- 1Department of Cardiology, Lanzhou University Second Hospital, Lanzhou, China
- 2Evidence-Based Medicine Center of Lanzhou University, Lanzhou, China
Since the pandemic of the novel 2019 coronavirus disease (COVID-19), in addition to the harm caused by the disease itself, the psychological damage caused to the public by the pandemic is also a serious problem. The aim of our study was to summarize the systematic reviews/meta-analyses (SRs/MAs) of the prevalence of anxiety, depression and insomnia in different populations during the COVID-19 pandemic and to qualitatively evaluate these SRs/MAs. We searched the Cochrane Library, PubMed and Web of Science to obtain SRs/MAs related to anxiety, depression, and insomnia in different populations during the COVID-19 pandemic. The main populations we studied were healthcare workers (HCWs), college students (CSs), COVID-19 patients (CPs), and the general populations (GPs). A subgroup analysis was performed of the prevalence of psychological disorders. A total of 42 SRs/MAs (8,200,330 participants) were included in calculating and assessing the prevalence of anxiety, depression, and insomnia in these populations. The results of subgroup analysis showed that the prevalence of anxiety in different populations were: HCWs (20–44%), CSs (24–41%), CPs (15–47%), and GPs (22–38%). The prevalence of depression were: HCWs (22–38%), CSs (22–52%), CPs (38–45%), and GPs (16–35%), statistically significant differences between subgroups (p < 0.05). The prevalence of insomnia were: HCWs (28–45%), CSs (27–33%), CPs (34–48%), and GPs (28–35%), statistically significant differences between subgroups (p < 0.05). The comparison revealed a higher prevalence of psychological disorders in the CP group, with insomnia being the most pronounced. The methodological quality of the included SRs/MAs was then evaluated using AMSTAR 2 tool. The results of the methodological quality evaluation showed that 13 SRs/MAs were rated “medium,” 13 were rated “low,” and 16 were rated “very low.” Through the subgroup analysis and evaluation of methodological quality, we found a higher prevalence of insomnia than anxiety and depression among the psychological disorders occurring in different populations during the pandemic, but the sample size on insomnia is small and more high-quality studies are needed to complement our findings.
Introduction
Since the outbreak of the COVID-19 pandemic in December 2019, the suddenness of the COVID-19 pandemic and the lack of effective preventive measures at the beginning has led to the rapid spread of the pandemic worldwide, and by the end of Jun 2022, the COVID-19 pandemic outbreak has caused about 50 million infections and 6 million deaths in more than 200 countries worldwide, resulting in incalculable human casualties and economic losses. As a result, the enormous toll of the COVID-19 pandemic has led to a significant increase in the incidence of psychological disorders in different segments of society, the most common of which are anxiety, depression, and insomnia (Bao et al., 2020). Psychological disorders occur mainly in healthcare workers (HCWs), college students (CSs), COVID-19 patients (CPs), and the general populations (GPs), who are also the groups more severely affected by the pandemic (Alsubaie et al., 2019; Chen Q. et al., 2020; Pfefferbaum and North, 2020; Wang C. et al., 2020; Zhang et al., 2020).
The fact that the CPs are already infected themselves, coupled with the increasing number of deaths each day, has led to anxiety for their lives and panic, coupled with being in quarantine and isolated from the outside world, creating a severe sense of isolation (Alsubaie et al., 2019). The large number of casualties caused by the pandemic has increased the burden and psychological stress on HCWs. In addition, many HCWs have unfortunately also been infected due to prolonged close contact with the CPs (Wang J. et al., 2020). It has been reported that more than 17,000 HCWs have died from COVID-19 (Huang et al., 2020; Wu et al., 2020). The prolonged pandemic has also caused serious psychological disorders among CSs. The lack of knowledge about the pandemic and excessive attention to internet information has increased anxiety and depression among some students, in addition to the lack of physical exercise and long hours of screen study, with senior students worrying about their graduation (Han et al., 2020). Since most factories and companies and other related places cannot function normally during the pandemic, a large number of people are isolated from home of economic resources and lack normal social communication, they are prone to psychological disorders. In addition, the shortage of food with high prices caused severe anxiety and depression in the minds of the people (Kawohl and Nordt, 2020; Lone and Ahmad, 2020; Browning et al., 2021).
For the above, there have been many systematic reviews/meta-analyses (SRs/MAs) incorporating different cross-sectional studies to calculate the prevalence of some common psychological disorders in different populations during the pandemic, especially the pooled prevalence of anxiety, depression, and insomnia. There are many SRs/MAs on the majority of anxiety, depression, and insomnia in different populations during the COVID-19 pandemic, but these reviews differ in quality and design. Therefore, it is needed to assess the methodological quality of these SRs/MAs, summarize the evidence for the important outcomes included in the SRs/MAs, state the conclusions of these SRs/MAs and combine these results to produce more accurate data for a large sample size.
Materials and methods
Sources of literature and search strategy
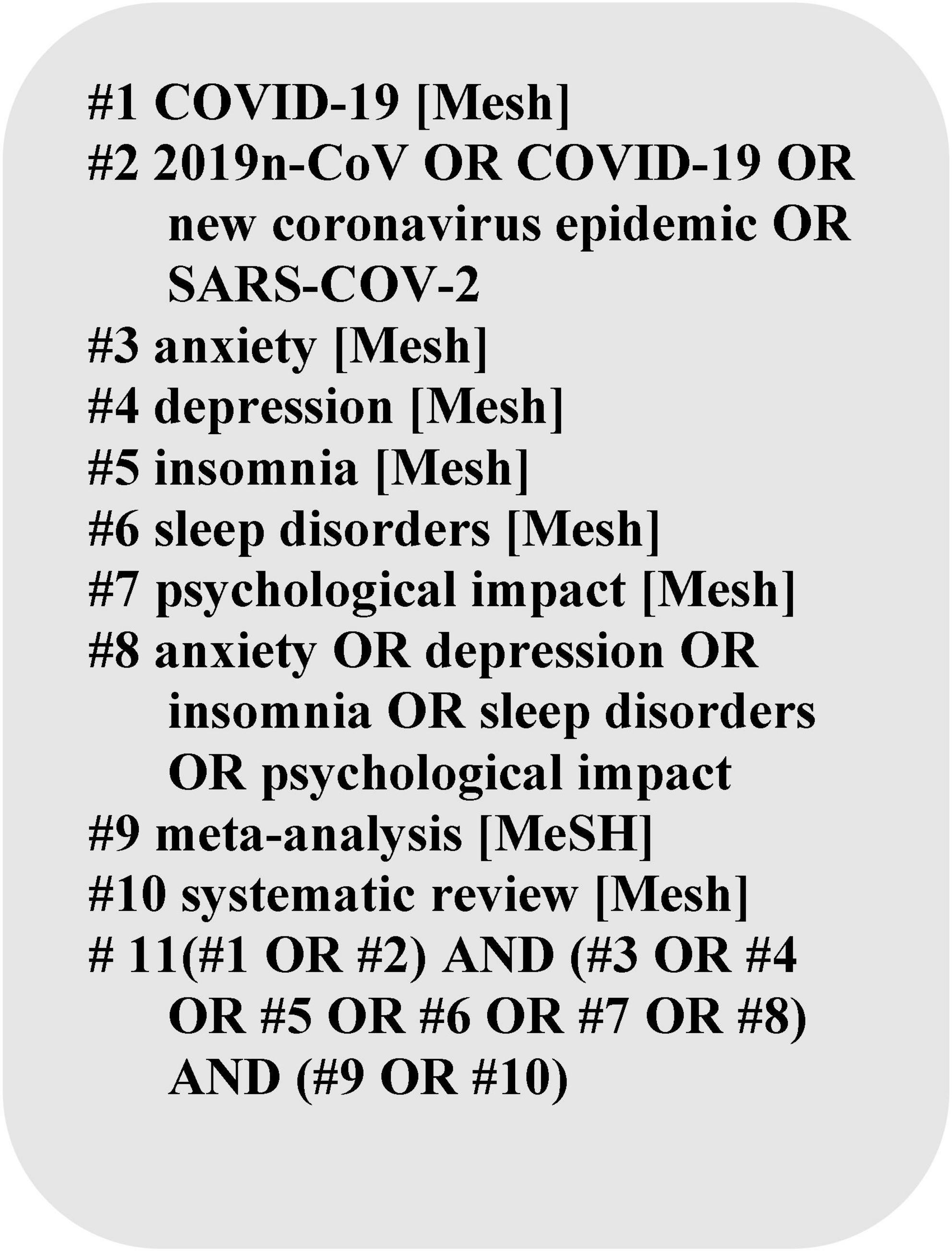
To identify the included literature, we searched for SRs/MAs published in the Cochrane Library, PubMed and Web of Science from December 2019 to June 2022 related to our study topic, without applying any language restrictions and the search terms included all identified keywords (“2019n-CoV,” “new coronavirus pandemic,” “COVID-19,” “anxiety,” “depression,” “insomnia,” “sleep disorders,” “psychological impact”) and adjusted for each database. The detailed search strategy is shown in Figure 1.
Inclusion and exclusion criteria
Systematic reviews/MAs were included if they met the following criteria: (1) published since the outbreak of COVID-19 in December 2019. (2) the studies included in the report involved study populations that experienced the COVID-19 pandemic. (3) the determination of anxiety, depression, and insomnia in the study populations included in the report was subject to the use of an authoritative assessment tool for psychological disorders. (4) the prevalence of anxiety, depression, or insomnia in the study population was provided. (5) the type of studies included in the report were cross-sectional studies. (6) The type of publication of the literature is systematic reviews/meta-analyses. We excluded literature reviews that (1) used informal and subjective methods to collect and interpret evidence, reviews, and non-peer reviews; and (2) our study population did not include pregnant mothers, chronic patients, elderly and children, so these populations were excluded from the study.
Study selection
All the retrieved literature was imported into NoteExpress software to identify and remove duplicate studies. Then the titles and abstracts of the papers were browsed to initially exclude literature that was far from the purpose of our research. Two evaluators (QZ and YT) then independently read and evaluated the full articles. Those that did not meet the pre-determined inclusion criteria were excluded, with a third evaluator (SS) making the determination when no agreement could be reached on any of them.
Data extraction
Two evaluators (CJ and PL) independently extracted data from the included reports based on a pre-designed Excel spreadsheet for quality assessment and data analysis. The data extraction spreadsheet summarized key characteristics: (1) year of publication and authors; (2) number of included studies; (3) total sample size; (4) outcome indicators and prevalence; (5) quality assessment tools; and (6) journal of publication. When agreement could not be reached on data from the literature, a third evaluator (SS) made the determination. When necessary, additional information was obtained from the original cross-sectional study reports.
Methodological quality assessment
The methodological quality of the included studies was independently evaluated by two evaluators using the AMSTAR 2 tool (Shea et al., 2017). The tool contains 16 entries, of which entries 2, 4, 7, 9, 11, 13, and 15 are vital entries, and the results were classified into 3 levels “satisfied,” “partially satisfied,” and “not satisfied.” AMSTAR 2 tools of satisfied and partially satisfied ≥70% were considered to be more complete for entry reporting. AMSTAR 2 Scoring Quality Levels. See Supplementary Table 1 for definitions of quality levels.
Managing overlapping systematic reviews
Some SRs/MAs may have repeatedly included the same study when discussing the same or similar topics. Multiple inclusion of the same study can lead to biased outcome data. Therefore, when conducting evidence summaries, these repeatedly included studies can have a greater impact on our primary outcomes. According to Cochrane’s guidance (Higgins et al., 2020), results from all relevant studies should be included if the purpose of the overview is to present and describe the current body of evidence on a topic, so we did not exclude overlapping systematic reviews. However, to avoid greater bias in the final results, we presented the results of the included SRs/MAs using only forest plots and did not pool the results.
Statistical analysis
To investigate the prevalence of anxiety, depression, and insomnia worldwide during the COVID-19 pandemic, we divided the target population into four subgroups (HCWs, CSs, CPs, GPs) and analyzed the prevalence of anxiety, depression, and insomnia in each subgroup. Meta-analysis was performed using Revman 5.4 software, with prevalence and its 95% CI as statistical effect measures. Heterogeneity among the included studies was analyzed using the χ2 test (test level α = 0.1), while the magnitude of heterogeneity was quantified by combining I2. When I2 > 50% or p < 0.10, a random-effects model was used, otherwise a fixed-effects model was used. To evaluate the robustness of the results of group comparisons, we performed statistical tests on the results of group comparisons, suggesting statistically significant differences when the p < 0.05. Microsoft Excel 2018 was used to record the relevant data and bubble plot of the results of the methodological quality assessment of the literature. We used percentages to describe the prevalence of psychological disorders.
Results
Study identification
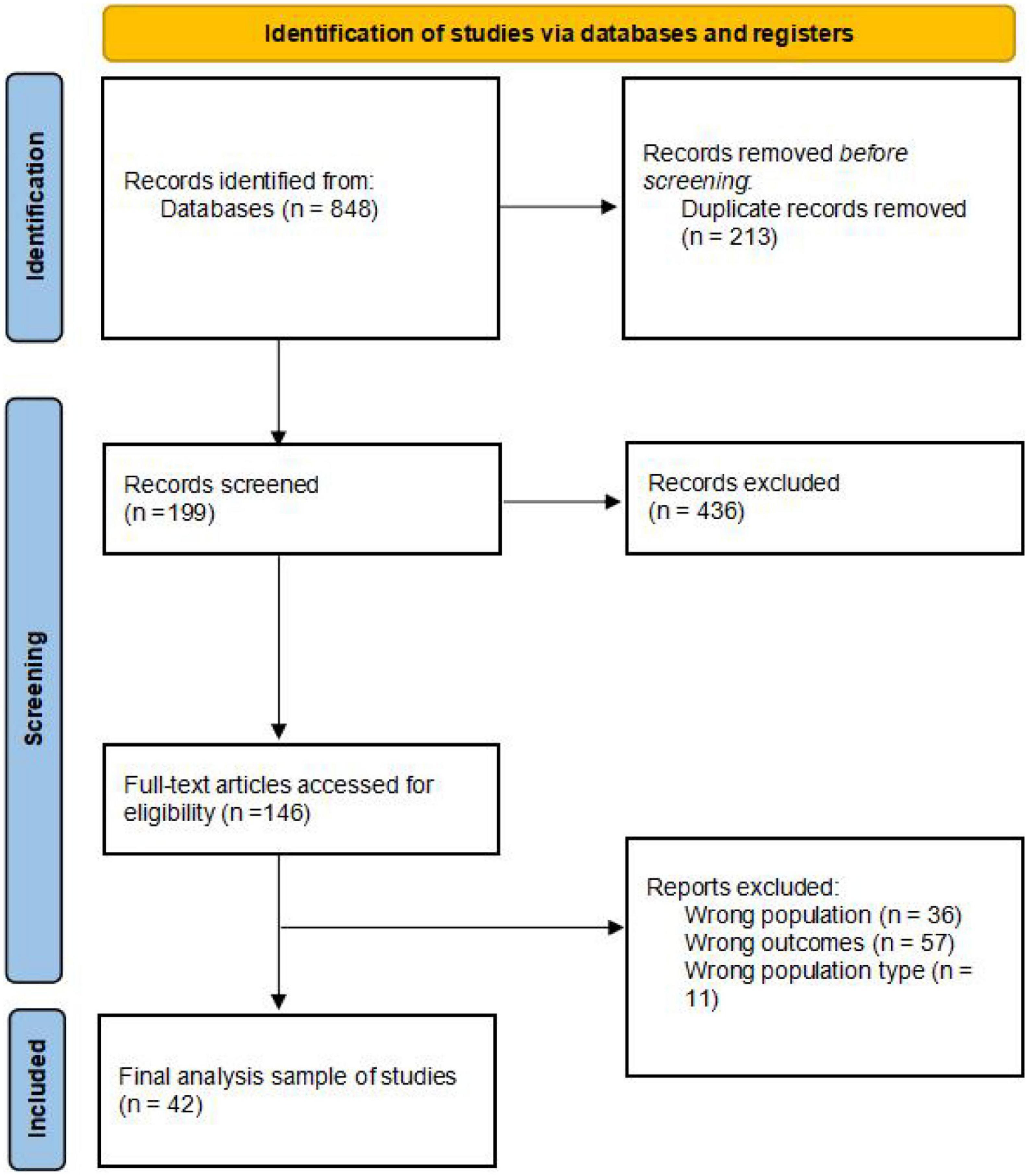
A total of 848 records were identified with our search. Of these, 635 were screened after the removal of duplicates. After screening titles and abstracts, 436 records were excluded. The full text of the remaining 199 records was retrieved for further scrutiny. Of these, 157 were excluded because they did not fulfill the eligibility criteria. Finally, 42 SRs/MAs ere included in this overview. The study selection process is summarized in Figure 2.
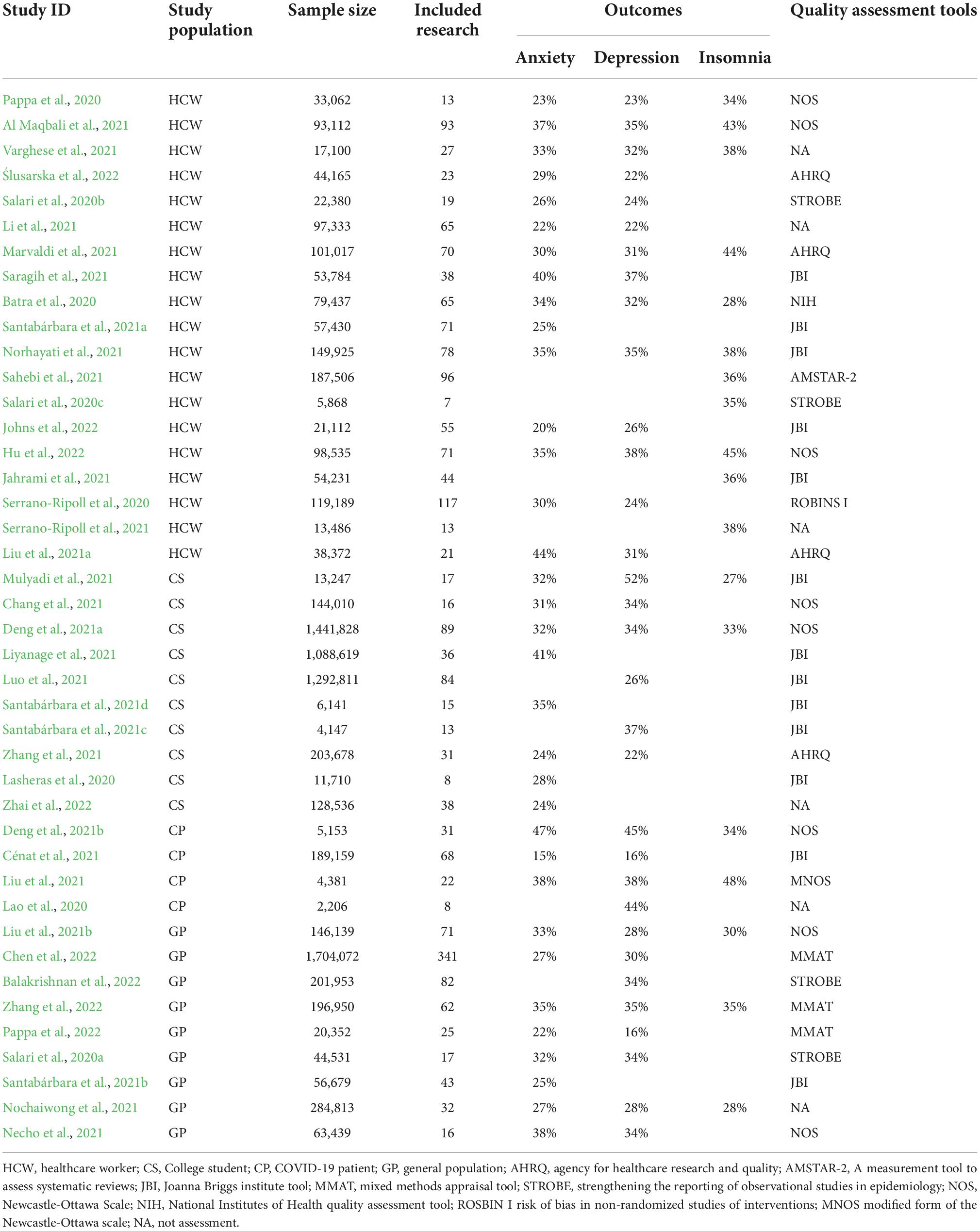
Characteristics of included systematic reviews/meta-analyses
Table 1 summarizes the general characteristics of the 42 SRs/MAs included (year of publication and authors, number of included studies, total sample size, outcome indicators and prevalence, quality assessment tools, and journal of publication). A total of 40 of the SRs/MAs were published in English and the remaining two were in Chinese. Of these 42 SRs/MAs, 19 were reported by HCWs, 10 by CSs, four by CPs and nine by the GPs. Among the 42 SRs/MAs, 36 used quality assessment tools, of which JBI was the most common assessment tool, with five SRs/MAs using AHRQ, followed by one using AMSTAR-2, 12 using JBI, three using MMAT, one using MNOS, eight using NOS, one using ROBINS I, and four using STROBE. The outcome indicators observed in our study were mainly anxiety, depression and insomnia, and not all SRs/MAs included contained these three indicators. There were 34 SRs/MAs on anxiety, with a total of 6,028,108 samples reporting a comorbidity of anxiety, 31 on depression, with a total of 6,200,110 samples reporting a comorbidity of depression, and 18 on insomnia, with a total of 492,314 samples reporting a comorbidity of insomnia.
The methodological quality of included systematic reviews/meta-analyses
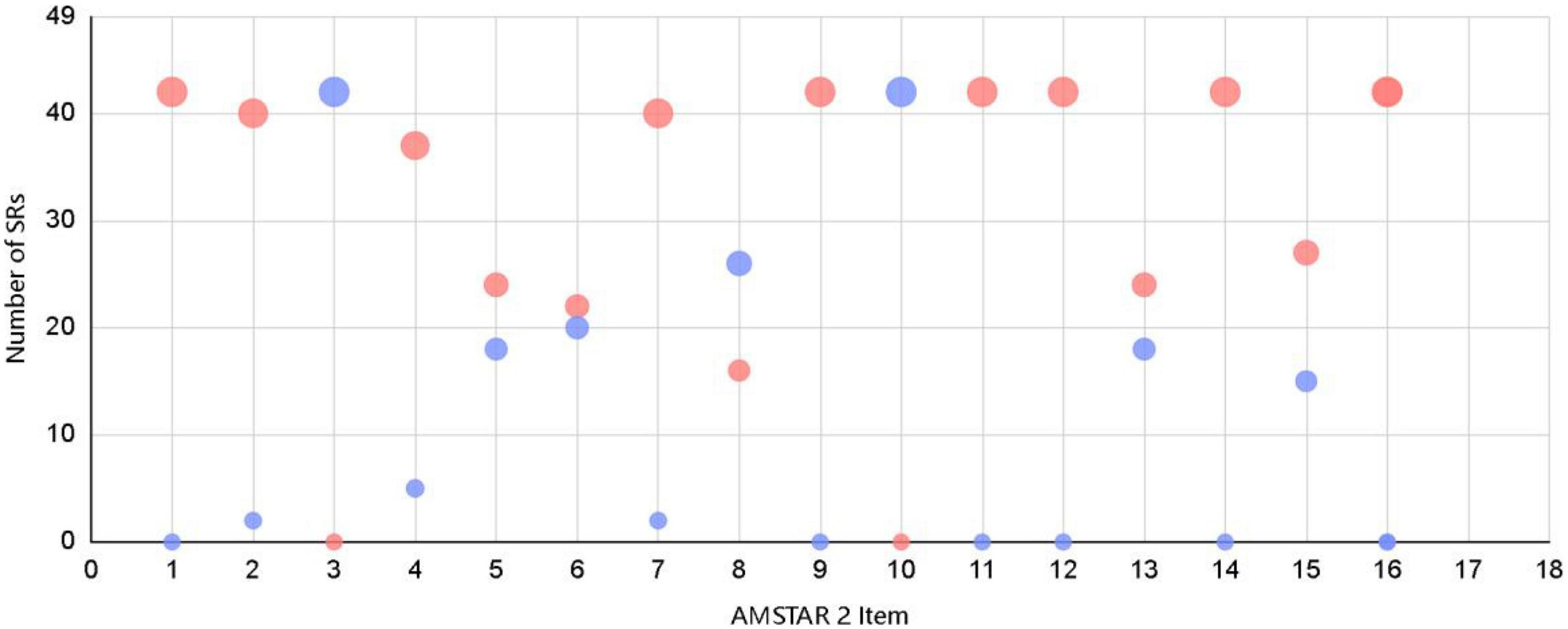
The methodological quality of the 42 SRs/MAs included in the overview was evaluated using the AMSTAR 2 tool and the results are presented in the Table 2. the median AMSTAR 2 score was 11. of these 42 SRs/MAs, a total of 13 SRs/MAs met and partially met ≥70% of the entries, indicating high quality. For each entry of the AMSTAR 2 tool, the satisfaction was: item 1 (42/42, 100%), item 2 (40/42, 95.2%), item 3 (0/42, 0%), item 4 (37/42, 88.1%), item 5 (24/42, 57.1%), item 6 (22/42, 52.4%), item 7 (40/42, 95.2%), item 8 (16/42, 38.1%), item 9 (42/42, 100%), item 10 (0/42, 0%), item 11 (42/42, 100%), item 12 (42/42, 100%), item 13 (24/42, 57.1%), item 14 (42/42, 100%), item 15 (27/42, 64.3%), item 16 (42/42, 100%). The methodological quality of each SRs/MAs varied greatly and had some limitations. Among them, items 1, 9, 11, 12, 14, and 16 could be satisfied in each report. However, items 3 and 10 were poorly satisfied. The rest of the items were satisfied to vary degrees per SRs/MAs. Thirteen SRs/MAs were rated as “medium” for methodological quality, 13 were rated as “low,” and 16 were rated as “very low.” Subsequently, we visualized the quality assessment results using bubble plot (see Figure 3).
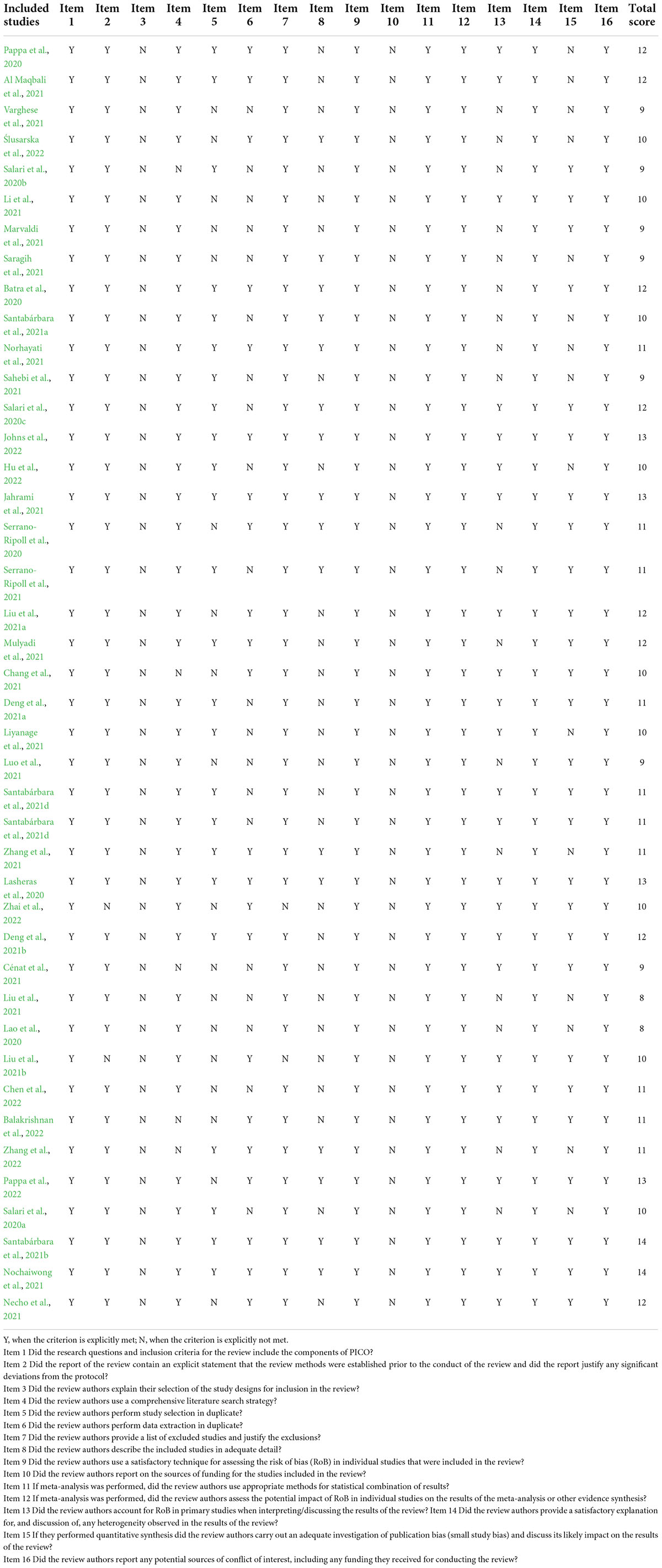
Table 2. A measurement tool to assess systematic reviews (AMSTAR 2) score for methodological quality of included systematic reviews.
Subgroup analysis of psychological disorder symptoms
Anxiety
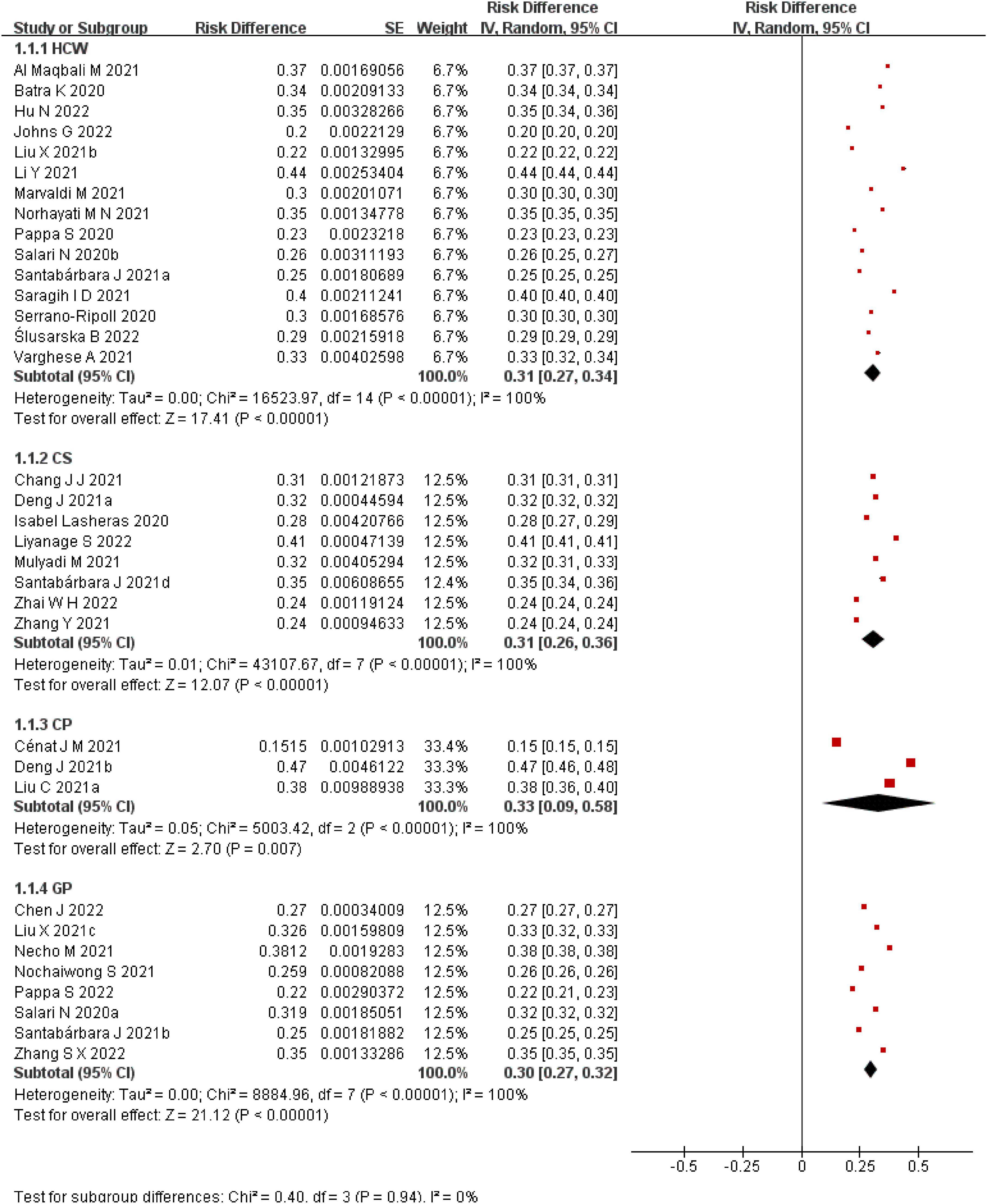
A total of 34 SRs/MAs on the prevalence of anxiety are available. The prevalence of anxiety in different populations during the COVID-19 pandemic is analyzed in this overview (see Figure 4). Significance tests of the results of the group comparisons revealed no statistically significant differences (p = 0.94). In the HCWs population, the results of 15 SRs/MAs were summarized and the interval of anxiety prevalence was found to be 20–44%, among which Batra et al. (2020), Liu et al. (2021a) and Saragih et al. (2021) reported significantly higher prevalence of anxiety in HCWs than others. Liu et al. (2021a) study subjects were all from the sentinel hospital (a hospital that concentrates mainly on treating CPs), and the work pressure of HCWs in this hospital was higher, resulting in a higher prevalence of anxiety. In the CSs group, a summary of eight reports found a prevalence range of 24–41%. In the CPs cohort, three reports had a prevalence range of 15–47%, and the results of these three reports differed significantly. The meta-analysis of Deng et al. (2021b) had a high AMSTAR 2 score and high confidence in the outcome. the reports of Cénat et al. (2021) and Liu et al. (2021) were “very low” quality studies in terms of methodological quality assessment and both reports had problems with literature search, data extraction and publication bias, resulting in low credibility of the final results. In the GPs population, a summary of the results of eight SRs/MAs found a prevalence range of 22–38%.
Depression
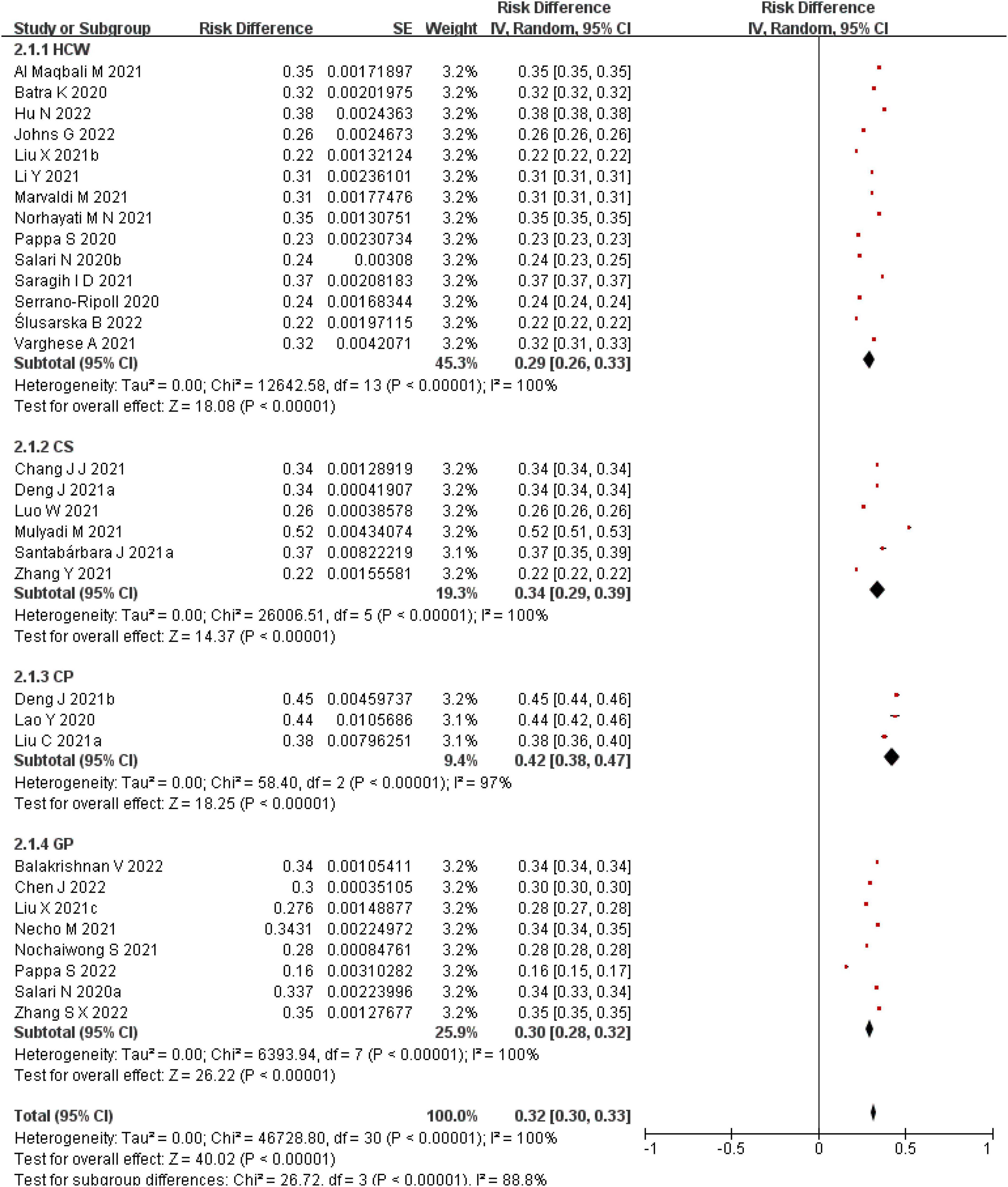
A total of 30 SRs/MAs on the prevalence of depression are presented in this overview to analyze the prevalence of depression in different populations during the COVID-19 pandemic (see Figure 5). The results of the comparison between groups were statistically significantly different (p < 0.05). In the HCWs group, the results of 14 SRs/MAs were summarized and the range of depression prevalence was found to be 22–38%. In the CSs group, summarizing the results of six SRs/MAs found a depression prevalence interval of 22–52%. The results of the meta-analysis by Mulyadi et al. (2021) differed from the others, but the study had a better qualitative assessment and higher confidence. We analyzed the reason for this and found that unlike others the study was conducted with all nursing medical students. The authors of this article explain that nursing students had a high prevalence of depression before the COVID-19 pandemic, probably due to educational and family factors, and that there was a significant increase in prevalence during the pandemic. The intervals of depression prevalence were 38–45% and 16–35% in the CPs and GPs groups, respectively.
Insomnia
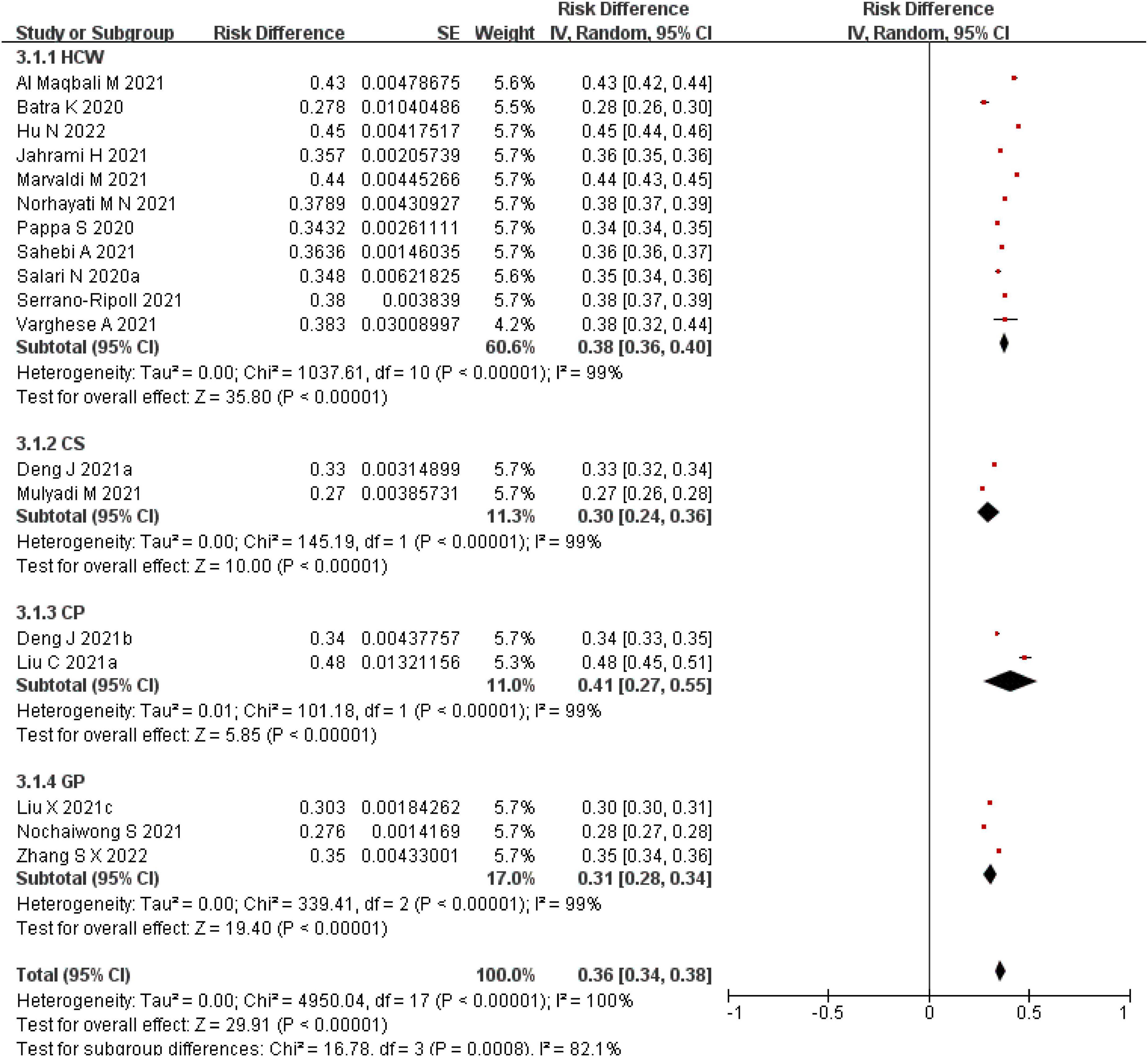
There were 18 SRs/MAs on the prevalence of insomnia in different groups (HCWs, CSs, CPs, GPs). The results of the comparison between groups were statistically significantly different (p < 0.05). Summary results found that the intervals of insomnia prevalence were 28–45%, 27–33%, 34–48%, 28–35%, respectively (see Figure 6).
Discussion
Statement of main findings
The prevalence of psychological disorders in various populations increased significantly during the COVID-19 pandemic (Pfefferbaum and North, 2020), and the purpose of this review was to assess the methodological quality of the SRs/MAs and to provide an description of the occurrence of anxiety, depression, and insomnia in different populations. We performed a meta-analysis of the prevalence of anxiety, depression and insomnia in the target study population. We found that the prevalence of anxiety in the different subgroups were: HCWs (20–44%), CSs (24–41%), CPs (15–47%), and GPs (22–38%), but there were no statistically significant differences between this subgroup comparison (p = 0.94). The prevalence of depression were: HCWs (22–38%), CSs (22–52%), CPs (38–45%), and GPs (16–35%). Our results show that the prevalence of depression is higher in CPs and CSs than in the rest of the population, with a statistically significant difference in the comparison between this subgroup (p < 0.05). We need to pay extra attention to the mental health problems of CSs. Chen et al. argued that adolescents are immature and belong to a vulnerable group, and that CSs are prone to depressive symptoms and subsequent development of depression after the outbreak of the new crown pandemic, when they spend long periods of time taking courses online and doing related activities indoors, and this change in lifestyle and the threat of possible infection (Chen F. et al., 2020). In terms of insomnia-related prevalence, the results for the different subgroups were: HCWs (28–45%), CSs (27–33%), CPs (34–48%), and GPs (28–35%), with statistically significant differences (p < 0.05). We then tested the heterogeneity of the included studies, first using a fixed-effects model for heterogeneity, and the results showed (I2 > 50%) a large heterogeneity among studies, and then we changed to a random-effects model, where the same heterogeneity existed. This may be due to the fact that the included SRs/MAs were from studies conducted by scholars in various countries around the world, and since the pandemic was global in nature, the raw data for the included SRs/MAs were from different countries and regions. The severity of the epidemic and prevention and control measures vary from country to country, resulting in differences in the prevalence of mental illness in the population, so there is a high degree of heterogeneity among studies. However, the purpose of our study was to summarize the prevalence of anxiety, depression, and insomnia in key populations worldwide during the COVID-19 pandemic, so the presence of heterogeneity was unavoidable for our study purpose and did not substantially affect our study purpose. For the results of inter-group comparison of insomnia prevalence, we found that patients with COVID-19 were the population with the highest occurrence of psychological disorders, and sleep disorders continued to be the most common psychological disorder in patients with COVID-19, possibly due to the core symptoms of COVID-19 including cough, fever and dyspnea, all of which are associated with sleep problems (Ferrando et al., 2016; Huang et al., 2020). It has been suggested that the higher risk of sleep problems in CPs may also be attributable to physical pain and side effects of medications used to treat the virus (Shi et al., 2020). The overall analysis showed that the prevalence of insomnia was the highest, and a previous meta-analysis showed that the bulk of sleep disorders in the GP was only 15% during non-COVID-19 pandemics (Cao et al., 2017). It has been suggested that the reason why insomnia is more common is because of the potential bidirectional relationship between sleep and psychiatric co-morbidities, especially when more co-morbidities are present (e.g., anxiety and depression), which suggests that sleep specialists treating this suggests that sleep specialists should consider psychiatric co-morbidities when treating sleep problems, and vice versa (Jahrami et al., 2021).
Our results indicate that insomnia-related symptoms were more common in different populations during the new crown epidemic relative to anxiety and depression. A previous meta-analysis showed that the bulk of sleep disorders in the GP was only 15% during non-COVID-19 pandemics (Cao et al., 2017). It has been suggested that the reason why insomnia is more common is because of the potential bidirectional relationship between sleep and psychiatric co-morbidities, especially when more co-morbidities are present (e.g., anxiety and depression), which suggests that sleep specialists treating this suggests that sleep specialists should consider psychiatric co-morbidities when treating sleep problems, and vice versa (Jahrami et al., 2021). In addition, due to the lack of knowledge about the COVID-19 and the huge lethality caused by the lack of effective treatment measures at the beginning of the pandemic, patients with the COVID-19 are filled with internal panic and fear for their lives (Gyasi, 2020), the lack of contact with the outside world during isolation or hospitalization, which makes them more likely to suffer from loneliness, anxiety and depression, and even suicidal thoughts (Kawohl and Nordt, 2020; Luchetti et al., 2020; Pappa et al., 2020; Varghese et al., 2021). The prevalence of psychological disorders among HCWs is also higher, probably due to the huge workload during the pandemic, the enormous psychological pressure on HCWs, coupled with the fear of being infected by contact with CPs, as well as the need for a series of measures such as isolation when leaving the hospital, creating a very obvious psychological barrier for HCWs (Pappa et al., 2020; Al Maqbali et al., 2021; Marvaldi et al., 2021; Saragih et al., 2021; Varghese et al., 2021).
Methodological quality of systematic reviews
In terms of methodological quality, of the 42 SRs/MAs included, 16 were of very low-quality, the rest were of low-quality and moderate-quality, and there was no high-quality SRs/MAs. Problems were more pronounced in three areas: (1) The inclusion criteria for the type of study were not specified, only the inclusion of cross-sectional studies was described, and the reasons for the inclusion of study types were not explained; and (2) All studies only described the reasons for exclusion of literature without providing a detailed list of excluded literature; Also for the very low quality 16 SRs/MAs, the problems were mainly related to the impact on the risk of bias not being explained in the discussion. These results suggest that the current SRs/MAs exploring the incidence of anxiety, depression, and insomnia in different populations during the pandemic generally follow the reporting norms. However, the methodological quality needs to be improved, and researchers still lack attention in explaining the type of study design, providing a list of excluded literature, and the reasons and sources of funding.
Strengths and limitations
This overview is the first study to assess the quality of evidence on the incidence of anxiety, depression, and insomnia in different populations during the COVID-19 pandemic using AMSTAR 2 tools. However, our study has some limitations. First, in this review, we included only SRs/MAs, while primary studies (e.g., cohort studies, observational studies, and case-control studies) were not reviewed. Second, only Chinese and English literature were included in this study, relevant gray literature was not obtained, and the search results may be subject to publication bias. Third, the subjectivity of the evaluators in evaluating the literature may lead to bias and thus affect the evaluation results.
Conclusion
The evidence summarized in this paper suggests that the methodological quality of SRs/MAs is not high. Therefore, they should be improved using the AMSTAR 2 tool to provide effective evidence-based medicine for targeted psychological interventions, psychological counseling services, and adequate social support help to alleviate psychological disorders due to pandemic factors.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
QZ and SS designed the study. QZ and YT searched the literature and performed screening. CJ and PL collected relevant data. QZ analyzed the data and drafted the manuscript. JT and SS revised and approved the final version of the manuscript. All authors have read and approved the submitted version.
Funding
This project was supported by the COVID-19 Prevention and Control Technology Research Project of Lanzhou City (grant number: 2020-XG-56).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.1024668/full#supplementary-material
References
Al Maqbali, M., Al Sinani, M., and Al-Lenjawi, B. (2021). Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and meta-analysis. J. Psychosom. Res. 141:110343. doi: 10.1016/j.jpsychores.2020.110343
Alsubaie, M. M., Stain, H. J., Webster, L. A. D., and Wadman, R. (2019). The role of sources of social support on depression and quality of life for university students. Int. J. Adolesc. Youth. 24, 484–496. doi: 10.1080/02673843.2019.1568887
Balakrishnan, V., Ng, K. S., Kaur, W., Govaichelvan, K., and Lee, Z. L. (2022). COVID-19 depression and its risk factors in Asia Pacific - A systematic review and meta-analysis. J Affect Disord. 298, 47–56. doi: 10.1016/j.jad.2021.11.048
Bao, Y., Sun, Y., Meng, S., Shi, J., and Lu, L. (2020). 2019-nCoV epidemic: Address mental health care to empower society. Lancet 395, e37–e38. doi: 10.1016/S0140-6736(20)30309-3
Batra, K., Singh, T. P., Sharma, M., Batra, R., and Schvaneveldt, N. (2020). Investigating the psychological impact of COVID-19 among healthcare workers: A meta-analysis. Int. J. Environ. Res. Public Health 17:9096. doi: 10.3390/ijerph17239096
Browning, M., Larson, L. R., Sharaievska, I., Rigolon, A., McAnirlin, O., Mullenbach, L., et al. (2021). Psychological impacts from COVID-19 among university students: Risk factors across seven states in the United States. PLoS One 16:e0245327. doi: 10.1371/journal.pone.0245327
Cao, X. L., Wang, S. B., Zhong, B. L., Zhang, L., Ungvari, G. S., Ng, C. H., et al. (2017). The prevalence of insomnia in the general population in China: A meta-analysis. PLoS One 12:e0170772. doi: 10.1371/journal.pone.0170772
Cénat, J. M., Blais-Rochette, C., Kokou-Kpolou, C. K., Noorishad, P. G., Mukunzi, J. N., McIntee, S. E., et al. (2021). Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 295:113599. doi: 10.1016/j.psychres.2020.113599
Chang, J. J., Ji, Y., Li, Y. H., Pan, H. F., and Su, P. Y. (2021). Prevalence of anxiety symptom and depressive symptom among college students during COVID-19 pandemic: A meta-analysis. J. Affect Disord. 292, 242–254. doi: 10.1016/j.jad.2021.05.109
Chen, F., Zheng, D., Liu, J., Gong, Y., Guan, Z., and Lou, D. (2020). Depression and anxiety among adolescents during COVID-19: A cross-sectional study. Brain Behav. Immun. 88, 36–38. doi: 10.1016/j.bbi.2020.05.061
Chen, J., Zhang, S. X., Yin, A., and Yáñez, J. A. (2022). Mental health symptoms during the COVID-19 pandemic in developing countries: A systematic review and meta-analysis. J. Glob. Health 12:05011. doi: 10.7189/jogh.12.05011
Chen, Q., Liang, M., Li, Y., Guo, J., Fei, D., Wang, L., et al. (2020). Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 7, e15–e16. doi: 10.1016/S2215-0366(20)30078-X
Deng, J., Zhou, F., Hou, W., Silver, Z., Wong, C. Y., Chang, O., et al. (2021a). The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 301:113863. doi: 10.1016/j.psychres.2021.113863
Deng, J., Zhou, F., Hou, W., Silver, Z., Wong, C. Y., Chang, O., et al. (2021b). The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: A meta-analysis. Ann N Y Acad. Sci. 1486, 90–111. doi: 10.1111/nyas.14506
Ferrando, M., Bagnasco, D., Roustan, V., Canonica, G. W., Braido, F., and Baiardini, I. (2016). Sleep complaints and sleep breathing disorders in upper and lower obstructive lung diseases. J. Thorac. Dis. 8, E716–E725. doi: 10.21037/jtd.2016.07.82
Gyasi, R. M. (2020). Fighting COVID-19: Fear and internal conflict among older adults in ghana. J. Gerontol. Soc. Work 63, 688–690. doi: 10.1080/01634372.2020.1766630
Han, L., Wong, F., She, D., Li, S. Y., Yang, Y. F., Jiang, M. Y., et al. (2020). Anxiety and depression of nurses in a north west province in China during the period of novel coronavirus pneumonia outbreak. J. Nurs. Scholarsh. 52, 564–573. doi: 10.1111/jnu.12590
Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., et al. (2020). Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020). Available online at: www.training.cochrane.org/handbook (accessed June 5, 2022).
Hu, N., Deng, H., Yang, H., Wang, C., Cui, Y., Chen, J., et al. (2022). The pooled prevalence of the mental problems of Chinese medical staff during the COVID-19 outbreak: A meta-analysis. J. Affect Disord. 303, 323–330. doi: 10.1016/j.jad.2022.02.045
Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., et al. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China. Lancet 395, 497–506. doi: 10.1016/S0140-6736(20)30183-5
Jahrami, H., BaHammam, A. S., Bragazzi, N. L., Saif, Z., Faris, M., and Vitiello, M. V. (2021). Sleep problems during the COVID-19 pandemic by population: A systematic review and meta-analysis. J. Clin. Sleep Med. 17, 299–313. doi: 10.5664/jcsm.8930
Johns, G., Samuel, V., Freemantle, L., Lewis, J., and Waddington, L. (2022). The global prevalence of depression and anxiety among doctors during the covid-19 pandemic: Systematic review and meta-analysis. J. Affect Disord. 298, 431–441. doi: 10.1016/j.jad.2021.11.026
Kawohl, W., and Nordt, C. (2020). COVID-19, unemployment, and suicide. Lancet Psychiatry 7, 389–390. doi: 10.1016/S2215-0366(20)30141-3
Lao, Y., Jiang, Y., Luo, X., and Liu, X. (2020). Focus on the depressive symptoms in COVID-19 patients: Perspective based on a rapid meta-analysis. Asian J. Psychiatr. 54:102421. doi: 10.1016/j.ajp.2020.102421
Lasheras, I., Gracia-García, P., Lipnicki, D. M., Bueno-Notivol, J., López-Antón, R., de la Cámara, C., et al. (2020). Prevalence of anxiety in medical students during the COVID-19 Pandemic: A rapid systematic review with meta-analysis. Int. J. Environ. Res. Public Health 17:6603. doi: 10.3390/ijerph17186603
Li, Y., Scherer, N., Felix, L., and Kuper, H. (2021). Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS One 16:e0246454. doi: 10.1371/journal.pone.0246454
Liu, C., Pan, W., Li, L., Li, B., Ren, Y., and Ma, X. (2021). Prevalence of depression, anxiety, and insomnia symptoms among patients with COVID-19: A meta-analysis of quality effects model. J. Psychosom. Res. 147:110516. doi: 10.1016/j.jpsychores.2021.110516
Liu, X., Wang, G., Zhang, J., and Wang, S. (2021a). Prevalence of depression and anxiety among health care workers in designated hospitals during the COVID-19 epidemic: A meta-analysis. Chin. J. Evidence Based Med. 21, 1035–1042. doi: 10.7507/1672-2531.202105079
Liu, X., Zhu, M., Zhang, R., Zhang, J., Zhang, C., Liu, P., et al. (2021b). Public mental health problems during COVID-19 pandemic: A large-scale meta-analysis of the evidence. Transl. Psychiatry 11:384. doi: 10.1038/s41398-021-01501-9
Liyanage, S., Saqib, K., Khan, A. F., Thobani, T. R., Tang, W. C., Chiarot, C. B., et al. (2021). Prevalence of anxiety in university students during the COVID-19 Pandemic: A systematic review. Int. J. Environ. Res. Public Health 19:62. doi: 10.3390/ijerph19010062
Lone, S. A., and Ahmad, A. (2020). COVID-19 pandemic - an African perspective. Emerg. Microb. Infect. 9, 1300–1308. doi: 10.1080/22221751.2020.1775132
Luchetti, M., Lee, J. H., Aschwanden, D., Sesker, A., Strickhouser, J. E., Terracciano, A., et al. (2020). The trajectory of loneliness in response to COVID-19. Am. Psychol. 75, 897–908. doi: 10.1037/amp0000690
Luo, W., Zhong, B. L., and Chiu, H. F. (2021). Prevalence of depressive symptoms among Chinese university students amid the COVID-19 pandemic: A systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 30:e31. doi: 10.1017/S2045796021000202
Marvaldi, M., Mallet, J., Dubertret, C., Moro, M. R., and Guessoum, S. B. (2021). Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 126, 252–264. doi: 10.1016/j.neubiorev.2021.03.024
Mulyadi, M., Tonapa, S. I., Luneto, S., Lin, W. T., and Lee, B. O. (2021). Prevalence of mental health problems and sleep disturbances in nursing students during the COVID-19 pandemic: A systematic review and meta-analysis. Nurs. Educ. Pract. 57:103228. doi: 10.1016/j.nepr.2021.103228
Necho, M., Tsehay, M., Birkie, M., Biset, G., and Tadesse, E. (2021). Prevalence of anxiety, depression, and psychological distress among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Int. J. Soc. Psychiatry 67, 892–906. doi: 10.1177/00207640211003121
Nochaiwong, S., Ruengorn, C., Thavorn, K., Hutton, B., Awiphan, R., Phosuya, C., et al. (2021). Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: A systematic review and meta-analysis. Sci. Rep. 11:10173. doi: 10.1038/s41598-021-89700-8
Norhayati, M. N., Che Yusof, R., and Azman, M. Y. (2021). Prevalence of psychological impacts on healthcare providers during COVID-19 pandemic in Asia. Int. J. Environ. Res. Public Health 18:9157. doi: 10.3390/ijerph18179157
Pappa, S., Chen, J., Barnett, J., Chang, A., Dong, R. K., Xu, W., et al. (2022). A systematic review and meta-analysis of the mental health symptoms during the Covid-19 pandemic in Southeast Asia. Psychiatry Clin. Neurosci. 76, 41–50. doi: 10.1111/pcn.13306
Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V. G., Papoutsi, E., and Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 88, 901–907. doi: 10.1016/j.bbi.2020.05.026
Pfefferbaum, B., and North, C. S. (2020). Mental health and the Covid-19 pandemic. N. Engl. J. Med. 383, 510–512. doi: 10.1056/NEJMp2008017
Sahebi, A., Abdi, K., Moayedi, S., Torres, M., and Golitaleb, M. (2021). The prevalence of insomnia among health care workers amid the COVID-19 pandemic: An umbrella review of meta-analyses. J. Psychosom. Res. 149:110597. doi: 10.1016/j.jpsychores.2021.110597
Salari, N., Hosseinian-Far, A., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Mohammadi, M., et al. (2020a). Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 16:57. doi: 10.1186/s12992-020-00589-w
Salari, N., Khazaie, H., Hosseinian-Far, A., Ghasemi, H., Mohammadi, M., Shohaimi, S., et al. (2020b). The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: A systematic review and meta-analysis. Glob. Health 16:92. doi: 10.1186/s12992-020-00620-0
Salari, N., Khazaie, H., Hosseinian-Far, A., Khaledi-Paveh, B., Kazeminia, M., Mohammadi, M., et al. (2020c). The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: A systematic review and meta-regression. Hum. Resour. Health 18:100. doi: 10.1186/s12960-020-00544-1
Santabárbara, J., Bueno-Notivol, J., Lipnicki, D. M., Olaya, B., Pérez-Moreno, M., Gracia-García, P., et al. (2021a). Prevalence of anxiety in health care professionals during the COVID-19 pandemic: A rapid systematic review (on published articles in Medline) with meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 107:110244. doi: 10.1016/j.pnpbp.2021.110244
Santabarbara, J., Idoiaga, N., Ozamiz-Etxebarria, N., and Bueno-Notivol, J. (2021d). Prevalence of anxiety in dental students during the COVID-19 Outbreak: A meta-analysis. Int. J. Environ. Res. Public Health 18:10978. doi: 10.3390/ijerph182010978
Santabárbara, J., Lasheras, I., Lipnicki, D. M., Bueno-Notivol, J., Pérez-Moreno, M., López-Antón, R., et al. (2021b). Prevalence of anxiety in the COVID-19 pandemic: An updated meta-analysis of community-based studies. Prog. Neuropsychopharmacol. Biol. Psychiatry 109:110207. doi: 10.1016/j.pnpbp.2020.110207
Santabárbara, J., Ozamiz-Etxebarria, N., Idoiaga, N., Olaya, B., and Bueno-Novitol, J. (2021c). Meta-Analysis of Prevalence of Depression in Dental Students during COVID-19 Pandemic. Medicina (Kaunas) 57:1278. doi: 10.3390/medicina57111278
Saragih, I. D., Tonapa, S. I., Saragih, I. S., Advani, S., Batubara, S. O., Suarilah, I., et al. (2021). Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: A systematic review and meta-analysis. Int. J. Nurs. Stud. 121:104002. doi: 10.1016/j.ijnurstu.2021.104002
Serrano-Ripoll, M. J., Meneses-Echavez, J. F., Ricci-Cabello, I., Fraile-Navarro, D., Fiol-deRoque, M. A., Pastor-Moreno, G., et al. (2020). Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta-analysis. J. Affect Disord. 277, 347–357. doi: 10.1016/j.jad.2020.08.034
Serrano-Ripoll, M. J., Zamanillo-Campos, R., Castro, A., Fiol-de Roque, M. A., and Ricci-Cabello, I. (2021). Insomnia and sleep quality in healthcare workers fighting against COVID-19: A systematic review of the literature and meta-analysis. Actas Esp Psiquiatr. 49, 155–179.
Shea, B. J., Reeves, B. C., Wells, G., Thuku, M., Hamel, C., Moran, J., et al. (2017). AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358:j4008. doi: 10.1136/bmj.j4008
Shi, L., Lu, Z. A., Que, J. Y., Huang, X. L., Liu, L., Ran, M. S., et al. (2020). Prevalence of and risk factors associated with mental health symptoms among the general population in china during the coronavirus disease 2019 Pandemic. JAMA Netw. Open 3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053
Ślusarska, B., Nowicki, G. J., Niedorys-Karczmarczyk, B., and Chrzan-Rodak, A. (2022). prevalence of depression and anxiety in nurses during the first eleven months of the COVID-19 Pandemic: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 19:1154. doi: 10.3390/ijerph19031154
Varghese, A., George, G., Kondaguli, S. V., Naser, A. Y., Khakha, D. C., and Chatterji, R. (2021). Decline in the mental health of nurses across the globe during COVID-19: A systematic review and meta-analysis. J. Glob. Health 11:05009. doi: 10.7189/jogh.11.05009
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., et al. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 17:1729. doi: 10.3390/ijerph17051729
Wang, J., Zhou, M., and Liu, F. (2020). Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J. Hosp. Infect. 105, 100–101. doi: 10.1016/j.jhin.2020.03.002
Wu, C., Hu, X., Song, J., Yang, D., Xu, J., Cheng, K., et al. (2020). Mental health status and related influencing factors of COVID-19 survivors in Wuhan. China. Clin. Transl. Med. 10:e52. doi: 10.1002/ctm2.52
Zhai, W., Zhang, Q., Hu, W., and Yan, J. (2022). A meta-analysis of anxiety symptom and related factors in chinese college students before and after the COVID-19 epidemic. Chin. Ment. Health J. 7, 626–632. doi: 10.3969/j.issn.1000-6729.2022.07.014
Zhang, S. X., Batra, K., Xu, W., Liu, T., Dong, R. K., Yin, A., et al. (2022). Mental disorder symptoms during the COVID-19 pandemic in Latin America - a systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 31:e23. doi: 10.1017/S2045796021000767
Zhang, W. R., Wang, K., Yin, L., Zhao, W. F., Xue, Q., Peng, M., et al. (2020). Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother. Psychosom. 89, 242–250. doi: 10.1159/000507639
Keywords: COVID-19, anxiety, depression, insomnia, systematic review, AMSTAR 2
Citation: Zou Q, Tang Y, Jiang C, Lin P, Tian J and Sun S (2022) Prevalence of anxiety, depressive and insomnia symptoms among the different groups of people during COVID-19 pandemic: An overview of systematic reviews and meta-analyses. Front. Psychol. 13:1024668. doi: 10.3389/fpsyg.2022.1024668
Received: 22 August 2022; Accepted: 25 October 2022;
Published: 16 November 2022.
Edited by:
Laisa Liane Paineiras-Domingos, Federal University of Bahia, BrazilReviewed by:
Seyed Mohammad Mahdi Moshirian Farahi, Carleton University, CanadaSamson Femi Agberotimi, North-West University, South Africa
Copyright © 2022 Zou, Tang, Jiang, Lin, Tian and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shougang Sun, c3Vuc2hnODA2QDEyNi5jb20=
 Qi Zou
Qi Zou Yuning Tang1
Yuning Tang1 Jinhui Tian
Jinhui Tian