outcomes (Hofmann and Hayes, 2019). The modules of the intervention are presented in Table 1.
The aim of the present study is to evaluate “ReStress Mindset” intervention (Karampas et al., 2022). To that end, this study will determine whether the findings of the pilot study regarding the intervention’s effectiveness on stress mindset and stress response among university students in the midst of the COVID-19 pandemic (Karampas et al., 2022), will remain for 3 months following the completion of the intervention.
The pilot study implemented the “ReStress Mindset” intervention led university students to cultivate a positive stress mindset even during COVID-19 pandemic, although further studies are required to establish the stability of the results over longer periods of time (Karampas et al., 2022). The results of the pilot study also indicated an increase in the levels of life satisfaction and psychological resilience of the intervention group, while the levels of life satisfaction and psychological resilience of the control group decreased after the intervention (Karampas et al., 2022). Additionally, no statistically significant changes in positive and negative emotions and psychological symptoms, were observed following the intervention, possibly due to the severe psychological impact of the COVID-19 pandemic (Karampas et al., 2022).
Thus, the present study will focus on answering the following research questions: (1) Does the “ReStress Mindset” intervention result in higher levels of SIEM, 3 months following the completion of the intervention? (2) Does the “ReStress Mindset” intervention result in lower levels of SIDM, 3 months following the completion of the intervention? (3) Does the “ReStress Mindset” intervention lead to an increase in levels of positive emotions, self-efficacy against stress, and life satisfaction, 3 months following the completion of the intervention? (4) Does the “ReStress Mindset” intervention result in lower levels of depression, anxiety, perceived helplessness against stress, and negative emotions, 3 months following the completion of the intervention?
The sample consisted of 26 undergraduate Psychology students (96.2% women), aging from 19 to 39 years old (Mage = 24.46). Participants were recruited from Panteion University of Social and Political Sciences in Greece by responding to an online invitation sent via newsletter email. The majority of the participants was unemployed (50%), while some participants were working part-time (30.8%) and others full-time (19.2%). Regarding the marital status of the participants, 43.2% of them were single, 46.2% were in a relationship, 7.7% were married, and 3.8% were divorced.
Participants were asked to report demographic information regarding their gender, age, marital and employment status.
(1) Stress Mindset Measure (SMM; Crum et al., 2013; Greek version: Karampas et al., 2020). In the SMM the participants are rating how strongly they agree or disagree with eight statements (e.g., the effects of stress are positive and should be utilized, the effects of stress are negative and should be avoided) on a 0 (strongly disagree) to 4 (strongly agree) scale. In the Greek study, two factors were identified instead of a single stress mindset factor representing two different mindsets on the effects of stress: either it is enhancing or debilitating.
(2) Satisfaction With Life Scale (SWLS; Diener et al., 1985; Greek version: Galanakis et al., 2017). The scale measures individual’s cognitive assessment of his/her life indicating satisfaction with life levels. The SWLS consists of five items rated on a 7-point Likert-type scale (1-Strongly disagree to 7-Strongly agree).
(3) Depression Anxiety Stress Scales-9 (DASS-9; Yusoff, 2013; Greek version: Kyriazos et al., 2018a). DASS-9 is an empirically derived version based on DASS-21 (Lovibond and Lovibond, 1995; Pezirkianidis et al., 2018). The DASS-9 measures three negative emotional states (a) depression, (b) anxiety, and (c) tension/stress. Respondents report the presence of 9 symptoms over the previous week using a Likert-type scale (0-Did not apply to me at all to 3-Applied to me very much or most of the time). The three subscales of the DASS-9 were each cumulatively scored between 0 and 9, with higher scores demonstrating poorer mental health.
(4) Perceived Stress Scale (PSS; Cohen et al., 1983; Greek version: Andreou et al., 2011). The PSS has been developed to measure general stress based on the conceptualization of stress as an appraisal of something threatening and that people cope with stress more or less effectively (Lazarus and Folkman, 1984). PSS items ask participants to reflect on the past month and includes questions such as “Have you been upset by something that happened unexpectedly?” and “Have you felt that you could not cope with all the things you had to do?” (Scale: 0 = never to 4 = very often).
(5) Scale of Positive and Negative Experience (SPANE; Diener et al., 2010; Greek version SPANE-8: Kyriazos et al., 2018b). SPANE-8 is a revised structure containing one general feeling per dimension instead of three in the original SPANE (Diener et al., 2010). This resulted in a briefer structure with four positive (Pleasant, Happy, Joyful, Contented) and four negative (Bad, Sad, Afraid, Angry) items. Items are scored on a Likert scale from 1 (very rarely or never) to 5 (very often or always).
All participants (N = 26) were informed on the purpose of the study and gave their informed consent online. Also, participants were randomly allocated in the intervention (N = 12) and control (N = 14) groups and completed an online battery of questionnaires, as described above, at the beginning (T1), at the end of the intervention (T2) and 3 months after the completion of the program (T3). The members of the control group were offered the opportunity to attend the intervention after the completion of the study. The intervention lasted 5 weeks and consisted of 2-h modules. The intervention took place in February and March 2021, between the second and third waves of the COVID-19 pandemic, with a follow-up in June 2021. The content for each module, as well as the assigned homework, are listed in Table 1.
The data was analyzed using the Statistical Package for Social Sciences (SPSS), version 28. Firstly, we conducted preliminary analyses to test if the data is appropriate and, then, a two-way (2 × 3) repeated measures mixed design ANOVA was performed to answer the research questions.
For each of the study variables we computed the mean, standard deviation, and Cronbach’s alpha coefficient (see Table 2). The means show differences in the levels of specific variables between the three time-points. Also, the results based on the internal consistency coefficient indicate adequate reliability of all subscales except for the subscale of DASS-9 measuring stress and the subscale of SPANE-8 measuring negative emotions, whose internal consistency range from 0.60 to 0.76. Moreover, the Kolmogorov-Smirnov tests indicate that all variables follow a normal distribution in almost every time-point.
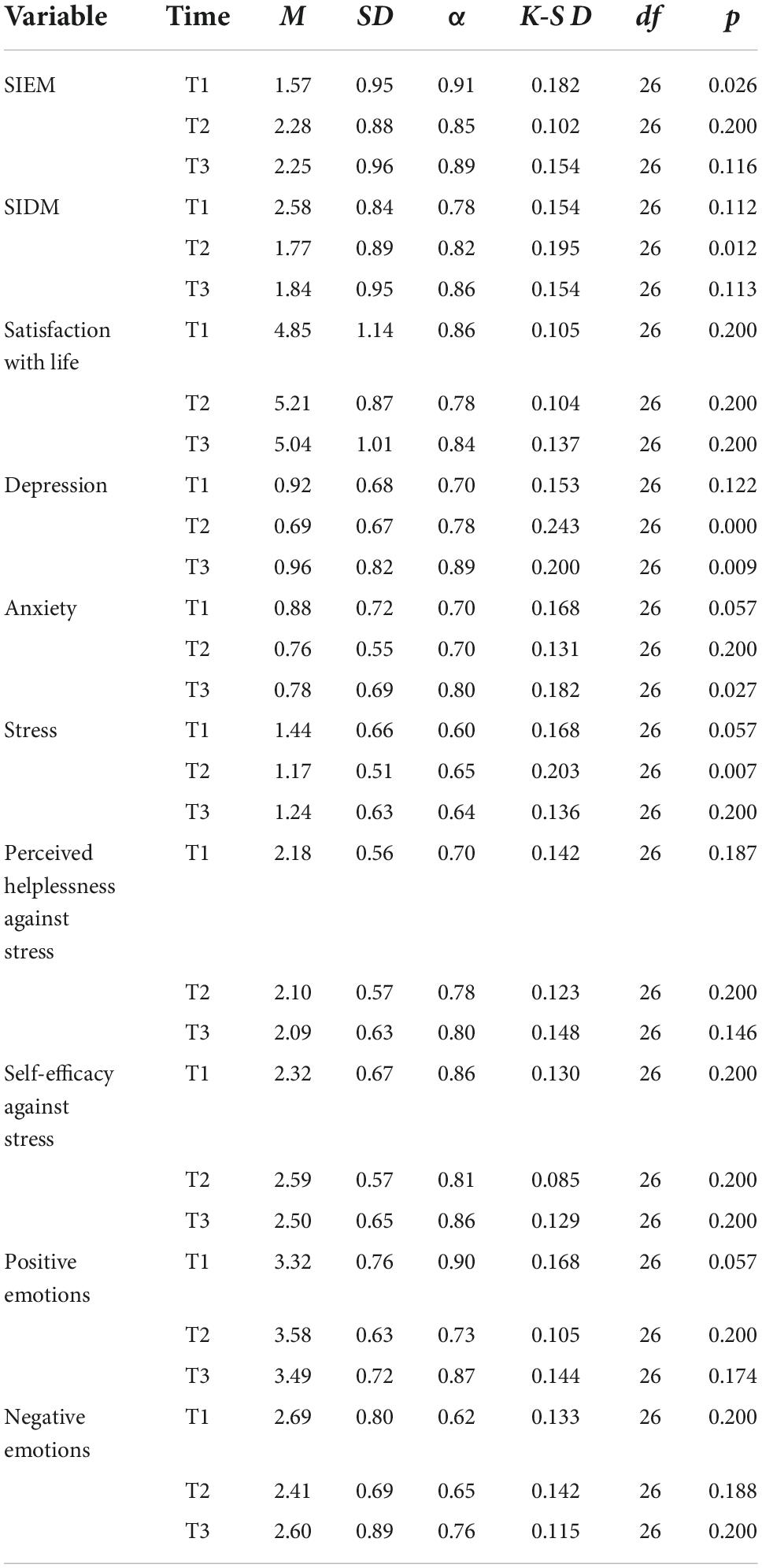
Table 2. Descriptive statistics, alpha levels, and normality coefficients of study variables for the three time-points (N = 26).
A two-way (2 × 3) repeated measures mixed design ANOVA was conducted to test the main effect of time (before, after the end, and 3 months after the intervention) and the two-way interaction amongst time and condition (intervention and control) on the levels of SIEM, SIDM, depression, anxiety, stress, positive and negative emotions, life satisfaction, perceived helplessness, and self-efficacy against stress. The required assumptions were met.
The results indicated a statistically significant main effect of Time on SIEM [F(2,48) = 21.627, MSE = 6.505, p < 0.001, ηp2 = 0.47], SIDM [F(2,48) = 23.196, MSE = 5.970, p < 0.001, ηp2 = 0.49], experiencing of positive emotions [F(2,48) = 3.205, MSE = 0.483, p = 0.049, ηp2 = 0.12], self-efficacy against stress [F(2,48) = 6.429, MSE = 0.539, p = 0.003, ηp2 = 0.21], satisfaction with life [F(2,48) = 5.922, MSE = 0.947, p = 0.005, ηp2 = 0.20], depression [F(2,48) = 3.345, MSE = 0.570, p = 0.044, ηp2 = 0.12], and stress [F(2,48) = 4.708, MSE = 0.616, p = 0.014, ηp2 = 0.16]. More specifically, the findings indicate that the participants in the study report higher mean SIEM, positive emotions, self-efficacy against stress, and satisfaction with life levels and lower mean SIDM, depression, and stress levels after the intervention.
To shed more light in the aforementioned results, we tested for possible interactions. A statistically significant interaction between Time and Condition was demonstrated for SIEM [F(2,48) = 13.118, MSE = 3.946, p < 0.001, ηp2 = 0.35], SIDM [F(2,48) = 18.040, MSE = 4.643, p < 0.001, ηp2 = 0.43], positive emotions [F(2,48) = 3.940, MSE = 0.593, p = 0.026, ηp2 = 0.14], negative emotions [F(2,48) = 3.362, MSE = 0.727, p = 0.043, ηp2 = 0.12], perceived helplessness against stress [F(2,48) = 3.629, MSE = 0.367, p = 0.034, ηp2 = 0.13], self-efficacy against stress [F(2,48) = 4.531, MSE = 0.380, p = 0.016, ηp2 = 0.16], life satisfaction [F(2,48) = 7.096, MSE = 1.135, p = 0.002, ηp2 = 0.23], and depression [F(2,48) = 4.282, MSE = 0.730, p = 0.019, ηp2 = 0.15].
Figures 1, 2 depict the interaction between Time and Condition for SIEM and SIDM, respectively. The first figure depicts an increase on the intervention group levels of SIEM after the intervention that remains 3 months after and slight changes on the levels of the control group. The second figure shows a decrease of SIDM on the intervention group at the second time-point that remains in the follow up measurement, while the SIDM levels of the control group remain unchanged.
Figures 3, 4 depict almost the same pattern in the interaction between Time and Condition for the experiencing of positive and negative emotions. The intervention group levels of positive emotions increase, and the negative emotions decrease after the intervention and these levels remain 3 months after the intervention. However, the control group levels on both variables do not change in the second time-point, but the levels of positive emotions seem to decrease, and the negative emotions increase during Time 3.
On the other hand, Figure 5 depict a decrease on the levels of perceived helplessness against stress in Time 2 for the intervention group, half of which remains 3 months after the intervention, while the levels of the control group seem to increase in the second time-point and bounce back to the previous levels in Time 3. The pattern of the interaction between Time and Condition for the self-efficacy against stress is different (see Figure 6). The intervention group levels clearly increase in Time 2 and the same levels remain in Time 3. However, the self-efficacy levels of the control group have slight changes between the three time-points.
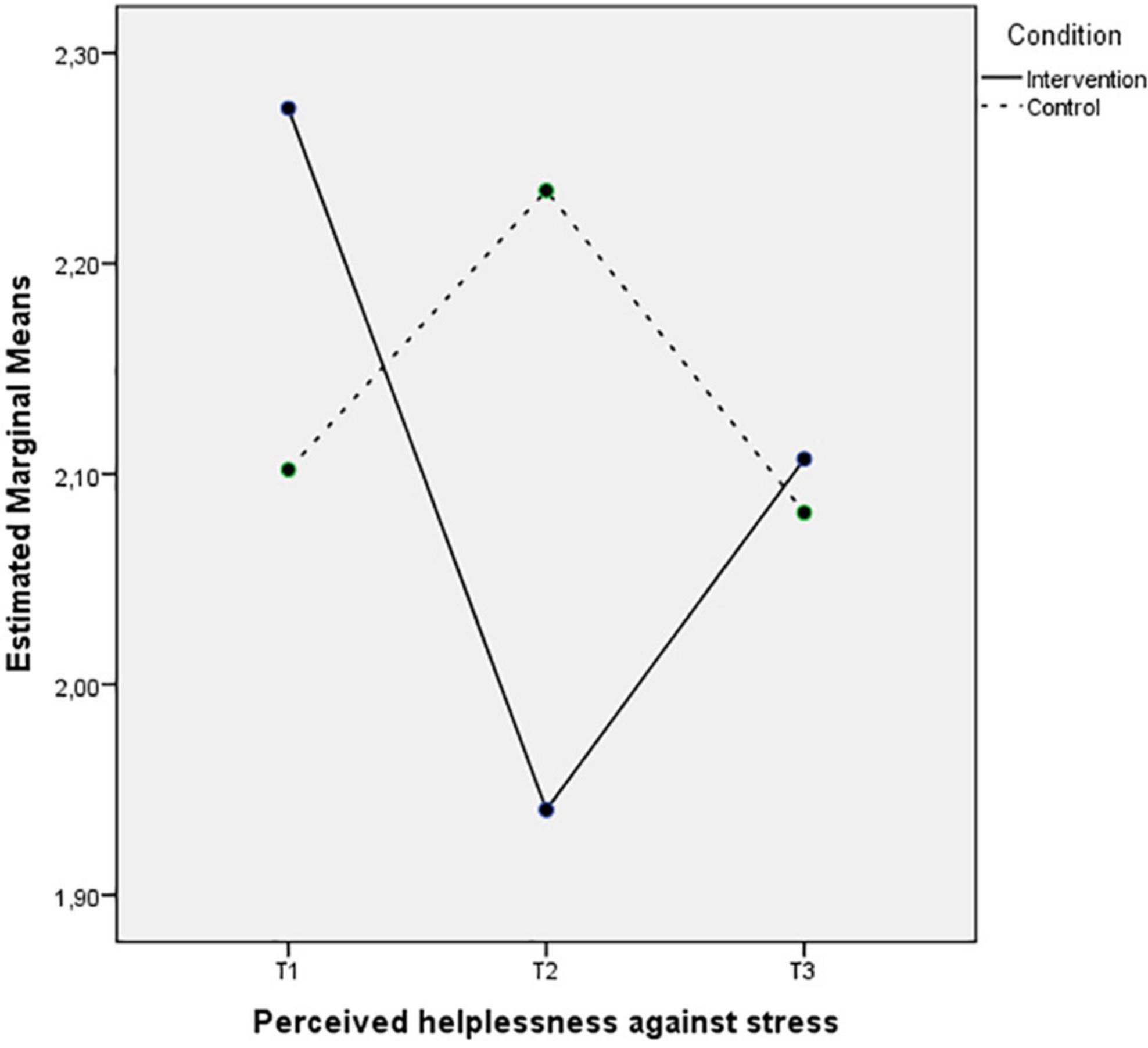
Figure 5. Mean of perceived helplessness against stress showing time effects for control and intervention groups.
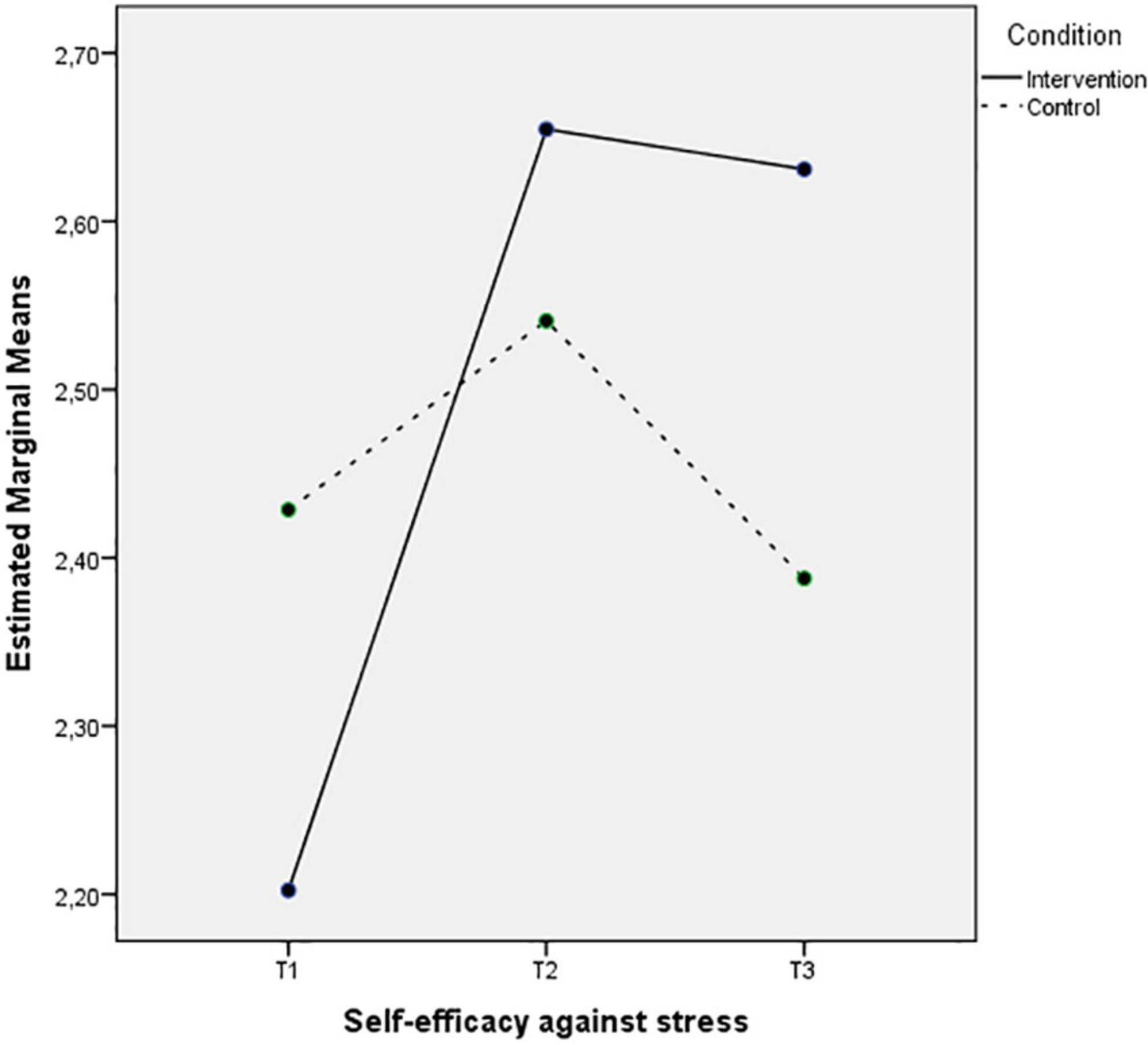
Figure 6. Mean of self-efficacy against stress showing time effects for control and intervention groups.
The last two Figures 7, 8 also depict an increase of the life satisfaction levels and a decrease of the depression levels in Time 2 that remain 3 months after the intervention, while the control group levels of these wellbeing indices remain the same or even decrease during the three measurements.
To interpret the interactions between Time and Condition more precisely, we ran paired t-tests for each group between pairs of the three time-points and independent samples t-test between the groups for the three time-points. A Bonferroni correction was applied to the significance level (0.05/6 = 0.008).
The results indicate statistically significant differences only for the intervention group (see Table 3) regarding (a) SIEM between T1–T2 [t(11) = −7.745, p < 0.001, Cohen’s D = −4,67] and T1–T3 [t(11) = −3.915, p = 0.002, Cohen’s D = −2,36], (b) SIDM between T1–T2 [t(11) = 7.487, p < 0.001, Cohen’s D = 4,51] and T1–T3 [t(11) = 5.500, p < 0.001, Cohen’s D = 3,32], (c) self-efficacy against stress between T1–T2 [t(11) = −3.681, p = 0.004, Cohen’s D = −2,21], and (d) life satisfaction between T1–T2 [t(11) = −3.300, p = 0.008, Cohen’s D = −1,99] and T1–T3 [t(11) = −3.341, p = 0.007, Cohen’s D = −2.01]. More specifically (see Table 4), the participants in the intervention group reported significantly higher levels of SIEM (T1: M = 1.15, SD = 0.71; T2: M = 2.56, SD = 0.72; T3: M = 2.29, SD = 1.09) and life satisfaction (T1: M = 2.20, SD = 0.57; T2: M = 2.65, SD = 0.44; T3: M = 2.63, SD = 0.42), and lower levels of SIDM that remain significant 3 months after the intervention (T1: M = 2.85, SD = 0.76; T2: M = 1.19, SD = 0.53; T3: M = 1.42, SD = 0.73). Moreover, the participants in the intervention group reported higher levels of self-efficacy against stress after the intervention (T1: M = 2.20, SD = 0.57; T2: M = 2.65, SD = 0.44). The small sample size in each group and the Bonferroni correction didn’t result to other significant results, even though the levels of several variables tend to change in different time-points. No statistically significant differences were found in the control group.
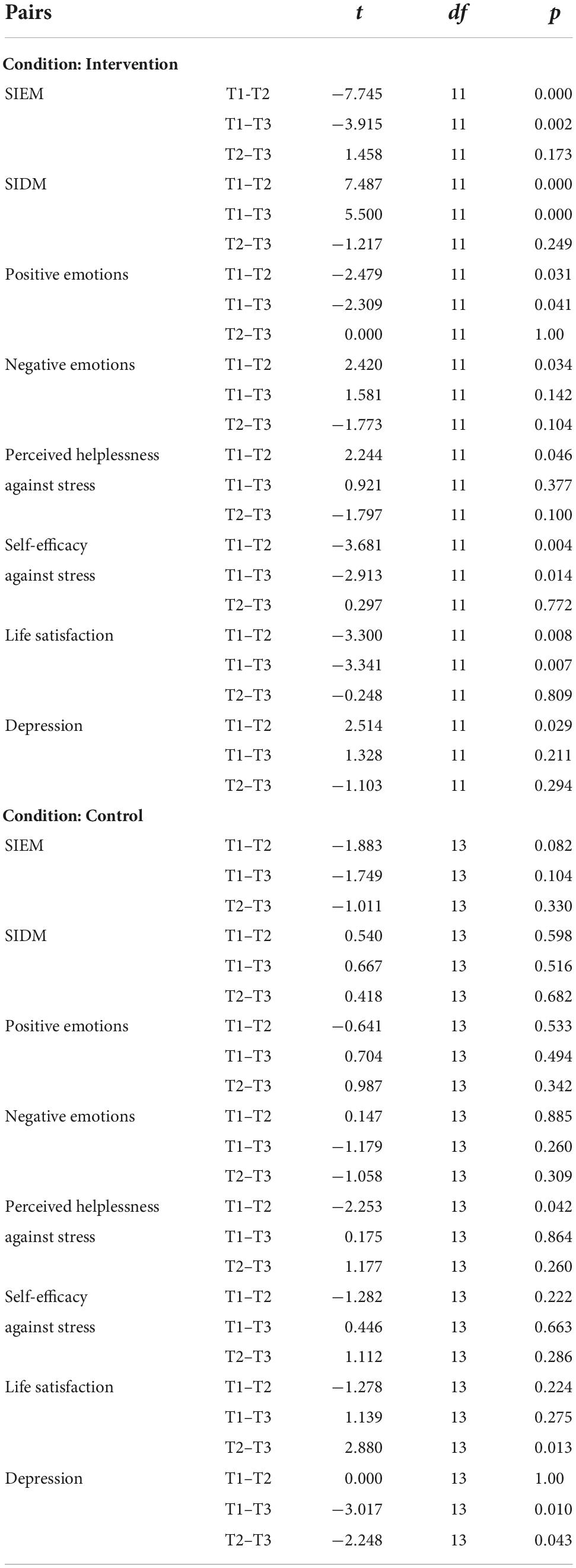
Table 3. Paired-samples t-test coefficients for the mean comparison of pairs between the three time-points as a function of condition.
Additionally, statistical significant differences were found between the two conditions in the second time-point regarding the SIDM levels [t(22.157) = −3.929, p = 0.001 Cohen’s D = 1,52; see Table 5]. Based on Table 4, the participants of the intervention group reported significantly lower levels of SIDM comparing to the control group (intervention: M = 1.19, SD = 0.53; control: M = 2.27, SD = 0.85). No other significant differences emerged, since the variable levels in the two groups were not equal in the first time-point.
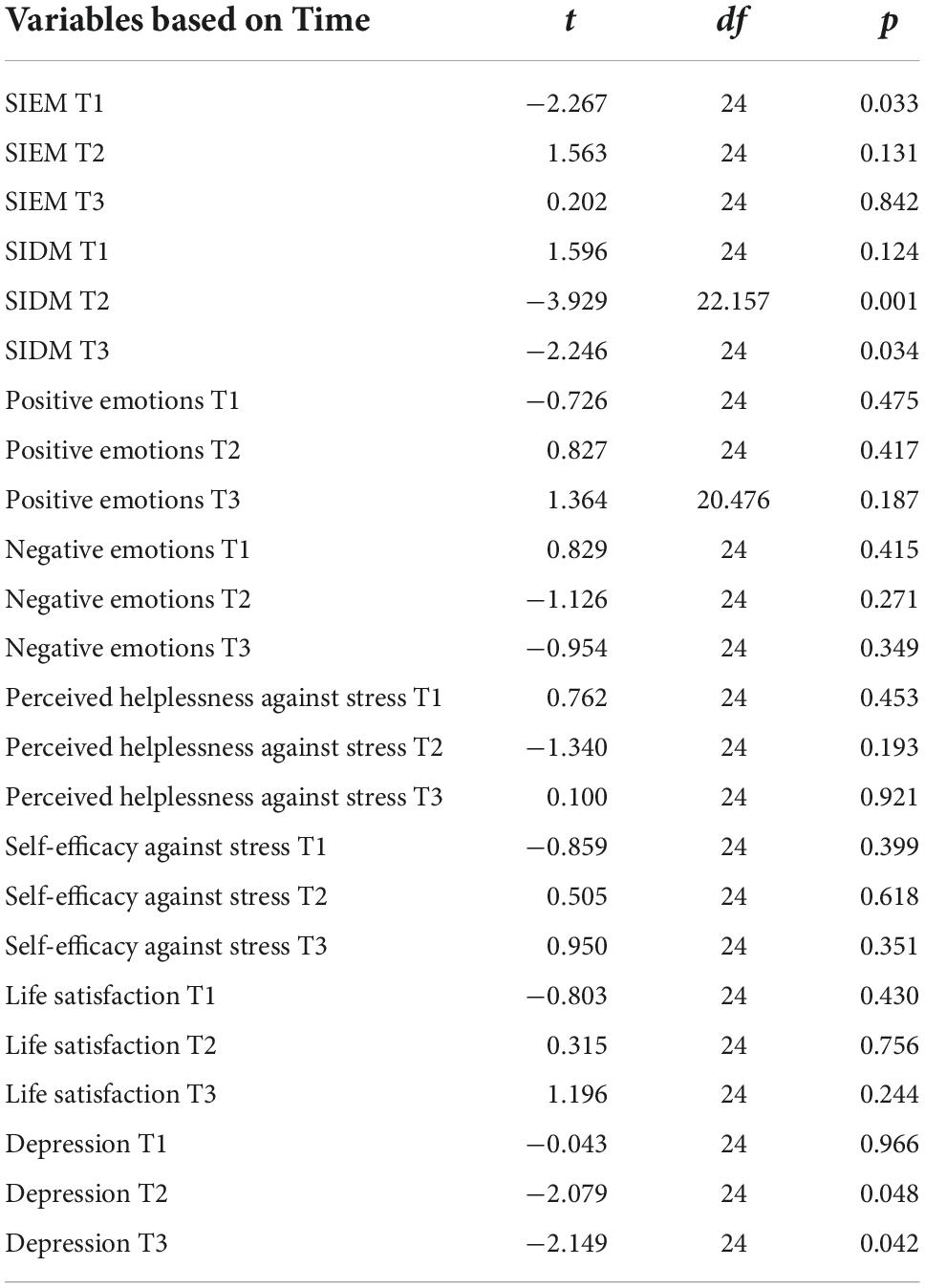
Table 5. Independent samples t-test coefficients for the mean comparison of control and intervention groups as a function of time.
The results of the present study support the notion that stress mindset can be changed to improve stress responses by influencing the way stress is psychologically experienced and behaviorally approached; thus, the findings support that a change in stress mindset affects individual levels of psychological symptoms and wellbeing (Crum et al., 2013, 2017).
More specifically, answering the first and second research question, the “ReStress Mindset” intervention led participants to a statistically significant increase in SIE mindset that remained 3 months after the completion of the program, and a statistically significant decrease in SID mindset that also remained in the follow up measurement. These results are confirming previous research findings regarding the shift of the university students’ stress mindset to a more SIE mindset and a less SID mindset following the completion of the “ReStress Mindset” intervention in the midst of COVID-19 pandemic (Karampas et al., 2022).
Furthermore, the results answered the third research question indicating a statistically significant increase in the levels of life satisfaction that remained significant 3 months after the intervention. Moreover, the participants in the intervention group reported statistically significant higher levels of self-efficacy against stress after the intervention. These findings are in line with previous research indicating that SIE mindset is positively correlated with increased life satisfaction, and positive ways of perceiving stress (self-efficacy when confronting stress) (Crum et al., 2013; Karampas et al., 2020).
The findings also answered the fourth research question, since it was found that the levels of positive emotions increased in the intervention group, while the levels of negative emotions, depression, and perceived helplessness against stress decreased after the intervention and remained unchanged 3 months later, while no statistically significant differences were found in the control group. These findings are consistent with previous research indicating that SIE mindset predicted positive affect, decreased depressive symptoms, and lower negative feelings (perceived helplessness when confronting stress and negative emotions) (Crum et al., 2013; Kilby and Sherman, 2016; Karampas et al., 2020).
The findings of this study have significant implications for university students during the COVID-19 pandemic, since they are facing severe lifestyle and mental health disruptions, which have profound ramifications for their wellbeing (Cao et al., 2020; Li et al., 2020; Liu et al., 2020; McGinty et al., 2020; Tang et al., 2020; Giuntella et al., 2021). To begin with, shifting to a more SIE mindset and away from a more SID mindset is critical since stress mindset affects both the extent to which stress is psychologically experienced and the way stress is behaviorally approached, two variables that are crucial in determining health and performance outcomes under stress (Crum et al., 2013; Jamieson et al., 2013). Moreover, satisfaction with life, defined as the judgmental component of subjective wellbeing, is thought to be a significant predictor of mental and physical health (Diener et al., 1985; Diener, 2012). Furthermore, self-efficacy is regarded as a powerful motivational, cognitive, and affective determinant of university student behavior, with a significant impact on involvement, effort, persistence, self-regulation, and achievement (Schunk and Pajares, 2010; Honicke and Broadbent, 2016; Ritchie, 2016; Zumbrunn et al., 2020). Self-efficacy is an important variable in stress management because of these characteristics (Bandura et al., 2003; Şahin and Çetin, 2017; Lannin et al., 2019), and it is considered as a protective factor against the impact of day-to-day stressors at university (Freire et al., 2018; Schönfeld et al., 2019).
To end up with, the findings of the present study support the notion that a vast repertoire of coping strategies, and flexibility in their selection, may be the best methods to effectively cope with stress and protect university students from decreased wellbeing, during the COVID-19 pandemic (Rogowska et al., 2021a).
The results of this study should be viewed in light of its methodological limitations, which should be addressed in future research. First, the study’s sample was small, with the vast majority of participants being women. Furthermore, the study’s sample only consists of Psychology university students, who are often motivated about the process. In addition, participants volunteered to participate in the survey in response to an online invitation, which may mean that they were actively seeking support in relation to stress. To ensure that the findings are generalizable, future studies should aim to recruit a larger and more diverse sample in terms of gender, age, career, and marital status. Furthermore, participants only completed self-reported scales, which by definition are highly subjective and can be influenced by external factors. In future surveys, interviews could be used to collect qualitative data. Future designs will also benefit from the addition of follow-up measures beyond the 3 months examined in this study to reinforce the findings and investigate the long-term impact of the changes identified following the program’s completion.
In the shadow of COVID-19 pandemic, the findings of this study have important research and clinical implications. To begin with, the material of this program is easily adoptable and implementable by campus-based resources such as health centers, counseling centers, health promotion offices, student affairs staff, and other support services to assist university students in effectively coping with stress and protecting themselves from decreased wellbeing during this period of unprecedented disruption and uncertainty. Moreover, since the material of the “ReStress Mindset” intervention is delivered online, it is easily transferable to other populations and or settings; thus, future research could focus on individuals who are at risk of developing stress-related physical or mental health problems. Finally, considering the effectiveness of the “ReStress Mindset” intervention, mental health practitioners and counseling psychologists may find inspiration for internet-delivered stress mindset interventions during COVID-19 pandemic.
The “ReStress Mindset” intervention resulted in a statistically significant increase in “stress-is-enhancing” mindset (SIEM), life satisfaction, and self-efficacy against stress, as well as a statistically significant decrease in “stress-is-debilitating” mindset (SIDM), with these effects lasting 3 months after the program’s completion. The findings of this study suggest that university students could benefit from the “ReStress Mindset” intervention in order to cultivate and maintain a positive stress mindset and increase their life satisfaction and self-efficacy against stress, even during the COVID-19 pandemic or any other highly stressful period or crisis.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
All authors have contributed equally to the development of the study’s idea, data acquisition, data analysis, and writing of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer KK declared a shared affiliation with several of the authors to the handling editor at the time of review.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Andreou, E., Alexopoulos, E., Lionis, C., Varvogli, L., Gnardellis, C., Chrousos, G., et al. (2011). Perceived stress scale: Reliability and validity study in Greece. Int. J. Environ. Res. Public Health 8, 3287–3298.
Aristovnik, A., Keržič, D., Ravšelj, D., Tomaževič, N., and Umek, L. (2021). Impacts of the Covid-19 pandemic on life of higher education students: Global survey dataset from the first wave. Data Brief 39:107659. doi: 10.1016/j.dib.2021.107659
Bandura, A., Caprara, G. V., Barbaranelli, C., Gerbino, M., and Pastorelli, C. (2003). Role of affective self-regulatory efficacy in diverse spheres of psychosocial functioning. Child Dev. 74, 769–782. doi: 10.1111/1467-8624.00567
Bareeqa, S. B., Ahmed, S. I., Samar, S. S., Yasin, W., Zehra, S., Monese, G. M., et al. (2021). Prevalence of depression, anxiety and stress in china during COVID-19 pandemic: A systematic review with meta-analysis. Int. J. Psychiatry Med. 56, 210–227. doi: 10.1177/0091217420978005
Bayram, N., and Bilgel, N. (2008). The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Psychiatr. Epidemiol. 43, 667–672.
Bewick, B., Koutsopoulou, G., Miles, J., Slaa, E., and Barkham, M. (2010). Changes in undergraduate students’ psychological well-being as they progress through university. Stud. High. Educ. 35, 633–645. doi: 10.1080/03075070903216643
Byrnes, Y. M., Civantos, A. M., Go, B. C., McWilliams, T. L., and Rajasekaran, K. (2020). Effect of the COVID-19 pandemic on medical student career perceptions: A national survey study. Med. Educ. Online 25:1798088. doi: 10.1080/10872981.2020.1798088
Cao, W., Fang, Z., Hou, G., Han, M., Xu, X., Dong, J., et al. (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 287:112934. doi: 10.1016/j.psychres.2020.112934
Cénat, J. M., Blais-Rochette, C., Kokou-Kpolou, C. K., Noorishad, P. G., Mukunzi, J. N., McIntee, S. E., et al. (2021). Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 295:113599. doi: 10.1016/j.psychres.2020.113599
Chen, T., and Lucock, M. (2022). The mental health of university students during the COVID-19 pandemic: An online survey in the UK. PLoS One 17:e0262562. doi: 10.1371/journal.pone.0262562
Cohen, S., Kamarck, T., and Mermelstein, R. (1983). A global measure of perceived stress. J. Health Soc. Behav. 24, 385–396. doi: 10.2307/2136404
Crum, A. J. (2011). Evaluating a mindset training program to unleash the enhancing nature of stress. Acad. Manag. Proc. 1, 1–6. doi: 10.5465/ambpp.2011.65870502
Crum, A. J., Akinola, M., Martin, A., and Fath, S. (2017). The role of stress mindset in shaping cognitive, emotional, and physiological responses to challenging and threatening stress. Anxiety Stress Coping 30, 379–395. doi: 10.1080/10615806.2016.1275585
Crum, A. J., Salovey, P., and Achor, S. (2013). Rethinking stress: The role of mindsets in determining the stress response. J. Pers. Soc. Psychol. 104:716. doi: 10.1037/a0031201
Deng, J., Zhou, F., Hou, W., Silver, Z., Wong, C. Y., Chang, O., et al. (2021). The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 301:113863. doi: 10.1016/j.psychres.2021.113863
Diener, E. (2012). New findings and future directions for subjective well-being research. Am. Psychol. 67, 590–597. doi: 10.1037/a0029541
Diener, E., Emmons, R. A., Larsen, R. J., and Griffin, S. (1985). The satisfaction with life scale. J. Pers. Assess. 49, 71–75. doi: 10.1207/s15327752jpa4901_13
Diener, E., Wirtz, D., Tov, W., Kim-Prieto, C., Choi, D. W., Oishi, S., et al. (2010). New well-being measures: Short scales to assess flourishing and positive and negative feelings. Soc. Indicat. Res. 97, 143–156. doi: 10.1007/s11205-009-9493-y
Dweck, C. (2008). Can personality be changed? The role of beliefs in personality and change. Curr. Direct. Psychol. Sci. 17, 391–394.
Eisenberg, D., Gollust, S. E., Goldberstein, E., and Hefner, J. L. (2007). Prevalence and correlates of depression, anxiety and suicidallity among university students. Am. J. Orthopsychiatry 77, 534–542.
Freire, C., Ferradás, M., Núñez, J. C., Valle, A., and Vallejo, G. (2018). Eudaimonic well-being and coping with stress in university students: The mediating/moderating role of self-efficacy. Int. J. Environ. Res. Public Health 16:48. doi: 10.3390/ijerph16010048
Galanakis, M., Lakioti, A., Pezirkianidis, C., Karakasidou, E., and Stalikas, A. (2017). Reliability and validity of the Satisfaction with Life Scale (SWLS) in a Greek sample. Int. J. Hum. Soc. Stud. 5, 120–127.
Gallagher, R. P. (2012). Thirty years of the national survey of counseling center directors: A personal account. J. College Student Psychother. 26, 172–184. doi: 10.1080/87568225.2012.685852
Giuntella, O., Hyde, K., Saccardo, S., and Sadoff, S. (2021). Lifestyle and mental health disruptions during COVID-19. Proc. Natl. Acad. Sci. U.S.A. 118:e2016632118. doi: 10.1073/pnas.2016632118
Grégoire, S., Lachance, L., Bouffard, T., and Dionne, F. (2018). The use of acceptance and commitment therapy to promote mental health and school engagement in University Students: A multisite randomized controlled trial. Behav. Ther. 49, 360–372. doi: 10.1016/j.beth.2017.10.003
Grubic, N., Badovinac, S., and Johri, A. M. (2020). Student mental health in the midst of the COVID-19 pandemic: A call for further research and immediate solutions. Int. J. Soc. Psychiatry 66, 517–518. doi: 10.1177/0020764020925108
Harrer, M., Adam, S. H., Baumeister, H., Cuijpers, P., Karyotaki, E., Auerbach, R. P., et al. (2019). Internet interventions for mental health in university students: A systematic review and meta-analysis. Int. J. Methods Psychiatr. Res. 28:e1759. doi: 10.1002/mpr.1759
Hayes, S. C., and Hofmann, S. G. (2018). Process-based CBT: The science and core clinical competencies of cognitive behavioral therapy. Oakland, CA: New Harbinger Publications.
Hayes, S. C., Hofmann, S. G., Stanton, C. E., Carpenter, J. K., Sanford, B. T., Curtiss, J. E., et al. (2019). The role of the individual in the coming era of process-based therapy. Behav. Res. Ther. 117, 40–53. doi: 10.1016/j.brat.2018.10.005
Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., and Lillis, J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behav. Res. Ther. 44, 1–25. doi: 10.1016/j.brat.2005.06.006
Hayes, S. C., Villatte, M., Levin, M. E., and Hildebrandt, M. (2011). Open, aware, and active: Contextual approaches as an emerging trend in the behavioral and cognitive therapies. Ann. Rev. Clin. Psychol. 7, 141–168. doi: 10.1146/annurev-clinpsy-032210-104449
Hofmann, S. G., and Hayes, S. C. (2019). The future of intervention science: Process-based therapy. Clin. Psychol. Sci. J. Assoc. Psychol. Sci. 7, 37–50. doi: 10.1177/2167702618772296
Hofmann, S. G., Hayes, S. C., and Lorscheid, D. N. (2021). Learning process-based therapy: A skills training manual for targeting the core processes of psychological change in clinical practice. Oakland, CA: New Harbinger Publications.
Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., et al. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 7, 547–560. doi: 10.1016/S2215-0366(20)30168-1
Honicke, T., and Broadbent, J. (2016). The influence of academic self-efficacy on academic performance: A systematic review. Educ. Res. Rev. 17, 63–84.
Jamieson, J. P., Mendes, W. B., and Nock, M. K. (2013). Improving acute stress responses: The power of reappraisal. Curr. Direct. Psychol. Sci. 22, 51–56. doi: 10.1177/0963721412461500
Kapasia, N., Paul, P., Roy, A., Saha, J., Zaveri, A., Mallick, R., et al. (2020). Impact of lockdown on learning status of undergraduate and postgraduate students during COVID-19 pandemic in West Bengal. India. Child. Youth Serv. Rev. 116:105194. doi: 10.1016/j.childyouth.2020.105194
Karampas, K., Pezirkianidis, C., and Stalikas, A. (2020). Psychometric Properties of the Stress Mindset Measure (SMM) in a Greek Sample. Psychology 11, 1185–1199. doi: 10.4236/psych.2020.118079
Karampas, K., Pezirkianidis, C., and Stalikas, A. (2022). “Combining stress mindset training with acceptance and commitment therapy (ACT): An internetdelivered intervention for emerging adults during the pandemic,” in Emerging adulthood in the COVID-19 pandemic and other crises: individual and relational resources: Cross-cultural advancements in positive psychology (Cham: Springer Nature).
Kashdan, T. B., and Rottenberg, J. (2010). Psychological flexibility as a fundamental aspect of health. Clin. Psychol. Rev. 30, 865–878. doi: 10.1016/j.cpr.2010.03.001
Kilby, C. J., and Sherman, K. A. (2016). Delineating the relationship between stress mindset and primary appraisals: Preliminary Findings. Springerplus 15, 188–336. doi: 10.1186/s40064-016-1937-7
Kocovski, N. L., Fleming, J. E., Hawley, L. L., Huta, V., and Antony, M. M. (2013). Mindfulness and acceptance-based group therapy versus traditional cognitive behavioral group therapy for social anxiety disorder: A randomized controlled trial. Behav. Res. Ther. 51, 889–898. doi: 10.1016/j.brat.2013.10.007
Kornilaki, E. N. (2022). The psychological effect of COVID-19 quarantine on Greek young adults: Risk factors and the protective role of daily routine and altruism. Int. J. Psychol. 57, 33–42. doi: 10.1002/ijop.12767
Kyriazos, T. A., Stalikas, A., Prassa, K., and Yotsidi, V. (2018a). Can the depression anxiety stress scales short be shorter? Factor structure and measurement invariance of DASS-21 and DASS-9 in a Greek, non-clinical sample. Psychology 9, 1095–1127. doi: 10.4236/psych.2018.95069
Kyriazos, T. A., Stalikas, A., Prassa, K., and Yotsidi, V. (2018b). A 3-faced construct validation and a bifactor subjective well-being model using the scale of positive and negative experience. Greek Version. Psychology 9, 1143–1175. doi: 10.4236/psych.2018.95071
Lannin, D. G., Guyll, M., Cornish, M., Vogel, D. L., and Madon, S. (2019). The importance of counseling self-efficacy: Physiologic stress in student helpers. J. College Stud. Psychother. 33, 14–24.
Lazarus, R. S., and Folkman, S. (1984). Stress, appraisal, and coping. New York, NY: Springer Pub. Co.
Lederer, A. M., Hoban, M. T., Lipson, S. K., Zhou, S., and Eisenberg, D. (2021). More than inconvenienced: The Unique Needs of U.S. College Students During the COVID-19 Pandemic. Health Educ. Behav. 48, 14–19. doi: 10.1177/1090198120969372
Levin, M. E., Haeger, J., Pierce, B., and Twohig, M. P. (2017). Web-based acceptance and commitment therapy for mental health problems in college students: A randomized controlled trial. Behav. Modif. 41, 141–162. doi: 10.1177/0145445516659645
Levy, B. R., and Myers, L. M. (2004). Preventive health behaviors influenced by self-perceptions of aging. Prev. Med. 39, 625–629. doi: 10.1016/j.ypmed.2004.02.029
Li, S. W., Wang, Y., Yang, Y. Y., Lei, X. M., and Yang, Y. F. (2020). Analysis of influencing factors of anxiety and emotional disorders in children and adolescents during home isolation during the epidemic of novel coronavirus pneumonia. Chinese J. Child Health, 28, 1–9.
Lipson, S. K., Kern, A., Eisenberg, D., and Breland-Noble, A. M. (2018). Mental health disparities among college students of color. J. Adolesc. Health 63, 348–356. doi: 10.1016/j.jadohealth.2018.04.014
Liu, C. H., Zhang, E., Wong, G., Hyun, S., and Hahm, H. C. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 290:113172. doi: 10.1016/j.psychres.2020.113172
Lovibond, S. H., and Lovibond, P. F. (1995). The structure of negative emotional States: Comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav. Res. Ther. 33, 335–343. doi: 10.1016/0005-7967(94)00075-U
Ma, Z., Zhao, J., Li, Y., Chen, D., Wang, T., Zhang, Z., et al. (2020). Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 29:e181. doi: 10.1017/S2045796020000931
McGinty, E. E., Presskreischer, R., Han, H., and Barry, C. L. (2020). Psychological distress and loneliness reported by US Adults in 2018 and April 2020. JAMA 324, 93–94. doi: 10.1001/jama.2020.9740
Nochaiwong, S., Ruengorn, C., Thavorn, K., Hutton, B., Awiphan, R., Phosuya, C., et al. (2021). Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: A systematic review and meta-analysis. Sci. Rep. 11:10173. doi: 10.1038/s41598-021-89700-8
O’Connor, D. B., Thayer, J. F., and Vedhara, K. (2021). Stress and health: A review of psychobiological processes. Ann. Rev. Psychol. 72, 663–688. doi: 10.1146/annurev-psych-062520-122331
Pezirkianidis, C., Karakasidou, E., Lakioti, A., Stalikas, A., and Galanakis, M. (2018). psychometric properties of the depression, anxiety, stress scales-21 (DASS-21) in a Greek Sample. Psychology 9, 2933–2950.
Polk, K. L., and Schoendorff, B. (2014). The ACT Matrix: A new approach to building psychological flexibility across settings and populations. Oakland, CA: New Harbinger Publications.
Ritchie, L. (2016). Fostering self-efficacy in higher education students. London: Palgrave MacMillan.
Rogowska, A. M., Kuśnierz, C., and Ochnik, D. (2021a). Changes in stress, coping styles, and life satisfaction between the first and second waves of the COVID-19 Pandemic: A longitudinal cross-lagged study in a sample of University Students. J. Clin. Med. 10:4025. doi: 10.3390/jcm10174025
Rogowska, A. M., Ochnik, D., Kuśnierz, C., Chilicka, K., Jakubiak, M., Paradowska, M., et al. (2021b). Changes in mental health during three waves of the COVID-19 pandemic: A repeated cross-sectional study among polish university students. BMC Psychiatry 21:627. doi: 10.1186/s12888-021-03615-2
Ryerson, N. C. (2022). Behavioral and Psychological Correlates of Well-Being during COVID-19. Psychol. Rep. 125, 200–217. doi: 10.1177/0033294120978160
Şahin, F., and Çetin, F. (2017). The mediating role of general self-efficacy in the relationship between the big five personality traits and perceived stress: A weekly assessment study. Psychol. Stud. 62, 35–46. doi: 10.1007/s12646-016-0382-6
Schönfeld, P., Brailovskaia, J., Zhang, X. C., and Margraf, J. (2019). Self-efficacy as a mechanism linking daily stress to mental health in students: A three-wave cross-lagged study. Psychol. Rep. 122, 2074–2095. doi: 10.1177/0033294118787496
Schunk, D., and Pajares, F. (2010). “Self-efficacy beliefs,” in International encyclopedia of education, 3rd Edn, eds P. Peterson, E. Baker, and B. McGaw (Amsterdam: Elsevier), 668–672.
Tang, W., Hu, T., Hu, B., Jin, C., Wang, G., Xie, C., et al. (2020). Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disorder. 274, 1–7. doi: 10.1016/j.jad.2020.05.009
World Health Organization [WHO] (2020). Mental health and psychosocial considerations during the COVID-19 outbreak. Geneva: World Health Organization.
Yusoff, M. S. B. (2013). Psychometric properties of the Depression Anxiety Stress Scale in a sample of medical degree applicants. Int. Med. J. 20, 295–300.
Zumbrunn, S., Broda, M., Varier, D., and Conklin, S. (2020). Examining the multidimensional role of self-efficacy for writing on student writing self-regulation and grades in elementary and high school. Br. J. Educ. Psychol. 90, 580–603. doi: 10.1111/bjep.12315
Keywords: stress, stress mindset, Acceptance and Commitment Therapy, internet-delivered interventions, university students stress, university students
Citation: Karampas K, Pezirkianidis C and Stalikas A (2022) ReStress mindset: An internet-delivered intervention that changes university students’ mindset about stress in the shadow of the COVID-19 pandemic. Front. Psychol. 13:1036564. doi: 10.3389/fpsyg.2022.1036564
Received: 04 September 2022; Accepted: 10 October 2022;
Published: 26 October 2022.
Edited by:
Claude-Hélène Mayer, University of Johannesburg, South AfricaReviewed by:
Katerina Kotsoni, Panteion University, GreeceCopyright © 2022 Karampas, Pezirkianidis and Stalikas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Konstantinos Karampas, a2FyYWJhc2tvbnN0YW50aW5vc0BnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.