
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 27 July 2021
Sec. Gender, Sex and Sexualities
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.689396
This article is part of the Research TopicGender Differentials in Times of COVID-19View all 11 articles
 Liliana Abreu1*†
Liliana Abreu1*† Anke Koebach1,2†
Anke Koebach1,2† Oscar Díaz3
Oscar Díaz3 Samuel Carleial2
Samuel Carleial2 Anke Hoeffler1
Anke Hoeffler1 Wolfgang Stojetz3
Wolfgang Stojetz3 Hanna Freudenreich4
Hanna Freudenreich4 Patricia Justino5
Patricia Justino5 Tilman Brück3,4,6
Tilman Brück3,4,6Gender differences (GD) in mental health have come under renewed scrutiny during the COVID-19 pandemic. While rapidly emerging evidence indicates a deterioration of mental health in general, it remains unknown whether the pandemic will have an impact on GD in mental health. To this end, we investigate the association of the pandemic and its countermeasures affecting everyday life, labor, and households with changes in GD in aggression, anxiety, depression, and the somatic symptom burden. We analyze cross-sectional data from 10,979 individuals who live in Germany and who responded to the online survey “Life with Corona” between October 1, 2020 and February 28, 2021. We estimate interaction effects from generalized linear models. The analyses reveal no pre-existing GD in aggression but exposure to COVID-19 and COVID-19 countermeasures is associated with sharper increases in aggression in men than in women. GD in anxiety decreased among participants with children in the household (with men becoming more anxious). We also observe pre-existing and increasing GD with regards to the severity of depression, with women presenting a larger increase in symptoms during the hard lockdown or with increasing stringency. In contrast to anxiety, GD in depression increased among participants who lived without children (women > men), but decreased for individuals who lived with children; here, men converged to the levels of depression presented by women. Finally, GD in somatic symptoms decreased during the hard lockdown (but not with higher stringency), with men showing a sharper increase in symptoms, especially when they lived with children or alone. Taken together, the findings indicate an increase in GD in mental health as the pandemic unfolded in Germany, with rising female vulnerability to depression and increasing male aggression. The combination of these two trends further suggests a worrying mental health situation for singles and families. Our results have important policy implications for the German health system and public health policy. This public health challenge requires addressing the rising burden of pandemic-related mental health challenges and the distribution of this burden between women and men, within families and for individuals who live alone.
More than 1 year has passed since the beginning of the COVID-19 pandemic and evidence on its profound psychological impacts is emerging rapidly from around the world (Wang C. et al., 2020; Williams et al., 2020). So far, the life-threatening and traumatic nature of the pandemic, as well as the increased stress load imposed by measures to contain the SARS-CoV-2 virus, the coronavirus causing COVID-19 (hereafter referred to as “the coronavirus”), are causing a deterioration in mental health (Xiang et al., 2020). Recent studies document higher levels of stress and anxiety, loneliness and insomnia, somatization, and depressive symptoms, as well as symptoms of post-traumatic stress (Ko et al., 2020; Ran et al., 2020; Shelef and Zalsman, 2020). A meta-study (Wu et al., 2021) conducted in May 2020 evaluated over 10 studies on anxiety and depression since the onset of the COVID-19 pandemic and found prevalence rates of over 30%. Accordingly, recent meta-analyses estimated the prevalence of depression in the general population during the pandemic at 25% (95% confidence interval: 18–33%) (Bueno-Notivol et al., 2021) and 33.7% (95% confidence interval: 27.5–40.6) (Salari et al., 2020); pre-pandemic prevalence rates between 1994 and 2014 across 30 communities averaged at 12.9% (95% confidence interval: 11.1–15.1%) and data from Global Burden of Disease showed a proportion of 3.4% in 2017 (Ritchie and Roser, 2018).
Given the gender-specific challenges associated with the pandemic, the latter may also impact mental health differently by gender. Gender, beyond the biological definition of sex, refers to socially allocated roles, behaviors, identities, and expectations. In the literature, gendered behavior is understood as a cultural phenomenon rather than merely biological, given its highly relational nature (Flanagan, 2012). Gender differences (GD) in mental health outcomes have been established previously. Anxiety and mood disorders have been shown to be more prevalent among women than men (Rosenfield and Mouzon, 2013), while externalizing behavior or aggression and substance use disorders are more prevalent among men than women (Seedat et al., 2009; Boyd et al., 2015). To varying extents, these differences are assumed to be the result of sex-specific genetic (Kang et al., 2020), epigenetic (Hodes et al., 2017), neural (Stewart et al., 2010), reproductive (Li and Graham, 2017), and social factors, e.g., social roles and gender norms (Alon et al., 2020). It is widely acknowledged that gender is experienced not just individually but also socially. These social roles were found to partially explain GD in the perception of psychological distress (Simon, 1995), and GD in mental health is one of the facets where they manifest themselves. As the pandemic imposes different stressors on individuals with different (gendered) roles due to, for example, unemployment, home schooling, and working from home, differences in the impact of psychological distress on mental health may emerge. However, to date, we have limited evidence about the pandemic-related stressors that affect gender roles differentially, and how they impact GD in mental health.
In summary, the aim of this paper is to address knowledge gaps about GDs of mental health outcomes that emerged with the COVID-19 pandemic. Specifically, we analyze GD in aggression, anxiety, and depression symptoms, as well as the somatic symptom burden for adult men and women in Germany during the winter period of 2020/2021. For the purpose of the current study, we categorize gender as male, female or other and analyze data on the binary spectrum. This is undoubtedly a coarse categorization, since growing empirical evidence affirms that gender is a non-binary construct. Recent awareness of gender diversity draws attention to the experience and rights of transgenders and individuals who perceive their gender identity as neither entirely male nor female (Ainsworth, 2015; Cameron and Stinson, 2019). In the methods and limitations sections, we describe why we chose the binary construct to answer our research questions, although we agree that research should move toward more gender inclusivity. To examine the impact of the COVID-19 pandemic, we specify three sets of analyses: first, the nature and intensity of containment measures imposed in Germany, comparing outcomes during light vs. hard lockdowns and across stringency levels of measures to contain the virus using the Oxford Stringency Index; second, exposure to the coronavirus by testing positive for the virus, knowing someone who died due to the pandemic and suffering income losses during the pandemic; third, household characteristics–being the main provider, living vs. not living with children, and living alone vs. with others in interaction with the stringency index.
Aggression can be defined as any behavior intended to cause harm in others motivated either reactively, thus occurring as a response to a perceived threat, or instrumentally/proactively (Anderson and Bushman, 2002). Increasing evidence points to the rewarding and thus self-perpetuating nature of aggression (Nell, 2006; Elbert et al., 2010, 2018; Koebach and Elbert, 2015; Golden and Shaham, 2018; Golden et al., 2019; Koebach et al., 2021). In recent aggression models, aggressive behavior is described as a consequence of situational (e.g., stress, frustration, discomfort, threatening stimuli) and personal factors (e.g., traits, attitudes, gender, trauma history), as well as internal states (e.g., cognition, affect, and arousal; e.g., Anderson and Bushman, 2002; Bushman, 2016; Elbert et al., 2018). In contrast, anger is considered a social emotion manifesting as a state or trait (Spielberger et al., 1983, 1995), and predisposing for an aggressive action in response to a (perceived) threat (Bettencourt et al., 2006). Inherent to the survival mode (Chemtob et al., 1997; Novaco and Chemtob, 1998) and with its property to suppress fear (Foa et al., 1995; Feeny et al., 2000), it is highly prevalent in trauma-exposed individuals (for review see Orth and Wieland, 2006). Within this framework, aversive situations such as the COVID-19 pandemic and its circumstances, e.g., confinement or economic hardship, may impose an increased level of threat, frustration and discomfort. We theorize that COVID-19-related stressors stimulate cognitive, emotional, and physiological reactions that are associated with threat, and thus trigger fight-or-flight tendencies that lead to a higher level of anger and reactive physical aggression (Gelles, 1993; Allen et al., 2018; Elbert et al., 2018).
In line with this hypothesis, Ye et al. (2021) found an increase of online aggressive behavior associated with fear about contagion with COVID-19. In 2016, during an epidemic of the Middle East Respiratory Syndrome (MERS), Jeong et al. (2016) examined the effects of a 2-week isolation period on anger and anxiety, and found about 16% of participants experienced anger when isolated due to MERS virus exposure. Several health experts and scientists have also observed increasing rates of family violence during the COVID-19 pandemic, particularly in situations of more stringent quarantines (Fraser, 2020; Perez-Vincent et al., 2020; Telles et al., 2020; Ebert and Steinert, 2021). In a recent meta-analysis, Piquero et al. (2021) found strong evidence for a moderate increase in domestic violence as a result of the pandemic based on 18 studies from the United States (n = 12), Mexico (n = 1), Argentina (n = 1), India (n = 1), Australia (n = 1), and Europe (n = 2). A study in Germany estimated the prevalence of violence against women and children during the pandemic, reporting 3.1% of women suffered verbal and physical conflict during the previous month; 7.8% reported emotional abuse; 3.1% felt threatened by their partner; and 6.7% reported child corporal punishment (Ebert and Steinert, 2021). The authors concluded that the risk of violence was more than double in households in quarantine, compared with households not in quarantine. Accordingly, Leslie and Wilson (2020) reported an increase of 7.5% of police calls in the United States due to an incident of intimate partner violence (IPV) during the first months of the pandemic. With regard to crime rates, evidence shows an overall decline in almost all types of crime during lockdowns, with exception to homicides and cyber crime (Halford et al., 2020; Hodgkinson and Andresen, 2020; Buil-Gil et al., 2021; Scott and Gross, 2021; Sutherland et al., 2021). A study from Australia recently showed that this effect might reverse once the measures are lifted (Andresen and Hodgkinson, 2020), but longer-term developments in crime indices remain to be explored. Thus, the literature suggests a shift of violence from the streets into the homes.
Traditionally, boys and men have been considered more aggressive than girls and women (Leslie and Wilson, 2020). However, more recent approaches claim gender-specific types of aggression with men being directly aggressive and women indirectly (e.g., spreading rumors) have come to the fore (Lagerspetz et al., 1988). This is also reflected in how women respond to anger: while it is recognized that men and women generally display comparable levels of anger (Deffenbacher et al., 1996), men tend to externalize their aggressive feelings more (Archer, 2004; Björkqvist, 2018), while women may respond to provocation with more anxiety and fear (Björkqvist, 2018). In a large sample from Denmark (>10,000 participants), found that hospitalization due to interpersonal violence predicted criminal behavior in men and self-harm in women. Moreover, about 80% of all global homicides are perpetrated by men (Global Study on Homicide, 2019). Yet, there are conditions when GD in aggression disappear. In a meta-analysis, Knight et al. (2002) found that GD in aggression was most pronounced when the context allowed for variance in emotional arousal (rather than secure or highly arousing situations). This is also in line with findings from war-affected men and women who both presented similar levels of appetitive aggression after involvement to similar levels of trauma and violent fighting (Augsburger et al., 2015; Meyer-Parlapanis et al., 2016). GD in aggression have been argued to be associated with biological (e.g., Turanovic et al., 2017; Denson et al., 2018; Ling et al., 2019), psychological (e.g., as sequelae of trauma) and social factors (e.g., social learning, etc.). Further, researchers plausibly theorize that GD in aggression are the result of sexual selection throughout evolution (Archer and Webb, 2006; Elbert et al., 2018). Indirect/female forms of aggression are psychologically not less harmful (see Eisenberger and Lieberman, 2004; Eisenberger, 2012; Norman et al., 2012; Arseneault, 2017; Começanha et al., 2017; on social pain), but physical aggression and crime on average present higher societal costs and escalate more often into extreme forms requiring hospital admission, psychological treatment, restorative justice, isolation of perpetrators/imprisonment, etc. (Forum on Global Violence Prevention, 2011). Building on these findings, we focus in this paper on GD in anger and physical aggression, and postulate that, in Germany, men may respond with more anger and physical aggression to the stress caused by the pandemic.
Symptoms of Generalized Anxiety Disorder (GAD) include restlessness, fatigue, excessive anxiety and worry, impaired concentration, and difficulty sleeping. About 5–6% of the population is estimated to present the full clinical diagnosis of GAD (Kessler et al., 1994). The COVID-19 pandemic has increased fear of acute threat of infection and death, which has been magnified by secondary stressors, e.g., social distancing, lockdowns, economic insecurity and unemployment. As a result, the incidence rates of anxiety have increased since the start of the pandemic (Alonzi et al., 2020; Bäuerle et al., 2020a; Canet-Juric et al., 2020; Kazmi, 2020; Mazza et al., 2020; Olaseni, 2020; Ozamiz-Etxebarria, 2020; Ausín et al., 2021; Moore et al., 2021; Msherghi et al., 2021).
Furthermore, anxiety, GAD in particular, is about 2–3 times more prevalent in women than in men (Beesdo et al., 2010; McLean et al., 2011); for review see Jalnapurkar et al. (2018). Differential biological, psychological, and social functioning have been found to underlie GD in anxiety. A large body of evidence emphasizes specific effects of reproductive hormones (Altemus, 2006; Altemus et al., 2014), e.g., estrogen that modulates brain regions relevant to the extinction of fear (Garcia et al., 2018), or testosterone which has anxiolytic effects (McHenry et al., 2014). Differential vulnerability to trauma and exposure to everyday stressors may further increase GD in anxiety (Donner and Lowry, 2013; Durbano, 2015). Gender theories emphasizes the identification of sex roles as factors determining GD in anxiety (Altemus, 2006; Altemus et al., 2014), namely when discussing how etiological factors of anxiety and individual differences are moderated by socialization processes (social, cultural, and developmental) and gender-specific expectations (McLean and Anderson, 2009). Traditionally, gender role theory advocates that, in socialization processes, men and women are socially prescribed with certain behaviors, traits, and skills, with considerable evidence reporting that gender roles significantly influence symptoms of anxiety (Bem, 1981). For instance, expression of anxiety is inconsistent with male gender roles, and anxiety may therefore be less tolerated in men (Chambless and Mason, 1986; Ollendick et al., 2002). Indeed, the magnitude of GD depends on the type of anxiety (Bander and Betz, 1981; Moscovitch et al., 2005).
Since the beginning of the COVID-19 pandemic, several studies have discussed the increased vulnerability of women during the crisis, as women tend to work in jobs that require face-to-face interaction, depend on part-time employment, and manage both family and work (Olaseni, 2020; Sánchez-Teruel, 2021). Szabo et al. (2020) investigated stress levels in 1,552 Hungarians during the first month of the COVID-19 crisis and found that women were more worried than men (Szabo et al., 2020) about the consequences of the pandemic. Frederiksen and Gomez (2020) found that women tend to be worried more about someone in their family getting infected by COVID-19 and about income decrease (50% vs. 42%). Losada-Baltar et al. (2020) showed that feelings of loneliness and psychological distress were higher in women in Spain. Higher stress levels in women during the early stage of the pandemic were also found in China (Yan et al., 2021). However, these studies are not able to identify the effect of the pandemic on GD in anxiety. So far, only the study of Ausín et al. (2021) investigated gender-specific consequences in mental health due to the pandemic, in the period immediately after the declaration of the state of emergency in Spain. We extend this analysis to another setting (Germany), focus on longer-term effects, and consider various pandemic-related stressors.
Depression refers to symptoms like depressed mood, loss of interest and pleasure, negative feelings and thoughts, and problems with sleeping and concentration, amongst others. Clinically relevant levels require these symptoms to persist for at least half a day and more than half of the days in a given time frame. Major depression is amongst the most prevalent mental disorders and a complex biopsychosocial interaction underlies the development of symptoms. In the advent of experimental psychology, Seligman (1972) introduced the concept of learned helplessness as he found that dogs exposed to electric shocks in an inescapable situation would later fail to escape electric shocks even when escape was possible (Overmier and Seligman, 1967). In humans, it was found that the attributional style (internal, global, and stable) is critical to whether subjects are able to cope with stressful situations (Abramson et al., 1978; Alloy, 1982; Raps et al., 1982). This model presents a prominent environmental theory for depression and its treatment in behavioral therapy at present (Rubenstein et al., 2016), besides other approaches that focus on traumatic or chronic environmental stressors (McCullough, 2003; O’Leary and Cryan, 2013; Wiborg, 2013). As with the electric shocks, the pandemic has been imposed on individuals as a sequence of inescapable and unavoidable adverse events emerging in the form of the threat of infection, lockdowns, economic crisis, and restrictions to individual freedoms. The ability of individuals to cope with these stressors is subject to personal characteristics. Studies comparing the prevalence of depressive symptoms before and after the start of the pandemic suggest an increase in depression since the pandemic. This has been in the order of around 10.1% (Bretschneider et al., 2017) before the pandemic and 14.3% during the pandemic (Bäuerle et al., 2020b) in Germany. An accumulation of depression symptoms was also reported in the United States, with a threefold increase during COVID-19 pandemic (Ettman et al., 2020).
Concerning the GD of depression during the pandemic, two studies from China found that women showed higher prevalence of depression during the crisis (Wang C. et al., 2020; Zhang and Ma, 2020). In a large online survey from Italy (N > 18,000), Rossi et al. (2020) found women were more likely to display higher levels of depression. GD in depression represent a major health disparity, as women suffer about twice as frequently from major depression than men (Weissman and Klerman, 1977; Salk et al., 2017). Hammarström et al. (2009) conducted a literature review on explanatory models for GD in depression. The authors found that the majority of studies focused on a biomedical explanation (Hammarström et al., 2009), followed by sociocultural and psychological models that were superior on intersectionality and multifactoriality. Converging evidence of recent studies emphasize the interaction of environmental stress (e.g., childhood adversity, physical, sexual or emotional abuse, or neglect) and biological vulnerability (e.g., due to sex hormones, inflammation, etc.; for review see ref). Interestingly, studies consistently report narrowing GD in depression when accompanied by changes in traditional gender roles (Wickramaratne et al., 1989; Joyce et al., 1990; Seedat et al., 2009).
Given the higher depression rates in women before and during the pandemic, studies that emphasize GD in depression fail to reflect whether this is exaggerated due to the pandemic. Only Ausín et al. (2021) investigated the change in GD in depression due to the pandemic in Spain but did not find any evidence. To extend their findings, we investigate the differential impact of the pandemic, its countermeasures and related stressors, as well as household characteristics as moderators in Germany.
Somatic symptoms are common in medical, psychiatric, and social conditions, and are associated with higher levels of stress, decreased quality of life, and an increased use of health structures (Kroenke et al., 1990, 1997, 2010; Simon et al., 1999; Barsky et al., 2005; Rief et al., 2005; Fink et al., 2007; Kohlmann et al., 2013). This outcome has been subject to limited research in gender studies and during the pandemic. However, the few studies carried out suggest that COVID-19 may have considerable and gendered effects on somatization. Women and men reportedly experience somatic symptoms differently. Women tend to report somatic symptoms more frequently than men and experience them more intensively (Barsky et al., 2001). The reasons presented for these differences vary widely across studies, since the same sensation may be differently described and labeled by women and men. Pennebaker and Roberts (1992) suggested that women use both situational information (external) and somatic (internal) signs to describe symptoms, while men rely more on internal signs. Again, gender roles may enforce GD in somatization. According to Ehlers (1993), women receive more positive reinforcement for expressing somatic symptoms than men, which may reinforce self-focus and partially explain GD in somatization, while men might suppress those symptoms more often, since they feel more discouraged from expressing them (Watt et al., 1998). Unlike mental health problems, somatic symptoms may not trigger stigmatization to the same extent, and we include them in this study as a global health indicator. Taking this into account, we seek to clarify GD in somatization associated with the COVID-19 pandemic and determine if these differences increased before and after the introduction of stricter measures to control the spread of the virus.
Similar to other countries, the German federal and state governments, as well as local authorities, responded to the COVID-19 crisis by imposing countermeasures that included closures of schools and non-essential services, travel restrictions, mandatory self-isolation for travelers, and prohibition of gatherings. The second round of the Life with Corona (LwC) survey (see below) was launched during what was referred to as a light lockdown in October 2020: restaurants and cafés could only sell takeaway food and a maximum of ten people from two households were allowed to meet (religious congregations and street protests were subject to exemptions). As infection rates increased, measures were increased to a hard lockdown: private meetings were limited to five persons from two households and there were major closures of services such as schools and kindergartens, retail stores, personal care units (hairdressers, beauty salons, and similars), restaurants (with takeaway allowed), pubs, and cultural facilities. The hard lockdown lasted from December 16, 2020 until March 1, 2021, when some minor relaxations were introduced, reinstating a form of light lockdown.
Life with Corona is a global online survey operated by an international academic consortium. LwC was implemented to gain a better understanding of how individuals experience and cope with the COVID-19 pandemic and its countermeasures. It was launched on March 23, 2020 (first round) and revised on October 1, 2020 (second round). The survey targets adult populations (>17 years inclusion criterion) across the globe and collects data on several topics, including individual exposure to COVID-19, compliance with recommended and mandated behaviors, food security, attitudes, life satisfaction, somatic and mental health, and the sociodemographic characteristics of the respondents (age, gender, marital status, household composition, location, and living conditions). The questions about recollection of events extend to a maximum of 14 days for the mental health variables. The LwC survey can be answered in 27 languages and is promoted by local and international partners and social media. Informed consent is obtained at the beginning of the survey. The study received ethical approval by UNU-WIDER (reference number: 202009/01). More details on LwC can be retrieved online at www.lifewithcorona.org. In this paper, we use data from the second round of the survey (October 1, 2020 until February 28, 2021) from individuals who reported they live in Germany.
Between October 1, 2020, and February 28, 2021, a total of 10,979 individuals (7,426 female; 67.6%) living in Germany completed the LwC online survey. 76.9% of answers related to the period of the hard lockdown (which started on December 16, 2020). On average, participants were 50.62 years old (SD = 16.16; range = 18–91), had 14.09 (SD = 3.99) years of formal education, and lived in a household composed of 3.03 (SD = 28.31) members. The majority of participants were either single (64.6%) or lived in a stable relationship (partner/married, 29.1%), and 52.9% lived in an urban area.
In this subsection, we describe the data we collected and how we use them to measure the four types of GD described above.
Demographic information was collected at the beginning of the online survey, including age, years of formal education, marital status, location of residence, household composition, and gender.
To assess gender, we asked the participants to choose between categories of male, female, and other. For the analysis, we excluded participants who responded other due to a low response rate (only 14 participants, or 0.13%).
The selected measures follow an established approach in the literature, validated in many countries, which allows comparison of results across different settings (Löwe et al., 2010; Gierk et al., 2014; Webster et al., 2014; Hinz et al., 2017).
We measure aggression by applying subscales of the short version of the Buss and Perry Brief Aggression Questionnaire (BAQ) (Bryant and Smith, 2001; Webster et al., 2014, 2015) for physical aggression (e.g., I have threatened people I know; I have trouble controlling my temper; Given enough provocation, I may hit another person) and anger (e.g., I flare up quickly but get over it quickly; Sometimes I fly off the handle for no good reason; I have trouble controlling my temper). The instrument consists of three items for each subscale rated from very unlike me (1) to very like me (5). We calculate a sum score with values ranging 0–24, with higher values indicating a more pronounced inclination to aggression. The instrument has been applied in a wide variety of cultures (Diamond and Magaletta, 2006; Vitoratou et al., 2009; Abd-El-Fattah, 2013; Zimonyi et al., 2021), including Germany (von Collani and Werner, 2005). Webster et al. (2015) found high test–retest reliability among the four subscales indicating it measures a stable trait. Note that the instrument does not measure violent behavior but has been shown to be associated with delinquent behavior (Jurczyk and Lalak, 2020), reactive aggressive behavior in a laboratory experiment (Fahlgren et al., 2021), and aggressive acts (Archer and Webb, 2006).
We measure anxiety with subscales from the seven-item Generalized Anxiety Disorder scale (GAD-7) (Spitzer et al., 2006). GAD-7 has proven to be effective in assessing severity of anxiety, and it is brief and self-administered (Spitzer et al., 2006). Response options were Not at all; Several Days; More than half days; and Nearly every day, which were coded as 0, 1, 2, and 3, respectively, for each item: Feeling nervous, anxious, or on edge; Not being able to stop or control worrying; Worrying too much about different things; Trouble relaxing; Being so restless that it’s hard to sit still; Becoming easily annoyed or irritable; and Feeling afraid as if something awful might happen. We calculate a sum score to indicate anxiety severity, with values ranging 0–27, with higher values indicating higher anxiety. This instrument has been validated for the German population, where anxiety was correlated with low quality of life, fatigue, low habitual optimism, physical complaints, sleep problems, low life satisfaction, low social support, low education, unemployment, and low income (Hinz et al., 2017). The instrument has also been successfully applied in online surveys before (Pieh et al., 2020; Rossi et al., 2020).
We measure the severity of depression using the depression module of the Patient Health Questionnaire (PHQ-9) (Kroenke and Spitzer, 2002). All nine items of the questionnaire include rating symptoms from 0 (not at all) to 3 (nearly every day), according to the presence of a certain symptom in the 2 weeks prior to completing the survey. Based on these questions, we calculate an individual sum score that indicates depression severity. The depression score takes values ranging 0–27, with higher values indicating higher depression. The instrument has been validated for the German population (Löwe et al., 2010) and has successfully been applied as an online measure in recent studies (Pieh et al., 2020; Rossi et al., 2020).
We measure subjective severity of somatic symptoms based on the 8-item self-reported Somatic Symptom Scale-8 (SSS8) (Gierk et al., 2014), which asks about fever, cough, diarrhea, headache, and other somatic symptoms during the 14 days before taking the survey. We calculate a sum score to indicate the symptomatic burden, taking values ranging 0–27, with higher values indicating a higher symptomatic burden. The high reliability and validity of the instrument has been demonstrated in a large sample not only in Germany (Gierk et al., 2014), but also elsewhere, including in self-administered online surveys (Matsudaira et al., 2017).
To account for public policies enacted to contain the spread of the virus and the levels of life disruption that people could have experienced during the time of the study, we use the following two measures:
To contain the COVID-19 pandemic, public life in Germany was largely shut down on December 16, 2020. One week before Christmas, the hard lockdown period was implemented as the number of deaths and infections from the coronavirus reached record levels. The stringency index during the hard lockdown period reached its highest levels 83–85 (see below) For our first set of analyses, we compare the group of people that responded to the questionnaire before December 16, 2020, the start of the hard lockdown, with those that responded after that date.
The Oxford Coronavirus Government Response Tracker (OxCGRT) project (Hale et al., 2021) provides a “Stringency Index,” which indicates the strictness of public policies implemented to contain the spread of the virus. The index is calculated based on nine metrics: school closures, workplace closures, cancelation of public events, restrictions on public gatherings, closures of public transport, stay-at-home requirements, public information campaigns, restrictions on internal movements, and international travel restrictions. The resulting index is a continuous variable at the day-country level. It ranges from 1 to 100, with higher values indicating harder restrictions. We use the values of the stringency index for the time period covered in our data set, which range from 50 to 85.
We measure COVID-19 exposure via three proxy variables, building on the measurement of shock exposure in surveys (Brück et al., 2016):
In the LwC survey, we asked participants if they had had an antibody coronavirus test, and whether it was positive or not.
We asked survey participants whether they personally knew someone who had died from the coronavirus, or from other causes due to medical complications arising from the COVID-19 crisis.
We also asked participants if and how their monthly net income had changed since the start of the COVID-19 crisis. We group our respondents based on whether they had suffered an income loss or not.
We use the following three measures of household characteristics and composition:
We identify those participants by asking who is the main provider of income in their household. We code the variable “yes” for participants who responded that they are the main providers and “no” if they responded that it is someone else or that they share this role with their partner.
Based on information provided on other household members’ age, we group respondents into two groups: those who indicated they live in a household with children (household members below the age of 18) and those who do not.
Based on information provided on the number of household members, we group respondents into two groups: those who indicated they live alone and those who do not.
We use generalized linear models (GLMs) to study GD in mental health outcomes (aggression, anxiety, depression, and symptomization) and three sets of explanatory factors: COVID-19 countermeasures, COVID-19 exposure, and household characteristics. For each factor, we included various model terms that provide interactions between a given factor with gender (two-way interactions) or with gender and another factor (three-way interactions). All models include a vector of control variables [age, years of education, location (urban or rural), and household size]. Lastly, all responses are statistically weighted based on the gender, age, education, and income distribution of the German population.
To analyze the relationship of gender and COVID-19 countermeasures with mental health outcomes, we estimate the following equation:
where Hit refers to mental health outcome of individual i who answered the survey at date t; Genderi is a dummy that equals one if the respondent was male; Anti−Coronameasuret refers to (a) the hard lockdown indicator or (b) the stringency index; Xi is the vector of individual-level time-invariant control variables, and εit is the idiosyncratic error term. The main coefficient of interest is β3, which estimates how strongly the association of a COVID-19 countermeasure with a mental health outcome varies with gender.
To analyze the relationship of gender and COVID-19 exposure with mental health outcomes, we estimate the following equation:
where Corona exposure is one of three separate dummy variables that indicate whether the individual (a) had had a positive result on a COVID-19 test, (b) knew someone who had died of COVID-19, or (c) had suffered an income decrease since the start of the pandemic. The main coefficient of interest is β3, which estimates how strongly the association of a COVID-19 exposure measure with a mental health outcome varies with gender.
To analyze how household characteristics shape the relationship of gender and anti-COVID-19 policy stringency with mental health outcomes, we estimate the following equation:
Hit = α + β1 Genderi + β2 Household characteristici + β3 Stringency indext + β4 Genderi * Household characteristici + β5 Genderi * Stringency indext + β6 Household characteristicsi * Stringency indext + β7 Genderi * Household characteristici * Stringency indext + Xi + εit
where Household characteristic is one of three separate dummy variables that indicate whether the individual reported (1) being the main provider of income in her household, (2) living with children, or (3) living alone. The main coefficient of interest is β7, which estimates how strongly the interactive effect of a household characteristic with the stringency measures varies with gender. We conduct all tests on a significance level of at least 90%.
Table 1 presents summary statistics of all variables used in the study, differentiated by gender.
The overall sum score is 5.61 (SD = 5.56) for aggression, 4.33 (SD = 4.83) for anxiety, 2.41 (SD = 3.18) for depression, and 4.92 (SD = 4.31) for somatic symptoms. T-tests of the difference in mean scores by gender indicate that women reported significantly higher levels for depression, anxiety, and the somatic symptom burden scores (p < 0.001), whereas men reported statistically higher levels of aggression (p < 0.001). Distributions by gender are presented in Figure 1.
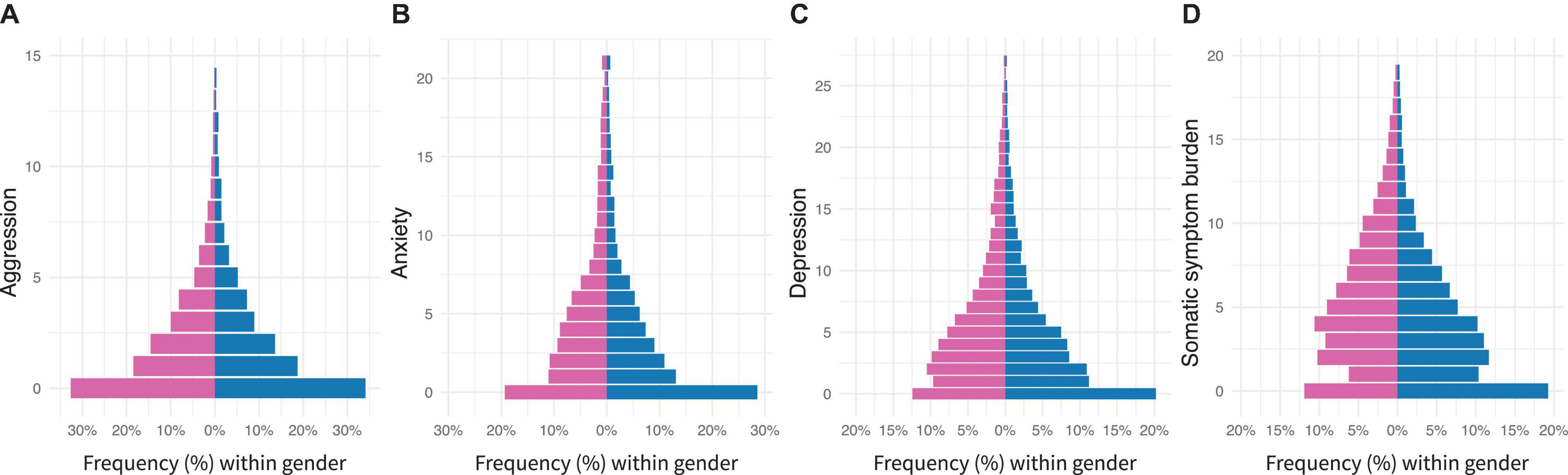
Figure 1. Differences between men (n = 3553) and women (n = 7426) at mental health measures: (A) aggression, (B) anxiety, (C) depression, and (D) somatic symptom burden. Gender is color-coded (blue for men). Bars represent relative percentages within gender.
We do not find gender-based differences in the probability of responding before or after the lockdown and the average stringency score participants experienced was 77.04 (SD = 11.3).
Regarding COVID-19 exposure, only 1% of the sample reported having tested positive for the coronavirus, but 13.9% knew someone who had died from COVID-19 or other causes arising from the pandemic. 23.4% of individuals had suffered an income decrease since the start of the pandemic. While there is no significant difference in the probability of reporting a positive test between genders, we find women were significantly more likely to know someone who had died of coronavirus (14.6% vs. 13.1%, p < 0.001), and more likely to suffer an income decrease (22.5% vs. 24.4%, p < 0.001).
With reference to household characteristics, 53.4% of the participants reported being the main income providers in their household, 22.9% of the participants live with children, and 24.8% live alone. We find women were significantly less likely to be main income providers compared to men (45.3% vs. 62.6%, p < 0.001); were more likely to live with children (23.5% vs. 22.2%); and were more likely to live alone (26.0% vs. 23.4%) (see Table 1).
Notably, we find variables associated with COVID-19 and household characteristics to be significantly associated with depression, anxiety, the somatic symptom burden, and aggression independently of gender (see Supplementary Material 1).
Generalized linear models are significant for the predictions of all aggression models (light vs. hard lockdown: R2 = 0.036, F(1, 10977) = 59.28, p < 0.01, stringency: R2 = 0.038, F(1, 10977) = 61.35, p < 0.01, positive COVID-19 test: R2 = 0.028, F(1, 10977) = 44.82, p = 0.01), knowing someone who died due to COVID-19: R2 = 0.03, F(1, 10977) = 48.98, p < 0.01), income decrease: R2 = 0.045, F(1, 10977) = 74.42, p < 0.01, being the main provider in the household R2 = 0.039, F(1, 10977) = 40.32, p < 0.01, living with children: R2 = 0.041, F(1, 10977) = 42.66, p < 0.01, and living alone: R2 = 0.039, F(1, 10977) = 40.61, p < 0.01). The positive and significant two-term interactions for light vs. hard lockdown (β = 0.47, p < 0.01), stringency (β = 0.02, p < 0.01), knowing someone who died (β = 0.46, p < 0.01), and income decrease (β = 0.52, p < 0.01) indicate increasing GD in aggression, with men consistently presenting a stronger increase in aggression than women. Two- and three-term interactions for the other variables are not significant (Figure 2). Notably, we do not find GD in aggression before the lockdown (β = −0.15, p < 0.21).
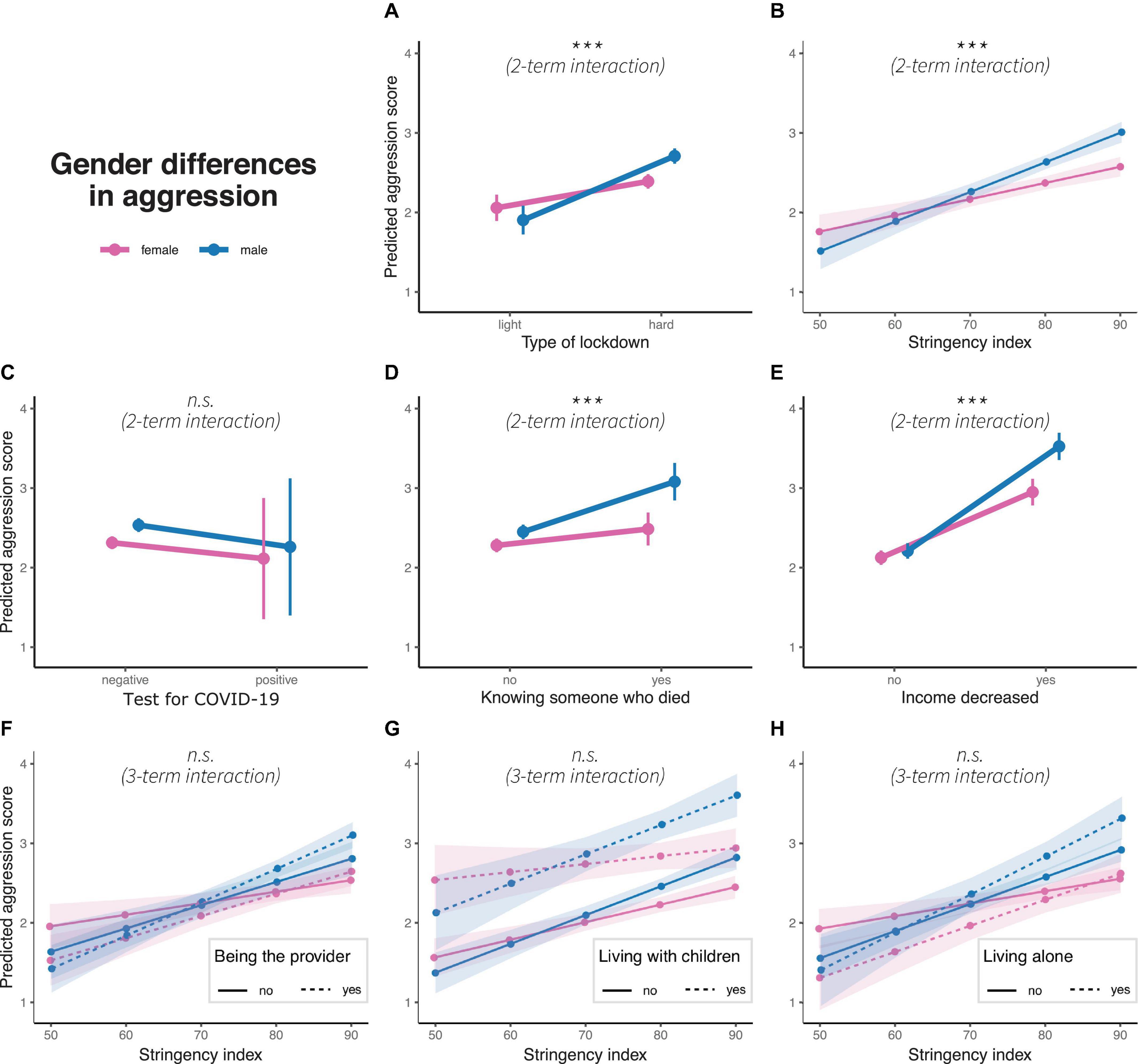
Figure 2. Gender differences in predicted aggression scores concerning (A) type of lockdown, (B) stringency index, (C) test for COVID-19, (D) knowing someone who died due to pandemic, (E) income decrease, and interaction of stringency index with (F) being the main household provider, (G) living with children and (H) living alone. Colors represent gender, dots represent marginal means, error bars or ribbons represent 95% confidence intervals. Linetypes represent at the bottom additional interaction terms. Significance of interaction effects are shown in italics; n.s.: non-significance. ***p < 0.01.
Generalized linear models are also significant for all anxiety models (light vs. hard lockdown: R2 = 0.053, F(1, 10977) = 87.34, p < 0.01, stringency: R2 = 0.054, F(1, 10977) = 90.33, p < 0.01, positive COVID-19 test: R2 = 0.045, F(1, 10977) = 73.98, p = 0.01, knowing someone who died due to COVID-19: R2 = 0.047, F(1, 10977) = 77.92, p < 0.01, income decrease: R2 = 0.086, F(1, 10977) = 147.1, p > 0.01, being the main provider in the household: R2 = 0.058, F(1, 10977) = 61.50, p < 0.01, living with children: R2 = 0.055, F(1, 10977) = 58.32, p < 0.01), and living alone: R2 = 0.059, F(1, 10977) = 62.94, p < 0.01. The positive and significant three-term interaction for living with children (β = 0.49, p < 0.01) indicates that GD decreases when living with children and increases when living without children (see Figure 3). Other interaction terms are not significant (see Supplementary Material).
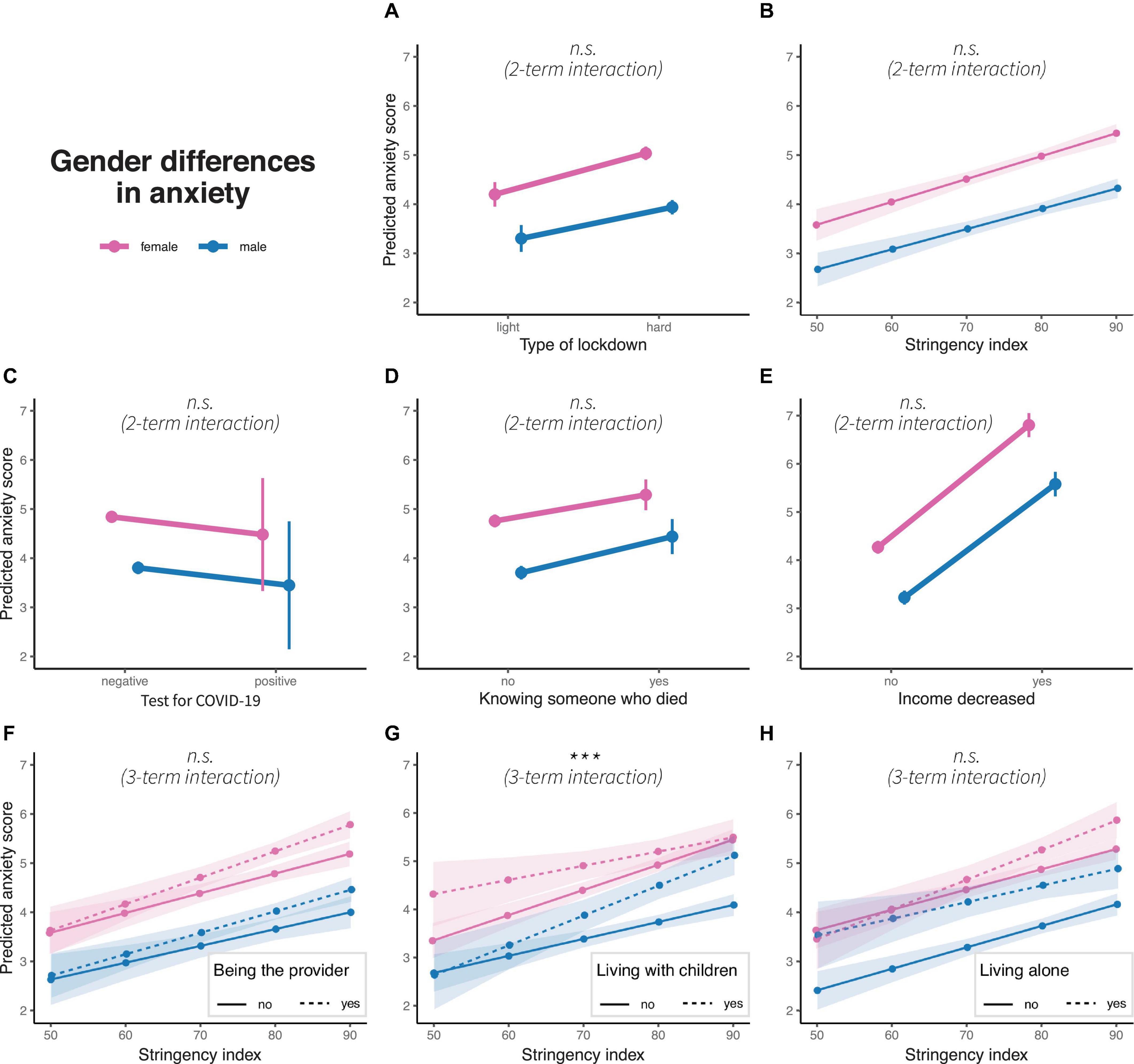
Figure 3. Gender differences in predicted anxiety scores concerning (A) type of lockdown, (B) stringency index, (C) test for COVID-19, (D) knowing someone who died due to pandemic, (E) income decrease, and interaction of stringency index with (F) being the main household provider, (G) living with children and (H) living alone. Colors represent gender, dots represent marginal means, error bars or ribbons represent 95% confidence intervals. Linetypes represent at the bottom additional interaction terms. Significance of interaction effects are shown in italics; n.s.: non-significance. ***p < 0.01.
Generalized linear models for depression models are significant for all variables (light vs. hard lockdown: R2 = 0.054, F(1, 10977) = 90.11, p < 0.01), stringency: R2 = 0.056, F(1, 10977) = 93.46, p < 0.01, positive COVID-19 test: R2 = 0.045, F(1, 10977) = 74.09, p = 0.01, knowing someone who died due to COVID-19: R2 = 0.046, F(1, 10977) = 75.60, p < 0.01, income decrease: R2 = 0.083, F(1, 10977) = 141.9, p > 0.01, being the main provider in the household: R2 = 0.065, F(1, 10977) = 69.77, p < 0.01, living with children: R2 = 0.058, F(1, 10977) = 61.54, p < 0.01, and living alone: R2 = 0.074, F(1, 10977) = 79.39, p < 0.01. Two-term interactions are significant for light vs. hard lockdown (β = −0.44, p < 0.1) and for stringency (β = −0.02, p < 0.1), both presenting increasing GD with tighter measures to control the pandemic. Three-term interactions are significant for living with children (β = 0.49, p < 0.05). Similar to anxiety, GD increases for individuals who do not live with children and decreases for those who live with children (see Figure 4). Other interaction terms are not significant (see Supplementary Material 2).
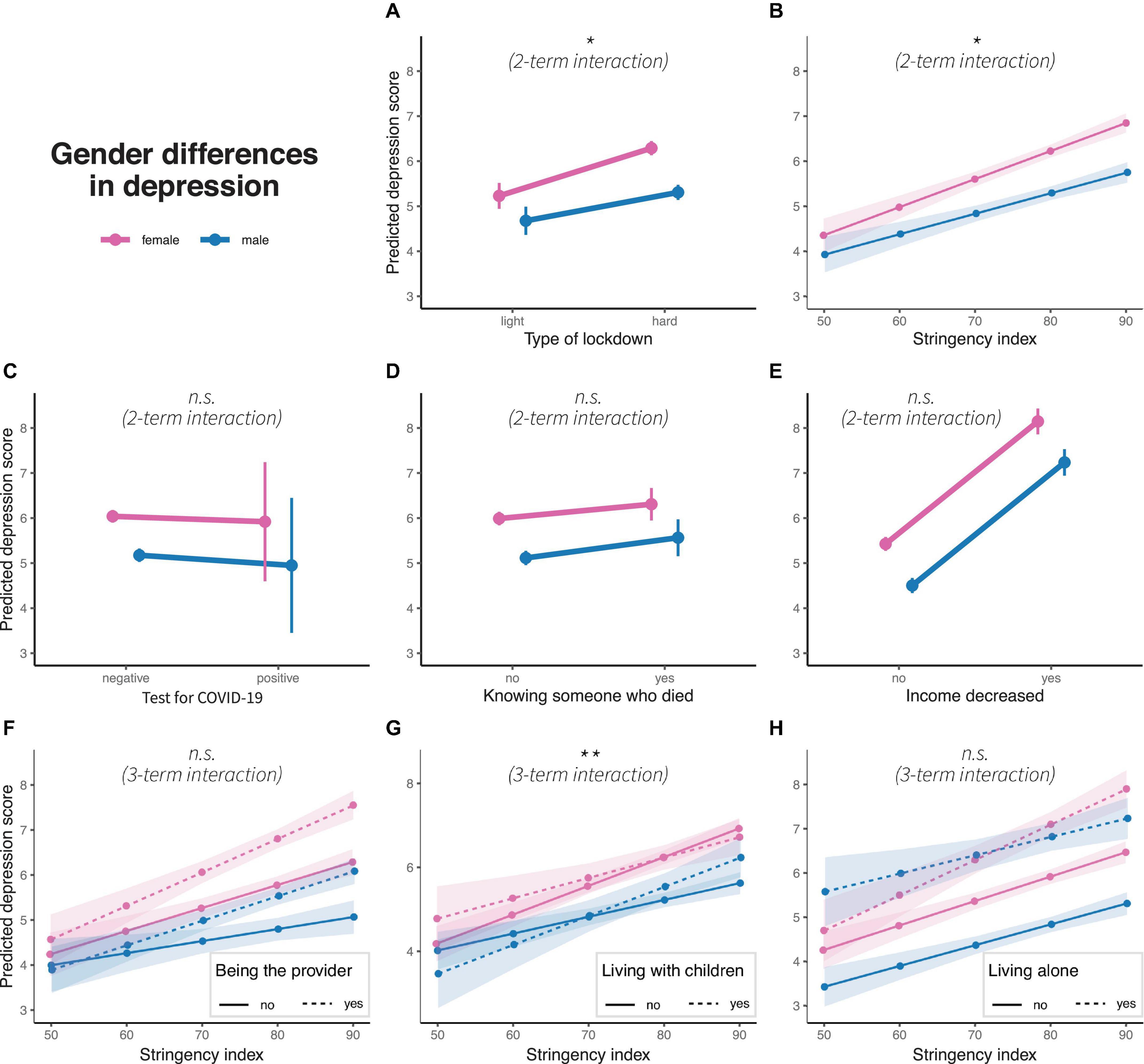
Figure 4. Gender differences in predicted depression scores concerning (A) type of lockdown, (B) stringency index, (C) test for COVID-19, (D) knowing someone who died due to pandemic, (E) income decrease, and interaction of stringency index with (F) being the main household provider, (G) living with children and (H) living alone. Colors represent gender, dots represent marginal means, error bars or ribbons represent 95% confidence intervals. Linetypes represent at the bottom additional interaction terms. Significance of interaction effects are shown in italics; n.s.: non-significance. *p < 0.1 and **p < 0.05.
Generalized linear models are also significant for the predictions of the somatic symptom burden (light vs. hard lockdown: R2 = 0.033, F(1, 10977) = 52.67, p < 0.01), stringency: R2 = 0.033, F(1, 10977) = 52.66, p < 0.01, positive COVID-19 test: R2 = 0.035, F(1, 10977) = 56.79, p = 0.01, knowing someone who died due to COVID-19: R2 = 0.034, F(1, 10977) = 54.43, p < 0.01, income decrease: R2 = 0.034, F(1, 10977) = 55.2, p < 0.01), being the main provider in the household: R2 = 0.034, F(1, 10977) = 34.61, p < 0.01, living with children: R2 = 0.034, F(1, 10977) = 34.97, p < 0.01), and living alone: R2 = 0.036, F(1, 10977) = 37.48, p < 0.01. Two-term interactions are significant for light vs. hard lockdown (β = 0.33, p < 0.01) and income decrease (β = 0.40, p < 0.05); both factors decrease GD. Three-term interaction is significant for living with children (β = −0.03, p < 0.1), with an increasing somatic symptom burden with increasing stringency for men living without children and a decreasing somatic symptom burden with rising stringency measures for men living with children (see Figure 5).
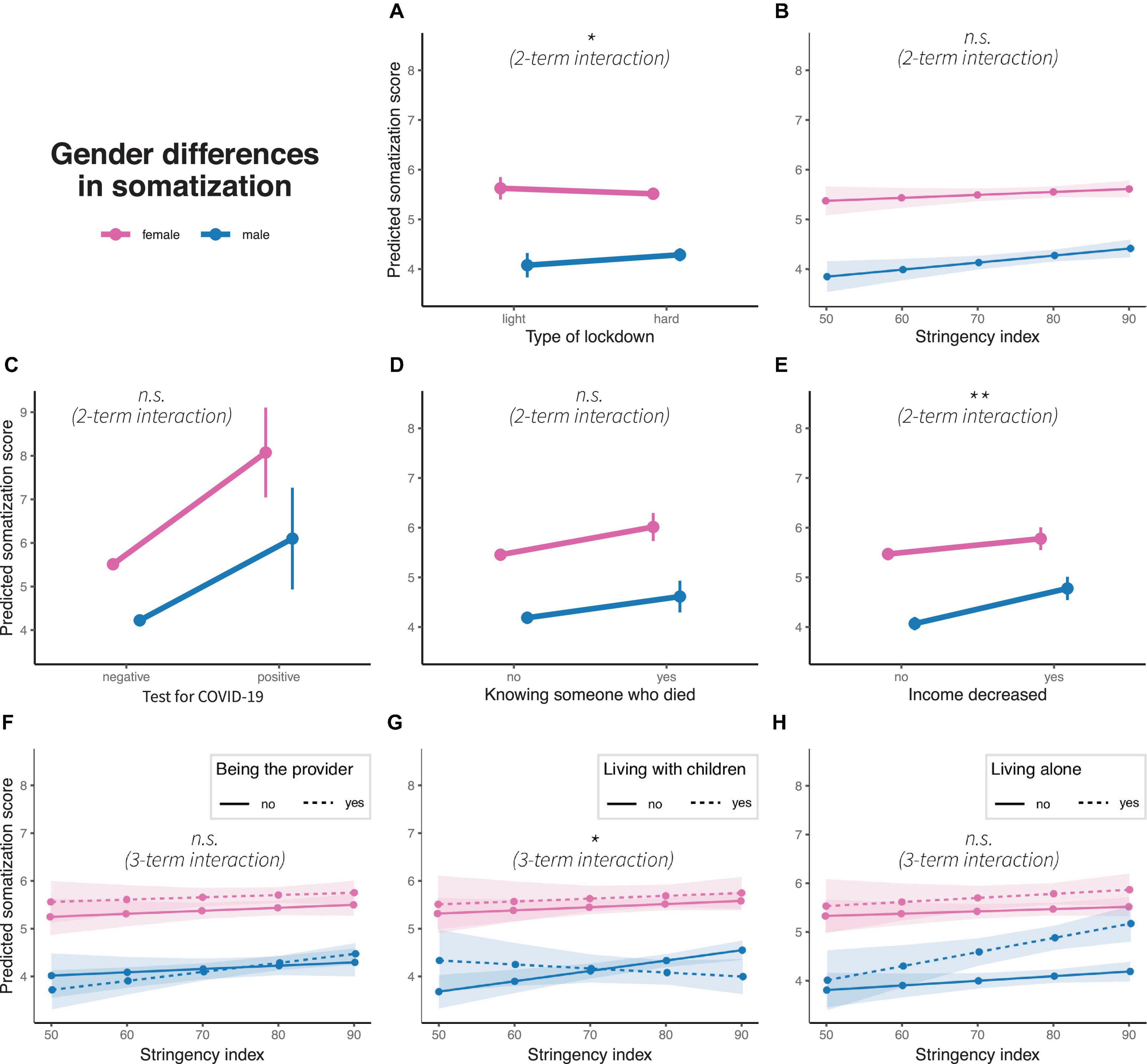
Figure 5. Gender differences in predicted somatic symptom burden scores concerning (A) type of lockdown, (B) stringency index, (C) test for COVID-19, (D) knowing someone who died due to pandemic, (E) income decrease, and interaction of stringency index with (F) being the main household provider, (G) living with children and (H) living alone. Colors represent gender, dots represent marginal means, error bars or ribbons represent 95% confidence intervals. Linetypes represent at the bottom additional interaction terms. Significance of interaction effects are shown in italics; n.s.: non-significance. *p < 0.1 and **p < 0.05.
In this study, we show that GD in aggression and depression increased as a consequence of stricter COVID-19 countermeasures in Germany. While, contrary to widespread findings, men and women did not differ in their aggressiveness during the light lockdown period or when stringency was low, we find significant differences in aggressiveness during the hard lockdown and when stringency was higher. Women presented more severe depression symptoms than men, and these symptoms increased more in women than in men in periods of stricter measures. In addition, we find GD in anxiety and somatization but the results do not indicate that these increased due to COVID-19 exposure, COVID-19 countermeasures or household characteristics. We find that somatic symptom burdens increased more in men than in women during the hard lockdown, resulting in a reduction in GD. In periods of higher stringency, we find living with children to decrease GD for depression and anxiety, and to increase GD in the somatic symptom burden. GD for the group who lived without children increased with higher stringency for depression and anxiety, but GD only emerged as stringency increased. We discuss the results below in more detail for each of the four main outcomes.
As the stringency of the lockdown increased, men developed higher levels of aggression than women. Moreover, GD in aggression further emerged when suffering an income decrease during the pandemic (men > women) and when participants knew someone who had died due to the pandemic (men > women). GD in aggression are not significant at baseline and for household characteristics (being the main provider, living with children, living alone). While previous studies have established strong evidence for an increase of domestic and cyberviolence during the pandemic (Fraser, 2020; Perez-Vincent et al., 2020; Ebert and Steinert, 2021), we show that the pandemic facilitates the development of aggression particularly in men. Previous studies have found robust correlations of the applied aggression questionnaire with act-based violence (Archer and Webb, 2006; Jurczyk and Lalak, 2020), and emerging evidence in neuroscience points to the rewarding properties and self-perpetuating nature of violent acts (Nell, 2006; Elbert et al., 2010; Golden and Shaham, 2018; Golden et al., 2019). Additionally, gendered expectations regarding stress response further maintain GD in aggression. Our study therefore suggests that violence perpetrated by men surges during the pandemic due to the accumulating stressors and gendered expectations. Based on the emerging evidence in regard to the rewarding properties of violence, heightened levels of aggression may remain after the pandemic and the relaxation of lockdown measures. Especially online aggression, such as cyberbullying, violent video games, or the consumption/publication of other violent online material, may be novel arenas that require attention. Violent behaviors impose high costs on society in regard to executive and justice measures, psychotherapy for victims and perpetrators, and prevention programs. At the same time they might also affect public thinking and opinion when ignored (Forum on Global Violence Prevention, 2011). More research is needed to understand the magnitude of this specific consequence of the pandemic, firstly, on the individuals who experience more anger and the urge to become physically aggressive and, secondly, on the individuals who share their lives with them at work, in their family, and on social media.
While our study replicates that women present more anxiety symptoms (e.g., Asher et al., 2017), we only find GD developing differently for men and women who lived with vs. without children. Here, the GD in individuals who lived with children are significant when stringency was low, but disappear–with men developing similarly high levels of depression as women–when they lived with children. In contrast, GD are not significant when stringency was low, but increase for men and women who lived without children with more stringent measures. Other interaction terms that we test are not significant. The latter is in line with the study of Ausín et al. (2021) from Spain. Following the rationale in the introduction, we would have expected women to be biologically more prone to develop, socially more prepared to express and in terms of gender roles more vulnerable to present higher levels of anxiety. This is not supported by our results, except for women who live without children, as they present a steeper increase of anxiety than men who live without children. In contrast, men who live with children seem to adopt “female levels of anxiety.” We did not expect this. What happens to the fathers who live with children during heightened stringency levels? One explanation may be that men faced high pressure both at work and as providers while having to arrange work from home or sharing responsibility for their children with their partner. There might also be a gender gap in the extent to which it is accepted for men to fail on tasks due to childcare. In turn, this could have allowed some relief to women who were not able to perform due to homeschooling and quarantines. Higher levels of empathy devoted to women might have facilitated this development. However, men and women respond equally to the crisis in terms of anxiety in general, though both showing an increase.
The lockdown and higher stringency measures are associated with higher levels of depression (replicating e.g., ref) and an increased GD in depression. According to our expectations, women developed higher levels of depression during the hard lockdown or when stringency increased, respectively. The findings are partly in contrast to the study of Ausín et al. (2021) from Spain who found that GD in depression was not increasing there.
As for anxiety, when living with or without children we find a more complex pattern of GD: no significant differences during the low stringency period in individuals without children but a steeper increase for women than for men when stringency increased. For individuals who reported living with children, we find a trend toward assimilating levels of depression in men when stringency levels intensified. We also find similar levels of depression for men and women who lived alone. This contradicts previous theories concerning the consequences of combining multiple roles (spouse, parent, and worker) on mental health with a stronger impact on women than men (Simon, 1995). Our result indicates that men are strongly affected by stricter stringency when they live alone or with children. Moreover, this contrasts with previous studies that found having children to constitute a protective factor for mental ill-health for men only, with men who had two or more children presenting a lower risk of developing mental disorders when compared to men without children (Klose and Jacobi, 2004).
On the other hand, the result that GD in mental disorders increased for women is in line with other COVID-19 studies that reported a new gap in psychological distress emerging between women with children at school age and women without children (Zamarro and Prados, 2021). Similarly, Mazza et al. (2020) suggested that women who lived alone or had children with behavioral problems may present an increase of mental disorders, such as stress or depression. An emerging research gap that results from this study is in regard to men who develop more depression in their dual role as fathers at home with children and providers. Does sharing responsibility at work and in the household mean that the burden is doubled and that both partners have to carry their weight? Or can the burden actually be shared?
Hard lockdown and increasing stringency are associated with a steeper increase in depression for women than for men. One factor that may contribute to this are the heightened levels of domestic and gender-based violence (GBV) documented during the lockdowns. Indeed, this has previously been claimed to be a major health concern during the pandemic (Bradbury-Jones and Isham, 2020; Telles et al., 2020), who argued that the impact of the pandemic has fueled stress and tensions within families, with an increased and continuous risk of domestic violence and divorce cases (Chang, 2020; Peterman et al., 2020; Usher et al., 2020). Accordingly, several studies reported that the increase of domestic violence occurred especially during stricter lockdowns or states of emergency (Campbell, 2020; Usher et al., 2020), e.g., a 55% increase of calls made to a domestic violence hotline during the lockdown in Argentina (Perez-Vincent et al., 2020), or the reported increased risk of domestic violence during the pandemic in Germany (Ebert and Steinert, 2021).
Furthermore, evidence shows that family violence, including IPV, child abuse and elder abuse, increase during and after large-scale crises or disasters (Neria et al., 2008; Perez-Vincent et al., 2020; Peterman et al., 2020). Families from socially deprived settings and with low socioeconomic status (e.g., low educational levels or unemployment) are particularly at risk in Germany (Ravens-Sieberer et al., 2021). Women and children are most affected by these incidents globally and, although data is still scarce, the domestic violence rates appear to be rising rapidly (Perez-Vincent et al., 2020). Yet, children and adolescents in Germany do not seem to be as negatively affected as, for example, youth from Spain and Italy, where higher levels of stress on families were observed, with 85.7% of the parents reporting emotional and behavioral changes in their children (Orgilés et al., 2020); or in China, where one study reported 22.6% of students having depressive symptoms, which is higher than the 17.2% previously reported in studies on primary schools (Xie et al., 2020).
In addition to GBV, a combination of the biologically determined heightened susceptibility of women for depressive symptoms (e.g., Slavich and Sacher), combined with gender-specific roles that come with restrictions and opportunities (Seedat et al., 2009; Salk et al., 2017), may underlie the enforced GD during periods of high-stringency lockdown measures. However, it is unclear why lockdowns and stringency do not increase GD in anxiety but only in depression. Both syndromes are more pronounced in women than in men and related to adversity (Kuzminskaite et al., 2021). One explanation, yet speculative, could be that the pandemic imposes a situation with both an invisible or implicit threat and also highly incisive inescapable consequences, connected with the uncertainty regarding what the post-pandemic period will look like and when it will start.
To the best of our knowledge, there is no study that investigates characteristics of threats in association with specific symptoms of depression and anxiety. However, it is known that emotional abuse and neglect (especially during childhood) may lead to more pronounced symptoms of depression than post-traumatic stress or anxiety. Indeed, the pandemic has imposed strong restrictions on meeting family, friends, and other community members. Accordingly, living alone has been shown to be a consistent moderator of symptom severity, both in anxiety and depression. The social deprivation may therefore have had a stronger weight than the actual threat to physical integrity. From a sociological perspective, these results indicate that, when traditional resources of social cohesion are interrupted (real life sociality), a substantial part of resilience may be undermined.
But why is there a difference by gender? One explanation may be the gendered labor patterns in Germany which are outlined in detail below in the section “Moderating Social Factors Associated With the COVID-19 Pandemic.” In summary, it means that, on average, men engage more in paid work while women remain occupied in informal care and part-time jobs–or poorly paid jobs, e.g., in supermarkets or as nurses. Since the German government avoided the wholesale closure of industries, men were less likely to be confined to their homes and thus able to socialize with their colleagues at work, whereas many retail businesses and the hospitality industry were shut. As female employment is relatively high in these sectors, more women were cut off from their social environments and isolated with their children at home.
Many of the children themselves had difficulties coping and developed abnormal behaviors (Wang G. et al., 2020), which impacted their parents (Calvano et al., 2021)–mothers and fathers alike–as indicated by our results. This is where the pandemic comes down to the concept of Seligman’s learned helplessness from about four decades ago. Many people have realized that there is no escape from this crisis. Policies and stepped care mental health programs could provide relief and help people reestablish social activities, regain a feeling of autonomy (external rather than internal), reprocess and contextualize the most important events (that the pandemic was a special situation requiring special measures rather than a global plan to serve the self-interest of anyone), and to close off the period (to counteract the attribution that the pandemic is a permanent condition).
The overall subjective burden of somatic symptoms was higher in women than in men. Yet, the hard lockdown period, an income decrease, and higher-stringency lockdown measures resulted, for participants who lived with children, in a steeper increase of somatic symptoms in men than in women (decreasing GD). Increased vulnerability of men in developing severe symptoms after a COVID-19 infection have been well established (Conti and Younes, 2020; Jin et al., 2020; Wenham, 2020). However, our study does not find a higher level of somatic symptoms in men for those who tested positive. On the other hand, our sample includes only a very small percentage of participants who tested positive for COVID-19. Given the potential long-term consequences of COVID-19 infections and the consistent association of the somatic symptoms with mental health problems, further research would be beneficial.
In the case of men who lived with children assimilating to the somatic symptom burden of women, it is noteworthy that the COVID-19 crisis does not actually seem to have increased GD in terms of levels of parental involvement in childcare. In Germany, for example, studies observed that both parents reported spending substantially more time with their children during the crisis than they did in the previous year (Kreyenfeld et al., 2020), and there are seemingly no elementary differences in established aggregate-level roles of division of labor in couples (Hank and Steinbach, 2020).
There is considerable evidence showing an overall magnifying of gender inequalities in paid and non-paid work during COVID-19 (Farré et al., 2020). Although women are as likely as men to have flexible jobs, women globally earn less than men and were already in a more vulnerable situation before the pandemic started (Carli, 2020). The pandemic increases this inequality, because women disproportionately occupy a share of jobs requiring face-to-face interactions, e.g., retail or personal care, meaning that the opportunities to work from home and the risk of unemployment are higher (Freund and Hamel, 2020). Moreover, an important share of women are essential workers (Boniol et al., 2019), e.g., healthcare workers, with an increased risk of infection from the coronavirus, putting them at a higher risk of stress and burnout (Carli, 2020).
In many OECD countries, including Germany, the domestic division of labor still predominantly follows a traditional system (Zimmert, 2019). Despite recent policy reforms that have resulted in some increase in maternal full-time work and an increase in fathers taking parental leave, equally shared care work among both partners is still the exception, especially in West Germany (Hank and Steinbach, 2020; Kreyenfeld et al., 2020). The same is observed in the United Kingdom, with mothers spending less time in paid work but more time on household responsibilities (mothers combined paid work with other activities–mostly childcare–47% of their time, compared with 30% for fathers, a 2:1 ratio) (Andrew et al., 2020). Similar results are reported in Spain, with mothers spending on average 28 h a week on childcare compared with 19 h for fathers (Farré et al., 2020) see also (Czymara et al., 2021) for further discussion).
COVID-19 and its countermeasures have impacted women and men differently in terms of family dynamics and the intra-household allocation of paid and family care work, with consequences for both physical and mental health. Gender norms fundamentally shape women’s and men’s lives and this pandemic has remarkably increased the need for care inside homes, which has a particularly large impact on working mothers (Alon et al., 2020). Women underpin a greater share of informal care, providing on average 3.3 times more care than men at home (Addati and Cattaneo, 2018; Manzo and Minello, 2020), with the consequence of limiting their work and economic opportunities (Wenham, 2020). Comprehensively, social isolation was found to affect women in particular, considering that, for example, school closures forced more women than men to take time off for childcare, which might provide some insights into women’s loneliness and depression (Chang, 2020). Thus, for the past three decades, studies have consistently reported that women are more likely to experience depression than men (Salk et al., 2017; Weissman and Klerman, 1977). However, as Brommelhoff et al. (2004) observes, reporting bias might also contribute to the higher rates of depression in women, since even when men and women present similar depression symptoms, women are tendentiously more likely to be diagnosed with depression, which might underlie a gender bias. In line with this, Bluhm (2011) argues that depressed women do not tend to simply act out passive behavior, but are more aware of their symptoms, despite the effects of their environment and their illness.
Our study highlights unresolved questions for research and policy. The first one regards aggression. How can increasing aggression in men be addressed effectively during and after the pandemic? Barriers to seek services as a victim, but also as a perpetrator, have to be distinguished into community and online programs. More research is necessary to estimate the demand during pandemics and adequately scale up these services. Furthermore, the focus in research and practice should shift toward prevention programs for perpetrators, since they may be at particular risk for developing a robust trait of (appetitive) aggression, antisocial personality disorder, or psychopathy (Powell et al., 1997; Cauffman et al., 1998; Fondacaro et al., 1999; Garieballa et al., 2006). Thus, screening for traumatic events should become a routine part of psychological treatment. Combined trauma therapy with extended group sessions allowing for skills training and help to abstain from aggression has shown promising results (Robjant et al., 2019; Koebach et al., 2021). In addition, systemic approaches help to de-escalate intrinsic family dynamics that lead to aggression and violence (e.g., Oka and Whiting, 2011). However, prevention should start with the adequate care of trauma-exposed children and youths, especially young men who learn to experience and control their aggression as part of their developmental milestones (Kröber, 2012).
Second, our data show that individuals living with children–male or female–present higher levels of depression and anxiety. Due to changes in the workplace and within families, more men will have to juggle paid work with housework. This will lead to higher stress loads and the question of how families can be protected. The increased stress load during the pandemic highlights the importance of well-functioning childcare services and schools, not only as a measure to raise and prepare the next generation for the workplace but also to facilitate mental health in society. Further research should explore the clinical relevance of the symptoms and whether gender assimilation in depression is maintained and how it develops after the pandemic. More research is needed to explore the specific challenges faced by men during the pandemic (see also Betron et al., 2020). It is also important to note that children growing up with a depressed parent have a higher risk of developing mental disorders themselves (Downey and Coyne, 1990).
Third, the higher levels of depression in women during crises lead to the question of whether depression in women can be prevented through gender equality programs. Programs to assist women to cope with the additional stress may be particularly important. In a large multinational study (Seedat et al., 2009) indeed found a decrease in GD in depression for countries with more gender equality. Given the hormonal aspects in the development of depression, this should nevertheless be complemented with early psychotherapeutic intervention. Mental health problems induced by the pandemic are likely to persist over time and mental health services should prepare for higher numbers of patients emerging after the COVID-19 pandemic. Currently, the demand for mental healthcare is rapidly increasing, but affected individuals experience higher barriers to care due to lockdown measures being in place and services being overstretched. According to a WHO survey of 130 member states launched in mid-June 2020, the COVID-19 pandemic disrupted or halted critical mental healthcare in 93% of these countries, with approximately only 30% of mental health services for children, adolescents or older adults reporting no disruptions (WHO, 2020).
Fourth, depression and anxiety are higher in individuals who live alone, leading to the question how we can improve their resilience. Targeted regulations and interventions are necessary to shield this population from the negative mental health effects. Again, it will be an essential question how many suffer at a clinically relevant level and what the recovery rate is after the crisis. A model example is the project Coping with Corona: Extended Psychosomatic care in Essen (CoPE) developed to target, prevent and address the psychological burden of the pandemic, via a community-based intervention. CoPE aims at providing health support with psychoeducation, mindfulness and cognitive behavioral skills training. The intervention addresses day structuring, fears and worries, conflicts, stress management, sleep, and loneliness (Bäuerle et al., 2020c).
Fifth, despite the diversity in individual experiences, COVID-19 has affected everyone. Community intervention may therefore help a collective reprocessing of the pandemic and thus prevent further divisions in society. The key question is whether there is a desire and a political will to form a collective memory. The pandemic has led to divergent adverse, sometimes traumatic experiences of the crisis in terms of age/generation, gender, socioeconomic status, and work group (e.g., for medical doctors and nurses). Immediate responses tend to avoid and close with the past while ignoring the personal wounds and societal cleavages that were generated. In the long run, this may divide society. Therefore, a collective process to restore a shared understanding of the pandemic is necessary to rebuild a sense of togetherness and community. To this end, the narratives of subgroups who experienced marginalization and disadvantage due to policies related to the pandemic can be merged and developed to be presented to the affected community and facilitate a shared collective memory of the living generation (Koebach and Robjant, sub).
Our study has several strengths. First, it is one of the largest samples to date to examine GD in mental health burdens globally and in Germany during COVID-19. Second, besides mental health issues that were known to be more common in women, we also investigate aggression as an important mental health outcome. Third, LwC collects data in real time, reducing memory bias and allowing a valid comparison on the impact of the introduction or relaxation of COVID-19 countermeasures over time. Fourth, we collect nuanced information on what we call the exposure to COVID-19, which covers both respondents’ own health experience of the pandemic, that of their social circle and an economic dimension. Finally, to our knowledge, there is no previous study that investigated gender effects in somatization dependent on the pandemic.
Nevertheless, our study also has some important limitations. First, the sampling technique we used to collect data is an online survey and we have to consider the possibility of selection bias, as suggested by the unbalanced gender ratio observed, e.g., when comparing cross-sectional data during the light and hard lockdown periods, which are based on answers by different individuals. Even though we statistically weighted sample responses based on population data on gender, age, level of education, and income, questions about representativeness and comparability over time may remain. Second, the responses were based on a self-administered online survey, which might create systematic differences in answers compared to answers from in-person interviews (though responses may suffer less from enumerator bias). Third, the variable whether the participant had previously contracted a COVID-19 infection is also a self-report rather than based on a test result. Fourth, we have limitations concerning sociodemographic data. since this is an international survey and the constructs of ethnicity and race are culturally specific, LwC does not include any questions on ethnicity or race. Also, LwC only includes a gender variable as: male, female or other, and does not include non-binary gender identity considerations. We acknowledge that a binary division of gender has been called into question and a more fluid and inclusive understanding of gender should be developed. Finally, our sample consisted of a very small part of individuals who tested positive for COVID-19 which restricts the relevance of the non-significant results and requires further investigation, possible using drawing on more data from the LwC survey or similar datasets.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by UNU-WIDER (reference number: 202009/01). The patients/participants provided their written informed consent to participate in this study.
LA and AK made substantial contributions to the conception or design of the work and drafting the work. AH, TB, WS, and PJ made substantial contributions to the conception and design and were project leaders of Life with Corona (LwC). LA, AK, OD, and SC made substantial contributions to the analysis or interpretation of data for the work. LA, AK, OD, SC, AH, WS, HF, PJ, and TB made substantial contribution to the revision of the analysis and interpretation of data for the work and revising it critically for important intellectual content. LA, AK, OD, SC, AH, WS, HF, PJ, and TB provided approval for publication of the content and agreed to be accountable for all aspects of the work in ensuring that questions related to accuracy of any part of the work are appropriately investigated and resolved. All the authors contributed and approved the submitted version of this article.
This research was supported by the Alexander von Humboldt Foundation, UNU-WIDER, and the United Kingdom Economic and Social Research Council (ESRC) under the Large Grant project “Inequality and Governance in Unstable Democracies: The Mediating Role of Trust” (grant number ES/S009965/1).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We are grateful for helpful comments and suggestions from Otto Meyer zu Schwabedissen and Frederike Kaiser, who provided excellent research assistance; and to Fedor van Rijn for excellent language editing. All remaining errors are our own.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.689396/full#supplementary-material
Abd-El-Fattah, S. M. (2013). A cross-cultural examination of the aggression questionnaire-short form among egyptian and Omani adolescents. J. Pers. Assessment 95, 539–548. doi: 10.1080/00223891.2013.791828
Abramson, L., Seligman, M., and Teasdale, J. (1978). Learned helplessness in humans: critique and reformulation. J. Abnorm. Psychol. 87, 49–74. doi: 10.1037/0021-843X.87.1.49
Addati, L., and Cattaneo, U. (2018). Care Work and Care Jobs For The Future Of Decent Work [Report]. Available online at: http://www.ilo.org/global/publications/books/WCMS_633135/lang–en/index.htm (accessed May 15, 2021).
Allen, J. J., Anderson, C. A., and Bushman, B. J. (2018). The general aggression model. Curr. Opin. Psychol. 19, 75–80. doi: 10.1016/j.copsyc.2017.03.034
Alloy, L. B. (1982). The role of perceptions and attributions for response-outcome noncontingency in learned helplessness: a commentary and discussion. J. Pers. 50, 443–479. doi: 10.1111/j.1467-6494.1982.tb00229.x
Alon, T., Doepke, M., Olmstead-Rumsey, J., and Tertilt, M. (2020). The Impact of COVID-19 on Gender Equality (No. w26947; p. w26947). Cambridge, MA: National Bureau of Economic Research, doi: 10.3386/w26947
Alonzi, S., La Torre, A., and Silverstein, M. W. (2020). The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychol. Trauma 12, S236–S238. doi: 10.1037/tra0000840
Altemus, M. (2006). Sex differences in depression and anxiety disorders: Potential biological determinants. Hormones Behav. 50, 534–538. doi: 10.1016/j.yhbeh.2006.06.031
Altemus, M., Sarvaiya, N., and Epperson, C. N. (2014). Sex differences in anxiety and depression clinical perspectives. Front. Neuroendocrinol. 35:320–330. doi: 10.1016/j.yfrne.2014.05.004
Anderson, C. A., and Bushman, B. J. (2002). Human aggression. Annu. Rev. Psychol. 53, 27–51. doi: 10.1146/annurev.psych.53.100901.135231
Andresen, M. A., and Hodgkinson, T. (2020). Somehow I always end up alone: COVID-19, social isolation and crime in Queensland, Australia. Crime Sci. 9:25. doi: 10.1186/s40163-020-00135-4
Andrew, A., Cattan, S., Dias, M. C., Farquharson, C., Kraftman, L., Krutikova, S., et al. (2020). How are Mothers and Fathers Balancing Work and Family under Lockdown?. London: Institute for Fiscal Studies, doi: 10.1920/BN.IFS.2020.BN0290
Archer, J. (2004). Sex differences in aggression in real-world settings: a meta-analytic review. Rev. Gen. Psychol. 8, 291–322. doi: 10.1037/1089-2680.8.4.291
Archer, J., and Webb, I. A. (2006). The relation between scores on the Buss–Perry Aggression Questionnaire and aggressive acts, impulsiveness, competitiveness, dominance, and sexual jealousy. Aggressive Behav. 32, 464–473. doi: 10.1002/ab.20146
Arseneault, L. (2017). The long-term impact of bullying victimization on mental health. World Psychiatry 16, 27–28. doi: 10.1002/wps.20399
Asher, M., Asnaani, A., and Aderka, I. M. (2017). Gender differences in social anxiety disorder: a review. Clin. Psychol. Rev. 56, 1–12. doi: 10.1016/j.cpr.2017.05.004
Augsburger, M., Meyer-Parlapanis, D., Bambonye, M., Elbert, T., and Crombach, A. (2015). Appetitive aggression and adverse childhood experiences shape violent behavior in females formerly associated with combat. Front. Psychol. 6:1756. doi: 10.3389/fpsyg.2015.01756
Ausín, B., Gonzalez-Sanguino, C., Castellanos, M., and Munoz, M. (2021). Gender-related differences in the psychological impact of confinement as a consequence of COVID-19 in Spain. J. Gender Stud. 30, 29–38. doi: 10.1080/09589236.2020.1799768
Bander, R. S., and Betz, N. E. (1981). The relationship of sex and sex role to trait and situationally specific anxiety types. J. Res. Pers. 15, 312–322. doi: 10.1016/0092-6566(81)90029-5
Barsky, A. J., Orav, E. J., and Bates, D. W. (2005). Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Arch. Gen. Psychiatry 62:903. doi: 10.1001/archpsyc.62.8.903
Barsky, A. J., Peekna, H. M., and Borus, J. F. (2001). Somatic symptom reporting in women and Men. J. Gen. Intern. Med. 16, 266–275. doi: 10.1046/j.1525-1497.2001.00229.x
Bäuerle, A., Graf, J., Jansen, C., Dörrie, N., Junne, F., Teufel, M., et al. (2020c). An e-mental health intervention to support burdened people in times of the COVID-19 pandemic: CoPE It. J. Public Health. 42, 647–648. doi: 10.1093/pubmed/fdaa058
Bäuerle, A., Steinbach, J., Schweda, A., Beckord, J., Hetkamp, M., Weismüller, B., et al. (2020a). Mental health burden of the COVID-19 outbreak in germany: predictors of mental health impairment. J. Primary Care Commun. Health 11:2150132720953682. doi: 10.1177/2150132720953682
Bäuerle, A., Teufel, M., Musche, V., Weismüller, B., Kohler, H., Hetkamp, M., et al. (2020b). Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J. Public Health 42, 672–678. doi: 10.1093/pubmed/fdaa106
Beesdo, K., Pine, D. S., Lieb, R., and Wittchen, H.-U. (2010). Incidence and risk patterns of anxiety and depressive disorders and categorization of generalized anxiety disorder. Arch. Gen. Psychiatry 67:47. doi: 10.1001/archgenpsychiatry.2009.177
Betron, M., Gottert, A., Pulerwitz, J., Shattuck, D., and Stevanovic-Fenn, N. (2020). Men and COVID-19: adding a gender lens. Glob. Public Health 15, 1090–1092. doi: 10.1080/17441692.2020.1769702
Bettencourt, B., Talley, A., Benjamin, A. Jr., and Valentine, J. (2006). Personality and aggressive behavior under provoking and neutral conditions: a meta-analytic review. Psychol. Bull. 132, 751–777. doi: 10.1037/0033-2909.132.5.751
Björkqvist, K. (2018). Gender differences in aggression. Curr. Opin. Psychol. 19, 39–42. doi: 10.1016/j.copsyc.2017.03.030
Bluhm, R. (2011). Gender differences in depression: explanations from feminist ethics. Int. J. Fem. Approaches Bioeth. 4, 69–88. doi: 10.2979/intjfemappbio.4.1.69
Boniol, M., McIsaac, M., Xu, L., Wuliji, T., Diallo, K., and Campbell, J. (2019). Gender Equity in the Health Workforce: Analysis of 104 Countries, Vol. 8. Geneva: World Health Organization.
Boyd, A., Van de Velde, S., Vilagut, G., de Graaf, R., O×Neill, S., Florescu, S., et al. (2015). Gender differences in mental disorders and suicidality in Europe: results from a large cross-sectional population-based study. J. Affect. Disord. 173, 245–254. doi: 10.1016/j.jad.2014.11.002
Bradbury-Jones, C., and Isham, L. (2020). The pandemic paradox: the consequences of COVID-19 on domestic violence. J. Clin. Nurs. 29, 2047–2049. doi: 10.1111/jocn.15296
Bretschneider, J., Kuhnert, R., and Hapke, U. (2017). Depressive symptoms among adults in Germany. J. Health Monit. 2, 77–83. doi: 10.17886/RKI-GBE-2017-070
Brommelhoff, J. A., Conway, K., Merikangas, K., and Levy, B. R. (2004). Higher rates of depression in women: role of gender bias within the family. J. Womens Health 13, 69–76. doi: 10.1089/154099904322836474
Brück, T., Justino, P., Verwimp, P., Avdeenko, A., and Tedesco, A. (2016). Measuring violent conflict in micro-level surveys: current practices and methodological challenges. World Bank Res. Observer 31, 29–58. doi: 10.1093/wbro/lkv011
Bryant, F. B., and Smith, B. D. (2001). Refining the architecture of aggression: a measurement model for the buss–perry aggression questionnaire. J. Res. Pers. 35, 138–167. doi: 10.1006/jrpe.2000.2302
Bueno-Notivol, J., Gracia-García, P., Olaya, B., Lasheras, I., López-Antón, R., and Santabárbara, J. (2021). Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 21:100196. doi: 10.1016/j.ijchp.2020.07.007
Buil-Gil, D., Miró-Llinares, F., Moneva, A., Kemp, S., and Díaz-Castaño, N. (2021). Cybercrime and shifts in opportunities during COVID-19: A preliminary analysis in the UK. Eur. Soc. 23(sup1), S47–S59. doi: 10.1080/14616696.2020.1804973
Bushman, B. (2016). Aggression and Violence – A social psychological perspective. Frontiers of Social Psychology. New York, NY: Routledge.
Calvano, C., Engelke, L., Di Bella, J., Kindermann, J., Renneberg, B., and Winter, S. M. (2021). Families in the COVID-19 pandemic: parental stress, parent mental health and the occurrence of adverse childhood experiences-results of a representative survey in Germany. Eur. Child Adolesc. Psychiatry 1–13. doi: 10.1007/s00787-021-01739-0
Cameron, J. J., and Stinson, D. A. (2019). Gender (mis)measurement: Guidelines for respecting gender diversity in psychological research. Soc. Pers. Psychol. Compass 13:e12506. doi: 10.1111/spc3.12506
Campbell, A. M. (2020). An increasing risk of family violence during the Covid-19 pandemic: Strengthening community collaborations to save lives. Foren. Sci. Int. Rep. 2:100089. doi: 10.1016/j.fsir.2020.100089
Canet-Juric, L., Andrés, M. L., del Valle, M., López-Morales, H., Poó, F., Galli, J. I., et al. (2020). A Longitudinal Study On The Emotional Impact Cause By The COVID-19 pandemic quarantine on general population. Front. Psychol. 11:565688. doi: 10.3389/fpsyg.2020.565688
Carli, L. L. (2020). Women, gender equality and COVID-19. Gender Manag. Int. J. 35, 647–655. doi: 10.1108/GM-07-2020-0236
Cauffman, E., Feldman, S., Watherman, J., and Steiner, H. (1998). Posttraumatic stress disorder among female juvenile offenders. J. Am. Acad. Child Adolesc. Psychiatry 37, 1209–1216. doi: 10.1097/00004583-199811000-00022
Chambless, D. L., and Mason, J. (1986). Sex, sex-role stereotyping and agoraphobia. Behav. Res. Ther. 24, 231–235. doi: 10.1016/0005-7967(86)90098-7
Chang, W.-H. (2020). Understanding the COVID-19 pandemic from a gender perspective. Taiwan. J. Obstet. Gynecol. 59, 801–807. doi: 10.1016/j.tjog.2020.09.004
Chemtob, C., Novaco, R., Hamada, R., Gross, D., and Smith, G. (1997). Anger regulation deficits in combat-related posttraumatic stress disorder. J. Traumatic Stress 10, 17–36. doi: 10.1023/A:1024852228908
Começanha, R., Basto-Pereira, M., and Maia, Â (2017). Clinically speaking, psychological abuse matters. Compr. Psychiatry 73, 120–126. doi: 10.1016/j.comppsych.2016.11.015
Conti, P., and Younes, A. (2020). Coronavirus COV-19/SARS-CoV-2 affects women less than men: clinical response to viral infection. J. Biol. Regul. Homeost. Agents 34, 339–343. doi: 10.23812/Editorial-Conti-3
Czymara, C. S., Langenkamp, A., and Cano, T. (2021). Cause for concerns: gender inequality in experiencing the COVID-19 lockdown in Germany. Eur. Soc. 23(sup1), S68–S81. doi: 10.1080/14616696.2020.1808692
Deffenbacher, J. L., Oetting, E. R., Lynch, R. S., and Morris, C. D. (1996). The expression of anger and its consequences. Behav. Res. Ther. 34, 575–590. doi: 10.1016/0005-7967(96)00018-6
Denson, T. F., O’Dean, S. M., Blake, K. R., and Beames, J. R. (2018). Aggression in Women: behavior, brain and hormones. Front. Behav. Neurosci. 12:18. doi: 10.3389/fnbeh.2018.00081
Diamond, P. M., and Magaletta, P. R. (2006). The short-form buss-perry aggression questionnaire (BPAQ-SF): a validation study with federal offenders. Assessment 13, 227–240. doi: 10.1177/1073191106287666
Donner, N. C., and Lowry, C. A. (2013). Sex differences in anxiety and emotional behavior. Pflügers Arch. Eur. J. Physiol. 465, 601–626. doi: 10.1007/s00424-013-1271-7
Downey, G., and Coyne, J. C. (1990). Children of depressed parents: an integrative review. Psychol. Bull. 108, 50–76. doi: 10.1037/0033-2909.108.1.50
Ebert, C., and Steinert, J. I. (2021). Prevalence and risk factors of violence against women and children during COVID-19 Germany. Bull. World Health Organ. 99, 429–438.
Ehlers, A. (1993). Somatic symptoms and panic attacks: a retrospective study of learning experiences. Behav. Res. Ther. 31, 269–278. doi: 10.1016/0005-7967(93)90025-p
Eisenberger, N. I. (2012). The pain of social disconnection: examining the shared neural underpinnings of physical and social pain. Nat. Rev. Neurosci. 13, 421–434. doi: 10.1038/nrn3231
Eisenberger, N. I., and Lieberman, M. D. (2004). Why rejection hurts: a common neural alarm system for physical and social pain. Trends Cogn. Sci. 8, 294–300. doi: 10.1016/j.tics.2004.05.010
Elbert, T., Schauer, M., and Moran, J. K. (2018). Two pedals drive the bi-cycle of violence: Reactive and appetitive aggression. Curr. Opin. Psychol. 19, 135–138. doi: 10.1016/j.copsyc.2017.03.016
Elbert, T., Weierstall, R., and Schauer, M. (2010). Fascination violence: on mind and brain of man hunters. Eur. Arch. Psychiatry Clin. Neurosci. 260 Suppl 2, S100–S105. doi: 10.1007/s00406-010-0144-8
Ettman, C. K., Abdalla, S. M., Cohen, G. H., Sampson, L., Vivier, P. M., and Galea, S. (2020). Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw. Open 3:e2019686. doi: 10.1001/jamanetworkopen.2020.19686
Fahlgren, M. K., Cheung, J. C., Ciesinski, N. K., McCloskey, M. S., and Coccaro, E. F. (2021). Gender differences in the relationship between anger and aggressive behavior. J. Interpers. Violence 5:886260521991870. doi: 10.1177/0886260521991870
Farré, L., Fawaz, Y., Gonzalez, L., and Graves, J. (2020). How the COVID-19 Lockdown Affected Gender Inequality in Paid and Unpaid Work in Spain. IZA Discussion Papers (No. 13434; IZA Discussion Papers). Bonn: Institute of Labor Economics (IZA).
Feeny, N. C., Zoellner, L. A., and Foa, E. B. (2000). Anger, dissociation, and posttraumatic stress disorder among female assault victims. J. Traumatic Stress 13, 89–100. doi: 10.1023/A:1007725015225
Fink, P., Toft, T., Hansen, M. S., Ørnbøl, E., and Olesen, F. (2007). Symptoms and syndromes of bodily distress: an exploratory study of 978 internal medical, neurological, and primary care patients. Psychosom. Med. 69, 30–39. doi: 10.1097/PSY.0b013e31802e46eb
Flanagan, V. (2012). “Gender studies,” in The Routledge Companion to Children’s Literature, ed. D. Rudd (Abingdon: Routledge), 42–54. doi: 10.4324/9780203889855-10
Foa, E. B., Riggs, D. S., Massie, E. D., and Yarczower, M. (1995). The impact of fear activation and anger on the efficacy of exposure treatment for posttraumatic stress disorder. Behav. Ther. 26, 487–499. doi: 10.1016/S0005-7894(05)80096-6
Fondacaro, K. M., Holt, J. C., and Powell, T. A. (1999). Psychological impact of childhood sexual abuse on male inmates: the importance of perception. Child Abuse Neglect 23, 361–369. doi: 10.1016/S0145-2134(99)00004-6
Forum on Global Violence Prevention (2011). Direct and Indirect Costs of Violence. Social and Economic Costs of Violence: Workshop Summary. Washington, DC: National Academies Press (US).
Fraser, D. E. (2020). Impact of COVID-19 Pandemic on Violence against Women and Girls. 16. New York, NY: UN WOMEN.
Frederiksen, B., and Gomez, I. (2020). Coronavirus: A Look at Gender Differences in Awareness and Actions. San Francisco, CA: KFF.
Freund, C., and Hamel, I. (2020). COVID is Hurting Women Economically, but Governments Have the Tools to Offset the Pain. World Bank. Available online at: https://blogs.worldbank.org/psd/covid-hurting-women-economically-governments-have-tools-offset-pain
Garcia, N. M., Walker, R. S., and Zoellner, L. A. (2018). Estrogen, progesterone, and the menstrual cycle: A systematic review of fear learning, intrusive memories, and PTSD. Clin. Psychol. Rev. 66, 80–96. doi: 10.1016/j.cpr.2018.06.005
Garieballa, S. S., Schauer, M., Neuner, F., Saleptsi, E., Kluttig, T., Elbert, T., et al. (2006). Traumatic events, PTSD, and psychiatric comorbidity in forensic patients – assessed by questionnaires and diagnostic interview. Clin. Pract. Epidemiol. Ment. Health 2:7. doi: 10.1186/1745-0179-2-7
Gelles, R. (1993). Aggression: Its Causes, Consequences, and Control by Leonard Berkowitz. Available ONLINE AT: https://www.proquest.com/openview/19221df0825f9b8b416cf005e9bef465/1?pq-origsite=gscholar&cbl=47867 (accessed May 15. 2021).
Gierk, B., Kohlmann, S., Kroenke, K., Spangenberg, L., Zenger, M., Brähler, E., et al. (2014). The somatic symptom scale–8 (SSS-8): a brief measure of somatic symptom burden. JAMA Intern. Med. 174:399. doi: 10.1001/jamainternmed.2013.12179
Global Study on Homicide (2019). Available online at: https://www.unodc.org/unodc/en/data-and-analysis/global-study-on-homicide.html (accessed May 18, 2021).
Golden, S. A., Jin, M., and Shaham, Y. (2019). Animal models of (or for) aggression reward, addiction, and relapse: behavior and circuits. J. Neurosci. 39, 3996–4008. doi: 10.1523/JNEUROSCI.0151-19.2019
Golden, S. A., and Shaham, Y. (2018). Aggression addiction and relapse: a new frontier in psychiatry. Neuropsychopharmacology 43, 224–225. doi: 10.1038/npp.2017.173
Hale, T., Angrist, N., Goldszmidt, R., Kira, B., Petherick, A., Phillips, T., et al. (2021). A global panel database of pandemic policies (Oxford COVID-19 government response tracker). Nat. Hum. Behav. 5, 529–538. doi: 10.1038/s41562-021-01079-8
Halford, E., Dixon, A., Farrell, G., Malleson, N., and Tilley, N. (2020). Crime and coronavirus: social distancing, lockdown, and the mobility elasticity of crime. Crime Sci. 9:11. doi: 10.1186/s40163-020-00121-w
Hammarström, A., Lehti, A., Danielsson, U., Bengs, C., and Johansson, E. E. (2009). Gender-related explanatory models of depression: a critical evaluation of medical articles. Public Health 123, 689–693. doi: 10.1016/j.puhe.2009.09.010
Hank, K., and Steinbach, A. (2020). The virus changed everything, didn’t it? Couples’ division of housework and childcare before and during the Corona crisis. J. Fam. Res. 33, 99–114. doi: 10.20377/jfr-488
Hinz, A., Klein, A. M., Brähler, E., Glaesmer, H., Luck, T., Riedel-Heller, S. G., et al. (2017). Psychometric evaluation of the generalized anxiety disorder screener GAD-7, based on a large German general population sample. J. Affect. Disord. 210, 338–344. doi: 10.1016/j.jad.2016.12.012
Hodes, G. E., Walker, D. M., Labonté, B., Nestler, E. J., and Russo, S. J. (2017). Understanding the epigenetic basis of sex differences in depression. J. Neurosci. Res. 95, 692–702. doi: 10.1002/jnr.23876
Hodgkinson, T., and Andresen, M. A. (2020). Show me a man or a woman alone and I’ll show you a saint: Changes in the frequency of criminal incidents during the COVID-19 pandemic. J. Crim. Justice 69:101706. doi: 10.1016/j.jcrimjus.2020.101706
Jalnapurkar, I., Allen, M., and Pigott, T. (2018). Sex differences in anxiety disorders: a review. J. Psychiatry Depress Anxiety 4:12. doi: 10.24966/PDA-0150/100012
Jeong, H., Yim, H. W., Song, Y.-J., Ki, M., Min, J.-A., Cho, J., et al. (2016). Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol. Health 38:e2016048. doi: 10.4178/epih.e2016048
Jin, J.-M., Bai, P., He, W., Wu, F., Liu, X.-F., Han, D.-M., et al. (2020). Gender differences in patients with COVID-19: focus on Severity and mortality. Front. Public Health 8:152. doi: 10.3389/fpubh.2020.00152
Joyce, P. R., Oakley-Browne, M. A., Wells, J. E., Bushnell, J. A., and Hornblow, A. R. (1990). Birth cohort trends in major depression: increasing rates and earlier onset in New Zealand. J. Affect. Disord. 18, 83–89. doi: 10.1016/0165-0327(90)90063-e
Jurczyk, M., and Lalak, D. (2020). Aggressive and delinquent behavior among youth: an empirical study in poland. Violence Gender 7, 188–199. doi: 10.1089/vio.2019.0065
Kang, H.-J., Park, Y., Yoo, K.-H., Kim, K.-T., Kim, E.-S., Kim, J.-W., et al. (2020). Sex differences in the genetic architecture of depression. Sci. Rep. 10:9927. doi: 10.1038/s41598-020-66672-9
Kazmi, S. S. H. (2020). COVID-19 and lockdown: a study on the impact on mental health. Mukt. Shabd. J. 9, 1477–1489.
Kessler, R. C., McGonagle, K. A., Zhao, S., Nelson, C. B., Hughes, M., Eshleman, S., et al. (1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the national comorbidity survey. Arch. Gen. Psychiatry 51, 8–19. doi: 10.1001/archpsyc.1994.03950010008002
Klose, M., and Jacobi, F. (2004). Can gender differences in the prevalence of mental disorders be explained by sociodemographic factors? Arch. Womens Ment. Health 7, 133–148. doi: 10.1007/s00737-004-0047-7
Knight, G. P., Guthrie, I. K., Page, M. C., and Fabes, R. A. (2002). Emotional arousal and gender differences in aggression: a meta-analysis. Aggres. Behav. 28, 366–393. doi: 10.1002/ab.80011
Ko, N.-Y., Lu, W.-H., Chen, Y.-L., Li, D.-J., Wang, P.-W., Hsu, S.-T., et al. (2020). COVID-19-related information sources and psychological well-being: An online survey study in Taiwan. Brain Behav. Immunity 87, 153–154. doi: 10.1016/j.bbi.2020.05.019
Koebach, A., Carleial, S., Elbert, T., Schmitt, S., and Robjant, K. (2021). Treating trauma and aggression with narrative exposure therapy in former child and adult soldiers: a randomized controlled trial in Eastern DR Congo. J. Consult. Clin. Psychol. 89, 143–155. doi: 10.1037/ccp0000632
Koebach, A., and Elbert, T. (2015). Sensitive periods for developing a robust trait of appetitive aggression. Front. Psychiatry 6:144. doi: 10.3389/fpsyt.2015.00144
Kohlmann, S., Gierk, B., Hümmelgen, M., Blankenberg, S., and Löwe, B. (2013). Somatic symptoms in patients with coronary heart disease: Prevalence, risk factors, and quality of life. JAMA Internal Med. 173, 1469–1471. doi: 10.1001/jamainternmed.2013.6835
Kreyenfeld, M., Zinn, S., Entringer, T., Goebel, J., Grabka, M., Graeber, D., et al. (2020). DIW Berlin: Coronavirus & Care: How the Coronavirus Crisis Affected Fathers’ Involvement in Germany. Berlin: DIW, l.
Kröber, H.-L. (2012). Zusammen kämpfen, zusammen schlagen? (Conjoint fighting, conjoint bashing? The young prosocial violent perpetrator). Forensische Psychiatr. Psychol. Kriminol. 6, 166–176. doi: 10.1007/s11757-012-0168-1
Kroenke, K., Arrington, M. E., and Mangelsdorff, A. D. (1990). The prevalence of symptoms in medical outpatients and the adequacy of therapy. Arch. Internal Med. 150, 1685–1689. doi: 10.1001/archinte.150.8.1685
Kroenke, K., Jackson, J. L., and Chamberlin, J. (1997). Depressive and anxiety disorders in patients presenting with physical complaints: clinical predictors and outcome. Am. J. Med. 103, 339–347. doi: 10.1016/s0002-9343(97)00241-6
Kroenke, K., and Spitzer, R. L. (2002). The PHQ-9: a new depression diagnostic and severity measure. Psychiatr. Ann. 32, 509–515. doi: 10.3928/0048-5713-20020901-06
Kroenke, K., Zhong, X., Theobald, D., Wu, J., Tu, W., and Carpenter, J. S. (2010). Somatic symptoms in patients with cancer experiencing pain or depression: prevalence, disability, and health care use. Arch. Internal Med. 170, 1686–1694. doi: 10.1001/archinternmed.2010.337
Kuzminskaite, E., Penninx, B. W. J. H., van Harmelen, A.-L., Elzinga, B. M., Hovens, J. G. F. M., and Vinkers, C. H. (2021). Childhood trauma in adult depressive and anxiety disorders: an integrated review on psychological and biological mechanisms in the NESDA cohort. J. Affect. Disord. 283, 179–191. doi: 10.1016/j.jad.2021.01.054
Lagerspetz, K. M., Björkqvist, K., and Peltonen, T. (1988). Is indirect aggression typical of females? Gender differences in aggressiveness in 11- to 12-year-old children. Aggressive Behav. 14, 403–414.
Leslie, E., and Wilson, R. (2020). Sheltering in place and domestic violence: evidence from calls for service during COVID-19. J. Public Econ. 189:104241. doi: 10.1016/j.jpubeco.2020.104241
Li, S. H., and Graham, B. M. (2017). Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. Lancet Psychiatry 4, 73–82. doi: 10.1016/S2215-0366(16)30358-3
Ling, S., Umbach, R., and Raine, A. (2019). Biological explanations of criminal behavior. Psychol. Crime Law 25, 626–640. doi: 10.1080/1068316X.2019.1572753
Losada-Baltar, A., Jiménez-Gonzalo, L., Gallego-Alberto, L., Pedroso-Chaparro, M., del, S., Fernandes-Pires, J., et al. (2020). “We’re staying at home”. Association of self-perceptions of aging, personal and family resources and loneliness with psychological distress during the lock-down period of COVID-19. J. Gerontol. Ser. B 76, 10–16. doi: 10.1093/geronb/gbaa048
Löwe, B., Wahl, I., Rose, M., Spitzer, C., Glaesmer, H., Wingenfeld, K., et al. (2010). A 4-item measure of depression and anxiety: validation and standardization of the patient health questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 122, 86–95. doi: 10.1016/j.jad.2009.06.019
Manzo, L. K. C., and Minello, A. (2020). Mothers, childcare duties, and remote working under COVID-19 lockdown in Italy: cultivating communities of care. Dialogues Hum. Geogr. 10, 120–123. doi: 10.1177/2043820620934268
Matsudaira, K., Oka, H., Kawaguchi, M., Murakami, M., Fukudo, S., Hashizume, M., et al. (2017). Development of a japanese version of the somatic symptom scale-8: psychometric validity and internal consistency. Gen. Hosp. Psychiatry 45, 7–11. doi: 10.1016/j.genhosppsych.2016.12.002
Mazza, C., Ricci, E., Marchetti, D., Fontanesi, L., Di Giandomenico, S., Verrocchio, M. C., et al. (2020). How personality relates to distress in parents during the Covid-19 lockdown: the mediating role of child’s emotional and behavioral difficulties and the moderating effect of living with other people. Int. J. Environ. Res. Public Health 17:6236. doi: 10.3390/ijerph17176236
McCullough, J. P. (2003). Treatment for chronic depression using cognitive behavioral analysis system of psychotherapy (CBASP). J. Clin. Psychol. 59, 833–846. doi: 10.1002/jclp.10176
McHenry, J., Carrier, N., Hull, E., and Kabbaj, M. (2014). Sex differences in anxiety and depression: role of testosterone. Front. Neuroendocrinol. 35:42–57. doi: 10.1016/j.yfrne.2013.09.001
McLean, C. P., and Anderson, E. R. (2009). Brave men and timid women? A review of the gender differences in fear and anxiety. Clin. Psychol. Rev. 29, 496–505. doi: 10.1016/j.cpr.2009.05.003
McLean, C. P., Asnaani, A., Litz, B. T., and Hofmann, S. G. (2011). Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J. Psychiatr. Res. 45, 1027–1035. doi: 10.1016/j.jpsychires.2011.03.006
Meyer-Parlapanis, D., Weierstall, R., Nandi, C., Bambonyé, M., Elbert, T., and Crombach, A. (2016). Appetitive aggression in women: comparing male and female war combatants. Front. Psychol. 6:1972. doi: 10.3389/fpsyg.2015.01972
Moore, S. E., Wierenga, K. L., Prince, D. M., Gillani, B., and Mintz, L. J. (2021). Disproportionate impact of the COVID-19 pandemic on perceived social support, mental health and somatic symptoms in sexual and gender minority populations. J. Homosex. 68, 577–591. doi: 10.1080/00918369.2020.1868184
Moscovitch, D. A., Hofmann, S. G., and Litz, B. T. (2005). The impact of self-construals on social anxiety: a gender-specific interaction. Pers. Individ. Diff. 38, 659–672. doi: 10.1016/j.paid.2004.05.021
Msherghi, A., Alsuyihili, A., Alsoufi, A., Ashini, A., Alkshik, Z., Alshareea, E., et al. (2021). Mental health consequences of lockdown during the COVID-19 pandemic: a cross-sectional study. Front. Psychol. 12:605279. doi: 10.3389/fpsyg.2021.605279
Nell, V. (2006). Cruelty’s rewards: the gratifications of perpetrators and spectators. Behav. Brain Sci. 29, 211–224; discussion 224-257. doi: 10.1017/s0140525x06009058
Neria, Y., Nandi, A., and Galea, S. (2008). Post-traumatic stress disorder following disasters: a systematic review. Psychol. Med. 38, 467–480. doi: 10.1017/S0033291707001353
Norman, R. E., Byambaa, M., De, R., Butchart, A., Scott, J., and Vos, T. (2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 9:e1001349. doi: 10.1371/journal.pmed.1001349
Novaco, R. W., and Chemtob, C. M. (1998). “Anger and trauma: conceptualization, assessment, and treatment,” in Cognitive-Behavioral Therapies for Trauma, eds F. R. Abueg, J. I. Ruzek, and V. M. Follette (New York, NY: The Guilford Press), 162–190.
Oka, M., and Whiting, J. B. (2011). Contemporary MFT theories and intimate partner violence: a review of systemic treatments. J. Couple Relationsh. Ther. 10, 34–52. doi: 10.1080/15332691.2011.539173
Olaseni, A. O. (2020). Psychological distress experiences of Nigerians during Covid-19 pandemic; the gender difference. Soc. Sci. 2:100052. doi: 10.1016/j.ssaho.2020.100052
O’Leary, O. F., and Cryan, J. F. (2013). Towards translational rodent models of depression. Cell Tissue Res. 354, 141–153. doi: 10.1007/s00441-013-1587-9
Ollendick, T. H., King, N. J., and Muris, P. (2002). Fears and phobias in children: phenomenology, epidemiology, and aetiology. Child Adolesc. Ment. Health 7, 98–106. doi: 10.1111/1475-3588.00019
Orgilés, M., Morales, A., Delvecchio, E., Mazzeschi, C., and Espada, J. P. (2020). Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. PsyArXiv[Preprint] doi: 10.31234/osf.io/5bpfz
Orth, U., and Wieland, E. (2006). Anger, hostility, and posttraumatic stress disorder in trauma-exposed adults: a meta-analysis. J. Consult. Clin. Psychol. 74, 698–706. doi: 10.1037/0022-006X.74.4.698
Overmier, J. B., and Seligman, M. E. (1967). Effects of inescapable shock upon subsequent escape and avoidance responding. J. Comp. Physiol. Psychol. 63, 28–33. doi: 10.1037/h0024166
Ozamiz-Etxebarria, N. (2020). Psychological symptoms during the two stages of lockdown in response to the COVID-19 outbreak: an investigation in a sample of citizens in northern spain. Front. Psychol. 11:9.
Pennebaker, J. W., and Roberts, T.-A. (1992). Toward a his and hers theory of emotion: gender differences in visceral perception. J. Soc. Clin. Psychol. 11, 199–212. doi: 10.1521/jscp.1992.11.3.199
Perez-Vincent, S., Carreras, E., Gibbons, M. A., Murphy, T., and Rossi, M. (2020). COVID-19 Lockdowns and Domestic Violence: Evidence from Two Studies in Argentina | Publications. Inter-American Development Bank.
Peterman, A., Potts, A., O’Donnell, M., Shah, N., Oertelt-Prigione, S., Thompson, K., et al. (2020). Pandemics and Violence Against Women and Children. CGD Working Paper 528. Washington, DC: Center for Global Development.
Pieh, C., Budimir, S., and Probst, T. (2020). The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 136:110186. doi: 10.1016/j.jpsychores.2020.110186
Piquero, A. R., Jennings, W. G., Jemison, E., Kaukinen, C., and Knaul, F. M. (2021). Domestic Violence During COVID-19: Evidence from a Systematic Review and Meta-Analysis. 21. Washington, D.C: Council on Criminal Justice.
Powell, T. A., Holt, J. C., and Fondacaro, K. M. (1997). The prevalence of mental illness among inmates in a rural state. Law Hum. Behav. 21, 427–438. doi: 10.1023/a:1024811303834
Ran, L., Wang, W., Ai, M., Kong, Y., Chen, J., and Kuang, L. (2020). Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID-19: a study of the general population in china at the peak of its epidemic. Soc. Sci. Med. 262:113261. doi: 10.1016/j.socscimed.2020.113261
Raps, C. S., Peterson, C., Reinhard, K. E., Abramson, L. Y., and Seligman, M. E. P. (1982). Attributional style among depressed patients. J. Abnorm. Psychol. 91, 102–108. doi: 10.1037/0021-843X.91.2.102
Ravens-Sieberer, U., Kaman, A., Erhart, M., Devine, J., Schlack, R., and Otto, C. (2021). Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur. Child Adolesc. Psychiatry 1–11. doi: 10.1007/s00787-021-01726-5
Rief, W., Martin, A., Klaiberg, A., and Brähler, E. (2005). Specific effects of depression, panic, and somatic symptoms on illness behavior. Psychosom. Med. 67, 596–601. doi: 10.1097/01.psy.0000171158.59706.e7
Ritchie, H., and Roser, M. (2018). Mental Health. Our World in Data. Available online at: https://ourworldindata.org/mental-health (accessed March 20, 2021).
Robjant, K., Koebach, A., Schmitt, S., Chibashimba, A., Carleial, S., and Elbert, T. (2019). The treatment of posttraumatic stress symptoms and aggression in female former child soldiers using adapted Narrative Exposure therapy—A RCT in Eastern Democratic Republic of Congo. Behav. Res. Ther. 123:103482. doi: 10.1016/j.brat.2019.103482
Rosenfield, S., and Mouzon, D. (2013). “Gender and mental health,” in Handbook of the Sociology of Mental Health, eds C. S. Aneshensel, J. C. Phelan, and A. Bierman (Dordrecht: Springer), 277–296. doi: 10.1007/978-94-007-4276-5_14
Rossi, R., Socci, V., Talevi, D., Mensi, S., Niolu, C., Pacitti, F., et al. (2020). COVID-19 pandemic and lockdown measures impact on mental health among the general population in italy. Front. Psychiatry 11:790. doi: 10.3389/fpsyt.2020.00790
Rubenstein, L. M., Freed, R. D., Shapero, B. G., Fauber, R. L., and Alloy, L. B. (2016). Cognitive attributions in depression: bridging the gap between research and clinical practice. J. Psychother. Integr. 26, 103–115. doi: 10.1037/int0000030
Salari, N., Hosseinian-Far, A., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Mohammadi, M., et al. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health 16:57. doi: 10.1186/s12992-020-00589-w
Salk, R. H., Hyde, J. S., and Abramson, L. Y. (2017). Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol. Bull. 143, 783–822. doi: 10.1037/bul0000102
Sánchez-Teruel, D. (2021). Do psychological strengths protect college students confined by COVID-19 to emotional distress? The role of gender. Pers. Individ. Diff. 171:110507.
Scott, S. M., and Gross, L. J. (2021). COVID-19 and crime: analysis of crime dynamics amidst social distancing protocols. PLoS One 16:e0249414. doi: 10.1371/journal.pone.0249414
Seedat, S., Scott, K. M., Angermeyer, M. C., Berglund, P., Bromet, E. J., Brugha, T. S., et al. (2009). Cross-national associations between gender and mental disorders in the WHO World Mental Health Surveys. Arch. Gen. Psychiatry 66, 785–795. doi: 10.1001/archgenpsychiatry.2009.36
Seligman, M. E. P. (1972). Learned helplessness. Annu. Rev. Med. 23, 407–412. doi: 10.1146/annurev.me.23.020172.002203
Shelef, L., and Zalsman, G. (2020). The psychological impact of COVID-19 on mental health – literature review. Harefuah 159, 320–325.
Simon, G. E., VonKorff, M., Piccinelli, M., Fullerton, C., and Ormel, J. (1999). An international study of the relation between somatic symptoms and depression. N. Engl. J. Med. 341, 1329–1335. doi: 10.1056/NEJM199910283411801
Simon, R. W. (1995). Gender, multiple roles, role meaning, and mental health. J. Health Soc. Behav. 36, 182–194. doi: 10.2307/2137224
Spielberger, C. D., Jacobs, G., Russel, S., and Crane, R. S. (1983). “Assessment of anger: the state-trait anger scale,” in Advances in Personality Assessment, Vol. 2, eds C. D. Spielberger and J. N. Butcher (Abingdon: Routledge).
Spielberger, C. D., Reheiser, E. C., and Sydeman, S. J. (1995). Measuring the experience, expression, and control of anger. Issues Compr. Pediatr. Nurs. 18, 207–232. doi: 10.3109/01460869509087271
Spitzer, R. L., Kroenke, K., Williams, J. B. W., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 166:1092. doi: 10.1001/archinte.166.10.1092
Stewart, J. L., Bismark, A. W., Towers, D. N., Coan, J. A., and Allen, J. J. B. (2010). Resting frontal EEG asymmetry as an endophenotype for depression risk: sex-specific patterns of frontal brain asymmetry. J. Abnorm. Psychol. 119, 502–512. doi: 10.1037/a0019196
Sutherland, M., McKenney, M., and Elkbuli, A. (2021). Gun violence during COVID-19 pandemic: paradoxical trends in New York city, chicago, los angeles and baltimore. Am. J. Emergency Med. 39, 225–226. doi: 10.1016/j.ajem.2020.05.006
Szabo, A., Ábel, K., and Boros, S. (2020). Attitudes toward COVID-19 and stress levels in hungary: effects of age, perceived health status, and gender. Psychol. Trauma 12, 572–575.
Telles, L. E., de, B., Valença, A. M., Barros, A. J. S., da Silva, A. G., Telles, L. E., et al. (2020). Domestic violence in the COVID-19 pandemic: a forensic psychiatric perspective. Braz. J. Psychiatry Ahead 43, 233–234. doi: 10.1590/1516-4446-2020-1060
Turanovic, J. J., Pratt, T. C., and Piquero, A. R. (2017). Exposure to fetal testosterone, aggression, and violent behavior: a meta-analysis of the 2D:4D digit ratio. Aggression Violent Behav. 33, 51–61. doi: 10.1016/j.avb.2017.01.008
Usher, K., Bhullar, N., Durkin, J., Gyamfi, N., and Jackson, D. (2020). Family violence and COVID-19: increased vulnerability and reduced options for support. Int. J. Ment. Health Nurs. 29, 549–552. doi: 10.1111/inm.12735
Vitoratou, S., Ntzoufras, I., Smyrnis, N., and Stefanis, N. C. (2009). Factorial composition of the aggression questionnaire: a multi-sample study in greek adults. Psychiatry Res. 168, 32–39. doi: 10.1016/j.psychres.2008.01.016
von Collani, G., and Werner, R. (2005). Self-related and motivational constructs as determinants of aggression. An analysis and validation of a German version of the Buss-Perry Aggression Questionnaire. Pers. Individ. Diff. 38, 1631–1643. doi: 10.1016/j.paid.2004.09.027
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., et al. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 17:1729. doi: 10.3390/ijerph17051729
Wang, G., Zhang, Y., Zhao, J., Zhang, J., and Jiang, F. (2020). Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet (London, England) 395, 945–947. doi: 10.1016/S0140-6736(20)30547-X
Watt, M. C., Stewart, S. H., and Cox, B. J. (1998). A retrospective study of the learning history origins of anxiety sensitivity. Behav. Res. Ther. 36, 505–525. doi: 10.1016/S0005-7967(97)10029-8
Webster, G. D., DeWall, C. N., Pond, R. S. Jr., Deckman, T., Jonason, P. K., Le, B. M., et al. (2014). The brief aggression questionnaire: psychometric and behavioral evidence for an efficient measure of trait aggression. Aggressive Behav. 40, 120–139. doi: 10.1002/ab.21507
Webster, G. D., DeWall, C. N., Pond, R. S. Jr., Deckman, T., Jonason, P. K., Le, B. M., et al. (2015). The brief aggression questionnaire: structure, validity, reliability, and generalizability. J. Pers. Assessment 97, 638–649. doi: 10.1080/00223891.2015.1044093
Weissman, M. M., and Klerman, G. L. (1977). Sex differences and the epidemiology of depression. Arch. Gen. Psychiatry 34, 98–111. doi: 10.1001/archpsyc.1977.01770130100011
Wenham, C. (2020). The Gendered Impact of the COVID-19 Crisis and Post-crisis Period. 68. London: LSE.
WHO (2020). The impact of COVID-19 on Mental, Neurological and Substance use Services. Available online at: https://www.who.int/publications-detail-redirect/978924012455 (accessed March 19, 2021).
Wiborg, O. (2013). Chronic mild stress for modeling anhedonia. Cell Tissue Res. 354, 155–169. doi: 10.1007/s00441-013-1664-0
Wickramaratne, P. J., Weissman, M. M., Leaf, P. J., and Holford, T. R. (1989). Age, period and cohort effects on the risk of major depression: results from five united states communities. J. Clin. Epidemiol. 42, 333–343. doi: 10.1016/0895-4356(89)90038-3
Williams, S. N., Armitage, C. J., Tampe, T., and Dienes, K. (2020). Public perceptions and experiences of social distancing and social isolation during the COVID-19 pandemic: A UK-based focus group study. MedRxiv [Preprint] doi: 10.1101/2020.04.10.20061267 MedRxiv: 2020.04.10.20061267
Wu, T., Jia, X., Shi, H., Niu, J., Yin, X., Xie, J., et al. (2021). Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 281, 91–98. doi: 10.1016/j.jad.2020.11.117
Xiang, Y.-T., Yang, Y., Li, W., Zhang, L., Zhang, Q., Cheung, T., et al. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7, 228–229. doi: 10.1016/S2215-0366(20)30046-8
Xie, X., Xue, Q., Zhou, Y., Zhu, K., Liu, Q., Zhang, J., et al. (2020). Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in hubei province, China. JAMA Pediatr. 174:898. doi: 10.1001/jamapediatrics.2020.1619
Yan, S., Xu, R., Stratton, T. D., Kavcic, V., Luo, D., Hou, F., et al. (2021). Sex differences and psychological stress: responses to the COVID-19 pandemic in China. BMC Public Health 21:79. doi: 10.1186/s12889-020-10085-w
Ye, B., Zeng, Y., Im, H., Liu, M., Wang, X., and Yang, Q. (2021). The relationship between fear of COVID-19 and online aggressive behavior: a moderated mediation model. Front. Psychol. 12:589615. doi: 10.3389/fpsyg.2021.589615
Zamarro, G., and Prados, M. J. (2021). Gender differences in couples’ division of childcare, work and mental health during COVID-19. Rev. Econ. Household 19, 11–40. doi: 10.1007/s11150-020-09534-7
Zhang, Y., and Ma, Z. F. (2020). Impact of the COVID-19 pandemic on mental health and quality of life among local residents in liaoning province, china: a cross-sectional study. Int. J. Environ. Res. Public Health 17:2381. doi: 10.3390/ijerph17072381
Zimmert, F. (2019). Early Child Care and Maternal Employment: Empirical Evidence from Germany. IAB-Discussion Paper, No.2. Nürnberg: Institut für Arbeitsmarkt-und Berufsforschung (IAB), 32.
Keywords: aggression, anxiety, depression, somatization, mental health, COVID-19 pandemic, gender differences
Citation: Abreu L, Koebach A, Díaz O, Carleial S, Hoeffler A, Stojetz W, Freudenreich H, Justino P and Brück T (2021) Life With Corona: Increased Gender Differences in Aggression and Depression Symptoms Due to the COVID-19 Pandemic Burden in Germany. Front. Psychol. 12:689396. doi: 10.3389/fpsyg.2021.689396
Received: 31 March 2021; Accepted: 11 June 2021;
Published: 27 July 2021.
Edited by:
Christiane Schwieren, Heidelberg University, GermanyReviewed by:
Cláudia Andrade, Instituto Politécnico de Coimbra, PortugalCopyright © 2021 Abreu, Koebach, Díaz, Carleial, Hoeffler, Stojetz, Freudenreich, Justino and Brück. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liliana Abreu, bGlsaWFuYS5hYnJldUB1bmkta29uc3RhbnouZGU=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.