
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 18 August 2021
Sec. Personality and Social Psychology
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.713070
This article is part of the Research TopicEating Disorders and Weight disorders: Assessment, Early Diagnosis, Prognosis, Treatment Outcome and the Role of Potential Psychological and Social FactorsView all 17 articles
A correction has been applied to this article in:
Corrigendum: From Deficits in Emotional Intelligence to Eating Disorder Symptoms: A Sequential Path Analysis Approach Through Self-Esteem and Anxiety
Past studies have reported emotional intelligence (EI) as a relevant factor in development and maintenance of eating disorders (ED), as well as in increasing self-esteem and reducing anxiety. Similarly, research has showed that anxiety and self-esteem are positively and negatively associated to ED criteria, respectively. However, no prior studies have yet tested the multiple intervening roles of both self-esteem and anxiety as potential mediators of the association between EI and ED symptomatology. The present study aims to bridge these gaps by testing a sequential path model. Specifically, we examine the potential sequential mediation effects of self-esteem-anxiety on the link between EI and ED. A sample composed of 516 Spanish undergraduate students and community adults completed measures of EI, self-esteem, anxiety, and ED symptomatology. The results show that high levels of EI were positively associated with self-esteem and negatively associated with anxiety and ED symptoms. Anxiety was positively associated to ED symptoms, while self-esteem levels were negatively linked to ED symptoms. Moreover, path analyses showed that self-esteem and anxiety fully mediated the relationship between EI and ED symptoms in sequence. These findings suggest that EI plays a key role in reducing symptomatology of ED through increased self-esteem and reduced anxiety symptoms, providing novel evidence regarding psychological mechanisms through which EI contributes to a reduction of ED symptomatology. Implications for assessing and improving these psychological resources in ED preventive programs are discussed.
Eating disorders (ED) are persistent disturbances of eating or eating-related behaviors that result in significant impairments in psychosocial functioning and physical health (American Psychiatric Association (APA), 2013). In the last two decades, the worldwide prevalence of ED has increased from 3.5 to 7.8% (Galmiche et al., 2019), and the rate remains significantly higher among females (American Psychiatric Association (APA), 2013). Anxiety disorders and depression are among the most common comorbid diagnoses in ED (Godart et al., 2002, 2007).
Theoretical background and empirical evidence have supported the idea that deficits in the processing and managing of emotions play a key role in the development and maintenance of ED (Polivy and Herman, 1993) and that difficulties with the regulation of emotions are related with ED psychopathology (Corstorphine, 2006; Fox, 2009; Haynos and Fruzzetti, 2011; Lavender et al., 2015; Rowsell et al., 2016). For example, some meta-analytic findings have confirmed that high levels of negative emotionality increase the risk of eating pathology (Stice, 2002). Accordingly, consistent with the transdiagnostic cognitive-behavioral model for ED (Fairburn et al., 2003), mood changes (along with external events) play a relevant role in both the maintenance and relapse of ED. In fact, a broad form of enhanced cognitive-behavioral therapy (CBT-Eb; Fairburn et al., 2009), including mood intolerance, clinical perfectionism, low self-esteem, and interpersonal difficulties, along with the well-established cognitive-behavioral therapy (CBT) for ED (National Institute for Clinical Excellence (NICE), 2004; Wilson, 2005) have shown better results compared to CBT alone, both for ED patients with minor and subclinical symptoms and for those with more relevant psychopathology symptoms (CBT-Eb; Fairburn et al., 2009). Similarly, the cognitive-emotional-behavioral therapy (CEBT) (Corstorphine, 2006), including assessment of emotions and emotional management techniques, has been shown to improve participants' emotional eating behaviors, as well as their self-esteem, depression, and anxiety (Campbell, 2012).
Emotional intelligence (EI) is a relatively new construct related to emotions that comprises a set of basic emotional skills. From an ability perspective, EI is defined as “the ability of people to perceive, use, understand and manage emotions” (Mayer and Salovey, 1997; p. 532). This EI theoretical framework involves four basic emotional dimensions: emotional perception and expression, emotional facilitation, emotional understanding, and emotional regulation. From this perspective, emotional regulation is defined as the ability to manage both positive and negative emotions in themselves and in others, integrating emotion and cognition effectively (Mayer et al., 2016). These emotional skills can be developed in clinical settings through systematic and comprehensive EI training (Mayer et al., 2000; Kotsou et al., 2018).
In the last decade, an emerging line of research has typically shown the significant relationship between EI and ED symptoms. For example, some prior research has found that individuals with some EI deficits are more prone to display disordered eating attitudes and behaviors (Costarelli et al., 2009; Pettit et al., 2009; Filaire et al., 2010; Zysberg and Rubanov, 2010; Hambrook et al., 2012; Zavala and López, 2012; Zysberg, 2013; Zysberg and Tell, 2013; Gardner et al., 2014; Koch and Pollatos, 2015; Cuesta et al., 2017; Peres et al., 2018; Foye et al., 2019). In addition, recent systematic reviews have reported that these abilities are relevant factors in both the development and maintenance of ED (Romero-Mesa et al., 2020; Giusti et al., 2021). These findings provide some preliminary support for the role of emotions in disordered eating attitudes with a view to the prevention and management of ED and point to the potential use of EI measures to identify individuals at risk of ED.
Beyond this direct association between EI and ED symptoms, other potential underlying processes have been theorized through which EI might impact ED symptoms. Two of these individual psychological mechanisms considered to be relevant mediators might be self-esteem and anxiety. A growing body of research has supported the theory that deficits in emotional skills are significant predictors of reduced self-esteem domains (Fernández-Berrocal et al., 2006; Hasanvand and Khaledian, 2012; Bibi et al., 2016). Likewise, it has been found that people with high levels of anxiety typically report difficulty in accurately perceiving, using, understanding, and managing their own emotions (Fernández-Berrocal et al., 2006; Connor and Slear, 2009; Kousha et al., 2018). Taken together, these findings suggest that people with high levels of EI feel more security and less stress and also believe in their abilities, showing higher feelings of self-worth, goodness, and self-respect.
On the other hand, there is some theoretical and empirical support that self-esteem and anxiety are risk factors for ED symptoms. As mentioned above, improving self-esteem in combination with other components resulted in a more effective treatment for ED patients compared to CBT therapy alone. In addition, several studies have consistently corroborated a negative relationship between self-esteem and ED criteria (Silverstone, 1990, 1992; Silvera et al., 1998). Besides, numerous studies have found that high levels of anxiety are a well-recognized symptom in individuals with ED (Arnow et al., 1995; Levinson and Rodebaugh, 2012; Menatti et al., 2015) and that anxiety worsens the ED psychopathology (Brand-Gothelf et al., 2014). Given the high comorbidity between ED and anxiety disorders and the fact that both disorders share the same components (evaluative, affective, and somatic; Kaye et al., 2004), the robust relationship between ED and anxiety is not surprising.
Along with the individual role of self-esteem and anxiety in ED symptomatology, several studies have tested the combined role of self-esteem and anxiety on ED. For example, a recent study found that self-esteem (together with mood dysregulation) moderated the association between levels of anxiety/depression and greater deterioration of ED (Sander et al., 2021). In addition, Aloi and Segura-García (2016) found that low self-esteem had an indirect effect on the risk of developing an ED through the mediating action of anxiety.
There is also evidence that anxiety and self-esteem (considered independently) play a relevant mediating role between EI and ED symptoms. For example, prior findings have found that social anxiety mediated the relationship between EI and ED risk (Li, 2018). Thus, Hambrook et al. (2012) found that self-reported anxiety levels mediated the observed relationship between EI and anorexia nervosa (AN).
In sum, there is empirical support for the link between EI, higher self-esteem, and reduced anxiety, as well as between levels of self-esteem and anxiety and ED symptomatology. It has also been pointed out that individuals with higher EI use their ability to maintain a global feeling of self-worth when appropriate and effectively manage a distressed mood when faced with negative events that are considered key in the development of ED symptoms. Hence, the assessment of self-esteem and anxiety as potential mediators in the association between EI and the symptomatology of ED seems to be justified (Hambrook et al., 2012; Li, 2018). However, most of these studies only examined the role of a single mediator in the linkage EI-ED symptomatology and have rarely evaluated effects of the mediators concurrently. Specifically, and to the best of our knowledge, no prior research has examined the cumulative effect of self-esteem and anxiety on the relationship between EI and ED symptomatology. Including these mediators in the serial model would help unveil the underlying mechanisms through which EI influences ED and would also help clinicians and educators to focus on the factors with the most clinical relevance for the prevention and treatment of ED symptomatology. Therefore, the purpose of the present study is 2-fold: first, we sought to examine the relations between EI, self-esteem, anxiety, and ED symptomatology. Second, we sought to determine whether self-esteem and anxiety mediated the relation between EI and ED symptoms in sequence. Since prior studies have found that individuals with higher self-esteem are more likely to have lower levels of anxiety (Sowislo and Orth, 2013), and that self-esteem has an indirect effect on ED risk, as mediated by anxiety (Aloi and Segura-García, 2016), we expected that both mediators might act in this sequence; that is, individuals with high positive cognitions about themselves would have lower levels of anxiety, which in turn would lead them to an amelioration of ED symptomatology. Overall, considering prior research on the significant associations between EI, self-esteem, anxiety and ED symptoms, we developed the following research hypotheses:
Hypothesis 1. EI is positively associated with higher self-esteem and negatively linked to anxiety and ED symptoms.
Hypothesis 2. (Single mediation). EI predicts higher levels of self-esteem and lower levels of anxiety. These variables, in turn, independently predict lower levels of ED symptomatology.
Hypothesis 3. (Sequential mediation). Self-esteem and anxiety might serve as mediators in a sequential mediation model between EI and ED symptoms; that is, EI positively predicts self-esteem, leading to lower levels of anxiety, further decreasing ED symptomatology.
The study sample consisted of 516 Spanish undergraduate students and community adults (319 females and 197 males) located in Southern Spain. Their ages ranged from 18 to 77 years, with a mean age of 38.89 years (SD = 14.76) (see Table 1). Given that the prevalence of ED in elderly women (aged 65–94 = 3.25%) has been found to be comparable to young women (Conceição et al., 2017) and that, according to a systematic review, late-life onset ED do continue to occur in the elderly (Lapid et al., 2010), we have not excluded older people from our study.
The educational level in the present sample was as follows: 15 (2.9%) had no formal education, 73 (14.1%) had a primary-level education, 120 (23.3%) had not completed secondary school, 57 (11.0%) had completed secondary school, 186 (36.0%) had completed University Studies, and 65 (12.6%) had post-graduate studies.
The percentage of at-risk participants (i.e., those scoring ≥ 20 in the EAT-26) was 6.2% (32 out of 516).
University and community participants were solicited using non-probabilistic convenience sampling techniques via an online survey format. A student-recruited sampling methodology was used following guidelines by Wheeler et al. (2014), which allowed us to access a community sample from a University setting. The community participants were recruited with the assistance of students enrolled in a psychology course at university, who were asked to recruit at minimum two adults over the age of 30 through their personal network and then administer the online version of the questionnaires to them. The online survey was designed so that incomplete questionnaires could not be saved, which allowed only the whole completed questionnaires to be received. Student participants earned points for their participation in the study. Before getting to the online survey, participants were informed that the survey was about eating habits and emotions, and that their participation was entirely voluntary. All participants provided written informed consent according to the Declaration of Helsinki. The procedure was approved by the ethics committee of the University of Málaga (104-2020-H). The administration procedure lasted for ~30 min. The sample was obtained from May 2019 to November 2020. The percentage of participation among students was of 78.28%.
The following well-validated measures were used.
The Wong Law Emotional Intelligence Scale (WLEIS; Wong and Law, 2002), in its Spanish version (WLEIS-S; Extremera et al., 2019), was selected as a self-reported ability EI scale based on the theoretical framework of Mayer and Salovey (1997). The WLEIS is a short and cost-free EI measure that consists of 16 items that measure four EI aspects: appraisal of one's own emotions, appraisal of others' emotions, use of emotion, and regulation of emotion, e.g., “I always tell myself I am a competent person.” Questions are scored on a 7-point scale ranging from totally disagree to totally agree. Total scores range from 16 to 112. Higher scores indicate a higher level of EI (Extremera et al., 2019). In this study, Cronbach's alpha was 0.91.
The Spanish version of the Eating Attitudes Test (EAT-26; Garner et al., 1982; Rivas et al., 2010) was used as a measure of risk of ED and the presence of disordered eating attitudes. The EAT-26 is a non-clinical self-report 26-item measure; e.g., “feel extremely guilty after eating.” It includes three subscales that measure: (1) diet and concern for thinness, (2) bulimia and concern for food, and (3) oral control. Questions are scored on a 6-point scale ranging from “always” scoring 3, “most often” scoring 2, “often” scoring 1, “sometimes” scoring 0, “rarely” scoring 0, and “never” scores as 0. Only one of its items scores reversely. The range of the total score is 0–78. A total score ≥ 20 often indicates a risk of ED. A higher score indicates a higher risk of ED. The Spanish version has shown satisfactory reliability (Rivas et al., 2010). Cronbach's alpha was 0.80.
The Rosenberg Self-Esteem Scale (RSE; Rosenberg, 1965), in its Spanish version (RSES; Martín-Albo et al., 2007), was selected as a self-reported scale for direct evaluation of global self-esteem. The RSE contains brief statements that reflect general feelings about oneself. It consists of 10 items that are answered on a 4-point Likert scale (from totally agree to totally disagree); e.g., “I wish I could have more respect for myself.” For correction, the scores of five of its items must be inverted. The total score ranges from 10 to 40. Scores ≥ 30 indicate optimal self-esteem, between 26 and 29 indicate average self-esteem (needs improvement), and scores ≤ 25 points indicate significant self-esteem problems (Martín-Albo et al., 2007). Cronbach's alpha was 0.78.
The self-reported anxiety dimension of the Spanish version of the Depression Anxiety Stress Scale (DASS-21; Lovibond and Lovibond, 1995; Bados et al., 2005) was used. It consists of 7 items with a Likert-type response format with four alternatives, which are ordered on a scale from 0 to 3 points; e.g., “I felt scared without any good reason.” The score varies between 0 and 21 points. The recommended cut-off scores for severity labels are: 0–7 = normal; 8–9 = mild; 10–14 = moderate; 15–19 = severe; 20+ = extremely severe. Cronbach's alpha in this study was 0.82.
After calculating descriptive statistics and computing the bivariate correlation between EI, self-esteem, anxiety, and ED symptoms, the SPSS macro PROCESS (Hayes, 2018) was used to conduct multiple mediation analyses for testing the potential mediating role of self-esteem and anxiety in the linkage between EI-ED symptomatology. A bootstrapping method with 5,000 esteem resamples was used to calculate overall indirect effects and specific indirect effects. The direct and indirect effects are considered to be statistically significant if 95% of the bootstrap confidence intervals do not contain zero. Thus, this procedure enables multiple mediators to be examined and determines the independent effect of each mediator while controlling for the other. Preliminary ANOVA and t-tests showed differences according to age and sex, respectively, in ED symptoms, self-esteem and anxiety. Female participants scored significantly higher than males in ED symptoms and anxiety, and lower in self-esteem (all ps < 0.01); younger participants scored marginally significantly higher than older ones in ED symptoms and anxiety (ps < 0.10) and significantly lower in self-esteem (p <0.001). Therefore, sex and age were entered as covariates to control any potential confounding effects.
Descriptive statistics, response ranges, normative data, reliability coefficients, and correlations among the study variables are presented in Table 2. The column “Response ranges” indicates the minimum and maximum possible scores in the questionnaires. The column “Normative data M (SD)” indicates means and standard deviations from normative data. For EI, self-esteem, and anxiety, normative data correspond to the information provided by Spanish adaptations of the questionnaires. For the EAT-26, since the Spanish adaptation of EAT-26 was performed with adolescents, we have included the data from Johnson and Bedford (2004), who employed a Canadian sample comparable to ours (men and women, age range 18–94). As Table 2 shows, EI was positively correlated to self-esteem and negatively associated to anxiety. As expected, self-esteem was significantly and negatively associated with ED symptoms, while anxiety levels showed significant and positive associations with symptoms of ED. Finally, EI was negative and significantly linked to ED symptomatology.
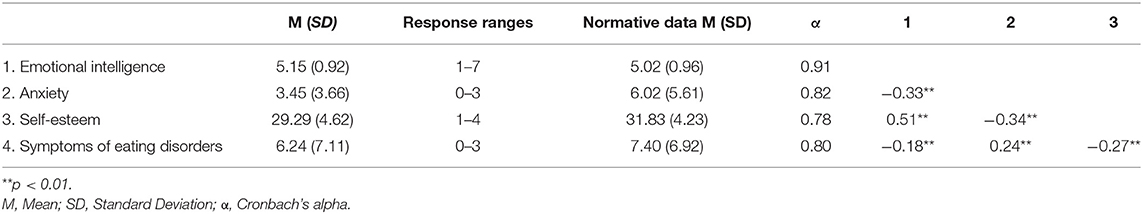
Table 2. Descriptive statistics, response ranges, normative data, reliability, and bivariate correlations.
We examined whether the relationship between EI and ED symptoms was sequentially mediated by self-esteem and anxiety. Both age and sex were added as control variables. Results of the mediation analyses are presented in Table 3.
As shown in Figure 1, the three hypothetical mediating effects were supported. First, the specific indirect effects of EI on ED symptoms through self-esteem [EI → Self-esteem → ED symptoms] were supported (B = −0.09, SE = 0.03; 95% CI = −0.15, −0.04). Second, anxiety was found to mediate the association between EI and ED symptoms [EI → Anxiety → ED symptoms] (B = −0.03, SE = 0.01; 95% CI = −0.066, −0.009). Third, the sequential pathway of EI → Self-esteem → Anxiety → ED symptoms, was significant (B = −0.02, SE = 0.01; 95% CI = −0.031, −0.005). Accordingly, higher levels of EI were serially associated with higher self-esteem, lower anxiety, and finally lower ED symptoms. Thus, the residual direct pathway between EI and ED symptoms was no longer significant (b = −0.03, p = 0.578). Therefore, self-esteem and anxiety fully mediated the link between EI and ED symptoms. This final serial mediation model was significant, accounting for 11% of the variance in ED symptoms [R2 adj = 0.11; F(5, 510) = 12.08; p <0.001].
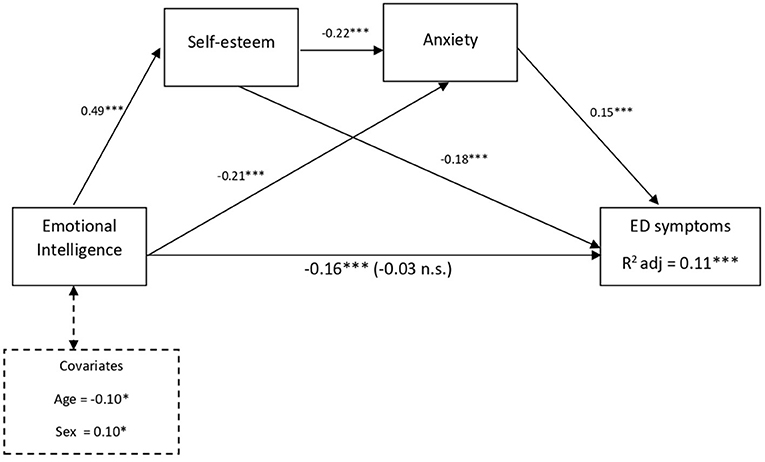
Figure 1. Multiple mediation model for the effect of EI and ED symptoms via self-esteem and anxiety controlling for age and sex as covariates. Total effect (c-path) is given in parentheses; standardized coefficients; *p < 0.05; ***p < 0.001.
The present study examined whether self-esteem and anxiety, which previous literature confirm as relevant variables related to ED symptomatology, mediated the relationship between EI and ED symptomatology within a Spanish college student and community sample.
The results of path analyses showed that self-esteem and anxiety play a fully sequential mediating role between EI and ED symptomatology, suggesting that EI was positively linked to higher self-esteem and lower anxiety, which in turn predicted lower levels of ED symptoms. The findings support the notion that EI decreases ED symptoms indirectly, suggesting that higher self-esteem and decreased anxiety may be possible underlying mechanisms through which emotional abilities contribute to reducing ED symptoms. These results are consistent with previous studies that found a mediating role for anxiety in the relationship between EI and ED (Hambrook et al., 2012; Li, 2018). Moreover, the serial mediation was also significant, suggesting that EI is associated with greater self-esteem, which subsequently reduces anxiety, thus predicting lower ED symptoms. These findings agree with previous meta-analytic research corroborating the robust effect of negative feelings of self-worth on anxiety (Sowislo and Orth, 2013). Our results are also consistent with past studies showing that anxiety mediates the role of self-esteem on the development of ED symptoms (Aloi and Segura-García, 2016) and contributes to the current literature by extending our understanding of the mechanism that underlies the linkage of EI and ED symptomatology.
The present study extends the understanding of the role of EI, self-esteem, and anxiety on ED symptoms in several ways. It provides further support for researchers who argue that low levels of self-esteem (Silverstone, 1990, 1992; Silvera et al., 1998) and high levels of anxiety (Arnow et al., 1995; Kaye et al., 2004; Levinson and Rodebaugh, 2012; Menatti et al., 2015) are significantly associated with ED symptoms. Our findings reinforce these models by suggesting that deficits in EI might lead to reduced levels of self-esteem and high levels of anxiety, which are associated with higher ED symptoms. Our data also support the transdiagnostic CBT model for ED (Fairburn et al., 2003), which includes mood changes as independent variables that affect ED symptomatology, as well as the suitability of including treatment for emotional abilities and low self-esteem, as did the broad form of enhanced CBT (CBT-Eb; Fairburn et al., 2009). Our results also support the suitability of CEBT (Corstorphine, 2006) for the treatment of ED, as this extended version of CBT incorporates the assessment as well as emotion-management techniques. Accordingly, the findings of this study have theoretical implications, as they suggest that alterations in self-esteem might be partially responsible for the mood changes that trigger dysfunctional eating behaviors (transdiagnostic CBT model; Fairburn et al., 2003). These findings also have practical implications for the prevention and treatment of ED. The inclusion of programs on EI training, self-esteem promotion, and anxiety management in school curricula could minimize the acquisition and maintenance of ED in the child-adolescent population. Likewise, clinicians could incorporate EI training and psychoeducation on how emotions relate to ED symptoms, which could help patients increase their ability to understand and manage their emotional states. Therapists could also include specific strategies for anxiety management along with the other components of CBT-Eb (Fairburn et al., 2009) and CEBT (Corstorphine, 2006). All of this could lead to promising and possibly more effective treatments for both ED patients and those at risk of ED. Even less complex ED interventions focused only on increasing emotional competences would enhance individuals' self-esteem, thereby reducing anxiety symptoms, which in turn would lead to an amelioration of ED symptomatology. Moreover, if interventions focused on EI training were reinforced with specific interventions that worked to enhance self-esteem and managing anxiety, the effects of EI on ED symptomatology could be optimized.
The findings of this research should be interpreted in the context of its limitations. Our study used a cross-sectional design, which precludes any causal inference. The order of the variables included in the serial model is based on empirical evidence (Sowislo and Orth, 2013; Aloi and Segura-García, 2016); however, the cross-sectional design of our study precludes causal assumptions. Further research in this area should incorporate longitudinal designs that allow for the study of causal directions between study variables. Also, we used non-clinical and non-representative convenience samples, so it is not possible to generalize these results to clinical samples with diagnoses of ED or to more stratified random samples. Comparing these results with a clinical sample and using cross-validation and random sampling would help confirm whether there are essential differences in the deficits and dynamics of personal resources associated with ED symptoms. Therefore, future studies should incorporate both clinical and non-clinical samples.
Despite its limitations, this research revealed that adults with higher levels of EI (compared to those with low EI) are more likely to have higher levels of self-esteem, which would lead to lower levels of anxiety, which in turn would lead to lower ED symptomatology. These findings open the door to future research concerning the role of emotional competences in ED symptoms; it might be fundamental to consider both levels of self-esteem and anxiety when working with adults who display both deficits in EI and ED symptoms. Also, this research supports the relevance of including training to improve EI skills, foster self-esteem, and reduce anxiety symptoms as a specific treatment for ED or even as additional components of the CBT-Eb.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by The Research Ethics Committee of the University of Málaga (104-2020-H). The patients/participants provided their written informed consent to participate in this study.
MP-F, JR-M, and NE created and organized the study. MP-F and JR-M collected the data. MP-F and NE analyzed the data, critically reviewed the manuscript, and provided constructive comments. JR-M wrote the first draft. MP-F wrote the reviewed draft. All authors contributed to the article and approved the submitted version.
This research has been supported and funded in part by research projects from the University of Málaga and Junta de Andalucía/FEDER (UMA18-FEDERJA-147) and PAIDI Group CTS-1048 (Junta de Andalucía). This work was also supported by the Spanish Ministry of Education and Vocational Training (FPU16/02238).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Aloi, M., and Segura-García, C. (2016). Anxiety and depression mediate the role of low self-esteem and low self-directedness in the development of eating disorders. Int. J. Adolesc. Med. Health. 31:84. doi: 10.1515/ijamh-2016-0084
American Psychiatric Association (APA) (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Washington, DC: American Psychiatric Pub.
Arnow, B., Kenardy, J., and Agras, W. S. (1995). The emotional eating scale: the development of a measure to assess coping with negative affect by eating. Int. J. Eat. Disord. 18, 79–90. doi: 10.1002/1098-108X(199507)18:13.0.CO;2-V
Bados, A., Solanas, A., and Andrés, R. (2005). Psychometric properties of the Spanish version of Depression, Anxiety and Stress Scales (DASS). Psicothema 17, 679–683.
Bibi, S., Saqlain, S., and Mussawar, B. (2016). Relationship between emotional intelligence and self-esteem among Pakistani University Students. J. Psychol. Psychother. 6:279. doi: 10.4172/2161-0487.1000279
Brand-Gothelf, A., Leor, S., Apter, A., and Fennig, S. (2014). The impact of comorbid depressive and anxiety disorders on severity of anorexia nervosa in adolescent girls. J. Nerv. Ment. Dis. 202, 759–762. doi: 10.1097/NMD.0000000000000194
Campbell, H. (2012). Managing emotional eating. Mental Health Pract. 15:8. doi: 10.7748/mhp2012.05.15.8.34.c9101
Conceição, E. M., Gomes, F. V., Vaz, A. R., Pinto-Bastos, A., and Machado, P. P. (2017). Prevalence of eating disorders and picking/nibbling in elderly women. Int. J. Eat. Disord. 50, 793–800. doi: 10.1002/eat.22700
Connor, B., and Slear, S. (2009). Emotional intelligence and anxiety; emotional intelligence and resiliency. Int. J. Learn. 16, 249–260. doi: 10.18848/1447-9494/CGP/v16i01/46089
Corstorphine, E. (2006). Cognitive-emotional-behavioural therapy for the eating disorders: working with beliefs about emotions. Eur. Eat. Disord. Rev. 14, 448–461. doi: 10.1002/erv.747
Costarelli, V., Demerzi, M., and Stamou, D. (2009). Disordered eating attitudes in relation to body image and emotional intelligence in young women. J. Hum. Nutr. Diet. 22, 239–245. doi: 10.1111/j.1365-277X.2009.00949.x
Cuesta, C., González, I., and García, L. M. (2017). The role of trait emotional intelligence in body dissatisfaction and eating disorder symptoms in preadolescents and adolescents. Pers. Individ. Differ. 126, 1–6. doi: 10.1016/j.paid.2017.12.021
Extremera, N., Rey, L., and Sánchez-Álvarez, N. (2019). Validation of the Spanish version of the Wong Law Emotional Intelligence Scale (WLEIS-S). Psicothema 31, 94–100. doi: 10.7334/psicothema2018.147
Fairburn, C. G., Cooper, Z., Doll, H., O'Connor, M., Bohn, K., Hawker, D., et al. (2009). Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am. J. Psychiatry 166, 311–319. doi: 10.1176/appi.ajp.2008.08040608
Fairburn, C. G., Cooper, Z., and Shafran, R. (2003). Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav. Res. Ther. 41, 509–528. doi: 10.1016/s0005-7967(02)00088-8
Fernández-Berrocal, P., Alcaide, R., Extremera, N., and Pizarro, D. (2006). The role of emotional intelligence in anxiety and depression among adolescents. Individ. Differ. Res. 4, 16–27.
Filaire, E., Larue, J., and Rouvieux, M. (2010). Eating behaviours in relation to emotional intelligence. Int. J. Sports Med. 32, 309–315. doi: 10.1055/s-0030-1269913
Fox, J. (2009). A qualitative exploration of the perception of emotions in anorexia nervosa: a basic emotion and developmental perspective. Clin. Psychol. Psychother. 16, 276–302. doi: 10.1002/cpp.631
Foye, U., Hazlett, D. E., and Irving, P. (2019). Exploring the role of emotional intelligence on disorder eating. Eat. Weight Disord. 24, 299–306. doi: 10.1007/s4051 9-018-0629-4
Galmiche, M., Déchelotte, P., Lambert, G., and Tavolacci, M. P. (2019). Prevalence of eating disorders over the 2000–2018 period: a systematic review literature. Am. J. Clin. Nutr. 109, 1402–1413. doi: 10.1093/ajcn/nqy342
Gardner, K. J., Quinton, S., and Qualter, P. (2014). The role of trait and ability emotional intelligence in bulimic symptoms. Eat. Behav. 15, 237–240. doi: 10.1016/j.eatbe h.2014.02.002
Garner, D. M., Olmsted, M. P., Bohr, Y., and Garfinkel, P. E. (1982). The eating attitudes test: psychometric features and clinical correlates. Psychol. Med. 12, 871–878. doi: 10.1017/s0033291700049163
Giusti, E. M., Manna, C., Scolari, M., Mestre, J. M., Prevendar, T., Castelnuovo, G., et al. (2021). The relationship between emotional intelligence, obesity and eating disorder in children and adolescents: a systematic mapping review. Int. J. Environ. Res. Public Health. 18:2054. doi: 10.3390/ijerph18042054
Godart, N. T., Flament, M. F., Perdereau, F., and Jeammet, P. (2002). Comorbidity between eating disorders and anxiety disorders: A review. Int. J. Eat. Disord. 2, 253–270. doi: 10.1002/eat.10096
Godart, N. T., Perdereau, F., Rein, Z., Berthoz, S., Wallier, J., Jeammet, P., et al. (2007). Comorbidity studies of eating disorders and mood disorders. Critical review of the literature. J. Affect. Disord. 97, 37–49. doi: 10.1016/j.jad.2006.06.023
Hambrook, D., Brown, G., and Tchanturia, K. (2012). Emotional intelligence in anorexia nervosa: is anxiety a missing piece of the puzzle? Psych. Res. 200, 12–19. doi: 10.1016/j.psych res.2012.05.017
Hasanvand, B., and Khaledian, M. (2012). The relationship of emotional intelligence with self-esteem and academic progress. Int. J. Psychol. Behav. Sci. 2, 231–236. doi: 10.5923/j.ijpbs.20120206.06
Hayes,. A. F. (2018). Introduction to Mediation, Moderation, and Conditional Process Analysis Second Edition: A Regression-Based Approach. New York, NY: The Guilford Press
Haynos, A. F., and Fruzzetti, A. E. (2011). Anorexia nervosa as a disorder of emotion dysregulation: evidence and treatment implications. Clin. Psychol. Sci. Pract. 18, 183–202. doi: 10.1111/j.1468-2850.2011.01250.x
Johnson, C. S., and Bedford, J. (2004). Eating attitudes across age and gender groups: a Canadian study. Eat Weight Disord. 9, 16–23.
Kaye, W. H., Bulik, C. M., Thornton, L., Barbarich, N., and Masters, K. (2004). Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am. J. Psychiatry 161, 2215–2221. doi: 10.1176/appi.ajp.161.12.2215
Koch, A., and Pollatos, O. (2015). Reduced facial emotion recognition in overweight and obese children. J. Psychosomat. Res. 79, 635–639. doi: 10.1016/j.jpsychores.2015.06.005
Kotsou, I., Mikolajczak, M., Heeren, A., Grégoire, J., and Leys, C. (2018). Improving emotional intelligence: a systematic review of existing workand future challenges. Emotion Rev. 11, 151–165. doi: 10.1177/1754073917735902
Kousha, M., Bagheri, H. A., and Heydarzadeh, A. (2018). Emotional intelligence and anxiety, stress, and depression in Iranian resident physicians. J. Family Med. Prim. Care. 7, 420–424. doi: 10.4103/jfmpc.jfmpc_154_17
Lapid, M. I., Prom, M. C., Burton, M. C., McAlpine, D. E., Sutor, B., and Rummans, T. A. (2010). Eating disorders in the elderly. Int. Psychogeriatr. 22:523. doi: 10.1017/S1041610210000104
Lavender, J., Wonderlich, S., Engel, S., Gordon, K., Kaye, W., and Mitchell, J. (2015). Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clin Psychol Rev. 40, 111–122. doi: 10.1016/j.cpr.2015.05.010
Levinson, C. A., and Rodebaugh, T. L. (2012). Social anxiety and eating disorder comorbidity: The role of negative social evaluation fears. Eat. Behav. 13, 27–35. doi: 10.1016/j.eatbeh.2011.11.006
Li,. Y. (2018). Social anxiety and eating disorder risk among Chinese adolescents: the role of emotional intelligence. Sch. Ment. Health. 10, 264–274. doi: 10.1007/s12310-018-9257-4
Lovibond, P. F., and Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck. Depression and anxiety inventories. Behav. Res. Ther. 33, 335–343. doi: 10.1016/0005-7967(94)00075-u
Martín-Albo, J., Núñez, J. L., Navarro, J. G., and Grijalvo, F. (2007). The rosenberg self-esteem scale: translation and validation in University students. Span. J. Psychol. 10, 458–467. doi: 10.1017/S1138741600006727
Mayer, J. D., Caruso, D. R., and Salovey, P. (2016). The ability model of emotional intelligence: principles and updates. Emot. Rev. 8, 290–300. doi: 10.1177/1754073916639667
Mayer, J. D., and Salovey, P. (1997). “What is emotional intelligence?” in Emotional Development and Emotional Intelligence: Implications for Educators, eds P. Salovey and D. Sluyter (New York, NY: Basic Books).
Mayer, J. D., Salovey, P., and Caruso, D. (2000). “Models of emotional intelligence,” in Handbook of Intelligence, ed R. J. Sternberg (New York, NY: Cambridge).
Menatti, A. R., Hopkins, L. B., DeBoer, L., Weeks, J. W., and Heimberg, R. G. (2015). Social anxiety and associations with eating psychopathology: mediating effects of fears of evaluation. Body Image 14, 20–28. doi: 10.1016/j.bodyim.2015.02.003
National Institute for Clinical Excellence (NICE) (2004). Eating Disorders—Core Interventions in the Treatment and Management of anoreXia Nervosa, Bulimia Nervosa and Related Eating Disorders. Available online at: http://www.nice.org.uk (accessed October 9, 2009).
Peres, V, Corcos, M., Robin, M., and Pham-Scottez, A. (2018). Emotional intelligence, empathy and alexithymia in anorexia nervosa during adolescence. Eat. Weight Disord. 25, 1–8. doi: 10.1007/s4051 9-018-0482-5
Pettit, M. L., Jacobs, S. C., Page, K. S., and Porras, C. V. (2009). An assessment of perceived emotional intelligence and eating attitudes among college students. Am. J. Health Educ. 41, 46–52. doi: 10.1080/19325 037.2010.10599126
Polivy, J., and Herman, C. P. (1993). Etiology of Binge Eating: Psychological Mechanisms. London: Guilford Press.
Rivas, T., Bersabé, R., Jiménez, M., and Berrocal, C. (2010). The Eating Attitudes Test (EAT-26): reliability and validity in Spanish female samples. Span. J. Psychol. 13, 1044–1056. doi: 10.1017/S1138741600002687
Romero-Mesa, J., Peláez-Fernández, M. A., and Extremera, N. (2020). Emotional intelligence and eating disorders: a systematic review. Eat. Weight Disord. 26, 1287–1301. doi: 10.1007/s40519-020-00968-7
Rosenberg, M. (1965). Society and the Adolescent Self-Image. Princeton, NJ: Princeton University Press
Rowsell, M., MacDonald, D. E., and Carter, J. C. (2016). Emotion regulation difficulties in anorexia nervosa: associations with improvements in eating psychopathology. J. Eat. Disord. 4:17. doi: 10.1186/s40337-016-0108-0
Sander, J., Moessner, M., and Bauer, S. (2021). Depression, anxiety and eating disorder-related impairment: moderators in female adolescents and young adults. Int. J. Environ. Res. Public Health 18:2779. doi: 10.3390/ijerph18052779
Silvera, D. H., Bergersen, T. D., Bjørgum, L., Perry, J. A., Rosenvinge, J. H., and Holte, A. (1998). Analyzing the relation between self-esteem and eating disorders: differential effects of self-liking and self-competence. Eat. Weight Disord. 3, 95–99. doi: 10.1007/BF03339995
Silverstone, P. H. (1990). Low self-esteem in eating disordered patients in the absence of depression. Psychol. Rep. 67, 276–278. doi: 10.2466/pr0.1990.67.1.276
Silverstone, P. H. (1992). Is chronic low self-esteem the cause of eating disorders? Med. Hypotheses. 39, 311–315. doi: 10.1016/0306-9877(92)90054-g
Sowislo, J. F., and Orth, U. (2013). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol. Bull 139:213. doi: 10.1037/a0028931
Stice, E. (2002). Risk and maintenance factors for eating pathology: A meta-analytic review. Psychol. Bull. 128, 825–848. doi: 10.1037/0033-2909.128.5.825
Wheeler, A. R., Shanine, K. K., Leon, M. R., and Whitman, M. V. (2014). Student-recruited samples in organizational research: A review, analysis, and guidelines for future research. J. Occup. Organ. Psychol. 87, 1–26. doi: 10.1111/joop.12042
Wilson, G. T. (2005). Psychological treatment of eating disorders. Annu. Rev. Clin. Psychol. 1, 439–465. doi: 10.1097/YCO.0b013e328365a30e
Wong, C. S., and Law, K. S. (2002). The effects of leader and follower emotional intelligence on performance and attitude: An exploratory study. Leadersh. Q. 13, 243–274. doi: 10.1016/S1048-9843(02)00099-1
Zavala, M. A., and López, I. (2012). Adolescentes en situación de riesgo psicosocial? ‘Qué papel juega la inteligencia emocional? Behav. Psychol. 20, 59–75.
Zysberg, L. (2013). Emotional intelligence, personality, and gender as factors in disordered eating patterns. J. Health Psychol. 19, 1035–1042. doi: 10.1177/135910531348315
Zysberg, L., and Rubanov, A. (2010). Emotional intelligence and emotional eating patterns: a new insight into the antecedents of eating disorders? J. Nutr. Educ. Behav. 42, 345–348. doi: 10.1016/j.jneb.2009.08.009
Keywords: emotional intelligence, eating disorders, anxiety, self-esteem, path analysis
Citation: Peláez-Fernández MA, Romero-Mesa J and Extremera N (2021) From Deficits in Emotional Intelligence to Eating Disorder Symptoms: A Sequential Path Analysis Approach Through Self-Esteem and Anxiety. Front. Psychol. 12:713070. doi: 10.3389/fpsyg.2021.713070
Received: 21 May 2021; Accepted: 23 July 2021;
Published: 18 August 2021.
Edited by:
Atsushi Oshio, Waseda University, JapanReviewed by:
Stefania Cella, University of Campania Luigi Vanvitelli, ItalyCopyright © 2021 Peláez-Fernández, Romero-Mesa and Extremera. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: María Angeles Peláez-Fernández, bWFwZWxhZXpAdW1hLmVz
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.