- 1National Forensic Sciences University, Gandhinagar, India
- 2Centre for Research in Psychology and Human Well-Being, Faculty of Social Sciences and Humanities, Universiti Kebangsaan Malaysia, Bangi, Malaysia
- 3Department of Pharmacology, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia
- 4Department of Family Medicine, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia
- 5Neuropharmacology Research Laboratory, Jeffrey Cheah School of Medicine and Health Sciences, Monash University Malaysia, Subang Jaya, Malaysia
- 6Department of Physiology, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia
Alcohol has been associated with violent crimes and domestic violence across many nations. Various etiological factors were linked to chronic alcohol use and violence including psychiatric comorbidities of perpetrators such as personality disorders, mood disorders, and intermittent explosive disorders. Aggression is the precursor of violence and individuals prone to aggressive behaviors are more likely to commit impulsive violent crimes, especially under the influence of alcohol. Findings from brain studies indicate long-term alcohol consumption induced morphological changes in brain regions involved in self-control, decision-making, and emotional processing. In line with this, the inherent dopaminergic and serotonergic anomalies seen in aggressive individuals increase their susceptibility to commit violent crimes when alcohol present in their system. In relation to this, this article intends to investigate the influence of alcohol on aggression with sociopsychological and neuroscientific perspectives by looking into comorbidity of personality or mood disorders, state of the mind during alcohol consumption, types of beverages, environmental trigger, neurochemical changes, and gender differences that influence individual responses to alcohol intake and susceptibility to intoxicated aggression.
Introduction
Alcohol use disorder (AUD) is one of the leading causes of the global burden of disease and injury (WHO), despite the continuous discovery of novel pharmacotherapeutic agents (Pakri Mohamed et al., 2018). Various factors such as environmental, social, situational, and cultural context have distinctive consequences toward substance use and its effects on individuals (Latkin et al., 2017). Alcohol alters the mental state of individuals, including emotional processing and rational thinking, making the users unpredictable and dangerous, especially young people (Australian Government, 2017) or those with pre-existing psychological or psychiatric comorbidities (Brem et al., 2018; Puhalla et al., 2020). Violence related to substance use has been widely reported and studied, particularly the potential for violent outcomes between the different substances of use (Duke et al., 2018). Studies from various countries have reported crimes and domestic violence owing to alcohol (Hagelstam and Häkkänen, 2006; Mayshak et al., 2020), especially during the recent state of global coronavirus disease 2019 (COVID-19) pandemic (Finlay and Gilmore, 2020).
Alcohol and Domestic Abuse/Violence
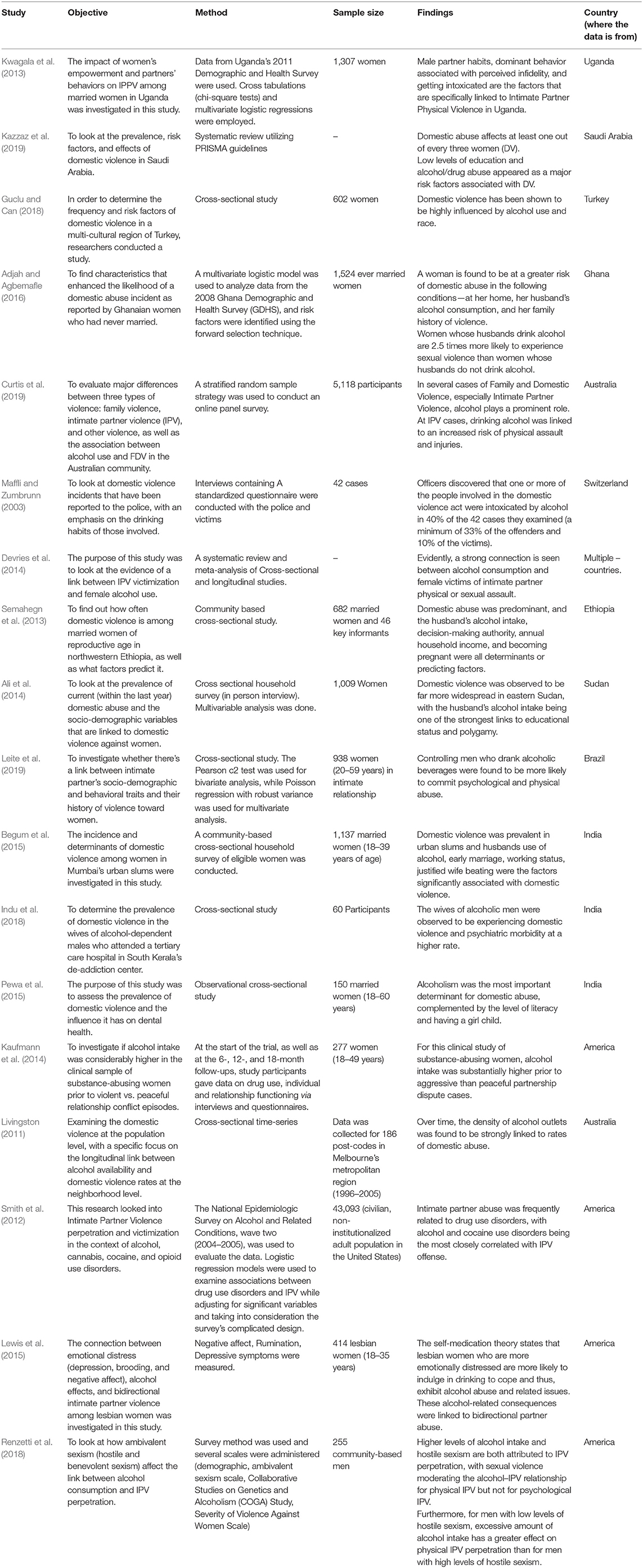
There is a strong evidence linking alcohol with domestic abuse or domestic violence (Gadd et al., 2019). A study conducted within the metropolitan area of Melbourne, Australia found that alcohol outlet density was significantly associated with domestic violence rates over time (Livingston, 2011). In Australia, alcohol-related domestic violence is twice more likely to involve physical violence including life-threatening injuries (Mayshak et al., 2020). In the UK police report audit, approximately two-thirds of domestic incidents reported to police involve “under the influence of alcohol” (Alcohol Research UK). The same study also noted more aggression if alcohol was involved and persons involved considered alcohol to have a direct effect on their behavior. International evidence reveals a similar pattern with men tend to cause worse assaults after drinking and women are more likely to suffer from abuse with living partners who are heavy drinkers (Reno et al., 2010; Graham et al., 2011). These behavioral patterns cannot be inferred from women. Studies have demonstrated that women who are heavy alcohol drinkers tend to suffer from abuse themselves and also suffer from higher aggression from their partners (Hutchison, 1999; Iverson et al., 2013). In India, those who had a heavy drinker in their lives (family, relative, neighbor, etc.) reported having been harmed by them through physical, sexual, psychological, financial, and social. In Kerala, India, a cross-sectional study involving spouses of alcohol-dependent males undergoing a deaddiction program reported a high correlation between domestic violence and years of marriage and the number of stressful events in the past year (Indu et al., 2018). In the USA, 40% of the reported domestic violence has the alcohol factor present during the time of the offense (Galbicsek, 2020). It is also found that the intensity of violence is greater when the offender is intoxicated compared to when he/she is not. Based on existing literature, alcohol consumption is more related to the severity of domestic violence rather than its occurrence (Graham et al., 2011) and exacerbated by an increase in consumption (Ferrari et al., 2016). Although there is a clear correlation between alcohol and domestic abuse, these correlations are limited to men and, therefore, form a complex relationship, hence establishing a unidirectional relationship between domestic violence and alcohol is not possible at present (De Paula Gebara et al., 2015). As per UN Women of the United Nations, the global prevalence of domestic violence against women was 1 in 3 prior to COVID-19 pandemic, mainly perpetrated by their intimate partners. Emerging data from a number of countries show an increase in calls to domestic violence helplines since the beginning of COVID-19 pandemic. The United Nations Secretary-General has referred to this surge in domestic violence amid COVID-19 pandemic as a “shadow pandemic” (Women UN, 2020). Several countries showed a shockingly increasing pattern of domestic violence cases globally, up to 50% in Brazil, 20% rise in helpline calls in Spain, 30% in Cyprus (The Guardian, 2020), 25% increase in helpline calls and about 150% rise in Refuge website in the UK (Bradbury-Jones and Isham, 2020), and almost doubled cases of domestic violence in the Hubei, China (Anju, 2019). COVID-19 pandemic-induced increase in global domestic violence was irrespective of the economic status of the countries (Finlay and Gilmore, 2020). In line with this, the alcohol sales in March 2020 were increased by 67% in the UK during lockdown (Finlay and Gilmore, 2020). Contrary to this, a recent systematic review revealed that there is insufficient evidence to suggest that COVID-19 pandemic has led to increased substance use and domestic violence (Abdo et al., 2020) (Table 1).
Alcohol, Aggression, and Violence: Psychiatric Comorbidities
There were various publications related to the etiological factors associating alcohol use and violence. Study has shown that alcohol was most commonly abused among adolescents and school children (Bland et al., 2018). Factors such as developmental milestones when a child is growing up can predict violence and substance abuse in adults (Hentges et al., 2018; Malti, 2020). Retrospectively, heavy drinking in later life can be predicted by early childhood aggression (Gottfried and Christopher, 2017). A combination of substance use and psychiatric disorders is associated with an above-average risk of adult violent behavior (Wiener et al., 2018). Mental disorders such as anxiety and mood disorders have also been commonly associated with AUD (Gimeno et al., 2017). AUD and depressive symptoms are commonly reported with other mood disorders and have greater severity and worse prognosis compared when it is concomitant with AUD (Higley and Linnoila, 2002). There are possibilities of the symptoms exhibited by the patients during withdrawal or acute intoxication that are pre-existing effective disorders or in a combination (Serafini et al., 2017). The most common symptoms of substance withdrawal include agitation. Other symptoms such as disinhibition and despair are commonly associated with substance abuse disorder that would be amplified into self-destructive acts and impulsivity (Goldstein et al., 2017; Duica et al., 2020). In addition, men with antisocial traits are at greater risk of binge alcohol consumption and commit intimate partner violence (Brem et al., 2018). In US, the prevalence of antisocial personality disorder and adulthood antisocial behavioral syndrome was 4.3 and 20%, respectively, and both the syndromes were significantly associated with 12-month and lifetime substance use (Goldstein et al., 2017). Based on a study conducted in Italy that had a population of 717 make subjects−404 alcoholics and 282 having a personality disorder, alcohol consumption was higher among those who suffer from psychiatric conditions, especially personality disorder (39%; antisocial personality disorder at the most) and 14.2% have a dual diagnosis (personality disorder and alcohol dependence). The antisocial personality population (more than any other personality disorder) had an early onset of alcohol abuse and its association with physical dependence and legal problems (Poldrugo, 1998). Similar studies were conducted in the prisons of North Italy, which also suggested that there is a positive correlation between AUD and personality disorders and the risk of engaging in criminal acts is higher within the individuals with dual diagnosis (alcoholics and sociopaths). Intermittent explosive disorder (IED), characterized by repeated, sudden explosive outbursts of anger or violence, has been associated with a history of childhood abuse and AUD is at a greater risk for intoxicated aggression (Puhalla et al., 2020) and also to develop substance use disorder compared to those without IED (Coccaro et al., 2017).
Alcohol, Aggression, and Crime
Aggression is the basic ingredient of acts of violence (Eisner and Malti, 2015). Violence as aggression has the goal of extreme harm including death. In this context, violent and criminal behavior is often associated with substance abuse (Anderson and Bushman, 2002). Alcohol is one of the major ingredients of violent incidents (i.e., murder) due to its disinhibiting effects along with loss of emotional control that increases the susceptibility to physical assaults and eventually murder (Karlsson, 1998). According to Mokdad et al. (2004) and Pinel and Barnes (2018), alcohol is involved in more than 2 million deaths (deaths due to ill health, accidents, and violence) each year across the world. A moderate dose of alcohol in the blood tends to cause cognitive, perceptual, verbal, and motor impairments as well as a loss of control, which eventually lead to unacceptable social behavior including violence (Pinel and Barnes, 2018). From a criminological perspective, alcohol is an important factor in violent interactions that culminate in murder (Wahlsten et al., 2007). Substance abuse, especially alcohol, is widely acknowledged as an important risk marker for criminal behavior and violent crimes including those with mental disorders (Brennan et al., 2000; Wallace et al., 2004; Erkiran et al., 2006). The strong link between alcohol use and violence is well-demonstrated (Mann et al., 2006), as alcohol consumption is an important factor for the prevalence of violence (Room and Rossow, 2001).
Alcohol facilitates conflicts with others and increases the potential for violent behavior among the drinkers and others (Wieczorek et al., 1990; Mann et al., 2006; Wahlsten et al., 2007). Expressive murders are most often preceded by arguments and altercations and the level of intoxication increases the viciousness of the attack (Karlsson, 1998). Block and Block (1992) defined expressive murders as a result of the expression, emotions, and psychological states. Emotional states such as anger, frustration, and hostility are said to lead an individual to perform expressive murders. In this context, alcohol is said to be the credible factor leading to emotional loss and instability and eventually leading to expressive-based murders. A national study of 16,698 inmates found that alcohol had a stronger role in violent offending such as homicide, physical assaults, and sexual assaults compared to offenses such as burglary and robbery. In this study, the majority of the respondents claimed to have been under the influence/intoxication of substance(s) such as alcohol during the commission of murder (Felson and Staff, 2010).
In 2011, 73 and 57% of the homicides recorded in the United States and Russia were alcohol related (Landberg and Norström, 2011), whereas, in countries including Finland, Netherlands, and Sweden, alcohol consumption led to lethal violent crimes reported from 2003 to 2006. In Finland alone, 491 persons were killed within 4 years period and ~82% of the perpetrators were intoxicated with alcohol, where 39% of them were alcoholics and 45% of the reported murders were committed with knives (Liem et al., 2013). In Singapore, out of 253 homicide offenders, 141 individuals (56%) were suffering from AUD and 121 offenders (48%) drank alcohol within 24 h preceding their criminal offense (Yeo et al., 2019). In the Brazilian city of Diadem, limiting the hours of alcoholic sales in bars to 11 p.m. significantly declined the crime rate to 9 homicides per month (Duailibi et al., 2007). Chervyakov et al. (2002) reported that 4 in every 5 Russians convicted of murder were intoxicated with alcohol during the murderous act. In a British prison sample, over a third of male homicide offenders had consumed alcohol and were considered drunk at the time of the offense and 14.0% had been using drugs (Dobash and Dobash, 2011).
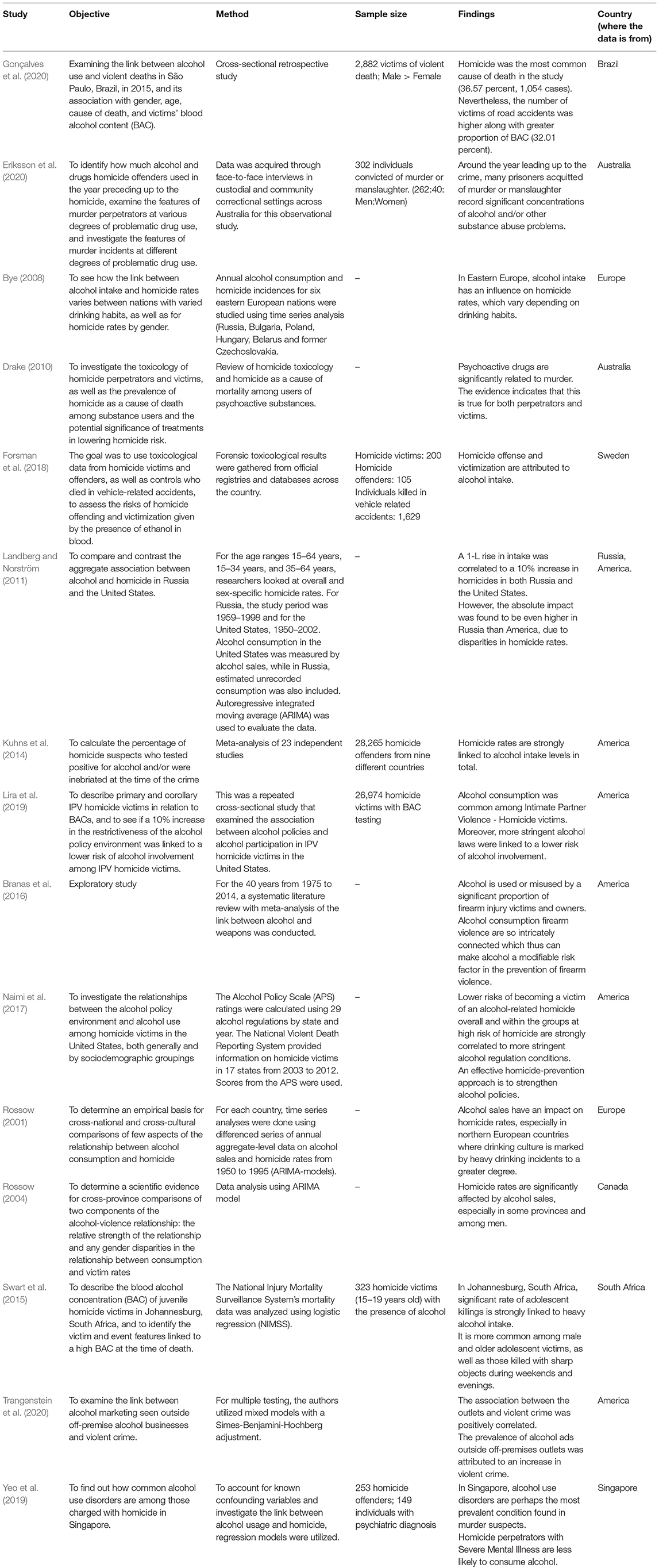
Even though many findings from various countries strongly concluded that alcohol is a risk factor for murderous acts, however, most of these studies correlated level of alcohol consumption rather than the pattern of hazardous intake or types of beverages consumed, which is more likely to cause severe disinhibition, hence more damages. In line with this, using a sample of 85 countries, Weiss et al. (2018) reported no association between alcohol consumption level and homicide rates; however, they found a positive association between hazardous drinking pattern and homicide rates. Contrary to this, a cross-sectional analysis of data from 83 countries that controlled for several possible covariates reported that countries with riskier drinking patterns did not have higher homicide rates compared to countries with less risky drinking patterns. However, the same investigators also reported that the association between homicide rates and alcohol was beverage specific, with beer and spirit consumption were positively correlated with homicide rates and wine negatively correlated with the rate of homicides (Hockin et al., 2018) (Table 2).
Alcohol and Aggression: A Neuroscience Perspective
Alcohol accentuates or promotes the mental state of the drinkers at the time of consumption, fueling negative emotions such as aggressive behavior or positive emotional outcomes such as gregariousness and warmth. Aggression is classified as impulsive, premeditated, and medically driven (Gollan et al., 2005). Even cognitively intact alcohol-dependent individuals showed higher psychopathological symptoms with trait impulsivity (Kovács et al., 2020) and other psychiatric comorbidities such as antisocial and borderline personalities (Helle et al., 2019) triggering medically driven aggression. Unlike impulse-driven aggression, which is reflective of an agitated state of mind, premeditated aggression is a planned aggressive act (Martin et al., 2019).
The aggressive acts at some points could be goal oriented, whereas in some instances could be impulse driven. Impulsivity is defined as fast actions taken without adequate or with little thought and conscious judgment of the consequences (Bakhshani, 2014). Assessment of various brain regions of 1,200 men and women of 18–35 years old along with their tendency to make rapid decisions seek for novel and intense experiences and risk-taking traits revealed a significant decrease in the cortical thickness of brain regions related to self-control and decision-making processes, particularly anterior cingulate and middle frontal gyrus (Holmes et al., 2016). Alcohol itself directly interrupts the executive cognitive functions by disrupting the functions of the prefrontal cortex (PFC), which has been associated with disinhibition and aggression (Heinrichs, 1989). The PFC, which regulates aggressive and social behavior (Davidson et al., 2000; Seo et al., 2008), was shown to be reduced in its volume in individuals with antisocial personality disorder (Raine et al., 2000). In addition, neuroimaging of individuals with IED revealed lower white matter integrity in long-range connections between the frontal and temporoparietal regions (Lee et al., 2016), reduced gray matter volume in the frontolimbic structures (Coccaro et al., 2016), and gray matter deficit and dysfunction of the left insula (Seok and Cheong, 2020). The orbitomedial region within the PFC regulates anger and impulsive aggression (Lapierre et al., 1995; Davidson et al., 2000) and assigns appropriate emotion to the consequences of actions (Bechara et al., 2000). During aggressive behaviors, reduced activity was reported within the orbitofrontal PFC (Goyer et al., 1994; Pietrini et al., 2000), where the impaired PFC is unable to inhibit the subcortical structures such as the amygdala, hippocampus, and nucleus accumbens from activating emotional output (Raine et al., 1998; Davidson et al., 2000). In line with this, an increase in amygdala limbic connectivity and a significant decrease in amygdala-medial PFC connectivity were reported among violent offenders (Siep et al., 2019). Hyperactivation of the amygdala is also reported in individuals with IED in response to angry faces compared to controls (McCloskey et al., 2016). Moreover, alcohol-dependent patients with a history of aggressive behavior also recorded elevated glutamate/creatine ratio in the bilateral amygdala (Liu et al., 2020) corroborating various other behavioral changes associated with glutamatergic hyperexcitability state in the amygdala reported in past studies (Kumar et al., 2013, 2016, 2018; Pakri Mohamed et al., 2018; Kamal et al., 2020).
Serotonin in AUD and Aggression
Aggression is a complex behavior involving interactions between the gene, environment, personality, and physiology (Armstrong et al., 2017; Zhang et al., 2017; Kanen et al., 2021). Dysregulation of serotonin is associated with many psychiatric disorders (Rappek et al., 2018; Conio et al., 2020; Fanning et al., 2020) due to the widespread distribution of serotonergic fibers originating from midbrain raphe nuclei to various other regions (Sharp and Barnes, 2020). Based on a systematic review, the association between serotonin and aggression is rather mixed, where reduced 5-hydroxytryptamine (5-HT) concentration in central nervous system (CNS) was associated with reactive aggression (impulsivity; response to provocation), whereas increased 5-HT (small number of findings) may be related to callous-unemotional traits, which is another possible pathway to aggressive behavior (Runions et al., 2019). In line with this, SLC6A4*HTTLPR or 5-HTTLPR (serotonin transporter) was associated with aggression within the population of Pakistan (Qadeer et al., 2021), China (Zhang et al., 2017), and the United States of America (Armstrong et al., 2017), whereas, in a study conducted among Russian inmates, such correlation was not found (Toshchakova et al., 2017). Furthermore, other genes of serotonin such as 5-hydroxytryptamine receptor 2A (5HTR2A), 5-hydroxytryptamine receptor 2B (5HTR2B), and 5-hydroxytryptamine receptor 2C (5HTR2C) also showed no association with aggressive behavior (Toshchakova et al., 2017; Qadeer et al., 2021), suggesting a stronger link between brain serotonin level and aggression rather than the receptors, which was also proven by studies using selective serotonin reuptake inhibitors (SSRIs) (Nord et al., 2013; Lagerberg et al., 2020). Likewise, a lower cerebrospinal level of 5-hydroxyindoleacetic acid (5-HIAA), the main metabolite of serotonin, was reported in the impulsive offenders than the premeditated murderers (Linnoila et al., 1983). Regions such as the cingulate cortex, ventromedial, and the orbitofrontal PFC were shown to have reduced serotonergic activity during impulsive aggression (Siever et al., 1999). Similar findings also reproduced in non-human animal models (Harrison et al., 1997; Kästner et al., 2019; Gorlova et al., 2020).
Some researchers have reported high serotonin transporter (SERT) bindings in the brains of deceased alcoholics (Underwood et al., 2018), whereas others have reported low binding (Mantere et al., 2002) and some reported no differences (Brown et al., 2007; Martinez et al., 2009). Similarly, mixed findings were also reported for 5-HT1A and 5-HT2A receptor bindings (Underwood et al., 2008, 2018; Storvik et al., 2009). Chronic alcohol intake increases the metabolites of serotonin in the raphe nuclei area, however reduces 5-HT2A protein levels in the mice cortex, indicating reduced serotonergic activity (Popova et al., 2020). Acute alcohol intake reduces tryptophan availability to the brain (non-aggressive), which leads to a decrease in serotonin synthesis and turnover, about 25% of the concentration of tryptophan following an oral intake of alcohol (Badawy et al., 1995). Hence, it is probable that in the aggressive brain, the drop in brain serotonin synthesis might even be greater (40–60%) during moderate intake of alcohol (Badawy, 2003). However, the inconsistent findings of serotonin markers in brain imaging studies of alcoholics suggest that comorbidity of AUD with other psychiatric disorders may complicate the serotonin hypothesis in real life. In addition, even individual differences in personality traits determine the types of emotion affected by the depletion of serotonin (Kanen et al., 2021).
Dopamine in AUD And Aggression
Serotonin and dopamine levels are significant predictors of aggression and suicide risk (Prepelita et al., 2019). A systematic review of pre-clinical findings suggests that adolescence chronic stress may lead to a hyperdopaminergic state of the PFC, which eventually blunts the adulthood prefrontal dopaminergic neurotransmission, increasing the vulnerability to maladaptive aggression in adulthood (Tielbeek et al., 2018). In relation to this, polymorphisms of catecholamine-converting enzymes such as monoamine oxidase and catechol-o-methyltransferase along with traumatic childhood significantly increase appetitive and Facilitative Aggression Scale (Fritz et al., 2021). Furthermore, a study conducted on convicted Pakistani murderers revealed a high prevalence of the 9R allele of DAT-1VNTR, which influences the intrasynaptic dopamine levels (Qadeer et al., 2017). Pharmacological modulation of dopamine D2 receptor via its antagonist, sulpiride, impaired the ability to discern angry facial expressions in humans (Lawrence et al., 2002). However, some researchers have reported the opposite, where polymorphism in DRD2 genotypes causes reduced dopamine functioning that is directly associated with increased aggression (Zai et al., 2012) which may occur through sensation seeking (Chester et al., 2016). Nevertheless, it was hypothesized that impaired serotonin neuromodulatory effects may lead to dopamine hyperactivity in subcortical structures and aggressive behaviors (Seo et al., 2008). Studies investigating the interaction between genetic polymorphism of dopamine system (dopamine receptors; DRD2, DRD4, transporter; DAT1), and environmental factors (financial stressor and adolescent social experiences) on intimate partner violence revealed a strong influence of negative environmental changes on increased odds of violence perpetration regardless of the alleles (Schwab-Reese et al., 2020).
In addition to aggression, alcohol alone modulates dopaminergic neurotransmission, where even the cues of alcohol could increase the dopamine release in the nucleus accumbens (Melendez et al., 2002). Dysregulation of dopaminergic neurotransmission in AUD has been demonstrated in several brain imaging studies (Leurquin-Sterk et al., 2018; Chukwueke et al., 2021). Factors such as personality traits and comorbidities with other psychiatric disorders along with environmental stressors influence how one could engage in violent behaviors. Hence, even though alcohol might be the precursor to violence for some, it certainly takes more than the beverage to increase the likelihood of someone shooting from the hip.
Alcohol, Aggression, and Violence: A Conundrum
Individual reports from multiple countries have associated alcohol with violent crimes and domestic abuse. Consumption of alcoholic beverages with higher alcohol content at a dose of 0.75 g/kg and higher was correlated with increased aggression (Hockin et al., 2018; Kuypers et al., 2020), whereas a comprehensive review found no association between homicide rates and alcohol consumption level (Weiss et al., 2018). Even countries with a riskier drinking pattern did not show a higher crime rate compared to countries with less risky drinking patterns (Hockin et al., 2018). This led us to the question, does alcohol alone is sufficient to trigger violent or aggressive behavior? Based on the pieces of literature gathered in this article and past findings, it is evident that several individual and environmental factors determine the likelihood of an intoxicated person engaging in an aggressive or violent act. Emotional dysregulation and impulsivity in combination with pre-existing psychiatric comorbidities such as personality disorders, intermittent explosive disorder along with genetic pre-disposition and environmental stressors, such as the most commonly associated childhood adversity, are one of the triggers of intoxicated aggression. Genetic polymorphism findings indicate that environmental stressors play a more significant role in perpetration violence compared to high-risk genotypes (Schwab-Reese et al., 2020). However, some have reported that epigenetic mechanisms mediate the interaction between genetic and environmental factors by altering genes of many systems including the nervous, immune, and neuroendocrine (Chistiakov and Chekhonin, 2017).
Stress during early life, also known as childhood adversity or childhood maltreatment, is associated with the development of personality disorders (Lemgruber and Juruena, 2013; Porter et al., 2020), affective disorders (Hoppen and Chalder, 2018), and alcohol use disorder (Evans et al., 2017). Among these, physical, emotional abuse, and maternal rejection are associated with the shaping of personality (Schouw et al., 2020) and maladaptive schemes in adulthood (Pilkington et al., 2021). For an instance, physical abuse and neglect lead to antisocial traits (Schorr et al., 2020). Factors such as family dysfunction, as violence in the family, show a strong correlation with adulthood aggression (Khodabandeh et al., 2018; Labella and Masten, 2018) through emotion-related impulsivity and behavioral response inhibition (Madole et al., 2020). In line with this, it has been reported that a high level of childhood adversity increases one's likelihood to substance use through reduced functioning of the anterior cingulate cortex in inhibitory control, indicating a higher impulsive response (Fava et al., 2019). The very nature of adversity (threat vs. deprivation) has a distinctive effect on emotional circuits. For an instance, childhood threat was reported to reduce the volume of the medial PFC, amygdala, and hippocampus along with increased activation of the amygdala in response to a threat, whereas childhood deprivation alters the function and volume of the frontoparietal regions, which are associated with goal oriented and executive functions (McLaughlin et al., 2019). In addition to the type of adversities, individual differences in threat and executive control-related brain regions also determine how one with childhood adversity would express adult trait anger. Individuals with the low amygdala and high dorsolateral PFC activity do not express high trait anger, despite having experienced stress in early life (Kim et al., 2018). Suppression of adult trait anger was owing to the higher microstructural integrity of white matter pathways, including the uncinate fasciculus, which anatomically links the PFC and amygdala in the regulation of negative emotion (Kim et al., 2019). However, the findings by Kim et al. (2019) were based on subjects free of borderline and personality disorders, which are the most commonly associated psychiatric comorbidities with intoxicated aggression and also known to have reduced white matter integrity in regions associated with risky behavior and impulsivity (Jiang et al., 2017; Ninomiya et al., 2018). Hence, more longitudinal studies are needed in the future to understand the effects of early life stress on the development of aggression-related psychiatric comorbidities from neurological perspectives. Furthermore, the role of white matter integrity in one's expression of anger despite the chronic stress in early life should be further explored to understand the cause behind such discrepancy and the consistent neurological changes noticed in conjunction with high-risk behaviors could be investigated as potential biomarkers to predict one's risk factor along with social experiences (Figure 1).
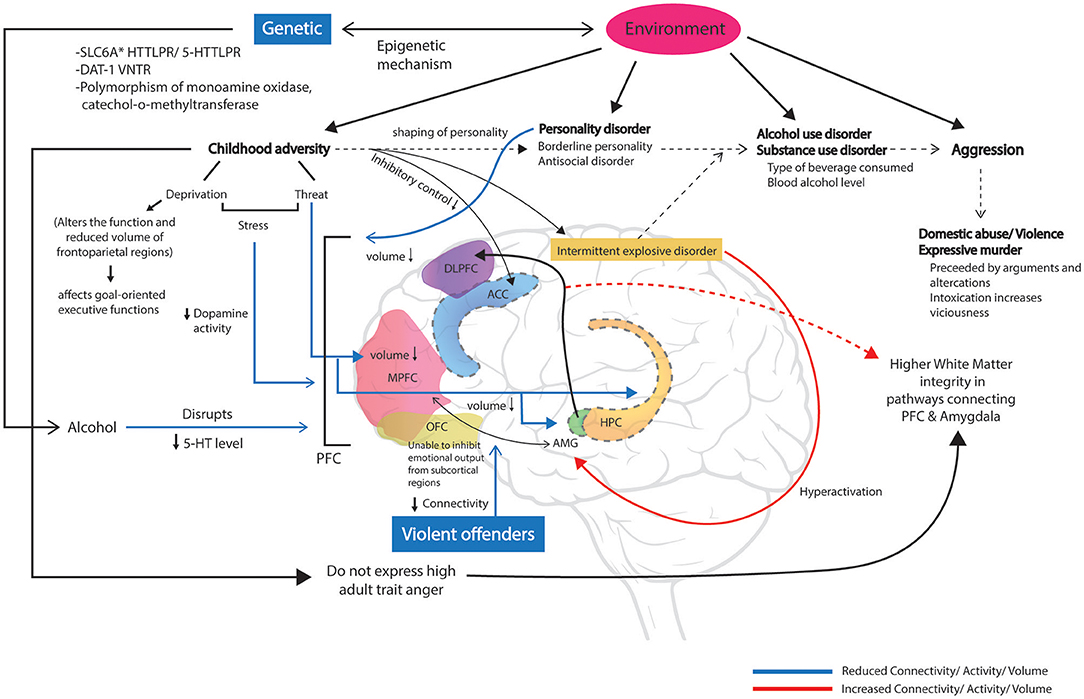
Figure 1. Childhood adversity affects the shaping of personality, which eventually leads to development of personality disorder, alcohol use disorder, substance use disorder, intermittent explosive disorder (IED), and aggressive behaviors such as domestic abuse or expressive murders in adulthood. Factors such as genetics and environment also interact with alcohol intake and causing neuroplasticity in brain regions associated with emotional and cognitive regulation. Childhood stress such as deprivation alters the function and reduces the volume of frontoparietal regions that associated with goal-oriented and executive functions. Childhood adversity including threat reduces the volume of the medial prefrontal cortex (MPFC), amygdala (AMG), and hippocampus (HPC). Chronic early life stress also blunts the dopaminergic activity in the PFC. Alcohol disrupts the serotonergic activity in the PFC. Altered functions of the orbitofrontal cortex (OFC) unable to inhibit the increased emotional output from subcortical structures such as the hyperactivation of AMG in IED. Reduced connectivity between MPFC and AMG was reported in violent offenders. Adults having experienced childhood adversity and do not express high adult trait anger were due to higher white matter integrity in pathways connecting the PFC and AMG.
Gender Differences in Binge Drinking, Alcohol-Induced Aggression, and Violence
It was initially reported that women are less likely to engage in binge drinking patterns than men (Bobrova et al., 2010). However, in the recent years, data from the United States indicate that the binge-drinking rate in adult women (age 21–49 years) has been rising (Hasin et al., 2019; Sarah and Keyes, 2020). Evidence suggests that there is a little convergence in the pattern of binge drinking in men and women. It was found that the prevalence was higher for females than males from 2000 to 2010 for any binge drinking in the preceding month. On the contrary, the reason for the convergence of frequency in the male and female binge drinking habits is estimated to occur due to the large decline in the binge drinking frequency within men than the women. Furthermore, evidence also shows that the convergence of men and women has usually been stronger in the age group of young adults in comparison to any other age group (Wilsnack et al., 2018). Data from 2006 to 2018 indicate that both the men and women increasingly binge drink; in women, the largest increase was found in the age group 30–44 years without children (Sarah and Keyes, 2019).
Several studies have investigated the risk factors pertaining to intimate partner violence (IPV)/domestic violence (DV) and found that gender-specific differences exist in DV. The likelihood of females being victimized is greater than the male victimization, whereas evidence for the males being the perpetrators is higher than that of the females. The risk factors that are found to be common in both the men and women reporting perpetration involved being exposed to parental violence and physical abuse during childhood and alcohol abuse. Risk factors that are thought to be associated with male perpetration include unemployment, lower income, cohabitation, mood disorders, and no or lower level of education (Gass et al., 2011; Lee et al., 2014). Lack of education is thought to play a role in both the perpetration and victimization of women (Capaldi et al., 2012). Moreover, factors such as pregnancy, young age, higher income than the partner, and previous relationships increase the risk of victimization for women (Capaldi et al., 2012).
Prior reports have established alcohol-induced aggression among males (Lipsey et al., 1997), which appears to vary across the ethnic groups and geographical regions (Caetano et al., 2001). Systematic comparison between males and females in relation to alcohol-induced aggression revealed greater effects of alcohol on males than females (Ito et al., 1996; Bushman, 2002); however, the analysis was limited by insufficient power to detect significant effects due to limited female data. In agreement with this, a separate study reported a small-to-moderate effect size for the association between alcohol use and male-to-female partner violence, whereas a small effect size for the association between alcohol intake and female-to-male partner violence (Foran and O'Leary, 2008). More recently, a significant, small effect size was reported for the association between alcohol intake and aggression in female subjects who consumed alcohol compared to those who did not drink, in response to a subsequent aggression paradigm (Crane et al., 2017).
Males are more likely to express aggression in a physical and/or direct form, whereas females are more likely to express it in an indirect form. It has also been reported that both the males and females are equally aggressive when verbal aggression is at play (Archer, 2004; Björkqvist, 2017). In an experiment conducted by Giancola and Zeichner (1995), 128 participants (64 males and 64 females) performed a task where they gave an electric shock to the fictional opponents, which included both the genders. The participants were assigned to either alcohol, a placebo, or a sober group. The researchers found that the intensity and duration of shock were higher in the men from the alcohol group, while only shock duration was increased in women. They also noted that men were highly aggressive toward the same gender, while women were aggressive regardless of gender. This indicated that alcohol-induced aggression affects both the genders in different ways, suggesting that men are likely to respond in a direct and indirect manner, whereas women exhibit aggression in an indirect manner. A slightly different finding to the previous study was seen in an investigation conducted by Hoaken and Pihl (2000). The researchers assigned the participants (54 males and 60 females) to compete in a competitive aggression paradigm in an intoxicated or sober state. The result was that the intoxicated men were more aggressive than the sober men; however, in the circumstances where the women were highly provoked, both the intoxicated and sober women displayed higher levels of aggression, which could resemble the men. This suggested that both the women and men can be equally aggressive and alcohol does not seem to play a prominent role in the gender biases in aggression.
Several brain imaging studies have examined the neurological changes in men and women during aggression either by including an equal number (almost) of male and female subjects or a single gender (against a control group) (Chester and DeWall, 2016; Emmerling et al., 2016; Denson et al., 2018). To date, very few studies have tested the gender difference hypothesis using both the male and female subjects. Generally, men have recorded higher activation of the amygdala (McRae et al., 2008) and the PFCs (Rahko et al., 2010) during emotional reactions. Investigation of sex differences in neural correlates of aggression using 22 male and 20 female subjects revealed differential brain activation patterns between both the genders in response to provocation. Aggressive men recorded higher activation of the left amygdala than aggressive women and a positive correlation with orbitofrontal cortex (OFC), rectal gyrus, and ACC activity, which was negatively correlated in women. The findings indicate that aggressive men are more inclined to automatic emotion regulation (attributed to OFC and rectal gyrus) in response to provocation compared to aggressive women (Repple et al., 2018). In a separate study involving 24 men and 11 women, alcohol alone had no effect on the amygdala and ventral striatum; however, their activities were positively correlated with aggression in response to provocation. Alcohol decreased their bold responses in the right PFC, thalamus, hippocampus, caudate, and putamen. Neither gender had any significant impact on the results (Gan et al., 2015). Contrary to this, a single administration of 0.5 per thousand alcohol was shown to reduce frontal interhemispheric connectivity in female participants, but not in male participants (Hoppenbrouwers et al., 2010). Intergender neurological and behavioral responses to alcohol are also influenced by ethanol metabolism (Arthur et al., 1984) and influences of hormones such as testosterone, cortisol, estradiol, progesterone, and oxytocin (Denson et al., 2018).
Conclusion
Alcohol intoxication-induced aggression is an interplay between gender, genetic, psychiatric comorbidities, blood alcohol level, and environmental factors. Risk factors associated with intoxicated aggression or aggression should be packaged into a scientific explanation to educate the public. Alcohol is a weak drug, which needs to be consumed in large amounts in order to cause intoxication. Hence, high-risk individuals should practice moderate drinking. Parental roles in shaping the personalities of children should be incorporated into the marriage course as one of the preventive measures. Future studies and policymakers should include more behavioral interventions in the high-risk adolescent groups.
Author Contributions
KS and JK contributed to the conceptual framework, design, and drafted the manuscript. MR, IN, RM, and MS searched references and critically revised the manuscript. HK prepared the figure and legend. All the authors critically reviewed content and approved the final version for publication of manuscript.
Funding
This study was funded by the Ministry of Higher Education Malaysia, FRGS/1/2020/SKK0/UKM/02/3.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank the Ministry of Higher Education, Malaysia, and Faculty of Medicine, UKM.
References
Abdo, C., Miranda, E. P., Santos, C. S., de Bessa Júnior, J., and Bernardo, W. M. (2020). Domestic violence and substance abuse during COVID19: a systematic review. Indian J. Psychiatry 62:S337. doi: 10.4103/psychiatry.IndianJPsychiatry_1049_20
Adjah, E. O., and Agbemafle, I. (2016). Determinants of domestic violence against women in Ghana. BMC Public Health 16:368. doi: 10.1186/s12889-016-3041-x
Ali, A. A., Yassin, K., and Omer, R. (2014). Domestic violence against women in Eastern Sudan. BMC Public Health 14:1136. doi: 10.1186/1471-2458-14-1136
Anderson, C. A., and Bushman, B. J. (2002). Human aggression. Ann. Rev. Psychol. 53, 27–51. doi: 10.1146/annurev.psych.53.100901.135231
Anju, S. R. (2019). A true experimental study to evaluate the effectiveness of structured teaching programme on knowledge regarding III–effects of alcohol consumption among adolescents in selected senior secondary school at panipat haryana. Amarjeet Kaur Sandhu 11:424. doi: 10.5958/0974-9357.2019.00081.3
Archer, J. (2004). Sex differences in aggression in real-world settings: a meta-analytic review. Rev Gen Psychol. 8:291. doi: 10.1037/1089-2680.8.4.291
Armstrong, T. A., Boisvert, D., Flores, S., Symonds, M., and Gangitano, D. (2017). Heart rate, serotonin transporter linked polymorphic region (5-HTTLPR) genotype, and violence in an incarcerated sample. J. Crim. Just. 51, 1–8. doi: 10.1016/j.jcrimjus.2017.05.012
Arthur, M. J. P., Lee, A., and Wright, R. (1984). Sex differences in the metabolism of ethanol and acetaldehyde in normal subjects. Clin. Sci. 67, 397–401. doi: 10.1042/cs0670397
Australian Government (2017). What are drugs? Department of Health. Available online at: https://www.health.gov.au/health-topics/drugs/about-drugs/what-are-drugs
Badawy, A. A. B. (2003). Alcohol and violence and the possible role of serotonin. Crim. Behav. Mental Health 13, 31–44. doi: 10.1002/cbm.529
Badawy, A. B., Morgan, C. J., Lovett, J. W. T., Bradley, D. M., and Thomas, R. (1995). Decrease in circulating tryptophan availability to the brain after acute ethanol consumption by normal volunteers: implications for alcohol-induced aggressive behaviour and depression. Pharmacopsychiatry 28, 93–97. doi: 10.1055/s-2007-979626
Bakhshani, N. M. (2014). Impulsivity: a predisposition toward risky behaviors. Int. J. High Risk Behav. Addic. 3:20428. doi: 10.5812/ijhrba.20428
Bechara, A., Damasio, H., and Damasio, A. R. (2000). Emotion, decision making and the orbitofrontal cortex. Cerebral Cortex 10, 295–307. doi: 10.1093/cercor/10.3.295
Begum, S., Donta, B., Nair, S., and Prakasam, C. P. (2015). Socio-demographic factors associated with domestic violence in urban slums, Mumbai, Maharashtra, India. Indian J. Med. Res. 141, 783–788. doi: 10.4103/0971-5916.160701
Björkqvist, K. (2017). Gender differences in aggression. Curr. Opin. Psychol. 19, 39–42. doi: 10.1016/j.copsyc.2017.03.030
Bland, V. J., Lambie, I., and Best, C. (2018). Does childhood neglect contribute to violent behavior in adulthood? A review of possible links. Clin. Psychol. Rev. 60, 126–135. doi: 10.1016/j.cpr.2018.02.001
Block, R., and Block, C. (1992). Homicide syndromes and vulnerability: violence in Chicago's community areas over 25 years. Stud. Crime Crime Prevent. 1, 61–87.
Bobrova, N., West, R., Malyutina, D., Malyutina, S., and Bobak, M. (2010). Gender differences in drinking practices in middle aged and older russians. Alcohol Alcohol. (Oxford, Oxfordshire) 45, 573–580. doi: 10.1093/alcalc/agq069
Bradbury-Jones, C., and Isham, L. (2020). The pandemic paradox: the consequences of COVID-19 on domestic violence. J. Clin. Nurs. 29, 2047–2049. doi: 10.1111/jocn.15296
Branas, C. C., Han, S., and Wiebe, D. J. (2016). Alcohol use and firearm violence. Epidemiol. Rev. 38, 32–45. doi: 10.1093/epirev/mxv010
Brem, M. J., Florimbio, A. R., Elmquist, J., Shorey, R. C., and Stuart, G. L. (2018). Antisocial traits, distress tolerance, and alcohol problems as predictors of intimate partner violence in men arrested for domestic violence. Psychol. Viol. 8:132. doi: 10.1037/vio0000088
Brennan, P., Mednick, S. A., and Hodgins, S. (2000). Major mental disorders and criminal violence in a Danish birth cohort. Arch. Gen. Psychiatry 57, 494–500. doi: 10.1001/archpsyc.57.5.494
Brown, A. K., George, D. T., Fujita, M., Liow, J. S., Ichise, M., Hibbeln, J., et al. (2007). PET [11C] DASB imaging of serotonin transporters in patients with alcoholism. Alcohol. Clin. Exp. Res. 31, 28–32. doi: 10.1111/j.1530-0277.2006.00261.x
Bushman, B. J. (2002). Effects of alcohol on human aggression. Recent Dev. Alcohol. 13, 227–243. doi: 10.1007/0-306-47141-8_13
Bye, E. K. (2008). Alcohol and homicide in eastern europe: a time series analysis of six countries. Homicide Stud. 12/1, 7–27. doi: 10.1177/1088767907310851
Caetano, R., John, S., and Cunradi, C. B. (2001). Alcohol-related intimate partner violence among white, black, and Hispanic couples in the United States. Alcohol Res Health 25:158.
Capaldi, D. M., Knoble, N. B., Shortt, J. W., and Kim, H. K. (2012). A systematic review of risk factors for intimate partner violence. Partner Abuse 3, 231–280. doi: 10.1891/1946-6560.3.2.231
Chervyakov, V. V., Shkdnikov, V. M., Pridemore, W. A., and McKee, M. (2002). The changing nature of murder in Russia. Soc. Sci. Med. 55:17131724. doi: 10.1016/S0277-9536(01)00299-4
Chester, D. S., and DeWall, C. N. (2016). Sound the alarm: the effect of narcissism on retaliatory aggression is moderated by dACC reactivity to rejection. J. Pers. 84, 361–368. doi: 10.1111/jopy.12164
Chester, D. S., DeWall, C. N., Derefinko, K. J., Estus, S., Lynam, D. R., Peters, J. R., and Jiang, Y. (2016). Looking for reward in all the wrong places: dopamine receptor gene polymorphisms indirectly affect aggression through sensation-seeking. Soc. Neurosci. 11, 487–494. doi: 10.1080/17470919.2015.1119191
Chistiakov, D. A., and Chekhonin, V. P. (2017). Early-life adversity-induced long-term epigenetic programming associated with early onset of chronic physical aggression: studies in humans and animals. World J. Biol. Psychiatry. 20, 258–277. doi: 10.1080/15622975.2017.1322714
Chukwueke, C. C., Nona, C. N., McPhee, M. D., Mansouri, E., Rubin-Kahana, D. S., Martinez, D., et al. (2021). Exploring regulation and function of dopamine D3 receptors in alcohol use disorder. A PET [11C]-(+)-PHNO study. Neuropsychopharmacology 46, 2112–2120. doi: 10.1038/s41386-021-01095-2
Coccaro, E. F., Fanning, J. R., and Lee, R. (2017). Intermittent explosive disorder and substance use disorder: analysis of the national comorbidity survey replication sample. J. Clin. Psychiatry 78, 697–702. doi: 10.4088/JCP.15m10306
Coccaro, E. F., Fitzgerald, D. A., Lee, R., McCloskey, M., and Phan, K. L. (2016). Frontolimbic morphometric abnormalities in intermittent explosive disorder and aggression. Biol. Psychiatry Cogn. Neurosci. Neuroimag. 1, 32–38. doi: 10.1016/j.bpsc.2015.09.006
Conio, B., Martino, M., Magioncalda, P., Escelsior, A., Inglese, M., Amore, M., and Northoff, G. (2020). Opposite effects of dopamine and serotonin on resting-state networks: review and implications for psychiatric disorders. Mol. Psychiatry 25, 82–93. doi: 10.1038/s41380-019-0406-4
Crane, C. A., MacKenzie, L., Schlauch, R. C., Testa, M., and Easton, C. J. (2017). The proximal effects of acute alcohol use on female aggression: a meta-analytic review of the experimental literature. Psychol. Addict. Behav. 31:21. doi: 10.1037/adb0000244
Curtis, A., Vandenberg, B., Mayshak, R., Coomber, K., Hyder, S., Walker, A., et al. (2019). Alcohol use in family, domestic and other violence: findings from a cross-sectional survey of the Australian population. Drug Alcohol Rev. 38, 349–358. doi: 10.1111/dar.12925
Davidson, R. J., Putnam, K. M., and Larson, C. L. (2000). Dysfunction in the neural circuitry of emotion regulation – a possible prelude to violence. Science 289, 591–594. doi: 10.1126/science.289.5479.591
De Paula Gebara, C. F., Ferri, C. P., Lourenço, L. M., de Toledo Vieira, M., de Castro Bhona, F. M., and Noto, A. R. (2015). Patterns of domestic violence and alcohol consumption among women and the effectiveness of a brief intervention in a household setting: a protocol study. BMC Womens Health 15, 1–8. doi: 10.1186/s12905-015-0236-8
Denson, T. F., O'Dean, S. M., Blake, K. T., and Beames, J. R. (2018). Aggression in women: behavior, brain and hormones. Front. Behav. Neurosci. 12:81. doi: 10.3389/fnbeh.2018.00081
Devries, K. M., Child, J. C., Bacchus, L. J., Mak, J., Falder, G., Graham, K., et al. (2014). Intimate partner violence victimization and alcohol consumption in women: a systematic review and meta-analysis. Addiction (Abingdon, England) 109, 379–391. doi: 10.1111/add.12393
Dobash, R. E., and Dobash, R. P. (2011). What were they thinking? Men who murder an intimate partner. Viol. Against Women 17, 111–134. doi: 10.1177/1077801210391219
Drake, S. (2010). The toxicology of homicide offenders and victims: a review. Drug Alcohol Rev. 29, 202–215 doi: 10.1111/j.1465-3362.2009.00099.x
Duailibi, S., Ponicki, W., Grube, J., Pinsky, I., Laranjeira, R., and Raw, M. (2007). The effect of restricting opening hours on alcohol-related violence. Am. J. Public Health. 97, 2276–2280. doi: 10.2105/AJPH.2006.092684
Duica, L., Dragulescu, V., and Pîrlog, M. (2020). Neurobiological elements of hopelessness and impulsivity in suicidal behavior. Int. J. Med. Rev. Case Rep. 4, 1–4. doi: 10.5455/IJMRCR.suicidal-behaviour-neuro
Duke, A. A., Smith, K. M., Oberleitner, L., Westphal, A., and McKee, S. A. (2018). Alcohol, drugs, and violence: a meta-meta-analysis. Psychol. Viol. 8:238. doi: 10.1037/vio0000106
Eisner, M. P., and Malti, T. (2015). Aggressive and violent behavior. Handbook Child Psychol. Dev. Sci. 794–841. doi: 10.1002/9781118963418.childpsy319
Emmerling, F., Schuhmann, T., Lobbestael, J., Arntz, A., Brugman, S., and Sack, A. T. (2016). The role of the insular cortex in retaliation. PLoS ONE 11:e0152000. doi: 10.1371/journal.pone.0152000
Eriksson, L., Bryant, S., McPhedran, S., Mazerolle, P., and Wortley, R. (2020). Alcohol and drug problems among Australian homicide offenders. Addiction. 116, 618–631. doi: 10.1111/add.15169
Erkiran, M., Özünalan, H., Evren, C., Aytaçlar, S., Kirisci, L., and Tarter, R. (2006). Substance abuse amplifies the risk for violence in schizophrenia spectrum disorder. Addict. Behav. 31, 1797–1805. doi: 10.1016/j.addbeh.2005.12.024
Evans, E. A., Grella, C. E., and Upchurch, D. M. (2017). Gender differences in the effects of childhood adversity on alcohol, drug, and polysubstance-related disorders. Soc. Psychiatry Psychiatr. Epidemiol. 52, 901–912. doi: 10.1007/s00127-017-1355-3
Fanning, J. R., Lee, R., and Coccaro, E. F. (2020). “Chapter 10: Neurotransmitter function in impulsive aggression and intermittent explosive disorder,” in The Wiley International Handbook on Psychopathic Disorders and the Law, 2nd Edn. p. 249–269. doi: 10.1002/9781119159322.ch10
Fava, N. M., Trucco, E. M., Martz, M. E., Cope, L. M., Jester, J. M., Zucker, R. A., et al. (2019). Childhood adversity, externalizing behavior, and substance use in adolescence: Mediating effects of anterior cingulate cortex activation during inhibitory errors. Dev. Psychopathol. 31, 1439–1450. doi: 10.1017/S0954579418001025
Felson, R. B., and Staff, J. (2010). The effects of alcohol intoxication on violent versus other offending. Crim. Just. Behav. 37:13431360. doi: 10.1177/0093854810382003
Ferrari, G., Agnew-Davies, R., Bailey, J., Howard, L., Howarth, E., Peters, T. J., et al. (2016). Domestic violence and mental health: a cross-sectional survey of women seeking help from domestic violence support services. Global Health Act. 9:29890. doi: 10.3402/gha.v9.29890
Finlay, I., and Gilmore, I. (2020). Covid-19 and alcohol—a dangerous cocktail. BMJ 369:m1987 doi: 10.1136/bmj.m1987
Foran, H. M., and O'Leary, K. D. (2008). Alcohol and intimate partner violence: a meta-analytic review. Clin. Psychol. Rev. 28, 1222–1234. doi: 10.1016/j.cpr.2008.05.001
Forsman, J., Sturup, J., and Masterman, T. (2018). Pre-offense alcohol intake in homicide offenders and victims: a forensic-toxicological case-control study. J. Foren. Legal Med. 56, 55–58. doi: 10.1016/j.jflm.2018.03.004
Fritz, M., Rösel, F., Dobler, H., Streb, J., and Dudeck, M. (2021). Childhood trauma, the combination of MAO-A and COMT genetic polymorphisms and the joy of being aggressive in forensic psychiatric patients. Brain Sci. 11:1008. doi: 10.3390/brainsci11081008
Gadd, D., Henderson, J., Radcliffe, P., Stephens-Lewis, D., Johnson, A., and Gilchrist, G. (2019). The dynamics of domestic abuse and drug and alcohol dependency. Br. J. Criminol. 59, 1035–1053. doi: 10.1093/bjc/azz011
Galbicsek, C. (2020). Alcohol-Related Crimes. Available online at: https://www.alcoholrehabguide.org/alcohol/crimes/ (accessed October 15, 2021).
Gan, G., Sterzer, P., Marxen, M., Zimmermann, U. S., and Smolka, M. N. (2015). Neural and behavioral correlates of alcohol-induced aggression under provocation. Neuropsychopharmacology 40, 2886–2896. doi: 10.1038/npp.2015.141
Gass, J. D., Stein, D. J., Williams, D. R., and Seedat, S. (2011). Gender differences in risk for intimate partner violence among South African adults. J. Interpers. Violence 26, 2764–2789. doi: 10.1177/0886260510390960
Giancola, P. R., and Zeichner, A. (1995). An investigation of gender differences in alcohol-related aggression. J. Stud Alcohol 56, 573–579. doi: 10.15288/jsa.1995.56.573
Gimeno, C., Dorado, M. L., Roncero, C., Szerman, N., Vega, P., Balanzá-Martínez, V., et al. (2017). Treatment of comorbid alcohol dependence and anxiety disorder: review of the scientific evidence and recommendations for treatment. Front. Psychiatry 8:173. doi: 10.3389/fpsyt.2017.00173
Goldstein, R. B., Chou, S. P., Saha, T. D., Smith, S. M., Jung, J., Zhang, H., et al. (2017). The epidemiology of antisocial behavioral syndromes in adulthood: results from the national epidemiologic survey on alcohol and related conditions-III. J. Clin. Psychiatry 78, 90–98. doi: 10.4088/JCP.15m10358
Gollan, J. K., Lee, R., and Coccaro, E. F. (2005). Developmental psychopathology and neurobiology of aggression. Dev. Psychopathol. 17, 1151–1171. doi: 10.1017/S0954579405050546
Gonçalves, R. E. M., Ponce, J. C., and Leyton, V. (2020). Alcohol consumption and violent deaths in the city of São Paulo in 2015. Subst. Use Misuse. 55, 1875–1880. doi: 10.1080/10826084.2020.1771596
Gorlova, A., Ortega, G., Waider, J., Bazhenova, N., Veniaminova, E., Proshin, A., et al. (2020). Stress-induced aggression in heterozygous TPH2 mutant mice is associated with alterations in serotonin turnover and expression of 5-HT6 and AMPA subunit 2A receptors. J. Affect. Disord. 272, 440–451. doi: 10.1016/j.jad.2020.04.014
Gottfried, E. D., and Christopher, S. C. (2017). Mental disorders among criminal offenders: a review of the literature. J. Correct. Health Care 23, 336–346. doi: 10.1177/1078345817716180
Goyer, P. F., Andreason, P. J., Semple, W. E., Clayton, A. H., King, A. C., Compton-Toth, B. A., et al. (1994). Positron-emission tomography and personality disorders. Neuropsychopharmacology 10:21. doi: 10.1038/npp.1994.3
Graham, K., Bernards, S., Wilsnack, S., and Gmel, G. (2011). Alcohol may not cause partner violence but it seems to make it worse. J. Interpers. Violence 26, 1503–1523. doi: 10.1177/0886260510370596
Guclu, Y. A., and Can, H. (2018). Ethnic background and alcohol use of the spouse emerge as major risk factors for domestic violence: an observational study from Turkey. JPMA. J. Pak. Med. Assoc. 68, 1782–1786.
Hagelstam, C., and Häkkänen, H. (2006). Homicidal adolescents: offense and offender characteristics. Foren. Sci. Int. 164, 110–115. doi: 10.1016/j.forsciint.2005.12.006
Harrison, A. A., Everitt, B. J., and Robbins, T. W. (1997). Central 5-HT depletion enhances impulsive responding without affecting the accuracy of attentional performance: interactions with dopaminergic mechanisms. Psychopharmacology (Berl) 133, 329–342. doi: 10.1007/s002130050410
Hasin, D. S., Dvora, S., and Katherine, K. (2019). Alcohol use and binge drinking among US men, pregnant and non-pregnant women ages 18–44: 2002–2017. Drug Alcohol Depend. 205:107590. doi: 10.1016/j.drugalcdep.2019.107590
Heinrichs, R. (1989). Frontal cerebral lesions and violent incidents in chronic neuropsychiatric patients. Biol. Psychiatry 25, 174–178. doi: 10.1016/0006-3223(89)90161-3
Helle, A. C., Watts, A. L., Trull, T. J., and Sher, K. J. (2019). Alcohol use disorder and antisocial and borderline personality disorders. Alcohol Res. Health. 40. doi: 10.35946/arcr.v40.1.05
Hentges, R. F., Shaw, D. S., and Wang, M. T. (2018). Early childhood parenting and child impulsivity as precursors to aggression, substance use, and risky sexual behavior in adolescence and early adulthood. Dev. Psychopathol. 30, 1305–1319. doi: 10.1017/S0954579417001596
Higley, J. D., and Linnoila, M. (2002). A nonhuman primate model of excessive alcohol intake. Recent Dev. Alcohol. 13, 191–219. doi: 10.1007/0-306-47141-8_11
Hoaken, P. N. S., and Pihl, R. O. (2000). The effects of alcohol intoxication on aggressive responses in men and women. Alcohol Alcohol. 35, 471–477. doi: 10.1093/alcalc/35.5.471
Hockin, S., Rogers, M. L., and Pridemore, W. A. (2018). Population-level alcohol consumption and national homicide rates. Eur. J. Criminol. 15, 235–252. doi: 10.1177/1477370817731042
Holmes, A. J., Hollinshead, M. O., Roffman, J. L., Smoller, J. W., and Buckner, R. L. (2016). Individual differences in cognitive control circuit anatomy link sensation seeking, impulsivity, and substance use. J.Neurosci. 36, 4038–4049. doi: 10.1523/JNEUROSCI.3206-15.2016
Hoppen, T. H., and Chalder, T. (2018). Childhood adversity as a transdiagnostic risk factor for affective disorders in adulthood: a systematic review focusing on biopsychosocial moderating and mediating variables. Clin. Psychol. Rev. 65, 81–151. doi: 10.1016/j.cpr.2018.08.002
Hoppenbrouwers, S. S., Hofman, D., and Schutter, D. J. (2010). Alcohol breaks down interhemispheric inhibition in females but not in males. Psychopharmacology 208, 469–474. doi: 10.1007/s00213-009-1747-5
Hutchison, I. W. (1999). Alcohol, fear and woman abuse. Sex Roles. 40, 893–920. doi: 10.1023/A:1018877106056
Indu, P. V., Jinu, C. R., Pallikkal, N. R., Sampathkumar, R., and Joy, J. (2018). Experience of domestic violence and psychological morbidity in spouses of alcohol-dependent males. Indian J. Psychol. Med. 40, 322–327. doi: 10.4103/IJPSYM.IJPSYM_38_18
Ito, T. A., Miller, N., and Pollock, V. E. (1996). Alcohol and aggression: a meta-analysis on the moderating effects of inhibitory cues, triggering events, and self-focused attention. Psychol. Bull. 120:60. doi: 10.1037/0033-2909.120.1.60
Iverson, K. M., Litwack, S. D., Pineles, S. L., Suvak, M. K., Vaughn, R. A., and Resick, P. A. (2013), Predictors of intimate partner violence revictimization. J. Traumatic Stress 26, 102–110. doi: 10.1002/jts.21781
Jiang, W., Shi, F., Liu, H., Li, G., Ding, Z., Shen, H., et al. (2017). Reduced white matter integrity in antisocial personality disorder: a diffusion tensor imaging study. Sci. Rep. 7, 1–11. doi: 10.1038/srep43002
Kamal, H., Tan, G. C., Ibrahim, S. F., Shaikh, M. F., Mohamed, I. N., Mohamed, R. M. P., et al. (2020). Alcohol use disorder, neurodegeneration, Alzheimer's and Parkinson's disease: interplay between oxidative stress, neuroimmune response and excitotoxicity. Front. Cell. Neurosci. 14:282. doi: 10.3389/fncel.2020.00282
Kanen, J. W., Arntz, F. E., Yellowlees, R., Cardinal, R. N., Price, A., Christmas, D. M., et al. (2021). Serotonin depletion amplifies distinct human social emotions as a function of individual differences in personality. Transl. Psychiatry 11, 1–12. doi: 10.1038/s41398-020-00880-9
Karlsson, T. (1998). Sharp force homicides in the Stockholm area, 1983-1992. Foren. Sci. Int. 94, 129–139. doi: 10.1016/S0379-0738(98)00067-X
Kästner, N., Richter, S. H., Urbanik, S., Kunert, J., Waider, J., Lesch, K. P., et al. (2019). Brain serotonin deficiency affects female aggression. Sci. Rep. 9:1366. doi: 10.1038/s41598-018-37613-4
Kaufmann, V. G., O'Farrell, T. J., Murphy, C. M., Murphy, M. M., and Muchowski, P. (2014). Alcohol consumption and partner violence among women entering substance use disorder treatment. Psychol. Addict. Behav. 28, 313–321. doi: 10.1037/a0034971
Kazzaz, Y. M., AlAmeer, K. M., AlAhmari, R. A., Househ, M., and El-Metwally, A. (2019). The epidemiology of domestic violence in Saudi Arabia: a systematic review. Int. J. Public Health 64, 1223–1232. doi: 10.1007/s00038-019-01303-3
Khodabandeh, F., Khalilzadeh, M., and Hemati, Z. (2018). The impact of adverse childhood experiences on adulthood aggression and self-esteem-a study on male forensic clients. Novelty Biomed. 6, 85–91.
Kim, M. J., Elliott, M. L., d'Arbeloff, T. C., Knodt, A. R., Radtke, S. R., Brigidi, B. D., et al. (2019). Microstructural integrity of white matter moderates an association between childhood adversity and adult trait anger. Aggressive Behav. 45, 310–318. doi: 10.1002/ab.21820
Kim, M. J., Scult, M. A., Knodt, A. R., Radtke, S. R., d'Arbeloff, T. C., Brigidi, B. D., et al. (2018). A link between childhood adversity and trait anger reflects relative activity of the amygdala and dorsolateral prefrontal cortex. Biol. Psychiatry Cogn. Neurosci. Neuroimag. 3, 644–649. doi: 10.1016/j.bpsc.2018.03.006
Kovács, I., Demeter, I., Janka, Z., Demetrovics, Z., Maraz, A., and Andó, B. (2020). Different aspects of impulsivity in chronic alcohol use disorder with and without comorbid problem gambling. PLoS ONE 15:e0227645. doi: 10.1371/journal.pone.0227645
Kuhns, J. B., Exum, M. L., Clodfelter, T. A., and Bottia, M. C. (2014). The prevalence of alcohol-involved homicide offending: a meta-analytic review. Homicide Stud. 18, 251–270. doi: 10.1177/1088767913493629
Kumar, J., Hapidin, H., Bee, Y. T. G., and Ismail, Z. (2013). Effects of the mGluR5 antagonist MPEP on ethanol withdrawal induced anxiety-like syndrome in rats. Behav. Brain Funct. 9, 1–13. doi: 10.1186/1744-9081-9-43
Kumar, J., Hapidin, H., Bee, Y. T. G., and Ismail, Z. (2016). The effects of acute ethanol administration on ethanol withdrawal-induced anxiety-like syndrome in rats: a biochemical study. Alcohol 50, 9–17. doi: 10.1016/j.alcohol.2015.10.001
Kumar, J., Ismail, Z., Hatta, N. H., Baharuddin, N., Hapidin, H., Get Bee, Y. T., et al. (2018). Alcohol addiction-metabotropic glutamate receptor subtype 5 and its ligands: How they all come together? Curr. Drug Targets 19, 907–915. doi: 10.2174/1389450118666170511144302
Kuypers, K. P. C., Verkes, R. J., Van den Brink, W., Van Amsterdam, J. G. C., and Ramaekers, J. G. (2020). Intoxicated aggression: do alcohol and stimulants cause dose-related aggression? A review. Eur. Neuropsychopharmacol. 30, 114–147. doi: 10.1016/j.euroneuro.2018.06.001
Kwagala, B., Wandera, S. O., Ndugga, P., and Kabagenyi, A. (2013). Empowerment, partner's behaviours and intimate partner physical violence among married women in Uganda. BMC Public Health 13:1112. doi: 10.1186/1471-2458-13-1112
Labella, M. H., and Masten, A. S. (2018). Family influences on the development of aggression and violence. Curr. Opin. Psychol. 19, 11–16. doi: 10.1016/j.copsyc.2017.03.028
Lagerberg, T., Fazel, S., Molero, Y., Franko, M. A., Chen, Q., Hellner, C., et al. (2020). Associations between selective serotonin reuptake inhibitors and violent crime in adolescents, young, and older adults–a Swedish register-based study. Eur. Neuropsychopharmacol. 36, 1–9. doi: 10.1016/j.euroneuro.2020.03.024
Landberg, J., and Norström, T. (2011). Alcohol and homicide in Russia and the United States: a comparative analysis. J. Stud. Alcohol Drugs 72, 723–730. doi: 10.15288/jsad.2011.72.723
Lapierre, D., Braun, C. M. J., and Hodgings, S. (1995). Ventral frontal deficits in psychopathy: neuropsychological test findings. Neuropsychologia 33, 139–151. doi: 10.1016/0028-3932(94)00110-B
Latkin, C. A., Edwards, C., Davey-Rothwell, M. A., and Tobin, K. E. (2017). The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland. Addict. Behav. 73, 133–136. doi: 10.1016/j.addbeh.2017.05.005
Lawrence, A. D., Calder, A. J., McGowan, S. W., and Grasby, P. M. (2002). Selective disruption of the recognition of facial expressions of anger. Neuroreport 13, 881–884. doi: 10.1097/00001756-200205070-00029
Lee, M., Stefani, K. M., and Park, E. C. (2014). Gender-specific differences in risk for intimate partner violence in South Korea. BMC Public Health 14:415. doi: 10.1186/1471-2458-14-415
Lee, R., Arfanakis, K., Evia, A. M., Fanning, J., Keedy, S., and Coccaro, E. F. (2016). White matter integrity reductions in intermittent explosive disorder. Neuropsychopharmacology 41, 2697–2703. doi: 10.1038/npp.2016.74
Leite, F., Luis, M. A., Amorim, M., Maciel, E., and Gigante, D. P. (2019). Violence against women and its association with the intimate partner's profile: a study with primary care users. Brazilian J. Epidemiol. 22:e190056.
Lemgruber, V. B., and Juruena, M. F. (2013). The role of early life stress in adult psychiatric disorders. J. Nerv. Ment. Dis. 201:1007Y1020. doi: 10.1097/NMD.0000000000000049
Leurquin-Sterk, G., Ceccarini, J., Crunelle, C. L., Weerasekera, A., de Laat, B., Himmelreich, U., et al. (2018). Cerebral dopaminergic and glutamatergic transmission relate to different subjective responses of acute alcohol intake: an in vivo multimodal imaging study. Addict. Biol. 23, 931–944. doi: 10.1111/adb.12542
Lewis, R. J., Padilla, M. A., Milletich, R. J., Kelley, M. L., Winstead, B. A., Lau-Barraco, C., et al. (2015). Emotional distress, alcohol use, and bidirectional partner violence among lesbian women. Violence Against Women 21, 917–938. doi: 10.1177/1077801215589375
Liem, M., Soenita, G., Sven, G., Johanna, H., Janne, K., Martti, L., et al. (2013). Homicide in Finland, the Netherlands, and Sweden: first findings from the European homicide monitor. Homicide Stud. 17, 75–95. doi: 10.1177/1088767912452130
Linnoila, M., Virkkunen, M., Scheinin, M., Nuutila, A., Rimon, R., and Goodwin, F. K. (1983). Low cerebrospinal fluid 5-hydroxyindoleacetic acid concentration differentiates impulsive from nonimpulsive violent behavior. Life Sci. 33, 2609–2614. doi: 10.1016/0024-3205(83)90344-2
Lipsey, M. W., Wilson, B. M., Cohen, M. A., and Derzon, J. H. (1997). “Is there a causal relationship between alcohol use and violence?,” in: Recent Developments in Alcoholism and Violence, eds. M. Galanter (New York, NY: Plenum Press), 245–282.
Lira, M. C., Xuan, Z., Coleman, S. M., Swahn, M. H., Heeren, T. C., and Naimi, T. S. (2019). Alcohol policies and alcohol involvement in intimate partner homicide in the U.S. Am. J. Prevent. Med. 57, 172–179. doi: 10.1016/j.amepre.2019.02.027
Liu, C., Tian, X., Ling, Y., Xu, J., and Zhou, X. (2020). Alterations of metabolites in the frontal cortex and amygdala are associated with cognitive impairment in alcohol dependent patients with aggressive behavior. Front. Psychiatry 11:684. doi: 10.3389/fpsyt.2020.00694
Livingston, M. (2011). A longitudinal analysis of alcohol outlet density and domestic violence. Addiction (Abingdon, England) 106, 919–925. doi: 10.1111/j.1360-0443.2010.03333.x
Madole, J. W., Johnson, S. L., and Carver, C. S. (2020). A model of aggressive behavior: early adversity, impulsivity, and response inhibition. J. Aggr. Maltreat. Trauma 29, 594–610. doi: 10.1080/10926771.2019.1591561
Maffli, E., and Zumbrunn, A. (2003). Alcohol and domestic violence in a sample of incidents reported to the police of Zurich City. Subst. Use Misuse 38, 881–893. doi: 10.1081/JA-120017615
Malti, T. (2020). Children and violence: nurturing social-emotional development to promote mental health. Soc. Policy Rep. 33, 1–27. doi: 10.1002/sop2.8
Mann, R. E., Zalcman, R. F., Smart, R. G., Rush, B. R., and Suurvali, H. (2006). Alcohol consumption, alcoholics anonymous membership, and homicide mortality rates in Ontario 1968 to 1991. Alcohol. Clin. Exp. Res. 30, 1743–1751. doi: 10.1111/j.1530-0277.2006.00216.x
Mantere, T., Tupala, E., Hall, H., Särkioja, T., Räsänen, P., Bergström, K., et al. (2002). Serotonin transporter distribution and density in the cerebral cortex of alcoholic and nonalcoholic comparison subjects: a whole-hemisphere autoradiography study. Am. J. Psychiatry. 159, 599–606. doi: 10.1176/appi.ajp.159.4.599
Martin, S., Zabala, C., Del-Monte, J., Graziani, P., Aizpurua, E., Barry, T. J., et al. (2019). Examining the relationships between impulsivity, aggression, and recidivism for prisoners with antisocial personality disorder. Aggr. Violent Behav. 49:101314. doi: 10.1016/j.avb.2019.07.009
Martinez, D., Slifstein, M., Gil, R., Hwang, D. R., Huang, Y., Perez, A., et al. (2009). Positron emission tomography imaging of the serotonin transporter and 5-HT1A receptor in alcohol dependence. Biol. Psychiatry. 65, 175–180. doi: 10.1016/j.biopsych.2008.08.034
Mayshak, R., Curtis, A., Coomber, K., Tonner, L., Walker, A., Hyder, S., et al. (2020). Alcohol-involved family and domestic violence reported to police in Australia. J. Interpers. Violence 886260520928633. doi: 10.1177/0886260520928633
McCloskey, M. S., Phan, K. L., Angstadt, M., Fettich, K. C., Keedy, S., and Coccaro, E. F. (2016). Amygdala hyperactivation to angry faces in intermittent explosive disorder. J. Psychiatr. Res. 79, 34–41. doi: 10.1016/j.jpsychires.2016.04.006
McLaughlin, K. A., Weissman, D., and Bitrán, D. (2019). Childhood adversity and neural development: a systematic review. Ann. Rev. Dev. Psychol. 1, 277–312. doi: 10.1146/annurev-devpsych-121318-084950
McRae, K., Ochsner, K. N., Mauss, I. B., Gabrieli, J. J. D., and Gross, J. J. (2008). Gender differences in emotion regulation: an fMRI study of cognitive reappraisal. Gr. Process Intergr. Relat. 11, 143–162. doi: 10.1177/1368430207088035
Melendez, R. I., Rodd-Henricks, Z. A., Engleman, E. A., Li, T. K., McBride, W. J., and Murphy, J. M. (2002). Microdialysis of dopamine in the nucleus accumbens of alcohol-preferring (P) rats during anticipation and operant self-administration of ethanol. Alcohol Clin. Exp. Res. 26, 318–325. doi: 10.1111/j.1530-0277.2002.tb02540.x
Mokdad, A. H., Marks, J. S., Stroup, D. F., and Geberding, J. L. (2004). Actual causes of death in the United States, 2000. J. Am. Med. Assoc. 291, 1238–1245. doi: 10.1001/jama.291.10.1238
Naimi, T. S., Xuan, Z., Coleman, S. M., Lira, M. C., Hadland, S. E., Cooper, S. E., et al. (2017). Alcohol policies and alcohol-involved homicide victimization in the United States. J. Stud. Alcohol Drugs 78, 781–788. doi: 10.15288/jsad.2017.78.781
Ninomiya, T., Oshita, H., Kawano, Y., Goto, C., Matsuhashi, M., Masuda, K., et al. (2018). Reduced white matter integrity in borderline personality disorder: a diffusion tensor imaging study. J. Affect. Disord. 225, 723–732. doi: 10.1016/j.jad.2017.09.007
Nord, M., Finnema, S. J., Halldin, C., and Farde, L. (2013). Effect of a single dose of escitalopram on serotonin concentration in the non-human and human primate brain. Int. J. Neuropsychopharmacol. 16, 1577–1586. doi: 10.1017/S1461145712001617
Pakri Mohamed, R. M., Kumar, J., Ahmad, S. U., and Mohamed, I. N. (2018). Novel pharmacotherapeutic approaches in treatment of alcohol addiction. Curr. Drug Targets 19, 1378–1390. doi: 10.2174/1389450119666180523092534
Pewa, P., Thomas, S., Dagli, R., Solanki, J., Arora, G., and Garla, B. (2015). Occurrence of domestic violence among women and its impact on oral health in Jodhpur City. J. Contemp. Dental Pract. 16, 227–233. doi: 10.5005/jp-journals-10024-1666
Pietrini, P., Guazzelli, M., Basso, G., Jaffe, K., and Grafman, J. (2000). Neural correlates of imaginal aggressive behavior assessed by positron emission tomography in healthy subjects. Am. J. Psychiatry 157, 1772–1781. doi: 10.1176/appi.ajp.157.11.1772
Pilkington, P. D., Bishop, A., and Younan, R. (2021). Adverse childhood experiences and early maladaptive schemas in adulthood: a systematic review and meta-analysis. Clin. Psychol. Psychother. 28, 569–565 doi: 10.1002/cpp.2533
Pinel, J. P. J., and Barnes, S. J. (2018). Biopsychology, 10th Edn. England: Pearson Education Limited.
Poldrugo, F. (1998). General clinical, ethical and medico-legal aspects - alcohol and criminal behaviour. Alcohol Alcohol. 33, 12–15. doi: 10.1093/oxfordjournals.alcalc.a008340
Popova, N. K., Ilchibaeva, T. V., Antonov, E. V., Pershina, A. V., Bazovkina, D. V., and Naumenko, V. S. (2020). On the interaction between BDNF and serotonin systems: the effects of long-term ethanol consumption in mice. Alcohol. 87, 1–15. doi: 10.1016/j.alcohol.2020.04.002
Porter, C., Palmier-Claus, J., Branitsky, A., Mansell, W., Warwick, H., and Varese, F. (2020). Childhood adversity and borderline personality disorder: a meta-analysis. Acta Psychiatr. Scand. 141, 6–20. doi: 10.1111/acps.13118
Prepelita, R., Cristofor, A. C., Dobrin, R., Trus, C., Ciobica, A., and Chirita, R. (2019). The serotonin-dopamine relationship on the aggression-suicidal risk axis in patients with major depression disorder: describing some social implications. Rev. Cercetare Interv. Soc. 65, 111–130. doi: 10.33788/rcis.65.8
Puhalla, A. A., Berman, M. E., Coccaro, E. F., Fahlgren, M. K., and McCloskey, M. S. (2020). History of childhood abuse and alcohol use disorder: relationship with intermittent explosive disorder and intoxicated aggression frequency. J. Psychiatr. Res. 125, 38–44. doi: 10.1016/j.jpsychires.2020.02.025
Qadeer, M. I., Amar, A., Huang, Y. Y., Min, E., Galfalvy, H., Hasnain, S., et al. (2021). Association of serotonin system-related genes with homicidal behavior and criminal aggression in a prison population of Pakistani Origin. Sci. Rep. 11, 1–12. doi: 10.1038/s41598-021-81198-4
Qadeer, M. I., Amar, A., Mann, J. J., and Hasnain, S. (2017). Polymorphisms in dopaminergic system genes; association with criminal behavior and self-reported aggression in violent prison inmates from Pakistan. PLoS ONE 12:e0173571. doi: 10.1371/journal.pone.0173571
Rahko, J., Paakki, J. J., Starck, T., Nikkinen, J., Remes, J., Hurtig, T., et al. (2010). Functional mapping of dynamic happy and fearful facial expression processing in adolescents. Brain Imaging Behav. 4, 164–176. doi: 10.1007/s11682-010-9096-x
Raine, A., Lencz, T., Bihrle, S., LaCasse, L., and Colletti, P. (2000). Reduced prefrontal gray matter volume and reduced autonomic activity in antisocial personality disorder. Arch. Gen. Psychiatry 57, 119–127. doi: 10.1001/archpsyc.57.2.119
Raine, A., Meloy, J. R., Bihrle, S., Stoddard, J., LaCasse, L., and Buchsbaum, M. S. (1998). Reduced prefrontal and increased subcortical brain functioning assessed using positron emission tomography in predatory and affective murderers. Behav. Sci. Law 16, 319–332. doi: 10.1002/(sici)1099-0798(199822)16:3<319::aid-bsl311>3.0.co;2-g
Rappek, N. A. M., Sidi, H., Kumar, J., Kamarazaman, S., Das, S., Masiran, R., et al. (2018). Serotonin selective reuptake inhibitors (SSRIs) and female sexual dysfunction (FSD): hypothesis on its association and options of treatment. Curr. Drug Targets 19, 1352–1358. doi: 10.2174/1389450117666161227142947
Reno, J., Marcus, D., Leary, M.-L., and Samuels, J. E. (2010). Full Report of the Prevalence, Incidence, and Consequences of Violence Against Women. Department of Justice. Available online at: https://www.ncjrs.gov/pdffiles1/nij/183781.pdf
Renzetti, C. M., Lynch, K. R., and DeWall, C. N. (2018). Ambivalent sexism, alcohol use, and intimate partner violence perpetration. J. Interp. Violence 33, 183–210. doi: 10.1177/0886260515604412
Repple, J., Ute, H., Lisa, W., Christina, M. P., Schneider, F., and Kohn, N. (2018). "Sex differences in the neural correlates of aggression. Brain Struct. Funct. 223, 4115–4124. doi: 10.1007/s00429-018-1739-5
Room, R., and Rossow, I. (2001). Share of violence attributable to drinking. J. Subst. Use 6, 218–228. doi: 10.1080/146598901753325048
Rossow, I. (2001). Alcohol and homicide: a cross-cultural comparison of the relationship in 14 European countries. Addiction 96(Suppl. 1), S77–92. doi: 10.1080/09652140020021198
Rossow, I. (2004). Alcohol consumption and homicides in Canada, 1950–1999. Contemp. Drug Prob. 31, 541–559. doi: 10.1177/009145090403100305
Runions, K. C., Morandini, H. A., Rao, P., Wong, J. W., Kolla, N. J., Pace, G., et al. (2019). Serotonin and aggressive behaviour in children and adolescents: a systematic review. Acta Psychiatr. Scand. 139, 117–144. doi: 10.1111/acps.12986
Sarah, M., and Keyes, K. M. (2019). Heavy and binge alcohol drinking and parenting status in the United States from 2006 to 2018: an analysis of nationally representative cross-sectional surveys. PLoS Med. 16:e1002954. doi: 10.1371/journal.pmed.1002954
Sarah, M., and Keyes, K. M. (2020). Trends in US women's binge drinking in middle adulthood by socioeconomic status, 2006–2018. Drug Alcohol Depend. 212:108026. doi: 10.1016/j.drugalcdep.2020.108026
Schorr, M. T., Tietbohl-Santos, B., de Oliveira, L. M., Terra, L., de Borba Telles, L. E., and Hauck, S. (2020). Association between different types of childhood trauma and parental bonding with antisocial traits in adulthood: a systematic review. Child Abuse Neglect 107:104621. doi: 10.1016/j.chiabu.2020.104621
Schouw, J. E., Verkes, R. J., Schene, A. H., and Schellekens, A. F. (2020). The relationship between childhood adversity and adult personality revealed by network analysis. Child Abuse Neglect 99:104254. doi: 10.1016/j.chiabu.2019.104254
Schwab-Reese, L. M., Parker, E. A., and Peek-Asa, C. (2020). Interactions of adolescent social experiences and dopamine genes to predict physical intimate partner violence perpetration. PLoS ONE 12:e0172840. doi: 10.1371/journal.pone.0172840
Semahegn, A., Belachew, T., and Abdulahi, M. (2013). Domestic violence and its predictors among married women in reproductive age in Fagitalekoma Woreda, Awi zone, Amhara regional state, North Western Ethiopia. Reprod. Health 10:63. doi: 10.1186/1742-4755-10-63
Seo, D., Patrick, C. J., and Kennealy, P. J. (2008). Role of serotonin and dopamine system interactions in the neurobiology of impulsive aggression and its comorbidity with other clinical disorders. Aggres. Violent Behav. 13, 383–395. doi: 10.1016/j.avb.2008.06.003
Seok, J. W., and Cheong, C. (2020). Gray matter deficits and dysfunction in the insula among individuals with intermittent explosive disorder. Front. Psychiatry 11:439. doi: 10.3389/fpsyt.2020.00439
Serafini, G., Gonda, X., Canepa, G., Pompili, M., Rihmer, Z., Amore, M., et al. (2017). Extreme sensory processing patterns show a complex association with depression, and impulsivity, alexithymia, and hopelessness. J. Affect. Disord. 210, 249–257. doi: 10.1016/j.jad.2016.12.019
Sharp, T., and Barnes, N. M. (2020). Central 5-HT receptors and their function; present and future. Neuropharmacology 177:108155. doi: 10.1016/j.neuropharm.2020.108155
Siep, N., Tonnaer, F., van de Ven, V., Arntz, A., Raine, A., and Cima, M. (2019). Anger provocation increases limbic and decreases medial prefrontal cortex connectivity with the left amygdala in reactive aggressive violent offenders. Brain Imaging Behav. 13, 1311–1323. doi: 10.1007/s11682-018-9945-6
Siever, L. J., Buchsbaum, M. S., New, A. S., Spiegel-Cohen, J., Wei, T., Hazlett, E. A., et al. (1999). l-fenfluramine response in impulsive personality disorder assessed with [18F] fluorodeoxyglucose positron emission tomography. Neuropsychopharmacology 20, 413–423. doi: 10.1016/S0893-133X(98)00111-0
Smith, P. H., Homish, G. G., Leonard, K. E., and Cornelius, J. R. (2012). Intimate partner violence and specific substance use disorders: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol. Addict. Behav. 26, 236–245. doi: 10.1037/a0024855
Storvik, M., Hakkinen, M., Tupala, E., and Tiihonen, J. (2009). 5-HT(1A) receptors in the frontal cortical brain areas in Cloninger type 1 and 2 alcoholics measured by whole-hemisphere autoradiography. Alcohol. Alcohol. 44, 2–7. doi: 10.1093/alcalc/agn090
Swart, L., Seedat, M., and Nel, J. (2015). Alcohol consumption in adolescent homicide victims in the city of Johannesburg, South Africa. Addiction. 110, 595–501. doi: 10.1111/add.12825
The Guardian (2020). Lockdowns Around the World Bring Rise in Domestic Violence. Available online at: https://www.theguardian.com/society/2020/mar/28/lockdowns-world-rise-domestic-violence?CMP=Share_iOSApp_Other
Tielbeek, J. J., Al-Itejawi, Z., Zijlmans, J., Polderman, T. J., Buckholtz, J. W., and Popma, A. (2018). The impact of chronic stress during adolescence on the development of aggressive behavior: a systematic review on the role of the dopaminergic system in rodents. Neurosci. Biobehav. Rev. 91, 187–197. doi: 10.1016/j.neubiorev.2016.10.009
Toshchakova, V. A., Bakhtiari, Y., Kulikov, A. V., Gusev, S. I., Trofimova, M. V., Fedorenko, O. Y., et al. (2017). Association of polymorphisms of serotonin transporter (5HTTLPR) and 5-HT2C receptor genes with criminal behavior in Russian criminal offenders. Neuropsychobiology 75, 200–210. doi: 10.1159/000487484
Trangenstein, P. J., Greene, N., Eck, R. H., Milam, A. J., Furr-Holden, C. D., and Jernigan, D. H. (2020). Alcohol advertising and violence. Am. J. Prevent. Med. 58, 343–351. doi: 10.1016/j.amepre.2019.10.024
Underwood, M. D., Kassir, S. A., Bakalian, M. J., Galfalvy, H., Dwork, A. J., Mann, J. J., et al. (2018). Serotonin receptors and suicide, major depression, alcohol use disorder and reported early life adversity. Transl. Psychiatry 8, 1–15. doi: 10.1038/s41398-018-0309-1
Underwood, M. D., Mann, J. J., Huang, Y. Y., and Arango, V. (2008). Family history of alcoholism is associated with lower, 5-H T2A receptor binding in the prefrontal cortex. Alcohol. Clin. Exp. Res. 32, 593–599. doi: 10.1111/j.1530-0277.2007.00610.x
Wahlsten, P., Koiranen, V., and Saukko, P. (2007). Survey of medico-legal investigation of homicides in the city of Turku, Finland. J. Clin. Foren. Med. 14, 243–252. doi: 10.1016/j.jcfm.2006.07.007
Wallace, C., Mullen, P. E., and Burgess, P. (2004). Criminal offending in schizophrenia over a 25-year period marked by deinstitutionalization and increasing prevalence of comorbid substance use disorders. Am. J. Psychiatry 161, 716–727. doi: 10.1176/appi.ajp.161.4.716
Weiss, D. B., Testa, A., and Rennó Santos, M. (2018). Hazardous alcohol drinking and cross-national homicide rates: the role of demographic, political, and cultural context. J. Drug Issues 48, 246–268. doi: 10.1177/0022042617750579
Wieczorek, W. F., Welte, J. W., and Abel, E. L. (1990). Alcohol, drugs, and murder: a study of convicted homicide offenders. J. Crim. Justice 18, 217–227. doi: 10.1016/0047-2352(90)90002-S
Wiener, C. D., Moreira, F. P., Zago, A., Souza, L. M., Branco, J. C., Oliveira, J. F. D., et al. (2018). Mood disorder, anxiety, and suicide risk among subjects with alcohol abuse and/or dependence: a population-based study. Braz. J. Psychiatry 40, 1–5. doi: 10.1590/1516-4446-2016-2170
Wilsnack, R. W., Wilsnack, S. C., Gmel, G., and Kantor, L. W. (2018). Gender differences in binge drinking. Alcohol Res. Curr. Rev. 39, 57–76.
Women UN. (2020). The Shadow Pandemic: Violence Against Women During COVID-19. Available online at: unwomen. org: https://www.unwomen.org/en/news/in-focus/in-focus-gender-equality-in-covid-19-response/violence-against-women-during-covid-19
Yeo, D. C. K., Singham, T., and Poremski, D. (2019). The presence of alcohol consumption prior to homicide in Singapore. Asian J. Psychiatry 44, 80–85. doi: 10.1016/j.ajp.2019.07.019
Zai, C. C., Ehtesham, S., Choi, E., Nowrouzi, B., De Luca, V., Stankovich, L., et al. (2012). Dopaminergic system genes in childhood aggression: possible role for DRD2. World J. Biol. Psychiatry 13, 65–74. doi: 10.3109/15622975.2010.543431
Zhang, Y., Ming, Q. S., Yi, J. Y., Wang, X., Chai, Q. L., and Yao, S. Q. (2017). Gene-gene-environment interactions of serotonin transporter, monoamine oxidase A and childhood maltreatment predict aggressive behavior in Chinese adolescents. Front. Behav. Neurosci. 11:17. doi: 10.3389/fnbeh.2017.00017
Keywords: alcohol, aggression, public health, brain, domestic, violence, violent, serotonin
Citation: Sontate KV, Rahim Kamaluddin M, Naina Mohamed I, Mohamed RMP, Shaikh MF, Kamal H and Kumar J (2021) Alcohol, Aggression, and Violence: From Public Health to Neuroscience. Front. Psychol. 12:699726. doi: 10.3389/fpsyg.2021.699726
Received: 24 April 2021; Accepted: 17 November 2021;
Published: 20 December 2021.
Edited by:
Berta Vall, Universitat Ramon Llull, SpainReviewed by:
Rafi Alnjadat, Al-Balqa Applied University, JordanSiamak Khodarahimi, Islamic Azad University, Iran
Copyright © 2021 Sontate, Rahim Kamaluddin, Naina Mohamed, Mohamed, Shaikh, Kamal and Kumar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jaya Kumar, amF5YWt1bWFyQHVrbS5lZHUubXk=
 Kajol V. Sontate1
Kajol V. Sontate1 Isa Naina Mohamed
Isa Naina Mohamed Rashidi Mohamed Pakri Mohamed
Rashidi Mohamed Pakri Mohamed Mohd. Farooq Shaikh
Mohd. Farooq Shaikh Jaya Kumar
Jaya Kumar