
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 14 October 2021
Sec. Positive Psychology
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.741546
People with reduced levels of mental well-being might be at risk for developing future mental illness. Although several positive psychology interventions successfully improve mental well-being and psychological distress, less is known about their efficacy in a sample at risk for mental disorders. A Dutch sample of 289 participants with low or moderate levels of well-being were randomly assigned to other-focused kindness with reflection, other-focused kindness without reflection, self-focused kindness, or waitlist control (Trial register: NTR6786). Results of multilevel growth curve analyses revealed that other-focused kindness, but not self-focused kindness, led to improvements in the primary outcome mental well-being relative to waitlist control up to 6-week follow-up. By contrast, only other-focused kindness without reflection led to improvements in psychological distress. The three kindness conditions mainly did not differ from one another, and mainly no differences were found up to 6-months follow-up. An exception was that perceived stress was significantly more reduced up to 6-week and 6-months follow-up when people practiced other-focused kindness without reflection then when participants had practiced self-focused kindness. These findings point to the benefits of practicing kindness for others when people might be at risk for future mental illness. The study also indicates that reflecting about practicing kindness does not seem to have added value.
Promoting mental well-being is now seen as an important direction for public mental health and clinical psychology (e.g., Keyes, 2007a; Wood and Tarrier, 2010; Kobau et al., 2011; Jeste et al., 2015; Huber et al., 2016). A potential new target group for positive mental health promotion consists of people who are not flourishing and have also no severe mental health complaints. For example, Keyes (2007b) has shown that 60.3% of the US population did not have a mental illness, but were also not able to flourish. Similarly, 53% of the people in the Netherlands reported reduced levels of mental well-being but were not diagnosed with a mental disorder (Schotanus-Dijkstra et al., 2016, 2017b). Recent evidence shows that people with low or moderate levels of well-being report infrequent positive emotions (Catalino and Fredrickson, 2011), less positive life-events (Schotanus-Dijkstra et al., 2016), and an increased risk of developing a diagnosed mood or anxiety disorder 3 years later (Schotanus-Dijkstra et al., 2017b). In addition, people who stay in the low or moderate range of well-being within a 10-year time span are three times more likely to have developed a mental disorder during that period than those who stayed flourishing (Keyes et al., 2010).
These and other findings indicate that flourishing mental health should be promoted in people with reduced levels of well-being (Keyes et al., 2010; Wood and Joseph, 2010; Grant et al., 2013; Lamers et al., 2015; Schotanus-Dijkstra et al., 2017b). Several meta-analyses have shown that mental well-being and psychological distress can be improved through a variety of interventions, such as gratitude interventions, kindness interventions, and self-compassion interventions (Sin and Lyubomirsky, 2009; Bolier et al., 2013; Galante et al., 2014; Weiss et al., 2016; Dickens, 2017; Curry et al., 2018; Hendriks et al., 2018, 2019). Yet, most studies have been conducted within student samples (e.g., Layous et al., 2013a), healthy populations (e.g., Fredrickson et al., 2008), or clinical populations (e.g., Chaves et al., 2016), and only a few specifically targeted those with low or moderate levels of well-being but without any clinical symptoms (e.g., Schotanus-Dijkstra et al., 2017a). Positive psychology interventions used for selective and indicated prevention purposes may be especially effective, as those people are likely motivated to improve their well-being (Lyubomirsky et al., 2011). People with low levels of well-being might also benefit more from positive psychology interventions than those with higher levels of well-being (Nelson et al., 2014). A good start to test the efficacy of positive interventions in those at risk for developing mental disorders, is by examining practicing kindness.
A great advantage of practicing kindness is that it is a simple intervention that could be easily integrated in daily life and clinical practice and may cost no money, although some studies specifically focus on prosocial spending of which its emotional benefits are well-established in the literature (Aknin et al., 2013, 2020). In the current study, the focus lies on performing acts of kindness in which participants are typically asked to perform nice things for others, such as picking up groceries for a sick neighbor or giving a compliment to a colleague. Performing acts of kindness has been reliably linked to improved well-being (see Curry et al., 2018 for a meta-analysis). However, Curry et al. (2018) noted in their review of the literature that the majority of kindness studies (including acts of kindness and prosocial spending) focus primarily on immediate benefits of kindness for subjective well-being. Yet, it remains unclear whether performing kindness is effective in improving overall mental well-being and psychological distress because most studies to date mainly focus on happiness, life satisfaction, and positive affect (e.g., Alden and Trew, 2013; Layous et al., 2013b; Curry et al., 2018), and the studies regarding psychological distress are inconclusive (Mongrain et al., 2011; Kerr et al., 2015). For example, practicing kindness significantly reduced stress and anxiety compared to keeping track of daily moods, but it had no effect on reducing depressive symptoms (Kerr et al., 2015). Another study also found no effect of practicing kindness on a daily basis for 1 week in comparison with an early-memory control condition (Mongrain et al., 2011).
To expand prior knowledge about the efficacy of kindness further, we also explored whether adding reflection to performing acts of kindness is more beneficial for mental health than performing acts of kindness without reflection. This hypothesis was based on prior studies suggesting that reliving a positive event might be even more important for feeling good than the activity itself (e.g., Emmons and McCullough, 2003; Van Boven and Gilovich, 2003). The emotional benefits of expressive writing is well-established in the literature, although the focus often lies in writing about traumatic or emotionally charged experiences (Pennebaker, 2018). However, when dating couples expressively wrote about their relationships, the chance of being together 3 months later was significantly higher compared to couples who wrote about daily activities (Slatcher and Pennebaker, 2006). In addition, a recent study demonstrated that recalling three kind acts on 1 day revealed similar improvements on different well-being outcomes (e.g., positive and negative affect, life-satisfaction) relative to performing three kind acts on 1 day or doing both (Ko et al., 2021). Although this was a 3-day trial, these findings might indicate that reflecting on past kind acts might be at least as effective as performing kind acts.
Furthermore, a study by Grant and Dutton (2012) demonstrated that participants who reflected about recent performed kind acts for others called more potential fundraisers and donated more money to charity compared to participants who reflected about receiving kind acts. However, a certain amount of engagement in a reflection task after performing kind acts seems a prerequisite for its beneficial effects (Aknin et al., 2020). For example, receiving instructions such as “describe your purchase as vividly and in as much detail as possible” (Aknin et al., 2020) was more generic which might have led to smaller effects than instructions such as “reflect on what brought it about, and describe how it affected your thoughts, feelings and actions” (Grant and Dutton, 2012). In the current study, we add specific reflection instructions about the kind acts they performed 1 day earlier and compared this with performing kind acts for others without reflection.
Interestingly, Western cultures often emphasize taking care of oneself first before helping others. The popularity of self-compassion may have strengthened this vision, as self-compassion is associated with higher levels of mental well-being (Leary et al., 2007; Neff et al., 2007; Gilbert, 2010). Being kind to one self, especially in the face of suffering and failure, is one of the three aspects of self-compassion (Neff, 2003). However, this aspect differs from popular perceptions of self-kindness, which may be more commonly interpreted as self-indulgent behavior.
In fact, accumulating evidence shows that it might be more worthwhile for people's mental well-being to help others and build positive relationships (Dunn et al., 2011; Nelson et al., 2016; Crocker et al., 2017; Schotanus-Dijkstra et al., 2019). For instance, a recent experimental study found greater increases in positive affect for participants who recalled an act of kindness with the intention to gain benefits for the other person compared to participants who recalled an act of kindness with the intention to gain benefits for themselves (Wiwad and Aknin, 2017). In addition, kindness to benefit others was coded as being more kind and impactful compared to performing kind acts for others with a focus on the self (Wiwad and Aknin, 2017). Similarly, a study among adults recruited from the general US population showed that performing five acts of kindness for others on 1 day was significantly more effective in enhancing mental well-being than performing such acts for oneself, or keeping track of daily activities (Nelson et al., 2016). These findings indicate that self-focused kindness might be less beneficial for one's mental health compared to practicing other-focused kindness, although studies regarding direct comparison of kindness for the self and others are scarce.
To best understand the potential benefits of other-focused kindness and self-focused kindness across a range of contexts, more work is needed focusing on participants from a range of backgrounds and on a range of mental health outcomes over longer periods of time (Curry et al., 2018). We answer this call in the current study by investigating the effects of kindness in a sample of adults who might be at risk for future mental illness, across a range of mental health outcomes. In addition, we measure the effects of practicing kindness up to 6 months following the kindness intervention.
The purpose of the current study was to examine the efficacy of other-focused kindness with and without reflection and self-focused kindness on mental well-being (including emotional, social, and psychological well-being), depressive symptoms, anxiety, and perceived stress relative to waitlist control. We expected that mental health would improve significantly more when participants reflected on their other-focused kindness compared to those only performing other-focused kindness. We also expected that performing kindness for others with and without reflection would outperform the other two conditions on all of the outcomes, of which more pronounced effects were expected in comparison with waitlist control than in comparison with self-focused kindness.
A parallel randomized controlled trial about the efficacy of different exercises to improve people's well-being was approved by the Ethics Committee of the University of Twente (BCE17240) and registered in the Dutch Trial Register (NTR6786). The current paper describes results according to the CONSORT guidelines (Moher et al., 2010) from four of the five conditions1, with an allocation ratio of 1:1:1:1.
Participants for the complete study1 were recruited from the general Dutch population by advertisements at Facebook/LinkedIn (n = 425), in a popular psychology magazine (n = 156), and in national and regional newspapers (n = 72). Participants were required to have sufficient Internet connection and a valid email address, as well as mastery of the Dutch language. Participants who completed the online informed consent procedure were automatically redirected to an online screening questionnaire. Eligible participants were at risk for future mental illness (i.e., low and moderate levels of well-being), but they had no severe complaints which could indicate a clinical disorder. Therefore, we excluded (1) participants who were already flourishing as measured with the Mental Health Continuum-Short Form and by using Keyes' classification guidelines of scoring a 4 or 5 on at least one emotional well-being item together with a score of a 4 or 5 on at least 6 of the 11 social and psychological well-being items (Keyes et al., 2008; Lamers et al., 2011), and (2) participants with severe depressive or anxiety symptoms, indicated by a score >34 on the Center for Epidemiological Studies Depression (CES-D) questionnaire (Radloff, 1977; Bouma et al., 1995; Santor et al., 1995) and a score > 15 on the Generalized Anxiety Disorder-7 (GAD-7) questionnaire (Spitzer et al., 2006; Donker et al., 2009). See Figure 1 for the flow of participants throughout the study.
The final sample for the current study consisted of 289 participants. Participants' ages ranged between 18 and 70 years (M = 48.8; SD = 9.6). The majority were women (89.6%), married (48.1%), in paid employment (75.4%), living with others (72.0%), and of Dutch nationality (86.2%). Also, the majority had at least a college degree (78.5%).
Prior to data collection, we conducted a power analysis, which showed that 78 participants per condition were needed to obtain a minimal effect size of d = 0.45 (Alden and Trew, 2013; Kerr et al., 2015) assuming a two-tailed test with alpha of 0.05 and a power of 0.80 (1 – β). Randomization was stratified by gender and education and conducted using randomizer.org all at once after the deadline for completing the baseline assessment. Participants were not blind for their own condition, but they were not aware of the number and content of the other conditions.
Participants were randomly assigned to one of four conditions: to perform five acts of kindness for others on 1 day per week followed by reflection on those actions on the following day (i.e., other-focused kindness with reflection; n = 73), to perform five acts of kindness for others on 1 day per week (i.e., other-focused kindness without reflection; n = 72), to perform five acts of kindness for themselves on 1 day per week (i.e., self-focused kindness; n = 73), or only to complete all well-being measures and choose a happiness activity after the 6-week follow-up (i.e., waitlist control, n = 71; see Supplementary Materials for complete instructions for each condition and the level of adherence per week)2. We instructed participants to perform five kind acts on 1 day per week based on prior research indicating that performing five acts of kindness in 1 day led to greater well-being improvements than performing five acts of kindness throughout the week (Lyubomirsky et al., 2005). Participants in the waitlist control group waited for 12 weeks before they chose which activity to improve their well-being they would like to perform. We did not want to wait longer because of the high drop-out risk and for ethical reasons as participants had signed up for receiving a happiness exercise.
As a manipulation check, the day after their kindness day, participants were instructed to list their actions relevant to their assigned conditions. Participants in the other-kindness with reflection were also asked to write briefly about their experiences performing the activity, including how they felt, who they were with, and what the activity meant to them and the recipient of their kindness. Participants performed their activities weekly for 6 weeks and completed online assessments at baseline (T0), post-test (T1), 6-week follow-up (T2), and 6-month follow-up (T3). Initially, we planned to do the follow-ups at 6 months and 12 months, but we did not want to risk losing too many participants in the waitlist control condition and decided to bring the dates forward.
Participants completed the 14-item Mental Health Continuum-Short Form (MHC-SF) to measure overall mental well-being, including the three-item emotional well-being subscale (e.g., “How often did you feel happy?”), the five-item social well-being subscale (e.g., “How often did you feel that you belonged to a community/social group?”), and the six-item psychological well-being subscale (e.g., “How often did you feel that you liked most aspects of your personality?”; Keyes et al., 2008; Lamers et al., 2011). Each item was rated on a scale from 0 (never) to 5 (every day). Higher average sores indicate higher levels of mental well-being over the past 4 weeks. Reliability of the total scale ranged between 0.84 and 0.91 for each measurement time point, and between 0.60 and 0.87 for the subscales.
Participants completed the 20-item CES-D at screening (1 week before baseline), post-test and at follow-up to measure depressive symptoms during the last week (Radloff, 1977; Bouma et al., 1995). Participants reported their symptoms of depression (e.g., “I felt lonely”) on a scale ranging from 0 (rarely or none of the time, <1 day) to 3 (most or all of the time, 5–7 days). Responses to all items were summed to create a score ranging from 0 to 60. Higher scores indicate greater symptoms of depression. The reliability was good, ranging between 0.84 and 0.93 between time points.
The GAD-7 consists of seven items that measure anxiety symptoms during the past 2 weeks (Spitzer et al., 2006; Donker et al., 2009). Participants reported at screening, post-test and follow-up how often they were bothered by several problems (e.g., “not being able to stop or control worrying”) on a scale ranging from 0 (not at all) to 3 (nearly every day). Responses were summed such that higher total scores (0–21) indicate more symptoms of generalized anxiety. Cronbach's α's showed that the reliability of the scale was acceptable to good, with alpha's ranging from 0.74 to 0.88.
The 10-item Perceived Stress Scale (PSS) assesses how often a person felt stressed during the past month (Cohen et al., 1994). Participants indicated at baseline, post-test, and follow-up their feelings of stress for each item (e.g., “In the last month, how often have you felt nervous and ‘stressed'?”) on a scale ranging from 0 (never) to 4 (very often). Responses were summed such that higher scores (0–40) indicate higher levels of perceived stress. The PSS showed good reliability in the present study, with alpha's ranging between 0.85 and 0.89 between time points.
At baseline and after 1 week when completing the first online diary, expectations and motivations were checked through self-developed items. The item about expectations differed slightly between assessments: (1) “How convinced are you about the utility of performing happiness exercises for your sustainable happiness and well-being?” (2) “You now know which happiness exercise you are going to perform. How convinced are you about the utility of performing this happiness exercise for your sustainable happiness and well-being?” Furthermore, motivation was measured with the item: “How motivated are you for doing the/this weekly happiness exercise during 6 weeks?” All these items were scored on a continuous scale from 1 to 10, of which 10 is indicating the highest level of expectations and motivation respectively.
At post-test, the participants who were in one of the kindness conditions also completed the 8-item Client Satisfaction Questionnaire-short form (CSQ-8) to assess the level of client satisfaction (Attkisson and Zwick, 1982). Each item has an answer scale from 1 to 4, but the labels differ per item. Five items were recoded as such that a higher sum score (8–32) indicated higher satisfaction with the exercise. The Cronbach's α showed excellent reliability in this study (0.91). An additional question asked participants how much time they had spent on doing the exercise each week, on average (1 = 0–30 min per week, 2 = 30–60 min per week, 3 = more than 2 h per week).
All analyses were performed with SPSS version 26.0, using two-tailed tests and p < 0.05. Descriptive statistics of demographic variables and outcome measures at baseline, of drop-out and completers, and of the process measures during and after the intervention were calculated and compared between conditions using χ2-tests and univariate analysis of variance (ANOVA). Drop-out was defined as participants who completed only the baseline assessment. In addition, the weekly happiness diaries were consulted to obtain the number and content of kind acts for others or themselves that the participants reported on a scale from 0 (no kind acts) to 5 (five kind acts).
All randomized individuals were analyzed in the allocated intervention arm regardless of whether they had followed the intervention instructions consequently (intention-to-treat principle). In addition, all randomized participants were invited to complete each survey at each time-point although they might have not completed a prior survey. We examined changes in mental well-being and all secondary outcomes over time using multilevel growth curve modeling in R (version 0.99.902, NLME package) to account for repeated measures nested within individuals (Singer and Willett, 2003). Within these analyses, we used maximum likelihood estimation based on the available data of the same and other participants.
Because participants were no longer instructed to engage in acts of kindness after 6 weeks, we hypothesized that changes in well-being would be non-linear. Thus, we specified linear and nonlinear changes in well-being. We began with an unconditional growth curve model, specifying linear and quadratic changes over time, which we then compared with hypothesis-testing models.
Composite model: Yij = γ00 + γ10Timeij + γ20Time2ij (εij + ζoi + ζ1iTimeij + ζ2iTime2ij)
Level 1 model: Yij = π0i + π1iTimeij + π2iTime2ij + εij
Level 2 models: π0i = γ00 + ζ0i, π1i = γ10 + ζ1i, and π2i = γ20 + ζ2i
After the 6-week follow-up, participants in the waitlist condition started with the self-chosen well-being activity. Therefore, we present two sets of analyses: one comparing the effects of kindness with waitlist control from baseline to the 6-week follow-up and a second analysis comparing the three kindness conditions from baseline to the 6-month follow-up. Time was centered on the second time point (post-test). In hypothesis-testing models, each condition was dummy-coded (waitlist control or self-kindness as reference group) and entered as between-subjects predictors in the second level models.
The four conditions did not differ on most of the characteristics mentioned in Table 1 (χ2s < 6.02, ps > 0.111) and on the outcome measures at baseline (see Table 2; Fs < 2.36, ps > 0.072). However, participants in the waitlist control were more often of Dutch nationality, χ2(3) = 8.21, p = 0.042, and less often living with children, χ2(3) = 8.17, p = 0.043, compared to the other three groups.
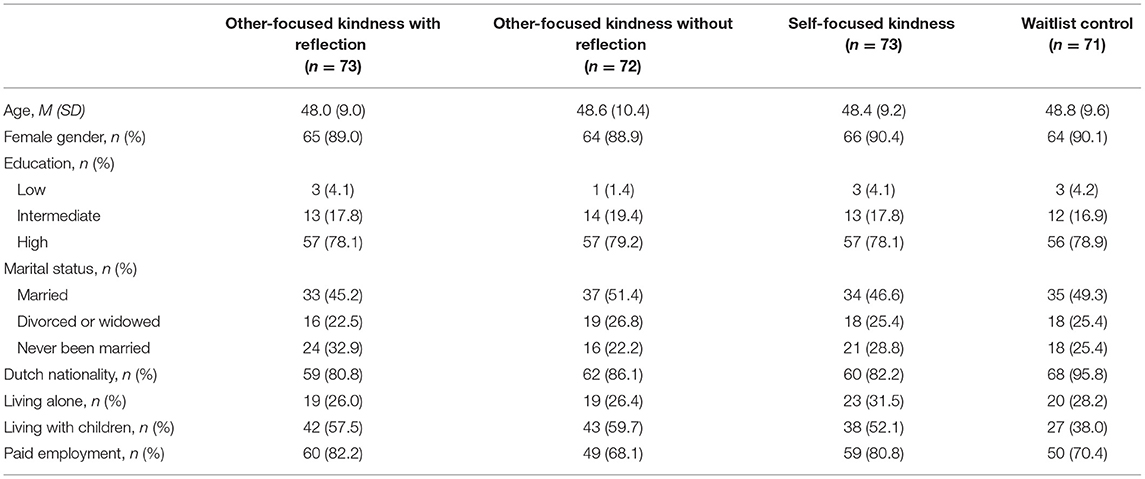
Table 1. Baseline characteristics of the participants performing kind acts for others or themselves, or who were on the waitlist.
Of the 289 participants who began the study, 58 participants (20.1%) did not complete any of the post-test or follow-up assessments. Participants in the three kindness conditions were significantly more likely to drop out compared to waitlist control (other-kindness with reflection = 16.4%, other-kindness without reflection = 30.6%, self-kindness = 27.4%, waitlist = 5.6%), χ2(3) = 17.20, p = 0.001. In addition, drop-outs were significantly younger (M = 43.3, SD = 10.5) than participants who completed at least two assessments (M = 50.1, SD = 8.9), F(287) = 25.60, p < 0.001. All 289 participants who completed at least the baseline survey were included in analyses.
Relative to waitlist control, other-focused kindness with and without reflection led to significant linear improvements in mental well-being up to 6-week follow-up (γs > 0.10, ps < 0.047, d3 = 0.38 and 0.42, respectively). Self-focused kindness did not lead to any changes in mental well-being compared to waitlist control, and the trajectories of the kindness conditions did also not differ from each other (γs <-0.12, ps >0.111). In addition, the three kindness conditions did not differ from each other in linear or non-linear changes in mental well-being up to 6-months follow-up (γs < −0.04, ps >0.332). See Tables 3, 4 for parameter estimates and model fit indices and Figure 2 for a visual presentation of the trajectories.
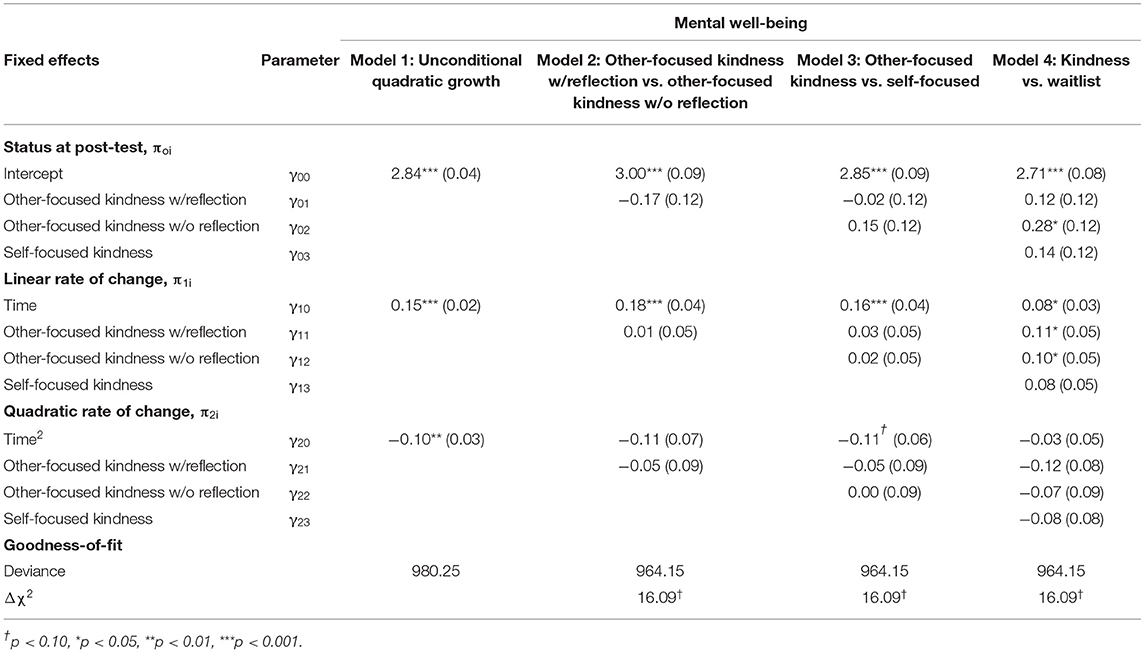
Table 3. Parameter estimates and goodness of fit indices for multilevel growth curve models predicting changes in mental well-being up to 6-weeks follow-up comparing other-focused kindness and self-focused kindness with waitlist control.
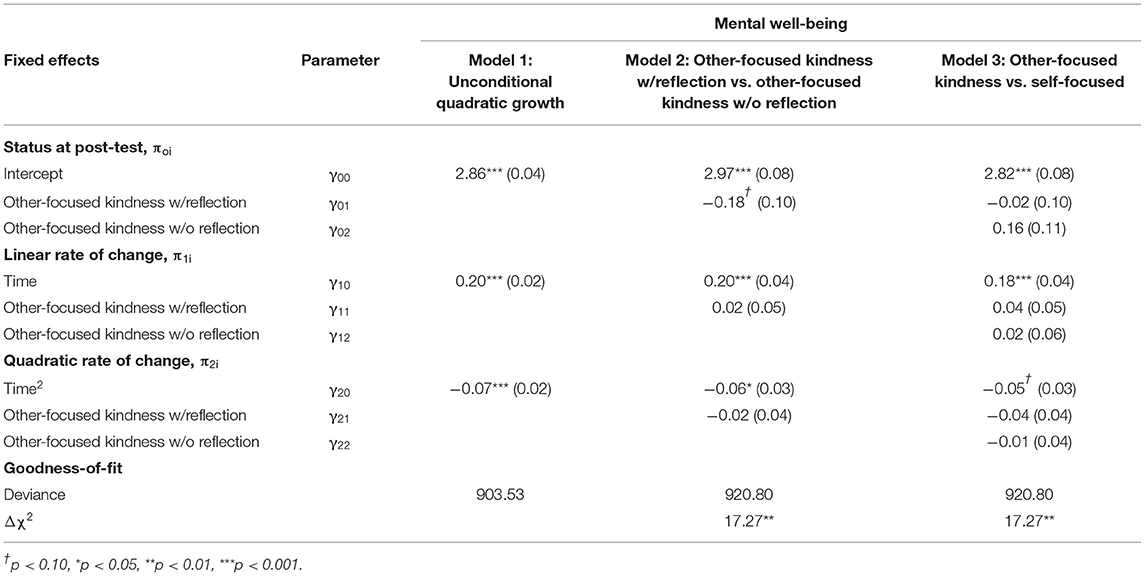
Table 4. Parameter estimates and goodness of fit indices for multilevel growth curve models predicting changes in mental well-being up to 6-months follow-up comparing other-focused kindness with self-focused kindness.
Relative to waitlist control, other-focused kindness without reflection led to significant linear improvements through the 6-week follow-up in depressive symptoms and perceived stress (γs >-1.31, ps < 0.035, d = 0.55 and 0.54, respectively) and to quadratic changes in anxiety, γ22 = 1.29, SE = 0.65, t(394) = 1.97, p = 0.050. Furthermore, other-focused kindness with reflection and other-focused kindness without reflection did not differ from each other in linear or non-linear trajectories in any outcome. Relative to self-focused kindness, other-focused kindness without reflection led to significant linear improvements in perceived stress up to 6-week follow-up, γ12 = −1.31, SE = 0.57, t(393) = −2.30, p = 0.022, d = 0.47.
Up to 6-months follow-up, most comparisons between the three kindness conditions did not significantly differ from each other. However, other-focused kindness without reflection led to significant linear improvements in perceived stress relative to self-focused kindness, γ12 = −1.26, SE = 0.59, t(388) = −2.12, p = 0.034, d = 0.67.
Participants in the three kindness conditions did not significantly differ regarding how convinced they were about the utility of doing happiness exercises at baseline (M = 7.15, SD = 1.38), F(215) = 1.53, p = 0.219, and after 1 week practicing (M = 6.32, SD = 1.79), F(192) = 0.02, p = 0.983. Participants were also highly motivated to practice a happiness exercise at baseline (M = 8.05, SD = 1.26), F(215) = 0.34, p =0.812, and after 1 week practicing (M = 7.28, SD = 1.81), F(192) = 1.30, p = 0.274, and highly interested in positive psychology (M = 8.48, SD = 1.13), F(215) = 0.81, p = 0.445, which all did not differ between conditions.
The level of satisfaction with the kindness exercises was moderate for each condition (other-kindness with reflection M = 19.4, SD = 5.06; other-kindness without reflection M = 19.9, SD = 3.89, self-kindness M = 19.8, SD = 4.80), F(153) = 0.20, p = 0.817. However, participants practicing other-focused kindness mainly spent 0–30 min per week on the intervention (other-kindness with reflection = 64.7%, other-kindness without reflection = 70.7%, self-kindness = 44.4%), while self-focused kindness mainly spent 30–60 min per week (other-kindness with reflection = 19.6%, other-kindness without reflection = 14.6%, self-kindness = 37.8%), χ2(4) = 8.38, p = 0.079.
Participants in the two other-focused kindness conditions performed 2,126 kind acts in total (other-kindness with reflection M = 15.7, SD = 7.87; other-kindness without reflection M = 16.8, SD = 8.68), F(130) = 0.50, p = 0.479. These kind acts could be mainly categorized in moral support (e.g., investing time, comforting, showing interest, greeting strangers; complementing, expressing gratitude) and physical support (e.g., helping, serving, doing chores, volunteering), but also donating material goods or money to others were mentioned (see Supplementary Materials for some specific examples). Participants in the self-focused kindness condition performed 1,143 kind acts (M = 16.8, SD = 8.61), F(198) = 0.35, p = 0.704, which could be mainly categorized in self-indulgent behavior (e.g., indulging in food or drinks, lazy leisure, material goods, wellness). In addition, some of these self-indulgent behaviors also involved other people (e.g., “watching a movie with my partner,” “having a nice lunch with a former colleague”; “went shopping with a friend”). A minority of the kind acts were mainly or partly about mindfulness and self-compassion, cherish meaningful relationships with others, and active leisure such as physical activity and hobbies.
Participants in the waitlist condition were provided instructions after the 6-week follow-up about the kindness and gratitude conditions and given the opportunity to choose an activity to improve their well-being. Of the 60 participants who completed the 6-weeks follow-up, 66.7% chose to perform the gratitude intervention, 25.0% chose to perform self-focused kindness, and 6.7% chose other-focused kindness. One person did not want to do an exercise (1.7%).
This randomized controlled trial demonstrated that other-focused kindness with and without reflection did not differ from each other on any of the outcome measures. Other-focused kindness with and without reflection were more effective in improving mental well-being up to 6-weeks follow-up in a sample at risk for future mental illness than waitlist control, but not up to 6-months follow-up. In addition, significant effects were found for other-focused kindness without reflection on depression, anxiety and perceived stress relative to waitlist control up to 6-weeks follow-up. Self-focused kindness fell usually somewhere between the other-focused kindness and waitlist control conditions, showing mainly no significant differences relative to these conditions. However, significant changes on perceived stress up to 6-months follow-up were found for other-focused kindness without reflection relative to self-focused kindness.
To our knowledge, the current study was the first to compare other-focused kindness with and without reflection. Contrary to expectations, adding reflection to other-focused kindness did not lead to greater improvements in any of the outcomes. In fact, kindness without reflection outperformed the other conditions on psychological distress when comparing each condition to waitlist control; however, no significant differences were found between the two other-focused kindness conditions. A possible explanation for not finding additional effects of reflection might be that the reflective questions were too brief and that adding an expressive writing exercise for at least 15 min on one or more days about their practiced kindness could have been more effective (Toepfer et al., 2016; Aknin et al., 2020).
Another possibility is that the instructions of performing five kind acts on 1 day was too difficult as also indicated by low adherence levels per week. The weekly reflections could have shifted from its content and possible benefits for themselves and others to reflections about the difficulty and repetitive character of the task. More variation is argued to be one of the factors for more lasting effects of positive interventions (Lyubomirsky and Layous, 2013). In addition, how participants reflect on their kind acts might diminish the benefits of reflection. For example, the reflection task might have led to critical reflections in which participants felt ambiguous by the fact that they felt good by doing good for others and might believe they were doing the acts too much for their own benefits instead of altruistically help others. Alternatively, to the extent that reflection led participants to explain or over-analyze their positive experiences, they may no longer reap the benefits of those actions (e.g., Lyubomirsky et al., 2006; Wilson and Gilbert, 2008).
The current study also adds to the literature that other-focused kindness is beneficial in enhancing overall mental health, as indicated by emotional, social, and psychological well-being and partly by improved levels of depression, anxiety, and perceived stress. To date, most studies about the efficacy of performing prosocial behavior assessed emotional well-being (happiness, life-satisfaction or positive affect; e.g., Ouweneel et al., 2014; Nelson et al., 2015) and sometimes also psychological distress (e.g., Mongrain et al., 2011; Kerr et al., 2015). Our study aligns most strongly with prior findings indicating practicing kindness toward others was more beneficial for one's multidimensional well-being in comparison with tracking daily activities (Nelson et al., 2016). We also demonstrated that kindness for others leads to reductions in depressive symptoms, anxiety and perceived stress, although these results were only significant for the group who did not reflect on their performed kind acts.
Importantly, the effects of the three kindness conditions mainly followed a nonlinear trajectory up to 6 months follow-up. These findings indicate that practicing kindness for others or for the self are both successful strategies for improving one's mental health, but that they may not lead to sustained well-being without continued practice. As indicated by our significant non-linear trajectories, most participants who practiced kindness for others or oneself demonstrated an improvement in well-being up to 6 weeks following the intervention, followed by a subsequent decline in well-being by 6 months follow-up. These findings also show that it is important for future research to follow participants for a longer time period because significant effects might diminish over time for some but not all activities or programs (e.g., Schotanus-Dijkstra et al., 2017a).
A surprising finding compared to prior research (e.g., Nelson et al., 2016) was that other-focused kindness was mainly not more effective relative to self-focused kindness, although self-focused kindness was also not more effective relative to waitlist control. A possible explanation may be that participants reported that they spent more time on their self-focused kind acts than on other-focused kind acts. This might be due to the nature and duration of the performed acts such as a wellness related treatment (self-focused) vs. encouraging a friend over the phone (other-focused). Future research could add a time frame of how long a kind activity for others or the self might last (e.g., between 5 and 15 min). In addition, some activities might be more easy to integrate in daily life and thereby be more effective (e.g., self-focused kindness), while other behaviors might be more effective by putting in greater effort (e.g., other-focused kindness; Schiffer and Roberts, 2018). Furthermore, where positive emotions might be an important underlying mechanism of positive psychological interventions in general and of acts of kindness in particular (Nelson et al., 2016; Hendriks et al., 2020), the type of emotions that influence well-being might differ per kindness type. For example, self-focused kindness might elicit low-arousal positive emotions such as relaxation and satisfaction, while other-focused kindness might elicit high-arousal positive emotions such as joy, happiness, and surprise.
Interestingly, other-focused kindness without reflection was more effective in relieving perceived stress compared to self-focused kindness. When people perceive stress, a common strategy is to be kind to yourself by seeking relaxation and self-indulgent behavior. However, the current study suggests that helping others might be a more sufficient strategy for relieving perceived stress. Focusing on others might offer distraction from one's perceived stress and may provide opportunities to put things in perspective, which might result in lowered feelings of stress. By contrast, prior studies have indicated that the level of self-compassion is more predictive for students' well-being than their levels of stress or social support (Neely et al., 2009), and research also found that self-compassionate people can better cope with daily stresses and chronic illnesses (Sirois et al., 2015). This discrepancy with our findings could be explained by the fact that self-compassion also involves common humanity and mindfulness and defines self-kindness more in terms of being less self-critical (Neff, 2003). The self-kindness activities conducted in the current study seem different from those encouraged by self-compassion research. Although our study indicates that other-focused and self-focused kindness can be beneficial for your mental health, when feeling stressed, it might pay off to help others first before you indulge yourself. Yet, this implication should be tested directly in a sample with elevated levels of (manipulated) stress, especially because we did not find an effect on perceived stress for other-focused kindness with reflection.
We expand prior evidence on the efficacy of performing acts of kindness by examining the value of adding reflection to the intervention and by comparing this positive psychology intervention with both a self-focused kindness condition and a waitlist control group. We also selected participants with low or moderate levels of well-being who manifested no severe clinical complaints and followed participants for a longer time span. However, some limitations also apply.
First, although we conducted the power analysis in line with prior kindness studies, the meta-analysis of Curry et al. (2018) suggest that a sample size of at least 202 per cell is needed. We might have more power than prior studies using student samples because our more vulnerable participants had more room to grow; however, future studies should pay attention to optimize power. Second, full adherence to the program gradually decreased from approximately 70 to 35% over the 6-week intervention period with participants in the other-focused kindness without reflection condition demonstrating the greatest attrition and waitlist participants demonstrating the lowest rates of attrition. Although all participants were included in our analyses, differential drop-out rates across conditions may have influenced our results. Third, although the use of a no-treatment control group gives more power, it also limits strong evidence for the efficacy of practicing kindness because of differences between groups attributed to differences in effort, motivation, receiving attention, or other factors unrelated to kindness behaviors. Fourth, the self-selected sample consisted mainly of higher-educated native Dutch females which is consistent with many prior positive intervention studies (e.g., Mongrain et al., 2011; Schotanus-Dijkstra et al., 2017a), but with the consequence that the results are not directly applicable to the general population.
In sum, our study demonstrated that focusing attention on others via acts of kindness not only improves positive psychological well-being, but also reduces perceived stress and symptoms of depression and anxiety in a sample of individuals vulnerable to mental illness. Positive psychologists should make greater efforts to recruit and target people with low or moderate well-being and to discover in larger samples for whom and why engaging in small kindnesses for others and the self is a useful strategy to feel better. In addition, researchers could apply the current methodology to other positive psychological interventions by focusing not only on student or clinical samples, but on those at risk for future mental illness as well.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of the University of Twente (BCE17240). The participants provided their written informed consent to participate in this study.
ETB and MSD contributed to conception and design of the study. SKNC and MSD performed the statistical analyses and wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank Elselotte van den Berge and Mariëtta Vogel for conducting the qualitative analyses of the acts of kindness diaries.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.741546/full#supplementary-material
1. ^A fifth condition, unrelated to the kindness conditions, was run simultaneously for comparison with waitlist control of which the results are described elsewhere (Bohlmeijer et al., 2020). The fifth condition consisted of a 6-week gratitude intervention in which six different exercises were used, while the current study focused on different kindness conditions in which the same activity was used each week, during 6 weeks. The distinct study aims were reported before the start of the study in the Dutch Trial Register (NTR6786). We report this fifth condition as a footnote for the sake of clarity.
2. ^Given that our power analysis indicated we would need 78 participants per condition, we opted to focus our study on the primary conditions of interest (other-focused kindness with and without reflection) to maximize power rather than to fully cross reflection with the focus of kindness.
3. ^Effect size d was calculated with this equation: γ *(duration – 1)/SDraw (Feingold, 2009, 2015). This effect size estimate is only appropriate for linear slopes and represents an estimate of the standardized mean difference (Cohen's d) between groups at the end of the study.
Aknin, L. B., Dunn, E. W., Proulx, J., Lok, I., and Norton, M. I. (2020). Does spending money on others promote happiness?: a registered replication report. J. Pers. Soc. Psychol. 119, e15–e26. doi: 10.1037/pspa0000191
Aknin, L. B., Dunn, E. W., Whillans, A. V., Grant, A. M., and Norton, M. I. (2013). Making a difference matters: impact unlocks the emotional benefits of prosocial spending. J. Econ. Behav. Organ. 88, 90–95. doi: 10.1016/j.jebo.2013.01.008
Alden, L. E., and Trew, J. L. (2013). If it makes you happy: engaging in kind acts increases positive affect in socially anxious individuals. Emotion 13, 64–75. doi: 10.1037/a0027761
Attkisson, C. C., and Zwick, R. (1982). The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval. Prog. Plann. 5, 233–237. doi: 10.1016/0149-7189(82)90074-x
Bohlmeijer, E., Kraiss, J. T., Watkins, P. C., and Schotanus-Dijkstra, M. (2020). Promoting gratitude as a resource for sustainable mental health: results of a 3-armed randomized controlled trial up to 6 months follow-up. J. Happiness Stud. 22, 1011–1032. doi: 10.1007/s10902-020-00261-5
Bolier, L., Haverman, M., Westerhof, G., Riper, H., Smit, F., and Bohlmeijer, E. (2013). Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Public Health 13, 119. doi: 10.1186/1471-2458-13-119
Bouma, J., Ranchor, A. V., Sanderman, R., and van Sonderen, E. (1995). Het Meten van Symptomen van Depressie met de CES-D. Een handleiding. UMCG/Rijksuniversiteit Groningen.
Catalino, L. I., and Fredrickson, B. L. (2011). A tuesday in the life of a flourisher: the role of positive emotional reactivity in optimal mental health. Emotion 11, 938–950. doi: 10.1037/a0024889
Chaves, C., Lopez-Gomez, I., Hervas, G., and Vazquez, C. (2016). A comparative study on the efficacy of a positive psychology intervention and a cognitive behavioral therapy for clinical depression. Cognit. Ther. Res. 41, 417–433. doi: 10.1007/s10608-016-9778-9
Cohen, S., Kamarck, T., and Mermelstein, R. (1994). “Perceived stress scale,” in Measuring Stress: A Guide for Health and Social Scientists, eds S. Cohen, R. C. Kessler, and L. Underwood Gordon (New York, NY: Oxford University Press).
Crocker, J., Canevello, A., and Brown, A. A. (2017). Social motivation: costs and benefits of selfishness and otherishness. Annu. Rev. Psychol. 68, 299–325. doi: 10.1146/annurev-psych-010416-044145
Curry, O. S., Rowland, L. A., Van Lissa, C. J., Zlotowitz, S., McAlaney, J., and Whitehouse, H. (2018). Happy to help? A systematic review and meta-analysis of the effects of performing acts of kindness on the well-being of the actor. J. Exp. Soc. Psychol. 76, 320–329. doi: 10.1016/j.jesp.2018.02.014
Dickens, L. R. (2017). Using gratitude to promote positive change: a series of meta-analyses investigating the effectiveness of gratitude interventions. Basic Appl. Soc. Psychol. 39, 193–208. doi: 10.1080/01973533.2017.1323638
Donker, T., van Straten, A., Marks, I., and Cuijpers, P. (2009). A brief web-based screening questionnaire for common mental disorders: development and validation. J. Med. Internet Res. 11, e19. doi: 10.2196/jmir.1134
Dunn, E. W., Gilbert, D. T., and Wilson, T. D. (2011). If money doesn't make you happy, then you probably aren't spending it right. J. Consum. Psychol. 21, 115–125. doi: 10.1016/j.jcps.2011.02.002
Emmons, R. A., and McCullough, M. E. (2003). Counting blessings versus burdens: an experimental investigation of gratitude and subjective well-being in daily life. J. Pers. Soc. Psychol. 84, 377–389. doi: 10.1037/0022-3514.84.2.377
Feingold, A. (2009). Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychol. Methods 14, 43–53. doi: 10.1037/a0014699
Feingold, A. (2015). Confidence interval estimation for standardized effect sizes in multilevel and latent growth modeling. J. Consult. Clin. Psychol. 83, 157–168. doi: 10.1037/a0037721
Fredrickson, B. L., Cohn, M. A., Coffey, K. A., Pek, J., and Finkel, S. M. (2008). Open hearts build lives: positive emotions, induced through loving-kindness meditation, build consequential personal resources. J. Pers. Soc. Psychol. 95, 1045–1062. doi: 10.1037/a0013262
Galante, J., Galante, I., Bekkers, M. J., and Gallacher, J. (2014). Effect of kindness-based meditation on health and well-being: a systematic review and meta-analysis. J. Consult. Clin. Psychol. 82, 1101–1114. doi: 10.1037/a0037249
Gilbert, P. (2010). The Compassionate Mind. How to Use Compassion to Develop Happiness, Self-Acceptance and Well-Being. London: Constable.
Grant, A., and Dutton, J. (2012). Beneficiary or benefactor: are people more prosocial when they reflect on receiving or giving? Psychol. Sci. 23, 1033–1039. doi: 10.1177/0956797612439424
Grant, F., Guille, C., and Sen, S. (2013). Well-being and the risk of depression under stress. PLoS ONE 8, e67395. doi: 10.1371/journal.pone.0067395
Hendriks, T., Schotanus-Dijkstra, M., Graafsma, T., Bohlmeijer, E., and de Jong, J. (2020). Positive emotions as a potential mediator of a multi-component positive psychology intervention aimed at increasing mental well-being and resilience. Int. J. Appl. Posit. Psychol. 6, 1–21. doi: 10.1007/s41042-020-00037-5
Hendriks, T., Schotanus-Dijkstra, M., Hassankhan, A., de Jong, J., and Bohlmeijer, E. (2019). The efficacy of multi-component positive psychology interventions: a systematic review and meta-analysis of randomized controlled trials. J. Happiness Stud. 21, 357–390. doi: 10.1007/s10902-019-00082-1
Hendriks, T., Schotanus-Dijkstra, M., Hassankhan, A., Graafsma, T., Bohlmeijer, E., and Jong, J. (2018). The efficacy of positive psychology interventions from non-Western countries: a systematic review and meta-analysis. Int. J. Wellbeing 8, 71–98. doi: 10.5502/ijw.v8i1.711
Huber, M., van Vliet, M., Giezenberg, M., Winkens, B., Heerkens, Y., Dagnelie, P., et al. (2016). Towards a ‘patient-centred’operationalisation of the new dynamic concept of health: a mixed methods study. BMJ Open 6, e010091. doi: 10.1136/bmjopen-2015-010091
Jeste, D. V., Palmer, B. W., Rettew, D. C., and Boardman, S. (2015). Positive psychiatry: its time has come. J. Clin. Psychiatry 76, 675–683. doi: 10.4088/JCP.14nr09599
Kerr, S. L., O'Donovan, A., and Pepping, C. A. (2015). Can gratitude and kindness interventions enhance well-being in a clinical sample? J. Happiness Stud. 16, 17–36. doi: 10.1007/s10902-013-9492-1
Keyes, C. (2007a). Towards a mentally flourishing society: mental health promotion, not cure. J. Public Ment. Health 6, 4–7. doi: 10.1108/17465729200700009
Keyes, C. L. (2007b). Promoting and protecting mental health as flourishing: a complementary strategy for improving national mental health. Am. Psychol. 62, 95–108. doi: 10.1037/0003-066X.62.2.95
Keyes, C. L., Wissing, M., Potgieter, J. P., Temane, M., Kruger, A., and van Rooy, S. (2008). Evaluation of the mental health continuum-short form (MHC-SF) in setswana-speaking South Africans. Clin. Psychol. Psychother. 15, 181–192. doi: 10.1002/cpp.572
Keyes, C. L. M., Dhingra, S. S., and Simoes, E. J. (2010). Change in level of positive mental health as a predictor of future risk of mental illness. Am. J. Public Health 100, 2366–2371. doi: 10.2105/AJPH.2010.192245
Ko, K., Margolis, S., Revord, J., and Lyubomirsky, S. (2021). Comparing the effects of performing and recalling acts of kindness. J. Posit. Psychol. 16, 73–81. doi: 10.1080/17439760.2019.1663252
Kobau, R., Seligman, M. E., Peterson, C., Diener, E., Zack, M. M., Chapman, D., et al. (2011). Mental health promotion in public health: perspectives and strategies from positive psychology. Am J Public Health 101, e1–e9. doi: 10.2105/AJPH.2010.300083
Lamers, S. M. A., Westerhof, G. J., Bohlmeijer, E. T., ten Klooster, P. M., and Keyes, C. L. M. (2011). Evaluating the psychometric properties of the Mental Health Continuum-Short Form (MHC-SF). J. Clin. Psychol. 67, 99–110. doi: 10.1002/jclp.20741
Lamers, S. M. A., Westerhof, G. J., Glas, C. A. W., and Bohlmeijer, E. T. (2015). The bidirectional relation between positive mental health and psychopathology in a longitudinal representative panel study. J. Posit. Psychol. 10, 553–560. doi: 10.1080/17439760.2015.1015156
Layous, K., Katherine Nelson, S., and Lyubomirsky, S. (2013a). What is the optimal way to deliver a positive activity intervention? The case of writing about one's best possible selves. J. Happiness Stud. 14, 635–654. doi: 10.1007/s10902-012-9346-2
Layous, K., Lee, H., Choi, I., and Lyubomirsky, S. (2013b). Culture matters when designing a successful happiness-increasing activity:a comparison of the United States and South Korea. J. Cross Cult. Psychol. 44, 1294–1303. doi: 10.1177/0022022113487591
Leary, M. R., Tate, E. B., Adams, C. E., Batts Allen, A., and Hancock, J. (2007). Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J. Pers. Soc. Psychol. 92, 887–904. doi: 10.1037/0022-3514.92.5.887
Lyubomirsky, S., Dickerhoof, R., Boehm, J. K., and Sheldon, K. M. (2011). Becoming happier takes both a will and a proper way: an experimental longitudinal intervention to boost well-being. Emotion 11, 391–402. doi: 10.1037/a0022575
Lyubomirsky, S., and Layous, K. (2013). How do simple positive activities increase well-being? Curr. Dir. Psychol. Sci. 22, 57–62. doi: 10.1177/0963721412469809
Lyubomirsky, S., Sheldon, K. M., and Schkade, D. (2005). Pursuing happiness: the architecture of sustainable change. Rev. Gen. Psychol. 9, 111–131. doi: 10.1037/1089-2680.9.2.111
Lyubomirsky, S., Sousa, L., and Dickerhoof, R. (2006). The costs and benefits of writing, talking, and thinking about life's triumphs and defeats. J. Pers. Soc. Psychol. 90, 692–708. doi: 10.1037/0022-3514.90.4.692
Moher, D., Hopewell, S., Schulz, K. F., Montori, V., Gotzsche, P. C., Devereaux, P. J., et al. (2010). CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 340, c869. doi: 10.1136/bmj.c869
Mongrain, M., Chin, J. M., and Shapira, L. B. (2011). Practicing compassion increases happiness and self-esteem. J. Happiness Stud. 12, 963–981. doi: 10.1007/s10902-010-9239-1
Neely, M. E., Schallert, D. L., Mohammed, S. S., Roberts, R. M., and Chen, Y.-J. (2009). Self-kindness when facing stress: the role of self-compassion, goal regulation, and support in college students' well-being. Motiv. Emot. 33, 88–97. doi: 10.1007/s11031-008-9119-8
Neff, K. (2003). Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self Ident. 2, 85–101. doi: 10.1080/15298860390129863
Neff, K. D., Rude, S. S., and Kirkpatrick, K. L. (2007). An examination of self-compassion in relation to positive psychological functioning and personality traits. J. Res. Pers. 41, 908–916. doi: 10.1016/j.jrp.2006.08.002
Nelson, S. K., Della Porta, M. D., Jacobs Bao, K., Lee, H. C., Choi, I., and Lyubomirsky, S. (2015). ‘It’s up to you': experimentally manipulated autonomy support for prosocial behavior improves well-being in two cultures over six weeks. J. Posit. Psychol. 10, 463–476. doi: 10.1080/17439760.2014.983959
Nelson, S. K., Fuller, J. A., Choi, I., and Lyubomirsky, S. (2014). Beyond self-protection: Self-affirmation benefits hedonic and eudaimonic well-being. Pers. Soc. Psychol. Bull, 40, 998–1011, doi: 10.1177/0146167214533389
Nelson, S. K., Layous, K., Cole, S. W., and Lyubomirsky, S. (2016). Do unto others or treat yourself? The effects of prosocial and self-focused behavior on psychological flourishing. Emotion 16, 850–861. doi: 10.1037/emo0000178
Ouweneel, E., Blanc, P., and Schaufeli, W. (2014). On being grateful and kind: results of two randomized controlled trials on study-related emotions and academic engagement. J. Psychol. 148, 37–60. doi: 10.1080/00223980.2012.742854
Pennebaker, J. W. (2018). Expressive writing in psychological science. Perspect. Psychol. Sci. 13, 226–229. doi: 10.1177/1745691617707315
Radloff, L. S. (1977). The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1, 385–401.
Santor, D. A., Zuroff, D. C., Ramsay, J., Cervantes, P., and Palacios, J. (1995). Examining scale discriminability in the BDI and CES-D as a function of depressive severity. Psychol. Assess. 7, 131. doi: 10.1037/1040-3590.7.2.131
Schiffer, L. P., and Roberts, T.-A. (2018). The paradox of happiness: why are we not doing what we know makes us happy? J. Posit. Psychol. 13, 252–259. doi: 10.1080/17439760.2017.1279209
Schotanus-Dijkstra, M., Drossaert, C. H. C., Pieterse, M. E., Boon, B., Walburg, J. A., and Bohlmeijer, E. T. (2017a). An early intervention to promote well-being and flourishing and reduce anxiety and depression: a randomized controlled trial. Int. Interv. 9, 15–24. doi: 10.1016/j.invent.2017.04.002
Schotanus-Dijkstra, M., Pieterse, M. E., Drossaert, C. H. C., Walburg, J. A., and Bohlmeijer, E. T. (2019). Possible mechanisms in a multicomponent email guided positive psychology intervention to improve mental well-being, anxiety and depression: a multiple mediation model. J. Posit. Psychol. 14, 141–155. doi: 10.1080/17439760.2017.1388430
Schotanus-Dijkstra, M., Pieterse, M. E., Drossaert, C. H. C., Westerhof, G. J., de Graaf, R., ten Have, M., et al. (2016). What factors are associated with flourishing? Results from a large representative national sample. J. Happiness Stud. 17, 1351–1370. doi: 10.1007/s10902-015-9647-3
Schotanus-Dijkstra, M., ten Have, M., Lamers, S., de Graaf, R., and Bohlmeijer, E. T. (2017b). The longitudinal relationship between flourishing mental health and incident mood, anxiety and substance use disorders. Eur. J. Public Health 27, 563–568. doi: 10.1093/eurpub/ckw202
Sin, N. L., and Lyubomirsky, S. (2009). Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J. Clin. Psychol. 65, 467–487. doi: 10.1002/jclp.20593
Singer, J. D., and Willett, J. B. (2003). Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, NY: Oxford University Press.
Sirois, F. M., Molnar, D. S., and Hirsch, J. K. (2015). Self-compassion, stress, and coping in the context of chronic illness. Self Ident. 14, 334–347. doi: 10.1080/15298868.2014.996249
Slatcher, R. B., and Pennebaker, J. W. (2006). How do I love thee? Let me count the words: The social effects of expressive writing. Psychol. Sci. 17, 660–664. doi: 10.1111/j.1467-9280.2006.01762.x
Spitzer, R. L., Kroenke, K., Williams, J. B., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166, 1092–1097. doi: 10.1001/archinte.166.10.1092
Toepfer, N. F., Altmann, U., Risch, A. K., and Wilz, G. (2016). Examining explanatory mechanisms of positive and expressive writing: towards a resource-oriented perspective. J. Posit. Psychol. 11, 124–134. doi: 10.1080/17439760.2015.1037856
Van Boven, L., and Gilovich, T. (2003). To do or to have? That is the question. J. Pers. Soc. Psychol. 85, 1193–1202. doi: 10.1037/0022-3514.85.6.1193
Weiss, L. A., Westerhof, G. J., and Bohlmeijer, E. T. (2016). Can we increase psychological well-being? The effects of interventions on psychological well-being: a meta-analysis of randomized controlled trials. PLoS ONE 11, e0158092. doi: 10.1371/journal.pone.0158092
Wilson, T. D., and Gilbert, D. T. (2008). Explaining away: a model of affective adaptation. Perspect. Psychol. Sci. 3, 370–386. doi: 10.1111/j.1745-6924.2008.00085.x
Wiwad, D., and Aknin, L. B. (2017). Motives matter: the emotional consequences of recalled self-and other-focused prosocial acts. Motiv. Emot. 41, 730–740. doi: 10.1007/s11031-017-9638-2
Wood, A. M., and Joseph, S. (2010). The absence of positive psychological (eudemonic) well-being as a risk factor for depression: a ten year cohort study. J. Affect. Disord. 122, 213–217. doi: 10.1016/j.jad.2009.06.032
Keywords: kindness, prosocial behavior, self-focused behavior, well-being, positive psychology intervention, flourishing, anxiety, depression
Citation: Nelson-Coffey SK, Bohlmeijer ET and Schotanus-Dijkstra M (2021) Practicing Other-Focused Kindness and Self-Focused Kindness Among Those at Risk for Mental Illness: Results of a Randomized Controlled Trial. Front. Psychol. 12:741546. doi: 10.3389/fpsyg.2021.741546
Received: 14 July 2021; Accepted: 13 September 2021;
Published: 14 October 2021.
Edited by:
Jesus Alfonso Daep Datu, The Education University of Hong Kong, Hong Kong, SAR ChinaReviewed by:
Humbelina Robles Ortega, University of Granada, SpainCopyright © 2021 Nelson-Coffey, Bohlmeijer and Schotanus-Dijkstra. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marijke Schotanus-Dijkstra, bS5zY2hvdGFudXNAdXR3ZW50ZS5ubA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.